User login
2021 Rare Diseases Report: Cancers
INTRODUCTIONS
Editor's Note: Looking forward
By Mark S. Lesney, PhD
The Rare Diseases Report: Cancers looks to the future from trial design to treatment for some of the most underserved diseases and patient populations.
NORD: Approaching rare cancers through a diversity lens
By Rebecca Aune and Debbie Drell
NORD advocates for all rare disease patients, no matter their race, ethnicity, religion, color, national origin, age, disability, sexual orientation, gender identity, etc.
CLINICAL REVIEWS
Precision medicine: A new approach to AML, other blood cancers
By Caleb Rans, PHARMD
Precision medicine makes groundbreaking strides in treating myeloid malignancies by integrating individual molecular data into patient care.
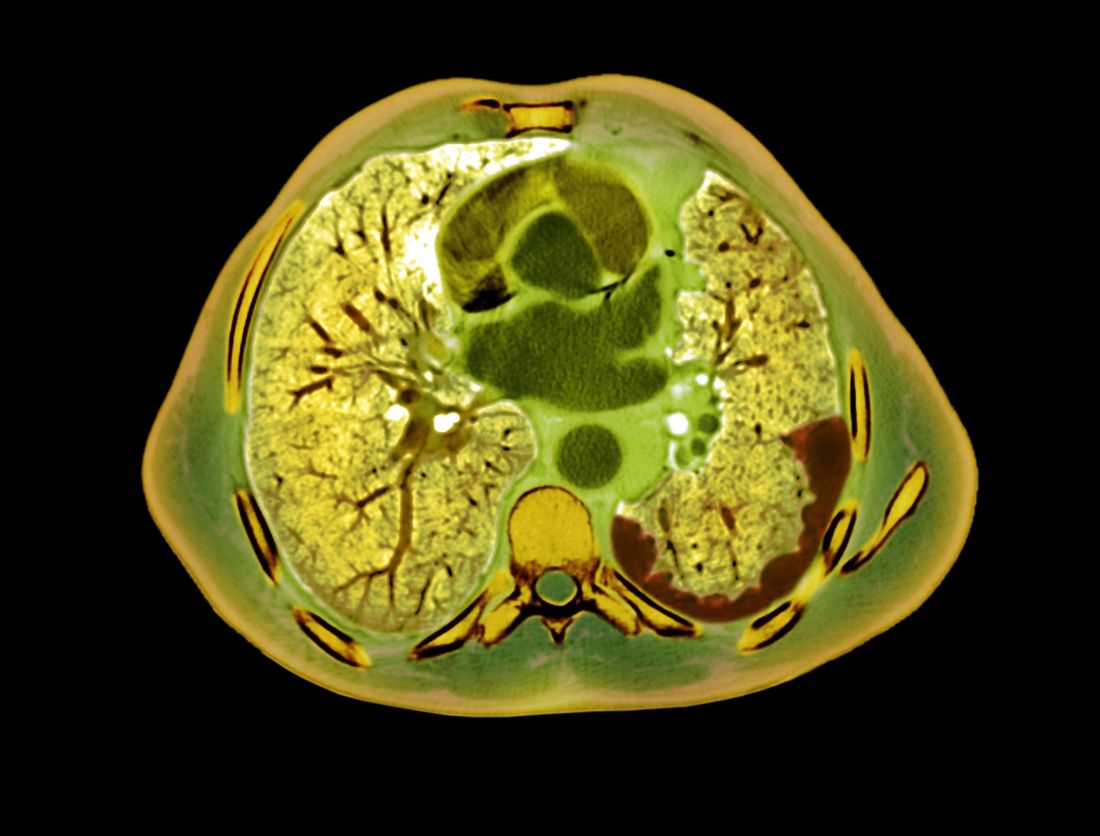
Coping with a shattered immune system: COVID and beyond
By Christine Kilgore
Questions abound about vaccine timing and the immune response in hematologic malignancies.
Racial disparities in blood cancer treatment
By Roxanne Nelson
An increasing number of studies have documented racial disparities among the study, treatment, and management of hematologic malignancies.
Overcoming obstacles in rare GU cancers
By Will Pass
Investigators are meeting the challenge of dealing with rare genitourinary cancers through collaboration, novel treatment efforts, and clinical trial design.
Mesothelioma trials: Moving toward improved survival
By Andrew D. Bowser
New and emerging therapy developments show promise of extended survival for select patients.
Metastatic uveal melanoma -- new drugs in pipeline, but prognoses still grim
By Randy Dotinga
As many as 50% of patients with this rare form of eye cancer develop tumors elsewhere.
Meeting the unmet need in multiple myeloma
By Walter Alexander
Multiple myeloma remains an incurable plasma cell disorder with near-certain relapse after successful treatment.
Rhabdomyosarcoma: Adaptive therapy borrows from nature
By Neil Osterweil
Researchers are applying evolutionary principles to the treatment of childhood, fusion-positive rhabdomyosarcoma.
INTRODUCTIONS
Editor's Note: Looking forward
By Mark S. Lesney, PhD
The Rare Diseases Report: Cancers looks to the future from trial design to treatment for some of the most underserved diseases and patient populations.
NORD: Approaching rare cancers through a diversity lens
By Rebecca Aune and Debbie Drell
NORD advocates for all rare disease patients, no matter their race, ethnicity, religion, color, national origin, age, disability, sexual orientation, gender identity, etc.
CLINICAL REVIEWS
Precision medicine: A new approach to AML, other blood cancers
By Caleb Rans, PHARMD
Precision medicine makes groundbreaking strides in treating myeloid malignancies by integrating individual molecular data into patient care.
Coping with a shattered immune system: COVID and beyond
By Christine Kilgore
Questions abound about vaccine timing and the immune response in hematologic malignancies.
Racial disparities in blood cancer treatment
By Roxanne Nelson
An increasing number of studies have documented racial disparities among the study, treatment, and management of hematologic malignancies.
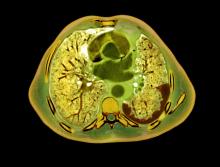
Overcoming obstacles in rare GU cancers
By Will Pass
Investigators are meeting the challenge of dealing with rare genitourinary cancers through collaboration, novel treatment efforts, and clinical trial design.
Mesothelioma trials: Moving toward improved survival
By Andrew D. Bowser
New and emerging therapy developments show promise of extended survival for select patients.
Metastatic uveal melanoma -- new drugs in pipeline, but prognoses still grim
By Randy Dotinga
As many as 50% of patients with this rare form of eye cancer develop tumors elsewhere.
Meeting the unmet need in multiple myeloma
By Walter Alexander
Multiple myeloma remains an incurable plasma cell disorder with near-certain relapse after successful treatment.
Rhabdomyosarcoma: Adaptive therapy borrows from nature
By Neil Osterweil
Researchers are applying evolutionary principles to the treatment of childhood, fusion-positive rhabdomyosarcoma.
INTRODUCTIONS
Editor's Note: Looking forward
By Mark S. Lesney, PhD
The Rare Diseases Report: Cancers looks to the future from trial design to treatment for some of the most underserved diseases and patient populations.
NORD: Approaching rare cancers through a diversity lens
By Rebecca Aune and Debbie Drell
NORD advocates for all rare disease patients, no matter their race, ethnicity, religion, color, national origin, age, disability, sexual orientation, gender identity, etc.
CLINICAL REVIEWS
Precision medicine: A new approach to AML, other blood cancers
By Caleb Rans, PHARMD
Precision medicine makes groundbreaking strides in treating myeloid malignancies by integrating individual molecular data into patient care.
Coping with a shattered immune system: COVID and beyond
By Christine Kilgore
Questions abound about vaccine timing and the immune response in hematologic malignancies.
Racial disparities in blood cancer treatment
By Roxanne Nelson
An increasing number of studies have documented racial disparities among the study, treatment, and management of hematologic malignancies.
Overcoming obstacles in rare GU cancers
By Will Pass
Investigators are meeting the challenge of dealing with rare genitourinary cancers through collaboration, novel treatment efforts, and clinical trial design.
Mesothelioma trials: Moving toward improved survival
By Andrew D. Bowser
New and emerging therapy developments show promise of extended survival for select patients.
Metastatic uveal melanoma -- new drugs in pipeline, but prognoses still grim
By Randy Dotinga
As many as 50% of patients with this rare form of eye cancer develop tumors elsewhere.
Meeting the unmet need in multiple myeloma
By Walter Alexander
Multiple myeloma remains an incurable plasma cell disorder with near-certain relapse after successful treatment.
Rhabdomyosarcoma: Adaptive therapy borrows from nature
By Neil Osterweil
Researchers are applying evolutionary principles to the treatment of childhood, fusion-positive rhabdomyosarcoma.
Adaptive therapy borrows from nature to keep rhabdomyosarcoma in check
In 1859, Charles Darwin published “On the Origin of Species,” which outlined his world-shaking theory of evolution and its core principle of natural selection caused by environmental pressures that may determine whether an organism adapts and survives, or remains static, languishes, and eventually dies out.
The same forces that have influenced the size and shape of the beaks of finches in the Galapagos Islands, the length of giraffe necks in Africa, and the intestinal microbiomes of the nearly 8 billion human inhabitants of this planet also control whether malignant cells thrive and multiply, wither and die when assaulted by chemotherapy, or go into hiding, mutating and waiting for their next opportunity to erupt again and metastasize.
The ability of malignant cells to adapt to environmental pressures is “cancer’s most lethal and sophisticated property,” said Damon R. Reed, MD, program leader of the adolescent/young adult program at Moffitt Cancer Center in Tampa, Fla.
Dr. Reed and colleagues are developing methods to meet cancer on its own terms, applying evolutionary principles to the treatment of childhood fusion-positive rhabdomyosarcoma in an innovative, and some would say audacious, clinical trial.
Adaptive versus conventional therapy
The trial, now recruiting, is designed to evaluate each of four different strategies for chemotherapy schedules in patients with newly diagnosed metastatic fusion-positive rhabdomyosarcoma.
The trial contains four arms, three of which consist of either conventional chemotherapy based on published clinical trials, moving a second-line therapy to the first line, or adding maintenance therapy, all of which have the goal of inducing as many complete remissions as possible.
The remaining adaptive therapy arm, however, is entirely novel in approach, with therapy using a combination of chemotherapy drugs that will be started and interrupted based on tumor responses, with resumption of therapy on an adaptive schedule unique to each patient. The goal of treatment for patients enrolled in this arm will be prolongation of the time to disease progression, rather than complete remission.
Although some people might consider the adaptive therapy approach to be sacrificing the hope for a cure in exchange for palliation, the hard truth is that patients with fusion-positive rhabdomyosarcoma (in contrast to those with fusion-negative disease) have a dismal prognosis following relapse after up-front intensified therapy.
Instead, because a cure is exceedingly unlikely in patients with metastatic disease, the conventional idea of delivering the maximum tolerated dose of chemotherapy until disease progression could be replaced by an approach based on understanding of the evolution of cancer cells under selective pressures, Dr. Reed and colleagues contend.
“Although adaptive therapy would represent a major paradigm shift in pediatric oncology, this approach would exploit the chemotherapy-sensitive population to prevent the emergence of resistant populations, optimizing tumor control with less toxicity,” they wrote in a commentary published online in the journal Cancer.1
Poor survival with advanced disease
Childhood rhabdomyosarcoma (RMS) is a form of soft tissue sarcoma of mesenchymal origin. Approximately 25% of cases are parameningeal, arising from sites adjacent to the meninges of the nasopharynx, middle ear, paranasal sinuses, orbit, and other regions of the head and neck. Approximately 31% of cases arise in the genitourinary tract and 13% in the extremities, and other tumors occur less commonly in the trunk, chest wall, perineal/anal region, and abdomen.
The overall 5-year survival rate is approximately 71%.1
However, for patients with high-risk disease, a group that includes children 10 years of age or older with widespread disease with or without an activating PAX/FOX01 gene fusion, 5-year survival ranges from just 20% to 30% (Cancer Facts & Figures 2020).
“Among patients with metastatic disease, there is a clear difference in overall survival between those who have fusion-positive disease, where the 5-year overall survival is about 19%, and patients with fusion-negative disease,” said Douglas S. Hawkins, MD, chair of the children’s oncology group and professor of pediatrics at the University of Washington, Seattle, and associate chief in the division of hematology/oncology at Seattle Children’s Hospital.
Patients with fusion-negative disease can be further classified into those with multiple metastatic sites, with a 5-year overall survival rate of approximately 45%, and those with a single metastatic site, with a 5-year overall survival rate of 70%, he said in an interview.
“So when we talk about metastatic rhabdomyosarcoma, there actually is a diversity of outcomes, between really bad – those with fusion-positive disease – and not terrible – not great, but not terrible – for a selected group of patients with fusion-negative disease,” Dr. Hawkins said.
The poor prognosis for patients with metastatic fusion-positive disease prompted Dr. Reed and colleagues to rethink the entire approach to advanced cancers.
“If someone has a sarcoma, we know that we need to do surgery and radiation to the area, we know that localized disease does better than metastatic disease, and we generally hit it with some kind of chemotherapy that we call ‘standard of care,’ ” he said in an interview.
This approach is largely effective in some forms of cancer of bone and soft tissues, such as Ewing sarcoma, he notes, which has 5-year survival rates below 20% when treated with surgery and radiation only, but with the addition of chemotherapy has 5-year overall survival rates as high as 80%.
“At other times, with other sarcomas, the cure rate is abysmal, but we still call it standard of care,” Dr. Reed said.
For example, patients with metastatic fusion-positive RMS may have an initial response to chemotherapy, but most will eventually experience relapse and die of the disease.
“With some of the most common treatments, 70% of patients will have their cancers shrink by more than 50%, which is a major response, but the vast majority of them will have a recurrence later on,” Dr. Hawkins said.
He noted that the standard of care for patients with metastatic rhabdomyosarcoma, both with and without the PAX/FOX01 fusion, is chemotherapy, generally with the VAC regimen (vincristine, actinomycin D, and cyclophosphamide), although other agents such as doxorubicin, ifosfamide, etoposide, or irinotecan have also been tried, with little effect on event-free survival or overall survival rates.
A life too brief
Ricky Huff and his family know the course that the disease can take only too well. In 2015, his 5-month-old son, Theo, was diagnosed with metastatic rhabdomyosarcoma and put under the care of Damon Reed at Moffitt.
“During the whole course of treatment – I’m sure like many other parents – apart from relying on Damon and his treatment expertise to try to determine the best treatment options, I was reading everything under the sun to try to get a working knowledge of what Theo was up against, what his treatment and clinical trial options were, and what was the state of the science,” Mr. Huff says.
Unfortunately, the characteristics of Theo’s disease, including his very young age at onset and diagnosis of stage 4 metastatic disease, conspired against him, and despite undergoing 14 months of chemotherapy, Theo died of the disease in October 2016, 5 months shy of what would have been his second birthday.
In their grief, Mr. Huff, a real estate lawyer with a practice in Clearwater, Fla., and his wife, Leah, were determined to help other families of children with cancer and settled on the National Pediatric Cancer Foundation. Mr. Huff joined the board of directors of the foundation, which is collaborating with Moffitt Cancer Center on the adaptive therapy trial.
An evolutionary primer (cancer edition)
To get a better idea of just how adaptive therapy works, it is helpful to view cancer cells through the lens of species development, adaptation, extinction, and evolution.
“Cancer cells compete against each other in a dynamic environment. Their tumor ecosystems exhibit spatial and temporal fluctuations in blood-borne nutrients, oxygen, growth factors, immune cells, and hormones,” Dr. Reed and colleagues wrote.
These influences can affect genetically identical cancer cells, which may begin to diverge from one another depending on their location in a tumor and the availability of nutrients, which in turn can result in two once-identical cells exhibiting different transcription rates for growth factors.
“Ultimately, this may affect the rate of progression through the cell cycle, leading to distinct rates of proliferation and mutational acquisition,” they wrote.
The diverging subpopulations will begin to develop different methods for adapting to the tumor microenvironment, with unique strategies for both accelerating growth and avoiding hazards such as chemotherapy drugs or radiation, the investigators explained.
“By the time a cancer becomes clinically apparent, cancer cells have transformed from a single clone into a diverse community of cell types evolving in response to a spatially and temporally heterogeneous tumor environment. Theoretically, a 10-gram cancer may contain the same order of magnitude of cancer cells as there are humans on earth, with tremendous diversity of phenotypes and environments,” they wrote.
Survival of the fittest
The competition of individuals within and between species described by Darwin also applies to cancer cells, in their interactions both with each other and with stromal cells and immune cells resulting in “the progressive replacement of less fit phenotypes by those that are more fit,” Dr. Reed and colleagues explained.
And just like the old joke about two hikers trying to escape from a charging grizzly bear (one says, “This is futile – we can’t outrun a grizzly,” and the other says, “I only have to outrun you!”), cancer cells only need to be more resistant to therapeutic attack than normal cells that are critical to function.
“This may explain why initial responses in certain solid tumors (notably rhabdomyosarcoma) do not predict eventual survival. The sensitivities of the dominant cancer cell populations dictate the initial response, but it is the ecology and evolution of the rare and more resistant populations that determine cure or relapse,” they wrote.
The endangered species list
As with many types of cancer, the current approach to treating pediatric sarcomas with curative intent is with a “first strike” approach, treating patients with surgery, radiation, and cytotoxic chemotherapy at the maximum tolerated dose for as long as needed or until unacceptable toxicities occur, with the intention of wiping out all cancer cells without permanently injuring normal cells.
The evolutionary analogy to this approach is a mass extinction event such as the meteor strike that is believed to have wiped out the dinosaurs roughly 66 million years ago. Fossil evidence suggests that the cataclysmic event resulted in the atmosphere being blanketed with dust particles that blocked sunlight and caused massive die-off of plants that dinosaurs needed to survive and were ill-adapted to do without.
In contrast, populations of smaller, more adaptable species of microbes, insects, and animals, including our mammalian ancestors, were able to survive and eventually flourish.
Many patients with localized cancers may be cured with up-front therapy, but others will have residual disease from populations of cells that are intrinsically resistant to therapy or have developed new evasion strategies.
Strike two and the MVP
Dr. Reed and colleagues liken the approach of second-line therapy for treatment of relapsed or refractory disease to the concept of “background extinctions,” using the fate of the passenger pigeon as an example of how a second-strike therapeutic strategy works.
Although the popular conception is that the passenger pigeon was hunted to extinction by humans, the species in fact died out because of many different factors, including loss of habitat, isolation of populations leading to a loss of genetic diversity, and disruption of breeding habits.
“Once first strikes of deforestation and hunting reduced the birds to small, fragmented populations, a series of what would otherwise have been minor second strikes pushed the passenger pigeon below its extinction threshold, or minimum viable population,” they said.
The analogy, as it applies to cancer therapy, is the use of second-line or follow-on therapy with one or more agents that the residual cells are at least in theory not resistant to. In the case of fusion-positive rhabdomyosarcoma, the drug most commonly added in the second-strike approach is vinorelbine.2
“Second strikes should be timed to occur around the time when the first strike has achieved its greatest effect, presumably at the point when the disease becomes clinically undetectable or at a measurable nadir,” Dr. Reed and colleagues wrote. “Ideally, second-strike therapies should have modes of action that require different resistance strategies by the cancer cells than those needed for resistance to the first strike.”
Adaptive therapy
As Dr. Reed and colleagues note, despite optimal therapy, 94% of patients with metastatic fusion-positive rhabdomyosarcoma will experience a relapse within 3 years of diagnosis.1 Clearly the scorched earth or “throw everything you have it” approach no longer works, and that’s where adaptive therapy comes in.
Here again, the authors rely on nature, or rather human interaction with nature, to devise a strategy for keeping the disease at bay when extinction of all cancerous cells cannot be achieved.
They cite the example of agricultural integrated pest management, which seeks to keep harmful insects in check by treating them to suppress but not completely destroy a population, then stopping the use of pesticides, and resuming only when the insect population spikes and again becomes a threat to crops.
“The goal is to limit crop damage while retaining the sensitivity of the insects to the pesticides. Resistance most often comes at a cost. In the absence of the pesticide, sensitive individuals will outcompete resistant individuals,” they wrote.
Adaptive therapy uses the same approach to reduce selection pressures that foster resistance, with patients treated only until a specific, predetermined response is achieved in the dominant population of chemosensitive cells. The treatment is then interrupted and reintroduced only when the tumor rebounds to a certain predetermined size.
In this scenario, cells that retain sensitivity to chemotherapy will be able to reproduce and proliferate more rapidly than drug-resistant cells, and the therapy can then be reintroduced. This strategy is less likely to cause the development and proliferation of resistant cells than conventional intensified chemotherapy, Dr. Reed and colleagues contend.
Putting it to the test
The clinical trial that Dr. Reed and colleagues have initiated, officially titled “Evolutionary Inspired Therapy for Newly Diagnosed, Metastatic, Fusion Positive Rhabdomyosarcoma,” (NCT04388839) contains four arms: three experimental and one active comparator arm.
“We won’t randomize; we don’t feel that it would be fair to randomize patients, because these arms are so different from each other,” Dr. Reed said.
Arm A is the experimental first-strike arm, a 42-week course containing cyclophosphamide delivered intravenously over 60 minutes at a dose ranging from 220 mg to 1200 mg, vinorelbine delivered in an IV push over 6-10 minutes with a dose ranging from 4 mg to 25 mg, and actinomycin D administered via IV over 3-5 minutes at a dose ranging from 0.025 mg to 0.04 mg.
“The idea is that we take the standard of care, and we add a drug – vinorelbine – to make it stronger,” Dr. Reed said. “The idea is that the resistant cell, the cell that escapes, if we start hitting it on day 1 with vinorelbine, we might be able to drive it to extinction.”
Arm B, the second experimental arm, is the second-strike and maintenance arm, in which patients will receive conventional doses of vincristine, actinomycin D, and cyclophosphamide (VAC) until complete response (CR) for 12-42 weeks, and will then be switched to up to 2 years of maintenance with vinorelbine and oral cyclophosphamide.
“Vinorelbine will be added when the cancer is declining or first goes into remission. We try not to wait 42 weeks, which is too long we think, by which time the cancer may be fully adapted and resistant,” he explained.
Arm C is the adaptive therapy arm, in which patients will receive VAC that starts and stops based on response, with the goal of prolonging time to disease progression rather than achieving CR.
Arm D is the active comparator arm, consisting of conventional chemotherapy based on published clinical trials, such as VAC for 42 weeks, or other standard-of-care regimens that may include irinotecan, doxorubicin, ifosfamide, and/or etoposide.
A change in thinking
Dr. Reed acknowledges that Arm C, the adaptive therapy arm, “definitely represents a change in thinking for pediatric oncology.”
“The idea is that if you could do this perfectly well, you would be able to take a patient who is diagnosed today and essentially ‘pause’ their disease for a while. Then 5 years from now, if there is a better medicine, you would have gotten that patient to that medicine.”
The optimal approach to treating metastatic fusion-positive rhabdomyosarcoma may be similar to that used for treatment of acute lymphoblastic leukemia, with induction, consolidation, and maintenance and the option of delayed intensification, he said.
“But we’re so far away from knowing which series to do that we just need to show that any series – any changing it up – is helpful.”
Dr. Reed said that when he started presenting the concept of adaptive therapy in clinical meetings in 2017, “I was told to come up with a better idea. There were several people who instantly got it, but most people would instantly get angry.”
The common refrain was that adaptive therapy was “giving up.”
But minds began to change in 2018, following presentation at the annual meeting of the American Society of Clinical Oncology of a European study showing that adding 6 months of low-dose chemotherapy maintenance to standard therapy improved the 5-year overall survival rate of pediatric rhabdomyosarcoma from 73.7% to 86.6%.2
Before presenting the idea of adaptive therapy to his colleagues, he ran it by the parents of children with advanced sarcomas, and many were on board with it, he said.
Ricky Huff said that had the option of adaptive therapy been available for Theo, he and his wife would have been willing to try it.
“Of course, everyone has the ability in hindsight to apply critical thinking to decisions that you made or could have made,” he said. “I think is true for many parents, who if they’re presented with information about options will say ‘well if there’s a 1 percent chance, I want that chance for my child, especially for a 5-month-old.”
The decision to choose adaptive therapy is a difficult decision to make, whether for oneself or for one’s son, because it isn’t curative.
“My wife and I have since had a conversation about this, and I do think we would have considered it, although through a lot of difficult conversations,” he said.
“After we got the pathology, knowing that it was metastatic, fusion-positive, and given his age, just doing a brief literature review on my own, I knew what we were up against using 20-year-old treatments, and that the chance of a cure was very, very small.”
If parents of children with metastatic, poor-prognosis rhabdomyosarcoma could be made to understand that adaptive therapy would entail shorter and fewer hospital stays, and cumulatively less toxic chemotherapy, and could prolong the lives of their children, the option might be more acceptable, he said.
And as Dr. Reed mentioned, prolonging time to progression offers hope of additional therapies to come.
“The whole time that my son was being treated, I hoped that there was going to be something else that came out, that a new trial would be launched because they found a way to drug a mutation, or treat it with immunotherapy – something that was going to give us a better option.”
Asked whether he would be willing to share his experiences in this article, Mr. Huff said that “I am willing to, in whatever small way I can, make an impact, and hopefully save another family from what we experienced.”
References
1. Reed DR et al. Cancer. 2020 Jun 1;126(11):2577-87 2. Bisogno G et al. J Clin Oncol. 2018;36:18_suppl,LBA-2
In 1859, Charles Darwin published “On the Origin of Species,” which outlined his world-shaking theory of evolution and its core principle of natural selection caused by environmental pressures that may determine whether an organism adapts and survives, or remains static, languishes, and eventually dies out.
The same forces that have influenced the size and shape of the beaks of finches in the Galapagos Islands, the length of giraffe necks in Africa, and the intestinal microbiomes of the nearly 8 billion human inhabitants of this planet also control whether malignant cells thrive and multiply, wither and die when assaulted by chemotherapy, or go into hiding, mutating and waiting for their next opportunity to erupt again and metastasize.
The ability of malignant cells to adapt to environmental pressures is “cancer’s most lethal and sophisticated property,” said Damon R. Reed, MD, program leader of the adolescent/young adult program at Moffitt Cancer Center in Tampa, Fla.
Dr. Reed and colleagues are developing methods to meet cancer on its own terms, applying evolutionary principles to the treatment of childhood fusion-positive rhabdomyosarcoma in an innovative, and some would say audacious, clinical trial.
Adaptive versus conventional therapy
The trial, now recruiting, is designed to evaluate each of four different strategies for chemotherapy schedules in patients with newly diagnosed metastatic fusion-positive rhabdomyosarcoma.
The trial contains four arms, three of which consist of either conventional chemotherapy based on published clinical trials, moving a second-line therapy to the first line, or adding maintenance therapy, all of which have the goal of inducing as many complete remissions as possible.
The remaining adaptive therapy arm, however, is entirely novel in approach, with therapy using a combination of chemotherapy drugs that will be started and interrupted based on tumor responses, with resumption of therapy on an adaptive schedule unique to each patient. The goal of treatment for patients enrolled in this arm will be prolongation of the time to disease progression, rather than complete remission.
Although some people might consider the adaptive therapy approach to be sacrificing the hope for a cure in exchange for palliation, the hard truth is that patients with fusion-positive rhabdomyosarcoma (in contrast to those with fusion-negative disease) have a dismal prognosis following relapse after up-front intensified therapy.
Instead, because a cure is exceedingly unlikely in patients with metastatic disease, the conventional idea of delivering the maximum tolerated dose of chemotherapy until disease progression could be replaced by an approach based on understanding of the evolution of cancer cells under selective pressures, Dr. Reed and colleagues contend.
“Although adaptive therapy would represent a major paradigm shift in pediatric oncology, this approach would exploit the chemotherapy-sensitive population to prevent the emergence of resistant populations, optimizing tumor control with less toxicity,” they wrote in a commentary published online in the journal Cancer.1
Poor survival with advanced disease
Childhood rhabdomyosarcoma (RMS) is a form of soft tissue sarcoma of mesenchymal origin. Approximately 25% of cases are parameningeal, arising from sites adjacent to the meninges of the nasopharynx, middle ear, paranasal sinuses, orbit, and other regions of the head and neck. Approximately 31% of cases arise in the genitourinary tract and 13% in the extremities, and other tumors occur less commonly in the trunk, chest wall, perineal/anal region, and abdomen.
The overall 5-year survival rate is approximately 71%.1
However, for patients with high-risk disease, a group that includes children 10 years of age or older with widespread disease with or without an activating PAX/FOX01 gene fusion, 5-year survival ranges from just 20% to 30% (Cancer Facts & Figures 2020).
“Among patients with metastatic disease, there is a clear difference in overall survival between those who have fusion-positive disease, where the 5-year overall survival is about 19%, and patients with fusion-negative disease,” said Douglas S. Hawkins, MD, chair of the children’s oncology group and professor of pediatrics at the University of Washington, Seattle, and associate chief in the division of hematology/oncology at Seattle Children’s Hospital.
Patients with fusion-negative disease can be further classified into those with multiple metastatic sites, with a 5-year overall survival rate of approximately 45%, and those with a single metastatic site, with a 5-year overall survival rate of 70%, he said in an interview.
“So when we talk about metastatic rhabdomyosarcoma, there actually is a diversity of outcomes, between really bad – those with fusion-positive disease – and not terrible – not great, but not terrible – for a selected group of patients with fusion-negative disease,” Dr. Hawkins said.
The poor prognosis for patients with metastatic fusion-positive disease prompted Dr. Reed and colleagues to rethink the entire approach to advanced cancers.
“If someone has a sarcoma, we know that we need to do surgery and radiation to the area, we know that localized disease does better than metastatic disease, and we generally hit it with some kind of chemotherapy that we call ‘standard of care,’ ” he said in an interview.
This approach is largely effective in some forms of cancer of bone and soft tissues, such as Ewing sarcoma, he notes, which has 5-year survival rates below 20% when treated with surgery and radiation only, but with the addition of chemotherapy has 5-year overall survival rates as high as 80%.
“At other times, with other sarcomas, the cure rate is abysmal, but we still call it standard of care,” Dr. Reed said.
For example, patients with metastatic fusion-positive RMS may have an initial response to chemotherapy, but most will eventually experience relapse and die of the disease.
“With some of the most common treatments, 70% of patients will have their cancers shrink by more than 50%, which is a major response, but the vast majority of them will have a recurrence later on,” Dr. Hawkins said.
He noted that the standard of care for patients with metastatic rhabdomyosarcoma, both with and without the PAX/FOX01 fusion, is chemotherapy, generally with the VAC regimen (vincristine, actinomycin D, and cyclophosphamide), although other agents such as doxorubicin, ifosfamide, etoposide, or irinotecan have also been tried, with little effect on event-free survival or overall survival rates.
A life too brief
Ricky Huff and his family know the course that the disease can take only too well. In 2015, his 5-month-old son, Theo, was diagnosed with metastatic rhabdomyosarcoma and put under the care of Damon Reed at Moffitt.
“During the whole course of treatment – I’m sure like many other parents – apart from relying on Damon and his treatment expertise to try to determine the best treatment options, I was reading everything under the sun to try to get a working knowledge of what Theo was up against, what his treatment and clinical trial options were, and what was the state of the science,” Mr. Huff says.
Unfortunately, the characteristics of Theo’s disease, including his very young age at onset and diagnosis of stage 4 metastatic disease, conspired against him, and despite undergoing 14 months of chemotherapy, Theo died of the disease in October 2016, 5 months shy of what would have been his second birthday.
In their grief, Mr. Huff, a real estate lawyer with a practice in Clearwater, Fla., and his wife, Leah, were determined to help other families of children with cancer and settled on the National Pediatric Cancer Foundation. Mr. Huff joined the board of directors of the foundation, which is collaborating with Moffitt Cancer Center on the adaptive therapy trial.
An evolutionary primer (cancer edition)
To get a better idea of just how adaptive therapy works, it is helpful to view cancer cells through the lens of species development, adaptation, extinction, and evolution.
“Cancer cells compete against each other in a dynamic environment. Their tumor ecosystems exhibit spatial and temporal fluctuations in blood-borne nutrients, oxygen, growth factors, immune cells, and hormones,” Dr. Reed and colleagues wrote.
These influences can affect genetically identical cancer cells, which may begin to diverge from one another depending on their location in a tumor and the availability of nutrients, which in turn can result in two once-identical cells exhibiting different transcription rates for growth factors.
“Ultimately, this may affect the rate of progression through the cell cycle, leading to distinct rates of proliferation and mutational acquisition,” they wrote.
The diverging subpopulations will begin to develop different methods for adapting to the tumor microenvironment, with unique strategies for both accelerating growth and avoiding hazards such as chemotherapy drugs or radiation, the investigators explained.
“By the time a cancer becomes clinically apparent, cancer cells have transformed from a single clone into a diverse community of cell types evolving in response to a spatially and temporally heterogeneous tumor environment. Theoretically, a 10-gram cancer may contain the same order of magnitude of cancer cells as there are humans on earth, with tremendous diversity of phenotypes and environments,” they wrote.
Survival of the fittest
The competition of individuals within and between species described by Darwin also applies to cancer cells, in their interactions both with each other and with stromal cells and immune cells resulting in “the progressive replacement of less fit phenotypes by those that are more fit,” Dr. Reed and colleagues explained.
And just like the old joke about two hikers trying to escape from a charging grizzly bear (one says, “This is futile – we can’t outrun a grizzly,” and the other says, “I only have to outrun you!”), cancer cells only need to be more resistant to therapeutic attack than normal cells that are critical to function.
“This may explain why initial responses in certain solid tumors (notably rhabdomyosarcoma) do not predict eventual survival. The sensitivities of the dominant cancer cell populations dictate the initial response, but it is the ecology and evolution of the rare and more resistant populations that determine cure or relapse,” they wrote.
The endangered species list
As with many types of cancer, the current approach to treating pediatric sarcomas with curative intent is with a “first strike” approach, treating patients with surgery, radiation, and cytotoxic chemotherapy at the maximum tolerated dose for as long as needed or until unacceptable toxicities occur, with the intention of wiping out all cancer cells without permanently injuring normal cells.
The evolutionary analogy to this approach is a mass extinction event such as the meteor strike that is believed to have wiped out the dinosaurs roughly 66 million years ago. Fossil evidence suggests that the cataclysmic event resulted in the atmosphere being blanketed with dust particles that blocked sunlight and caused massive die-off of plants that dinosaurs needed to survive and were ill-adapted to do without.
In contrast, populations of smaller, more adaptable species of microbes, insects, and animals, including our mammalian ancestors, were able to survive and eventually flourish.
Many patients with localized cancers may be cured with up-front therapy, but others will have residual disease from populations of cells that are intrinsically resistant to therapy or have developed new evasion strategies.
Strike two and the MVP
Dr. Reed and colleagues liken the approach of second-line therapy for treatment of relapsed or refractory disease to the concept of “background extinctions,” using the fate of the passenger pigeon as an example of how a second-strike therapeutic strategy works.
Although the popular conception is that the passenger pigeon was hunted to extinction by humans, the species in fact died out because of many different factors, including loss of habitat, isolation of populations leading to a loss of genetic diversity, and disruption of breeding habits.
“Once first strikes of deforestation and hunting reduced the birds to small, fragmented populations, a series of what would otherwise have been minor second strikes pushed the passenger pigeon below its extinction threshold, or minimum viable population,” they said.
The analogy, as it applies to cancer therapy, is the use of second-line or follow-on therapy with one or more agents that the residual cells are at least in theory not resistant to. In the case of fusion-positive rhabdomyosarcoma, the drug most commonly added in the second-strike approach is vinorelbine.2
“Second strikes should be timed to occur around the time when the first strike has achieved its greatest effect, presumably at the point when the disease becomes clinically undetectable or at a measurable nadir,” Dr. Reed and colleagues wrote. “Ideally, second-strike therapies should have modes of action that require different resistance strategies by the cancer cells than those needed for resistance to the first strike.”
Adaptive therapy
As Dr. Reed and colleagues note, despite optimal therapy, 94% of patients with metastatic fusion-positive rhabdomyosarcoma will experience a relapse within 3 years of diagnosis.1 Clearly the scorched earth or “throw everything you have it” approach no longer works, and that’s where adaptive therapy comes in.
Here again, the authors rely on nature, or rather human interaction with nature, to devise a strategy for keeping the disease at bay when extinction of all cancerous cells cannot be achieved.
They cite the example of agricultural integrated pest management, which seeks to keep harmful insects in check by treating them to suppress but not completely destroy a population, then stopping the use of pesticides, and resuming only when the insect population spikes and again becomes a threat to crops.
“The goal is to limit crop damage while retaining the sensitivity of the insects to the pesticides. Resistance most often comes at a cost. In the absence of the pesticide, sensitive individuals will outcompete resistant individuals,” they wrote.
Adaptive therapy uses the same approach to reduce selection pressures that foster resistance, with patients treated only until a specific, predetermined response is achieved in the dominant population of chemosensitive cells. The treatment is then interrupted and reintroduced only when the tumor rebounds to a certain predetermined size.
In this scenario, cells that retain sensitivity to chemotherapy will be able to reproduce and proliferate more rapidly than drug-resistant cells, and the therapy can then be reintroduced. This strategy is less likely to cause the development and proliferation of resistant cells than conventional intensified chemotherapy, Dr. Reed and colleagues contend.
Putting it to the test
The clinical trial that Dr. Reed and colleagues have initiated, officially titled “Evolutionary Inspired Therapy for Newly Diagnosed, Metastatic, Fusion Positive Rhabdomyosarcoma,” (NCT04388839) contains four arms: three experimental and one active comparator arm.
“We won’t randomize; we don’t feel that it would be fair to randomize patients, because these arms are so different from each other,” Dr. Reed said.
Arm A is the experimental first-strike arm, a 42-week course containing cyclophosphamide delivered intravenously over 60 minutes at a dose ranging from 220 mg to 1200 mg, vinorelbine delivered in an IV push over 6-10 minutes with a dose ranging from 4 mg to 25 mg, and actinomycin D administered via IV over 3-5 minutes at a dose ranging from 0.025 mg to 0.04 mg.
“The idea is that we take the standard of care, and we add a drug – vinorelbine – to make it stronger,” Dr. Reed said. “The idea is that the resistant cell, the cell that escapes, if we start hitting it on day 1 with vinorelbine, we might be able to drive it to extinction.”
Arm B, the second experimental arm, is the second-strike and maintenance arm, in which patients will receive conventional doses of vincristine, actinomycin D, and cyclophosphamide (VAC) until complete response (CR) for 12-42 weeks, and will then be switched to up to 2 years of maintenance with vinorelbine and oral cyclophosphamide.
“Vinorelbine will be added when the cancer is declining or first goes into remission. We try not to wait 42 weeks, which is too long we think, by which time the cancer may be fully adapted and resistant,” he explained.
Arm C is the adaptive therapy arm, in which patients will receive VAC that starts and stops based on response, with the goal of prolonging time to disease progression rather than achieving CR.
Arm D is the active comparator arm, consisting of conventional chemotherapy based on published clinical trials, such as VAC for 42 weeks, or other standard-of-care regimens that may include irinotecan, doxorubicin, ifosfamide, and/or etoposide.
A change in thinking
Dr. Reed acknowledges that Arm C, the adaptive therapy arm, “definitely represents a change in thinking for pediatric oncology.”
“The idea is that if you could do this perfectly well, you would be able to take a patient who is diagnosed today and essentially ‘pause’ their disease for a while. Then 5 years from now, if there is a better medicine, you would have gotten that patient to that medicine.”
The optimal approach to treating metastatic fusion-positive rhabdomyosarcoma may be similar to that used for treatment of acute lymphoblastic leukemia, with induction, consolidation, and maintenance and the option of delayed intensification, he said.
“But we’re so far away from knowing which series to do that we just need to show that any series – any changing it up – is helpful.”
Dr. Reed said that when he started presenting the concept of adaptive therapy in clinical meetings in 2017, “I was told to come up with a better idea. There were several people who instantly got it, but most people would instantly get angry.”
The common refrain was that adaptive therapy was “giving up.”
But minds began to change in 2018, following presentation at the annual meeting of the American Society of Clinical Oncology of a European study showing that adding 6 months of low-dose chemotherapy maintenance to standard therapy improved the 5-year overall survival rate of pediatric rhabdomyosarcoma from 73.7% to 86.6%.2
Before presenting the idea of adaptive therapy to his colleagues, he ran it by the parents of children with advanced sarcomas, and many were on board with it, he said.
Ricky Huff said that had the option of adaptive therapy been available for Theo, he and his wife would have been willing to try it.
“Of course, everyone has the ability in hindsight to apply critical thinking to decisions that you made or could have made,” he said. “I think is true for many parents, who if they’re presented with information about options will say ‘well if there’s a 1 percent chance, I want that chance for my child, especially for a 5-month-old.”
The decision to choose adaptive therapy is a difficult decision to make, whether for oneself or for one’s son, because it isn’t curative.
“My wife and I have since had a conversation about this, and I do think we would have considered it, although through a lot of difficult conversations,” he said.
“After we got the pathology, knowing that it was metastatic, fusion-positive, and given his age, just doing a brief literature review on my own, I knew what we were up against using 20-year-old treatments, and that the chance of a cure was very, very small.”
If parents of children with metastatic, poor-prognosis rhabdomyosarcoma could be made to understand that adaptive therapy would entail shorter and fewer hospital stays, and cumulatively less toxic chemotherapy, and could prolong the lives of their children, the option might be more acceptable, he said.
And as Dr. Reed mentioned, prolonging time to progression offers hope of additional therapies to come.
“The whole time that my son was being treated, I hoped that there was going to be something else that came out, that a new trial would be launched because they found a way to drug a mutation, or treat it with immunotherapy – something that was going to give us a better option.”
Asked whether he would be willing to share his experiences in this article, Mr. Huff said that “I am willing to, in whatever small way I can, make an impact, and hopefully save another family from what we experienced.”
References
1. Reed DR et al. Cancer. 2020 Jun 1;126(11):2577-87 2. Bisogno G et al. J Clin Oncol. 2018;36:18_suppl,LBA-2
In 1859, Charles Darwin published “On the Origin of Species,” which outlined his world-shaking theory of evolution and its core principle of natural selection caused by environmental pressures that may determine whether an organism adapts and survives, or remains static, languishes, and eventually dies out.
The same forces that have influenced the size and shape of the beaks of finches in the Galapagos Islands, the length of giraffe necks in Africa, and the intestinal microbiomes of the nearly 8 billion human inhabitants of this planet also control whether malignant cells thrive and multiply, wither and die when assaulted by chemotherapy, or go into hiding, mutating and waiting for their next opportunity to erupt again and metastasize.
The ability of malignant cells to adapt to environmental pressures is “cancer’s most lethal and sophisticated property,” said Damon R. Reed, MD, program leader of the adolescent/young adult program at Moffitt Cancer Center in Tampa, Fla.
Dr. Reed and colleagues are developing methods to meet cancer on its own terms, applying evolutionary principles to the treatment of childhood fusion-positive rhabdomyosarcoma in an innovative, and some would say audacious, clinical trial.
Adaptive versus conventional therapy
The trial, now recruiting, is designed to evaluate each of four different strategies for chemotherapy schedules in patients with newly diagnosed metastatic fusion-positive rhabdomyosarcoma.
The trial contains four arms, three of which consist of either conventional chemotherapy based on published clinical trials, moving a second-line therapy to the first line, or adding maintenance therapy, all of which have the goal of inducing as many complete remissions as possible.
The remaining adaptive therapy arm, however, is entirely novel in approach, with therapy using a combination of chemotherapy drugs that will be started and interrupted based on tumor responses, with resumption of therapy on an adaptive schedule unique to each patient. The goal of treatment for patients enrolled in this arm will be prolongation of the time to disease progression, rather than complete remission.
Although some people might consider the adaptive therapy approach to be sacrificing the hope for a cure in exchange for palliation, the hard truth is that patients with fusion-positive rhabdomyosarcoma (in contrast to those with fusion-negative disease) have a dismal prognosis following relapse after up-front intensified therapy.
Instead, because a cure is exceedingly unlikely in patients with metastatic disease, the conventional idea of delivering the maximum tolerated dose of chemotherapy until disease progression could be replaced by an approach based on understanding of the evolution of cancer cells under selective pressures, Dr. Reed and colleagues contend.
“Although adaptive therapy would represent a major paradigm shift in pediatric oncology, this approach would exploit the chemotherapy-sensitive population to prevent the emergence of resistant populations, optimizing tumor control with less toxicity,” they wrote in a commentary published online in the journal Cancer.1
Poor survival with advanced disease
Childhood rhabdomyosarcoma (RMS) is a form of soft tissue sarcoma of mesenchymal origin. Approximately 25% of cases are parameningeal, arising from sites adjacent to the meninges of the nasopharynx, middle ear, paranasal sinuses, orbit, and other regions of the head and neck. Approximately 31% of cases arise in the genitourinary tract and 13% in the extremities, and other tumors occur less commonly in the trunk, chest wall, perineal/anal region, and abdomen.
The overall 5-year survival rate is approximately 71%.1
However, for patients with high-risk disease, a group that includes children 10 years of age or older with widespread disease with or without an activating PAX/FOX01 gene fusion, 5-year survival ranges from just 20% to 30% (Cancer Facts & Figures 2020).
“Among patients with metastatic disease, there is a clear difference in overall survival between those who have fusion-positive disease, where the 5-year overall survival is about 19%, and patients with fusion-negative disease,” said Douglas S. Hawkins, MD, chair of the children’s oncology group and professor of pediatrics at the University of Washington, Seattle, and associate chief in the division of hematology/oncology at Seattle Children’s Hospital.
Patients with fusion-negative disease can be further classified into those with multiple metastatic sites, with a 5-year overall survival rate of approximately 45%, and those with a single metastatic site, with a 5-year overall survival rate of 70%, he said in an interview.
“So when we talk about metastatic rhabdomyosarcoma, there actually is a diversity of outcomes, between really bad – those with fusion-positive disease – and not terrible – not great, but not terrible – for a selected group of patients with fusion-negative disease,” Dr. Hawkins said.
The poor prognosis for patients with metastatic fusion-positive disease prompted Dr. Reed and colleagues to rethink the entire approach to advanced cancers.
“If someone has a sarcoma, we know that we need to do surgery and radiation to the area, we know that localized disease does better than metastatic disease, and we generally hit it with some kind of chemotherapy that we call ‘standard of care,’ ” he said in an interview.
This approach is largely effective in some forms of cancer of bone and soft tissues, such as Ewing sarcoma, he notes, which has 5-year survival rates below 20% when treated with surgery and radiation only, but with the addition of chemotherapy has 5-year overall survival rates as high as 80%.
“At other times, with other sarcomas, the cure rate is abysmal, but we still call it standard of care,” Dr. Reed said.
For example, patients with metastatic fusion-positive RMS may have an initial response to chemotherapy, but most will eventually experience relapse and die of the disease.
“With some of the most common treatments, 70% of patients will have their cancers shrink by more than 50%, which is a major response, but the vast majority of them will have a recurrence later on,” Dr. Hawkins said.
He noted that the standard of care for patients with metastatic rhabdomyosarcoma, both with and without the PAX/FOX01 fusion, is chemotherapy, generally with the VAC regimen (vincristine, actinomycin D, and cyclophosphamide), although other agents such as doxorubicin, ifosfamide, etoposide, or irinotecan have also been tried, with little effect on event-free survival or overall survival rates.
A life too brief
Ricky Huff and his family know the course that the disease can take only too well. In 2015, his 5-month-old son, Theo, was diagnosed with metastatic rhabdomyosarcoma and put under the care of Damon Reed at Moffitt.
“During the whole course of treatment – I’m sure like many other parents – apart from relying on Damon and his treatment expertise to try to determine the best treatment options, I was reading everything under the sun to try to get a working knowledge of what Theo was up against, what his treatment and clinical trial options were, and what was the state of the science,” Mr. Huff says.
Unfortunately, the characteristics of Theo’s disease, including his very young age at onset and diagnosis of stage 4 metastatic disease, conspired against him, and despite undergoing 14 months of chemotherapy, Theo died of the disease in October 2016, 5 months shy of what would have been his second birthday.
In their grief, Mr. Huff, a real estate lawyer with a practice in Clearwater, Fla., and his wife, Leah, were determined to help other families of children with cancer and settled on the National Pediatric Cancer Foundation. Mr. Huff joined the board of directors of the foundation, which is collaborating with Moffitt Cancer Center on the adaptive therapy trial.
An evolutionary primer (cancer edition)
To get a better idea of just how adaptive therapy works, it is helpful to view cancer cells through the lens of species development, adaptation, extinction, and evolution.
“Cancer cells compete against each other in a dynamic environment. Their tumor ecosystems exhibit spatial and temporal fluctuations in blood-borne nutrients, oxygen, growth factors, immune cells, and hormones,” Dr. Reed and colleagues wrote.
These influences can affect genetically identical cancer cells, which may begin to diverge from one another depending on their location in a tumor and the availability of nutrients, which in turn can result in two once-identical cells exhibiting different transcription rates for growth factors.
“Ultimately, this may affect the rate of progression through the cell cycle, leading to distinct rates of proliferation and mutational acquisition,” they wrote.
The diverging subpopulations will begin to develop different methods for adapting to the tumor microenvironment, with unique strategies for both accelerating growth and avoiding hazards such as chemotherapy drugs or radiation, the investigators explained.
“By the time a cancer becomes clinically apparent, cancer cells have transformed from a single clone into a diverse community of cell types evolving in response to a spatially and temporally heterogeneous tumor environment. Theoretically, a 10-gram cancer may contain the same order of magnitude of cancer cells as there are humans on earth, with tremendous diversity of phenotypes and environments,” they wrote.
Survival of the fittest
The competition of individuals within and between species described by Darwin also applies to cancer cells, in their interactions both with each other and with stromal cells and immune cells resulting in “the progressive replacement of less fit phenotypes by those that are more fit,” Dr. Reed and colleagues explained.
And just like the old joke about two hikers trying to escape from a charging grizzly bear (one says, “This is futile – we can’t outrun a grizzly,” and the other says, “I only have to outrun you!”), cancer cells only need to be more resistant to therapeutic attack than normal cells that are critical to function.
“This may explain why initial responses in certain solid tumors (notably rhabdomyosarcoma) do not predict eventual survival. The sensitivities of the dominant cancer cell populations dictate the initial response, but it is the ecology and evolution of the rare and more resistant populations that determine cure or relapse,” they wrote.
The endangered species list
As with many types of cancer, the current approach to treating pediatric sarcomas with curative intent is with a “first strike” approach, treating patients with surgery, radiation, and cytotoxic chemotherapy at the maximum tolerated dose for as long as needed or until unacceptable toxicities occur, with the intention of wiping out all cancer cells without permanently injuring normal cells.
The evolutionary analogy to this approach is a mass extinction event such as the meteor strike that is believed to have wiped out the dinosaurs roughly 66 million years ago. Fossil evidence suggests that the cataclysmic event resulted in the atmosphere being blanketed with dust particles that blocked sunlight and caused massive die-off of plants that dinosaurs needed to survive and were ill-adapted to do without.
In contrast, populations of smaller, more adaptable species of microbes, insects, and animals, including our mammalian ancestors, were able to survive and eventually flourish.
Many patients with localized cancers may be cured with up-front therapy, but others will have residual disease from populations of cells that are intrinsically resistant to therapy or have developed new evasion strategies.
Strike two and the MVP
Dr. Reed and colleagues liken the approach of second-line therapy for treatment of relapsed or refractory disease to the concept of “background extinctions,” using the fate of the passenger pigeon as an example of how a second-strike therapeutic strategy works.
Although the popular conception is that the passenger pigeon was hunted to extinction by humans, the species in fact died out because of many different factors, including loss of habitat, isolation of populations leading to a loss of genetic diversity, and disruption of breeding habits.
“Once first strikes of deforestation and hunting reduced the birds to small, fragmented populations, a series of what would otherwise have been minor second strikes pushed the passenger pigeon below its extinction threshold, or minimum viable population,” they said.
The analogy, as it applies to cancer therapy, is the use of second-line or follow-on therapy with one or more agents that the residual cells are at least in theory not resistant to. In the case of fusion-positive rhabdomyosarcoma, the drug most commonly added in the second-strike approach is vinorelbine.2
“Second strikes should be timed to occur around the time when the first strike has achieved its greatest effect, presumably at the point when the disease becomes clinically undetectable or at a measurable nadir,” Dr. Reed and colleagues wrote. “Ideally, second-strike therapies should have modes of action that require different resistance strategies by the cancer cells than those needed for resistance to the first strike.”
Adaptive therapy
As Dr. Reed and colleagues note, despite optimal therapy, 94% of patients with metastatic fusion-positive rhabdomyosarcoma will experience a relapse within 3 years of diagnosis.1 Clearly the scorched earth or “throw everything you have it” approach no longer works, and that’s where adaptive therapy comes in.
Here again, the authors rely on nature, or rather human interaction with nature, to devise a strategy for keeping the disease at bay when extinction of all cancerous cells cannot be achieved.
They cite the example of agricultural integrated pest management, which seeks to keep harmful insects in check by treating them to suppress but not completely destroy a population, then stopping the use of pesticides, and resuming only when the insect population spikes and again becomes a threat to crops.
“The goal is to limit crop damage while retaining the sensitivity of the insects to the pesticides. Resistance most often comes at a cost. In the absence of the pesticide, sensitive individuals will outcompete resistant individuals,” they wrote.
Adaptive therapy uses the same approach to reduce selection pressures that foster resistance, with patients treated only until a specific, predetermined response is achieved in the dominant population of chemosensitive cells. The treatment is then interrupted and reintroduced only when the tumor rebounds to a certain predetermined size.
In this scenario, cells that retain sensitivity to chemotherapy will be able to reproduce and proliferate more rapidly than drug-resistant cells, and the therapy can then be reintroduced. This strategy is less likely to cause the development and proliferation of resistant cells than conventional intensified chemotherapy, Dr. Reed and colleagues contend.
Putting it to the test
The clinical trial that Dr. Reed and colleagues have initiated, officially titled “Evolutionary Inspired Therapy for Newly Diagnosed, Metastatic, Fusion Positive Rhabdomyosarcoma,” (NCT04388839) contains four arms: three experimental and one active comparator arm.
“We won’t randomize; we don’t feel that it would be fair to randomize patients, because these arms are so different from each other,” Dr. Reed said.
Arm A is the experimental first-strike arm, a 42-week course containing cyclophosphamide delivered intravenously over 60 minutes at a dose ranging from 220 mg to 1200 mg, vinorelbine delivered in an IV push over 6-10 minutes with a dose ranging from 4 mg to 25 mg, and actinomycin D administered via IV over 3-5 minutes at a dose ranging from 0.025 mg to 0.04 mg.
“The idea is that we take the standard of care, and we add a drug – vinorelbine – to make it stronger,” Dr. Reed said. “The idea is that the resistant cell, the cell that escapes, if we start hitting it on day 1 with vinorelbine, we might be able to drive it to extinction.”
Arm B, the second experimental arm, is the second-strike and maintenance arm, in which patients will receive conventional doses of vincristine, actinomycin D, and cyclophosphamide (VAC) until complete response (CR) for 12-42 weeks, and will then be switched to up to 2 years of maintenance with vinorelbine and oral cyclophosphamide.
“Vinorelbine will be added when the cancer is declining or first goes into remission. We try not to wait 42 weeks, which is too long we think, by which time the cancer may be fully adapted and resistant,” he explained.
Arm C is the adaptive therapy arm, in which patients will receive VAC that starts and stops based on response, with the goal of prolonging time to disease progression rather than achieving CR.
Arm D is the active comparator arm, consisting of conventional chemotherapy based on published clinical trials, such as VAC for 42 weeks, or other standard-of-care regimens that may include irinotecan, doxorubicin, ifosfamide, and/or etoposide.
A change in thinking
Dr. Reed acknowledges that Arm C, the adaptive therapy arm, “definitely represents a change in thinking for pediatric oncology.”
“The idea is that if you could do this perfectly well, you would be able to take a patient who is diagnosed today and essentially ‘pause’ their disease for a while. Then 5 years from now, if there is a better medicine, you would have gotten that patient to that medicine.”
The optimal approach to treating metastatic fusion-positive rhabdomyosarcoma may be similar to that used for treatment of acute lymphoblastic leukemia, with induction, consolidation, and maintenance and the option of delayed intensification, he said.
“But we’re so far away from knowing which series to do that we just need to show that any series – any changing it up – is helpful.”
Dr. Reed said that when he started presenting the concept of adaptive therapy in clinical meetings in 2017, “I was told to come up with a better idea. There were several people who instantly got it, but most people would instantly get angry.”
The common refrain was that adaptive therapy was “giving up.”
But minds began to change in 2018, following presentation at the annual meeting of the American Society of Clinical Oncology of a European study showing that adding 6 months of low-dose chemotherapy maintenance to standard therapy improved the 5-year overall survival rate of pediatric rhabdomyosarcoma from 73.7% to 86.6%.2
Before presenting the idea of adaptive therapy to his colleagues, he ran it by the parents of children with advanced sarcomas, and many were on board with it, he said.
Ricky Huff said that had the option of adaptive therapy been available for Theo, he and his wife would have been willing to try it.
“Of course, everyone has the ability in hindsight to apply critical thinking to decisions that you made or could have made,” he said. “I think is true for many parents, who if they’re presented with information about options will say ‘well if there’s a 1 percent chance, I want that chance for my child, especially for a 5-month-old.”
The decision to choose adaptive therapy is a difficult decision to make, whether for oneself or for one’s son, because it isn’t curative.
“My wife and I have since had a conversation about this, and I do think we would have considered it, although through a lot of difficult conversations,” he said.
“After we got the pathology, knowing that it was metastatic, fusion-positive, and given his age, just doing a brief literature review on my own, I knew what we were up against using 20-year-old treatments, and that the chance of a cure was very, very small.”
If parents of children with metastatic, poor-prognosis rhabdomyosarcoma could be made to understand that adaptive therapy would entail shorter and fewer hospital stays, and cumulatively less toxic chemotherapy, and could prolong the lives of their children, the option might be more acceptable, he said.
And as Dr. Reed mentioned, prolonging time to progression offers hope of additional therapies to come.
“The whole time that my son was being treated, I hoped that there was going to be something else that came out, that a new trial would be launched because they found a way to drug a mutation, or treat it with immunotherapy – something that was going to give us a better option.”
Asked whether he would be willing to share his experiences in this article, Mr. Huff said that “I am willing to, in whatever small way I can, make an impact, and hopefully save another family from what we experienced.”
References
1. Reed DR et al. Cancer. 2020 Jun 1;126(11):2577-87 2. Bisogno G et al. J Clin Oncol. 2018;36:18_suppl,LBA-2
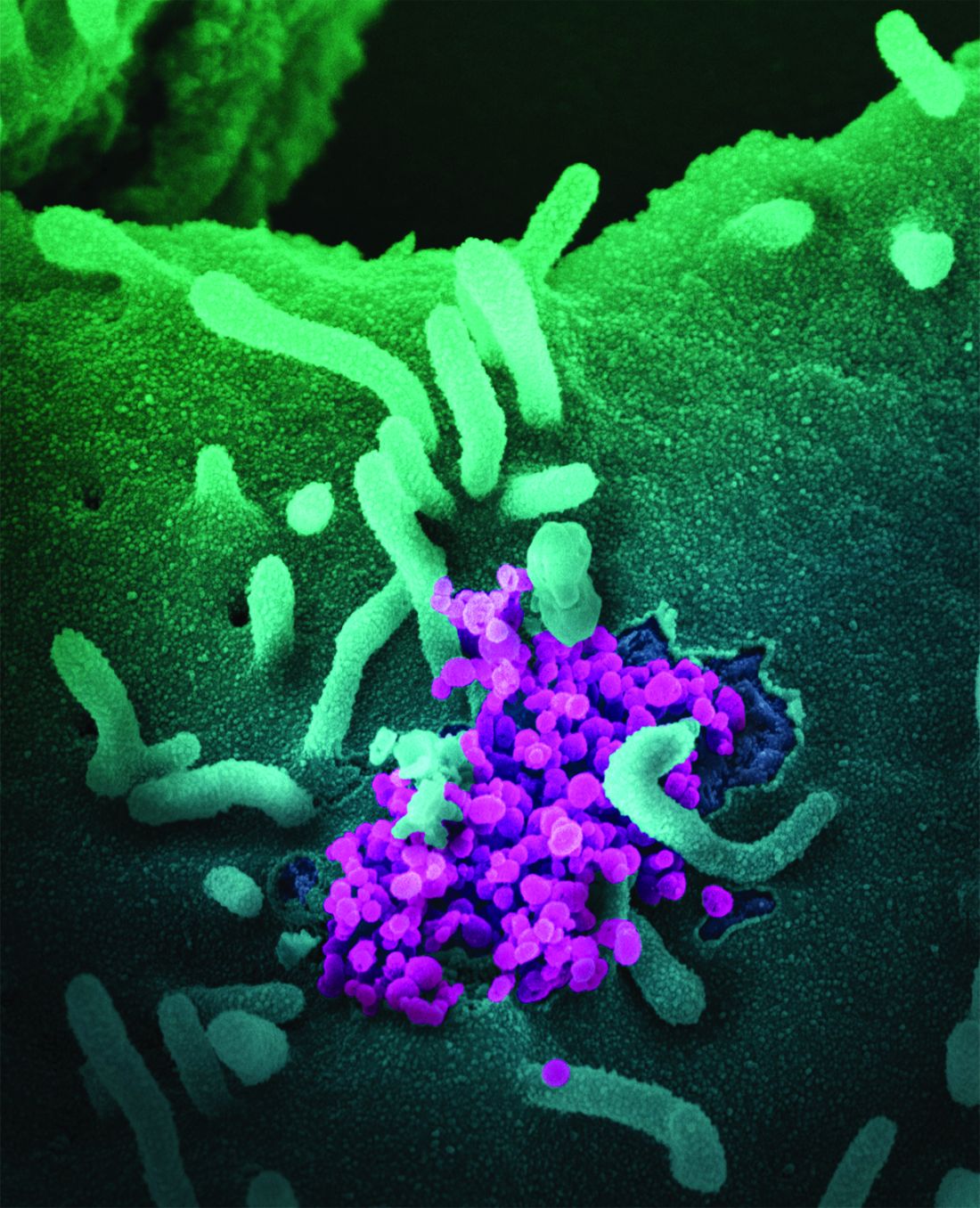
Meeting the unmet need in multiple myeloma
In multiple myeloma, survival has been very significantly improved by immunomodulatory drugs, proteasome inhibitors, and CD38-targeting antibodies. Despite these advances, multiple myeloma, which is characterized by malignant proliferation of clonal plasma cells in bone marrow, remains an incurable plasma cell disorder with near-certain relapse after successful treatment. Prognosis for patients who develop triple-class refractory disease is poor, with less than 1-year survival. The substantial unmet therapeutic need extends further to other poor survival multiple myeloma populations that include newly diagnosed patients with high cytogenic risk profiles and those with early relapse after first-line therapy. For all of these, interest in drugs with novel mechanisms of action is naturally high.
More specific, less toxic
Post allogeneic hematopoietic stem-cell transplantation and donor lymphocyte infusion sustained remissions reflect a graft-versus-myeloma effect mediated by donor T cells.1 The substantial morbidity and mortality associated with graft-versus-host disease and opportunistic infections, however, have spurred searches for alternative, more specific, and less toxic T-cell therapies with stronger antitumor activity.
Chimeric antigen receptors (CARs)
In CAR T-cell therapies for multiple myeloma, autologous T cells are harvested from the patient and reprogrammed to target multiple myeloma cells through the introduction of genes that encode CARs, which are fusion proteins coupling an antigen-recognition moiety and a transmembrane-spanning element to a T-cell activation domain (typically CD3 zeta [CD247]). The T cells are then expanded and reinfused to the patient following a lymphodepletion regimen. Five strategies using autologous CAR T cells are currently approved for diffuse large B-cell lymphomas, acute lymphoblastic leukemia, multiple myeloma, and other hematologic malignancies. Notably, in patients with heavily pretreated multiple myeloma, CAR T cells have demonstrated impressive activity.
BCMA-targeting CAR T cells
The B-cell maturation antigen (BCMA; TNFRSF17), which plays an important role in the survival of long-lived plasma cells in bone marrow, is an attractive target for CAR T-cell therapy because it is expressed on normal and malignant plasma cell surfaces and by mature B cells. When ligands (TNFSF 13B/TNFSF13) bind to BCMA expressed on multiple myeloma cell surfaces, survival and proliferation pathways and drug resistance are activated.
High-quality responses have been demonstrated in several trials of anti-BCMA CAR T cells, which kill multiple myeloma cell lines and primary multiple myeloma cells through degranulation of T cells and lysis of tumor cells, even those with low BCMA expression. Based on efficacy in triple-class exposed multiple myeloma that compared favorably to conventional care with improved health-related quality of life, the U.S. Food and Drug Administration gave breakthrough designation to ciltacabtagene autoleucel in December 2019 and approval for idecabtagene vicleucel in March 2021.
Idecabtagene vicleucel
Idecabtagene vicleucel expresses a murine BCMA-targeting single-chain variable fragment with a 4-1BB costimulatory motif. The phase 2 KarMMa study2 evaluated idecabtagene vicleucel (target dose of 450 × 106 CAR T cells; range 150 × 106 to 450 × 106) activity in 128 patients with triple-class exposed multiple myeloma. Partial responses or better were observed in 94 of 128 patients (73%) (95% confidence interval, 66-81); 42 (33%) had a complete response or better (95% CI, 25-41), with a median progression-free survival of 8.8 months (95% CI, 5.6-11.6). Outcomes were improved in the highest fixed-dose group, with partial response or better in 81% (44 of 55), complete response or better in 39% (21), and median overall survival of 12.1 months (95% CI, 8.8-12.3). Patients with high-risk cytogenetic profiles, extramedullary disease, and high tumor burden also had deep and durable responses. Outcomes were less favorable in patients with revised International Staging System stage 3 disease.
Ciltacabtagene autoleucel
Ciltacabtagene autoleucel, a 4-1BB–based CAR T-cell therapy with two BCMA-targeting domains, confers high-avidity binding. In the phase 1b/2 CARTITUDE-1 study, conducted in the United States and Europe, preliminary results in 97 patients showed a 97% response rate with ciltacabtagene autoleucel (target dose 0.75 × 106 CAR T cells per kg), and in 65 patients, a complete response (67%). Progression-free survival at 12 months was 77% (95% CI, 66-84) and overall survival was 89% (95% CI, 80-94).3
In the phase 1 LEGEND-2 study4 that was conducted at four sites in China among less heavily pretreated multiple myeloma patients, while all used the same CAR construct, sites used variable conditioning regimens (split versus single). In the site using cyclophosphamide as the lymphodepletion therapy and three split CAR T-cell infusions, partial response or better was achieved in 50 patients (88%) with a median of three prior therapy lines. The complete response rate was high (74%) and minimal residual disease negativity was reached in 39 patients (68%). Median progression-free survival was 19.9 months (95% CI, 9.6-31.0), but 28.2 months among those with complete responses (95% CI, 19.9-not estimable). Median overall survival was also favorable at 36.1 months (95% CI, 26.4-not estimable); it was 35.0 months-not estimable among patients with complete responses. Results from the other three sites were comparable.
Noteworthy among other BCMA-targeting CAR T-cell products in earlier stages of clinical development is orvacabtagene autoleucel, which has a fully human BCMA-specific binding domain. At higher doses (300 × 106 to 600 × 106 CAR T cells) among 62 patients with triple-class–exposed multiple myeloma in the EVOLVE trial, 92% had a partial or better response, with complete responses or better in 36%, all with an encouraging safety profile.
BCMA-targeting CAR T cell toxicity
While van de Donk, Usmani, and Yong, in their review1 note a lack of evidence of off-target toxicity with BCMA-targeting CAR T-cell therapy in clinical studies so far, they do point to several clinical syndromes (cytokine release syndrome, infections, respiratory failure, neurotoxicity, pulmonary aspergillosis, gastrointestinal hemorrhage) caused by cytokines produced during CAR T-cell expansion and to cytopenias and infections arising from prior treatment, bridging therapy, and lymphodepleting conditioning. Deaths attributed to treatment in the above-mentioned trials underscore the need for careful monitoring and early intervention.
Cytokine release syndrome
In the BCMA-targeting CAR T-cell therapy studies, the frequency of cytokine release syndrome varies widely from 17% to 95% but is generally attributed to CAR T-cell activation and is associated with increased serum ferritin concentrations, high c-reactive proteins, and proinflammatory cytokines. High tumor load, in multiple myeloma patients receiving CD19-targeting CAR T cells, was associated with a higher incidence of severe cytokine release syndrome. In a small number of patients, macrophage activation syndrome and hemophagocytic lymphohistiocytosis, the most aggressive variants of cytokine release syndrome, are caused by severe immune activation and lead to multiorgan dysfunction.
Neurotoxicity
Immune effector cell–-associated neurotoxicity syndrome (ICANS) symptoms, in multiple myeloma patients treated with BCMA-targeting CAR T cells, may include delirium, transient confusion, aphasia, lethargy, tremor, dysgraphia, seizures, cerebral edema, and rarely, posterior reversible encephalopathy syndrome.1 While the pathophysiology of CAR T cell–related neurotoxicity is not well understood, high tumor load, higher peak concentrations of CAR T cells, and more severe cytokine release syndrome are more common in patients with severe neurotoxicity. “The frequency of neurotoxicities,” Dr. Yong noted in an interview, “has been reduced by steps taken to mitigate these risk factors.”
High interest in phase I study
A phase I study presented in Blood has attracted interest because the novel BCMA-targeting CAR agent (CT103A) being tested is fully human.4 In an accompanying editorial, Lee and Yong note that doubt for any real potential for durable CAR T therapy responses in multiple myeloma is raised by the poor persistence of multiple myeloma CAR T cells in multiple myeloma patients.3
In the earliest trials of BCMA CARs, while reported rates of objective antimyeloma responses were in the approximately 33%-88% range among patients with relapsed/refractory multiple myeloma (RRMM), persistence was typically 6 months or less. Lee and Yong point out, however, that while correlation between persistence and duration of response (DOR) has been variable, median persistence was 308 days in the phase I study. Wang and colleagues, the phase I study authors, state that levels of CAR T-cell proliferation and duration of cellular persistence may be determinants of DOR in CAR T therapy for multiple myeloma. They observe that the multiple mechanisms potentially responsible for the inability of some CAR T cells to survive in vivo, may include antigen escape, T-cell intrinsic mechanisms, tumor microenvironment–mediated suppression, and host anti-CAR immunity. CARs with humanized or fully human single-chain variable fragments (scFvs), prior studies suggest, may retain antitumor activity through bypassing potential host anti-CAR immunogenicity.
In the study, CT103A, a fully human scFv, was tested in an open-label, single-arm design for safety and preliminary efficacy in 18 patients (8 female; median age 53.5 years) with RRMM (at least three lines of prior therapies including a proteasome inhibitor and an immunomodulatory agent) who had undergone leukapheresis and had received lymphodepletion chemotherapy with fludarabine and cyclophosphamide. Four patients (22.2%) had been treated previously with murine anti-BCMA CAR T cells. Safety and tolerability (including dose-limiting toxicity) were the primary endpoints, with efficacy and pharmacokinetics secondary.
Rapid responses
Two weeks after infusion, the overall response rate (ORR) was 77.8% (14 of 18) and by 1 month it was 88.9% (16 of 18). Eventually, all responded and 72.2% (13 of 18) achieved a complete response (CR) or stringent complete response (sCR). All 17 patients evaluated for minimum residual disease (MRD) in bone marrow were MRD-negative at 10-4 nucleated cells by flow cytometry within 1 month. Median DOR was 325 days (range, 7-573 days) for all patients and 412 days (range, 213-573 days) for the 13 with CR/sCR. CAR transgenes were detectable at the cutoff date in 77.8% of patients, with a median CAR transgene persistence of 307.5 days.
During follow-up, four deaths were reported, including one patient with persistent sCR (sudden severe infection). Progression-free survival (PFS) and overall survival (OS) rates at 1 year were 58.3% and 75%, respectively. Extramedullary myeloma was associated with a shortened PFS (79.1% versus 20.0%, P = .015), but not OS (79.1% versus 60.0%, P = .328) at 1 year.
All patients experienced grade 3 or higher adverse events, most of which were expected hematologic effects of lymphodepleting chemotherapy and CT103A infusions. Grade 1 and 2 cytokine release syndromes occurred in 70.6% patients (17 of 18), with 1 grade 4 event (5.9%). The patients receiving a dose of up to 3.0 × 106 CAR+ T cells/kg required less treatment of cytokine release syndrome than the patients who received a dose of 6.0 × 106 CAR+ T cells/kg. No immune effector cell–associated neurotoxicity syndrome was observed. Antidrug antibody positivity occurred in only 1 patient.
Two characteristics of CT103A may contribute to its long persistence, stated study senior author Jianfeng Zhou, MD, PhD, chairman and professor of the department of hematology, Tongji Hospital in Wuhan, China. “One is the reduced immunogenicity achieved by the fully human construct; another is the relatively low binding affinity of the CAR binder. Notably, four patients who previously received murine BCMA CAR were included and still benefit from CT103A. It demonstrates the possibility of retreatment with a different CAR.” Dr. Zhou also emphasized that the lack of ICANS in the entire cohort reflects the excellent safety profile of CT103A.
The editorial commentary in Blood by Lydia Sarah Hui Lee, MD, and Kwee L. Yong, PhD, underscored impressive responses to CT103A, specifically to the median time to response of 15 days, the 100% ORR, and the not reached median progression-free survival at 394 days).5 The best results in other published nonhuman BCMA CAR T-cell trials, they note, were about 1 month (time to response), approximately 33%-88% (ORR), and median progression-free survival of 7-15 months.
Immune responses, Dr. Yong said in an interview, can guide subsequent treatment. “For example, if a patient previously exposed to BCMA CAR T cells in which the construct is either chimeric or humanized, but retains some murine elements, and had detectable antimurine antibodies, we may aim for a fully human one if we are considering treating with a different BCMA CAR T-cell product.” She added, “On the other hand, a similar patient whose serum did not contain such antibodies may be a candidate for a humanized product that retained some murine elements.”
Wang and colleagues concluded, “Altogether, CT103A is safe and highly active in patients with relapsed/refractory multiple myeloma and can be developed as a promising therapy for relapsed/refractory multiple myeloma.”4 An ongoing multicenter phase II trial with single-arm design is recruiting 100 patients. The infusion dosage, suggested by the phase I trial, is 1 × 106 cells/kg. Endpoints include efficacy and safety.
Improving CAR T
Optimizing CAR design and adapting manufacturing processes to generate cell products enriched for T-cell subsets, such as early memory cells, are among strategies being explored to improve CAR T effectiveness.1 Also, dual-antigen targeting to interdict antigen escape and rational combination treatments to enhance persistence are under investigation, along with efforts to improve CAR T-cell therapy safety (for example, incorporation of a suicide gene safety system). They note further that several groups are researching use of induced pluripotent stem cells to generate large quantities of off-the-shelf CAR T-cell immunotherapies that would circumvent the complex, costly, and time-consuming process of manufacturing patient-specific autologous CAR T cells.
References
1. van de Donk N et al. Lancet Haematol. 2021 June;8(6):e446-61.
2. Munshi NC et al. N Engl J Med 2021; 384:705-716.
3. Berdeja JG et al. The Lancet. 2021 July; 398:314-24.
4. Wang D et al. Blood. 2021 May;137(21):2890-901.
5. Lee L and Yong K. Blood. 2021 May;137(21):2859-60.
In multiple myeloma, survival has been very significantly improved by immunomodulatory drugs, proteasome inhibitors, and CD38-targeting antibodies. Despite these advances, multiple myeloma, which is characterized by malignant proliferation of clonal plasma cells in bone marrow, remains an incurable plasma cell disorder with near-certain relapse after successful treatment. Prognosis for patients who develop triple-class refractory disease is poor, with less than 1-year survival. The substantial unmet therapeutic need extends further to other poor survival multiple myeloma populations that include newly diagnosed patients with high cytogenic risk profiles and those with early relapse after first-line therapy. For all of these, interest in drugs with novel mechanisms of action is naturally high.
More specific, less toxic
Post allogeneic hematopoietic stem-cell transplantation and donor lymphocyte infusion sustained remissions reflect a graft-versus-myeloma effect mediated by donor T cells.1 The substantial morbidity and mortality associated with graft-versus-host disease and opportunistic infections, however, have spurred searches for alternative, more specific, and less toxic T-cell therapies with stronger antitumor activity.
Chimeric antigen receptors (CARs)
In CAR T-cell therapies for multiple myeloma, autologous T cells are harvested from the patient and reprogrammed to target multiple myeloma cells through the introduction of genes that encode CARs, which are fusion proteins coupling an antigen-recognition moiety and a transmembrane-spanning element to a T-cell activation domain (typically CD3 zeta [CD247]). The T cells are then expanded and reinfused to the patient following a lymphodepletion regimen. Five strategies using autologous CAR T cells are currently approved for diffuse large B-cell lymphomas, acute lymphoblastic leukemia, multiple myeloma, and other hematologic malignancies. Notably, in patients with heavily pretreated multiple myeloma, CAR T cells have demonstrated impressive activity.
BCMA-targeting CAR T cells
The B-cell maturation antigen (BCMA; TNFRSF17), which plays an important role in the survival of long-lived plasma cells in bone marrow, is an attractive target for CAR T-cell therapy because it is expressed on normal and malignant plasma cell surfaces and by mature B cells. When ligands (TNFSF 13B/TNFSF13) bind to BCMA expressed on multiple myeloma cell surfaces, survival and proliferation pathways and drug resistance are activated.
High-quality responses have been demonstrated in several trials of anti-BCMA CAR T cells, which kill multiple myeloma cell lines and primary multiple myeloma cells through degranulation of T cells and lysis of tumor cells, even those with low BCMA expression. Based on efficacy in triple-class exposed multiple myeloma that compared favorably to conventional care with improved health-related quality of life, the U.S. Food and Drug Administration gave breakthrough designation to ciltacabtagene autoleucel in December 2019 and approval for idecabtagene vicleucel in March 2021.
Idecabtagene vicleucel
Idecabtagene vicleucel expresses a murine BCMA-targeting single-chain variable fragment with a 4-1BB costimulatory motif. The phase 2 KarMMa study2 evaluated idecabtagene vicleucel (target dose of 450 × 106 CAR T cells; range 150 × 106 to 450 × 106) activity in 128 patients with triple-class exposed multiple myeloma. Partial responses or better were observed in 94 of 128 patients (73%) (95% confidence interval, 66-81); 42 (33%) had a complete response or better (95% CI, 25-41), with a median progression-free survival of 8.8 months (95% CI, 5.6-11.6). Outcomes were improved in the highest fixed-dose group, with partial response or better in 81% (44 of 55), complete response or better in 39% (21), and median overall survival of 12.1 months (95% CI, 8.8-12.3). Patients with high-risk cytogenetic profiles, extramedullary disease, and high tumor burden also had deep and durable responses. Outcomes were less favorable in patients with revised International Staging System stage 3 disease.
Ciltacabtagene autoleucel
Ciltacabtagene autoleucel, a 4-1BB–based CAR T-cell therapy with two BCMA-targeting domains, confers high-avidity binding. In the phase 1b/2 CARTITUDE-1 study, conducted in the United States and Europe, preliminary results in 97 patients showed a 97% response rate with ciltacabtagene autoleucel (target dose 0.75 × 106 CAR T cells per kg), and in 65 patients, a complete response (67%). Progression-free survival at 12 months was 77% (95% CI, 66-84) and overall survival was 89% (95% CI, 80-94).3
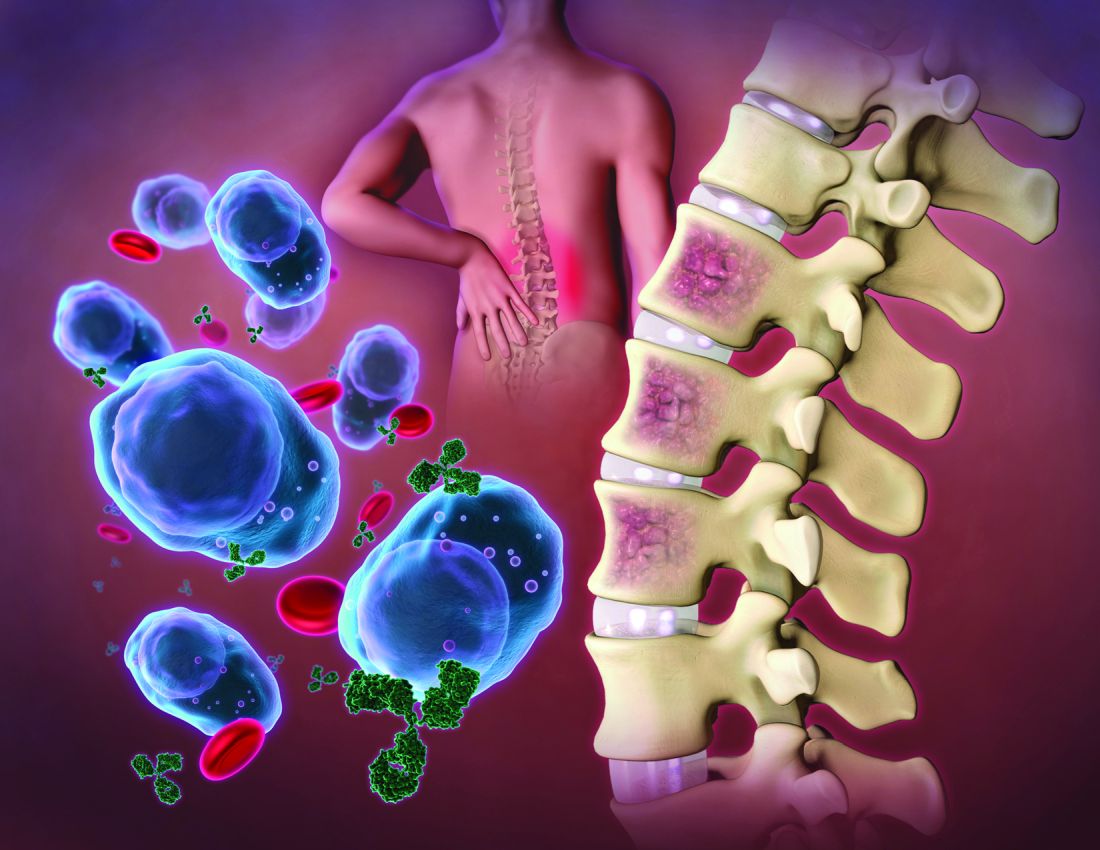
In the phase 1 LEGEND-2 study4 that was conducted at four sites in China among less heavily pretreated multiple myeloma patients, while all used the same CAR construct, sites used variable conditioning regimens (split versus single). In the site using cyclophosphamide as the lymphodepletion therapy and three split CAR T-cell infusions, partial response or better was achieved in 50 patients (88%) with a median of three prior therapy lines. The complete response rate was high (74%) and minimal residual disease negativity was reached in 39 patients (68%). Median progression-free survival was 19.9 months (95% CI, 9.6-31.0), but 28.2 months among those with complete responses (95% CI, 19.9-not estimable). Median overall survival was also favorable at 36.1 months (95% CI, 26.4-not estimable); it was 35.0 months-not estimable among patients with complete responses. Results from the other three sites were comparable.
Noteworthy among other BCMA-targeting CAR T-cell products in earlier stages of clinical development is orvacabtagene autoleucel, which has a fully human BCMA-specific binding domain. At higher doses (300 × 106 to 600 × 106 CAR T cells) among 62 patients with triple-class–exposed multiple myeloma in the EVOLVE trial, 92% had a partial or better response, with complete responses or better in 36%, all with an encouraging safety profile.
BCMA-targeting CAR T cell toxicity
While van de Donk, Usmani, and Yong, in their review1 note a lack of evidence of off-target toxicity with BCMA-targeting CAR T-cell therapy in clinical studies so far, they do point to several clinical syndromes (cytokine release syndrome, infections, respiratory failure, neurotoxicity, pulmonary aspergillosis, gastrointestinal hemorrhage) caused by cytokines produced during CAR T-cell expansion and to cytopenias and infections arising from prior treatment, bridging therapy, and lymphodepleting conditioning. Deaths attributed to treatment in the above-mentioned trials underscore the need for careful monitoring and early intervention.
Cytokine release syndrome
In the BCMA-targeting CAR T-cell therapy studies, the frequency of cytokine release syndrome varies widely from 17% to 95% but is generally attributed to CAR T-cell activation and is associated with increased serum ferritin concentrations, high c-reactive proteins, and proinflammatory cytokines. High tumor load, in multiple myeloma patients receiving CD19-targeting CAR T cells, was associated with a higher incidence of severe cytokine release syndrome. In a small number of patients, macrophage activation syndrome and hemophagocytic lymphohistiocytosis, the most aggressive variants of cytokine release syndrome, are caused by severe immune activation and lead to multiorgan dysfunction.
Neurotoxicity
Immune effector cell–-associated neurotoxicity syndrome (ICANS) symptoms, in multiple myeloma patients treated with BCMA-targeting CAR T cells, may include delirium, transient confusion, aphasia, lethargy, tremor, dysgraphia, seizures, cerebral edema, and rarely, posterior reversible encephalopathy syndrome.1 While the pathophysiology of CAR T cell–related neurotoxicity is not well understood, high tumor load, higher peak concentrations of CAR T cells, and more severe cytokine release syndrome are more common in patients with severe neurotoxicity. “The frequency of neurotoxicities,” Dr. Yong noted in an interview, “has been reduced by steps taken to mitigate these risk factors.”
High interest in phase I study
A phase I study presented in Blood has attracted interest because the novel BCMA-targeting CAR agent (CT103A) being tested is fully human.4 In an accompanying editorial, Lee and Yong note that doubt for any real potential for durable CAR T therapy responses in multiple myeloma is raised by the poor persistence of multiple myeloma CAR T cells in multiple myeloma patients.3
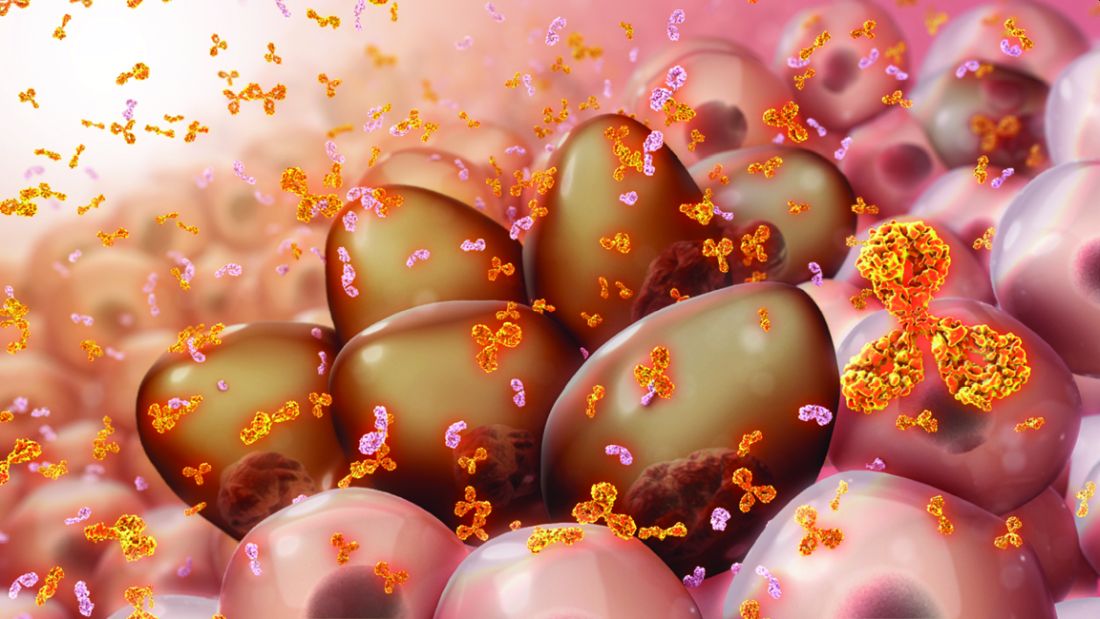
In the earliest trials of BCMA CARs, while reported rates of objective antimyeloma responses were in the approximately 33%-88% range among patients with relapsed/refractory multiple myeloma (RRMM), persistence was typically 6 months or less. Lee and Yong point out, however, that while correlation between persistence and duration of response (DOR) has been variable, median persistence was 308 days in the phase I study. Wang and colleagues, the phase I study authors, state that levels of CAR T-cell proliferation and duration of cellular persistence may be determinants of DOR in CAR T therapy for multiple myeloma. They observe that the multiple mechanisms potentially responsible for the inability of some CAR T cells to survive in vivo, may include antigen escape, T-cell intrinsic mechanisms, tumor microenvironment–mediated suppression, and host anti-CAR immunity. CARs with humanized or fully human single-chain variable fragments (scFvs), prior studies suggest, may retain antitumor activity through bypassing potential host anti-CAR immunogenicity.
In the study, CT103A, a fully human scFv, was tested in an open-label, single-arm design for safety and preliminary efficacy in 18 patients (8 female; median age 53.5 years) with RRMM (at least three lines of prior therapies including a proteasome inhibitor and an immunomodulatory agent) who had undergone leukapheresis and had received lymphodepletion chemotherapy with fludarabine and cyclophosphamide. Four patients (22.2%) had been treated previously with murine anti-BCMA CAR T cells. Safety and tolerability (including dose-limiting toxicity) were the primary endpoints, with efficacy and pharmacokinetics secondary.
Rapid responses
Two weeks after infusion, the overall response rate (ORR) was 77.8% (14 of 18) and by 1 month it was 88.9% (16 of 18). Eventually, all responded and 72.2% (13 of 18) achieved a complete response (CR) or stringent complete response (sCR). All 17 patients evaluated for minimum residual disease (MRD) in bone marrow were MRD-negative at 10-4 nucleated cells by flow cytometry within 1 month. Median DOR was 325 days (range, 7-573 days) for all patients and 412 days (range, 213-573 days) for the 13 with CR/sCR. CAR transgenes were detectable at the cutoff date in 77.8% of patients, with a median CAR transgene persistence of 307.5 days.
During follow-up, four deaths were reported, including one patient with persistent sCR (sudden severe infection). Progression-free survival (PFS) and overall survival (OS) rates at 1 year were 58.3% and 75%, respectively. Extramedullary myeloma was associated with a shortened PFS (79.1% versus 20.0%, P = .015), but not OS (79.1% versus 60.0%, P = .328) at 1 year.
All patients experienced grade 3 or higher adverse events, most of which were expected hematologic effects of lymphodepleting chemotherapy and CT103A infusions. Grade 1 and 2 cytokine release syndromes occurred in 70.6% patients (17 of 18), with 1 grade 4 event (5.9%). The patients receiving a dose of up to 3.0 × 106 CAR+ T cells/kg required less treatment of cytokine release syndrome than the patients who received a dose of 6.0 × 106 CAR+ T cells/kg. No immune effector cell–associated neurotoxicity syndrome was observed. Antidrug antibody positivity occurred in only 1 patient.
Two characteristics of CT103A may contribute to its long persistence, stated study senior author Jianfeng Zhou, MD, PhD, chairman and professor of the department of hematology, Tongji Hospital in Wuhan, China. “One is the reduced immunogenicity achieved by the fully human construct; another is the relatively low binding affinity of the CAR binder. Notably, four patients who previously received murine BCMA CAR were included and still benefit from CT103A. It demonstrates the possibility of retreatment with a different CAR.” Dr. Zhou also emphasized that the lack of ICANS in the entire cohort reflects the excellent safety profile of CT103A.
The editorial commentary in Blood by Lydia Sarah Hui Lee, MD, and Kwee L. Yong, PhD, underscored impressive responses to CT103A, specifically to the median time to response of 15 days, the 100% ORR, and the not reached median progression-free survival at 394 days).5 The best results in other published nonhuman BCMA CAR T-cell trials, they note, were about 1 month (time to response), approximately 33%-88% (ORR), and median progression-free survival of 7-15 months.
Immune responses, Dr. Yong said in an interview, can guide subsequent treatment. “For example, if a patient previously exposed to BCMA CAR T cells in which the construct is either chimeric or humanized, but retains some murine elements, and had detectable antimurine antibodies, we may aim for a fully human one if we are considering treating with a different BCMA CAR T-cell product.” She added, “On the other hand, a similar patient whose serum did not contain such antibodies may be a candidate for a humanized product that retained some murine elements.”
Wang and colleagues concluded, “Altogether, CT103A is safe and highly active in patients with relapsed/refractory multiple myeloma and can be developed as a promising therapy for relapsed/refractory multiple myeloma.”4 An ongoing multicenter phase II trial with single-arm design is recruiting 100 patients. The infusion dosage, suggested by the phase I trial, is 1 × 106 cells/kg. Endpoints include efficacy and safety.
Improving CAR T
Optimizing CAR design and adapting manufacturing processes to generate cell products enriched for T-cell subsets, such as early memory cells, are among strategies being explored to improve CAR T effectiveness.1 Also, dual-antigen targeting to interdict antigen escape and rational combination treatments to enhance persistence are under investigation, along with efforts to improve CAR T-cell therapy safety (for example, incorporation of a suicide gene safety system). They note further that several groups are researching use of induced pluripotent stem cells to generate large quantities of off-the-shelf CAR T-cell immunotherapies that would circumvent the complex, costly, and time-consuming process of manufacturing patient-specific autologous CAR T cells.
References
1. van de Donk N et al. Lancet Haematol. 2021 June;8(6):e446-61.
2. Munshi NC et al. N Engl J Med 2021; 384:705-716.
3. Berdeja JG et al. The Lancet. 2021 July; 398:314-24.
4. Wang D et al. Blood. 2021 May;137(21):2890-901.
5. Lee L and Yong K. Blood. 2021 May;137(21):2859-60.
In multiple myeloma, survival has been very significantly improved by immunomodulatory drugs, proteasome inhibitors, and CD38-targeting antibodies. Despite these advances, multiple myeloma, which is characterized by malignant proliferation of clonal plasma cells in bone marrow, remains an incurable plasma cell disorder with near-certain relapse after successful treatment. Prognosis for patients who develop triple-class refractory disease is poor, with less than 1-year survival. The substantial unmet therapeutic need extends further to other poor survival multiple myeloma populations that include newly diagnosed patients with high cytogenic risk profiles and those with early relapse after first-line therapy. For all of these, interest in drugs with novel mechanisms of action is naturally high.
More specific, less toxic
Post allogeneic hematopoietic stem-cell transplantation and donor lymphocyte infusion sustained remissions reflect a graft-versus-myeloma effect mediated by donor T cells.1 The substantial morbidity and mortality associated with graft-versus-host disease and opportunistic infections, however, have spurred searches for alternative, more specific, and less toxic T-cell therapies with stronger antitumor activity.
Chimeric antigen receptors (CARs)
In CAR T-cell therapies for multiple myeloma, autologous T cells are harvested from the patient and reprogrammed to target multiple myeloma cells through the introduction of genes that encode CARs, which are fusion proteins coupling an antigen-recognition moiety and a transmembrane-spanning element to a T-cell activation domain (typically CD3 zeta [CD247]). The T cells are then expanded and reinfused to the patient following a lymphodepletion regimen. Five strategies using autologous CAR T cells are currently approved for diffuse large B-cell lymphomas, acute lymphoblastic leukemia, multiple myeloma, and other hematologic malignancies. Notably, in patients with heavily pretreated multiple myeloma, CAR T cells have demonstrated impressive activity.
BCMA-targeting CAR T cells
The B-cell maturation antigen (BCMA; TNFRSF17), which plays an important role in the survival of long-lived plasma cells in bone marrow, is an attractive target for CAR T-cell therapy because it is expressed on normal and malignant plasma cell surfaces and by mature B cells. When ligands (TNFSF 13B/TNFSF13) bind to BCMA expressed on multiple myeloma cell surfaces, survival and proliferation pathways and drug resistance are activated.
High-quality responses have been demonstrated in several trials of anti-BCMA CAR T cells, which kill multiple myeloma cell lines and primary multiple myeloma cells through degranulation of T cells and lysis of tumor cells, even those with low BCMA expression. Based on efficacy in triple-class exposed multiple myeloma that compared favorably to conventional care with improved health-related quality of life, the U.S. Food and Drug Administration gave breakthrough designation to ciltacabtagene autoleucel in December 2019 and approval for idecabtagene vicleucel in March 2021.
Idecabtagene vicleucel
Idecabtagene vicleucel expresses a murine BCMA-targeting single-chain variable fragment with a 4-1BB costimulatory motif. The phase 2 KarMMa study2 evaluated idecabtagene vicleucel (target dose of 450 × 106 CAR T cells; range 150 × 106 to 450 × 106) activity in 128 patients with triple-class exposed multiple myeloma. Partial responses or better were observed in 94 of 128 patients (73%) (95% confidence interval, 66-81); 42 (33%) had a complete response or better (95% CI, 25-41), with a median progression-free survival of 8.8 months (95% CI, 5.6-11.6). Outcomes were improved in the highest fixed-dose group, with partial response or better in 81% (44 of 55), complete response or better in 39% (21), and median overall survival of 12.1 months (95% CI, 8.8-12.3). Patients with high-risk cytogenetic profiles, extramedullary disease, and high tumor burden also had deep and durable responses. Outcomes were less favorable in patients with revised International Staging System stage 3 disease.
Ciltacabtagene autoleucel
Ciltacabtagene autoleucel, a 4-1BB–based CAR T-cell therapy with two BCMA-targeting domains, confers high-avidity binding. In the phase 1b/2 CARTITUDE-1 study, conducted in the United States and Europe, preliminary results in 97 patients showed a 97% response rate with ciltacabtagene autoleucel (target dose 0.75 × 106 CAR T cells per kg), and in 65 patients, a complete response (67%). Progression-free survival at 12 months was 77% (95% CI, 66-84) and overall survival was 89% (95% CI, 80-94).3
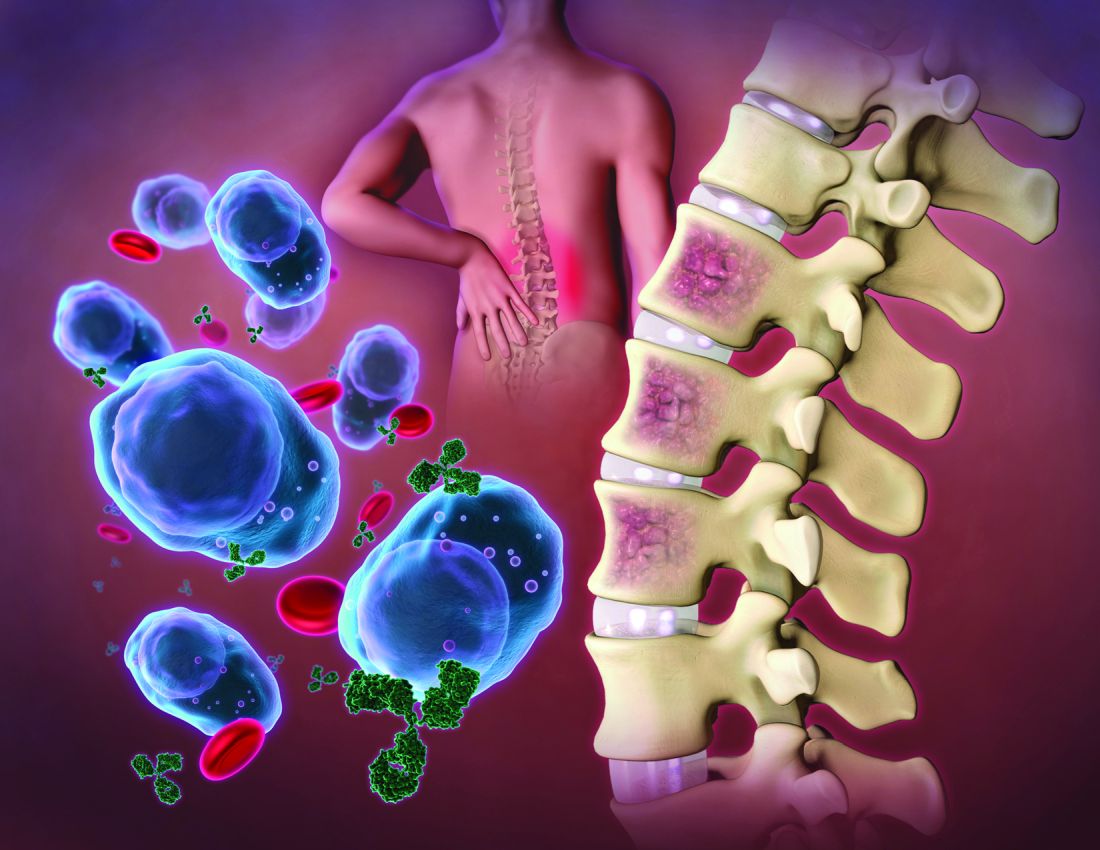
In the phase 1 LEGEND-2 study4 that was conducted at four sites in China among less heavily pretreated multiple myeloma patients, while all used the same CAR construct, sites used variable conditioning regimens (split versus single). In the site using cyclophosphamide as the lymphodepletion therapy and three split CAR T-cell infusions, partial response or better was achieved in 50 patients (88%) with a median of three prior therapy lines. The complete response rate was high (74%) and minimal residual disease negativity was reached in 39 patients (68%). Median progression-free survival was 19.9 months (95% CI, 9.6-31.0), but 28.2 months among those with complete responses (95% CI, 19.9-not estimable). Median overall survival was also favorable at 36.1 months (95% CI, 26.4-not estimable); it was 35.0 months-not estimable among patients with complete responses. Results from the other three sites were comparable.
Noteworthy among other BCMA-targeting CAR T-cell products in earlier stages of clinical development is orvacabtagene autoleucel, which has a fully human BCMA-specific binding domain. At higher doses (300 × 106 to 600 × 106 CAR T cells) among 62 patients with triple-class–exposed multiple myeloma in the EVOLVE trial, 92% had a partial or better response, with complete responses or better in 36%, all with an encouraging safety profile.
BCMA-targeting CAR T cell toxicity
While van de Donk, Usmani, and Yong, in their review1 note a lack of evidence of off-target toxicity with BCMA-targeting CAR T-cell therapy in clinical studies so far, they do point to several clinical syndromes (cytokine release syndrome, infections, respiratory failure, neurotoxicity, pulmonary aspergillosis, gastrointestinal hemorrhage) caused by cytokines produced during CAR T-cell expansion and to cytopenias and infections arising from prior treatment, bridging therapy, and lymphodepleting conditioning. Deaths attributed to treatment in the above-mentioned trials underscore the need for careful monitoring and early intervention.
Cytokine release syndrome
In the BCMA-targeting CAR T-cell therapy studies, the frequency of cytokine release syndrome varies widely from 17% to 95% but is generally attributed to CAR T-cell activation and is associated with increased serum ferritin concentrations, high c-reactive proteins, and proinflammatory cytokines. High tumor load, in multiple myeloma patients receiving CD19-targeting CAR T cells, was associated with a higher incidence of severe cytokine release syndrome. In a small number of patients, macrophage activation syndrome and hemophagocytic lymphohistiocytosis, the most aggressive variants of cytokine release syndrome, are caused by severe immune activation and lead to multiorgan dysfunction.
Neurotoxicity
Immune effector cell–-associated neurotoxicity syndrome (ICANS) symptoms, in multiple myeloma patients treated with BCMA-targeting CAR T cells, may include delirium, transient confusion, aphasia, lethargy, tremor, dysgraphia, seizures, cerebral edema, and rarely, posterior reversible encephalopathy syndrome.1 While the pathophysiology of CAR T cell–related neurotoxicity is not well understood, high tumor load, higher peak concentrations of CAR T cells, and more severe cytokine release syndrome are more common in patients with severe neurotoxicity. “The frequency of neurotoxicities,” Dr. Yong noted in an interview, “has been reduced by steps taken to mitigate these risk factors.”
High interest in phase I study
A phase I study presented in Blood has attracted interest because the novel BCMA-targeting CAR agent (CT103A) being tested is fully human.4 In an accompanying editorial, Lee and Yong note that doubt for any real potential for durable CAR T therapy responses in multiple myeloma is raised by the poor persistence of multiple myeloma CAR T cells in multiple myeloma patients.3
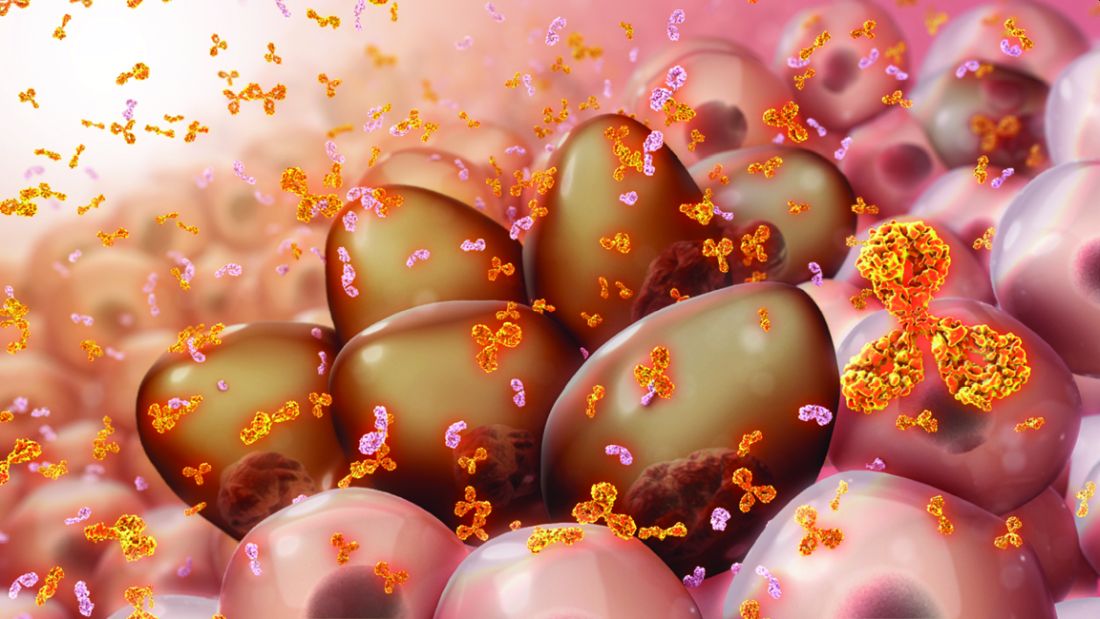
In the earliest trials of BCMA CARs, while reported rates of objective antimyeloma responses were in the approximately 33%-88% range among patients with relapsed/refractory multiple myeloma (RRMM), persistence was typically 6 months or less. Lee and Yong point out, however, that while correlation between persistence and duration of response (DOR) has been variable, median persistence was 308 days in the phase I study. Wang and colleagues, the phase I study authors, state that levels of CAR T-cell proliferation and duration of cellular persistence may be determinants of DOR in CAR T therapy for multiple myeloma. They observe that the multiple mechanisms potentially responsible for the inability of some CAR T cells to survive in vivo, may include antigen escape, T-cell intrinsic mechanisms, tumor microenvironment–mediated suppression, and host anti-CAR immunity. CARs with humanized or fully human single-chain variable fragments (scFvs), prior studies suggest, may retain antitumor activity through bypassing potential host anti-CAR immunogenicity.
In the study, CT103A, a fully human scFv, was tested in an open-label, single-arm design for safety and preliminary efficacy in 18 patients (8 female; median age 53.5 years) with RRMM (at least three lines of prior therapies including a proteasome inhibitor and an immunomodulatory agent) who had undergone leukapheresis and had received lymphodepletion chemotherapy with fludarabine and cyclophosphamide. Four patients (22.2%) had been treated previously with murine anti-BCMA CAR T cells. Safety and tolerability (including dose-limiting toxicity) were the primary endpoints, with efficacy and pharmacokinetics secondary.
Rapid responses
Two weeks after infusion, the overall response rate (ORR) was 77.8% (14 of 18) and by 1 month it was 88.9% (16 of 18). Eventually, all responded and 72.2% (13 of 18) achieved a complete response (CR) or stringent complete response (sCR). All 17 patients evaluated for minimum residual disease (MRD) in bone marrow were MRD-negative at 10-4 nucleated cells by flow cytometry within 1 month. Median DOR was 325 days (range, 7-573 days) for all patients and 412 days (range, 213-573 days) for the 13 with CR/sCR. CAR transgenes were detectable at the cutoff date in 77.8% of patients, with a median CAR transgene persistence of 307.5 days.
During follow-up, four deaths were reported, including one patient with persistent sCR (sudden severe infection). Progression-free survival (PFS) and overall survival (OS) rates at 1 year were 58.3% and 75%, respectively. Extramedullary myeloma was associated with a shortened PFS (79.1% versus 20.0%, P = .015), but not OS (79.1% versus 60.0%, P = .328) at 1 year.
All patients experienced grade 3 or higher adverse events, most of which were expected hematologic effects of lymphodepleting chemotherapy and CT103A infusions. Grade 1 and 2 cytokine release syndromes occurred in 70.6% patients (17 of 18), with 1 grade 4 event (5.9%). The patients receiving a dose of up to 3.0 × 106 CAR+ T cells/kg required less treatment of cytokine release syndrome than the patients who received a dose of 6.0 × 106 CAR+ T cells/kg. No immune effector cell–associated neurotoxicity syndrome was observed. Antidrug antibody positivity occurred in only 1 patient.
Two characteristics of CT103A may contribute to its long persistence, stated study senior author Jianfeng Zhou, MD, PhD, chairman and professor of the department of hematology, Tongji Hospital in Wuhan, China. “One is the reduced immunogenicity achieved by the fully human construct; another is the relatively low binding affinity of the CAR binder. Notably, four patients who previously received murine BCMA CAR were included and still benefit from CT103A. It demonstrates the possibility of retreatment with a different CAR.” Dr. Zhou also emphasized that the lack of ICANS in the entire cohort reflects the excellent safety profile of CT103A.
The editorial commentary in Blood by Lydia Sarah Hui Lee, MD, and Kwee L. Yong, PhD, underscored impressive responses to CT103A, specifically to the median time to response of 15 days, the 100% ORR, and the not reached median progression-free survival at 394 days).5 The best results in other published nonhuman BCMA CAR T-cell trials, they note, were about 1 month (time to response), approximately 33%-88% (ORR), and median progression-free survival of 7-15 months.
Immune responses, Dr. Yong said in an interview, can guide subsequent treatment. “For example, if a patient previously exposed to BCMA CAR T cells in which the construct is either chimeric or humanized, but retains some murine elements, and had detectable antimurine antibodies, we may aim for a fully human one if we are considering treating with a different BCMA CAR T-cell product.” She added, “On the other hand, a similar patient whose serum did not contain such antibodies may be a candidate for a humanized product that retained some murine elements.”
Wang and colleagues concluded, “Altogether, CT103A is safe and highly active in patients with relapsed/refractory multiple myeloma and can be developed as a promising therapy for relapsed/refractory multiple myeloma.”4 An ongoing multicenter phase II trial with single-arm design is recruiting 100 patients. The infusion dosage, suggested by the phase I trial, is 1 × 106 cells/kg. Endpoints include efficacy and safety.
Improving CAR T
Optimizing CAR design and adapting manufacturing processes to generate cell products enriched for T-cell subsets, such as early memory cells, are among strategies being explored to improve CAR T effectiveness.1 Also, dual-antigen targeting to interdict antigen escape and rational combination treatments to enhance persistence are under investigation, along with efforts to improve CAR T-cell therapy safety (for example, incorporation of a suicide gene safety system). They note further that several groups are researching use of induced pluripotent stem cells to generate large quantities of off-the-shelf CAR T-cell immunotherapies that would circumvent the complex, costly, and time-consuming process of manufacturing patient-specific autologous CAR T cells.
References
1. van de Donk N et al. Lancet Haematol. 2021 June;8(6):e446-61.
2. Munshi NC et al. N Engl J Med 2021; 384:705-716.
3. Berdeja JG et al. The Lancet. 2021 July; 398:314-24.
4. Wang D et al. Blood. 2021 May;137(21):2890-901.
5. Lee L and Yong K. Blood. 2021 May;137(21):2859-60.
Mesothelioma trials: Moving toward improved survival
Although mesothelioma continues to be a very difficult disease to treat and one with a poor prognosis, new and emerging therapeutic developments hold the promise of extending survival for appropriately selected patients.
Following years of little to no movement, encouraging advances in treatment have been seen on the immunotherapy front. Immune checkpoint inhibitors have demonstrated acceptable safety and promising efficacy in the treatment of unresectable malignant pleural mesothelioma (MPM), including an overall survival advantage over standard-of-care first-line chemotherapy. Beyond systemic therapy, the development of new radiation techniques to complement current, more conservative surgical approaches is likewise encouraging, though further randomized clinical trial data is awaited to determine the potential impact on survival.
Longer survival would be good news for the estimated 3,000 individuals diagnosed with MPM each year in the United States. Overall, the outlook for patients with this rare cancer remains unfavorable, with a 5-year survival rate of about 11%, according to data from the U.S. Surveillance, Epidemiology and End Results (SEER) Program.
One factor underlying that grim survival statistic is a relative lack of investment in the development of drugs specific to rare cancers, as compared to more common malignancies, said Anne S. Tsao, MD, professor and director of the mesothelioma program at the University of Texas MD Anderson Cancer Center in Houston.
On the plus side, the wave of research for more common cancers has yielded a number of agents, including the immune checkpoint inhibitors such as nivolumab, ipilimumab, pembrolizumab, and durvalumab, that hold promise in rare tumor types as well.
“I think that mesothelioma has benefited from that, because these all are agents that have been developed for other solid tumors that are then brought into mesothelioma,” Dr. Tsao said in an interview. “So there’s always a lag time, but nevertheless, of course we are thrilled that we have additional treatment options for these patients.”
Checkpoint inhibitors
Multiple checkpoint inhibitors have received Food and Drug Administration approval for the treatment of non–small cell lung cancer (NSCLC) over the past few years. Because many mesothelioma doctors also treat NSCLC, bringing those agents into the mesothelioma sphere was not a very difficult jump, Dr. Tsao said.
Checkpoint inhibitors got a foothold in mesothelioma, much like in NSCLC, by demonstrating clear benefit in the salvage setting, according to Dr. Tsao.
Pembrolizumab, nivolumab, and avelumab were evaluated in phase 1b/2 clinical trials and real-world cohorts that demonstrated response rates of around 20%, median progression-free survival of 4 months, and median overall survival (OS) around 12 months in patients with previously treated MPM.
Although results of those early-stage studies had to be interpreted with caution, they nonetheless suggested a slight edge for these checkpoint inhibitors over historical data, according to the authors of a recent article in Cancer Treatment Reviews.1 On the basis of phase 1 and 2 data, current clinical practice guidelines from the National Comprehensive Cancer Network2 list pembrolizumab and the combination of nivolumab and ipilimumab as options for MPM patients who have received previous therapy. Phase 3 trials have also been launched, including PROMISE-meso, which is comparing pembrolizumab to single-agent chemotherapy in advanced, pretreated MPM3, and CONFIRM, which pits nivolumab against placebo in relapsed MPM.4
On the front lines
Encouraging results in previously treated MPM led to the evaluation of checkpoint inhibitors as first-line therapy. Notably, the FDA approved nivolumab given with ipilimumab for the treatment of patients with unresectable MPM in October 2020, making that combination the first immunotherapy regimen to receive an indication in this disease.
The FDA approval was based on prespecified interim analysis of CheckMate 743, a phase 3 study that included 605 patients randomly allocated to nivolumab plus ipilimumab or to placebo.
At the interim analysis, median OS was 18.1 months for nivolumab plus ipilimumab, versus just 14.1 months for placebo (hazard ratio, 0.74; 96.6% confidence interval, 0.60-0.91; P = 0.0020), according to results of the study published in the Lancet.5 The 2-year OS rate was 41% for the immunotherapy combination and 27% for placebo. Grade 3-4 treatment-related adverse events were seen in 30% of the immunotherapy-treated patients and 32% of the chemotherapy-treated patients.
The magnitude of nivolumab-ipilimumab benefit appeared to be largest among patients with non-epithelioid MPM subtypes (sarcomatoid and biphasic), owing to the inferior impact of chemotherapy in these patients, with a median OS of just 8.8 months, according to investigators.
That’s not to say that immunotherapy didn’t work for patients with epithelioid histology. The benefit of nivolumab-ipilimumab was consistent for non-epithelioid and epithelioid patient subsets, with median OS of 18.1 and 18.7 months, respectively, results of subgroup analysis showed.
According to Dr. Tsao, those results reflect the extremely poor prognosis and pressing need for effective therapy early in the course of treatment for patients with non-epithelioid histology.
“You have to get the most effective therapy into these patients as quickly as you can,” she explained. “If you can get the more effective treatment and early, then you’ll see a longer-term benefit for them.”
Role of the PD-L1 biomarker
Despite this progress, one key hurdle has been determining the role of the PD-L1 biomarker in mesothelioma. In NSCLC, PD-L1 is often used to determine which patients will benefit from immune checkpoint inhibitors. In mesothelioma, the correlations have been more elusive.
Among patients in the CheckMate 743 study treated with nivolumab plus ipilimumab, OS was not significantly different for those with PD-L1 expression levels of less than 1% and those with 1% or greater, investigators said. Moreover, PD-L1 expression wasn’t a stratification factor in the study.
“When looking at all of the studies, it appears that the checkpoint inhibitors can truly benefit a certain percentage of mesothelioma patients, but we can’t pick them out just yet,” Dr. Tsao said.
“So our recommendation is to offer [checkpoint inhibitor therapy] at some point in their treatment, whether it’s first, second, or third line,” she continued. “They can get some benefit, and even in those if you don’t get a great response, you can still get disease stabilization, which in and of itself can be highly beneficial.”
Future directions
Immune checkpoint inhibitor–based combination regimens and cellular therapy represent promising directions forward in MPM research. There are several notable phase 3 trials of checkpoint inhibitors plus chemotherapy and targeted therapy going forward, plus intriguing data emerging on the potential role of chimeric antigen receptor (CAR) T-cell therapy in this setting.
One phase 3 trial to watch is IND277, which is comparing pembrolizumab plus cisplatin/pemetrexed chemotherapy to cisplatin/pemetrexed alone; that trial has enrolled 520 participants and has an estimated primary completion date in July 2022, according to the ClinicalTrials.gov website. Another is BEAT-Meso, a comparison of atezolizumab plus bevacizumab and chemotherapy against bevacizumab and chemotherapy, which has an estimated enrollment of 400 participants and primary completion date of January 2024. A third trial of interest is DREAM3R, which compares durvalumab plus chemotherapy followed by durvalumab maintenance to standard chemotherapy followed by observation. That study should enroll 480 participants and has an estimated primary completion date of April 2025.
CAR T-cell therapy, while best known for its emerging role in the treatment of hematologic malignancies, may also have a place in mesothelioma therapy one day. In a recently published report, investigators described a first-in-human phase I study of a mesothelin-targeted CAR T-cell therapy given in combination with pembrolizumab. Among 18 MPM patients who received pembrolizumab safely, median OS from time of CAR T-cell infusion was 23.9 months and 1-year OS was 83%, according to investigators.6An OS of nearly 24 months is “very encouraging” and compares favorably with historical results with systemic therapy in this difficult-to-treat disease, said Jacques P. Fontaine, MD, a thoracic surgeon and section head of mesothelioma research and treatment center at Moffitt Cancer Center in Tampa, Fla.
“It’s huge, but you have to take into account that this [OS] is still less than 2 years,” Dr. Fontaine said in an interview. “There’s still a lot of work to be done.”
Radiotherapy making an IMPRINT
Meanwhile, new developments in the multimodality treatment of resectable MPM are progressing and have the potential to extend survival among patients who undergo lung-sparing surgery.
Less aggressive intervention is increasingly the preferred approach to surgery in this patient population. That shift is supported by studies showing that lung-sparing pleurectomy-decortication (P/D) resulted in less morbidity and potentially better survival outcomes than extrapleural pneumonectomy (EPP), according to Andreas Rimner, MD, associate attending physician and director of thoracic radiation oncology research at Memorial Sloan Kettering Cancer Center in New York.
However, it is more challenging to deliver radiotherapy safely in patients who have undergone P/D as compared with patients who have undergone EPP, according to Dr. Rimner.
“When there’s no lung in place [as in EPP], it’s pretty simple – you just treat the entire empty chest to kill any microscopic cells that may still be left behind,” he said in an interview. “But now we have a situation where both lungs are still in place, and they are very radiation sensitive, so that’s not an easy feat.”
Driven by the limitations of conventional radiation, Dr. Rimner and colleagues developed a novel technique known as hemithoracic intensity-modulated pleural radiation therapy (IMPRINT) that allows more precise application of radiotherapy.
In a phase 2 study published in 2016, IMPRINT was found to be safe, with an acceptable rate of radiation pneumonitis (30% grade 2 or 3), according to investigators.7
Subsequent studies have demonstrated encouraging clinical outcomes, including a 20.2-month median OS for IMPRINT versus 12.3 months for conventional adjuvant radiotherapy in a retrospective study of 209 patients who underwent P/D between 1975 and 2015.8 Those findings led to the development of a phase 3 trial known as NRG-LU006 that is evaluating P/D plus chemotherapy with or without adjuvant IMPRINT in an estimated 150 patients. The study has a primary endpoint of OS, and an estimated primary completion date in July 2025, according to ClinicalTrials.gov.
Dr. Rimner said he’s optimistic about the prospects of this study, particularly with recently published results of a phase 3 study in which Italian investigators demonstrated an OS benefit of IMPRINT over palliative radiation in patients with nonmetastatic MPM.9
“That’s more data and rationale that shows there is good reason to believe that we are adding something here with this radiation technique,” said Dr. Rimner.
Dr. Fontaine, the thoracic surgeon and mesothelioma research head at Moffitt Cancer Center, said he’s hoping to see a substantial impact of IMPRINT on disease-free survival (DFS) once results of NRG-LU006 are available.
“I think DFS plays a role that we’ve underestimated over the last few years for sure,” he said.
For a patient with MPM, a short DFS can be anxiety provoking and may have negative impacts on quality of life, even despite a long OS, he explained.
“In terms of your outlook on life, how many times you have to go see a doctor, and how you enjoy life, there’s a big difference between the two,” he said.
Dr. Tsao provided disclosures related to Ariad, AstraZeneca, BMS, Boehringer Ingelheim, Eli Lilly, EMD Serono, Epizyme, Genentech, Huron, Merck, Millennium, Novartis, Polaris, Roche, Seattle Genetics, SELLAS Life Sciences Group, and Takeda. Dr. Fontaine reported no relevant disclosures. Dr. Rimner reported disclosures related to Bristol-Myers Squibb, GE Healthcare, Varian Medical Systems, and Boehringer Ingelheim.
References
1. Parikh K et al. Cancer Treat Rev. 2021 Sept 1;99:102250.
2. National Comprehensive Cancer Network (NCCN) Guidelines. Malignant Pleural Mesothelioma. Version 2.2021, published 2021 Feb 16. Accessed 2021 Aug 30. https://www.nccn.org/professionals/physician_gls/pdf/mpm.pdf
3. Popat S et al. Ann Oncol. 2020;31(12):1734-45.
4. Fennell D et al. Journal of Thoracic Oncology. 2021 Mar 1;16(3):S62.
5. Baas P et al. [published correction appears in Lancet. 2021 Feb 20;397(10275):670]. Lancet. 2021 Jan 30;397(10272):375-86.
6. Adusumilli PS et al. Cancer Discov. 2021 Jul 15;candisc.0407.2021.
7. Rimner A et al. J Clin Oncol. 2016;34(23):2761-8.
8. Shaikh F et al. J Thorac Oncol. 2017;12(6):993-1000.
9. Trovo M et al. Int J Radiat Oncol Biol Phys. 2021;109(5):1368-76.
Although mesothelioma continues to be a very difficult disease to treat and one with a poor prognosis, new and emerging therapeutic developments hold the promise of extending survival for appropriately selected patients.
Following years of little to no movement, encouraging advances in treatment have been seen on the immunotherapy front. Immune checkpoint inhibitors have demonstrated acceptable safety and promising efficacy in the treatment of unresectable malignant pleural mesothelioma (MPM), including an overall survival advantage over standard-of-care first-line chemotherapy. Beyond systemic therapy, the development of new radiation techniques to complement current, more conservative surgical approaches is likewise encouraging, though further randomized clinical trial data is awaited to determine the potential impact on survival.
Longer survival would be good news for the estimated 3,000 individuals diagnosed with MPM each year in the United States. Overall, the outlook for patients with this rare cancer remains unfavorable, with a 5-year survival rate of about 11%, according to data from the U.S. Surveillance, Epidemiology and End Results (SEER) Program.
One factor underlying that grim survival statistic is a relative lack of investment in the development of drugs specific to rare cancers, as compared to more common malignancies, said Anne S. Tsao, MD, professor and director of the mesothelioma program at the University of Texas MD Anderson Cancer Center in Houston.
On the plus side, the wave of research for more common cancers has yielded a number of agents, including the immune checkpoint inhibitors such as nivolumab, ipilimumab, pembrolizumab, and durvalumab, that hold promise in rare tumor types as well.
“I think that mesothelioma has benefited from that, because these all are agents that have been developed for other solid tumors that are then brought into mesothelioma,” Dr. Tsao said in an interview. “So there’s always a lag time, but nevertheless, of course we are thrilled that we have additional treatment options for these patients.”
Checkpoint inhibitors
Multiple checkpoint inhibitors have received Food and Drug Administration approval for the treatment of non–small cell lung cancer (NSCLC) over the past few years. Because many mesothelioma doctors also treat NSCLC, bringing those agents into the mesothelioma sphere was not a very difficult jump, Dr. Tsao said.
Checkpoint inhibitors got a foothold in mesothelioma, much like in NSCLC, by demonstrating clear benefit in the salvage setting, according to Dr. Tsao.
Pembrolizumab, nivolumab, and avelumab were evaluated in phase 1b/2 clinical trials and real-world cohorts that demonstrated response rates of around 20%, median progression-free survival of 4 months, and median overall survival (OS) around 12 months in patients with previously treated MPM.
Although results of those early-stage studies had to be interpreted with caution, they nonetheless suggested a slight edge for these checkpoint inhibitors over historical data, according to the authors of a recent article in Cancer Treatment Reviews.1 On the basis of phase 1 and 2 data, current clinical practice guidelines from the National Comprehensive Cancer Network2 list pembrolizumab and the combination of nivolumab and ipilimumab as options for MPM patients who have received previous therapy. Phase 3 trials have also been launched, including PROMISE-meso, which is comparing pembrolizumab to single-agent chemotherapy in advanced, pretreated MPM3, and CONFIRM, which pits nivolumab against placebo in relapsed MPM.4
On the front lines
Encouraging results in previously treated MPM led to the evaluation of checkpoint inhibitors as first-line therapy. Notably, the FDA approved nivolumab given with ipilimumab for the treatment of patients with unresectable MPM in October 2020, making that combination the first immunotherapy regimen to receive an indication in this disease.
The FDA approval was based on prespecified interim analysis of CheckMate 743, a phase 3 study that included 605 patients randomly allocated to nivolumab plus ipilimumab or to placebo.
At the interim analysis, median OS was 18.1 months for nivolumab plus ipilimumab, versus just 14.1 months for placebo (hazard ratio, 0.74; 96.6% confidence interval, 0.60-0.91; P = 0.0020), according to results of the study published in the Lancet.5 The 2-year OS rate was 41% for the immunotherapy combination and 27% for placebo. Grade 3-4 treatment-related adverse events were seen in 30% of the immunotherapy-treated patients and 32% of the chemotherapy-treated patients.
The magnitude of nivolumab-ipilimumab benefit appeared to be largest among patients with non-epithelioid MPM subtypes (sarcomatoid and biphasic), owing to the inferior impact of chemotherapy in these patients, with a median OS of just 8.8 months, according to investigators.
That’s not to say that immunotherapy didn’t work for patients with epithelioid histology. The benefit of nivolumab-ipilimumab was consistent for non-epithelioid and epithelioid patient subsets, with median OS of 18.1 and 18.7 months, respectively, results of subgroup analysis showed.
According to Dr. Tsao, those results reflect the extremely poor prognosis and pressing need for effective therapy early in the course of treatment for patients with non-epithelioid histology.
“You have to get the most effective therapy into these patients as quickly as you can,” she explained. “If you can get the more effective treatment and early, then you’ll see a longer-term benefit for them.”
Role of the PD-L1 biomarker
Despite this progress, one key hurdle has been determining the role of the PD-L1 biomarker in mesothelioma. In NSCLC, PD-L1 is often used to determine which patients will benefit from immune checkpoint inhibitors. In mesothelioma, the correlations have been more elusive.
Among patients in the CheckMate 743 study treated with nivolumab plus ipilimumab, OS was not significantly different for those with PD-L1 expression levels of less than 1% and those with 1% or greater, investigators said. Moreover, PD-L1 expression wasn’t a stratification factor in the study.
“When looking at all of the studies, it appears that the checkpoint inhibitors can truly benefit a certain percentage of mesothelioma patients, but we can’t pick them out just yet,” Dr. Tsao said.
“So our recommendation is to offer [checkpoint inhibitor therapy] at some point in their treatment, whether it’s first, second, or third line,” she continued. “They can get some benefit, and even in those if you don’t get a great response, you can still get disease stabilization, which in and of itself can be highly beneficial.”
Future directions
Immune checkpoint inhibitor–based combination regimens and cellular therapy represent promising directions forward in MPM research. There are several notable phase 3 trials of checkpoint inhibitors plus chemotherapy and targeted therapy going forward, plus intriguing data emerging on the potential role of chimeric antigen receptor (CAR) T-cell therapy in this setting.
One phase 3 trial to watch is IND277, which is comparing pembrolizumab plus cisplatin/pemetrexed chemotherapy to cisplatin/pemetrexed alone; that trial has enrolled 520 participants and has an estimated primary completion date in July 2022, according to the ClinicalTrials.gov website. Another is BEAT-Meso, a comparison of atezolizumab plus bevacizumab and chemotherapy against bevacizumab and chemotherapy, which has an estimated enrollment of 400 participants and primary completion date of January 2024. A third trial of interest is DREAM3R, which compares durvalumab plus chemotherapy followed by durvalumab maintenance to standard chemotherapy followed by observation. That study should enroll 480 participants and has an estimated primary completion date of April 2025.
CAR T-cell therapy, while best known for its emerging role in the treatment of hematologic malignancies, may also have a place in mesothelioma therapy one day. In a recently published report, investigators described a first-in-human phase I study of a mesothelin-targeted CAR T-cell therapy given in combination with pembrolizumab. Among 18 MPM patients who received pembrolizumab safely, median OS from time of CAR T-cell infusion was 23.9 months and 1-year OS was 83%, according to investigators.6An OS of nearly 24 months is “very encouraging” and compares favorably with historical results with systemic therapy in this difficult-to-treat disease, said Jacques P. Fontaine, MD, a thoracic surgeon and section head of mesothelioma research and treatment center at Moffitt Cancer Center in Tampa, Fla.
“It’s huge, but you have to take into account that this [OS] is still less than 2 years,” Dr. Fontaine said in an interview. “There’s still a lot of work to be done.”
Radiotherapy making an IMPRINT
Meanwhile, new developments in the multimodality treatment of resectable MPM are progressing and have the potential to extend survival among patients who undergo lung-sparing surgery.
Less aggressive intervention is increasingly the preferred approach to surgery in this patient population. That shift is supported by studies showing that lung-sparing pleurectomy-decortication (P/D) resulted in less morbidity and potentially better survival outcomes than extrapleural pneumonectomy (EPP), according to Andreas Rimner, MD, associate attending physician and director of thoracic radiation oncology research at Memorial Sloan Kettering Cancer Center in New York.
However, it is more challenging to deliver radiotherapy safely in patients who have undergone P/D as compared with patients who have undergone EPP, according to Dr. Rimner.
“When there’s no lung in place [as in EPP], it’s pretty simple – you just treat the entire empty chest to kill any microscopic cells that may still be left behind,” he said in an interview. “But now we have a situation where both lungs are still in place, and they are very radiation sensitive, so that’s not an easy feat.”
Driven by the limitations of conventional radiation, Dr. Rimner and colleagues developed a novel technique known as hemithoracic intensity-modulated pleural radiation therapy (IMPRINT) that allows more precise application of radiotherapy.
In a phase 2 study published in 2016, IMPRINT was found to be safe, with an acceptable rate of radiation pneumonitis (30% grade 2 or 3), according to investigators.7
Subsequent studies have demonstrated encouraging clinical outcomes, including a 20.2-month median OS for IMPRINT versus 12.3 months for conventional adjuvant radiotherapy in a retrospective study of 209 patients who underwent P/D between 1975 and 2015.8 Those findings led to the development of a phase 3 trial known as NRG-LU006 that is evaluating P/D plus chemotherapy with or without adjuvant IMPRINT in an estimated 150 patients. The study has a primary endpoint of OS, and an estimated primary completion date in July 2025, according to ClinicalTrials.gov.
Dr. Rimner said he’s optimistic about the prospects of this study, particularly with recently published results of a phase 3 study in which Italian investigators demonstrated an OS benefit of IMPRINT over palliative radiation in patients with nonmetastatic MPM.9
“That’s more data and rationale that shows there is good reason to believe that we are adding something here with this radiation technique,” said Dr. Rimner.
Dr. Fontaine, the thoracic surgeon and mesothelioma research head at Moffitt Cancer Center, said he’s hoping to see a substantial impact of IMPRINT on disease-free survival (DFS) once results of NRG-LU006 are available.
“I think DFS plays a role that we’ve underestimated over the last few years for sure,” he said.
For a patient with MPM, a short DFS can be anxiety provoking and may have negative impacts on quality of life, even despite a long OS, he explained.
“In terms of your outlook on life, how many times you have to go see a doctor, and how you enjoy life, there’s a big difference between the two,” he said.
Dr. Tsao provided disclosures related to Ariad, AstraZeneca, BMS, Boehringer Ingelheim, Eli Lilly, EMD Serono, Epizyme, Genentech, Huron, Merck, Millennium, Novartis, Polaris, Roche, Seattle Genetics, SELLAS Life Sciences Group, and Takeda. Dr. Fontaine reported no relevant disclosures. Dr. Rimner reported disclosures related to Bristol-Myers Squibb, GE Healthcare, Varian Medical Systems, and Boehringer Ingelheim.
References
1. Parikh K et al. Cancer Treat Rev. 2021 Sept 1;99:102250.
2. National Comprehensive Cancer Network (NCCN) Guidelines. Malignant Pleural Mesothelioma. Version 2.2021, published 2021 Feb 16. Accessed 2021 Aug 30. https://www.nccn.org/professionals/physician_gls/pdf/mpm.pdf
3. Popat S et al. Ann Oncol. 2020;31(12):1734-45.
4. Fennell D et al. Journal of Thoracic Oncology. 2021 Mar 1;16(3):S62.
5. Baas P et al. [published correction appears in Lancet. 2021 Feb 20;397(10275):670]. Lancet. 2021 Jan 30;397(10272):375-86.
6. Adusumilli PS et al. Cancer Discov. 2021 Jul 15;candisc.0407.2021.
7. Rimner A et al. J Clin Oncol. 2016;34(23):2761-8.
8. Shaikh F et al. J Thorac Oncol. 2017;12(6):993-1000.
9. Trovo M et al. Int J Radiat Oncol Biol Phys. 2021;109(5):1368-76.
Although mesothelioma continues to be a very difficult disease to treat and one with a poor prognosis, new and emerging therapeutic developments hold the promise of extending survival for appropriately selected patients.
Following years of little to no movement, encouraging advances in treatment have been seen on the immunotherapy front. Immune checkpoint inhibitors have demonstrated acceptable safety and promising efficacy in the treatment of unresectable malignant pleural mesothelioma (MPM), including an overall survival advantage over standard-of-care first-line chemotherapy. Beyond systemic therapy, the development of new radiation techniques to complement current, more conservative surgical approaches is likewise encouraging, though further randomized clinical trial data is awaited to determine the potential impact on survival.
Longer survival would be good news for the estimated 3,000 individuals diagnosed with MPM each year in the United States. Overall, the outlook for patients with this rare cancer remains unfavorable, with a 5-year survival rate of about 11%, according to data from the U.S. Surveillance, Epidemiology and End Results (SEER) Program.
One factor underlying that grim survival statistic is a relative lack of investment in the development of drugs specific to rare cancers, as compared to more common malignancies, said Anne S. Tsao, MD, professor and director of the mesothelioma program at the University of Texas MD Anderson Cancer Center in Houston.
On the plus side, the wave of research for more common cancers has yielded a number of agents, including the immune checkpoint inhibitors such as nivolumab, ipilimumab, pembrolizumab, and durvalumab, that hold promise in rare tumor types as well.
“I think that mesothelioma has benefited from that, because these all are agents that have been developed for other solid tumors that are then brought into mesothelioma,” Dr. Tsao said in an interview. “So there’s always a lag time, but nevertheless, of course we are thrilled that we have additional treatment options for these patients.”
Checkpoint inhibitors
Multiple checkpoint inhibitors have received Food and Drug Administration approval for the treatment of non–small cell lung cancer (NSCLC) over the past few years. Because many mesothelioma doctors also treat NSCLC, bringing those agents into the mesothelioma sphere was not a very difficult jump, Dr. Tsao said.
Checkpoint inhibitors got a foothold in mesothelioma, much like in NSCLC, by demonstrating clear benefit in the salvage setting, according to Dr. Tsao.
Pembrolizumab, nivolumab, and avelumab were evaluated in phase 1b/2 clinical trials and real-world cohorts that demonstrated response rates of around 20%, median progression-free survival of 4 months, and median overall survival (OS) around 12 months in patients with previously treated MPM.
Although results of those early-stage studies had to be interpreted with caution, they nonetheless suggested a slight edge for these checkpoint inhibitors over historical data, according to the authors of a recent article in Cancer Treatment Reviews.1 On the basis of phase 1 and 2 data, current clinical practice guidelines from the National Comprehensive Cancer Network2 list pembrolizumab and the combination of nivolumab and ipilimumab as options for MPM patients who have received previous therapy. Phase 3 trials have also been launched, including PROMISE-meso, which is comparing pembrolizumab to single-agent chemotherapy in advanced, pretreated MPM3, and CONFIRM, which pits nivolumab against placebo in relapsed MPM.4
On the front lines
Encouraging results in previously treated MPM led to the evaluation of checkpoint inhibitors as first-line therapy. Notably, the FDA approved nivolumab given with ipilimumab for the treatment of patients with unresectable MPM in October 2020, making that combination the first immunotherapy regimen to receive an indication in this disease.
The FDA approval was based on prespecified interim analysis of CheckMate 743, a phase 3 study that included 605 patients randomly allocated to nivolumab plus ipilimumab or to placebo.
At the interim analysis, median OS was 18.1 months for nivolumab plus ipilimumab, versus just 14.1 months for placebo (hazard ratio, 0.74; 96.6% confidence interval, 0.60-0.91; P = 0.0020), according to results of the study published in the Lancet.5 The 2-year OS rate was 41% for the immunotherapy combination and 27% for placebo. Grade 3-4 treatment-related adverse events were seen in 30% of the immunotherapy-treated patients and 32% of the chemotherapy-treated patients.
The magnitude of nivolumab-ipilimumab benefit appeared to be largest among patients with non-epithelioid MPM subtypes (sarcomatoid and biphasic), owing to the inferior impact of chemotherapy in these patients, with a median OS of just 8.8 months, according to investigators.
That’s not to say that immunotherapy didn’t work for patients with epithelioid histology. The benefit of nivolumab-ipilimumab was consistent for non-epithelioid and epithelioid patient subsets, with median OS of 18.1 and 18.7 months, respectively, results of subgroup analysis showed.
According to Dr. Tsao, those results reflect the extremely poor prognosis and pressing need for effective therapy early in the course of treatment for patients with non-epithelioid histology.
“You have to get the most effective therapy into these patients as quickly as you can,” she explained. “If you can get the more effective treatment and early, then you’ll see a longer-term benefit for them.”
Role of the PD-L1 biomarker
Despite this progress, one key hurdle has been determining the role of the PD-L1 biomarker in mesothelioma. In NSCLC, PD-L1 is often used to determine which patients will benefit from immune checkpoint inhibitors. In mesothelioma, the correlations have been more elusive.
Among patients in the CheckMate 743 study treated with nivolumab plus ipilimumab, OS was not significantly different for those with PD-L1 expression levels of less than 1% and those with 1% or greater, investigators said. Moreover, PD-L1 expression wasn’t a stratification factor in the study.
“When looking at all of the studies, it appears that the checkpoint inhibitors can truly benefit a certain percentage of mesothelioma patients, but we can’t pick them out just yet,” Dr. Tsao said.
“So our recommendation is to offer [checkpoint inhibitor therapy] at some point in their treatment, whether it’s first, second, or third line,” she continued. “They can get some benefit, and even in those if you don’t get a great response, you can still get disease stabilization, which in and of itself can be highly beneficial.”
Future directions
Immune checkpoint inhibitor–based combination regimens and cellular therapy represent promising directions forward in MPM research. There are several notable phase 3 trials of checkpoint inhibitors plus chemotherapy and targeted therapy going forward, plus intriguing data emerging on the potential role of chimeric antigen receptor (CAR) T-cell therapy in this setting.
One phase 3 trial to watch is IND277, which is comparing pembrolizumab plus cisplatin/pemetrexed chemotherapy to cisplatin/pemetrexed alone; that trial has enrolled 520 participants and has an estimated primary completion date in July 2022, according to the ClinicalTrials.gov website. Another is BEAT-Meso, a comparison of atezolizumab plus bevacizumab and chemotherapy against bevacizumab and chemotherapy, which has an estimated enrollment of 400 participants and primary completion date of January 2024. A third trial of interest is DREAM3R, which compares durvalumab plus chemotherapy followed by durvalumab maintenance to standard chemotherapy followed by observation. That study should enroll 480 participants and has an estimated primary completion date of April 2025.
CAR T-cell therapy, while best known for its emerging role in the treatment of hematologic malignancies, may also have a place in mesothelioma therapy one day. In a recently published report, investigators described a first-in-human phase I study of a mesothelin-targeted CAR T-cell therapy given in combination with pembrolizumab. Among 18 MPM patients who received pembrolizumab safely, median OS from time of CAR T-cell infusion was 23.9 months and 1-year OS was 83%, according to investigators.6An OS of nearly 24 months is “very encouraging” and compares favorably with historical results with systemic therapy in this difficult-to-treat disease, said Jacques P. Fontaine, MD, a thoracic surgeon and section head of mesothelioma research and treatment center at Moffitt Cancer Center in Tampa, Fla.
“It’s huge, but you have to take into account that this [OS] is still less than 2 years,” Dr. Fontaine said in an interview. “There’s still a lot of work to be done.”
Radiotherapy making an IMPRINT
Meanwhile, new developments in the multimodality treatment of resectable MPM are progressing and have the potential to extend survival among patients who undergo lung-sparing surgery.
Less aggressive intervention is increasingly the preferred approach to surgery in this patient population. That shift is supported by studies showing that lung-sparing pleurectomy-decortication (P/D) resulted in less morbidity and potentially better survival outcomes than extrapleural pneumonectomy (EPP), according to Andreas Rimner, MD, associate attending physician and director of thoracic radiation oncology research at Memorial Sloan Kettering Cancer Center in New York.
However, it is more challenging to deliver radiotherapy safely in patients who have undergone P/D as compared with patients who have undergone EPP, according to Dr. Rimner.
“When there’s no lung in place [as in EPP], it’s pretty simple – you just treat the entire empty chest to kill any microscopic cells that may still be left behind,” he said in an interview. “But now we have a situation where both lungs are still in place, and they are very radiation sensitive, so that’s not an easy feat.”
Driven by the limitations of conventional radiation, Dr. Rimner and colleagues developed a novel technique known as hemithoracic intensity-modulated pleural radiation therapy (IMPRINT) that allows more precise application of radiotherapy.
In a phase 2 study published in 2016, IMPRINT was found to be safe, with an acceptable rate of radiation pneumonitis (30% grade 2 or 3), according to investigators.7
Subsequent studies have demonstrated encouraging clinical outcomes, including a 20.2-month median OS for IMPRINT versus 12.3 months for conventional adjuvant radiotherapy in a retrospective study of 209 patients who underwent P/D between 1975 and 2015.8 Those findings led to the development of a phase 3 trial known as NRG-LU006 that is evaluating P/D plus chemotherapy with or without adjuvant IMPRINT in an estimated 150 patients. The study has a primary endpoint of OS, and an estimated primary completion date in July 2025, according to ClinicalTrials.gov.
Dr. Rimner said he’s optimistic about the prospects of this study, particularly with recently published results of a phase 3 study in which Italian investigators demonstrated an OS benefit of IMPRINT over palliative radiation in patients with nonmetastatic MPM.9
“That’s more data and rationale that shows there is good reason to believe that we are adding something here with this radiation technique,” said Dr. Rimner.
Dr. Fontaine, the thoracic surgeon and mesothelioma research head at Moffitt Cancer Center, said he’s hoping to see a substantial impact of IMPRINT on disease-free survival (DFS) once results of NRG-LU006 are available.
“I think DFS plays a role that we’ve underestimated over the last few years for sure,” he said.
For a patient with MPM, a short DFS can be anxiety provoking and may have negative impacts on quality of life, even despite a long OS, he explained.
“In terms of your outlook on life, how many times you have to go see a doctor, and how you enjoy life, there’s a big difference between the two,” he said.
Dr. Tsao provided disclosures related to Ariad, AstraZeneca, BMS, Boehringer Ingelheim, Eli Lilly, EMD Serono, Epizyme, Genentech, Huron, Merck, Millennium, Novartis, Polaris, Roche, Seattle Genetics, SELLAS Life Sciences Group, and Takeda. Dr. Fontaine reported no relevant disclosures. Dr. Rimner reported disclosures related to Bristol-Myers Squibb, GE Healthcare, Varian Medical Systems, and Boehringer Ingelheim.
References
1. Parikh K et al. Cancer Treat Rev. 2021 Sept 1;99:102250.
2. National Comprehensive Cancer Network (NCCN) Guidelines. Malignant Pleural Mesothelioma. Version 2.2021, published 2021 Feb 16. Accessed 2021 Aug 30. https://www.nccn.org/professionals/physician_gls/pdf/mpm.pdf
3. Popat S et al. Ann Oncol. 2020;31(12):1734-45.
4. Fennell D et al. Journal of Thoracic Oncology. 2021 Mar 1;16(3):S62.
5. Baas P et al. [published correction appears in Lancet. 2021 Feb 20;397(10275):670]. Lancet. 2021 Jan 30;397(10272):375-86.
6. Adusumilli PS et al. Cancer Discov. 2021 Jul 15;candisc.0407.2021.
7. Rimner A et al. J Clin Oncol. 2016;34(23):2761-8.
8. Shaikh F et al. J Thorac Oncol. 2017;12(6):993-1000.
9. Trovo M et al. Int J Radiat Oncol Biol Phys. 2021;109(5):1368-76.
Metastatic uveal melanoma: New drugs in pipeline, but prognoses remain grim
No one’s quite sure what causes uveal melanoma (UM). Unlike skin cancers, UM doesn’t seem to have any link to exposure to ultraviolet rays, although it’s most likely to strike people who are vulnerable to sun damage, like Caucasians and people with lighter eyes and lighter skin (but not lighter hair), and an inability to tan. Up to half of those affected by the disease will recover after treatment. In the other half, the cancer spreads from the eye – typically to the liver – and patient prognoses remain extremely poor despite extensive efforts to develop effective treatments.
“The median survival is probably about 2 years, and there are a number of papers out there that talk about life expectancy as short as 6 months,” said Marlana Orloff, MD, an associate professor of medical oncology at Thomas Jefferson University Hospital, Philadelphia.
But there is hope on the horizon, even if it’s not as near as patients would prefer. “Just over the last 5-10 years, we’ve gained a lot more knowledge about this disease as we try to understand how distinctly different it is, how mutations drive it, and how we can approach it using immunotherapy,” Dr. Orloff said. “I hope we’ll come up with better options for prolonging survival.”
Tracking uveal melanoma’s dangerous course
All melanomas, including UM, strike the melanocytes (cells) that provide pigment. According to a 2017 report1 in the journal Eye, “uveal melanoma is the most common primary intraocular tumor in adults with a mean age-adjusted incidence of 5.1 cases per million per year. Tumors are located either in the iris (4%), ciliary body (6%), or choroid (90%) . … As in many other cancer indications, both early detection and early treatment could be critical for a positive long-term survival outcome in uveal melanoma.”
The median age of diagnosis is 59-62 years, the report says, although non-Whites seem to develop the disease earlier.
The vast majority of patients receive treatment by plaque brachytherapy via radioactive seeds. “It’s like brachytherapy of the prostate,” said medical oncologist Rino S. Seedor, MD, of Thomas Jefferson University Hospital. “If the eye tumor is too big or invasive, they’ll cut out the eye.”
As many as 50% of patients will develop metastasis, sometimes within 2-3 years in those who have large tumors and high genetic risk, said ophthalmologist and radiation oncologist Miguel Materin, MD, of Duke University Eye Center, Durham, N.C. “There’s probably micrometastasis early in the development of the tumor,” he said. “The metastasis might develop before we or the patient knows there’s a tumor.”
Some physicians question the value of prognostic testing in patients who don’t yet show signs of metastasis, Dr. Materin said, because the findings can be grim.
Unlike his more cautious colleagues, Dr. Materin prefers to pursue testing, he said. Most patients agree to it. “It’s up to them to decide if they want to know if they have a bad prognosis,” he said, and the findings can be helpful to physicians because they provide useful genetic information about tumors.
Monitoring for liver metastasis is key
UM metastases are most likely to strike the liver, and prognoses are especially poor when they do. According to a 2019 analysis of 175 patients with metastatic UM in the Netherlands, “the presence of liver metastases is negatively associated with survival (hazard ratio = 2.09; 95% confidence interval, 1.07-4.08). … In 154 (88%) patients, the liver was affected, and only 3 patients were reported to have brain metastases.”2
As a result, physicians recommend close monitoring in patients with UM. Thomas Jefferson University’s Dr. Orloff uses tumor stages and genetic risk profiles to guide surveillance. “Very large tumors and/or monosomy 3 and 8q amplification or a Class 2 gene signature would suggest a higher-risk tumor,” she said. “For these patients we recommend MRI of the abdomen every 3 months for 2 years, CT of the chest every 6 months for 2 years, labs every 3 months for 2 years, then MRI every 6 months until year 5 with chest imaging yearly, then at 5 years everything yearly. For lower- or intermediate-risk patients we recommend MRI of the abdomen every 6 months for 5 years, chest imaging yearly, labs every 6 months, then at 5 years everything yearly.”
In the United States, patients with metastatic disease are typically sent to referral centers at institutions such as Duke, Yale (New Haven, Conn.), and Thomas Jefferson universities.
Metastasis treatments offer limited relief
There are no FDA-approved treatments for metastatic MU, and the treatments that physicians do use don’t seem to have much of an effect on life span. A 2019 study examined 73 patients with MU metastasis to the liver who were treated from 2004 to 2011 and 2012 to 2016. Among both cohorts, those who had no treatment lived nearly as long (median of 15 months) as those treated with local therapy (median of 18.7 months). Median survival for the entire population was 15 months (95% CI: 11–18 months). There was no statistically significant difference between the periods.3
However, there are signs that a move away from first-line chemotherapy in recent decades has led to longer life spans. Dr. Seedor led a 2018 study4 that compared two cohorts of MU patients with liver metastasis at her university: 98 patients from 1971 to 1993 (81% received systemic chemotherapy as their initial therapy) and 574 from 2000 to 2017 (they received various liver-directed initial treatments such as chemoembolization, drug-eluting beads, immunoembolization, and radioembolization).
The patients in the second group lived longer after treatment of initial UM than the first group (5.1 years vs. 3.3 years, P < .001) and after the development of liver metastasis (16.4 months vs. 4.8 months, P < .001). A 2020 follow-up study reported similar findings and noted that a “combination of liver-directed and newly developed systemic treatments may further improve the survival of these patients.”5
At Thomas Jefferson Medical Center, liver-directed therapy includes radioembolization, chemomobilization, and microwave ablation, Dr. Seedor said. “Which one we choose is based on how big the tumors are.”
Treatments in development could make advances
Physicians are working on several fronts to develop new treatments. A 2021 review of clinical trials found numerous trials regarding checkpoint inhibition, one devoted to a vaccine, and several involving checkpoint inhibitors. The review author notes that “the low mutational burden and poor immunogenicity of UM tumors may underlie poor responses and resistance to [immune checkpoint inhibitors] alone.”6
Earlier this year, grant-funded researchers reported encouraging news on the G protein inhibitor front. Their study found that FR900359, a selective inhibitor of the Gq/11/14 subfamily of heterotrimeric G proteins, could hold promise for “treating UM and potentially other diseases caused by constitutively active Gq/11.”7
In another 2021 study, this one with no reported funding, researchers explored the tumor microenvironment of UM and reported that their findings “provided a robust gene-based prognostic signature for predicting prognosis of UM patients and proposed a potential targeted therapy for preventing UM metastasis.”8
Experimental drug may add months of life
Physicians often recommend that patients take part in clinical trials. Earlier this year, researchers reported that a drug called tebentafusp – a bispecific fusion protein – slightly boosted metastatic UM survival in an open-label, phase 3 clinical trial when used as a first-line treatment. Patients were randomly assigned to tebentafusp, 1 of 2 immunotherapy drugs (ipilimumab or pembrolizumab), or the chemotherapy drug dacarbazine. Those who took tebentafusp vs. the other options lived longer with an estimated 1-year overall rate of 73.2% (95% CI: 66.3-78.9) vs. 57.5% (95% CI: 47.0-66.6), respectively. Fewer than 4% of those on tebentafusp needed to stop it because of adverse effects, and no treatment-related deaths occurred.9
Dr. Orloff is one of the coauthors of this study.
The National Cancer Institute provided more details about the industry-funded research and noted that median overall survival for patients who received the drug was 21.7 months vs. 16 months for the control group.
Not every patient is eligible for this treatment, however. A coauthor told the American Association for Cancer Research that “the major limitation of tebentafusp is that it can only be used in patients who have a specific HLA [human leukocyte antigen] type.” Patients must be HLA-A*0201-positive.10
In August 2021, the FDA granted priority review for tebentafusp.11 And in September 2021, a company called TriSalus announced the first patient enrollment in a “clinical study evaluating the administration of SD-101, an investigational toll-like receptor 9 (TLR9) agonist in adults with metastatic uveal melanoma.”12
According to the company, the research “is designed to evaluate the intravascular administration of SD-101 into uveal melanoma liver metastasis lesions in combination with checkpoint inhibitors using the novel Pressure-Enabled Drug Delivery (PEDD) approach.” This strategy is “designed to overcome the inherent intratumoral pressure of solid tumors,” the company said.
Dr. Materin serves on a scientific advisory board for Castle Biosciences. Dr. Orloff is a consultant for Immunocore, which funded the tebentafusp study, and serves on a scientific advisory board for TriSalus. Dr. Seedor reports no disclosures.
References
1.Kaliki S and Shields C. Eye. 2017 Feb;31:241-57.
2.Jochems A et al. Cancers. 2019 July;11(7):1007.
3.Xu LT et al. Ocul Oncol Pathol. 2019;5:323-32.
4.Seedor RS et al. J Clin Oncol. 2018 May;36(15_suppl):9592.
5.Seedor RS et al. Cancers (Basel). 2020 Jan 1;12(1):117.
6.Orloff M. Ocul Oncol Pathol. 2021 July;7:168-76.
7.Onken MD et al. J Biol Chem. 2021;296:100403.
8.Lei S and Zhang Y. Int Immunopharmacol. 2021 July;96:107816.
9.Piperno-Neumann S et al. Proceedings of the 112th Annual Meeting of the American Association for Cancer Research; 2021 April 10-15. Philadelphia (Pa.): AACR; 2021. Abstract nr 5133.
10.National Cancer Institute: https://www.cancer.gov/news-events/cancer-currents-blog/2021/tebentafusp-uveal-melanoma-improves-survival
11.Immunocore press release: https://ir.immunocore.com/news-releases/news-release-details/immunocore-announces-us-food-and-drug-administration-and
12.Trisalus announcement: https://finance.yahoo.com/news/trisalus-life-sciences-announces-first-130000215.html?guccounter=1
No one’s quite sure what causes uveal melanoma (UM). Unlike skin cancers, UM doesn’t seem to have any link to exposure to ultraviolet rays, although it’s most likely to strike people who are vulnerable to sun damage, like Caucasians and people with lighter eyes and lighter skin (but not lighter hair), and an inability to tan. Up to half of those affected by the disease will recover after treatment. In the other half, the cancer spreads from the eye – typically to the liver – and patient prognoses remain extremely poor despite extensive efforts to develop effective treatments.
“The median survival is probably about 2 years, and there are a number of papers out there that talk about life expectancy as short as 6 months,” said Marlana Orloff, MD, an associate professor of medical oncology at Thomas Jefferson University Hospital, Philadelphia.
But there is hope on the horizon, even if it’s not as near as patients would prefer. “Just over the last 5-10 years, we’ve gained a lot more knowledge about this disease as we try to understand how distinctly different it is, how mutations drive it, and how we can approach it using immunotherapy,” Dr. Orloff said. “I hope we’ll come up with better options for prolonging survival.”
Tracking uveal melanoma’s dangerous course
All melanomas, including UM, strike the melanocytes (cells) that provide pigment. According to a 2017 report1 in the journal Eye, “uveal melanoma is the most common primary intraocular tumor in adults with a mean age-adjusted incidence of 5.1 cases per million per year. Tumors are located either in the iris (4%), ciliary body (6%), or choroid (90%) . … As in many other cancer indications, both early detection and early treatment could be critical for a positive long-term survival outcome in uveal melanoma.”
The median age of diagnosis is 59-62 years, the report says, although non-Whites seem to develop the disease earlier.
The vast majority of patients receive treatment by plaque brachytherapy via radioactive seeds. “It’s like brachytherapy of the prostate,” said medical oncologist Rino S. Seedor, MD, of Thomas Jefferson University Hospital. “If the eye tumor is too big or invasive, they’ll cut out the eye.”
As many as 50% of patients will develop metastasis, sometimes within 2-3 years in those who have large tumors and high genetic risk, said ophthalmologist and radiation oncologist Miguel Materin, MD, of Duke University Eye Center, Durham, N.C. “There’s probably micrometastasis early in the development of the tumor,” he said. “The metastasis might develop before we or the patient knows there’s a tumor.”
Some physicians question the value of prognostic testing in patients who don’t yet show signs of metastasis, Dr. Materin said, because the findings can be grim.
Unlike his more cautious colleagues, Dr. Materin prefers to pursue testing, he said. Most patients agree to it. “It’s up to them to decide if they want to know if they have a bad prognosis,” he said, and the findings can be helpful to physicians because they provide useful genetic information about tumors.
Monitoring for liver metastasis is key
UM metastases are most likely to strike the liver, and prognoses are especially poor when they do. According to a 2019 analysis of 175 patients with metastatic UM in the Netherlands, “the presence of liver metastases is negatively associated with survival (hazard ratio = 2.09; 95% confidence interval, 1.07-4.08). … In 154 (88%) patients, the liver was affected, and only 3 patients were reported to have brain metastases.”2
As a result, physicians recommend close monitoring in patients with UM. Thomas Jefferson University’s Dr. Orloff uses tumor stages and genetic risk profiles to guide surveillance. “Very large tumors and/or monosomy 3 and 8q amplification or a Class 2 gene signature would suggest a higher-risk tumor,” she said. “For these patients we recommend MRI of the abdomen every 3 months for 2 years, CT of the chest every 6 months for 2 years, labs every 3 months for 2 years, then MRI every 6 months until year 5 with chest imaging yearly, then at 5 years everything yearly. For lower- or intermediate-risk patients we recommend MRI of the abdomen every 6 months for 5 years, chest imaging yearly, labs every 6 months, then at 5 years everything yearly.”
In the United States, patients with metastatic disease are typically sent to referral centers at institutions such as Duke, Yale (New Haven, Conn.), and Thomas Jefferson universities.
Metastasis treatments offer limited relief
There are no FDA-approved treatments for metastatic MU, and the treatments that physicians do use don’t seem to have much of an effect on life span. A 2019 study examined 73 patients with MU metastasis to the liver who were treated from 2004 to 2011 and 2012 to 2016. Among both cohorts, those who had no treatment lived nearly as long (median of 15 months) as those treated with local therapy (median of 18.7 months). Median survival for the entire population was 15 months (95% CI: 11–18 months). There was no statistically significant difference between the periods.3
However, there are signs that a move away from first-line chemotherapy in recent decades has led to longer life spans. Dr. Seedor led a 2018 study4 that compared two cohorts of MU patients with liver metastasis at her university: 98 patients from 1971 to 1993 (81% received systemic chemotherapy as their initial therapy) and 574 from 2000 to 2017 (they received various liver-directed initial treatments such as chemoembolization, drug-eluting beads, immunoembolization, and radioembolization).
The patients in the second group lived longer after treatment of initial UM than the first group (5.1 years vs. 3.3 years, P < .001) and after the development of liver metastasis (16.4 months vs. 4.8 months, P < .001). A 2020 follow-up study reported similar findings and noted that a “combination of liver-directed and newly developed systemic treatments may further improve the survival of these patients.”5
At Thomas Jefferson Medical Center, liver-directed therapy includes radioembolization, chemomobilization, and microwave ablation, Dr. Seedor said. “Which one we choose is based on how big the tumors are.”
Treatments in development could make advances
Physicians are working on several fronts to develop new treatments. A 2021 review of clinical trials found numerous trials regarding checkpoint inhibition, one devoted to a vaccine, and several involving checkpoint inhibitors. The review author notes that “the low mutational burden and poor immunogenicity of UM tumors may underlie poor responses and resistance to [immune checkpoint inhibitors] alone.”6
Earlier this year, grant-funded researchers reported encouraging news on the G protein inhibitor front. Their study found that FR900359, a selective inhibitor of the Gq/11/14 subfamily of heterotrimeric G proteins, could hold promise for “treating UM and potentially other diseases caused by constitutively active Gq/11.”7
In another 2021 study, this one with no reported funding, researchers explored the tumor microenvironment of UM and reported that their findings “provided a robust gene-based prognostic signature for predicting prognosis of UM patients and proposed a potential targeted therapy for preventing UM metastasis.”8
Experimental drug may add months of life
Physicians often recommend that patients take part in clinical trials. Earlier this year, researchers reported that a drug called tebentafusp – a bispecific fusion protein – slightly boosted metastatic UM survival in an open-label, phase 3 clinical trial when used as a first-line treatment. Patients were randomly assigned to tebentafusp, 1 of 2 immunotherapy drugs (ipilimumab or pembrolizumab), or the chemotherapy drug dacarbazine. Those who took tebentafusp vs. the other options lived longer with an estimated 1-year overall rate of 73.2% (95% CI: 66.3-78.9) vs. 57.5% (95% CI: 47.0-66.6), respectively. Fewer than 4% of those on tebentafusp needed to stop it because of adverse effects, and no treatment-related deaths occurred.9
Dr. Orloff is one of the coauthors of this study.
The National Cancer Institute provided more details about the industry-funded research and noted that median overall survival for patients who received the drug was 21.7 months vs. 16 months for the control group.
Not every patient is eligible for this treatment, however. A coauthor told the American Association for Cancer Research that “the major limitation of tebentafusp is that it can only be used in patients who have a specific HLA [human leukocyte antigen] type.” Patients must be HLA-A*0201-positive.10
In August 2021, the FDA granted priority review for tebentafusp.11 And in September 2021, a company called TriSalus announced the first patient enrollment in a “clinical study evaluating the administration of SD-101, an investigational toll-like receptor 9 (TLR9) agonist in adults with metastatic uveal melanoma.”12
According to the company, the research “is designed to evaluate the intravascular administration of SD-101 into uveal melanoma liver metastasis lesions in combination with checkpoint inhibitors using the novel Pressure-Enabled Drug Delivery (PEDD) approach.” This strategy is “designed to overcome the inherent intratumoral pressure of solid tumors,” the company said.
Dr. Materin serves on a scientific advisory board for Castle Biosciences. Dr. Orloff is a consultant for Immunocore, which funded the tebentafusp study, and serves on a scientific advisory board for TriSalus. Dr. Seedor reports no disclosures.
References
1.Kaliki S and Shields C. Eye. 2017 Feb;31:241-57.
2.Jochems A et al. Cancers. 2019 July;11(7):1007.
3.Xu LT et al. Ocul Oncol Pathol. 2019;5:323-32.
4.Seedor RS et al. J Clin Oncol. 2018 May;36(15_suppl):9592.
5.Seedor RS et al. Cancers (Basel). 2020 Jan 1;12(1):117.
6.Orloff M. Ocul Oncol Pathol. 2021 July;7:168-76.
7.Onken MD et al. J Biol Chem. 2021;296:100403.
8.Lei S and Zhang Y. Int Immunopharmacol. 2021 July;96:107816.
9.Piperno-Neumann S et al. Proceedings of the 112th Annual Meeting of the American Association for Cancer Research; 2021 April 10-15. Philadelphia (Pa.): AACR; 2021. Abstract nr 5133.
10.National Cancer Institute: https://www.cancer.gov/news-events/cancer-currents-blog/2021/tebentafusp-uveal-melanoma-improves-survival
11.Immunocore press release: https://ir.immunocore.com/news-releases/news-release-details/immunocore-announces-us-food-and-drug-administration-and
12.Trisalus announcement: https://finance.yahoo.com/news/trisalus-life-sciences-announces-first-130000215.html?guccounter=1
No one’s quite sure what causes uveal melanoma (UM). Unlike skin cancers, UM doesn’t seem to have any link to exposure to ultraviolet rays, although it’s most likely to strike people who are vulnerable to sun damage, like Caucasians and people with lighter eyes and lighter skin (but not lighter hair), and an inability to tan. Up to half of those affected by the disease will recover after treatment. In the other half, the cancer spreads from the eye – typically to the liver – and patient prognoses remain extremely poor despite extensive efforts to develop effective treatments.
“The median survival is probably about 2 years, and there are a number of papers out there that talk about life expectancy as short as 6 months,” said Marlana Orloff, MD, an associate professor of medical oncology at Thomas Jefferson University Hospital, Philadelphia.
But there is hope on the horizon, even if it’s not as near as patients would prefer. “Just over the last 5-10 years, we’ve gained a lot more knowledge about this disease as we try to understand how distinctly different it is, how mutations drive it, and how we can approach it using immunotherapy,” Dr. Orloff said. “I hope we’ll come up with better options for prolonging survival.”
Tracking uveal melanoma’s dangerous course
All melanomas, including UM, strike the melanocytes (cells) that provide pigment. According to a 2017 report1 in the journal Eye, “uveal melanoma is the most common primary intraocular tumor in adults with a mean age-adjusted incidence of 5.1 cases per million per year. Tumors are located either in the iris (4%), ciliary body (6%), or choroid (90%) . … As in many other cancer indications, both early detection and early treatment could be critical for a positive long-term survival outcome in uveal melanoma.”
The median age of diagnosis is 59-62 years, the report says, although non-Whites seem to develop the disease earlier.
The vast majority of patients receive treatment by plaque brachytherapy via radioactive seeds. “It’s like brachytherapy of the prostate,” said medical oncologist Rino S. Seedor, MD, of Thomas Jefferson University Hospital. “If the eye tumor is too big or invasive, they’ll cut out the eye.”
As many as 50% of patients will develop metastasis, sometimes within 2-3 years in those who have large tumors and high genetic risk, said ophthalmologist and radiation oncologist Miguel Materin, MD, of Duke University Eye Center, Durham, N.C. “There’s probably micrometastasis early in the development of the tumor,” he said. “The metastasis might develop before we or the patient knows there’s a tumor.”
Some physicians question the value of prognostic testing in patients who don’t yet show signs of metastasis, Dr. Materin said, because the findings can be grim.
Unlike his more cautious colleagues, Dr. Materin prefers to pursue testing, he said. Most patients agree to it. “It’s up to them to decide if they want to know if they have a bad prognosis,” he said, and the findings can be helpful to physicians because they provide useful genetic information about tumors.
Monitoring for liver metastasis is key
UM metastases are most likely to strike the liver, and prognoses are especially poor when they do. According to a 2019 analysis of 175 patients with metastatic UM in the Netherlands, “the presence of liver metastases is negatively associated with survival (hazard ratio = 2.09; 95% confidence interval, 1.07-4.08). … In 154 (88%) patients, the liver was affected, and only 3 patients were reported to have brain metastases.”2
As a result, physicians recommend close monitoring in patients with UM. Thomas Jefferson University’s Dr. Orloff uses tumor stages and genetic risk profiles to guide surveillance. “Very large tumors and/or monosomy 3 and 8q amplification or a Class 2 gene signature would suggest a higher-risk tumor,” she said. “For these patients we recommend MRI of the abdomen every 3 months for 2 years, CT of the chest every 6 months for 2 years, labs every 3 months for 2 years, then MRI every 6 months until year 5 with chest imaging yearly, then at 5 years everything yearly. For lower- or intermediate-risk patients we recommend MRI of the abdomen every 6 months for 5 years, chest imaging yearly, labs every 6 months, then at 5 years everything yearly.”
In the United States, patients with metastatic disease are typically sent to referral centers at institutions such as Duke, Yale (New Haven, Conn.), and Thomas Jefferson universities.
Metastasis treatments offer limited relief
There are no FDA-approved treatments for metastatic MU, and the treatments that physicians do use don’t seem to have much of an effect on life span. A 2019 study examined 73 patients with MU metastasis to the liver who were treated from 2004 to 2011 and 2012 to 2016. Among both cohorts, those who had no treatment lived nearly as long (median of 15 months) as those treated with local therapy (median of 18.7 months). Median survival for the entire population was 15 months (95% CI: 11–18 months). There was no statistically significant difference between the periods.3
However, there are signs that a move away from first-line chemotherapy in recent decades has led to longer life spans. Dr. Seedor led a 2018 study4 that compared two cohorts of MU patients with liver metastasis at her university: 98 patients from 1971 to 1993 (81% received systemic chemotherapy as their initial therapy) and 574 from 2000 to 2017 (they received various liver-directed initial treatments such as chemoembolization, drug-eluting beads, immunoembolization, and radioembolization).
The patients in the second group lived longer after treatment of initial UM than the first group (5.1 years vs. 3.3 years, P < .001) and after the development of liver metastasis (16.4 months vs. 4.8 months, P < .001). A 2020 follow-up study reported similar findings and noted that a “combination of liver-directed and newly developed systemic treatments may further improve the survival of these patients.”5
At Thomas Jefferson Medical Center, liver-directed therapy includes radioembolization, chemomobilization, and microwave ablation, Dr. Seedor said. “Which one we choose is based on how big the tumors are.”
Treatments in development could make advances
Physicians are working on several fronts to develop new treatments. A 2021 review of clinical trials found numerous trials regarding checkpoint inhibition, one devoted to a vaccine, and several involving checkpoint inhibitors. The review author notes that “the low mutational burden and poor immunogenicity of UM tumors may underlie poor responses and resistance to [immune checkpoint inhibitors] alone.”6
Earlier this year, grant-funded researchers reported encouraging news on the G protein inhibitor front. Their study found that FR900359, a selective inhibitor of the Gq/11/14 subfamily of heterotrimeric G proteins, could hold promise for “treating UM and potentially other diseases caused by constitutively active Gq/11.”7
In another 2021 study, this one with no reported funding, researchers explored the tumor microenvironment of UM and reported that their findings “provided a robust gene-based prognostic signature for predicting prognosis of UM patients and proposed a potential targeted therapy for preventing UM metastasis.”8
Experimental drug may add months of life
Physicians often recommend that patients take part in clinical trials. Earlier this year, researchers reported that a drug called tebentafusp – a bispecific fusion protein – slightly boosted metastatic UM survival in an open-label, phase 3 clinical trial when used as a first-line treatment. Patients were randomly assigned to tebentafusp, 1 of 2 immunotherapy drugs (ipilimumab or pembrolizumab), or the chemotherapy drug dacarbazine. Those who took tebentafusp vs. the other options lived longer with an estimated 1-year overall rate of 73.2% (95% CI: 66.3-78.9) vs. 57.5% (95% CI: 47.0-66.6), respectively. Fewer than 4% of those on tebentafusp needed to stop it because of adverse effects, and no treatment-related deaths occurred.9
Dr. Orloff is one of the coauthors of this study.
The National Cancer Institute provided more details about the industry-funded research and noted that median overall survival for patients who received the drug was 21.7 months vs. 16 months for the control group.
Not every patient is eligible for this treatment, however. A coauthor told the American Association for Cancer Research that “the major limitation of tebentafusp is that it can only be used in patients who have a specific HLA [human leukocyte antigen] type.” Patients must be HLA-A*0201-positive.10
In August 2021, the FDA granted priority review for tebentafusp.11 And in September 2021, a company called TriSalus announced the first patient enrollment in a “clinical study evaluating the administration of SD-101, an investigational toll-like receptor 9 (TLR9) agonist in adults with metastatic uveal melanoma.”12
According to the company, the research “is designed to evaluate the intravascular administration of SD-101 into uveal melanoma liver metastasis lesions in combination with checkpoint inhibitors using the novel Pressure-Enabled Drug Delivery (PEDD) approach.” This strategy is “designed to overcome the inherent intratumoral pressure of solid tumors,” the company said.
Dr. Materin serves on a scientific advisory board for Castle Biosciences. Dr. Orloff is a consultant for Immunocore, which funded the tebentafusp study, and serves on a scientific advisory board for TriSalus. Dr. Seedor reports no disclosures.
References
1.Kaliki S and Shields C. Eye. 2017 Feb;31:241-57.
2.Jochems A et al. Cancers. 2019 July;11(7):1007.
3.Xu LT et al. Ocul Oncol Pathol. 2019;5:323-32.
4.Seedor RS et al. J Clin Oncol. 2018 May;36(15_suppl):9592.
5.Seedor RS et al. Cancers (Basel). 2020 Jan 1;12(1):117.
6.Orloff M. Ocul Oncol Pathol. 2021 July;7:168-76.
7.Onken MD et al. J Biol Chem. 2021;296:100403.
8.Lei S and Zhang Y. Int Immunopharmacol. 2021 July;96:107816.
9.Piperno-Neumann S et al. Proceedings of the 112th Annual Meeting of the American Association for Cancer Research; 2021 April 10-15. Philadelphia (Pa.): AACR; 2021. Abstract nr 5133.
10.National Cancer Institute: https://www.cancer.gov/news-events/cancer-currents-blog/2021/tebentafusp-uveal-melanoma-improves-survival
11.Immunocore press release: https://ir.immunocore.com/news-releases/news-release-details/immunocore-announces-us-food-and-drug-administration-and
12.Trisalus announcement: https://finance.yahoo.com/news/trisalus-life-sciences-announces-first-130000215.html?guccounter=1
Rare GU cancers: Overcoming obstacles through collaboration, novel trial design
In a field of poor outcomes, few standards of care, and small populations of patients scattered across the world, investigators studying rare genitourinary (GU) cancers are gaining ground through international collaboration and novel trial design.
Fundamental clinical questions in the area remain unanswered, including the value of conventional treatments, such as chemotherapy and surgery, vs. emerging immunotherapy combinations.
Managing patients with rare GU cancers presents a variety of challenges, as does conducting research in the field, according to Philippe E. Spiess, MD, MS, FACS, assistant chief of surgical services and senior member in the department of GU oncology at Moffitt Cancer Center, Tampa.
“Unfortunately, there are limited resources for patients – from an education, from a patient advocacy, and ultimately also from a research standpoint,” Dr. Spiess said in an interview, noting difficulties in attaining funding and reaching meaningful endpoints.
The Global Society of Rare Genitourinary Tumors
Last year Dr. Spiess teamed up with Andrea Necchi, MD, of the department of medical oncology at Fondazione IRCCS Istituto Nazionale dei Tumori, Milan, to found the Global Society of Rare Genitourinary Tumors (GSRGT), the first organization of its kind.
“We’ve formally established a society and gotten some of the world leaders [in the field] … to work with us in developing educational tools and patient advocacy efforts to really promote and improve the care of patients impacted with rare cancers,” Dr. Spiess said.
He went on to highlight the truly global makeup of GSRGT, which includes members from leading centers in North America, South America, Europe, and India, and described it as a “grass-roots” organization that he and Dr. Necchi privately funded without financial backing from pharmaceutical companies.
The first GSRGT summit took place in 2020; it focused on penile and testis cancers and was attended by more than 350 participants. The second summit, planned for March 2022, in a virtual format, will focus on rare kidney cancers and upper tract cancers.
“We’ll definitely be having a lot of important conversations about important unmet needs, and some of the important clinical trials that patients and clinicians should be aware of,” Dr. Spiess said.
Dr. Spiess is currently involved in the International Penile Advanced Cancer Trial(InPACT), which is aiming to enroll 200 patients with squamous cell carcinoma of the penis. The randomized study will compare outcomes across patients treated with standard surgery alone, neoadjuvant chemotherapy plus surgery, and neoadjuvant chemoradiotherapy plus surgery.
“I think this is going to be a landmark study because it’s going to give really baseline high-quality data on the effectiveness of these therapies,” Dr. Spiess said.
Results are expected in 2024.
Basket trials open doors for patients in need
Other investigators are testing immunotherapy combinations in patients with rare GU tumors via nonrandomized basket trials, which widen inclusion criteria and improve local availability.
According to Bradley McGregor, MD, clinical director of the Lank Center for GU Oncology at the Dana-Farber Cancer Institute in Boston, early results from these trials are promising, both in terms of therapeutic efficacy and the approach itself.
“Patients [with rare GU tumors] would come to us saying, ‘Well, what can we do? What trial?’,” Dr. McGregor said. “But really, there was no trial to get them on.”Basket trials are therefore needed, he said, as they accelerate progress in the field and help meet patient needs.
“For some of these relatively rare diseases … there is no standard of care,” Dr. McGregor said. “And low incidence makes it challenging to conduct a dedicated clinical trial. Those patients are left with minimal therapeutic options. … We look to provide care for that unmet need.”Andrea B. Apolo, MD, described similar experiences as head of the bladder cancer section of the GU malignancies branch of the National Cancer Institute (NCI), Bethesda, Md.
“I’ve been at the NCI for the past 10 years and I’ve gotten a lot of referrals for rare tumors,” Dr. Apolo said. “[These patients] have tried all available standard of care options, and therefore are often looking for clinical trials and new drugs – any kind of therapy that may be effective for their disease.”This call for help, along with a growing scientific curiosity, motivated Dr. Apolo to design trials that would include patients who had nowhere else to go.
“I became very interested in … understanding more about the mechanism of tumorigenesis and understanding rare tumors, biologically, within the lab,” she said, “but also clinically, in terms of finding more effective therapies.”
Both Dr. McGregor and Dr. Apolo are currently conducting basket trials for patients with rare GU tumors. While Dr. McGregor is testing a combination of PD-1 inhibitor nivolumab and CTLA-4 inhibitor ipilimumab, Dr. Apolo is exploring the benefit of cabozantinib, a targeted therapy, given with either nivolumab or nivolumab plus ipilimumab.
When asked about these trials, Dr. Spiess said that “basket trials are important because they may give us an understanding of some potentially useful therapies or combinations;” however, he also pointed out their limitations, noting that they may inaccurately characterize the efficacy of given therapies over a broad array of disease entities even if they are of similar histology. As an example, he noted “very different” genomic profiles across squamous cell carcinomas of the pelvis depending on exact anatomical location, suggesting that these differences may affect responses to therapy, citing a recent study in European Urology that he conducted with Dr. Necchi.1
“[Basket trials] are probably not going to be the be-all-end-all,” Dr. Spiess said. “It really requires a global initiative to do these types of studies, which the Global Society of Rare Genitourinary Tumors will allow.”
Exploring immunotherapy combinations
Despite the potential limitations, recent basket trials involving immunotherapy regimens have been associated with overall response rates, in some subgroups, that exceed 35%.2,3
In comparison with previous trials, many of which had response rates in the single digits, or no responses at all, these results are, in Dr. McGregor’s words, “very thought provoking.”Most rare GU malignancies fall into one of four categories: bladder cancer variant histology (BCVH), adrenal tumors, penile squamous cell carcinoma (PSCC), and chemotherapy-refractory germ cell tumors (CRGCT). Among these, BCVH has the strongest evidence supporting clinical use of immunotherapy, based on U.S. approval for urothelial histology, according to Dr. McGregor.4Data supporting immunotherapy for the remaining disease subtypes are scarce. Although pembrolizumab is approved for patients with solid tumors that exhibit microsatellite instability (MSI), MSI is uncommon among patients with rare GU cancers; estimated incidence rates are less than 10%.4
“As such, clinical trials to address this unmet need are imperative,” Dr. McGregor wrote in a recent review article.4
According to Dr. McGregor, programmed death ligand 1 (PD-L1) expression in rare GU tumors may be relatively common in some disease subtypes, such as PSCC, which has a PD-L1 expression rate of up to 60%.4
But rare GU tumor trials involving a single checkpoint inhibitor have produced limited results, if any.
The largest trial for adrenocortical carcinoma (ACC), for example, which included 50 patients, showed that avelumab resulted in an objective response rate (ORR) of just 6%.5
Pembrolizumab was slightly more effective for ACC, based on a trial involving 39 patients, which returned an ORR of 23%, and another trial involving 15 patients that had a 15% ORR.6,7
Two other trials, which tested single-agent pembrolizumab or durvalumab in patients with CRGCT, resulted in no responses at all, whereas a trial testing pembrolizumab alone for penile squamous cell carcinoma was terminated in 2020, citing poor accrual.8,9 Still, the durvalumab trial for CRGCT, led by Dr. Necchi, did offer a glimpse at what might be possible with a combination of immunotherapies. Although no responses were observed among 11 patients who received durvalumab alone, an efficacy signal was observed in a second cohort of 11 patients who were given durvalumab in combination with the CTLA-4 inhibitor tremilimumab.9
Out of those 11 patients, 1 had a partial response, and another achieved stable disease.
In light of these findings, and more that have been published since then, the clinical trial landscape for rare GU tumors is shifting toward a combination immunotherapy approach, according to Dr. McGregor.4
Nivolumab and ipilimumab
Dr. McGregor is leading a phase II trial (NCT03333616) testing a combination of nivolumab and ipilimumab in patients with a variety of advanced rare GU malignancies, including bladder and upper tract carcinoma of variant histology (BUTCVH), adrenal tumors, CRGCT, PSCC, and prostate cancer of variant histology (PCVH).
“When trials are designed, these patients are often forgotten,” Dr. McGregor noted. “We said, let’s do a trial for all rare GU tumors and just sort of assess and look for a signal, and, hopefully, find a signal that we can then take to the next level.”
Along with appropriate disease phenotype, trial eligibility depended upon an ECOG performance status of 0-2 and no prior exposure to checkpoint inhibitors. Treatment-naive patients were allowed. All participants received nivolumab 3 mg/kg and ipilimumab 1 mg/kg IV every 3 weeks for four doses, followed by maintenance nivolumab at a dose of 480 mg every 4 weeks.
Most recent results, published in Cancer, included data from 55 patients, including 19 with BUTCVH, 18 with adrenal tumors, and 18 with other tumors.3 After a median follow-up of 9.9 months, 28 patients (51%) received all four doses of the regimen, 25 of whom received maintenance therapy with a median of four cycles.
Overall, nine patients (16%) responded to therapy, six of whom (67%) maintained their response for at least 9 months. Two responses were complete, and seven were partial. Median progression-free survival was 2.8 months.
Twenty-two patients (39%) had grade 3 or higher treatment-related adverse events, approximately one-quarter (23%) needed high-dose steroids, and a slightly greater proportion (27%) discontinued the regimen because of adverse events. Three patients exhibited grade 5 toxicity, and one patient death was treatment related. A closer look at the efficacy data suggested that one disease subgroup benefited much more than the others. The overall response rate among 19 patients with BUTCVH was 37%, compared with 6% in the other two cohorts.
“A response rate of 37% compares quite favorably to anything we’ve seen to date,” Dr. McGregor said. “It’s remarkable that [this response] was seen across histologies – we saw this in urachal, we saw this in adenocarcinoma – we really saw this across the board. This is very, very, very intriguing data.”
The phase II trial is ongoing at multiple centers across the country, including the Dana-Farber/Harvard Cancer Center, Boston, the University of Texas MD Anderson Cancer Center, Houston, the Moores Cancer Center at University of California Health, San Diego, the Ohio State University Comprehensive Cancer Center, Columbus, and the Winship Cancer Institute of Emory University, Atlanta.
“We accrued this trial in just under 18 months,” Dr. McGregor said. “I think this shows that with a well-designed trial, we can actually study these diseases and improve outcomes in these patients.” According to Dr. McGregor, the current findings deserve further investigation, potentially including expansion of the BUTCVH cohort. Recruitment is ongoing for a fourth cohort involving patients with tumors that exhibit neuroendocrine differentiation.
Cabozantinib and nivolumab with or without ipilimumab
Dr. Apolo is leading a similar basket trial (NCT02496208) that is testing cabozantinib plus nivolumab with or without ipilimumab.
“What we’re doing is using immunotherapy and a targeted therapy that work in standard urothelial carcinoma and renal cell carcinoma,” Dr. Apolo said. “But really, we don’t know the activity in these rare GU tumors. … There’s still so much we don’t understand about what the driving mutations are, and how we can best target them.”
Most recent data, published in Journal of Clinical Oncology, include 122 patients with metastatic GU tumors, including urothelial carcinoma, clear cell renal cell carcinoma, bladder adenocarcinoma, and other rare GU cancers.2
Among these patients, 54 were in the phase I dose-finding cohort (eight escalating doses) and 64 were in the dose-expansion cohorts.
After a median follow-up of 40.4 months, 64 patients received the dual combination, whereas 56 received the triplet regimen. The ORR for 108 evaluable patients was 38%, including 12 complete responses (11.1%) and 29 partial responses (26.9%). The largest disease cohort, for urothelial carcinoma, included 33 patients and was associated with an ORR of 42.4%, with a complete response rate of 21.2%. Objective response rate was highest for squamous bladder cancer (85.7%; n = 7), followed by clear cell renal carcinoma (62.5%; n = 16), renal medullary cancer (50%; n = 2), penile cancer (44.4%; n = 9), small cell bladder cancer (33.1%; n = 3), bladder adenocarcinoma (20%; n = 15), and prostate cancer (11.1%; n = 9). No responses were seen in six patients with germ cell tumors.
Adding ipilimumab appeared to have a minimal impact on toxicity. Grade 3 or 4 treatment-related adverse events (AEs) occurred in 84% of patients in the dual combination group, compared with 80% receiving the triplet regimen. Most common AEs were hypophosphatemia (16-25%), lipase elevation (20%), fatigue (18-20%), ALT elevation (5-14%), AST elevation (9-11%), diarrhea (9-11%), and thromboembolic event (4-11%). One patient taking the triplet regimen had grade 5 pneumonitis.
These positive phase I results have paved the way for the phase II ICONIC trial (NCT03866382), a national study available through the Alliance Cooperative Group. The trial is currently recruiting, with an estimated enrollment of 224 patients with rare GU tumors.
The ICONIC trial is just one of several studies that Dr. Apolo is conducting for patients with rare GU cancer. “I have several bladder cancer trials where I’m accepting rare GU tumors to enroll,” she said, noting that efficacy signals in these exploratory cohorts may be pursued with expansion studies like ICONIC.
This inclusive strategy is uncovering promising new treatments for some rare GU malignancies, but the rarest of the rare tumor types remain challenging to study, Dr. Apolo said, because very small sample sizes can preclude significant data. “Although we do have the referral base at the NCI, we still get a small number of a lot of rare tumors,” Dr. Apolo said. “What I end up having, a lot of time, are small subsets of rare tumors – I’ll have 4 of one kind, 10 of another.” This situation means that sometimes, time and resources must be focused where they are needed most.
“Sometimes I actually have to decide which are the more common rare tumors so I can study them in a larger cohort,” Dr. Apolo said. “It can have more clinical impact within the community of that rare tumor.” Dr. Apolo described the inherent conflict involved in this decision, but also, its ultimate necessity.
“It’s what you don’t want to do, but you end up doing,” she said. “Because you want to be inclusive and include the rare, rare tumor, but sometimes you just can’t get enough numbers to see if there’s actually a difference [in efficacy]. If it doesn’t work in one patient, does that mean it doesn’t work at all? You need more numbers to really test the efficacy of therapy.”
From clinical trials to clinical practice
To accrue the number of patients needed for practice-altering findings, both Dr. McGregor and Dr. Apolo emphasized the importance of institutional support and collaborative trial designs.
“The FDA is a great ally,” Dr. McGregor said. “They’re acutely aware of the challenges facing patients with rare malignancies – not just GU malignancies. They’re continuing to evaluate the best way to move these drugs forward for those patients. … They’re constantly working with investigators, with industry, looking at data and trying to determine at what threshold these will be practice-changing studies.”
Dr. McGregor suggested that larger trials could shift national guideline recommendations toward combination immunotherapies for patients with rare GU tumors, which would lead to inclusion in compendia, and from there, broader clinical usage.
“At end of the day, luckily, we’re not dealing with drugs that aren’t available,” Dr. McGregor said. “These are drugs that are readily available, approved by the FDA in other settings.”
Dr. Apolo also described strong support from the NCI.
“The NCI really encourages the conduction and enrollment of these rare GU tumor trials, because they understand that the NCI is a really good place to study these rare tumors,” she said. “We have unique resources that make it feasible to conduct some of these trials.”
Dr. Apolo also praised the Alliance Cooperative Group for helping expand patient access to rare GU tumor trials.
“[The Alliance Cooperative Group] makes trials available at community centers across the country,” Dr. Apolo said. “Patients don’t have to travel to the NCI, and they can get the same therapies.”
Still, Dr. Apolo recommended that, when possible, clinicians refer patients with newly diagnosed, rare GU tumors to centers that see a higher number of such cases.
“It’s hard to keep up with all the different treatments that are available right now for different cancers,” Dr. Apolo said. “And sometimes for the rare tumors, there may be great opportunities within a clinical trial that a cancer center may have available that may not be available locally in the community.”
For patients who would like to learn more about rare bladder cancers, Dr. Apolo recommended a visit to the Bladder Cancer Advocacy Network (BCAN) website (bcan.org).
“I’m a big fan of these patient-centered advocacy networks,” Dr. Apolo said. “I like BCAN a lot. It’s a patient-run organization for patients with bladder cancer. With them, I have done a couple of webinars for rare bladder tumors that Ive had some patients tell me are very helpful. They’re a terrific organization that really provides not only emotional support but also educational support for patients that have a diagnosis of bladder cancer and now, rare bladder tumors.” Dr. Spiess offered similar advice for clinicians managing patients with rare GU tumors. He emphasized the key role played by patient advocacy groups, and recommended referral to institutions specializing in specific GU tumor types. For example, he recommended that patients with penile cancer be treated at Moffitt (Tampa) or MD Anderson (Houston), as these centers have the greatest relevant experience. Dr. McGregor disclosed relationships with Bayer, Astellas, Nektar, and others. Dr. Apolo and Dr. Spiess disclosed no conflicts of interest.
References
1.Necchi A et al. Eur Urol. 2021 June;79:S929-30.
2.Apolo AB et al. J Clin Oncol. 2021;39(6_suppl):3.
3.McGregor BA et al. Cancer. 2021 Mar 15;127(6):840-9.
4.McGregor BA and Sonpavde GP. Eur Urol Focus. 2020;6(1):14-16.5.Le Tourneau C et al. J Immunother Cancer. 2018 Oct 22;6(1):111.6.Naing A et al. J Immunother Cancer. 2020;8(1).
7.Raj N et al. J Clin Oncol. 2020;38(1):71-80.
8.Adra N et al. Ann Oncol. 2018;29(1):209-14.
9.Necchi A et al. Eur Urol. 2019;75(1):201-3.
In a field of poor outcomes, few standards of care, and small populations of patients scattered across the world, investigators studying rare genitourinary (GU) cancers are gaining ground through international collaboration and novel trial design.
Fundamental clinical questions in the area remain unanswered, including the value of conventional treatments, such as chemotherapy and surgery, vs. emerging immunotherapy combinations.
Managing patients with rare GU cancers presents a variety of challenges, as does conducting research in the field, according to Philippe E. Spiess, MD, MS, FACS, assistant chief of surgical services and senior member in the department of GU oncology at Moffitt Cancer Center, Tampa.
“Unfortunately, there are limited resources for patients – from an education, from a patient advocacy, and ultimately also from a research standpoint,” Dr. Spiess said in an interview, noting difficulties in attaining funding and reaching meaningful endpoints.
The Global Society of Rare Genitourinary Tumors
Last year Dr. Spiess teamed up with Andrea Necchi, MD, of the department of medical oncology at Fondazione IRCCS Istituto Nazionale dei Tumori, Milan, to found the Global Society of Rare Genitourinary Tumors (GSRGT), the first organization of its kind.
“We’ve formally established a society and gotten some of the world leaders [in the field] … to work with us in developing educational tools and patient advocacy efforts to really promote and improve the care of patients impacted with rare cancers,” Dr. Spiess said.
He went on to highlight the truly global makeup of GSRGT, which includes members from leading centers in North America, South America, Europe, and India, and described it as a “grass-roots” organization that he and Dr. Necchi privately funded without financial backing from pharmaceutical companies.
The first GSRGT summit took place in 2020; it focused on penile and testis cancers and was attended by more than 350 participants. The second summit, planned for March 2022, in a virtual format, will focus on rare kidney cancers and upper tract cancers.
“We’ll definitely be having a lot of important conversations about important unmet needs, and some of the important clinical trials that patients and clinicians should be aware of,” Dr. Spiess said.
Dr. Spiess is currently involved in the International Penile Advanced Cancer Trial(InPACT), which is aiming to enroll 200 patients with squamous cell carcinoma of the penis. The randomized study will compare outcomes across patients treated with standard surgery alone, neoadjuvant chemotherapy plus surgery, and neoadjuvant chemoradiotherapy plus surgery.
“I think this is going to be a landmark study because it’s going to give really baseline high-quality data on the effectiveness of these therapies,” Dr. Spiess said.
Results are expected in 2024.
Basket trials open doors for patients in need
Other investigators are testing immunotherapy combinations in patients with rare GU tumors via nonrandomized basket trials, which widen inclusion criteria and improve local availability.
According to Bradley McGregor, MD, clinical director of the Lank Center for GU Oncology at the Dana-Farber Cancer Institute in Boston, early results from these trials are promising, both in terms of therapeutic efficacy and the approach itself.
“Patients [with rare GU tumors] would come to us saying, ‘Well, what can we do? What trial?’,” Dr. McGregor said. “But really, there was no trial to get them on.”Basket trials are therefore needed, he said, as they accelerate progress in the field and help meet patient needs.
“For some of these relatively rare diseases … there is no standard of care,” Dr. McGregor said. “And low incidence makes it challenging to conduct a dedicated clinical trial. Those patients are left with minimal therapeutic options. … We look to provide care for that unmet need.”Andrea B. Apolo, MD, described similar experiences as head of the bladder cancer section of the GU malignancies branch of the National Cancer Institute (NCI), Bethesda, Md.
“I’ve been at the NCI for the past 10 years and I’ve gotten a lot of referrals for rare tumors,” Dr. Apolo said. “[These patients] have tried all available standard of care options, and therefore are often looking for clinical trials and new drugs – any kind of therapy that may be effective for their disease.”This call for help, along with a growing scientific curiosity, motivated Dr. Apolo to design trials that would include patients who had nowhere else to go.
“I became very interested in … understanding more about the mechanism of tumorigenesis and understanding rare tumors, biologically, within the lab,” she said, “but also clinically, in terms of finding more effective therapies.”
Both Dr. McGregor and Dr. Apolo are currently conducting basket trials for patients with rare GU tumors. While Dr. McGregor is testing a combination of PD-1 inhibitor nivolumab and CTLA-4 inhibitor ipilimumab, Dr. Apolo is exploring the benefit of cabozantinib, a targeted therapy, given with either nivolumab or nivolumab plus ipilimumab.
When asked about these trials, Dr. Spiess said that “basket trials are important because they may give us an understanding of some potentially useful therapies or combinations;” however, he also pointed out their limitations, noting that they may inaccurately characterize the efficacy of given therapies over a broad array of disease entities even if they are of similar histology. As an example, he noted “very different” genomic profiles across squamous cell carcinomas of the pelvis depending on exact anatomical location, suggesting that these differences may affect responses to therapy, citing a recent study in European Urology that he conducted with Dr. Necchi.1
“[Basket trials] are probably not going to be the be-all-end-all,” Dr. Spiess said. “It really requires a global initiative to do these types of studies, which the Global Society of Rare Genitourinary Tumors will allow.”
Exploring immunotherapy combinations
Despite the potential limitations, recent basket trials involving immunotherapy regimens have been associated with overall response rates, in some subgroups, that exceed 35%.2,3
In comparison with previous trials, many of which had response rates in the single digits, or no responses at all, these results are, in Dr. McGregor’s words, “very thought provoking.”Most rare GU malignancies fall into one of four categories: bladder cancer variant histology (BCVH), adrenal tumors, penile squamous cell carcinoma (PSCC), and chemotherapy-refractory germ cell tumors (CRGCT). Among these, BCVH has the strongest evidence supporting clinical use of immunotherapy, based on U.S. approval for urothelial histology, according to Dr. McGregor.4Data supporting immunotherapy for the remaining disease subtypes are scarce. Although pembrolizumab is approved for patients with solid tumors that exhibit microsatellite instability (MSI), MSI is uncommon among patients with rare GU cancers; estimated incidence rates are less than 10%.4
“As such, clinical trials to address this unmet need are imperative,” Dr. McGregor wrote in a recent review article.4
According to Dr. McGregor, programmed death ligand 1 (PD-L1) expression in rare GU tumors may be relatively common in some disease subtypes, such as PSCC, which has a PD-L1 expression rate of up to 60%.4
But rare GU tumor trials involving a single checkpoint inhibitor have produced limited results, if any.
The largest trial for adrenocortical carcinoma (ACC), for example, which included 50 patients, showed that avelumab resulted in an objective response rate (ORR) of just 6%.5
Pembrolizumab was slightly more effective for ACC, based on a trial involving 39 patients, which returned an ORR of 23%, and another trial involving 15 patients that had a 15% ORR.6,7
Two other trials, which tested single-agent pembrolizumab or durvalumab in patients with CRGCT, resulted in no responses at all, whereas a trial testing pembrolizumab alone for penile squamous cell carcinoma was terminated in 2020, citing poor accrual.8,9 Still, the durvalumab trial for CRGCT, led by Dr. Necchi, did offer a glimpse at what might be possible with a combination of immunotherapies. Although no responses were observed among 11 patients who received durvalumab alone, an efficacy signal was observed in a second cohort of 11 patients who were given durvalumab in combination with the CTLA-4 inhibitor tremilimumab.9
Out of those 11 patients, 1 had a partial response, and another achieved stable disease.
In light of these findings, and more that have been published since then, the clinical trial landscape for rare GU tumors is shifting toward a combination immunotherapy approach, according to Dr. McGregor.4
Nivolumab and ipilimumab
Dr. McGregor is leading a phase II trial (NCT03333616) testing a combination of nivolumab and ipilimumab in patients with a variety of advanced rare GU malignancies, including bladder and upper tract carcinoma of variant histology (BUTCVH), adrenal tumors, CRGCT, PSCC, and prostate cancer of variant histology (PCVH).
“When trials are designed, these patients are often forgotten,” Dr. McGregor noted. “We said, let’s do a trial for all rare GU tumors and just sort of assess and look for a signal, and, hopefully, find a signal that we can then take to the next level.”
Along with appropriate disease phenotype, trial eligibility depended upon an ECOG performance status of 0-2 and no prior exposure to checkpoint inhibitors. Treatment-naive patients were allowed. All participants received nivolumab 3 mg/kg and ipilimumab 1 mg/kg IV every 3 weeks for four doses, followed by maintenance nivolumab at a dose of 480 mg every 4 weeks.
Most recent results, published in Cancer, included data from 55 patients, including 19 with BUTCVH, 18 with adrenal tumors, and 18 with other tumors.3 After a median follow-up of 9.9 months, 28 patients (51%) received all four doses of the regimen, 25 of whom received maintenance therapy with a median of four cycles.
Overall, nine patients (16%) responded to therapy, six of whom (67%) maintained their response for at least 9 months. Two responses were complete, and seven were partial. Median progression-free survival was 2.8 months.
Twenty-two patients (39%) had grade 3 or higher treatment-related adverse events, approximately one-quarter (23%) needed high-dose steroids, and a slightly greater proportion (27%) discontinued the regimen because of adverse events. Three patients exhibited grade 5 toxicity, and one patient death was treatment related. A closer look at the efficacy data suggested that one disease subgroup benefited much more than the others. The overall response rate among 19 patients with BUTCVH was 37%, compared with 6% in the other two cohorts.
“A response rate of 37% compares quite favorably to anything we’ve seen to date,” Dr. McGregor said. “It’s remarkable that [this response] was seen across histologies – we saw this in urachal, we saw this in adenocarcinoma – we really saw this across the board. This is very, very, very intriguing data.”
The phase II trial is ongoing at multiple centers across the country, including the Dana-Farber/Harvard Cancer Center, Boston, the University of Texas MD Anderson Cancer Center, Houston, the Moores Cancer Center at University of California Health, San Diego, the Ohio State University Comprehensive Cancer Center, Columbus, and the Winship Cancer Institute of Emory University, Atlanta.
“We accrued this trial in just under 18 months,” Dr. McGregor said. “I think this shows that with a well-designed trial, we can actually study these diseases and improve outcomes in these patients.” According to Dr. McGregor, the current findings deserve further investigation, potentially including expansion of the BUTCVH cohort. Recruitment is ongoing for a fourth cohort involving patients with tumors that exhibit neuroendocrine differentiation.
Cabozantinib and nivolumab with or without ipilimumab
Dr. Apolo is leading a similar basket trial (NCT02496208) that is testing cabozantinib plus nivolumab with or without ipilimumab.
“What we’re doing is using immunotherapy and a targeted therapy that work in standard urothelial carcinoma and renal cell carcinoma,” Dr. Apolo said. “But really, we don’t know the activity in these rare GU tumors. … There’s still so much we don’t understand about what the driving mutations are, and how we can best target them.”
Most recent data, published in Journal of Clinical Oncology, include 122 patients with metastatic GU tumors, including urothelial carcinoma, clear cell renal cell carcinoma, bladder adenocarcinoma, and other rare GU cancers.2
Among these patients, 54 were in the phase I dose-finding cohort (eight escalating doses) and 64 were in the dose-expansion cohorts.
After a median follow-up of 40.4 months, 64 patients received the dual combination, whereas 56 received the triplet regimen. The ORR for 108 evaluable patients was 38%, including 12 complete responses (11.1%) and 29 partial responses (26.9%). The largest disease cohort, for urothelial carcinoma, included 33 patients and was associated with an ORR of 42.4%, with a complete response rate of 21.2%. Objective response rate was highest for squamous bladder cancer (85.7%; n = 7), followed by clear cell renal carcinoma (62.5%; n = 16), renal medullary cancer (50%; n = 2), penile cancer (44.4%; n = 9), small cell bladder cancer (33.1%; n = 3), bladder adenocarcinoma (20%; n = 15), and prostate cancer (11.1%; n = 9). No responses were seen in six patients with germ cell tumors.
Adding ipilimumab appeared to have a minimal impact on toxicity. Grade 3 or 4 treatment-related adverse events (AEs) occurred in 84% of patients in the dual combination group, compared with 80% receiving the triplet regimen. Most common AEs were hypophosphatemia (16-25%), lipase elevation (20%), fatigue (18-20%), ALT elevation (5-14%), AST elevation (9-11%), diarrhea (9-11%), and thromboembolic event (4-11%). One patient taking the triplet regimen had grade 5 pneumonitis.
These positive phase I results have paved the way for the phase II ICONIC trial (NCT03866382), a national study available through the Alliance Cooperative Group. The trial is currently recruiting, with an estimated enrollment of 224 patients with rare GU tumors.
The ICONIC trial is just one of several studies that Dr. Apolo is conducting for patients with rare GU cancer. “I have several bladder cancer trials where I’m accepting rare GU tumors to enroll,” she said, noting that efficacy signals in these exploratory cohorts may be pursued with expansion studies like ICONIC.
This inclusive strategy is uncovering promising new treatments for some rare GU malignancies, but the rarest of the rare tumor types remain challenging to study, Dr. Apolo said, because very small sample sizes can preclude significant data. “Although we do have the referral base at the NCI, we still get a small number of a lot of rare tumors,” Dr. Apolo said. “What I end up having, a lot of time, are small subsets of rare tumors – I’ll have 4 of one kind, 10 of another.” This situation means that sometimes, time and resources must be focused where they are needed most.
“Sometimes I actually have to decide which are the more common rare tumors so I can study them in a larger cohort,” Dr. Apolo said. “It can have more clinical impact within the community of that rare tumor.” Dr. Apolo described the inherent conflict involved in this decision, but also, its ultimate necessity.
“It’s what you don’t want to do, but you end up doing,” she said. “Because you want to be inclusive and include the rare, rare tumor, but sometimes you just can’t get enough numbers to see if there’s actually a difference [in efficacy]. If it doesn’t work in one patient, does that mean it doesn’t work at all? You need more numbers to really test the efficacy of therapy.”
From clinical trials to clinical practice
To accrue the number of patients needed for practice-altering findings, both Dr. McGregor and Dr. Apolo emphasized the importance of institutional support and collaborative trial designs.
“The FDA is a great ally,” Dr. McGregor said. “They’re acutely aware of the challenges facing patients with rare malignancies – not just GU malignancies. They’re continuing to evaluate the best way to move these drugs forward for those patients. … They’re constantly working with investigators, with industry, looking at data and trying to determine at what threshold these will be practice-changing studies.”
Dr. McGregor suggested that larger trials could shift national guideline recommendations toward combination immunotherapies for patients with rare GU tumors, which would lead to inclusion in compendia, and from there, broader clinical usage.
“At end of the day, luckily, we’re not dealing with drugs that aren’t available,” Dr. McGregor said. “These are drugs that are readily available, approved by the FDA in other settings.”
Dr. Apolo also described strong support from the NCI.
“The NCI really encourages the conduction and enrollment of these rare GU tumor trials, because they understand that the NCI is a really good place to study these rare tumors,” she said. “We have unique resources that make it feasible to conduct some of these trials.”
Dr. Apolo also praised the Alliance Cooperative Group for helping expand patient access to rare GU tumor trials.
“[The Alliance Cooperative Group] makes trials available at community centers across the country,” Dr. Apolo said. “Patients don’t have to travel to the NCI, and they can get the same therapies.”
Still, Dr. Apolo recommended that, when possible, clinicians refer patients with newly diagnosed, rare GU tumors to centers that see a higher number of such cases.
“It’s hard to keep up with all the different treatments that are available right now for different cancers,” Dr. Apolo said. “And sometimes for the rare tumors, there may be great opportunities within a clinical trial that a cancer center may have available that may not be available locally in the community.”
For patients who would like to learn more about rare bladder cancers, Dr. Apolo recommended a visit to the Bladder Cancer Advocacy Network (BCAN) website (bcan.org).
“I’m a big fan of these patient-centered advocacy networks,” Dr. Apolo said. “I like BCAN a lot. It’s a patient-run organization for patients with bladder cancer. With them, I have done a couple of webinars for rare bladder tumors that Ive had some patients tell me are very helpful. They’re a terrific organization that really provides not only emotional support but also educational support for patients that have a diagnosis of bladder cancer and now, rare bladder tumors.” Dr. Spiess offered similar advice for clinicians managing patients with rare GU tumors. He emphasized the key role played by patient advocacy groups, and recommended referral to institutions specializing in specific GU tumor types. For example, he recommended that patients with penile cancer be treated at Moffitt (Tampa) or MD Anderson (Houston), as these centers have the greatest relevant experience. Dr. McGregor disclosed relationships with Bayer, Astellas, Nektar, and others. Dr. Apolo and Dr. Spiess disclosed no conflicts of interest.
References
1.Necchi A et al. Eur Urol. 2021 June;79:S929-30.
2.Apolo AB et al. J Clin Oncol. 2021;39(6_suppl):3.
3.McGregor BA et al. Cancer. 2021 Mar 15;127(6):840-9.
4.McGregor BA and Sonpavde GP. Eur Urol Focus. 2020;6(1):14-16.5.Le Tourneau C et al. J Immunother Cancer. 2018 Oct 22;6(1):111.6.Naing A et al. J Immunother Cancer. 2020;8(1).
7.Raj N et al. J Clin Oncol. 2020;38(1):71-80.
8.Adra N et al. Ann Oncol. 2018;29(1):209-14.
9.Necchi A et al. Eur Urol. 2019;75(1):201-3.
In a field of poor outcomes, few standards of care, and small populations of patients scattered across the world, investigators studying rare genitourinary (GU) cancers are gaining ground through international collaboration and novel trial design.
Fundamental clinical questions in the area remain unanswered, including the value of conventional treatments, such as chemotherapy and surgery, vs. emerging immunotherapy combinations.
Managing patients with rare GU cancers presents a variety of challenges, as does conducting research in the field, according to Philippe E. Spiess, MD, MS, FACS, assistant chief of surgical services and senior member in the department of GU oncology at Moffitt Cancer Center, Tampa.
“Unfortunately, there are limited resources for patients – from an education, from a patient advocacy, and ultimately also from a research standpoint,” Dr. Spiess said in an interview, noting difficulties in attaining funding and reaching meaningful endpoints.
The Global Society of Rare Genitourinary Tumors
Last year Dr. Spiess teamed up with Andrea Necchi, MD, of the department of medical oncology at Fondazione IRCCS Istituto Nazionale dei Tumori, Milan, to found the Global Society of Rare Genitourinary Tumors (GSRGT), the first organization of its kind.
“We’ve formally established a society and gotten some of the world leaders [in the field] … to work with us in developing educational tools and patient advocacy efforts to really promote and improve the care of patients impacted with rare cancers,” Dr. Spiess said.
He went on to highlight the truly global makeup of GSRGT, which includes members from leading centers in North America, South America, Europe, and India, and described it as a “grass-roots” organization that he and Dr. Necchi privately funded without financial backing from pharmaceutical companies.
The first GSRGT summit took place in 2020; it focused on penile and testis cancers and was attended by more than 350 participants. The second summit, planned for March 2022, in a virtual format, will focus on rare kidney cancers and upper tract cancers.
“We’ll definitely be having a lot of important conversations about important unmet needs, and some of the important clinical trials that patients and clinicians should be aware of,” Dr. Spiess said.
Dr. Spiess is currently involved in the International Penile Advanced Cancer Trial(InPACT), which is aiming to enroll 200 patients with squamous cell carcinoma of the penis. The randomized study will compare outcomes across patients treated with standard surgery alone, neoadjuvant chemotherapy plus surgery, and neoadjuvant chemoradiotherapy plus surgery.
“I think this is going to be a landmark study because it’s going to give really baseline high-quality data on the effectiveness of these therapies,” Dr. Spiess said.
Results are expected in 2024.
Basket trials open doors for patients in need
Other investigators are testing immunotherapy combinations in patients with rare GU tumors via nonrandomized basket trials, which widen inclusion criteria and improve local availability.
According to Bradley McGregor, MD, clinical director of the Lank Center for GU Oncology at the Dana-Farber Cancer Institute in Boston, early results from these trials are promising, both in terms of therapeutic efficacy and the approach itself.
“Patients [with rare GU tumors] would come to us saying, ‘Well, what can we do? What trial?’,” Dr. McGregor said. “But really, there was no trial to get them on.”Basket trials are therefore needed, he said, as they accelerate progress in the field and help meet patient needs.
“For some of these relatively rare diseases … there is no standard of care,” Dr. McGregor said. “And low incidence makes it challenging to conduct a dedicated clinical trial. Those patients are left with minimal therapeutic options. … We look to provide care for that unmet need.”Andrea B. Apolo, MD, described similar experiences as head of the bladder cancer section of the GU malignancies branch of the National Cancer Institute (NCI), Bethesda, Md.
“I’ve been at the NCI for the past 10 years and I’ve gotten a lot of referrals for rare tumors,” Dr. Apolo said. “[These patients] have tried all available standard of care options, and therefore are often looking for clinical trials and new drugs – any kind of therapy that may be effective for their disease.”This call for help, along with a growing scientific curiosity, motivated Dr. Apolo to design trials that would include patients who had nowhere else to go.
“I became very interested in … understanding more about the mechanism of tumorigenesis and understanding rare tumors, biologically, within the lab,” she said, “but also clinically, in terms of finding more effective therapies.”
Both Dr. McGregor and Dr. Apolo are currently conducting basket trials for patients with rare GU tumors. While Dr. McGregor is testing a combination of PD-1 inhibitor nivolumab and CTLA-4 inhibitor ipilimumab, Dr. Apolo is exploring the benefit of cabozantinib, a targeted therapy, given with either nivolumab or nivolumab plus ipilimumab.
When asked about these trials, Dr. Spiess said that “basket trials are important because they may give us an understanding of some potentially useful therapies or combinations;” however, he also pointed out their limitations, noting that they may inaccurately characterize the efficacy of given therapies over a broad array of disease entities even if they are of similar histology. As an example, he noted “very different” genomic profiles across squamous cell carcinomas of the pelvis depending on exact anatomical location, suggesting that these differences may affect responses to therapy, citing a recent study in European Urology that he conducted with Dr. Necchi.1
“[Basket trials] are probably not going to be the be-all-end-all,” Dr. Spiess said. “It really requires a global initiative to do these types of studies, which the Global Society of Rare Genitourinary Tumors will allow.”
Exploring immunotherapy combinations
Despite the potential limitations, recent basket trials involving immunotherapy regimens have been associated with overall response rates, in some subgroups, that exceed 35%.2,3
In comparison with previous trials, many of which had response rates in the single digits, or no responses at all, these results are, in Dr. McGregor’s words, “very thought provoking.”Most rare GU malignancies fall into one of four categories: bladder cancer variant histology (BCVH), adrenal tumors, penile squamous cell carcinoma (PSCC), and chemotherapy-refractory germ cell tumors (CRGCT). Among these, BCVH has the strongest evidence supporting clinical use of immunotherapy, based on U.S. approval for urothelial histology, according to Dr. McGregor.4Data supporting immunotherapy for the remaining disease subtypes are scarce. Although pembrolizumab is approved for patients with solid tumors that exhibit microsatellite instability (MSI), MSI is uncommon among patients with rare GU cancers; estimated incidence rates are less than 10%.4
“As such, clinical trials to address this unmet need are imperative,” Dr. McGregor wrote in a recent review article.4
According to Dr. McGregor, programmed death ligand 1 (PD-L1) expression in rare GU tumors may be relatively common in some disease subtypes, such as PSCC, which has a PD-L1 expression rate of up to 60%.4
But rare GU tumor trials involving a single checkpoint inhibitor have produced limited results, if any.
The largest trial for adrenocortical carcinoma (ACC), for example, which included 50 patients, showed that avelumab resulted in an objective response rate (ORR) of just 6%.5
Pembrolizumab was slightly more effective for ACC, based on a trial involving 39 patients, which returned an ORR of 23%, and another trial involving 15 patients that had a 15% ORR.6,7
Two other trials, which tested single-agent pembrolizumab or durvalumab in patients with CRGCT, resulted in no responses at all, whereas a trial testing pembrolizumab alone for penile squamous cell carcinoma was terminated in 2020, citing poor accrual.8,9 Still, the durvalumab trial for CRGCT, led by Dr. Necchi, did offer a glimpse at what might be possible with a combination of immunotherapies. Although no responses were observed among 11 patients who received durvalumab alone, an efficacy signal was observed in a second cohort of 11 patients who were given durvalumab in combination with the CTLA-4 inhibitor tremilimumab.9
Out of those 11 patients, 1 had a partial response, and another achieved stable disease.
In light of these findings, and more that have been published since then, the clinical trial landscape for rare GU tumors is shifting toward a combination immunotherapy approach, according to Dr. McGregor.4
Nivolumab and ipilimumab
Dr. McGregor is leading a phase II trial (NCT03333616) testing a combination of nivolumab and ipilimumab in patients with a variety of advanced rare GU malignancies, including bladder and upper tract carcinoma of variant histology (BUTCVH), adrenal tumors, CRGCT, PSCC, and prostate cancer of variant histology (PCVH).
“When trials are designed, these patients are often forgotten,” Dr. McGregor noted. “We said, let’s do a trial for all rare GU tumors and just sort of assess and look for a signal, and, hopefully, find a signal that we can then take to the next level.”
Along with appropriate disease phenotype, trial eligibility depended upon an ECOG performance status of 0-2 and no prior exposure to checkpoint inhibitors. Treatment-naive patients were allowed. All participants received nivolumab 3 mg/kg and ipilimumab 1 mg/kg IV every 3 weeks for four doses, followed by maintenance nivolumab at a dose of 480 mg every 4 weeks.
Most recent results, published in Cancer, included data from 55 patients, including 19 with BUTCVH, 18 with adrenal tumors, and 18 with other tumors.3 After a median follow-up of 9.9 months, 28 patients (51%) received all four doses of the regimen, 25 of whom received maintenance therapy with a median of four cycles.
Overall, nine patients (16%) responded to therapy, six of whom (67%) maintained their response for at least 9 months. Two responses were complete, and seven were partial. Median progression-free survival was 2.8 months.
Twenty-two patients (39%) had grade 3 or higher treatment-related adverse events, approximately one-quarter (23%) needed high-dose steroids, and a slightly greater proportion (27%) discontinued the regimen because of adverse events. Three patients exhibited grade 5 toxicity, and one patient death was treatment related. A closer look at the efficacy data suggested that one disease subgroup benefited much more than the others. The overall response rate among 19 patients with BUTCVH was 37%, compared with 6% in the other two cohorts.
“A response rate of 37% compares quite favorably to anything we’ve seen to date,” Dr. McGregor said. “It’s remarkable that [this response] was seen across histologies – we saw this in urachal, we saw this in adenocarcinoma – we really saw this across the board. This is very, very, very intriguing data.”
The phase II trial is ongoing at multiple centers across the country, including the Dana-Farber/Harvard Cancer Center, Boston, the University of Texas MD Anderson Cancer Center, Houston, the Moores Cancer Center at University of California Health, San Diego, the Ohio State University Comprehensive Cancer Center, Columbus, and the Winship Cancer Institute of Emory University, Atlanta.
“We accrued this trial in just under 18 months,” Dr. McGregor said. “I think this shows that with a well-designed trial, we can actually study these diseases and improve outcomes in these patients.” According to Dr. McGregor, the current findings deserve further investigation, potentially including expansion of the BUTCVH cohort. Recruitment is ongoing for a fourth cohort involving patients with tumors that exhibit neuroendocrine differentiation.
Cabozantinib and nivolumab with or without ipilimumab
Dr. Apolo is leading a similar basket trial (NCT02496208) that is testing cabozantinib plus nivolumab with or without ipilimumab.
“What we’re doing is using immunotherapy and a targeted therapy that work in standard urothelial carcinoma and renal cell carcinoma,” Dr. Apolo said. “But really, we don’t know the activity in these rare GU tumors. … There’s still so much we don’t understand about what the driving mutations are, and how we can best target them.”
Most recent data, published in Journal of Clinical Oncology, include 122 patients with metastatic GU tumors, including urothelial carcinoma, clear cell renal cell carcinoma, bladder adenocarcinoma, and other rare GU cancers.2
Among these patients, 54 were in the phase I dose-finding cohort (eight escalating doses) and 64 were in the dose-expansion cohorts.
After a median follow-up of 40.4 months, 64 patients received the dual combination, whereas 56 received the triplet regimen. The ORR for 108 evaluable patients was 38%, including 12 complete responses (11.1%) and 29 partial responses (26.9%). The largest disease cohort, for urothelial carcinoma, included 33 patients and was associated with an ORR of 42.4%, with a complete response rate of 21.2%. Objective response rate was highest for squamous bladder cancer (85.7%; n = 7), followed by clear cell renal carcinoma (62.5%; n = 16), renal medullary cancer (50%; n = 2), penile cancer (44.4%; n = 9), small cell bladder cancer (33.1%; n = 3), bladder adenocarcinoma (20%; n = 15), and prostate cancer (11.1%; n = 9). No responses were seen in six patients with germ cell tumors.
Adding ipilimumab appeared to have a minimal impact on toxicity. Grade 3 or 4 treatment-related adverse events (AEs) occurred in 84% of patients in the dual combination group, compared with 80% receiving the triplet regimen. Most common AEs were hypophosphatemia (16-25%), lipase elevation (20%), fatigue (18-20%), ALT elevation (5-14%), AST elevation (9-11%), diarrhea (9-11%), and thromboembolic event (4-11%). One patient taking the triplet regimen had grade 5 pneumonitis.
These positive phase I results have paved the way for the phase II ICONIC trial (NCT03866382), a national study available through the Alliance Cooperative Group. The trial is currently recruiting, with an estimated enrollment of 224 patients with rare GU tumors.
The ICONIC trial is just one of several studies that Dr. Apolo is conducting for patients with rare GU cancer. “I have several bladder cancer trials where I’m accepting rare GU tumors to enroll,” she said, noting that efficacy signals in these exploratory cohorts may be pursued with expansion studies like ICONIC.
This inclusive strategy is uncovering promising new treatments for some rare GU malignancies, but the rarest of the rare tumor types remain challenging to study, Dr. Apolo said, because very small sample sizes can preclude significant data. “Although we do have the referral base at the NCI, we still get a small number of a lot of rare tumors,” Dr. Apolo said. “What I end up having, a lot of time, are small subsets of rare tumors – I’ll have 4 of one kind, 10 of another.” This situation means that sometimes, time and resources must be focused where they are needed most.
“Sometimes I actually have to decide which are the more common rare tumors so I can study them in a larger cohort,” Dr. Apolo said. “It can have more clinical impact within the community of that rare tumor.” Dr. Apolo described the inherent conflict involved in this decision, but also, its ultimate necessity.
“It’s what you don’t want to do, but you end up doing,” she said. “Because you want to be inclusive and include the rare, rare tumor, but sometimes you just can’t get enough numbers to see if there’s actually a difference [in efficacy]. If it doesn’t work in one patient, does that mean it doesn’t work at all? You need more numbers to really test the efficacy of therapy.”
From clinical trials to clinical practice
To accrue the number of patients needed for practice-altering findings, both Dr. McGregor and Dr. Apolo emphasized the importance of institutional support and collaborative trial designs.
“The FDA is a great ally,” Dr. McGregor said. “They’re acutely aware of the challenges facing patients with rare malignancies – not just GU malignancies. They’re continuing to evaluate the best way to move these drugs forward for those patients. … They’re constantly working with investigators, with industry, looking at data and trying to determine at what threshold these will be practice-changing studies.”
Dr. McGregor suggested that larger trials could shift national guideline recommendations toward combination immunotherapies for patients with rare GU tumors, which would lead to inclusion in compendia, and from there, broader clinical usage.
“At end of the day, luckily, we’re not dealing with drugs that aren’t available,” Dr. McGregor said. “These are drugs that are readily available, approved by the FDA in other settings.”
Dr. Apolo also described strong support from the NCI.
“The NCI really encourages the conduction and enrollment of these rare GU tumor trials, because they understand that the NCI is a really good place to study these rare tumors,” she said. “We have unique resources that make it feasible to conduct some of these trials.”
Dr. Apolo also praised the Alliance Cooperative Group for helping expand patient access to rare GU tumor trials.
“[The Alliance Cooperative Group] makes trials available at community centers across the country,” Dr. Apolo said. “Patients don’t have to travel to the NCI, and they can get the same therapies.”
Still, Dr. Apolo recommended that, when possible, clinicians refer patients with newly diagnosed, rare GU tumors to centers that see a higher number of such cases.
“It’s hard to keep up with all the different treatments that are available right now for different cancers,” Dr. Apolo said. “And sometimes for the rare tumors, there may be great opportunities within a clinical trial that a cancer center may have available that may not be available locally in the community.”
For patients who would like to learn more about rare bladder cancers, Dr. Apolo recommended a visit to the Bladder Cancer Advocacy Network (BCAN) website (bcan.org).
“I’m a big fan of these patient-centered advocacy networks,” Dr. Apolo said. “I like BCAN a lot. It’s a patient-run organization for patients with bladder cancer. With them, I have done a couple of webinars for rare bladder tumors that Ive had some patients tell me are very helpful. They’re a terrific organization that really provides not only emotional support but also educational support for patients that have a diagnosis of bladder cancer and now, rare bladder tumors.” Dr. Spiess offered similar advice for clinicians managing patients with rare GU tumors. He emphasized the key role played by patient advocacy groups, and recommended referral to institutions specializing in specific GU tumor types. For example, he recommended that patients with penile cancer be treated at Moffitt (Tampa) or MD Anderson (Houston), as these centers have the greatest relevant experience. Dr. McGregor disclosed relationships with Bayer, Astellas, Nektar, and others. Dr. Apolo and Dr. Spiess disclosed no conflicts of interest.
References
1.Necchi A et al. Eur Urol. 2021 June;79:S929-30.
2.Apolo AB et al. J Clin Oncol. 2021;39(6_suppl):3.
3.McGregor BA et al. Cancer. 2021 Mar 15;127(6):840-9.
4.McGregor BA and Sonpavde GP. Eur Urol Focus. 2020;6(1):14-16.5.Le Tourneau C et al. J Immunother Cancer. 2018 Oct 22;6(1):111.6.Naing A et al. J Immunother Cancer. 2020;8(1).
7.Raj N et al. J Clin Oncol. 2020;38(1):71-80.
8.Adra N et al. Ann Oncol. 2018;29(1):209-14.
9.Necchi A et al. Eur Urol. 2019;75(1):201-3.
Racial, other disparities in blood cancer treatment
As compared with White individuals, minorities often face higher barriers to cancer care. Racial and ethnic disparities in patients with solid tumors, particularly those of the prostate and breast, have been well documented. Hematologic malignancies are less common, but an increasing number of studies have documented disparities within this subgroup of cancer, particularly among Black and non-White Hispanics. An increasing armamentarium of therapeutics, including novel chemotherapy agents and targeted molecular, cellular, and immunologic therapies, has highlighted the need for understanding and exploring the differences in care as well as biology, which may lead to disparate outcomes.
Overall, an estimated 186,400 people living in the United States are expected to be diagnosed with leukemia, lymphoma, or myeloma in 2021, and new cases of hematologic malignancies are expected to account for 9.8% of the estimated 1,898,160 new cancer cases diagnosed this year.1
The underlying reasons for disparities are highly complex and multifactorial, and clinicians must consider how the biologic, clinical, demographic, and socioeconomic characteristics of their patients interact. All of these factors can play a role in prognosis and/or access to care.
Disparities in leukemia
Leukemia is a heterogeneous group of diseases affecting both children and adults, but during the past few decades survival rates have steadily improved, particularly among children. Response to therapy and prognosis do vary among leukemia types, but one large analysis reported that there were overall improvements in survival seen across racial/ethnic groups, most age groups, and genders during a 40-year period.2
From 1973 through 2014, survival trends were assessed across four leukemia types: acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), chronic myeloid leukemia (CML), and chronic lymphoid leukemia (CLL). After stratifying survival for each leukemia type by race/ethnicity, improvement rates were not uniform among all groups.
For example, there were substantial improvements of leukemia-specific survival in 2010-2014 among Black (81.0%) and Asian (80.0%) patients with CML, as well as younger patients (20-49 years) with CLL (96.0%). But in contrast, Black patients, those with AML, and individuals over the age of 75 years experienced the lowest improvement in survival.
Studies have found that Hispanics have increased rates of ALL and acute promyelocytic leukemia (APL), but lower rates of AML, as compared to Whites. They also tend to be diagnosed at a younger age and have poorer overall survival.3
Demographics may also play a role, as Hispanics born outside the United States had a higher incidence rate of APL versus U.S.-born Hispanics (incidence rate ratio, 1.79; 1.11-2.94). Thus, the higher incidence rates of increased B-cell ALL may be due to heritable genetic factors, while APL may also be attributable to environmental exposures.4
Hispanics living on the Texas-Mexico border were also found to have a higher incidence of chronic myeloid leukemia (RR, 1.28; 95% CI, 1.07-1.51; P = .02) and acute myeloid leukemia (RR, 1.17; 95% CI, 1.04-1.33; P = .0009) as compared with Hispanics living elsewhere in Texas5 AML and CML were more likely to be observed in patients who resided in this border region, and those with ALL, AML, and CML had worse outcomes compared with Hispanics living elsewhere in Texas. In addition, both Hispanic and non-Hispanic patients along the border have a worse prognosis for ALL than patients in other areas of Texas.
“We don’t yet understand if the differences are due to nonbiologic factors, or if biology plays a role because of the more aggressive disease that we’re seeing,” said study author Anna Eiring, PhD, an assistant professor at Texas Tech University, El Paso. “This is a medically underserved region, and even though we are a safety net hospital, many of the Hispanic patients don’t have health insurance.”
They also tend to have worse socioeconomic status compared with non-Hispanic populations, and there may also be lifestyle and environmental factors. “Exposure to environmental toxins may also play a role, as many work in jobs that could put them at risk,” she said. “Lifestyle factors may also play a role.”
AML is a hematopoietic disorder that is characterized by numerous cytogenetic and molecular aberrations, with poor overall survival. Researchers found that Black patients had shorter survival than White patients, based on an analysis of Surveillance Epidemiology and End Results (SEER) Program data, and performing and performed mutational profiling of 1,339 patients with AML treated on frontline Alliance for Clinical Trials in Oncology (Alliance) protocols.6 The disparity was especially pronounced in Black patients under 60 years old, after adjustment for socioeconomic (SEER) and molecular (Alliance) factors. Black race was an independent prognosticator of poor survival.
“Based on our analyses in Black and White AML patients under the age of 60 years, we believe that a differential impact of molecular aberrations, specifically AML-associated gene mutations, contribute to the observed survival disparities,” said study author Ann-Kathrin Eisfeld, MD, an assistant professor in the division of hematology at the Ohio State University, Columbus, and a member of the leukemia research program at the university’s comprehensive cancer center, the James. “For example, NPM1 mutations seem to lack the known positive prognostic impact we are used to seeing in previous studies with White AML patients.”
She noted that when looking at molecular prognosticators just within Black AML patients, researchers found that FLT3-ITD and also IDH2 mutations were associated with poor overall survival. “While FLT3-ITD is a known adverse prognosticator, the significant impact of IDH2 mutations was surprising to us and is currently being further explored,” said Dr. Eisfeld.
“In general, however, it can’t be highlighted enough that while this study suggests an impact of somatic tumor genomics that needs a lot more attention and investigation and ideally, also prospective studies, structural racism and its impact is still the problem,” she emphasized. “It’s the ‘elephant in the room’ and the major factor that needs to be addressed in order to improve and overcome these survival disparities.”
Disparities in lymphoma
Similar to leukemia, lymphomas are a heterogenous and diverse group of malignancies that range from indolent to highly aggressive. The two main types are listed below:
Non-Hodgkin lymphoma (NHL), the most common subtype, with about 80,000 new cases a year in the United States. There are more than 90 types of NHL, the most common being B-cell lymphomas, which include diffuse large B cell, primary mediastinal B cell, follicular, small lymphocytic lymphoma, and chronic lymphocytic leukemia; marginal zone, mantle zone, and Burkitt lymphomas; and Waldenström macroglobulinemia.
Hodgkin lymphoma (HL), less common than NHL, with about 9,000 people diagnosed every year. There are five types of HL, and it is primarily seen in children and young adults.
Disparities in incidence, age at diagnosis, and overall survival have been observed in lymphoma, which, aside from marginal zone and follicular lymphoma, are more common among men. The incidence of most lymphoma subtypes is generally lower in racial and ethnic minority groups, although Black and Hispanic patients tend to be diagnosed at a younger age, and in Black patients, at a more advanced stage and the lymphomas have higher risk features at initial presentation.7
One study that looked at racial disparities in Hodgkin lymphoma found that HL was significantly more common in Hispanics versus Whites under the age of 65 years. The 5-, 10-, and 15-year overall survival rates were also inferior for Blacks and Hispanics compared with Whites (P less than 0.005 and P less than 0.001, respectively).8
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma in the United States, comprising approximately one-third of lymphomas diagnosed in adults (Lee et al. 2020). In one study that examined ancestry and tumor genomics, recurrent somatic mutations in established driver genes, such as ATM, MGA, SETD2, TET2, DNMT3A, and MLL3, were observed more frequently in patients with African ancestry versus those of European ancestry.9 Other data suggest a variety of disparities in receipt of treatment. For example, patients with localized disease who were Black, uninsured/Medicaid insured, or of lower socioeconomic status were less likely to receive any form of chemotherapy (all P less than 0.0001), and Black race was also associated with being less likely to receive chemoimmunotherapy.
Leveling the field of disparities is complex and requires a multifaceted approach. But one facility found that they could help minority patients overcome some of the hurdles related to nonbiologic factors by the support of a nurse navigator in addition to therapy.10 Their study included 204 patients with DLBCL (47 minority patients and 157 White patients) and following the initiation of the nurse navigator program, virtually all patients received frontline chemotherapy (98% versus 96%). The incidence of relapsed/refractory disease was similar (40% versus 38%) and in the relapsed/refractory population, similar proportions of patients underwent hematopoietic stem cell transplantation (32% versus 29%) or received chimeric antigen receptor T-cell therapy (16% versus 19%). The 2-year overall survival rates were 81% and 76% for minorities and Whites, respectively, and 2-year progression-free survival rates were 62% and 65%, respectively.
“We found that the minority patients often needed more help to get care, and they utilized the nurse navigator more intensively,” said study author Bei Hu, MD, who is with the department of hematologic oncology and blood disorders, Levine Cancer Institute/Atrium Health, Charlotte, N.C. “The nurse navigator was able to help them with things like finances, transportation, and insurance.”
Minorities tended to face more barriers than White patients. “Even something as simple as needing money for gas to get to the clinic can be a barrier to care,” said Dr. Hu. “And many of the patients are often uncomfortable discussing these things with their physician – plus a lot is covered in our appointments and we focus on the cancer. So, they may be more comfortable discussing these issues with the nurse.”
Disparities in multiple myeloma
Multiple myeloma is the malignant clonal proliferation of plasma B cells in the bone marrow and, despite the advent of new therapies, remains incurable and generally fatal. It progresses from the more common but often subclinical precursor states of monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM) to overt and symptomatic multiple myeloma. Racial disparities have been observed in all stages of the disease, and as compared with Whites, individuals who are Black have a higher risk of MGUS and myeloma and a higher mortality rate.11 They have not experienced the same survival gains seen in White patients.
Some research suggests that these disparities may be more related to socioeconomic status as opposed to race. One analysis of 562 patients found that those with higher socioeconomic status had a median overall survival of 62.8 months compared with 53.7 and 48.6 months for middle and low socioeconomic status (P = 0.015).12
After controlling for confounders including race, patients with low socioeconomic status had a 54% increase in mortality rate relative to those with high status. The authors then performed a similar analysis of 45,505 patients with multiple myeloma from the S
“In some homogeneous health systems, such as the VA, we are seeing that Black patients do as well or better than White patients,” said Catherine Marinac, PhD, an assistant professor of medicine, Harvard Medical School, Boston. “Survival is equal or better, as long as treatment is not delayed and they receive the standard of care.”
Black patients generally have a more indolent disease subtype and may experience less aggressive disease, but they have not experienced the same magnitude in survival as White patients following the introduction of new therapeutics. This disparity lends support to the influence of socioeconomic factors, such as unequal access to novel therapies and/or differences in treatment response, and lower rates of autologous stem cell transplantation.13
However, there are racial/ethnic differences in risk for both myeloma and its premalignant conditions, as well as incidence. Blacks have a twofold increased risk of myeloma compared with White individuals and are diagnosed at younger ages. Differences in myeloma incidence is less marked in other racial/ethnic groups, such as Hispanics, where it is only slightly higher than in Whites at 6.7 per 100,00.11 In contrast, the incidence of myeloma is markedly lower in Asians as compared with non-Hispanic Whites (incidence rate of 3.8 versus 6.2 per 100,000). Black persons also have a markedly higher prevalence of MGUS, and these differences suggest that biology, and clinical characteristics, differ by race or ancestry.
“Mortality among Black patients is also higher,” said Dr. Marinac, who is also on the faculty in the division of population sciences at the Dana Farber Cancer Institute, also in Boston. “The higher mortality rate is driven by the higher incidence.”
There are also differences in the prevalence of immunoglobulin isotypes observed across racial/ethnic groups of MGUS patients, Dr. Marinac explained, which is consistent with the hypothesis that there is a biological basis for disparities arising in precursor lesions.
“What we are looking at now is cancer prevention and early intervention,” she said. “There are well-defined precursors to myeloma, and Blacks are three times more likely to have a precursor condition.”
Early detection of precursors followed by preventing progression to full-blown multiple myeloma is one way of addressing disparities, but right now, there are no real screening guidelines. “Most patients now are diagnosed incidentally, and then the only intervention is to monitor them,” Dr. Marinac said. “At Dana Farber, we are now looking to see if we can refine screening, and then see who may need additional monitoring.”
The Promise study, being conducted at Dana Farber, is recruiting participants to examine the molecular changes that occur when precursor conditions develop into full-blown multiple myeloma and is open to individuals considered to be at high risk: Black race and/or have a first-degree relative with multiple myeloma or one of its precursor conditions.
Dr. Marinac also pointed out that there are ongoing clinical trials that are looking at low-risk early interventions in patients with precursor conditions. “We are now looking at lifestyle and metformin,” she said. “The thought is that if we treat them now, we can prevent myeloma from developing.”
Lessening barriers to care
When trying to tease out the strongest/most prominent reasons for the disparities that have been observed in the care of patients with blood cancers, Stephanie Lee, M.D., M.P.H, professor and associate director of the clinical research division at Fred Hutchinson Cancer Research Center, Seattle, thinks that the problem is truly multifactorial.
“Access has been cited many times because some studies show that if access is equitable, sometimes racial/ethnic minorities do the same as non-Hispanic Whites,” she said. “Same thing with quality of care – if all people are treated on clinical trials, sometimes the outcomes are the same.”
That said, many things have to go right to get the best outcomes, and if one factor isn’t optimal, then treatment may never achieve the success that is possible, she noted.
Considering how complex the issue of disparities is, addressing it can seem daunting. Dr. Lee points out that the place to begin is with clinical trials. “I would like to see more studies that test interventions to correct disparities,” said Dr. Lee. “But I have actually seen in my own work that racial and ethnic minorities are less likely to participate in studies, even survey and observational studies where physical risks are low or nonexistent.”
People are studying how to increase minority participation in clinical trials, but thus far, there isn’t one solution. “As with routine care, there are probably a lot of logistical barriers to trial participation that disproportionately affect minority populations,” she noted. “There is also greater distrust of studies.”
But for now, there are some steps that clinicians can take to start to improve these disparities. “I think we can start inquiring about and documenting barriers to care and clinical trial participation, just like we document other aspects of the social history,” Dr. Lee explained. “Truly understanding the problem is the first step toward trying to solve it.”
References
1. Leukemia & Lymphoma Society. 2021. www.lls.org/facts-and-statistics/facts-and-statistics-overview.
2. Utuama O et al. PLoS One. 2019 Aug 19;14(8):e0220864.
3. Pollyea DA et al. J Cancer Prev Curr Res. 2014;1(1):14-19.
4. Bencomo-Alvarez AE et al. Cancer. 2021 Apr 1;127(7):1068-79.
5. Nabhan C et al. Cancer. 2012 Oct 1;118(19):4842-50.
6. Bhatnagar B et al. Blood. 2020;136(Suppl 1):5-7.
7. Shenoy PJ et al. Cancer. 2011;117:2530-40.
8. Evens AM et al. Ann Oncol. 2012 Aug 1;23(8):2128-37.
9. Lee MJ et al. Cancer. 2020;126:3493-3503.
10. Hu B et al. Cancer. 2021 Jul 21. doi: 10.1002/cncr.33779.
11. Marinac CR et al. Blood Cancer J. 2020 Feb 17;10(2):19.
12. Fiala MA et al. Leuk Lymphoma. 2015;56(9):2643-9.
13. Costa LJ et al. Biol Blood Marrow Transplant. 2015 Apr;21(4):701-6.
As compared with White individuals, minorities often face higher barriers to cancer care. Racial and ethnic disparities in patients with solid tumors, particularly those of the prostate and breast, have been well documented. Hematologic malignancies are less common, but an increasing number of studies have documented disparities within this subgroup of cancer, particularly among Black and non-White Hispanics. An increasing armamentarium of therapeutics, including novel chemotherapy agents and targeted molecular, cellular, and immunologic therapies, has highlighted the need for understanding and exploring the differences in care as well as biology, which may lead to disparate outcomes.
Overall, an estimated 186,400 people living in the United States are expected to be diagnosed with leukemia, lymphoma, or myeloma in 2021, and new cases of hematologic malignancies are expected to account for 9.8% of the estimated 1,898,160 new cancer cases diagnosed this year.1
The underlying reasons for disparities are highly complex and multifactorial, and clinicians must consider how the biologic, clinical, demographic, and socioeconomic characteristics of their patients interact. All of these factors can play a role in prognosis and/or access to care.
Disparities in leukemia
Leukemia is a heterogeneous group of diseases affecting both children and adults, but during the past few decades survival rates have steadily improved, particularly among children. Response to therapy and prognosis do vary among leukemia types, but one large analysis reported that there were overall improvements in survival seen across racial/ethnic groups, most age groups, and genders during a 40-year period.2
From 1973 through 2014, survival trends were assessed across four leukemia types: acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), chronic myeloid leukemia (CML), and chronic lymphoid leukemia (CLL). After stratifying survival for each leukemia type by race/ethnicity, improvement rates were not uniform among all groups.
For example, there were substantial improvements of leukemia-specific survival in 2010-2014 among Black (81.0%) and Asian (80.0%) patients with CML, as well as younger patients (20-49 years) with CLL (96.0%). But in contrast, Black patients, those with AML, and individuals over the age of 75 years experienced the lowest improvement in survival.
Studies have found that Hispanics have increased rates of ALL and acute promyelocytic leukemia (APL), but lower rates of AML, as compared to Whites. They also tend to be diagnosed at a younger age and have poorer overall survival.3
Demographics may also play a role, as Hispanics born outside the United States had a higher incidence rate of APL versus U.S.-born Hispanics (incidence rate ratio, 1.79; 1.11-2.94). Thus, the higher incidence rates of increased B-cell ALL may be due to heritable genetic factors, while APL may also be attributable to environmental exposures.4
Hispanics living on the Texas-Mexico border were also found to have a higher incidence of chronic myeloid leukemia (RR, 1.28; 95% CI, 1.07-1.51; P = .02) and acute myeloid leukemia (RR, 1.17; 95% CI, 1.04-1.33; P = .0009) as compared with Hispanics living elsewhere in Texas5 AML and CML were more likely to be observed in patients who resided in this border region, and those with ALL, AML, and CML had worse outcomes compared with Hispanics living elsewhere in Texas. In addition, both Hispanic and non-Hispanic patients along the border have a worse prognosis for ALL than patients in other areas of Texas.
“We don’t yet understand if the differences are due to nonbiologic factors, or if biology plays a role because of the more aggressive disease that we’re seeing,” said study author Anna Eiring, PhD, an assistant professor at Texas Tech University, El Paso. “This is a medically underserved region, and even though we are a safety net hospital, many of the Hispanic patients don’t have health insurance.”
They also tend to have worse socioeconomic status compared with non-Hispanic populations, and there may also be lifestyle and environmental factors. “Exposure to environmental toxins may also play a role, as many work in jobs that could put them at risk,” she said. “Lifestyle factors may also play a role.”
AML is a hematopoietic disorder that is characterized by numerous cytogenetic and molecular aberrations, with poor overall survival. Researchers found that Black patients had shorter survival than White patients, based on an analysis of Surveillance Epidemiology and End Results (SEER) Program data, and performing and performed mutational profiling of 1,339 patients with AML treated on frontline Alliance for Clinical Trials in Oncology (Alliance) protocols.6 The disparity was especially pronounced in Black patients under 60 years old, after adjustment for socioeconomic (SEER) and molecular (Alliance) factors. Black race was an independent prognosticator of poor survival.
“Based on our analyses in Black and White AML patients under the age of 60 years, we believe that a differential impact of molecular aberrations, specifically AML-associated gene mutations, contribute to the observed survival disparities,” said study author Ann-Kathrin Eisfeld, MD, an assistant professor in the division of hematology at the Ohio State University, Columbus, and a member of the leukemia research program at the university’s comprehensive cancer center, the James. “For example, NPM1 mutations seem to lack the known positive prognostic impact we are used to seeing in previous studies with White AML patients.”
She noted that when looking at molecular prognosticators just within Black AML patients, researchers found that FLT3-ITD and also IDH2 mutations were associated with poor overall survival. “While FLT3-ITD is a known adverse prognosticator, the significant impact of IDH2 mutations was surprising to us and is currently being further explored,” said Dr. Eisfeld.
“In general, however, it can’t be highlighted enough that while this study suggests an impact of somatic tumor genomics that needs a lot more attention and investigation and ideally, also prospective studies, structural racism and its impact is still the problem,” she emphasized. “It’s the ‘elephant in the room’ and the major factor that needs to be addressed in order to improve and overcome these survival disparities.”
Disparities in lymphoma
Similar to leukemia, lymphomas are a heterogenous and diverse group of malignancies that range from indolent to highly aggressive. The two main types are listed below:
Non-Hodgkin lymphoma (NHL), the most common subtype, with about 80,000 new cases a year in the United States. There are more than 90 types of NHL, the most common being B-cell lymphomas, which include diffuse large B cell, primary mediastinal B cell, follicular, small lymphocytic lymphoma, and chronic lymphocytic leukemia; marginal zone, mantle zone, and Burkitt lymphomas; and Waldenström macroglobulinemia.
Hodgkin lymphoma (HL), less common than NHL, with about 9,000 people diagnosed every year. There are five types of HL, and it is primarily seen in children and young adults.
Disparities in incidence, age at diagnosis, and overall survival have been observed in lymphoma, which, aside from marginal zone and follicular lymphoma, are more common among men. The incidence of most lymphoma subtypes is generally lower in racial and ethnic minority groups, although Black and Hispanic patients tend to be diagnosed at a younger age, and in Black patients, at a more advanced stage and the lymphomas have higher risk features at initial presentation.7
One study that looked at racial disparities in Hodgkin lymphoma found that HL was significantly more common in Hispanics versus Whites under the age of 65 years. The 5-, 10-, and 15-year overall survival rates were also inferior for Blacks and Hispanics compared with Whites (P less than 0.005 and P less than 0.001, respectively).8
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma in the United States, comprising approximately one-third of lymphomas diagnosed in adults (Lee et al. 2020). In one study that examined ancestry and tumor genomics, recurrent somatic mutations in established driver genes, such as ATM, MGA, SETD2, TET2, DNMT3A, and MLL3, were observed more frequently in patients with African ancestry versus those of European ancestry.9 Other data suggest a variety of disparities in receipt of treatment. For example, patients with localized disease who were Black, uninsured/Medicaid insured, or of lower socioeconomic status were less likely to receive any form of chemotherapy (all P less than 0.0001), and Black race was also associated with being less likely to receive chemoimmunotherapy.
Leveling the field of disparities is complex and requires a multifaceted approach. But one facility found that they could help minority patients overcome some of the hurdles related to nonbiologic factors by the support of a nurse navigator in addition to therapy.10 Their study included 204 patients with DLBCL (47 minority patients and 157 White patients) and following the initiation of the nurse navigator program, virtually all patients received frontline chemotherapy (98% versus 96%). The incidence of relapsed/refractory disease was similar (40% versus 38%) and in the relapsed/refractory population, similar proportions of patients underwent hematopoietic stem cell transplantation (32% versus 29%) or received chimeric antigen receptor T-cell therapy (16% versus 19%). The 2-year overall survival rates were 81% and 76% for minorities and Whites, respectively, and 2-year progression-free survival rates were 62% and 65%, respectively.
“We found that the minority patients often needed more help to get care, and they utilized the nurse navigator more intensively,” said study author Bei Hu, MD, who is with the department of hematologic oncology and blood disorders, Levine Cancer Institute/Atrium Health, Charlotte, N.C. “The nurse navigator was able to help them with things like finances, transportation, and insurance.”
Minorities tended to face more barriers than White patients. “Even something as simple as needing money for gas to get to the clinic can be a barrier to care,” said Dr. Hu. “And many of the patients are often uncomfortable discussing these things with their physician – plus a lot is covered in our appointments and we focus on the cancer. So, they may be more comfortable discussing these issues with the nurse.”
Disparities in multiple myeloma
Multiple myeloma is the malignant clonal proliferation of plasma B cells in the bone marrow and, despite the advent of new therapies, remains incurable and generally fatal. It progresses from the more common but often subclinical precursor states of monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM) to overt and symptomatic multiple myeloma. Racial disparities have been observed in all stages of the disease, and as compared with Whites, individuals who are Black have a higher risk of MGUS and myeloma and a higher mortality rate.11 They have not experienced the same survival gains seen in White patients.
Some research suggests that these disparities may be more related to socioeconomic status as opposed to race. One analysis of 562 patients found that those with higher socioeconomic status had a median overall survival of 62.8 months compared with 53.7 and 48.6 months for middle and low socioeconomic status (P = 0.015).12
After controlling for confounders including race, patients with low socioeconomic status had a 54% increase in mortality rate relative to those with high status. The authors then performed a similar analysis of 45,505 patients with multiple myeloma from the S
“In some homogeneous health systems, such as the VA, we are seeing that Black patients do as well or better than White patients,” said Catherine Marinac, PhD, an assistant professor of medicine, Harvard Medical School, Boston. “Survival is equal or better, as long as treatment is not delayed and they receive the standard of care.”
Black patients generally have a more indolent disease subtype and may experience less aggressive disease, but they have not experienced the same magnitude in survival as White patients following the introduction of new therapeutics. This disparity lends support to the influence of socioeconomic factors, such as unequal access to novel therapies and/or differences in treatment response, and lower rates of autologous stem cell transplantation.13
However, there are racial/ethnic differences in risk for both myeloma and its premalignant conditions, as well as incidence. Blacks have a twofold increased risk of myeloma compared with White individuals and are diagnosed at younger ages. Differences in myeloma incidence is less marked in other racial/ethnic groups, such as Hispanics, where it is only slightly higher than in Whites at 6.7 per 100,00.11 In contrast, the incidence of myeloma is markedly lower in Asians as compared with non-Hispanic Whites (incidence rate of 3.8 versus 6.2 per 100,000). Black persons also have a markedly higher prevalence of MGUS, and these differences suggest that biology, and clinical characteristics, differ by race or ancestry.
“Mortality among Black patients is also higher,” said Dr. Marinac, who is also on the faculty in the division of population sciences at the Dana Farber Cancer Institute, also in Boston. “The higher mortality rate is driven by the higher incidence.”
There are also differences in the prevalence of immunoglobulin isotypes observed across racial/ethnic groups of MGUS patients, Dr. Marinac explained, which is consistent with the hypothesis that there is a biological basis for disparities arising in precursor lesions.
“What we are looking at now is cancer prevention and early intervention,” she said. “There are well-defined precursors to myeloma, and Blacks are three times more likely to have a precursor condition.”
Early detection of precursors followed by preventing progression to full-blown multiple myeloma is one way of addressing disparities, but right now, there are no real screening guidelines. “Most patients now are diagnosed incidentally, and then the only intervention is to monitor them,” Dr. Marinac said. “At Dana Farber, we are now looking to see if we can refine screening, and then see who may need additional monitoring.”
The Promise study, being conducted at Dana Farber, is recruiting participants to examine the molecular changes that occur when precursor conditions develop into full-blown multiple myeloma and is open to individuals considered to be at high risk: Black race and/or have a first-degree relative with multiple myeloma or one of its precursor conditions.
Dr. Marinac also pointed out that there are ongoing clinical trials that are looking at low-risk early interventions in patients with precursor conditions. “We are now looking at lifestyle and metformin,” she said. “The thought is that if we treat them now, we can prevent myeloma from developing.”
Lessening barriers to care
When trying to tease out the strongest/most prominent reasons for the disparities that have been observed in the care of patients with blood cancers, Stephanie Lee, M.D., M.P.H, professor and associate director of the clinical research division at Fred Hutchinson Cancer Research Center, Seattle, thinks that the problem is truly multifactorial.
“Access has been cited many times because some studies show that if access is equitable, sometimes racial/ethnic minorities do the same as non-Hispanic Whites,” she said. “Same thing with quality of care – if all people are treated on clinical trials, sometimes the outcomes are the same.”
That said, many things have to go right to get the best outcomes, and if one factor isn’t optimal, then treatment may never achieve the success that is possible, she noted.
Considering how complex the issue of disparities is, addressing it can seem daunting. Dr. Lee points out that the place to begin is with clinical trials. “I would like to see more studies that test interventions to correct disparities,” said Dr. Lee. “But I have actually seen in my own work that racial and ethnic minorities are less likely to participate in studies, even survey and observational studies where physical risks are low or nonexistent.”
People are studying how to increase minority participation in clinical trials, but thus far, there isn’t one solution. “As with routine care, there are probably a lot of logistical barriers to trial participation that disproportionately affect minority populations,” she noted. “There is also greater distrust of studies.”
But for now, there are some steps that clinicians can take to start to improve these disparities. “I think we can start inquiring about and documenting barriers to care and clinical trial participation, just like we document other aspects of the social history,” Dr. Lee explained. “Truly understanding the problem is the first step toward trying to solve it.”
References
1. Leukemia & Lymphoma Society. 2021. www.lls.org/facts-and-statistics/facts-and-statistics-overview.
2. Utuama O et al. PLoS One. 2019 Aug 19;14(8):e0220864.
3. Pollyea DA et al. J Cancer Prev Curr Res. 2014;1(1):14-19.
4. Bencomo-Alvarez AE et al. Cancer. 2021 Apr 1;127(7):1068-79.
5. Nabhan C et al. Cancer. 2012 Oct 1;118(19):4842-50.
6. Bhatnagar B et al. Blood. 2020;136(Suppl 1):5-7.
7. Shenoy PJ et al. Cancer. 2011;117:2530-40.
8. Evens AM et al. Ann Oncol. 2012 Aug 1;23(8):2128-37.
9. Lee MJ et al. Cancer. 2020;126:3493-3503.
10. Hu B et al. Cancer. 2021 Jul 21. doi: 10.1002/cncr.33779.
11. Marinac CR et al. Blood Cancer J. 2020 Feb 17;10(2):19.
12. Fiala MA et al. Leuk Lymphoma. 2015;56(9):2643-9.
13. Costa LJ et al. Biol Blood Marrow Transplant. 2015 Apr;21(4):701-6.
As compared with White individuals, minorities often face higher barriers to cancer care. Racial and ethnic disparities in patients with solid tumors, particularly those of the prostate and breast, have been well documented. Hematologic malignancies are less common, but an increasing number of studies have documented disparities within this subgroup of cancer, particularly among Black and non-White Hispanics. An increasing armamentarium of therapeutics, including novel chemotherapy agents and targeted molecular, cellular, and immunologic therapies, has highlighted the need for understanding and exploring the differences in care as well as biology, which may lead to disparate outcomes.
Overall, an estimated 186,400 people living in the United States are expected to be diagnosed with leukemia, lymphoma, or myeloma in 2021, and new cases of hematologic malignancies are expected to account for 9.8% of the estimated 1,898,160 new cancer cases diagnosed this year.1
The underlying reasons for disparities are highly complex and multifactorial, and clinicians must consider how the biologic, clinical, demographic, and socioeconomic characteristics of their patients interact. All of these factors can play a role in prognosis and/or access to care.
Disparities in leukemia
Leukemia is a heterogeneous group of diseases affecting both children and adults, but during the past few decades survival rates have steadily improved, particularly among children. Response to therapy and prognosis do vary among leukemia types, but one large analysis reported that there were overall improvements in survival seen across racial/ethnic groups, most age groups, and genders during a 40-year period.2
From 1973 through 2014, survival trends were assessed across four leukemia types: acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), chronic myeloid leukemia (CML), and chronic lymphoid leukemia (CLL). After stratifying survival for each leukemia type by race/ethnicity, improvement rates were not uniform among all groups.
For example, there were substantial improvements of leukemia-specific survival in 2010-2014 among Black (81.0%) and Asian (80.0%) patients with CML, as well as younger patients (20-49 years) with CLL (96.0%). But in contrast, Black patients, those with AML, and individuals over the age of 75 years experienced the lowest improvement in survival.
Studies have found that Hispanics have increased rates of ALL and acute promyelocytic leukemia (APL), but lower rates of AML, as compared to Whites. They also tend to be diagnosed at a younger age and have poorer overall survival.3
Demographics may also play a role, as Hispanics born outside the United States had a higher incidence rate of APL versus U.S.-born Hispanics (incidence rate ratio, 1.79; 1.11-2.94). Thus, the higher incidence rates of increased B-cell ALL may be due to heritable genetic factors, while APL may also be attributable to environmental exposures.4
Hispanics living on the Texas-Mexico border were also found to have a higher incidence of chronic myeloid leukemia (RR, 1.28; 95% CI, 1.07-1.51; P = .02) and acute myeloid leukemia (RR, 1.17; 95% CI, 1.04-1.33; P = .0009) as compared with Hispanics living elsewhere in Texas5 AML and CML were more likely to be observed in patients who resided in this border region, and those with ALL, AML, and CML had worse outcomes compared with Hispanics living elsewhere in Texas. In addition, both Hispanic and non-Hispanic patients along the border have a worse prognosis for ALL than patients in other areas of Texas.
“We don’t yet understand if the differences are due to nonbiologic factors, or if biology plays a role because of the more aggressive disease that we’re seeing,” said study author Anna Eiring, PhD, an assistant professor at Texas Tech University, El Paso. “This is a medically underserved region, and even though we are a safety net hospital, many of the Hispanic patients don’t have health insurance.”
They also tend to have worse socioeconomic status compared with non-Hispanic populations, and there may also be lifestyle and environmental factors. “Exposure to environmental toxins may also play a role, as many work in jobs that could put them at risk,” she said. “Lifestyle factors may also play a role.”
AML is a hematopoietic disorder that is characterized by numerous cytogenetic and molecular aberrations, with poor overall survival. Researchers found that Black patients had shorter survival than White patients, based on an analysis of Surveillance Epidemiology and End Results (SEER) Program data, and performing and performed mutational profiling of 1,339 patients with AML treated on frontline Alliance for Clinical Trials in Oncology (Alliance) protocols.6 The disparity was especially pronounced in Black patients under 60 years old, after adjustment for socioeconomic (SEER) and molecular (Alliance) factors. Black race was an independent prognosticator of poor survival.
“Based on our analyses in Black and White AML patients under the age of 60 years, we believe that a differential impact of molecular aberrations, specifically AML-associated gene mutations, contribute to the observed survival disparities,” said study author Ann-Kathrin Eisfeld, MD, an assistant professor in the division of hematology at the Ohio State University, Columbus, and a member of the leukemia research program at the university’s comprehensive cancer center, the James. “For example, NPM1 mutations seem to lack the known positive prognostic impact we are used to seeing in previous studies with White AML patients.”
She noted that when looking at molecular prognosticators just within Black AML patients, researchers found that FLT3-ITD and also IDH2 mutations were associated with poor overall survival. “While FLT3-ITD is a known adverse prognosticator, the significant impact of IDH2 mutations was surprising to us and is currently being further explored,” said Dr. Eisfeld.
“In general, however, it can’t be highlighted enough that while this study suggests an impact of somatic tumor genomics that needs a lot more attention and investigation and ideally, also prospective studies, structural racism and its impact is still the problem,” she emphasized. “It’s the ‘elephant in the room’ and the major factor that needs to be addressed in order to improve and overcome these survival disparities.”
Disparities in lymphoma
Similar to leukemia, lymphomas are a heterogenous and diverse group of malignancies that range from indolent to highly aggressive. The two main types are listed below:
Non-Hodgkin lymphoma (NHL), the most common subtype, with about 80,000 new cases a year in the United States. There are more than 90 types of NHL, the most common being B-cell lymphomas, which include diffuse large B cell, primary mediastinal B cell, follicular, small lymphocytic lymphoma, and chronic lymphocytic leukemia; marginal zone, mantle zone, and Burkitt lymphomas; and Waldenström macroglobulinemia.
Hodgkin lymphoma (HL), less common than NHL, with about 9,000 people diagnosed every year. There are five types of HL, and it is primarily seen in children and young adults.
Disparities in incidence, age at diagnosis, and overall survival have been observed in lymphoma, which, aside from marginal zone and follicular lymphoma, are more common among men. The incidence of most lymphoma subtypes is generally lower in racial and ethnic minority groups, although Black and Hispanic patients tend to be diagnosed at a younger age, and in Black patients, at a more advanced stage and the lymphomas have higher risk features at initial presentation.7
One study that looked at racial disparities in Hodgkin lymphoma found that HL was significantly more common in Hispanics versus Whites under the age of 65 years. The 5-, 10-, and 15-year overall survival rates were also inferior for Blacks and Hispanics compared with Whites (P less than 0.005 and P less than 0.001, respectively).8
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma in the United States, comprising approximately one-third of lymphomas diagnosed in adults (Lee et al. 2020). In one study that examined ancestry and tumor genomics, recurrent somatic mutations in established driver genes, such as ATM, MGA, SETD2, TET2, DNMT3A, and MLL3, were observed more frequently in patients with African ancestry versus those of European ancestry.9 Other data suggest a variety of disparities in receipt of treatment. For example, patients with localized disease who were Black, uninsured/Medicaid insured, or of lower socioeconomic status were less likely to receive any form of chemotherapy (all P less than 0.0001), and Black race was also associated with being less likely to receive chemoimmunotherapy.
Leveling the field of disparities is complex and requires a multifaceted approach. But one facility found that they could help minority patients overcome some of the hurdles related to nonbiologic factors by the support of a nurse navigator in addition to therapy.10 Their study included 204 patients with DLBCL (47 minority patients and 157 White patients) and following the initiation of the nurse navigator program, virtually all patients received frontline chemotherapy (98% versus 96%). The incidence of relapsed/refractory disease was similar (40% versus 38%) and in the relapsed/refractory population, similar proportions of patients underwent hematopoietic stem cell transplantation (32% versus 29%) or received chimeric antigen receptor T-cell therapy (16% versus 19%). The 2-year overall survival rates were 81% and 76% for minorities and Whites, respectively, and 2-year progression-free survival rates were 62% and 65%, respectively.
“We found that the minority patients often needed more help to get care, and they utilized the nurse navigator more intensively,” said study author Bei Hu, MD, who is with the department of hematologic oncology and blood disorders, Levine Cancer Institute/Atrium Health, Charlotte, N.C. “The nurse navigator was able to help them with things like finances, transportation, and insurance.”
Minorities tended to face more barriers than White patients. “Even something as simple as needing money for gas to get to the clinic can be a barrier to care,” said Dr. Hu. “And many of the patients are often uncomfortable discussing these things with their physician – plus a lot is covered in our appointments and we focus on the cancer. So, they may be more comfortable discussing these issues with the nurse.”
Disparities in multiple myeloma
Multiple myeloma is the malignant clonal proliferation of plasma B cells in the bone marrow and, despite the advent of new therapies, remains incurable and generally fatal. It progresses from the more common but often subclinical precursor states of monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM) to overt and symptomatic multiple myeloma. Racial disparities have been observed in all stages of the disease, and as compared with Whites, individuals who are Black have a higher risk of MGUS and myeloma and a higher mortality rate.11 They have not experienced the same survival gains seen in White patients.
Some research suggests that these disparities may be more related to socioeconomic status as opposed to race. One analysis of 562 patients found that those with higher socioeconomic status had a median overall survival of 62.8 months compared with 53.7 and 48.6 months for middle and low socioeconomic status (P = 0.015).12
After controlling for confounders including race, patients with low socioeconomic status had a 54% increase in mortality rate relative to those with high status. The authors then performed a similar analysis of 45,505 patients with multiple myeloma from the S
“In some homogeneous health systems, such as the VA, we are seeing that Black patients do as well or better than White patients,” said Catherine Marinac, PhD, an assistant professor of medicine, Harvard Medical School, Boston. “Survival is equal or better, as long as treatment is not delayed and they receive the standard of care.”
Black patients generally have a more indolent disease subtype and may experience less aggressive disease, but they have not experienced the same magnitude in survival as White patients following the introduction of new therapeutics. This disparity lends support to the influence of socioeconomic factors, such as unequal access to novel therapies and/or differences in treatment response, and lower rates of autologous stem cell transplantation.13
However, there are racial/ethnic differences in risk for both myeloma and its premalignant conditions, as well as incidence. Blacks have a twofold increased risk of myeloma compared with White individuals and are diagnosed at younger ages. Differences in myeloma incidence is less marked in other racial/ethnic groups, such as Hispanics, where it is only slightly higher than in Whites at 6.7 per 100,00.11 In contrast, the incidence of myeloma is markedly lower in Asians as compared with non-Hispanic Whites (incidence rate of 3.8 versus 6.2 per 100,000). Black persons also have a markedly higher prevalence of MGUS, and these differences suggest that biology, and clinical characteristics, differ by race or ancestry.
“Mortality among Black patients is also higher,” said Dr. Marinac, who is also on the faculty in the division of population sciences at the Dana Farber Cancer Institute, also in Boston. “The higher mortality rate is driven by the higher incidence.”
There are also differences in the prevalence of immunoglobulin isotypes observed across racial/ethnic groups of MGUS patients, Dr. Marinac explained, which is consistent with the hypothesis that there is a biological basis for disparities arising in precursor lesions.
“What we are looking at now is cancer prevention and early intervention,” she said. “There are well-defined precursors to myeloma, and Blacks are three times more likely to have a precursor condition.”
Early detection of precursors followed by preventing progression to full-blown multiple myeloma is one way of addressing disparities, but right now, there are no real screening guidelines. “Most patients now are diagnosed incidentally, and then the only intervention is to monitor them,” Dr. Marinac said. “At Dana Farber, we are now looking to see if we can refine screening, and then see who may need additional monitoring.”
The Promise study, being conducted at Dana Farber, is recruiting participants to examine the molecular changes that occur when precursor conditions develop into full-blown multiple myeloma and is open to individuals considered to be at high risk: Black race and/or have a first-degree relative with multiple myeloma or one of its precursor conditions.
Dr. Marinac also pointed out that there are ongoing clinical trials that are looking at low-risk early interventions in patients with precursor conditions. “We are now looking at lifestyle and metformin,” she said. “The thought is that if we treat them now, we can prevent myeloma from developing.”
Lessening barriers to care
When trying to tease out the strongest/most prominent reasons for the disparities that have been observed in the care of patients with blood cancers, Stephanie Lee, M.D., M.P.H, professor and associate director of the clinical research division at Fred Hutchinson Cancer Research Center, Seattle, thinks that the problem is truly multifactorial.
“Access has been cited many times because some studies show that if access is equitable, sometimes racial/ethnic minorities do the same as non-Hispanic Whites,” she said. “Same thing with quality of care – if all people are treated on clinical trials, sometimes the outcomes are the same.”
That said, many things have to go right to get the best outcomes, and if one factor isn’t optimal, then treatment may never achieve the success that is possible, she noted.
Considering how complex the issue of disparities is, addressing it can seem daunting. Dr. Lee points out that the place to begin is with clinical trials. “I would like to see more studies that test interventions to correct disparities,” said Dr. Lee. “But I have actually seen in my own work that racial and ethnic minorities are less likely to participate in studies, even survey and observational studies where physical risks are low or nonexistent.”
People are studying how to increase minority participation in clinical trials, but thus far, there isn’t one solution. “As with routine care, there are probably a lot of logistical barriers to trial participation that disproportionately affect minority populations,” she noted. “There is also greater distrust of studies.”
But for now, there are some steps that clinicians can take to start to improve these disparities. “I think we can start inquiring about and documenting barriers to care and clinical trial participation, just like we document other aspects of the social history,” Dr. Lee explained. “Truly understanding the problem is the first step toward trying to solve it.”
References
1. Leukemia & Lymphoma Society. 2021. www.lls.org/facts-and-statistics/facts-and-statistics-overview.
2. Utuama O et al. PLoS One. 2019 Aug 19;14(8):e0220864.
3. Pollyea DA et al. J Cancer Prev Curr Res. 2014;1(1):14-19.
4. Bencomo-Alvarez AE et al. Cancer. 2021 Apr 1;127(7):1068-79.
5. Nabhan C et al. Cancer. 2012 Oct 1;118(19):4842-50.
6. Bhatnagar B et al. Blood. 2020;136(Suppl 1):5-7.
7. Shenoy PJ et al. Cancer. 2011;117:2530-40.
8. Evens AM et al. Ann Oncol. 2012 Aug 1;23(8):2128-37.
9. Lee MJ et al. Cancer. 2020;126:3493-3503.
10. Hu B et al. Cancer. 2021 Jul 21. doi: 10.1002/cncr.33779.
11. Marinac CR et al. Blood Cancer J. 2020 Feb 17;10(2):19.
12. Fiala MA et al. Leuk Lymphoma. 2015;56(9):2643-9.
13. Costa LJ et al. Biol Blood Marrow Transplant. 2015 Apr;21(4):701-6.
Coping with a shattered immune system: COVID and beyond
The co-opting and weakening of the immune system by hematologic malignancies and many of their treatments – and the blunting of the immune system’s response to vaccines – may be more salient during the COVID-19 pandemic than ever before.
Hematologic malignancies have been associated in large cancer-and-COVID-19 registries with more severe COVID-19 outcomes than solid tumors, and COVID-19 mRNA vaccines have yielded suboptimal responses across multiple studies. Clinicians and researchers have no shortage of questions, like what is the optimal timing of vaccines relative to cancer-directed therapy? What is the durability and impact of the immune response? What is the status of the immune system in patients who do not produce antispike antibodies after COVID-19 vaccination?
Moreover, will there be novel nonvaccine strategies – such as antibody cocktails or convalescent plasma – to ensure protection against COVID-19 and other future viral threats? And what really defines immunocompromise today and moving forward?
“We don’t know what we don’t know,” said Jeremy L. Warner, MD, associate professor of medicine (hematology/oncology) and biomedical informatics at Vanderbilt University, Nashville, Tenn., and cofounder of the international COVID-19 and Cancer Consortium. “The immune system is incredibly complex and there are numerous defenses, in addition to the humoral response that we routinely measure.”
Another of the pressing pandemic-time questions for infectious disease specialists working in cancer centers concerns a different infectious threat: measles. “There is a lot of concern in this space about the reported drop in childhood vaccinations and the possibility of measles outbreaks as a follow-up to COVID-19,” said Steven A. Pergam, MD, MPH, associate professor in the vaccine and infectious disease division and the clinical research division of the Fred Hutchinson Cancer Research Center, Seattle Cancer Care Alliance.
Whether recipients of hematopoietic cell transplantation (HCT) and cellular therapy should be revaccinated earlier than 2 years post treatment is a question worthy of preemptive discussion, he said.
What about timing?
“A silver lining of the pandemic is that it’s improving our understanding of response to vaccinations and outcomes with respiratory viruses in patients with hematologic malignancies,” said Samuel Rubinstein, MD, of the division of hematology at the University of North Carolina at Chapel Hill. “We’re going to learn a lot more about how to ensure that our patients are optimally protected from respiratory viruses.”
Dr. Rubinstein focuses on plasma cell disorders, mostly multiple myeloma, and routinely explains to patients consenting to use daratumumab, an anti-CD38 monoclonal antibody, or a BCMA-directed therapy, that these therapies “in particular probably do impair vaccine immune response.”
He has handled the timing of the COVID-19 vaccines – currently boosters, in most cases – as he has with influenza and other immunizations such as the pneumococcal vaccine, administering the vaccines agnostic to therapy unless the patient is about to start daratumumab or a BCMA-directed therapy. In this case, he considers vaccinating and waiting 2 weeks (for an immune response to occur) before starting therapy.
However, “if I have any concern that a delay will result in suboptimal cancer control, then I don’t wait,” Dr. Rubinstein said. Poor control of a primary malignancy has been consistently associated with worse COVID-19–specific outcomes in cancer–COVID-19 studies, he said, including an analysis of almost 5,000 patients recorded to the COVID-19 and Cancer Consortium .1
(The analysis also documented that patients with a hematologic malignancy had an odds ratio of higher COVID-19 severity of 1.7, compared with patients with a solid tumor, and an odds ratio of 30-day mortality of 1.44.)
Ideally, said Dr. Warner, patients will get vaccinated with the COVID-19 vaccines or others, “before starting on any cytotoxic chemotherapy and when they do not have low blood counts or perhaps autoimmune complications of immunotherapy.” However, “perfect being the enemy of good, it’s better to get vaccinated than to wait for the exact ideal time.”
Peter Paul Yu, MD, physician-in-chief at Hartford (Conn.) Healthcare Cancer Institute, said that for most patients, there’s no evidence to support an optimal timing of vaccine administration during the chemotherapy cycle. “We looked into that [to guide administration of the COVID-19 vaccines], thinking there might be some data about influenza vaccination,” he said. “But there isn’t much. … And if we make things more complicated than the evidence suggests, we may have fewer people getting vaccinations.”
The National Comprehensive Cancer Network offered several timing recommendations in its August 2021 COVID-19 vaccination guidance – mainly that patients receiving intensive cytotoxic chemotherapy (such as those on cytarabine/anthracycline-based induction regimens for acute myeloid leukemia) delay COVID-19 vaccination until absolute neutrophil count recovery, and that patients on long-term maintenance therapy (for instance, targeted agents for chronic lymphocytic leukemia or myeloproliferative neoplasms) be vaccinated as soon as possible.
Vaccination should be delayed for at least 3 months, the NCCN noted, following HCT or engineered cell therapy (for example, chimeric antigen receptor [CAR] T cells) “in order to maximize vaccine efficacy.”
More known unknowns
The tempered efficacy of the COVID-19 vaccines in patients with hematologic malignancies “has been shown in multiple studies of multiple myeloma, chronic lymphocytic leukemia (CLL), and other malignancies, and we know it’s true in transplant,” said Dr. Pergam.
In a study of 67 patients with hematologic malignancies at the University of Pittsburgh Medical Center Hillman Cancer Center, for instance, 46.3% did not generate IgG antibodies against the SARS-CoV-2 spike protein receptor–binding domain after completing their two-dose mRNA vaccine series. Patients with B-cell CLL were especially unlikely to develop antibodies.2A much larger study of more than 1,400 patients from investigators at the Mayo Clinics in Rochester, Minn., and Jacksonville, Fla., found that approximately 25% of all patients with hematologic malignancies did not produce antispike IgG antibodies, and that those with the most common B-cell malignancies had the lowest rate of seropositivity (44%-79%).3There’s a clear but challenging delineation between antibody testing in the research space and in clinical practice, however. Various national and cancer societies recommended earlier this year against routine postvaccine serological monitoring outside of clinical trials, and the sources interviewed for this story all emphasized that antibody titer measurements should not guide decisions about boosters or about the precautions advised for patients.
Titers checked at a single point in time do not capture the kinetics, multidimensional nature, or durability of an immune response, Dr. Warner said. “There are papers out there that say zero patients with CCL seroconverted … but they do still have some immunity, and maybe even a lot of immunity.”
Antibody testing can create a false sense of security, or a false sense of dread, he said. Yet in practice, the use of serological monitoring “has been all over the place [with] no consistency … and decisions probably being made at the individual clinic level or health system level,” he said.
To a lesser degree, so have definitions of what composes significant immunocompromise in the context of COVID-19 vaccine eligibility. “The question comes up, what does immunocompromised really mean?” said Dr. Yu, whose institution is a member of the Memorial Sloan Kettering (MSK) Cancer Alliance.
As of September, the MSK Cancer Center had taken a more granular approach to describing moderate to severe immunocompromise than did the Centers for Disease Control and Prevention. The CDC said this level of immunocompromise includes people receiving active cancer treatment for tumors or cancers of the blood, and those who’ve received a stem cell transplant within the past 2 years. MSK extended the recommendation, as it concerns hematologic malignancies, to patients who are within 12 months after treatment with B-cell depleting drugs, patients who have been treated for blood cancers within the last 6 months, and patients who received CAR T therapy within the past 2 years.
Dr. Yu, who was not involved in creating the MSK recommendations for third COVID-19 vaccines, said that he has been thinking more broadly during the pandemic about the notion of immunocompetence. “It’s my opinion that patients with hematologic malignancies, even if they’re not on treatment, are not fully immune competent,” he said. This includes patients with CLL stage 0 and patients with plasma cell dyscrasias who don’t yet meet the criteria for multiple myeloma but have a monoclonal gammopathy, and those with lower-risk myelodysplastic syndromes, he said.
“We’re seeing [variable] recommendations based on expert opinion, and I think that’s justifiable in such a dynamic situation,” Dr. Yu said. “I would [even] argue it’s desirable so we can learn from different approaches” and collect more rigorous observational data.
Immunocompetence needs to be “viewed in the context of the threat,” he added. “COVID changes the equation. … What’s immunocompromised in my mind has changed [from prepandemic times].”
Preparing for measles
Measles lit up on Dr. Pergam’s radar screen in 2019, when an outbreak occurred in nearby Clark County, Wash. This and other outbreaks in New York, California, and other states highlighted declines in measles herd immunity in the United States and prompted him to investigate the seroprevalence of measles antibodies in the Fred Hutchinson Cancer Research Center’s outpatient population.
Of 959 consecutive patients seen at the center, they found, 25% lacked protective antibodies for measles. For patients with hematologic malignancies and those with a history of HCT, seroprevalence was worse: 37% and 54%, respectively, were without the IgG antibodies.4 Measles “is the most contagious human virus we have at the moment,” he said, and “revaccinating people is hard when it comes to cancer because it is a live virus vaccine.”
Vaccine hesitancy, a rise in nonmedical exemptions, and other factors were threatening herd immunity before the pandemic began. Now, with declines in routine childhood medical visits and other vaccination opportunities and resources here and in other countries – and declining immunization rates documented by the CDC in May 2021 – the pandemic has made measles outbreaks more likely, he said. (Measles outbreaks in West Africa on the tail end of the Ebola outbreak in 2014-2015 caused more deaths in children than Ebola, he noted.)
The first priority is vaccination “cocooning,” a strategy that has long been important for patients with hematologic malignancies. But it also possible, Dr. Pergam said, that in the setting of any future community transmission, revaccination for HCT recipients could occur earlier than the standard 2-year post-transplantation recommendation.
In a 2019 position statement endorsed by the American Society for Transplantation and Cellular Therapy, Dr. Pergam and other infectious disease physicians and oncologists provide criteria for considering early revaccination on a case-by-case basis for patients on minimal immunosuppressive therapy who are at least 1-year post transplantation.5
“Our thinking was that there may be lower-risk patients to whom we could offer the vaccine” – patients for whom the risk of developing measles might outweigh the risk of potential vaccine-related complications, he said.
And if there were community cases, he added, there might be a place for testing antibody levels in post-transplant patients, however imperfect the window to immunity may be. “We’re thinking through potential scenarios,” he said. “Oncologists should think about measles again and have it on their back burner.”
References
1. Grivas P et al. Ann Oncol. 2021 Jun;32(6):787-800.
2. Agha ME et al. Open Forum Infect Dis. 2021 July;8(7):ofab353.
3. Greenberger LM et al. Cancer Cell. 2021 Aug 9;39(8):1031-3.
4. Marquis SR et al. JAMA Netw Open. 2021 July;4(7):e2118508.
5. Pergam SA et al. Biol Blood Marrow Transplant. 2019 Nov;25:e321-30.
The co-opting and weakening of the immune system by hematologic malignancies and many of their treatments – and the blunting of the immune system’s response to vaccines – may be more salient during the COVID-19 pandemic than ever before.
Hematologic malignancies have been associated in large cancer-and-COVID-19 registries with more severe COVID-19 outcomes than solid tumors, and COVID-19 mRNA vaccines have yielded suboptimal responses across multiple studies. Clinicians and researchers have no shortage of questions, like what is the optimal timing of vaccines relative to cancer-directed therapy? What is the durability and impact of the immune response? What is the status of the immune system in patients who do not produce antispike antibodies after COVID-19 vaccination?
Moreover, will there be novel nonvaccine strategies – such as antibody cocktails or convalescent plasma – to ensure protection against COVID-19 and other future viral threats? And what really defines immunocompromise today and moving forward?
“We don’t know what we don’t know,” said Jeremy L. Warner, MD, associate professor of medicine (hematology/oncology) and biomedical informatics at Vanderbilt University, Nashville, Tenn., and cofounder of the international COVID-19 and Cancer Consortium. “The immune system is incredibly complex and there are numerous defenses, in addition to the humoral response that we routinely measure.”
Another of the pressing pandemic-time questions for infectious disease specialists working in cancer centers concerns a different infectious threat: measles. “There is a lot of concern in this space about the reported drop in childhood vaccinations and the possibility of measles outbreaks as a follow-up to COVID-19,” said Steven A. Pergam, MD, MPH, associate professor in the vaccine and infectious disease division and the clinical research division of the Fred Hutchinson Cancer Research Center, Seattle Cancer Care Alliance.
Whether recipients of hematopoietic cell transplantation (HCT) and cellular therapy should be revaccinated earlier than 2 years post treatment is a question worthy of preemptive discussion, he said.
What about timing?
“A silver lining of the pandemic is that it’s improving our understanding of response to vaccinations and outcomes with respiratory viruses in patients with hematologic malignancies,” said Samuel Rubinstein, MD, of the division of hematology at the University of North Carolina at Chapel Hill. “We’re going to learn a lot more about how to ensure that our patients are optimally protected from respiratory viruses.”
Dr. Rubinstein focuses on plasma cell disorders, mostly multiple myeloma, and routinely explains to patients consenting to use daratumumab, an anti-CD38 monoclonal antibody, or a BCMA-directed therapy, that these therapies “in particular probably do impair vaccine immune response.”
He has handled the timing of the COVID-19 vaccines – currently boosters, in most cases – as he has with influenza and other immunizations such as the pneumococcal vaccine, administering the vaccines agnostic to therapy unless the patient is about to start daratumumab or a BCMA-directed therapy. In this case, he considers vaccinating and waiting 2 weeks (for an immune response to occur) before starting therapy.
However, “if I have any concern that a delay will result in suboptimal cancer control, then I don’t wait,” Dr. Rubinstein said. Poor control of a primary malignancy has been consistently associated with worse COVID-19–specific outcomes in cancer–COVID-19 studies, he said, including an analysis of almost 5,000 patients recorded to the COVID-19 and Cancer Consortium .1
(The analysis also documented that patients with a hematologic malignancy had an odds ratio of higher COVID-19 severity of 1.7, compared with patients with a solid tumor, and an odds ratio of 30-day mortality of 1.44.)
Ideally, said Dr. Warner, patients will get vaccinated with the COVID-19 vaccines or others, “before starting on any cytotoxic chemotherapy and when they do not have low blood counts or perhaps autoimmune complications of immunotherapy.” However, “perfect being the enemy of good, it’s better to get vaccinated than to wait for the exact ideal time.”
Peter Paul Yu, MD, physician-in-chief at Hartford (Conn.) Healthcare Cancer Institute, said that for most patients, there’s no evidence to support an optimal timing of vaccine administration during the chemotherapy cycle. “We looked into that [to guide administration of the COVID-19 vaccines], thinking there might be some data about influenza vaccination,” he said. “But there isn’t much. … And if we make things more complicated than the evidence suggests, we may have fewer people getting vaccinations.”
The National Comprehensive Cancer Network offered several timing recommendations in its August 2021 COVID-19 vaccination guidance – mainly that patients receiving intensive cytotoxic chemotherapy (such as those on cytarabine/anthracycline-based induction regimens for acute myeloid leukemia) delay COVID-19 vaccination until absolute neutrophil count recovery, and that patients on long-term maintenance therapy (for instance, targeted agents for chronic lymphocytic leukemia or myeloproliferative neoplasms) be vaccinated as soon as possible.
Vaccination should be delayed for at least 3 months, the NCCN noted, following HCT or engineered cell therapy (for example, chimeric antigen receptor [CAR] T cells) “in order to maximize vaccine efficacy.”
More known unknowns
The tempered efficacy of the COVID-19 vaccines in patients with hematologic malignancies “has been shown in multiple studies of multiple myeloma, chronic lymphocytic leukemia (CLL), and other malignancies, and we know it’s true in transplant,” said Dr. Pergam.
In a study of 67 patients with hematologic malignancies at the University of Pittsburgh Medical Center Hillman Cancer Center, for instance, 46.3% did not generate IgG antibodies against the SARS-CoV-2 spike protein receptor–binding domain after completing their two-dose mRNA vaccine series. Patients with B-cell CLL were especially unlikely to develop antibodies.2A much larger study of more than 1,400 patients from investigators at the Mayo Clinics in Rochester, Minn., and Jacksonville, Fla., found that approximately 25% of all patients with hematologic malignancies did not produce antispike IgG antibodies, and that those with the most common B-cell malignancies had the lowest rate of seropositivity (44%-79%).3There’s a clear but challenging delineation between antibody testing in the research space and in clinical practice, however. Various national and cancer societies recommended earlier this year against routine postvaccine serological monitoring outside of clinical trials, and the sources interviewed for this story all emphasized that antibody titer measurements should not guide decisions about boosters or about the precautions advised for patients.
Titers checked at a single point in time do not capture the kinetics, multidimensional nature, or durability of an immune response, Dr. Warner said. “There are papers out there that say zero patients with CCL seroconverted … but they do still have some immunity, and maybe even a lot of immunity.”
Antibody testing can create a false sense of security, or a false sense of dread, he said. Yet in practice, the use of serological monitoring “has been all over the place [with] no consistency … and decisions probably being made at the individual clinic level or health system level,” he said.
To a lesser degree, so have definitions of what composes significant immunocompromise in the context of COVID-19 vaccine eligibility. “The question comes up, what does immunocompromised really mean?” said Dr. Yu, whose institution is a member of the Memorial Sloan Kettering (MSK) Cancer Alliance.
As of September, the MSK Cancer Center had taken a more granular approach to describing moderate to severe immunocompromise than did the Centers for Disease Control and Prevention. The CDC said this level of immunocompromise includes people receiving active cancer treatment for tumors or cancers of the blood, and those who’ve received a stem cell transplant within the past 2 years. MSK extended the recommendation, as it concerns hematologic malignancies, to patients who are within 12 months after treatment with B-cell depleting drugs, patients who have been treated for blood cancers within the last 6 months, and patients who received CAR T therapy within the past 2 years.
Dr. Yu, who was not involved in creating the MSK recommendations for third COVID-19 vaccines, said that he has been thinking more broadly during the pandemic about the notion of immunocompetence. “It’s my opinion that patients with hematologic malignancies, even if they’re not on treatment, are not fully immune competent,” he said. This includes patients with CLL stage 0 and patients with plasma cell dyscrasias who don’t yet meet the criteria for multiple myeloma but have a monoclonal gammopathy, and those with lower-risk myelodysplastic syndromes, he said.
“We’re seeing [variable] recommendations based on expert opinion, and I think that’s justifiable in such a dynamic situation,” Dr. Yu said. “I would [even] argue it’s desirable so we can learn from different approaches” and collect more rigorous observational data.
Immunocompetence needs to be “viewed in the context of the threat,” he added. “COVID changes the equation. … What’s immunocompromised in my mind has changed [from prepandemic times].”
Preparing for measles
Measles lit up on Dr. Pergam’s radar screen in 2019, when an outbreak occurred in nearby Clark County, Wash. This and other outbreaks in New York, California, and other states highlighted declines in measles herd immunity in the United States and prompted him to investigate the seroprevalence of measles antibodies in the Fred Hutchinson Cancer Research Center’s outpatient population.
Of 959 consecutive patients seen at the center, they found, 25% lacked protective antibodies for measles. For patients with hematologic malignancies and those with a history of HCT, seroprevalence was worse: 37% and 54%, respectively, were without the IgG antibodies.4 Measles “is the most contagious human virus we have at the moment,” he said, and “revaccinating people is hard when it comes to cancer because it is a live virus vaccine.”
Vaccine hesitancy, a rise in nonmedical exemptions, and other factors were threatening herd immunity before the pandemic began. Now, with declines in routine childhood medical visits and other vaccination opportunities and resources here and in other countries – and declining immunization rates documented by the CDC in May 2021 – the pandemic has made measles outbreaks more likely, he said. (Measles outbreaks in West Africa on the tail end of the Ebola outbreak in 2014-2015 caused more deaths in children than Ebola, he noted.)
The first priority is vaccination “cocooning,” a strategy that has long been important for patients with hematologic malignancies. But it also possible, Dr. Pergam said, that in the setting of any future community transmission, revaccination for HCT recipients could occur earlier than the standard 2-year post-transplantation recommendation.
In a 2019 position statement endorsed by the American Society for Transplantation and Cellular Therapy, Dr. Pergam and other infectious disease physicians and oncologists provide criteria for considering early revaccination on a case-by-case basis for patients on minimal immunosuppressive therapy who are at least 1-year post transplantation.5
“Our thinking was that there may be lower-risk patients to whom we could offer the vaccine” – patients for whom the risk of developing measles might outweigh the risk of potential vaccine-related complications, he said.
And if there were community cases, he added, there might be a place for testing antibody levels in post-transplant patients, however imperfect the window to immunity may be. “We’re thinking through potential scenarios,” he said. “Oncologists should think about measles again and have it on their back burner.”
References
1. Grivas P et al. Ann Oncol. 2021 Jun;32(6):787-800.
2. Agha ME et al. Open Forum Infect Dis. 2021 July;8(7):ofab353.
3. Greenberger LM et al. Cancer Cell. 2021 Aug 9;39(8):1031-3.
4. Marquis SR et al. JAMA Netw Open. 2021 July;4(7):e2118508.
5. Pergam SA et al. Biol Blood Marrow Transplant. 2019 Nov;25:e321-30.
The co-opting and weakening of the immune system by hematologic malignancies and many of their treatments – and the blunting of the immune system’s response to vaccines – may be more salient during the COVID-19 pandemic than ever before.
Hematologic malignancies have been associated in large cancer-and-COVID-19 registries with more severe COVID-19 outcomes than solid tumors, and COVID-19 mRNA vaccines have yielded suboptimal responses across multiple studies. Clinicians and researchers have no shortage of questions, like what is the optimal timing of vaccines relative to cancer-directed therapy? What is the durability and impact of the immune response? What is the status of the immune system in patients who do not produce antispike antibodies after COVID-19 vaccination?
Moreover, will there be novel nonvaccine strategies – such as antibody cocktails or convalescent plasma – to ensure protection against COVID-19 and other future viral threats? And what really defines immunocompromise today and moving forward?
“We don’t know what we don’t know,” said Jeremy L. Warner, MD, associate professor of medicine (hematology/oncology) and biomedical informatics at Vanderbilt University, Nashville, Tenn., and cofounder of the international COVID-19 and Cancer Consortium. “The immune system is incredibly complex and there are numerous defenses, in addition to the humoral response that we routinely measure.”
Another of the pressing pandemic-time questions for infectious disease specialists working in cancer centers concerns a different infectious threat: measles. “There is a lot of concern in this space about the reported drop in childhood vaccinations and the possibility of measles outbreaks as a follow-up to COVID-19,” said Steven A. Pergam, MD, MPH, associate professor in the vaccine and infectious disease division and the clinical research division of the Fred Hutchinson Cancer Research Center, Seattle Cancer Care Alliance.
Whether recipients of hematopoietic cell transplantation (HCT) and cellular therapy should be revaccinated earlier than 2 years post treatment is a question worthy of preemptive discussion, he said.
What about timing?
“A silver lining of the pandemic is that it’s improving our understanding of response to vaccinations and outcomes with respiratory viruses in patients with hematologic malignancies,” said Samuel Rubinstein, MD, of the division of hematology at the University of North Carolina at Chapel Hill. “We’re going to learn a lot more about how to ensure that our patients are optimally protected from respiratory viruses.”
Dr. Rubinstein focuses on plasma cell disorders, mostly multiple myeloma, and routinely explains to patients consenting to use daratumumab, an anti-CD38 monoclonal antibody, or a BCMA-directed therapy, that these therapies “in particular probably do impair vaccine immune response.”
He has handled the timing of the COVID-19 vaccines – currently boosters, in most cases – as he has with influenza and other immunizations such as the pneumococcal vaccine, administering the vaccines agnostic to therapy unless the patient is about to start daratumumab or a BCMA-directed therapy. In this case, he considers vaccinating and waiting 2 weeks (for an immune response to occur) before starting therapy.
However, “if I have any concern that a delay will result in suboptimal cancer control, then I don’t wait,” Dr. Rubinstein said. Poor control of a primary malignancy has been consistently associated with worse COVID-19–specific outcomes in cancer–COVID-19 studies, he said, including an analysis of almost 5,000 patients recorded to the COVID-19 and Cancer Consortium .1
(The analysis also documented that patients with a hematologic malignancy had an odds ratio of higher COVID-19 severity of 1.7, compared with patients with a solid tumor, and an odds ratio of 30-day mortality of 1.44.)
Ideally, said Dr. Warner, patients will get vaccinated with the COVID-19 vaccines or others, “before starting on any cytotoxic chemotherapy and when they do not have low blood counts or perhaps autoimmune complications of immunotherapy.” However, “perfect being the enemy of good, it’s better to get vaccinated than to wait for the exact ideal time.”
Peter Paul Yu, MD, physician-in-chief at Hartford (Conn.) Healthcare Cancer Institute, said that for most patients, there’s no evidence to support an optimal timing of vaccine administration during the chemotherapy cycle. “We looked into that [to guide administration of the COVID-19 vaccines], thinking there might be some data about influenza vaccination,” he said. “But there isn’t much. … And if we make things more complicated than the evidence suggests, we may have fewer people getting vaccinations.”
The National Comprehensive Cancer Network offered several timing recommendations in its August 2021 COVID-19 vaccination guidance – mainly that patients receiving intensive cytotoxic chemotherapy (such as those on cytarabine/anthracycline-based induction regimens for acute myeloid leukemia) delay COVID-19 vaccination until absolute neutrophil count recovery, and that patients on long-term maintenance therapy (for instance, targeted agents for chronic lymphocytic leukemia or myeloproliferative neoplasms) be vaccinated as soon as possible.
Vaccination should be delayed for at least 3 months, the NCCN noted, following HCT or engineered cell therapy (for example, chimeric antigen receptor [CAR] T cells) “in order to maximize vaccine efficacy.”
More known unknowns
The tempered efficacy of the COVID-19 vaccines in patients with hematologic malignancies “has been shown in multiple studies of multiple myeloma, chronic lymphocytic leukemia (CLL), and other malignancies, and we know it’s true in transplant,” said Dr. Pergam.
In a study of 67 patients with hematologic malignancies at the University of Pittsburgh Medical Center Hillman Cancer Center, for instance, 46.3% did not generate IgG antibodies against the SARS-CoV-2 spike protein receptor–binding domain after completing their two-dose mRNA vaccine series. Patients with B-cell CLL were especially unlikely to develop antibodies.2A much larger study of more than 1,400 patients from investigators at the Mayo Clinics in Rochester, Minn., and Jacksonville, Fla., found that approximately 25% of all patients with hematologic malignancies did not produce antispike IgG antibodies, and that those with the most common B-cell malignancies had the lowest rate of seropositivity (44%-79%).3There’s a clear but challenging delineation between antibody testing in the research space and in clinical practice, however. Various national and cancer societies recommended earlier this year against routine postvaccine serological monitoring outside of clinical trials, and the sources interviewed for this story all emphasized that antibody titer measurements should not guide decisions about boosters or about the precautions advised for patients.
Titers checked at a single point in time do not capture the kinetics, multidimensional nature, or durability of an immune response, Dr. Warner said. “There are papers out there that say zero patients with CCL seroconverted … but they do still have some immunity, and maybe even a lot of immunity.”
Antibody testing can create a false sense of security, or a false sense of dread, he said. Yet in practice, the use of serological monitoring “has been all over the place [with] no consistency … and decisions probably being made at the individual clinic level or health system level,” he said.
To a lesser degree, so have definitions of what composes significant immunocompromise in the context of COVID-19 vaccine eligibility. “The question comes up, what does immunocompromised really mean?” said Dr. Yu, whose institution is a member of the Memorial Sloan Kettering (MSK) Cancer Alliance.
As of September, the MSK Cancer Center had taken a more granular approach to describing moderate to severe immunocompromise than did the Centers for Disease Control and Prevention. The CDC said this level of immunocompromise includes people receiving active cancer treatment for tumors or cancers of the blood, and those who’ve received a stem cell transplant within the past 2 years. MSK extended the recommendation, as it concerns hematologic malignancies, to patients who are within 12 months after treatment with B-cell depleting drugs, patients who have been treated for blood cancers within the last 6 months, and patients who received CAR T therapy within the past 2 years.
Dr. Yu, who was not involved in creating the MSK recommendations for third COVID-19 vaccines, said that he has been thinking more broadly during the pandemic about the notion of immunocompetence. “It’s my opinion that patients with hematologic malignancies, even if they’re not on treatment, are not fully immune competent,” he said. This includes patients with CLL stage 0 and patients with plasma cell dyscrasias who don’t yet meet the criteria for multiple myeloma but have a monoclonal gammopathy, and those with lower-risk myelodysplastic syndromes, he said.
“We’re seeing [variable] recommendations based on expert opinion, and I think that’s justifiable in such a dynamic situation,” Dr. Yu said. “I would [even] argue it’s desirable so we can learn from different approaches” and collect more rigorous observational data.
Immunocompetence needs to be “viewed in the context of the threat,” he added. “COVID changes the equation. … What’s immunocompromised in my mind has changed [from prepandemic times].”
Preparing for measles
Measles lit up on Dr. Pergam’s radar screen in 2019, when an outbreak occurred in nearby Clark County, Wash. This and other outbreaks in New York, California, and other states highlighted declines in measles herd immunity in the United States and prompted him to investigate the seroprevalence of measles antibodies in the Fred Hutchinson Cancer Research Center’s outpatient population.
Of 959 consecutive patients seen at the center, they found, 25% lacked protective antibodies for measles. For patients with hematologic malignancies and those with a history of HCT, seroprevalence was worse: 37% and 54%, respectively, were without the IgG antibodies.4 Measles “is the most contagious human virus we have at the moment,” he said, and “revaccinating people is hard when it comes to cancer because it is a live virus vaccine.”
Vaccine hesitancy, a rise in nonmedical exemptions, and other factors were threatening herd immunity before the pandemic began. Now, with declines in routine childhood medical visits and other vaccination opportunities and resources here and in other countries – and declining immunization rates documented by the CDC in May 2021 – the pandemic has made measles outbreaks more likely, he said. (Measles outbreaks in West Africa on the tail end of the Ebola outbreak in 2014-2015 caused more deaths in children than Ebola, he noted.)
The first priority is vaccination “cocooning,” a strategy that has long been important for patients with hematologic malignancies. But it also possible, Dr. Pergam said, that in the setting of any future community transmission, revaccination for HCT recipients could occur earlier than the standard 2-year post-transplantation recommendation.
In a 2019 position statement endorsed by the American Society for Transplantation and Cellular Therapy, Dr. Pergam and other infectious disease physicians and oncologists provide criteria for considering early revaccination on a case-by-case basis for patients on minimal immunosuppressive therapy who are at least 1-year post transplantation.5
“Our thinking was that there may be lower-risk patients to whom we could offer the vaccine” – patients for whom the risk of developing measles might outweigh the risk of potential vaccine-related complications, he said.
And if there were community cases, he added, there might be a place for testing antibody levels in post-transplant patients, however imperfect the window to immunity may be. “We’re thinking through potential scenarios,” he said. “Oncologists should think about measles again and have it on their back burner.”
References
1. Grivas P et al. Ann Oncol. 2021 Jun;32(6):787-800.
2. Agha ME et al. Open Forum Infect Dis. 2021 July;8(7):ofab353.
3. Greenberger LM et al. Cancer Cell. 2021 Aug 9;39(8):1031-3.
4. Marquis SR et al. JAMA Netw Open. 2021 July;4(7):e2118508.
5. Pergam SA et al. Biol Blood Marrow Transplant. 2019 Nov;25:e321-30.
Precision medicine: A new approach to AML, other blood cancers
The emergence of precision medicine has ushered in a groundbreaking era for the treatment of myeloid malignancies, with the ability to integrate individual molecular data into patient care.
Over the past decade, insights from research focusing on the mutations driving the malignant transformation of myeloid cells have provided the basis for the development of novel targeted therapies.1 With the recent U.S. Food and Drug Administration approval of several novel therapies for different acute myeloid leukemia (AML) indications, the current treatment landscape for AML is evolving rapidly.2
In addition, there has been substantial progress in the development of novel therapeutic strategies for other myeloid neoplasms, with numerous molecularly based therapies in early clinical trials in myeloproliferative neoplasms (MPNs) and myelodysplastic syndromes (MDSs). These advancements have been translated into optimized algorithms for diagnosis, prognostication, and treatment.
AML: Historical perspective
AML comprises a heterogeneous group of blood cell malignancies that require different treatment approaches and confer different prognoses.2 These include acute promyelocytic leukemia (APL) and core binding factor (CBF) AML, both of which have high rates of remission and prolonged survival. The remaining non-APL, non-CBF types can be divided by their cytogenetic-molecular profiles, as well as fitness for intensive chemotherapy. AML can also arise secondary to other myeloid neoplasms, especially after exposure to hypomethylating agents (HMAs), chemotherapy, or irradiation as prior treatment for the primary malignancy.
Historically, anthracycline- and cytarabine-based chemotherapy with or without allogeneic hematopoietic stem-cell transplant (allo-HSCT) was the standard of care in AML treatment with curative intent.1 In the palliative setting, low-dose cytarabine or HMAs were also treatment options. Despite 5 decades of clinical use of these options, researchers have continued to evaluate different dosing schedules of cytosine arabinoside (cytarabine or ara-C) and daunorubicin – the first two agents approved for the treatment of AML – during induction and consolidation treatment phases.
However, recent discoveries have led to the clinical development of targeted agents directed at isocitrate dehydrogenase (IDH), FMS-like tyrosine kinase 3 (FLT3), and BCL2.2 These developments, and the highly anticipated combinations arising from them, continue to challenge traditional treatment approaches, raising the question of whether intensive chemotherapy should remain the optimal standard of care.
Novel therapeutics in AML
Since 2017, several new therapies have been approved for the treatment of AML, including gemtuzumab ozogamicin, two FLT3 inhibitors (gilteritinib and midostaurin), two IDH inhibitors (ivosidenib and enasidenib), a BCL2 inhibitor (venetoclax), an oral HMA agent (azacitidine), a hedgehog inhibitor (glasdegib), and a liposomal formulation of CPX351. In addition, oral decitabine/cedazuridine may be used as an alternative oral HMA in AML, but it is currently the only FDA-approved treatment for chronic myelomonocytic leukemia (CMML) and MDS.2 Because AML subsets are very heterogeneous, an open question remains about how to best integrate these new agents into frontline and salvage combination regimens.
Acute promyelocytic leukemia
APL composes 5%-10% of AML and is characterized by the cytogenetic translocation between chromosomes 15 and 17, which leads to the PML-RAR alpha fusion oncogene and its encoded oncoprotein.2 Two therapies, all-trans retinoic acid (ATRA) and arsenic trioxide, when administered in combination with chemotherapy during induction, have been shown to improve outcomes in APL. At present, the combination of idarubicin and ATRA is the standard-of-care treatment for APL. In addition, patients with high-risk disease have been shown to benefit from the addition of gemtuzumab ozogamicin or anthracyclines.
Core binding factor AML
CBF AML includes patients with the cytogenetic-molecular subsets of inversion 16. Chemotherapy combined with gemtuzumab ozogamicin results in cure rates of 75% or higher and an estimated 5-year survival of 75%. Fludarabine, high-dose cytarabine, and gemtuzumab ozogamicin during induction and consolidation, and an alternative treatment modality (for example, allo-HSCT), for persistent minimal residual disease (MRD) in patients who achieve complete response (CR) is a commonly used regimen. Patients who cannot tolerate this regimen or who have persistent MRD may be treated with an HMA (for instance, decitabine or azacitidine) in combination with venetoclax and gemtuzumab ozogamicin, with the treatment duration adjusted according to MRD status or for 12 months or longer.
Mutations, such as N/KRAS (30%-50%), KIT (25%-30%), and FLT3 (15%-20%), also occur in CBF AML. Targeted agents may also be considered in some cases (for example, dasatinib or avapritinib for KIT mutations; FLT3 inhibitors for FLT3 mutations).
Intensive chemotherapy in younger/fit AML
Several AML regimens have demonstrated better outcomes than the conventional “3 + 7 regimen” (3 days of daunorubicin plus 7 days of cytarabine). Recently, the treatment paradigm has shifted from intensive chemotherapy alone to multidrug combination regimens, including regimens that incorporate targeted therapies, such as FLT3 inhibitors in FLT3-mutated AML, and venetoclax and/or IDH inhibitors as indicated. In addition, the recent FDA approval of oral azacitidine as maintenance therapy for patients in first CR (CR duration, 4 months or less; patients unable to complete the curative intensive chemotherapy) may allow for expanded combination regimens.
Older/unfit patients with AML: Low-intensity therapy
Prior to 2000, the majority of older/unfit patients with AML were offered supportive/palliative treatment. Today, the HMAs azacitidine and decitabine are the most commonly used drugs for the treatment of older/unfit AML. Recently, the FDA approved an oral formulation of decitabine plus oral cedazuridine for the treatment of CMML and MDS. This could provide an opportunity to investigate and develop an effective oral therapy regimen for older/unfit AML, such as oral decitabine/cedazuridine in combination with venetoclax, which may ease administration and improve quality of life for patients in CR post induction in the community setting.
Other studies have shown benefit for combining an HMA with venetoclax in patients with TP53-mutated AML. In addition, triplet regimens may also improve outcomes, with combinations such as HMA plus FLT3 inhibitor (for instance, midostaurin or gilteritinib) with or without venetoclax now being investigated. However, the potential increased risk of myelosuppression also needs to be considered with use of triplet regimens. The results of these and other combinatorial trials are greatly anticipated.
Two oral IDH inhibitors, ivosidenib (IDH1 inhibitor) and enasidenib (IDH2 inhibitor) were recently FDA approved as monotherapy for the treatment of IDH-mutated AML. Combination regimens of IDH inhibitors with chemotherapy are currently being investigated in patients with IDH-mutated AML and appear promising based on preliminary data demonstrating improved response rates and event-free survival.
Other FDA-approved therapies in AML
CPX-351 is a nanoscale liposome with a fixed 5:1 molar ratio of cytarabine and daunorubicin. Results from a phase 3 trial showed that CPX-351 resulted in higher response rates and longer survival compared with 3 + 7 chemotherapy in patients with secondary AML, a subgroup of patients with a very poor prognosis. Additional studies are ongoing, combining CPX-351 with gemtuzumab ozogamicin, venetoclax, and other targeted agents.
Results from a phase 2 trial led to the FDA approval of the hedgehog inhibitor glasdegib when given with low-dose cytarabine. The combination improved survival compared with low-dose cytarabine alone in older/unfit AML and high-risk MDS. However, because of poor survival relative to venetoclax-based combinations, glasdegib is not widely used in clinical practice; other trials exploring combinations with azacitidine and with intensive chemotherapy are ongoing.
Expert perspectives: Future of AML therapy
Amir T. Fathi, MD, associate professor of medicine at Harvard Medical School, Boston, and Farhad Ravandi, MD, professor of medicine at the University of Texas MD Anderson Cancer Center, Houston, are coauthors of a recent review that summarized the current treatment landscape in AML, including areas of evolving research.1
“In the next several years, I am hopeful there will be a series of regulatory approvals of novel, effective agents for myeloid malignancies,” Dr. Fathi explained. “Even if approvals are not as numerous as we’ve seen in AML, any additional effective options would be very welcome.”
Dr. Ravandi also noted that increased understanding of the biology underlying myeloid neoplasms has helped to develop novel therapies.
“As we’ve increased our understanding of the biology of these blood cancers, particularly the mechanisms of leukemogenesis and neoplastic change, we’ve been able to develop more effective therapies in AML,” Dr. Ravandi said.
“In the future, we are likely to see a similar trend in other myeloid neoplasms, such as MDSs and MPNs, as we better understand their underlying pathogenesis,” he further explained.
They both acknowledged that the future treatment paradigm in AML will focus on maximizing the potential of new drug approvals, largely through the development of new combination regimens; however, this could be limited by timely validation and regulatory concerns as the disease has become increasingly segmented into smaller subgroups, each with access to a variety of potentially effective therapies.
Dr. Fathi reported consulting/advisory services for Agios, BMS/Celgene, Astellas, and a variety of other pharmaceutical and biotechnology companies. He also reported receiving research support from Agios, BMS/Celgene, and AbbVie. Dr. Ravandi reported no conflicts of interest.
References
1. Westermann J and Bullinger L. Cancer Biol. 2021 April;S1044-579X(21)00084-5.
2. Kantarjian HM et al. Clin Lymphoma Myeloma Leuk. 2021 Sept;21(9):580-97.
The emergence of precision medicine has ushered in a groundbreaking era for the treatment of myeloid malignancies, with the ability to integrate individual molecular data into patient care.
Over the past decade, insights from research focusing on the mutations driving the malignant transformation of myeloid cells have provided the basis for the development of novel targeted therapies.1 With the recent U.S. Food and Drug Administration approval of several novel therapies for different acute myeloid leukemia (AML) indications, the current treatment landscape for AML is evolving rapidly.2
In addition, there has been substantial progress in the development of novel therapeutic strategies for other myeloid neoplasms, with numerous molecularly based therapies in early clinical trials in myeloproliferative neoplasms (MPNs) and myelodysplastic syndromes (MDSs). These advancements have been translated into optimized algorithms for diagnosis, prognostication, and treatment.
AML: Historical perspective
AML comprises a heterogeneous group of blood cell malignancies that require different treatment approaches and confer different prognoses.2 These include acute promyelocytic leukemia (APL) and core binding factor (CBF) AML, both of which have high rates of remission and prolonged survival. The remaining non-APL, non-CBF types can be divided by their cytogenetic-molecular profiles, as well as fitness for intensive chemotherapy. AML can also arise secondary to other myeloid neoplasms, especially after exposure to hypomethylating agents (HMAs), chemotherapy, or irradiation as prior treatment for the primary malignancy.
Historically, anthracycline- and cytarabine-based chemotherapy with or without allogeneic hematopoietic stem-cell transplant (allo-HSCT) was the standard of care in AML treatment with curative intent.1 In the palliative setting, low-dose cytarabine or HMAs were also treatment options. Despite 5 decades of clinical use of these options, researchers have continued to evaluate different dosing schedules of cytosine arabinoside (cytarabine or ara-C) and daunorubicin – the first two agents approved for the treatment of AML – during induction and consolidation treatment phases.
However, recent discoveries have led to the clinical development of targeted agents directed at isocitrate dehydrogenase (IDH), FMS-like tyrosine kinase 3 (FLT3), and BCL2.2 These developments, and the highly anticipated combinations arising from them, continue to challenge traditional treatment approaches, raising the question of whether intensive chemotherapy should remain the optimal standard of care.
Novel therapeutics in AML
Since 2017, several new therapies have been approved for the treatment of AML, including gemtuzumab ozogamicin, two FLT3 inhibitors (gilteritinib and midostaurin), two IDH inhibitors (ivosidenib and enasidenib), a BCL2 inhibitor (venetoclax), an oral HMA agent (azacitidine), a hedgehog inhibitor (glasdegib), and a liposomal formulation of CPX351. In addition, oral decitabine/cedazuridine may be used as an alternative oral HMA in AML, but it is currently the only FDA-approved treatment for chronic myelomonocytic leukemia (CMML) and MDS.2 Because AML subsets are very heterogeneous, an open question remains about how to best integrate these new agents into frontline and salvage combination regimens.
Acute promyelocytic leukemia
APL composes 5%-10% of AML and is characterized by the cytogenetic translocation between chromosomes 15 and 17, which leads to the PML-RAR alpha fusion oncogene and its encoded oncoprotein.2 Two therapies, all-trans retinoic acid (ATRA) and arsenic trioxide, when administered in combination with chemotherapy during induction, have been shown to improve outcomes in APL. At present, the combination of idarubicin and ATRA is the standard-of-care treatment for APL. In addition, patients with high-risk disease have been shown to benefit from the addition of gemtuzumab ozogamicin or anthracyclines.
Core binding factor AML
CBF AML includes patients with the cytogenetic-molecular subsets of inversion 16. Chemotherapy combined with gemtuzumab ozogamicin results in cure rates of 75% or higher and an estimated 5-year survival of 75%. Fludarabine, high-dose cytarabine, and gemtuzumab ozogamicin during induction and consolidation, and an alternative treatment modality (for example, allo-HSCT), for persistent minimal residual disease (MRD) in patients who achieve complete response (CR) is a commonly used regimen. Patients who cannot tolerate this regimen or who have persistent MRD may be treated with an HMA (for instance, decitabine or azacitidine) in combination with venetoclax and gemtuzumab ozogamicin, with the treatment duration adjusted according to MRD status or for 12 months or longer.
Mutations, such as N/KRAS (30%-50%), KIT (25%-30%), and FLT3 (15%-20%), also occur in CBF AML. Targeted agents may also be considered in some cases (for example, dasatinib or avapritinib for KIT mutations; FLT3 inhibitors for FLT3 mutations).
Intensive chemotherapy in younger/fit AML
Several AML regimens have demonstrated better outcomes than the conventional “3 + 7 regimen” (3 days of daunorubicin plus 7 days of cytarabine). Recently, the treatment paradigm has shifted from intensive chemotherapy alone to multidrug combination regimens, including regimens that incorporate targeted therapies, such as FLT3 inhibitors in FLT3-mutated AML, and venetoclax and/or IDH inhibitors as indicated. In addition, the recent FDA approval of oral azacitidine as maintenance therapy for patients in first CR (CR duration, 4 months or less; patients unable to complete the curative intensive chemotherapy) may allow for expanded combination regimens.
Older/unfit patients with AML: Low-intensity therapy
Prior to 2000, the majority of older/unfit patients with AML were offered supportive/palliative treatment. Today, the HMAs azacitidine and decitabine are the most commonly used drugs for the treatment of older/unfit AML. Recently, the FDA approved an oral formulation of decitabine plus oral cedazuridine for the treatment of CMML and MDS. This could provide an opportunity to investigate and develop an effective oral therapy regimen for older/unfit AML, such as oral decitabine/cedazuridine in combination with venetoclax, which may ease administration and improve quality of life for patients in CR post induction in the community setting.
Other studies have shown benefit for combining an HMA with venetoclax in patients with TP53-mutated AML. In addition, triplet regimens may also improve outcomes, with combinations such as HMA plus FLT3 inhibitor (for instance, midostaurin or gilteritinib) with or without venetoclax now being investigated. However, the potential increased risk of myelosuppression also needs to be considered with use of triplet regimens. The results of these and other combinatorial trials are greatly anticipated.
Two oral IDH inhibitors, ivosidenib (IDH1 inhibitor) and enasidenib (IDH2 inhibitor) were recently FDA approved as monotherapy for the treatment of IDH-mutated AML. Combination regimens of IDH inhibitors with chemotherapy are currently being investigated in patients with IDH-mutated AML and appear promising based on preliminary data demonstrating improved response rates and event-free survival.
Other FDA-approved therapies in AML
CPX-351 is a nanoscale liposome with a fixed 5:1 molar ratio of cytarabine and daunorubicin. Results from a phase 3 trial showed that CPX-351 resulted in higher response rates and longer survival compared with 3 + 7 chemotherapy in patients with secondary AML, a subgroup of patients with a very poor prognosis. Additional studies are ongoing, combining CPX-351 with gemtuzumab ozogamicin, venetoclax, and other targeted agents.
Results from a phase 2 trial led to the FDA approval of the hedgehog inhibitor glasdegib when given with low-dose cytarabine. The combination improved survival compared with low-dose cytarabine alone in older/unfit AML and high-risk MDS. However, because of poor survival relative to venetoclax-based combinations, glasdegib is not widely used in clinical practice; other trials exploring combinations with azacitidine and with intensive chemotherapy are ongoing.
Expert perspectives: Future of AML therapy
Amir T. Fathi, MD, associate professor of medicine at Harvard Medical School, Boston, and Farhad Ravandi, MD, professor of medicine at the University of Texas MD Anderson Cancer Center, Houston, are coauthors of a recent review that summarized the current treatment landscape in AML, including areas of evolving research.1
“In the next several years, I am hopeful there will be a series of regulatory approvals of novel, effective agents for myeloid malignancies,” Dr. Fathi explained. “Even if approvals are not as numerous as we’ve seen in AML, any additional effective options would be very welcome.”
Dr. Ravandi also noted that increased understanding of the biology underlying myeloid neoplasms has helped to develop novel therapies.
“As we’ve increased our understanding of the biology of these blood cancers, particularly the mechanisms of leukemogenesis and neoplastic change, we’ve been able to develop more effective therapies in AML,” Dr. Ravandi said.
“In the future, we are likely to see a similar trend in other myeloid neoplasms, such as MDSs and MPNs, as we better understand their underlying pathogenesis,” he further explained.
They both acknowledged that the future treatment paradigm in AML will focus on maximizing the potential of new drug approvals, largely through the development of new combination regimens; however, this could be limited by timely validation and regulatory concerns as the disease has become increasingly segmented into smaller subgroups, each with access to a variety of potentially effective therapies.
Dr. Fathi reported consulting/advisory services for Agios, BMS/Celgene, Astellas, and a variety of other pharmaceutical and biotechnology companies. He also reported receiving research support from Agios, BMS/Celgene, and AbbVie. Dr. Ravandi reported no conflicts of interest.
References
1. Westermann J and Bullinger L. Cancer Biol. 2021 April;S1044-579X(21)00084-5.
2. Kantarjian HM et al. Clin Lymphoma Myeloma Leuk. 2021 Sept;21(9):580-97.
The emergence of precision medicine has ushered in a groundbreaking era for the treatment of myeloid malignancies, with the ability to integrate individual molecular data into patient care.
Over the past decade, insights from research focusing on the mutations driving the malignant transformation of myeloid cells have provided the basis for the development of novel targeted therapies.1 With the recent U.S. Food and Drug Administration approval of several novel therapies for different acute myeloid leukemia (AML) indications, the current treatment landscape for AML is evolving rapidly.2
In addition, there has been substantial progress in the development of novel therapeutic strategies for other myeloid neoplasms, with numerous molecularly based therapies in early clinical trials in myeloproliferative neoplasms (MPNs) and myelodysplastic syndromes (MDSs). These advancements have been translated into optimized algorithms for diagnosis, prognostication, and treatment.
AML: Historical perspective
AML comprises a heterogeneous group of blood cell malignancies that require different treatment approaches and confer different prognoses.2 These include acute promyelocytic leukemia (APL) and core binding factor (CBF) AML, both of which have high rates of remission and prolonged survival. The remaining non-APL, non-CBF types can be divided by their cytogenetic-molecular profiles, as well as fitness for intensive chemotherapy. AML can also arise secondary to other myeloid neoplasms, especially after exposure to hypomethylating agents (HMAs), chemotherapy, or irradiation as prior treatment for the primary malignancy.
Historically, anthracycline- and cytarabine-based chemotherapy with or without allogeneic hematopoietic stem-cell transplant (allo-HSCT) was the standard of care in AML treatment with curative intent.1 In the palliative setting, low-dose cytarabine or HMAs were also treatment options. Despite 5 decades of clinical use of these options, researchers have continued to evaluate different dosing schedules of cytosine arabinoside (cytarabine or ara-C) and daunorubicin – the first two agents approved for the treatment of AML – during induction and consolidation treatment phases.
However, recent discoveries have led to the clinical development of targeted agents directed at isocitrate dehydrogenase (IDH), FMS-like tyrosine kinase 3 (FLT3), and BCL2.2 These developments, and the highly anticipated combinations arising from them, continue to challenge traditional treatment approaches, raising the question of whether intensive chemotherapy should remain the optimal standard of care.
Novel therapeutics in AML
Since 2017, several new therapies have been approved for the treatment of AML, including gemtuzumab ozogamicin, two FLT3 inhibitors (gilteritinib and midostaurin), two IDH inhibitors (ivosidenib and enasidenib), a BCL2 inhibitor (venetoclax), an oral HMA agent (azacitidine), a hedgehog inhibitor (glasdegib), and a liposomal formulation of CPX351. In addition, oral decitabine/cedazuridine may be used as an alternative oral HMA in AML, but it is currently the only FDA-approved treatment for chronic myelomonocytic leukemia (CMML) and MDS.2 Because AML subsets are very heterogeneous, an open question remains about how to best integrate these new agents into frontline and salvage combination regimens.
Acute promyelocytic leukemia
APL composes 5%-10% of AML and is characterized by the cytogenetic translocation between chromosomes 15 and 17, which leads to the PML-RAR alpha fusion oncogene and its encoded oncoprotein.2 Two therapies, all-trans retinoic acid (ATRA) and arsenic trioxide, when administered in combination with chemotherapy during induction, have been shown to improve outcomes in APL. At present, the combination of idarubicin and ATRA is the standard-of-care treatment for APL. In addition, patients with high-risk disease have been shown to benefit from the addition of gemtuzumab ozogamicin or anthracyclines.
Core binding factor AML
CBF AML includes patients with the cytogenetic-molecular subsets of inversion 16. Chemotherapy combined with gemtuzumab ozogamicin results in cure rates of 75% or higher and an estimated 5-year survival of 75%. Fludarabine, high-dose cytarabine, and gemtuzumab ozogamicin during induction and consolidation, and an alternative treatment modality (for example, allo-HSCT), for persistent minimal residual disease (MRD) in patients who achieve complete response (CR) is a commonly used regimen. Patients who cannot tolerate this regimen or who have persistent MRD may be treated with an HMA (for instance, decitabine or azacitidine) in combination with venetoclax and gemtuzumab ozogamicin, with the treatment duration adjusted according to MRD status or for 12 months or longer.
Mutations, such as N/KRAS (30%-50%), KIT (25%-30%), and FLT3 (15%-20%), also occur in CBF AML. Targeted agents may also be considered in some cases (for example, dasatinib or avapritinib for KIT mutations; FLT3 inhibitors for FLT3 mutations).
Intensive chemotherapy in younger/fit AML
Several AML regimens have demonstrated better outcomes than the conventional “3 + 7 regimen” (3 days of daunorubicin plus 7 days of cytarabine). Recently, the treatment paradigm has shifted from intensive chemotherapy alone to multidrug combination regimens, including regimens that incorporate targeted therapies, such as FLT3 inhibitors in FLT3-mutated AML, and venetoclax and/or IDH inhibitors as indicated. In addition, the recent FDA approval of oral azacitidine as maintenance therapy for patients in first CR (CR duration, 4 months or less; patients unable to complete the curative intensive chemotherapy) may allow for expanded combination regimens.
Older/unfit patients with AML: Low-intensity therapy
Prior to 2000, the majority of older/unfit patients with AML were offered supportive/palliative treatment. Today, the HMAs azacitidine and decitabine are the most commonly used drugs for the treatment of older/unfit AML. Recently, the FDA approved an oral formulation of decitabine plus oral cedazuridine for the treatment of CMML and MDS. This could provide an opportunity to investigate and develop an effective oral therapy regimen for older/unfit AML, such as oral decitabine/cedazuridine in combination with venetoclax, which may ease administration and improve quality of life for patients in CR post induction in the community setting.
Other studies have shown benefit for combining an HMA with venetoclax in patients with TP53-mutated AML. In addition, triplet regimens may also improve outcomes, with combinations such as HMA plus FLT3 inhibitor (for instance, midostaurin or gilteritinib) with or without venetoclax now being investigated. However, the potential increased risk of myelosuppression also needs to be considered with use of triplet regimens. The results of these and other combinatorial trials are greatly anticipated.
Two oral IDH inhibitors, ivosidenib (IDH1 inhibitor) and enasidenib (IDH2 inhibitor) were recently FDA approved as monotherapy for the treatment of IDH-mutated AML. Combination regimens of IDH inhibitors with chemotherapy are currently being investigated in patients with IDH-mutated AML and appear promising based on preliminary data demonstrating improved response rates and event-free survival.
Other FDA-approved therapies in AML
CPX-351 is a nanoscale liposome with a fixed 5:1 molar ratio of cytarabine and daunorubicin. Results from a phase 3 trial showed that CPX-351 resulted in higher response rates and longer survival compared with 3 + 7 chemotherapy in patients with secondary AML, a subgroup of patients with a very poor prognosis. Additional studies are ongoing, combining CPX-351 with gemtuzumab ozogamicin, venetoclax, and other targeted agents.
Results from a phase 2 trial led to the FDA approval of the hedgehog inhibitor glasdegib when given with low-dose cytarabine. The combination improved survival compared with low-dose cytarabine alone in older/unfit AML and high-risk MDS. However, because of poor survival relative to venetoclax-based combinations, glasdegib is not widely used in clinical practice; other trials exploring combinations with azacitidine and with intensive chemotherapy are ongoing.
Expert perspectives: Future of AML therapy
Amir T. Fathi, MD, associate professor of medicine at Harvard Medical School, Boston, and Farhad Ravandi, MD, professor of medicine at the University of Texas MD Anderson Cancer Center, Houston, are coauthors of a recent review that summarized the current treatment landscape in AML, including areas of evolving research.1
“In the next several years, I am hopeful there will be a series of regulatory approvals of novel, effective agents for myeloid malignancies,” Dr. Fathi explained. “Even if approvals are not as numerous as we’ve seen in AML, any additional effective options would be very welcome.”
Dr. Ravandi also noted that increased understanding of the biology underlying myeloid neoplasms has helped to develop novel therapies.
“As we’ve increased our understanding of the biology of these blood cancers, particularly the mechanisms of leukemogenesis and neoplastic change, we’ve been able to develop more effective therapies in AML,” Dr. Ravandi said.
“In the future, we are likely to see a similar trend in other myeloid neoplasms, such as MDSs and MPNs, as we better understand their underlying pathogenesis,” he further explained.
They both acknowledged that the future treatment paradigm in AML will focus on maximizing the potential of new drug approvals, largely through the development of new combination regimens; however, this could be limited by timely validation and regulatory concerns as the disease has become increasingly segmented into smaller subgroups, each with access to a variety of potentially effective therapies.
Dr. Fathi reported consulting/advisory services for Agios, BMS/Celgene, Astellas, and a variety of other pharmaceutical and biotechnology companies. He also reported receiving research support from Agios, BMS/Celgene, and AbbVie. Dr. Ravandi reported no conflicts of interest.
References
1. Westermann J and Bullinger L. Cancer Biol. 2021 April;S1044-579X(21)00084-5.
2. Kantarjian HM et al. Clin Lymphoma Myeloma Leuk. 2021 Sept;21(9):580-97.
NORD: Approaching rare cancers through a diversity lens
The National Organization for Rare Disorders (NORD® ) advocates for all rare disease patients, no matter their race, ethnicity, religion, color, national origin, age, disability, sexual orientation, gender identity, etc. Since its inception in 1983, NORD has advocated for marginalized individuals – people living with rare diseases, diagnosed and undiagnosed – who were excluded from conventional clinical care, research, and drug development.
People living with rare diseases often experience a long and arduous journey to diagnosis, due to a dearth of information in medical textbooks, lack of knowledge in the clinical setting, lack of research, and lack of FDA-approved treatments. Furthermore, a substantial amount of research has shown inequity in access to and quality of health care for marginalized groups, especially Black, Brown, indigenous and people of color (BIPOC). The barriers to be accurately diagnosed and provided quality care by specialists already poses threats to quality and length of life of the community at large, but the additional barriers faced by BIPOC communities have deadly consequences due to the lack of access to culturally proficient health care and access to rare disease specialists, in addition to socioeconomic considerations (i.e., insurance access and medical literacy).
In addition to further delayed diagnosis and inequities in care, people of color are consistently underrepresented in clinical trials and registries, resulting in a lack of diversity in clinical studies and some mystery in how effective therapies will be across diverse populations of patients. Because many rare diseases are genetic and certain genetic conditions disproportionately affect communities of color, having a vast majority of white participants creates significant knowledge gaps that can affect patient care and drug development and effectiveness.
Unfortunately, when looking at the rare cancer population within the rare disease community, the same problems persist. Of the approximately 7,000 known rare diseases, 1 more than 500 are rare cancers, 2 and combined, all rare cancers account for slightly more than one out of ever four cancer diagnoses each year and one out of every four cancer-related deaths. 3 Black people have the highest death rate and shortest survival of any racial/ethnic group in the U.S. for most cancers, and Black men have the highest cancer incidence rate. 4 NORD and the NORD Rare Cancer Coalition™, including 27 rare cancer member organizations, are committed to shining a light on the causes of these inequities for rare cancer patients, including but not limited to systemic racism, economic disparities, cultural differences, and issues concerning access to quality health care and inclusive research.
To raise awareness of rare cancers and the issues rare cancer patients face throughout the diagnostic odyssey, in seeking and receiving specialized care and in advocating for awareness, and increased research and drug development, NORD and the NORD Rare Cancer Coalition spearheaded Rare Cancer Day, observed annually on September 30. Through the universal hashtag campaign #RareCancerDay and our social media toolkit of infographics and messaging, NORD brings together the global community of advocates to promote awareness of rare cancers and provide opportunities to educate patients, caregivers, clinicians, and researchers. NORD hosted a free webinar for the rare disease community, Rare Cancers: Breaking Down Barriers to Diagnosis, Treatment and Research, to explore rare cancer challenges and offer insights to assist those who are impacted. Throughout August and September, NORD highlighted the powerful, important, and inspiring stories of the rare cancer community on the NORD blog.
In addition, the 2021 NORD Rare Diseases + Orphan Products Breakthrough Summit, held October 18 and 19, featured a breakout session and a follow-up discussion group on Advancing Rare Cancer Awareness & Education Among Healthcare Professionals. These sessions explored educational gaps and approaches for increasing awareness and delivering quality education for healthcare professionals in optimizing care for rare cancer patients, genomic testing, personalized medicine, and collaboration with researchers and patient advocacy groups.
This issue of Rare Diseases Report: Cancers helps us further our mission to foster the identification, treatment, and cure of rare disorders through programs of education, advocacy, research, and patient services, as well as the work of NORD’s Rare Cancer Coalition™ which aims to unite NORD member organizations working in rare cancers to collaborate on issues facing the greater rare cancer community.
NORD remains steadfastly committed to advocating for all rare disease patients, no matter their race, ethnicity, religion, color, national origin, age, disability, sexual orientation, gender identity, parental status, marital status, political affiliation, gender expression, mental illness, socioeconomic status or background, neuro(a)typicality, or physical appearance. NORD’s work includes advocating for rare cancer patients, raising awareness of rare cancer patients, sharing the stories of people living with rare cancers, and educating patients, caregivers and healthcare professionals about accurate diagnosis, quality care, advancements in research, and available treatment options. Learn more at rarediseases.org.
Rebecca Aune
Director of Education Programs
Debbie Drell
Director of Membership
References
1. Genetic and Rare Diseases Information Center; National Center for Advancing Translational Sciences; FAQs About Rare Diseases; 11/30/2017. https://rarediseases.info.nih.gov/diseases/pages/31/faqs-about-rare-diseases
2. Genetic and Rare Diseases Information Center; National Center for Advancing Translational Sciences; Rare Cancers; 1/25/2019. https://www.youtube.com/watch?v=ES5KylRT1qY, https://rarediseases.info.nih.gov/diseases/diseases-by-category/1/rare-cancers, or https://rarediseases.info.nih.gov/diseases/diseases-by-category/1/rare-cancers
3. NIH National Cancer Institute. Rare Cancer Statistics | Did You Know? [Video]. Youtube. https://www.youtube.com/watch?v=ES5KylRT1qY&t=155s. Published April 5, 2018. Accessed Oct. 20, 2021.
4. American Cancer Society. Cancer Facts; Figures for African Americans 2019-2021. Atlanta: American Cancer Society, 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-african-americans/cancer-facts-and-figures-for-african-americans-2019-2021.pdf1.
The National Organization for Rare Disorders (NORD® ) advocates for all rare disease patients, no matter their race, ethnicity, religion, color, national origin, age, disability, sexual orientation, gender identity, etc. Since its inception in 1983, NORD has advocated for marginalized individuals – people living with rare diseases, diagnosed and undiagnosed – who were excluded from conventional clinical care, research, and drug development.
People living with rare diseases often experience a long and arduous journey to diagnosis, due to a dearth of information in medical textbooks, lack of knowledge in the clinical setting, lack of research, and lack of FDA-approved treatments. Furthermore, a substantial amount of research has shown inequity in access to and quality of health care for marginalized groups, especially Black, Brown, indigenous and people of color (BIPOC). The barriers to be accurately diagnosed and provided quality care by specialists already poses threats to quality and length of life of the community at large, but the additional barriers faced by BIPOC communities have deadly consequences due to the lack of access to culturally proficient health care and access to rare disease specialists, in addition to socioeconomic considerations (i.e., insurance access and medical literacy).
In addition to further delayed diagnosis and inequities in care, people of color are consistently underrepresented in clinical trials and registries, resulting in a lack of diversity in clinical studies and some mystery in how effective therapies will be across diverse populations of patients. Because many rare diseases are genetic and certain genetic conditions disproportionately affect communities of color, having a vast majority of white participants creates significant knowledge gaps that can affect patient care and drug development and effectiveness.
Unfortunately, when looking at the rare cancer population within the rare disease community, the same problems persist. Of the approximately 7,000 known rare diseases, 1 more than 500 are rare cancers, 2 and combined, all rare cancers account for slightly more than one out of ever four cancer diagnoses each year and one out of every four cancer-related deaths. 3 Black people have the highest death rate and shortest survival of any racial/ethnic group in the U.S. for most cancers, and Black men have the highest cancer incidence rate. 4 NORD and the NORD Rare Cancer Coalition™, including 27 rare cancer member organizations, are committed to shining a light on the causes of these inequities for rare cancer patients, including but not limited to systemic racism, economic disparities, cultural differences, and issues concerning access to quality health care and inclusive research.
To raise awareness of rare cancers and the issues rare cancer patients face throughout the diagnostic odyssey, in seeking and receiving specialized care and in advocating for awareness, and increased research and drug development, NORD and the NORD Rare Cancer Coalition spearheaded Rare Cancer Day, observed annually on September 30. Through the universal hashtag campaign #RareCancerDay and our social media toolkit of infographics and messaging, NORD brings together the global community of advocates to promote awareness of rare cancers and provide opportunities to educate patients, caregivers, clinicians, and researchers. NORD hosted a free webinar for the rare disease community, Rare Cancers: Breaking Down Barriers to Diagnosis, Treatment and Research, to explore rare cancer challenges and offer insights to assist those who are impacted. Throughout August and September, NORD highlighted the powerful, important, and inspiring stories of the rare cancer community on the NORD blog.
In addition, the 2021 NORD Rare Diseases + Orphan Products Breakthrough Summit, held October 18 and 19, featured a breakout session and a follow-up discussion group on Advancing Rare Cancer Awareness & Education Among Healthcare Professionals. These sessions explored educational gaps and approaches for increasing awareness and delivering quality education for healthcare professionals in optimizing care for rare cancer patients, genomic testing, personalized medicine, and collaboration with researchers and patient advocacy groups.
This issue of Rare Diseases Report: Cancers helps us further our mission to foster the identification, treatment, and cure of rare disorders through programs of education, advocacy, research, and patient services, as well as the work of NORD’s Rare Cancer Coalition™ which aims to unite NORD member organizations working in rare cancers to collaborate on issues facing the greater rare cancer community.
NORD remains steadfastly committed to advocating for all rare disease patients, no matter their race, ethnicity, religion, color, national origin, age, disability, sexual orientation, gender identity, parental status, marital status, political affiliation, gender expression, mental illness, socioeconomic status or background, neuro(a)typicality, or physical appearance. NORD’s work includes advocating for rare cancer patients, raising awareness of rare cancer patients, sharing the stories of people living with rare cancers, and educating patients, caregivers and healthcare professionals about accurate diagnosis, quality care, advancements in research, and available treatment options. Learn more at rarediseases.org.
Rebecca Aune
Director of Education Programs
Debbie Drell
Director of Membership
References
1. Genetic and Rare Diseases Information Center; National Center for Advancing Translational Sciences; FAQs About Rare Diseases; 11/30/2017. https://rarediseases.info.nih.gov/diseases/pages/31/faqs-about-rare-diseases
2. Genetic and Rare Diseases Information Center; National Center for Advancing Translational Sciences; Rare Cancers; 1/25/2019. https://www.youtube.com/watch?v=ES5KylRT1qY, https://rarediseases.info.nih.gov/diseases/diseases-by-category/1/rare-cancers, or https://rarediseases.info.nih.gov/diseases/diseases-by-category/1/rare-cancers
3. NIH National Cancer Institute. Rare Cancer Statistics | Did You Know? [Video]. Youtube. https://www.youtube.com/watch?v=ES5KylRT1qY&t=155s. Published April 5, 2018. Accessed Oct. 20, 2021.
4. American Cancer Society. Cancer Facts; Figures for African Americans 2019-2021. Atlanta: American Cancer Society, 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-african-americans/cancer-facts-and-figures-for-african-americans-2019-2021.pdf1.
The National Organization for Rare Disorders (NORD® ) advocates for all rare disease patients, no matter their race, ethnicity, religion, color, national origin, age, disability, sexual orientation, gender identity, etc. Since its inception in 1983, NORD has advocated for marginalized individuals – people living with rare diseases, diagnosed and undiagnosed – who were excluded from conventional clinical care, research, and drug development.
People living with rare diseases often experience a long and arduous journey to diagnosis, due to a dearth of information in medical textbooks, lack of knowledge in the clinical setting, lack of research, and lack of FDA-approved treatments. Furthermore, a substantial amount of research has shown inequity in access to and quality of health care for marginalized groups, especially Black, Brown, indigenous and people of color (BIPOC). The barriers to be accurately diagnosed and provided quality care by specialists already poses threats to quality and length of life of the community at large, but the additional barriers faced by BIPOC communities have deadly consequences due to the lack of access to culturally proficient health care and access to rare disease specialists, in addition to socioeconomic considerations (i.e., insurance access and medical literacy).
In addition to further delayed diagnosis and inequities in care, people of color are consistently underrepresented in clinical trials and registries, resulting in a lack of diversity in clinical studies and some mystery in how effective therapies will be across diverse populations of patients. Because many rare diseases are genetic and certain genetic conditions disproportionately affect communities of color, having a vast majority of white participants creates significant knowledge gaps that can affect patient care and drug development and effectiveness.
Unfortunately, when looking at the rare cancer population within the rare disease community, the same problems persist. Of the approximately 7,000 known rare diseases, 1 more than 500 are rare cancers, 2 and combined, all rare cancers account for slightly more than one out of ever four cancer diagnoses each year and one out of every four cancer-related deaths. 3 Black people have the highest death rate and shortest survival of any racial/ethnic group in the U.S. for most cancers, and Black men have the highest cancer incidence rate. 4 NORD and the NORD Rare Cancer Coalition™, including 27 rare cancer member organizations, are committed to shining a light on the causes of these inequities for rare cancer patients, including but not limited to systemic racism, economic disparities, cultural differences, and issues concerning access to quality health care and inclusive research.
To raise awareness of rare cancers and the issues rare cancer patients face throughout the diagnostic odyssey, in seeking and receiving specialized care and in advocating for awareness, and increased research and drug development, NORD and the NORD Rare Cancer Coalition spearheaded Rare Cancer Day, observed annually on September 30. Through the universal hashtag campaign #RareCancerDay and our social media toolkit of infographics and messaging, NORD brings together the global community of advocates to promote awareness of rare cancers and provide opportunities to educate patients, caregivers, clinicians, and researchers. NORD hosted a free webinar for the rare disease community, Rare Cancers: Breaking Down Barriers to Diagnosis, Treatment and Research, to explore rare cancer challenges and offer insights to assist those who are impacted. Throughout August and September, NORD highlighted the powerful, important, and inspiring stories of the rare cancer community on the NORD blog.
In addition, the 2021 NORD Rare Diseases + Orphan Products Breakthrough Summit, held October 18 and 19, featured a breakout session and a follow-up discussion group on Advancing Rare Cancer Awareness & Education Among Healthcare Professionals. These sessions explored educational gaps and approaches for increasing awareness and delivering quality education for healthcare professionals in optimizing care for rare cancer patients, genomic testing, personalized medicine, and collaboration with researchers and patient advocacy groups.
This issue of Rare Diseases Report: Cancers helps us further our mission to foster the identification, treatment, and cure of rare disorders through programs of education, advocacy, research, and patient services, as well as the work of NORD’s Rare Cancer Coalition™ which aims to unite NORD member organizations working in rare cancers to collaborate on issues facing the greater rare cancer community.
NORD remains steadfastly committed to advocating for all rare disease patients, no matter their race, ethnicity, religion, color, national origin, age, disability, sexual orientation, gender identity, parental status, marital status, political affiliation, gender expression, mental illness, socioeconomic status or background, neuro(a)typicality, or physical appearance. NORD’s work includes advocating for rare cancer patients, raising awareness of rare cancer patients, sharing the stories of people living with rare cancers, and educating patients, caregivers and healthcare professionals about accurate diagnosis, quality care, advancements in research, and available treatment options. Learn more at rarediseases.org.
Rebecca Aune
Director of Education Programs
Debbie Drell
Director of Membership
References
1. Genetic and Rare Diseases Information Center; National Center for Advancing Translational Sciences; FAQs About Rare Diseases; 11/30/2017. https://rarediseases.info.nih.gov/diseases/pages/31/faqs-about-rare-diseases
2. Genetic and Rare Diseases Information Center; National Center for Advancing Translational Sciences; Rare Cancers; 1/25/2019. https://www.youtube.com/watch?v=ES5KylRT1qY, https://rarediseases.info.nih.gov/diseases/diseases-by-category/1/rare-cancers, or https://rarediseases.info.nih.gov/diseases/diseases-by-category/1/rare-cancers
3. NIH National Cancer Institute. Rare Cancer Statistics | Did You Know? [Video]. Youtube. https://www.youtube.com/watch?v=ES5KylRT1qY&t=155s. Published April 5, 2018. Accessed Oct. 20, 2021.
4. American Cancer Society. Cancer Facts; Figures for African Americans 2019-2021. Atlanta: American Cancer Society, 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-african-americans/cancer-facts-and-figures-for-african-americans-2019-2021.pdf1.