User login
Child of The New Gastroenterologist
Top 12 tips for research success in fellowship and early academic faculty years
Congratulations! You have matched in a competitive medical subspecialty or you have secured your first faculty position. But what do you do now? Success in your early career – as a new fellow or a new attending – requires both hard work and perseverance. We present our top 12 tips for how to be successful as you transition into your new position.
Tip #1: Be kind to yourself
As you transition from medical resident to GI fellow or from GI fellow to first-time attending, it is important to recognize that you are going through a major career transition (not as major as fourth year to intern, but probably a close second). First and foremost, remember to be kind to yourself and set reasonable expectations. You need to allow yourself time to transition to a new role which may also be in a new city or state. Take care of yourself – don’t forget to exercise, eat well, and sleep. You are in the long game now. Work to get yourself in a routine that is sustainable. Block out time to exercise, explore your new city, meal plan, and pursue your interests outside of medicine.
Tip #2: Set up for success
Since you are going through this major life/career transition, it is really helpful if you can set yourself up for success by having some projects that are easily completed during this challenging time so that you can demonstrate success. If you have projects in different stages of development, you will always have something you can work on when some projects are delayed for reasons outside of your control. In particular, it is great to have a few papers ready to go during late fellowship so they are published during your first year as an academic attending! This will allow you to continue your research trajectory as you learn the ropes of your new position.
Tip #3: Ask for help
It turns out you cannot do everything on your own! Make sure you are getting help professionally and personally so that you are set up for success. It’s okay to feel overwhelmed or confused; we all do at some point or another. Fellowship and early academic faculty years are stressful and nobody expects you to do it alone. Chances are your mentors or cofellows have had similar struggles, and in opening up, this dialogue may help you both.
Tip #4: Write out your 5-year plan
You need to know where you are going before you can figure out how to get there. Take some time for “soul searching”: Think about where you would like to be in 5 years and work backward (along with help from your mentors; see Tip #5) to determine how best to get there. If you think a career in academia might be for you, it’s never too soon to start networking and involving yourself in research. If a specific institution or clinical position draws your attention, check out the current faculty. You can use their CVs as a roadmap of types of experiences and honors that should be on your radar throughout these 5 years. Remember that your 5-year plan is not written in stone – this is something that you should re-evaluate as your interests and priorities change throughout your career.
Tip #5: Develop your personal ‘Board of Directors’
Instead of trying to find the perfect mentor, we suggest you seek out a personal “Board of Directors” who can serve as your mentoring team. There will never be a single perfect mentor for you and it is likely that you will need separate mentors to help guide you on different aspects of your career. I personally have separate individuals serving as my clinical mentor, my research content mentor, my research methods mentor, my career mentor, and my personal/life mentor. Having multiple mentors allows you to maximize the impact of your different mentors’ strengths across each component of your career. Further, your mentors themselves may have past histories of collaboration that you may then leverage to buoy your own fledgling career. When deciding on who to choose as a mentor, it is important to talk to prior mentees about their experiences with a mentor to help you decide if you may be a good match.
Tip #6: Master the art of “Menteering”
Now that you have identified mentors, you need to do your part in nurturing this mentee-mentor relationship. Be an excellent mentee: Show up, stick to a timeline, bring ideas and enthusiasm, and make it easy for your mentor. Your mentors want to see you succeed and sometimes this requires you to help them help you. If you know your own learning style and how you like to interact, have that conversation with your mentor upfront (for example, you may need strict deadlines or you may prefer having more time to develop ideas). Having these conversations before you start a project or a relationship will help set the expectations and ensure effective communication with your mentor. If you find that your mentor is doing something that hinders your progress, such as asking for updates too often or not checking in enough, have a constructive conversation with them about how you feel. Come prepared for meetings with your mentor with an agenda and timeline. Be specific if there is something you need from your mentor and be respectful of their other commitments. For example, if you would like your mentor to review your grant application, let them know the grant deadline and find out when you need to get them a draft so that they will have time to provide meaningful feedback.
Tip #7: Identify sponsors
Equally, if not more important than your mentoring team, are sponsors. These are people in positions of power who will promote you and help push your career forward. Sponsors can be people more senior to you, cofellows, or even acquaintances in industry or pharmaceuticals. Your mentor may also be your sponsor, but not always. As early academic faculty, it is important to get your name out there with speaking engagements related to your clinical and research niche, and that is one way a sponsor can help bolster your career.
Tip #8: Develop your personal brand – what is on your T-shirt?
As medicine becomes more and more subspecialized, finding your brand is becoming increasingly important. A brand could be anything from your academic niche to social justice, or even social media utilization. Your brand should encompass what you are naturally excited by within your field. Finding your brand will not only distinguish you from your peers but will also provide you with expertise which you can then offer to your colleagues, near and far. Practice the “elevator pitch” of your personal brand so that you can effectively (and efficiently) describe yourself and your interests when meeting new people and networking.
Tip #9: Meet thought leaders in your field
Think of the top five or six most prominent and influential people in your area of clinical or research interest and introduce yourself. This can be done at a national meeting or simply over email, though in person is always best if possible. Although thought leaders are busy, in my experience, if you are persistent, you can always find a few minutes to make an introduction. I’ve shared cab rides just to get a few minutes of someone’s time. In my first few years on faculty, I met with most of the thought leaders in my field; some of these meetings led to fruitful collaborations and important introductions (see tip #7). Meet others at your career level too. They can be great to bounce ideas off, and they will be future leaders in the field. Inviting thought leaders to come to your institution to give talks (in-person or virtually) is another great way to show your interest in their work and also find time to introduce yourself.
Tip #10: Apply, apply, apply
Remember that feedback is a gift and the best way to receive feedback is to apply to as many opportunities as you can. Any successful person in GI will have a ‘CV of failures’ far longer than their actual CV documenting their successes. I applied to 8 grants before landing my first one, but I received invaluable feedback and improved my writing skills in the process. Success in fellowship and early faculty takes immense grit – work on building a thick skin and finding the learning opportunity within any outcome.
Tip #11: Don’t get sucked into the email abyss
It is easy to fill your time completing low priority, but easy to complete, tasks such as responding to emails. Time management is key and you need to make sure that you dedicate time to more time-consuming tasks – such as writing and developing projects/grants – that have a high reward. Dedicate time on your calendar for high-priority tasks and make sure you don’t open your email during this time. Turn off the email pop-up window and do emails at the end of the day (or whenever you are done writing and thinking). Limiting distractions will help get your creative juices flowing.
Tip #12: Don’t always say yes
In fact, don’t ever say yes to a career or research opportunity within the first 24 hours to allow yourself time to weigh the pros and cons of the commitment, to assess the timeline feasibility, and to decide it fits into your 5-year plan. You can say you need to talk to your mentor about it first. If you decide you cannot accept an opportunity, a great way to mitigate that is to simply say “I’d love to, but my mentor says no.” Act as a sponsor to someone else by suggesting a potential colleague who might be interested in the opportunity. As you accept more responsibilities, think about what you might be able to give up to give yourself time to be successful in this new opportunity (and not distract from yourself or your 5-year plan).
Conclusion
Success in research and early academic faculty years takes planning and determination. We hope these tips provide a broad outline for what to think about and how to approach planning your future career. First and foremost, you must put in the time to think about what you really want and what will make you happy in the long run. Academic success is a broad term that each of us defines differently. What does it mean to you? Once you figure that out, make your 5-year plan and run with it!
Dr. Rebello and Dr. Long are with section of gastroenterology at Boston Medical Center and Boston University. They have no conflicts to report.
Congratulations! You have matched in a competitive medical subspecialty or you have secured your first faculty position. But what do you do now? Success in your early career – as a new fellow or a new attending – requires both hard work and perseverance. We present our top 12 tips for how to be successful as you transition into your new position.
Tip #1: Be kind to yourself
As you transition from medical resident to GI fellow or from GI fellow to first-time attending, it is important to recognize that you are going through a major career transition (not as major as fourth year to intern, but probably a close second). First and foremost, remember to be kind to yourself and set reasonable expectations. You need to allow yourself time to transition to a new role which may also be in a new city or state. Take care of yourself – don’t forget to exercise, eat well, and sleep. You are in the long game now. Work to get yourself in a routine that is sustainable. Block out time to exercise, explore your new city, meal plan, and pursue your interests outside of medicine.
Tip #2: Set up for success
Since you are going through this major life/career transition, it is really helpful if you can set yourself up for success by having some projects that are easily completed during this challenging time so that you can demonstrate success. If you have projects in different stages of development, you will always have something you can work on when some projects are delayed for reasons outside of your control. In particular, it is great to have a few papers ready to go during late fellowship so they are published during your first year as an academic attending! This will allow you to continue your research trajectory as you learn the ropes of your new position.
Tip #3: Ask for help
It turns out you cannot do everything on your own! Make sure you are getting help professionally and personally so that you are set up for success. It’s okay to feel overwhelmed or confused; we all do at some point or another. Fellowship and early academic faculty years are stressful and nobody expects you to do it alone. Chances are your mentors or cofellows have had similar struggles, and in opening up, this dialogue may help you both.
Tip #4: Write out your 5-year plan
You need to know where you are going before you can figure out how to get there. Take some time for “soul searching”: Think about where you would like to be in 5 years and work backward (along with help from your mentors; see Tip #5) to determine how best to get there. If you think a career in academia might be for you, it’s never too soon to start networking and involving yourself in research. If a specific institution or clinical position draws your attention, check out the current faculty. You can use their CVs as a roadmap of types of experiences and honors that should be on your radar throughout these 5 years. Remember that your 5-year plan is not written in stone – this is something that you should re-evaluate as your interests and priorities change throughout your career.
Tip #5: Develop your personal ‘Board of Directors’
Instead of trying to find the perfect mentor, we suggest you seek out a personal “Board of Directors” who can serve as your mentoring team. There will never be a single perfect mentor for you and it is likely that you will need separate mentors to help guide you on different aspects of your career. I personally have separate individuals serving as my clinical mentor, my research content mentor, my research methods mentor, my career mentor, and my personal/life mentor. Having multiple mentors allows you to maximize the impact of your different mentors’ strengths across each component of your career. Further, your mentors themselves may have past histories of collaboration that you may then leverage to buoy your own fledgling career. When deciding on who to choose as a mentor, it is important to talk to prior mentees about their experiences with a mentor to help you decide if you may be a good match.
Tip #6: Master the art of “Menteering”
Now that you have identified mentors, you need to do your part in nurturing this mentee-mentor relationship. Be an excellent mentee: Show up, stick to a timeline, bring ideas and enthusiasm, and make it easy for your mentor. Your mentors want to see you succeed and sometimes this requires you to help them help you. If you know your own learning style and how you like to interact, have that conversation with your mentor upfront (for example, you may need strict deadlines or you may prefer having more time to develop ideas). Having these conversations before you start a project or a relationship will help set the expectations and ensure effective communication with your mentor. If you find that your mentor is doing something that hinders your progress, such as asking for updates too often or not checking in enough, have a constructive conversation with them about how you feel. Come prepared for meetings with your mentor with an agenda and timeline. Be specific if there is something you need from your mentor and be respectful of their other commitments. For example, if you would like your mentor to review your grant application, let them know the grant deadline and find out when you need to get them a draft so that they will have time to provide meaningful feedback.
Tip #7: Identify sponsors
Equally, if not more important than your mentoring team, are sponsors. These are people in positions of power who will promote you and help push your career forward. Sponsors can be people more senior to you, cofellows, or even acquaintances in industry or pharmaceuticals. Your mentor may also be your sponsor, but not always. As early academic faculty, it is important to get your name out there with speaking engagements related to your clinical and research niche, and that is one way a sponsor can help bolster your career.
Tip #8: Develop your personal brand – what is on your T-shirt?
As medicine becomes more and more subspecialized, finding your brand is becoming increasingly important. A brand could be anything from your academic niche to social justice, or even social media utilization. Your brand should encompass what you are naturally excited by within your field. Finding your brand will not only distinguish you from your peers but will also provide you with expertise which you can then offer to your colleagues, near and far. Practice the “elevator pitch” of your personal brand so that you can effectively (and efficiently) describe yourself and your interests when meeting new people and networking.
Tip #9: Meet thought leaders in your field
Think of the top five or six most prominent and influential people in your area of clinical or research interest and introduce yourself. This can be done at a national meeting or simply over email, though in person is always best if possible. Although thought leaders are busy, in my experience, if you are persistent, you can always find a few minutes to make an introduction. I’ve shared cab rides just to get a few minutes of someone’s time. In my first few years on faculty, I met with most of the thought leaders in my field; some of these meetings led to fruitful collaborations and important introductions (see tip #7). Meet others at your career level too. They can be great to bounce ideas off, and they will be future leaders in the field. Inviting thought leaders to come to your institution to give talks (in-person or virtually) is another great way to show your interest in their work and also find time to introduce yourself.
Tip #10: Apply, apply, apply
Remember that feedback is a gift and the best way to receive feedback is to apply to as many opportunities as you can. Any successful person in GI will have a ‘CV of failures’ far longer than their actual CV documenting their successes. I applied to 8 grants before landing my first one, but I received invaluable feedback and improved my writing skills in the process. Success in fellowship and early faculty takes immense grit – work on building a thick skin and finding the learning opportunity within any outcome.
Tip #11: Don’t get sucked into the email abyss
It is easy to fill your time completing low priority, but easy to complete, tasks such as responding to emails. Time management is key and you need to make sure that you dedicate time to more time-consuming tasks – such as writing and developing projects/grants – that have a high reward. Dedicate time on your calendar for high-priority tasks and make sure you don’t open your email during this time. Turn off the email pop-up window and do emails at the end of the day (or whenever you are done writing and thinking). Limiting distractions will help get your creative juices flowing.
Tip #12: Don’t always say yes
In fact, don’t ever say yes to a career or research opportunity within the first 24 hours to allow yourself time to weigh the pros and cons of the commitment, to assess the timeline feasibility, and to decide it fits into your 5-year plan. You can say you need to talk to your mentor about it first. If you decide you cannot accept an opportunity, a great way to mitigate that is to simply say “I’d love to, but my mentor says no.” Act as a sponsor to someone else by suggesting a potential colleague who might be interested in the opportunity. As you accept more responsibilities, think about what you might be able to give up to give yourself time to be successful in this new opportunity (and not distract from yourself or your 5-year plan).
Conclusion
Success in research and early academic faculty years takes planning and determination. We hope these tips provide a broad outline for what to think about and how to approach planning your future career. First and foremost, you must put in the time to think about what you really want and what will make you happy in the long run. Academic success is a broad term that each of us defines differently. What does it mean to you? Once you figure that out, make your 5-year plan and run with it!
Dr. Rebello and Dr. Long are with section of gastroenterology at Boston Medical Center and Boston University. They have no conflicts to report.
Congratulations! You have matched in a competitive medical subspecialty or you have secured your first faculty position. But what do you do now? Success in your early career – as a new fellow or a new attending – requires both hard work and perseverance. We present our top 12 tips for how to be successful as you transition into your new position.
Tip #1: Be kind to yourself
As you transition from medical resident to GI fellow or from GI fellow to first-time attending, it is important to recognize that you are going through a major career transition (not as major as fourth year to intern, but probably a close second). First and foremost, remember to be kind to yourself and set reasonable expectations. You need to allow yourself time to transition to a new role which may also be in a new city or state. Take care of yourself – don’t forget to exercise, eat well, and sleep. You are in the long game now. Work to get yourself in a routine that is sustainable. Block out time to exercise, explore your new city, meal plan, and pursue your interests outside of medicine.
Tip #2: Set up for success
Since you are going through this major life/career transition, it is really helpful if you can set yourself up for success by having some projects that are easily completed during this challenging time so that you can demonstrate success. If you have projects in different stages of development, you will always have something you can work on when some projects are delayed for reasons outside of your control. In particular, it is great to have a few papers ready to go during late fellowship so they are published during your first year as an academic attending! This will allow you to continue your research trajectory as you learn the ropes of your new position.
Tip #3: Ask for help
It turns out you cannot do everything on your own! Make sure you are getting help professionally and personally so that you are set up for success. It’s okay to feel overwhelmed or confused; we all do at some point or another. Fellowship and early academic faculty years are stressful and nobody expects you to do it alone. Chances are your mentors or cofellows have had similar struggles, and in opening up, this dialogue may help you both.
Tip #4: Write out your 5-year plan
You need to know where you are going before you can figure out how to get there. Take some time for “soul searching”: Think about where you would like to be in 5 years and work backward (along with help from your mentors; see Tip #5) to determine how best to get there. If you think a career in academia might be for you, it’s never too soon to start networking and involving yourself in research. If a specific institution or clinical position draws your attention, check out the current faculty. You can use their CVs as a roadmap of types of experiences and honors that should be on your radar throughout these 5 years. Remember that your 5-year plan is not written in stone – this is something that you should re-evaluate as your interests and priorities change throughout your career.
Tip #5: Develop your personal ‘Board of Directors’
Instead of trying to find the perfect mentor, we suggest you seek out a personal “Board of Directors” who can serve as your mentoring team. There will never be a single perfect mentor for you and it is likely that you will need separate mentors to help guide you on different aspects of your career. I personally have separate individuals serving as my clinical mentor, my research content mentor, my research methods mentor, my career mentor, and my personal/life mentor. Having multiple mentors allows you to maximize the impact of your different mentors’ strengths across each component of your career. Further, your mentors themselves may have past histories of collaboration that you may then leverage to buoy your own fledgling career. When deciding on who to choose as a mentor, it is important to talk to prior mentees about their experiences with a mentor to help you decide if you may be a good match.
Tip #6: Master the art of “Menteering”
Now that you have identified mentors, you need to do your part in nurturing this mentee-mentor relationship. Be an excellent mentee: Show up, stick to a timeline, bring ideas and enthusiasm, and make it easy for your mentor. Your mentors want to see you succeed and sometimes this requires you to help them help you. If you know your own learning style and how you like to interact, have that conversation with your mentor upfront (for example, you may need strict deadlines or you may prefer having more time to develop ideas). Having these conversations before you start a project or a relationship will help set the expectations and ensure effective communication with your mentor. If you find that your mentor is doing something that hinders your progress, such as asking for updates too often or not checking in enough, have a constructive conversation with them about how you feel. Come prepared for meetings with your mentor with an agenda and timeline. Be specific if there is something you need from your mentor and be respectful of their other commitments. For example, if you would like your mentor to review your grant application, let them know the grant deadline and find out when you need to get them a draft so that they will have time to provide meaningful feedback.
Tip #7: Identify sponsors
Equally, if not more important than your mentoring team, are sponsors. These are people in positions of power who will promote you and help push your career forward. Sponsors can be people more senior to you, cofellows, or even acquaintances in industry or pharmaceuticals. Your mentor may also be your sponsor, but not always. As early academic faculty, it is important to get your name out there with speaking engagements related to your clinical and research niche, and that is one way a sponsor can help bolster your career.
Tip #8: Develop your personal brand – what is on your T-shirt?
As medicine becomes more and more subspecialized, finding your brand is becoming increasingly important. A brand could be anything from your academic niche to social justice, or even social media utilization. Your brand should encompass what you are naturally excited by within your field. Finding your brand will not only distinguish you from your peers but will also provide you with expertise which you can then offer to your colleagues, near and far. Practice the “elevator pitch” of your personal brand so that you can effectively (and efficiently) describe yourself and your interests when meeting new people and networking.
Tip #9: Meet thought leaders in your field
Think of the top five or six most prominent and influential people in your area of clinical or research interest and introduce yourself. This can be done at a national meeting or simply over email, though in person is always best if possible. Although thought leaders are busy, in my experience, if you are persistent, you can always find a few minutes to make an introduction. I’ve shared cab rides just to get a few minutes of someone’s time. In my first few years on faculty, I met with most of the thought leaders in my field; some of these meetings led to fruitful collaborations and important introductions (see tip #7). Meet others at your career level too. They can be great to bounce ideas off, and they will be future leaders in the field. Inviting thought leaders to come to your institution to give talks (in-person or virtually) is another great way to show your interest in their work and also find time to introduce yourself.
Tip #10: Apply, apply, apply
Remember that feedback is a gift and the best way to receive feedback is to apply to as many opportunities as you can. Any successful person in GI will have a ‘CV of failures’ far longer than their actual CV documenting their successes. I applied to 8 grants before landing my first one, but I received invaluable feedback and improved my writing skills in the process. Success in fellowship and early faculty takes immense grit – work on building a thick skin and finding the learning opportunity within any outcome.
Tip #11: Don’t get sucked into the email abyss
It is easy to fill your time completing low priority, but easy to complete, tasks such as responding to emails. Time management is key and you need to make sure that you dedicate time to more time-consuming tasks – such as writing and developing projects/grants – that have a high reward. Dedicate time on your calendar for high-priority tasks and make sure you don’t open your email during this time. Turn off the email pop-up window and do emails at the end of the day (or whenever you are done writing and thinking). Limiting distractions will help get your creative juices flowing.
Tip #12: Don’t always say yes
In fact, don’t ever say yes to a career or research opportunity within the first 24 hours to allow yourself time to weigh the pros and cons of the commitment, to assess the timeline feasibility, and to decide it fits into your 5-year plan. You can say you need to talk to your mentor about it first. If you decide you cannot accept an opportunity, a great way to mitigate that is to simply say “I’d love to, but my mentor says no.” Act as a sponsor to someone else by suggesting a potential colleague who might be interested in the opportunity. As you accept more responsibilities, think about what you might be able to give up to give yourself time to be successful in this new opportunity (and not distract from yourself or your 5-year plan).
Conclusion
Success in research and early academic faculty years takes planning and determination. We hope these tips provide a broad outline for what to think about and how to approach planning your future career. First and foremost, you must put in the time to think about what you really want and what will make you happy in the long run. Academic success is a broad term that each of us defines differently. What does it mean to you? Once you figure that out, make your 5-year plan and run with it!
Dr. Rebello and Dr. Long are with section of gastroenterology at Boston Medical Center and Boston University. They have no conflicts to report.
Microaggressions, racism, and antiracism: The role of gastroenterology
On a busy call day, Oviea (a second-year gastroenterology fellow), paused in the hallway to listen to a conversation between an endoscopy nurse and a patient. The nurse was requesting the patient’s permission for a gastroenterology fellow to participate in their care and the patient, well acquainted with the role from prior procedures, immediately agreed. Oviea entered the patient’s room, introduced himself as “Dr. Akpotaire, the gastroenterology fellow,” as he had with hundreds of other patients during his fellowship, and completed the informed consent. The interaction was brief but pleasant. As Oviea was leaving the room, the patient asked: “When will I meet the doctor”?
This question was familiar to Oviea. Despite always introducing himself by title and wearing matching identification, many patients had dismissed his credentials since graduating from medical school. His answer was equally familiar: “I am a doctor, and Dr. X, the supervising physician, will meet you soon.” With the patient seemingly placated, Oviea delivered the consent form to the procedure room. Minutes later, he was surprised to learn that the patient specifically requested that he not be allowed to participate in their care. This in combination with the patient’s initial dismissal of Oviea’s credentials, left a sting. While none of the other team members outwardly questioned the reason for the patient’s change of heart, Oviea continued to wonder if the patient’s decision was because of his race.
Beyond gastroenterology, similar experiences are common in other spheres. The Twitter thread #BlackintheIvory recounts stories of microaggressions and structural racism in medicine and academia. The cumulative toll of these experiences leads to departures of Black physicians including Uché Blackstock, MD;1 Aysha Khoury, MD, MPH;2 Ben Danielson, MD;3 Princess Dennar, MD;4 and others.
Microaggressions as proxy for bias
The term microaggression was coined by Chester Pierce, MD, the first Black tenured professor at Massachusetts General Hospital in the 1970’s, to describe the frequent, yet subtle dismissals Black Americans experienced in society. Over time, the term has been expanded to include “brief and commonplace daily verbal, behavioral, or environmental indignities, intentional or unintentional, that communicate hostile, derogatory, or negative slights and insults” to any marginalized group.5
While the term microaggressions is useful in contextualizing individual experiences, it narrowly focuses on conscious or unconscious interpersonal prejudices. In medicine, this misdirects attention away from the policies and practices that create and reinforce prejudices; these policies and practices do so by systematically excluding underrepresented minority (URM) physicians,6 defined by the American Association of Medical Colleges as physicians who are Black, Hispanic, Native Americans, and Alaska Natives,7 from the medical workforce. Ultimately, this leads to and exacerbates poor health outcomes for racial and ethnic minority patients.
Microaggressions represent our society’s deepest and oldest biases and are rooted in structural racism, as well as misogyny, homophobia, transphobia, xenophobia, ableism, and other prejudices.8 For URM physicians, experiences like the example above are frequently caused by structural racism.
Structural racism in medicine
Structural racism refers to the policies, practices, cultural representations, and norms that reinforce inequities by providing privileges to White people at the disadvantage of non-White people.9 In 1910, Abraham Flexner, commissioned by the Carnegie Foundation and the American Medical Association, wrote that African American physicians should be trained in hygiene rather than surgery and should primarily serve as “sanitarians” whose purpose was to “protect Whites” from common diseases like tuberculosis.10 The 1910 Flexner Report also emphasized the importance of prerequisite basic sciences education and recommended that only two of the seven existing Black medical schools remain open because Flexner believed that only these schools had the potential to meet the new requirements for medical education.11 A recent analysis found that, had the other five medical schools affiliated with historically Black colleges and universities remained open, this would have resulted in an additional 33,315 Black medical school graduates by 2019.12 Structural racism explains why the majority of practicing physicians, medical educators, National Institutes of Health–funded researchers, and hospital executives are White and, similarly, why White patients are overrepresented in clinical trials, have better health outcomes, and live longer lives than several racial and ethnic minority groups.13
The murders of Ahmaud Arbery, Breonna Taylor, and George Floyd and the inequitable toll of the COVID-19 pandemic on Black, Hispanic, and Native American people renewed the dialogue regarding structural racism in America. Beyond criminal justice and police reform, the current social justice movement demands that structural racism is examined in all spheres. In medicine and health care, acknowledging the history of exclusion and exploitation of Black people and other URM groups is an important first step, but this must be followed by a commitment to an antiracist future for the benefit of all medical professionals and patients.14,15
Antiracism as a path forward
Antiracism refers to actions and policies that seek to dismantle structural racism. While individuals can and should engage in antiracist actions, it is equally important for organizations and government to actively participate in this process as well.
Individual and interpersonal levels
Gastroenterologists should advocate an end to racist practices within their organizations (e.g., unjustified use of race-based corrections in diagnostic algorithms and practice guidelines),16 and interrupt microaggressions and racist actions in real time (e.g., overpolicing of underrepresented groups in health care settings).17 Gastroenterologists from underrepresented groups may also need to unlearn internalized racism, which is defined as acceptance by members of disadvantaged races of the negative messages about their own abilities and intrinsic worth.18
Organizational level
Gastroenterology divisions and practices must ensure that the entire workforce, including leadership, reflects the diversity of our country. Underrepresented groups represent 33% of the U.S. population, but only 9.1% of gastroenterology fellows and 10% of gastroenterology faculty are from underrepresented groups.19 In addition to diversifying the field of gastroenterology through financial and operational support of pipeline educational programs, organizations should also promote the scholarship of URM groups, whose work is often undervalued, and redistribute power by elevating voices that have been historically absent.20 Gastroenterology practices should also collect high-quality patient data disaggregated by demographic factors. Doing so will enable rapid identification of disparate health outcomes by demographic variables and inform interventions to eliminate identified disparities.
Government level
The “Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government” issued by President Biden on Jan. 20, 2021, is an example of how government can promote antiracism.21 The executive order states that domestic policies cause group inequities and calls for the removal of systemic barriers in current and future domestic policies. The executive order outlines several additional ways to improve equity in current and future policy, including engagement, consultation, and coordination with members of underserved communities. The details outlined in the executive order should serve as the foundation for establishing new standards at the state, county, and city levels as well. Gastroenterologists can influence government by voting for officials at all levels that support and promote these standards.
Conclusion
Beyond calling out microaggressions in real time, we must also interrogate the biases, policies, and practices that support them in medicine and beyond. As Black gastroenterologists who have experienced microaggressions and overt acts of racism, we ground Oviea’s experience in structural racism and offer strategies that individuals, organizations, and governing institutions can adopt toward an antiracist future. This model can be applied to experiences rooted in misogyny, homophobia, transphobia, xenophobia, ableism, and other prejudices.
As a nation, we must make an active and collective choice to address structural racism. In health care, doing so will strengthen communities, enhance the lived experiences of URM physician colleagues, and save patient lives. Gastroenterologists, as trusted health care providers, are uniquely positioned to lead the way.
Dr. Akpotaire is a second-year GI fellow in the division of gastroenterology at the University of Washington, Seattle. Dr. Issaka is an assistant professor with both the Fred Hutchinson Cancer Research Center, Seattle, and the division of gastroenterology at the University of Washington.
References
1. Blackstock U. “Why Black doctors like me are leaving faculty positions in academic medical centers.” STAT News, 2020.
2. Asare JG. “One Doctor Shares Her Story of Racism in Medicine.” Forbes. 2021 Feb 1.
3. Kroman D. “Revered doctor steps down, accusing Seattle Children’s Hospital of racism.” Crosscut. 2020 Dec 31.
4. United States District Court Eastern District of Louisiana. Princess Dennar, M.D. v. The Administrators of the Tulane Educational Fund, 2020.
5. Sue DW. Microaggressions in Everyday Life: Race, Gender, and Sexual Orientation. Hoboken, N.J.: Wiley, 2010.
6. Boyd RW. Lancet. 2019 Jun 22;393(10190):2484-5.
7. AAMC. Diversity in Medicine Facts and Figures 2019. Washington, D.C., 2019.
8. Overland MK et al. PM R. 2019 Sep;11(9):1004-12.
9. Jones CP. Ethn Dis. 2018 Aug 9;28(Suppl 1):231-4.
10. Hlavinka E. “Racial Bias in Flexner Report Permeates Medical Education Today.” Medpage Today. 2020 Jun 18.
11. Flexner A. Medical Education in the United States and Canada. New York: 1910. Republished: Bull World Health Organ. 2002;80(7):594-602.
12. Campbell KM et al. JAMA Netw Open. 2020 Aug 3;3(8):e2015220.
13. Malat J et al. Soc Sci Med. 2018 Feb;199:148-56.
14. Kendi IX. How to be an antiracist. New York: Random House Books, 2019.
15. Gray DM 2nd et al. Nat Rev Gastroenterol Hepatol. 2020 Oct;17(10):589-90.
16. Vyas DA et al. N Engl J Med. 2020 Aug 27;383(9):874-82.
17. Green CR et al. J Natl Med Assoc. 2018 Feb;110(1):37-43.
18. Jones CP. Am J Public Health. 2000 Aug;90(8):1212-5.
19. Anyane-Yeboa A et al. Am J Gastroenterol. 2020 Aug;115(8):1147-9.
20. Issaka RB. JAMA. 2020 Aug 11;324(6):556-7.
21. Biden JR. Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government. Washington, D.C.: The White House, 2021.
On a busy call day, Oviea (a second-year gastroenterology fellow), paused in the hallway to listen to a conversation between an endoscopy nurse and a patient. The nurse was requesting the patient’s permission for a gastroenterology fellow to participate in their care and the patient, well acquainted with the role from prior procedures, immediately agreed. Oviea entered the patient’s room, introduced himself as “Dr. Akpotaire, the gastroenterology fellow,” as he had with hundreds of other patients during his fellowship, and completed the informed consent. The interaction was brief but pleasant. As Oviea was leaving the room, the patient asked: “When will I meet the doctor”?
This question was familiar to Oviea. Despite always introducing himself by title and wearing matching identification, many patients had dismissed his credentials since graduating from medical school. His answer was equally familiar: “I am a doctor, and Dr. X, the supervising physician, will meet you soon.” With the patient seemingly placated, Oviea delivered the consent form to the procedure room. Minutes later, he was surprised to learn that the patient specifically requested that he not be allowed to participate in their care. This in combination with the patient’s initial dismissal of Oviea’s credentials, left a sting. While none of the other team members outwardly questioned the reason for the patient’s change of heart, Oviea continued to wonder if the patient’s decision was because of his race.
Beyond gastroenterology, similar experiences are common in other spheres. The Twitter thread #BlackintheIvory recounts stories of microaggressions and structural racism in medicine and academia. The cumulative toll of these experiences leads to departures of Black physicians including Uché Blackstock, MD;1 Aysha Khoury, MD, MPH;2 Ben Danielson, MD;3 Princess Dennar, MD;4 and others.
Microaggressions as proxy for bias
The term microaggression was coined by Chester Pierce, MD, the first Black tenured professor at Massachusetts General Hospital in the 1970’s, to describe the frequent, yet subtle dismissals Black Americans experienced in society. Over time, the term has been expanded to include “brief and commonplace daily verbal, behavioral, or environmental indignities, intentional or unintentional, that communicate hostile, derogatory, or negative slights and insults” to any marginalized group.5
While the term microaggressions is useful in contextualizing individual experiences, it narrowly focuses on conscious or unconscious interpersonal prejudices. In medicine, this misdirects attention away from the policies and practices that create and reinforce prejudices; these policies and practices do so by systematically excluding underrepresented minority (URM) physicians,6 defined by the American Association of Medical Colleges as physicians who are Black, Hispanic, Native Americans, and Alaska Natives,7 from the medical workforce. Ultimately, this leads to and exacerbates poor health outcomes for racial and ethnic minority patients.
Microaggressions represent our society’s deepest and oldest biases and are rooted in structural racism, as well as misogyny, homophobia, transphobia, xenophobia, ableism, and other prejudices.8 For URM physicians, experiences like the example above are frequently caused by structural racism.
Structural racism in medicine
Structural racism refers to the policies, practices, cultural representations, and norms that reinforce inequities by providing privileges to White people at the disadvantage of non-White people.9 In 1910, Abraham Flexner, commissioned by the Carnegie Foundation and the American Medical Association, wrote that African American physicians should be trained in hygiene rather than surgery and should primarily serve as “sanitarians” whose purpose was to “protect Whites” from common diseases like tuberculosis.10 The 1910 Flexner Report also emphasized the importance of prerequisite basic sciences education and recommended that only two of the seven existing Black medical schools remain open because Flexner believed that only these schools had the potential to meet the new requirements for medical education.11 A recent analysis found that, had the other five medical schools affiliated with historically Black colleges and universities remained open, this would have resulted in an additional 33,315 Black medical school graduates by 2019.12 Structural racism explains why the majority of practicing physicians, medical educators, National Institutes of Health–funded researchers, and hospital executives are White and, similarly, why White patients are overrepresented in clinical trials, have better health outcomes, and live longer lives than several racial and ethnic minority groups.13
The murders of Ahmaud Arbery, Breonna Taylor, and George Floyd and the inequitable toll of the COVID-19 pandemic on Black, Hispanic, and Native American people renewed the dialogue regarding structural racism in America. Beyond criminal justice and police reform, the current social justice movement demands that structural racism is examined in all spheres. In medicine and health care, acknowledging the history of exclusion and exploitation of Black people and other URM groups is an important first step, but this must be followed by a commitment to an antiracist future for the benefit of all medical professionals and patients.14,15
Antiracism as a path forward
Antiracism refers to actions and policies that seek to dismantle structural racism. While individuals can and should engage in antiracist actions, it is equally important for organizations and government to actively participate in this process as well.
Individual and interpersonal levels
Gastroenterologists should advocate an end to racist practices within their organizations (e.g., unjustified use of race-based corrections in diagnostic algorithms and practice guidelines),16 and interrupt microaggressions and racist actions in real time (e.g., overpolicing of underrepresented groups in health care settings).17 Gastroenterologists from underrepresented groups may also need to unlearn internalized racism, which is defined as acceptance by members of disadvantaged races of the negative messages about their own abilities and intrinsic worth.18
Organizational level
Gastroenterology divisions and practices must ensure that the entire workforce, including leadership, reflects the diversity of our country. Underrepresented groups represent 33% of the U.S. population, but only 9.1% of gastroenterology fellows and 10% of gastroenterology faculty are from underrepresented groups.19 In addition to diversifying the field of gastroenterology through financial and operational support of pipeline educational programs, organizations should also promote the scholarship of URM groups, whose work is often undervalued, and redistribute power by elevating voices that have been historically absent.20 Gastroenterology practices should also collect high-quality patient data disaggregated by demographic factors. Doing so will enable rapid identification of disparate health outcomes by demographic variables and inform interventions to eliminate identified disparities.
Government level
The “Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government” issued by President Biden on Jan. 20, 2021, is an example of how government can promote antiracism.21 The executive order states that domestic policies cause group inequities and calls for the removal of systemic barriers in current and future domestic policies. The executive order outlines several additional ways to improve equity in current and future policy, including engagement, consultation, and coordination with members of underserved communities. The details outlined in the executive order should serve as the foundation for establishing new standards at the state, county, and city levels as well. Gastroenterologists can influence government by voting for officials at all levels that support and promote these standards.
Conclusion
Beyond calling out microaggressions in real time, we must also interrogate the biases, policies, and practices that support them in medicine and beyond. As Black gastroenterologists who have experienced microaggressions and overt acts of racism, we ground Oviea’s experience in structural racism and offer strategies that individuals, organizations, and governing institutions can adopt toward an antiracist future. This model can be applied to experiences rooted in misogyny, homophobia, transphobia, xenophobia, ableism, and other prejudices.
As a nation, we must make an active and collective choice to address structural racism. In health care, doing so will strengthen communities, enhance the lived experiences of URM physician colleagues, and save patient lives. Gastroenterologists, as trusted health care providers, are uniquely positioned to lead the way.
Dr. Akpotaire is a second-year GI fellow in the division of gastroenterology at the University of Washington, Seattle. Dr. Issaka is an assistant professor with both the Fred Hutchinson Cancer Research Center, Seattle, and the division of gastroenterology at the University of Washington.
References
1. Blackstock U. “Why Black doctors like me are leaving faculty positions in academic medical centers.” STAT News, 2020.
2. Asare JG. “One Doctor Shares Her Story of Racism in Medicine.” Forbes. 2021 Feb 1.
3. Kroman D. “Revered doctor steps down, accusing Seattle Children’s Hospital of racism.” Crosscut. 2020 Dec 31.
4. United States District Court Eastern District of Louisiana. Princess Dennar, M.D. v. The Administrators of the Tulane Educational Fund, 2020.
5. Sue DW. Microaggressions in Everyday Life: Race, Gender, and Sexual Orientation. Hoboken, N.J.: Wiley, 2010.
6. Boyd RW. Lancet. 2019 Jun 22;393(10190):2484-5.
7. AAMC. Diversity in Medicine Facts and Figures 2019. Washington, D.C., 2019.
8. Overland MK et al. PM R. 2019 Sep;11(9):1004-12.
9. Jones CP. Ethn Dis. 2018 Aug 9;28(Suppl 1):231-4.
10. Hlavinka E. “Racial Bias in Flexner Report Permeates Medical Education Today.” Medpage Today. 2020 Jun 18.
11. Flexner A. Medical Education in the United States and Canada. New York: 1910. Republished: Bull World Health Organ. 2002;80(7):594-602.
12. Campbell KM et al. JAMA Netw Open. 2020 Aug 3;3(8):e2015220.
13. Malat J et al. Soc Sci Med. 2018 Feb;199:148-56.
14. Kendi IX. How to be an antiracist. New York: Random House Books, 2019.
15. Gray DM 2nd et al. Nat Rev Gastroenterol Hepatol. 2020 Oct;17(10):589-90.
16. Vyas DA et al. N Engl J Med. 2020 Aug 27;383(9):874-82.
17. Green CR et al. J Natl Med Assoc. 2018 Feb;110(1):37-43.
18. Jones CP. Am J Public Health. 2000 Aug;90(8):1212-5.
19. Anyane-Yeboa A et al. Am J Gastroenterol. 2020 Aug;115(8):1147-9.
20. Issaka RB. JAMA. 2020 Aug 11;324(6):556-7.
21. Biden JR. Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government. Washington, D.C.: The White House, 2021.
On a busy call day, Oviea (a second-year gastroenterology fellow), paused in the hallway to listen to a conversation between an endoscopy nurse and a patient. The nurse was requesting the patient’s permission for a gastroenterology fellow to participate in their care and the patient, well acquainted with the role from prior procedures, immediately agreed. Oviea entered the patient’s room, introduced himself as “Dr. Akpotaire, the gastroenterology fellow,” as he had with hundreds of other patients during his fellowship, and completed the informed consent. The interaction was brief but pleasant. As Oviea was leaving the room, the patient asked: “When will I meet the doctor”?
This question was familiar to Oviea. Despite always introducing himself by title and wearing matching identification, many patients had dismissed his credentials since graduating from medical school. His answer was equally familiar: “I am a doctor, and Dr. X, the supervising physician, will meet you soon.” With the patient seemingly placated, Oviea delivered the consent form to the procedure room. Minutes later, he was surprised to learn that the patient specifically requested that he not be allowed to participate in their care. This in combination with the patient’s initial dismissal of Oviea’s credentials, left a sting. While none of the other team members outwardly questioned the reason for the patient’s change of heart, Oviea continued to wonder if the patient’s decision was because of his race.
Beyond gastroenterology, similar experiences are common in other spheres. The Twitter thread #BlackintheIvory recounts stories of microaggressions and structural racism in medicine and academia. The cumulative toll of these experiences leads to departures of Black physicians including Uché Blackstock, MD;1 Aysha Khoury, MD, MPH;2 Ben Danielson, MD;3 Princess Dennar, MD;4 and others.
Microaggressions as proxy for bias
The term microaggression was coined by Chester Pierce, MD, the first Black tenured professor at Massachusetts General Hospital in the 1970’s, to describe the frequent, yet subtle dismissals Black Americans experienced in society. Over time, the term has been expanded to include “brief and commonplace daily verbal, behavioral, or environmental indignities, intentional or unintentional, that communicate hostile, derogatory, or negative slights and insults” to any marginalized group.5
While the term microaggressions is useful in contextualizing individual experiences, it narrowly focuses on conscious or unconscious interpersonal prejudices. In medicine, this misdirects attention away from the policies and practices that create and reinforce prejudices; these policies and practices do so by systematically excluding underrepresented minority (URM) physicians,6 defined by the American Association of Medical Colleges as physicians who are Black, Hispanic, Native Americans, and Alaska Natives,7 from the medical workforce. Ultimately, this leads to and exacerbates poor health outcomes for racial and ethnic minority patients.
Microaggressions represent our society’s deepest and oldest biases and are rooted in structural racism, as well as misogyny, homophobia, transphobia, xenophobia, ableism, and other prejudices.8 For URM physicians, experiences like the example above are frequently caused by structural racism.
Structural racism in medicine
Structural racism refers to the policies, practices, cultural representations, and norms that reinforce inequities by providing privileges to White people at the disadvantage of non-White people.9 In 1910, Abraham Flexner, commissioned by the Carnegie Foundation and the American Medical Association, wrote that African American physicians should be trained in hygiene rather than surgery and should primarily serve as “sanitarians” whose purpose was to “protect Whites” from common diseases like tuberculosis.10 The 1910 Flexner Report also emphasized the importance of prerequisite basic sciences education and recommended that only two of the seven existing Black medical schools remain open because Flexner believed that only these schools had the potential to meet the new requirements for medical education.11 A recent analysis found that, had the other five medical schools affiliated with historically Black colleges and universities remained open, this would have resulted in an additional 33,315 Black medical school graduates by 2019.12 Structural racism explains why the majority of practicing physicians, medical educators, National Institutes of Health–funded researchers, and hospital executives are White and, similarly, why White patients are overrepresented in clinical trials, have better health outcomes, and live longer lives than several racial and ethnic minority groups.13
The murders of Ahmaud Arbery, Breonna Taylor, and George Floyd and the inequitable toll of the COVID-19 pandemic on Black, Hispanic, and Native American people renewed the dialogue regarding structural racism in America. Beyond criminal justice and police reform, the current social justice movement demands that structural racism is examined in all spheres. In medicine and health care, acknowledging the history of exclusion and exploitation of Black people and other URM groups is an important first step, but this must be followed by a commitment to an antiracist future for the benefit of all medical professionals and patients.14,15
Antiracism as a path forward
Antiracism refers to actions and policies that seek to dismantle structural racism. While individuals can and should engage in antiracist actions, it is equally important for organizations and government to actively participate in this process as well.
Individual and interpersonal levels
Gastroenterologists should advocate an end to racist practices within their organizations (e.g., unjustified use of race-based corrections in diagnostic algorithms and practice guidelines),16 and interrupt microaggressions and racist actions in real time (e.g., overpolicing of underrepresented groups in health care settings).17 Gastroenterologists from underrepresented groups may also need to unlearn internalized racism, which is defined as acceptance by members of disadvantaged races of the negative messages about their own abilities and intrinsic worth.18
Organizational level
Gastroenterology divisions and practices must ensure that the entire workforce, including leadership, reflects the diversity of our country. Underrepresented groups represent 33% of the U.S. population, but only 9.1% of gastroenterology fellows and 10% of gastroenterology faculty are from underrepresented groups.19 In addition to diversifying the field of gastroenterology through financial and operational support of pipeline educational programs, organizations should also promote the scholarship of URM groups, whose work is often undervalued, and redistribute power by elevating voices that have been historically absent.20 Gastroenterology practices should also collect high-quality patient data disaggregated by demographic factors. Doing so will enable rapid identification of disparate health outcomes by demographic variables and inform interventions to eliminate identified disparities.
Government level
The “Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government” issued by President Biden on Jan. 20, 2021, is an example of how government can promote antiracism.21 The executive order states that domestic policies cause group inequities and calls for the removal of systemic barriers in current and future domestic policies. The executive order outlines several additional ways to improve equity in current and future policy, including engagement, consultation, and coordination with members of underserved communities. The details outlined in the executive order should serve as the foundation for establishing new standards at the state, county, and city levels as well. Gastroenterologists can influence government by voting for officials at all levels that support and promote these standards.
Conclusion
Beyond calling out microaggressions in real time, we must also interrogate the biases, policies, and practices that support them in medicine and beyond. As Black gastroenterologists who have experienced microaggressions and overt acts of racism, we ground Oviea’s experience in structural racism and offer strategies that individuals, organizations, and governing institutions can adopt toward an antiracist future. This model can be applied to experiences rooted in misogyny, homophobia, transphobia, xenophobia, ableism, and other prejudices.
As a nation, we must make an active and collective choice to address structural racism. In health care, doing so will strengthen communities, enhance the lived experiences of URM physician colleagues, and save patient lives. Gastroenterologists, as trusted health care providers, are uniquely positioned to lead the way.
Dr. Akpotaire is a second-year GI fellow in the division of gastroenterology at the University of Washington, Seattle. Dr. Issaka is an assistant professor with both the Fred Hutchinson Cancer Research Center, Seattle, and the division of gastroenterology at the University of Washington.
References
1. Blackstock U. “Why Black doctors like me are leaving faculty positions in academic medical centers.” STAT News, 2020.
2. Asare JG. “One Doctor Shares Her Story of Racism in Medicine.” Forbes. 2021 Feb 1.
3. Kroman D. “Revered doctor steps down, accusing Seattle Children’s Hospital of racism.” Crosscut. 2020 Dec 31.
4. United States District Court Eastern District of Louisiana. Princess Dennar, M.D. v. The Administrators of the Tulane Educational Fund, 2020.
5. Sue DW. Microaggressions in Everyday Life: Race, Gender, and Sexual Orientation. Hoboken, N.J.: Wiley, 2010.
6. Boyd RW. Lancet. 2019 Jun 22;393(10190):2484-5.
7. AAMC. Diversity in Medicine Facts and Figures 2019. Washington, D.C., 2019.
8. Overland MK et al. PM R. 2019 Sep;11(9):1004-12.
9. Jones CP. Ethn Dis. 2018 Aug 9;28(Suppl 1):231-4.
10. Hlavinka E. “Racial Bias in Flexner Report Permeates Medical Education Today.” Medpage Today. 2020 Jun 18.
11. Flexner A. Medical Education in the United States and Canada. New York: 1910. Republished: Bull World Health Organ. 2002;80(7):594-602.
12. Campbell KM et al. JAMA Netw Open. 2020 Aug 3;3(8):e2015220.
13. Malat J et al. Soc Sci Med. 2018 Feb;199:148-56.
14. Kendi IX. How to be an antiracist. New York: Random House Books, 2019.
15. Gray DM 2nd et al. Nat Rev Gastroenterol Hepatol. 2020 Oct;17(10):589-90.
16. Vyas DA et al. N Engl J Med. 2020 Aug 27;383(9):874-82.
17. Green CR et al. J Natl Med Assoc. 2018 Feb;110(1):37-43.
18. Jones CP. Am J Public Health. 2000 Aug;90(8):1212-5.
19. Anyane-Yeboa A et al. Am J Gastroenterol. 2020 Aug;115(8):1147-9.
20. Issaka RB. JAMA. 2020 Aug 11;324(6):556-7.
21. Biden JR. Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government. Washington, D.C.: The White House, 2021.
Impostor syndrome: Implications for medical professionals
A few years ago, I was asked to give a talk on impostor syndrome at a national conference. My initial thought was “I am not even remotely qualified to give this talk.” Upon reflection, I think that was the first time I acknowledged that I, too, suffer from this syndrome.
There are many definitions and designations (e.g., impostor phenomenon or fraud syndrome), but the one I use most often is high-achieving individuals who are marked by an inability to internalize their accomplishments and a persistent fear of being exposed as a fraud. They live in fear that their incompetence will be exposed and they will be revealed as a fraud both intellectually and within their job or role. First described by Clance and Imes in 1978,1 the original authors observed that many highly respected and accomplished women did not experience an internal sense of success despite their education and evidence of academic achievement. Based in part on previous observations regarding the differential attribution of success in men and women,2 the authors suggested that two general principles were found to be at the heart of this syndrome. The first was that an unexpected performance outcome will be attributed to a temporary cause. The second was that an expected performance outcome will be attributed to a stable cause. As such, the authors originally suggested that women tended to explain failure with lack of ability, whereas men attributed failure to luck or task difficulty. Furthermore, the authors emphasized environmental factors – such as mentorship, competition, and isolation – as the primary influence in the development of these tendencies.
Although originally described in women, this phenomenon can also affect men, as well as a wide variety of people from different occupations and cultures.3-6 Furthermore, although environmental factors were originally linked as the primary driver of these tendencies, further research has suggested that personality factors play a larger role, and that up to 70% of people may experience this phenomenon in their lifetime.7 Personality traits such as perfectionism and neuroticism may be linked to the development of this phenomenon.3,8
There are several online screening questionnaires that can be used to gauge whether individuals experience some or most of these traits. On one such questionnaire, the Clance IP Scale,9 poses such questions as: “I have often succeeded on a test or task even though I was afraid that I would not do well before I undertook the task” and “I am afraid people important to me may find out that I am not as capable as they think I am.” There are 20 questions scored from 1 to 5 and a score of 40 or below suggests few impostor tendencies, while a score of 80 or above suggests the respondent often has intense IP experiences. The higher the score, the more frequently and seriously the impostor syndrome interferes in a person’s life. What is unclear is whether this worsens, improves, or stays the same throughout one’s career. Of interest is that my personal score at this time is 43; however, it would have been 89 had I taken the test during college and medical school. What is unclear to me from the literature is what factors may play a role in a person’s perception of their abilities and their personal confidence over time.
Why is this important? Given that we are all professionals, impostor tendencies appear to have significant impact in the context of our work. This may have impact on us both as employers and as employees.10 Individuals with impostor syndrome tendencies often characterize themselves negatively and perform poorly on self-appraisals.11 In a study of 201 Belgian white-collar workers, Vergauwe and colleagues found that impostor syndrome tendencies were negatively related to job satisfaction and organizational citizenship behavior; both of which could be influenced by a high degree of social support.10 Individuals with impostor syndrome tendencies do less career planning, explore career options less frequently, and are less inclined to lead.12,13 These tendencies can be detrimental as the most qualified people for a position or opportunity may not step forward for consideration. Employers may tend to overlook these individuals for promotions or for pay raises which could negatively influence future earnings. Furthermore, a person may experience increased burnout as they continuously try to overcompensate for what they perceive as their shortcomings. They may feel concerned they are letting others down or not performing to standards. They may derive less enjoyment from life because of the constant focus on feelings of inadequacy.14 Research along these lines suggest impostor syndrome tendencies can have adverse personal and health-related consequences and may increase social anxiety, depression, and overall psychological distress.15,16
What can we do about it? In a very interesting study by Zanchetta and colleagues, the authors studied 103 young employees and randomized them to receive coaching, training, or no intervention.17 Their findings showed that coaching was an effective mindset intervention which resulted in reduced impostor syndrome scores. Furthermore, fear of negative evaluation and the effect of coaching appeared to be significantly associated with a reduction in the impostor syndrome scores. Coaching appeared to improve self-enhancing attributions and self-efficacy with a reduction in the tendency of subjects to fear negative evaluation. The authors concluded that fostering a mindset shift by reducing the fear of negative evaluations through coaching demonstrated measurable and sustained improvements in overall impostor syndrome scores for participants.17
What do I suggest? It is clear this affects a significant percentage of physicians, health care professionals, and professionals in general. Harboring these tendencies can have a negative impact on health, professional achievement, income, and happiness. It is important to self-reflect, identify if you are at risk, and if so, take the opportunity to explore solutions. My recommendations are:
- Name it: Take the test and see how you score.
- Be mindful: Self-reflection will help you identify the behaviors that are interfering with your happiness and success.
- Write it down: Be strategic and document your plan for success to reinforce your accomplishments.
- Create a feedback group: Friends and colleagues can help to mitigate the negative effects of impostor syndrome tendencies.
- Speak up: Ask for help; coaching has been documented to reduce impostor syndrome scores and help lessen the burden of these tendencies.
- Step out of your comfort zone: Develop a mantra, break bigger challenges into smaller pieces, and acknowledge little wins along the way.
In conclusion, impostor syndrome appears to be highly prevalent in professionals including those of us in medicine. The experience can adversely affect our careers and ability to secure key leadership positions. As managers, we also must keep in mind our role in mentoring others and recognizing the potential impact of impostor syndrome on those who report to us. Recognition of this phenomenon – and understanding of the effects on oneself – is the first step in overcoming the negative effects and moving toward realization of one’s potential.
Dr. Brown is a professor of medicine at Wayne State University, division chief of gastroenterology and hepatology at Henry Ford Hospital, and associate medical director at the Henry Ford Hospital Transplant Institute, all in Detroit.
References
1. Clance PR, Imes S. Psychother Theory Res Pract. 1978 Fall;15(3):1-7.
2. Deaux D. In J.H.Harvey, W.J.Ickes and R.F. Kidd (Eds). New directions in attribution research. Vol. 1. New York: Halsted Press Division, Wiley. 1976; p 335-42.
3. Bernard NS et al. J Pers Assess. 2002;78(2):321-33.
4. Topping ME et al. Acad Psychol Bull. 1985;(7):213-26.
5. Langford J et al. Psychotherapy. 1993;30(3):495-501.
6. Chae JH et al. J Pers Assess. 1995;65(3):468-85.
7. Harvey JC et al. If I’m successful, why do I feel like a fake? New York: Random House, 1985.
8. Ross SR et al. Pers Individ Diff. 2001;31:1347-55.
9. Clance PR. The impostor phenomenon: When success makes you feel like a fake. Toronto: Bantam Books, 1985; p 20-2.
10. Vergauwe J et al. J Bus Psychol. 2015;30:565-81.
11. Leary MR et al. J Pers. 2000;68(4):725-56.
12. Neureiter M et al. Front Psychol. 2016;7:48.
13. Neureiter M et al. J Vocat Behav. 2017;98:56-69.
14. Duhigg C. The power of habit: Why we do what we do in life and business. New York: Random House, 2012.
15. Henning K et al. Med Educ. 1998 Sep;32(5):456-64.
16. Oriel K et al. Fam Med. 2004 Apr;36(4):248-52.
17. Zanchetta M et al. Front Psychol. 2020 May 15;11:405.
A few years ago, I was asked to give a talk on impostor syndrome at a national conference. My initial thought was “I am not even remotely qualified to give this talk.” Upon reflection, I think that was the first time I acknowledged that I, too, suffer from this syndrome.
There are many definitions and designations (e.g., impostor phenomenon or fraud syndrome), but the one I use most often is high-achieving individuals who are marked by an inability to internalize their accomplishments and a persistent fear of being exposed as a fraud. They live in fear that their incompetence will be exposed and they will be revealed as a fraud both intellectually and within their job or role. First described by Clance and Imes in 1978,1 the original authors observed that many highly respected and accomplished women did not experience an internal sense of success despite their education and evidence of academic achievement. Based in part on previous observations regarding the differential attribution of success in men and women,2 the authors suggested that two general principles were found to be at the heart of this syndrome. The first was that an unexpected performance outcome will be attributed to a temporary cause. The second was that an expected performance outcome will be attributed to a stable cause. As such, the authors originally suggested that women tended to explain failure with lack of ability, whereas men attributed failure to luck or task difficulty. Furthermore, the authors emphasized environmental factors – such as mentorship, competition, and isolation – as the primary influence in the development of these tendencies.
Although originally described in women, this phenomenon can also affect men, as well as a wide variety of people from different occupations and cultures.3-6 Furthermore, although environmental factors were originally linked as the primary driver of these tendencies, further research has suggested that personality factors play a larger role, and that up to 70% of people may experience this phenomenon in their lifetime.7 Personality traits such as perfectionism and neuroticism may be linked to the development of this phenomenon.3,8
There are several online screening questionnaires that can be used to gauge whether individuals experience some or most of these traits. On one such questionnaire, the Clance IP Scale,9 poses such questions as: “I have often succeeded on a test or task even though I was afraid that I would not do well before I undertook the task” and “I am afraid people important to me may find out that I am not as capable as they think I am.” There are 20 questions scored from 1 to 5 and a score of 40 or below suggests few impostor tendencies, while a score of 80 or above suggests the respondent often has intense IP experiences. The higher the score, the more frequently and seriously the impostor syndrome interferes in a person’s life. What is unclear is whether this worsens, improves, or stays the same throughout one’s career. Of interest is that my personal score at this time is 43; however, it would have been 89 had I taken the test during college and medical school. What is unclear to me from the literature is what factors may play a role in a person’s perception of their abilities and their personal confidence over time.
Why is this important? Given that we are all professionals, impostor tendencies appear to have significant impact in the context of our work. This may have impact on us both as employers and as employees.10 Individuals with impostor syndrome tendencies often characterize themselves negatively and perform poorly on self-appraisals.11 In a study of 201 Belgian white-collar workers, Vergauwe and colleagues found that impostor syndrome tendencies were negatively related to job satisfaction and organizational citizenship behavior; both of which could be influenced by a high degree of social support.10 Individuals with impostor syndrome tendencies do less career planning, explore career options less frequently, and are less inclined to lead.12,13 These tendencies can be detrimental as the most qualified people for a position or opportunity may not step forward for consideration. Employers may tend to overlook these individuals for promotions or for pay raises which could negatively influence future earnings. Furthermore, a person may experience increased burnout as they continuously try to overcompensate for what they perceive as their shortcomings. They may feel concerned they are letting others down or not performing to standards. They may derive less enjoyment from life because of the constant focus on feelings of inadequacy.14 Research along these lines suggest impostor syndrome tendencies can have adverse personal and health-related consequences and may increase social anxiety, depression, and overall psychological distress.15,16
What can we do about it? In a very interesting study by Zanchetta and colleagues, the authors studied 103 young employees and randomized them to receive coaching, training, or no intervention.17 Their findings showed that coaching was an effective mindset intervention which resulted in reduced impostor syndrome scores. Furthermore, fear of negative evaluation and the effect of coaching appeared to be significantly associated with a reduction in the impostor syndrome scores. Coaching appeared to improve self-enhancing attributions and self-efficacy with a reduction in the tendency of subjects to fear negative evaluation. The authors concluded that fostering a mindset shift by reducing the fear of negative evaluations through coaching demonstrated measurable and sustained improvements in overall impostor syndrome scores for participants.17
What do I suggest? It is clear this affects a significant percentage of physicians, health care professionals, and professionals in general. Harboring these tendencies can have a negative impact on health, professional achievement, income, and happiness. It is important to self-reflect, identify if you are at risk, and if so, take the opportunity to explore solutions. My recommendations are:
- Name it: Take the test and see how you score.
- Be mindful: Self-reflection will help you identify the behaviors that are interfering with your happiness and success.
- Write it down: Be strategic and document your plan for success to reinforce your accomplishments.
- Create a feedback group: Friends and colleagues can help to mitigate the negative effects of impostor syndrome tendencies.
- Speak up: Ask for help; coaching has been documented to reduce impostor syndrome scores and help lessen the burden of these tendencies.
- Step out of your comfort zone: Develop a mantra, break bigger challenges into smaller pieces, and acknowledge little wins along the way.
In conclusion, impostor syndrome appears to be highly prevalent in professionals including those of us in medicine. The experience can adversely affect our careers and ability to secure key leadership positions. As managers, we also must keep in mind our role in mentoring others and recognizing the potential impact of impostor syndrome on those who report to us. Recognition of this phenomenon – and understanding of the effects on oneself – is the first step in overcoming the negative effects and moving toward realization of one’s potential.
Dr. Brown is a professor of medicine at Wayne State University, division chief of gastroenterology and hepatology at Henry Ford Hospital, and associate medical director at the Henry Ford Hospital Transplant Institute, all in Detroit.
References
1. Clance PR, Imes S. Psychother Theory Res Pract. 1978 Fall;15(3):1-7.
2. Deaux D. In J.H.Harvey, W.J.Ickes and R.F. Kidd (Eds). New directions in attribution research. Vol. 1. New York: Halsted Press Division, Wiley. 1976; p 335-42.
3. Bernard NS et al. J Pers Assess. 2002;78(2):321-33.
4. Topping ME et al. Acad Psychol Bull. 1985;(7):213-26.
5. Langford J et al. Psychotherapy. 1993;30(3):495-501.
6. Chae JH et al. J Pers Assess. 1995;65(3):468-85.
7. Harvey JC et al. If I’m successful, why do I feel like a fake? New York: Random House, 1985.
8. Ross SR et al. Pers Individ Diff. 2001;31:1347-55.
9. Clance PR. The impostor phenomenon: When success makes you feel like a fake. Toronto: Bantam Books, 1985; p 20-2.
10. Vergauwe J et al. J Bus Psychol. 2015;30:565-81.
11. Leary MR et al. J Pers. 2000;68(4):725-56.
12. Neureiter M et al. Front Psychol. 2016;7:48.
13. Neureiter M et al. J Vocat Behav. 2017;98:56-69.
14. Duhigg C. The power of habit: Why we do what we do in life and business. New York: Random House, 2012.
15. Henning K et al. Med Educ. 1998 Sep;32(5):456-64.
16. Oriel K et al. Fam Med. 2004 Apr;36(4):248-52.
17. Zanchetta M et al. Front Psychol. 2020 May 15;11:405.
A few years ago, I was asked to give a talk on impostor syndrome at a national conference. My initial thought was “I am not even remotely qualified to give this talk.” Upon reflection, I think that was the first time I acknowledged that I, too, suffer from this syndrome.
There are many definitions and designations (e.g., impostor phenomenon or fraud syndrome), but the one I use most often is high-achieving individuals who are marked by an inability to internalize their accomplishments and a persistent fear of being exposed as a fraud. They live in fear that their incompetence will be exposed and they will be revealed as a fraud both intellectually and within their job or role. First described by Clance and Imes in 1978,1 the original authors observed that many highly respected and accomplished women did not experience an internal sense of success despite their education and evidence of academic achievement. Based in part on previous observations regarding the differential attribution of success in men and women,2 the authors suggested that two general principles were found to be at the heart of this syndrome. The first was that an unexpected performance outcome will be attributed to a temporary cause. The second was that an expected performance outcome will be attributed to a stable cause. As such, the authors originally suggested that women tended to explain failure with lack of ability, whereas men attributed failure to luck or task difficulty. Furthermore, the authors emphasized environmental factors – such as mentorship, competition, and isolation – as the primary influence in the development of these tendencies.
Although originally described in women, this phenomenon can also affect men, as well as a wide variety of people from different occupations and cultures.3-6 Furthermore, although environmental factors were originally linked as the primary driver of these tendencies, further research has suggested that personality factors play a larger role, and that up to 70% of people may experience this phenomenon in their lifetime.7 Personality traits such as perfectionism and neuroticism may be linked to the development of this phenomenon.3,8
There are several online screening questionnaires that can be used to gauge whether individuals experience some or most of these traits. On one such questionnaire, the Clance IP Scale,9 poses such questions as: “I have often succeeded on a test or task even though I was afraid that I would not do well before I undertook the task” and “I am afraid people important to me may find out that I am not as capable as they think I am.” There are 20 questions scored from 1 to 5 and a score of 40 or below suggests few impostor tendencies, while a score of 80 or above suggests the respondent often has intense IP experiences. The higher the score, the more frequently and seriously the impostor syndrome interferes in a person’s life. What is unclear is whether this worsens, improves, or stays the same throughout one’s career. Of interest is that my personal score at this time is 43; however, it would have been 89 had I taken the test during college and medical school. What is unclear to me from the literature is what factors may play a role in a person’s perception of their abilities and their personal confidence over time.
Why is this important? Given that we are all professionals, impostor tendencies appear to have significant impact in the context of our work. This may have impact on us both as employers and as employees.10 Individuals with impostor syndrome tendencies often characterize themselves negatively and perform poorly on self-appraisals.11 In a study of 201 Belgian white-collar workers, Vergauwe and colleagues found that impostor syndrome tendencies were negatively related to job satisfaction and organizational citizenship behavior; both of which could be influenced by a high degree of social support.10 Individuals with impostor syndrome tendencies do less career planning, explore career options less frequently, and are less inclined to lead.12,13 These tendencies can be detrimental as the most qualified people for a position or opportunity may not step forward for consideration. Employers may tend to overlook these individuals for promotions or for pay raises which could negatively influence future earnings. Furthermore, a person may experience increased burnout as they continuously try to overcompensate for what they perceive as their shortcomings. They may feel concerned they are letting others down or not performing to standards. They may derive less enjoyment from life because of the constant focus on feelings of inadequacy.14 Research along these lines suggest impostor syndrome tendencies can have adverse personal and health-related consequences and may increase social anxiety, depression, and overall psychological distress.15,16
What can we do about it? In a very interesting study by Zanchetta and colleagues, the authors studied 103 young employees and randomized them to receive coaching, training, or no intervention.17 Their findings showed that coaching was an effective mindset intervention which resulted in reduced impostor syndrome scores. Furthermore, fear of negative evaluation and the effect of coaching appeared to be significantly associated with a reduction in the impostor syndrome scores. Coaching appeared to improve self-enhancing attributions and self-efficacy with a reduction in the tendency of subjects to fear negative evaluation. The authors concluded that fostering a mindset shift by reducing the fear of negative evaluations through coaching demonstrated measurable and sustained improvements in overall impostor syndrome scores for participants.17
What do I suggest? It is clear this affects a significant percentage of physicians, health care professionals, and professionals in general. Harboring these tendencies can have a negative impact on health, professional achievement, income, and happiness. It is important to self-reflect, identify if you are at risk, and if so, take the opportunity to explore solutions. My recommendations are:
- Name it: Take the test and see how you score.
- Be mindful: Self-reflection will help you identify the behaviors that are interfering with your happiness and success.
- Write it down: Be strategic and document your plan for success to reinforce your accomplishments.
- Create a feedback group: Friends and colleagues can help to mitigate the negative effects of impostor syndrome tendencies.
- Speak up: Ask for help; coaching has been documented to reduce impostor syndrome scores and help lessen the burden of these tendencies.
- Step out of your comfort zone: Develop a mantra, break bigger challenges into smaller pieces, and acknowledge little wins along the way.
In conclusion, impostor syndrome appears to be highly prevalent in professionals including those of us in medicine. The experience can adversely affect our careers and ability to secure key leadership positions. As managers, we also must keep in mind our role in mentoring others and recognizing the potential impact of impostor syndrome on those who report to us. Recognition of this phenomenon – and understanding of the effects on oneself – is the first step in overcoming the negative effects and moving toward realization of one’s potential.
Dr. Brown is a professor of medicine at Wayne State University, division chief of gastroenterology and hepatology at Henry Ford Hospital, and associate medical director at the Henry Ford Hospital Transplant Institute, all in Detroit.
References
1. Clance PR, Imes S. Psychother Theory Res Pract. 1978 Fall;15(3):1-7.
2. Deaux D. In J.H.Harvey, W.J.Ickes and R.F. Kidd (Eds). New directions in attribution research. Vol. 1. New York: Halsted Press Division, Wiley. 1976; p 335-42.
3. Bernard NS et al. J Pers Assess. 2002;78(2):321-33.
4. Topping ME et al. Acad Psychol Bull. 1985;(7):213-26.
5. Langford J et al. Psychotherapy. 1993;30(3):495-501.
6. Chae JH et al. J Pers Assess. 1995;65(3):468-85.
7. Harvey JC et al. If I’m successful, why do I feel like a fake? New York: Random House, 1985.
8. Ross SR et al. Pers Individ Diff. 2001;31:1347-55.
9. Clance PR. The impostor phenomenon: When success makes you feel like a fake. Toronto: Bantam Books, 1985; p 20-2.
10. Vergauwe J et al. J Bus Psychol. 2015;30:565-81.
11. Leary MR et al. J Pers. 2000;68(4):725-56.
12. Neureiter M et al. Front Psychol. 2016;7:48.
13. Neureiter M et al. J Vocat Behav. 2017;98:56-69.
14. Duhigg C. The power of habit: Why we do what we do in life and business. New York: Random House, 2012.
15. Henning K et al. Med Educ. 1998 Sep;32(5):456-64.
16. Oriel K et al. Fam Med. 2004 Apr;36(4):248-52.
17. Zanchetta M et al. Front Psychol. 2020 May 15;11:405.
@GiJournal: An online platform to discuss the latest gastroenterology and hepatology publications
The last decade has seen an increased focus on the use of social media for medical education. Twitter, with over 330 million active users, is the most popular social media platform for medical education. We describe here our recent initiative to establish a weekly online gastroenterology-focused journal club on Twitter.
How was the idea conceived?
Sultan Mahmood, MD (@SultanMahmoodMD)
I joined #GITwitter at the end of 2019 and started following some of the leading experts in the field of gastroenterology and hepatology. It was a pleasant surprise to see how easy it was to engage with them and get expert opinions from across the world in real time. #MondayNightIBD, led by Aline Charabaty, MD, had become a phenomenon in the GI community and changed the perception of medical education in the digital world. There were online journal clubs for different medical subspecialties, including #NephroJC, #HOJournalClub, and #DermJC, but none for gastroenterology. Realizing this opportunity, and with guidance from Dr. Charabaty, we started @GiJournal in December of 2019 with weekly discussions.
@GiJournal started off as an informal discussion in which we would post a summary of the article and invite an expert in the field to comment. However, the interest in the journal club quickly took off as we gained more followers and a worldwide audience joined our journal club discussions on a weekly basis. As the COVID-19 pandemic took hold and endoscopy suites around the word closed, interest in online medical education grew. @GIJournal provided a platform for trainees and practicing physicians alike to stay up to date with the latest publications from the comfort of their homes. Needless to say, the journal club has evolved since its inception in that we now work with a team of experts and trainees who run the journal club on a rotating basis.
How does @GiJournal work?
Ijlal Akbar Ali, MD (@IjlalAkbar)
We have a large editorial board with volunteer faculty and trainees, all divided into four special interest groups (general GI/inflammatory bowel disease, interventional endoscopy/bariatric endoscopy, hepatology, and esophageal/motility disorders). Each week, a faculty member and a trainee pick a recently published article from a high-impact GI-focused journal. We also try to invite an expert of international repute (often the authors of the article themselves!) to engage as well. The faculty moderator and invited expert then work with the trainee to plan the session content. We post the topic and article on Monday. At 8 p.m. EST on Wednesday, the trainee posts a series of six to eight tweets summarizing the article. The faculty then asks the invited expert (and audience at large) a series of predetermined questions. Anyone can respond, share their opinion, and direct their own questions toward the moderator and expert who continually check their notifications and respond in real time. This brews into an hour-long discussion which covers not only the methodologic aspects of the article, but clinical practice in general. Discussions often trickle into the next day as people from different time zones participate. Everyone uses #GIJC at the end of their tweets which assists those following the article and facilitates indexing for future review. For those who miss or want to review sessions, we conveniently summarize all articles and corresponding discussions in a monthly publication, @GiJournal Digest, that is posted on Twitter for anyone to download, read and enjoy (Figure 1).
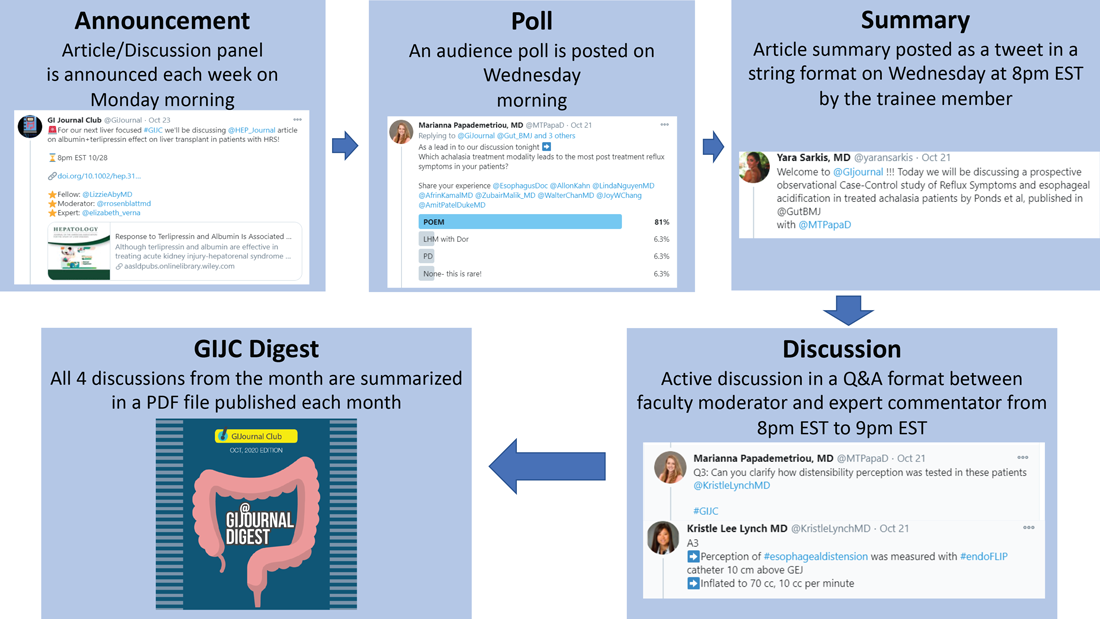
How is this different from any other journal club?
Atoosa Rabiee, MD (@AtoosaRabiee)
@GiJournal is unique in that it provides trainees and practicing gastroenterologists access to interactive discussions with both authors and world-renowned experts in the field. Online journal clubs operate with a flattened hierarchy; as such, they inherently break down access barriers to both the researchers who performed the study and key opinion leaders who commonly participate. There is no boundary as far as institutions or even countries. As a result, our platform has uncovered an unexpected degree of interest in live online discussion, and we have enjoyed collaborating and learning from experts from all over the world. @GiJournal also differs from conventional journal clubs by allowing trainees the opportunity to collaborate and engage with mentors from other institutions. As such, trainees develop relationships with experts in the field outside their home institutions, experts with whom they may not have had contact otherwise.
Although worldwide participation is a key strength of the online @GiJournal platform, it may be challenging for some members to attend the live discussion based on time difference. We account for this in two ways. First, participants are encouraged to continue with comments and questions afterward at their convenience, which allows experts and moderators to continue the conversation, often for several days. Second, to promote inclusivity, we have created a unique, customized publication to summarize and present the key points of conversation for each session. This asynchronous access is a quality not found in more traditional journal club formats. Finally, studies have shown that articles shared on social media tend to have increased citations and higher Altmetric scores.
What are the opportunities for trainees and recent graduates?
Sunil Amin, MD, MPH (@SunilAminMD)
Our surveys have shown that 30%-45% of the @GiJournal discussion participants are trainees. Both gastroenterology fellows and internal medicine residents from around the world are an integral part of each specialty panel for the weekly @GIjournal discussions. Trainees are paired up with a specific faculty mentor and together they choose an article for discussion, create a summary, informal twitter poll, and questions for the discussion. This direct access provides an opportunity for trainees to interact, ask questions, and learn from faculty in an informal atmosphere.
We have heard from multiple trainees who have developed long-term relationships with the experts and faculty mentors they worked with and are now also working on research projects. Additionally, trainees can bring the expertise they have now acquired back to their home institutions to pick articles, add specific teaching points, and enrich their local journal club discussions. Finally, trainees who present on the @GiJournal platform are given unique visibility to the many faculty members and opinion leaders participating in each discussion. This may facilitate future networking opportunities and enhance their CVs for future fellowship or employment applications.
Plans for the future?
Allon Kahn, MD (@AllonKahn)
Despite significant evolution and growth in @GiJournal over the past year, we are still actively working to expand our platform. Modes of online medical education, specifically Twitter-based GI journal club discussions, remain in their infancy. We see this @GiJournal as an opportunity for innovation as we plan for the year ahead. Our top priority for the upcoming year includes obtaining CME approval, which we are currently developing with Integrity CE (an Accreditation Council for Continuing Medical Education–accredited provider of CME for health care professionals). This will give an opportunity for the participants to be awarded CME credit when they participate in our weekly discussions. Other options being explored include starting a podcast and translation of @GiJournal Digest in different languages to reach a wider international audience. Furthermore, with the continued expansion of GI leaders and experts joining and engaging in Twitter, our options for unique and multidisciplinary discussion topics will continue to grow.
How can you join the @GiJournal discussions?
@SultanMahmoodMD
Joining the journal club discussion is easy. Just follow the @GiJournal handle on Twitter and turn on the notifications icon. Although we encourage everyone to “actively” participate in the discussion by asking questions or sharing your personal experience, joining the discussion as an “observer” is also a great way to learn. The discussion starts at 8 p.m. EST every Wednesday. Follow the #GIJC and the @GiJournal handle as questions are posted by the faculty moderator and answered by the experts. Even if you miss the discussion, the @GiJournal Digest is a great way to recap the discussions in an easy-to-read PDF format. The @GiJournal Digest is a monthly publication that archives the four @GiJournal club discussions in the previous month. Follow the link below to access the recent publications: http://ow.ly/uu2550C3RXX
Conclusion
In summary, we believe Twitter-based journal clubs offer an engaging way of virtual learning from the comfort of one’s home and a convenient way to directly interact with the experts. The success of @GiJournal highlights the importance of social media for medical education in the field of gastroenterology and hepatology and we look forward to developing this endeavor further.
Dr. Mahmood is clinical assistant professor of medicine, co–program director of the GI fellowship program, UB division of gastroenterology, hepatology & nutrition, State University of New York at Buffalo; Dr. Rabiee is assistant professor of medicine, director of hepatology, division of gastroenterology and hepatology, Washington DC VA Medical Center, Washington; Dr. Amin is assistant professor of medicine, director of endoscopy, The Lennar Foundation Medical Center, division of digestive health and liver disease, department of medicine, University of Miami; Dr. Kahn is assistant professor of medicine, division of gastroenterology & hepatology, Mayo Clinic, Scottsdale, Ariz.; and Dr. Akbar Ali is a gastroenterology fellow in the division of digestive diseases and nutrition, University of Oklahoma Health Sciences Center, Oklahoma City.
The last decade has seen an increased focus on the use of social media for medical education. Twitter, with over 330 million active users, is the most popular social media platform for medical education. We describe here our recent initiative to establish a weekly online gastroenterology-focused journal club on Twitter.
How was the idea conceived?
Sultan Mahmood, MD (@SultanMahmoodMD)
I joined #GITwitter at the end of 2019 and started following some of the leading experts in the field of gastroenterology and hepatology. It was a pleasant surprise to see how easy it was to engage with them and get expert opinions from across the world in real time. #MondayNightIBD, led by Aline Charabaty, MD, had become a phenomenon in the GI community and changed the perception of medical education in the digital world. There were online journal clubs for different medical subspecialties, including #NephroJC, #HOJournalClub, and #DermJC, but none for gastroenterology. Realizing this opportunity, and with guidance from Dr. Charabaty, we started @GiJournal in December of 2019 with weekly discussions.
@GiJournal started off as an informal discussion in which we would post a summary of the article and invite an expert in the field to comment. However, the interest in the journal club quickly took off as we gained more followers and a worldwide audience joined our journal club discussions on a weekly basis. As the COVID-19 pandemic took hold and endoscopy suites around the word closed, interest in online medical education grew. @GIJournal provided a platform for trainees and practicing physicians alike to stay up to date with the latest publications from the comfort of their homes. Needless to say, the journal club has evolved since its inception in that we now work with a team of experts and trainees who run the journal club on a rotating basis.
How does @GiJournal work?
Ijlal Akbar Ali, MD (@IjlalAkbar)
We have a large editorial board with volunteer faculty and trainees, all divided into four special interest groups (general GI/inflammatory bowel disease, interventional endoscopy/bariatric endoscopy, hepatology, and esophageal/motility disorders). Each week, a faculty member and a trainee pick a recently published article from a high-impact GI-focused journal. We also try to invite an expert of international repute (often the authors of the article themselves!) to engage as well. The faculty moderator and invited expert then work with the trainee to plan the session content. We post the topic and article on Monday. At 8 p.m. EST on Wednesday, the trainee posts a series of six to eight tweets summarizing the article. The faculty then asks the invited expert (and audience at large) a series of predetermined questions. Anyone can respond, share their opinion, and direct their own questions toward the moderator and expert who continually check their notifications and respond in real time. This brews into an hour-long discussion which covers not only the methodologic aspects of the article, but clinical practice in general. Discussions often trickle into the next day as people from different time zones participate. Everyone uses #GIJC at the end of their tweets which assists those following the article and facilitates indexing for future review. For those who miss or want to review sessions, we conveniently summarize all articles and corresponding discussions in a monthly publication, @GiJournal Digest, that is posted on Twitter for anyone to download, read and enjoy (Figure 1).
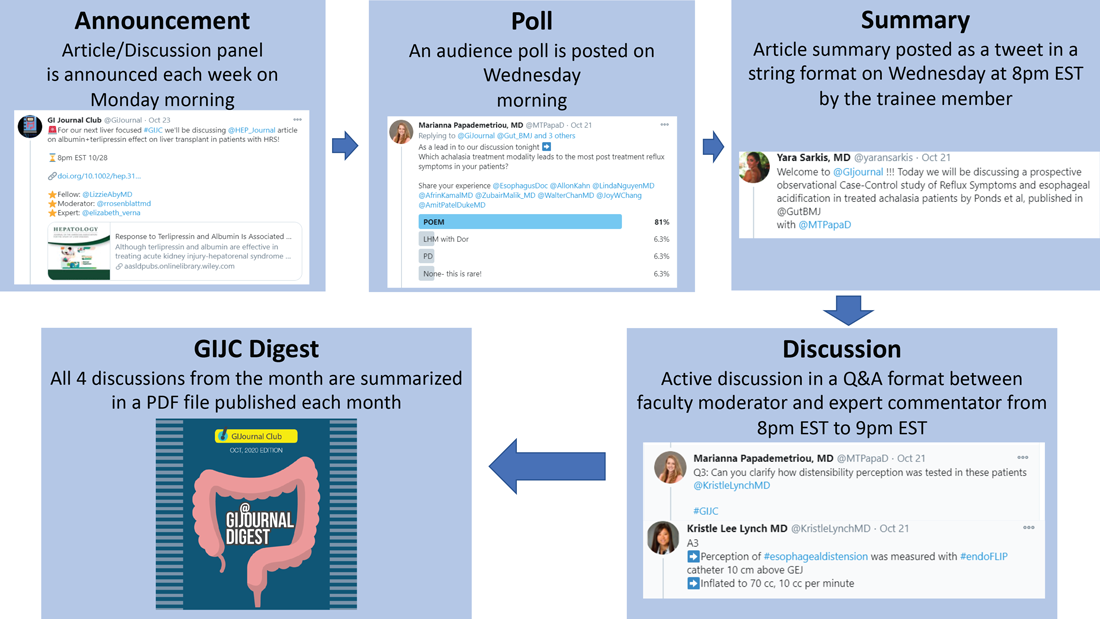
How is this different from any other journal club?
Atoosa Rabiee, MD (@AtoosaRabiee)
@GiJournal is unique in that it provides trainees and practicing gastroenterologists access to interactive discussions with both authors and world-renowned experts in the field. Online journal clubs operate with a flattened hierarchy; as such, they inherently break down access barriers to both the researchers who performed the study and key opinion leaders who commonly participate. There is no boundary as far as institutions or even countries. As a result, our platform has uncovered an unexpected degree of interest in live online discussion, and we have enjoyed collaborating and learning from experts from all over the world. @GiJournal also differs from conventional journal clubs by allowing trainees the opportunity to collaborate and engage with mentors from other institutions. As such, trainees develop relationships with experts in the field outside their home institutions, experts with whom they may not have had contact otherwise.
Although worldwide participation is a key strength of the online @GiJournal platform, it may be challenging for some members to attend the live discussion based on time difference. We account for this in two ways. First, participants are encouraged to continue with comments and questions afterward at their convenience, which allows experts and moderators to continue the conversation, often for several days. Second, to promote inclusivity, we have created a unique, customized publication to summarize and present the key points of conversation for each session. This asynchronous access is a quality not found in more traditional journal club formats. Finally, studies have shown that articles shared on social media tend to have increased citations and higher Altmetric scores.
What are the opportunities for trainees and recent graduates?
Sunil Amin, MD, MPH (@SunilAminMD)
Our surveys have shown that 30%-45% of the @GiJournal discussion participants are trainees. Both gastroenterology fellows and internal medicine residents from around the world are an integral part of each specialty panel for the weekly @GIjournal discussions. Trainees are paired up with a specific faculty mentor and together they choose an article for discussion, create a summary, informal twitter poll, and questions for the discussion. This direct access provides an opportunity for trainees to interact, ask questions, and learn from faculty in an informal atmosphere.
We have heard from multiple trainees who have developed long-term relationships with the experts and faculty mentors they worked with and are now also working on research projects. Additionally, trainees can bring the expertise they have now acquired back to their home institutions to pick articles, add specific teaching points, and enrich their local journal club discussions. Finally, trainees who present on the @GiJournal platform are given unique visibility to the many faculty members and opinion leaders participating in each discussion. This may facilitate future networking opportunities and enhance their CVs for future fellowship or employment applications.
Plans for the future?
Allon Kahn, MD (@AllonKahn)
Despite significant evolution and growth in @GiJournal over the past year, we are still actively working to expand our platform. Modes of online medical education, specifically Twitter-based GI journal club discussions, remain in their infancy. We see this @GiJournal as an opportunity for innovation as we plan for the year ahead. Our top priority for the upcoming year includes obtaining CME approval, which we are currently developing with Integrity CE (an Accreditation Council for Continuing Medical Education–accredited provider of CME for health care professionals). This will give an opportunity for the participants to be awarded CME credit when they participate in our weekly discussions. Other options being explored include starting a podcast and translation of @GiJournal Digest in different languages to reach a wider international audience. Furthermore, with the continued expansion of GI leaders and experts joining and engaging in Twitter, our options for unique and multidisciplinary discussion topics will continue to grow.
How can you join the @GiJournal discussions?
@SultanMahmoodMD
Joining the journal club discussion is easy. Just follow the @GiJournal handle on Twitter and turn on the notifications icon. Although we encourage everyone to “actively” participate in the discussion by asking questions or sharing your personal experience, joining the discussion as an “observer” is also a great way to learn. The discussion starts at 8 p.m. EST every Wednesday. Follow the #GIJC and the @GiJournal handle as questions are posted by the faculty moderator and answered by the experts. Even if you miss the discussion, the @GiJournal Digest is a great way to recap the discussions in an easy-to-read PDF format. The @GiJournal Digest is a monthly publication that archives the four @GiJournal club discussions in the previous month. Follow the link below to access the recent publications: http://ow.ly/uu2550C3RXX
Conclusion
In summary, we believe Twitter-based journal clubs offer an engaging way of virtual learning from the comfort of one’s home and a convenient way to directly interact with the experts. The success of @GiJournal highlights the importance of social media for medical education in the field of gastroenterology and hepatology and we look forward to developing this endeavor further.
Dr. Mahmood is clinical assistant professor of medicine, co–program director of the GI fellowship program, UB division of gastroenterology, hepatology & nutrition, State University of New York at Buffalo; Dr. Rabiee is assistant professor of medicine, director of hepatology, division of gastroenterology and hepatology, Washington DC VA Medical Center, Washington; Dr. Amin is assistant professor of medicine, director of endoscopy, The Lennar Foundation Medical Center, division of digestive health and liver disease, department of medicine, University of Miami; Dr. Kahn is assistant professor of medicine, division of gastroenterology & hepatology, Mayo Clinic, Scottsdale, Ariz.; and Dr. Akbar Ali is a gastroenterology fellow in the division of digestive diseases and nutrition, University of Oklahoma Health Sciences Center, Oklahoma City.
The last decade has seen an increased focus on the use of social media for medical education. Twitter, with over 330 million active users, is the most popular social media platform for medical education. We describe here our recent initiative to establish a weekly online gastroenterology-focused journal club on Twitter.
How was the idea conceived?
Sultan Mahmood, MD (@SultanMahmoodMD)
I joined #GITwitter at the end of 2019 and started following some of the leading experts in the field of gastroenterology and hepatology. It was a pleasant surprise to see how easy it was to engage with them and get expert opinions from across the world in real time. #MondayNightIBD, led by Aline Charabaty, MD, had become a phenomenon in the GI community and changed the perception of medical education in the digital world. There were online journal clubs for different medical subspecialties, including #NephroJC, #HOJournalClub, and #DermJC, but none for gastroenterology. Realizing this opportunity, and with guidance from Dr. Charabaty, we started @GiJournal in December of 2019 with weekly discussions.
@GiJournal started off as an informal discussion in which we would post a summary of the article and invite an expert in the field to comment. However, the interest in the journal club quickly took off as we gained more followers and a worldwide audience joined our journal club discussions on a weekly basis. As the COVID-19 pandemic took hold and endoscopy suites around the word closed, interest in online medical education grew. @GIJournal provided a platform for trainees and practicing physicians alike to stay up to date with the latest publications from the comfort of their homes. Needless to say, the journal club has evolved since its inception in that we now work with a team of experts and trainees who run the journal club on a rotating basis.
How does @GiJournal work?
Ijlal Akbar Ali, MD (@IjlalAkbar)
We have a large editorial board with volunteer faculty and trainees, all divided into four special interest groups (general GI/inflammatory bowel disease, interventional endoscopy/bariatric endoscopy, hepatology, and esophageal/motility disorders). Each week, a faculty member and a trainee pick a recently published article from a high-impact GI-focused journal. We also try to invite an expert of international repute (often the authors of the article themselves!) to engage as well. The faculty moderator and invited expert then work with the trainee to plan the session content. We post the topic and article on Monday. At 8 p.m. EST on Wednesday, the trainee posts a series of six to eight tweets summarizing the article. The faculty then asks the invited expert (and audience at large) a series of predetermined questions. Anyone can respond, share their opinion, and direct their own questions toward the moderator and expert who continually check their notifications and respond in real time. This brews into an hour-long discussion which covers not only the methodologic aspects of the article, but clinical practice in general. Discussions often trickle into the next day as people from different time zones participate. Everyone uses #GIJC at the end of their tweets which assists those following the article and facilitates indexing for future review. For those who miss or want to review sessions, we conveniently summarize all articles and corresponding discussions in a monthly publication, @GiJournal Digest, that is posted on Twitter for anyone to download, read and enjoy (Figure 1).
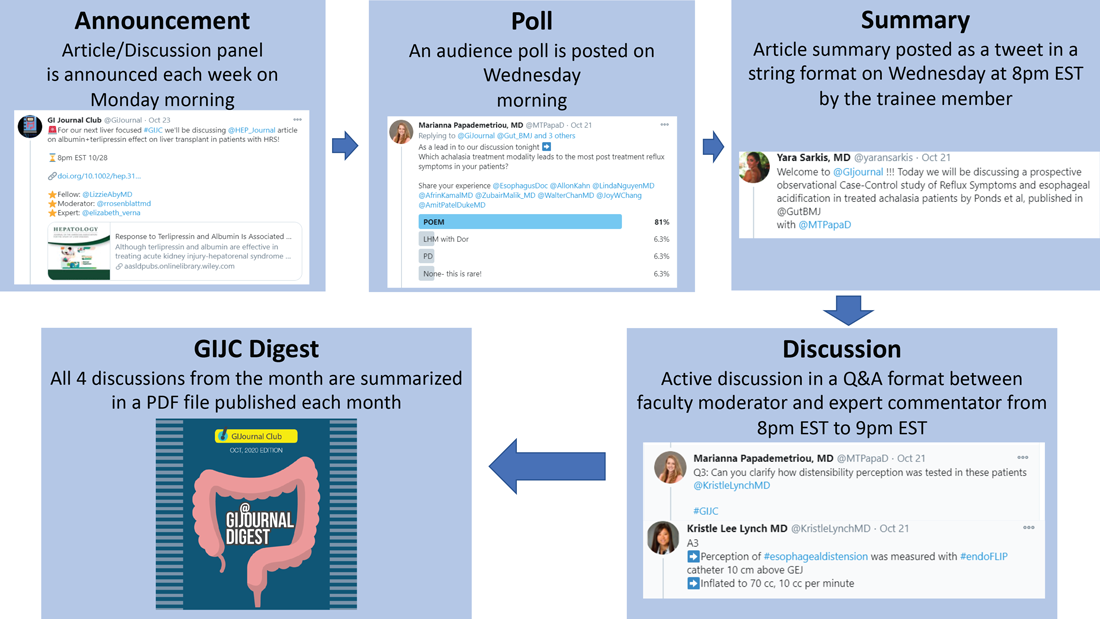
How is this different from any other journal club?
Atoosa Rabiee, MD (@AtoosaRabiee)
@GiJournal is unique in that it provides trainees and practicing gastroenterologists access to interactive discussions with both authors and world-renowned experts in the field. Online journal clubs operate with a flattened hierarchy; as such, they inherently break down access barriers to both the researchers who performed the study and key opinion leaders who commonly participate. There is no boundary as far as institutions or even countries. As a result, our platform has uncovered an unexpected degree of interest in live online discussion, and we have enjoyed collaborating and learning from experts from all over the world. @GiJournal also differs from conventional journal clubs by allowing trainees the opportunity to collaborate and engage with mentors from other institutions. As such, trainees develop relationships with experts in the field outside their home institutions, experts with whom they may not have had contact otherwise.
Although worldwide participation is a key strength of the online @GiJournal platform, it may be challenging for some members to attend the live discussion based on time difference. We account for this in two ways. First, participants are encouraged to continue with comments and questions afterward at their convenience, which allows experts and moderators to continue the conversation, often for several days. Second, to promote inclusivity, we have created a unique, customized publication to summarize and present the key points of conversation for each session. This asynchronous access is a quality not found in more traditional journal club formats. Finally, studies have shown that articles shared on social media tend to have increased citations and higher Altmetric scores.
What are the opportunities for trainees and recent graduates?
Sunil Amin, MD, MPH (@SunilAminMD)
Our surveys have shown that 30%-45% of the @GiJournal discussion participants are trainees. Both gastroenterology fellows and internal medicine residents from around the world are an integral part of each specialty panel for the weekly @GIjournal discussions. Trainees are paired up with a specific faculty mentor and together they choose an article for discussion, create a summary, informal twitter poll, and questions for the discussion. This direct access provides an opportunity for trainees to interact, ask questions, and learn from faculty in an informal atmosphere.
We have heard from multiple trainees who have developed long-term relationships with the experts and faculty mentors they worked with and are now also working on research projects. Additionally, trainees can bring the expertise they have now acquired back to their home institutions to pick articles, add specific teaching points, and enrich their local journal club discussions. Finally, trainees who present on the @GiJournal platform are given unique visibility to the many faculty members and opinion leaders participating in each discussion. This may facilitate future networking opportunities and enhance their CVs for future fellowship or employment applications.
Plans for the future?
Allon Kahn, MD (@AllonKahn)
Despite significant evolution and growth in @GiJournal over the past year, we are still actively working to expand our platform. Modes of online medical education, specifically Twitter-based GI journal club discussions, remain in their infancy. We see this @GiJournal as an opportunity for innovation as we plan for the year ahead. Our top priority for the upcoming year includes obtaining CME approval, which we are currently developing with Integrity CE (an Accreditation Council for Continuing Medical Education–accredited provider of CME for health care professionals). This will give an opportunity for the participants to be awarded CME credit when they participate in our weekly discussions. Other options being explored include starting a podcast and translation of @GiJournal Digest in different languages to reach a wider international audience. Furthermore, with the continued expansion of GI leaders and experts joining and engaging in Twitter, our options for unique and multidisciplinary discussion topics will continue to grow.
How can you join the @GiJournal discussions?
@SultanMahmoodMD
Joining the journal club discussion is easy. Just follow the @GiJournal handle on Twitter and turn on the notifications icon. Although we encourage everyone to “actively” participate in the discussion by asking questions or sharing your personal experience, joining the discussion as an “observer” is also a great way to learn. The discussion starts at 8 p.m. EST every Wednesday. Follow the #GIJC and the @GiJournal handle as questions are posted by the faculty moderator and answered by the experts. Even if you miss the discussion, the @GiJournal Digest is a great way to recap the discussions in an easy-to-read PDF format. The @GiJournal Digest is a monthly publication that archives the four @GiJournal club discussions in the previous month. Follow the link below to access the recent publications: http://ow.ly/uu2550C3RXX
Conclusion
In summary, we believe Twitter-based journal clubs offer an engaging way of virtual learning from the comfort of one’s home and a convenient way to directly interact with the experts. The success of @GiJournal highlights the importance of social media for medical education in the field of gastroenterology and hepatology and we look forward to developing this endeavor further.
Dr. Mahmood is clinical assistant professor of medicine, co–program director of the GI fellowship program, UB division of gastroenterology, hepatology & nutrition, State University of New York at Buffalo; Dr. Rabiee is assistant professor of medicine, director of hepatology, division of gastroenterology and hepatology, Washington DC VA Medical Center, Washington; Dr. Amin is assistant professor of medicine, director of endoscopy, The Lennar Foundation Medical Center, division of digestive health and liver disease, department of medicine, University of Miami; Dr. Kahn is assistant professor of medicine, division of gastroenterology & hepatology, Mayo Clinic, Scottsdale, Ariz.; and Dr. Akbar Ali is a gastroenterology fellow in the division of digestive diseases and nutrition, University of Oklahoma Health Sciences Center, Oklahoma City.
Coaching in medicine: A perspective
Coaching is a new topic in medicine. I first heard about coaching several years ago and met the term with skepticism. I was unsure how coaching was different than mentoring or advising and I wondered about its usefulness. However, the reason that I even started to learn about coaching was because I was struggling. I had finally arrived in my career, I had my dream job with two healthy kids, a perfect house, and good marriage. I kept hearing the refrain in my head: “Is this all there is?” I had this arrival fallacy that after all this striving and straining that I would finally be content. I felt unfulfilled and was dissatisfied with where I was that was affecting all parts of my life.
As I was wrestling with these thoughts, I had an opportunity to become a coach to residents around the country through the Association of Women Surgeons. I discussed with them what fills them up, what gets them down, how to set goals, and what their goals were for the year, as well as imposter syndrome. Impostor syndrome is defined as a pattern in which an individual doubts their accomplishments or talents and has a persistent internalized fear of being exposed as a “fraud.” Despite external evidence of their competence, those experiencing this phenomenon remain convinced that they are fooling everyone around them and do not deserve all they have achieved. Individuals incorrectly attribute their success to luck or interpret it as a result of deceiving others into thinking they are more intelligent than they perceive themselves to be. Imposter syndrome is prevalent and deep in medicine. As perfectionists, we are especially vulnerable to imposter syndrome as we set unrealistic ideals for ourselves. When we fail to reach these ideals, we feel like frauds, setting up this cycle of self-doubt that is toxic. When we feel that we can’t achieve the goals that we are striving for we will always find ourselves lacking. There is a slow, insidious erosion of self over the years. Imposter syndrome is well documented in medicine and is even felt as early as medical school.1,2
When I began coaching these residents the most profound thing that came out of these sessions was that my life was getting better – I knew what filled me up, what got me down, what my goals were for the year, and how I still deal with imposter syndrome. Coaching gave me a framework for helping determine what I wanted for the rest of my life. As I began coaching, I started learning all the ways in which I could figure out my values, my personal and professional goals, and perhaps most importantly, my relationships with myself and others.
Another perspective on coaching is to look at a professional athlete such as Tom Brady, one of the greatest quarterbacks of all time. He has a quarterback coach. No coach is going to be a better quarterback than Tom Brady. A coach for him is to be there as an advocate, break his fundamentals down technically, and help him improve upon what he already knows. A coach also identifies strengths and weaknesses, and helps him capitalize on both by bringing awareness, reflection, accountability, and support. If world-class athletes still want and benefit from coaching in a sport they have already mastered, coaching for physicians is just another tool to help us improve our abilities in and out of medicine.
Coaching is more encompassing than advising or mentoring. It is about examining deeply held beliefs to see if they are really serving us, if they are in line with our values and how we want to live our lives.
Coaching has also been validated in medicine in several papers. In an article by Dyrbye et al. in JAMA Internal Medicine, measures of emotional exhaustion and burnout decreased in physicians who were coached and increased in those who were not.3 In another study from this year by McGonagle et al., a randomized, controlled trial showed that primary care physicians who had sessions (as short as 6 weeks) to address burnout, psychological capital, and job satisfaction experienced an improvement in measures which persisted for 6 months after intervention.4 Numerous other articles in medicine also exist to demonstrate the effect of coaching on mitigating burnout at an institutional level.
Physicians are inherently driven by their love of learning. As physicians, we love getting to the root cause of any problem and coming up with creative solutions. Any challenge we have, or just wanting to improve the quality of our lives, can be addressed with coaching. As perpetual students we can use coaching to truly master ourselves.
Dr. Shah is associate professor of surgery, Rush University Medical Center, Chicago. Instagram: ami.shahmdcoaching.
References
1. Gottlieb M et al. Med Educ. 2020 Feb;54(2):116-24.
2. Villwock JA et al. Int J Med Educ. 2016 Oct 31;7:364-9.
3. Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5;179(10):1406-14.
4. McGonagle AK et al. J Occup Health Psychol. 2020 Apr 16. doi: 10.1037/ocp0000180.
Coaching is a new topic in medicine. I first heard about coaching several years ago and met the term with skepticism. I was unsure how coaching was different than mentoring or advising and I wondered about its usefulness. However, the reason that I even started to learn about coaching was because I was struggling. I had finally arrived in my career, I had my dream job with two healthy kids, a perfect house, and good marriage. I kept hearing the refrain in my head: “Is this all there is?” I had this arrival fallacy that after all this striving and straining that I would finally be content. I felt unfulfilled and was dissatisfied with where I was that was affecting all parts of my life.
As I was wrestling with these thoughts, I had an opportunity to become a coach to residents around the country through the Association of Women Surgeons. I discussed with them what fills them up, what gets them down, how to set goals, and what their goals were for the year, as well as imposter syndrome. Impostor syndrome is defined as a pattern in which an individual doubts their accomplishments or talents and has a persistent internalized fear of being exposed as a “fraud.” Despite external evidence of their competence, those experiencing this phenomenon remain convinced that they are fooling everyone around them and do not deserve all they have achieved. Individuals incorrectly attribute their success to luck or interpret it as a result of deceiving others into thinking they are more intelligent than they perceive themselves to be. Imposter syndrome is prevalent and deep in medicine. As perfectionists, we are especially vulnerable to imposter syndrome as we set unrealistic ideals for ourselves. When we fail to reach these ideals, we feel like frauds, setting up this cycle of self-doubt that is toxic. When we feel that we can’t achieve the goals that we are striving for we will always find ourselves lacking. There is a slow, insidious erosion of self over the years. Imposter syndrome is well documented in medicine and is even felt as early as medical school.1,2
When I began coaching these residents the most profound thing that came out of these sessions was that my life was getting better – I knew what filled me up, what got me down, what my goals were for the year, and how I still deal with imposter syndrome. Coaching gave me a framework for helping determine what I wanted for the rest of my life. As I began coaching, I started learning all the ways in which I could figure out my values, my personal and professional goals, and perhaps most importantly, my relationships with myself and others.
Another perspective on coaching is to look at a professional athlete such as Tom Brady, one of the greatest quarterbacks of all time. He has a quarterback coach. No coach is going to be a better quarterback than Tom Brady. A coach for him is to be there as an advocate, break his fundamentals down technically, and help him improve upon what he already knows. A coach also identifies strengths and weaknesses, and helps him capitalize on both by bringing awareness, reflection, accountability, and support. If world-class athletes still want and benefit from coaching in a sport they have already mastered, coaching for physicians is just another tool to help us improve our abilities in and out of medicine.
Coaching is more encompassing than advising or mentoring. It is about examining deeply held beliefs to see if they are really serving us, if they are in line with our values and how we want to live our lives.
Coaching has also been validated in medicine in several papers. In an article by Dyrbye et al. in JAMA Internal Medicine, measures of emotional exhaustion and burnout decreased in physicians who were coached and increased in those who were not.3 In another study from this year by McGonagle et al., a randomized, controlled trial showed that primary care physicians who had sessions (as short as 6 weeks) to address burnout, psychological capital, and job satisfaction experienced an improvement in measures which persisted for 6 months after intervention.4 Numerous other articles in medicine also exist to demonstrate the effect of coaching on mitigating burnout at an institutional level.
Physicians are inherently driven by their love of learning. As physicians, we love getting to the root cause of any problem and coming up with creative solutions. Any challenge we have, or just wanting to improve the quality of our lives, can be addressed with coaching. As perpetual students we can use coaching to truly master ourselves.
Dr. Shah is associate professor of surgery, Rush University Medical Center, Chicago. Instagram: ami.shahmdcoaching.
References
1. Gottlieb M et al. Med Educ. 2020 Feb;54(2):116-24.
2. Villwock JA et al. Int J Med Educ. 2016 Oct 31;7:364-9.
3. Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5;179(10):1406-14.
4. McGonagle AK et al. J Occup Health Psychol. 2020 Apr 16. doi: 10.1037/ocp0000180.
Coaching is a new topic in medicine. I first heard about coaching several years ago and met the term with skepticism. I was unsure how coaching was different than mentoring or advising and I wondered about its usefulness. However, the reason that I even started to learn about coaching was because I was struggling. I had finally arrived in my career, I had my dream job with two healthy kids, a perfect house, and good marriage. I kept hearing the refrain in my head: “Is this all there is?” I had this arrival fallacy that after all this striving and straining that I would finally be content. I felt unfulfilled and was dissatisfied with where I was that was affecting all parts of my life.
As I was wrestling with these thoughts, I had an opportunity to become a coach to residents around the country through the Association of Women Surgeons. I discussed with them what fills them up, what gets them down, how to set goals, and what their goals were for the year, as well as imposter syndrome. Impostor syndrome is defined as a pattern in which an individual doubts their accomplishments or talents and has a persistent internalized fear of being exposed as a “fraud.” Despite external evidence of their competence, those experiencing this phenomenon remain convinced that they are fooling everyone around them and do not deserve all they have achieved. Individuals incorrectly attribute their success to luck or interpret it as a result of deceiving others into thinking they are more intelligent than they perceive themselves to be. Imposter syndrome is prevalent and deep in medicine. As perfectionists, we are especially vulnerable to imposter syndrome as we set unrealistic ideals for ourselves. When we fail to reach these ideals, we feel like frauds, setting up this cycle of self-doubt that is toxic. When we feel that we can’t achieve the goals that we are striving for we will always find ourselves lacking. There is a slow, insidious erosion of self over the years. Imposter syndrome is well documented in medicine and is even felt as early as medical school.1,2
When I began coaching these residents the most profound thing that came out of these sessions was that my life was getting better – I knew what filled me up, what got me down, what my goals were for the year, and how I still deal with imposter syndrome. Coaching gave me a framework for helping determine what I wanted for the rest of my life. As I began coaching, I started learning all the ways in which I could figure out my values, my personal and professional goals, and perhaps most importantly, my relationships with myself and others.
Another perspective on coaching is to look at a professional athlete such as Tom Brady, one of the greatest quarterbacks of all time. He has a quarterback coach. No coach is going to be a better quarterback than Tom Brady. A coach for him is to be there as an advocate, break his fundamentals down technically, and help him improve upon what he already knows. A coach also identifies strengths and weaknesses, and helps him capitalize on both by bringing awareness, reflection, accountability, and support. If world-class athletes still want and benefit from coaching in a sport they have already mastered, coaching for physicians is just another tool to help us improve our abilities in and out of medicine.
Coaching is more encompassing than advising or mentoring. It is about examining deeply held beliefs to see if they are really serving us, if they are in line with our values and how we want to live our lives.
Coaching has also been validated in medicine in several papers. In an article by Dyrbye et al. in JAMA Internal Medicine, measures of emotional exhaustion and burnout decreased in physicians who were coached and increased in those who were not.3 In another study from this year by McGonagle et al., a randomized, controlled trial showed that primary care physicians who had sessions (as short as 6 weeks) to address burnout, psychological capital, and job satisfaction experienced an improvement in measures which persisted for 6 months after intervention.4 Numerous other articles in medicine also exist to demonstrate the effect of coaching on mitigating burnout at an institutional level.
Physicians are inherently driven by their love of learning. As physicians, we love getting to the root cause of any problem and coming up with creative solutions. Any challenge we have, or just wanting to improve the quality of our lives, can be addressed with coaching. As perpetual students we can use coaching to truly master ourselves.
Dr. Shah is associate professor of surgery, Rush University Medical Center, Chicago. Instagram: ami.shahmdcoaching.
References
1. Gottlieb M et al. Med Educ. 2020 Feb;54(2):116-24.
2. Villwock JA et al. Int J Med Educ. 2016 Oct 31;7:364-9.
3. Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5;179(10):1406-14.
4. McGonagle AK et al. J Occup Health Psychol. 2020 Apr 16. doi: 10.1037/ocp0000180.
Lessons learned as a gastroenterologist on social media
I have always been a strong believer in meeting patients where they obtain their health information. Early in my clinical training, I realized that patients are exposed to health information through traditional media formats and, increasingly, social media, rather than brief clinical encounters. Unlike traditional media, social media allows individuals the opportunity to post information without a third-party filter. However, this opens the door for untrained individuals to spread misinformation and disinformation. In health care, this could potentially disrupt public health efforts. Even innocent mistakes like overlooking the appropriate clinical context can cause issues. Traditional media outlets also have agendas that may leave certain conditions, therapies, and other facets of health care underrepresented. My belief is that experts should therefore be trained and incentivized to be spokespeople for their own areas of expertise. Furthermore, social media provides a novel opportunity to improve health literacy while humanizing and restoring fading trust in health care.
There are several items to consider before initiating on one’s social media journey: whether you are committed to exploring the space, what one’s purpose is on social media, who the intended target audience is, which platform is most appropriate to serve that purpose and audience, and what potential pitfalls there may be.
The first question to ask oneself is whether you are prepared to devote time to cultivating a social media presence and speak or be heard publicly. Regardless of the platform, a social media presence requires consistency and audience interaction. The decision to partake can be personal; I view social media as an extension of in-person interaction, but not everyone is willing to commit to increased accessibility and visibility. Social media can still be valuable to those who choose to observe and learn rather than post.
Next is what one’s purpose is with being on social media. This can vary from peer education, boosting health literacy for patients, or using social media as a news source, networking tool, or a creative outlet. While my social media activity supports all these, my primary purpose is the distribution of accurate health information as a trained expert. When I started, I was one of few academic gastroenterologists uniquely positioned to bridge the elusive gap between the young, Gen Z crowd and academic medicine. Of similar importance is defining one’s target audience: patients, trainees, colleagues, or the general public.
Because there are numerous social media platforms, and only more to come in the future, it is critical to focus only on platforms that will serve one’s purpose and audience. Additionally, some may find more joy or agility in using one platform over the other. While I am one of the few clinicians who are adept at building communities across multiple rapidly evolving social media platforms, I will be the first to admit that it takes time to fully understand each platform with its ever-growing array of features. I find myself better at some platforms over others and, depending on my goals, I often will shift my focus from one to another.
Each platform has its pros and cons. Twitter is perhaps the most appropriate platform for starters. Easy to use with the least preparation necessary for every post, it also serves as the primary platform for academic discussion among all the popular social media platforms. Over the past few years, hundreds of gastroenterologists have become active on Twitter, which allows for ample networking opportunities and potential collaborations. The space has evolved to house various structured chats and learning opportunities as described by accounts like @MondayNightIBD, @ScopingSundays, #TracingTuesday, and @GIJournal. All major GI journals and societies are also present on Twitter and disseminating the latest information. Now a vestige of the past when text within tweets was not searchable, hashtags were used to curate discussion because searching by hashtag could reveal the latest discussion surrounding a topic and help identify others with a similar interest. Hashtags now remain relevant when crafting tweets, as the strategic inclusion of hashtags can help your content reach those who share an interest. A hashtag ontology was previously published to standardize academic conversation online in gastroenterology. Twitter also boasts features like polls that also help audiences engage.
Twitter has its disadvantages, however. Conversation is often siloed and difficult to reach audiences who don’t already follow you or others associated with you. Tweets disappear quickly in one’s feed and are often not seen by your followers. It lacks the visual appeal of other image- and video-based platforms that tend to attract more members of the general public. (Twitter lags behind these other platforms in monthly users) Other platforms like Facebook, Instagram, YouTube, LinkedIn, and TikTok have other benefits. Facebook may help foster community discussions in groups and business pages are also helpful for practice promotion. Instagram has gained popularity for educational purposes over the past 2 years, given its pairing with imagery and room for a lengthier caption. It has a variety of additional features like the temporary Instagram Stories that last 24 hours (which also allows for polling), question and answer, and livestream options. Other platforms like YouTube and TikTok have greater potential to reach audiences who otherwise would not see your content, with the former having the benefit of being highly searchable and the latter being the social media app with fastest growing popularity.
Having grown up with the Internet-based instant messaging and social media platforms, I have always enjoyed the medium as a way to connect with others. However, productive engagement on these platforms came much later. During a brief stint as part of the ABC News medical unit, I learned how Twitter was used to facilitate weekly chats around a specific topic online. I began exploring my own social media voice, which quickly gave way to live-tweeting medical conferences, hosting and participating Twitter chats myself, and guiding colleagues and professional societies to greater adoption of social media. In an attempt to introduce a divisional social media account during my fellowship, I learned of institutional barriers including antiquated policies that actively dissuaded social media use. I became increasingly involved on committees in our main GI societies after engaging in multiple research projects using social media data looking at how GI journals promote their content online, the associations between social media presence and institutional ranking, social media behavior at medical conferences, and the evolving perspectives of training program leadership regarding social media.
The pitfalls of social media remain a major concern for physicians and employers alike. First and foremost, it is important to review one’s institutional social media policy prior to starting, as individuals are ultimately held to their local policies. Not only can social media activity be a major liability for a health care employer, but also in the general public’s trust in health professionals. Protecting patient privacy and safety are of utmost concern, and physicians must be mindful not to inadvertently reveal patient identity. HIPAA violations are not limited to only naming patients by name or photo; descriptions of procedural cases and posting patient-related images such as radiographs or endoscopic images may reveal patient identity if there are unique details on these images (e.g., a radio-opaque necklace on x-ray or a particular swallowed foreign body).
Another disadvantage of social media is being approached with personal medical questions. I universally decline to answer these inquiries, citing the need to perform a comprehensive review of one’s medical chart and perform an in-person physical exam to fully assess a patient. The distinction between education and advice is subtle, yet important to recognize. Similarly, the need to uphold professionalism online is important. Short messages on social media can be misinterpreted by colleagues and the public. Not only can these interactions be potentially detrimental to one’s career, but it can further erode trust in health care if patients perceive this as fragmentation of the health care system. On platforms that encourage humor and creativity like TikTok, there have also been medical professionals and students publicly criticized and penalized for posting unprofessional content mocking patients.
With the introduction of social media influencers in recent years, some professionals have amassed followings, introducing yet another set of concerns. One is being approached with sponsorship and endorsement offers, as any agreements must be in accordance with institutional policy. As one’s following grows, there may be other concerns of safety both online and in real life. Online concerns include issues with impersonation and use of photos or written content without permission. On the surface this may not seem like a significant concern, but there have been situations where family photos are distributed to intended audiences or one’s likeness is used to endorse a product.
In addition to physical safety, another unintended consequence of social media use is its impact on one’s mental health. As social media tends to be a highlight reel, it is easy to be consumed by comparison with colleagues and their lives on social media, whether it truly reflects one’s actual life or not.
My ability to understand multiple social media platforms and anticipate a growing set of risks and concerns with using social media is what led to my involvement with multiple GI societies and appointment by my institution’s CEO to serve as the first chief medical social media officer. My desire to help other professionals with the journey also led to the formation of the Association for Healthcare Social Media, the first 501(c)(3) nonprofit professional organization devoted to health professionals on social media. There is tremendous opportunity to impact public health through social media, especially with regards to raising awareness about underrepresented conditions and presenting information that is accurate. Many barriers remain to the widespread adoption of social media by health professionals, such as the lack of financial or academic incentives. For now, there is every indication that social media is here to stay, and it will likely continue to play an important role in how we communicate with our patients.
AGA can be found online at @AmerGastroAssn (Facebook, Instagram, and Twitter) and @AGA_Gastro, @AGA_CGH, and @AGA_CMGH (Facebook and Twitter).
Dr. Chiang is assistant professor of medicine, division of gastroenterology & hepatology, director, endoscopic bariatric program, chief medical social media officer, Jefferson Health, Philadelphia, and president, Association for Healthcare Social Media, @austinchiangmd
I have always been a strong believer in meeting patients where they obtain their health information. Early in my clinical training, I realized that patients are exposed to health information through traditional media formats and, increasingly, social media, rather than brief clinical encounters. Unlike traditional media, social media allows individuals the opportunity to post information without a third-party filter. However, this opens the door for untrained individuals to spread misinformation and disinformation. In health care, this could potentially disrupt public health efforts. Even innocent mistakes like overlooking the appropriate clinical context can cause issues. Traditional media outlets also have agendas that may leave certain conditions, therapies, and other facets of health care underrepresented. My belief is that experts should therefore be trained and incentivized to be spokespeople for their own areas of expertise. Furthermore, social media provides a novel opportunity to improve health literacy while humanizing and restoring fading trust in health care.
There are several items to consider before initiating on one’s social media journey: whether you are committed to exploring the space, what one’s purpose is on social media, who the intended target audience is, which platform is most appropriate to serve that purpose and audience, and what potential pitfalls there may be.
The first question to ask oneself is whether you are prepared to devote time to cultivating a social media presence and speak or be heard publicly. Regardless of the platform, a social media presence requires consistency and audience interaction. The decision to partake can be personal; I view social media as an extension of in-person interaction, but not everyone is willing to commit to increased accessibility and visibility. Social media can still be valuable to those who choose to observe and learn rather than post.
Next is what one’s purpose is with being on social media. This can vary from peer education, boosting health literacy for patients, or using social media as a news source, networking tool, or a creative outlet. While my social media activity supports all these, my primary purpose is the distribution of accurate health information as a trained expert. When I started, I was one of few academic gastroenterologists uniquely positioned to bridge the elusive gap between the young, Gen Z crowd and academic medicine. Of similar importance is defining one’s target audience: patients, trainees, colleagues, or the general public.
Because there are numerous social media platforms, and only more to come in the future, it is critical to focus only on platforms that will serve one’s purpose and audience. Additionally, some may find more joy or agility in using one platform over the other. While I am one of the few clinicians who are adept at building communities across multiple rapidly evolving social media platforms, I will be the first to admit that it takes time to fully understand each platform with its ever-growing array of features. I find myself better at some platforms over others and, depending on my goals, I often will shift my focus from one to another.
Each platform has its pros and cons. Twitter is perhaps the most appropriate platform for starters. Easy to use with the least preparation necessary for every post, it also serves as the primary platform for academic discussion among all the popular social media platforms. Over the past few years, hundreds of gastroenterologists have become active on Twitter, which allows for ample networking opportunities and potential collaborations. The space has evolved to house various structured chats and learning opportunities as described by accounts like @MondayNightIBD, @ScopingSundays, #TracingTuesday, and @GIJournal. All major GI journals and societies are also present on Twitter and disseminating the latest information. Now a vestige of the past when text within tweets was not searchable, hashtags were used to curate discussion because searching by hashtag could reveal the latest discussion surrounding a topic and help identify others with a similar interest. Hashtags now remain relevant when crafting tweets, as the strategic inclusion of hashtags can help your content reach those who share an interest. A hashtag ontology was previously published to standardize academic conversation online in gastroenterology. Twitter also boasts features like polls that also help audiences engage.
Twitter has its disadvantages, however. Conversation is often siloed and difficult to reach audiences who don’t already follow you or others associated with you. Tweets disappear quickly in one’s feed and are often not seen by your followers. It lacks the visual appeal of other image- and video-based platforms that tend to attract more members of the general public. (Twitter lags behind these other platforms in monthly users) Other platforms like Facebook, Instagram, YouTube, LinkedIn, and TikTok have other benefits. Facebook may help foster community discussions in groups and business pages are also helpful for practice promotion. Instagram has gained popularity for educational purposes over the past 2 years, given its pairing with imagery and room for a lengthier caption. It has a variety of additional features like the temporary Instagram Stories that last 24 hours (which also allows for polling), question and answer, and livestream options. Other platforms like YouTube and TikTok have greater potential to reach audiences who otherwise would not see your content, with the former having the benefit of being highly searchable and the latter being the social media app with fastest growing popularity.
Having grown up with the Internet-based instant messaging and social media platforms, I have always enjoyed the medium as a way to connect with others. However, productive engagement on these platforms came much later. During a brief stint as part of the ABC News medical unit, I learned how Twitter was used to facilitate weekly chats around a specific topic online. I began exploring my own social media voice, which quickly gave way to live-tweeting medical conferences, hosting and participating Twitter chats myself, and guiding colleagues and professional societies to greater adoption of social media. In an attempt to introduce a divisional social media account during my fellowship, I learned of institutional barriers including antiquated policies that actively dissuaded social media use. I became increasingly involved on committees in our main GI societies after engaging in multiple research projects using social media data looking at how GI journals promote their content online, the associations between social media presence and institutional ranking, social media behavior at medical conferences, and the evolving perspectives of training program leadership regarding social media.
The pitfalls of social media remain a major concern for physicians and employers alike. First and foremost, it is important to review one’s institutional social media policy prior to starting, as individuals are ultimately held to their local policies. Not only can social media activity be a major liability for a health care employer, but also in the general public’s trust in health professionals. Protecting patient privacy and safety are of utmost concern, and physicians must be mindful not to inadvertently reveal patient identity. HIPAA violations are not limited to only naming patients by name or photo; descriptions of procedural cases and posting patient-related images such as radiographs or endoscopic images may reveal patient identity if there are unique details on these images (e.g., a radio-opaque necklace on x-ray or a particular swallowed foreign body).
Another disadvantage of social media is being approached with personal medical questions. I universally decline to answer these inquiries, citing the need to perform a comprehensive review of one’s medical chart and perform an in-person physical exam to fully assess a patient. The distinction between education and advice is subtle, yet important to recognize. Similarly, the need to uphold professionalism online is important. Short messages on social media can be misinterpreted by colleagues and the public. Not only can these interactions be potentially detrimental to one’s career, but it can further erode trust in health care if patients perceive this as fragmentation of the health care system. On platforms that encourage humor and creativity like TikTok, there have also been medical professionals and students publicly criticized and penalized for posting unprofessional content mocking patients.
With the introduction of social media influencers in recent years, some professionals have amassed followings, introducing yet another set of concerns. One is being approached with sponsorship and endorsement offers, as any agreements must be in accordance with institutional policy. As one’s following grows, there may be other concerns of safety both online and in real life. Online concerns include issues with impersonation and use of photos or written content without permission. On the surface this may not seem like a significant concern, but there have been situations where family photos are distributed to intended audiences or one’s likeness is used to endorse a product.
In addition to physical safety, another unintended consequence of social media use is its impact on one’s mental health. As social media tends to be a highlight reel, it is easy to be consumed by comparison with colleagues and their lives on social media, whether it truly reflects one’s actual life or not.
My ability to understand multiple social media platforms and anticipate a growing set of risks and concerns with using social media is what led to my involvement with multiple GI societies and appointment by my institution’s CEO to serve as the first chief medical social media officer. My desire to help other professionals with the journey also led to the formation of the Association for Healthcare Social Media, the first 501(c)(3) nonprofit professional organization devoted to health professionals on social media. There is tremendous opportunity to impact public health through social media, especially with regards to raising awareness about underrepresented conditions and presenting information that is accurate. Many barriers remain to the widespread adoption of social media by health professionals, such as the lack of financial or academic incentives. For now, there is every indication that social media is here to stay, and it will likely continue to play an important role in how we communicate with our patients.
AGA can be found online at @AmerGastroAssn (Facebook, Instagram, and Twitter) and @AGA_Gastro, @AGA_CGH, and @AGA_CMGH (Facebook and Twitter).
Dr. Chiang is assistant professor of medicine, division of gastroenterology & hepatology, director, endoscopic bariatric program, chief medical social media officer, Jefferson Health, Philadelphia, and president, Association for Healthcare Social Media, @austinchiangmd
I have always been a strong believer in meeting patients where they obtain their health information. Early in my clinical training, I realized that patients are exposed to health information through traditional media formats and, increasingly, social media, rather than brief clinical encounters. Unlike traditional media, social media allows individuals the opportunity to post information without a third-party filter. However, this opens the door for untrained individuals to spread misinformation and disinformation. In health care, this could potentially disrupt public health efforts. Even innocent mistakes like overlooking the appropriate clinical context can cause issues. Traditional media outlets also have agendas that may leave certain conditions, therapies, and other facets of health care underrepresented. My belief is that experts should therefore be trained and incentivized to be spokespeople for their own areas of expertise. Furthermore, social media provides a novel opportunity to improve health literacy while humanizing and restoring fading trust in health care.
There are several items to consider before initiating on one’s social media journey: whether you are committed to exploring the space, what one’s purpose is on social media, who the intended target audience is, which platform is most appropriate to serve that purpose and audience, and what potential pitfalls there may be.
The first question to ask oneself is whether you are prepared to devote time to cultivating a social media presence and speak or be heard publicly. Regardless of the platform, a social media presence requires consistency and audience interaction. The decision to partake can be personal; I view social media as an extension of in-person interaction, but not everyone is willing to commit to increased accessibility and visibility. Social media can still be valuable to those who choose to observe and learn rather than post.
Next is what one’s purpose is with being on social media. This can vary from peer education, boosting health literacy for patients, or using social media as a news source, networking tool, or a creative outlet. While my social media activity supports all these, my primary purpose is the distribution of accurate health information as a trained expert. When I started, I was one of few academic gastroenterologists uniquely positioned to bridge the elusive gap between the young, Gen Z crowd and academic medicine. Of similar importance is defining one’s target audience: patients, trainees, colleagues, or the general public.
Because there are numerous social media platforms, and only more to come in the future, it is critical to focus only on platforms that will serve one’s purpose and audience. Additionally, some may find more joy or agility in using one platform over the other. While I am one of the few clinicians who are adept at building communities across multiple rapidly evolving social media platforms, I will be the first to admit that it takes time to fully understand each platform with its ever-growing array of features. I find myself better at some platforms over others and, depending on my goals, I often will shift my focus from one to another.
Each platform has its pros and cons. Twitter is perhaps the most appropriate platform for starters. Easy to use with the least preparation necessary for every post, it also serves as the primary platform for academic discussion among all the popular social media platforms. Over the past few years, hundreds of gastroenterologists have become active on Twitter, which allows for ample networking opportunities and potential collaborations. The space has evolved to house various structured chats and learning opportunities as described by accounts like @MondayNightIBD, @ScopingSundays, #TracingTuesday, and @GIJournal. All major GI journals and societies are also present on Twitter and disseminating the latest information. Now a vestige of the past when text within tweets was not searchable, hashtags were used to curate discussion because searching by hashtag could reveal the latest discussion surrounding a topic and help identify others with a similar interest. Hashtags now remain relevant when crafting tweets, as the strategic inclusion of hashtags can help your content reach those who share an interest. A hashtag ontology was previously published to standardize academic conversation online in gastroenterology. Twitter also boasts features like polls that also help audiences engage.
Twitter has its disadvantages, however. Conversation is often siloed and difficult to reach audiences who don’t already follow you or others associated with you. Tweets disappear quickly in one’s feed and are often not seen by your followers. It lacks the visual appeal of other image- and video-based platforms that tend to attract more members of the general public. (Twitter lags behind these other platforms in monthly users) Other platforms like Facebook, Instagram, YouTube, LinkedIn, and TikTok have other benefits. Facebook may help foster community discussions in groups and business pages are also helpful for practice promotion. Instagram has gained popularity for educational purposes over the past 2 years, given its pairing with imagery and room for a lengthier caption. It has a variety of additional features like the temporary Instagram Stories that last 24 hours (which also allows for polling), question and answer, and livestream options. Other platforms like YouTube and TikTok have greater potential to reach audiences who otherwise would not see your content, with the former having the benefit of being highly searchable and the latter being the social media app with fastest growing popularity.
Having grown up with the Internet-based instant messaging and social media platforms, I have always enjoyed the medium as a way to connect with others. However, productive engagement on these platforms came much later. During a brief stint as part of the ABC News medical unit, I learned how Twitter was used to facilitate weekly chats around a specific topic online. I began exploring my own social media voice, which quickly gave way to live-tweeting medical conferences, hosting and participating Twitter chats myself, and guiding colleagues and professional societies to greater adoption of social media. In an attempt to introduce a divisional social media account during my fellowship, I learned of institutional barriers including antiquated policies that actively dissuaded social media use. I became increasingly involved on committees in our main GI societies after engaging in multiple research projects using social media data looking at how GI journals promote their content online, the associations between social media presence and institutional ranking, social media behavior at medical conferences, and the evolving perspectives of training program leadership regarding social media.
The pitfalls of social media remain a major concern for physicians and employers alike. First and foremost, it is important to review one’s institutional social media policy prior to starting, as individuals are ultimately held to their local policies. Not only can social media activity be a major liability for a health care employer, but also in the general public’s trust in health professionals. Protecting patient privacy and safety are of utmost concern, and physicians must be mindful not to inadvertently reveal patient identity. HIPAA violations are not limited to only naming patients by name or photo; descriptions of procedural cases and posting patient-related images such as radiographs or endoscopic images may reveal patient identity if there are unique details on these images (e.g., a radio-opaque necklace on x-ray or a particular swallowed foreign body).
Another disadvantage of social media is being approached with personal medical questions. I universally decline to answer these inquiries, citing the need to perform a comprehensive review of one’s medical chart and perform an in-person physical exam to fully assess a patient. The distinction between education and advice is subtle, yet important to recognize. Similarly, the need to uphold professionalism online is important. Short messages on social media can be misinterpreted by colleagues and the public. Not only can these interactions be potentially detrimental to one’s career, but it can further erode trust in health care if patients perceive this as fragmentation of the health care system. On platforms that encourage humor and creativity like TikTok, there have also been medical professionals and students publicly criticized and penalized for posting unprofessional content mocking patients.
With the introduction of social media influencers in recent years, some professionals have amassed followings, introducing yet another set of concerns. One is being approached with sponsorship and endorsement offers, as any agreements must be in accordance with institutional policy. As one’s following grows, there may be other concerns of safety both online and in real life. Online concerns include issues with impersonation and use of photos or written content without permission. On the surface this may not seem like a significant concern, but there have been situations where family photos are distributed to intended audiences or one’s likeness is used to endorse a product.
In addition to physical safety, another unintended consequence of social media use is its impact on one’s mental health. As social media tends to be a highlight reel, it is easy to be consumed by comparison with colleagues and their lives on social media, whether it truly reflects one’s actual life or not.
My ability to understand multiple social media platforms and anticipate a growing set of risks and concerns with using social media is what led to my involvement with multiple GI societies and appointment by my institution’s CEO to serve as the first chief medical social media officer. My desire to help other professionals with the journey also led to the formation of the Association for Healthcare Social Media, the first 501(c)(3) nonprofit professional organization devoted to health professionals on social media. There is tremendous opportunity to impact public health through social media, especially with regards to raising awareness about underrepresented conditions and presenting information that is accurate. Many barriers remain to the widespread adoption of social media by health professionals, such as the lack of financial or academic incentives. For now, there is every indication that social media is here to stay, and it will likely continue to play an important role in how we communicate with our patients.
AGA can be found online at @AmerGastroAssn (Facebook, Instagram, and Twitter) and @AGA_Gastro, @AGA_CGH, and @AGA_CMGH (Facebook and Twitter).
Dr. Chiang is assistant professor of medicine, division of gastroenterology & hepatology, director, endoscopic bariatric program, chief medical social media officer, Jefferson Health, Philadelphia, and president, Association for Healthcare Social Media, @austinchiangmd
Gastroenterology practice evaluations: Can patients get satisfaction?
Although largely untouched by the first and second industrial revolutions in the 18th and 20th centuries, the practice of medicine in the 21st century is increasingly susceptible to the vast transformative power of the third – and rapidly approaching fourth – industrial revolutions. New technological advances and their associated distribution of knowledge and connectedness have allowed patients unprecedented access to health care information. The salutary effects of this change is manifest in a diversity of areas, including registries that facilitate participation in state of the art research such as ClinicalTrials.gov and the ability to track nascent trends in infectious diseases with Google searches.1
Although the stakes may seem lower when patients go online to choose a practitioner, the reality demonstrates just how important those search results can be. With parallels of similar trends in other sectors, there is an increasing emphasis on ranking health care facilities, practitioners, and medical experiences. This phenomenon extends beyond private Internet sites into government scorecards, which has significant implications. But even with widespread access to information, there is frequently a lack of context for interpreting these data. Consequently, it is worth exploring why measuring satisfaction can be important, how patients can rate practitioners, and what to do with the available information to improve care delivery.
The idea to measure patient satisfaction of delivered health care began in earnest during the 1980s with Irwin Press and Rodney Ganey collaborating to create formal processes for collecting data on the “salient aspects of ... health care experience, [involving] the interaction of expectations, preferences, and satisfaction with medical care.”2,3 The enthusiasm for collecting these data has grown greatly since that time. More recently, the federal government began obtaining data in 2002 when the Centers for Medicaid & Medicare Services and the Agency for Healthcare Research and Quality (AHRQ) collaborated to develop a standardized questionnaire for hospitalized patients known as the Hospital Consumer Assessment of Healthcare Providers and Systems, or HCAHPS.4 Subsequently, standardized survey instruments have been developed for nearly every phase of care, including outpatient care (CG-CAHPS), emergency care (ED-CAHPS), and ambulatory surgery care (OAS-CAHPS). These instruments are particularly relevant to gastroenterologists, with questions querying patients about preprocedure instructions, surgery center check-in processes, comfort of procedure and waiting rooms, friendliness of providers, and quality of postprocedure information.
The focus on rating satisfaction intensified in 2010 after the passage of the Affordable Care Act (ACA). Around this time, patient satisfaction and health outcomes became more deeply integrated concepts in health care quality. As part of a broader emphasis in this area, CMS initiated the hospital value-based purchasing (VBP) program, which tied incentive payments for Medicare beneficiaries to hospital-based health care quality and patient satisfaction. Within this schema, 25% of performance, and its associated economic stakes, is measured by HCAHPS scores.5 Other value programs such as the Merit-Based Incentive Payment Program (MIPS) include CAHPS instruments as optional assessments of quality.
Given the financial risks linked to satisfaction rankings and their online visibility, many argue that patient satisfaction is prioritized in organizations above more clinically meaningful metrics. Studies have shown, however, that high levels of patient satisfaction can lead to increased patient loyalty, treatment adherence, patient retention, staff morale, and personal and professional satisfaction.6,7 In fact, not surprisingly, there is an inverse correlation between patient satisfaction and the rates of malpractice lawsuits.7-10
Despite the growing relevance of patient perceptions to clinical practice, measuring satisfaction remains a challenge. While current metrics are particular to an individual patient’s experiences, underlying health conditions influence opinions of these episodes of care. Specifically, patients with depression and anxiety are, in general, less satisfied with the care they receive.11,12 Similarly, patients with chronic diseases on multiple medications and those with more severe symptoms are commonly less satisfied with their care than are patients with acute issues2 and with milder symptoms.3 As gastroenterologists, seeing sicker patients with chronic conditions is not uncommon, and this could serve as a disadvantage when compared with peers in other specialties because scores are not typically adjusted.
Since patient-centered metrics are likely to remain relevant in the future, and with the unique challenges this can present to practicing gastroenterologists, achieving higher degrees of patient satisfaction remains both aspirational and difficult. We will be asked to reconcile and manage not only clinical conundrums but also seemingly conflicting realities of patient preferences. For example, it has been shown that, among patients with irritable bowel syndrome (IBS), more testing led to higher satisfaction only until that testing was performed within the context of a gastroenterologist’s care.13 In contrast, within the endoscopy setting, a preprocedure diagnosis of IBS did not increase the risk for procedure-related dissatisfaction, provided patients were not prescribed chronic psychotropic medication, nervous prior to the procedure, distressed or in pain during the procedure, or had unmet physical or emotional needs during the procedure.14 Furthermore, there is poor correlation between endoscopic quality measures with strong evidence – such as adenoma detection rate, withdrawal time, and cecal intubation rate – and patient satisfaction.15
So, when considering these conflicting findings and evidence that patients’ global rating of their health care is not reliably associated with the quality of the care they receive,16 should we emphasize experience over outcome? As clinicians practicing in an increasingly transparent and value-based health care environment, we are subject to many priorities contending for our attention. We strive to provide care that is at once patient centric, evidence based, and low cost; however, achieving these goals often requires different strategies. At the end of the day, our primary aim is to provide consistently excellent patient care. We believe that quality and experience are not competing principles. Patient satisfaction is relevant and important, but it should not preclude adherence to our primary responsibility of providing high-quality care.
When trying to make clinical decisions that may compromise one of these goals for another, it can be helpful to recall the “me and my family” rule: What kind of care would I want for myself or my loved ones in this situation?
Acknowledgement
We thank Dr. Ziad Gellad (Duke University, Durham, N.C.) for his assistance in reviewing and providing feedback on this manuscript.
1. Proc Natl Acad Sci U S A. 2015;112(47):14473-8. 2. Am J Manag Care. 1997;3(4):579-94.
3. Gut. 2004;53(SUPPL. 4):40-4.
4. Virtual Mentor. 2013;15(11):982-7.
5. J Hosp Med. 2013;8(5):271-7.
6. Int J Health Care Qual Assur. 2011;24(4):266-73.
7. J Cutan Aesthet Surg. 2010;3(3):151-5.
8. Am J Med. 2005;118(10):1126-33.
9. JAMA. 2002;287(22):2951-7. 10. JAMA. 1994;272(20):1583-7.
11. J Diabetes Metab. 2012;3(7):1000210.
12. Am Heart J. 2000;140(1):105-10.
13. J Clin Gastroenterol. 2018;52(7):614-21.
14. Dig Dis Sci. 2005;50(10):1860-71.15. Am J Gastroenterol. 2014;109(7):1089-91.
16. Ann Intern Med. 2006;144(9):665-72.
Dr. Finn is a gastroenterologist with the Palo Alto Medical Foundation, Mountain View, Calif.; Dr. Leiman is assistant professor of medicine, director of esophageal research and quality in the division of gastroenterology, Duke University, Duke Clinical Research Institute, and chair-elect of the AGA Quality Committee.
Although largely untouched by the first and second industrial revolutions in the 18th and 20th centuries, the practice of medicine in the 21st century is increasingly susceptible to the vast transformative power of the third – and rapidly approaching fourth – industrial revolutions. New technological advances and their associated distribution of knowledge and connectedness have allowed patients unprecedented access to health care information. The salutary effects of this change is manifest in a diversity of areas, including registries that facilitate participation in state of the art research such as ClinicalTrials.gov and the ability to track nascent trends in infectious diseases with Google searches.1
Although the stakes may seem lower when patients go online to choose a practitioner, the reality demonstrates just how important those search results can be. With parallels of similar trends in other sectors, there is an increasing emphasis on ranking health care facilities, practitioners, and medical experiences. This phenomenon extends beyond private Internet sites into government scorecards, which has significant implications. But even with widespread access to information, there is frequently a lack of context for interpreting these data. Consequently, it is worth exploring why measuring satisfaction can be important, how patients can rate practitioners, and what to do with the available information to improve care delivery.
The idea to measure patient satisfaction of delivered health care began in earnest during the 1980s with Irwin Press and Rodney Ganey collaborating to create formal processes for collecting data on the “salient aspects of ... health care experience, [involving] the interaction of expectations, preferences, and satisfaction with medical care.”2,3 The enthusiasm for collecting these data has grown greatly since that time. More recently, the federal government began obtaining data in 2002 when the Centers for Medicaid & Medicare Services and the Agency for Healthcare Research and Quality (AHRQ) collaborated to develop a standardized questionnaire for hospitalized patients known as the Hospital Consumer Assessment of Healthcare Providers and Systems, or HCAHPS.4 Subsequently, standardized survey instruments have been developed for nearly every phase of care, including outpatient care (CG-CAHPS), emergency care (ED-CAHPS), and ambulatory surgery care (OAS-CAHPS). These instruments are particularly relevant to gastroenterologists, with questions querying patients about preprocedure instructions, surgery center check-in processes, comfort of procedure and waiting rooms, friendliness of providers, and quality of postprocedure information.
The focus on rating satisfaction intensified in 2010 after the passage of the Affordable Care Act (ACA). Around this time, patient satisfaction and health outcomes became more deeply integrated concepts in health care quality. As part of a broader emphasis in this area, CMS initiated the hospital value-based purchasing (VBP) program, which tied incentive payments for Medicare beneficiaries to hospital-based health care quality and patient satisfaction. Within this schema, 25% of performance, and its associated economic stakes, is measured by HCAHPS scores.5 Other value programs such as the Merit-Based Incentive Payment Program (MIPS) include CAHPS instruments as optional assessments of quality.
Given the financial risks linked to satisfaction rankings and their online visibility, many argue that patient satisfaction is prioritized in organizations above more clinically meaningful metrics. Studies have shown, however, that high levels of patient satisfaction can lead to increased patient loyalty, treatment adherence, patient retention, staff morale, and personal and professional satisfaction.6,7 In fact, not surprisingly, there is an inverse correlation between patient satisfaction and the rates of malpractice lawsuits.7-10
Despite the growing relevance of patient perceptions to clinical practice, measuring satisfaction remains a challenge. While current metrics are particular to an individual patient’s experiences, underlying health conditions influence opinions of these episodes of care. Specifically, patients with depression and anxiety are, in general, less satisfied with the care they receive.11,12 Similarly, patients with chronic diseases on multiple medications and those with more severe symptoms are commonly less satisfied with their care than are patients with acute issues2 and with milder symptoms.3 As gastroenterologists, seeing sicker patients with chronic conditions is not uncommon, and this could serve as a disadvantage when compared with peers in other specialties because scores are not typically adjusted.
Since patient-centered metrics are likely to remain relevant in the future, and with the unique challenges this can present to practicing gastroenterologists, achieving higher degrees of patient satisfaction remains both aspirational and difficult. We will be asked to reconcile and manage not only clinical conundrums but also seemingly conflicting realities of patient preferences. For example, it has been shown that, among patients with irritable bowel syndrome (IBS), more testing led to higher satisfaction only until that testing was performed within the context of a gastroenterologist’s care.13 In contrast, within the endoscopy setting, a preprocedure diagnosis of IBS did not increase the risk for procedure-related dissatisfaction, provided patients were not prescribed chronic psychotropic medication, nervous prior to the procedure, distressed or in pain during the procedure, or had unmet physical or emotional needs during the procedure.14 Furthermore, there is poor correlation between endoscopic quality measures with strong evidence – such as adenoma detection rate, withdrawal time, and cecal intubation rate – and patient satisfaction.15
So, when considering these conflicting findings and evidence that patients’ global rating of their health care is not reliably associated with the quality of the care they receive,16 should we emphasize experience over outcome? As clinicians practicing in an increasingly transparent and value-based health care environment, we are subject to many priorities contending for our attention. We strive to provide care that is at once patient centric, evidence based, and low cost; however, achieving these goals often requires different strategies. At the end of the day, our primary aim is to provide consistently excellent patient care. We believe that quality and experience are not competing principles. Patient satisfaction is relevant and important, but it should not preclude adherence to our primary responsibility of providing high-quality care.
When trying to make clinical decisions that may compromise one of these goals for another, it can be helpful to recall the “me and my family” rule: What kind of care would I want for myself or my loved ones in this situation?
Acknowledgement
We thank Dr. Ziad Gellad (Duke University, Durham, N.C.) for his assistance in reviewing and providing feedback on this manuscript.
1. Proc Natl Acad Sci U S A. 2015;112(47):14473-8. 2. Am J Manag Care. 1997;3(4):579-94.
3. Gut. 2004;53(SUPPL. 4):40-4.
4. Virtual Mentor. 2013;15(11):982-7.
5. J Hosp Med. 2013;8(5):271-7.
6. Int J Health Care Qual Assur. 2011;24(4):266-73.
7. J Cutan Aesthet Surg. 2010;3(3):151-5.
8. Am J Med. 2005;118(10):1126-33.
9. JAMA. 2002;287(22):2951-7. 10. JAMA. 1994;272(20):1583-7.
11. J Diabetes Metab. 2012;3(7):1000210.
12. Am Heart J. 2000;140(1):105-10.
13. J Clin Gastroenterol. 2018;52(7):614-21.
14. Dig Dis Sci. 2005;50(10):1860-71.15. Am J Gastroenterol. 2014;109(7):1089-91.
16. Ann Intern Med. 2006;144(9):665-72.
Dr. Finn is a gastroenterologist with the Palo Alto Medical Foundation, Mountain View, Calif.; Dr. Leiman is assistant professor of medicine, director of esophageal research and quality in the division of gastroenterology, Duke University, Duke Clinical Research Institute, and chair-elect of the AGA Quality Committee.
Although largely untouched by the first and second industrial revolutions in the 18th and 20th centuries, the practice of medicine in the 21st century is increasingly susceptible to the vast transformative power of the third – and rapidly approaching fourth – industrial revolutions. New technological advances and their associated distribution of knowledge and connectedness have allowed patients unprecedented access to health care information. The salutary effects of this change is manifest in a diversity of areas, including registries that facilitate participation in state of the art research such as ClinicalTrials.gov and the ability to track nascent trends in infectious diseases with Google searches.1
Although the stakes may seem lower when patients go online to choose a practitioner, the reality demonstrates just how important those search results can be. With parallels of similar trends in other sectors, there is an increasing emphasis on ranking health care facilities, practitioners, and medical experiences. This phenomenon extends beyond private Internet sites into government scorecards, which has significant implications. But even with widespread access to information, there is frequently a lack of context for interpreting these data. Consequently, it is worth exploring why measuring satisfaction can be important, how patients can rate practitioners, and what to do with the available information to improve care delivery.
The idea to measure patient satisfaction of delivered health care began in earnest during the 1980s with Irwin Press and Rodney Ganey collaborating to create formal processes for collecting data on the “salient aspects of ... health care experience, [involving] the interaction of expectations, preferences, and satisfaction with medical care.”2,3 The enthusiasm for collecting these data has grown greatly since that time. More recently, the federal government began obtaining data in 2002 when the Centers for Medicaid & Medicare Services and the Agency for Healthcare Research and Quality (AHRQ) collaborated to develop a standardized questionnaire for hospitalized patients known as the Hospital Consumer Assessment of Healthcare Providers and Systems, or HCAHPS.4 Subsequently, standardized survey instruments have been developed for nearly every phase of care, including outpatient care (CG-CAHPS), emergency care (ED-CAHPS), and ambulatory surgery care (OAS-CAHPS). These instruments are particularly relevant to gastroenterologists, with questions querying patients about preprocedure instructions, surgery center check-in processes, comfort of procedure and waiting rooms, friendliness of providers, and quality of postprocedure information.
The focus on rating satisfaction intensified in 2010 after the passage of the Affordable Care Act (ACA). Around this time, patient satisfaction and health outcomes became more deeply integrated concepts in health care quality. As part of a broader emphasis in this area, CMS initiated the hospital value-based purchasing (VBP) program, which tied incentive payments for Medicare beneficiaries to hospital-based health care quality and patient satisfaction. Within this schema, 25% of performance, and its associated economic stakes, is measured by HCAHPS scores.5 Other value programs such as the Merit-Based Incentive Payment Program (MIPS) include CAHPS instruments as optional assessments of quality.
Given the financial risks linked to satisfaction rankings and their online visibility, many argue that patient satisfaction is prioritized in organizations above more clinically meaningful metrics. Studies have shown, however, that high levels of patient satisfaction can lead to increased patient loyalty, treatment adherence, patient retention, staff morale, and personal and professional satisfaction.6,7 In fact, not surprisingly, there is an inverse correlation between patient satisfaction and the rates of malpractice lawsuits.7-10
Despite the growing relevance of patient perceptions to clinical practice, measuring satisfaction remains a challenge. While current metrics are particular to an individual patient’s experiences, underlying health conditions influence opinions of these episodes of care. Specifically, patients with depression and anxiety are, in general, less satisfied with the care they receive.11,12 Similarly, patients with chronic diseases on multiple medications and those with more severe symptoms are commonly less satisfied with their care than are patients with acute issues2 and with milder symptoms.3 As gastroenterologists, seeing sicker patients with chronic conditions is not uncommon, and this could serve as a disadvantage when compared with peers in other specialties because scores are not typically adjusted.
Since patient-centered metrics are likely to remain relevant in the future, and with the unique challenges this can present to practicing gastroenterologists, achieving higher degrees of patient satisfaction remains both aspirational and difficult. We will be asked to reconcile and manage not only clinical conundrums but also seemingly conflicting realities of patient preferences. For example, it has been shown that, among patients with irritable bowel syndrome (IBS), more testing led to higher satisfaction only until that testing was performed within the context of a gastroenterologist’s care.13 In contrast, within the endoscopy setting, a preprocedure diagnosis of IBS did not increase the risk for procedure-related dissatisfaction, provided patients were not prescribed chronic psychotropic medication, nervous prior to the procedure, distressed or in pain during the procedure, or had unmet physical or emotional needs during the procedure.14 Furthermore, there is poor correlation between endoscopic quality measures with strong evidence – such as adenoma detection rate, withdrawal time, and cecal intubation rate – and patient satisfaction.15
So, when considering these conflicting findings and evidence that patients’ global rating of their health care is not reliably associated with the quality of the care they receive,16 should we emphasize experience over outcome? As clinicians practicing in an increasingly transparent and value-based health care environment, we are subject to many priorities contending for our attention. We strive to provide care that is at once patient centric, evidence based, and low cost; however, achieving these goals often requires different strategies. At the end of the day, our primary aim is to provide consistently excellent patient care. We believe that quality and experience are not competing principles. Patient satisfaction is relevant and important, but it should not preclude adherence to our primary responsibility of providing high-quality care.
When trying to make clinical decisions that may compromise one of these goals for another, it can be helpful to recall the “me and my family” rule: What kind of care would I want for myself or my loved ones in this situation?
Acknowledgement
We thank Dr. Ziad Gellad (Duke University, Durham, N.C.) for his assistance in reviewing and providing feedback on this manuscript.
1. Proc Natl Acad Sci U S A. 2015;112(47):14473-8. 2. Am J Manag Care. 1997;3(4):579-94.
3. Gut. 2004;53(SUPPL. 4):40-4.
4. Virtual Mentor. 2013;15(11):982-7.
5. J Hosp Med. 2013;8(5):271-7.
6. Int J Health Care Qual Assur. 2011;24(4):266-73.
7. J Cutan Aesthet Surg. 2010;3(3):151-5.
8. Am J Med. 2005;118(10):1126-33.
9. JAMA. 2002;287(22):2951-7. 10. JAMA. 1994;272(20):1583-7.
11. J Diabetes Metab. 2012;3(7):1000210.
12. Am Heart J. 2000;140(1):105-10.
13. J Clin Gastroenterol. 2018;52(7):614-21.
14. Dig Dis Sci. 2005;50(10):1860-71.15. Am J Gastroenterol. 2014;109(7):1089-91.
16. Ann Intern Med. 2006;144(9):665-72.
Dr. Finn is a gastroenterologist with the Palo Alto Medical Foundation, Mountain View, Calif.; Dr. Leiman is assistant professor of medicine, director of esophageal research and quality in the division of gastroenterology, Duke University, Duke Clinical Research Institute, and chair-elect of the AGA Quality Committee.
Mentoring during fellowship to improve career fit, decrease burnout, and optimize career satisfaction among young gastroenterologists
Introduction
Burnout in physicians has received significant attention within the past several years, particularly among trainees and early-career physicians. The subspecialties of gastroenterology and hepatology are not immune to burnout, with multiple studies indicating that early career gastroenterologists may be disproportionately affected, compared with their more-established counterparts.1-4 Although the drivers of depersonalization, emotional exhaustion, and a reduced sense of personal accomplishment among trainees and early-career gastroenterologists are not fully understood, maximizing career fit during the transition from fellowship into the first posttraining position has been promoted as a potential method to decrease burnout in this population.4,5
While most trainees enter gastroenterology fellowships with a set of predefined career goals, mentorship during fellowship can provide critical guidance along with exposure to new areas and career tracks that were not previously considered. In a survey of gastroenterology and transplant hepatology fellows, 94% of participants with a mentor reported that the mentor significantly influenced their career decision.6 Effective mentoring also has been identified as one possible method to decrease burnout among trainees.7,8
Formal mentoring in gastroenterology fellowship programs might decrease burnout through effectively identifying risk factors such as work hour violations or a lack of social support. Additionally, when fellows are being prepared for transition to their first positions as attending gastroenterologists, there is a critical opportunity to improve career fit and decrease burnout rates among early-career gastroenterologists. Making the correct choice of subsequent career path after fellowship might be a source of stress, but this should allow early-career gastroenterologists to maximize the time spent doing those activities they feel are the most rewarding. A formal mentoring system and an accessible career mentor can be invaluable in allowing the mentee to identify and select that position.
Career fit
The concept of career fit has been described as the ability of individuals to focus their effort on the aspect or aspects of their work that they find most meaningful.5 Multiple specialties have recognized the importance of career fit and the need to choose appropriately when selecting a position and career path upon completing fellowship. In one evaluation of faculty members from the department of medicine at a large academic medical center, those individuals who spent less than 20% of their time working on the activity that they found most meaningful were significantly more likely to demonstrate burnout.5
In a relatively short time period, gastroenterology fellows are required to gather multiple new skill sets, including functioning as a consultant, performing endoscopic procedures, and potentially gaining formal training in clinical, basic, or translational research methods. During this same period, an intense phase of self-assessment should begin, with one critical aim of training being to identify those factors most likely to lead to a long, satisfying career. The growth that occurs during fellowship may allow for the identification of a career track that is likely to be the most rewarding, such as a career as a clinical investigator, clinician educator, or in clinical practice. Importantly, the trainee must decide which career track will most likely lead to self-fulfillment, even if the chosen path does not align with a mentor or advisor. Additionally, self-assessment also may aid in the identification of a niche that an individual finds most intellectually stimulating, which may lead to an area of research or clinical expertise.
While the demonstrated relationship between career fit and burnout is only an association without demonstrated causation, this does merit further consideration. For the first time in most trainees’ careers, the position after fellowship represents an opportunity to choose a job as opposed to going through a “match” process. Therefore, the trainee must strongly consider the factors that will ultimately lead to career satisfaction. If a large disconnect is present between self-identified career goals and the actual tasks required within daily workflow, this may lead to burnout relatively early in a career. Perhaps more importantly, if an individual did not perform adequate self-reflection when choosing a career path or did not receive effective guidance from career mentors, this also might lead to decreased career satisfaction, poor career fit, and an increased risk for burnout as an early-career gastroenterologist.
The mentor’s role
Although a structured career mentoring program is in place within many gastroenterology training programs, other fellowships encourage the mentee to select from a pool of potential mentors. In many cases, trainees and early career gastroenterologists will benefit from building a mentorship team, including career mentor or mentors, research mentors, and other advisors.9
While the mentor-mentee relationship can be an extremely rewarding experience for both parties, the effective mentor must meet a high standard. Several qualities have been identified that will maximize the benefit of the mentor-mentee relationship for the trainee, including the mentor taking a selfless approach to the relationship, working to assist the mentee in choosing a career path that will be the most rewarding, and then aiding the mentee in making helpful connections to promote growth along that chosen path.9 A good mentors should inspire a mentees, but also should be willing to provide honest and at times critical feedback to ensure that mentees maximizes their potential and ultimately assume the appropriate career trajectory. Unbiased mentorship, as well as continued reevaluations of strengths, weaknesses, and career goals by the mentor and mentee, will ultimately offer an opportunity to ensure the best combination of career fit,5 work-life balance,10 and satisfaction with career choice.11
The mentor-mentee relationship after training is complete
Once a trainee has completed gastroenterology fellowship, another stressful transition to the role of an attending physician commences. It is critical that early-career gastroenterologists not only have confidence in the guidance that their mentor has provided to ensure appropriate career fit in their new role but also maintain these critical mentor-mentee relationships during this transition. A good mentor does not disappear because one phase of training is complete. The need for effective mentoring at the junior faculty level also is well recognized,12 and early-career gastroenterologists should continue to rely on established mentoring relationships when new decision points are encountered.
Depending on the career track of an early-career gastroenterologist, formal mentoring also may be offered in the new role as a junior faculty member.12 Additionally, external mentoring can exist within foundations or other subspecialty groups. One example of extramural mentoring is the Career Connection Program offered through the Crohn’s & Colitis Foundation’s Rising Educators Academics and Clinicians Helping IBD (REACH-IBD) platform. In this program, early-career gastroenterologists are selected and paired with national opinion leaders for one-on-one mentoring relationships. Such a program offers further opportunities for career growth, establishing connections within a smaller subspecialty of gastroenterology, and maximizing career fit.
Conclusion
In an era where the toll of burnout and other influences on early-career gastroenterologists are increasingly being recognized, the importance of career fit during the transition into the role of an attending should not be underestimated. In conjunction with appropriate self-reflection, unbiased and critical mentorship during fellowship can promote significant growth among trainees and allow for the ultimate selection of a career track or career path that will promote happiness, work-life balance, and long-term success as defined by the mentee.
Edward L. Barnes, MD, MPH, is with the Multidisciplinary Center for Inflammatory Bowel Diseases and the Center for Gastrointestinal Biology and Disease in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. Dr. Barnes reports no relevant disclosures.
References
1. Keswani RN et al. Am J Gastroenterol. 2011;106(10):1734-40.
2. Burke C et al. Am J Gastroenterol. 2017;112:S593-4.
3. DeCross AJ. AGA Perspectives. 2017.
4. Barnes EL et al. Dig Dis Sci. 2019;64(2):302-6.
5. Shanafelt TD et al. Arch Intern Med. 2009;169(10):990-5.
6. Ordway SM et al. Hepatol Commun. 2017;1(4):347-53.
7. Janko MR, Smeds MR. J Vasc Surg. 2019;69(4):1233-42.
8. Eckleberry-Hunt J et al. Acad Med. 2009;84(2):269-77.
9. Lieberman D. Gastroenterology. 2016;151(1):17-9.
10. Shanafelt TD et al. Mayo Clin Proc. 2015;90(12):1600-13.
11. Shanafelt TD et al. Ann Surg. 2009;250(3):463-71.
12. Shaheen NJ, Sandler RS. Gastroenterology. 2018;155(5):1293-7.
Introduction
Burnout in physicians has received significant attention within the past several years, particularly among trainees and early-career physicians. The subspecialties of gastroenterology and hepatology are not immune to burnout, with multiple studies indicating that early career gastroenterologists may be disproportionately affected, compared with their more-established counterparts.1-4 Although the drivers of depersonalization, emotional exhaustion, and a reduced sense of personal accomplishment among trainees and early-career gastroenterologists are not fully understood, maximizing career fit during the transition from fellowship into the first posttraining position has been promoted as a potential method to decrease burnout in this population.4,5
While most trainees enter gastroenterology fellowships with a set of predefined career goals, mentorship during fellowship can provide critical guidance along with exposure to new areas and career tracks that were not previously considered. In a survey of gastroenterology and transplant hepatology fellows, 94% of participants with a mentor reported that the mentor significantly influenced their career decision.6 Effective mentoring also has been identified as one possible method to decrease burnout among trainees.7,8
Formal mentoring in gastroenterology fellowship programs might decrease burnout through effectively identifying risk factors such as work hour violations or a lack of social support. Additionally, when fellows are being prepared for transition to their first positions as attending gastroenterologists, there is a critical opportunity to improve career fit and decrease burnout rates among early-career gastroenterologists. Making the correct choice of subsequent career path after fellowship might be a source of stress, but this should allow early-career gastroenterologists to maximize the time spent doing those activities they feel are the most rewarding. A formal mentoring system and an accessible career mentor can be invaluable in allowing the mentee to identify and select that position.
Career fit
The concept of career fit has been described as the ability of individuals to focus their effort on the aspect or aspects of their work that they find most meaningful.5 Multiple specialties have recognized the importance of career fit and the need to choose appropriately when selecting a position and career path upon completing fellowship. In one evaluation of faculty members from the department of medicine at a large academic medical center, those individuals who spent less than 20% of their time working on the activity that they found most meaningful were significantly more likely to demonstrate burnout.5
In a relatively short time period, gastroenterology fellows are required to gather multiple new skill sets, including functioning as a consultant, performing endoscopic procedures, and potentially gaining formal training in clinical, basic, or translational research methods. During this same period, an intense phase of self-assessment should begin, with one critical aim of training being to identify those factors most likely to lead to a long, satisfying career. The growth that occurs during fellowship may allow for the identification of a career track that is likely to be the most rewarding, such as a career as a clinical investigator, clinician educator, or in clinical practice. Importantly, the trainee must decide which career track will most likely lead to self-fulfillment, even if the chosen path does not align with a mentor or advisor. Additionally, self-assessment also may aid in the identification of a niche that an individual finds most intellectually stimulating, which may lead to an area of research or clinical expertise.
While the demonstrated relationship between career fit and burnout is only an association without demonstrated causation, this does merit further consideration. For the first time in most trainees’ careers, the position after fellowship represents an opportunity to choose a job as opposed to going through a “match” process. Therefore, the trainee must strongly consider the factors that will ultimately lead to career satisfaction. If a large disconnect is present between self-identified career goals and the actual tasks required within daily workflow, this may lead to burnout relatively early in a career. Perhaps more importantly, if an individual did not perform adequate self-reflection when choosing a career path or did not receive effective guidance from career mentors, this also might lead to decreased career satisfaction, poor career fit, and an increased risk for burnout as an early-career gastroenterologist.
The mentor’s role
Although a structured career mentoring program is in place within many gastroenterology training programs, other fellowships encourage the mentee to select from a pool of potential mentors. In many cases, trainees and early career gastroenterologists will benefit from building a mentorship team, including career mentor or mentors, research mentors, and other advisors.9
While the mentor-mentee relationship can be an extremely rewarding experience for both parties, the effective mentor must meet a high standard. Several qualities have been identified that will maximize the benefit of the mentor-mentee relationship for the trainee, including the mentor taking a selfless approach to the relationship, working to assist the mentee in choosing a career path that will be the most rewarding, and then aiding the mentee in making helpful connections to promote growth along that chosen path.9 A good mentors should inspire a mentees, but also should be willing to provide honest and at times critical feedback to ensure that mentees maximizes their potential and ultimately assume the appropriate career trajectory. Unbiased mentorship, as well as continued reevaluations of strengths, weaknesses, and career goals by the mentor and mentee, will ultimately offer an opportunity to ensure the best combination of career fit,5 work-life balance,10 and satisfaction with career choice.11
The mentor-mentee relationship after training is complete
Once a trainee has completed gastroenterology fellowship, another stressful transition to the role of an attending physician commences. It is critical that early-career gastroenterologists not only have confidence in the guidance that their mentor has provided to ensure appropriate career fit in their new role but also maintain these critical mentor-mentee relationships during this transition. A good mentor does not disappear because one phase of training is complete. The need for effective mentoring at the junior faculty level also is well recognized,12 and early-career gastroenterologists should continue to rely on established mentoring relationships when new decision points are encountered.
Depending on the career track of an early-career gastroenterologist, formal mentoring also may be offered in the new role as a junior faculty member.12 Additionally, external mentoring can exist within foundations or other subspecialty groups. One example of extramural mentoring is the Career Connection Program offered through the Crohn’s & Colitis Foundation’s Rising Educators Academics and Clinicians Helping IBD (REACH-IBD) platform. In this program, early-career gastroenterologists are selected and paired with national opinion leaders for one-on-one mentoring relationships. Such a program offers further opportunities for career growth, establishing connections within a smaller subspecialty of gastroenterology, and maximizing career fit.
Conclusion
In an era where the toll of burnout and other influences on early-career gastroenterologists are increasingly being recognized, the importance of career fit during the transition into the role of an attending should not be underestimated. In conjunction with appropriate self-reflection, unbiased and critical mentorship during fellowship can promote significant growth among trainees and allow for the ultimate selection of a career track or career path that will promote happiness, work-life balance, and long-term success as defined by the mentee.
Edward L. Barnes, MD, MPH, is with the Multidisciplinary Center for Inflammatory Bowel Diseases and the Center for Gastrointestinal Biology and Disease in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. Dr. Barnes reports no relevant disclosures.
References
1. Keswani RN et al. Am J Gastroenterol. 2011;106(10):1734-40.
2. Burke C et al. Am J Gastroenterol. 2017;112:S593-4.
3. DeCross AJ. AGA Perspectives. 2017.
4. Barnes EL et al. Dig Dis Sci. 2019;64(2):302-6.
5. Shanafelt TD et al. Arch Intern Med. 2009;169(10):990-5.
6. Ordway SM et al. Hepatol Commun. 2017;1(4):347-53.
7. Janko MR, Smeds MR. J Vasc Surg. 2019;69(4):1233-42.
8. Eckleberry-Hunt J et al. Acad Med. 2009;84(2):269-77.
9. Lieberman D. Gastroenterology. 2016;151(1):17-9.
10. Shanafelt TD et al. Mayo Clin Proc. 2015;90(12):1600-13.
11. Shanafelt TD et al. Ann Surg. 2009;250(3):463-71.
12. Shaheen NJ, Sandler RS. Gastroenterology. 2018;155(5):1293-7.
Introduction
Burnout in physicians has received significant attention within the past several years, particularly among trainees and early-career physicians. The subspecialties of gastroenterology and hepatology are not immune to burnout, with multiple studies indicating that early career gastroenterologists may be disproportionately affected, compared with their more-established counterparts.1-4 Although the drivers of depersonalization, emotional exhaustion, and a reduced sense of personal accomplishment among trainees and early-career gastroenterologists are not fully understood, maximizing career fit during the transition from fellowship into the first posttraining position has been promoted as a potential method to decrease burnout in this population.4,5
While most trainees enter gastroenterology fellowships with a set of predefined career goals, mentorship during fellowship can provide critical guidance along with exposure to new areas and career tracks that were not previously considered. In a survey of gastroenterology and transplant hepatology fellows, 94% of participants with a mentor reported that the mentor significantly influenced their career decision.6 Effective mentoring also has been identified as one possible method to decrease burnout among trainees.7,8
Formal mentoring in gastroenterology fellowship programs might decrease burnout through effectively identifying risk factors such as work hour violations or a lack of social support. Additionally, when fellows are being prepared for transition to their first positions as attending gastroenterologists, there is a critical opportunity to improve career fit and decrease burnout rates among early-career gastroenterologists. Making the correct choice of subsequent career path after fellowship might be a source of stress, but this should allow early-career gastroenterologists to maximize the time spent doing those activities they feel are the most rewarding. A formal mentoring system and an accessible career mentor can be invaluable in allowing the mentee to identify and select that position.
Career fit
The concept of career fit has been described as the ability of individuals to focus their effort on the aspect or aspects of their work that they find most meaningful.5 Multiple specialties have recognized the importance of career fit and the need to choose appropriately when selecting a position and career path upon completing fellowship. In one evaluation of faculty members from the department of medicine at a large academic medical center, those individuals who spent less than 20% of their time working on the activity that they found most meaningful were significantly more likely to demonstrate burnout.5
In a relatively short time period, gastroenterology fellows are required to gather multiple new skill sets, including functioning as a consultant, performing endoscopic procedures, and potentially gaining formal training in clinical, basic, or translational research methods. During this same period, an intense phase of self-assessment should begin, with one critical aim of training being to identify those factors most likely to lead to a long, satisfying career. The growth that occurs during fellowship may allow for the identification of a career track that is likely to be the most rewarding, such as a career as a clinical investigator, clinician educator, or in clinical practice. Importantly, the trainee must decide which career track will most likely lead to self-fulfillment, even if the chosen path does not align with a mentor or advisor. Additionally, self-assessment also may aid in the identification of a niche that an individual finds most intellectually stimulating, which may lead to an area of research or clinical expertise.
While the demonstrated relationship between career fit and burnout is only an association without demonstrated causation, this does merit further consideration. For the first time in most trainees’ careers, the position after fellowship represents an opportunity to choose a job as opposed to going through a “match” process. Therefore, the trainee must strongly consider the factors that will ultimately lead to career satisfaction. If a large disconnect is present between self-identified career goals and the actual tasks required within daily workflow, this may lead to burnout relatively early in a career. Perhaps more importantly, if an individual did not perform adequate self-reflection when choosing a career path or did not receive effective guidance from career mentors, this also might lead to decreased career satisfaction, poor career fit, and an increased risk for burnout as an early-career gastroenterologist.
The mentor’s role
Although a structured career mentoring program is in place within many gastroenterology training programs, other fellowships encourage the mentee to select from a pool of potential mentors. In many cases, trainees and early career gastroenterologists will benefit from building a mentorship team, including career mentor or mentors, research mentors, and other advisors.9
While the mentor-mentee relationship can be an extremely rewarding experience for both parties, the effective mentor must meet a high standard. Several qualities have been identified that will maximize the benefit of the mentor-mentee relationship for the trainee, including the mentor taking a selfless approach to the relationship, working to assist the mentee in choosing a career path that will be the most rewarding, and then aiding the mentee in making helpful connections to promote growth along that chosen path.9 A good mentors should inspire a mentees, but also should be willing to provide honest and at times critical feedback to ensure that mentees maximizes their potential and ultimately assume the appropriate career trajectory. Unbiased mentorship, as well as continued reevaluations of strengths, weaknesses, and career goals by the mentor and mentee, will ultimately offer an opportunity to ensure the best combination of career fit,5 work-life balance,10 and satisfaction with career choice.11
The mentor-mentee relationship after training is complete
Once a trainee has completed gastroenterology fellowship, another stressful transition to the role of an attending physician commences. It is critical that early-career gastroenterologists not only have confidence in the guidance that their mentor has provided to ensure appropriate career fit in their new role but also maintain these critical mentor-mentee relationships during this transition. A good mentor does not disappear because one phase of training is complete. The need for effective mentoring at the junior faculty level also is well recognized,12 and early-career gastroenterologists should continue to rely on established mentoring relationships when new decision points are encountered.
Depending on the career track of an early-career gastroenterologist, formal mentoring also may be offered in the new role as a junior faculty member.12 Additionally, external mentoring can exist within foundations or other subspecialty groups. One example of extramural mentoring is the Career Connection Program offered through the Crohn’s & Colitis Foundation’s Rising Educators Academics and Clinicians Helping IBD (REACH-IBD) platform. In this program, early-career gastroenterologists are selected and paired with national opinion leaders for one-on-one mentoring relationships. Such a program offers further opportunities for career growth, establishing connections within a smaller subspecialty of gastroenterology, and maximizing career fit.
Conclusion
In an era where the toll of burnout and other influences on early-career gastroenterologists are increasingly being recognized, the importance of career fit during the transition into the role of an attending should not be underestimated. In conjunction with appropriate self-reflection, unbiased and critical mentorship during fellowship can promote significant growth among trainees and allow for the ultimate selection of a career track or career path that will promote happiness, work-life balance, and long-term success as defined by the mentee.
Edward L. Barnes, MD, MPH, is with the Multidisciplinary Center for Inflammatory Bowel Diseases and the Center for Gastrointestinal Biology and Disease in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. Dr. Barnes reports no relevant disclosures.
References
1. Keswani RN et al. Am J Gastroenterol. 2011;106(10):1734-40.
2. Burke C et al. Am J Gastroenterol. 2017;112:S593-4.
3. DeCross AJ. AGA Perspectives. 2017.
4. Barnes EL et al. Dig Dis Sci. 2019;64(2):302-6.
5. Shanafelt TD et al. Arch Intern Med. 2009;169(10):990-5.
6. Ordway SM et al. Hepatol Commun. 2017;1(4):347-53.
7. Janko MR, Smeds MR. J Vasc Surg. 2019;69(4):1233-42.
8. Eckleberry-Hunt J et al. Acad Med. 2009;84(2):269-77.
9. Lieberman D. Gastroenterology. 2016;151(1):17-9.
10. Shanafelt TD et al. Mayo Clin Proc. 2015;90(12):1600-13.
11. Shanafelt TD et al. Ann Surg. 2009;250(3):463-71.
12. Shaheen NJ, Sandler RS. Gastroenterology. 2018;155(5):1293-7.
A career in industry: Is it right for me?
As gastroenterology fellows ponder their futures, one career path is often overlooked. Working in the pharmaceutical or biotechnology industry is a path that is not often at the top of career option lists. It is a rare occurrence for fellows to transition immediately into an industry position as opposed to a clinical or academic post. Initial clinical experience, caring for patients, and gaining experience with health economic challenges in today’s complex environment are considered invaluable assets for job applicants seeking industry positions. A minimum of 3-5 years of real-world clinical care experience will greatly enhance applicants’ marketability as “clinical experts” who can provide meaningful value to industry employers.
What exactly does “industry” mean? Traditionally it includes pharmaceutical and/or biotechnology (discovery, development, manufacture, sales, and marketing of small or large molecules), contract research organizations (CROs), and medical device companies. The variety in terms of size, scope, and reach of these companies is truly staggering and includes: entrepreneurial small startups (fewer than 20 employees, one location), midsize companies (more than 200 employees), and global multinational worldwide behemoths (“big pharma” with more than 50,000 employees and numerous facilities with diverse geographic locations). There are certain geographic regions of the United States where many companies’ headquarters are concentrated. At present (although this certainly can change over time), Cambridge, Mass.; New Jersey; Philadelphia; Raleigh-Durham, N.C.; and the San Francisco Bay Area are “hot areas.”
The breadth of “specialty” areas in industry for experienced clinicians is wide and includes: discovery, translational medicine, early- and late-stage clinical development, medical affairs, patient safety, epidemiology, and commercial development. For those interested in transitioning into industry, it is ideal to have a preferred area in mind so that training and education while in fellowship and clinical practice can be directed to that topic.
Discovery and translational medicine
These areas focus on preclinical development of small and large molecules from first concept until first-in-human studies and filing of an investigational new drug application (IND) with regulatory agencies. Translation of basic science concepts into potentially clinically useful “candidate” molecules requires a strong basic knowledge of science in addition to clinical experience. A passion for bridging novel concepts from “bench” to nonhuman studies is critical for success in this area.
Early-stage clinical development
Early-stage clinical development focuses on progressing discovery candidates to first-in-human studies (phase 1 in healthy volunteers) through phase 2 proof-of-concept studies (PoC). PoC studies typically involve first proof in a clinical trial in the target population that the drug under development may provide clinical benefit. These studies typically include 50-200 subjects with tight inclusion and exclusion controls. Intellectual rigor and scientific curiosity, as well as a passion for protecting patient safety, are essential for success as an early-stage drug developer.
Late-stage clinical development
Late-stage clinical development involves designing, conducting, and executing very large clinical studies (typically with hundreds to thousands of patients) that will provide the necessary rigorous pivotal clinical data supporting new drug marketing applications (NDAs). Relatively few drug candidates successfully make it to this stage of development and these studies are extremely expensive (sometimes hundreds of millions of dollars). This stage of development requires close collaboration with numerous company functions including regulatory, biostatistics, patient safety, clinical pharmacology, clinical operations, and manufacturing, as well as commercial colleagues. In addition to strong clinical expertise, this stage of drug development requires excellent communication, with leadership skills and attention to detail as well. Successfully shepherding a drug candidate through to Food and Drug Administration or other regulatory agency approval is an extremely satisfying experience, which can lead to meaningful differences for patients.
Medical affairs
This is a very important and challenging specialty area that, at its core, demands value demonstration of a medicine and communication to key stakeholders such as patients, physicians, and payers. This objective has become increasingly challenging over the past decade while evolving from a qualitative specialty to a rigorous quantitative one. Scientific and commercial success depends on efficient design, execution, and dissemination of results for real-world evidence and postapproval studies. Ideally, these data will demonstrate the medicine’s benefit-risk profile and how it fits into treatment algorithms. Communication requires leadership of physician and payer advisory boards, as well as publication planning. Close collaboration with marketing teams to advise on ethical and scientifically accurate promotional activities is another key component.
Patient safety
As the name implies, patient safety focuses on evaluating signals both from clinical trials and from literature that can accurately map out risks to patients that can arise from taking these medications. This is a critical function for proper and ethical prescription and use of medicine in today’s society. In addition to signal recognition and consultation with clinical development teams, collaboration with regulatory agencies is an important component.
Epidemiology
Epidemiologists with clinical expertise have become an increasingly important need for pharmaceutical and biotech companies over the past decade – specifically, for the design of real-world studies that demonstrate benefit-risk profiles for medicines in real-world use. These data are in demand for both private and governmental payers, as well as for regulatory agencies who are interested in evolving postapproval safety data. Successful epidemiologists often have acquired MPH degrees and expertise in study design and biostatistics.
Commercial development
Those with more financial or business acumen and clinical experience sometimes staff commercial careers. Typically commercial leads also have an MBA degree and are responsible for assessing commercial markets and forecasting and executing a path to commercial viability. Ultimately this career path can lead to a CEO position.
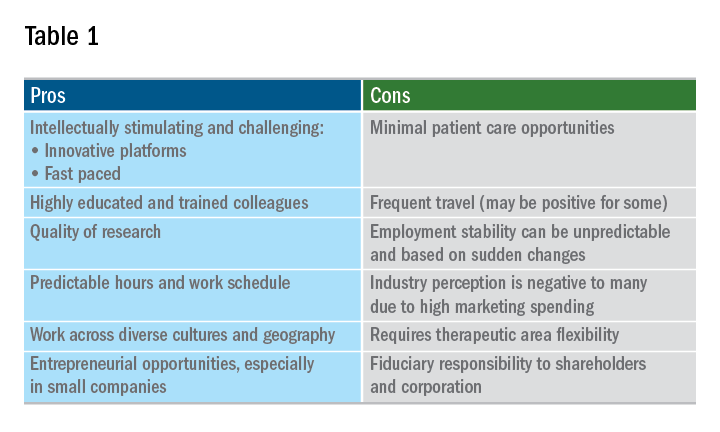
A career in industry is a perfect fit for some, but not so much for others. Table 1 outlines some pros and cons. Commercial factors do come into play with regard to corporate objectives and areas of focus. The top pharmaceutical product therapeutic categories, according to the number of drugs under development in 2017, were cancer, vaccines, diabetes, ophthalmology, gene therapy, anti-inflammatory, and antivirals and immunosuppressants; inflammatory bowel disease was 15th. Therapeutic research and development areas in gastroenterology that are relatively in demand in 2019 include IBD, irritable bowel syndrome, and nonalcoholic steatohepatitis. The high demand areas seem to change with the science and also payers’ willingness to reimburse.
Is industry a good career choice for you? Consider the following factors:
- Travel capabilities.
- Small biotech versus big pharma versus CRO.
- Capability to function in a team environment.
- Communication skills, resilience, self-awareness.
- Therapeutic area and category.
- Early stage versus late stage versus translational versus medical affairs.
- Additional education: MBA, MPH, PhD.
- Geography.
The pharmaceutical industry evolves and undergoes transformation extremely quickly in response to changes in the external environment. If you are considering a current or future career in industry, staying informed about changes in the delivery of health care and health economics is important. There is an ongoing need in industry for trainees and experienced gastroenterologists who can deploy their clinical expertise in development and communication of new medicines and devices that will make a positive difference in patients’ lives.
As gastroenterology fellows ponder their futures, one career path is often overlooked. Working in the pharmaceutical or biotechnology industry is a path that is not often at the top of career option lists. It is a rare occurrence for fellows to transition immediately into an industry position as opposed to a clinical or academic post. Initial clinical experience, caring for patients, and gaining experience with health economic challenges in today’s complex environment are considered invaluable assets for job applicants seeking industry positions. A minimum of 3-5 years of real-world clinical care experience will greatly enhance applicants’ marketability as “clinical experts” who can provide meaningful value to industry employers.
What exactly does “industry” mean? Traditionally it includes pharmaceutical and/or biotechnology (discovery, development, manufacture, sales, and marketing of small or large molecules), contract research organizations (CROs), and medical device companies. The variety in terms of size, scope, and reach of these companies is truly staggering and includes: entrepreneurial small startups (fewer than 20 employees, one location), midsize companies (more than 200 employees), and global multinational worldwide behemoths (“big pharma” with more than 50,000 employees and numerous facilities with diverse geographic locations). There are certain geographic regions of the United States where many companies’ headquarters are concentrated. At present (although this certainly can change over time), Cambridge, Mass.; New Jersey; Philadelphia; Raleigh-Durham, N.C.; and the San Francisco Bay Area are “hot areas.”
The breadth of “specialty” areas in industry for experienced clinicians is wide and includes: discovery, translational medicine, early- and late-stage clinical development, medical affairs, patient safety, epidemiology, and commercial development. For those interested in transitioning into industry, it is ideal to have a preferred area in mind so that training and education while in fellowship and clinical practice can be directed to that topic.
Discovery and translational medicine
These areas focus on preclinical development of small and large molecules from first concept until first-in-human studies and filing of an investigational new drug application (IND) with regulatory agencies. Translation of basic science concepts into potentially clinically useful “candidate” molecules requires a strong basic knowledge of science in addition to clinical experience. A passion for bridging novel concepts from “bench” to nonhuman studies is critical for success in this area.
Early-stage clinical development
Early-stage clinical development focuses on progressing discovery candidates to first-in-human studies (phase 1 in healthy volunteers) through phase 2 proof-of-concept studies (PoC). PoC studies typically involve first proof in a clinical trial in the target population that the drug under development may provide clinical benefit. These studies typically include 50-200 subjects with tight inclusion and exclusion controls. Intellectual rigor and scientific curiosity, as well as a passion for protecting patient safety, are essential for success as an early-stage drug developer.
Late-stage clinical development
Late-stage clinical development involves designing, conducting, and executing very large clinical studies (typically with hundreds to thousands of patients) that will provide the necessary rigorous pivotal clinical data supporting new drug marketing applications (NDAs). Relatively few drug candidates successfully make it to this stage of development and these studies are extremely expensive (sometimes hundreds of millions of dollars). This stage of development requires close collaboration with numerous company functions including regulatory, biostatistics, patient safety, clinical pharmacology, clinical operations, and manufacturing, as well as commercial colleagues. In addition to strong clinical expertise, this stage of drug development requires excellent communication, with leadership skills and attention to detail as well. Successfully shepherding a drug candidate through to Food and Drug Administration or other regulatory agency approval is an extremely satisfying experience, which can lead to meaningful differences for patients.
Medical affairs
This is a very important and challenging specialty area that, at its core, demands value demonstration of a medicine and communication to key stakeholders such as patients, physicians, and payers. This objective has become increasingly challenging over the past decade while evolving from a qualitative specialty to a rigorous quantitative one. Scientific and commercial success depends on efficient design, execution, and dissemination of results for real-world evidence and postapproval studies. Ideally, these data will demonstrate the medicine’s benefit-risk profile and how it fits into treatment algorithms. Communication requires leadership of physician and payer advisory boards, as well as publication planning. Close collaboration with marketing teams to advise on ethical and scientifically accurate promotional activities is another key component.
Patient safety
As the name implies, patient safety focuses on evaluating signals both from clinical trials and from literature that can accurately map out risks to patients that can arise from taking these medications. This is a critical function for proper and ethical prescription and use of medicine in today’s society. In addition to signal recognition and consultation with clinical development teams, collaboration with regulatory agencies is an important component.
Epidemiology
Epidemiologists with clinical expertise have become an increasingly important need for pharmaceutical and biotech companies over the past decade – specifically, for the design of real-world studies that demonstrate benefit-risk profiles for medicines in real-world use. These data are in demand for both private and governmental payers, as well as for regulatory agencies who are interested in evolving postapproval safety data. Successful epidemiologists often have acquired MPH degrees and expertise in study design and biostatistics.
Commercial development
Those with more financial or business acumen and clinical experience sometimes staff commercial careers. Typically commercial leads also have an MBA degree and are responsible for assessing commercial markets and forecasting and executing a path to commercial viability. Ultimately this career path can lead to a CEO position.
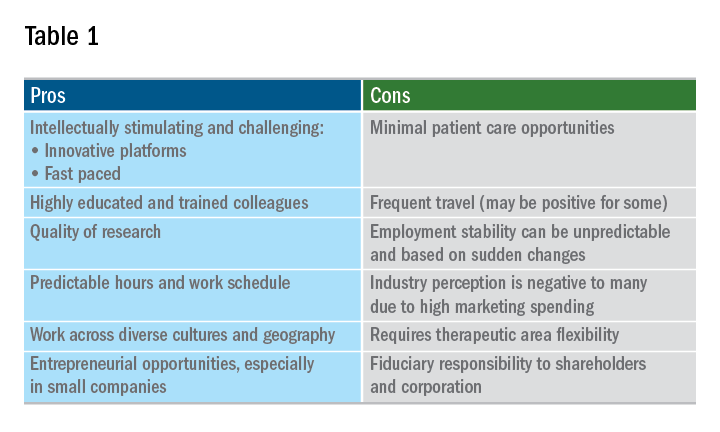
A career in industry is a perfect fit for some, but not so much for others. Table 1 outlines some pros and cons. Commercial factors do come into play with regard to corporate objectives and areas of focus. The top pharmaceutical product therapeutic categories, according to the number of drugs under development in 2017, were cancer, vaccines, diabetes, ophthalmology, gene therapy, anti-inflammatory, and antivirals and immunosuppressants; inflammatory bowel disease was 15th. Therapeutic research and development areas in gastroenterology that are relatively in demand in 2019 include IBD, irritable bowel syndrome, and nonalcoholic steatohepatitis. The high demand areas seem to change with the science and also payers’ willingness to reimburse.
Is industry a good career choice for you? Consider the following factors:
- Travel capabilities.
- Small biotech versus big pharma versus CRO.
- Capability to function in a team environment.
- Communication skills, resilience, self-awareness.
- Therapeutic area and category.
- Early stage versus late stage versus translational versus medical affairs.
- Additional education: MBA, MPH, PhD.
- Geography.
The pharmaceutical industry evolves and undergoes transformation extremely quickly in response to changes in the external environment. If you are considering a current or future career in industry, staying informed about changes in the delivery of health care and health economics is important. There is an ongoing need in industry for trainees and experienced gastroenterologists who can deploy their clinical expertise in development and communication of new medicines and devices that will make a positive difference in patients’ lives.
As gastroenterology fellows ponder their futures, one career path is often overlooked. Working in the pharmaceutical or biotechnology industry is a path that is not often at the top of career option lists. It is a rare occurrence for fellows to transition immediately into an industry position as opposed to a clinical or academic post. Initial clinical experience, caring for patients, and gaining experience with health economic challenges in today’s complex environment are considered invaluable assets for job applicants seeking industry positions. A minimum of 3-5 years of real-world clinical care experience will greatly enhance applicants’ marketability as “clinical experts” who can provide meaningful value to industry employers.
What exactly does “industry” mean? Traditionally it includes pharmaceutical and/or biotechnology (discovery, development, manufacture, sales, and marketing of small or large molecules), contract research organizations (CROs), and medical device companies. The variety in terms of size, scope, and reach of these companies is truly staggering and includes: entrepreneurial small startups (fewer than 20 employees, one location), midsize companies (more than 200 employees), and global multinational worldwide behemoths (“big pharma” with more than 50,000 employees and numerous facilities with diverse geographic locations). There are certain geographic regions of the United States where many companies’ headquarters are concentrated. At present (although this certainly can change over time), Cambridge, Mass.; New Jersey; Philadelphia; Raleigh-Durham, N.C.; and the San Francisco Bay Area are “hot areas.”
The breadth of “specialty” areas in industry for experienced clinicians is wide and includes: discovery, translational medicine, early- and late-stage clinical development, medical affairs, patient safety, epidemiology, and commercial development. For those interested in transitioning into industry, it is ideal to have a preferred area in mind so that training and education while in fellowship and clinical practice can be directed to that topic.
Discovery and translational medicine
These areas focus on preclinical development of small and large molecules from first concept until first-in-human studies and filing of an investigational new drug application (IND) with regulatory agencies. Translation of basic science concepts into potentially clinically useful “candidate” molecules requires a strong basic knowledge of science in addition to clinical experience. A passion for bridging novel concepts from “bench” to nonhuman studies is critical for success in this area.
Early-stage clinical development
Early-stage clinical development focuses on progressing discovery candidates to first-in-human studies (phase 1 in healthy volunteers) through phase 2 proof-of-concept studies (PoC). PoC studies typically involve first proof in a clinical trial in the target population that the drug under development may provide clinical benefit. These studies typically include 50-200 subjects with tight inclusion and exclusion controls. Intellectual rigor and scientific curiosity, as well as a passion for protecting patient safety, are essential for success as an early-stage drug developer.
Late-stage clinical development
Late-stage clinical development involves designing, conducting, and executing very large clinical studies (typically with hundreds to thousands of patients) that will provide the necessary rigorous pivotal clinical data supporting new drug marketing applications (NDAs). Relatively few drug candidates successfully make it to this stage of development and these studies are extremely expensive (sometimes hundreds of millions of dollars). This stage of development requires close collaboration with numerous company functions including regulatory, biostatistics, patient safety, clinical pharmacology, clinical operations, and manufacturing, as well as commercial colleagues. In addition to strong clinical expertise, this stage of drug development requires excellent communication, with leadership skills and attention to detail as well. Successfully shepherding a drug candidate through to Food and Drug Administration or other regulatory agency approval is an extremely satisfying experience, which can lead to meaningful differences for patients.
Medical affairs
This is a very important and challenging specialty area that, at its core, demands value demonstration of a medicine and communication to key stakeholders such as patients, physicians, and payers. This objective has become increasingly challenging over the past decade while evolving from a qualitative specialty to a rigorous quantitative one. Scientific and commercial success depends on efficient design, execution, and dissemination of results for real-world evidence and postapproval studies. Ideally, these data will demonstrate the medicine’s benefit-risk profile and how it fits into treatment algorithms. Communication requires leadership of physician and payer advisory boards, as well as publication planning. Close collaboration with marketing teams to advise on ethical and scientifically accurate promotional activities is another key component.
Patient safety
As the name implies, patient safety focuses on evaluating signals both from clinical trials and from literature that can accurately map out risks to patients that can arise from taking these medications. This is a critical function for proper and ethical prescription and use of medicine in today’s society. In addition to signal recognition and consultation with clinical development teams, collaboration with regulatory agencies is an important component.
Epidemiology
Epidemiologists with clinical expertise have become an increasingly important need for pharmaceutical and biotech companies over the past decade – specifically, for the design of real-world studies that demonstrate benefit-risk profiles for medicines in real-world use. These data are in demand for both private and governmental payers, as well as for regulatory agencies who are interested in evolving postapproval safety data. Successful epidemiologists often have acquired MPH degrees and expertise in study design and biostatistics.
Commercial development
Those with more financial or business acumen and clinical experience sometimes staff commercial careers. Typically commercial leads also have an MBA degree and are responsible for assessing commercial markets and forecasting and executing a path to commercial viability. Ultimately this career path can lead to a CEO position.
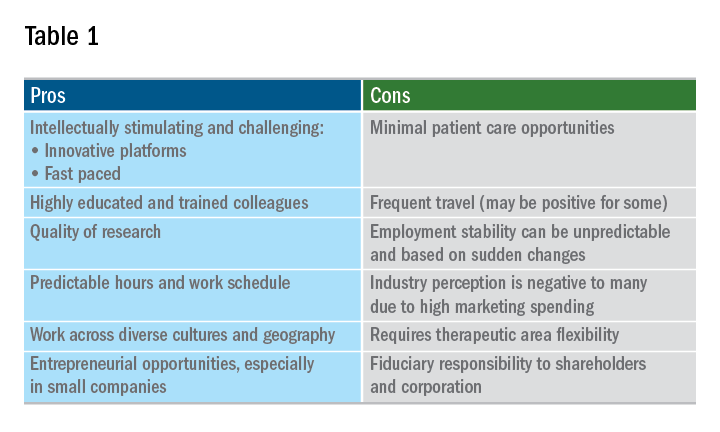
A career in industry is a perfect fit for some, but not so much for others. Table 1 outlines some pros and cons. Commercial factors do come into play with regard to corporate objectives and areas of focus. The top pharmaceutical product therapeutic categories, according to the number of drugs under development in 2017, were cancer, vaccines, diabetes, ophthalmology, gene therapy, anti-inflammatory, and antivirals and immunosuppressants; inflammatory bowel disease was 15th. Therapeutic research and development areas in gastroenterology that are relatively in demand in 2019 include IBD, irritable bowel syndrome, and nonalcoholic steatohepatitis. The high demand areas seem to change with the science and also payers’ willingness to reimburse.
Is industry a good career choice for you? Consider the following factors:
- Travel capabilities.
- Small biotech versus big pharma versus CRO.
- Capability to function in a team environment.
- Communication skills, resilience, self-awareness.
- Therapeutic area and category.
- Early stage versus late stage versus translational versus medical affairs.
- Additional education: MBA, MPH, PhD.
- Geography.
The pharmaceutical industry evolves and undergoes transformation extremely quickly in response to changes in the external environment. If you are considering a current or future career in industry, staying informed about changes in the delivery of health care and health economics is important. There is an ongoing need in industry for trainees and experienced gastroenterologists who can deploy their clinical expertise in development and communication of new medicines and devices that will make a positive difference in patients’ lives.
Dealing with difficult people
Dealing with difficult people is not a new problem. As long as there are at least two people, the potential for conflict will arise. Unfortunately, the workplace or hospital is not immune from tragedies that are born out of poor conflict resolution. Before we go further, please do not ignore the fact that more than 1 million workers are assaulted each year, and more than 60% of Americans are aware of some type of abusive conduct occurring on the job.
Who are those difficult people we may encounter? Anyone and everyone. Difficult people may include our significant others, family members, supervisors, department chairs, colleagues, competitors, trainees, patients and their families, and ancillary personnel. Looking at this list, it is amazing that we aren’t either stymied by never-ending conflict resolution seminars, or rendered completely ineffective in all aspects of life. Daily conflicts can vary in intensity and degree. At one end one can be disgruntled at the person who secured the last doughnut in the break room, and at the other extreme end one is committed to moving forward with a multimillion dollar lawsuit against the company.
Conflicts arise because of a multiplicity of reasons – work style differences, background differences, attitude difference, personality types, and competitive versus cooperative differences. To be effective, each of us must realize that we are more alike than different, and it is our differences that should fuel our passion for providing excellent patient care and customer service.
In particular, be aware of things that can accelerate the potential for conflicts – performance ratings, evaluations, recommendation for promotion, absence of role models or mentors, lack of support amongst colleagues, and failures on the part of leadership to keep promises, appreciate people, maintain personal integrity, or take responsibility for their own errors.
When conflict arises – deal with it! Identify the problem, and if it is legitimate address it as soon as possible. Always remember to document the details in writing; never forget the old adage most of us learned during training: “If it’s not written/documented it wasn’t done or didn’t happen.” More than likely you won’t need to retrieve your written documents concerning a particular conflict, but if the conflict escalates, this type of documentation will prove invaluable.
Communicate with the person or persons with whom you have the conflict – it is essential that you have the “difficult” conversation. This conversation must be done face-to-face and in private. Never communicate by email, social media, or through gossip. Remain calm, professional, and show respect even if the other person does not. At this meeting detail the problem, but also come prepared with suggestions as to how the conflict might be resolved.
Take responsibility – you can’t control situations or people – but you can choose how you will respond to every situation. This is the appropriate time to establish boundaries; avoid any behavior that might be considered bullying or harassment. Redirect negativity that emanates from the person with whom you have the conflict as well as any potentially self-imposed negativity. Make every effort to avoid statements that include “you never” and “you always,” as there are very few absolutes in life. Consider the other person’s perspective as well; try to see it from their point of view because your “personal truth” is not the only “truth.” Our individual personal life experiences form the foundation for much of our opinions and views; therefore, it should be obvious that persons from widely varied backgrounds and cultures will differ in their approaches. If at all possible, give the person another chance; even the most difficult person has good attributes.
Once you have had the “difficult” conversation and there is still no resolution in sight you should take it to management. Everyone has a boss – even the Boss! There is much to gain from involving an impartial party or mediator. This impartial individual is able to understand the viewpoint of all parties involved and frequently that person’s solution may be considered acceptable because it is coming from someone not directly affected by the conflict.
Unresolved conflicts result in many negative effects – interference with one’s career is foremost – and that alone can be a source of undue stress. Other negative effects are the development of a hostile work environment, diminished productivity, low morale, and high employee turnover. Physicians in particular are prone to experiencing an increase in medical errors, litigation claims, and poor patient care when there are unresolved conflicts on the table.
In an ideal world, there are no difficult people; there are either no conflicts or all conflicts are resolved immediately without any lasting deleterious effects. Unfortunately, the world abounds in conflict at varying stages of resolution. As a final bit of advice, in dealing with difficult persons, do not allow conflicts to obscure your goals for successful patient care and/or customer service. Focus on why you decided to join your place of employment and realize that everyone has a role in making the team work! If you are dedicated to addressing conflicts as they arise, and utilizing the strategies outlined, you will often find that foes can truly become friends.
Dr. Cole is associate section chief, gastroenterology, and chief, GI endoscopy, Michael E. DeBakey VA Medical Center; and associate professor, internal medicine, Baylor College of Medicine, Houston.
Dealing with difficult people is not a new problem. As long as there are at least two people, the potential for conflict will arise. Unfortunately, the workplace or hospital is not immune from tragedies that are born out of poor conflict resolution. Before we go further, please do not ignore the fact that more than 1 million workers are assaulted each year, and more than 60% of Americans are aware of some type of abusive conduct occurring on the job.
Who are those difficult people we may encounter? Anyone and everyone. Difficult people may include our significant others, family members, supervisors, department chairs, colleagues, competitors, trainees, patients and their families, and ancillary personnel. Looking at this list, it is amazing that we aren’t either stymied by never-ending conflict resolution seminars, or rendered completely ineffective in all aspects of life. Daily conflicts can vary in intensity and degree. At one end one can be disgruntled at the person who secured the last doughnut in the break room, and at the other extreme end one is committed to moving forward with a multimillion dollar lawsuit against the company.
Conflicts arise because of a multiplicity of reasons – work style differences, background differences, attitude difference, personality types, and competitive versus cooperative differences. To be effective, each of us must realize that we are more alike than different, and it is our differences that should fuel our passion for providing excellent patient care and customer service.
In particular, be aware of things that can accelerate the potential for conflicts – performance ratings, evaluations, recommendation for promotion, absence of role models or mentors, lack of support amongst colleagues, and failures on the part of leadership to keep promises, appreciate people, maintain personal integrity, or take responsibility for their own errors.
When conflict arises – deal with it! Identify the problem, and if it is legitimate address it as soon as possible. Always remember to document the details in writing; never forget the old adage most of us learned during training: “If it’s not written/documented it wasn’t done or didn’t happen.” More than likely you won’t need to retrieve your written documents concerning a particular conflict, but if the conflict escalates, this type of documentation will prove invaluable.
Communicate with the person or persons with whom you have the conflict – it is essential that you have the “difficult” conversation. This conversation must be done face-to-face and in private. Never communicate by email, social media, or through gossip. Remain calm, professional, and show respect even if the other person does not. At this meeting detail the problem, but also come prepared with suggestions as to how the conflict might be resolved.
Take responsibility – you can’t control situations or people – but you can choose how you will respond to every situation. This is the appropriate time to establish boundaries; avoid any behavior that might be considered bullying or harassment. Redirect negativity that emanates from the person with whom you have the conflict as well as any potentially self-imposed negativity. Make every effort to avoid statements that include “you never” and “you always,” as there are very few absolutes in life. Consider the other person’s perspective as well; try to see it from their point of view because your “personal truth” is not the only “truth.” Our individual personal life experiences form the foundation for much of our opinions and views; therefore, it should be obvious that persons from widely varied backgrounds and cultures will differ in their approaches. If at all possible, give the person another chance; even the most difficult person has good attributes.
Once you have had the “difficult” conversation and there is still no resolution in sight you should take it to management. Everyone has a boss – even the Boss! There is much to gain from involving an impartial party or mediator. This impartial individual is able to understand the viewpoint of all parties involved and frequently that person’s solution may be considered acceptable because it is coming from someone not directly affected by the conflict.
Unresolved conflicts result in many negative effects – interference with one’s career is foremost – and that alone can be a source of undue stress. Other negative effects are the development of a hostile work environment, diminished productivity, low morale, and high employee turnover. Physicians in particular are prone to experiencing an increase in medical errors, litigation claims, and poor patient care when there are unresolved conflicts on the table.
In an ideal world, there are no difficult people; there are either no conflicts or all conflicts are resolved immediately without any lasting deleterious effects. Unfortunately, the world abounds in conflict at varying stages of resolution. As a final bit of advice, in dealing with difficult persons, do not allow conflicts to obscure your goals for successful patient care and/or customer service. Focus on why you decided to join your place of employment and realize that everyone has a role in making the team work! If you are dedicated to addressing conflicts as they arise, and utilizing the strategies outlined, you will often find that foes can truly become friends.
Dr. Cole is associate section chief, gastroenterology, and chief, GI endoscopy, Michael E. DeBakey VA Medical Center; and associate professor, internal medicine, Baylor College of Medicine, Houston.
Dealing with difficult people is not a new problem. As long as there are at least two people, the potential for conflict will arise. Unfortunately, the workplace or hospital is not immune from tragedies that are born out of poor conflict resolution. Before we go further, please do not ignore the fact that more than 1 million workers are assaulted each year, and more than 60% of Americans are aware of some type of abusive conduct occurring on the job.
Who are those difficult people we may encounter? Anyone and everyone. Difficult people may include our significant others, family members, supervisors, department chairs, colleagues, competitors, trainees, patients and their families, and ancillary personnel. Looking at this list, it is amazing that we aren’t either stymied by never-ending conflict resolution seminars, or rendered completely ineffective in all aspects of life. Daily conflicts can vary in intensity and degree. At one end one can be disgruntled at the person who secured the last doughnut in the break room, and at the other extreme end one is committed to moving forward with a multimillion dollar lawsuit against the company.
Conflicts arise because of a multiplicity of reasons – work style differences, background differences, attitude difference, personality types, and competitive versus cooperative differences. To be effective, each of us must realize that we are more alike than different, and it is our differences that should fuel our passion for providing excellent patient care and customer service.
In particular, be aware of things that can accelerate the potential for conflicts – performance ratings, evaluations, recommendation for promotion, absence of role models or mentors, lack of support amongst colleagues, and failures on the part of leadership to keep promises, appreciate people, maintain personal integrity, or take responsibility for their own errors.
When conflict arises – deal with it! Identify the problem, and if it is legitimate address it as soon as possible. Always remember to document the details in writing; never forget the old adage most of us learned during training: “If it’s not written/documented it wasn’t done or didn’t happen.” More than likely you won’t need to retrieve your written documents concerning a particular conflict, but if the conflict escalates, this type of documentation will prove invaluable.
Communicate with the person or persons with whom you have the conflict – it is essential that you have the “difficult” conversation. This conversation must be done face-to-face and in private. Never communicate by email, social media, or through gossip. Remain calm, professional, and show respect even if the other person does not. At this meeting detail the problem, but also come prepared with suggestions as to how the conflict might be resolved.
Take responsibility – you can’t control situations or people – but you can choose how you will respond to every situation. This is the appropriate time to establish boundaries; avoid any behavior that might be considered bullying or harassment. Redirect negativity that emanates from the person with whom you have the conflict as well as any potentially self-imposed negativity. Make every effort to avoid statements that include “you never” and “you always,” as there are very few absolutes in life. Consider the other person’s perspective as well; try to see it from their point of view because your “personal truth” is not the only “truth.” Our individual personal life experiences form the foundation for much of our opinions and views; therefore, it should be obvious that persons from widely varied backgrounds and cultures will differ in their approaches. If at all possible, give the person another chance; even the most difficult person has good attributes.
Once you have had the “difficult” conversation and there is still no resolution in sight you should take it to management. Everyone has a boss – even the Boss! There is much to gain from involving an impartial party or mediator. This impartial individual is able to understand the viewpoint of all parties involved and frequently that person’s solution may be considered acceptable because it is coming from someone not directly affected by the conflict.
Unresolved conflicts result in many negative effects – interference with one’s career is foremost – and that alone can be a source of undue stress. Other negative effects are the development of a hostile work environment, diminished productivity, low morale, and high employee turnover. Physicians in particular are prone to experiencing an increase in medical errors, litigation claims, and poor patient care when there are unresolved conflicts on the table.
In an ideal world, there are no difficult people; there are either no conflicts or all conflicts are resolved immediately without any lasting deleterious effects. Unfortunately, the world abounds in conflict at varying stages of resolution. As a final bit of advice, in dealing with difficult persons, do not allow conflicts to obscure your goals for successful patient care and/or customer service. Focus on why you decided to join your place of employment and realize that everyone has a role in making the team work! If you are dedicated to addressing conflicts as they arise, and utilizing the strategies outlined, you will often find that foes can truly become friends.
Dr. Cole is associate section chief, gastroenterology, and chief, GI endoscopy, Michael E. DeBakey VA Medical Center; and associate professor, internal medicine, Baylor College of Medicine, Houston.