User login
Surprisingly more nonsustained VT shown in HCM using extended ECG monitoring
BARCELONA – , suggests a study that questions current risk stratification practices in HCM.
In the registry study, such arrythmias were observed in about six times as many HCM patients during 30 days of ambulatory electrocardiographic monitoring as would have been identified based on the first 24 hours of the monitoring period: 65% vs. 11% of the cohort.
Also, about 62% of the patients showed NSVT at “extended” 30-day monitoring, compared with an 8% prevalence of the arrhythmia based on the more conventional ECG monitoring period of 24 hours.
Nonsustained ventricular tachycardia, an important arrhythmia used every day in clinical practice to make decisions, is “much, much more prevalent than we thought” in patients with HCM, Juan Caro Codón, MD, the study’s principal investigator, said in an interview. “We should invest in further research regarding extended ECG monitoring in these patients.”
Dr. Caro Codón, of La Paz University Hospital, Madrid, presented the findings from the TEMPO-HCM study at the European Heart Rhythm Association 2023 Congress, held in Barcelona and virtually.
Its results, he said, have implications for stratifying HCM patients according to their risk for sudden cardiac death in deciding who should be offered an implantable cardioverter-defibrillator (ICD).
The life-incidence of atrial fibrillation (AF) in patients like those in the current analysis has previously been found to be about 20%, and the life-prevalence of NSVT about 20%-30%, using traditional 24- or 48-hour Holter monitoring, Dr. Caro Codón said.
“These arrhythmias are clinically relevant events because they are linked to very meaningful clinical endpoints,” including stroke and thromboembolism, he said, “but also for sudden cardiac death.”
Extended ECG monitoring has been shown useful in the setting of cryptogenic stroke and after AF ablation, but similar findings have been scarce in HCM. Patients using personal wearable monitors such as smart watches, Dr. Caro Codón said, have come to his clinic with concerns that the devices may have signaled a problem. But the lack of relevant data leaves them without a sufficient answer.
In other findings, invited discussant Isabelle van Gelder, MD, PhD, observed after Dr. Caro Codón’s presentation that the number of patients with AF almost doubled based on extended monitoring, compared with the first 24 hours of monitoring.
Based on European Society of Cardiology guidelines from 2020, “Once clinical AF has been documented, there is a class IIA recommendation to start anticoagulation,” said Dr. van Gelder, University of Groningen, the Netherlands. “Therefore, your data really are a call for more data on screening for AF in hypertrophic cardiomyopathy patients.”
Prospective multicenter registry
The TEMPO-HCM registry includes patients with HCM and a clinical indication for standard Holter monitoring at five hospitals in Spain. It excludes patients with an HCM-like phenotype but who lack the telltale genotype, as well as those already implanted with an ICD.
Those in the current analysis underwent 30-day ECG monitoring with a small, wearable device that Dr. Caro Codón described as about 7 cm long, worn in what is essentially a T-shirt with a pocket. Patients could remove the shirt and device to bathe or go swimming, for example, and still be monitored for most of the day.
The analysis included the registry’s first 100 patients (mean age, 57 years; 78% male). Hypertension was present in 47%, 58% were on beta-blockers, 16% had prior AF or atrial flutter, and 19% were taking anticoagulants. Only 8% were on antiarrhythmic drugs, Dr. Caro Codón reported.
The patients had good functional status (68% and 29% were in NYHA class 1 and 2, respectively) and their left ventricular ejection fraction averaged 66%. Of the 71 patients who underwent MRI, 28.2% showed late gadolinium enhancement suggesting myocardial scarring.
More arrhythmias on 30-day monitoring
The primary endpoint of clinically relevant arrhythmia (AF, atrial flutter, or NSVT) was identified during the first 24 hours of monitoring in 11% of patients. The prevalence rose to 65% (P < .001) based on 30-day monitoring.
Similarly, prevalences of the composite primary endpoint components grew on extended monitoring, but the increases reached statistical significance only for NSVT; its prevalence went from 8% to 62% (P < .001). Prevalences rose nonsignificantly from 6% to 10% for AF and 0% to 1% for sustained ventricular tachycardia.
The incidence of NSVT during monitoring climbed fastest from day 0 through about day 19 and then rose more slowly through day 30, Dr. Caro Codón said. “It actually didn’t reach a plateau during this time period, so there is the possibility that if we had continued monitoring patients, the difference between both periods may have been even higher.”
Three variables predicted the incidence of nonsustained VT during monitoring, he said: age, atrial wall thickness, and whether there was late gadolinium enhancement at MRI.
An exploratory analysis looked at the 5-year risk of sudden cardiac death using the European Society of Cardiology HCM-SCD risk calculator recommended in guidelines. Risk assessment based on the 30-day extended monitoring period, compared with the first 24 hours of monitoring alone, predicted a significantly higher 5-year risk of sudden death, Dr. Caro Codón said.
“Even more importantly,” he added, “over 20%” of patients would have been reclassified into a higher-risk group and possibly considered for an ICD based on extended monitoring, compared to 24-hour monitoring.
However, given that more than 50% of patients were found to have NSVT during extended monitoring, Dr. Caro Codón proposed that decisions on whether to implant an ICD should not be so “binary” based on the presence or absence of symptoms, and proposed further investigations be conducted into the complete phenotype of these arrhythmias.
The study has limitations, he observed, including a relatively small size; but it was able to detect important differences between 24-hour and 30-day monitoring outcomes even with only 100 patients. It was also limited by a lack of clinical follow-up for information on endpoints like stroke, thromboembolism, and sudden cardiac death.
Extended monitoring detected more cases of NSVT in the study’s relatively low-risk HCM patients who would not generally have an indication for ICD implantation, observed Dr. van Gelder. Also, at present the prognostic value of NSVT for SCD “seems to be more important at younger age” – that is, younger than 30 years – in patients with HCM.
Dr. van Gelder echoed Dr. Caro Codón’s call for more data from prolonged monitoring to help stratify patients according to risk; she proposed NSVT frequency, duration, and rate as possible targets.
The study was supported by an unrestricted grant from Nuubo, which provided the ECG monitoring systems. Dr. Caro Codón and Dr. van Gelder reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BARCELONA – , suggests a study that questions current risk stratification practices in HCM.
In the registry study, such arrythmias were observed in about six times as many HCM patients during 30 days of ambulatory electrocardiographic monitoring as would have been identified based on the first 24 hours of the monitoring period: 65% vs. 11% of the cohort.
Also, about 62% of the patients showed NSVT at “extended” 30-day monitoring, compared with an 8% prevalence of the arrhythmia based on the more conventional ECG monitoring period of 24 hours.
Nonsustained ventricular tachycardia, an important arrhythmia used every day in clinical practice to make decisions, is “much, much more prevalent than we thought” in patients with HCM, Juan Caro Codón, MD, the study’s principal investigator, said in an interview. “We should invest in further research regarding extended ECG monitoring in these patients.”
Dr. Caro Codón, of La Paz University Hospital, Madrid, presented the findings from the TEMPO-HCM study at the European Heart Rhythm Association 2023 Congress, held in Barcelona and virtually.
Its results, he said, have implications for stratifying HCM patients according to their risk for sudden cardiac death in deciding who should be offered an implantable cardioverter-defibrillator (ICD).
The life-incidence of atrial fibrillation (AF) in patients like those in the current analysis has previously been found to be about 20%, and the life-prevalence of NSVT about 20%-30%, using traditional 24- or 48-hour Holter monitoring, Dr. Caro Codón said.
“These arrhythmias are clinically relevant events because they are linked to very meaningful clinical endpoints,” including stroke and thromboembolism, he said, “but also for sudden cardiac death.”
Extended ECG monitoring has been shown useful in the setting of cryptogenic stroke and after AF ablation, but similar findings have been scarce in HCM. Patients using personal wearable monitors such as smart watches, Dr. Caro Codón said, have come to his clinic with concerns that the devices may have signaled a problem. But the lack of relevant data leaves them without a sufficient answer.
In other findings, invited discussant Isabelle van Gelder, MD, PhD, observed after Dr. Caro Codón’s presentation that the number of patients with AF almost doubled based on extended monitoring, compared with the first 24 hours of monitoring.
Based on European Society of Cardiology guidelines from 2020, “Once clinical AF has been documented, there is a class IIA recommendation to start anticoagulation,” said Dr. van Gelder, University of Groningen, the Netherlands. “Therefore, your data really are a call for more data on screening for AF in hypertrophic cardiomyopathy patients.”
Prospective multicenter registry
The TEMPO-HCM registry includes patients with HCM and a clinical indication for standard Holter monitoring at five hospitals in Spain. It excludes patients with an HCM-like phenotype but who lack the telltale genotype, as well as those already implanted with an ICD.
Those in the current analysis underwent 30-day ECG monitoring with a small, wearable device that Dr. Caro Codón described as about 7 cm long, worn in what is essentially a T-shirt with a pocket. Patients could remove the shirt and device to bathe or go swimming, for example, and still be monitored for most of the day.
The analysis included the registry’s first 100 patients (mean age, 57 years; 78% male). Hypertension was present in 47%, 58% were on beta-blockers, 16% had prior AF or atrial flutter, and 19% were taking anticoagulants. Only 8% were on antiarrhythmic drugs, Dr. Caro Codón reported.
The patients had good functional status (68% and 29% were in NYHA class 1 and 2, respectively) and their left ventricular ejection fraction averaged 66%. Of the 71 patients who underwent MRI, 28.2% showed late gadolinium enhancement suggesting myocardial scarring.
More arrhythmias on 30-day monitoring
The primary endpoint of clinically relevant arrhythmia (AF, atrial flutter, or NSVT) was identified during the first 24 hours of monitoring in 11% of patients. The prevalence rose to 65% (P < .001) based on 30-day monitoring.
Similarly, prevalences of the composite primary endpoint components grew on extended monitoring, but the increases reached statistical significance only for NSVT; its prevalence went from 8% to 62% (P < .001). Prevalences rose nonsignificantly from 6% to 10% for AF and 0% to 1% for sustained ventricular tachycardia.
The incidence of NSVT during monitoring climbed fastest from day 0 through about day 19 and then rose more slowly through day 30, Dr. Caro Codón said. “It actually didn’t reach a plateau during this time period, so there is the possibility that if we had continued monitoring patients, the difference between both periods may have been even higher.”
Three variables predicted the incidence of nonsustained VT during monitoring, he said: age, atrial wall thickness, and whether there was late gadolinium enhancement at MRI.
An exploratory analysis looked at the 5-year risk of sudden cardiac death using the European Society of Cardiology HCM-SCD risk calculator recommended in guidelines. Risk assessment based on the 30-day extended monitoring period, compared with the first 24 hours of monitoring alone, predicted a significantly higher 5-year risk of sudden death, Dr. Caro Codón said.
“Even more importantly,” he added, “over 20%” of patients would have been reclassified into a higher-risk group and possibly considered for an ICD based on extended monitoring, compared to 24-hour monitoring.
However, given that more than 50% of patients were found to have NSVT during extended monitoring, Dr. Caro Codón proposed that decisions on whether to implant an ICD should not be so “binary” based on the presence or absence of symptoms, and proposed further investigations be conducted into the complete phenotype of these arrhythmias.
The study has limitations, he observed, including a relatively small size; but it was able to detect important differences between 24-hour and 30-day monitoring outcomes even with only 100 patients. It was also limited by a lack of clinical follow-up for information on endpoints like stroke, thromboembolism, and sudden cardiac death.
Extended monitoring detected more cases of NSVT in the study’s relatively low-risk HCM patients who would not generally have an indication for ICD implantation, observed Dr. van Gelder. Also, at present the prognostic value of NSVT for SCD “seems to be more important at younger age” – that is, younger than 30 years – in patients with HCM.
Dr. van Gelder echoed Dr. Caro Codón’s call for more data from prolonged monitoring to help stratify patients according to risk; she proposed NSVT frequency, duration, and rate as possible targets.
The study was supported by an unrestricted grant from Nuubo, which provided the ECG monitoring systems. Dr. Caro Codón and Dr. van Gelder reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BARCELONA – , suggests a study that questions current risk stratification practices in HCM.
In the registry study, such arrythmias were observed in about six times as many HCM patients during 30 days of ambulatory electrocardiographic monitoring as would have been identified based on the first 24 hours of the monitoring period: 65% vs. 11% of the cohort.
Also, about 62% of the patients showed NSVT at “extended” 30-day monitoring, compared with an 8% prevalence of the arrhythmia based on the more conventional ECG monitoring period of 24 hours.
Nonsustained ventricular tachycardia, an important arrhythmia used every day in clinical practice to make decisions, is “much, much more prevalent than we thought” in patients with HCM, Juan Caro Codón, MD, the study’s principal investigator, said in an interview. “We should invest in further research regarding extended ECG monitoring in these patients.”
Dr. Caro Codón, of La Paz University Hospital, Madrid, presented the findings from the TEMPO-HCM study at the European Heart Rhythm Association 2023 Congress, held in Barcelona and virtually.
Its results, he said, have implications for stratifying HCM patients according to their risk for sudden cardiac death in deciding who should be offered an implantable cardioverter-defibrillator (ICD).
The life-incidence of atrial fibrillation (AF) in patients like those in the current analysis has previously been found to be about 20%, and the life-prevalence of NSVT about 20%-30%, using traditional 24- or 48-hour Holter monitoring, Dr. Caro Codón said.
“These arrhythmias are clinically relevant events because they are linked to very meaningful clinical endpoints,” including stroke and thromboembolism, he said, “but also for sudden cardiac death.”
Extended ECG monitoring has been shown useful in the setting of cryptogenic stroke and after AF ablation, but similar findings have been scarce in HCM. Patients using personal wearable monitors such as smart watches, Dr. Caro Codón said, have come to his clinic with concerns that the devices may have signaled a problem. But the lack of relevant data leaves them without a sufficient answer.
In other findings, invited discussant Isabelle van Gelder, MD, PhD, observed after Dr. Caro Codón’s presentation that the number of patients with AF almost doubled based on extended monitoring, compared with the first 24 hours of monitoring.
Based on European Society of Cardiology guidelines from 2020, “Once clinical AF has been documented, there is a class IIA recommendation to start anticoagulation,” said Dr. van Gelder, University of Groningen, the Netherlands. “Therefore, your data really are a call for more data on screening for AF in hypertrophic cardiomyopathy patients.”
Prospective multicenter registry
The TEMPO-HCM registry includes patients with HCM and a clinical indication for standard Holter monitoring at five hospitals in Spain. It excludes patients with an HCM-like phenotype but who lack the telltale genotype, as well as those already implanted with an ICD.
Those in the current analysis underwent 30-day ECG monitoring with a small, wearable device that Dr. Caro Codón described as about 7 cm long, worn in what is essentially a T-shirt with a pocket. Patients could remove the shirt and device to bathe or go swimming, for example, and still be monitored for most of the day.
The analysis included the registry’s first 100 patients (mean age, 57 years; 78% male). Hypertension was present in 47%, 58% were on beta-blockers, 16% had prior AF or atrial flutter, and 19% were taking anticoagulants. Only 8% were on antiarrhythmic drugs, Dr. Caro Codón reported.
The patients had good functional status (68% and 29% were in NYHA class 1 and 2, respectively) and their left ventricular ejection fraction averaged 66%. Of the 71 patients who underwent MRI, 28.2% showed late gadolinium enhancement suggesting myocardial scarring.
More arrhythmias on 30-day monitoring
The primary endpoint of clinically relevant arrhythmia (AF, atrial flutter, or NSVT) was identified during the first 24 hours of monitoring in 11% of patients. The prevalence rose to 65% (P < .001) based on 30-day monitoring.
Similarly, prevalences of the composite primary endpoint components grew on extended monitoring, but the increases reached statistical significance only for NSVT; its prevalence went from 8% to 62% (P < .001). Prevalences rose nonsignificantly from 6% to 10% for AF and 0% to 1% for sustained ventricular tachycardia.
The incidence of NSVT during monitoring climbed fastest from day 0 through about day 19 and then rose more slowly through day 30, Dr. Caro Codón said. “It actually didn’t reach a plateau during this time period, so there is the possibility that if we had continued monitoring patients, the difference between both periods may have been even higher.”
Three variables predicted the incidence of nonsustained VT during monitoring, he said: age, atrial wall thickness, and whether there was late gadolinium enhancement at MRI.
An exploratory analysis looked at the 5-year risk of sudden cardiac death using the European Society of Cardiology HCM-SCD risk calculator recommended in guidelines. Risk assessment based on the 30-day extended monitoring period, compared with the first 24 hours of monitoring alone, predicted a significantly higher 5-year risk of sudden death, Dr. Caro Codón said.
“Even more importantly,” he added, “over 20%” of patients would have been reclassified into a higher-risk group and possibly considered for an ICD based on extended monitoring, compared to 24-hour monitoring.
However, given that more than 50% of patients were found to have NSVT during extended monitoring, Dr. Caro Codón proposed that decisions on whether to implant an ICD should not be so “binary” based on the presence or absence of symptoms, and proposed further investigations be conducted into the complete phenotype of these arrhythmias.
The study has limitations, he observed, including a relatively small size; but it was able to detect important differences between 24-hour and 30-day monitoring outcomes even with only 100 patients. It was also limited by a lack of clinical follow-up for information on endpoints like stroke, thromboembolism, and sudden cardiac death.
Extended monitoring detected more cases of NSVT in the study’s relatively low-risk HCM patients who would not generally have an indication for ICD implantation, observed Dr. van Gelder. Also, at present the prognostic value of NSVT for SCD “seems to be more important at younger age” – that is, younger than 30 years – in patients with HCM.
Dr. van Gelder echoed Dr. Caro Codón’s call for more data from prolonged monitoring to help stratify patients according to risk; she proposed NSVT frequency, duration, and rate as possible targets.
The study was supported by an unrestricted grant from Nuubo, which provided the ECG monitoring systems. Dr. Caro Codón and Dr. van Gelder reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EHRA
Statins tied to lower stroke risk in atrial fibrillation
Among patients with atrial fibrillation (AFib), initiation of statins soon after diagnosis was protective against stroke and related vascular events, and longer duration of use was associated with greater protection, a new cohort study shows.
Statin use was associated with lower risks of ischemic stroke or systemic embolism, hemorrhagic stroke, and transient ischemic attack (TIA), regardless of whether patients were also taking anticoagulant medications.
Lead author Jiayi Huang, a PhD student at Hong Kong University at Shenzhen (China) Hospital, concluded that the study’s findings support the use of statins to prevent stroke for patients with new-onset AFib.
“The findings have important clinical implications, particularly given that in atrial fibrillation, patients’ ischemic strokes are often fatal or disabling and have a high risk of recurrence,” she said.
The results were presented in a moderated poster session at the European Heart Rhythm Association 2023 Congress.
Widely prescribed
Anticoagulant drugs are prescribed to lower the fivefold increased risk of stroke among individuals with AFib, compared with those without AFib, but the therapy does not eliminate the higher risk, Ms. Huang explained. And although statins are widely prescribed to reduce the likelihood of myocardial infarction and stroke, “the benefit of statins for stroke prevention in patients with atrial fibrillation has been unclear.”
Ms. Huang and colleagues analyzed data from 51,472 patients newly diagnosed with AFib between 2010 and 2018. The population was divided into statin users (n = 11,866), defined as patients who had taken statins for at least 19 consecutive days in the first year after AFib diagnosis, and statin nonusers (n = 39,606), based on whether they were prescribed statin therapy after their first diagnosis of AFib.
The median age of the cohort was 74.9 years, and 47.7% were women. The investigators used statistical methods to balance baseline covariates between the two groups.
The primary outcomes were ischemic stroke or systemic embolism, hemorrhagic stroke, and TIA. Median follow-up was 5.1 years.
Statin use was associated with a significantly lower risk of all outcomes, compared with nonuse. Statin users had a 17% reduced risk of ischemic stroke or systemic embolism, a 7% reduced risk of hemorrhagic stroke, and a 15% rate of reduced risk of TIA, Ms. Huang reported.
“We also found long-term statin use was associated with greater protection than short-term use,” she said. For statin use of 6 years or longer, in comparison with use of 3 months to 2 years, the risk of ischemic stroke or systemic embolism was lowered by 43%; for hemorrhagic stroke, it was lowered by 44%, and for TIA, it was lowered by 42%.
These associations were consistent regardless of whether patients used anticoagulant medications or the type of anticoagulant.
Oussama Wazni, MD, MBA, section head of cardiac electrophysiology and pacing at the Cleveland Clinic, was a moderator of the poster session at which Ms. Huang presented her study. In an interview, he called the study “very important.”
“The message should be that all patients who have atrial fibrillation should be checked for cholesterol levels, and we should consider placing them on statins,” he said. “Is there an opportunity? Probably there is, and that’s why we’re seeing this effect in this group of patients.”
When asked about a possible mechanism by which statins produced the effects seen in the study, he pointed to LDL cholesterol lowering and possibly an effect on inflammation. “If a patient had a carotid atheroma, for example, maybe it helped with that,” he said. Previous work has shown that inflammation is related to or is associated with higher risk of thrombogenic effects, including MI or stroke.
It may be a bit less clear how statins reduced the incidence of hemorrhagic strokes, but Dr. Wazni proposed that some strokes could have started as an ischemic stroke “and then had hemorrhagic conversion, so we don’t have the granularity in here to know whether that was the case or not.”
Given the fact that the effect was stronger the longer a patient had been taking a statin, Dr. Wazni said that if a patient is tolerating the drug well, there should be no reason to discontinue it, regardless of age.
He said the study provides “welcome data and evidence because it’s pointing in the right direction,” but prospective studies would be useful “so that we can see what is driving what. Otherwise, this is just an association.”
The study was supported by Sanming Project Shenzhen. Ms. Huang and Dr. Wazni disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Among patients with atrial fibrillation (AFib), initiation of statins soon after diagnosis was protective against stroke and related vascular events, and longer duration of use was associated with greater protection, a new cohort study shows.
Statin use was associated with lower risks of ischemic stroke or systemic embolism, hemorrhagic stroke, and transient ischemic attack (TIA), regardless of whether patients were also taking anticoagulant medications.
Lead author Jiayi Huang, a PhD student at Hong Kong University at Shenzhen (China) Hospital, concluded that the study’s findings support the use of statins to prevent stroke for patients with new-onset AFib.
“The findings have important clinical implications, particularly given that in atrial fibrillation, patients’ ischemic strokes are often fatal or disabling and have a high risk of recurrence,” she said.
The results were presented in a moderated poster session at the European Heart Rhythm Association 2023 Congress.
Widely prescribed
Anticoagulant drugs are prescribed to lower the fivefold increased risk of stroke among individuals with AFib, compared with those without AFib, but the therapy does not eliminate the higher risk, Ms. Huang explained. And although statins are widely prescribed to reduce the likelihood of myocardial infarction and stroke, “the benefit of statins for stroke prevention in patients with atrial fibrillation has been unclear.”
Ms. Huang and colleagues analyzed data from 51,472 patients newly diagnosed with AFib between 2010 and 2018. The population was divided into statin users (n = 11,866), defined as patients who had taken statins for at least 19 consecutive days in the first year after AFib diagnosis, and statin nonusers (n = 39,606), based on whether they were prescribed statin therapy after their first diagnosis of AFib.
The median age of the cohort was 74.9 years, and 47.7% were women. The investigators used statistical methods to balance baseline covariates between the two groups.
The primary outcomes were ischemic stroke or systemic embolism, hemorrhagic stroke, and TIA. Median follow-up was 5.1 years.
Statin use was associated with a significantly lower risk of all outcomes, compared with nonuse. Statin users had a 17% reduced risk of ischemic stroke or systemic embolism, a 7% reduced risk of hemorrhagic stroke, and a 15% rate of reduced risk of TIA, Ms. Huang reported.
“We also found long-term statin use was associated with greater protection than short-term use,” she said. For statin use of 6 years or longer, in comparison with use of 3 months to 2 years, the risk of ischemic stroke or systemic embolism was lowered by 43%; for hemorrhagic stroke, it was lowered by 44%, and for TIA, it was lowered by 42%.
These associations were consistent regardless of whether patients used anticoagulant medications or the type of anticoagulant.
Oussama Wazni, MD, MBA, section head of cardiac electrophysiology and pacing at the Cleveland Clinic, was a moderator of the poster session at which Ms. Huang presented her study. In an interview, he called the study “very important.”
“The message should be that all patients who have atrial fibrillation should be checked for cholesterol levels, and we should consider placing them on statins,” he said. “Is there an opportunity? Probably there is, and that’s why we’re seeing this effect in this group of patients.”
When asked about a possible mechanism by which statins produced the effects seen in the study, he pointed to LDL cholesterol lowering and possibly an effect on inflammation. “If a patient had a carotid atheroma, for example, maybe it helped with that,” he said. Previous work has shown that inflammation is related to or is associated with higher risk of thrombogenic effects, including MI or stroke.
It may be a bit less clear how statins reduced the incidence of hemorrhagic strokes, but Dr. Wazni proposed that some strokes could have started as an ischemic stroke “and then had hemorrhagic conversion, so we don’t have the granularity in here to know whether that was the case or not.”
Given the fact that the effect was stronger the longer a patient had been taking a statin, Dr. Wazni said that if a patient is tolerating the drug well, there should be no reason to discontinue it, regardless of age.
He said the study provides “welcome data and evidence because it’s pointing in the right direction,” but prospective studies would be useful “so that we can see what is driving what. Otherwise, this is just an association.”
The study was supported by Sanming Project Shenzhen. Ms. Huang and Dr. Wazni disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Among patients with atrial fibrillation (AFib), initiation of statins soon after diagnosis was protective against stroke and related vascular events, and longer duration of use was associated with greater protection, a new cohort study shows.
Statin use was associated with lower risks of ischemic stroke or systemic embolism, hemorrhagic stroke, and transient ischemic attack (TIA), regardless of whether patients were also taking anticoagulant medications.
Lead author Jiayi Huang, a PhD student at Hong Kong University at Shenzhen (China) Hospital, concluded that the study’s findings support the use of statins to prevent stroke for patients with new-onset AFib.
“The findings have important clinical implications, particularly given that in atrial fibrillation, patients’ ischemic strokes are often fatal or disabling and have a high risk of recurrence,” she said.
The results were presented in a moderated poster session at the European Heart Rhythm Association 2023 Congress.
Widely prescribed
Anticoagulant drugs are prescribed to lower the fivefold increased risk of stroke among individuals with AFib, compared with those without AFib, but the therapy does not eliminate the higher risk, Ms. Huang explained. And although statins are widely prescribed to reduce the likelihood of myocardial infarction and stroke, “the benefit of statins for stroke prevention in patients with atrial fibrillation has been unclear.”
Ms. Huang and colleagues analyzed data from 51,472 patients newly diagnosed with AFib between 2010 and 2018. The population was divided into statin users (n = 11,866), defined as patients who had taken statins for at least 19 consecutive days in the first year after AFib diagnosis, and statin nonusers (n = 39,606), based on whether they were prescribed statin therapy after their first diagnosis of AFib.
The median age of the cohort was 74.9 years, and 47.7% were women. The investigators used statistical methods to balance baseline covariates between the two groups.
The primary outcomes were ischemic stroke or systemic embolism, hemorrhagic stroke, and TIA. Median follow-up was 5.1 years.
Statin use was associated with a significantly lower risk of all outcomes, compared with nonuse. Statin users had a 17% reduced risk of ischemic stroke or systemic embolism, a 7% reduced risk of hemorrhagic stroke, and a 15% rate of reduced risk of TIA, Ms. Huang reported.
“We also found long-term statin use was associated with greater protection than short-term use,” she said. For statin use of 6 years or longer, in comparison with use of 3 months to 2 years, the risk of ischemic stroke or systemic embolism was lowered by 43%; for hemorrhagic stroke, it was lowered by 44%, and for TIA, it was lowered by 42%.
These associations were consistent regardless of whether patients used anticoagulant medications or the type of anticoagulant.
Oussama Wazni, MD, MBA, section head of cardiac electrophysiology and pacing at the Cleveland Clinic, was a moderator of the poster session at which Ms. Huang presented her study. In an interview, he called the study “very important.”
“The message should be that all patients who have atrial fibrillation should be checked for cholesterol levels, and we should consider placing them on statins,” he said. “Is there an opportunity? Probably there is, and that’s why we’re seeing this effect in this group of patients.”
When asked about a possible mechanism by which statins produced the effects seen in the study, he pointed to LDL cholesterol lowering and possibly an effect on inflammation. “If a patient had a carotid atheroma, for example, maybe it helped with that,” he said. Previous work has shown that inflammation is related to or is associated with higher risk of thrombogenic effects, including MI or stroke.
It may be a bit less clear how statins reduced the incidence of hemorrhagic strokes, but Dr. Wazni proposed that some strokes could have started as an ischemic stroke “and then had hemorrhagic conversion, so we don’t have the granularity in here to know whether that was the case or not.”
Given the fact that the effect was stronger the longer a patient had been taking a statin, Dr. Wazni said that if a patient is tolerating the drug well, there should be no reason to discontinue it, regardless of age.
He said the study provides “welcome data and evidence because it’s pointing in the right direction,” but prospective studies would be useful “so that we can see what is driving what. Otherwise, this is just an association.”
The study was supported by Sanming Project Shenzhen. Ms. Huang and Dr. Wazni disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM EHRA 2023
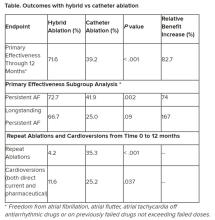
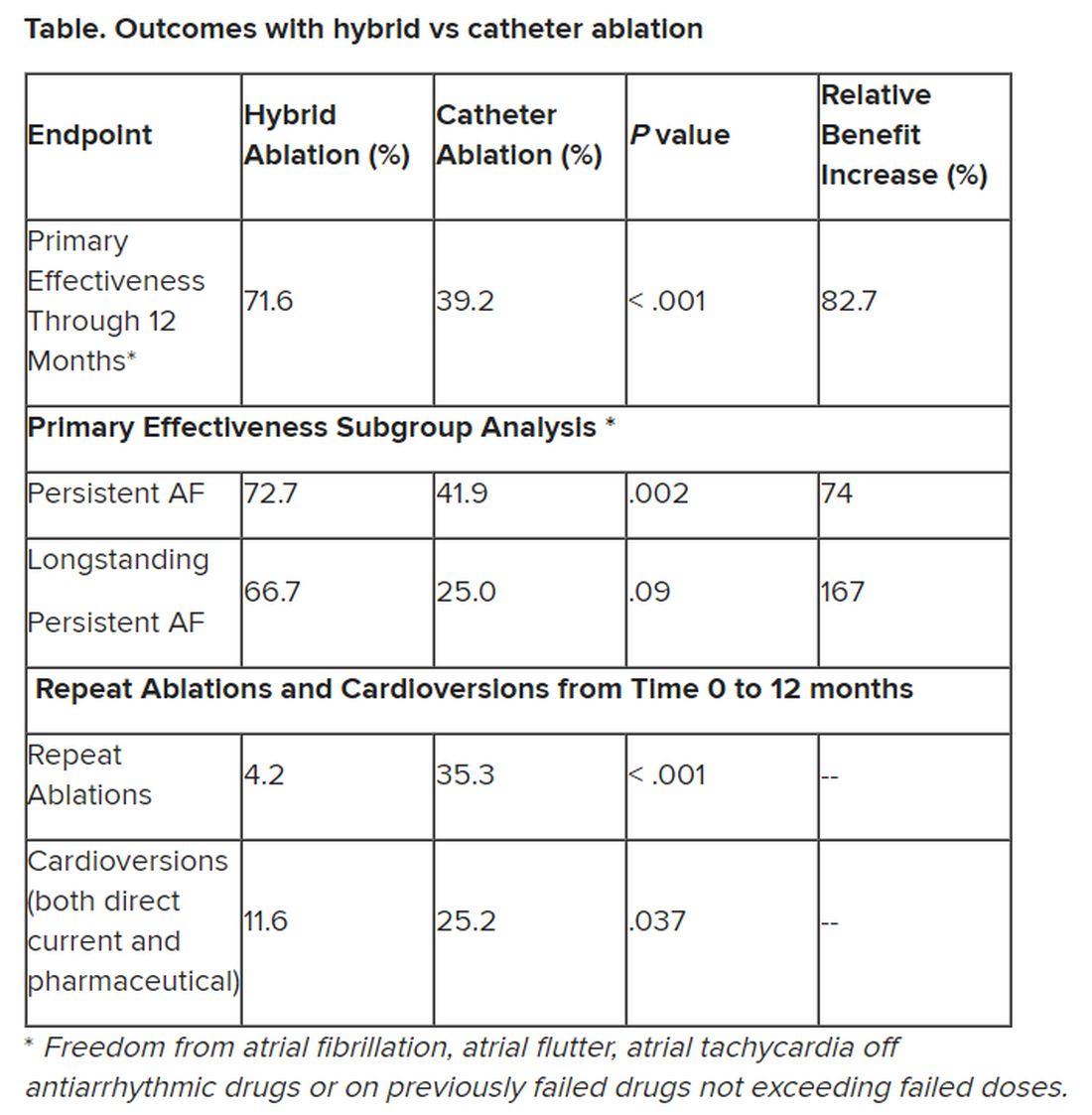
Hybrid ablation superior for persistent AFib: CEASE-AF
BARCELONA – Staged hybrid ablation provided superior freedom from atrial arrhythmias compared with endocardial catheter ablation alone, including the need for repeat ablations in patients with advanced atrial fibrillation (AF), new data show.
“We have seen that hybrid ablation resulted in 32.4% absolute benefit increase in effectiveness and 83% relative benefit increase, so this is a huge difference,” concluded cardiac surgeon Nicholas Doll, MD, PhD, Schüchtermann Clinic, Bad Rothenfelde, Germany.
Dr. Doll presented the 12-month follow up results of the Combined Endoscopic Epicardial and Percutaneous Endocardial Ablation Versus Repeated Catheter Ablation in Persistent and Longstanding Persistent Atrial Fibrillation (CEASE-AF) trial at the European Heart Rhythm Association 2023 Congress, held recently in Barcelona and virtually.
He said CEASE-AF is the largest multicenter randomized clinical trial comparing these two approaches for control of atrial arrhythmias.
Safety outcomes were numerically higher in the hybrid ablation (HA) group of the trial but not statistically different from the catheter ablation (CA) group.
Unstable wavefront
As background, Dr. Doll explained that in advanced AF, there is a high degree of endocardial-epicardial dissociation with unstable wavefront propagation transitioning between the endocardial and epicardial surfaces. Endocardial mapping and ablation alone may be insufficient to address the mechanism of AF.
“So, the hypothesis of the CEASE-AF study was a minimally invasive hybrid ablation approach which combines endocardial and epicardial ablation to achieve superior effectiveness when compared to endocardial catheter ablation alone,” he said.
This prospective clinical trial randomized patients 2:1 at nine sites in five countries to HA (n = 102) or CA (n = 52). All had left atrial diameter of 4 cm to 6 cm and persistent AF for up to 1 year or longstanding persistent AF for greater than 1 year up to 10 years.
Any patient with a previous ablation procedure, BMI greater than 35 kg/m2, or left ventricular ejection fraction less than 30% was excluded.
For HA, stage 1 consisted of epicardial lesions for pulmonary vein isolation (PVI) plus the posterior wall box plus left atrial appendage exclusion using the AtriClip (AtriCure Inc.) left atrial appendage exclusion device. Stage 2 involved endocardial mapping and catheter ablation to address gaps.
For CA, the index procedure involved catheter-mediated PVI plus repeat endocardial ablation as clinically indicated. For both HA and CA, additional ablation techniques and lesions were allowed for nonparoxysmal AF.
The HA timeline was the first stage, index procedure at time 0 (n = 102), a 90-day blanking period, and then the second stage, endocardial procedure at 90 to 180 days from the index procedure (n = 93).
For the CA arm of the trial, endocardial catheter ablation was performed on a minimal endocardial lesion set at time 0. Then after a 90-day blanking period, repeat catheter ablation was performed if clinically indicated (6/52).
Repeat ablations and electrical or pharmaceutical cardioversions were allowed during the 12-month follow-up period from time 0.
The primary efficacy endpoint was freedom from AF, atrial flutter, or atrial tachycardia of greater than 30 seconds through 12 months in the absence of class I/III antiarrhythmic drugs except ones that previously had failed, at doses not exceeding those previously failed doses. The safety endpoint was a composite rate of major complications over the course of the study.
Even with relatively modest cohort sizes, the HA and CA arms of the trial were well matched at baseline for age (approximately 60 years), gender (75.5% and 73.1% male, respectively), BMI (29.7 and 29.8 kg/m2), and persistent AF (79.4% and 82.7%).
The groups had persistent AF for 2.94 ± 3.29 years and 3.34 ± 3.52 years, respectively. The mean left atrial size was 4.7 ± 0.5 cm for the HA group and 4.7 ± 0.4 cm for the CA group.
Outcomes favored hybrid ablation over catheter ablation, the researchers reported. “We never would have expected these huge differences,” Dr. Doll told the congress. “We have seen that hybrid ablation resulted in 32.4% absolute benefit increase in effectiveness and 83% relative benefit increase.”
Subgroup analyses were consistent with the primary endpoint, but he said they would not be published because the trial was not powered for such comparisons.
Still, he noted that “there are only slightly reduced outcomes in the long-standing [persistent AF subgroup] in a really challenging patient arm, and we still have a success rate of 67%.” And the repeat ablations in about one-third of patients in the CA arm and need for cardioversions in about one quarter of them may have implications for reduced quality of life.
The total procedure duration was higher for the hybrid group at 336.4 ± 97 minutes, taking into account the index procedure plus the second stage procedure, vs. endocardial ablation at 251.9 ± 114 minutes, which includes the index procedure plus any repeat ablations (HA vs AF total duration, P < .001). Overall fluoroscopy time was approximately 8 minutes shorter for the HA arm.
Complications were assessed for 30 days post index procedure and 30 days post second stage procedure for the HA arm and for 30 days post index procedure and any repeat ablation for the CA arm.
The HA arm showed a complication rate of 7.8% vs. 5.8% for the CA arm (P = .751). Two patients in the former and three patients in the latter group had more than one major complication. There was one death in the HA group 93 days after the index procedure, and it was adjudicated as unrelated to the procedure.
“If you look back in the past, other studies showed a ... higher complication rate in the hybrid arm, so we feel very comfortable with these complication rates, which [are] very low and almost comparable,” Dr. Doll said.
Limitations of the study included symptom-driven electrocardiogram monitoring performed at unscheduled visits. Also, ablation beyond PVI in the CA arm and PVI/posterior box in the HA arm was not standardized and was performed according to standard practices in the participating countries.
“Success of epicardial-endocardial approach emphasizes the role of the collaborative heart team approach in the treatment of nonparoxysmal atrial fibrillation, and if I sum it up together, we can do it better” together, Dr. Doll advised.
‘Exceptional’ trial
After Dr. Doll’s presentation, appointed discussant Stylianos Tzeis, MD, PhD, head of the cardiology clinic and electrophysiology and pacing department at Mitera Hospital in Athens, congratulated the investigators and called CEASE-AF “an exceptional trial. It was really challenging to enroll patients in such a randomized controlled clinical trial.”
But Dr. Tzeis questioned whether pitting CA against HA was a fair comparison.
“Were the ablation targets similar between the two groups?” he asked. He noted that for the HA group, in the first stage the patients had PVI, posterior wall isolation, exclusion of the left atrial appendage, and additional lesions at the discretion of the operator. Ninety percent proceeded to the second stage, which was endocardial catheter ablation with verification of posterior wall isolation and PVI and additional lesions made if needed.
In the CA group, repeat catheter ablation could be performed after the 90-day blanking period if clinically indicated. “Please take note that only 10% were offered the second ablation. So at least in my perspective, this was a comparison of a two-stage approach versus a single-stage approach with a much more aggressive ablation protocol in the hybrid ablation group as compared to the endocardial group,” he said.
Seeing the higher success rate of the HA group in achieving the primary efficacy endpoint of freedom from all arrhythmias at 12 months, Dr. Tzeis asked, “Does this reflect the superiority of the epi-endo approach, or does it reflect the suboptimal performance of the catheter ablation approach?”
There was a 40% success rate in the CA patient population, a cohort that he deemed “not the most challenging persistent AF population in the world”: those with left atrial diameter of 47 millimeters and with 80% having an AF duration less than 12 months.
He also noted that “the average duration of the catheter ablation for the PVI in the vast majority of cases was 4 hours, which does not reflect what really happens in the everyday practice.”
All those critiques having been advanced, Dr. Tzeis said, “Definitely do not doubt my first comment that the authors should be congratulated, and I strongly believe that the main objective has been achieved to bring electrophysiologist and cardiac surgeons ... closer.”
The study sponsor was AtriCure Inc. with collaboration of Cardialysis BV. Doll has received consulting fees or royalties and/or has ownership or stockholder interest in AtriCure. Tzeis reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
BARCELONA – Staged hybrid ablation provided superior freedom from atrial arrhythmias compared with endocardial catheter ablation alone, including the need for repeat ablations in patients with advanced atrial fibrillation (AF), new data show.
“We have seen that hybrid ablation resulted in 32.4% absolute benefit increase in effectiveness and 83% relative benefit increase, so this is a huge difference,” concluded cardiac surgeon Nicholas Doll, MD, PhD, Schüchtermann Clinic, Bad Rothenfelde, Germany.
Dr. Doll presented the 12-month follow up results of the Combined Endoscopic Epicardial and Percutaneous Endocardial Ablation Versus Repeated Catheter Ablation in Persistent and Longstanding Persistent Atrial Fibrillation (CEASE-AF) trial at the European Heart Rhythm Association 2023 Congress, held recently in Barcelona and virtually.
He said CEASE-AF is the largest multicenter randomized clinical trial comparing these two approaches for control of atrial arrhythmias.
Safety outcomes were numerically higher in the hybrid ablation (HA) group of the trial but not statistically different from the catheter ablation (CA) group.
Unstable wavefront
As background, Dr. Doll explained that in advanced AF, there is a high degree of endocardial-epicardial dissociation with unstable wavefront propagation transitioning between the endocardial and epicardial surfaces. Endocardial mapping and ablation alone may be insufficient to address the mechanism of AF.
“So, the hypothesis of the CEASE-AF study was a minimally invasive hybrid ablation approach which combines endocardial and epicardial ablation to achieve superior effectiveness when compared to endocardial catheter ablation alone,” he said.
This prospective clinical trial randomized patients 2:1 at nine sites in five countries to HA (n = 102) or CA (n = 52). All had left atrial diameter of 4 cm to 6 cm and persistent AF for up to 1 year or longstanding persistent AF for greater than 1 year up to 10 years.
Any patient with a previous ablation procedure, BMI greater than 35 kg/m2, or left ventricular ejection fraction less than 30% was excluded.
For HA, stage 1 consisted of epicardial lesions for pulmonary vein isolation (PVI) plus the posterior wall box plus left atrial appendage exclusion using the AtriClip (AtriCure Inc.) left atrial appendage exclusion device. Stage 2 involved endocardial mapping and catheter ablation to address gaps.
For CA, the index procedure involved catheter-mediated PVI plus repeat endocardial ablation as clinically indicated. For both HA and CA, additional ablation techniques and lesions were allowed for nonparoxysmal AF.
The HA timeline was the first stage, index procedure at time 0 (n = 102), a 90-day blanking period, and then the second stage, endocardial procedure at 90 to 180 days from the index procedure (n = 93).
For the CA arm of the trial, endocardial catheter ablation was performed on a minimal endocardial lesion set at time 0. Then after a 90-day blanking period, repeat catheter ablation was performed if clinically indicated (6/52).
Repeat ablations and electrical or pharmaceutical cardioversions were allowed during the 12-month follow-up period from time 0.
The primary efficacy endpoint was freedom from AF, atrial flutter, or atrial tachycardia of greater than 30 seconds through 12 months in the absence of class I/III antiarrhythmic drugs except ones that previously had failed, at doses not exceeding those previously failed doses. The safety endpoint was a composite rate of major complications over the course of the study.
Even with relatively modest cohort sizes, the HA and CA arms of the trial were well matched at baseline for age (approximately 60 years), gender (75.5% and 73.1% male, respectively), BMI (29.7 and 29.8 kg/m2), and persistent AF (79.4% and 82.7%).
The groups had persistent AF for 2.94 ± 3.29 years and 3.34 ± 3.52 years, respectively. The mean left atrial size was 4.7 ± 0.5 cm for the HA group and 4.7 ± 0.4 cm for the CA group.
Outcomes favored hybrid ablation over catheter ablation, the researchers reported. “We never would have expected these huge differences,” Dr. Doll told the congress. “We have seen that hybrid ablation resulted in 32.4% absolute benefit increase in effectiveness and 83% relative benefit increase.”
Subgroup analyses were consistent with the primary endpoint, but he said they would not be published because the trial was not powered for such comparisons.
Still, he noted that “there are only slightly reduced outcomes in the long-standing [persistent AF subgroup] in a really challenging patient arm, and we still have a success rate of 67%.” And the repeat ablations in about one-third of patients in the CA arm and need for cardioversions in about one quarter of them may have implications for reduced quality of life.
The total procedure duration was higher for the hybrid group at 336.4 ± 97 minutes, taking into account the index procedure plus the second stage procedure, vs. endocardial ablation at 251.9 ± 114 minutes, which includes the index procedure plus any repeat ablations (HA vs AF total duration, P < .001). Overall fluoroscopy time was approximately 8 minutes shorter for the HA arm.
Complications were assessed for 30 days post index procedure and 30 days post second stage procedure for the HA arm and for 30 days post index procedure and any repeat ablation for the CA arm.
The HA arm showed a complication rate of 7.8% vs. 5.8% for the CA arm (P = .751). Two patients in the former and three patients in the latter group had more than one major complication. There was one death in the HA group 93 days after the index procedure, and it was adjudicated as unrelated to the procedure.
“If you look back in the past, other studies showed a ... higher complication rate in the hybrid arm, so we feel very comfortable with these complication rates, which [are] very low and almost comparable,” Dr. Doll said.
Limitations of the study included symptom-driven electrocardiogram monitoring performed at unscheduled visits. Also, ablation beyond PVI in the CA arm and PVI/posterior box in the HA arm was not standardized and was performed according to standard practices in the participating countries.
“Success of epicardial-endocardial approach emphasizes the role of the collaborative heart team approach in the treatment of nonparoxysmal atrial fibrillation, and if I sum it up together, we can do it better” together, Dr. Doll advised.
‘Exceptional’ trial
After Dr. Doll’s presentation, appointed discussant Stylianos Tzeis, MD, PhD, head of the cardiology clinic and electrophysiology and pacing department at Mitera Hospital in Athens, congratulated the investigators and called CEASE-AF “an exceptional trial. It was really challenging to enroll patients in such a randomized controlled clinical trial.”
But Dr. Tzeis questioned whether pitting CA against HA was a fair comparison.
“Were the ablation targets similar between the two groups?” he asked. He noted that for the HA group, in the first stage the patients had PVI, posterior wall isolation, exclusion of the left atrial appendage, and additional lesions at the discretion of the operator. Ninety percent proceeded to the second stage, which was endocardial catheter ablation with verification of posterior wall isolation and PVI and additional lesions made if needed.
In the CA group, repeat catheter ablation could be performed after the 90-day blanking period if clinically indicated. “Please take note that only 10% were offered the second ablation. So at least in my perspective, this was a comparison of a two-stage approach versus a single-stage approach with a much more aggressive ablation protocol in the hybrid ablation group as compared to the endocardial group,” he said.
Seeing the higher success rate of the HA group in achieving the primary efficacy endpoint of freedom from all arrhythmias at 12 months, Dr. Tzeis asked, “Does this reflect the superiority of the epi-endo approach, or does it reflect the suboptimal performance of the catheter ablation approach?”
There was a 40% success rate in the CA patient population, a cohort that he deemed “not the most challenging persistent AF population in the world”: those with left atrial diameter of 47 millimeters and with 80% having an AF duration less than 12 months.
He also noted that “the average duration of the catheter ablation for the PVI in the vast majority of cases was 4 hours, which does not reflect what really happens in the everyday practice.”
All those critiques having been advanced, Dr. Tzeis said, “Definitely do not doubt my first comment that the authors should be congratulated, and I strongly believe that the main objective has been achieved to bring electrophysiologist and cardiac surgeons ... closer.”
The study sponsor was AtriCure Inc. with collaboration of Cardialysis BV. Doll has received consulting fees or royalties and/or has ownership or stockholder interest in AtriCure. Tzeis reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
BARCELONA – Staged hybrid ablation provided superior freedom from atrial arrhythmias compared with endocardial catheter ablation alone, including the need for repeat ablations in patients with advanced atrial fibrillation (AF), new data show.
“We have seen that hybrid ablation resulted in 32.4% absolute benefit increase in effectiveness and 83% relative benefit increase, so this is a huge difference,” concluded cardiac surgeon Nicholas Doll, MD, PhD, Schüchtermann Clinic, Bad Rothenfelde, Germany.
Dr. Doll presented the 12-month follow up results of the Combined Endoscopic Epicardial and Percutaneous Endocardial Ablation Versus Repeated Catheter Ablation in Persistent and Longstanding Persistent Atrial Fibrillation (CEASE-AF) trial at the European Heart Rhythm Association 2023 Congress, held recently in Barcelona and virtually.
He said CEASE-AF is the largest multicenter randomized clinical trial comparing these two approaches for control of atrial arrhythmias.
Safety outcomes were numerically higher in the hybrid ablation (HA) group of the trial but not statistically different from the catheter ablation (CA) group.
Unstable wavefront
As background, Dr. Doll explained that in advanced AF, there is a high degree of endocardial-epicardial dissociation with unstable wavefront propagation transitioning between the endocardial and epicardial surfaces. Endocardial mapping and ablation alone may be insufficient to address the mechanism of AF.
“So, the hypothesis of the CEASE-AF study was a minimally invasive hybrid ablation approach which combines endocardial and epicardial ablation to achieve superior effectiveness when compared to endocardial catheter ablation alone,” he said.
This prospective clinical trial randomized patients 2:1 at nine sites in five countries to HA (n = 102) or CA (n = 52). All had left atrial diameter of 4 cm to 6 cm and persistent AF for up to 1 year or longstanding persistent AF for greater than 1 year up to 10 years.
Any patient with a previous ablation procedure, BMI greater than 35 kg/m2, or left ventricular ejection fraction less than 30% was excluded.
For HA, stage 1 consisted of epicardial lesions for pulmonary vein isolation (PVI) plus the posterior wall box plus left atrial appendage exclusion using the AtriClip (AtriCure Inc.) left atrial appendage exclusion device. Stage 2 involved endocardial mapping and catheter ablation to address gaps.
For CA, the index procedure involved catheter-mediated PVI plus repeat endocardial ablation as clinically indicated. For both HA and CA, additional ablation techniques and lesions were allowed for nonparoxysmal AF.
The HA timeline was the first stage, index procedure at time 0 (n = 102), a 90-day blanking period, and then the second stage, endocardial procedure at 90 to 180 days from the index procedure (n = 93).
For the CA arm of the trial, endocardial catheter ablation was performed on a minimal endocardial lesion set at time 0. Then after a 90-day blanking period, repeat catheter ablation was performed if clinically indicated (6/52).
Repeat ablations and electrical or pharmaceutical cardioversions were allowed during the 12-month follow-up period from time 0.
The primary efficacy endpoint was freedom from AF, atrial flutter, or atrial tachycardia of greater than 30 seconds through 12 months in the absence of class I/III antiarrhythmic drugs except ones that previously had failed, at doses not exceeding those previously failed doses. The safety endpoint was a composite rate of major complications over the course of the study.
Even with relatively modest cohort sizes, the HA and CA arms of the trial were well matched at baseline for age (approximately 60 years), gender (75.5% and 73.1% male, respectively), BMI (29.7 and 29.8 kg/m2), and persistent AF (79.4% and 82.7%).
The groups had persistent AF for 2.94 ± 3.29 years and 3.34 ± 3.52 years, respectively. The mean left atrial size was 4.7 ± 0.5 cm for the HA group and 4.7 ± 0.4 cm for the CA group.
Outcomes favored hybrid ablation over catheter ablation, the researchers reported. “We never would have expected these huge differences,” Dr. Doll told the congress. “We have seen that hybrid ablation resulted in 32.4% absolute benefit increase in effectiveness and 83% relative benefit increase.”
Subgroup analyses were consistent with the primary endpoint, but he said they would not be published because the trial was not powered for such comparisons.
Still, he noted that “there are only slightly reduced outcomes in the long-standing [persistent AF subgroup] in a really challenging patient arm, and we still have a success rate of 67%.” And the repeat ablations in about one-third of patients in the CA arm and need for cardioversions in about one quarter of them may have implications for reduced quality of life.
The total procedure duration was higher for the hybrid group at 336.4 ± 97 minutes, taking into account the index procedure plus the second stage procedure, vs. endocardial ablation at 251.9 ± 114 minutes, which includes the index procedure plus any repeat ablations (HA vs AF total duration, P < .001). Overall fluoroscopy time was approximately 8 minutes shorter for the HA arm.
Complications were assessed for 30 days post index procedure and 30 days post second stage procedure for the HA arm and for 30 days post index procedure and any repeat ablation for the CA arm.
The HA arm showed a complication rate of 7.8% vs. 5.8% for the CA arm (P = .751). Two patients in the former and three patients in the latter group had more than one major complication. There was one death in the HA group 93 days after the index procedure, and it was adjudicated as unrelated to the procedure.
“If you look back in the past, other studies showed a ... higher complication rate in the hybrid arm, so we feel very comfortable with these complication rates, which [are] very low and almost comparable,” Dr. Doll said.
Limitations of the study included symptom-driven electrocardiogram monitoring performed at unscheduled visits. Also, ablation beyond PVI in the CA arm and PVI/posterior box in the HA arm was not standardized and was performed according to standard practices in the participating countries.
“Success of epicardial-endocardial approach emphasizes the role of the collaborative heart team approach in the treatment of nonparoxysmal atrial fibrillation, and if I sum it up together, we can do it better” together, Dr. Doll advised.
‘Exceptional’ trial
After Dr. Doll’s presentation, appointed discussant Stylianos Tzeis, MD, PhD, head of the cardiology clinic and electrophysiology and pacing department at Mitera Hospital in Athens, congratulated the investigators and called CEASE-AF “an exceptional trial. It was really challenging to enroll patients in such a randomized controlled clinical trial.”
But Dr. Tzeis questioned whether pitting CA against HA was a fair comparison.
“Were the ablation targets similar between the two groups?” he asked. He noted that for the HA group, in the first stage the patients had PVI, posterior wall isolation, exclusion of the left atrial appendage, and additional lesions at the discretion of the operator. Ninety percent proceeded to the second stage, which was endocardial catheter ablation with verification of posterior wall isolation and PVI and additional lesions made if needed.
In the CA group, repeat catheter ablation could be performed after the 90-day blanking period if clinically indicated. “Please take note that only 10% were offered the second ablation. So at least in my perspective, this was a comparison of a two-stage approach versus a single-stage approach with a much more aggressive ablation protocol in the hybrid ablation group as compared to the endocardial group,” he said.
Seeing the higher success rate of the HA group in achieving the primary efficacy endpoint of freedom from all arrhythmias at 12 months, Dr. Tzeis asked, “Does this reflect the superiority of the epi-endo approach, or does it reflect the suboptimal performance of the catheter ablation approach?”
There was a 40% success rate in the CA patient population, a cohort that he deemed “not the most challenging persistent AF population in the world”: those with left atrial diameter of 47 millimeters and with 80% having an AF duration less than 12 months.
He also noted that “the average duration of the catheter ablation for the PVI in the vast majority of cases was 4 hours, which does not reflect what really happens in the everyday practice.”
All those critiques having been advanced, Dr. Tzeis said, “Definitely do not doubt my first comment that the authors should be congratulated, and I strongly believe that the main objective has been achieved to bring electrophysiologist and cardiac surgeons ... closer.”
The study sponsor was AtriCure Inc. with collaboration of Cardialysis BV. Doll has received consulting fees or royalties and/or has ownership or stockholder interest in AtriCure. Tzeis reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AT EHRA 2023