User login
Cervical pessary didn’t prevent preterm birth in selected women
GRAPEVINE, TEX. – or a composite measure of adverse neonatal outcomes, according to a randomized, open-label study.
“The Arabin pessary should not be used to prevent preterm birth in women with twin pregnancy,” Jane E. Norman, MD, dean of health sciences at the University of Bristol (England), said at the Pregnancy Meeting.
“Preterm birth is very common in twin pregnancy” and leads to “excess neonatal mortality amongst twins,” Dr. Norman said at the meeting, which is sponsored by the Society for Maternal-Fetal Medicine. “Preventing preterm birth is important for both singletons and twins, but it could have even more benefits in twins.”
Emerging evidence has suggested that the Arabin cervical pessary may be useful for the prevention of preterm birth in women with singleton pregnancy and a short cervix. In twin pregnancy, data are more limited.
The ProTwin study randomized 813 women with twin pregnancy to a cervical pessary or standard care. Although the pessary had no impact on preterm birth overall, among women with cervical length of less than 38 mm, those who received a pessary were less likely to have preterm birth. The sample size was small, however, and the average length of the cervix in ProTwin differed from that in a previous U.K. study, Dr. Norman said.
Inspired by the study, Dr. Norman and coinvestigators conducted STOPPIT-2, a multicenter, open-label, randomized, controlled trial to further study whether a certain cervical length threshold was associated with benefit of a cervical pessary in preventing preterm birth. The trial included women with twin pregnancy who had a cervical length ultrasound between 18 and 20 weeks and 6 days of gestation. Women with a cervical length of 35 mm or less were eligible for randomization. Patients received an Arabin pessary plus standard care or standard care alone.
The primary obstetric outcome was spontaneous onset of labor leading to delivery before 34 weeks and 6 days of gestation. The primary neonatal outcome was a composite of outcomes – stillbirth, neonatal death, periventricular leukomalacia, respiratory morbidity, intraventricular hemorrhage, necrotizing enterocolitis, or sepsis – measured up to 28 days after the expected date of delivery.
The investigators randomized 503 women in all, including 250 to the pessary and 253 to standard care. Both groups had similar baseline characteristics, Dr. Norman said. The average age was about 33 years, and the average cervical length was about 29 mm. A total of 20% had monochorionic diamniotic pregnancies, and 80% had dichorionic pregnancies. The researchers excluded women with monochorionic monoamniotic pregnancies. In the pessary group, 16 patients declined the intervention, and 4 were unable to have the pessary inserted.
Spontaneous preterm birth occurred in 18% of patients in the Arabin pessary group, compared with 21% in the standard treatment group. The adjusted odds ratio, 0.87, was not statistically significant. In subgroups of patients with monochorionic pregnancy, cervical length less than 28 mm, or cervical length less than 25 mm, there was no significant benefit.
The composite measure of adverse neonatal outcomes also did not significantly differ between the groups. None of the individual components indicated benefit of the pessary either, Dr. Norman said.
In subgroup analyses, odds ratios for adverse neonatal outcomes were “tending towards harm for the Arabin pessary group ... although clearly none of them conferring statistical significance,” she said. Among women with cervical length less than 28 mm, a primary neonatal outcome – at least one of the adverse outcomes – occurred in 23% of patients in the Arabin pessary group, compared with 20% of patients in the standard care group.
Approximately two-thirds of patients found pessary insertion painless or slightly uncomfortable, whereas about 10% described the experience of device fitting as very uncomfortable, and about 1% described it as the worse pain imaginable.
“Since we started STOPPIT-2, in addition to ProTwin, another three studies have been published on the efficacy of the Arabin pessary in twins,” said Dr. Norman. Combined data show no significant effect of the pessary on preventing preterm birth in twin pregnancy. Still, the meta-analysis does not rule out the possibility that there could subgroups of patients who may benefit from the intervention, Dr. Norman said.
STOPPIT-2 was funded by the National Institute for Health Research (NIHR) in the United Kingdom. Dr. Norman chaired the UK National Institute for Health and Care Excellence guidelines on preterm labor and birth in 2015. In addition, Dr. Norman was a member of a GlaxoSmithKline data safety and monitoring group for a trial of a preterm birth prevention agent, has consulted for Dilafor, and has received research grants for preterm birth prevention from the U.K. Medical Research Council, NIHR, and Tommy’s: Together, for every baby charity.
SOURCE: Norman JE et al. Am J Obstet Gynecol. 2020 Jan;222(1):S756. Abstract LB 1.
GRAPEVINE, TEX. – or a composite measure of adverse neonatal outcomes, according to a randomized, open-label study.
“The Arabin pessary should not be used to prevent preterm birth in women with twin pregnancy,” Jane E. Norman, MD, dean of health sciences at the University of Bristol (England), said at the Pregnancy Meeting.
“Preterm birth is very common in twin pregnancy” and leads to “excess neonatal mortality amongst twins,” Dr. Norman said at the meeting, which is sponsored by the Society for Maternal-Fetal Medicine. “Preventing preterm birth is important for both singletons and twins, but it could have even more benefits in twins.”
Emerging evidence has suggested that the Arabin cervical pessary may be useful for the prevention of preterm birth in women with singleton pregnancy and a short cervix. In twin pregnancy, data are more limited.
The ProTwin study randomized 813 women with twin pregnancy to a cervical pessary or standard care. Although the pessary had no impact on preterm birth overall, among women with cervical length of less than 38 mm, those who received a pessary were less likely to have preterm birth. The sample size was small, however, and the average length of the cervix in ProTwin differed from that in a previous U.K. study, Dr. Norman said.
Inspired by the study, Dr. Norman and coinvestigators conducted STOPPIT-2, a multicenter, open-label, randomized, controlled trial to further study whether a certain cervical length threshold was associated with benefit of a cervical pessary in preventing preterm birth. The trial included women with twin pregnancy who had a cervical length ultrasound between 18 and 20 weeks and 6 days of gestation. Women with a cervical length of 35 mm or less were eligible for randomization. Patients received an Arabin pessary plus standard care or standard care alone.
The primary obstetric outcome was spontaneous onset of labor leading to delivery before 34 weeks and 6 days of gestation. The primary neonatal outcome was a composite of outcomes – stillbirth, neonatal death, periventricular leukomalacia, respiratory morbidity, intraventricular hemorrhage, necrotizing enterocolitis, or sepsis – measured up to 28 days after the expected date of delivery.
The investigators randomized 503 women in all, including 250 to the pessary and 253 to standard care. Both groups had similar baseline characteristics, Dr. Norman said. The average age was about 33 years, and the average cervical length was about 29 mm. A total of 20% had monochorionic diamniotic pregnancies, and 80% had dichorionic pregnancies. The researchers excluded women with monochorionic monoamniotic pregnancies. In the pessary group, 16 patients declined the intervention, and 4 were unable to have the pessary inserted.
Spontaneous preterm birth occurred in 18% of patients in the Arabin pessary group, compared with 21% in the standard treatment group. The adjusted odds ratio, 0.87, was not statistically significant. In subgroups of patients with monochorionic pregnancy, cervical length less than 28 mm, or cervical length less than 25 mm, there was no significant benefit.
The composite measure of adverse neonatal outcomes also did not significantly differ between the groups. None of the individual components indicated benefit of the pessary either, Dr. Norman said.
In subgroup analyses, odds ratios for adverse neonatal outcomes were “tending towards harm for the Arabin pessary group ... although clearly none of them conferring statistical significance,” she said. Among women with cervical length less than 28 mm, a primary neonatal outcome – at least one of the adverse outcomes – occurred in 23% of patients in the Arabin pessary group, compared with 20% of patients in the standard care group.
Approximately two-thirds of patients found pessary insertion painless or slightly uncomfortable, whereas about 10% described the experience of device fitting as very uncomfortable, and about 1% described it as the worse pain imaginable.
“Since we started STOPPIT-2, in addition to ProTwin, another three studies have been published on the efficacy of the Arabin pessary in twins,” said Dr. Norman. Combined data show no significant effect of the pessary on preventing preterm birth in twin pregnancy. Still, the meta-analysis does not rule out the possibility that there could subgroups of patients who may benefit from the intervention, Dr. Norman said.
STOPPIT-2 was funded by the National Institute for Health Research (NIHR) in the United Kingdom. Dr. Norman chaired the UK National Institute for Health and Care Excellence guidelines on preterm labor and birth in 2015. In addition, Dr. Norman was a member of a GlaxoSmithKline data safety and monitoring group for a trial of a preterm birth prevention agent, has consulted for Dilafor, and has received research grants for preterm birth prevention from the U.K. Medical Research Council, NIHR, and Tommy’s: Together, for every baby charity.
SOURCE: Norman JE et al. Am J Obstet Gynecol. 2020 Jan;222(1):S756. Abstract LB 1.
GRAPEVINE, TEX. – or a composite measure of adverse neonatal outcomes, according to a randomized, open-label study.
“The Arabin pessary should not be used to prevent preterm birth in women with twin pregnancy,” Jane E. Norman, MD, dean of health sciences at the University of Bristol (England), said at the Pregnancy Meeting.
“Preterm birth is very common in twin pregnancy” and leads to “excess neonatal mortality amongst twins,” Dr. Norman said at the meeting, which is sponsored by the Society for Maternal-Fetal Medicine. “Preventing preterm birth is important for both singletons and twins, but it could have even more benefits in twins.”
Emerging evidence has suggested that the Arabin cervical pessary may be useful for the prevention of preterm birth in women with singleton pregnancy and a short cervix. In twin pregnancy, data are more limited.
The ProTwin study randomized 813 women with twin pregnancy to a cervical pessary or standard care. Although the pessary had no impact on preterm birth overall, among women with cervical length of less than 38 mm, those who received a pessary were less likely to have preterm birth. The sample size was small, however, and the average length of the cervix in ProTwin differed from that in a previous U.K. study, Dr. Norman said.
Inspired by the study, Dr. Norman and coinvestigators conducted STOPPIT-2, a multicenter, open-label, randomized, controlled trial to further study whether a certain cervical length threshold was associated with benefit of a cervical pessary in preventing preterm birth. The trial included women with twin pregnancy who had a cervical length ultrasound between 18 and 20 weeks and 6 days of gestation. Women with a cervical length of 35 mm or less were eligible for randomization. Patients received an Arabin pessary plus standard care or standard care alone.
The primary obstetric outcome was spontaneous onset of labor leading to delivery before 34 weeks and 6 days of gestation. The primary neonatal outcome was a composite of outcomes – stillbirth, neonatal death, periventricular leukomalacia, respiratory morbidity, intraventricular hemorrhage, necrotizing enterocolitis, or sepsis – measured up to 28 days after the expected date of delivery.
The investigators randomized 503 women in all, including 250 to the pessary and 253 to standard care. Both groups had similar baseline characteristics, Dr. Norman said. The average age was about 33 years, and the average cervical length was about 29 mm. A total of 20% had monochorionic diamniotic pregnancies, and 80% had dichorionic pregnancies. The researchers excluded women with monochorionic monoamniotic pregnancies. In the pessary group, 16 patients declined the intervention, and 4 were unable to have the pessary inserted.
Spontaneous preterm birth occurred in 18% of patients in the Arabin pessary group, compared with 21% in the standard treatment group. The adjusted odds ratio, 0.87, was not statistically significant. In subgroups of patients with monochorionic pregnancy, cervical length less than 28 mm, or cervical length less than 25 mm, there was no significant benefit.
The composite measure of adverse neonatal outcomes also did not significantly differ between the groups. None of the individual components indicated benefit of the pessary either, Dr. Norman said.
In subgroup analyses, odds ratios for adverse neonatal outcomes were “tending towards harm for the Arabin pessary group ... although clearly none of them conferring statistical significance,” she said. Among women with cervical length less than 28 mm, a primary neonatal outcome – at least one of the adverse outcomes – occurred in 23% of patients in the Arabin pessary group, compared with 20% of patients in the standard care group.
Approximately two-thirds of patients found pessary insertion painless or slightly uncomfortable, whereas about 10% described the experience of device fitting as very uncomfortable, and about 1% described it as the worse pain imaginable.
“Since we started STOPPIT-2, in addition to ProTwin, another three studies have been published on the efficacy of the Arabin pessary in twins,” said Dr. Norman. Combined data show no significant effect of the pessary on preventing preterm birth in twin pregnancy. Still, the meta-analysis does not rule out the possibility that there could subgroups of patients who may benefit from the intervention, Dr. Norman said.
STOPPIT-2 was funded by the National Institute for Health Research (NIHR) in the United Kingdom. Dr. Norman chaired the UK National Institute for Health and Care Excellence guidelines on preterm labor and birth in 2015. In addition, Dr. Norman was a member of a GlaxoSmithKline data safety and monitoring group for a trial of a preterm birth prevention agent, has consulted for Dilafor, and has received research grants for preterm birth prevention from the U.K. Medical Research Council, NIHR, and Tommy’s: Together, for every baby charity.
SOURCE: Norman JE et al. Am J Obstet Gynecol. 2020 Jan;222(1):S756. Abstract LB 1.
REPORTING FROM THE PREGNANCY MEETING
Maternal methadone opioid maintenance therapy may be tied to smaller postnatal head circumference
GRAPEVINE, TEX. – compared with opioid maintenance therapy with buprenorphine, according to a study presented at the Pregnancy Meeting.
Antenatal ultrasound measurements do not differ by treatment, however, the researchers said. A separate study suggests that serial ultrasound examinations of fetal brain and biometry measurements may not be helpful in patients who receive these medications for opioid use disorder.
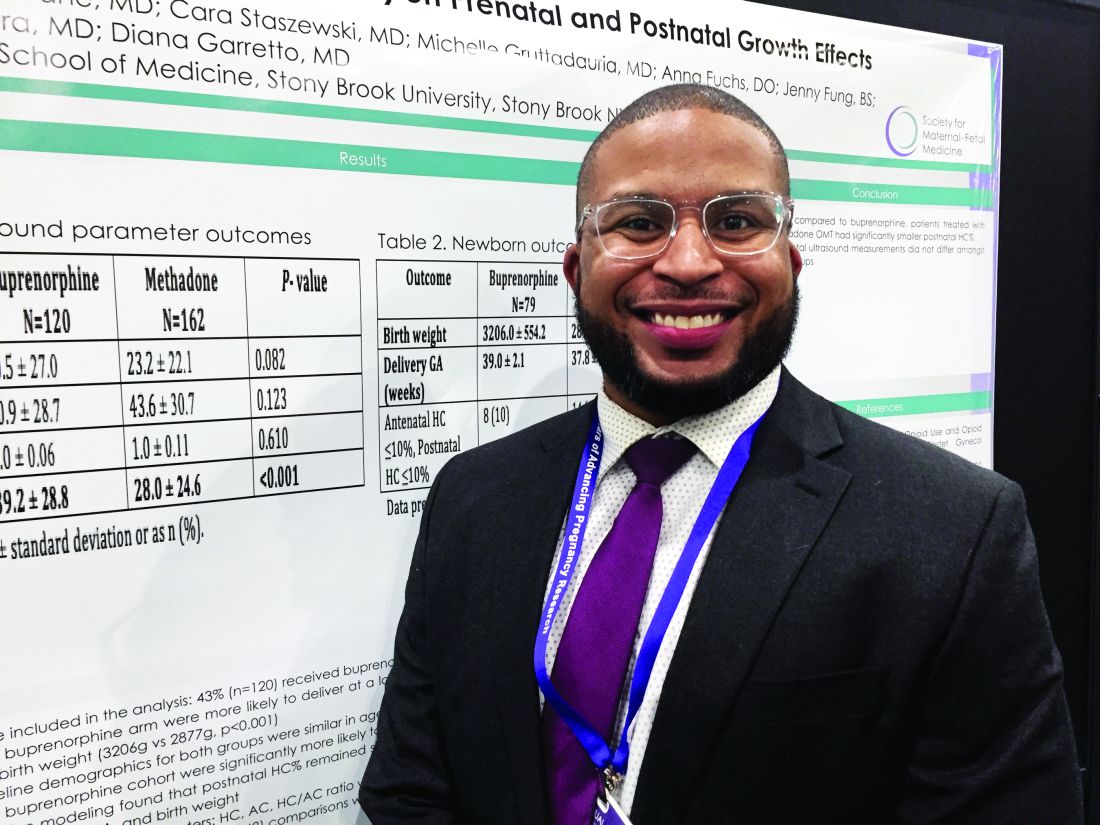
To examine the effects of methadone and buprenorphine opioid maintenance therapy on prenatal and postnatal growth parameters, Jay Davis, MD, a maternal-fetal medicine fellow at Stony Brook University in New York, and coinvestigators conducted a retrospective cohort study using medical records from an academic center during 2007-2017. They included women with singleton pregnancies receiving opioid maintenance therapy with methadone or buprenorphine. They compared head circumference percentile, abdominal circumference percentile, head circumference/abdominal circumference ratio, and postnatal head circumference percentile between the two groups. The investigators analyzed the data using the Wilcoxon–Mann–Whitney test, chi-square test, and logistic regression.
The researchers studied 282 cases, including 120 patients who received buprenorphine and 162 who received methadone. Patients who received buprenorphine delivered at a later average gestational age (39 weeks vs. 37.8 weeks) and had newborns with greater average birth weights (3,206 g vs. 2,877 g). Compared with patients who received methadone, patients who received buprenorphine were significantly more likely to have a larger postnatal head circumference percentile (39 vs. 30), Dr. Davis and colleagues reported. This difference remained significant after controlling for race, prescriber, gestational age at delivery, and birth weight.
In a separate study presented at the meeting sponsored by the Society for Maternal-Fetal Medicine, Jose M. Perez Yordan, MD, of the University of New Mexico, Albuquerque, and colleagues examined effects of medications for opioid use disorder on fetal brain and body measurements.
They found that maternal medications for opioid use disorder do not have a clinically significant effect on fetal brain and body measurements, compared with controls. “No consistent pattern of decreased fetal growth was identified, since the body measurement affected did not persist with serial ultrasounds,” they said. “Serial ultrasound examinations do not appear to be helpful in patients” who take medications of opioid use disorder, with or without alcohol coexposure, unless other risk factors are present.
To evaluate the effects of medications of opioid use disorder and alcohol coexposure on fetal brain and biometric measurements at the second- and third-trimester ultrasound measurements, the investigators are conducting a prospective study known as ENRICH-1. The study includes healthy controls, patients taking medications of opioid use disorder (that is, buprenorphine or methadone), and patients taking medications of opioid use disorder with alcohol coexposure.
Ultrasound measurements from the second and third trimesters evaluated biparietal diameter, femur length, frontal lobe width and length, front-thalamic distance, and caval-calvarial distance. Univariate and multivariate analyses assessed differences in measurements adjusting for gestational age and other factors.
The present analysis included data from 171 participants, including 56 healthy controls, 75 patients taking medications of opioid use disorder, and 40 patients taking medications of opioid use disorder with alcohol coexposure. There was no consistent pattern of decreased fetal growth. Affected measurements did not persist over time.
The study presented by Dr. Perez Yordan was supported by a National Institute on Alcohol Abuse and Alcoholism grant. The remaining investigators in both studies had no relevant financial disclosures.
SOURCE: Perez Yordan JM et al. Am J Obstet Gynecol. 2020 Jan;222(1):S110, Abstract 149; Davis J et al. Am J Obstet Gynecol. 2020 Jan;222(1):S430, Abstract 678.
GRAPEVINE, TEX. – compared with opioid maintenance therapy with buprenorphine, according to a study presented at the Pregnancy Meeting.
Antenatal ultrasound measurements do not differ by treatment, however, the researchers said. A separate study suggests that serial ultrasound examinations of fetal brain and biometry measurements may not be helpful in patients who receive these medications for opioid use disorder.
To examine the effects of methadone and buprenorphine opioid maintenance therapy on prenatal and postnatal growth parameters, Jay Davis, MD, a maternal-fetal medicine fellow at Stony Brook University in New York, and coinvestigators conducted a retrospective cohort study using medical records from an academic center during 2007-2017. They included women with singleton pregnancies receiving opioid maintenance therapy with methadone or buprenorphine. They compared head circumference percentile, abdominal circumference percentile, head circumference/abdominal circumference ratio, and postnatal head circumference percentile between the two groups. The investigators analyzed the data using the Wilcoxon–Mann–Whitney test, chi-square test, and logistic regression.
The researchers studied 282 cases, including 120 patients who received buprenorphine and 162 who received methadone. Patients who received buprenorphine delivered at a later average gestational age (39 weeks vs. 37.8 weeks) and had newborns with greater average birth weights (3,206 g vs. 2,877 g). Compared with patients who received methadone, patients who received buprenorphine were significantly more likely to have a larger postnatal head circumference percentile (39 vs. 30), Dr. Davis and colleagues reported. This difference remained significant after controlling for race, prescriber, gestational age at delivery, and birth weight.
In a separate study presented at the meeting sponsored by the Society for Maternal-Fetal Medicine, Jose M. Perez Yordan, MD, of the University of New Mexico, Albuquerque, and colleagues examined effects of medications for opioid use disorder on fetal brain and body measurements.
They found that maternal medications for opioid use disorder do not have a clinically significant effect on fetal brain and body measurements, compared with controls. “No consistent pattern of decreased fetal growth was identified, since the body measurement affected did not persist with serial ultrasounds,” they said. “Serial ultrasound examinations do not appear to be helpful in patients” who take medications of opioid use disorder, with or without alcohol coexposure, unless other risk factors are present.
To evaluate the effects of medications of opioid use disorder and alcohol coexposure on fetal brain and biometric measurements at the second- and third-trimester ultrasound measurements, the investigators are conducting a prospective study known as ENRICH-1. The study includes healthy controls, patients taking medications of opioid use disorder (that is, buprenorphine or methadone), and patients taking medications of opioid use disorder with alcohol coexposure.
Ultrasound measurements from the second and third trimesters evaluated biparietal diameter, femur length, frontal lobe width and length, front-thalamic distance, and caval-calvarial distance. Univariate and multivariate analyses assessed differences in measurements adjusting for gestational age and other factors.
The present analysis included data from 171 participants, including 56 healthy controls, 75 patients taking medications of opioid use disorder, and 40 patients taking medications of opioid use disorder with alcohol coexposure. There was no consistent pattern of decreased fetal growth. Affected measurements did not persist over time.
The study presented by Dr. Perez Yordan was supported by a National Institute on Alcohol Abuse and Alcoholism grant. The remaining investigators in both studies had no relevant financial disclosures.
SOURCE: Perez Yordan JM et al. Am J Obstet Gynecol. 2020 Jan;222(1):S110, Abstract 149; Davis J et al. Am J Obstet Gynecol. 2020 Jan;222(1):S430, Abstract 678.
GRAPEVINE, TEX. – compared with opioid maintenance therapy with buprenorphine, according to a study presented at the Pregnancy Meeting.
Antenatal ultrasound measurements do not differ by treatment, however, the researchers said. A separate study suggests that serial ultrasound examinations of fetal brain and biometry measurements may not be helpful in patients who receive these medications for opioid use disorder.
To examine the effects of methadone and buprenorphine opioid maintenance therapy on prenatal and postnatal growth parameters, Jay Davis, MD, a maternal-fetal medicine fellow at Stony Brook University in New York, and coinvestigators conducted a retrospective cohort study using medical records from an academic center during 2007-2017. They included women with singleton pregnancies receiving opioid maintenance therapy with methadone or buprenorphine. They compared head circumference percentile, abdominal circumference percentile, head circumference/abdominal circumference ratio, and postnatal head circumference percentile between the two groups. The investigators analyzed the data using the Wilcoxon–Mann–Whitney test, chi-square test, and logistic regression.
The researchers studied 282 cases, including 120 patients who received buprenorphine and 162 who received methadone. Patients who received buprenorphine delivered at a later average gestational age (39 weeks vs. 37.8 weeks) and had newborns with greater average birth weights (3,206 g vs. 2,877 g). Compared with patients who received methadone, patients who received buprenorphine were significantly more likely to have a larger postnatal head circumference percentile (39 vs. 30), Dr. Davis and colleagues reported. This difference remained significant after controlling for race, prescriber, gestational age at delivery, and birth weight.
In a separate study presented at the meeting sponsored by the Society for Maternal-Fetal Medicine, Jose M. Perez Yordan, MD, of the University of New Mexico, Albuquerque, and colleagues examined effects of medications for opioid use disorder on fetal brain and body measurements.
They found that maternal medications for opioid use disorder do not have a clinically significant effect on fetal brain and body measurements, compared with controls. “No consistent pattern of decreased fetal growth was identified, since the body measurement affected did not persist with serial ultrasounds,” they said. “Serial ultrasound examinations do not appear to be helpful in patients” who take medications of opioid use disorder, with or without alcohol coexposure, unless other risk factors are present.
To evaluate the effects of medications of opioid use disorder and alcohol coexposure on fetal brain and biometric measurements at the second- and third-trimester ultrasound measurements, the investigators are conducting a prospective study known as ENRICH-1. The study includes healthy controls, patients taking medications of opioid use disorder (that is, buprenorphine or methadone), and patients taking medications of opioid use disorder with alcohol coexposure.
Ultrasound measurements from the second and third trimesters evaluated biparietal diameter, femur length, frontal lobe width and length, front-thalamic distance, and caval-calvarial distance. Univariate and multivariate analyses assessed differences in measurements adjusting for gestational age and other factors.
The present analysis included data from 171 participants, including 56 healthy controls, 75 patients taking medications of opioid use disorder, and 40 patients taking medications of opioid use disorder with alcohol coexposure. There was no consistent pattern of decreased fetal growth. Affected measurements did not persist over time.
The study presented by Dr. Perez Yordan was supported by a National Institute on Alcohol Abuse and Alcoholism grant. The remaining investigators in both studies had no relevant financial disclosures.
SOURCE: Perez Yordan JM et al. Am J Obstet Gynecol. 2020 Jan;222(1):S110, Abstract 149; Davis J et al. Am J Obstet Gynecol. 2020 Jan;222(1):S430, Abstract 678.
REPORTING FROM THE PREGNANCY MEETING
High BMI does not complicate postpartum tubal ligation
GRAPEVINE, TEXAS – Higher body mass index is not associated with increased morbidity in women undergoing postpartum tubal ligation, according to a study of more than 1,000 patients.
John J. Byrne, MD, said at the Pregnancy Meeting. Dr. Byrne is affiliated with the department of obstetrics and gynecology at University of Texas Southwestern Medical Center in Dallas.
Physicians may recommend contraception within 6 weeks of delivery, but many patients do not attend postpartum visits. “One option for women who have completed childbearing is bilateral midsegment salpingectomy via minilaparotomy,” Dr. Byrne said at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine. “Offering this procedure immediately after delivery makes it available to women who face obstacles to follow-up care.”
The procedure entails the risk of anesthetic complications, bowel injury, and vascular injury. Subsequent pregnancy or ectopic pregnancy also may occur. Some centers will not perform the procedure if a patient’s size affects the surgeon’s ability to feel the relevant anatomy, Dr. Byrne said. “Although operative complications are presumed to be higher among obese women,” prior studies have not examined whether BMI affects rates of procedure completion, complication, or subsequent pregnancy, the researchers said.
To study this question, Dr. Byrne and colleagues examined data from women who requested postpartum sterilization following vaginal delivery at their center in 2018. The center uses the Parkland tubal ligation technique. The researchers assessed complication rates using a composite measure that included surgical complications (that is, blood transfusion, aborted procedure, or extension of incision), anesthetic complications, readmission, superficial or deep wound infection, venous thromboembolism, ileus or small bowel obstruction, incomplete transection, and subsequent pregnancy. The investigators used statistical tests to assess the relationship between BMI and morbidity.
In all, 1,014 patients underwent a postpartum tubal ligation; 17% had undergone prior abdominal surgery. The researchers classified patients’ BMI as normal (7% of the population), overweight (28%), class I obesity (38%), class II obesity (18%), or class III obesity (9%). A composite morbidity event occurred in 2%, and the proportion of patients with a complication did not significantly differ across BMI categories. No morbid events occurred in patients with normal BMI, which indicates “minimal risk” in this population, Dr. Byrne said. One incomplete transection occurred in a patient with class I obesity, and one subsequent pregnancy occurred in a patient with class II obesity. Estimated blood loss ranged from 9 mL in patients with normal BMI to 13 mL in patients with class III obesity, and length of surgery ranged from 32 minutes to 40 minutes. Neither difference is clinically significant, Dr. Byrne said.
“For the woman who desires permanent contraception, BMI should not impede her access to the procedure,” he noted.
The researchers had no relevant disclosures.
SOURCE: Byrne JJ et al. Am J Obstet Gynecol. 2020 Jan;222(1):S290, Abstract 442.
GRAPEVINE, TEXAS – Higher body mass index is not associated with increased morbidity in women undergoing postpartum tubal ligation, according to a study of more than 1,000 patients.
John J. Byrne, MD, said at the Pregnancy Meeting. Dr. Byrne is affiliated with the department of obstetrics and gynecology at University of Texas Southwestern Medical Center in Dallas.
Physicians may recommend contraception within 6 weeks of delivery, but many patients do not attend postpartum visits. “One option for women who have completed childbearing is bilateral midsegment salpingectomy via minilaparotomy,” Dr. Byrne said at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine. “Offering this procedure immediately after delivery makes it available to women who face obstacles to follow-up care.”
The procedure entails the risk of anesthetic complications, bowel injury, and vascular injury. Subsequent pregnancy or ectopic pregnancy also may occur. Some centers will not perform the procedure if a patient’s size affects the surgeon’s ability to feel the relevant anatomy, Dr. Byrne said. “Although operative complications are presumed to be higher among obese women,” prior studies have not examined whether BMI affects rates of procedure completion, complication, or subsequent pregnancy, the researchers said.
To study this question, Dr. Byrne and colleagues examined data from women who requested postpartum sterilization following vaginal delivery at their center in 2018. The center uses the Parkland tubal ligation technique. The researchers assessed complication rates using a composite measure that included surgical complications (that is, blood transfusion, aborted procedure, or extension of incision), anesthetic complications, readmission, superficial or deep wound infection, venous thromboembolism, ileus or small bowel obstruction, incomplete transection, and subsequent pregnancy. The investigators used statistical tests to assess the relationship between BMI and morbidity.
In all, 1,014 patients underwent a postpartum tubal ligation; 17% had undergone prior abdominal surgery. The researchers classified patients’ BMI as normal (7% of the population), overweight (28%), class I obesity (38%), class II obesity (18%), or class III obesity (9%). A composite morbidity event occurred in 2%, and the proportion of patients with a complication did not significantly differ across BMI categories. No morbid events occurred in patients with normal BMI, which indicates “minimal risk” in this population, Dr. Byrne said. One incomplete transection occurred in a patient with class I obesity, and one subsequent pregnancy occurred in a patient with class II obesity. Estimated blood loss ranged from 9 mL in patients with normal BMI to 13 mL in patients with class III obesity, and length of surgery ranged from 32 minutes to 40 minutes. Neither difference is clinically significant, Dr. Byrne said.
“For the woman who desires permanent contraception, BMI should not impede her access to the procedure,” he noted.
The researchers had no relevant disclosures.
SOURCE: Byrne JJ et al. Am J Obstet Gynecol. 2020 Jan;222(1):S290, Abstract 442.
GRAPEVINE, TEXAS – Higher body mass index is not associated with increased morbidity in women undergoing postpartum tubal ligation, according to a study of more than 1,000 patients.
John J. Byrne, MD, said at the Pregnancy Meeting. Dr. Byrne is affiliated with the department of obstetrics and gynecology at University of Texas Southwestern Medical Center in Dallas.
Physicians may recommend contraception within 6 weeks of delivery, but many patients do not attend postpartum visits. “One option for women who have completed childbearing is bilateral midsegment salpingectomy via minilaparotomy,” Dr. Byrne said at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine. “Offering this procedure immediately after delivery makes it available to women who face obstacles to follow-up care.”
The procedure entails the risk of anesthetic complications, bowel injury, and vascular injury. Subsequent pregnancy or ectopic pregnancy also may occur. Some centers will not perform the procedure if a patient’s size affects the surgeon’s ability to feel the relevant anatomy, Dr. Byrne said. “Although operative complications are presumed to be higher among obese women,” prior studies have not examined whether BMI affects rates of procedure completion, complication, or subsequent pregnancy, the researchers said.
To study this question, Dr. Byrne and colleagues examined data from women who requested postpartum sterilization following vaginal delivery at their center in 2018. The center uses the Parkland tubal ligation technique. The researchers assessed complication rates using a composite measure that included surgical complications (that is, blood transfusion, aborted procedure, or extension of incision), anesthetic complications, readmission, superficial or deep wound infection, venous thromboembolism, ileus or small bowel obstruction, incomplete transection, and subsequent pregnancy. The investigators used statistical tests to assess the relationship between BMI and morbidity.
In all, 1,014 patients underwent a postpartum tubal ligation; 17% had undergone prior abdominal surgery. The researchers classified patients’ BMI as normal (7% of the population), overweight (28%), class I obesity (38%), class II obesity (18%), or class III obesity (9%). A composite morbidity event occurred in 2%, and the proportion of patients with a complication did not significantly differ across BMI categories. No morbid events occurred in patients with normal BMI, which indicates “minimal risk” in this population, Dr. Byrne said. One incomplete transection occurred in a patient with class I obesity, and one subsequent pregnancy occurred in a patient with class II obesity. Estimated blood loss ranged from 9 mL in patients with normal BMI to 13 mL in patients with class III obesity, and length of surgery ranged from 32 minutes to 40 minutes. Neither difference is clinically significant, Dr. Byrne said.
“For the woman who desires permanent contraception, BMI should not impede her access to the procedure,” he noted.
The researchers had no relevant disclosures.
SOURCE: Byrne JJ et al. Am J Obstet Gynecol. 2020 Jan;222(1):S290, Abstract 442.
REPORTING FROM THE PREGNANCY MEETING
ERAS protocol for cesarean delivery reduces opioid usage
GRAPEVINE, TEX. – An enhanced recovery after surgery (ERAS) pathway for cesarean delivery decreased postoperative opioid usage by 62% in one health care organization, researchers reported at the Pregnancy Meeting. The protocol incorporates a stepwise approach to pain control with no scheduled postoperative opioids.
Abington Jefferson Health, which includes two hospitals in Pennsylvania, implemented an ERAS pathway for all cesarean deliveries in October 2018. Kathryn Ruymann, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Dr. Ruymann is an obstetrics and gynecology resident at Abington Jefferson Health.
Prior to the ERAS protocol, 99%-100% of patients took an opioid during the postoperative period. “With ERAS, 26% of patients never took an opioid during the postop period,” Dr. Ruymann and her associates reported. “Pain scores decreased with ERAS for postoperative days 1-3 and remained unchanged on day 4.”
One in 300 opioid-naive patients who receives opioids after cesarean delivery becomes a persistent user, one study has shown (Am J Obstet Gynecol. 2016 Sep; 215(3):353.e1-18). “ERAS pathways integrate evidence-based interventions before, during, and after surgery to optimize outcomes, specifically to decrease postoperative opioid use,” the researchers said.
While other surgical fields have adopted ERAS pathways, more research is needed in obstetrics, said Dr. Ruymann. More than 4,500 women deliver at Abington Jefferson Health each year, and about a third undergo cesarean deliveries.
The organization’s ERAS pathway incorporates preoperative education, fasting guidelines, and intraoperative analgesia, nausea prophylaxis, and antimicrobial therapy. Under the new protocol, postoperative analgesia includes scheduled administration of nonopioid medications, including celecoxib and acetaminophen. In addition, patients may take 5-10 mg of oxycodone orally every 4 hours as needed, and hydromorphone 0.4 mg IV as needed may be used for refractory pain. In addition, patients should resume eating as soon as tolerated and be out of bed within 4 hours after surgery, according to the protocol. Postoperative management of pruritus and instructions on how to wean off opioids at home are among the other elements of the enhanced recovery plan.
To examine postoperative opioid usage before and after implementation of the ERAS pathway, the investigators conducted a retrospective cohort study of 316 women who underwent cesarean delivery 3 months before the start of the ERAS pathway and 267 who underwent cesarean delivery 3 months after. The researchers used an application developed in Qlik Sense, a data analytics platform, to calculate opioid usage.
Mean postoperative opioid use decreased by 62%. The reduction in opioid use remained 8 months after starting the ERAS pathway.
“An ERAS pathway for [cesarean delivery] decreases postoperative opioid usage by integrating a multimodal stepwise approach to pain control and recovery,” the researchers said. “Standardized order sets and departmentwide education were crucial in the success of ERAS. Additional research is needed to evaluate the impact of unique components of ERAS in order to optimize this pathway.”
The researchers had no disclosures.
SOURCE: Ruymann K et al. Am J Obstet Gynecol. 2020 Jan;222(1):S212, Abstract 315.
GRAPEVINE, TEX. – An enhanced recovery after surgery (ERAS) pathway for cesarean delivery decreased postoperative opioid usage by 62% in one health care organization, researchers reported at the Pregnancy Meeting. The protocol incorporates a stepwise approach to pain control with no scheduled postoperative opioids.
Abington Jefferson Health, which includes two hospitals in Pennsylvania, implemented an ERAS pathway for all cesarean deliveries in October 2018. Kathryn Ruymann, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Dr. Ruymann is an obstetrics and gynecology resident at Abington Jefferson Health.
Prior to the ERAS protocol, 99%-100% of patients took an opioid during the postoperative period. “With ERAS, 26% of patients never took an opioid during the postop period,” Dr. Ruymann and her associates reported. “Pain scores decreased with ERAS for postoperative days 1-3 and remained unchanged on day 4.”
One in 300 opioid-naive patients who receives opioids after cesarean delivery becomes a persistent user, one study has shown (Am J Obstet Gynecol. 2016 Sep; 215(3):353.e1-18). “ERAS pathways integrate evidence-based interventions before, during, and after surgery to optimize outcomes, specifically to decrease postoperative opioid use,” the researchers said.
While other surgical fields have adopted ERAS pathways, more research is needed in obstetrics, said Dr. Ruymann. More than 4,500 women deliver at Abington Jefferson Health each year, and about a third undergo cesarean deliveries.
The organization’s ERAS pathway incorporates preoperative education, fasting guidelines, and intraoperative analgesia, nausea prophylaxis, and antimicrobial therapy. Under the new protocol, postoperative analgesia includes scheduled administration of nonopioid medications, including celecoxib and acetaminophen. In addition, patients may take 5-10 mg of oxycodone orally every 4 hours as needed, and hydromorphone 0.4 mg IV as needed may be used for refractory pain. In addition, patients should resume eating as soon as tolerated and be out of bed within 4 hours after surgery, according to the protocol. Postoperative management of pruritus and instructions on how to wean off opioids at home are among the other elements of the enhanced recovery plan.
To examine postoperative opioid usage before and after implementation of the ERAS pathway, the investigators conducted a retrospective cohort study of 316 women who underwent cesarean delivery 3 months before the start of the ERAS pathway and 267 who underwent cesarean delivery 3 months after. The researchers used an application developed in Qlik Sense, a data analytics platform, to calculate opioid usage.
Mean postoperative opioid use decreased by 62%. The reduction in opioid use remained 8 months after starting the ERAS pathway.
“An ERAS pathway for [cesarean delivery] decreases postoperative opioid usage by integrating a multimodal stepwise approach to pain control and recovery,” the researchers said. “Standardized order sets and departmentwide education were crucial in the success of ERAS. Additional research is needed to evaluate the impact of unique components of ERAS in order to optimize this pathway.”
The researchers had no disclosures.
SOURCE: Ruymann K et al. Am J Obstet Gynecol. 2020 Jan;222(1):S212, Abstract 315.
GRAPEVINE, TEX. – An enhanced recovery after surgery (ERAS) pathway for cesarean delivery decreased postoperative opioid usage by 62% in one health care organization, researchers reported at the Pregnancy Meeting. The protocol incorporates a stepwise approach to pain control with no scheduled postoperative opioids.
Abington Jefferson Health, which includes two hospitals in Pennsylvania, implemented an ERAS pathway for all cesarean deliveries in October 2018. Kathryn Ruymann, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Dr. Ruymann is an obstetrics and gynecology resident at Abington Jefferson Health.
Prior to the ERAS protocol, 99%-100% of patients took an opioid during the postoperative period. “With ERAS, 26% of patients never took an opioid during the postop period,” Dr. Ruymann and her associates reported. “Pain scores decreased with ERAS for postoperative days 1-3 and remained unchanged on day 4.”
One in 300 opioid-naive patients who receives opioids after cesarean delivery becomes a persistent user, one study has shown (Am J Obstet Gynecol. 2016 Sep; 215(3):353.e1-18). “ERAS pathways integrate evidence-based interventions before, during, and after surgery to optimize outcomes, specifically to decrease postoperative opioid use,” the researchers said.
While other surgical fields have adopted ERAS pathways, more research is needed in obstetrics, said Dr. Ruymann. More than 4,500 women deliver at Abington Jefferson Health each year, and about a third undergo cesarean deliveries.
The organization’s ERAS pathway incorporates preoperative education, fasting guidelines, and intraoperative analgesia, nausea prophylaxis, and antimicrobial therapy. Under the new protocol, postoperative analgesia includes scheduled administration of nonopioid medications, including celecoxib and acetaminophen. In addition, patients may take 5-10 mg of oxycodone orally every 4 hours as needed, and hydromorphone 0.4 mg IV as needed may be used for refractory pain. In addition, patients should resume eating as soon as tolerated and be out of bed within 4 hours after surgery, according to the protocol. Postoperative management of pruritus and instructions on how to wean off opioids at home are among the other elements of the enhanced recovery plan.
To examine postoperative opioid usage before and after implementation of the ERAS pathway, the investigators conducted a retrospective cohort study of 316 women who underwent cesarean delivery 3 months before the start of the ERAS pathway and 267 who underwent cesarean delivery 3 months after. The researchers used an application developed in Qlik Sense, a data analytics platform, to calculate opioid usage.
Mean postoperative opioid use decreased by 62%. The reduction in opioid use remained 8 months after starting the ERAS pathway.
“An ERAS pathway for [cesarean delivery] decreases postoperative opioid usage by integrating a multimodal stepwise approach to pain control and recovery,” the researchers said. “Standardized order sets and departmentwide education were crucial in the success of ERAS. Additional research is needed to evaluate the impact of unique components of ERAS in order to optimize this pathway.”
The researchers had no disclosures.
SOURCE: Ruymann K et al. Am J Obstet Gynecol. 2020 Jan;222(1):S212, Abstract 315.
REPORTING FROM THE PREGNANCY MEETING
Salpingectomy adds little time and no complications to cesarean delivery
GRAPEVINE, TEXAS – Performing a total salpingectomy at the time of cesarean delivery added just over 6 minutes of operative time, compared with cesarean delivery and conventional sterilization, according to a recent systematic review and meta-analysis.
Although surgery took a little longer with salpingectomy, there was no increase in surgical complications, Jared Roeckner, MD, said in an interview at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine. “Total salpingectomy could provide an effective means of contraception and reduce the risk of future ovarian cancer,” he said.
Dr. Roeckner, a maternal-fetal medicine fellow at the University of South Florida, Tampa, explained in an interview that the systematic review and meta-analysis comprised 11 studies and included 320,443 women who received salpingectomy or standard sterilization methods. Eight cohort studies and three randomized controlled trials were included in the analysis, which was presented in a poster session at the meeting and in a simultaneous publication in Obstetrics & Gynecology.
The review’s results, wrote Dr. Roeckner and colleagues, “suggest total salpingectomy should be offered to women interested in ovarian cancer risk-reduction interventions [who] plan to undergo sterilization at the time of cesarean delivery.”
The eight cohort studies included 7,303 women. In these studies, women who received total salpingectomy at the time of cesarean delivery had operative time – defined as the time from skin incision to skin closure – 6.3 minutes longer than women who received a standard sterilization method (95% confidence interval, 3.5-9.1). The difference in duration of procedure for the three randomized controlled trials was not statistically significant between the two procedures.
Dr. Roeckner and colleagues noted that two of the randomized controlled trials reported times for the sterilization procedures. One study found a duration of 5.6 minutes for salpingectomy with a bipolar device and 6.1 minutes for tubal interruption; the other study compared salpingectomy with suture ligation and tubal interruption, finding operative times of 18.5 and 6.9 minutes, respectively.
In addition to the primary outcome of operative time, Dr. Roeckner and colleagues looked at rates of a variety of complications. These included transfusion, estimated blood loss, change in hemoglobin, wound infection, internal organ damage, readmission, reoperation, and length of stay. Salpingectomy was not associated with higher rates of any of these complications.
“Our main finding was that salpingectomy at the time of cesarean delivery may be associated with a small increase in operative time, but it doesn’t appear to be associated with an increased rate of surgical complications,” the researchers wrote.
One concern that’s been raised about the strategy of salpingectomy is the possibility of reduction of ovarian reserve related to decreased blood supply to the ovaries. However, noted Dr. Roeckner and coinvestigators, other studies have not shown decreases in anti-Müllerian hormone levels or other real-world signals for reduced ovarian reserve.
It’s true, the investigators acknowledged, that there is no possibility for reanastomosis and future fertility with salpingectomy. However, they observed that if the possibility for future fertility exists, conventional tubal ligation should not be performed.
Despite the thoroughness of the review and the investigators’ emphasis on adhering to best practices for systematic reviews and meta-analysis, they acknowledged that there were few studies, which resulted in some difficulties with statistical power. Still, they said, “there does not appear to be a trend toward increased complications among the salpingectomy cohort.”
Dr. Roeckner reported no outside sources of funding and no conflicts of interest.
SOURCE: Roeckner J et al. Pregnancy Meeting, Abstract P180; Obstet Gynecol. 2020 Feb;135:3:550-7.
GRAPEVINE, TEXAS – Performing a total salpingectomy at the time of cesarean delivery added just over 6 minutes of operative time, compared with cesarean delivery and conventional sterilization, according to a recent systematic review and meta-analysis.
Although surgery took a little longer with salpingectomy, there was no increase in surgical complications, Jared Roeckner, MD, said in an interview at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine. “Total salpingectomy could provide an effective means of contraception and reduce the risk of future ovarian cancer,” he said.
Dr. Roeckner, a maternal-fetal medicine fellow at the University of South Florida, Tampa, explained in an interview that the systematic review and meta-analysis comprised 11 studies and included 320,443 women who received salpingectomy or standard sterilization methods. Eight cohort studies and three randomized controlled trials were included in the analysis, which was presented in a poster session at the meeting and in a simultaneous publication in Obstetrics & Gynecology.
The review’s results, wrote Dr. Roeckner and colleagues, “suggest total salpingectomy should be offered to women interested in ovarian cancer risk-reduction interventions [who] plan to undergo sterilization at the time of cesarean delivery.”
The eight cohort studies included 7,303 women. In these studies, women who received total salpingectomy at the time of cesarean delivery had operative time – defined as the time from skin incision to skin closure – 6.3 minutes longer than women who received a standard sterilization method (95% confidence interval, 3.5-9.1). The difference in duration of procedure for the three randomized controlled trials was not statistically significant between the two procedures.
Dr. Roeckner and colleagues noted that two of the randomized controlled trials reported times for the sterilization procedures. One study found a duration of 5.6 minutes for salpingectomy with a bipolar device and 6.1 minutes for tubal interruption; the other study compared salpingectomy with suture ligation and tubal interruption, finding operative times of 18.5 and 6.9 minutes, respectively.
In addition to the primary outcome of operative time, Dr. Roeckner and colleagues looked at rates of a variety of complications. These included transfusion, estimated blood loss, change in hemoglobin, wound infection, internal organ damage, readmission, reoperation, and length of stay. Salpingectomy was not associated with higher rates of any of these complications.
“Our main finding was that salpingectomy at the time of cesarean delivery may be associated with a small increase in operative time, but it doesn’t appear to be associated with an increased rate of surgical complications,” the researchers wrote.
One concern that’s been raised about the strategy of salpingectomy is the possibility of reduction of ovarian reserve related to decreased blood supply to the ovaries. However, noted Dr. Roeckner and coinvestigators, other studies have not shown decreases in anti-Müllerian hormone levels or other real-world signals for reduced ovarian reserve.
It’s true, the investigators acknowledged, that there is no possibility for reanastomosis and future fertility with salpingectomy. However, they observed that if the possibility for future fertility exists, conventional tubal ligation should not be performed.
Despite the thoroughness of the review and the investigators’ emphasis on adhering to best practices for systematic reviews and meta-analysis, they acknowledged that there were few studies, which resulted in some difficulties with statistical power. Still, they said, “there does not appear to be a trend toward increased complications among the salpingectomy cohort.”
Dr. Roeckner reported no outside sources of funding and no conflicts of interest.
SOURCE: Roeckner J et al. Pregnancy Meeting, Abstract P180; Obstet Gynecol. 2020 Feb;135:3:550-7.
GRAPEVINE, TEXAS – Performing a total salpingectomy at the time of cesarean delivery added just over 6 minutes of operative time, compared with cesarean delivery and conventional sterilization, according to a recent systematic review and meta-analysis.
Although surgery took a little longer with salpingectomy, there was no increase in surgical complications, Jared Roeckner, MD, said in an interview at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine. “Total salpingectomy could provide an effective means of contraception and reduce the risk of future ovarian cancer,” he said.
Dr. Roeckner, a maternal-fetal medicine fellow at the University of South Florida, Tampa, explained in an interview that the systematic review and meta-analysis comprised 11 studies and included 320,443 women who received salpingectomy or standard sterilization methods. Eight cohort studies and three randomized controlled trials were included in the analysis, which was presented in a poster session at the meeting and in a simultaneous publication in Obstetrics & Gynecology.
The review’s results, wrote Dr. Roeckner and colleagues, “suggest total salpingectomy should be offered to women interested in ovarian cancer risk-reduction interventions [who] plan to undergo sterilization at the time of cesarean delivery.”
The eight cohort studies included 7,303 women. In these studies, women who received total salpingectomy at the time of cesarean delivery had operative time – defined as the time from skin incision to skin closure – 6.3 minutes longer than women who received a standard sterilization method (95% confidence interval, 3.5-9.1). The difference in duration of procedure for the three randomized controlled trials was not statistically significant between the two procedures.
Dr. Roeckner and colleagues noted that two of the randomized controlled trials reported times for the sterilization procedures. One study found a duration of 5.6 minutes for salpingectomy with a bipolar device and 6.1 minutes for tubal interruption; the other study compared salpingectomy with suture ligation and tubal interruption, finding operative times of 18.5 and 6.9 minutes, respectively.
In addition to the primary outcome of operative time, Dr. Roeckner and colleagues looked at rates of a variety of complications. These included transfusion, estimated blood loss, change in hemoglobin, wound infection, internal organ damage, readmission, reoperation, and length of stay. Salpingectomy was not associated with higher rates of any of these complications.
“Our main finding was that salpingectomy at the time of cesarean delivery may be associated with a small increase in operative time, but it doesn’t appear to be associated with an increased rate of surgical complications,” the researchers wrote.
One concern that’s been raised about the strategy of salpingectomy is the possibility of reduction of ovarian reserve related to decreased blood supply to the ovaries. However, noted Dr. Roeckner and coinvestigators, other studies have not shown decreases in anti-Müllerian hormone levels or other real-world signals for reduced ovarian reserve.
It’s true, the investigators acknowledged, that there is no possibility for reanastomosis and future fertility with salpingectomy. However, they observed that if the possibility for future fertility exists, conventional tubal ligation should not be performed.
Despite the thoroughness of the review and the investigators’ emphasis on adhering to best practices for systematic reviews and meta-analysis, they acknowledged that there were few studies, which resulted in some difficulties with statistical power. Still, they said, “there does not appear to be a trend toward increased complications among the salpingectomy cohort.”
Dr. Roeckner reported no outside sources of funding and no conflicts of interest.
SOURCE: Roeckner J et al. Pregnancy Meeting, Abstract P180; Obstet Gynecol. 2020 Feb;135:3:550-7.
REPORTING FROM THE PREGNANCY MEETING
In gestational diabetes, early postpartum glucose testing is a winner
GRAPEVINE, TEX. – Early postpartum glucose tolerance testing for women with gestational diabetes resulted in a 99% adherence rate, with similar sensitivity and specificity as the currently recommended 4- to 12-week postpartum testing schedule.
“Two-day postpartum glucose tolerance testing has similar diagnostic utility as the 4- to 12-week postpartum glucose tolerance test to identify impaired glucose metabolism and diabetes at 1 year postpartum,” said Erika Werner, MD, speaking at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Overall, 29% of women studied had impaired glucose metabolism at 2 days postpartum, as did 25% in the 4- to 12-weeks postpartum window. At 1 year, that figure was 35%. The number of women meeting diagnostic criteria for diabetes held steady at 4% for all three time points.
The findings warrant “consideration for the 2-day postpartum glucose tolerance test (GTT) as the initial postpartum test for women who have gestational diabetes, with repeat testing at 1 year,” said Dr. Werner, a maternal-fetal medicine physician at Brown University, Providence, R.I.
Glucose testing for women with gestational diabetes mellitus (GDM) is recommended at 4-12 weeks postpartum by both the American Diabetes Association and the American College of Obstetricians and Gynecologists.
Testing can allow detection and treatment of impaired glucose metabolism, seen in 15%-40% of women with a history of GDM. Up to 1 in 20 women with GDM will receive a postpartum diagnosis of type 2 diabetes.
However, fewer than one in five women will actually have postpartum glucose testing, representing a large missed opportunity, said Dr. Werner.
Several factors likely contribute to those screening failures, she added. In addition to the potential for public insurance to lapse at 6 weeks postpartum, the logistical realities and time demands of parenting a newborn are themselves a significant barrier.
“What if we changed the timing?” and shifted glucose testing to the early postpartum days, before hospital discharge, asked Dr. Werner. Several pilot studies had already compared glucose screening in the first few days postpartum with the routine schedule, finding good correlation between the early and routine GTT schedule.
Importantly, the earlier studies achieved an adherence rate of more than 90% for early GTT. By contrast, fewer than half of the participants in the usual-care arms actually returned for postpartum GTT in the 4- to 12-week postpartum window, even under the optimized conditions associated with a medical study.
The single-center prospective cohort study conducted by Dr. Werner and collaborators enrolled 300 women with GDM. Women agreed to participate in glucose tolerance testing as inpatients, at 2 days postpartum, in addition to receiving a GTT between 4 and 12 weeks postpartum, and additional screening that included a glycosylated hemoglobin (HbA1c) test at 1 year postpartum.
The investigators obtained postpartum day 2 GTTs for all but four of the patients. A total of 201 patients returned in the 4- to 12-week postpartum window, and 168 of those participants returned for HbA1c testing at 1 year. Of the 95 patients who didn’t come back for the 4- to 12-week test, 33 did return at 1 year for HbA1c testing.
Dr. Werner and her coinvestigators included adult women who spoke either fluent Spanish or English and had GDM diagnosed by the Carpenter-Coustan criteria, or by having a blood glucose level of 200 mg/dL or more in a 1-hour glucose challenge test.
The early GTT results weren’t shared with patients or their health care providers. For outpatient visits, participants were offered financial incentives and received multiple reminder phone calls and the offer of free transportation.
For the purposes of the study, impaired glucose metabolism was defined as fasting blood glucose of 100 mg/dL or greater, a 2-hour GTT blood glucose level of 140 mg/dL or greater, or HbA1c of 5.7% or greater.
Participants were diagnosed with diabetes if they had a fasting blood glucose of 126 mg/dL or greater, a 2-hour GTT blood glucose level of 200 mg/dL or greater, or HbA1c of 6.5% or greater.
Dr. Werner and colleagues conducted two analyses of their results. In the first, they included only women in both arms who had complete data. In the second analysis, they looked at all women who had data for the 1-year postpartum mark, assuming that interval GTTs were negative for women who were missing these values.
The statistical analysis showed that, for women with complete data, both early and later postpartum GTTs were similar in predicting impaired glucose metabolism at 1 year postpartum (areas under the receiver operating curve [AUC], 0.63 and 0.60, respectively).
For identifying diabetes at 1 year, both early and late testing had high negative predictive value (98% and 99%, respectively), but the later testing strategy had higher sensitivity and specificity, yielding an AUC of 0.83, compared with 0.65 for early testing.
Turning to the second analysis that included all women who had 1-year postpartum HbA1c values, negative predictive values for diabetes were similarly high (98%) for both the early and late testing strategies. For identifying impaired glucose metabolism at 1 year in this group, both the positive and negative predictive value of the early and late strategies were similar.
Patients were about 32 years old at baseline, with a mean body mass index of 31.7 kg/m2. More than half of patients (52.3%) had private insurance, and 22% had GDM in a pregnancy prior to the index pregnancy. Black patients made up about 9% of the study population; 54% of participants were white, and 23% Hispanic. About one-third of patients were nulliparous, and two-thirds had education beyond high school.
During their pregnancies, about 44% of patients managed GDM by diet alone, 40% required insulin, with an additional 1% also requiring an oral agent. The remainder required oral agents alone. Patients delivered at a mean 38.3 weeks gestation, with about 40% receiving cesarean deliveries.
Some of the study’s strengths included its prospective nature, the diverse population recruited, and the fact that participants and providers were both blinded to the 2-day GTT results. Although more than half of participants completed the study – besting the previous pilots – 44% of patients still had incomplete data, noted Dr. Werner.
The American Diabetes Association sponsored the study. Dr. Werner reported no other conflicts of interest.
SOURCE: Werner E et al. SMFM 2020. Abstract 72.
GRAPEVINE, TEX. – Early postpartum glucose tolerance testing for women with gestational diabetes resulted in a 99% adherence rate, with similar sensitivity and specificity as the currently recommended 4- to 12-week postpartum testing schedule.
“Two-day postpartum glucose tolerance testing has similar diagnostic utility as the 4- to 12-week postpartum glucose tolerance test to identify impaired glucose metabolism and diabetes at 1 year postpartum,” said Erika Werner, MD, speaking at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Overall, 29% of women studied had impaired glucose metabolism at 2 days postpartum, as did 25% in the 4- to 12-weeks postpartum window. At 1 year, that figure was 35%. The number of women meeting diagnostic criteria for diabetes held steady at 4% for all three time points.
The findings warrant “consideration for the 2-day postpartum glucose tolerance test (GTT) as the initial postpartum test for women who have gestational diabetes, with repeat testing at 1 year,” said Dr. Werner, a maternal-fetal medicine physician at Brown University, Providence, R.I.
Glucose testing for women with gestational diabetes mellitus (GDM) is recommended at 4-12 weeks postpartum by both the American Diabetes Association and the American College of Obstetricians and Gynecologists.
Testing can allow detection and treatment of impaired glucose metabolism, seen in 15%-40% of women with a history of GDM. Up to 1 in 20 women with GDM will receive a postpartum diagnosis of type 2 diabetes.
However, fewer than one in five women will actually have postpartum glucose testing, representing a large missed opportunity, said Dr. Werner.
Several factors likely contribute to those screening failures, she added. In addition to the potential for public insurance to lapse at 6 weeks postpartum, the logistical realities and time demands of parenting a newborn are themselves a significant barrier.
“What if we changed the timing?” and shifted glucose testing to the early postpartum days, before hospital discharge, asked Dr. Werner. Several pilot studies had already compared glucose screening in the first few days postpartum with the routine schedule, finding good correlation between the early and routine GTT schedule.
Importantly, the earlier studies achieved an adherence rate of more than 90% for early GTT. By contrast, fewer than half of the participants in the usual-care arms actually returned for postpartum GTT in the 4- to 12-week postpartum window, even under the optimized conditions associated with a medical study.
The single-center prospective cohort study conducted by Dr. Werner and collaborators enrolled 300 women with GDM. Women agreed to participate in glucose tolerance testing as inpatients, at 2 days postpartum, in addition to receiving a GTT between 4 and 12 weeks postpartum, and additional screening that included a glycosylated hemoglobin (HbA1c) test at 1 year postpartum.
The investigators obtained postpartum day 2 GTTs for all but four of the patients. A total of 201 patients returned in the 4- to 12-week postpartum window, and 168 of those participants returned for HbA1c testing at 1 year. Of the 95 patients who didn’t come back for the 4- to 12-week test, 33 did return at 1 year for HbA1c testing.
Dr. Werner and her coinvestigators included adult women who spoke either fluent Spanish or English and had GDM diagnosed by the Carpenter-Coustan criteria, or by having a blood glucose level of 200 mg/dL or more in a 1-hour glucose challenge test.
The early GTT results weren’t shared with patients or their health care providers. For outpatient visits, participants were offered financial incentives and received multiple reminder phone calls and the offer of free transportation.
For the purposes of the study, impaired glucose metabolism was defined as fasting blood glucose of 100 mg/dL or greater, a 2-hour GTT blood glucose level of 140 mg/dL or greater, or HbA1c of 5.7% or greater.
Participants were diagnosed with diabetes if they had a fasting blood glucose of 126 mg/dL or greater, a 2-hour GTT blood glucose level of 200 mg/dL or greater, or HbA1c of 6.5% or greater.
Dr. Werner and colleagues conducted two analyses of their results. In the first, they included only women in both arms who had complete data. In the second analysis, they looked at all women who had data for the 1-year postpartum mark, assuming that interval GTTs were negative for women who were missing these values.
The statistical analysis showed that, for women with complete data, both early and later postpartum GTTs were similar in predicting impaired glucose metabolism at 1 year postpartum (areas under the receiver operating curve [AUC], 0.63 and 0.60, respectively).
For identifying diabetes at 1 year, both early and late testing had high negative predictive value (98% and 99%, respectively), but the later testing strategy had higher sensitivity and specificity, yielding an AUC of 0.83, compared with 0.65 for early testing.
Turning to the second analysis that included all women who had 1-year postpartum HbA1c values, negative predictive values for diabetes were similarly high (98%) for both the early and late testing strategies. For identifying impaired glucose metabolism at 1 year in this group, both the positive and negative predictive value of the early and late strategies were similar.
Patients were about 32 years old at baseline, with a mean body mass index of 31.7 kg/m2. More than half of patients (52.3%) had private insurance, and 22% had GDM in a pregnancy prior to the index pregnancy. Black patients made up about 9% of the study population; 54% of participants were white, and 23% Hispanic. About one-third of patients were nulliparous, and two-thirds had education beyond high school.
During their pregnancies, about 44% of patients managed GDM by diet alone, 40% required insulin, with an additional 1% also requiring an oral agent. The remainder required oral agents alone. Patients delivered at a mean 38.3 weeks gestation, with about 40% receiving cesarean deliveries.
Some of the study’s strengths included its prospective nature, the diverse population recruited, and the fact that participants and providers were both blinded to the 2-day GTT results. Although more than half of participants completed the study – besting the previous pilots – 44% of patients still had incomplete data, noted Dr. Werner.
The American Diabetes Association sponsored the study. Dr. Werner reported no other conflicts of interest.
SOURCE: Werner E et al. SMFM 2020. Abstract 72.
GRAPEVINE, TEX. – Early postpartum glucose tolerance testing for women with gestational diabetes resulted in a 99% adherence rate, with similar sensitivity and specificity as the currently recommended 4- to 12-week postpartum testing schedule.
“Two-day postpartum glucose tolerance testing has similar diagnostic utility as the 4- to 12-week postpartum glucose tolerance test to identify impaired glucose metabolism and diabetes at 1 year postpartum,” said Erika Werner, MD, speaking at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Overall, 29% of women studied had impaired glucose metabolism at 2 days postpartum, as did 25% in the 4- to 12-weeks postpartum window. At 1 year, that figure was 35%. The number of women meeting diagnostic criteria for diabetes held steady at 4% for all three time points.
The findings warrant “consideration for the 2-day postpartum glucose tolerance test (GTT) as the initial postpartum test for women who have gestational diabetes, with repeat testing at 1 year,” said Dr. Werner, a maternal-fetal medicine physician at Brown University, Providence, R.I.
Glucose testing for women with gestational diabetes mellitus (GDM) is recommended at 4-12 weeks postpartum by both the American Diabetes Association and the American College of Obstetricians and Gynecologists.
Testing can allow detection and treatment of impaired glucose metabolism, seen in 15%-40% of women with a history of GDM. Up to 1 in 20 women with GDM will receive a postpartum diagnosis of type 2 diabetes.
However, fewer than one in five women will actually have postpartum glucose testing, representing a large missed opportunity, said Dr. Werner.
Several factors likely contribute to those screening failures, she added. In addition to the potential for public insurance to lapse at 6 weeks postpartum, the logistical realities and time demands of parenting a newborn are themselves a significant barrier.
“What if we changed the timing?” and shifted glucose testing to the early postpartum days, before hospital discharge, asked Dr. Werner. Several pilot studies had already compared glucose screening in the first few days postpartum with the routine schedule, finding good correlation between the early and routine GTT schedule.
Importantly, the earlier studies achieved an adherence rate of more than 90% for early GTT. By contrast, fewer than half of the participants in the usual-care arms actually returned for postpartum GTT in the 4- to 12-week postpartum window, even under the optimized conditions associated with a medical study.
The single-center prospective cohort study conducted by Dr. Werner and collaborators enrolled 300 women with GDM. Women agreed to participate in glucose tolerance testing as inpatients, at 2 days postpartum, in addition to receiving a GTT between 4 and 12 weeks postpartum, and additional screening that included a glycosylated hemoglobin (HbA1c) test at 1 year postpartum.
The investigators obtained postpartum day 2 GTTs for all but four of the patients. A total of 201 patients returned in the 4- to 12-week postpartum window, and 168 of those participants returned for HbA1c testing at 1 year. Of the 95 patients who didn’t come back for the 4- to 12-week test, 33 did return at 1 year for HbA1c testing.
Dr. Werner and her coinvestigators included adult women who spoke either fluent Spanish or English and had GDM diagnosed by the Carpenter-Coustan criteria, or by having a blood glucose level of 200 mg/dL or more in a 1-hour glucose challenge test.
The early GTT results weren’t shared with patients or their health care providers. For outpatient visits, participants were offered financial incentives and received multiple reminder phone calls and the offer of free transportation.
For the purposes of the study, impaired glucose metabolism was defined as fasting blood glucose of 100 mg/dL or greater, a 2-hour GTT blood glucose level of 140 mg/dL or greater, or HbA1c of 5.7% or greater.
Participants were diagnosed with diabetes if they had a fasting blood glucose of 126 mg/dL or greater, a 2-hour GTT blood glucose level of 200 mg/dL or greater, or HbA1c of 6.5% or greater.
Dr. Werner and colleagues conducted two analyses of their results. In the first, they included only women in both arms who had complete data. In the second analysis, they looked at all women who had data for the 1-year postpartum mark, assuming that interval GTTs were negative for women who were missing these values.
The statistical analysis showed that, for women with complete data, both early and later postpartum GTTs were similar in predicting impaired glucose metabolism at 1 year postpartum (areas under the receiver operating curve [AUC], 0.63 and 0.60, respectively).
For identifying diabetes at 1 year, both early and late testing had high negative predictive value (98% and 99%, respectively), but the later testing strategy had higher sensitivity and specificity, yielding an AUC of 0.83, compared with 0.65 for early testing.
Turning to the second analysis that included all women who had 1-year postpartum HbA1c values, negative predictive values for diabetes were similarly high (98%) for both the early and late testing strategies. For identifying impaired glucose metabolism at 1 year in this group, both the positive and negative predictive value of the early and late strategies were similar.
Patients were about 32 years old at baseline, with a mean body mass index of 31.7 kg/m2. More than half of patients (52.3%) had private insurance, and 22% had GDM in a pregnancy prior to the index pregnancy. Black patients made up about 9% of the study population; 54% of participants were white, and 23% Hispanic. About one-third of patients were nulliparous, and two-thirds had education beyond high school.
During their pregnancies, about 44% of patients managed GDM by diet alone, 40% required insulin, with an additional 1% also requiring an oral agent. The remainder required oral agents alone. Patients delivered at a mean 38.3 weeks gestation, with about 40% receiving cesarean deliveries.
Some of the study’s strengths included its prospective nature, the diverse population recruited, and the fact that participants and providers were both blinded to the 2-day GTT results. Although more than half of participants completed the study – besting the previous pilots – 44% of patients still had incomplete data, noted Dr. Werner.
The American Diabetes Association sponsored the study. Dr. Werner reported no other conflicts of interest.
SOURCE: Werner E et al. SMFM 2020. Abstract 72.
REPORTING FROM THE PREGNANCY MEETING
Racial disparities persist in preterm birth risk
Education, status are not protective for non-Hispanic black women
GRAPEVINE, TEX. – College education and high socioeconomic status do not erase U.S. racial disparities in birth outcomes, according to a new analysis of all U.S. live births from 2015-2017.
Very early preterm birth – birth before 28 weeks gestational age – was five times more likely to occur in non-Hispanic black women of high socioeconomic status as similarly situated white women, even after statistical adjustment for a host of potentially confounding factors.
Being of non-Hispanic black race was the single strongest predictor of preterm birth (PTB) at less than 28 weeks’ gestation. The adjusted odds ratio (aOR) of 4.99 surpassed an interpregnancy interval under 1 year (aOR, 4.47), chronic hypertension (aOR, 2.84), and prior history of preterm birth (aOR, 2.81).
“Even among college-educated women with private insurance who are not receiving (Women, Infants, and Children support), racial disparities in prematurity persist. These results suggest that factors other than sociodemographics are important in the underlying pathogenesis of PTB and in etiologies of racial disparities,” wrote Jasmine Johnson, MD, and her coauthors in the abstract accompanying the presentation at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The analysis that Dr. Johnson and her coinvestigators used, she explained during her plenary session presentation, still found significantly elevated risks for preterm birth for non-Hispanic black women after accounting for marital status, prior history of preterm birth, tobacco use, an interpregnancy interval of fewer than 12 months, and carrying a male fetus.
“Birth certificates do not inform the lived experiences of one’s self-identified race, and how that experience – or possibly just one’s identification with a particular racial group – may positively or negatively affect their clinical risk of preterm birth,” said Dr. Johnson. “In this study, as in others, race is a social construct. It’s a surrogate for social and societal racism that disproportionately affects birth outcomes of women of color.”
Using non-Hispanic white (NHW) women as a reference, women who described themselves as non-Hispanic black (NHB) had increased odds of preterm birth at 34 and 37 weeks gestation as well. Women identifying as both NHB and NHW had numerically elevated odds for preterm birth at all time points as well, but the odds at 37 weeks didn’t reach statistical significance.
The results were based on a retrospective population-based study of a cohort drawn from the National Vital Statistics birth certificate data of all live births in the United States between 2015 and 2017, explained Dr. Johnson, a maternal-fetal medicine fellow at the University of North Carolina, Chapel Hill. Drawing from a nationally representative sample and having a population-level design drawn were strengths of the study, she said.
Women with singleton pregnancies without anomalies who identified as NHB, NHW, or as both NHB and NHW were included if they also had high socioeconomic status. Including women who identify as both black and white was another strength of the study, Dr. Johnson added.
She explained that, for the purposes of the study, high socioeconomic status was defined as having 16 or more years of education and private insurance, and not receiving WIC benefits.
In addition to the primary outcome measure of preterm birth at fewer than 37 weeks gestation, secondary outcomes included preterm birth at fewer than 34 and fewer than 28 weeks’ gestation, as well as low birthweight (LBW) and very low birthweight (VLBW).
About 11.8 million live births occurred during the study period, and 11.3 million of those were singleton pregnancies without fetal anomaly. After excluding women who did not meet the racial self-identification or socioeconomic status inclusion criteria, the investigators arrived at the final study population of 2,170,688 individuals.
Of those, 2,017,470, or 92.9%, were non-Hispanic white, while 144,612, or 6.7%, were non-Hispanic black. The remaining 8,604 participants, or 0.4%, identified their race as non-Hispanic black and non-Hispanic white.
The groups identified in the study differed significantly in demographic characteristics, Dr. Johnson said. Women in the NHB and NHB + NHW groups were less likely to be married than NHW women – about 75% of the former two groups were married, compared with 92.5% of NHW women. This difference was statistically significant with a P value of .001, as were all the differences Dr. Johnson reported.
Pre-pregnancy body mass index (BMI) was highest in NHB women at 27.1 kg/m sq, followed by NHB = NHW women at 25.7 kg/m sq, with NHW women having the lowest BMI at 23.8 kg/m sq.
Prior preterm birth of 37 weeks’ gestation or less was more common in NHB women and NHB + NHW women, as was an interpregnancy interval of fewer than 12 months.
Chronic hypertension was more than twice as common in NHB women than in either NHB = NHW or NHW women, occurring in 3.9%, 1.8%, and 1.4% of participants, respectively.
Pregestational diabetes was about twice as common in NHB women than NHW women, occurring in 1% and 0.52% of those groups, respectively. Prevalence of pregestational diabetes was intermediate in NHB = NHW women, at 0.72%.
Tobacco use was rare overall, and less common in NHB women than NHB + NHW and NHW women.
In terms of pregnancy characteristics, though 85% of NHB women initiated prenatal care in the first trimester, they were less likely to have done so than either of the other two groups. Few women overall had no prenatal care, but 0.7% of NHB women fell into this category, more than the 0.4% and 0.3% reported for NHB + NHW and NHW women, respectively.
During their pregnancies, NHB women were more likely to develop gestational hypertension and/or pre-eclampsia as well as gestational diabetes than either of the other two groups (7.6% compared with 6% for the other two groups). Of the NHB women, 5.9% developed gestational diabetes, compared with 4.8% of NHB + NHW and 4.8% of NHW women.
Delivering a baby with a birthweight less than the 10th percentile was twice as common for NHB, compared with NHW women (7.2% versus 3.4%). The risk for NHB + NHW women was intermediate, at 4.7%.
Dr. Johnson said she and her team performed further analyses, including using initiation of prenatal care in the first trimester of pregnancy as a surrogate for high socioeconomic status; the association of race and risk for preterm birth persisted.
The study had the usual limitations of using National Vital Statistics data, such as the inability to evaluate underlying etiologies for preterm birth.
However, Dr. Johnson highlighted additional limitations that pertain to the experience of race in 21st century America. “Our definition of high socioeconomic status does not guarantee that all women in this analysis have financial stability,” she said, pointing out that the study’s definition of high socioeconomic status was insensitive to wealth accumulation. She also noted that high educational attainment does not necessarily correlate with high income. Hence, the potential burden of economic stressors could not fully be captured.
The study was supported by the National Institutes of Health. Dr. Johnson reported no conflicts of interest.
SOURCE: Johnson J et al. Obstet Gynecol. 2020 Jan;222(1):S-37-8, Abstract 44.
Education, status are not protective for non-Hispanic black women
Education, status are not protective for non-Hispanic black women
GRAPEVINE, TEX. – College education and high socioeconomic status do not erase U.S. racial disparities in birth outcomes, according to a new analysis of all U.S. live births from 2015-2017.
Very early preterm birth – birth before 28 weeks gestational age – was five times more likely to occur in non-Hispanic black women of high socioeconomic status as similarly situated white women, even after statistical adjustment for a host of potentially confounding factors.
Being of non-Hispanic black race was the single strongest predictor of preterm birth (PTB) at less than 28 weeks’ gestation. The adjusted odds ratio (aOR) of 4.99 surpassed an interpregnancy interval under 1 year (aOR, 4.47), chronic hypertension (aOR, 2.84), and prior history of preterm birth (aOR, 2.81).
“Even among college-educated women with private insurance who are not receiving (Women, Infants, and Children support), racial disparities in prematurity persist. These results suggest that factors other than sociodemographics are important in the underlying pathogenesis of PTB and in etiologies of racial disparities,” wrote Jasmine Johnson, MD, and her coauthors in the abstract accompanying the presentation at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The analysis that Dr. Johnson and her coinvestigators used, she explained during her plenary session presentation, still found significantly elevated risks for preterm birth for non-Hispanic black women after accounting for marital status, prior history of preterm birth, tobacco use, an interpregnancy interval of fewer than 12 months, and carrying a male fetus.
“Birth certificates do not inform the lived experiences of one’s self-identified race, and how that experience – or possibly just one’s identification with a particular racial group – may positively or negatively affect their clinical risk of preterm birth,” said Dr. Johnson. “In this study, as in others, race is a social construct. It’s a surrogate for social and societal racism that disproportionately affects birth outcomes of women of color.”
Using non-Hispanic white (NHW) women as a reference, women who described themselves as non-Hispanic black (NHB) had increased odds of preterm birth at 34 and 37 weeks gestation as well. Women identifying as both NHB and NHW had numerically elevated odds for preterm birth at all time points as well, but the odds at 37 weeks didn’t reach statistical significance.
The results were based on a retrospective population-based study of a cohort drawn from the National Vital Statistics birth certificate data of all live births in the United States between 2015 and 2017, explained Dr. Johnson, a maternal-fetal medicine fellow at the University of North Carolina, Chapel Hill. Drawing from a nationally representative sample and having a population-level design drawn were strengths of the study, she said.
Women with singleton pregnancies without anomalies who identified as NHB, NHW, or as both NHB and NHW were included if they also had high socioeconomic status. Including women who identify as both black and white was another strength of the study, Dr. Johnson added.
She explained that, for the purposes of the study, high socioeconomic status was defined as having 16 or more years of education and private insurance, and not receiving WIC benefits.
In addition to the primary outcome measure of preterm birth at fewer than 37 weeks gestation, secondary outcomes included preterm birth at fewer than 34 and fewer than 28 weeks’ gestation, as well as low birthweight (LBW) and very low birthweight (VLBW).
About 11.8 million live births occurred during the study period, and 11.3 million of those were singleton pregnancies without fetal anomaly. After excluding women who did not meet the racial self-identification or socioeconomic status inclusion criteria, the investigators arrived at the final study population of 2,170,688 individuals.
Of those, 2,017,470, or 92.9%, were non-Hispanic white, while 144,612, or 6.7%, were non-Hispanic black. The remaining 8,604 participants, or 0.4%, identified their race as non-Hispanic black and non-Hispanic white.
The groups identified in the study differed significantly in demographic characteristics, Dr. Johnson said. Women in the NHB and NHB + NHW groups were less likely to be married than NHW women – about 75% of the former two groups were married, compared with 92.5% of NHW women. This difference was statistically significant with a P value of .001, as were all the differences Dr. Johnson reported.
Pre-pregnancy body mass index (BMI) was highest in NHB women at 27.1 kg/m sq, followed by NHB = NHW women at 25.7 kg/m sq, with NHW women having the lowest BMI at 23.8 kg/m sq.
Prior preterm birth of 37 weeks’ gestation or less was more common in NHB women and NHB + NHW women, as was an interpregnancy interval of fewer than 12 months.
Chronic hypertension was more than twice as common in NHB women than in either NHB = NHW or NHW women, occurring in 3.9%, 1.8%, and 1.4% of participants, respectively.
Pregestational diabetes was about twice as common in NHB women than NHW women, occurring in 1% and 0.52% of those groups, respectively. Prevalence of pregestational diabetes was intermediate in NHB = NHW women, at 0.72%.
Tobacco use was rare overall, and less common in NHB women than NHB + NHW and NHW women.
In terms of pregnancy characteristics, though 85% of NHB women initiated prenatal care in the first trimester, they were less likely to have done so than either of the other two groups. Few women overall had no prenatal care, but 0.7% of NHB women fell into this category, more than the 0.4% and 0.3% reported for NHB + NHW and NHW women, respectively.
During their pregnancies, NHB women were more likely to develop gestational hypertension and/or pre-eclampsia as well as gestational diabetes than either of the other two groups (7.6% compared with 6% for the other two groups). Of the NHB women, 5.9% developed gestational diabetes, compared with 4.8% of NHB + NHW and 4.8% of NHW women.
Delivering a baby with a birthweight less than the 10th percentile was twice as common for NHB, compared with NHW women (7.2% versus 3.4%). The risk for NHB + NHW women was intermediate, at 4.7%.
Dr. Johnson said she and her team performed further analyses, including using initiation of prenatal care in the first trimester of pregnancy as a surrogate for high socioeconomic status; the association of race and risk for preterm birth persisted.
The study had the usual limitations of using National Vital Statistics data, such as the inability to evaluate underlying etiologies for preterm birth.
However, Dr. Johnson highlighted additional limitations that pertain to the experience of race in 21st century America. “Our definition of high socioeconomic status does not guarantee that all women in this analysis have financial stability,” she said, pointing out that the study’s definition of high socioeconomic status was insensitive to wealth accumulation. She also noted that high educational attainment does not necessarily correlate with high income. Hence, the potential burden of economic stressors could not fully be captured.
The study was supported by the National Institutes of Health. Dr. Johnson reported no conflicts of interest.
SOURCE: Johnson J et al. Obstet Gynecol. 2020 Jan;222(1):S-37-8, Abstract 44.
GRAPEVINE, TEX. – College education and high socioeconomic status do not erase U.S. racial disparities in birth outcomes, according to a new analysis of all U.S. live births from 2015-2017.
Very early preterm birth – birth before 28 weeks gestational age – was five times more likely to occur in non-Hispanic black women of high socioeconomic status as similarly situated white women, even after statistical adjustment for a host of potentially confounding factors.
Being of non-Hispanic black race was the single strongest predictor of preterm birth (PTB) at less than 28 weeks’ gestation. The adjusted odds ratio (aOR) of 4.99 surpassed an interpregnancy interval under 1 year (aOR, 4.47), chronic hypertension (aOR, 2.84), and prior history of preterm birth (aOR, 2.81).
“Even among college-educated women with private insurance who are not receiving (Women, Infants, and Children support), racial disparities in prematurity persist. These results suggest that factors other than sociodemographics are important in the underlying pathogenesis of PTB and in etiologies of racial disparities,” wrote Jasmine Johnson, MD, and her coauthors in the abstract accompanying the presentation at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The analysis that Dr. Johnson and her coinvestigators used, she explained during her plenary session presentation, still found significantly elevated risks for preterm birth for non-Hispanic black women after accounting for marital status, prior history of preterm birth, tobacco use, an interpregnancy interval of fewer than 12 months, and carrying a male fetus.
“Birth certificates do not inform the lived experiences of one’s self-identified race, and how that experience – or possibly just one’s identification with a particular racial group – may positively or negatively affect their clinical risk of preterm birth,” said Dr. Johnson. “In this study, as in others, race is a social construct. It’s a surrogate for social and societal racism that disproportionately affects birth outcomes of women of color.”
Using non-Hispanic white (NHW) women as a reference, women who described themselves as non-Hispanic black (NHB) had increased odds of preterm birth at 34 and 37 weeks gestation as well. Women identifying as both NHB and NHW had numerically elevated odds for preterm birth at all time points as well, but the odds at 37 weeks didn’t reach statistical significance.
The results were based on a retrospective population-based study of a cohort drawn from the National Vital Statistics birth certificate data of all live births in the United States between 2015 and 2017, explained Dr. Johnson, a maternal-fetal medicine fellow at the University of North Carolina, Chapel Hill. Drawing from a nationally representative sample and having a population-level design drawn were strengths of the study, she said.
Women with singleton pregnancies without anomalies who identified as NHB, NHW, or as both NHB and NHW were included if they also had high socioeconomic status. Including women who identify as both black and white was another strength of the study, Dr. Johnson added.
She explained that, for the purposes of the study, high socioeconomic status was defined as having 16 or more years of education and private insurance, and not receiving WIC benefits.
In addition to the primary outcome measure of preterm birth at fewer than 37 weeks gestation, secondary outcomes included preterm birth at fewer than 34 and fewer than 28 weeks’ gestation, as well as low birthweight (LBW) and very low birthweight (VLBW).
About 11.8 million live births occurred during the study period, and 11.3 million of those were singleton pregnancies without fetal anomaly. After excluding women who did not meet the racial self-identification or socioeconomic status inclusion criteria, the investigators arrived at the final study population of 2,170,688 individuals.
Of those, 2,017,470, or 92.9%, were non-Hispanic white, while 144,612, or 6.7%, were non-Hispanic black. The remaining 8,604 participants, or 0.4%, identified their race as non-Hispanic black and non-Hispanic white.
The groups identified in the study differed significantly in demographic characteristics, Dr. Johnson said. Women in the NHB and NHB + NHW groups were less likely to be married than NHW women – about 75% of the former two groups were married, compared with 92.5% of NHW women. This difference was statistically significant with a P value of .001, as were all the differences Dr. Johnson reported.
Pre-pregnancy body mass index (BMI) was highest in NHB women at 27.1 kg/m sq, followed by NHB = NHW women at 25.7 kg/m sq, with NHW women having the lowest BMI at 23.8 kg/m sq.
Prior preterm birth of 37 weeks’ gestation or less was more common in NHB women and NHB + NHW women, as was an interpregnancy interval of fewer than 12 months.
Chronic hypertension was more than twice as common in NHB women than in either NHB = NHW or NHW women, occurring in 3.9%, 1.8%, and 1.4% of participants, respectively.
Pregestational diabetes was about twice as common in NHB women than NHW women, occurring in 1% and 0.52% of those groups, respectively. Prevalence of pregestational diabetes was intermediate in NHB = NHW women, at 0.72%.
Tobacco use was rare overall, and less common in NHB women than NHB + NHW and NHW women.
In terms of pregnancy characteristics, though 85% of NHB women initiated prenatal care in the first trimester, they were less likely to have done so than either of the other two groups. Few women overall had no prenatal care, but 0.7% of NHB women fell into this category, more than the 0.4% and 0.3% reported for NHB + NHW and NHW women, respectively.
During their pregnancies, NHB women were more likely to develop gestational hypertension and/or pre-eclampsia as well as gestational diabetes than either of the other two groups (7.6% compared with 6% for the other two groups). Of the NHB women, 5.9% developed gestational diabetes, compared with 4.8% of NHB + NHW and 4.8% of NHW women.
Delivering a baby with a birthweight less than the 10th percentile was twice as common for NHB, compared with NHW women (7.2% versus 3.4%). The risk for NHB + NHW women was intermediate, at 4.7%.
Dr. Johnson said she and her team performed further analyses, including using initiation of prenatal care in the first trimester of pregnancy as a surrogate for high socioeconomic status; the association of race and risk for preterm birth persisted.
The study had the usual limitations of using National Vital Statistics data, such as the inability to evaluate underlying etiologies for preterm birth.
However, Dr. Johnson highlighted additional limitations that pertain to the experience of race in 21st century America. “Our definition of high socioeconomic status does not guarantee that all women in this analysis have financial stability,” she said, pointing out that the study’s definition of high socioeconomic status was insensitive to wealth accumulation. She also noted that high educational attainment does not necessarily correlate with high income. Hence, the potential burden of economic stressors could not fully be captured.
The study was supported by the National Institutes of Health. Dr. Johnson reported no conflicts of interest.
SOURCE: Johnson J et al. Obstet Gynecol. 2020 Jan;222(1):S-37-8, Abstract 44.
AT THE PREGNANCY MEETING
Blood pressure categories may signal maternal, perinatal risks
GRAPEVINE, TEX. – Blood pressure categories created by the American College of Cardiology (ACC) and American Heart Association (AHA) in 2017 identify patients with increased risk of preeclampsia, preterm birth, and perinatal death when applied to the first 20 weeks of pregnancy, according to a retrospective study presented at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The absolute risk increases are small, and it is unknown whether treating these patients differently would be beneficial, said study author Martha Tesfalul, MD, maternal-fetal medicine clinical fellow at University of California, San Francisco. Nevertheless, , Dr. Tesfalul said.
Cutoffs with unclear implications
The ACC/AHA in November 2017 reclassified blood pressure in nonpregnant adults, but “implications of these categories in pregnancy are still unclear,” Dr. Tesfalul and colleagues said. Under the guidelines, normal blood pressure is systolic blood pressure less than 120 mm Hg and diastolic blood pressure less than 80 mm Hg. Elevated blood pressure is defined as systolic blood pressure between 120 and 129 mm Hg and diastolic blood pressure less than 80 mm Hg. Stage 1 hypertension is systolic blood pressure between 130 and 139 mm Hg or diastolic blood pressure between 80 and 89 mm Hg. And stage 2 hypertension is systolic blood pressure of at least 140 mm Hg or diastolic blood pressure of at least 90 mm Hg.
For the present analysis, the researchers retrospectively compared obstetric and perinatal outcomes for approximately 6,000 pregnancies at an academic center for which they had at least one blood pressure measurement prior to 20 weeks. The highest measurement was used to identify women with normal blood pressure, elevated blood pressure, or stage 1 hypertension according to the 2017 thresholds.
The researchers included singleton pregnancies with delivery between January 2014 and October 2017. They excluded patients with a prior diagnosis of chronic hypertension, autoimmune or chronic renal disease, or fetal anomalies. They examined rates of gestational hypertension, preeclampsia, preterm birth, neonatal intensive care admission, and perinatal death.
Adjusted relative risks
Dr. Tesfalul and colleagues identified about 3,500 pregnancies with normal blood pressure, more than 1,300 pregnancies with elevated blood pressure, and nearly 1,100 pregnancies with stage 1 hypertension.
After adjusting for relevant covariates – maternal age, nulliparity, race, body mass index, in vitro fertilization, tobacco use, pregestational diabetes, and aspirin use – elevated blood pressure and stage 1 hypertension were associated with a higher risk of preeclampsia and severe preeclampsia, relative to normal blood pressure. The proportion of patients with preeclampsia was 5.7% in the normal blood pressure group, 11.7% in the elevated blood pressure group (adjusted relative risk, 1.8), and 15% in the stage 1 hypertension group (adjusted RR, 2.1). The proportion with preeclampsia with severe features was 3.1% in the normal blood pressure group, 5.7% in the elevated blood pressure group (adjusted RR, 1.6), and 6.8% in the stage 1 hypertension group (adjusted RR, 1.8).
In addition, stage 1 hypertension, compared with normal blood pressure, was associated with increased odds of preterm birth at less than 37 weeks (7.9% vs. 5.1%; adjusted RR, 1.4) and perinatal death (0.7% vs. 0.4%; adjusted RR, 2.8).
“Patients with elevated blood pressure and stage 1 hypertension prior to 20 weeks are at increased risk of adverse outcomes,” the authors concluded. “Further research [is] needed to determine optimal care of patients with elevated blood pressure and stage 1 hypertension in pregnancy.”
Dr. Tesfalul receives support from the Foundation for SMFM.
SOURCE: Tesfalul M et al. Am J Obstet Gynecol. 2020 Jan;222(1):S92-3, Abstract 119.
GRAPEVINE, TEX. – Blood pressure categories created by the American College of Cardiology (ACC) and American Heart Association (AHA) in 2017 identify patients with increased risk of preeclampsia, preterm birth, and perinatal death when applied to the first 20 weeks of pregnancy, according to a retrospective study presented at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The absolute risk increases are small, and it is unknown whether treating these patients differently would be beneficial, said study author Martha Tesfalul, MD, maternal-fetal medicine clinical fellow at University of California, San Francisco. Nevertheless, , Dr. Tesfalul said.
Cutoffs with unclear implications
The ACC/AHA in November 2017 reclassified blood pressure in nonpregnant adults, but “implications of these categories in pregnancy are still unclear,” Dr. Tesfalul and colleagues said. Under the guidelines, normal blood pressure is systolic blood pressure less than 120 mm Hg and diastolic blood pressure less than 80 mm Hg. Elevated blood pressure is defined as systolic blood pressure between 120 and 129 mm Hg and diastolic blood pressure less than 80 mm Hg. Stage 1 hypertension is systolic blood pressure between 130 and 139 mm Hg or diastolic blood pressure between 80 and 89 mm Hg. And stage 2 hypertension is systolic blood pressure of at least 140 mm Hg or diastolic blood pressure of at least 90 mm Hg.
For the present analysis, the researchers retrospectively compared obstetric and perinatal outcomes for approximately 6,000 pregnancies at an academic center for which they had at least one blood pressure measurement prior to 20 weeks. The highest measurement was used to identify women with normal blood pressure, elevated blood pressure, or stage 1 hypertension according to the 2017 thresholds.
The researchers included singleton pregnancies with delivery between January 2014 and October 2017. They excluded patients with a prior diagnosis of chronic hypertension, autoimmune or chronic renal disease, or fetal anomalies. They examined rates of gestational hypertension, preeclampsia, preterm birth, neonatal intensive care admission, and perinatal death.
Adjusted relative risks
Dr. Tesfalul and colleagues identified about 3,500 pregnancies with normal blood pressure, more than 1,300 pregnancies with elevated blood pressure, and nearly 1,100 pregnancies with stage 1 hypertension.
After adjusting for relevant covariates – maternal age, nulliparity, race, body mass index, in vitro fertilization, tobacco use, pregestational diabetes, and aspirin use – elevated blood pressure and stage 1 hypertension were associated with a higher risk of preeclampsia and severe preeclampsia, relative to normal blood pressure. The proportion of patients with preeclampsia was 5.7% in the normal blood pressure group, 11.7% in the elevated blood pressure group (adjusted relative risk, 1.8), and 15% in the stage 1 hypertension group (adjusted RR, 2.1). The proportion with preeclampsia with severe features was 3.1% in the normal blood pressure group, 5.7% in the elevated blood pressure group (adjusted RR, 1.6), and 6.8% in the stage 1 hypertension group (adjusted RR, 1.8).
In addition, stage 1 hypertension, compared with normal blood pressure, was associated with increased odds of preterm birth at less than 37 weeks (7.9% vs. 5.1%; adjusted RR, 1.4) and perinatal death (0.7% vs. 0.4%; adjusted RR, 2.8).
“Patients with elevated blood pressure and stage 1 hypertension prior to 20 weeks are at increased risk of adverse outcomes,” the authors concluded. “Further research [is] needed to determine optimal care of patients with elevated blood pressure and stage 1 hypertension in pregnancy.”
Dr. Tesfalul receives support from the Foundation for SMFM.
SOURCE: Tesfalul M et al. Am J Obstet Gynecol. 2020 Jan;222(1):S92-3, Abstract 119.
GRAPEVINE, TEX. – Blood pressure categories created by the American College of Cardiology (ACC) and American Heart Association (AHA) in 2017 identify patients with increased risk of preeclampsia, preterm birth, and perinatal death when applied to the first 20 weeks of pregnancy, according to a retrospective study presented at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The absolute risk increases are small, and it is unknown whether treating these patients differently would be beneficial, said study author Martha Tesfalul, MD, maternal-fetal medicine clinical fellow at University of California, San Francisco. Nevertheless, , Dr. Tesfalul said.
Cutoffs with unclear implications
The ACC/AHA in November 2017 reclassified blood pressure in nonpregnant adults, but “implications of these categories in pregnancy are still unclear,” Dr. Tesfalul and colleagues said. Under the guidelines, normal blood pressure is systolic blood pressure less than 120 mm Hg and diastolic blood pressure less than 80 mm Hg. Elevated blood pressure is defined as systolic blood pressure between 120 and 129 mm Hg and diastolic blood pressure less than 80 mm Hg. Stage 1 hypertension is systolic blood pressure between 130 and 139 mm Hg or diastolic blood pressure between 80 and 89 mm Hg. And stage 2 hypertension is systolic blood pressure of at least 140 mm Hg or diastolic blood pressure of at least 90 mm Hg.
For the present analysis, the researchers retrospectively compared obstetric and perinatal outcomes for approximately 6,000 pregnancies at an academic center for which they had at least one blood pressure measurement prior to 20 weeks. The highest measurement was used to identify women with normal blood pressure, elevated blood pressure, or stage 1 hypertension according to the 2017 thresholds.
The researchers included singleton pregnancies with delivery between January 2014 and October 2017. They excluded patients with a prior diagnosis of chronic hypertension, autoimmune or chronic renal disease, or fetal anomalies. They examined rates of gestational hypertension, preeclampsia, preterm birth, neonatal intensive care admission, and perinatal death.
Adjusted relative risks
Dr. Tesfalul and colleagues identified about 3,500 pregnancies with normal blood pressure, more than 1,300 pregnancies with elevated blood pressure, and nearly 1,100 pregnancies with stage 1 hypertension.
After adjusting for relevant covariates – maternal age, nulliparity, race, body mass index, in vitro fertilization, tobacco use, pregestational diabetes, and aspirin use – elevated blood pressure and stage 1 hypertension were associated with a higher risk of preeclampsia and severe preeclampsia, relative to normal blood pressure. The proportion of patients with preeclampsia was 5.7% in the normal blood pressure group, 11.7% in the elevated blood pressure group (adjusted relative risk, 1.8), and 15% in the stage 1 hypertension group (adjusted RR, 2.1). The proportion with preeclampsia with severe features was 3.1% in the normal blood pressure group, 5.7% in the elevated blood pressure group (adjusted RR, 1.6), and 6.8% in the stage 1 hypertension group (adjusted RR, 1.8).
In addition, stage 1 hypertension, compared with normal blood pressure, was associated with increased odds of preterm birth at less than 37 weeks (7.9% vs. 5.1%; adjusted RR, 1.4) and perinatal death (0.7% vs. 0.4%; adjusted RR, 2.8).
“Patients with elevated blood pressure and stage 1 hypertension prior to 20 weeks are at increased risk of adverse outcomes,” the authors concluded. “Further research [is] needed to determine optimal care of patients with elevated blood pressure and stage 1 hypertension in pregnancy.”
Dr. Tesfalul receives support from the Foundation for SMFM.
SOURCE: Tesfalul M et al. Am J Obstet Gynecol. 2020 Jan;222(1):S92-3, Abstract 119.
REPORTING FROM THE PREGNANCY MEETING
Patients remain satisfied despite reduced use of opioids post partum
GRAPEVINE, TEX. – The amount of opioids prescribed post partum may decline over time without affecting levels of pain control satisfaction, according to research presented at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Data from a large center indicate that trends in opioid use significantly declined from 2017 to 2019, but not at the expense of adequate pain control, said Nevert Badreldin, MD, assistant professor of obstetrics and gynecology at Northwestern University in Chicago. Patients consistently reported that they were satisfied with inpatient pain control, while opioid use per inpatient day decreased from about 30 morphine milligram equivalents (MME) to less than 20 MME during that time.
To assess trends in postpartum opioid prescribing, opioid use, and pain control satisfaction, Dr. Badreldin and colleagues evaluated data from a prospective observational study. Their analysis included data from women who used an opioid during postpartum hospitalization between May 2017 and July 2019. The researchers excluded women with NSAID or morphine allergies or recent opioid use, as well as those who received general anesthesia without concurrent neuraxial anesthesia, those who underwent peripartum hysterectomy, and women admitted to the ICU.
The investigators used nonparametric tests of trend to assess the difference over time in the proportion of patients who received an opioid prescription at discharge and in the total MME prescribed post partum.
Of 900 women with inpatient opioid use, 471 agreed to be followed after discharge. In that group, the amount of opioid use per inpatient day significantly declined. In addition, the percentage who received an opioid prescription at discharge significantly declined, as did the total MME prescribed at discharge.
“Both inpatient and outpatient satisfaction with pain control were unchanged,” the researchers reported. “In this population, both the frequency and amount of opioid use in the postpartum period declined from 2017 to 2019, without any change in satisfaction with pain control.”
The study was supported by the Society for Maternal-Fetal Medicine/AMAG 2017 Health Policy Award, and a coauthor received support from the National Institute of Child Health and Human Development.
Source: Badreldin N et al. Am J Obstet Gynecol. 2020 Jan;222(1):S93, Abstract 120.
GRAPEVINE, TEX. – The amount of opioids prescribed post partum may decline over time without affecting levels of pain control satisfaction, according to research presented at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Data from a large center indicate that trends in opioid use significantly declined from 2017 to 2019, but not at the expense of adequate pain control, said Nevert Badreldin, MD, assistant professor of obstetrics and gynecology at Northwestern University in Chicago. Patients consistently reported that they were satisfied with inpatient pain control, while opioid use per inpatient day decreased from about 30 morphine milligram equivalents (MME) to less than 20 MME during that time.
To assess trends in postpartum opioid prescribing, opioid use, and pain control satisfaction, Dr. Badreldin and colleagues evaluated data from a prospective observational study. Their analysis included data from women who used an opioid during postpartum hospitalization between May 2017 and July 2019. The researchers excluded women with NSAID or morphine allergies or recent opioid use, as well as those who received general anesthesia without concurrent neuraxial anesthesia, those who underwent peripartum hysterectomy, and women admitted to the ICU.
The investigators used nonparametric tests of trend to assess the difference over time in the proportion of patients who received an opioid prescription at discharge and in the total MME prescribed post partum.
Of 900 women with inpatient opioid use, 471 agreed to be followed after discharge. In that group, the amount of opioid use per inpatient day significantly declined. In addition, the percentage who received an opioid prescription at discharge significantly declined, as did the total MME prescribed at discharge.
“Both inpatient and outpatient satisfaction with pain control were unchanged,” the researchers reported. “In this population, both the frequency and amount of opioid use in the postpartum period declined from 2017 to 2019, without any change in satisfaction with pain control.”
The study was supported by the Society for Maternal-Fetal Medicine/AMAG 2017 Health Policy Award, and a coauthor received support from the National Institute of Child Health and Human Development.
Source: Badreldin N et al. Am J Obstet Gynecol. 2020 Jan;222(1):S93, Abstract 120.
GRAPEVINE, TEX. – The amount of opioids prescribed post partum may decline over time without affecting levels of pain control satisfaction, according to research presented at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Data from a large center indicate that trends in opioid use significantly declined from 2017 to 2019, but not at the expense of adequate pain control, said Nevert Badreldin, MD, assistant professor of obstetrics and gynecology at Northwestern University in Chicago. Patients consistently reported that they were satisfied with inpatient pain control, while opioid use per inpatient day decreased from about 30 morphine milligram equivalents (MME) to less than 20 MME during that time.
To assess trends in postpartum opioid prescribing, opioid use, and pain control satisfaction, Dr. Badreldin and colleagues evaluated data from a prospective observational study. Their analysis included data from women who used an opioid during postpartum hospitalization between May 2017 and July 2019. The researchers excluded women with NSAID or morphine allergies or recent opioid use, as well as those who received general anesthesia without concurrent neuraxial anesthesia, those who underwent peripartum hysterectomy, and women admitted to the ICU.
The investigators used nonparametric tests of trend to assess the difference over time in the proportion of patients who received an opioid prescription at discharge and in the total MME prescribed post partum.
Of 900 women with inpatient opioid use, 471 agreed to be followed after discharge. In that group, the amount of opioid use per inpatient day significantly declined. In addition, the percentage who received an opioid prescription at discharge significantly declined, as did the total MME prescribed at discharge.
“Both inpatient and outpatient satisfaction with pain control were unchanged,” the researchers reported. “In this population, both the frequency and amount of opioid use in the postpartum period declined from 2017 to 2019, without any change in satisfaction with pain control.”
The study was supported by the Society for Maternal-Fetal Medicine/AMAG 2017 Health Policy Award, and a coauthor received support from the National Institute of Child Health and Human Development.
Source: Badreldin N et al. Am J Obstet Gynecol. 2020 Jan;222(1):S93, Abstract 120.
REPORTING FROM THE PREGNANCY MEETING
Less gestational weight gain seen with metformin
GRAPEVINE, TEX.* – Pregnant women with type 2 diabetes or prediabetes had significantly less gestational weight gain if they had metformin exposure at any point in their pregnancies, with no differences in infant birth weight or postnatal infant hypoglycemia, according to research presented at the meeting sponsored by the Society for Maternal-Fetal Medicine.
In a retrospective single-center review of 284 women without metformin exposure and 227 with metformin exposure in pregnancy, metformin exposure at any point in pregnancy was associated with a significantly greater chance of appropriate – rather than excessive – weight gain.
The relationship held true for the 169 women who had metformin in their first trimester of pregnancy. Here, 69% of women had appropriate weight gain using Institute of Medicine and American College of Obstetricians and Gynecologists standards, compared with 54% of the 282 women who had no metformin exposure (adjusted odds ratio 1.92, P = .003). A further 22% of women receiving metformin in their first trimester of pregnancy lost weight, compared with 9% of women without metformin exposure (aOR 2.11, P = .019). There was no significant difference between the two groups in infant birth weight.
Separately, study author Jacquelyn Adams, MD, and her colleagues analyzed outcomes for the full cohort of 227 women who received metformin at any point in their pregnancy, comparing them again to the 282 women who had not received metformin. Most women (85%) were on 2 g of metformin at the time of delivery. These results again showed a greater likelihood of appropriate weight gain in the metformin group (69%; aOR 1.85; P = .002). Maternal weight loss was seen in 20% of this group (aOR 1.98, P = .018). Infant birth weights were not significantly different between these two groups.
“We found that women who had been on metformin at any point in their pregnancy had more appropriate weight gain and less excessive weight gain,” said Dr. Adams, a maternal-fetal medicine fellow at the University of Wisconsin–Madison. “Actually, some women on metformin had even had a little bit of weight loss, with no difference in their baby’s birth weight. So that’s really exciting, because our starting prepregnancy body mass index was 33-36 [kg/m2], which is considered obese,” she said in an interview.
This is an important finding, said Dr. Adams, because previous work has shown that less weight gain in pregnancy is associated with lower risk for hypertension and preeclampsia, and lower rates of fetal macrosomia.
What about infant outcomes? Dr. Adams said that there were many concerns about metformin: “Would it affect baby outcome? Were those babies more likely to be hypoglycemic? Were they more likely to be growth restricted? Were they more likely to have issues in the NICU? And the answer was really, ‘No.’ ”
“So we can both help these women have appropriate weight gain and not have any negative effects on these babies,” she added.
Specifically, Dr. Adams and her coinvestigators found no significant differences between the groups in gestational age at birth, likelihood of neonatal ICU admission, Apgar scores, neonatal hypoglycemia, respiratory distress syndrome, or fetal death. Fetal growth restriction and anomalies occurred at a low and similar rate between the groups.
Dr. Adams said that she was not surprised to see that metformin was associated with less weight gain in pregnancy, but she was surprised at how highly significant the differences were with metformin use. “Metformin is first-line for diabetes in nonpregnant individuals because it’s associated with things like weight loss, and because of ease of use and lack of hypoglycemia – so I was really hoping to see this kind of result.”
Women receiving metformin were a mean 34 years old, while those who didn’t get metformin were 32 years old, a significant difference. Prepregnancy body mass index also was higher in those receiving metformin, and they were more likely to have a type 2 diabetes diagnosis. A similar proportion of both groups – about two-thirds – were white, and about 20% were Hispanic.
The lower weight gain seen in metformin-takers also might smooth the way post partum, said Dr. Adams. “My perception is that, when these women leave us, they might not have any primary care follow-up; they might not have anybody following their diabetes; and metformin is a very viable way to help them in their life outside of pregnancy.
“Not to mention that all the weight you gain in pregnancy, you do eventually have to lose post partum,” she added, “so having less pregnancy weight gain kind of sets them up for success in their postpregnancy life as well.”
Asked whether these results inform the ongoing question of whether insulin or metformin is the most appropriate first-line treatment for gestational diabetes, Dr. Adams first noted that “there’s a lot of crossover,” pointing out that over 60% of the participants in her study eventually also required insulin.
“It’s a question I would love to address in a head-to-head trial,” she said, adding that questions about metformin’s effects on the placenta and the potential for later deleterious effects require more study.
In her practice, Dr. Adams said that patients generally are discharged with a metformin prescription, and then meet with a diabetes educator 1 week after delivery to assess blood glucose levels and adjust medical management. Following that, a warm hand-off to a primary care practice who can continue management and education is optimal, she said.
In terms of next steps, “We would really love to look at metformin in the postpartum period,” said Dr. Adams. Ideally, future work could look for outcomes that extend beyond the 6- to 8-week postpartum follow-up visit. For example, she said, there are indications that women with insulin insensitivity might benefit from metformin while breastfeeding; it’s also possible that metformin might reduce the risk of postpartum preeclampsia.
Dr. Adams reported that she had no conflicts of interest and no outside sources of funding.
SOURCE: Adams J et al. SMFM 2020, Abstract 335.
*This story was updated 2/10/2020.
GRAPEVINE, TEX.* – Pregnant women with type 2 diabetes or prediabetes had significantly less gestational weight gain if they had metformin exposure at any point in their pregnancies, with no differences in infant birth weight or postnatal infant hypoglycemia, according to research presented at the meeting sponsored by the Society for Maternal-Fetal Medicine.
In a retrospective single-center review of 284 women without metformin exposure and 227 with metformin exposure in pregnancy, metformin exposure at any point in pregnancy was associated with a significantly greater chance of appropriate – rather than excessive – weight gain.
The relationship held true for the 169 women who had metformin in their first trimester of pregnancy. Here, 69% of women had appropriate weight gain using Institute of Medicine and American College of Obstetricians and Gynecologists standards, compared with 54% of the 282 women who had no metformin exposure (adjusted odds ratio 1.92, P = .003). A further 22% of women receiving metformin in their first trimester of pregnancy lost weight, compared with 9% of women without metformin exposure (aOR 2.11, P = .019). There was no significant difference between the two groups in infant birth weight.
Separately, study author Jacquelyn Adams, MD, and her colleagues analyzed outcomes for the full cohort of 227 women who received metformin at any point in their pregnancy, comparing them again to the 282 women who had not received metformin. Most women (85%) were on 2 g of metformin at the time of delivery. These results again showed a greater likelihood of appropriate weight gain in the metformin group (69%; aOR 1.85; P = .002). Maternal weight loss was seen in 20% of this group (aOR 1.98, P = .018). Infant birth weights were not significantly different between these two groups.
“We found that women who had been on metformin at any point in their pregnancy had more appropriate weight gain and less excessive weight gain,” said Dr. Adams, a maternal-fetal medicine fellow at the University of Wisconsin–Madison. “Actually, some women on metformin had even had a little bit of weight loss, with no difference in their baby’s birth weight. So that’s really exciting, because our starting prepregnancy body mass index was 33-36 [kg/m2], which is considered obese,” she said in an interview.
This is an important finding, said Dr. Adams, because previous work has shown that less weight gain in pregnancy is associated with lower risk for hypertension and preeclampsia, and lower rates of fetal macrosomia.
What about infant outcomes? Dr. Adams said that there were many concerns about metformin: “Would it affect baby outcome? Were those babies more likely to be hypoglycemic? Were they more likely to be growth restricted? Were they more likely to have issues in the NICU? And the answer was really, ‘No.’ ”
“So we can both help these women have appropriate weight gain and not have any negative effects on these babies,” she added.
Specifically, Dr. Adams and her coinvestigators found no significant differences between the groups in gestational age at birth, likelihood of neonatal ICU admission, Apgar scores, neonatal hypoglycemia, respiratory distress syndrome, or fetal death. Fetal growth restriction and anomalies occurred at a low and similar rate between the groups.
Dr. Adams said that she was not surprised to see that metformin was associated with less weight gain in pregnancy, but she was surprised at how highly significant the differences were with metformin use. “Metformin is first-line for diabetes in nonpregnant individuals because it’s associated with things like weight loss, and because of ease of use and lack of hypoglycemia – so I was really hoping to see this kind of result.”
Women receiving metformin were a mean 34 years old, while those who didn’t get metformin were 32 years old, a significant difference. Prepregnancy body mass index also was higher in those receiving metformin, and they were more likely to have a type 2 diabetes diagnosis. A similar proportion of both groups – about two-thirds – were white, and about 20% were Hispanic.
The lower weight gain seen in metformin-takers also might smooth the way post partum, said Dr. Adams. “My perception is that, when these women leave us, they might not have any primary care follow-up; they might not have anybody following their diabetes; and metformin is a very viable way to help them in their life outside of pregnancy.
“Not to mention that all the weight you gain in pregnancy, you do eventually have to lose post partum,” she added, “so having less pregnancy weight gain kind of sets them up for success in their postpregnancy life as well.”
Asked whether these results inform the ongoing question of whether insulin or metformin is the most appropriate first-line treatment for gestational diabetes, Dr. Adams first noted that “there’s a lot of crossover,” pointing out that over 60% of the participants in her study eventually also required insulin.
“It’s a question I would love to address in a head-to-head trial,” she said, adding that questions about metformin’s effects on the placenta and the potential for later deleterious effects require more study.
In her practice, Dr. Adams said that patients generally are discharged with a metformin prescription, and then meet with a diabetes educator 1 week after delivery to assess blood glucose levels and adjust medical management. Following that, a warm hand-off to a primary care practice who can continue management and education is optimal, she said.
In terms of next steps, “We would really love to look at metformin in the postpartum period,” said Dr. Adams. Ideally, future work could look for outcomes that extend beyond the 6- to 8-week postpartum follow-up visit. For example, she said, there are indications that women with insulin insensitivity might benefit from metformin while breastfeeding; it’s also possible that metformin might reduce the risk of postpartum preeclampsia.
Dr. Adams reported that she had no conflicts of interest and no outside sources of funding.
SOURCE: Adams J et al. SMFM 2020, Abstract 335.
*This story was updated 2/10/2020.
GRAPEVINE, TEX.* – Pregnant women with type 2 diabetes or prediabetes had significantly less gestational weight gain if they had metformin exposure at any point in their pregnancies, with no differences in infant birth weight or postnatal infant hypoglycemia, according to research presented at the meeting sponsored by the Society for Maternal-Fetal Medicine.
In a retrospective single-center review of 284 women without metformin exposure and 227 with metformin exposure in pregnancy, metformin exposure at any point in pregnancy was associated with a significantly greater chance of appropriate – rather than excessive – weight gain.
The relationship held true for the 169 women who had metformin in their first trimester of pregnancy. Here, 69% of women had appropriate weight gain using Institute of Medicine and American College of Obstetricians and Gynecologists standards, compared with 54% of the 282 women who had no metformin exposure (adjusted odds ratio 1.92, P = .003). A further 22% of women receiving metformin in their first trimester of pregnancy lost weight, compared with 9% of women without metformin exposure (aOR 2.11, P = .019). There was no significant difference between the two groups in infant birth weight.
Separately, study author Jacquelyn Adams, MD, and her colleagues analyzed outcomes for the full cohort of 227 women who received metformin at any point in their pregnancy, comparing them again to the 282 women who had not received metformin. Most women (85%) were on 2 g of metformin at the time of delivery. These results again showed a greater likelihood of appropriate weight gain in the metformin group (69%; aOR 1.85; P = .002). Maternal weight loss was seen in 20% of this group (aOR 1.98, P = .018). Infant birth weights were not significantly different between these two groups.
“We found that women who had been on metformin at any point in their pregnancy had more appropriate weight gain and less excessive weight gain,” said Dr. Adams, a maternal-fetal medicine fellow at the University of Wisconsin–Madison. “Actually, some women on metformin had even had a little bit of weight loss, with no difference in their baby’s birth weight. So that’s really exciting, because our starting prepregnancy body mass index was 33-36 [kg/m2], which is considered obese,” she said in an interview.
This is an important finding, said Dr. Adams, because previous work has shown that less weight gain in pregnancy is associated with lower risk for hypertension and preeclampsia, and lower rates of fetal macrosomia.
What about infant outcomes? Dr. Adams said that there were many concerns about metformin: “Would it affect baby outcome? Were those babies more likely to be hypoglycemic? Were they more likely to be growth restricted? Were they more likely to have issues in the NICU? And the answer was really, ‘No.’ ”
“So we can both help these women have appropriate weight gain and not have any negative effects on these babies,” she added.
Specifically, Dr. Adams and her coinvestigators found no significant differences between the groups in gestational age at birth, likelihood of neonatal ICU admission, Apgar scores, neonatal hypoglycemia, respiratory distress syndrome, or fetal death. Fetal growth restriction and anomalies occurred at a low and similar rate between the groups.
Dr. Adams said that she was not surprised to see that metformin was associated with less weight gain in pregnancy, but she was surprised at how highly significant the differences were with metformin use. “Metformin is first-line for diabetes in nonpregnant individuals because it’s associated with things like weight loss, and because of ease of use and lack of hypoglycemia – so I was really hoping to see this kind of result.”
Women receiving metformin were a mean 34 years old, while those who didn’t get metformin were 32 years old, a significant difference. Prepregnancy body mass index also was higher in those receiving metformin, and they were more likely to have a type 2 diabetes diagnosis. A similar proportion of both groups – about two-thirds – were white, and about 20% were Hispanic.
The lower weight gain seen in metformin-takers also might smooth the way post partum, said Dr. Adams. “My perception is that, when these women leave us, they might not have any primary care follow-up; they might not have anybody following their diabetes; and metformin is a very viable way to help them in their life outside of pregnancy.
“Not to mention that all the weight you gain in pregnancy, you do eventually have to lose post partum,” she added, “so having less pregnancy weight gain kind of sets them up for success in their postpregnancy life as well.”
Asked whether these results inform the ongoing question of whether insulin or metformin is the most appropriate first-line treatment for gestational diabetes, Dr. Adams first noted that “there’s a lot of crossover,” pointing out that over 60% of the participants in her study eventually also required insulin.
“It’s a question I would love to address in a head-to-head trial,” she said, adding that questions about metformin’s effects on the placenta and the potential for later deleterious effects require more study.
In her practice, Dr. Adams said that patients generally are discharged with a metformin prescription, and then meet with a diabetes educator 1 week after delivery to assess blood glucose levels and adjust medical management. Following that, a warm hand-off to a primary care practice who can continue management and education is optimal, she said.
In terms of next steps, “We would really love to look at metformin in the postpartum period,” said Dr. Adams. Ideally, future work could look for outcomes that extend beyond the 6- to 8-week postpartum follow-up visit. For example, she said, there are indications that women with insulin insensitivity might benefit from metformin while breastfeeding; it’s also possible that metformin might reduce the risk of postpartum preeclampsia.
Dr. Adams reported that she had no conflicts of interest and no outside sources of funding.
SOURCE: Adams J et al. SMFM 2020, Abstract 335.
*This story was updated 2/10/2020.
REPORTING FROM THE PREGNANCY MEETING