User login
Combo elicits lasting responses in metastatic melanoma
NATIONAL HARBOR, MD. – The combination of bempegaldesleukin and nivolumab produced durable responses in a phase 1/2 trial of patients with previously untreated metastatic melanoma.
The overall response rate was 53%, and most responders were still in response at a median follow-up of about 19 months. The median progression-free survival was not reached, and the combination was considered well tolerated.
Adi Diab, MD, of the University of Texas MD Anderson Cancer Center, Houston, presented these results from the PIVOT-02 study at the annual meeting of the Society for Immunotherapy of Cancer.
Dr. Diab explained that bempegaldesleukin (bempeg) is a CD122-preferential interleukin-2 pathway agonist, and earlier results from the PIVOT-02 trial showed that adding bempeg to nivolumab can convert baseline tumors from programmed death–ligand 1 (PD-L1) negative to PD-L1 positive (SITC 2018, Abstract O4).
Dr. Diab presented updated results from PIVOT-02 (NCT02983045) in 41 patients with metastatic melanoma who received bempeg plus nivolumab as first-line treatment. The patients had a median age of 63 years (range, 22-80 years) at baseline, and 58.5% were male. Most patients (58.5%) were PD-L1 positive, although PD-L1 status was unknown in 7.3% of patients.
Patients received bempeg at 0.006 mg/kg and nivolumab at 360 mg every 3 weeks. They received a median of nine cycles (range, 1-34), and the median follow-up was 18.6 months.
Efficacy
In the 38 patients who were evaluable for efficacy, the overall response rate was 53% (n = 20), and the complete response rate was 34% (n = 13). The median time to response was 2.0 months, and the median time to complete response was 7.9 months.
Dr. Diab noted that responses were seen regardless of PD-L1 expression at baseline. The response rate was 39% among PD-L1-negative patients, 64% among PD-L1-positive patients, and 33% among patients whose PD-L1 status was unknown.
Dr. Diab also pointed out that responses were durable and deepened over time. The median duration of response was not reached, and 17 of the 20 responders had ongoing responses at last follow-up. The median progression-free survival has not been reached.
Safety
“This combination is safe and tolerable, there’s no overlapping immune-related adverse events, and the most common side effects are grade 1/2 flu-like symptoms,” Dr. Diab said.
The most common grade 1/2 treatment-related adverse events (AEs) were flu-like symptoms (80.5%), rash (70.7%), fatigue (65.9%), pruritus (48.8%), nausea (46.3%), arthralgia (43.9%), decreased appetite (36.6%), and myalgia (36.6%).
Dr. Diab noted that cytokine-related AEs (flu-like symptoms, rash, and pruritus) were easily managed with NSAIDs; decreased with subsequent cycles of treatment; and did not necessitate dose delays, reductions, or discontinuations.
Grade 3/4 treatment-related AEs included two cases of acute kidney injury, two cases of atrial fibrillation, one case of dizziness, one case of dyspnea, one case of hypoxia, one case of hyperglycemia, and one case of hypernatremia.
Five patients discontinued treatment because of related AEs, including cerebrovascular accident, peripheral edema, blood creatinine increase, malaise, and pharyngitis. There were no treatment-related deaths.
Dr. Diab said these results were used to support the recent breakthrough therapy designation granted to bempeg in combination with nivolumab. The results have also prompted a phase 3 trial in which researchers are comparing the combination with nivolumab alone (NCT03635983).
The phase 1/2 trial is sponsored by Nektar Therapeutics in collaboration with Bristol-Myers Squibb. Dr. Diab reported relationships with Nektar, Celgene, CureVac, Idera, and Pfizer.
SOURCE: Diab A et al. SITC 2019, Abstract O35.
NATIONAL HARBOR, MD. – The combination of bempegaldesleukin and nivolumab produced durable responses in a phase 1/2 trial of patients with previously untreated metastatic melanoma.
The overall response rate was 53%, and most responders were still in response at a median follow-up of about 19 months. The median progression-free survival was not reached, and the combination was considered well tolerated.
Adi Diab, MD, of the University of Texas MD Anderson Cancer Center, Houston, presented these results from the PIVOT-02 study at the annual meeting of the Society for Immunotherapy of Cancer.
Dr. Diab explained that bempegaldesleukin (bempeg) is a CD122-preferential interleukin-2 pathway agonist, and earlier results from the PIVOT-02 trial showed that adding bempeg to nivolumab can convert baseline tumors from programmed death–ligand 1 (PD-L1) negative to PD-L1 positive (SITC 2018, Abstract O4).
Dr. Diab presented updated results from PIVOT-02 (NCT02983045) in 41 patients with metastatic melanoma who received bempeg plus nivolumab as first-line treatment. The patients had a median age of 63 years (range, 22-80 years) at baseline, and 58.5% were male. Most patients (58.5%) were PD-L1 positive, although PD-L1 status was unknown in 7.3% of patients.
Patients received bempeg at 0.006 mg/kg and nivolumab at 360 mg every 3 weeks. They received a median of nine cycles (range, 1-34), and the median follow-up was 18.6 months.
Efficacy
In the 38 patients who were evaluable for efficacy, the overall response rate was 53% (n = 20), and the complete response rate was 34% (n = 13). The median time to response was 2.0 months, and the median time to complete response was 7.9 months.
Dr. Diab noted that responses were seen regardless of PD-L1 expression at baseline. The response rate was 39% among PD-L1-negative patients, 64% among PD-L1-positive patients, and 33% among patients whose PD-L1 status was unknown.
Dr. Diab also pointed out that responses were durable and deepened over time. The median duration of response was not reached, and 17 of the 20 responders had ongoing responses at last follow-up. The median progression-free survival has not been reached.
Safety
“This combination is safe and tolerable, there’s no overlapping immune-related adverse events, and the most common side effects are grade 1/2 flu-like symptoms,” Dr. Diab said.
The most common grade 1/2 treatment-related adverse events (AEs) were flu-like symptoms (80.5%), rash (70.7%), fatigue (65.9%), pruritus (48.8%), nausea (46.3%), arthralgia (43.9%), decreased appetite (36.6%), and myalgia (36.6%).
Dr. Diab noted that cytokine-related AEs (flu-like symptoms, rash, and pruritus) were easily managed with NSAIDs; decreased with subsequent cycles of treatment; and did not necessitate dose delays, reductions, or discontinuations.
Grade 3/4 treatment-related AEs included two cases of acute kidney injury, two cases of atrial fibrillation, one case of dizziness, one case of dyspnea, one case of hypoxia, one case of hyperglycemia, and one case of hypernatremia.
Five patients discontinued treatment because of related AEs, including cerebrovascular accident, peripheral edema, blood creatinine increase, malaise, and pharyngitis. There were no treatment-related deaths.
Dr. Diab said these results were used to support the recent breakthrough therapy designation granted to bempeg in combination with nivolumab. The results have also prompted a phase 3 trial in which researchers are comparing the combination with nivolumab alone (NCT03635983).
The phase 1/2 trial is sponsored by Nektar Therapeutics in collaboration with Bristol-Myers Squibb. Dr. Diab reported relationships with Nektar, Celgene, CureVac, Idera, and Pfizer.
SOURCE: Diab A et al. SITC 2019, Abstract O35.
NATIONAL HARBOR, MD. – The combination of bempegaldesleukin and nivolumab produced durable responses in a phase 1/2 trial of patients with previously untreated metastatic melanoma.
The overall response rate was 53%, and most responders were still in response at a median follow-up of about 19 months. The median progression-free survival was not reached, and the combination was considered well tolerated.
Adi Diab, MD, of the University of Texas MD Anderson Cancer Center, Houston, presented these results from the PIVOT-02 study at the annual meeting of the Society for Immunotherapy of Cancer.
Dr. Diab explained that bempegaldesleukin (bempeg) is a CD122-preferential interleukin-2 pathway agonist, and earlier results from the PIVOT-02 trial showed that adding bempeg to nivolumab can convert baseline tumors from programmed death–ligand 1 (PD-L1) negative to PD-L1 positive (SITC 2018, Abstract O4).
Dr. Diab presented updated results from PIVOT-02 (NCT02983045) in 41 patients with metastatic melanoma who received bempeg plus nivolumab as first-line treatment. The patients had a median age of 63 years (range, 22-80 years) at baseline, and 58.5% were male. Most patients (58.5%) were PD-L1 positive, although PD-L1 status was unknown in 7.3% of patients.
Patients received bempeg at 0.006 mg/kg and nivolumab at 360 mg every 3 weeks. They received a median of nine cycles (range, 1-34), and the median follow-up was 18.6 months.
Efficacy
In the 38 patients who were evaluable for efficacy, the overall response rate was 53% (n = 20), and the complete response rate was 34% (n = 13). The median time to response was 2.0 months, and the median time to complete response was 7.9 months.
Dr. Diab noted that responses were seen regardless of PD-L1 expression at baseline. The response rate was 39% among PD-L1-negative patients, 64% among PD-L1-positive patients, and 33% among patients whose PD-L1 status was unknown.
Dr. Diab also pointed out that responses were durable and deepened over time. The median duration of response was not reached, and 17 of the 20 responders had ongoing responses at last follow-up. The median progression-free survival has not been reached.
Safety
“This combination is safe and tolerable, there’s no overlapping immune-related adverse events, and the most common side effects are grade 1/2 flu-like symptoms,” Dr. Diab said.
The most common grade 1/2 treatment-related adverse events (AEs) were flu-like symptoms (80.5%), rash (70.7%), fatigue (65.9%), pruritus (48.8%), nausea (46.3%), arthralgia (43.9%), decreased appetite (36.6%), and myalgia (36.6%).
Dr. Diab noted that cytokine-related AEs (flu-like symptoms, rash, and pruritus) were easily managed with NSAIDs; decreased with subsequent cycles of treatment; and did not necessitate dose delays, reductions, or discontinuations.
Grade 3/4 treatment-related AEs included two cases of acute kidney injury, two cases of atrial fibrillation, one case of dizziness, one case of dyspnea, one case of hypoxia, one case of hyperglycemia, and one case of hypernatremia.
Five patients discontinued treatment because of related AEs, including cerebrovascular accident, peripheral edema, blood creatinine increase, malaise, and pharyngitis. There were no treatment-related deaths.
Dr. Diab said these results were used to support the recent breakthrough therapy designation granted to bempeg in combination with nivolumab. The results have also prompted a phase 3 trial in which researchers are comparing the combination with nivolumab alone (NCT03635983).
The phase 1/2 trial is sponsored by Nektar Therapeutics in collaboration with Bristol-Myers Squibb. Dr. Diab reported relationships with Nektar, Celgene, CureVac, Idera, and Pfizer.
SOURCE: Diab A et al. SITC 2019, Abstract O35.
REPORTING FROM SITC 2019
Will TP53-mutated AML respond to immunotherapy?
NATIONAL HARBOR, MD. – New research has shown increased immune infiltration in patients with TP53-mutated acute myeloid leukemia (AML).
Patients with TP53-mutated AML had higher levels of T-cell infiltration, immune checkpoint molecules, and interferon (IFN)–gamma signaling than patients with wild-type TP53.
These findings may indicate that patients with TP53-mutated AML will respond to T-cell targeting immunotherapies, but more investigation is needed, according to Sergio Rutella, MD, PhD, of Nottingham (England) Trent University.
Dr. Rutella described the findings at the annual meeting of the Society for Immunotherapy of Cancer.
He and his colleagues recently identified subgroups of AML, called “immune infiltrated” and “immune depleted,” that can predict chemotherapy resistance and response to flotetuzumab (ASH 2019, Abstract 460). However, the team has not determined the genetic drivers of immune infiltration in AML.*
With the current study, Dr. Rutella and his colleagues wanted to determine if TP53 mutations are associated with the AML immune milieu and see if TP53-mutated patients might benefit from immunotherapy.
Discovery cohort
The researchers first analyzed 147 patients with non-promyelocytic AML from the Cancer Genome Atlas. In total, 9% of these patients (n = 13) had TP53-mutated AML. The researchers assessed how 45 immune gene and biological activity signatures correlated with prognostic molecular lesions (TP53 mutations, FLT3-ITD, etc.) and clinical outcomes in this cohort.
The data showed that immune subtypes were associated with overall survival (OS). The median OS was 11.8 months in patients with immune-infiltrated AML, 16.4 months in patients with intermediate AML, and 25.8 months in patients with immune-depleted AML.
The inflammatory chemokine score (P = .011), IDO1 score (P = .027), IFN-gamma score (P = .036), and B7H3 score (P = .045) were all significantly associated with OS. In fact, these factors were all better predictors of OS than cytogenetic risk score (P = .049).
The IFN-gamma score, inflammatory chemokine score, and lymphoid score were all significantly higher in TP53-mutated patients than in patients with RUNX1 mutations, NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .05).
Likewise, the tumor inflammation signature score was significantly higher among TP53-mutated patients than among patients with NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .01).
Validation cohort and bone marrow samples
The researchers also looked at data from a validation cohort, which consisted of 140 patients with non-promyelocytic AML in the Beat AML Master Trial. Twelve percent of these patients (n = 17) had TP53 mutations.
Data in this cohort showed that CD3G messenger RNA (mRNA) was significantly higher in TP53-mutated AML than in TP53-wild-type AML (P = .04). The same was true for CD8A mRNA (P = .0002) and GZMB mRNA (P = .0005).
Likewise, IFN-gamma mRNA (P = .0052), IFIT2 mRNA (P = .0064), and IFIT3 mRNA (P = .003) were all significantly higher in patients with TP53-mutated AML.
Lastly, the researchers analyzed gene expression profiles of bone marrow samples from patients with AML, 36 with mutated TP53 and 24 with wild-type TP53.
The team found that IFN-gamma–induced genes (IFNG and IRF1), markers of T-cell infiltration (CD8A and CD3G) and senescence (EOMES, KLRD1, and HRAS), immune checkpoint molecules (IDO1, LAG3, PDL1, and VISTA), effector function molecules (GZMB, GZMK, and GZMM), and proinflammatory cytokines (IL17A and TNF) were all significantly overexpressed in TP53-mutated AML.
Among the top overexpressed genes in TP53-mutated AML were genes associated with IFN signaling and inflammation pathways – IL-33, IL-6, IFN-gamma, OASL, RIPK2, TNFAIP3, CSF1, and PTGER4. The IL-17 and TNF signaling pathways were the most enriched pathways in TP53-mutated AML.
“Our analysis of primary bone marrow samples showed that TP53-mutated samples are enriched in IL-17, TNF, and IFN signaling molecules, and show higher levels of T-cell infiltrations and immune checkpoints relative to their wild-type counterparts,” Dr. Rutella said.
“The in silico analysis indicated that TP53-mutated cases will show higher levels of T-cell infiltration, immune checkpoints, and IFN-gamma signaling, compared with AML subgroups without risk-defining molecular lesions,” he added. “This is speculative. Whether TP53-mutated AML can be amenable to respond to T-cell targeting immunotherapies is still to be determined.”
Dr. Rutella reported research support from NanoString Technologies, MacroGenics, and Kura Oncology.
SOURCE: Rutella S et al. SITC 2019. Abstract O3.
*This article was updated on 11/19/2019.
NATIONAL HARBOR, MD. – New research has shown increased immune infiltration in patients with TP53-mutated acute myeloid leukemia (AML).
Patients with TP53-mutated AML had higher levels of T-cell infiltration, immune checkpoint molecules, and interferon (IFN)–gamma signaling than patients with wild-type TP53.
These findings may indicate that patients with TP53-mutated AML will respond to T-cell targeting immunotherapies, but more investigation is needed, according to Sergio Rutella, MD, PhD, of Nottingham (England) Trent University.
Dr. Rutella described the findings at the annual meeting of the Society for Immunotherapy of Cancer.
He and his colleagues recently identified subgroups of AML, called “immune infiltrated” and “immune depleted,” that can predict chemotherapy resistance and response to flotetuzumab (ASH 2019, Abstract 460). However, the team has not determined the genetic drivers of immune infiltration in AML.*
With the current study, Dr. Rutella and his colleagues wanted to determine if TP53 mutations are associated with the AML immune milieu and see if TP53-mutated patients might benefit from immunotherapy.
Discovery cohort
The researchers first analyzed 147 patients with non-promyelocytic AML from the Cancer Genome Atlas. In total, 9% of these patients (n = 13) had TP53-mutated AML. The researchers assessed how 45 immune gene and biological activity signatures correlated with prognostic molecular lesions (TP53 mutations, FLT3-ITD, etc.) and clinical outcomes in this cohort.
The data showed that immune subtypes were associated with overall survival (OS). The median OS was 11.8 months in patients with immune-infiltrated AML, 16.4 months in patients with intermediate AML, and 25.8 months in patients with immune-depleted AML.
The inflammatory chemokine score (P = .011), IDO1 score (P = .027), IFN-gamma score (P = .036), and B7H3 score (P = .045) were all significantly associated with OS. In fact, these factors were all better predictors of OS than cytogenetic risk score (P = .049).
The IFN-gamma score, inflammatory chemokine score, and lymphoid score were all significantly higher in TP53-mutated patients than in patients with RUNX1 mutations, NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .05).
Likewise, the tumor inflammation signature score was significantly higher among TP53-mutated patients than among patients with NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .01).
Validation cohort and bone marrow samples
The researchers also looked at data from a validation cohort, which consisted of 140 patients with non-promyelocytic AML in the Beat AML Master Trial. Twelve percent of these patients (n = 17) had TP53 mutations.
Data in this cohort showed that CD3G messenger RNA (mRNA) was significantly higher in TP53-mutated AML than in TP53-wild-type AML (P = .04). The same was true for CD8A mRNA (P = .0002) and GZMB mRNA (P = .0005).
Likewise, IFN-gamma mRNA (P = .0052), IFIT2 mRNA (P = .0064), and IFIT3 mRNA (P = .003) were all significantly higher in patients with TP53-mutated AML.
Lastly, the researchers analyzed gene expression profiles of bone marrow samples from patients with AML, 36 with mutated TP53 and 24 with wild-type TP53.
The team found that IFN-gamma–induced genes (IFNG and IRF1), markers of T-cell infiltration (CD8A and CD3G) and senescence (EOMES, KLRD1, and HRAS), immune checkpoint molecules (IDO1, LAG3, PDL1, and VISTA), effector function molecules (GZMB, GZMK, and GZMM), and proinflammatory cytokines (IL17A and TNF) were all significantly overexpressed in TP53-mutated AML.
Among the top overexpressed genes in TP53-mutated AML were genes associated with IFN signaling and inflammation pathways – IL-33, IL-6, IFN-gamma, OASL, RIPK2, TNFAIP3, CSF1, and PTGER4. The IL-17 and TNF signaling pathways were the most enriched pathways in TP53-mutated AML.
“Our analysis of primary bone marrow samples showed that TP53-mutated samples are enriched in IL-17, TNF, and IFN signaling molecules, and show higher levels of T-cell infiltrations and immune checkpoints relative to their wild-type counterparts,” Dr. Rutella said.
“The in silico analysis indicated that TP53-mutated cases will show higher levels of T-cell infiltration, immune checkpoints, and IFN-gamma signaling, compared with AML subgroups without risk-defining molecular lesions,” he added. “This is speculative. Whether TP53-mutated AML can be amenable to respond to T-cell targeting immunotherapies is still to be determined.”
Dr. Rutella reported research support from NanoString Technologies, MacroGenics, and Kura Oncology.
SOURCE: Rutella S et al. SITC 2019. Abstract O3.
*This article was updated on 11/19/2019.
NATIONAL HARBOR, MD. – New research has shown increased immune infiltration in patients with TP53-mutated acute myeloid leukemia (AML).
Patients with TP53-mutated AML had higher levels of T-cell infiltration, immune checkpoint molecules, and interferon (IFN)–gamma signaling than patients with wild-type TP53.
These findings may indicate that patients with TP53-mutated AML will respond to T-cell targeting immunotherapies, but more investigation is needed, according to Sergio Rutella, MD, PhD, of Nottingham (England) Trent University.
Dr. Rutella described the findings at the annual meeting of the Society for Immunotherapy of Cancer.
He and his colleagues recently identified subgroups of AML, called “immune infiltrated” and “immune depleted,” that can predict chemotherapy resistance and response to flotetuzumab (ASH 2019, Abstract 460). However, the team has not determined the genetic drivers of immune infiltration in AML.*
With the current study, Dr. Rutella and his colleagues wanted to determine if TP53 mutations are associated with the AML immune milieu and see if TP53-mutated patients might benefit from immunotherapy.
Discovery cohort
The researchers first analyzed 147 patients with non-promyelocytic AML from the Cancer Genome Atlas. In total, 9% of these patients (n = 13) had TP53-mutated AML. The researchers assessed how 45 immune gene and biological activity signatures correlated with prognostic molecular lesions (TP53 mutations, FLT3-ITD, etc.) and clinical outcomes in this cohort.
The data showed that immune subtypes were associated with overall survival (OS). The median OS was 11.8 months in patients with immune-infiltrated AML, 16.4 months in patients with intermediate AML, and 25.8 months in patients with immune-depleted AML.
The inflammatory chemokine score (P = .011), IDO1 score (P = .027), IFN-gamma score (P = .036), and B7H3 score (P = .045) were all significantly associated with OS. In fact, these factors were all better predictors of OS than cytogenetic risk score (P = .049).
The IFN-gamma score, inflammatory chemokine score, and lymphoid score were all significantly higher in TP53-mutated patients than in patients with RUNX1 mutations, NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .05).
Likewise, the tumor inflammation signature score was significantly higher among TP53-mutated patients than among patients with NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .01).
Validation cohort and bone marrow samples
The researchers also looked at data from a validation cohort, which consisted of 140 patients with non-promyelocytic AML in the Beat AML Master Trial. Twelve percent of these patients (n = 17) had TP53 mutations.
Data in this cohort showed that CD3G messenger RNA (mRNA) was significantly higher in TP53-mutated AML than in TP53-wild-type AML (P = .04). The same was true for CD8A mRNA (P = .0002) and GZMB mRNA (P = .0005).
Likewise, IFN-gamma mRNA (P = .0052), IFIT2 mRNA (P = .0064), and IFIT3 mRNA (P = .003) were all significantly higher in patients with TP53-mutated AML.
Lastly, the researchers analyzed gene expression profiles of bone marrow samples from patients with AML, 36 with mutated TP53 and 24 with wild-type TP53.
The team found that IFN-gamma–induced genes (IFNG and IRF1), markers of T-cell infiltration (CD8A and CD3G) and senescence (EOMES, KLRD1, and HRAS), immune checkpoint molecules (IDO1, LAG3, PDL1, and VISTA), effector function molecules (GZMB, GZMK, and GZMM), and proinflammatory cytokines (IL17A and TNF) were all significantly overexpressed in TP53-mutated AML.
Among the top overexpressed genes in TP53-mutated AML were genes associated with IFN signaling and inflammation pathways – IL-33, IL-6, IFN-gamma, OASL, RIPK2, TNFAIP3, CSF1, and PTGER4. The IL-17 and TNF signaling pathways were the most enriched pathways in TP53-mutated AML.
“Our analysis of primary bone marrow samples showed that TP53-mutated samples are enriched in IL-17, TNF, and IFN signaling molecules, and show higher levels of T-cell infiltrations and immune checkpoints relative to their wild-type counterparts,” Dr. Rutella said.
“The in silico analysis indicated that TP53-mutated cases will show higher levels of T-cell infiltration, immune checkpoints, and IFN-gamma signaling, compared with AML subgroups without risk-defining molecular lesions,” he added. “This is speculative. Whether TP53-mutated AML can be amenable to respond to T-cell targeting immunotherapies is still to be determined.”
Dr. Rutella reported research support from NanoString Technologies, MacroGenics, and Kura Oncology.
SOURCE: Rutella S et al. SITC 2019. Abstract O3.
*This article was updated on 11/19/2019.
REPORTING FROM SITC 2019
Neoantigen vaccine appears safe and active in NSCLC
NATIONAL HARBOR, MD. – Trial results suggest a personalized vaccination approach is feasible and safe, and the vaccine can produce clinical responses in patients with non–small cell lung cancer (NSCLC).
The neoantigen vaccine produced only grade 1 adverse events, yielded responses in patients with epidermal growth factor receptor (EGFR) mutations, and proved particularly effective in patients who were also receiving an EGFR inhibitor.
“EGFR inhibitors seemed to reduce tumor immunosuppression barriers and may enhance antitumor immune responses before and during immunization, suggesting there may be a potential synergy of EGFR with immunotherapies,” Gregory A. Lizee, PhD, of University of Texas MD Anderson Cancer Center, Houston, said at the annual meeting of the Society for Immunotherapy of Cancer.
The research began with an elderly patient who had heavily pretreated NSCLC (Oncoimmunology. 2016;5[12]:e1238539). Dr. Lizee and colleagues used tumor mutational profiling and human leukocyte antigen (HLA) typing to develop a personalized peptide vaccine for the patient. He received the vaccine along with topical imiquimod and had multiple lung tumor nodules regress. However, the patient also had liver metastasis that remained refractory to treatment, and he ultimately died.
To investigate this treatment approach in a larger group, Dr. Lizee and colleagues began a phase 1b trial of patients with advanced NSCLC (ChiCTR-IIR-16009867). As with the prior patient, the researchers designed personalized peptide vaccines for the trial subjects based on mutational profiling of 508 cancer-associated genes and high-resolution HLA typing. The peptides were selected based on nonsynonymous somatic tumor–associated mutations with variant allele frequency greater than 0.04 and the highest predicted neoantigen peptide binding to each patient’s HLA class I and II molecules. The vaccines targeted up to eight independent somatic mutations (mean, 3.75 mutations).
In all, 31 patients provided lung tumor biopsies and peripheral blood for mutational and HLA analyses. The researchers designed 27 personalized neoantigen vaccines, and 24 patients were ultimately vaccinated. This translates to a vaccination rate of 77%, which suggests this treatment approach is feasible, Dr. Lizee said.
Of the 24 vaccinated patients, 18 had adenocarcinoma, and 6 had squamous cell carcinoma. All patients had received multiple prior therapies, including surgery, chemotherapy, radiation, and EGFR inhibitors.
Each patient was vaccinated with a personalized mixture of short and long neoantigen peptides (mean, 9.4 peptides) dissolved in isotonic saline. Patients received at least 12 weekly immunizations and had topical imiquimod applied over the injection site for costimulation through toll-like receptor 7. The 16 patients with EGFR mutations were given the option of continuing on an EGFR inhibitor, and 9 patients elected to do so.
Results
Dr. Lizee said this treatment approach was “very safe,” with only grade 1 treatment-related adverse events. The events were fatigue (n = 2), rash (n = 1), and fever (n = 1).
Seven patients achieved a response after vaccination, and one patient achieved a complete response. All seven responders had EGFR mutations, and four of them were receiving an EGFR inhibitor.
The patients on an EGFR inhibitor had significantly better overall survival than that of EGFR-mutated patients who had stopped taking an EGFR inhibitor – 13.8 months and 7.6 months, respectively (P = .038).
Immune profiling revealed that neoantigen-specific T-cell reactivity was associated with clinical responses. The researchers observed EGFR neoantigen-specific T-cell responses in five responders. In three responders, the strongest response was against a peptide encompassing the L858R driver mutation.
The researchers also found evidence of synergy between EGFR inhibitor therapy and the peptide vaccine. EGFR inhibition caused immunomodulatory pathways in EGFR-mutated cancer cells to favor immune-cell infiltration and HLA-mediated antigen presentation.
“Our mechanistic working model is that, in the circulation, the personalized vaccine increased the T-cell frequency,” Dr. Lizee said. “The EGFR inhibitor increased chemokines and antigen presentation at the tumor site, which then attracted those T cells to migrate to the tumor. Then, recognition of the antigen caused interferon gamma [to increase], which caused, potentially, a feed-forward loop by increasing chemokines and antigen presentation further.”
This research is sponsored by Tianjin Beichen Hospital and funded by Tianjin HengJia Biotechnology Development Co. Ltd. Dr. Lizee disclosed a consulting relationship with Tianjin HengJia Biotechnology Development Co. Ltd.
SOURCE: Lizee G et al. SITC 2019. Abstract O18.
NATIONAL HARBOR, MD. – Trial results suggest a personalized vaccination approach is feasible and safe, and the vaccine can produce clinical responses in patients with non–small cell lung cancer (NSCLC).
The neoantigen vaccine produced only grade 1 adverse events, yielded responses in patients with epidermal growth factor receptor (EGFR) mutations, and proved particularly effective in patients who were also receiving an EGFR inhibitor.
“EGFR inhibitors seemed to reduce tumor immunosuppression barriers and may enhance antitumor immune responses before and during immunization, suggesting there may be a potential synergy of EGFR with immunotherapies,” Gregory A. Lizee, PhD, of University of Texas MD Anderson Cancer Center, Houston, said at the annual meeting of the Society for Immunotherapy of Cancer.
The research began with an elderly patient who had heavily pretreated NSCLC (Oncoimmunology. 2016;5[12]:e1238539). Dr. Lizee and colleagues used tumor mutational profiling and human leukocyte antigen (HLA) typing to develop a personalized peptide vaccine for the patient. He received the vaccine along with topical imiquimod and had multiple lung tumor nodules regress. However, the patient also had liver metastasis that remained refractory to treatment, and he ultimately died.
To investigate this treatment approach in a larger group, Dr. Lizee and colleagues began a phase 1b trial of patients with advanced NSCLC (ChiCTR-IIR-16009867). As with the prior patient, the researchers designed personalized peptide vaccines for the trial subjects based on mutational profiling of 508 cancer-associated genes and high-resolution HLA typing. The peptides were selected based on nonsynonymous somatic tumor–associated mutations with variant allele frequency greater than 0.04 and the highest predicted neoantigen peptide binding to each patient’s HLA class I and II molecules. The vaccines targeted up to eight independent somatic mutations (mean, 3.75 mutations).
In all, 31 patients provided lung tumor biopsies and peripheral blood for mutational and HLA analyses. The researchers designed 27 personalized neoantigen vaccines, and 24 patients were ultimately vaccinated. This translates to a vaccination rate of 77%, which suggests this treatment approach is feasible, Dr. Lizee said.
Of the 24 vaccinated patients, 18 had adenocarcinoma, and 6 had squamous cell carcinoma. All patients had received multiple prior therapies, including surgery, chemotherapy, radiation, and EGFR inhibitors.
Each patient was vaccinated with a personalized mixture of short and long neoantigen peptides (mean, 9.4 peptides) dissolved in isotonic saline. Patients received at least 12 weekly immunizations and had topical imiquimod applied over the injection site for costimulation through toll-like receptor 7. The 16 patients with EGFR mutations were given the option of continuing on an EGFR inhibitor, and 9 patients elected to do so.
Results
Dr. Lizee said this treatment approach was “very safe,” with only grade 1 treatment-related adverse events. The events were fatigue (n = 2), rash (n = 1), and fever (n = 1).
Seven patients achieved a response after vaccination, and one patient achieved a complete response. All seven responders had EGFR mutations, and four of them were receiving an EGFR inhibitor.
The patients on an EGFR inhibitor had significantly better overall survival than that of EGFR-mutated patients who had stopped taking an EGFR inhibitor – 13.8 months and 7.6 months, respectively (P = .038).
Immune profiling revealed that neoantigen-specific T-cell reactivity was associated with clinical responses. The researchers observed EGFR neoantigen-specific T-cell responses in five responders. In three responders, the strongest response was against a peptide encompassing the L858R driver mutation.
The researchers also found evidence of synergy between EGFR inhibitor therapy and the peptide vaccine. EGFR inhibition caused immunomodulatory pathways in EGFR-mutated cancer cells to favor immune-cell infiltration and HLA-mediated antigen presentation.
“Our mechanistic working model is that, in the circulation, the personalized vaccine increased the T-cell frequency,” Dr. Lizee said. “The EGFR inhibitor increased chemokines and antigen presentation at the tumor site, which then attracted those T cells to migrate to the tumor. Then, recognition of the antigen caused interferon gamma [to increase], which caused, potentially, a feed-forward loop by increasing chemokines and antigen presentation further.”
This research is sponsored by Tianjin Beichen Hospital and funded by Tianjin HengJia Biotechnology Development Co. Ltd. Dr. Lizee disclosed a consulting relationship with Tianjin HengJia Biotechnology Development Co. Ltd.
SOURCE: Lizee G et al. SITC 2019. Abstract O18.
NATIONAL HARBOR, MD. – Trial results suggest a personalized vaccination approach is feasible and safe, and the vaccine can produce clinical responses in patients with non–small cell lung cancer (NSCLC).
The neoantigen vaccine produced only grade 1 adverse events, yielded responses in patients with epidermal growth factor receptor (EGFR) mutations, and proved particularly effective in patients who were also receiving an EGFR inhibitor.
“EGFR inhibitors seemed to reduce tumor immunosuppression barriers and may enhance antitumor immune responses before and during immunization, suggesting there may be a potential synergy of EGFR with immunotherapies,” Gregory A. Lizee, PhD, of University of Texas MD Anderson Cancer Center, Houston, said at the annual meeting of the Society for Immunotherapy of Cancer.
The research began with an elderly patient who had heavily pretreated NSCLC (Oncoimmunology. 2016;5[12]:e1238539). Dr. Lizee and colleagues used tumor mutational profiling and human leukocyte antigen (HLA) typing to develop a personalized peptide vaccine for the patient. He received the vaccine along with topical imiquimod and had multiple lung tumor nodules regress. However, the patient also had liver metastasis that remained refractory to treatment, and he ultimately died.
To investigate this treatment approach in a larger group, Dr. Lizee and colleagues began a phase 1b trial of patients with advanced NSCLC (ChiCTR-IIR-16009867). As with the prior patient, the researchers designed personalized peptide vaccines for the trial subjects based on mutational profiling of 508 cancer-associated genes and high-resolution HLA typing. The peptides were selected based on nonsynonymous somatic tumor–associated mutations with variant allele frequency greater than 0.04 and the highest predicted neoantigen peptide binding to each patient’s HLA class I and II molecules. The vaccines targeted up to eight independent somatic mutations (mean, 3.75 mutations).
In all, 31 patients provided lung tumor biopsies and peripheral blood for mutational and HLA analyses. The researchers designed 27 personalized neoantigen vaccines, and 24 patients were ultimately vaccinated. This translates to a vaccination rate of 77%, which suggests this treatment approach is feasible, Dr. Lizee said.
Of the 24 vaccinated patients, 18 had adenocarcinoma, and 6 had squamous cell carcinoma. All patients had received multiple prior therapies, including surgery, chemotherapy, radiation, and EGFR inhibitors.
Each patient was vaccinated with a personalized mixture of short and long neoantigen peptides (mean, 9.4 peptides) dissolved in isotonic saline. Patients received at least 12 weekly immunizations and had topical imiquimod applied over the injection site for costimulation through toll-like receptor 7. The 16 patients with EGFR mutations were given the option of continuing on an EGFR inhibitor, and 9 patients elected to do so.
Results
Dr. Lizee said this treatment approach was “very safe,” with only grade 1 treatment-related adverse events. The events were fatigue (n = 2), rash (n = 1), and fever (n = 1).
Seven patients achieved a response after vaccination, and one patient achieved a complete response. All seven responders had EGFR mutations, and four of them were receiving an EGFR inhibitor.
The patients on an EGFR inhibitor had significantly better overall survival than that of EGFR-mutated patients who had stopped taking an EGFR inhibitor – 13.8 months and 7.6 months, respectively (P = .038).
Immune profiling revealed that neoantigen-specific T-cell reactivity was associated with clinical responses. The researchers observed EGFR neoantigen-specific T-cell responses in five responders. In three responders, the strongest response was against a peptide encompassing the L858R driver mutation.
The researchers also found evidence of synergy between EGFR inhibitor therapy and the peptide vaccine. EGFR inhibition caused immunomodulatory pathways in EGFR-mutated cancer cells to favor immune-cell infiltration and HLA-mediated antigen presentation.
“Our mechanistic working model is that, in the circulation, the personalized vaccine increased the T-cell frequency,” Dr. Lizee said. “The EGFR inhibitor increased chemokines and antigen presentation at the tumor site, which then attracted those T cells to migrate to the tumor. Then, recognition of the antigen caused interferon gamma [to increase], which caused, potentially, a feed-forward loop by increasing chemokines and antigen presentation further.”
This research is sponsored by Tianjin Beichen Hospital and funded by Tianjin HengJia Biotechnology Development Co. Ltd. Dr. Lizee disclosed a consulting relationship with Tianjin HengJia Biotechnology Development Co. Ltd.
SOURCE: Lizee G et al. SITC 2019. Abstract O18.
REPORTING FROM SITC 2019
Combo produces disappointing PFS, promising OS in metastatic colorectal cancer
NATIONAL HARBOR, MD. – An immunochemotherapy regimen produced mixed results in a phase 2 trial of patients with previously untreated metastatic colorectal cancer.
The regimen – avelumab and cetuximab plus oxaliplatin, leucovorin, and 5-fluorouracil (mFOLFOX6) – failed to meet the primary endpoint for progression-free survival (PFS) but was associated with “promising” yet “preliminary” overall survival, according to Joseph Tintelnot, MD, of University Medical Center Hamburg-Eppendorf (Germany).
Dr. Tintelnot presented these results from the AVETUX trial (NCT03174405) at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled 43 patients with previously untreated, metastatic colorectal cancer, and 39 of them had wild-type RAS and BRAF mutations. Among those 39 patients, the median age was 62 years (range, 29-82 years), 13 patients were female, and 36 patients had left-sided tumors.
A total of 30 patients had liver metastasis, 12 had lung metastasis, and 18 had lymph node metastasis. Most patients (n = 36) had microsatellite stable tumors, 2 were microsatellite instability high, and 1 was microsatellite instability low.
Patients received IV cetuximab at 250 mg/m2 over 60-90 minutes (day 1 and 8), with a first dose of 400 mg/m2; mFOLFOX6 according to local standard – IV oxaliplatin at 85 mg/m2 IV (day 1), IV leucovorin at 400 mg/m2 IV (day 1), and IV bolus 5-fluorouracil at 400 mg/m2 (day 1) and IV at 2,400 mg/m2 (days 1-3); and IV avelumab at 10 mg/kg over 60-90 minutes (day 1 from cycle 2 onward).
The median number of treatment cycles was 8 (range, 1-34) for oxaliplatin, 13 (range, 1-35) for 5-fluorouracil, 12 (range, 1-35) for cetuximab, and 16 (range, 0-34) for avelumab. The median duration of cetuximab/avelumab treatment was 5.4 months (range, 0.7-18.4 months).
The study’s primary endpoint was 12-month PFS, and the researchers expected the PFS to rise from 40% to 57%. Unfortunately, the 12-month PFS was 40%, so the primary endpoint was not met.
However, the treatment produced a “very high” overall response rate at 81% (30/37), according to Dr. Tintelnot. A total of 4 patients achieved a complete response, 26 had a partial response, 4 had stable disease, and 3 progressed.
Dr. Tintelnot also noted a “promising” but “preliminary” overall survival rate – 84% at a median follow-up of 16.2 months. He said these results suggest PFS may not be the ideal endpoint for this combination.
Dr. Tintelnot said the combination was safe, with no unexpected toxicities. The most common grade 3-4 adverse events were infection of catheter, device, urinary tract, etc. (32%); abdominal pain, diarrhea, etc. (24%); skin reaction (21%); anemia, blood disorders, and hemolytic-uremic syndrome (18%); administration, infusion-related, and allergic reactions (16%); cognitive disturbance, meningism, syncope, and psychiatric disorders (16%); and peripheral sensory polyneuropathy and paresthesia (16%).
Dr. Tintelnot and colleagues also conducted translational research evaluating programmed death-ligand 1 (PD-L1) expression and serial circulating tumor DNA in patients on this trial.
The team found no clear correlation between PFS and T-cell diversification, tumor-infiltrating lymphocytes, or tumor proportion score. Dr. Tintelnot said this suggests classical predictive factors for PD-1/PD-L1 inhibitor treatment have a limited role with this combination.
The researchers did find that circulating tumor mutations might help predict early relapse with the regimen. The team identified 26 patients with mutations detectable in their blood. There was an immediate decline of circulating tumor mutations after treatment initiation, and reemergence of mutation clones was associated with progression.
Lastly, the researchers found that avelumab, cetuximab, and mFOLFOX6 suppressed the development of epidermal growth factor receptor–resistant subclones. There were no epidermal growth factor receptor mutations detected during follow-up.
This research was sponsored by AIO-Studien-gGmbH. Dr. Tintelnot disclosed no conflicts of interest.
SOURCE: Tintelnot J et al. SITC 2019, Abstract O16.
NATIONAL HARBOR, MD. – An immunochemotherapy regimen produced mixed results in a phase 2 trial of patients with previously untreated metastatic colorectal cancer.
The regimen – avelumab and cetuximab plus oxaliplatin, leucovorin, and 5-fluorouracil (mFOLFOX6) – failed to meet the primary endpoint for progression-free survival (PFS) but was associated with “promising” yet “preliminary” overall survival, according to Joseph Tintelnot, MD, of University Medical Center Hamburg-Eppendorf (Germany).
Dr. Tintelnot presented these results from the AVETUX trial (NCT03174405) at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled 43 patients with previously untreated, metastatic colorectal cancer, and 39 of them had wild-type RAS and BRAF mutations. Among those 39 patients, the median age was 62 years (range, 29-82 years), 13 patients were female, and 36 patients had left-sided tumors.
A total of 30 patients had liver metastasis, 12 had lung metastasis, and 18 had lymph node metastasis. Most patients (n = 36) had microsatellite stable tumors, 2 were microsatellite instability high, and 1 was microsatellite instability low.
Patients received IV cetuximab at 250 mg/m2 over 60-90 minutes (day 1 and 8), with a first dose of 400 mg/m2; mFOLFOX6 according to local standard – IV oxaliplatin at 85 mg/m2 IV (day 1), IV leucovorin at 400 mg/m2 IV (day 1), and IV bolus 5-fluorouracil at 400 mg/m2 (day 1) and IV at 2,400 mg/m2 (days 1-3); and IV avelumab at 10 mg/kg over 60-90 minutes (day 1 from cycle 2 onward).
The median number of treatment cycles was 8 (range, 1-34) for oxaliplatin, 13 (range, 1-35) for 5-fluorouracil, 12 (range, 1-35) for cetuximab, and 16 (range, 0-34) for avelumab. The median duration of cetuximab/avelumab treatment was 5.4 months (range, 0.7-18.4 months).
The study’s primary endpoint was 12-month PFS, and the researchers expected the PFS to rise from 40% to 57%. Unfortunately, the 12-month PFS was 40%, so the primary endpoint was not met.
However, the treatment produced a “very high” overall response rate at 81% (30/37), according to Dr. Tintelnot. A total of 4 patients achieved a complete response, 26 had a partial response, 4 had stable disease, and 3 progressed.
Dr. Tintelnot also noted a “promising” but “preliminary” overall survival rate – 84% at a median follow-up of 16.2 months. He said these results suggest PFS may not be the ideal endpoint for this combination.
Dr. Tintelnot said the combination was safe, with no unexpected toxicities. The most common grade 3-4 adverse events were infection of catheter, device, urinary tract, etc. (32%); abdominal pain, diarrhea, etc. (24%); skin reaction (21%); anemia, blood disorders, and hemolytic-uremic syndrome (18%); administration, infusion-related, and allergic reactions (16%); cognitive disturbance, meningism, syncope, and psychiatric disorders (16%); and peripheral sensory polyneuropathy and paresthesia (16%).
Dr. Tintelnot and colleagues also conducted translational research evaluating programmed death-ligand 1 (PD-L1) expression and serial circulating tumor DNA in patients on this trial.
The team found no clear correlation between PFS and T-cell diversification, tumor-infiltrating lymphocytes, or tumor proportion score. Dr. Tintelnot said this suggests classical predictive factors for PD-1/PD-L1 inhibitor treatment have a limited role with this combination.
The researchers did find that circulating tumor mutations might help predict early relapse with the regimen. The team identified 26 patients with mutations detectable in their blood. There was an immediate decline of circulating tumor mutations after treatment initiation, and reemergence of mutation clones was associated with progression.
Lastly, the researchers found that avelumab, cetuximab, and mFOLFOX6 suppressed the development of epidermal growth factor receptor–resistant subclones. There were no epidermal growth factor receptor mutations detected during follow-up.
This research was sponsored by AIO-Studien-gGmbH. Dr. Tintelnot disclosed no conflicts of interest.
SOURCE: Tintelnot J et al. SITC 2019, Abstract O16.
NATIONAL HARBOR, MD. – An immunochemotherapy regimen produced mixed results in a phase 2 trial of patients with previously untreated metastatic colorectal cancer.
The regimen – avelumab and cetuximab plus oxaliplatin, leucovorin, and 5-fluorouracil (mFOLFOX6) – failed to meet the primary endpoint for progression-free survival (PFS) but was associated with “promising” yet “preliminary” overall survival, according to Joseph Tintelnot, MD, of University Medical Center Hamburg-Eppendorf (Germany).
Dr. Tintelnot presented these results from the AVETUX trial (NCT03174405) at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled 43 patients with previously untreated, metastatic colorectal cancer, and 39 of them had wild-type RAS and BRAF mutations. Among those 39 patients, the median age was 62 years (range, 29-82 years), 13 patients were female, and 36 patients had left-sided tumors.
A total of 30 patients had liver metastasis, 12 had lung metastasis, and 18 had lymph node metastasis. Most patients (n = 36) had microsatellite stable tumors, 2 were microsatellite instability high, and 1 was microsatellite instability low.
Patients received IV cetuximab at 250 mg/m2 over 60-90 minutes (day 1 and 8), with a first dose of 400 mg/m2; mFOLFOX6 according to local standard – IV oxaliplatin at 85 mg/m2 IV (day 1), IV leucovorin at 400 mg/m2 IV (day 1), and IV bolus 5-fluorouracil at 400 mg/m2 (day 1) and IV at 2,400 mg/m2 (days 1-3); and IV avelumab at 10 mg/kg over 60-90 minutes (day 1 from cycle 2 onward).
The median number of treatment cycles was 8 (range, 1-34) for oxaliplatin, 13 (range, 1-35) for 5-fluorouracil, 12 (range, 1-35) for cetuximab, and 16 (range, 0-34) for avelumab. The median duration of cetuximab/avelumab treatment was 5.4 months (range, 0.7-18.4 months).
The study’s primary endpoint was 12-month PFS, and the researchers expected the PFS to rise from 40% to 57%. Unfortunately, the 12-month PFS was 40%, so the primary endpoint was not met.
However, the treatment produced a “very high” overall response rate at 81% (30/37), according to Dr. Tintelnot. A total of 4 patients achieved a complete response, 26 had a partial response, 4 had stable disease, and 3 progressed.
Dr. Tintelnot also noted a “promising” but “preliminary” overall survival rate – 84% at a median follow-up of 16.2 months. He said these results suggest PFS may not be the ideal endpoint for this combination.
Dr. Tintelnot said the combination was safe, with no unexpected toxicities. The most common grade 3-4 adverse events were infection of catheter, device, urinary tract, etc. (32%); abdominal pain, diarrhea, etc. (24%); skin reaction (21%); anemia, blood disorders, and hemolytic-uremic syndrome (18%); administration, infusion-related, and allergic reactions (16%); cognitive disturbance, meningism, syncope, and psychiatric disorders (16%); and peripheral sensory polyneuropathy and paresthesia (16%).
Dr. Tintelnot and colleagues also conducted translational research evaluating programmed death-ligand 1 (PD-L1) expression and serial circulating tumor DNA in patients on this trial.
The team found no clear correlation between PFS and T-cell diversification, tumor-infiltrating lymphocytes, or tumor proportion score. Dr. Tintelnot said this suggests classical predictive factors for PD-1/PD-L1 inhibitor treatment have a limited role with this combination.
The researchers did find that circulating tumor mutations might help predict early relapse with the regimen. The team identified 26 patients with mutations detectable in their blood. There was an immediate decline of circulating tumor mutations after treatment initiation, and reemergence of mutation clones was associated with progression.
Lastly, the researchers found that avelumab, cetuximab, and mFOLFOX6 suppressed the development of epidermal growth factor receptor–resistant subclones. There were no epidermal growth factor receptor mutations detected during follow-up.
This research was sponsored by AIO-Studien-gGmbH. Dr. Tintelnot disclosed no conflicts of interest.
SOURCE: Tintelnot J et al. SITC 2019, Abstract O16.
REPORTING FROM SITC 2019
Armored CAR T cells elicit responses in NHL patients
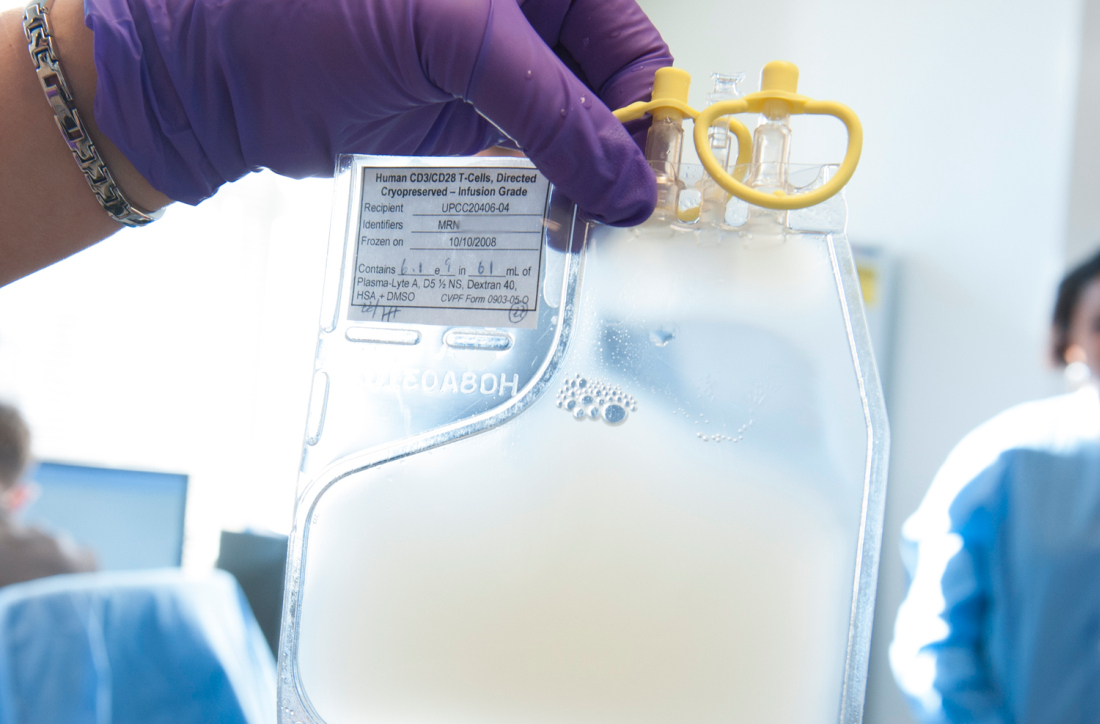
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
REPORTING FROM SITC 2019
Combo shows promise for checkpoint inhibitor-refractory urothelial carcinoma
NATIONAL HARBOR, MD. – Sitravatinib may “restore or enhance” the activity of anti-PD-1 therapy in patients with checkpoint inhibitor–refractory urothelial carcinoma, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
Clinical activity was observed with combination sitravatinib and nivolumab in patients with urothelial carcinoma who had disease progression on or after an immune checkpoint inhibitor and were previously treated with platinum-based chemotherapy.
“Up until a few years ago, the only therapies we had [for urothelial carcinoma] were cytotoxic, platinum-based chemotherapies,” said Pavlos Msaouel, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston.
“Thankfully, since 2016, immune checkpoint therapy has become part of our toolbox. But even with single-agent, approved immune checkpoint therapies, anti-PD-1/anti-PD-L1, the response rates are still low, around 20%, and durable responses are only seen in a subset of patients. So we have to do better, if possible, potentially by combining immune checkpoint therapies with other immunotherapies such as sitravatinib.”
Dr. Msaouel explained that sitravatinib inhibits a spectrum of related receptor tyrosine kinases, including TAM family receptors (TYRO3, Axl, and Mer), split family receptors (VEGFR2/PDGFR and c-KIT), and c-Met. Researchers are investigating sitravatinib in combination with nivolumab in a phase 2 trial of patients with urothelial carcinoma (NCT03606174). Dr. Msaouel presented results from one cohort on this trial – 33 patients who had previously received platinum-based chemotherapy and a PD-1/PD-L1 inhibitor.
At baseline, the patients’ median age was 68 years (range, 47-83 years), and 70% were male. Patients had metastatic (n = 30) or locally advanced (n = 3) disease. They had received a median of two (range, one to four) prior systemic therapies.
For this study, patients received oral sitravatinib at 120 mg daily and intravenous nivolumab at 240 mg every 2 weeks or 480 mg every 4 weeks on continuous 28-day cycles. Tumor assessments were performed every 8 weeks.
Results
Of the 22 patients evaluable for efficacy, 1 patient achieved a complete response, 5 had a partial response, 15 had stable disease, and 1 progressed. Eight patients had tumor regression greater than 30%.
Treatment duration exceeded 26 weeks in six patients. Nine patients, including four responders, were still on study at the data cutoff in mid-October.
“This ongoing trial continues to show promising clinical activity, including tumor regression and prolonged duration on treatment,” Dr. Msaouel said.
He added that combination sitravatinib and nivolumab has “an acceptable side effect profile, with manageable adverse events.”
Common treatment-related adverse events, in all 33 patients, were fatigue (58%), diarrhea (48%), decreased appetite (33%), dysphonia (33%), nausea (33%), and alanine aminotransferase increase (21%).
Grade 3 treatment-related adverse events included fatigue (12%), hypertension (12%), diarrhea (9%), lipase increase (9%), decreased appetite (3%), and palmar-plantar erythrodysesthesia syndrome (3%). There were no grade 4 or 5 treatment-related events.
Mirati Therapeutics sponsored the trial. Dr. Msaouel disclosed relationships with Mirati, Bristol-Myers Squibb, Exelixis, Pfizer, and Takeda.
SOURCE: Msaouel P et al. SITC 2019. Abstract O23.
NATIONAL HARBOR, MD. – Sitravatinib may “restore or enhance” the activity of anti-PD-1 therapy in patients with checkpoint inhibitor–refractory urothelial carcinoma, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
Clinical activity was observed with combination sitravatinib and nivolumab in patients with urothelial carcinoma who had disease progression on or after an immune checkpoint inhibitor and were previously treated with platinum-based chemotherapy.
“Up until a few years ago, the only therapies we had [for urothelial carcinoma] were cytotoxic, platinum-based chemotherapies,” said Pavlos Msaouel, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston.
“Thankfully, since 2016, immune checkpoint therapy has become part of our toolbox. But even with single-agent, approved immune checkpoint therapies, anti-PD-1/anti-PD-L1, the response rates are still low, around 20%, and durable responses are only seen in a subset of patients. So we have to do better, if possible, potentially by combining immune checkpoint therapies with other immunotherapies such as sitravatinib.”
Dr. Msaouel explained that sitravatinib inhibits a spectrum of related receptor tyrosine kinases, including TAM family receptors (TYRO3, Axl, and Mer), split family receptors (VEGFR2/PDGFR and c-KIT), and c-Met. Researchers are investigating sitravatinib in combination with nivolumab in a phase 2 trial of patients with urothelial carcinoma (NCT03606174). Dr. Msaouel presented results from one cohort on this trial – 33 patients who had previously received platinum-based chemotherapy and a PD-1/PD-L1 inhibitor.
At baseline, the patients’ median age was 68 years (range, 47-83 years), and 70% were male. Patients had metastatic (n = 30) or locally advanced (n = 3) disease. They had received a median of two (range, one to four) prior systemic therapies.
For this study, patients received oral sitravatinib at 120 mg daily and intravenous nivolumab at 240 mg every 2 weeks or 480 mg every 4 weeks on continuous 28-day cycles. Tumor assessments were performed every 8 weeks.
Results
Of the 22 patients evaluable for efficacy, 1 patient achieved a complete response, 5 had a partial response, 15 had stable disease, and 1 progressed. Eight patients had tumor regression greater than 30%.
Treatment duration exceeded 26 weeks in six patients. Nine patients, including four responders, were still on study at the data cutoff in mid-October.
“This ongoing trial continues to show promising clinical activity, including tumor regression and prolonged duration on treatment,” Dr. Msaouel said.
He added that combination sitravatinib and nivolumab has “an acceptable side effect profile, with manageable adverse events.”
Common treatment-related adverse events, in all 33 patients, were fatigue (58%), diarrhea (48%), decreased appetite (33%), dysphonia (33%), nausea (33%), and alanine aminotransferase increase (21%).
Grade 3 treatment-related adverse events included fatigue (12%), hypertension (12%), diarrhea (9%), lipase increase (9%), decreased appetite (3%), and palmar-plantar erythrodysesthesia syndrome (3%). There were no grade 4 or 5 treatment-related events.
Mirati Therapeutics sponsored the trial. Dr. Msaouel disclosed relationships with Mirati, Bristol-Myers Squibb, Exelixis, Pfizer, and Takeda.
SOURCE: Msaouel P et al. SITC 2019. Abstract O23.
NATIONAL HARBOR, MD. – Sitravatinib may “restore or enhance” the activity of anti-PD-1 therapy in patients with checkpoint inhibitor–refractory urothelial carcinoma, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
Clinical activity was observed with combination sitravatinib and nivolumab in patients with urothelial carcinoma who had disease progression on or after an immune checkpoint inhibitor and were previously treated with platinum-based chemotherapy.
“Up until a few years ago, the only therapies we had [for urothelial carcinoma] were cytotoxic, platinum-based chemotherapies,” said Pavlos Msaouel, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston.
“Thankfully, since 2016, immune checkpoint therapy has become part of our toolbox. But even with single-agent, approved immune checkpoint therapies, anti-PD-1/anti-PD-L1, the response rates are still low, around 20%, and durable responses are only seen in a subset of patients. So we have to do better, if possible, potentially by combining immune checkpoint therapies with other immunotherapies such as sitravatinib.”
Dr. Msaouel explained that sitravatinib inhibits a spectrum of related receptor tyrosine kinases, including TAM family receptors (TYRO3, Axl, and Mer), split family receptors (VEGFR2/PDGFR and c-KIT), and c-Met. Researchers are investigating sitravatinib in combination with nivolumab in a phase 2 trial of patients with urothelial carcinoma (NCT03606174). Dr. Msaouel presented results from one cohort on this trial – 33 patients who had previously received platinum-based chemotherapy and a PD-1/PD-L1 inhibitor.
At baseline, the patients’ median age was 68 years (range, 47-83 years), and 70% were male. Patients had metastatic (n = 30) or locally advanced (n = 3) disease. They had received a median of two (range, one to four) prior systemic therapies.
For this study, patients received oral sitravatinib at 120 mg daily and intravenous nivolumab at 240 mg every 2 weeks or 480 mg every 4 weeks on continuous 28-day cycles. Tumor assessments were performed every 8 weeks.
Results
Of the 22 patients evaluable for efficacy, 1 patient achieved a complete response, 5 had a partial response, 15 had stable disease, and 1 progressed. Eight patients had tumor regression greater than 30%.
Treatment duration exceeded 26 weeks in six patients. Nine patients, including four responders, were still on study at the data cutoff in mid-October.
“This ongoing trial continues to show promising clinical activity, including tumor regression and prolonged duration on treatment,” Dr. Msaouel said.
He added that combination sitravatinib and nivolumab has “an acceptable side effect profile, with manageable adverse events.”
Common treatment-related adverse events, in all 33 patients, were fatigue (58%), diarrhea (48%), decreased appetite (33%), dysphonia (33%), nausea (33%), and alanine aminotransferase increase (21%).
Grade 3 treatment-related adverse events included fatigue (12%), hypertension (12%), diarrhea (9%), lipase increase (9%), decreased appetite (3%), and palmar-plantar erythrodysesthesia syndrome (3%). There were no grade 4 or 5 treatment-related events.
Mirati Therapeutics sponsored the trial. Dr. Msaouel disclosed relationships with Mirati, Bristol-Myers Squibb, Exelixis, Pfizer, and Takeda.
SOURCE: Msaouel P et al. SITC 2019. Abstract O23.
REPORTING FROM SITC 2019
TLR9 agonist may overcome resistance to anti–PD-1 therapy in melanoma
NATIONAL HARBOR, MD. – A TLR9 agonist called CMP-001 can reverse resistance to anti–programmed death-1 (PD-1) therapy in patients with melanoma, a phase 1 trial suggests.
Combination CMP-001 and pembrolizumab produced durable responses in patients who had progressed on prior anti–PD-1 therapy, and the combination was considered well tolerated.
CMP-001 is a CpG-A TLR9 agonist packaged in a viruslike particle, John Kirkwood, MD, of University of Pittsburgh Medical Center, explained in a late-breaking abstract at the annual meeting of the Society for Immunotherapy of Cancer. CMP-001 activates tumor-associated plasmacytoid dendritic cells and induces systemic tumor-specific CD8+ T-cell responses.
Dr. Kirkwood and associates are investigating CMP-001, given alone or in combination with pembrolizumab, in a phase 1 trial (NCT02680184) of patients with metastatic or unresectable melanoma who are refractory to anti–PD-1 therapy.
Data were presented on 144 patients who received CMP-001 in combination with pembrolizumab. About 40% of patients (39.6%) had elevated lactate dehydrogenase at baseline, and 32.6% had BRAF mutations.
All patients had received prior anti–PD-1 therapy alone (75%) and/or in combination (50%). For most patients (93.1%), their last response to anti–PD-1 therapy was progression.
For this study, the patients received intratumoral CMP-001 injections at a range of doses (1 mg, 3 mg, 5 mg, 7.5 mg, and 10 mg). CMP-001 was given weekly for either 2 weeks or 7 weeks, then every 3 weeks until discontinuation. There were two different formulations of CMP-001 given – 0.01% polysorbate 20 (PS20; n = 83) and 0.00167% PS20 (n = 61).
Safety
“CMP-001 in combination with pembrolizumab is very well tolerated, with no apparent increase in autoimmune toxicities associated with anti–PD-1,” Dr. Kirkwood said.
The most common treatment-related adverse events were flulike symptoms, including chills (72%), pyrexia (56%), fatigue (51%), nausea (45%), vomiting (29%), and headache (28%). Another common event was injection-site pain (28%).
The most common grade 3 adverse events were hypotension (n = 9) and hypertension (n = 7). Grade 4 events included hypotension, aspartate aminotransferase increase, and alanine aminotransferase increase (n = 1 for all). There were no grade 5 events.
Six patients discontinued treatment because of adverse events.
Response
The overall response rate was 25% (21/83) among patients who received the 0.01% PS20 formulation of CMP-001 and 11.5% (7/61) among patients who received the 0.00167% PS20 formulation.
Responses were similar in injected and noninjected target lesions. The median duration of response has not been reached at a median follow-up of 16.9 months.
“Intratumoral CMP-001 reverses resistance to anti–PD-1 in patients who have progressed on prior anti–PD-1 therapy,” Dr. Kirkwood said, adding that these data support further clinical development of CMP-001.
The research is sponsored by Checkmate Pharmaceuticals. Dr. Kirkwood disclosed relationships with Amgen, BMS, Immunocore, Iovance, Novartis, Elsevier, Castle, Merck, and Checkmate.
SOURCE: Kirkwood J et al. SITC 2019, Abstract O85.
NATIONAL HARBOR, MD. – A TLR9 agonist called CMP-001 can reverse resistance to anti–programmed death-1 (PD-1) therapy in patients with melanoma, a phase 1 trial suggests.
Combination CMP-001 and pembrolizumab produced durable responses in patients who had progressed on prior anti–PD-1 therapy, and the combination was considered well tolerated.
CMP-001 is a CpG-A TLR9 agonist packaged in a viruslike particle, John Kirkwood, MD, of University of Pittsburgh Medical Center, explained in a late-breaking abstract at the annual meeting of the Society for Immunotherapy of Cancer. CMP-001 activates tumor-associated plasmacytoid dendritic cells and induces systemic tumor-specific CD8+ T-cell responses.
Dr. Kirkwood and associates are investigating CMP-001, given alone or in combination with pembrolizumab, in a phase 1 trial (NCT02680184) of patients with metastatic or unresectable melanoma who are refractory to anti–PD-1 therapy.
Data were presented on 144 patients who received CMP-001 in combination with pembrolizumab. About 40% of patients (39.6%) had elevated lactate dehydrogenase at baseline, and 32.6% had BRAF mutations.
All patients had received prior anti–PD-1 therapy alone (75%) and/or in combination (50%). For most patients (93.1%), their last response to anti–PD-1 therapy was progression.
For this study, the patients received intratumoral CMP-001 injections at a range of doses (1 mg, 3 mg, 5 mg, 7.5 mg, and 10 mg). CMP-001 was given weekly for either 2 weeks or 7 weeks, then every 3 weeks until discontinuation. There were two different formulations of CMP-001 given – 0.01% polysorbate 20 (PS20; n = 83) and 0.00167% PS20 (n = 61).
Safety
“CMP-001 in combination with pembrolizumab is very well tolerated, with no apparent increase in autoimmune toxicities associated with anti–PD-1,” Dr. Kirkwood said.
The most common treatment-related adverse events were flulike symptoms, including chills (72%), pyrexia (56%), fatigue (51%), nausea (45%), vomiting (29%), and headache (28%). Another common event was injection-site pain (28%).
The most common grade 3 adverse events were hypotension (n = 9) and hypertension (n = 7). Grade 4 events included hypotension, aspartate aminotransferase increase, and alanine aminotransferase increase (n = 1 for all). There were no grade 5 events.
Six patients discontinued treatment because of adverse events.
Response
The overall response rate was 25% (21/83) among patients who received the 0.01% PS20 formulation of CMP-001 and 11.5% (7/61) among patients who received the 0.00167% PS20 formulation.
Responses were similar in injected and noninjected target lesions. The median duration of response has not been reached at a median follow-up of 16.9 months.
“Intratumoral CMP-001 reverses resistance to anti–PD-1 in patients who have progressed on prior anti–PD-1 therapy,” Dr. Kirkwood said, adding that these data support further clinical development of CMP-001.
The research is sponsored by Checkmate Pharmaceuticals. Dr. Kirkwood disclosed relationships with Amgen, BMS, Immunocore, Iovance, Novartis, Elsevier, Castle, Merck, and Checkmate.
SOURCE: Kirkwood J et al. SITC 2019, Abstract O85.
NATIONAL HARBOR, MD. – A TLR9 agonist called CMP-001 can reverse resistance to anti–programmed death-1 (PD-1) therapy in patients with melanoma, a phase 1 trial suggests.
Combination CMP-001 and pembrolizumab produced durable responses in patients who had progressed on prior anti–PD-1 therapy, and the combination was considered well tolerated.
CMP-001 is a CpG-A TLR9 agonist packaged in a viruslike particle, John Kirkwood, MD, of University of Pittsburgh Medical Center, explained in a late-breaking abstract at the annual meeting of the Society for Immunotherapy of Cancer. CMP-001 activates tumor-associated plasmacytoid dendritic cells and induces systemic tumor-specific CD8+ T-cell responses.
Dr. Kirkwood and associates are investigating CMP-001, given alone or in combination with pembrolizumab, in a phase 1 trial (NCT02680184) of patients with metastatic or unresectable melanoma who are refractory to anti–PD-1 therapy.
Data were presented on 144 patients who received CMP-001 in combination with pembrolizumab. About 40% of patients (39.6%) had elevated lactate dehydrogenase at baseline, and 32.6% had BRAF mutations.
All patients had received prior anti–PD-1 therapy alone (75%) and/or in combination (50%). For most patients (93.1%), their last response to anti–PD-1 therapy was progression.
For this study, the patients received intratumoral CMP-001 injections at a range of doses (1 mg, 3 mg, 5 mg, 7.5 mg, and 10 mg). CMP-001 was given weekly for either 2 weeks or 7 weeks, then every 3 weeks until discontinuation. There were two different formulations of CMP-001 given – 0.01% polysorbate 20 (PS20; n = 83) and 0.00167% PS20 (n = 61).
Safety
“CMP-001 in combination with pembrolizumab is very well tolerated, with no apparent increase in autoimmune toxicities associated with anti–PD-1,” Dr. Kirkwood said.
The most common treatment-related adverse events were flulike symptoms, including chills (72%), pyrexia (56%), fatigue (51%), nausea (45%), vomiting (29%), and headache (28%). Another common event was injection-site pain (28%).
The most common grade 3 adverse events were hypotension (n = 9) and hypertension (n = 7). Grade 4 events included hypotension, aspartate aminotransferase increase, and alanine aminotransferase increase (n = 1 for all). There were no grade 5 events.
Six patients discontinued treatment because of adverse events.
Response
The overall response rate was 25% (21/83) among patients who received the 0.01% PS20 formulation of CMP-001 and 11.5% (7/61) among patients who received the 0.00167% PS20 formulation.
Responses were similar in injected and noninjected target lesions. The median duration of response has not been reached at a median follow-up of 16.9 months.
“Intratumoral CMP-001 reverses resistance to anti–PD-1 in patients who have progressed on prior anti–PD-1 therapy,” Dr. Kirkwood said, adding that these data support further clinical development of CMP-001.
The research is sponsored by Checkmate Pharmaceuticals. Dr. Kirkwood disclosed relationships with Amgen, BMS, Immunocore, Iovance, Novartis, Elsevier, Castle, Merck, and Checkmate.
SOURCE: Kirkwood J et al. SITC 2019, Abstract O85.
REPORTING FROM SITC 2019
Molecule exhibits activity in heavily pretreated, HER2-positive solid tumors
NATIONAL HARBOR, MD – PRS-343, a 4-1BB/HER2 bispecific molecule, has demonstrated safety and antitumor activity in patients with heavily pretreated, HER2-positive solid tumors, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
In a phase 1 trial of 18 evaluable patients, PRS-343 produced partial responses in 2 patients and enabled 8 patients to maintain stable disease. PRS-343 was considered well tolerated at all doses and schedules tested.
“PRS-343 is a bispecific construct targeting HER2 as well as 4-1BB,” said Geoffrey Y. Ku, MD, of Memorial Sloan Kettering Cancer Center in New York. “The HER2 component of the molecule localizes it into the tumor microenvironment of any HER2-positive cells. If the density of the HER2 protein is high enough, that facilitates cross-linkage of 4-1BB.
“4-1BB is an immune agonist that’s present in activated T cells, and cross-linkage helps to improve T-cell exhaustion and is also critical for T-cell expansion. The idea is that, by localizing 4-1BB activation to the tumor microenvironment, we can avoid some of the systemic toxicities associated with naked 4-1BB antibodies,” Dr. Ku added.
The ongoing, phase 1 trial of PRS-343 (NCT03330561) has enrolled 53 patients with a range of HER2-positive malignancies. To be eligible, patients must have progressed on standard therapy or have a tumor for which no standard therapy is available.
The most common diagnosis among enrolled patients is gastroesophageal cancer (n = 19), followed by breast cancer (n = 14), gynecologic cancers (n = 6), colorectal cancer (n = 5), and other malignancies.
The patients’ median age at baseline was 61 years (range, 29-92 years), and a majority were female (62%). Most patients (79%) had received three or more prior lines of therapy, including anti-HER2 treatments. Breast cancer patients had received a median of four anti-HER2 treatments, and gastric cancer patients had received a median of two.
The patients have been treated with PRS-343 at 11 dose levels, ranging from 0.0005 mg/kg to 8 mg/kg, given every 3 weeks. The highest dose, 8 mg/kg, was also given every 2 weeks.
Treatment-related adverse events (TRAEs) included infusion-related reactions (9%), fatigue (9%), chills (6%), flushing (6%), nausea (6%), diarrhea (6%), vomiting (5%), and noncardiac chest pain (4%).
“This was an extremely well-tolerated drug,” Dr. Ku said. “Out of 111 TRAEs, only a tiny proportion were grade 3, and toxicities mostly clustered around infusion-related reactions, constitutional symptoms, as well as gastrointestinal symptoms.”
Grade 3 TRAEs included infusion-related reactions (2%), fatigue (1%), flushing (3%), and noncardiac chest pain (1%). There were no grade 4-5 TRAEs.
At the data cutoff (Oct. 23, 2019), 18 patients were evaluable for a response at active dose levels (2.5 mg/kg, 5 mg/kg, and 8 mg/kg).
Two patients achieved a partial response, and eight had stable disease. “This translates to a response rate of 11% and a disease control rate of 55%,” Dr. Ku noted.
Both responders received PRS-343 at 8 mg/kg every 2 weeks. One of these patients had stage 4 gastric adenocarcinoma, and one had stage 4 gynecologic carcinoma.
Of the eight patients with stable disease, three received PRS-343 at 8 mg/kg every 2 weeks, two received 8 mg/kg every 3 weeks, one received the 5 mg/kg dose, and two received the 2.5 mg/kg dose.
Dr. Ku noted that the average time on treatment significantly increased in patients who received PRS-343 at 8 mg/kg every 2 weeks. Additionally, both responders and patients with stable disease had a “clear increase” in CD8+ T cells.
“[PRS-343] has demonstrated antitumor activity in heavily pretreated patients across multiple tumor types, and the treatment history, specifically the receipt of prior anti-HER2 therapy, indicates this is a 4-1BB-driven mechanism of action,” Dr. Ku said. “Based on these results, future studies are planned for continued development in defined HER2-positive indications.”
The current study is sponsored by Pieris Pharmaceuticals. Dr. Ku disclosed relationships with Arog Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, Daiichi Sankyo, Eli Lilly, Merck, Zymeworks, and Pieris Pharmaceuticals.
SOURCE: Ku GY et al. SITC 2019, Abstract O82.
NATIONAL HARBOR, MD – PRS-343, a 4-1BB/HER2 bispecific molecule, has demonstrated safety and antitumor activity in patients with heavily pretreated, HER2-positive solid tumors, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
In a phase 1 trial of 18 evaluable patients, PRS-343 produced partial responses in 2 patients and enabled 8 patients to maintain stable disease. PRS-343 was considered well tolerated at all doses and schedules tested.
“PRS-343 is a bispecific construct targeting HER2 as well as 4-1BB,” said Geoffrey Y. Ku, MD, of Memorial Sloan Kettering Cancer Center in New York. “The HER2 component of the molecule localizes it into the tumor microenvironment of any HER2-positive cells. If the density of the HER2 protein is high enough, that facilitates cross-linkage of 4-1BB.
“4-1BB is an immune agonist that’s present in activated T cells, and cross-linkage helps to improve T-cell exhaustion and is also critical for T-cell expansion. The idea is that, by localizing 4-1BB activation to the tumor microenvironment, we can avoid some of the systemic toxicities associated with naked 4-1BB antibodies,” Dr. Ku added.
The ongoing, phase 1 trial of PRS-343 (NCT03330561) has enrolled 53 patients with a range of HER2-positive malignancies. To be eligible, patients must have progressed on standard therapy or have a tumor for which no standard therapy is available.
The most common diagnosis among enrolled patients is gastroesophageal cancer (n = 19), followed by breast cancer (n = 14), gynecologic cancers (n = 6), colorectal cancer (n = 5), and other malignancies.
The patients’ median age at baseline was 61 years (range, 29-92 years), and a majority were female (62%). Most patients (79%) had received three or more prior lines of therapy, including anti-HER2 treatments. Breast cancer patients had received a median of four anti-HER2 treatments, and gastric cancer patients had received a median of two.
The patients have been treated with PRS-343 at 11 dose levels, ranging from 0.0005 mg/kg to 8 mg/kg, given every 3 weeks. The highest dose, 8 mg/kg, was also given every 2 weeks.
Treatment-related adverse events (TRAEs) included infusion-related reactions (9%), fatigue (9%), chills (6%), flushing (6%), nausea (6%), diarrhea (6%), vomiting (5%), and noncardiac chest pain (4%).
“This was an extremely well-tolerated drug,” Dr. Ku said. “Out of 111 TRAEs, only a tiny proportion were grade 3, and toxicities mostly clustered around infusion-related reactions, constitutional symptoms, as well as gastrointestinal symptoms.”
Grade 3 TRAEs included infusion-related reactions (2%), fatigue (1%), flushing (3%), and noncardiac chest pain (1%). There were no grade 4-5 TRAEs.
At the data cutoff (Oct. 23, 2019), 18 patients were evaluable for a response at active dose levels (2.5 mg/kg, 5 mg/kg, and 8 mg/kg).
Two patients achieved a partial response, and eight had stable disease. “This translates to a response rate of 11% and a disease control rate of 55%,” Dr. Ku noted.
Both responders received PRS-343 at 8 mg/kg every 2 weeks. One of these patients had stage 4 gastric adenocarcinoma, and one had stage 4 gynecologic carcinoma.
Of the eight patients with stable disease, three received PRS-343 at 8 mg/kg every 2 weeks, two received 8 mg/kg every 3 weeks, one received the 5 mg/kg dose, and two received the 2.5 mg/kg dose.
Dr. Ku noted that the average time on treatment significantly increased in patients who received PRS-343 at 8 mg/kg every 2 weeks. Additionally, both responders and patients with stable disease had a “clear increase” in CD8+ T cells.
“[PRS-343] has demonstrated antitumor activity in heavily pretreated patients across multiple tumor types, and the treatment history, specifically the receipt of prior anti-HER2 therapy, indicates this is a 4-1BB-driven mechanism of action,” Dr. Ku said. “Based on these results, future studies are planned for continued development in defined HER2-positive indications.”
The current study is sponsored by Pieris Pharmaceuticals. Dr. Ku disclosed relationships with Arog Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, Daiichi Sankyo, Eli Lilly, Merck, Zymeworks, and Pieris Pharmaceuticals.
SOURCE: Ku GY et al. SITC 2019, Abstract O82.
NATIONAL HARBOR, MD – PRS-343, a 4-1BB/HER2 bispecific molecule, has demonstrated safety and antitumor activity in patients with heavily pretreated, HER2-positive solid tumors, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
In a phase 1 trial of 18 evaluable patients, PRS-343 produced partial responses in 2 patients and enabled 8 patients to maintain stable disease. PRS-343 was considered well tolerated at all doses and schedules tested.
“PRS-343 is a bispecific construct targeting HER2 as well as 4-1BB,” said Geoffrey Y. Ku, MD, of Memorial Sloan Kettering Cancer Center in New York. “The HER2 component of the molecule localizes it into the tumor microenvironment of any HER2-positive cells. If the density of the HER2 protein is high enough, that facilitates cross-linkage of 4-1BB.
“4-1BB is an immune agonist that’s present in activated T cells, and cross-linkage helps to improve T-cell exhaustion and is also critical for T-cell expansion. The idea is that, by localizing 4-1BB activation to the tumor microenvironment, we can avoid some of the systemic toxicities associated with naked 4-1BB antibodies,” Dr. Ku added.
The ongoing, phase 1 trial of PRS-343 (NCT03330561) has enrolled 53 patients with a range of HER2-positive malignancies. To be eligible, patients must have progressed on standard therapy or have a tumor for which no standard therapy is available.
The most common diagnosis among enrolled patients is gastroesophageal cancer (n = 19), followed by breast cancer (n = 14), gynecologic cancers (n = 6), colorectal cancer (n = 5), and other malignancies.
The patients’ median age at baseline was 61 years (range, 29-92 years), and a majority were female (62%). Most patients (79%) had received three or more prior lines of therapy, including anti-HER2 treatments. Breast cancer patients had received a median of four anti-HER2 treatments, and gastric cancer patients had received a median of two.
The patients have been treated with PRS-343 at 11 dose levels, ranging from 0.0005 mg/kg to 8 mg/kg, given every 3 weeks. The highest dose, 8 mg/kg, was also given every 2 weeks.
Treatment-related adverse events (TRAEs) included infusion-related reactions (9%), fatigue (9%), chills (6%), flushing (6%), nausea (6%), diarrhea (6%), vomiting (5%), and noncardiac chest pain (4%).
“This was an extremely well-tolerated drug,” Dr. Ku said. “Out of 111 TRAEs, only a tiny proportion were grade 3, and toxicities mostly clustered around infusion-related reactions, constitutional symptoms, as well as gastrointestinal symptoms.”
Grade 3 TRAEs included infusion-related reactions (2%), fatigue (1%), flushing (3%), and noncardiac chest pain (1%). There were no grade 4-5 TRAEs.
At the data cutoff (Oct. 23, 2019), 18 patients were evaluable for a response at active dose levels (2.5 mg/kg, 5 mg/kg, and 8 mg/kg).
Two patients achieved a partial response, and eight had stable disease. “This translates to a response rate of 11% and a disease control rate of 55%,” Dr. Ku noted.
Both responders received PRS-343 at 8 mg/kg every 2 weeks. One of these patients had stage 4 gastric adenocarcinoma, and one had stage 4 gynecologic carcinoma.
Of the eight patients with stable disease, three received PRS-343 at 8 mg/kg every 2 weeks, two received 8 mg/kg every 3 weeks, one received the 5 mg/kg dose, and two received the 2.5 mg/kg dose.
Dr. Ku noted that the average time on treatment significantly increased in patients who received PRS-343 at 8 mg/kg every 2 weeks. Additionally, both responders and patients with stable disease had a “clear increase” in CD8+ T cells.
“[PRS-343] has demonstrated antitumor activity in heavily pretreated patients across multiple tumor types, and the treatment history, specifically the receipt of prior anti-HER2 therapy, indicates this is a 4-1BB-driven mechanism of action,” Dr. Ku said. “Based on these results, future studies are planned for continued development in defined HER2-positive indications.”
The current study is sponsored by Pieris Pharmaceuticals. Dr. Ku disclosed relationships with Arog Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, Daiichi Sankyo, Eli Lilly, Merck, Zymeworks, and Pieris Pharmaceuticals.
SOURCE: Ku GY et al. SITC 2019, Abstract O82.
REPORTING FROM SITC 2019
Atezolizumab bests chemo in NSCLC patients with high PD-L1 expression
NATIONAL HARBOR, MD – interim results of a phase 3 trial suggest.
When compared with platinum-based chemotherapy, atezolizumab significantly improved OS in patients who had PD-L1 expression of 50% or greater on tumor cells (TC) or 10% or greater on tumor-infiltrating immune cells (IC).
Patients with lower levels of PD-L1 expression had a numerical, but not statistically significant, benefit in OS with atezolizumab.
Giuseppe Giaccone, MD, PhD, of Georgetown University, Washington, presented these results, from the IMpower110 trial, as a late-breaking abstract at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled treatment-naive, PD-L1–selected patients with stage IV NSCLC. Patients with EGFR-positive or ALK-positive NSCLC were excluded.
The overall population consisted of 554 patients with PD-L1 expression of at least 1% on TC or IC (TC1/2/3 or IC1/2/3). There were 328 patients with PD-L1 expression of at least 5% on TC or IC (TC2/3 or IC2/3) and 205 patients with PD-L1 expression of at least 50% on TC or 10% on IC (TC3 or IC3).
All patients were randomized to receive atezolizumab or platinum-based chemotherapy. Atezolizumab was given at 1,200 mg every 3 weeks until disease progression or loss of clinical benefit. In the chemotherapy arm, patients with nonsquamous NSCLC received cisplatin or carboplatin plus pemetrexed, and patients with squamous NSCLC received cisplatin or carboplatin plus gemcitabine. Chemotherapy was given for 4-6 cycles, after which patients received pemetrexed (nonsquamous) or best supportive care (squamous) until progression.
Baseline characteristics were similar between the treatment arms and across the PD-L1 subgroups.
Overall survival
OS was evaluated hierarchically, starting with the TC3 or IC3 population. This group had a significant improvement in OS with atezolizumab. At a median follow-up of 15.7 months, the median OS was 13.1 months with chemotherapy and 20.2 months with atezolizumab (hazard ratio, 0.59; P = .0106).
The TC2/3 or IC2/3 population had a numerical, but not significant, improvement in OS with atezolizumab. At a median follow-up of 15.2 months, the median OS was 14.9 months with chemotherapy and 18.2 months with atezolizumab (HR, 0.72; P = .0416).
“The prespecified alpha boundary was not crossed in this analysis,” Dr. Giaccone said. “Therefore, it cannot be considered statistically significant, although, numerically, there is clearly an advantage with atezolizumab versus chemotherapy.”
There was no significant improvement in OS in the overall population (TC1/2/3 or IC1/2/3). At a median follow-up of 13.4 months, the median OS was 14.1 months in the chemotherapy arm and 17.5 months in the atezolizumab arm (HR, 0.83; P = .1481).
Dr. Giaccone noted that 29.6% of patients in the atezolizumab arm and 49.5% of those in the chemotherapy arm received at least one subsequent cancer therapy. The proportion of patients that received second-line cancer therapies was similar across the PD-L1 subgroups.
Progression-free survival
Progression-free survival (PFS) was significantly better with atezolizumab, regardless of PD-L1 expression.
In the TC3/IC3 population, the median PFS was 5.0 months with chemotherapy and 8.1 months with atezolizumab (HR, 0.63; P = .0070). In the TC2/3 or IC2/3 group, the median PFS was 5.5 months with chemotherapy and 7.2 months with atezolizumab (HR, 0.67; P = .0030). In the overall population, the median PFS was 5.5 months with chemotherapy and 5.7 months with atezolizumab (HR, 0.77; P = .0104).
Safety
“The safety profile of atezolizumab was consistent with prior observations,” Dr. Giaccone said.
The incidence of treatment-related adverse events (AEs) was 90.2% in the atezolizumab arm and 94.7% in the chemotherapy arm. Rates of grade 3/4 related AEs were 12.9% and 44.1%, respectively. There was one grade 5 AE in the chemotherapy arm and none in the atezolizumab arm.
AEs that were more frequent with atezolizumab included increased aspartate aminotransferase, pruritus, and hypothyroidism.
This trial is sponsored by Hoffmann-La Roche, and Dr. Giaccone disclosed grants and nonfinancial support from the company.
SOURCE: Giaccone G et al. SITC 2019, Abstract O81.
NATIONAL HARBOR, MD – interim results of a phase 3 trial suggest.
When compared with platinum-based chemotherapy, atezolizumab significantly improved OS in patients who had PD-L1 expression of 50% or greater on tumor cells (TC) or 10% or greater on tumor-infiltrating immune cells (IC).
Patients with lower levels of PD-L1 expression had a numerical, but not statistically significant, benefit in OS with atezolizumab.
Giuseppe Giaccone, MD, PhD, of Georgetown University, Washington, presented these results, from the IMpower110 trial, as a late-breaking abstract at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled treatment-naive, PD-L1–selected patients with stage IV NSCLC. Patients with EGFR-positive or ALK-positive NSCLC were excluded.
The overall population consisted of 554 patients with PD-L1 expression of at least 1% on TC or IC (TC1/2/3 or IC1/2/3). There were 328 patients with PD-L1 expression of at least 5% on TC or IC (TC2/3 or IC2/3) and 205 patients with PD-L1 expression of at least 50% on TC or 10% on IC (TC3 or IC3).
All patients were randomized to receive atezolizumab or platinum-based chemotherapy. Atezolizumab was given at 1,200 mg every 3 weeks until disease progression or loss of clinical benefit. In the chemotherapy arm, patients with nonsquamous NSCLC received cisplatin or carboplatin plus pemetrexed, and patients with squamous NSCLC received cisplatin or carboplatin plus gemcitabine. Chemotherapy was given for 4-6 cycles, after which patients received pemetrexed (nonsquamous) or best supportive care (squamous) until progression.
Baseline characteristics were similar between the treatment arms and across the PD-L1 subgroups.
Overall survival
OS was evaluated hierarchically, starting with the TC3 or IC3 population. This group had a significant improvement in OS with atezolizumab. At a median follow-up of 15.7 months, the median OS was 13.1 months with chemotherapy and 20.2 months with atezolizumab (hazard ratio, 0.59; P = .0106).
The TC2/3 or IC2/3 population had a numerical, but not significant, improvement in OS with atezolizumab. At a median follow-up of 15.2 months, the median OS was 14.9 months with chemotherapy and 18.2 months with atezolizumab (HR, 0.72; P = .0416).
“The prespecified alpha boundary was not crossed in this analysis,” Dr. Giaccone said. “Therefore, it cannot be considered statistically significant, although, numerically, there is clearly an advantage with atezolizumab versus chemotherapy.”
There was no significant improvement in OS in the overall population (TC1/2/3 or IC1/2/3). At a median follow-up of 13.4 months, the median OS was 14.1 months in the chemotherapy arm and 17.5 months in the atezolizumab arm (HR, 0.83; P = .1481).
Dr. Giaccone noted that 29.6% of patients in the atezolizumab arm and 49.5% of those in the chemotherapy arm received at least one subsequent cancer therapy. The proportion of patients that received second-line cancer therapies was similar across the PD-L1 subgroups.
Progression-free survival
Progression-free survival (PFS) was significantly better with atezolizumab, regardless of PD-L1 expression.
In the TC3/IC3 population, the median PFS was 5.0 months with chemotherapy and 8.1 months with atezolizumab (HR, 0.63; P = .0070). In the TC2/3 or IC2/3 group, the median PFS was 5.5 months with chemotherapy and 7.2 months with atezolizumab (HR, 0.67; P = .0030). In the overall population, the median PFS was 5.5 months with chemotherapy and 5.7 months with atezolizumab (HR, 0.77; P = .0104).
Safety
“The safety profile of atezolizumab was consistent with prior observations,” Dr. Giaccone said.
The incidence of treatment-related adverse events (AEs) was 90.2% in the atezolizumab arm and 94.7% in the chemotherapy arm. Rates of grade 3/4 related AEs were 12.9% and 44.1%, respectively. There was one grade 5 AE in the chemotherapy arm and none in the atezolizumab arm.
AEs that were more frequent with atezolizumab included increased aspartate aminotransferase, pruritus, and hypothyroidism.
This trial is sponsored by Hoffmann-La Roche, and Dr. Giaccone disclosed grants and nonfinancial support from the company.
SOURCE: Giaccone G et al. SITC 2019, Abstract O81.
NATIONAL HARBOR, MD – interim results of a phase 3 trial suggest.
When compared with platinum-based chemotherapy, atezolizumab significantly improved OS in patients who had PD-L1 expression of 50% or greater on tumor cells (TC) or 10% or greater on tumor-infiltrating immune cells (IC).
Patients with lower levels of PD-L1 expression had a numerical, but not statistically significant, benefit in OS with atezolizumab.
Giuseppe Giaccone, MD, PhD, of Georgetown University, Washington, presented these results, from the IMpower110 trial, as a late-breaking abstract at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled treatment-naive, PD-L1–selected patients with stage IV NSCLC. Patients with EGFR-positive or ALK-positive NSCLC were excluded.
The overall population consisted of 554 patients with PD-L1 expression of at least 1% on TC or IC (TC1/2/3 or IC1/2/3). There were 328 patients with PD-L1 expression of at least 5% on TC or IC (TC2/3 or IC2/3) and 205 patients with PD-L1 expression of at least 50% on TC or 10% on IC (TC3 or IC3).
All patients were randomized to receive atezolizumab or platinum-based chemotherapy. Atezolizumab was given at 1,200 mg every 3 weeks until disease progression or loss of clinical benefit. In the chemotherapy arm, patients with nonsquamous NSCLC received cisplatin or carboplatin plus pemetrexed, and patients with squamous NSCLC received cisplatin or carboplatin plus gemcitabine. Chemotherapy was given for 4-6 cycles, after which patients received pemetrexed (nonsquamous) or best supportive care (squamous) until progression.
Baseline characteristics were similar between the treatment arms and across the PD-L1 subgroups.
Overall survival
OS was evaluated hierarchically, starting with the TC3 or IC3 population. This group had a significant improvement in OS with atezolizumab. At a median follow-up of 15.7 months, the median OS was 13.1 months with chemotherapy and 20.2 months with atezolizumab (hazard ratio, 0.59; P = .0106).
The TC2/3 or IC2/3 population had a numerical, but not significant, improvement in OS with atezolizumab. At a median follow-up of 15.2 months, the median OS was 14.9 months with chemotherapy and 18.2 months with atezolizumab (HR, 0.72; P = .0416).
“The prespecified alpha boundary was not crossed in this analysis,” Dr. Giaccone said. “Therefore, it cannot be considered statistically significant, although, numerically, there is clearly an advantage with atezolizumab versus chemotherapy.”
There was no significant improvement in OS in the overall population (TC1/2/3 or IC1/2/3). At a median follow-up of 13.4 months, the median OS was 14.1 months in the chemotherapy arm and 17.5 months in the atezolizumab arm (HR, 0.83; P = .1481).
Dr. Giaccone noted that 29.6% of patients in the atezolizumab arm and 49.5% of those in the chemotherapy arm received at least one subsequent cancer therapy. The proportion of patients that received second-line cancer therapies was similar across the PD-L1 subgroups.
Progression-free survival
Progression-free survival (PFS) was significantly better with atezolizumab, regardless of PD-L1 expression.
In the TC3/IC3 population, the median PFS was 5.0 months with chemotherapy and 8.1 months with atezolizumab (HR, 0.63; P = .0070). In the TC2/3 or IC2/3 group, the median PFS was 5.5 months with chemotherapy and 7.2 months with atezolizumab (HR, 0.67; P = .0030). In the overall population, the median PFS was 5.5 months with chemotherapy and 5.7 months with atezolizumab (HR, 0.77; P = .0104).
Safety
“The safety profile of atezolizumab was consistent with prior observations,” Dr. Giaccone said.
The incidence of treatment-related adverse events (AEs) was 90.2% in the atezolizumab arm and 94.7% in the chemotherapy arm. Rates of grade 3/4 related AEs were 12.9% and 44.1%, respectively. There was one grade 5 AE in the chemotherapy arm and none in the atezolizumab arm.
AEs that were more frequent with atezolizumab included increased aspartate aminotransferase, pruritus, and hypothyroidism.
This trial is sponsored by Hoffmann-La Roche, and Dr. Giaccone disclosed grants and nonfinancial support from the company.
SOURCE: Giaccone G et al. SITC 2019, Abstract O81.
REPORTING FROM SITC 2019