User login
TRED-HF: Despite recovery, dilated cardiomyopathy returns after halting HF drugs
CHICAGO – Phased withdrawal of guideline-directed medical therapy in patients who seemed to have recovered from dilated cardiomyopathy resulted in relapses in 40% of patients within 6 months in the TRED-HF trial.
The clinical implications of this small pilot randomized trial are clear: “Withdrawal of therapy should not usually be attempted, at least until we can predict who’s going to relapse and who’s not,” Brian P. Halliday, MD, PhD, said at the American Heart Association scientific sessions.
“Improvement in function represents remission rather than permanent recovery for many patients,” added Dr. Halliday of Imperial College London.
The study was performed to address a question that arises with increasing frequency in clinical practice as a result of the impressive advances in heart failure therapy in recent years, he said. “Patients frequently come to us in clinic and ask us, ‘Do I need to continue to take these medications forever?’ They’re frequently young, and they want to know if they really need to be subject to 40 or 50 years of medication. Some are concerned about side effects, others are interested in pregnancy, and then there is the financial cost.”
Simultaneously published in The Lancet, TRED-HF was a single-center, open-label study of 51 patients who had prior dilated cardiomyopathy (DCM) and a median left ventricular ejection fraction (LVEF) of 25% at the time of diagnosis 4.9 years earlier and who subsequently recovered in response to therapy. That is, they became symptom-free with an LVEF greater than 50%, a normal left ventricular end diastolic volume index, and a reassuringly low median N-terminal pro b-type natriuretic peptide (NP-pro-BNP) level of 72 ng/L.
For the study, 25 patients were randomized to phased withdrawal of their heart failure drugs over a 16-week period: First they reduced or stopped loop diuretics, then mineralocorticoid antagonists, then beta-blockers, and finally their ACE inhibitor or angiotensin receptor blocker. The other 26 participants continued therapy during the first 6 months of the study, then 25 of the 26 crossed over to phased withdrawal. The outlier didn’t cross over because of atrial fibrillation.
The primary endpoint was relapse of DCM within 6 months of the start of the study. Relapse was defined as either a drop in LVEF of more than 10% to a level below 50%, at least a doubling of NT-pro-BNP to greater than 400 ng/L, clinical evidence of heart failure, or a greater than 10% increase in LV end diastolic volume as assessed by cardiac MRI.
The results
During the first half of the study, 11 of 25 patients (44%) relapsed during or after medication withdrawal. None of the controls relapsed. In the crossover phase, 9 of 25 patients (35%) relapsed in response to treatment withdrawal. Of the 20 patients who relapsed, 13 did so within 16 weeks of beginning medication withdrawal. Indeed, most patients relapsed within 8 weeks of their last medication. Ten of the twenty fulfilled multiple criteria for relapse.
Medication withdrawal was accompanied not only by a mean 9.5% reduction in LVEF, compared with baseline, but by a 15.4-bpm rise in heart rate, a 7.0–mm Hg increase in diastolic blood pressure, and 5.1-point deterioration in Kansas City Cardiomyopathy Questionnaire scores, demonstrating that what happened off treatment was true DCM recurrence and not simply an imaging artifact.
Everyone who relapsed immediately restarted treatment. At their next follow-up visit, all were once again asymptomatic, and 17 of the 20 (85%) had an LVEF greater than 50%. Two of the other three had an LVEF of 45%-50%, and the other had an LVEF of 43%.
“So they did seem to recover when they went back on medication,” Dr. Halliday observed.
Underpowered exploratory analyses designed for hypothesis generation identified several potential baseline predictors of DCM relapse, including older age, being on three or more heart failure drugs, and use of a mineralocorticoid antagonist.
Experts react
Designated discussant Jane E. Wilcox, MD, commented, “Currently, in 2018, we have no true signature of recovery. These patients are indeed in cardiac remission and have an indefinite indication for continuing their evidence-based medical therapy without interruption.”
“The clinical implication here is, I think, we should TRED-lightly,” quipped Dr. Wilcox of Northwestern University in Chicago.
Her own research indicates that even patients who have recovered their LVEF and no longer seem to have a heart failure phenotype still have an abnormal myocardial substrate as evidenced by persistent dysfunctional cardiac mechanics on echocardiography. Nonetheless, she remains optimistic.
“I don’t think [TRED-HF] squelches the future of myocardial recovery. I think it actually invigorates the field for an assessment of genomics, proteomics, and metabolomics looking for that true signature of cardiac recovery,” she said.
Donald Lloyd-Jones, MD, who chaired a press conference where Dr. Halliday presented the TRED-HF results, complimented the investigators for tackling what he termed “an incredibly important clinical question that comes up all the time.”
“I really want to commend the investigators for taking on what, on its face, might be an ethically challenging question by taking treatment away when we don’t know what the answer is likely to be. But they really checked all the boxes to make sure this was done in a very safe and monitored way, so that even though the outcome was what it turned out to be, the harm to patients was minimalized,” said Dr. Lloyd-Jones, professor and chair of the department of preventive medicine and director of the Northwestern University Clinical and Translational Sciences Institute, Chicago.
“No patient wants to be on more medication than they need to be, but I think for the time being this class of patients is going to have to be maintained on medications until we understand a little more,” Dr. Lloyd-Jones concluded.
Dr. Halliday reported having no financial conflicts regarding the study, funded by the British Heart Foundation.
SOURCE: Halliday BP. AHA scientific sessions, Abstract 18621. Simulpub The Lancet. 2018 Nov 11. doi: 10.1016/S0140-6736(18)32484-X.
CHICAGO – Phased withdrawal of guideline-directed medical therapy in patients who seemed to have recovered from dilated cardiomyopathy resulted in relapses in 40% of patients within 6 months in the TRED-HF trial.
The clinical implications of this small pilot randomized trial are clear: “Withdrawal of therapy should not usually be attempted, at least until we can predict who’s going to relapse and who’s not,” Brian P. Halliday, MD, PhD, said at the American Heart Association scientific sessions.
“Improvement in function represents remission rather than permanent recovery for many patients,” added Dr. Halliday of Imperial College London.
The study was performed to address a question that arises with increasing frequency in clinical practice as a result of the impressive advances in heart failure therapy in recent years, he said. “Patients frequently come to us in clinic and ask us, ‘Do I need to continue to take these medications forever?’ They’re frequently young, and they want to know if they really need to be subject to 40 or 50 years of medication. Some are concerned about side effects, others are interested in pregnancy, and then there is the financial cost.”
Simultaneously published in The Lancet, TRED-HF was a single-center, open-label study of 51 patients who had prior dilated cardiomyopathy (DCM) and a median left ventricular ejection fraction (LVEF) of 25% at the time of diagnosis 4.9 years earlier and who subsequently recovered in response to therapy. That is, they became symptom-free with an LVEF greater than 50%, a normal left ventricular end diastolic volume index, and a reassuringly low median N-terminal pro b-type natriuretic peptide (NP-pro-BNP) level of 72 ng/L.
For the study, 25 patients were randomized to phased withdrawal of their heart failure drugs over a 16-week period: First they reduced or stopped loop diuretics, then mineralocorticoid antagonists, then beta-blockers, and finally their ACE inhibitor or angiotensin receptor blocker. The other 26 participants continued therapy during the first 6 months of the study, then 25 of the 26 crossed over to phased withdrawal. The outlier didn’t cross over because of atrial fibrillation.
The primary endpoint was relapse of DCM within 6 months of the start of the study. Relapse was defined as either a drop in LVEF of more than 10% to a level below 50%, at least a doubling of NT-pro-BNP to greater than 400 ng/L, clinical evidence of heart failure, or a greater than 10% increase in LV end diastolic volume as assessed by cardiac MRI.
The results
During the first half of the study, 11 of 25 patients (44%) relapsed during or after medication withdrawal. None of the controls relapsed. In the crossover phase, 9 of 25 patients (35%) relapsed in response to treatment withdrawal. Of the 20 patients who relapsed, 13 did so within 16 weeks of beginning medication withdrawal. Indeed, most patients relapsed within 8 weeks of their last medication. Ten of the twenty fulfilled multiple criteria for relapse.
Medication withdrawal was accompanied not only by a mean 9.5% reduction in LVEF, compared with baseline, but by a 15.4-bpm rise in heart rate, a 7.0–mm Hg increase in diastolic blood pressure, and 5.1-point deterioration in Kansas City Cardiomyopathy Questionnaire scores, demonstrating that what happened off treatment was true DCM recurrence and not simply an imaging artifact.
Everyone who relapsed immediately restarted treatment. At their next follow-up visit, all were once again asymptomatic, and 17 of the 20 (85%) had an LVEF greater than 50%. Two of the other three had an LVEF of 45%-50%, and the other had an LVEF of 43%.
“So they did seem to recover when they went back on medication,” Dr. Halliday observed.
Underpowered exploratory analyses designed for hypothesis generation identified several potential baseline predictors of DCM relapse, including older age, being on three or more heart failure drugs, and use of a mineralocorticoid antagonist.
Experts react
Designated discussant Jane E. Wilcox, MD, commented, “Currently, in 2018, we have no true signature of recovery. These patients are indeed in cardiac remission and have an indefinite indication for continuing their evidence-based medical therapy without interruption.”
“The clinical implication here is, I think, we should TRED-lightly,” quipped Dr. Wilcox of Northwestern University in Chicago.
Her own research indicates that even patients who have recovered their LVEF and no longer seem to have a heart failure phenotype still have an abnormal myocardial substrate as evidenced by persistent dysfunctional cardiac mechanics on echocardiography. Nonetheless, she remains optimistic.
“I don’t think [TRED-HF] squelches the future of myocardial recovery. I think it actually invigorates the field for an assessment of genomics, proteomics, and metabolomics looking for that true signature of cardiac recovery,” she said.
Donald Lloyd-Jones, MD, who chaired a press conference where Dr. Halliday presented the TRED-HF results, complimented the investigators for tackling what he termed “an incredibly important clinical question that comes up all the time.”
“I really want to commend the investigators for taking on what, on its face, might be an ethically challenging question by taking treatment away when we don’t know what the answer is likely to be. But they really checked all the boxes to make sure this was done in a very safe and monitored way, so that even though the outcome was what it turned out to be, the harm to patients was minimalized,” said Dr. Lloyd-Jones, professor and chair of the department of preventive medicine and director of the Northwestern University Clinical and Translational Sciences Institute, Chicago.
“No patient wants to be on more medication than they need to be, but I think for the time being this class of patients is going to have to be maintained on medications until we understand a little more,” Dr. Lloyd-Jones concluded.
Dr. Halliday reported having no financial conflicts regarding the study, funded by the British Heart Foundation.
SOURCE: Halliday BP. AHA scientific sessions, Abstract 18621. Simulpub The Lancet. 2018 Nov 11. doi: 10.1016/S0140-6736(18)32484-X.
CHICAGO – Phased withdrawal of guideline-directed medical therapy in patients who seemed to have recovered from dilated cardiomyopathy resulted in relapses in 40% of patients within 6 months in the TRED-HF trial.
The clinical implications of this small pilot randomized trial are clear: “Withdrawal of therapy should not usually be attempted, at least until we can predict who’s going to relapse and who’s not,” Brian P. Halliday, MD, PhD, said at the American Heart Association scientific sessions.
“Improvement in function represents remission rather than permanent recovery for many patients,” added Dr. Halliday of Imperial College London.
The study was performed to address a question that arises with increasing frequency in clinical practice as a result of the impressive advances in heart failure therapy in recent years, he said. “Patients frequently come to us in clinic and ask us, ‘Do I need to continue to take these medications forever?’ They’re frequently young, and they want to know if they really need to be subject to 40 or 50 years of medication. Some are concerned about side effects, others are interested in pregnancy, and then there is the financial cost.”
Simultaneously published in The Lancet, TRED-HF was a single-center, open-label study of 51 patients who had prior dilated cardiomyopathy (DCM) and a median left ventricular ejection fraction (LVEF) of 25% at the time of diagnosis 4.9 years earlier and who subsequently recovered in response to therapy. That is, they became symptom-free with an LVEF greater than 50%, a normal left ventricular end diastolic volume index, and a reassuringly low median N-terminal pro b-type natriuretic peptide (NP-pro-BNP) level of 72 ng/L.
For the study, 25 patients were randomized to phased withdrawal of their heart failure drugs over a 16-week period: First they reduced or stopped loop diuretics, then mineralocorticoid antagonists, then beta-blockers, and finally their ACE inhibitor or angiotensin receptor blocker. The other 26 participants continued therapy during the first 6 months of the study, then 25 of the 26 crossed over to phased withdrawal. The outlier didn’t cross over because of atrial fibrillation.
The primary endpoint was relapse of DCM within 6 months of the start of the study. Relapse was defined as either a drop in LVEF of more than 10% to a level below 50%, at least a doubling of NT-pro-BNP to greater than 400 ng/L, clinical evidence of heart failure, or a greater than 10% increase in LV end diastolic volume as assessed by cardiac MRI.
The results
During the first half of the study, 11 of 25 patients (44%) relapsed during or after medication withdrawal. None of the controls relapsed. In the crossover phase, 9 of 25 patients (35%) relapsed in response to treatment withdrawal. Of the 20 patients who relapsed, 13 did so within 16 weeks of beginning medication withdrawal. Indeed, most patients relapsed within 8 weeks of their last medication. Ten of the twenty fulfilled multiple criteria for relapse.
Medication withdrawal was accompanied not only by a mean 9.5% reduction in LVEF, compared with baseline, but by a 15.4-bpm rise in heart rate, a 7.0–mm Hg increase in diastolic blood pressure, and 5.1-point deterioration in Kansas City Cardiomyopathy Questionnaire scores, demonstrating that what happened off treatment was true DCM recurrence and not simply an imaging artifact.
Everyone who relapsed immediately restarted treatment. At their next follow-up visit, all were once again asymptomatic, and 17 of the 20 (85%) had an LVEF greater than 50%. Two of the other three had an LVEF of 45%-50%, and the other had an LVEF of 43%.
“So they did seem to recover when they went back on medication,” Dr. Halliday observed.
Underpowered exploratory analyses designed for hypothesis generation identified several potential baseline predictors of DCM relapse, including older age, being on three or more heart failure drugs, and use of a mineralocorticoid antagonist.
Experts react
Designated discussant Jane E. Wilcox, MD, commented, “Currently, in 2018, we have no true signature of recovery. These patients are indeed in cardiac remission and have an indefinite indication for continuing their evidence-based medical therapy without interruption.”
“The clinical implication here is, I think, we should TRED-lightly,” quipped Dr. Wilcox of Northwestern University in Chicago.
Her own research indicates that even patients who have recovered their LVEF and no longer seem to have a heart failure phenotype still have an abnormal myocardial substrate as evidenced by persistent dysfunctional cardiac mechanics on echocardiography. Nonetheless, she remains optimistic.
“I don’t think [TRED-HF] squelches the future of myocardial recovery. I think it actually invigorates the field for an assessment of genomics, proteomics, and metabolomics looking for that true signature of cardiac recovery,” she said.
Donald Lloyd-Jones, MD, who chaired a press conference where Dr. Halliday presented the TRED-HF results, complimented the investigators for tackling what he termed “an incredibly important clinical question that comes up all the time.”
“I really want to commend the investigators for taking on what, on its face, might be an ethically challenging question by taking treatment away when we don’t know what the answer is likely to be. But they really checked all the boxes to make sure this was done in a very safe and monitored way, so that even though the outcome was what it turned out to be, the harm to patients was minimalized,” said Dr. Lloyd-Jones, professor and chair of the department of preventive medicine and director of the Northwestern University Clinical and Translational Sciences Institute, Chicago.
“No patient wants to be on more medication than they need to be, but I think for the time being this class of patients is going to have to be maintained on medications until we understand a little more,” Dr. Lloyd-Jones concluded.
Dr. Halliday reported having no financial conflicts regarding the study, funded by the British Heart Foundation.
SOURCE: Halliday BP. AHA scientific sessions, Abstract 18621. Simulpub The Lancet. 2018 Nov 11. doi: 10.1016/S0140-6736(18)32484-X.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: The heart failure relapse rate is high after medication withdrawal.
Major finding: Of patients who were seemingly recovered from dilated cardiomyopathy, 40% experienced early relapse following structured medication withdrawal.
Study details: This randomized crossover trial included 51 patients whose medications were withdrawn after their apparent recovery from dilated cardiomyopathy.
Disclosures: The study was funded by the British Heart Foundation. The presenter reported having no financial conflicts.
Source: Halliday BP. AHA scientific sessions, Abstract 18621. Simulpub The Lancet. 2018 Nov 11. doi: 10.1016/S0140-6736(18)32484-X.
ARISTOPHANES: Apixaban edges other DOACS for octogenarians
The findings come from an analysis of insurance claims data from more than 50,000 U.S. patients – the largest observational study to date to compare these three direct-acting oral anticoagulants (DOACs) in octogenarians with nonvalvular atrial fibrillation, Steven B. Deitelzweig, MD, said at the American Heart Association scientific sessions.
“The results may help clinicians evaluate the risk-benefit ratio of the DOACs” in this population, said Dr. Deitelzweig, vice president for medical affairs at Ochsner Medical Center in New Orleans.
He noted that the results were consistent with prior reports from observational data and registries, as well as the results in a recent analysis commissioned by the Agency for Healthcare Research and Quality. “We see a consistent message that apixaban always has less risk for major bleeding, and at least comparable efficacy” when compared with other DOACs, he said in a video interview.
And for the foreseeable future, this sort of data will need to suffice for clinicians trying to decide which DOAC to use because “I know of no head-to-head trials, nor do I anticipate any head-to-head trials” that could provide a more definitive comparison of the DOACs, Dr. Deitelzweig said.
The data came from a large number of patients – about 38% of the U.S. population – which boosts the generalizability of the finding. “I think our data are useful” for helping to make treatment decisions, he concluded.
The analysis he reported came from the ARISTOPHANES (Anticoagulants for Reduction in Stroke: Observational Pooled Analysis on Health Outcomes and Experience of Patients) study, which pooled U.S. insurance claims data from several sources. For the octogenarian study, Dr. Deitelzweig and his associates used data from about 123 million U.S. residents collected between January 2012 and September 2015 by Medicare and three different commercial insurance databases. The overall level of beneficiary overlap between these four data sources was less than 0.5%.
The researchers identified patients with nonvalvular atrial fibrillation who started anticoagulant treatment with a DOAC and were at least 80 years old. This included 19,752 patients started on apixaban (Eliquis), 6,741 started on dabigatran (Pradaxa), and 27,217 started on rivaroxaban (Xarelto). A majority of the patients were at least 84 years old.
The analysis used propensity-score matching to compare similar patients and to minimize the impact of potentially confounding differences among the patients in each treatment subgroup. During a median follow-up of 7-9 months, the incidence of stroke or systemic embolism was 35% lower in the apixaban-treated patients, compared with those who received dabigatran, and 28% lower in the apixaban patients, compared with those treated with rivaroxaban, both statistically significant differences, Dr. Deitelzweig reported. The incidence of major bleeding episodes was 40% lower with apixaban than with dabigatran and 50% lower with apixaban, compared with rivaroxaban, also statistically significant differences.
When the analysis compared dabigatran with rivaroxaban it showed no statistically significant difference for the efficacy endpoint, but dabigatran produced 23% fewer major bleeds than rivaroxaban, a statistically significant difference.
These findings jibed with a recently published analysis from Dr. Deitelzweig and his associates that used data from all adults with nonvalvular atrial fibrillation started on an oral anticoagulant in an expanded ARISTOPHANES database for 2012-2015 that included more than 180 million U.S. beneficiaries. After propensity-score matching, this created subgroups of about 58,000 patients started on apixaban, nearly 27,000 started on dabigatran, and more than 83,000 started on rivaroxaban. The patients averaged about 73 years old. Again, with about 7-9 months of follow-up, very similar outcomes occurred. Patients on apixaban had significantly fewer strokes and systemic embolic events as well as significantly fewer major bleeds compared with patients treated with one of the other DOACs (Stroke. 2018 Dec;49[12]:2933-44).
The study was funded by Bristol-Myers Squibb and Pfizer, the companies that market apixaban (Eliquis). Dr. Deitelzweig is a consultant to and speaker on behalf of Bristol-Myers Squibb and Pfizer. He is also a consultant to or speaker on behalf of Boehringer Ingelheim, Daiichi-Sankyo, Janssen, and Portola Pharmaceuticals.
SOURCE: Deitelzweig SB et al. Circulation. 2018 Nov 6;138(suppl 1):A14900.
The findings come from an analysis of insurance claims data from more than 50,000 U.S. patients – the largest observational study to date to compare these three direct-acting oral anticoagulants (DOACs) in octogenarians with nonvalvular atrial fibrillation, Steven B. Deitelzweig, MD, said at the American Heart Association scientific sessions.
“The results may help clinicians evaluate the risk-benefit ratio of the DOACs” in this population, said Dr. Deitelzweig, vice president for medical affairs at Ochsner Medical Center in New Orleans.
He noted that the results were consistent with prior reports from observational data and registries, as well as the results in a recent analysis commissioned by the Agency for Healthcare Research and Quality. “We see a consistent message that apixaban always has less risk for major bleeding, and at least comparable efficacy” when compared with other DOACs, he said in a video interview.
And for the foreseeable future, this sort of data will need to suffice for clinicians trying to decide which DOAC to use because “I know of no head-to-head trials, nor do I anticipate any head-to-head trials” that could provide a more definitive comparison of the DOACs, Dr. Deitelzweig said.
The data came from a large number of patients – about 38% of the U.S. population – which boosts the generalizability of the finding. “I think our data are useful” for helping to make treatment decisions, he concluded.
The analysis he reported came from the ARISTOPHANES (Anticoagulants for Reduction in Stroke: Observational Pooled Analysis on Health Outcomes and Experience of Patients) study, which pooled U.S. insurance claims data from several sources. For the octogenarian study, Dr. Deitelzweig and his associates used data from about 123 million U.S. residents collected between January 2012 and September 2015 by Medicare and three different commercial insurance databases. The overall level of beneficiary overlap between these four data sources was less than 0.5%.
The researchers identified patients with nonvalvular atrial fibrillation who started anticoagulant treatment with a DOAC and were at least 80 years old. This included 19,752 patients started on apixaban (Eliquis), 6,741 started on dabigatran (Pradaxa), and 27,217 started on rivaroxaban (Xarelto). A majority of the patients were at least 84 years old.
The analysis used propensity-score matching to compare similar patients and to minimize the impact of potentially confounding differences among the patients in each treatment subgroup. During a median follow-up of 7-9 months, the incidence of stroke or systemic embolism was 35% lower in the apixaban-treated patients, compared with those who received dabigatran, and 28% lower in the apixaban patients, compared with those treated with rivaroxaban, both statistically significant differences, Dr. Deitelzweig reported. The incidence of major bleeding episodes was 40% lower with apixaban than with dabigatran and 50% lower with apixaban, compared with rivaroxaban, also statistically significant differences.
When the analysis compared dabigatran with rivaroxaban it showed no statistically significant difference for the efficacy endpoint, but dabigatran produced 23% fewer major bleeds than rivaroxaban, a statistically significant difference.
These findings jibed with a recently published analysis from Dr. Deitelzweig and his associates that used data from all adults with nonvalvular atrial fibrillation started on an oral anticoagulant in an expanded ARISTOPHANES database for 2012-2015 that included more than 180 million U.S. beneficiaries. After propensity-score matching, this created subgroups of about 58,000 patients started on apixaban, nearly 27,000 started on dabigatran, and more than 83,000 started on rivaroxaban. The patients averaged about 73 years old. Again, with about 7-9 months of follow-up, very similar outcomes occurred. Patients on apixaban had significantly fewer strokes and systemic embolic events as well as significantly fewer major bleeds compared with patients treated with one of the other DOACs (Stroke. 2018 Dec;49[12]:2933-44).
The study was funded by Bristol-Myers Squibb and Pfizer, the companies that market apixaban (Eliquis). Dr. Deitelzweig is a consultant to and speaker on behalf of Bristol-Myers Squibb and Pfizer. He is also a consultant to or speaker on behalf of Boehringer Ingelheim, Daiichi-Sankyo, Janssen, and Portola Pharmaceuticals.
SOURCE: Deitelzweig SB et al. Circulation. 2018 Nov 6;138(suppl 1):A14900.
The findings come from an analysis of insurance claims data from more than 50,000 U.S. patients – the largest observational study to date to compare these three direct-acting oral anticoagulants (DOACs) in octogenarians with nonvalvular atrial fibrillation, Steven B. Deitelzweig, MD, said at the American Heart Association scientific sessions.
“The results may help clinicians evaluate the risk-benefit ratio of the DOACs” in this population, said Dr. Deitelzweig, vice president for medical affairs at Ochsner Medical Center in New Orleans.
He noted that the results were consistent with prior reports from observational data and registries, as well as the results in a recent analysis commissioned by the Agency for Healthcare Research and Quality. “We see a consistent message that apixaban always has less risk for major bleeding, and at least comparable efficacy” when compared with other DOACs, he said in a video interview.
And for the foreseeable future, this sort of data will need to suffice for clinicians trying to decide which DOAC to use because “I know of no head-to-head trials, nor do I anticipate any head-to-head trials” that could provide a more definitive comparison of the DOACs, Dr. Deitelzweig said.
The data came from a large number of patients – about 38% of the U.S. population – which boosts the generalizability of the finding. “I think our data are useful” for helping to make treatment decisions, he concluded.
The analysis he reported came from the ARISTOPHANES (Anticoagulants for Reduction in Stroke: Observational Pooled Analysis on Health Outcomes and Experience of Patients) study, which pooled U.S. insurance claims data from several sources. For the octogenarian study, Dr. Deitelzweig and his associates used data from about 123 million U.S. residents collected between January 2012 and September 2015 by Medicare and three different commercial insurance databases. The overall level of beneficiary overlap between these four data sources was less than 0.5%.
The researchers identified patients with nonvalvular atrial fibrillation who started anticoagulant treatment with a DOAC and were at least 80 years old. This included 19,752 patients started on apixaban (Eliquis), 6,741 started on dabigatran (Pradaxa), and 27,217 started on rivaroxaban (Xarelto). A majority of the patients were at least 84 years old.
The analysis used propensity-score matching to compare similar patients and to minimize the impact of potentially confounding differences among the patients in each treatment subgroup. During a median follow-up of 7-9 months, the incidence of stroke or systemic embolism was 35% lower in the apixaban-treated patients, compared with those who received dabigatran, and 28% lower in the apixaban patients, compared with those treated with rivaroxaban, both statistically significant differences, Dr. Deitelzweig reported. The incidence of major bleeding episodes was 40% lower with apixaban than with dabigatran and 50% lower with apixaban, compared with rivaroxaban, also statistically significant differences.
When the analysis compared dabigatran with rivaroxaban it showed no statistically significant difference for the efficacy endpoint, but dabigatran produced 23% fewer major bleeds than rivaroxaban, a statistically significant difference.
These findings jibed with a recently published analysis from Dr. Deitelzweig and his associates that used data from all adults with nonvalvular atrial fibrillation started on an oral anticoagulant in an expanded ARISTOPHANES database for 2012-2015 that included more than 180 million U.S. beneficiaries. After propensity-score matching, this created subgroups of about 58,000 patients started on apixaban, nearly 27,000 started on dabigatran, and more than 83,000 started on rivaroxaban. The patients averaged about 73 years old. Again, with about 7-9 months of follow-up, very similar outcomes occurred. Patients on apixaban had significantly fewer strokes and systemic embolic events as well as significantly fewer major bleeds compared with patients treated with one of the other DOACs (Stroke. 2018 Dec;49[12]:2933-44).
The study was funded by Bristol-Myers Squibb and Pfizer, the companies that market apixaban (Eliquis). Dr. Deitelzweig is a consultant to and speaker on behalf of Bristol-Myers Squibb and Pfizer. He is also a consultant to or speaker on behalf of Boehringer Ingelheim, Daiichi-Sankyo, Janssen, and Portola Pharmaceuticals.
SOURCE: Deitelzweig SB et al. Circulation. 2018 Nov 6;138(suppl 1):A14900.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: Apixaban surpassed two other direct-acting oral anticoagulants in a large, observational database.
Major finding: The adjusted stroke or systemic embolism rate with apixaban was 35% less than dabigatran and 28% less than rivaroxaban.
Study details: A retrospective analysis of observational data collected in insurance claims from 53,710 U.S. octogenarians.
Disclosures: The study was funded by Bristol-Myers Squibb and Pfizer, the companies that market apixaban (Eliquis). Dr. Deitelzweig is a consultant to and speaker on behalf of Bristol-Myers Squibb and Pfizer. He is also a consultant to or speaker on behalf of Boehringer Ingelheim, Daiichi-Sankyo, Janssen, and Portola Pharmaceuticals.
Source: Deitelzweig SB et al. Circulation. 2018 Nov 6;138[suppl 1]:A14900.
AHA 2018: Part II
MDedge reporters Mitchel Zoler and Bruce Jancin join MDedge Cardiology Editor Catherine Hackett to continue their recap of the important highlights of the 2018 annual Scientific Sessions of the American Heart Association. You can click here to find more coverage from AHA 2018.
MDedge reporters Mitchel Zoler and Bruce Jancin join MDedge Cardiology Editor Catherine Hackett to continue their recap of the important highlights of the 2018 annual Scientific Sessions of the American Heart Association. You can click here to find more coverage from AHA 2018.
MDedge reporters Mitchel Zoler and Bruce Jancin join MDedge Cardiology Editor Catherine Hackett to continue their recap of the important highlights of the 2018 annual Scientific Sessions of the American Heart Association. You can click here to find more coverage from AHA 2018.
‘Phenomenal’ REDUCE-IT establishes triglyceride theory
CHICAGO – REDUCE-IT is a phenomenal trial and a game changer because it has shown for the first time that triglyceride reduction with an appropriate therapy – in this case icosapent ethyl – when used in appropriate doses can make a significant difference.
That’s according to Prakash C. Deedwania, MD, chief of the cardiology division at the Veterans Affairs Medical Center/University of California San Francisco Program in Fresno, who joined MDedge reporter Richard Mark Kirkner for a video interview at the American Heart Association scientific sessions.
In the large, placebo-controlled REDUCE-IT trial in patients with or at high risk for cardiovascular disease received who received 2 g of icosapent ethyl (Vascepa) twice daily or placebo saw a 25% lower risk of cardiovascular death or an ischemic event, compared with placebo.
CHICAGO – REDUCE-IT is a phenomenal trial and a game changer because it has shown for the first time that triglyceride reduction with an appropriate therapy – in this case icosapent ethyl – when used in appropriate doses can make a significant difference.
That’s according to Prakash C. Deedwania, MD, chief of the cardiology division at the Veterans Affairs Medical Center/University of California San Francisco Program in Fresno, who joined MDedge reporter Richard Mark Kirkner for a video interview at the American Heart Association scientific sessions.
In the large, placebo-controlled REDUCE-IT trial in patients with or at high risk for cardiovascular disease received who received 2 g of icosapent ethyl (Vascepa) twice daily or placebo saw a 25% lower risk of cardiovascular death or an ischemic event, compared with placebo.
CHICAGO – REDUCE-IT is a phenomenal trial and a game changer because it has shown for the first time that triglyceride reduction with an appropriate therapy – in this case icosapent ethyl – when used in appropriate doses can make a significant difference.
That’s according to Prakash C. Deedwania, MD, chief of the cardiology division at the Veterans Affairs Medical Center/University of California San Francisco Program in Fresno, who joined MDedge reporter Richard Mark Kirkner for a video interview at the American Heart Association scientific sessions.
In the large, placebo-controlled REDUCE-IT trial in patients with or at high risk for cardiovascular disease received who received 2 g of icosapent ethyl (Vascepa) twice daily or placebo saw a 25% lower risk of cardiovascular death or an ischemic event, compared with placebo.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
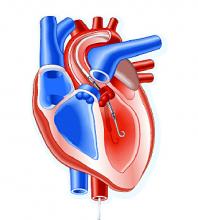
Impella heart pump may enable 30-minute reperfusion delay
CHICAGO – An investigative heart pump for unloading the left ventricle in patients who had an ST-elevation myocardial infarction (STEMI) yielded similar safety and efficacy outcomes with a 30-minute delay in reperfusion or the standard approach of immediate reperfusion.
That’s according to results of a pilot feasibility trial presented at the American Heart Association scientific sessions.
The trial, titled the DTU (Door to Unload)–STEMI trial, evaluated the Impella CP (Abiomed) device used for unloading the left ventricle (LV). “No prohibitive safety signals that would preclude proceeding to a larger pivotal study of left ventricle unloading and delaying reperfusion for 30 minutes were identified,” said principal investigator Navin Kapur, MD, of Tufts Medical Center.
The trial evaluated 50 patients who received the Impella device in two different groups: one that underwent immediate reperfusion after LV unloading, the other that had a 30-minute delay before reperfusion. The study found no significant difference in major adverse cardiovascular or cerebral events between the two groups (there were two in the delayed group vs. none in the immediate group), and no difference in infarct size increase as a percentage of LV mass at 30 days between the groups, Dr. Kapur said.
Door-to-balloon times averaged 73 minutes in the immediate reperfusion group and 97 minutes in the delayed reperfusion group, with door-to-unload times averaging around 60 minutes in both groups. “We were able to see successful enrollment and distribution across multiple sites and multiple operators, suggesting the feasibility of this approach,” Dr. Kapur said.
He noted “one of the most important messages” of the study was that no patients in either arm required percutaneous coronary intervention. “What this suggests is that, when we look at operator behavior, operators were comfortable with initiating LV unloading and waiting 30 minutes,” Dr. Kapur said.
The primary endpoint of the trial was to determine if delayed reperfusion led to an increase in infarct size. “We did not see that,” he noted. “And among patients with an anterior ST-segment elevation sum in leads V1-V4 of more than 6 mm Hg, infarct size normalized to the area at risk was significantly lower with 30 minutes of LV unloading before reperfusion, compared to LV unloading with immediate reperfusion.”
The next step is to initiate a pivotal trial of the device, Dr. Kapur said. “The findings from the DTU-STEMI pilot trial will inform the pivotal trial based on preclinical data showing that LV unloading attenuates myocardial ischemia and also preconditions the myocardium to allow it to be more receptive to reperfusion with a reduction in reperfusion injury,” he said. The pivotal trial will have two similar arms: one using the standard of care of immediate reperfusion and the other utilizing the 30-minute delay.
In his discussion of the DTU-STEMI trial, Holger Thiele, MD, of the Leipzig (Germany) Heart Institute and the University of Leipzig, expressed concern with the lack of a standard-of-care group in the trial. “Thus, the primary efficacy endpoint on infarct size cannot be reliably compared,” he said. “Based on the small sample size, there’s no reliable information on safety.”
Dr. Kapur reported financial relationships with Abiomed, Boston Scientific, Abbott, Medtronic, and MD Start. Dr. Thiele had no financial disclosures.
SOURCE: Kapur NK et al. AHA scientific sessions, LBCT-19578
CHICAGO – An investigative heart pump for unloading the left ventricle in patients who had an ST-elevation myocardial infarction (STEMI) yielded similar safety and efficacy outcomes with a 30-minute delay in reperfusion or the standard approach of immediate reperfusion.
That’s according to results of a pilot feasibility trial presented at the American Heart Association scientific sessions.
The trial, titled the DTU (Door to Unload)–STEMI trial, evaluated the Impella CP (Abiomed) device used for unloading the left ventricle (LV). “No prohibitive safety signals that would preclude proceeding to a larger pivotal study of left ventricle unloading and delaying reperfusion for 30 minutes were identified,” said principal investigator Navin Kapur, MD, of Tufts Medical Center.
The trial evaluated 50 patients who received the Impella device in two different groups: one that underwent immediate reperfusion after LV unloading, the other that had a 30-minute delay before reperfusion. The study found no significant difference in major adverse cardiovascular or cerebral events between the two groups (there were two in the delayed group vs. none in the immediate group), and no difference in infarct size increase as a percentage of LV mass at 30 days between the groups, Dr. Kapur said.
Door-to-balloon times averaged 73 minutes in the immediate reperfusion group and 97 minutes in the delayed reperfusion group, with door-to-unload times averaging around 60 minutes in both groups. “We were able to see successful enrollment and distribution across multiple sites and multiple operators, suggesting the feasibility of this approach,” Dr. Kapur said.
He noted “one of the most important messages” of the study was that no patients in either arm required percutaneous coronary intervention. “What this suggests is that, when we look at operator behavior, operators were comfortable with initiating LV unloading and waiting 30 minutes,” Dr. Kapur said.
The primary endpoint of the trial was to determine if delayed reperfusion led to an increase in infarct size. “We did not see that,” he noted. “And among patients with an anterior ST-segment elevation sum in leads V1-V4 of more than 6 mm Hg, infarct size normalized to the area at risk was significantly lower with 30 minutes of LV unloading before reperfusion, compared to LV unloading with immediate reperfusion.”
The next step is to initiate a pivotal trial of the device, Dr. Kapur said. “The findings from the DTU-STEMI pilot trial will inform the pivotal trial based on preclinical data showing that LV unloading attenuates myocardial ischemia and also preconditions the myocardium to allow it to be more receptive to reperfusion with a reduction in reperfusion injury,” he said. The pivotal trial will have two similar arms: one using the standard of care of immediate reperfusion and the other utilizing the 30-minute delay.
In his discussion of the DTU-STEMI trial, Holger Thiele, MD, of the Leipzig (Germany) Heart Institute and the University of Leipzig, expressed concern with the lack of a standard-of-care group in the trial. “Thus, the primary efficacy endpoint on infarct size cannot be reliably compared,” he said. “Based on the small sample size, there’s no reliable information on safety.”
Dr. Kapur reported financial relationships with Abiomed, Boston Scientific, Abbott, Medtronic, and MD Start. Dr. Thiele had no financial disclosures.
SOURCE: Kapur NK et al. AHA scientific sessions, LBCT-19578
CHICAGO – An investigative heart pump for unloading the left ventricle in patients who had an ST-elevation myocardial infarction (STEMI) yielded similar safety and efficacy outcomes with a 30-minute delay in reperfusion or the standard approach of immediate reperfusion.
That’s according to results of a pilot feasibility trial presented at the American Heart Association scientific sessions.
The trial, titled the DTU (Door to Unload)–STEMI trial, evaluated the Impella CP (Abiomed) device used for unloading the left ventricle (LV). “No prohibitive safety signals that would preclude proceeding to a larger pivotal study of left ventricle unloading and delaying reperfusion for 30 minutes were identified,” said principal investigator Navin Kapur, MD, of Tufts Medical Center.
The trial evaluated 50 patients who received the Impella device in two different groups: one that underwent immediate reperfusion after LV unloading, the other that had a 30-minute delay before reperfusion. The study found no significant difference in major adverse cardiovascular or cerebral events between the two groups (there were two in the delayed group vs. none in the immediate group), and no difference in infarct size increase as a percentage of LV mass at 30 days between the groups, Dr. Kapur said.
Door-to-balloon times averaged 73 minutes in the immediate reperfusion group and 97 minutes in the delayed reperfusion group, with door-to-unload times averaging around 60 minutes in both groups. “We were able to see successful enrollment and distribution across multiple sites and multiple operators, suggesting the feasibility of this approach,” Dr. Kapur said.
He noted “one of the most important messages” of the study was that no patients in either arm required percutaneous coronary intervention. “What this suggests is that, when we look at operator behavior, operators were comfortable with initiating LV unloading and waiting 30 minutes,” Dr. Kapur said.
The primary endpoint of the trial was to determine if delayed reperfusion led to an increase in infarct size. “We did not see that,” he noted. “And among patients with an anterior ST-segment elevation sum in leads V1-V4 of more than 6 mm Hg, infarct size normalized to the area at risk was significantly lower with 30 minutes of LV unloading before reperfusion, compared to LV unloading with immediate reperfusion.”
The next step is to initiate a pivotal trial of the device, Dr. Kapur said. “The findings from the DTU-STEMI pilot trial will inform the pivotal trial based on preclinical data showing that LV unloading attenuates myocardial ischemia and also preconditions the myocardium to allow it to be more receptive to reperfusion with a reduction in reperfusion injury,” he said. The pivotal trial will have two similar arms: one using the standard of care of immediate reperfusion and the other utilizing the 30-minute delay.
In his discussion of the DTU-STEMI trial, Holger Thiele, MD, of the Leipzig (Germany) Heart Institute and the University of Leipzig, expressed concern with the lack of a standard-of-care group in the trial. “Thus, the primary efficacy endpoint on infarct size cannot be reliably compared,” he said. “Based on the small sample size, there’s no reliable information on safety.”
Dr. Kapur reported financial relationships with Abiomed, Boston Scientific, Abbott, Medtronic, and MD Start. Dr. Thiele had no financial disclosures.
SOURCE: Kapur NK et al. AHA scientific sessions, LBCT-19578
REPORTING FROM AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: Door-to-balloon times averaged 73 minutes in the immediate reperfusion group and 97 minutes in the delayed reperfusion group.
Study details: A phase 1, randomized, exploratory safety and feasibility trial in 50 patients with anterior STEMI to left ventricle unloading using the Impella CP followed by immediate reperfusion versus delayed reperfusion after 30 minutes of unloading.
Disclosures: Dr. Kapur reported financial relationships with Abiomed, Boston Scientific, Abbott, Medtronic and MD Start/Precardia.
Source: Kapur NK et al. AHA scientific sessions, LBCT-19578.
CAC scores in type 1 diabetes no higher than general population
CHICAGO – Roughly 70% of some 1,200 adult patients with type 1 diabetes screened for coronary artery calcium had a score of zero, about the same prevalence as in the general, U.S. adult population, suggesting the unexpected conclusion that a majority of middle-aged patients with type 1 diabetes do not have an elevated risk for coronary artery disease, in contrast to patients with type 2 diabetes.
Among 1,205 asymptomatic people with type 1 diabetes who underwent coronary artery calcium (CAC) measurement and were followed for an average of about 11 years, 71% had a CAC score of zero at baseline followed by a cardiovascular disease event rate of 5.6 events/1,000 patient years of follow-up, a “very low” event rate that made these patients no more likely to have an event than any adult of similar age and sex in the general U.S. population, Matthew J. Budoff, MD, said at the American Heart Association scientific sessions.
In prior reports, about half of patients with type 2 diabetes had a CAC score of zero, noted Dr. Budoff, professor of medicine and a specialist in cardiac CT imaging and preventive cardiology at the University of California, Los Angeles. In a general adult population that’s about 45 years old roughly three-quarters would have a CAC score of zero, he noted.
Until now, little has been known about CAC scores in asymptomatic, middle-aged adults with type 1 diabetes. The findings reported by Dr. Budoff raise questions about the 2018 revision of the cholesterol guideline from the American College of Cardiology and American Heart Association, released during the meeting (J Am Coll Cardiol. 2018. doi: 10.1016/j.jacc.2018.11.003), which lumps type 1 and type 2 diabetes together as a special high-risk category for cholesterol management.
The guideline should instead “advocate for more therapy with a CAC score of more than 100 and less therapy with a CAC score of zero in patients with type 1 diabetes,” Dr. Budoff suggested. “A statin for someone with a CAC score of zero probably won’t result in event reduction. The 70% of patients with type 1 diabetes who have a CAC score of zero potentially may not benefit from a statin,” he said in a video interview.
Dr. Budoff and his associates used CAC scores and outcomes data collected on 1,205 asymptomatic people with type 1 diabetes enrolled in the EDIC (Epidemiology of Diabetes Interventions and Complications) trial who underwent CAC scoring as part of the study protocol when they averaged 43 years of age. Follow-up tracked the incidence of cardiovascular disease events in 1,156 of these patients for an average of about 11 years. During follow-up, 105 patients had a cardiovascular disease event, an overall rate of 8.5 events/1,000 patient years of follow-up.
The results also confirmed the prognostic power of the CAC score in these patients. Compared with the very low event rate among those with a zero score, patients with a score of 1-100 had 71% more events, patients with a CAC score of 101-300 had a 5.4-fold higher event rate as those with no coronary calcium, and patients with a CAC score of greater than 300 had a 6.9-fold higher event rate than those with no coronary calcium, Dr. Budoff reported.
Coronary calcium deposits, a direct reflection of atheroma load, can change over time, but somewhat slowly. A CAC score of zero is very reliable for predicting a very low rate of cardiovascular disease events over the subsequent 5 years, and in many people it can reliably predict for as long as 10 years, Dr. Budoff said. Beyond that, follow-up CAC scoring is necessary to check for changes in coronary status, “especially in patients with type 1 diabetes,”
SOURCE: Budoff M et al. Abstract 13133.
CHICAGO – Roughly 70% of some 1,200 adult patients with type 1 diabetes screened for coronary artery calcium had a score of zero, about the same prevalence as in the general, U.S. adult population, suggesting the unexpected conclusion that a majority of middle-aged patients with type 1 diabetes do not have an elevated risk for coronary artery disease, in contrast to patients with type 2 diabetes.
Among 1,205 asymptomatic people with type 1 diabetes who underwent coronary artery calcium (CAC) measurement and were followed for an average of about 11 years, 71% had a CAC score of zero at baseline followed by a cardiovascular disease event rate of 5.6 events/1,000 patient years of follow-up, a “very low” event rate that made these patients no more likely to have an event than any adult of similar age and sex in the general U.S. population, Matthew J. Budoff, MD, said at the American Heart Association scientific sessions.
In prior reports, about half of patients with type 2 diabetes had a CAC score of zero, noted Dr. Budoff, professor of medicine and a specialist in cardiac CT imaging and preventive cardiology at the University of California, Los Angeles. In a general adult population that’s about 45 years old roughly three-quarters would have a CAC score of zero, he noted.
Until now, little has been known about CAC scores in asymptomatic, middle-aged adults with type 1 diabetes. The findings reported by Dr. Budoff raise questions about the 2018 revision of the cholesterol guideline from the American College of Cardiology and American Heart Association, released during the meeting (J Am Coll Cardiol. 2018. doi: 10.1016/j.jacc.2018.11.003), which lumps type 1 and type 2 diabetes together as a special high-risk category for cholesterol management.
The guideline should instead “advocate for more therapy with a CAC score of more than 100 and less therapy with a CAC score of zero in patients with type 1 diabetes,” Dr. Budoff suggested. “A statin for someone with a CAC score of zero probably won’t result in event reduction. The 70% of patients with type 1 diabetes who have a CAC score of zero potentially may not benefit from a statin,” he said in a video interview.
Dr. Budoff and his associates used CAC scores and outcomes data collected on 1,205 asymptomatic people with type 1 diabetes enrolled in the EDIC (Epidemiology of Diabetes Interventions and Complications) trial who underwent CAC scoring as part of the study protocol when they averaged 43 years of age. Follow-up tracked the incidence of cardiovascular disease events in 1,156 of these patients for an average of about 11 years. During follow-up, 105 patients had a cardiovascular disease event, an overall rate of 8.5 events/1,000 patient years of follow-up.
The results also confirmed the prognostic power of the CAC score in these patients. Compared with the very low event rate among those with a zero score, patients with a score of 1-100 had 71% more events, patients with a CAC score of 101-300 had a 5.4-fold higher event rate as those with no coronary calcium, and patients with a CAC score of greater than 300 had a 6.9-fold higher event rate than those with no coronary calcium, Dr. Budoff reported.
Coronary calcium deposits, a direct reflection of atheroma load, can change over time, but somewhat slowly. A CAC score of zero is very reliable for predicting a very low rate of cardiovascular disease events over the subsequent 5 years, and in many people it can reliably predict for as long as 10 years, Dr. Budoff said. Beyond that, follow-up CAC scoring is necessary to check for changes in coronary status, “especially in patients with type 1 diabetes,”
SOURCE: Budoff M et al. Abstract 13133.
CHICAGO – Roughly 70% of some 1,200 adult patients with type 1 diabetes screened for coronary artery calcium had a score of zero, about the same prevalence as in the general, U.S. adult population, suggesting the unexpected conclusion that a majority of middle-aged patients with type 1 diabetes do not have an elevated risk for coronary artery disease, in contrast to patients with type 2 diabetes.
Among 1,205 asymptomatic people with type 1 diabetes who underwent coronary artery calcium (CAC) measurement and were followed for an average of about 11 years, 71% had a CAC score of zero at baseline followed by a cardiovascular disease event rate of 5.6 events/1,000 patient years of follow-up, a “very low” event rate that made these patients no more likely to have an event than any adult of similar age and sex in the general U.S. population, Matthew J. Budoff, MD, said at the American Heart Association scientific sessions.
In prior reports, about half of patients with type 2 diabetes had a CAC score of zero, noted Dr. Budoff, professor of medicine and a specialist in cardiac CT imaging and preventive cardiology at the University of California, Los Angeles. In a general adult population that’s about 45 years old roughly three-quarters would have a CAC score of zero, he noted.
Until now, little has been known about CAC scores in asymptomatic, middle-aged adults with type 1 diabetes. The findings reported by Dr. Budoff raise questions about the 2018 revision of the cholesterol guideline from the American College of Cardiology and American Heart Association, released during the meeting (J Am Coll Cardiol. 2018. doi: 10.1016/j.jacc.2018.11.003), which lumps type 1 and type 2 diabetes together as a special high-risk category for cholesterol management.
The guideline should instead “advocate for more therapy with a CAC score of more than 100 and less therapy with a CAC score of zero in patients with type 1 diabetes,” Dr. Budoff suggested. “A statin for someone with a CAC score of zero probably won’t result in event reduction. The 70% of patients with type 1 diabetes who have a CAC score of zero potentially may not benefit from a statin,” he said in a video interview.
Dr. Budoff and his associates used CAC scores and outcomes data collected on 1,205 asymptomatic people with type 1 diabetes enrolled in the EDIC (Epidemiology of Diabetes Interventions and Complications) trial who underwent CAC scoring as part of the study protocol when they averaged 43 years of age. Follow-up tracked the incidence of cardiovascular disease events in 1,156 of these patients for an average of about 11 years. During follow-up, 105 patients had a cardiovascular disease event, an overall rate of 8.5 events/1,000 patient years of follow-up.
The results also confirmed the prognostic power of the CAC score in these patients. Compared with the very low event rate among those with a zero score, patients with a score of 1-100 had 71% more events, patients with a CAC score of 101-300 had a 5.4-fold higher event rate as those with no coronary calcium, and patients with a CAC score of greater than 300 had a 6.9-fold higher event rate than those with no coronary calcium, Dr. Budoff reported.
Coronary calcium deposits, a direct reflection of atheroma load, can change over time, but somewhat slowly. A CAC score of zero is very reliable for predicting a very low rate of cardiovascular disease events over the subsequent 5 years, and in many people it can reliably predict for as long as 10 years, Dr. Budoff said. Beyond that, follow-up CAC scoring is necessary to check for changes in coronary status, “especially in patients with type 1 diabetes,”
SOURCE: Budoff M et al. Abstract 13133.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: .
Major finding: Seventy-one percent of patients with type 1 diabetes had a coronary artery calcium score of zero.
Study details: Review of data collected from 1,205 patients in the EDIC trial.
Disclosures: The EDIC trial had no commercial funding. Dr. Budoff has received research funding from General Electric.
Source: Budoff M et al. AHA 2018, Abstract 13133.
Empagliflozin reduces left ventricular mass
CHICAGO – Empagliflozin significantly reduced left ventricular mass compared with placebo over the course of 6 months in patients with type 2 diabetes and stable coronary artery disease in the randomized EMPA-HEART CardioLink-6 trial.
Use of empagliflozin (Jardiance), a sodium-glucose cotransporter 2 inhibitor (SGLT2i), also was associated with a clinically meaningful reduction in ambulatory systolic blood pressure and a boost in hematocrit in this population of normotensive patients with preserved left ventricular ejection fraction and high utilization of background guideline-directed medical therapy, Subodh Verma, MD, reported at the American Heart Association scientific sessions.
“Taken together, these data suggest that empagliflozin promotes early statistically and clinically significant reverse remodeling, which may contribute to the cardiovascular and heart failure benefits observed in the EMPA-REG OUTCOME trial and other SGLT2i studies,” added Dr. Verma, professor of surgery, pharmacology, and toxicology at the University of Toronto.
EMPA-REG OUTCOME was a landmark randomized trial that included 7,020 patients with type 2 diabetes and established ischemic cardiovascular disease in which the SGLT2i reduced all-cause mortality by 32%, compared with placebo over a median 3.1 years of follow-up, cardiovascular mortality by 38%, and hospitalizations for heart failure by 35% (N Engl J Med. 2015 Nov 26;373[22]:2117-28).
The mechanism responsible for these impressive clinical benefits has been unclear. The EMPA-HEART CardioLink-6 trial was a small study – 97 randomized patients – designed to shed light on this issue. The hypothesis was that SGLT2i therapy facilitates cardiac reverse remodeling. This indeed turned out to be the case when cardiac MRI findings at baseline and after 6 months were compared by blinded evaluators.
From a baseline mean left ventricular mass indexed to body surface area of 60 g/m2, which is within normal range, left ventricular mass decreased by a mean of 4.71 g in the empagliflozin group, compared with a mere 0.39-g reduction in placebo-treated controls.
Dr. Verma underscored the importance of this result: “Left ventricular mass is a strong and independent predictor of major cardiovascular events, including cardiovascular and all-cause mortality, myocardial infarction, and heart failure. Furthermore, the magnitude of left ventricular mass regression correlates with the extent of clinical outcome benefit seen with pharmacological and device therapies.”
In a prespecified subgroup analysis stratified by baseline LV mass index, patients with a baseline value greater than 60 g/m2 experienced a much greater benefit from empagliflozin, with a mean between-group difference in LV mass index reduction of 7.26 g/m2, compared with a 0.46-g/m2 difference between the SGLT2i and placebo among those with a baseline LV mass index of 60 g/m2 or less.
Ambulatory systolic blood pressure fell from a baseline of 139 mm Hg by a mean of 7.9 mm Hg in the empagliflozin group and 0.7 mm Hg with placebo. From a baseline hematocrit of 42%, hematocrit improved by an absolute 1.91% more with empagliflozin than placebo. However, there were no significant between-group differences in the secondary cardiac MRI outcomes of change in LV end-systolic volume index, LV end-diastolic volume index, or LV ejection fraction.
Discussant Elliott M. Antman, MD, hailed EMPA-HEART CardioLink-6 as “a very important mechanistic study.”
“As I leave Chicago for home, I plan to further increase the use of SGLT2 inhibitors in my patients with type 2 diabetes, especially if they have a history of heart failure, and especially if they have coronary artery disease. I would encourage you to think about doing the same, and I would also recommend that we urge our colleagues in general medicine, endocrinology, and nephrology to consider this information as well,” said Dr. Antman, professor of medicine and associate dean for clinical and translational research at Harvard Medical School, Boston, as well as an AHA past president.
He noted that EMPA-HEART CardioLink-6 provides “biologically plausible data” to explain the mechanism for the major clinical benefits of empagliflozin earlier documented in EMPA-REG OUTCOME. The likely driver of the reduction in left ventricular mass seen in EMPA-HEART CardioLink-6 was the combination of lower systolic blood pressure and higher hematocrit.
“These surrogates suggest that our traditional concepts of afterload and preload appear to be favorably affected by SGLT2 inhibition,” according to the cardiologist.
The EMPA-HEART CardioLink-6 study was funded by Boehringer Ingelheim. Dr. Verma reported receiving research support and/or speaker payments from that pharmaceutical company and roughly a dozen others. Dr. Antman had no disclosures.
SOURCE: Verma S. AHA 2018, Abstract 19332.
CHICAGO – Empagliflozin significantly reduced left ventricular mass compared with placebo over the course of 6 months in patients with type 2 diabetes and stable coronary artery disease in the randomized EMPA-HEART CardioLink-6 trial.
Use of empagliflozin (Jardiance), a sodium-glucose cotransporter 2 inhibitor (SGLT2i), also was associated with a clinically meaningful reduction in ambulatory systolic blood pressure and a boost in hematocrit in this population of normotensive patients with preserved left ventricular ejection fraction and high utilization of background guideline-directed medical therapy, Subodh Verma, MD, reported at the American Heart Association scientific sessions.
“Taken together, these data suggest that empagliflozin promotes early statistically and clinically significant reverse remodeling, which may contribute to the cardiovascular and heart failure benefits observed in the EMPA-REG OUTCOME trial and other SGLT2i studies,” added Dr. Verma, professor of surgery, pharmacology, and toxicology at the University of Toronto.
EMPA-REG OUTCOME was a landmark randomized trial that included 7,020 patients with type 2 diabetes and established ischemic cardiovascular disease in which the SGLT2i reduced all-cause mortality by 32%, compared with placebo over a median 3.1 years of follow-up, cardiovascular mortality by 38%, and hospitalizations for heart failure by 35% (N Engl J Med. 2015 Nov 26;373[22]:2117-28).
The mechanism responsible for these impressive clinical benefits has been unclear. The EMPA-HEART CardioLink-6 trial was a small study – 97 randomized patients – designed to shed light on this issue. The hypothesis was that SGLT2i therapy facilitates cardiac reverse remodeling. This indeed turned out to be the case when cardiac MRI findings at baseline and after 6 months were compared by blinded evaluators.
From a baseline mean left ventricular mass indexed to body surface area of 60 g/m2, which is within normal range, left ventricular mass decreased by a mean of 4.71 g in the empagliflozin group, compared with a mere 0.39-g reduction in placebo-treated controls.
Dr. Verma underscored the importance of this result: “Left ventricular mass is a strong and independent predictor of major cardiovascular events, including cardiovascular and all-cause mortality, myocardial infarction, and heart failure. Furthermore, the magnitude of left ventricular mass regression correlates with the extent of clinical outcome benefit seen with pharmacological and device therapies.”
In a prespecified subgroup analysis stratified by baseline LV mass index, patients with a baseline value greater than 60 g/m2 experienced a much greater benefit from empagliflozin, with a mean between-group difference in LV mass index reduction of 7.26 g/m2, compared with a 0.46-g/m2 difference between the SGLT2i and placebo among those with a baseline LV mass index of 60 g/m2 or less.
Ambulatory systolic blood pressure fell from a baseline of 139 mm Hg by a mean of 7.9 mm Hg in the empagliflozin group and 0.7 mm Hg with placebo. From a baseline hematocrit of 42%, hematocrit improved by an absolute 1.91% more with empagliflozin than placebo. However, there were no significant between-group differences in the secondary cardiac MRI outcomes of change in LV end-systolic volume index, LV end-diastolic volume index, or LV ejection fraction.
Discussant Elliott M. Antman, MD, hailed EMPA-HEART CardioLink-6 as “a very important mechanistic study.”
“As I leave Chicago for home, I plan to further increase the use of SGLT2 inhibitors in my patients with type 2 diabetes, especially if they have a history of heart failure, and especially if they have coronary artery disease. I would encourage you to think about doing the same, and I would also recommend that we urge our colleagues in general medicine, endocrinology, and nephrology to consider this information as well,” said Dr. Antman, professor of medicine and associate dean for clinical and translational research at Harvard Medical School, Boston, as well as an AHA past president.
He noted that EMPA-HEART CardioLink-6 provides “biologically plausible data” to explain the mechanism for the major clinical benefits of empagliflozin earlier documented in EMPA-REG OUTCOME. The likely driver of the reduction in left ventricular mass seen in EMPA-HEART CardioLink-6 was the combination of lower systolic blood pressure and higher hematocrit.
“These surrogates suggest that our traditional concepts of afterload and preload appear to be favorably affected by SGLT2 inhibition,” according to the cardiologist.
The EMPA-HEART CardioLink-6 study was funded by Boehringer Ingelheim. Dr. Verma reported receiving research support and/or speaker payments from that pharmaceutical company and roughly a dozen others. Dr. Antman had no disclosures.
SOURCE: Verma S. AHA 2018, Abstract 19332.
CHICAGO – Empagliflozin significantly reduced left ventricular mass compared with placebo over the course of 6 months in patients with type 2 diabetes and stable coronary artery disease in the randomized EMPA-HEART CardioLink-6 trial.
Use of empagliflozin (Jardiance), a sodium-glucose cotransporter 2 inhibitor (SGLT2i), also was associated with a clinically meaningful reduction in ambulatory systolic blood pressure and a boost in hematocrit in this population of normotensive patients with preserved left ventricular ejection fraction and high utilization of background guideline-directed medical therapy, Subodh Verma, MD, reported at the American Heart Association scientific sessions.
“Taken together, these data suggest that empagliflozin promotes early statistically and clinically significant reverse remodeling, which may contribute to the cardiovascular and heart failure benefits observed in the EMPA-REG OUTCOME trial and other SGLT2i studies,” added Dr. Verma, professor of surgery, pharmacology, and toxicology at the University of Toronto.
EMPA-REG OUTCOME was a landmark randomized trial that included 7,020 patients with type 2 diabetes and established ischemic cardiovascular disease in which the SGLT2i reduced all-cause mortality by 32%, compared with placebo over a median 3.1 years of follow-up, cardiovascular mortality by 38%, and hospitalizations for heart failure by 35% (N Engl J Med. 2015 Nov 26;373[22]:2117-28).
The mechanism responsible for these impressive clinical benefits has been unclear. The EMPA-HEART CardioLink-6 trial was a small study – 97 randomized patients – designed to shed light on this issue. The hypothesis was that SGLT2i therapy facilitates cardiac reverse remodeling. This indeed turned out to be the case when cardiac MRI findings at baseline and after 6 months were compared by blinded evaluators.
From a baseline mean left ventricular mass indexed to body surface area of 60 g/m2, which is within normal range, left ventricular mass decreased by a mean of 4.71 g in the empagliflozin group, compared with a mere 0.39-g reduction in placebo-treated controls.
Dr. Verma underscored the importance of this result: “Left ventricular mass is a strong and independent predictor of major cardiovascular events, including cardiovascular and all-cause mortality, myocardial infarction, and heart failure. Furthermore, the magnitude of left ventricular mass regression correlates with the extent of clinical outcome benefit seen with pharmacological and device therapies.”
In a prespecified subgroup analysis stratified by baseline LV mass index, patients with a baseline value greater than 60 g/m2 experienced a much greater benefit from empagliflozin, with a mean between-group difference in LV mass index reduction of 7.26 g/m2, compared with a 0.46-g/m2 difference between the SGLT2i and placebo among those with a baseline LV mass index of 60 g/m2 or less.
Ambulatory systolic blood pressure fell from a baseline of 139 mm Hg by a mean of 7.9 mm Hg in the empagliflozin group and 0.7 mm Hg with placebo. From a baseline hematocrit of 42%, hematocrit improved by an absolute 1.91% more with empagliflozin than placebo. However, there were no significant between-group differences in the secondary cardiac MRI outcomes of change in LV end-systolic volume index, LV end-diastolic volume index, or LV ejection fraction.
Discussant Elliott M. Antman, MD, hailed EMPA-HEART CardioLink-6 as “a very important mechanistic study.”
“As I leave Chicago for home, I plan to further increase the use of SGLT2 inhibitors in my patients with type 2 diabetes, especially if they have a history of heart failure, and especially if they have coronary artery disease. I would encourage you to think about doing the same, and I would also recommend that we urge our colleagues in general medicine, endocrinology, and nephrology to consider this information as well,” said Dr. Antman, professor of medicine and associate dean for clinical and translational research at Harvard Medical School, Boston, as well as an AHA past president.
He noted that EMPA-HEART CardioLink-6 provides “biologically plausible data” to explain the mechanism for the major clinical benefits of empagliflozin earlier documented in EMPA-REG OUTCOME. The likely driver of the reduction in left ventricular mass seen in EMPA-HEART CardioLink-6 was the combination of lower systolic blood pressure and higher hematocrit.
“These surrogates suggest that our traditional concepts of afterload and preload appear to be favorably affected by SGLT2 inhibition,” according to the cardiologist.
The EMPA-HEART CardioLink-6 study was funded by Boehringer Ingelheim. Dr. Verma reported receiving research support and/or speaker payments from that pharmaceutical company and roughly a dozen others. Dr. Antman had no disclosures.
SOURCE: Verma S. AHA 2018, Abstract 19332.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: .
Major finding: Six months of empagliflozin reduced left ventricular mass by a mean of 4.71 g, vs. 0.39 g with placebo.
Study details: This 97-patient, 6-month, randomized trial evaluated the impact of SGLT2 inhibition with empagliflozin on left ventricular remodeling.
Disclosures: The EMPA-HEART CardioLink-6 study was funded by Boehringer Ingelheim. The presenter reported receiving research support and/or speaker payments from that pharmaceutical company and roughly a dozen others. Source: Verma S. AHA 2018, Abstract 19332.
New HHS physical activity guidelines break fresh ground
CHICAGO – The newly released comprehensive second edition of the federal physical activity guidelines have a lofty goal.
Adm. Brett P. Giroir, MD, declared in introducing the recommendations at the American Heart Association scientific sessions.
“Physical activity is one of the most effective preventive health interventions available, and we need more emphasis on prevention as we transition to a value-based reimbursement structure that rewards better health maintenance and avoids chronic conditions,” added Adm. Giroir, assistant secretary for health at the U.S. Department of Health & Human Services.
Although the agency opted to unveil the new guidelines before an audience of cardiologists at the AHA scientific sessions, the report includes sections relevant for a wide range of medical specialists, including primary care physicians, pediatricians, psychiatrists, neurologists, endocrinologists, and geriatricians.
Before launching into a description of what’s new in the second edition, Adm. Giroir set the stage with blunt talk about the nation’s poor state of physical fitness.
“Inactivity causes 10% of premature mortality in the United States. That means if we can just get 25% of inactive people to be active and meet the recommendations, almost 75,000 deaths per year would be prevented in the United States. And on an even larger scale worldwide, if 25% of those same people who are inactive started moving and met the guidelines, more than 1.3 million deaths would be prevented,” according to Adm. Giroir.
At present, only 26% of men, 19% of women, and 20% of teenagers meet the physical activity recommendations.
Failure to meet the federal aerobic physical activity recommendations accounts for an estimated nearly $117 billion in annual health care costs. And it poses a national security threat, too: Nearly one-third of all 17- to 24-year-olds are disqualified from military service because of obesity. Even more eye-opening, he continued, is that fully 71% of all 17- to 24-year-olds are ineligible for military service because of obesity, lack of physical fitness, lack of education, or substance use.
The actual recommendations contained in the second edition of the Physical Activity Guidelines for Americans remain unchanged from those in the first, issued a decade earlier. That is, in order to gain substantial health benefits, adults and adolescents should engage in at least 150-300 min/week of moderate intensity aerobic physical activity or 75-150 min/week of vigorous intensity aerobic activity. Plus they should do muscle-strengthening exercises such as weight lifting or push-ups at moderate or greater intensity at least 2 days/week.
Asked why the guidelines are sticking with time-based physical activity recommendations in an era when popular smartwatches and other mobile devices can readily spit out number of steps walked, calories burned, and heart-rate data, cardiologist William E. Kraus, MD, one of the 17 members of the scientific advisory committee who reviewed and graded the scientific evidence on physical activity, sedentary behavior, and health, answered. He said the group’s careful review concluded that “there’s just not enough evidence at this time to make a recommendation” with regard to mobile device–based measurements of physical activity and their relationship with health benefits.
“We’re hoping to spur more research in this area, so that the next time we make recommendations, that can be incorporated,” added Dr. Kraus, a professor of medicine and cardiologist at Duke University, Durham, N.C., as well as president-elect of the American College of Sports Medicine.
What’s new in the guidelines
“This edition tells us that it’s easier to meet the recommendations in the physical activity guidelines,” according to Adm. Giroir. “The new guidelines demonstrate, based on the best science, everyone can dramatically improve their health just by moving: anytime, anywhere, and by any means that gets you active.” He broke the guidelines down as follows:
- We have new evidence about the risks of sedentary behavior, and new evidence that any amount – any amount – of moderate to vigorous physical activity, like walking, dancing, line dancing if you’re from Texas, and household chores is beneficial,” Adm. Giroir observed.
- While the first edition of the federal guidelines cited strong evidence that physical activity reduces the risk of two types of cancer, breast and colon, the intervening decade has brought forth strong evidence of a protective effect against an additional six types of cancer: bladder, endometrial, kidney, stomach, esophageal, and lung cancer.
- The guidelines formulate for the first time physical activity standards for children aged 3-5 years. The recommended target is at least 3 hr/day of varied physical activity, consistent with existing guidelines in Australia Canada, and the United Kingdom.
- Updated recommendations for children aged 6-17 years call for an hour or more/day of moderate- or vigorous-intensity physical activity on a daily basis, with that activity level falling within the vigorous category on at least 3 days/week. Plus, it recommends bone- and muscle-strengthening activity on at least 3 days.
- The pediatric guidelines are linked to a planned HHS national strategy to expand children’s participation in youth sports as part of an effort to curb childhood obesity, rates of which have more than tripled since the 1970s.
“We’ll soon announce funding opportunities for communities to increase participation in sports among children and teens through participation in affordable programs with trained coaches,” said Dr. Giroir, a pediatrician.
The new guidelines endorse what is called “the comprehensive school physical activity model.”
“I strongly believe our schools should take action to implement this approach. There is a lot of interest right now to affect change in the schools across our country. Part of the answer, I think, is to provide kids with high-quality physical education, but I think we recognize that alone will not be enough.” The comprehensive school activity model calls for not only enriching school PE programs but also incorporating active transport to school, classroom activity, active learning, and after school programs – activity in all settings during the school day. “I’m very hopeful that this model, which is endorsed in the guidelines document, will be widely adopted by schools in this country over the next decade,” Dr. Giroir said.
The first edition declared that only bouts of physical activity of at least 10 minutes duration should count toward meeting the guidelines. That requirement is gone in the second edition. It was an impediment to being active, and upon close examination it wasn’t based on scientific evidence. That means taking the stairs instead of the escalator or parking farther away from the store count toward the weekly physical activity goal, Dr. Kraus said.
“It makes it easier to achieve the guidelines and to encourage Americans to move more and sit less just by making a better choice at many times during the day,” observed Dr. Giroir, a four-star admiral in the U.S. Public Health Service Commissioned Corps.
The latest guidelines contain up-to-date information on the benefits of regular physical activity in terms of brain health, including reduced risk of developing Alzheimer’s disease, and improved cognition, including performance on academic achievement tests and measures of executive function, memory, and processing speed, in preadolescent children as well as older adults. Solid evidence also is cited for improved cognition in patients with MS, dementia, ADHD, and Parkinson’s disease.
The guidelines provide new recommendations for physical activity for women during pregnancy and post partum.
A section of the guidelines is devoted to proven evidence-based strategies to promote physical activity at the individual, small group, and community level.
Physicians now have a resource to aid them in prescribing an individualized physical activity prescription for their patients with existing health conditions, including osteoarthritis, type 2 diabetes, cancer survivors, and physical disabilities.
The new physical activity guidelines and related resources for health care professionals are available at the Health.gov website.
SOURCE: Giroir BP. AHA Scientific Sessions, Session ME.05.
CHICAGO – The newly released comprehensive second edition of the federal physical activity guidelines have a lofty goal.
Adm. Brett P. Giroir, MD, declared in introducing the recommendations at the American Heart Association scientific sessions.
“Physical activity is one of the most effective preventive health interventions available, and we need more emphasis on prevention as we transition to a value-based reimbursement structure that rewards better health maintenance and avoids chronic conditions,” added Adm. Giroir, assistant secretary for health at the U.S. Department of Health & Human Services.
Although the agency opted to unveil the new guidelines before an audience of cardiologists at the AHA scientific sessions, the report includes sections relevant for a wide range of medical specialists, including primary care physicians, pediatricians, psychiatrists, neurologists, endocrinologists, and geriatricians.
Before launching into a description of what’s new in the second edition, Adm. Giroir set the stage with blunt talk about the nation’s poor state of physical fitness.
“Inactivity causes 10% of premature mortality in the United States. That means if we can just get 25% of inactive people to be active and meet the recommendations, almost 75,000 deaths per year would be prevented in the United States. And on an even larger scale worldwide, if 25% of those same people who are inactive started moving and met the guidelines, more than 1.3 million deaths would be prevented,” according to Adm. Giroir.
At present, only 26% of men, 19% of women, and 20% of teenagers meet the physical activity recommendations.
Failure to meet the federal aerobic physical activity recommendations accounts for an estimated nearly $117 billion in annual health care costs. And it poses a national security threat, too: Nearly one-third of all 17- to 24-year-olds are disqualified from military service because of obesity. Even more eye-opening, he continued, is that fully 71% of all 17- to 24-year-olds are ineligible for military service because of obesity, lack of physical fitness, lack of education, or substance use.
The actual recommendations contained in the second edition of the Physical Activity Guidelines for Americans remain unchanged from those in the first, issued a decade earlier. That is, in order to gain substantial health benefits, adults and adolescents should engage in at least 150-300 min/week of moderate intensity aerobic physical activity or 75-150 min/week of vigorous intensity aerobic activity. Plus they should do muscle-strengthening exercises such as weight lifting or push-ups at moderate or greater intensity at least 2 days/week.
Asked why the guidelines are sticking with time-based physical activity recommendations in an era when popular smartwatches and other mobile devices can readily spit out number of steps walked, calories burned, and heart-rate data, cardiologist William E. Kraus, MD, one of the 17 members of the scientific advisory committee who reviewed and graded the scientific evidence on physical activity, sedentary behavior, and health, answered. He said the group’s careful review concluded that “there’s just not enough evidence at this time to make a recommendation” with regard to mobile device–based measurements of physical activity and their relationship with health benefits.
“We’re hoping to spur more research in this area, so that the next time we make recommendations, that can be incorporated,” added Dr. Kraus, a professor of medicine and cardiologist at Duke University, Durham, N.C., as well as president-elect of the American College of Sports Medicine.
What’s new in the guidelines
“This edition tells us that it’s easier to meet the recommendations in the physical activity guidelines,” according to Adm. Giroir. “The new guidelines demonstrate, based on the best science, everyone can dramatically improve their health just by moving: anytime, anywhere, and by any means that gets you active.” He broke the guidelines down as follows:
- We have new evidence about the risks of sedentary behavior, and new evidence that any amount – any amount – of moderate to vigorous physical activity, like walking, dancing, line dancing if you’re from Texas, and household chores is beneficial,” Adm. Giroir observed.
- While the first edition of the federal guidelines cited strong evidence that physical activity reduces the risk of two types of cancer, breast and colon, the intervening decade has brought forth strong evidence of a protective effect against an additional six types of cancer: bladder, endometrial, kidney, stomach, esophageal, and lung cancer.
- The guidelines formulate for the first time physical activity standards for children aged 3-5 years. The recommended target is at least 3 hr/day of varied physical activity, consistent with existing guidelines in Australia Canada, and the United Kingdom.
- Updated recommendations for children aged 6-17 years call for an hour or more/day of moderate- or vigorous-intensity physical activity on a daily basis, with that activity level falling within the vigorous category on at least 3 days/week. Plus, it recommends bone- and muscle-strengthening activity on at least 3 days.
- The pediatric guidelines are linked to a planned HHS national strategy to expand children’s participation in youth sports as part of an effort to curb childhood obesity, rates of which have more than tripled since the 1970s.
“We’ll soon announce funding opportunities for communities to increase participation in sports among children and teens through participation in affordable programs with trained coaches,” said Dr. Giroir, a pediatrician.
The new guidelines endorse what is called “the comprehensive school physical activity model.”
“I strongly believe our schools should take action to implement this approach. There is a lot of interest right now to affect change in the schools across our country. Part of the answer, I think, is to provide kids with high-quality physical education, but I think we recognize that alone will not be enough.” The comprehensive school activity model calls for not only enriching school PE programs but also incorporating active transport to school, classroom activity, active learning, and after school programs – activity in all settings during the school day. “I’m very hopeful that this model, which is endorsed in the guidelines document, will be widely adopted by schools in this country over the next decade,” Dr. Giroir said.
The first edition declared that only bouts of physical activity of at least 10 minutes duration should count toward meeting the guidelines. That requirement is gone in the second edition. It was an impediment to being active, and upon close examination it wasn’t based on scientific evidence. That means taking the stairs instead of the escalator or parking farther away from the store count toward the weekly physical activity goal, Dr. Kraus said.
“It makes it easier to achieve the guidelines and to encourage Americans to move more and sit less just by making a better choice at many times during the day,” observed Dr. Giroir, a four-star admiral in the U.S. Public Health Service Commissioned Corps.
The latest guidelines contain up-to-date information on the benefits of regular physical activity in terms of brain health, including reduced risk of developing Alzheimer’s disease, and improved cognition, including performance on academic achievement tests and measures of executive function, memory, and processing speed, in preadolescent children as well as older adults. Solid evidence also is cited for improved cognition in patients with MS, dementia, ADHD, and Parkinson’s disease.
The guidelines provide new recommendations for physical activity for women during pregnancy and post partum.
A section of the guidelines is devoted to proven evidence-based strategies to promote physical activity at the individual, small group, and community level.
Physicians now have a resource to aid them in prescribing an individualized physical activity prescription for their patients with existing health conditions, including osteoarthritis, type 2 diabetes, cancer survivors, and physical disabilities.
The new physical activity guidelines and related resources for health care professionals are available at the Health.gov website.
SOURCE: Giroir BP. AHA Scientific Sessions, Session ME.05.
CHICAGO – The newly released comprehensive second edition of the federal physical activity guidelines have a lofty goal.
Adm. Brett P. Giroir, MD, declared in introducing the recommendations at the American Heart Association scientific sessions.
“Physical activity is one of the most effective preventive health interventions available, and we need more emphasis on prevention as we transition to a value-based reimbursement structure that rewards better health maintenance and avoids chronic conditions,” added Adm. Giroir, assistant secretary for health at the U.S. Department of Health & Human Services.
Although the agency opted to unveil the new guidelines before an audience of cardiologists at the AHA scientific sessions, the report includes sections relevant for a wide range of medical specialists, including primary care physicians, pediatricians, psychiatrists, neurologists, endocrinologists, and geriatricians.
Before launching into a description of what’s new in the second edition, Adm. Giroir set the stage with blunt talk about the nation’s poor state of physical fitness.
“Inactivity causes 10% of premature mortality in the United States. That means if we can just get 25% of inactive people to be active and meet the recommendations, almost 75,000 deaths per year would be prevented in the United States. And on an even larger scale worldwide, if 25% of those same people who are inactive started moving and met the guidelines, more than 1.3 million deaths would be prevented,” according to Adm. Giroir.
At present, only 26% of men, 19% of women, and 20% of teenagers meet the physical activity recommendations.
Failure to meet the federal aerobic physical activity recommendations accounts for an estimated nearly $117 billion in annual health care costs. And it poses a national security threat, too: Nearly one-third of all 17- to 24-year-olds are disqualified from military service because of obesity. Even more eye-opening, he continued, is that fully 71% of all 17- to 24-year-olds are ineligible for military service because of obesity, lack of physical fitness, lack of education, or substance use.
The actual recommendations contained in the second edition of the Physical Activity Guidelines for Americans remain unchanged from those in the first, issued a decade earlier. That is, in order to gain substantial health benefits, adults and adolescents should engage in at least 150-300 min/week of moderate intensity aerobic physical activity or 75-150 min/week of vigorous intensity aerobic activity. Plus they should do muscle-strengthening exercises such as weight lifting or push-ups at moderate or greater intensity at least 2 days/week.
Asked why the guidelines are sticking with time-based physical activity recommendations in an era when popular smartwatches and other mobile devices can readily spit out number of steps walked, calories burned, and heart-rate data, cardiologist William E. Kraus, MD, one of the 17 members of the scientific advisory committee who reviewed and graded the scientific evidence on physical activity, sedentary behavior, and health, answered. He said the group’s careful review concluded that “there’s just not enough evidence at this time to make a recommendation” with regard to mobile device–based measurements of physical activity and their relationship with health benefits.
“We’re hoping to spur more research in this area, so that the next time we make recommendations, that can be incorporated,” added Dr. Kraus, a professor of medicine and cardiologist at Duke University, Durham, N.C., as well as president-elect of the American College of Sports Medicine.
What’s new in the guidelines
“This edition tells us that it’s easier to meet the recommendations in the physical activity guidelines,” according to Adm. Giroir. “The new guidelines demonstrate, based on the best science, everyone can dramatically improve their health just by moving: anytime, anywhere, and by any means that gets you active.” He broke the guidelines down as follows:
- We have new evidence about the risks of sedentary behavior, and new evidence that any amount – any amount – of moderate to vigorous physical activity, like walking, dancing, line dancing if you’re from Texas, and household chores is beneficial,” Adm. Giroir observed.
- While the first edition of the federal guidelines cited strong evidence that physical activity reduces the risk of two types of cancer, breast and colon, the intervening decade has brought forth strong evidence of a protective effect against an additional six types of cancer: bladder, endometrial, kidney, stomach, esophageal, and lung cancer.
- The guidelines formulate for the first time physical activity standards for children aged 3-5 years. The recommended target is at least 3 hr/day of varied physical activity, consistent with existing guidelines in Australia Canada, and the United Kingdom.
- Updated recommendations for children aged 6-17 years call for an hour or more/day of moderate- or vigorous-intensity physical activity on a daily basis, with that activity level falling within the vigorous category on at least 3 days/week. Plus, it recommends bone- and muscle-strengthening activity on at least 3 days.
- The pediatric guidelines are linked to a planned HHS national strategy to expand children’s participation in youth sports as part of an effort to curb childhood obesity, rates of which have more than tripled since the 1970s.
“We’ll soon announce funding opportunities for communities to increase participation in sports among children and teens through participation in affordable programs with trained coaches,” said Dr. Giroir, a pediatrician.
The new guidelines endorse what is called “the comprehensive school physical activity model.”
“I strongly believe our schools should take action to implement this approach. There is a lot of interest right now to affect change in the schools across our country. Part of the answer, I think, is to provide kids with high-quality physical education, but I think we recognize that alone will not be enough.” The comprehensive school activity model calls for not only enriching school PE programs but also incorporating active transport to school, classroom activity, active learning, and after school programs – activity in all settings during the school day. “I’m very hopeful that this model, which is endorsed in the guidelines document, will be widely adopted by schools in this country over the next decade,” Dr. Giroir said.
The first edition declared that only bouts of physical activity of at least 10 minutes duration should count toward meeting the guidelines. That requirement is gone in the second edition. It was an impediment to being active, and upon close examination it wasn’t based on scientific evidence. That means taking the stairs instead of the escalator or parking farther away from the store count toward the weekly physical activity goal, Dr. Kraus said.
“It makes it easier to achieve the guidelines and to encourage Americans to move more and sit less just by making a better choice at many times during the day,” observed Dr. Giroir, a four-star admiral in the U.S. Public Health Service Commissioned Corps.
The latest guidelines contain up-to-date information on the benefits of regular physical activity in terms of brain health, including reduced risk of developing Alzheimer’s disease, and improved cognition, including performance on academic achievement tests and measures of executive function, memory, and processing speed, in preadolescent children as well as older adults. Solid evidence also is cited for improved cognition in patients with MS, dementia, ADHD, and Parkinson’s disease.
The guidelines provide new recommendations for physical activity for women during pregnancy and post partum.
A section of the guidelines is devoted to proven evidence-based strategies to promote physical activity at the individual, small group, and community level.
Physicians now have a resource to aid them in prescribing an individualized physical activity prescription for their patients with existing health conditions, including osteoarthritis, type 2 diabetes, cancer survivors, and physical disabilities.
The new physical activity guidelines and related resources for health care professionals are available at the Health.gov website.
SOURCE: Giroir BP. AHA Scientific Sessions, Session ME.05.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
AHA 2018: Part I
Endoscopic vein-graft harvest equals open harvest at 3 years
CHICAGO – Patients who underwent coronary artery bypass grafting using saphenous veins harvested endoscopically had similar clinical outcomes after nearly 3 years of follow-up as those seen with patients who received vein grafts taken by open harvesting in a multicenter, randomized trial in the United States with 1,150 patients.
As expected, follow-up also showed that endoscopic vein-graft harvesting (EVH) resulted in about half the number of wound infections as did open vein-graft harvesting (OVH). This combination of similar clinical outcomes after a median 2.8 years of follow-up, as well as fewer leg-wound adverse events, makes EVH “the preferred vein-harvesting modality,” Marco A. Zenati, MD, said at the American Heart Association scientific sessions.
Although patients far and away prefer EVH because of the reduced pain and faster healing, questions about its clinical efficacy when compared with that of OVH have lingered. That’s because observational data published almost a decade ago taken from the PREVENT IV (Project of Ex-Vivo Vein Graft Engineering via Transfection IV) trial suggested that patients who underwent coronary artery bypass grafting (CABG) using vein grafts collected by EVH had more vein-graft failures after 12-18 months and a higher rate of death, MI, or need for revascularization after 3 years, compared with patients treated using OVH (N Engl J Med. 2009 July 16;361[3]:235-44).
The results from the prospective, randomized trial reported by Dr. Zenati “take the cloud away from endovascular vein-graft harvesting that PREVENT IV had made,” commented Timothy J. Gardner, MD, a cardiac surgeon who chaired the session.
“I think this answers the question,” commented Marc Ruel, MD, a professor of surgery and the chief of cardiac surgery at the University of Ottawa. “The results show that endoscopic harvesting of vein grafts is as good as open harvesting for preventing major adverse cardiac events, which is the goal of CABG. This is a definitive trial, with no trend toward more events with endoscopic harvested vein grafts,” said Dr. Ruel, the designated discussant for Dr. Zenati’s report.
However, the study did have some significant limitations, Dr. Ruel added. The new, randomized trial, run at 16 U.S. VA cardiac surgery centers, exclusively used surgeons who were experts in endovascular vein harvesting, which could have meant that they and their surgical teams were not as expert in open vein harvesting, he said. Also, in the broader context of CABG and conduit selection, new evidence suggests the superiority of pedicled vein grafts (Ann Thoracic Surg. 2017 Oct;104[4]1313-17), and “we could also do better by using the radial artery” rather than a saphenous vein graft, Dr. Ruel said. He cited a meta-analysis published in 2018 that showed the superiority of CABG when it combined an internal thoracic artery graft with a radial artery graft rather than with a vein graft (N Engl J Med. 2018 May 31;378[22]:2069-77).
“The operation of the future is not necessarily what you saw” in Dr. Zenati’s study, Dr. Ruel cautioned.
The results Dr. Zenati reported came from the REGROUP (Randomized End-Vein Graft Prospective) trial, which enrolled patients who underwent CABG during 2014-2017. All patients received an internal thoracic artery graft and were randomized to receive additional saphenous vein grafts with the conduits collected either by the EVH or OVH method. The study’s primary endpoint of all-cause death, nonfatal MI, or need for repeat revascularization after a median follow-up of 2.8 years occurred in 14% of the patients who received vein grafts with EVH and in 16% of the patients who received grafts with OVH, a difference that was not statistically significant, reported Dr. Zenati, a professor of surgery at Harvard Medical School in Boston and the chief of cardiothoracic surgery for the VA Boston Health System. The incidence of wound infection was 3.1% in the OVH patients and 1.4% in the EVH patients, a difference that came close to but did not reach statistical significance. Concurrently with Dr. Zenati’s report, an article with the results appeared online (N Engl J Med. 2018 Nov 11. doi: 0.1056/NEJMoa1812390).
The REGROUP trial did not collect data on vein-graft patency following CABG. The investigators were concerned about having enough patients return for follow-up angiography to produce a meaningful result for this endpoint, and they believed that the clinical endpoint they used sufficed for demonstrating equivalence of the two harvesting methods, Dr. Zenati said during his talk.
“The more arterial conduit used in CABG, the better the durability of the grafts, but often surgeons use vein grafts because there is not enough arterial conduit,” commented Donald M. Lloyd-Jones, MD, professor and chair of preventive medicine at Northwestern University in Chicago.* “The recovery from endoscopic vein-graft harvesting is very different from open harvesting. Endoscopic harvesting produces much less pain and infection, and recovery is much easier for patients, so it’s reassuring to see that the quality of the vein is not affected by endoscopic harvesting when done by experts,” he said.
Dr. Zenati, Dr. Gardner, Dr. Ruel, and Dr. Lloyd-Jones had no disclosures.
SOURCE: Zenati M et al. AHA 2018, Abstract 19055.
*Correction, 11/12/18: An earlier version of this article misstated the name of Dr. Donald M. Lloyd-Jones.
This article was updated 11/14/18.
The results from the REGROUP trial are interesting and open the field for additional comparisons of endoscopic and open saphenous vein-graft harvesting, but this trial is not the definitive answer regarding whether these two harvesting approaches produce similar results. Greater reassurance of equivalence would come from studies that included more patients and a more diverse patient population; REGROUP largely enrolled male veterans and patients with multiple comorbidities. Longer follow-up is also needed. A median follow-up of 3 years is too brief for complete reassurance that long-term patency is the same with both approaches. It would also help to have follow-up data on graft patency. Many factors besides patency can lead to differences in clinical outcomes following coronary bypass surgery.
Endoscopic vein harvesting is preferred by patients, and it results in fewer wound infections, as was confirmed in REGROUP. Because of these advantages for endoscopic harvesting, it would be great if we could definitively document that these vein grafts functioned as well as those taken with open harvesting.
Evidence now suggests that the more arterial conduits used during coronary bypass, the better. If I were having triple-vessel bypass surgery, I’d want to get two thoracic-artery bypass grafts and a radial artery graft. But studies like REGROUP are important because a majority of heart surgeons use vein grafts for several reasons including convenience. Surgeons will likely continue to use vein grafts for the foreseeable future, so we need to know whether endoscopic harvesting is an acceptable approach.
Jennifer S. Lawton, MD , is a professor of surgery and chief of cardiac surgery at Johns Hopkins Medicine in Baltimore. She had no disclosures. She made these comments in an interview.
The results from the REGROUP trial are interesting and open the field for additional comparisons of endoscopic and open saphenous vein-graft harvesting, but this trial is not the definitive answer regarding whether these two harvesting approaches produce similar results. Greater reassurance of equivalence would come from studies that included more patients and a more diverse patient population; REGROUP largely enrolled male veterans and patients with multiple comorbidities. Longer follow-up is also needed. A median follow-up of 3 years is too brief for complete reassurance that long-term patency is the same with both approaches. It would also help to have follow-up data on graft patency. Many factors besides patency can lead to differences in clinical outcomes following coronary bypass surgery.
Endoscopic vein harvesting is preferred by patients, and it results in fewer wound infections, as was confirmed in REGROUP. Because of these advantages for endoscopic harvesting, it would be great if we could definitively document that these vein grafts functioned as well as those taken with open harvesting.
Evidence now suggests that the more arterial conduits used during coronary bypass, the better. If I were having triple-vessel bypass surgery, I’d want to get two thoracic-artery bypass grafts and a radial artery graft. But studies like REGROUP are important because a majority of heart surgeons use vein grafts for several reasons including convenience. Surgeons will likely continue to use vein grafts for the foreseeable future, so we need to know whether endoscopic harvesting is an acceptable approach.
Jennifer S. Lawton, MD , is a professor of surgery and chief of cardiac surgery at Johns Hopkins Medicine in Baltimore. She had no disclosures. She made these comments in an interview.
The results from the REGROUP trial are interesting and open the field for additional comparisons of endoscopic and open saphenous vein-graft harvesting, but this trial is not the definitive answer regarding whether these two harvesting approaches produce similar results. Greater reassurance of equivalence would come from studies that included more patients and a more diverse patient population; REGROUP largely enrolled male veterans and patients with multiple comorbidities. Longer follow-up is also needed. A median follow-up of 3 years is too brief for complete reassurance that long-term patency is the same with both approaches. It would also help to have follow-up data on graft patency. Many factors besides patency can lead to differences in clinical outcomes following coronary bypass surgery.
Endoscopic vein harvesting is preferred by patients, and it results in fewer wound infections, as was confirmed in REGROUP. Because of these advantages for endoscopic harvesting, it would be great if we could definitively document that these vein grafts functioned as well as those taken with open harvesting.
Evidence now suggests that the more arterial conduits used during coronary bypass, the better. If I were having triple-vessel bypass surgery, I’d want to get two thoracic-artery bypass grafts and a radial artery graft. But studies like REGROUP are important because a majority of heart surgeons use vein grafts for several reasons including convenience. Surgeons will likely continue to use vein grafts for the foreseeable future, so we need to know whether endoscopic harvesting is an acceptable approach.
Jennifer S. Lawton, MD , is a professor of surgery and chief of cardiac surgery at Johns Hopkins Medicine in Baltimore. She had no disclosures. She made these comments in an interview.
CHICAGO – Patients who underwent coronary artery bypass grafting using saphenous veins harvested endoscopically had similar clinical outcomes after nearly 3 years of follow-up as those seen with patients who received vein grafts taken by open harvesting in a multicenter, randomized trial in the United States with 1,150 patients.
As expected, follow-up also showed that endoscopic vein-graft harvesting (EVH) resulted in about half the number of wound infections as did open vein-graft harvesting (OVH). This combination of similar clinical outcomes after a median 2.8 years of follow-up, as well as fewer leg-wound adverse events, makes EVH “the preferred vein-harvesting modality,” Marco A. Zenati, MD, said at the American Heart Association scientific sessions.
Although patients far and away prefer EVH because of the reduced pain and faster healing, questions about its clinical efficacy when compared with that of OVH have lingered. That’s because observational data published almost a decade ago taken from the PREVENT IV (Project of Ex-Vivo Vein Graft Engineering via Transfection IV) trial suggested that patients who underwent coronary artery bypass grafting (CABG) using vein grafts collected by EVH had more vein-graft failures after 12-18 months and a higher rate of death, MI, or need for revascularization after 3 years, compared with patients treated using OVH (N Engl J Med. 2009 July 16;361[3]:235-44).
The results from the prospective, randomized trial reported by Dr. Zenati “take the cloud away from endovascular vein-graft harvesting that PREVENT IV had made,” commented Timothy J. Gardner, MD, a cardiac surgeon who chaired the session.
“I think this answers the question,” commented Marc Ruel, MD, a professor of surgery and the chief of cardiac surgery at the University of Ottawa. “The results show that endoscopic harvesting of vein grafts is as good as open harvesting for preventing major adverse cardiac events, which is the goal of CABG. This is a definitive trial, with no trend toward more events with endoscopic harvested vein grafts,” said Dr. Ruel, the designated discussant for Dr. Zenati’s report.
However, the study did have some significant limitations, Dr. Ruel added. The new, randomized trial, run at 16 U.S. VA cardiac surgery centers, exclusively used surgeons who were experts in endovascular vein harvesting, which could have meant that they and their surgical teams were not as expert in open vein harvesting, he said. Also, in the broader context of CABG and conduit selection, new evidence suggests the superiority of pedicled vein grafts (Ann Thoracic Surg. 2017 Oct;104[4]1313-17), and “we could also do better by using the radial artery” rather than a saphenous vein graft, Dr. Ruel said. He cited a meta-analysis published in 2018 that showed the superiority of CABG when it combined an internal thoracic artery graft with a radial artery graft rather than with a vein graft (N Engl J Med. 2018 May 31;378[22]:2069-77).
“The operation of the future is not necessarily what you saw” in Dr. Zenati’s study, Dr. Ruel cautioned.
The results Dr. Zenati reported came from the REGROUP (Randomized End-Vein Graft Prospective) trial, which enrolled patients who underwent CABG during 2014-2017. All patients received an internal thoracic artery graft and were randomized to receive additional saphenous vein grafts with the conduits collected either by the EVH or OVH method. The study’s primary endpoint of all-cause death, nonfatal MI, or need for repeat revascularization after a median follow-up of 2.8 years occurred in 14% of the patients who received vein grafts with EVH and in 16% of the patients who received grafts with OVH, a difference that was not statistically significant, reported Dr. Zenati, a professor of surgery at Harvard Medical School in Boston and the chief of cardiothoracic surgery for the VA Boston Health System. The incidence of wound infection was 3.1% in the OVH patients and 1.4% in the EVH patients, a difference that came close to but did not reach statistical significance. Concurrently with Dr. Zenati’s report, an article with the results appeared online (N Engl J Med. 2018 Nov 11. doi: 0.1056/NEJMoa1812390).
The REGROUP trial did not collect data on vein-graft patency following CABG. The investigators were concerned about having enough patients return for follow-up angiography to produce a meaningful result for this endpoint, and they believed that the clinical endpoint they used sufficed for demonstrating equivalence of the two harvesting methods, Dr. Zenati said during his talk.
“The more arterial conduit used in CABG, the better the durability of the grafts, but often surgeons use vein grafts because there is not enough arterial conduit,” commented Donald M. Lloyd-Jones, MD, professor and chair of preventive medicine at Northwestern University in Chicago.* “The recovery from endoscopic vein-graft harvesting is very different from open harvesting. Endoscopic harvesting produces much less pain and infection, and recovery is much easier for patients, so it’s reassuring to see that the quality of the vein is not affected by endoscopic harvesting when done by experts,” he said.
Dr. Zenati, Dr. Gardner, Dr. Ruel, and Dr. Lloyd-Jones had no disclosures.
SOURCE: Zenati M et al. AHA 2018, Abstract 19055.
*Correction, 11/12/18: An earlier version of this article misstated the name of Dr. Donald M. Lloyd-Jones.
This article was updated 11/14/18.
CHICAGO – Patients who underwent coronary artery bypass grafting using saphenous veins harvested endoscopically had similar clinical outcomes after nearly 3 years of follow-up as those seen with patients who received vein grafts taken by open harvesting in a multicenter, randomized trial in the United States with 1,150 patients.
As expected, follow-up also showed that endoscopic vein-graft harvesting (EVH) resulted in about half the number of wound infections as did open vein-graft harvesting (OVH). This combination of similar clinical outcomes after a median 2.8 years of follow-up, as well as fewer leg-wound adverse events, makes EVH “the preferred vein-harvesting modality,” Marco A. Zenati, MD, said at the American Heart Association scientific sessions.
Although patients far and away prefer EVH because of the reduced pain and faster healing, questions about its clinical efficacy when compared with that of OVH have lingered. That’s because observational data published almost a decade ago taken from the PREVENT IV (Project of Ex-Vivo Vein Graft Engineering via Transfection IV) trial suggested that patients who underwent coronary artery bypass grafting (CABG) using vein grafts collected by EVH had more vein-graft failures after 12-18 months and a higher rate of death, MI, or need for revascularization after 3 years, compared with patients treated using OVH (N Engl J Med. 2009 July 16;361[3]:235-44).
The results from the prospective, randomized trial reported by Dr. Zenati “take the cloud away from endovascular vein-graft harvesting that PREVENT IV had made,” commented Timothy J. Gardner, MD, a cardiac surgeon who chaired the session.
“I think this answers the question,” commented Marc Ruel, MD, a professor of surgery and the chief of cardiac surgery at the University of Ottawa. “The results show that endoscopic harvesting of vein grafts is as good as open harvesting for preventing major adverse cardiac events, which is the goal of CABG. This is a definitive trial, with no trend toward more events with endoscopic harvested vein grafts,” said Dr. Ruel, the designated discussant for Dr. Zenati’s report.
However, the study did have some significant limitations, Dr. Ruel added. The new, randomized trial, run at 16 U.S. VA cardiac surgery centers, exclusively used surgeons who were experts in endovascular vein harvesting, which could have meant that they and their surgical teams were not as expert in open vein harvesting, he said. Also, in the broader context of CABG and conduit selection, new evidence suggests the superiority of pedicled vein grafts (Ann Thoracic Surg. 2017 Oct;104[4]1313-17), and “we could also do better by using the radial artery” rather than a saphenous vein graft, Dr. Ruel said. He cited a meta-analysis published in 2018 that showed the superiority of CABG when it combined an internal thoracic artery graft with a radial artery graft rather than with a vein graft (N Engl J Med. 2018 May 31;378[22]:2069-77).
“The operation of the future is not necessarily what you saw” in Dr. Zenati’s study, Dr. Ruel cautioned.
The results Dr. Zenati reported came from the REGROUP (Randomized End-Vein Graft Prospective) trial, which enrolled patients who underwent CABG during 2014-2017. All patients received an internal thoracic artery graft and were randomized to receive additional saphenous vein grafts with the conduits collected either by the EVH or OVH method. The study’s primary endpoint of all-cause death, nonfatal MI, or need for repeat revascularization after a median follow-up of 2.8 years occurred in 14% of the patients who received vein grafts with EVH and in 16% of the patients who received grafts with OVH, a difference that was not statistically significant, reported Dr. Zenati, a professor of surgery at Harvard Medical School in Boston and the chief of cardiothoracic surgery for the VA Boston Health System. The incidence of wound infection was 3.1% in the OVH patients and 1.4% in the EVH patients, a difference that came close to but did not reach statistical significance. Concurrently with Dr. Zenati’s report, an article with the results appeared online (N Engl J Med. 2018 Nov 11. doi: 0.1056/NEJMoa1812390).
The REGROUP trial did not collect data on vein-graft patency following CABG. The investigators were concerned about having enough patients return for follow-up angiography to produce a meaningful result for this endpoint, and they believed that the clinical endpoint they used sufficed for demonstrating equivalence of the two harvesting methods, Dr. Zenati said during his talk.
“The more arterial conduit used in CABG, the better the durability of the grafts, but often surgeons use vein grafts because there is not enough arterial conduit,” commented Donald M. Lloyd-Jones, MD, professor and chair of preventive medicine at Northwestern University in Chicago.* “The recovery from endoscopic vein-graft harvesting is very different from open harvesting. Endoscopic harvesting produces much less pain and infection, and recovery is much easier for patients, so it’s reassuring to see that the quality of the vein is not affected by endoscopic harvesting when done by experts,” he said.
Dr. Zenati, Dr. Gardner, Dr. Ruel, and Dr. Lloyd-Jones had no disclosures.
SOURCE: Zenati M et al. AHA 2018, Abstract 19055.
*Correction, 11/12/18: An earlier version of this article misstated the name of Dr. Donald M. Lloyd-Jones.
This article was updated 11/14/18.
REPORTING FROM THE AHA SCIENTIFIC SESSION
Key clinical point:
Major finding: Clinical events occurred in 16% of open-harvest vein-graft patients and in 14% who received endoscopically harvested veins.
Study details: REGROUP, a multicenter, randomized trial with 1,150 patients.
Disclosures: Dr. Zenati, Dr. Gardner, Dr. Ruel, and Dr. Lloyd-Jones had no disclosures.
Source: Zenati M et al. AHA 2018, Abstract 19055.