User login
MIAMI – As patients with psoriasis develop psoriatic arthritis, the abundance of particular genera in the skin microbiome decreases, according to a preliminary study characterizing cutaneous microbiota in these populations.
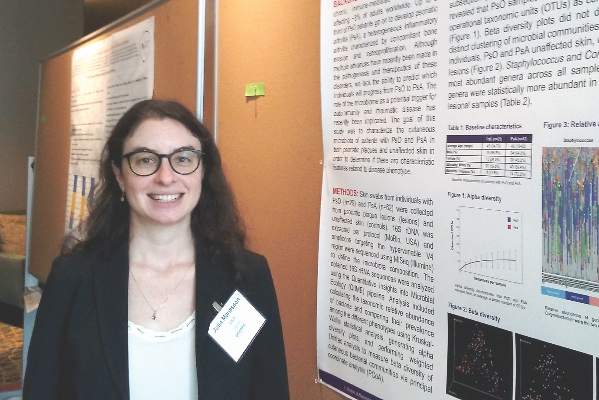
“The big overall message is there might be a decrease in microbiota diversity as you progress through the disease spectrum,” Julia Manasson, MD, a fellow in the division of rheumatology at New York University said. “This is the first study characterizing the cutaneous microbial compositions of subjects with psoriasis and psoriatic arthritis in both psoriatic lesions and unaffected skin.”
A previous study that revealed changes in gut microbiome between psoriasis and psoriatic arthritis patient stool samples (Arthritis Rheumatol. 2015;67:128-39) prompted the current research, which is “trying to see if the skin has a similar manifestation,” Dr. Manasson said during an oral presentation of her poster at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“The microbiome has been implicated as a potential trigger for inflammation and autoimmune disease,” Dr. Manasson noted.
To investigate a potential role of the skin microbiome, the investigators swabbed lesions and unaffected skin (on a contralateral site) in 29 people with psoriasis and 62 others with psoriatic arthritis. They extracted, amplified, and sequenced DNA from the samples. No participants in the study were on treatment with biologics, disease-modifying antirheumatic drugs, or steroids at the time of assessment. The psoriasis group was 66% men and had an average age of 45 years; the psoriatic arthritis group was 55% men and the average age was 42.
Dr. Manasson and her colleagues calculated the taxonomic relative abundance and contrasted their prevalence among the four skin phenotypes examined: lesions and unaffected skin of psoriasis patients and lesions and unaffected skin of psoriatic arthritis patients. Alpha diversity plots revealed a similar number of operational taxonomic units (OTUs) between psoriasis and psoriatic arthritis samples. Beta diversity analysis showed no distinct clustering or significant difference in microbiota communities among different phenotypes.
“We saw more of a decrease in nonlesional skin and across clinical severity, too,” Dr. Manasson said. “Globally, we didn’t see significant differences [in microbiota present].”
Staphylococcus and Corynebacterium were the predominant bacteria in all samples, but there were also specific genera that were less common in psoriatic arthritis patients and in lesional skin. These less abundant genera included unclassified Bradyrhizobiaceae, Rahnella, unclassified Prevotellaceae, and Parvibaculum.
“It looks like you had some differences between lesion and nonlesional skin,” Alice Gottlieb, MD, chair and dermatologist in chief at Tufts Medical Center in Boston. “In psoriasis, the barrier function is not normal. You may want to look at atopic dermatitis where you clearly have altered barrier function.”
Dr. Manasson said they used a skin swab, so they did not assess barrier function.
“The nonlesional skin may be more interesting to look at,” Dr. Gottlieb added. “If you see a difference in nonlesional skin, it could be more [conclusive].”
Microbiome stability often changes in individuals from week to week, commented Philip Helliwell, DM, PhD, a rheumatologist at the University of Leeds in England and president of GRAPPA. Dr. Manasson said she could assess variability over time in the future. She also would like to evaluate how therapies, including antibiotics, alter the skin microbiome.
Lack of a healthy control group is a potential limitation of the study. Some unanswered questions remain, Dr. Manasson said, such as what are the regional differences in skin microbiota, for example, between a patient’s scalp and forearm? She added, “The most interesting question is what does this actually mean? What are the downstream effects?”
If a decrease in skin microbiome flora diversity is verified in future research as a sign that a patient with psoriasis is at elevated risk for developing psoriatic arthritis, it could help physicians predict who will progress. Currently, about 30% of psoriatic patients go on to develop joint disease, but methods to identify this subpopulation remain elusive.
Dr. Manasson, Dr. Gottlieb, and Dr. Helliwell had no relevant financial disclosures.
MIAMI – As patients with psoriasis develop psoriatic arthritis, the abundance of particular genera in the skin microbiome decreases, according to a preliminary study characterizing cutaneous microbiota in these populations.
“The big overall message is there might be a decrease in microbiota diversity as you progress through the disease spectrum,” Julia Manasson, MD, a fellow in the division of rheumatology at New York University said. “This is the first study characterizing the cutaneous microbial compositions of subjects with psoriasis and psoriatic arthritis in both psoriatic lesions and unaffected skin.”
A previous study that revealed changes in gut microbiome between psoriasis and psoriatic arthritis patient stool samples (Arthritis Rheumatol. 2015;67:128-39) prompted the current research, which is “trying to see if the skin has a similar manifestation,” Dr. Manasson said during an oral presentation of her poster at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“The microbiome has been implicated as a potential trigger for inflammation and autoimmune disease,” Dr. Manasson noted.
To investigate a potential role of the skin microbiome, the investigators swabbed lesions and unaffected skin (on a contralateral site) in 29 people with psoriasis and 62 others with psoriatic arthritis. They extracted, amplified, and sequenced DNA from the samples. No participants in the study were on treatment with biologics, disease-modifying antirheumatic drugs, or steroids at the time of assessment. The psoriasis group was 66% men and had an average age of 45 years; the psoriatic arthritis group was 55% men and the average age was 42.
Dr. Manasson and her colleagues calculated the taxonomic relative abundance and contrasted their prevalence among the four skin phenotypes examined: lesions and unaffected skin of psoriasis patients and lesions and unaffected skin of psoriatic arthritis patients. Alpha diversity plots revealed a similar number of operational taxonomic units (OTUs) between psoriasis and psoriatic arthritis samples. Beta diversity analysis showed no distinct clustering or significant difference in microbiota communities among different phenotypes.
“We saw more of a decrease in nonlesional skin and across clinical severity, too,” Dr. Manasson said. “Globally, we didn’t see significant differences [in microbiota present].”
Staphylococcus and Corynebacterium were the predominant bacteria in all samples, but there were also specific genera that were less common in psoriatic arthritis patients and in lesional skin. These less abundant genera included unclassified Bradyrhizobiaceae, Rahnella, unclassified Prevotellaceae, and Parvibaculum.
“It looks like you had some differences between lesion and nonlesional skin,” Alice Gottlieb, MD, chair and dermatologist in chief at Tufts Medical Center in Boston. “In psoriasis, the barrier function is not normal. You may want to look at atopic dermatitis where you clearly have altered barrier function.”
Dr. Manasson said they used a skin swab, so they did not assess barrier function.
“The nonlesional skin may be more interesting to look at,” Dr. Gottlieb added. “If you see a difference in nonlesional skin, it could be more [conclusive].”
Microbiome stability often changes in individuals from week to week, commented Philip Helliwell, DM, PhD, a rheumatologist at the University of Leeds in England and president of GRAPPA. Dr. Manasson said she could assess variability over time in the future. She also would like to evaluate how therapies, including antibiotics, alter the skin microbiome.
Lack of a healthy control group is a potential limitation of the study. Some unanswered questions remain, Dr. Manasson said, such as what are the regional differences in skin microbiota, for example, between a patient’s scalp and forearm? She added, “The most interesting question is what does this actually mean? What are the downstream effects?”
If a decrease in skin microbiome flora diversity is verified in future research as a sign that a patient with psoriasis is at elevated risk for developing psoriatic arthritis, it could help physicians predict who will progress. Currently, about 30% of psoriatic patients go on to develop joint disease, but methods to identify this subpopulation remain elusive.
Dr. Manasson, Dr. Gottlieb, and Dr. Helliwell had no relevant financial disclosures.
MIAMI – As patients with psoriasis develop psoriatic arthritis, the abundance of particular genera in the skin microbiome decreases, according to a preliminary study characterizing cutaneous microbiota in these populations.
“The big overall message is there might be a decrease in microbiota diversity as you progress through the disease spectrum,” Julia Manasson, MD, a fellow in the division of rheumatology at New York University said. “This is the first study characterizing the cutaneous microbial compositions of subjects with psoriasis and psoriatic arthritis in both psoriatic lesions and unaffected skin.”
A previous study that revealed changes in gut microbiome between psoriasis and psoriatic arthritis patient stool samples (Arthritis Rheumatol. 2015;67:128-39) prompted the current research, which is “trying to see if the skin has a similar manifestation,” Dr. Manasson said during an oral presentation of her poster at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“The microbiome has been implicated as a potential trigger for inflammation and autoimmune disease,” Dr. Manasson noted.
To investigate a potential role of the skin microbiome, the investigators swabbed lesions and unaffected skin (on a contralateral site) in 29 people with psoriasis and 62 others with psoriatic arthritis. They extracted, amplified, and sequenced DNA from the samples. No participants in the study were on treatment with biologics, disease-modifying antirheumatic drugs, or steroids at the time of assessment. The psoriasis group was 66% men and had an average age of 45 years; the psoriatic arthritis group was 55% men and the average age was 42.
Dr. Manasson and her colleagues calculated the taxonomic relative abundance and contrasted their prevalence among the four skin phenotypes examined: lesions and unaffected skin of psoriasis patients and lesions and unaffected skin of psoriatic arthritis patients. Alpha diversity plots revealed a similar number of operational taxonomic units (OTUs) between psoriasis and psoriatic arthritis samples. Beta diversity analysis showed no distinct clustering or significant difference in microbiota communities among different phenotypes.
“We saw more of a decrease in nonlesional skin and across clinical severity, too,” Dr. Manasson said. “Globally, we didn’t see significant differences [in microbiota present].”
Staphylococcus and Corynebacterium were the predominant bacteria in all samples, but there were also specific genera that were less common in psoriatic arthritis patients and in lesional skin. These less abundant genera included unclassified Bradyrhizobiaceae, Rahnella, unclassified Prevotellaceae, and Parvibaculum.
“It looks like you had some differences between lesion and nonlesional skin,” Alice Gottlieb, MD, chair and dermatologist in chief at Tufts Medical Center in Boston. “In psoriasis, the barrier function is not normal. You may want to look at atopic dermatitis where you clearly have altered barrier function.”
Dr. Manasson said they used a skin swab, so they did not assess barrier function.
“The nonlesional skin may be more interesting to look at,” Dr. Gottlieb added. “If you see a difference in nonlesional skin, it could be more [conclusive].”
Microbiome stability often changes in individuals from week to week, commented Philip Helliwell, DM, PhD, a rheumatologist at the University of Leeds in England and president of GRAPPA. Dr. Manasson said she could assess variability over time in the future. She also would like to evaluate how therapies, including antibiotics, alter the skin microbiome.
Lack of a healthy control group is a potential limitation of the study. Some unanswered questions remain, Dr. Manasson said, such as what are the regional differences in skin microbiota, for example, between a patient’s scalp and forearm? She added, “The most interesting question is what does this actually mean? What are the downstream effects?”
If a decrease in skin microbiome flora diversity is verified in future research as a sign that a patient with psoriasis is at elevated risk for developing psoriatic arthritis, it could help physicians predict who will progress. Currently, about 30% of psoriatic patients go on to develop joint disease, but methods to identify this subpopulation remain elusive.
Dr. Manasson, Dr. Gottlieb, and Dr. Helliwell had no relevant financial disclosures.
AT 2016 GRAPPA ANNUAL MEETING
Key clinical point:Changes in skin microbiome diversity in patients with psoriasis might someday help to predict progression to psoriatic arthritis.
Major finding: The abundance of specific genera was decreased in psoriatic arthritis patients and in their lesional skin relative to patients with psoriasis only.
Data source: Comparison of 29 people with psoriasis versus 62 with psoriatic arthritis.
Disclosures: Dr. Manasson, Dr. Gottlieb, and Dr. Helliwell had no relevant disclosures.