User login
The medical dictum primum non nocere (first, do no harm) is a fundamental rule by which physicians have lived for centuries.1 Physicians are familiar with the term placebo (I shall please) and the placebo effect of improvement based on expectation of positive results; however, many are not familiar with the term nocebo (I shall harm) and the nocebo effect of lack of improvement or deterioration based on the expectation of negative results. The patient’s expectation of being pleased and/or being harmed may be on the conscious level and/or on one or more subconscious and unconscious levels.
Words can have as much of an impact on some patients as medications or procedures. Rudyard Kipling said, “Words are, of course, the most powerful drug used by mankind.” The words that a dermatologist chooses to use can have either a placebo or a nocebo effect on the patient. The purpose of this commentary is to elevate awareness that there are positive alternatives to unintended negative suggestions that are commonly used in dermatologic practice.
A search of PubMed articles indexed for MEDLINE and Scopus published from January 1966 through July 28, 2016, was conducted using the terms placebo or nocebo and cutaneous or skin. Prior publications in this area related specifically to dermatology include those of Poletti2 and Sonthalia et al.3
Patient expectations play an important role in both positive and negative treatment outcomes. Patient-physician communication can moderate these effects both positively and negatively.4 Nocebo effects can substantially reduce treatment efficacy and patient compliance. Patient expectations of negative results or side effects of a treatment or medication can be self-induced or can be induced by inappropriate physician-patient communication, drug information leaflets, influence of family or peers, or discovery of reported adverse effects through reading materials on the Internet.4 Expectation of negative effects can reduce patient adherence and compliance with treatment, reducing treatment efficacy. The psychosocial context around the patient and the treatment may change the neuronal biochemistry and circuitry in the patient’s brain, and the central and peripheral mechanisms activated by placebos and nocebos have been found to be the same as those activated by the medications, suggesting cognitive/affective enhancing or impeding of drug action.5
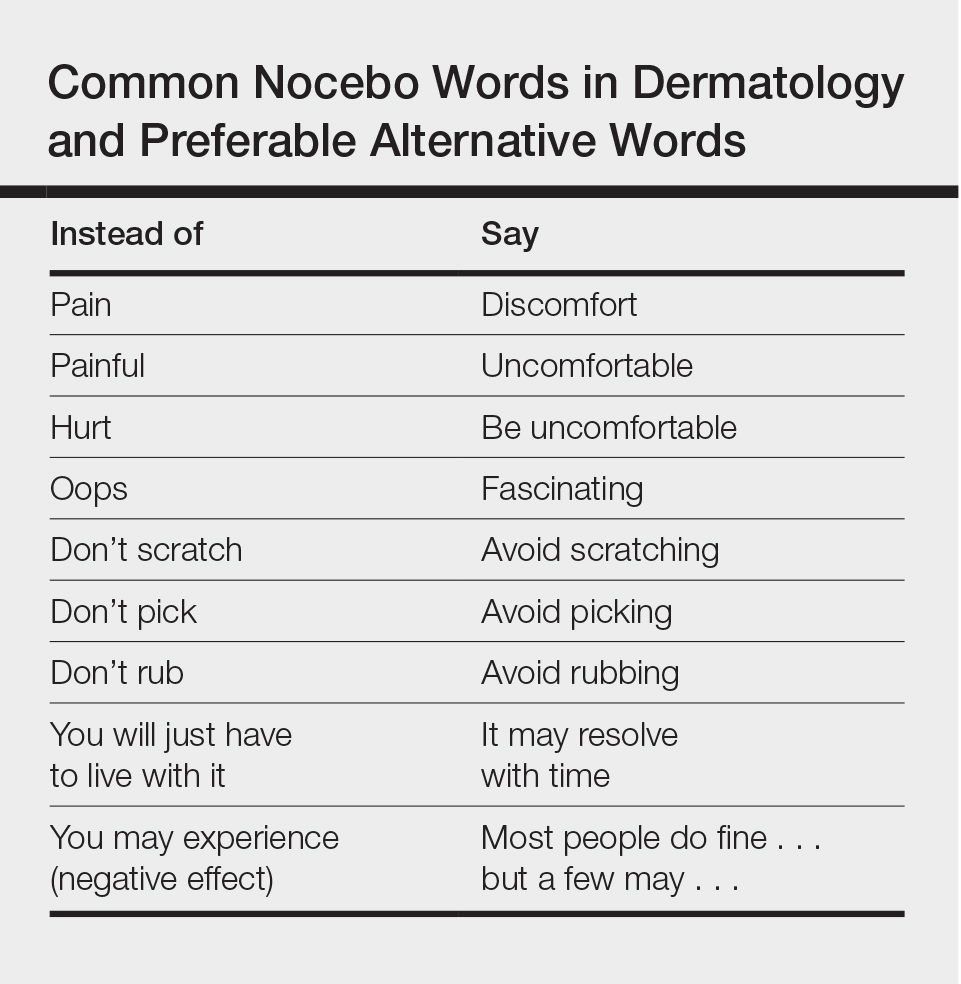
The subconscious and unconscious habitual automated parts of the brain hear words on the level of a 5- or 6-year-old child with literal unconscious cognitive interpretation of the words. These parts also do not connect words in a sentence with each other.5 For example, if the dermatologist or nurse says “This will not hurt,” the unconscious brain hears not and hurt but does not connect the two. On the other hand, if the dermatologist or nurse says “ You may experience some discomfort,” the unconscious brain hears comfort. Telling the patient “Don’t scratch” may be heard unconsciously as scratch. See the Table for suggested rephrasing of common nocebos used in dermatology. The conscious parts of the brain help determine cognitions influenced by associated unconscious memories, positive or negative. Both the conscious and unconscious parts of the brain influence affect or emotion.
When excess stress occurs, there is a natural shift downward from social communicative newer parasympathetic nervous system to fight or flight sympathetic nervous system, and possibly further shift to the freeze response of older parasympathetic nervous system dominance. Memories that are associated with a strong surge of norepinephrine tend to be much more strongly fixed in the memory than ordinary memories and frequently are associated with overwhelming traumatic experiences. When a threat is perceived, negative interpretations and perceptions generally win out over positive interpretations and perceptions. Unconscious fears generally prevail over conscious thoughts, and stronger emotions generally prevail over weaker emotions. Anxiety often is associated with rapid breathing and activation of the sympathetic nervous system. It can be countered by slow breathing to a rate of approximately 6 breaths per minute, helping to bring back more parasympathetic balance. Pacing a patient’s breathing to slow it and using a soothing tone of voice can help reduce patient anxiety. Reducing anxiety can decrease the patient’s tendency to jump to negative conclusions or have negative perceptions or emotions that can invoke the nocebo effect.
For the dermatologist, as for the patient, changing an old habit and creating a new habit requires repeating something differently and consistently 20 to 40 times. Becoming more conscious of the effects of language on the patient is an important part of the art of medicine. By carefully choosing words, intonation, and body language, it is possible to enhance the placebo effect and decrease the nocebo effect for the benefit of the patient. When describing possible adverse effects of treatments or medications, if the dermatologist says that most people do fine with the treatment but a few can experience the described adverse effect, it usually takes the edge off the potential suggested nocebo effect.
In conclusion, primum non nocere includes careful consideration and use of language, tone, and body language to maximize the placebo effect and minimize the nocebo effect.
- Hippocrates. Epidemics. Jones WHS, trans. Loeb Classical Library: Hippocrates. Vol 1. Cambridge, MA: Harvard University Press; 1923:164-165.
- Poletti ED. El efecto nocebo in dermatología. Dermatol Cosmet Quirg. 2007;5:74.
- Sonthalia S, Sahaya K, Arora R, et al. Nocebo effect in dermatology. Indian J Dermatol Venereol Leprol. 2015;81:242-250.
- Bingel U. Avoiding nocebo effects to optimize treatment outcomes. JAMA. 2014;312:693-694.
- Greenwald AG. New look 3: unconscious cognition reclaimed. Am Psychol. 1992;47:766-779.
- Porges SW. The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-regulation. New York, NY: W.W. Norton & Co; 2011.
The medical dictum primum non nocere (first, do no harm) is a fundamental rule by which physicians have lived for centuries.1 Physicians are familiar with the term placebo (I shall please) and the placebo effect of improvement based on expectation of positive results; however, many are not familiar with the term nocebo (I shall harm) and the nocebo effect of lack of improvement or deterioration based on the expectation of negative results. The patient’s expectation of being pleased and/or being harmed may be on the conscious level and/or on one or more subconscious and unconscious levels.
Words can have as much of an impact on some patients as medications or procedures. Rudyard Kipling said, “Words are, of course, the most powerful drug used by mankind.” The words that a dermatologist chooses to use can have either a placebo or a nocebo effect on the patient. The purpose of this commentary is to elevate awareness that there are positive alternatives to unintended negative suggestions that are commonly used in dermatologic practice.
A search of PubMed articles indexed for MEDLINE and Scopus published from January 1966 through July 28, 2016, was conducted using the terms placebo or nocebo and cutaneous or skin. Prior publications in this area related specifically to dermatology include those of Poletti2 and Sonthalia et al.3
Patient expectations play an important role in both positive and negative treatment outcomes. Patient-physician communication can moderate these effects both positively and negatively.4 Nocebo effects can substantially reduce treatment efficacy and patient compliance. Patient expectations of negative results or side effects of a treatment or medication can be self-induced or can be induced by inappropriate physician-patient communication, drug information leaflets, influence of family or peers, or discovery of reported adverse effects through reading materials on the Internet.4 Expectation of negative effects can reduce patient adherence and compliance with treatment, reducing treatment efficacy. The psychosocial context around the patient and the treatment may change the neuronal biochemistry and circuitry in the patient’s brain, and the central and peripheral mechanisms activated by placebos and nocebos have been found to be the same as those activated by the medications, suggesting cognitive/affective enhancing or impeding of drug action.5
The subconscious and unconscious habitual automated parts of the brain hear words on the level of a 5- or 6-year-old child with literal unconscious cognitive interpretation of the words. These parts also do not connect words in a sentence with each other.5 For example, if the dermatologist or nurse says “This will not hurt,” the unconscious brain hears not and hurt but does not connect the two. On the other hand, if the dermatologist or nurse says “ You may experience some discomfort,” the unconscious brain hears comfort. Telling the patient “Don’t scratch” may be heard unconsciously as scratch. See the Table for suggested rephrasing of common nocebos used in dermatology. The conscious parts of the brain help determine cognitions influenced by associated unconscious memories, positive or negative. Both the conscious and unconscious parts of the brain influence affect or emotion.
When excess stress occurs, there is a natural shift downward from social communicative newer parasympathetic nervous system to fight or flight sympathetic nervous system, and possibly further shift to the freeze response of older parasympathetic nervous system dominance. Memories that are associated with a strong surge of norepinephrine tend to be much more strongly fixed in the memory than ordinary memories and frequently are associated with overwhelming traumatic experiences. When a threat is perceived, negative interpretations and perceptions generally win out over positive interpretations and perceptions. Unconscious fears generally prevail over conscious thoughts, and stronger emotions generally prevail over weaker emotions. Anxiety often is associated with rapid breathing and activation of the sympathetic nervous system. It can be countered by slow breathing to a rate of approximately 6 breaths per minute, helping to bring back more parasympathetic balance. Pacing a patient’s breathing to slow it and using a soothing tone of voice can help reduce patient anxiety. Reducing anxiety can decrease the patient’s tendency to jump to negative conclusions or have negative perceptions or emotions that can invoke the nocebo effect.
For the dermatologist, as for the patient, changing an old habit and creating a new habit requires repeating something differently and consistently 20 to 40 times. Becoming more conscious of the effects of language on the patient is an important part of the art of medicine. By carefully choosing words, intonation, and body language, it is possible to enhance the placebo effect and decrease the nocebo effect for the benefit of the patient. When describing possible adverse effects of treatments or medications, if the dermatologist says that most people do fine with the treatment but a few can experience the described adverse effect, it usually takes the edge off the potential suggested nocebo effect.
In conclusion, primum non nocere includes careful consideration and use of language, tone, and body language to maximize the placebo effect and minimize the nocebo effect.
The medical dictum primum non nocere (first, do no harm) is a fundamental rule by which physicians have lived for centuries.1 Physicians are familiar with the term placebo (I shall please) and the placebo effect of improvement based on expectation of positive results; however, many are not familiar with the term nocebo (I shall harm) and the nocebo effect of lack of improvement or deterioration based on the expectation of negative results. The patient’s expectation of being pleased and/or being harmed may be on the conscious level and/or on one or more subconscious and unconscious levels.
Words can have as much of an impact on some patients as medications or procedures. Rudyard Kipling said, “Words are, of course, the most powerful drug used by mankind.” The words that a dermatologist chooses to use can have either a placebo or a nocebo effect on the patient. The purpose of this commentary is to elevate awareness that there are positive alternatives to unintended negative suggestions that are commonly used in dermatologic practice.
A search of PubMed articles indexed for MEDLINE and Scopus published from January 1966 through July 28, 2016, was conducted using the terms placebo or nocebo and cutaneous or skin. Prior publications in this area related specifically to dermatology include those of Poletti2 and Sonthalia et al.3
Patient expectations play an important role in both positive and negative treatment outcomes. Patient-physician communication can moderate these effects both positively and negatively.4 Nocebo effects can substantially reduce treatment efficacy and patient compliance. Patient expectations of negative results or side effects of a treatment or medication can be self-induced or can be induced by inappropriate physician-patient communication, drug information leaflets, influence of family or peers, or discovery of reported adverse effects through reading materials on the Internet.4 Expectation of negative effects can reduce patient adherence and compliance with treatment, reducing treatment efficacy. The psychosocial context around the patient and the treatment may change the neuronal biochemistry and circuitry in the patient’s brain, and the central and peripheral mechanisms activated by placebos and nocebos have been found to be the same as those activated by the medications, suggesting cognitive/affective enhancing or impeding of drug action.5
The subconscious and unconscious habitual automated parts of the brain hear words on the level of a 5- or 6-year-old child with literal unconscious cognitive interpretation of the words. These parts also do not connect words in a sentence with each other.5 For example, if the dermatologist or nurse says “This will not hurt,” the unconscious brain hears not and hurt but does not connect the two. On the other hand, if the dermatologist or nurse says “ You may experience some discomfort,” the unconscious brain hears comfort. Telling the patient “Don’t scratch” may be heard unconsciously as scratch. See the Table for suggested rephrasing of common nocebos used in dermatology. The conscious parts of the brain help determine cognitions influenced by associated unconscious memories, positive or negative. Both the conscious and unconscious parts of the brain influence affect or emotion.
When excess stress occurs, there is a natural shift downward from social communicative newer parasympathetic nervous system to fight or flight sympathetic nervous system, and possibly further shift to the freeze response of older parasympathetic nervous system dominance. Memories that are associated with a strong surge of norepinephrine tend to be much more strongly fixed in the memory than ordinary memories and frequently are associated with overwhelming traumatic experiences. When a threat is perceived, negative interpretations and perceptions generally win out over positive interpretations and perceptions. Unconscious fears generally prevail over conscious thoughts, and stronger emotions generally prevail over weaker emotions. Anxiety often is associated with rapid breathing and activation of the sympathetic nervous system. It can be countered by slow breathing to a rate of approximately 6 breaths per minute, helping to bring back more parasympathetic balance. Pacing a patient’s breathing to slow it and using a soothing tone of voice can help reduce patient anxiety. Reducing anxiety can decrease the patient’s tendency to jump to negative conclusions or have negative perceptions or emotions that can invoke the nocebo effect.
For the dermatologist, as for the patient, changing an old habit and creating a new habit requires repeating something differently and consistently 20 to 40 times. Becoming more conscious of the effects of language on the patient is an important part of the art of medicine. By carefully choosing words, intonation, and body language, it is possible to enhance the placebo effect and decrease the nocebo effect for the benefit of the patient. When describing possible adverse effects of treatments or medications, if the dermatologist says that most people do fine with the treatment but a few can experience the described adverse effect, it usually takes the edge off the potential suggested nocebo effect.
In conclusion, primum non nocere includes careful consideration and use of language, tone, and body language to maximize the placebo effect and minimize the nocebo effect.
- Hippocrates. Epidemics. Jones WHS, trans. Loeb Classical Library: Hippocrates. Vol 1. Cambridge, MA: Harvard University Press; 1923:164-165.
- Poletti ED. El efecto nocebo in dermatología. Dermatol Cosmet Quirg. 2007;5:74.
- Sonthalia S, Sahaya K, Arora R, et al. Nocebo effect in dermatology. Indian J Dermatol Venereol Leprol. 2015;81:242-250.
- Bingel U. Avoiding nocebo effects to optimize treatment outcomes. JAMA. 2014;312:693-694.
- Greenwald AG. New look 3: unconscious cognition reclaimed. Am Psychol. 1992;47:766-779.
- Porges SW. The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-regulation. New York, NY: W.W. Norton & Co; 2011.
- Hippocrates. Epidemics. Jones WHS, trans. Loeb Classical Library: Hippocrates. Vol 1. Cambridge, MA: Harvard University Press; 1923:164-165.
- Poletti ED. El efecto nocebo in dermatología. Dermatol Cosmet Quirg. 2007;5:74.
- Sonthalia S, Sahaya K, Arora R, et al. Nocebo effect in dermatology. Indian J Dermatol Venereol Leprol. 2015;81:242-250.
- Bingel U. Avoiding nocebo effects to optimize treatment outcomes. JAMA. 2014;312:693-694.
- Greenwald AG. New look 3: unconscious cognition reclaimed. Am Psychol. 1992;47:766-779.
- Porges SW. The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-regulation. New York, NY: W.W. Norton & Co; 2011.