User login
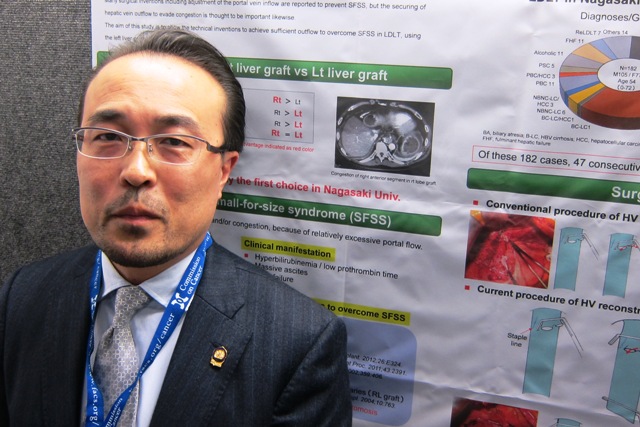
WASHINGTON – A novel anastomosis technique may help avoid small-for-size syndrome in adult living donor liver transplantation, according to Dr. Mitsuhisa Takatsuki.
Reconstructing the hepatic vein by cross-clamping with the inferior vena cava creates improved outflow from the graft. This can avert the potential failure of a left liver graft, which, because of its smaller size, is more prone to the syndrome than is a right liver graft, said Dr. Takatsuki of Nagasaki (Japan) University.
A left liver graft is the first choice for living donor transplant in Japan because this graft is less likely to experience congestion than is a right lobe graft. Donors with a left graft are also less likely to have serious postoperative complications or to die. However, the graft volume of the left liver is less than that of the right, making it susceptible to the problems of a high portal inflow. Dr. Takatsuki’s novel securing of the hepatic vein to the inferior vena cava increases liver outflow and, hopefully, prevents graft congestion, he said at the annual clinical congress of the American College of Surgeons.
The conventional hepatic vein reconstruction side clamps the middle and left hepatic veins. This common trunk is then joined to the graft hepatic vein. Dr. Takatsuki’s technique takes advantage of the inferior vena cava to increase graft outflow, he noted.
He closes the right hepatic vein with a vascular stapler. He then opens the common trunk of the middle and left hepatic veins and creates a wide cavotomy in the inferior vena cava. "This wide orifice of hepatic vein is anastomosed to the graft hepatic vein. The size of the hepatic vein orifice is easily adjustable to suit the size of the graft hepatic vein," Dr. Takatsuki said.
He reported the results of a study of 47 adult living donor transplants. Of these 47 patients, 21 had the side clamp hepatic vein reconstruction and 26, the new technique of cross-clamping the inferior vena cava.
The patients were a mean of 56 years old and evenly split between men and women. The mean Model for End-Stage Liver Disease(MELD) score was 15.5. Surgery lasted a mean of 915 minutes in the side clamp group and 746 minutes in the cross-clamp group – a significant difference. Blood loss was also significantly less in the cross-clamp group (3,800 g vs.5,450 g).
By postoperative day 7, there were no significant between-group differences in total bilirubin or prothrombin time. There was significantly less ascites in the cross-clamp group.
Dr. Takatsuki saw the same results in a subgroup of 17 patients (7 in the side clamp group and 10 in the cross-clamp group) in whom the graft weight/recipient standard liver volume was less than 30%.
Among these patients – who were at the highest risk for graft failure because of the weight/volume differential – those with the cross-clamped anastomosis had significantly higher graft survival (90% vs. 71%) at 1 year.
Dr. Takatsuki said he had no relevant financial disclosures.
WASHINGTON – A novel anastomosis technique may help avoid small-for-size syndrome in adult living donor liver transplantation, according to Dr. Mitsuhisa Takatsuki.
Reconstructing the hepatic vein by cross-clamping with the inferior vena cava creates improved outflow from the graft. This can avert the potential failure of a left liver graft, which, because of its smaller size, is more prone to the syndrome than is a right liver graft, said Dr. Takatsuki of Nagasaki (Japan) University.
A left liver graft is the first choice for living donor transplant in Japan because this graft is less likely to experience congestion than is a right lobe graft. Donors with a left graft are also less likely to have serious postoperative complications or to die. However, the graft volume of the left liver is less than that of the right, making it susceptible to the problems of a high portal inflow. Dr. Takatsuki’s novel securing of the hepatic vein to the inferior vena cava increases liver outflow and, hopefully, prevents graft congestion, he said at the annual clinical congress of the American College of Surgeons.
The conventional hepatic vein reconstruction side clamps the middle and left hepatic veins. This common trunk is then joined to the graft hepatic vein. Dr. Takatsuki’s technique takes advantage of the inferior vena cava to increase graft outflow, he noted.
He closes the right hepatic vein with a vascular stapler. He then opens the common trunk of the middle and left hepatic veins and creates a wide cavotomy in the inferior vena cava. "This wide orifice of hepatic vein is anastomosed to the graft hepatic vein. The size of the hepatic vein orifice is easily adjustable to suit the size of the graft hepatic vein," Dr. Takatsuki said.
He reported the results of a study of 47 adult living donor transplants. Of these 47 patients, 21 had the side clamp hepatic vein reconstruction and 26, the new technique of cross-clamping the inferior vena cava.
The patients were a mean of 56 years old and evenly split between men and women. The mean Model for End-Stage Liver Disease(MELD) score was 15.5. Surgery lasted a mean of 915 minutes in the side clamp group and 746 minutes in the cross-clamp group – a significant difference. Blood loss was also significantly less in the cross-clamp group (3,800 g vs.5,450 g).
By postoperative day 7, there were no significant between-group differences in total bilirubin or prothrombin time. There was significantly less ascites in the cross-clamp group.
Dr. Takatsuki saw the same results in a subgroup of 17 patients (7 in the side clamp group and 10 in the cross-clamp group) in whom the graft weight/recipient standard liver volume was less than 30%.
Among these patients – who were at the highest risk for graft failure because of the weight/volume differential – those with the cross-clamped anastomosis had significantly higher graft survival (90% vs. 71%) at 1 year.
Dr. Takatsuki said he had no relevant financial disclosures.
WASHINGTON – A novel anastomosis technique may help avoid small-for-size syndrome in adult living donor liver transplantation, according to Dr. Mitsuhisa Takatsuki.
Reconstructing the hepatic vein by cross-clamping with the inferior vena cava creates improved outflow from the graft. This can avert the potential failure of a left liver graft, which, because of its smaller size, is more prone to the syndrome than is a right liver graft, said Dr. Takatsuki of Nagasaki (Japan) University.
A left liver graft is the first choice for living donor transplant in Japan because this graft is less likely to experience congestion than is a right lobe graft. Donors with a left graft are also less likely to have serious postoperative complications or to die. However, the graft volume of the left liver is less than that of the right, making it susceptible to the problems of a high portal inflow. Dr. Takatsuki’s novel securing of the hepatic vein to the inferior vena cava increases liver outflow and, hopefully, prevents graft congestion, he said at the annual clinical congress of the American College of Surgeons.
The conventional hepatic vein reconstruction side clamps the middle and left hepatic veins. This common trunk is then joined to the graft hepatic vein. Dr. Takatsuki’s technique takes advantage of the inferior vena cava to increase graft outflow, he noted.
He closes the right hepatic vein with a vascular stapler. He then opens the common trunk of the middle and left hepatic veins and creates a wide cavotomy in the inferior vena cava. "This wide orifice of hepatic vein is anastomosed to the graft hepatic vein. The size of the hepatic vein orifice is easily adjustable to suit the size of the graft hepatic vein," Dr. Takatsuki said.
He reported the results of a study of 47 adult living donor transplants. Of these 47 patients, 21 had the side clamp hepatic vein reconstruction and 26, the new technique of cross-clamping the inferior vena cava.
The patients were a mean of 56 years old and evenly split between men and women. The mean Model for End-Stage Liver Disease(MELD) score was 15.5. Surgery lasted a mean of 915 minutes in the side clamp group and 746 minutes in the cross-clamp group – a significant difference. Blood loss was also significantly less in the cross-clamp group (3,800 g vs.5,450 g).
By postoperative day 7, there were no significant between-group differences in total bilirubin or prothrombin time. There was significantly less ascites in the cross-clamp group.
Dr. Takatsuki saw the same results in a subgroup of 17 patients (7 in the side clamp group and 10 in the cross-clamp group) in whom the graft weight/recipient standard liver volume was less than 30%.
Among these patients – who were at the highest risk for graft failure because of the weight/volume differential – those with the cross-clamped anastomosis had significantly higher graft survival (90% vs. 71%) at 1 year.
Dr. Takatsuki said he had no relevant financial disclosures.
AT THE ACS Clincal Congress
Major finding: One-year liver graft survival was significantly better in patients with a hepatic vein/inferior vena cava anastomosis than in those who had the traditional hepatic vein side clamp (90% vs. 71%).
Data source: A randomized study involving 47 patients who received a living donor left liver transplant.
Disclosures: Dr. Takatsuki said he had no relevant financial disclosures.