User login
A growing body of literature suggests that patient‐ and family‐centered care can improve patient outcomes[1, 2, 3, 4, 5] as well as patient, family, and provider satisfaction.[6, 7, 8, 9, 10] Engaging patients and families as a way to improve the quality and safety of care has been widely endorsed by leading healthcare organizations,[11, 12, 13] including the Institute of Medicine.[14] In the pediatric inpatient setting, family‐centered rounds (FCR), defined as bedside rounds in which the patient and family share in the control of the management plan as well as in the evaluation of the process itself,[15] potentially provide a consistent venue for family engagement and are recommended by the American Academy of Pediatrics as standard practice.[13]
According to a recent study by Mittal et al.,[16] FCR are the most common type of rounds practiced among pediatric hospitalists surveyed in the United States and Canada. Despite this widespread shift from rounding in a conference room to the bedside with patients and families, there exist only a few studies that provide specific recommendations on conducting FCR.[15, 17, 18] This research has been limited, primarily focusing how rounds are conducted, and further investigation is needed to identify the impact of other processes and elements within the hospital work system that may also affect family engagement during rounds.
The objectives of this study were to: 1) identify strategies to enhance family engagement during FCR drawing from the viewpoints of the various stakeholders on rounds, and 2) characterize these strategies into known elements of hospital work systems and rounding processes using a recognized human factors engineering approach, The Systems Engineering Initiative for Patient Safety (SEIPS) model.[19] According to the SEIPS model, barriers and facilitators to family engagement during FCR are likely embedded in the design of the hospital work systems and rounding process; therefore, we hypothesized that strategies that influence engagement will target all work system and process elements. This work is part of a larger study in which, after prioritization of this group of strategies based on feasibility and sustainability, a bundle of best practices for conducting FCR will be developed, implemented, and evaluated.
METHODS
Study Design
Semistructured interviews using the stimulated recall approach[20, 21] were conducted to understand the cognitive processes of families and healthcare team (HCT) members during FCR. This qualitative study design allowed us to capture comprehensive information from the perspectives of a diverse group of stakeholders on strategies for improving family engagement during FCR.
Setting and Participants
This study was conducted at a children's hospital in Wisconsin, where FCR were initiated in 2007 with the transition to a new hospital facility. The expectation is that FCR are conducted daily with the family and the patient's HCT, consisting of at least an attending physician and nurse. Typically, multiple residents, interns, and medical students are present along with a combination of other providers, including consulting subspecialists, a fellow, nurse practitioner, respiratory therapist, or pharmacist. When this study was conducted, attendees received little to no formal training regarding their role on FCR. As part of a larger study, English‐speaking patients and/or families admitted to 1 of 4 inpatient services (2 hospitalist, 1 pulmonary, and 1 hematology/oncology), and their associated HCT members were enrolled and their bedside rounds were video recorded. A purposive sampling technique[22, 23] was employed, recruiting interviewees that represented the various groups of stakeholders of rounds, including parents, children, attending physicians, resident physicians, medical students, and nurses. For child interviews, we restricted selection to children aged 8 to 17 years to ensure the ability to understand the interviewing process and provide feedback. Families were consented and children were assented. The University of Wisconsin‐Madison Health Sciences Institutional Review Board approved this study.
Interviews and analysis occurred concurrently in an iterative process, informing each other. Thus, recruitment continued until we reached theoretical saturation,[24, 25] the point at which additional interviews did not provide new information or further conceptual development.
Study Procedures
All interviews were conducted by trained researchers, who used the same semistructured interview guide. During each interview, the interviewee was instructed to watch his/her own rounding video and pause when noticing something that made it easy (facilitator) or hard (barrier) to engage the family. Every time the interviewee paused the video to describe what was noticed, the interviewer then asked follow‐up, open‐ended questions to solicit specific information that focused on strategies for enhancing family engagement during FCR. For instance, if the issue identified was a barrier, the interviewer asked, What would you have wanted to happen differently? and if the issue identified was a facilitator, the interviewer asked, How could we ensure that would happen for everyone? The interviewee rewound the video as needed. If the interviewee had not stopped the video by the halfway point, the interviewer would pause the video and review the instructions. After the interviewee had viewed and commented on the entire rounding video, an opportunity was offered to reflect on other factors that influence family engagement during rounds, and additional questions were asked as necessary to fully understand the interviewee's views. All interviews were audio recorded and personal identifiers were removed prior to data analysis.
Data Analysis
Two research assistants reviewed the audio recordings and identified all instances related to strategies for improving family engagement during FCR. There was no screening of strategies (ie, if an interviewee suggested a strategy was related to improving family engagement, it was categorized as such). To ensure intercoder reliability, these assistants, under the supervision of a researcher (L.D.), reviewed the coding process together, held consensus meetings, and crosschecked interviews for coding consensus. A researcher (A.X.) transcribed all strategy‐related instances, which were then reviewed by two additional researchers (M.K., P.C.). To organize, sort, and code the data, interview transcripts were imported in the NVivo qualitative data analysis software (QSR International, Doncaster, Victoria, Australia). The research group then performed a qualitative content analysis of the transcripts[26] and categorized the strategies in an iterative process (information provided on request).
To ensure that all strategies remained conceptually similar within categories, the constant comparative method[27, 28] was applied to the coding process. This involved comparing: 1) strategy‐related instances from the same participants, 2) strategy‐related instances from different participants in the same groups, 3) strategy‐related instances from different participants in different groups, 4) a coded strategy with other coded strategies, 5) coded strategies with categories, and 6) a category with other categories. A strategy‐related instance could be coded under more than one strategy or category. For instance, one interviewee said conducting things that can be done without family beforehand, and presenting and reviewing the plan with family. This was coded under both the strategy conducting rounds in another location without family and then at the bedside with family in the location of FCR category and the strategy focusing presentation on assessment and plan in the communication style category.
RESULTS
A total of 37 interviews were conducted with 11 parents, 4 children, and 22 HCT members (8 attending physicians, 6 resident physicians, 5 medical students, and 3 nurses) in 24 videos of rounding sessions. The duration of the interviews ranged from 30 to 60 minutes.
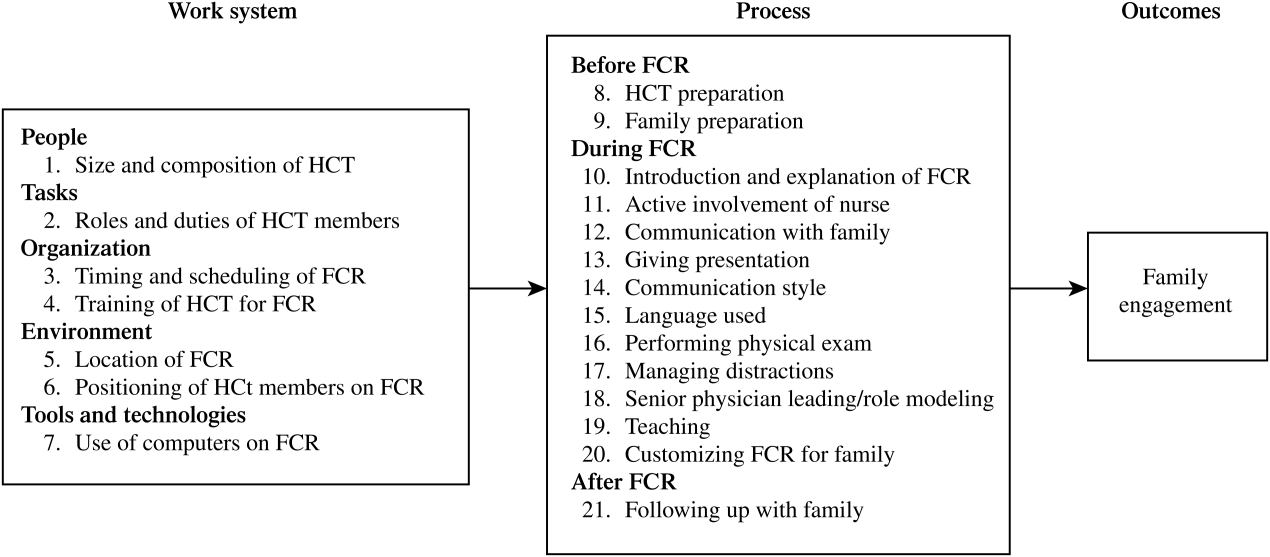
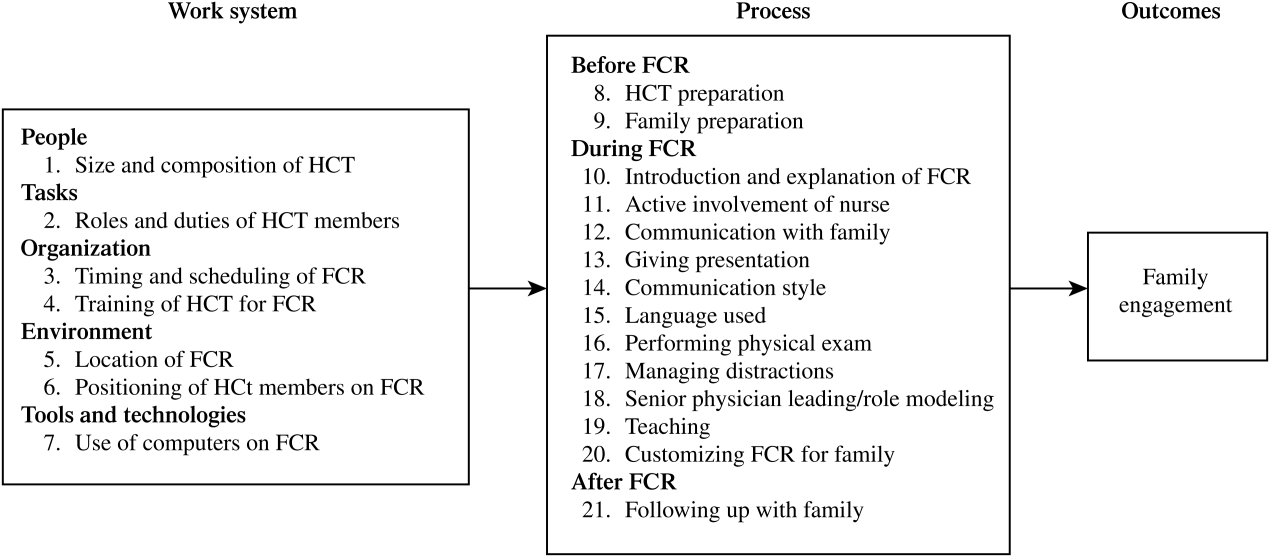
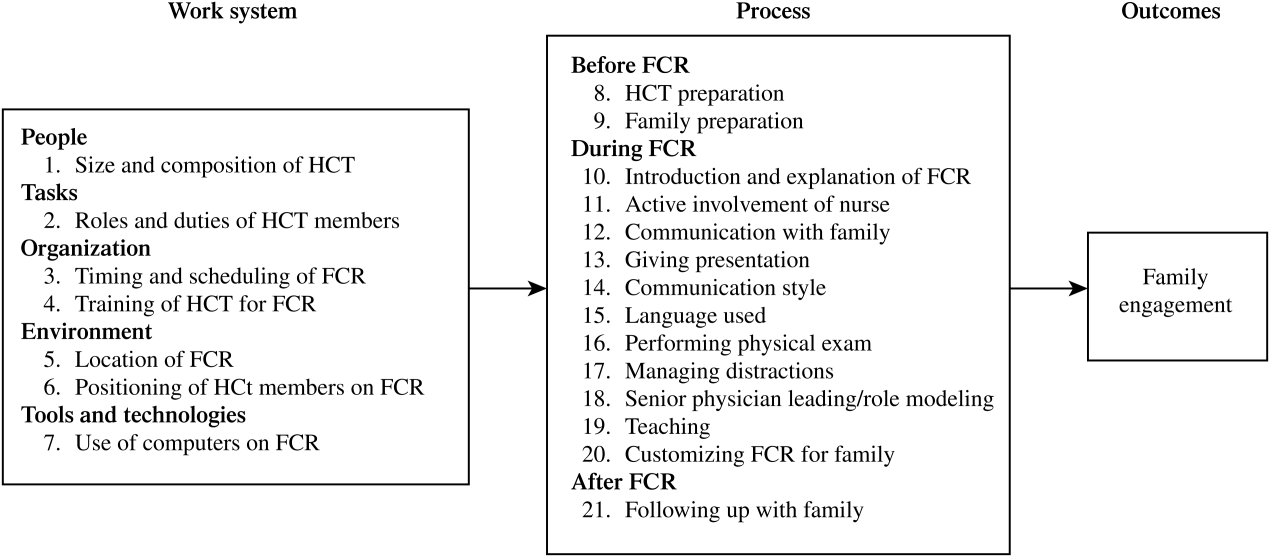
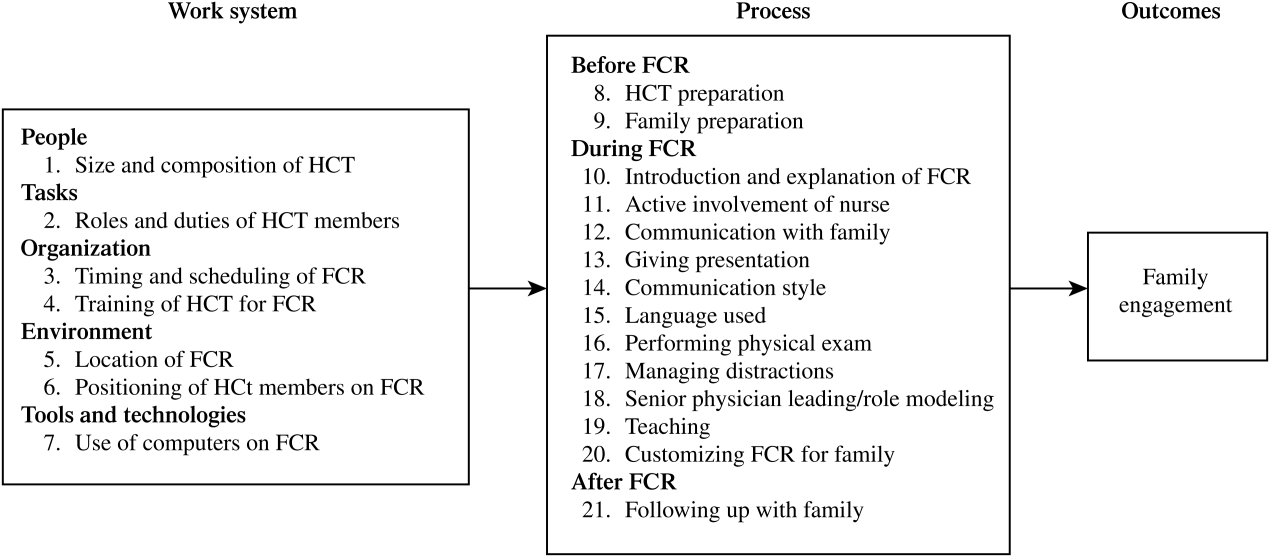
A total of 338 separate instances related to strategies for improving family engagement on FCR were identified and sorted into 21 categories. Using the SEIPS model, these categories were organized into 2 themes: the work system and process of FCR (Figure 1). Of the 21 categories, 12 were mentioned by both families (parents and/or children) and HCT members and 9 were solely mentioned by the HCT.
Work System of FCR
Table 1 shows the categories of strategies related to the 5 elements of the FCR work system.[29, 30] Illustrative quotes from the interviews (Q) are presented in Table 2.
| Work System Elements | Categories | Strategies | P (11) | C (4) | Att. (8) | Res. (6) | MS (5) | RN (3) |
|---|---|---|---|---|---|---|---|---|
| ||||||||
| People | 1. Size and composition of HCT | Have a smaller HCT conduct FCR | X | X | X | X | ||
| Ensure all relevant disciplines present on FCR | X | X | X | X | X | |||
| Task | 2. Roles and duties of HCT members | Define roles/duties of HCT members on FCR | X | X | ||||
| Organization | 3. Timing and scheduling of FCR | Schedule FCR, inform participants beforehand | X | X | X | |||
| 4. Training of HCT for FCR | Train HCT on how to present on FCR | X | X | |||||
| Environment | 5. Location of FCR | At bedside with family and patient | X | X | ||||
| In another location with HCT, then at bedside | X | X | X | X | ||||
| In another location with family but without child | X | |||||||
| 6. Positioning of HCT members on FCR | Sit down with family | X | X | X | X | X | ||
| Stand close to or in a semicircle around family | X | X | X | X | X | |||
| Tools and technologies | 7. Use of computers on FCR | Use computer to support family interaction | X | X | X | X | ||
| Don't use a computer | X | X | ||||||
|
| Q1: I'm intimidated to ask a question. It seems like there are too many peopleI like a smaller group. (P5) |
| Q2: Sometimes rounds are the only time that the parents are there to see the entire teamso in that way, including [the entire team] at the rounds makes more sense. (MS1) |
| Q3: There needs to be much more clear roles about who is supposed to do what, and it should be predictable. (Att.2) |
| Q4: ([T]iming of rounds) is a huge source of frustration for families. If [physicians] know in which order they will go for patients, they can call our charge nurse or unit clerk or page nurses with that information. (RN1) |
| Q5: ([W]ith a notice of the rounding schedule), I can be ahead of time, trying to think of questions. (P10) |
| Q6: [I]t would be really nice to see somebody do a presentation in a medical eye's version and then also in the family‐centered version. (MS5) |
| Q7: [H]aving the medical students practice with the senior residentis a good way of doing it. (Res.4) |
| Q8: [M]aybe some small groups where you practice this among students. (MS5) |
| Q9: It would be better to be in the room for communication. (Att.1) |
| Q10: You could have sort of hallway rounds, which is much more medical oriented, and inside‐the‐room rounds, which is much more talking with the parent. (P1) |
| Q11: [H]ave sit‐down rounds with parents and families. (Res.5) |
| Q12: I've seen some attending physicians who sat down. I think that could be helpful to be on the same level as the patient and family. (Res.2) |
| Q13: [M]aybe formation of semicircle or something like that, where we can see everybody a little more clearly, I think that would be very helpful. (P10) |
| Q14: I find the presence of a computer incredibly offensive and obstructivewhen you are supposed to be able to interact with the patient. (Att.6) |
| Q15: One of the things I started doing is having one of the other resident physicians have the computer, so just relying on them to do the orders, and me just being there mainly for being the presenter of rounds. (Res.4) |
People
Two seemingly contradictory strategies were proposed. Some interviewees suggested a smaller HCT with members most familiar to the family (Q1), whereas other interviewees stressed the need to involve different relevant disciplines (eg, social worker, nutritionist) during rounds (Q2).
Tasks
Both attending and resident physicians emphasized the importance of defining the role of each HCT member before rounding (Q3). Interviewees also suggested these roles should be explained to families, ideally at admission.
Organization
Many interviewees suggested the need to consistently schedule rounds (Q4) and to inform families and nurses of the schedule so all parties could plan ahead (Q5). Some resident physicians and medical students recommended training of learners on how to give a family‐centered presentation using methods such as role modeling (Q6) and practicing with the senior resident physician (Q7) or in small groups (Q8).
Environment
Some interviewees suggested conducting rounds in patient rooms (Q9). Others suggested conducting rounds first in another location (eg, hallway) without the family and then going to the bedside to round with the family (Q10). There were also interviewees who suggested conducting rounds in another location (eg, conference room) with the family (Q11). When conducting rounds in the patient room, some interviewees suggested that some HCT members (eg, attending and senior resident physicians) could sit down with the family (Q12), with the rest of the HCT standing close to the family in a semicircle (Q13).
Tools and Technologies
Some interviewees thought that conversation with families could be negatively affected by the use of computers, and therefore suggested not using them on FCR (Q14). Alternatively, other interviewees considered computers a tool to facilitate the interaction between the HCT and families, such as showing x‐rays or lab values. Several interviewees suggested that computers should not be positioned to block eye contact between HCT members and families; therefore, only HCT members not presenting should use computers (Q15).
Process of FCR
Table 3 shows the categories of strategies related to the process of FCR, which were categorized into 3 phases. Illustrative quotes are presented in Table 4.
| Process Phases | Categories | Strategies | P (11) | C (4) | Att. (8) | Res. (6) | MS (5) | RN (3) |
|---|---|---|---|---|---|---|---|---|
| ||||||||
| Before FCR | 8. HCT preparation | Collect and prepare pertinent information | X | X | X | X | ||
| 9. Family preparation | Orient family to rounding process | X | X | X | X | X | ||
| Build relationship with family | X | X | X | |||||
| Ask family for permission and preferences | X | X | X | |||||
| During FCR | 10. Introduction and explanation of FCR | Introduce HCT and family to each other | X | X | X | X | X | |
| Explain interactive rounding process | X | X | X | |||||
| 11. Active involvement of nurse | Giving nurse opportunity to actively participate | X | X | |||||
| 12. Communication with family | Give family opportunity to actively participate | X | X | X | X | X | X | |
| Address family's questions/concerns | X | X | X | X | X | |||
| Explain tests, findings and results to family | X | X | X | X | X | |||
| Confirm family understanding | X | X | X | |||||
| 13. Giving presentation | Restructure the presentation | X | X | |||||
| Shorten the presentation | X | X | X | |||||
| Focus presentation on assessment and plan | X | X | X | X | X | |||
| Summarize plan for family | X | X | X | |||||
| Avoid discussion of sensitive topics | X | X | X | |||||
| 14. Communication style | Present in a conversational manner | X | X | X | ||||
| Use an engaging communication style | X | X | X | X | X | |||
| 15. Language used | Use qualitative language | X | X | X | ||||
| Use plain language | X | X | X | X | X | |||
| 16. Performing physical exam | Pause and confirm physical exam | X | ||||||
| 17. Managing distractions | Minimize distractions and interruptions | X | X | X | X | X | X | |
| 18. Senior physician leading/role modeling | Attending/senior resident physician should lead, direct and be a role model on FCR rounds | X | X | |||||
| 19. Teaching | Ask family permission and involve in teaching | X | X | |||||
| 20. Customizing FCR for family | Adapt rounds to family's needs | X | X | X | X | |||
| After FCR | 21. Following up with family | HCT members follow up with family | X | X | X | |||
|
| Q1: [Medical students and residents] actually had a chance to do a quick round, an abbreviated presentation to put together an outline of what we're going to talk about before we even do it. (MS2) |
| Q2: I would like to know exactly what's going onbefore I walk in. (Att.6) |
| Q3: [T]he nurse did give me the fore‐warning that rounds would be coming and it was usually like a group of 8 to 10so I was prepared for that. (P7) |
| Q4: What went well is that I had already connected with this mom and the daughter prior to this rounding encounter. (Res.3) |
| Q5: [Y]ou could ask the patient or the parents if they want the child there. (P3) |
| Q6: [Families] really want to know what your role is on the team. (Att.5) |
| Q7: I guess it would be easier to figure out who you need to direct questions to. (P3) |
| Q8: [L]etting the family anticipate what rounding is going to be like and when the opportunity is going to come up to talk. I think that can help. (Res.2) |
| Q9: I think the decision making is probably the most critical partthere is really no substitute for [families] being involved in the decisionwithout a lot of medical conversation and analysis. (P1) |
| Q10: The family was proactive enough to ask questions, but they were never really given entrance to ask questions.No one had said do you have any questions?' (Res.4) |
| Q11: It is really important for the doctors to listen to them, to know that they are the parents and they know their children best. (RN3) |
| Q12: I think sometimes when you are teaching, some of the information could potentially be scary to the family. What I would hope is letting the family feel like they are part of the education process. (Res.2) |
| Q13: Sometimes nurses are asked initially, do you have anything to add,' which I think is a good way to startbecause we have probably the most current and updated information. (RN1) |
| Q14: When I was talking about the physical exam partmaybe at that point, if I could just stop talking, we couldconfirm that exam. (Res.3) |
| Q15: It's distracting if different groups have individual discussions when you are trying to keep the group focused on this particular patient for rounds. (Att.7) |
| Q16: It's just the basic thing that I try to tell residents. I do this hopefully at least once every time I am on services with the team. (Att.1) |
| Q17: ([C]hanging rounds depending on the families) would be the ideal situationthinking about what's helpful for a family. (Att.6) |
| Q18: What I usually see when things work well after we leave is that the nurse can still stick around the family. (Res.4) |
| Q19: [T]he students have to go back in the afternoon to talk with the family about what the treatment point is and answer any questions. (MS2) |
Before FCR
To engage families during FCR, many interviewees suggested that both the HCT and families need preparation. HCT members suggested that medical students should collect up‐to‐date patient information and review it with the senior resident physicians (Q1) to reach a consensus before starting FCR (Q2). To prepare families for rounds, parents and HCT members suggested that the HCT should orient families to the rounding process (Q3), build relationships with families (Q4), and ask for their permission and preference regarding participation in rounds (Q5).
During FCR
A number of strategies focused on the beginning of rounds. Parents, children, and HCT members stressed the need to introduce HCT members by role (Q6) and inform families to whom to direct questions (Q7). It was also suggested that parents introduce themselves to the team. Some interviewees recommended that the HCT explain the rounding process to families at this time (Q8).
Interviewees recommended strategies related to communication between the HCT and families during rounds. Many interviewees suggested restructuring and shortening the presentation by focusing on the assessment and plan (Q9). According to all interviewees, the HCT should present in a conversational manner and use an engaging communication style (eg, smiling, making eye contact, using appropriate humor) and appropriate language (eg, qualitative trend instead of numbers, plain language instead of medical jargon) to communicate with families. To ensure families understanding, HCT members should encourage and address their questions and concerns (Q10). In addition, families should be given the opportunity to provide information (eg, patient history and overnight events) and to express their opinions about the plan (Q11). If teaching is done during rounds, the HCT should involve families and ask for permission (Q12).
Other strategies on rounds were suggested, such as giving nurses the opportunity to actively participate (Q13), pausing and confirming physical exam findings (Q14), minimizing distractions and interruptions (Q15), attending and/or senior resident physicians leading and being role models for FCR (Q16), and adapting rounds to families' needs (Q17).
After FCR
Some HCT members talked about the importance of following up with families after rounds. Specifically, suggestions that nurses could stay with families immediately after rounds (Q18) were made, whereas physicians could return to families later in the day (Q19).
DISCUSSION
Using recognized qualitative systems engineering methods, we identified a broad range of strategies for enhancing family engagement on FCR from the perspectives of a diverse group of stakeholders on rounds and described how these strategies target known fundamental elements in both the hospital work system and rounding process. We highlight recommendations on the content and style of communication during rounds with families, but also introduce more complex system‐wide elements that likely play a role in family engagement, such as the composition of the HCT; organization and environment of rounds; tools and technologies used; and preparation of the HCT, families, and patients beforehand.
Our research both confirms and builds upon practices previously described in the FCR literature.[17, 31, 32] In a case report by Muething et al.,[17] recommendations were developed using a series of plan‐do‐study‐act cycles to determine the components needed to conduct FCR. These components included: 1) determining family preference prior to rounds, 2) defining HCT roles, 3) introducing HCT to family and explaining the purpose of rounds, 4) describing what is shared and how it is said on rounds, 5) describing the contribution of families, nurses, and ancillary staff, and 6) providing teaching recommendations to senior physicians on rounds. All of these components are suggested by one or more of the participants in our study. In addition, our research identifies a variety of new work system‐related strategies, such as scheduling rounds, using computers appropriately on rounds, and providing training of HCT members beforehand.
Of particular interest was the discordance between strategies mentioned by families and the various members of the HCT. Although HCT members mentioned all identified strategies, families were interested in certain ones. Regarding the structure of FCR, families showed particular interest in HCT composition, timing and scheduling of rounds, location of rounds, and positioning of the HCT. In comparison, families did not mention the importance of the roles and duties of HCT members, HCT preparation for rounds, and use of computers during rounds. With respect to the FCR process, families stressed the importance of family preparation beforehand, introduction and explanation of rounds at the beginning, presentation style and communication style, customization, and management of distractions during rounds. None of the families, however, mentioned the rest of the strategies, including HCT preparation before rounds, involvement of the nurse, teaching and performing the physical exam, the role of the attending and senior resident roles during rounds, and following up with the family after rounds. These different perspectives are likely, in part, inherent to the different roles and experiences of parents and HCT members. For example, parents' knowledge of what goes on in the hospital outside of FCR, such as orientation and preparation of HCT members for rounds, is relatively limited. Future research using methods to evaluate and prioritize strategies as well as understanding reasons for contradicting strategies is warranted.
We recognize that, although family engagement is recommended as a critical component of care, strategies to improve engagement may be in direct opposition to other goals of the HCT. For example, some of our participants suggest having a smaller team may be more beneficial for family engagement on rounds. In some settings, it may be feasible to have a small team; however, in institutions that accommodate a large number of learners, excluding students from the teaching opportunity of rounds may actually compromise educational experiences. In patients with chronic and/or complex care, a larger multidisciplinary team may better facilitate information exchange among disciplines and expedite discharge planning. Moreover, one might speculate that it may not be that the size affects family engagement as much as the composition of the team, especially if tailored to the needs of the patient. For example, a large team consisting of primarily physicians and trainees may not be as engaging as the same sized team with one attending physician and a respiratory therapist, case manager, and consulting subspecialist. Finding a balance between engaging families, teaching learners, and maintaining efficiency is paramount and needs to be studied further.
This study has several limitations. Our data are from a single academic children's hospital, which may limit generalizability due to a small sampling of multiple stakeholders on different services, our specific patient population, HCT composition and roles, and teaching needs. However, we face similar barriers to engaging families during rounds as those published from both another single institution[17] and a national sampling of pediatric hospitalists.[16] Furthermore, our recommended strategies to address the FCR process are supported by prior work.[17] Because this study was voluntary, our interviewees were likely more engaged participants in general. Specifically, the viewpoints of engaged families and HCT members may not represent the viewpoints of those who are less engaged or supportive of FCR. We did not enroll nonEnglish‐speaking patients and families, which is a potential direction for future research. In our interviews, we also relied solely on the perceptions of rounding participants, rather than those of outside observers or researchers, which may only provide a partial perspective of potential strategies to improve family engagement. Last, this qualitative research approach does not provide quantitative information regarding whether certain strategies are preferred by a majority of participants, which we hope to address in future research.
This work is part of a larger study that aims to implement a bundle of these strategies after stakeholder prioritization based on impact on family engagement, feasibility, and sustainability. We plan to systematically evaluate the implementation process of these strategies and measure their impact on family engagement and, ultimately, patient safety. One or more of these strategies could be implemented in a similar manner at other hospitals depending on specific institutional needs.
In conclusion, as recently reflected by Barry et al. in The New England Journal of Medicine, Although talk about patient‐centered care is ubiquitous in modern health care, one of the greatest challenges of turning the rhetoric into reality continues to be routinely engaging patients in decision making.[33] FCR provide a crucial opportunity for family involvement in daily care decisions in the pediatric inpatient setting. This study highlights the importance of prior work defining the components of involving families in this process, while emphasizing new systems‐based strategies that further facilitate the expectation of family engagement in the care of hospitalized children.
Disclosures
This work was funded through an Agency for Healthcare Research and Quality Health Services Research Dissemination and Demonstration Grant, R18 HS018680, and also supported by the Arthur Vining Davis Foundation and the National Patient Safety Foundation through the James S. Todd Memorial Research Award. Funding organizations did not contribute to the design and conduct of study; collection, management, analysis, and interpretation of data; or preparation, review, or approval of the manuscript. The authors report no conflicts of interest.
- , , , et al. The impact of patient‐centered care on outcomes. J Fam Pract. 2000;49:796–804.
- , , , et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ. 2001;323:908–911.
- , , . Improvement in the family‐centered medical home enhances outcomes for children and youth with special healthcare needs. J Ambul Care Manage. 2009;32:188–196.
- , , . Associations of family‐centered care with health care outcomes for children with special health care needs. Matern Child Health J. 2011;15:794–805.
- , , , , Can a patient‐centered medical home lead to better patient outcomes? The quality implications of Geisinger's ProvenHealth Navigator. Am J Med Qual. 2012;27:210–216.
- , , . Perceptions of health care providers' communication: relationships between patient‐centered communication and satisfaction. Health Commun. 2004;16:363–383.
- , . Satisfaction with care and ease of using health care services among parents of children with special health care needs: the roles of race/ethnicity, insurance, language, and adequacy of family‐centered care. Pediatrics. 2006;117:1184–1196.
- , , , . A randomized, controlled trial of bedside versus conference‐room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120:275–280.
- , , , , . Effect of patient‐centered care on patient satisfaction and quality of care. J Nurs Care Qual. 2008;23:316–321.
- , , . Implementing family‐centered rounds: pediatric residents' perceptions. Clin Pediatr (Phila) 2010;49:228–234.
- ACGME Program Requirements for Graduate Medical Education in Pediatrics. 2007. Available at: http://www.acgme.org/acWebsite/downloads/RRC_progReq320_pediatrics_07012007.pdf. Accessed February 10, 2012.
- Speak up: prevent errors in your child's care. 2011. The Joint Commission Web site. Available at: http://www.jointcommission.org/Speak_Up_Prevent_Errors_in_Your_Childs_Care/. Accessed May 11, 2012.
- Patient‐ and family‐centered care and the pediatrician's role. Pediatrics. 2012;129:394–404.
- Committee on Quality of Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press; 2001.
- , , , . Defining family‐centered rounds. Teach Learn Med. 2007;19:319–322.
- , , , et al. Family‐centered rounds on pediatric wards: A PRIS network survey of US and Canadian hospitalists. Pediatrics. 2010;126:37–43.
- , , , , . Family‐centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119:829–832.
- , , , . Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: a qualitative study. Acad Med. 2008;83:292–297.
- , , , et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care. 2006;15:i50–i58.
- , . IPR—a validated model for the 1990s and beyond. Couns Psychol. 1990;18:436–440.
- , . Auto‐ and allo‐confrontation as tools for reflective activities. Appl Ergon. 2004;35:531–540.
- . Qualitative Research and Evaluation Methods. 3rd ed. Thousand Oaks, CA: Sage Publications; 2002.
- , . Doing Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publications; 1999.
- . Sample size in qualitative research. Res Nurs Health. 1995;18:179–183.
- , . Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Newbury Park, CA: Sage Publications; 1998.
- , . Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–112.
- . A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Qual Quant. 2002;36:391–409.
- . Theoretical Sensitivity: Advances in the Methodology of Grounded Theory. Mill Valley, CA: Sociology Press; 1978.
- , . Balance theory of job design. In: Karwowski W, ed. International Encyclopedia of Ergonomics and Human Factors. London: Taylor 2000:1181–1184.
- , . A balance theory of job design for stress reduction. Int J Ind Ergon. 1989;4:67–79.
- Institute for Patient‐ and Family‐Centered Care. Applying patient‐ and family‐centered concepts to bedside rounds. 2010. Available at: http://www.ipfcc.org/advance/topics/PH_RD_Applying_PFCC_Rounds_012009.pdf. Accessed May 11, 2012.
- . A fundamental shift: family‐centered rounds in an academic medical center. Hospitalist. 2006;10:45–46.
- , Shared decision making—pinnacle of patient‐centered care. N Engl J Med. 2012;366:780–781.
A growing body of literature suggests that patient‐ and family‐centered care can improve patient outcomes[1, 2, 3, 4, 5] as well as patient, family, and provider satisfaction.[6, 7, 8, 9, 10] Engaging patients and families as a way to improve the quality and safety of care has been widely endorsed by leading healthcare organizations,[11, 12, 13] including the Institute of Medicine.[14] In the pediatric inpatient setting, family‐centered rounds (FCR), defined as bedside rounds in which the patient and family share in the control of the management plan as well as in the evaluation of the process itself,[15] potentially provide a consistent venue for family engagement and are recommended by the American Academy of Pediatrics as standard practice.[13]
According to a recent study by Mittal et al.,[16] FCR are the most common type of rounds practiced among pediatric hospitalists surveyed in the United States and Canada. Despite this widespread shift from rounding in a conference room to the bedside with patients and families, there exist only a few studies that provide specific recommendations on conducting FCR.[15, 17, 18] This research has been limited, primarily focusing how rounds are conducted, and further investigation is needed to identify the impact of other processes and elements within the hospital work system that may also affect family engagement during rounds.
The objectives of this study were to: 1) identify strategies to enhance family engagement during FCR drawing from the viewpoints of the various stakeholders on rounds, and 2) characterize these strategies into known elements of hospital work systems and rounding processes using a recognized human factors engineering approach, The Systems Engineering Initiative for Patient Safety (SEIPS) model.[19] According to the SEIPS model, barriers and facilitators to family engagement during FCR are likely embedded in the design of the hospital work systems and rounding process; therefore, we hypothesized that strategies that influence engagement will target all work system and process elements. This work is part of a larger study in which, after prioritization of this group of strategies based on feasibility and sustainability, a bundle of best practices for conducting FCR will be developed, implemented, and evaluated.
METHODS
Study Design
Semistructured interviews using the stimulated recall approach[20, 21] were conducted to understand the cognitive processes of families and healthcare team (HCT) members during FCR. This qualitative study design allowed us to capture comprehensive information from the perspectives of a diverse group of stakeholders on strategies for improving family engagement during FCR.
Setting and Participants
This study was conducted at a children's hospital in Wisconsin, where FCR were initiated in 2007 with the transition to a new hospital facility. The expectation is that FCR are conducted daily with the family and the patient's HCT, consisting of at least an attending physician and nurse. Typically, multiple residents, interns, and medical students are present along with a combination of other providers, including consulting subspecialists, a fellow, nurse practitioner, respiratory therapist, or pharmacist. When this study was conducted, attendees received little to no formal training regarding their role on FCR. As part of a larger study, English‐speaking patients and/or families admitted to 1 of 4 inpatient services (2 hospitalist, 1 pulmonary, and 1 hematology/oncology), and their associated HCT members were enrolled and their bedside rounds were video recorded. A purposive sampling technique[22, 23] was employed, recruiting interviewees that represented the various groups of stakeholders of rounds, including parents, children, attending physicians, resident physicians, medical students, and nurses. For child interviews, we restricted selection to children aged 8 to 17 years to ensure the ability to understand the interviewing process and provide feedback. Families were consented and children were assented. The University of Wisconsin‐Madison Health Sciences Institutional Review Board approved this study.
Interviews and analysis occurred concurrently in an iterative process, informing each other. Thus, recruitment continued until we reached theoretical saturation,[24, 25] the point at which additional interviews did not provide new information or further conceptual development.
Study Procedures
All interviews were conducted by trained researchers, who used the same semistructured interview guide. During each interview, the interviewee was instructed to watch his/her own rounding video and pause when noticing something that made it easy (facilitator) or hard (barrier) to engage the family. Every time the interviewee paused the video to describe what was noticed, the interviewer then asked follow‐up, open‐ended questions to solicit specific information that focused on strategies for enhancing family engagement during FCR. For instance, if the issue identified was a barrier, the interviewer asked, What would you have wanted to happen differently? and if the issue identified was a facilitator, the interviewer asked, How could we ensure that would happen for everyone? The interviewee rewound the video as needed. If the interviewee had not stopped the video by the halfway point, the interviewer would pause the video and review the instructions. After the interviewee had viewed and commented on the entire rounding video, an opportunity was offered to reflect on other factors that influence family engagement during rounds, and additional questions were asked as necessary to fully understand the interviewee's views. All interviews were audio recorded and personal identifiers were removed prior to data analysis.
Data Analysis
Two research assistants reviewed the audio recordings and identified all instances related to strategies for improving family engagement during FCR. There was no screening of strategies (ie, if an interviewee suggested a strategy was related to improving family engagement, it was categorized as such). To ensure intercoder reliability, these assistants, under the supervision of a researcher (L.D.), reviewed the coding process together, held consensus meetings, and crosschecked interviews for coding consensus. A researcher (A.X.) transcribed all strategy‐related instances, which were then reviewed by two additional researchers (M.K., P.C.). To organize, sort, and code the data, interview transcripts were imported in the NVivo qualitative data analysis software (QSR International, Doncaster, Victoria, Australia). The research group then performed a qualitative content analysis of the transcripts[26] and categorized the strategies in an iterative process (information provided on request).
To ensure that all strategies remained conceptually similar within categories, the constant comparative method[27, 28] was applied to the coding process. This involved comparing: 1) strategy‐related instances from the same participants, 2) strategy‐related instances from different participants in the same groups, 3) strategy‐related instances from different participants in different groups, 4) a coded strategy with other coded strategies, 5) coded strategies with categories, and 6) a category with other categories. A strategy‐related instance could be coded under more than one strategy or category. For instance, one interviewee said conducting things that can be done without family beforehand, and presenting and reviewing the plan with family. This was coded under both the strategy conducting rounds in another location without family and then at the bedside with family in the location of FCR category and the strategy focusing presentation on assessment and plan in the communication style category.
RESULTS
A total of 37 interviews were conducted with 11 parents, 4 children, and 22 HCT members (8 attending physicians, 6 resident physicians, 5 medical students, and 3 nurses) in 24 videos of rounding sessions. The duration of the interviews ranged from 30 to 60 minutes.
A total of 338 separate instances related to strategies for improving family engagement on FCR were identified and sorted into 21 categories. Using the SEIPS model, these categories were organized into 2 themes: the work system and process of FCR (Figure 1). Of the 21 categories, 12 were mentioned by both families (parents and/or children) and HCT members and 9 were solely mentioned by the HCT.
Work System of FCR
Table 1 shows the categories of strategies related to the 5 elements of the FCR work system.[29, 30] Illustrative quotes from the interviews (Q) are presented in Table 2.
| Work System Elements | Categories | Strategies | P (11) | C (4) | Att. (8) | Res. (6) | MS (5) | RN (3) |
|---|---|---|---|---|---|---|---|---|
| ||||||||
| People | 1. Size and composition of HCT | Have a smaller HCT conduct FCR | X | X | X | X | ||
| Ensure all relevant disciplines present on FCR | X | X | X | X | X | |||
| Task | 2. Roles and duties of HCT members | Define roles/duties of HCT members on FCR | X | X | ||||
| Organization | 3. Timing and scheduling of FCR | Schedule FCR, inform participants beforehand | X | X | X | |||
| 4. Training of HCT for FCR | Train HCT on how to present on FCR | X | X | |||||
| Environment | 5. Location of FCR | At bedside with family and patient | X | X | ||||
| In another location with HCT, then at bedside | X | X | X | X | ||||
| In another location with family but without child | X | |||||||
| 6. Positioning of HCT members on FCR | Sit down with family | X | X | X | X | X | ||
| Stand close to or in a semicircle around family | X | X | X | X | X | |||
| Tools and technologies | 7. Use of computers on FCR | Use computer to support family interaction | X | X | X | X | ||
| Don't use a computer | X | X | ||||||
|
| Q1: I'm intimidated to ask a question. It seems like there are too many peopleI like a smaller group. (P5) |
| Q2: Sometimes rounds are the only time that the parents are there to see the entire teamso in that way, including [the entire team] at the rounds makes more sense. (MS1) |
| Q3: There needs to be much more clear roles about who is supposed to do what, and it should be predictable. (Att.2) |
| Q4: ([T]iming of rounds) is a huge source of frustration for families. If [physicians] know in which order they will go for patients, they can call our charge nurse or unit clerk or page nurses with that information. (RN1) |
| Q5: ([W]ith a notice of the rounding schedule), I can be ahead of time, trying to think of questions. (P10) |
| Q6: [I]t would be really nice to see somebody do a presentation in a medical eye's version and then also in the family‐centered version. (MS5) |
| Q7: [H]aving the medical students practice with the senior residentis a good way of doing it. (Res.4) |
| Q8: [M]aybe some small groups where you practice this among students. (MS5) |
| Q9: It would be better to be in the room for communication. (Att.1) |
| Q10: You could have sort of hallway rounds, which is much more medical oriented, and inside‐the‐room rounds, which is much more talking with the parent. (P1) |
| Q11: [H]ave sit‐down rounds with parents and families. (Res.5) |
| Q12: I've seen some attending physicians who sat down. I think that could be helpful to be on the same level as the patient and family. (Res.2) |
| Q13: [M]aybe formation of semicircle or something like that, where we can see everybody a little more clearly, I think that would be very helpful. (P10) |
| Q14: I find the presence of a computer incredibly offensive and obstructivewhen you are supposed to be able to interact with the patient. (Att.6) |
| Q15: One of the things I started doing is having one of the other resident physicians have the computer, so just relying on them to do the orders, and me just being there mainly for being the presenter of rounds. (Res.4) |
People
Two seemingly contradictory strategies were proposed. Some interviewees suggested a smaller HCT with members most familiar to the family (Q1), whereas other interviewees stressed the need to involve different relevant disciplines (eg, social worker, nutritionist) during rounds (Q2).
Tasks
Both attending and resident physicians emphasized the importance of defining the role of each HCT member before rounding (Q3). Interviewees also suggested these roles should be explained to families, ideally at admission.
Organization
Many interviewees suggested the need to consistently schedule rounds (Q4) and to inform families and nurses of the schedule so all parties could plan ahead (Q5). Some resident physicians and medical students recommended training of learners on how to give a family‐centered presentation using methods such as role modeling (Q6) and practicing with the senior resident physician (Q7) or in small groups (Q8).
Environment
Some interviewees suggested conducting rounds in patient rooms (Q9). Others suggested conducting rounds first in another location (eg, hallway) without the family and then going to the bedside to round with the family (Q10). There were also interviewees who suggested conducting rounds in another location (eg, conference room) with the family (Q11). When conducting rounds in the patient room, some interviewees suggested that some HCT members (eg, attending and senior resident physicians) could sit down with the family (Q12), with the rest of the HCT standing close to the family in a semicircle (Q13).
Tools and Technologies
Some interviewees thought that conversation with families could be negatively affected by the use of computers, and therefore suggested not using them on FCR (Q14). Alternatively, other interviewees considered computers a tool to facilitate the interaction between the HCT and families, such as showing x‐rays or lab values. Several interviewees suggested that computers should not be positioned to block eye contact between HCT members and families; therefore, only HCT members not presenting should use computers (Q15).
Process of FCR
Table 3 shows the categories of strategies related to the process of FCR, which were categorized into 3 phases. Illustrative quotes are presented in Table 4.
| Process Phases | Categories | Strategies | P (11) | C (4) | Att. (8) | Res. (6) | MS (5) | RN (3) |
|---|---|---|---|---|---|---|---|---|
| ||||||||
| Before FCR | 8. HCT preparation | Collect and prepare pertinent information | X | X | X | X | ||
| 9. Family preparation | Orient family to rounding process | X | X | X | X | X | ||
| Build relationship with family | X | X | X | |||||
| Ask family for permission and preferences | X | X | X | |||||
| During FCR | 10. Introduction and explanation of FCR | Introduce HCT and family to each other | X | X | X | X | X | |
| Explain interactive rounding process | X | X | X | |||||
| 11. Active involvement of nurse | Giving nurse opportunity to actively participate | X | X | |||||
| 12. Communication with family | Give family opportunity to actively participate | X | X | X | X | X | X | |
| Address family's questions/concerns | X | X | X | X | X | |||
| Explain tests, findings and results to family | X | X | X | X | X | |||
| Confirm family understanding | X | X | X | |||||
| 13. Giving presentation | Restructure the presentation | X | X | |||||
| Shorten the presentation | X | X | X | |||||
| Focus presentation on assessment and plan | X | X | X | X | X | |||
| Summarize plan for family | X | X | X | |||||
| Avoid discussion of sensitive topics | X | X | X | |||||
| 14. Communication style | Present in a conversational manner | X | X | X | ||||
| Use an engaging communication style | X | X | X | X | X | |||
| 15. Language used | Use qualitative language | X | X | X | ||||
| Use plain language | X | X | X | X | X | |||
| 16. Performing physical exam | Pause and confirm physical exam | X | ||||||
| 17. Managing distractions | Minimize distractions and interruptions | X | X | X | X | X | X | |
| 18. Senior physician leading/role modeling | Attending/senior resident physician should lead, direct and be a role model on FCR rounds | X | X | |||||
| 19. Teaching | Ask family permission and involve in teaching | X | X | |||||
| 20. Customizing FCR for family | Adapt rounds to family's needs | X | X | X | X | |||
| After FCR | 21. Following up with family | HCT members follow up with family | X | X | X | |||
|
| Q1: [Medical students and residents] actually had a chance to do a quick round, an abbreviated presentation to put together an outline of what we're going to talk about before we even do it. (MS2) |
| Q2: I would like to know exactly what's going onbefore I walk in. (Att.6) |
| Q3: [T]he nurse did give me the fore‐warning that rounds would be coming and it was usually like a group of 8 to 10so I was prepared for that. (P7) |
| Q4: What went well is that I had already connected with this mom and the daughter prior to this rounding encounter. (Res.3) |
| Q5: [Y]ou could ask the patient or the parents if they want the child there. (P3) |
| Q6: [Families] really want to know what your role is on the team. (Att.5) |
| Q7: I guess it would be easier to figure out who you need to direct questions to. (P3) |
| Q8: [L]etting the family anticipate what rounding is going to be like and when the opportunity is going to come up to talk. I think that can help. (Res.2) |
| Q9: I think the decision making is probably the most critical partthere is really no substitute for [families] being involved in the decisionwithout a lot of medical conversation and analysis. (P1) |
| Q10: The family was proactive enough to ask questions, but they were never really given entrance to ask questions.No one had said do you have any questions?' (Res.4) |
| Q11: It is really important for the doctors to listen to them, to know that they are the parents and they know their children best. (RN3) |
| Q12: I think sometimes when you are teaching, some of the information could potentially be scary to the family. What I would hope is letting the family feel like they are part of the education process. (Res.2) |
| Q13: Sometimes nurses are asked initially, do you have anything to add,' which I think is a good way to startbecause we have probably the most current and updated information. (RN1) |
| Q14: When I was talking about the physical exam partmaybe at that point, if I could just stop talking, we couldconfirm that exam. (Res.3) |
| Q15: It's distracting if different groups have individual discussions when you are trying to keep the group focused on this particular patient for rounds. (Att.7) |
| Q16: It's just the basic thing that I try to tell residents. I do this hopefully at least once every time I am on services with the team. (Att.1) |
| Q17: ([C]hanging rounds depending on the families) would be the ideal situationthinking about what's helpful for a family. (Att.6) |
| Q18: What I usually see when things work well after we leave is that the nurse can still stick around the family. (Res.4) |
| Q19: [T]he students have to go back in the afternoon to talk with the family about what the treatment point is and answer any questions. (MS2) |
Before FCR
To engage families during FCR, many interviewees suggested that both the HCT and families need preparation. HCT members suggested that medical students should collect up‐to‐date patient information and review it with the senior resident physicians (Q1) to reach a consensus before starting FCR (Q2). To prepare families for rounds, parents and HCT members suggested that the HCT should orient families to the rounding process (Q3), build relationships with families (Q4), and ask for their permission and preference regarding participation in rounds (Q5).
During FCR
A number of strategies focused on the beginning of rounds. Parents, children, and HCT members stressed the need to introduce HCT members by role (Q6) and inform families to whom to direct questions (Q7). It was also suggested that parents introduce themselves to the team. Some interviewees recommended that the HCT explain the rounding process to families at this time (Q8).
Interviewees recommended strategies related to communication between the HCT and families during rounds. Many interviewees suggested restructuring and shortening the presentation by focusing on the assessment and plan (Q9). According to all interviewees, the HCT should present in a conversational manner and use an engaging communication style (eg, smiling, making eye contact, using appropriate humor) and appropriate language (eg, qualitative trend instead of numbers, plain language instead of medical jargon) to communicate with families. To ensure families understanding, HCT members should encourage and address their questions and concerns (Q10). In addition, families should be given the opportunity to provide information (eg, patient history and overnight events) and to express their opinions about the plan (Q11). If teaching is done during rounds, the HCT should involve families and ask for permission (Q12).
Other strategies on rounds were suggested, such as giving nurses the opportunity to actively participate (Q13), pausing and confirming physical exam findings (Q14), minimizing distractions and interruptions (Q15), attending and/or senior resident physicians leading and being role models for FCR (Q16), and adapting rounds to families' needs (Q17).
After FCR
Some HCT members talked about the importance of following up with families after rounds. Specifically, suggestions that nurses could stay with families immediately after rounds (Q18) were made, whereas physicians could return to families later in the day (Q19).
DISCUSSION
Using recognized qualitative systems engineering methods, we identified a broad range of strategies for enhancing family engagement on FCR from the perspectives of a diverse group of stakeholders on rounds and described how these strategies target known fundamental elements in both the hospital work system and rounding process. We highlight recommendations on the content and style of communication during rounds with families, but also introduce more complex system‐wide elements that likely play a role in family engagement, such as the composition of the HCT; organization and environment of rounds; tools and technologies used; and preparation of the HCT, families, and patients beforehand.
Our research both confirms and builds upon practices previously described in the FCR literature.[17, 31, 32] In a case report by Muething et al.,[17] recommendations were developed using a series of plan‐do‐study‐act cycles to determine the components needed to conduct FCR. These components included: 1) determining family preference prior to rounds, 2) defining HCT roles, 3) introducing HCT to family and explaining the purpose of rounds, 4) describing what is shared and how it is said on rounds, 5) describing the contribution of families, nurses, and ancillary staff, and 6) providing teaching recommendations to senior physicians on rounds. All of these components are suggested by one or more of the participants in our study. In addition, our research identifies a variety of new work system‐related strategies, such as scheduling rounds, using computers appropriately on rounds, and providing training of HCT members beforehand.
Of particular interest was the discordance between strategies mentioned by families and the various members of the HCT. Although HCT members mentioned all identified strategies, families were interested in certain ones. Regarding the structure of FCR, families showed particular interest in HCT composition, timing and scheduling of rounds, location of rounds, and positioning of the HCT. In comparison, families did not mention the importance of the roles and duties of HCT members, HCT preparation for rounds, and use of computers during rounds. With respect to the FCR process, families stressed the importance of family preparation beforehand, introduction and explanation of rounds at the beginning, presentation style and communication style, customization, and management of distractions during rounds. None of the families, however, mentioned the rest of the strategies, including HCT preparation before rounds, involvement of the nurse, teaching and performing the physical exam, the role of the attending and senior resident roles during rounds, and following up with the family after rounds. These different perspectives are likely, in part, inherent to the different roles and experiences of parents and HCT members. For example, parents' knowledge of what goes on in the hospital outside of FCR, such as orientation and preparation of HCT members for rounds, is relatively limited. Future research using methods to evaluate and prioritize strategies as well as understanding reasons for contradicting strategies is warranted.
We recognize that, although family engagement is recommended as a critical component of care, strategies to improve engagement may be in direct opposition to other goals of the HCT. For example, some of our participants suggest having a smaller team may be more beneficial for family engagement on rounds. In some settings, it may be feasible to have a small team; however, in institutions that accommodate a large number of learners, excluding students from the teaching opportunity of rounds may actually compromise educational experiences. In patients with chronic and/or complex care, a larger multidisciplinary team may better facilitate information exchange among disciplines and expedite discharge planning. Moreover, one might speculate that it may not be that the size affects family engagement as much as the composition of the team, especially if tailored to the needs of the patient. For example, a large team consisting of primarily physicians and trainees may not be as engaging as the same sized team with one attending physician and a respiratory therapist, case manager, and consulting subspecialist. Finding a balance between engaging families, teaching learners, and maintaining efficiency is paramount and needs to be studied further.
This study has several limitations. Our data are from a single academic children's hospital, which may limit generalizability due to a small sampling of multiple stakeholders on different services, our specific patient population, HCT composition and roles, and teaching needs. However, we face similar barriers to engaging families during rounds as those published from both another single institution[17] and a national sampling of pediatric hospitalists.[16] Furthermore, our recommended strategies to address the FCR process are supported by prior work.[17] Because this study was voluntary, our interviewees were likely more engaged participants in general. Specifically, the viewpoints of engaged families and HCT members may not represent the viewpoints of those who are less engaged or supportive of FCR. We did not enroll nonEnglish‐speaking patients and families, which is a potential direction for future research. In our interviews, we also relied solely on the perceptions of rounding participants, rather than those of outside observers or researchers, which may only provide a partial perspective of potential strategies to improve family engagement. Last, this qualitative research approach does not provide quantitative information regarding whether certain strategies are preferred by a majority of participants, which we hope to address in future research.
This work is part of a larger study that aims to implement a bundle of these strategies after stakeholder prioritization based on impact on family engagement, feasibility, and sustainability. We plan to systematically evaluate the implementation process of these strategies and measure their impact on family engagement and, ultimately, patient safety. One or more of these strategies could be implemented in a similar manner at other hospitals depending on specific institutional needs.
In conclusion, as recently reflected by Barry et al. in The New England Journal of Medicine, Although talk about patient‐centered care is ubiquitous in modern health care, one of the greatest challenges of turning the rhetoric into reality continues to be routinely engaging patients in decision making.[33] FCR provide a crucial opportunity for family involvement in daily care decisions in the pediatric inpatient setting. This study highlights the importance of prior work defining the components of involving families in this process, while emphasizing new systems‐based strategies that further facilitate the expectation of family engagement in the care of hospitalized children.
Disclosures
This work was funded through an Agency for Healthcare Research and Quality Health Services Research Dissemination and Demonstration Grant, R18 HS018680, and also supported by the Arthur Vining Davis Foundation and the National Patient Safety Foundation through the James S. Todd Memorial Research Award. Funding organizations did not contribute to the design and conduct of study; collection, management, analysis, and interpretation of data; or preparation, review, or approval of the manuscript. The authors report no conflicts of interest.
A growing body of literature suggests that patient‐ and family‐centered care can improve patient outcomes[1, 2, 3, 4, 5] as well as patient, family, and provider satisfaction.[6, 7, 8, 9, 10] Engaging patients and families as a way to improve the quality and safety of care has been widely endorsed by leading healthcare organizations,[11, 12, 13] including the Institute of Medicine.[14] In the pediatric inpatient setting, family‐centered rounds (FCR), defined as bedside rounds in which the patient and family share in the control of the management plan as well as in the evaluation of the process itself,[15] potentially provide a consistent venue for family engagement and are recommended by the American Academy of Pediatrics as standard practice.[13]
According to a recent study by Mittal et al.,[16] FCR are the most common type of rounds practiced among pediatric hospitalists surveyed in the United States and Canada. Despite this widespread shift from rounding in a conference room to the bedside with patients and families, there exist only a few studies that provide specific recommendations on conducting FCR.[15, 17, 18] This research has been limited, primarily focusing how rounds are conducted, and further investigation is needed to identify the impact of other processes and elements within the hospital work system that may also affect family engagement during rounds.
The objectives of this study were to: 1) identify strategies to enhance family engagement during FCR drawing from the viewpoints of the various stakeholders on rounds, and 2) characterize these strategies into known elements of hospital work systems and rounding processes using a recognized human factors engineering approach, The Systems Engineering Initiative for Patient Safety (SEIPS) model.[19] According to the SEIPS model, barriers and facilitators to family engagement during FCR are likely embedded in the design of the hospital work systems and rounding process; therefore, we hypothesized that strategies that influence engagement will target all work system and process elements. This work is part of a larger study in which, after prioritization of this group of strategies based on feasibility and sustainability, a bundle of best practices for conducting FCR will be developed, implemented, and evaluated.
METHODS
Study Design
Semistructured interviews using the stimulated recall approach[20, 21] were conducted to understand the cognitive processes of families and healthcare team (HCT) members during FCR. This qualitative study design allowed us to capture comprehensive information from the perspectives of a diverse group of stakeholders on strategies for improving family engagement during FCR.
Setting and Participants
This study was conducted at a children's hospital in Wisconsin, where FCR were initiated in 2007 with the transition to a new hospital facility. The expectation is that FCR are conducted daily with the family and the patient's HCT, consisting of at least an attending physician and nurse. Typically, multiple residents, interns, and medical students are present along with a combination of other providers, including consulting subspecialists, a fellow, nurse practitioner, respiratory therapist, or pharmacist. When this study was conducted, attendees received little to no formal training regarding their role on FCR. As part of a larger study, English‐speaking patients and/or families admitted to 1 of 4 inpatient services (2 hospitalist, 1 pulmonary, and 1 hematology/oncology), and their associated HCT members were enrolled and their bedside rounds were video recorded. A purposive sampling technique[22, 23] was employed, recruiting interviewees that represented the various groups of stakeholders of rounds, including parents, children, attending physicians, resident physicians, medical students, and nurses. For child interviews, we restricted selection to children aged 8 to 17 years to ensure the ability to understand the interviewing process and provide feedback. Families were consented and children were assented. The University of Wisconsin‐Madison Health Sciences Institutional Review Board approved this study.
Interviews and analysis occurred concurrently in an iterative process, informing each other. Thus, recruitment continued until we reached theoretical saturation,[24, 25] the point at which additional interviews did not provide new information or further conceptual development.
Study Procedures
All interviews were conducted by trained researchers, who used the same semistructured interview guide. During each interview, the interviewee was instructed to watch his/her own rounding video and pause when noticing something that made it easy (facilitator) or hard (barrier) to engage the family. Every time the interviewee paused the video to describe what was noticed, the interviewer then asked follow‐up, open‐ended questions to solicit specific information that focused on strategies for enhancing family engagement during FCR. For instance, if the issue identified was a barrier, the interviewer asked, What would you have wanted to happen differently? and if the issue identified was a facilitator, the interviewer asked, How could we ensure that would happen for everyone? The interviewee rewound the video as needed. If the interviewee had not stopped the video by the halfway point, the interviewer would pause the video and review the instructions. After the interviewee had viewed and commented on the entire rounding video, an opportunity was offered to reflect on other factors that influence family engagement during rounds, and additional questions were asked as necessary to fully understand the interviewee's views. All interviews were audio recorded and personal identifiers were removed prior to data analysis.
Data Analysis
Two research assistants reviewed the audio recordings and identified all instances related to strategies for improving family engagement during FCR. There was no screening of strategies (ie, if an interviewee suggested a strategy was related to improving family engagement, it was categorized as such). To ensure intercoder reliability, these assistants, under the supervision of a researcher (L.D.), reviewed the coding process together, held consensus meetings, and crosschecked interviews for coding consensus. A researcher (A.X.) transcribed all strategy‐related instances, which were then reviewed by two additional researchers (M.K., P.C.). To organize, sort, and code the data, interview transcripts were imported in the NVivo qualitative data analysis software (QSR International, Doncaster, Victoria, Australia). The research group then performed a qualitative content analysis of the transcripts[26] and categorized the strategies in an iterative process (information provided on request).
To ensure that all strategies remained conceptually similar within categories, the constant comparative method[27, 28] was applied to the coding process. This involved comparing: 1) strategy‐related instances from the same participants, 2) strategy‐related instances from different participants in the same groups, 3) strategy‐related instances from different participants in different groups, 4) a coded strategy with other coded strategies, 5) coded strategies with categories, and 6) a category with other categories. A strategy‐related instance could be coded under more than one strategy or category. For instance, one interviewee said conducting things that can be done without family beforehand, and presenting and reviewing the plan with family. This was coded under both the strategy conducting rounds in another location without family and then at the bedside with family in the location of FCR category and the strategy focusing presentation on assessment and plan in the communication style category.
RESULTS
A total of 37 interviews were conducted with 11 parents, 4 children, and 22 HCT members (8 attending physicians, 6 resident physicians, 5 medical students, and 3 nurses) in 24 videos of rounding sessions. The duration of the interviews ranged from 30 to 60 minutes.
A total of 338 separate instances related to strategies for improving family engagement on FCR were identified and sorted into 21 categories. Using the SEIPS model, these categories were organized into 2 themes: the work system and process of FCR (Figure 1). Of the 21 categories, 12 were mentioned by both families (parents and/or children) and HCT members and 9 were solely mentioned by the HCT.
Work System of FCR
Table 1 shows the categories of strategies related to the 5 elements of the FCR work system.[29, 30] Illustrative quotes from the interviews (Q) are presented in Table 2.
| Work System Elements | Categories | Strategies | P (11) | C (4) | Att. (8) | Res. (6) | MS (5) | RN (3) |
|---|---|---|---|---|---|---|---|---|
| ||||||||
| People | 1. Size and composition of HCT | Have a smaller HCT conduct FCR | X | X | X | X | ||
| Ensure all relevant disciplines present on FCR | X | X | X | X | X | |||
| Task | 2. Roles and duties of HCT members | Define roles/duties of HCT members on FCR | X | X | ||||
| Organization | 3. Timing and scheduling of FCR | Schedule FCR, inform participants beforehand | X | X | X | |||
| 4. Training of HCT for FCR | Train HCT on how to present on FCR | X | X | |||||
| Environment | 5. Location of FCR | At bedside with family and patient | X | X | ||||
| In another location with HCT, then at bedside | X | X | X | X | ||||
| In another location with family but without child | X | |||||||
| 6. Positioning of HCT members on FCR | Sit down with family | X | X | X | X | X | ||
| Stand close to or in a semicircle around family | X | X | X | X | X | |||
| Tools and technologies | 7. Use of computers on FCR | Use computer to support family interaction | X | X | X | X | ||
| Don't use a computer | X | X | ||||||
|
| Q1: I'm intimidated to ask a question. It seems like there are too many peopleI like a smaller group. (P5) |
| Q2: Sometimes rounds are the only time that the parents are there to see the entire teamso in that way, including [the entire team] at the rounds makes more sense. (MS1) |
| Q3: There needs to be much more clear roles about who is supposed to do what, and it should be predictable. (Att.2) |
| Q4: ([T]iming of rounds) is a huge source of frustration for families. If [physicians] know in which order they will go for patients, they can call our charge nurse or unit clerk or page nurses with that information. (RN1) |
| Q5: ([W]ith a notice of the rounding schedule), I can be ahead of time, trying to think of questions. (P10) |
| Q6: [I]t would be really nice to see somebody do a presentation in a medical eye's version and then also in the family‐centered version. (MS5) |
| Q7: [H]aving the medical students practice with the senior residentis a good way of doing it. (Res.4) |
| Q8: [M]aybe some small groups where you practice this among students. (MS5) |
| Q9: It would be better to be in the room for communication. (Att.1) |
| Q10: You could have sort of hallway rounds, which is much more medical oriented, and inside‐the‐room rounds, which is much more talking with the parent. (P1) |
| Q11: [H]ave sit‐down rounds with parents and families. (Res.5) |
| Q12: I've seen some attending physicians who sat down. I think that could be helpful to be on the same level as the patient and family. (Res.2) |
| Q13: [M]aybe formation of semicircle or something like that, where we can see everybody a little more clearly, I think that would be very helpful. (P10) |
| Q14: I find the presence of a computer incredibly offensive and obstructivewhen you are supposed to be able to interact with the patient. (Att.6) |
| Q15: One of the things I started doing is having one of the other resident physicians have the computer, so just relying on them to do the orders, and me just being there mainly for being the presenter of rounds. (Res.4) |
People
Two seemingly contradictory strategies were proposed. Some interviewees suggested a smaller HCT with members most familiar to the family (Q1), whereas other interviewees stressed the need to involve different relevant disciplines (eg, social worker, nutritionist) during rounds (Q2).
Tasks
Both attending and resident physicians emphasized the importance of defining the role of each HCT member before rounding (Q3). Interviewees also suggested these roles should be explained to families, ideally at admission.
Organization
Many interviewees suggested the need to consistently schedule rounds (Q4) and to inform families and nurses of the schedule so all parties could plan ahead (Q5). Some resident physicians and medical students recommended training of learners on how to give a family‐centered presentation using methods such as role modeling (Q6) and practicing with the senior resident physician (Q7) or in small groups (Q8).
Environment
Some interviewees suggested conducting rounds in patient rooms (Q9). Others suggested conducting rounds first in another location (eg, hallway) without the family and then going to the bedside to round with the family (Q10). There were also interviewees who suggested conducting rounds in another location (eg, conference room) with the family (Q11). When conducting rounds in the patient room, some interviewees suggested that some HCT members (eg, attending and senior resident physicians) could sit down with the family (Q12), with the rest of the HCT standing close to the family in a semicircle (Q13).
Tools and Technologies
Some interviewees thought that conversation with families could be negatively affected by the use of computers, and therefore suggested not using them on FCR (Q14). Alternatively, other interviewees considered computers a tool to facilitate the interaction between the HCT and families, such as showing x‐rays or lab values. Several interviewees suggested that computers should not be positioned to block eye contact between HCT members and families; therefore, only HCT members not presenting should use computers (Q15).
Process of FCR
Table 3 shows the categories of strategies related to the process of FCR, which were categorized into 3 phases. Illustrative quotes are presented in Table 4.
| Process Phases | Categories | Strategies | P (11) | C (4) | Att. (8) | Res. (6) | MS (5) | RN (3) |
|---|---|---|---|---|---|---|---|---|
| ||||||||
| Before FCR | 8. HCT preparation | Collect and prepare pertinent information | X | X | X | X | ||
| 9. Family preparation | Orient family to rounding process | X | X | X | X | X | ||
| Build relationship with family | X | X | X | |||||
| Ask family for permission and preferences | X | X | X | |||||
| During FCR | 10. Introduction and explanation of FCR | Introduce HCT and family to each other | X | X | X | X | X | |
| Explain interactive rounding process | X | X | X | |||||
| 11. Active involvement of nurse | Giving nurse opportunity to actively participate | X | X | |||||
| 12. Communication with family | Give family opportunity to actively participate | X | X | X | X | X | X | |
| Address family's questions/concerns | X | X | X | X | X | |||
| Explain tests, findings and results to family | X | X | X | X | X | |||
| Confirm family understanding | X | X | X | |||||
| 13. Giving presentation | Restructure the presentation | X | X | |||||
| Shorten the presentation | X | X | X | |||||
| Focus presentation on assessment and plan | X | X | X | X | X | |||
| Summarize plan for family | X | X | X | |||||
| Avoid discussion of sensitive topics | X | X | X | |||||
| 14. Communication style | Present in a conversational manner | X | X | X | ||||
| Use an engaging communication style | X | X | X | X | X | |||
| 15. Language used | Use qualitative language | X | X | X | ||||
| Use plain language | X | X | X | X | X | |||
| 16. Performing physical exam | Pause and confirm physical exam | X | ||||||
| 17. Managing distractions | Minimize distractions and interruptions | X | X | X | X | X | X | |
| 18. Senior physician leading/role modeling | Attending/senior resident physician should lead, direct and be a role model on FCR rounds | X | X | |||||
| 19. Teaching | Ask family permission and involve in teaching | X | X | |||||
| 20. Customizing FCR for family | Adapt rounds to family's needs | X | X | X | X | |||
| After FCR | 21. Following up with family | HCT members follow up with family | X | X | X | |||
|
| Q1: [Medical students and residents] actually had a chance to do a quick round, an abbreviated presentation to put together an outline of what we're going to talk about before we even do it. (MS2) |
| Q2: I would like to know exactly what's going onbefore I walk in. (Att.6) |
| Q3: [T]he nurse did give me the fore‐warning that rounds would be coming and it was usually like a group of 8 to 10so I was prepared for that. (P7) |
| Q4: What went well is that I had already connected with this mom and the daughter prior to this rounding encounter. (Res.3) |
| Q5: [Y]ou could ask the patient or the parents if they want the child there. (P3) |
| Q6: [Families] really want to know what your role is on the team. (Att.5) |
| Q7: I guess it would be easier to figure out who you need to direct questions to. (P3) |
| Q8: [L]etting the family anticipate what rounding is going to be like and when the opportunity is going to come up to talk. I think that can help. (Res.2) |
| Q9: I think the decision making is probably the most critical partthere is really no substitute for [families] being involved in the decisionwithout a lot of medical conversation and analysis. (P1) |
| Q10: The family was proactive enough to ask questions, but they were never really given entrance to ask questions.No one had said do you have any questions?' (Res.4) |
| Q11: It is really important for the doctors to listen to them, to know that they are the parents and they know their children best. (RN3) |
| Q12: I think sometimes when you are teaching, some of the information could potentially be scary to the family. What I would hope is letting the family feel like they are part of the education process. (Res.2) |
| Q13: Sometimes nurses are asked initially, do you have anything to add,' which I think is a good way to startbecause we have probably the most current and updated information. (RN1) |
| Q14: When I was talking about the physical exam partmaybe at that point, if I could just stop talking, we couldconfirm that exam. (Res.3) |
| Q15: It's distracting if different groups have individual discussions when you are trying to keep the group focused on this particular patient for rounds. (Att.7) |
| Q16: It's just the basic thing that I try to tell residents. I do this hopefully at least once every time I am on services with the team. (Att.1) |
| Q17: ([C]hanging rounds depending on the families) would be the ideal situationthinking about what's helpful for a family. (Att.6) |
| Q18: What I usually see when things work well after we leave is that the nurse can still stick around the family. (Res.4) |
| Q19: [T]he students have to go back in the afternoon to talk with the family about what the treatment point is and answer any questions. (MS2) |
Before FCR
To engage families during FCR, many interviewees suggested that both the HCT and families need preparation. HCT members suggested that medical students should collect up‐to‐date patient information and review it with the senior resident physicians (Q1) to reach a consensus before starting FCR (Q2). To prepare families for rounds, parents and HCT members suggested that the HCT should orient families to the rounding process (Q3), build relationships with families (Q4), and ask for their permission and preference regarding participation in rounds (Q5).
During FCR
A number of strategies focused on the beginning of rounds. Parents, children, and HCT members stressed the need to introduce HCT members by role (Q6) and inform families to whom to direct questions (Q7). It was also suggested that parents introduce themselves to the team. Some interviewees recommended that the HCT explain the rounding process to families at this time (Q8).
Interviewees recommended strategies related to communication between the HCT and families during rounds. Many interviewees suggested restructuring and shortening the presentation by focusing on the assessment and plan (Q9). According to all interviewees, the HCT should present in a conversational manner and use an engaging communication style (eg, smiling, making eye contact, using appropriate humor) and appropriate language (eg, qualitative trend instead of numbers, plain language instead of medical jargon) to communicate with families. To ensure families understanding, HCT members should encourage and address their questions and concerns (Q10). In addition, families should be given the opportunity to provide information (eg, patient history and overnight events) and to express their opinions about the plan (Q11). If teaching is done during rounds, the HCT should involve families and ask for permission (Q12).
Other strategies on rounds were suggested, such as giving nurses the opportunity to actively participate (Q13), pausing and confirming physical exam findings (Q14), minimizing distractions and interruptions (Q15), attending and/or senior resident physicians leading and being role models for FCR (Q16), and adapting rounds to families' needs (Q17).
After FCR
Some HCT members talked about the importance of following up with families after rounds. Specifically, suggestions that nurses could stay with families immediately after rounds (Q18) were made, whereas physicians could return to families later in the day (Q19).
DISCUSSION
Using recognized qualitative systems engineering methods, we identified a broad range of strategies for enhancing family engagement on FCR from the perspectives of a diverse group of stakeholders on rounds and described how these strategies target known fundamental elements in both the hospital work system and rounding process. We highlight recommendations on the content and style of communication during rounds with families, but also introduce more complex system‐wide elements that likely play a role in family engagement, such as the composition of the HCT; organization and environment of rounds; tools and technologies used; and preparation of the HCT, families, and patients beforehand.
Our research both confirms and builds upon practices previously described in the FCR literature.[17, 31, 32] In a case report by Muething et al.,[17] recommendations were developed using a series of plan‐do‐study‐act cycles to determine the components needed to conduct FCR. These components included: 1) determining family preference prior to rounds, 2) defining HCT roles, 3) introducing HCT to family and explaining the purpose of rounds, 4) describing what is shared and how it is said on rounds, 5) describing the contribution of families, nurses, and ancillary staff, and 6) providing teaching recommendations to senior physicians on rounds. All of these components are suggested by one or more of the participants in our study. In addition, our research identifies a variety of new work system‐related strategies, such as scheduling rounds, using computers appropriately on rounds, and providing training of HCT members beforehand.
Of particular interest was the discordance between strategies mentioned by families and the various members of the HCT. Although HCT members mentioned all identified strategies, families were interested in certain ones. Regarding the structure of FCR, families showed particular interest in HCT composition, timing and scheduling of rounds, location of rounds, and positioning of the HCT. In comparison, families did not mention the importance of the roles and duties of HCT members, HCT preparation for rounds, and use of computers during rounds. With respect to the FCR process, families stressed the importance of family preparation beforehand, introduction and explanation of rounds at the beginning, presentation style and communication style, customization, and management of distractions during rounds. None of the families, however, mentioned the rest of the strategies, including HCT preparation before rounds, involvement of the nurse, teaching and performing the physical exam, the role of the attending and senior resident roles during rounds, and following up with the family after rounds. These different perspectives are likely, in part, inherent to the different roles and experiences of parents and HCT members. For example, parents' knowledge of what goes on in the hospital outside of FCR, such as orientation and preparation of HCT members for rounds, is relatively limited. Future research using methods to evaluate and prioritize strategies as well as understanding reasons for contradicting strategies is warranted.
We recognize that, although family engagement is recommended as a critical component of care, strategies to improve engagement may be in direct opposition to other goals of the HCT. For example, some of our participants suggest having a smaller team may be more beneficial for family engagement on rounds. In some settings, it may be feasible to have a small team; however, in institutions that accommodate a large number of learners, excluding students from the teaching opportunity of rounds may actually compromise educational experiences. In patients with chronic and/or complex care, a larger multidisciplinary team may better facilitate information exchange among disciplines and expedite discharge planning. Moreover, one might speculate that it may not be that the size affects family engagement as much as the composition of the team, especially if tailored to the needs of the patient. For example, a large team consisting of primarily physicians and trainees may not be as engaging as the same sized team with one attending physician and a respiratory therapist, case manager, and consulting subspecialist. Finding a balance between engaging families, teaching learners, and maintaining efficiency is paramount and needs to be studied further.
This study has several limitations. Our data are from a single academic children's hospital, which may limit generalizability due to a small sampling of multiple stakeholders on different services, our specific patient population, HCT composition and roles, and teaching needs. However, we face similar barriers to engaging families during rounds as those published from both another single institution[17] and a national sampling of pediatric hospitalists.[16] Furthermore, our recommended strategies to address the FCR process are supported by prior work.[17] Because this study was voluntary, our interviewees were likely more engaged participants in general. Specifically, the viewpoints of engaged families and HCT members may not represent the viewpoints of those who are less engaged or supportive of FCR. We did not enroll nonEnglish‐speaking patients and families, which is a potential direction for future research. In our interviews, we also relied solely on the perceptions of rounding participants, rather than those of outside observers or researchers, which may only provide a partial perspective of potential strategies to improve family engagement. Last, this qualitative research approach does not provide quantitative information regarding whether certain strategies are preferred by a majority of participants, which we hope to address in future research.
This work is part of a larger study that aims to implement a bundle of these strategies after stakeholder prioritization based on impact on family engagement, feasibility, and sustainability. We plan to systematically evaluate the implementation process of these strategies and measure their impact on family engagement and, ultimately, patient safety. One or more of these strategies could be implemented in a similar manner at other hospitals depending on specific institutional needs.
In conclusion, as recently reflected by Barry et al. in The New England Journal of Medicine, Although talk about patient‐centered care is ubiquitous in modern health care, one of the greatest challenges of turning the rhetoric into reality continues to be routinely engaging patients in decision making.[33] FCR provide a crucial opportunity for family involvement in daily care decisions in the pediatric inpatient setting. This study highlights the importance of prior work defining the components of involving families in this process, while emphasizing new systems‐based strategies that further facilitate the expectation of family engagement in the care of hospitalized children.
Disclosures
This work was funded through an Agency for Healthcare Research and Quality Health Services Research Dissemination and Demonstration Grant, R18 HS018680, and also supported by the Arthur Vining Davis Foundation and the National Patient Safety Foundation through the James S. Todd Memorial Research Award. Funding organizations did not contribute to the design and conduct of study; collection, management, analysis, and interpretation of data; or preparation, review, or approval of the manuscript. The authors report no conflicts of interest.
- , , , et al. The impact of patient‐centered care on outcomes. J Fam Pract. 2000;49:796–804.
- , , , et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ. 2001;323:908–911.
- , , . Improvement in the family‐centered medical home enhances outcomes for children and youth with special healthcare needs. J Ambul Care Manage. 2009;32:188–196.
- , , . Associations of family‐centered care with health care outcomes for children with special health care needs. Matern Child Health J. 2011;15:794–805.
- , , , , Can a patient‐centered medical home lead to better patient outcomes? The quality implications of Geisinger's ProvenHealth Navigator. Am J Med Qual. 2012;27:210–216.
- , , . Perceptions of health care providers' communication: relationships between patient‐centered communication and satisfaction. Health Commun. 2004;16:363–383.
- , . Satisfaction with care and ease of using health care services among parents of children with special health care needs: the roles of race/ethnicity, insurance, language, and adequacy of family‐centered care. Pediatrics. 2006;117:1184–1196.
- , , , . A randomized, controlled trial of bedside versus conference‐room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120:275–280.
- , , , , . Effect of patient‐centered care on patient satisfaction and quality of care. J Nurs Care Qual. 2008;23:316–321.
- , , . Implementing family‐centered rounds: pediatric residents' perceptions. Clin Pediatr (Phila) 2010;49:228–234.
- ACGME Program Requirements for Graduate Medical Education in Pediatrics. 2007. Available at: http://www.acgme.org/acWebsite/downloads/RRC_progReq320_pediatrics_07012007.pdf. Accessed February 10, 2012.
- Speak up: prevent errors in your child's care. 2011. The Joint Commission Web site. Available at: http://www.jointcommission.org/Speak_Up_Prevent_Errors_in_Your_Childs_Care/. Accessed May 11, 2012.
- Patient‐ and family‐centered care and the pediatrician's role. Pediatrics. 2012;129:394–404.
- Committee on Quality of Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press; 2001.
- , , , . Defining family‐centered rounds. Teach Learn Med. 2007;19:319–322.
- , , , et al. Family‐centered rounds on pediatric wards: A PRIS network survey of US and Canadian hospitalists. Pediatrics. 2010;126:37–43.
- , , , , . Family‐centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119:829–832.
- , , , . Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: a qualitative study. Acad Med. 2008;83:292–297.
- , , , et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care. 2006;15:i50–i58.
- , . IPR—a validated model for the 1990s and beyond. Couns Psychol. 1990;18:436–440.
- , . Auto‐ and allo‐confrontation as tools for reflective activities. Appl Ergon. 2004;35:531–540.
- . Qualitative Research and Evaluation Methods. 3rd ed. Thousand Oaks, CA: Sage Publications; 2002.
- , . Doing Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publications; 1999.
- . Sample size in qualitative research. Res Nurs Health. 1995;18:179–183.
- , . Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Newbury Park, CA: Sage Publications; 1998.
- , . Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–112.
- . A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Qual Quant. 2002;36:391–409.
- . Theoretical Sensitivity: Advances in the Methodology of Grounded Theory. Mill Valley, CA: Sociology Press; 1978.
- , . Balance theory of job design. In: Karwowski W, ed. International Encyclopedia of Ergonomics and Human Factors. London: Taylor 2000:1181–1184.
- , . A balance theory of job design for stress reduction. Int J Ind Ergon. 1989;4:67–79.
- Institute for Patient‐ and Family‐Centered Care. Applying patient‐ and family‐centered concepts to bedside rounds. 2010. Available at: http://www.ipfcc.org/advance/topics/PH_RD_Applying_PFCC_Rounds_012009.pdf. Accessed May 11, 2012.
- . A fundamental shift: family‐centered rounds in an academic medical center. Hospitalist. 2006;10:45–46.
- , Shared decision making—pinnacle of patient‐centered care. N Engl J Med. 2012;366:780–781.
- , , , et al. The impact of patient‐centered care on outcomes. J Fam Pract. 2000;49:796–804.
- , , , et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ. 2001;323:908–911.
- , , . Improvement in the family‐centered medical home enhances outcomes for children and youth with special healthcare needs. J Ambul Care Manage. 2009;32:188–196.
- , , . Associations of family‐centered care with health care outcomes for children with special health care needs. Matern Child Health J. 2011;15:794–805.
- , , , , Can a patient‐centered medical home lead to better patient outcomes? The quality implications of Geisinger's ProvenHealth Navigator. Am J Med Qual. 2012;27:210–216.
- , , . Perceptions of health care providers' communication: relationships between patient‐centered communication and satisfaction. Health Commun. 2004;16:363–383.
- , . Satisfaction with care and ease of using health care services among parents of children with special health care needs: the roles of race/ethnicity, insurance, language, and adequacy of family‐centered care. Pediatrics. 2006;117:1184–1196.
- , , , . A randomized, controlled trial of bedside versus conference‐room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120:275–280.
- , , , , . Effect of patient‐centered care on patient satisfaction and quality of care. J Nurs Care Qual. 2008;23:316–321.
- , , . Implementing family‐centered rounds: pediatric residents' perceptions. Clin Pediatr (Phila) 2010;49:228–234.
- ACGME Program Requirements for Graduate Medical Education in Pediatrics. 2007. Available at: http://www.acgme.org/acWebsite/downloads/RRC_progReq320_pediatrics_07012007.pdf. Accessed February 10, 2012.
- Speak up: prevent errors in your child's care. 2011. The Joint Commission Web site. Available at: http://www.jointcommission.org/Speak_Up_Prevent_Errors_in_Your_Childs_Care/. Accessed May 11, 2012.
- Patient‐ and family‐centered care and the pediatrician's role. Pediatrics. 2012;129:394–404.
- Committee on Quality of Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press; 2001.
- , , , . Defining family‐centered rounds. Teach Learn Med. 2007;19:319–322.
- , , , et al. Family‐centered rounds on pediatric wards: A PRIS network survey of US and Canadian hospitalists. Pediatrics. 2010;126:37–43.
- , , , , . Family‐centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119:829–832.
- , , , . Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: a qualitative study. Acad Med. 2008;83:292–297.
- , , , et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care. 2006;15:i50–i58.
- , . IPR—a validated model for the 1990s and beyond. Couns Psychol. 1990;18:436–440.
- , . Auto‐ and allo‐confrontation as tools for reflective activities. Appl Ergon. 2004;35:531–540.
- . Qualitative Research and Evaluation Methods. 3rd ed. Thousand Oaks, CA: Sage Publications; 2002.
- , . Doing Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publications; 1999.
- . Sample size in qualitative research. Res Nurs Health. 1995;18:179–183.
- , . Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Newbury Park, CA: Sage Publications; 1998.
- , . Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–112.
- . A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Qual Quant. 2002;36:391–409.
- . Theoretical Sensitivity: Advances in the Methodology of Grounded Theory. Mill Valley, CA: Sociology Press; 1978.
- , . Balance theory of job design. In: Karwowski W, ed. International Encyclopedia of Ergonomics and Human Factors. London: Taylor 2000:1181–1184.
- , . A balance theory of job design for stress reduction. Int J Ind Ergon. 1989;4:67–79.
- Institute for Patient‐ and Family‐Centered Care. Applying patient‐ and family‐centered concepts to bedside rounds. 2010. Available at: http://www.ipfcc.org/advance/topics/PH_RD_Applying_PFCC_Rounds_012009.pdf. Accessed May 11, 2012.
- . A fundamental shift: family‐centered rounds in an academic medical center. Hospitalist. 2006;10:45–46.
- , Shared decision making—pinnacle of patient‐centered care. N Engl J Med. 2012;366:780–781.
Copyright © 2013 Society of Hospital Medicine