User login
In recent years, the demand for hospitalists has outstripped the supply, creating a national shortage.1, 2 A recent Society of Hospital Medicine (SHM) survey found that in the last 2 years there has been a 31% mean growth increase in the number of hospitalist groups.3 As hospitalists are becoming more difficult to recruit, many practices are utilizing physician assistants (PAs) and nurse practitioners (NPs), collectively referred to as nonphysician providers (NPPs) to help offset the workload.4 The SHM survey also noted that the number of hospitalist groups utilizing NPPs increased from 29% to 38%.3 The exact number of NPPs working for hospitalist groups is unknown.
Hospitalist NPPs are in demand for reasons other than just physician shortages. NPPs have been utilized to fill the gap in many institutions where the workforce was impacted by the 2002 Accreditation Council for Graduate Medical Education (ACGME) ruling to restrict resident work hours. Several studies have documented NPPs' ability to assist with the compliance of ACCGME resident work‐hour restrictions while maintaining patient continuity of care, improving length of stays, and reducing health care costs on various hospital services.59 Dresselhaus et al.10 found that 56% of medical resident's time on service was delegated to tasks not related to direct patient care. They proposed that these tasks can be delegated to the NPPs, leaving more time for the residents to focus on direct patient care. In a recent study performed at a Pennsylvania hospital, patients presenting to the emergency department with low‐risk chest pain (based upon thrombolysis in myocardial infarction [TIMI] risk score) were admitted to a nonteaching service staffed with NPPs and attending physicians. Simultaneously, a similar group of low‐risk chest pain patients were admitted to a traditional internal medicine resident service. The results demonstrated lower median length of stay and hospital charges on the nonteaching service. This study suggested that NPPs can offset the workload volume for medical residents, allowing them to focus on patients with higher acuity and greater learning value.11
Barriers to Finding Experienced NPPs in Hospital Medicine
Although many hospitalist groups are interested in hiring NPPs, there can be significant obstacles to recruitment. For example, most experienced PAs and NPs have clinical backgrounds in either surgical or medical subspecialties and therefore typically need extensive on‐the‐job training in hospital medicine, which can often take at least 6 to 12 months to acquire the basic skill set.12 Hiring new graduates may require even longer training periods.
The inexperience of new graduates has become an even more pertinent issue due to recent changes in PA education. Traditionally, PA programs attracted older students with prior healthcare experience, who wished to return to school for additional training. However, in 2005 a major shift occurred in PA education: programs began transitioning from graduating trainees with a bachelor's degree to now requiring a master's level degree for completion of the PA program.13 The acquisition of more advanced degrees has changed the demographics of the students matriculating into PA programs, attracting younger students, straight from undergraduate institutions, with less prior healthcare experience.14 As a result, not only are new PA graduates less experienced overall, but they are particularly lacking in exposure to hospital medicine. After PA students complete their first 12 months of PA school in the basic sciences and didactic coursework, they embark on 12 to 15 months of clinical rotations, which are largely rooted in primary care. In fact, many PA programs find it difficult to offer hospital‐based rotations while fulfilling the required rotations in primary care. These factors have resulted in the need for more extensive on‐the‐job training particularly for those new graduates interested in hospital medicine. In light of these challenges, our institution created a 12‐month postgraduate PA fellowship program in Hospital Medicine.
Postgraduate PA Training Programs
Postgraduate PA fellowships, interchangeably called residencies, are voluntary 1‐year training programs that provide both didactic instruction and clinical experience in a medical or surgical subspecialty, thereby lessening the need for on‐the‐job training. These programs are recognized by the Association of Postgraduate Physician Assistant Programs.15 Currently, there are 44 postgraduate training programs in the United States, in a wide range of medical and surgical specialties. At the end of these 1‐year postgraduate PA programs, most graduates receive a certificate of completion. Until now, the only postgraduate education option for PAs interested in Hospital Medicine was a master's completion program only available to PAs who were already employed by a hospitalist group.15 This work reviews the first reported postgraduate hospitalist training program for PAs. Specifically, the program's background, curriculum, anticipated program outcomes, and future plans are discussed.
Background for A Hospitalist Postgraduate PA Fellowship
Mayo Clinic Arizona is a multispecialty private group comprised of both outpatient services and a tertiary care hospital medical center, located in the metropolitan Phoenix, AZ, area. The Mayo Clinic Hospital is a 7‐story facility with 244 licensed beds, 18 operating rooms, and a Level II emergency department. The Mayo Hospitalist group is composed of 15 full time hospitalists and 6 part‐time hospitalists, all of whom are salaried Mayo employees. The group provides 24‐hour in‐house staffing, covering both resident services (teams composed of interns and residents supervised by a staff hospitalist) and nonresident services (staff hospitalists). Over the years there has been steady growth in the number of nonresident services, in part due to resident work‐hour restrictions. To support the physicians working on these nonresident services, the first PA was hired in 2001. Since then, the number of NPPs in our Hospitalist group has increased to 9.35 full‐time equivalents (FTEs), including 1 nurse practitioner. However, one of the greatest challenges in expanding the NPP service was the difficulty finding candidates with experience in hospital internal medicine. This need inspired the creation of a PA fellowship in Hospital Medicine. At the time, there were 2 other postgraduate PA training programs at the Mayo Clinic Arizona in Hepatology and Otolaryngology/Ear, Nose, and Throat (ENT) Surgery.
Program Description
The Mayo Clinic Arizona PA fellowship in Hospital Medicine began in October 2007 and currently accepts 1 fellow per year. Applicants must be graduates of an Accreditation Review Commission in Education for the Physician Assistant (ARC‐PA)‐accredited PA program and be certified through the National Commission on Certification of Physician Assistants (NCCPA). Furthermore, they must be licensed to work as a PA in the state of Arizona. The program is 12 months in duration, and is comprised of both didactic and clinical components. Upon graduation, the fellow earns a certificate of completion from the Mayo Clinic College of Medicine. The program has received recognition with the Association of Postgraduate Physician Assistant Programs (APPAP).
Two physician assistants act as co‐program directors of the PA fellowship in hospital medicine. They are given 0.10 full‐time equivalent (FTE) for management of the program, which includes day‐to‐day operations, curriculum development, and candidate selection. The program also has 2 volunteer physician medical directors, both of whom have previous medical residency experience. The physicians and NPPs in our hospitalist group volunteer their time to serve as faculty for the program, assisting with much of the didactic and clinical education. The program receives a budget of $99,500 per year, which is funded by the organization's foundation through the department of education. This includes the fellow stipend of $44,000 per 12 months and institutional malpractice insurance coverage. The fellow also receives health and dental insurance, 2 weeks of paid vacation, and $500 stipend toward attendance of a continuing medical education (CME) conference.
CURRICULUM
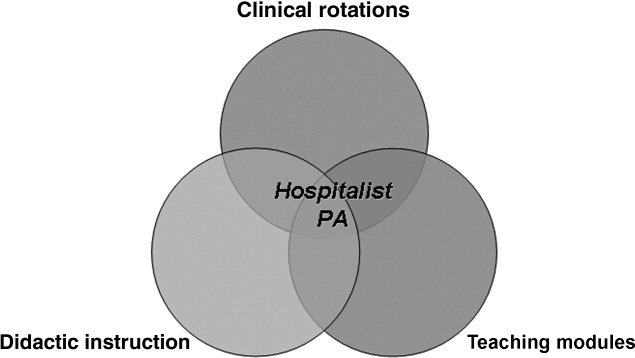
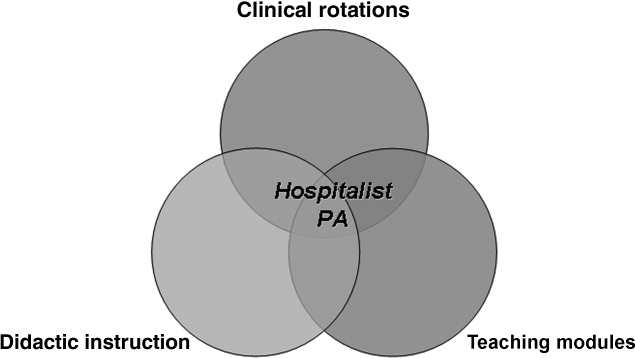
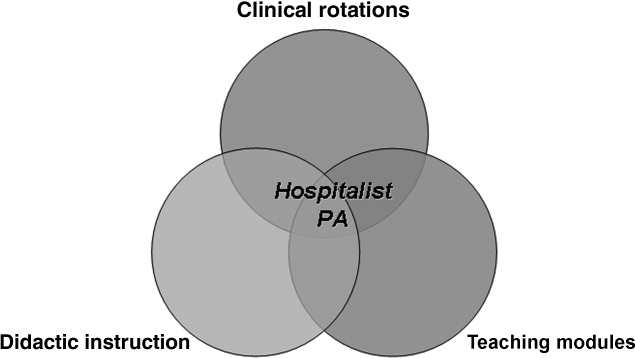
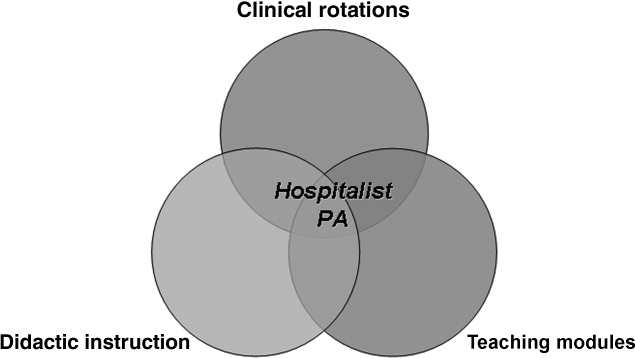
The PA fellowship curriculum is designed in a diverse unique format that strives to accommodate all types of learners. It includes clinical rotations in various medicine/surgical subspecialties, didactic instruction, and teaching modules (Figure 1). The curriculum is based upon the SHM Core Competencies.15
Clinical Rotations
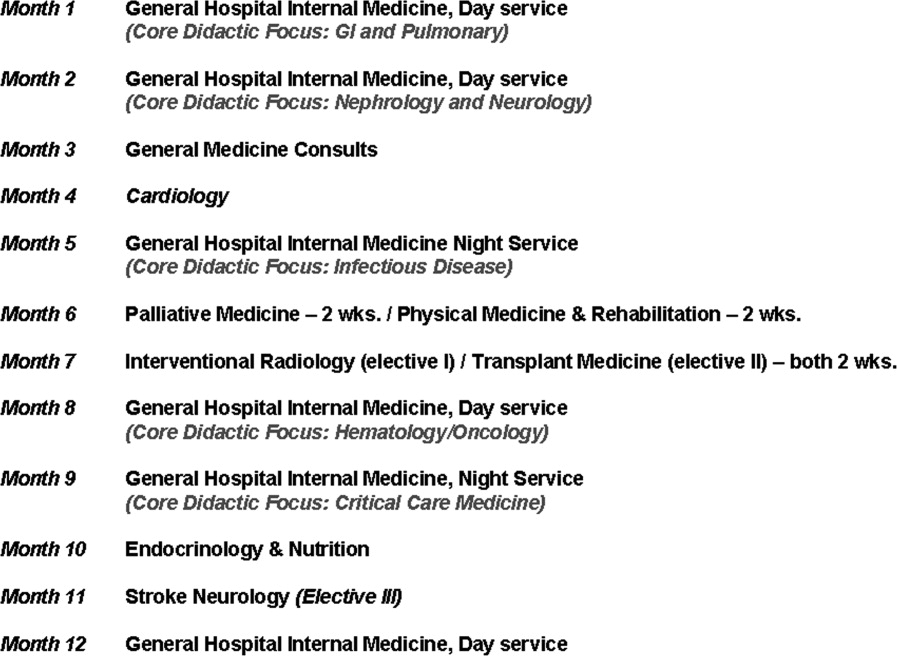
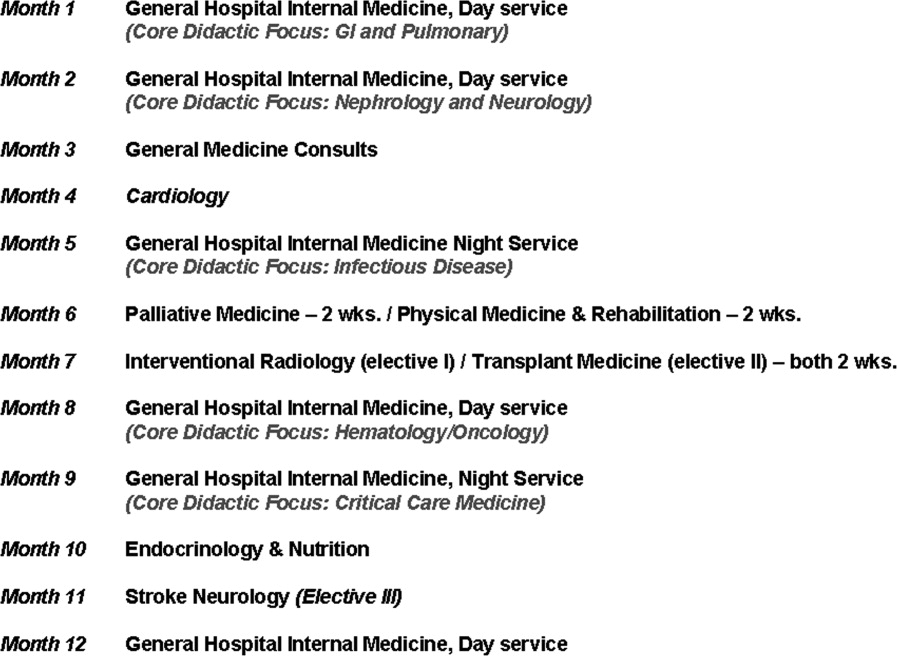
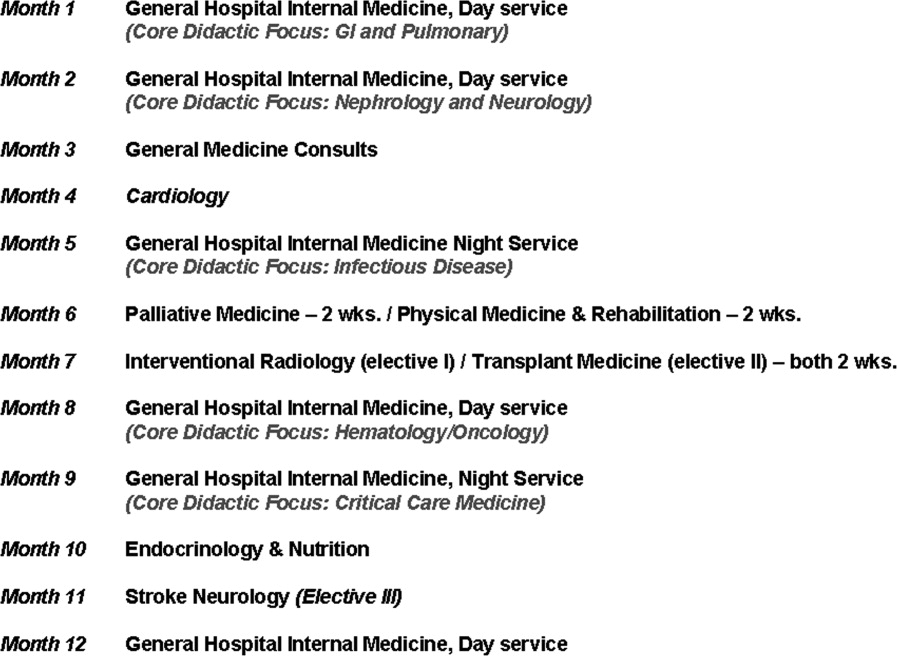
The PA fellow completes 12 to 14 general hospital medicine and medical specialty rotations, each 2 to 4 weeks in duration. The rotation calendar for the current fellow is given in Figure 2. These rotations are all inpatient‐based and are supervised by either the hospitalist or the respective inpatient subspecialists. The PA fellow's specific clinical responsibilities vary from rotation to rotation, and are designed to maximize the fellow's exposure to that particular specialty. Each rotation has specific written objectives created by the program directors and reviewed by the rotation's preceptor(s) (Figure 2). During the clinical rotations, complementary didactic lectures, coursework, and readings are provided to ensure the PA fellow receives a strong foundation. Didactic instruction is designed by the program directors, physician preceptors and staff NPPs, and is coordinated with the clinical rotation specialty. At the end of each rotation the fellow is evaluated by the preceptor and given direct feedback on their performance.
Didactic Instruction
The didactic instruction is organized in a system‐based manner and occurs on a weekly basis during the Hospital Internal Medicine service and Medicine Consults rotations. Hospitalist NPPs and physician faculty are responsible for most of the teaching. This formal didactic instruction is supplemented by journal club presentations given by the PA fellow to faculty in the division of hospital internal medicine. The fellow is also required to attend daily medical resident lunchtime educational lectures, weekly medical grand rounds, and any lectures provided by the medicine subspecialties while the PA is on that particular rotation.
Teaching Modules
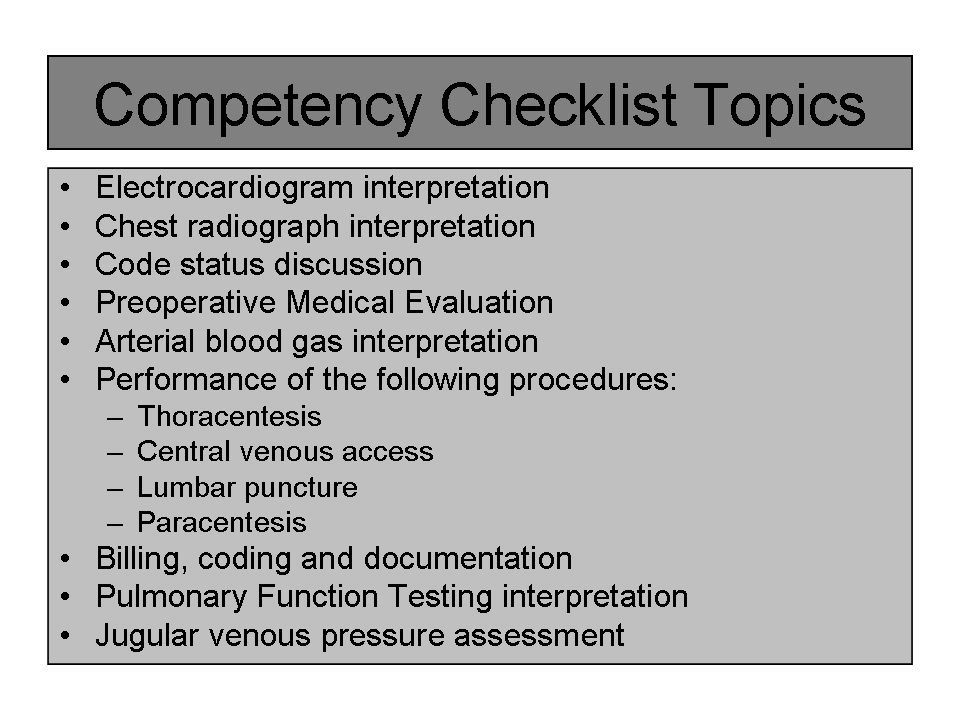
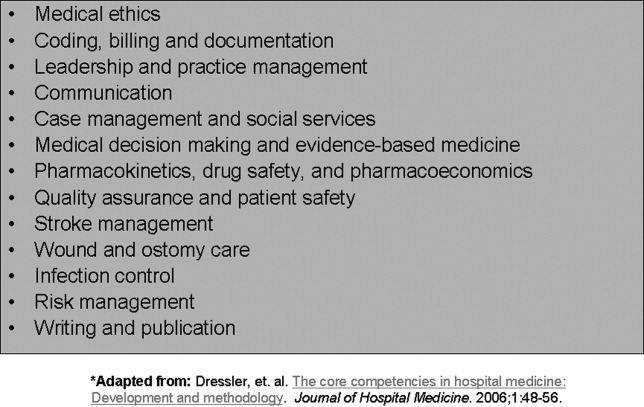
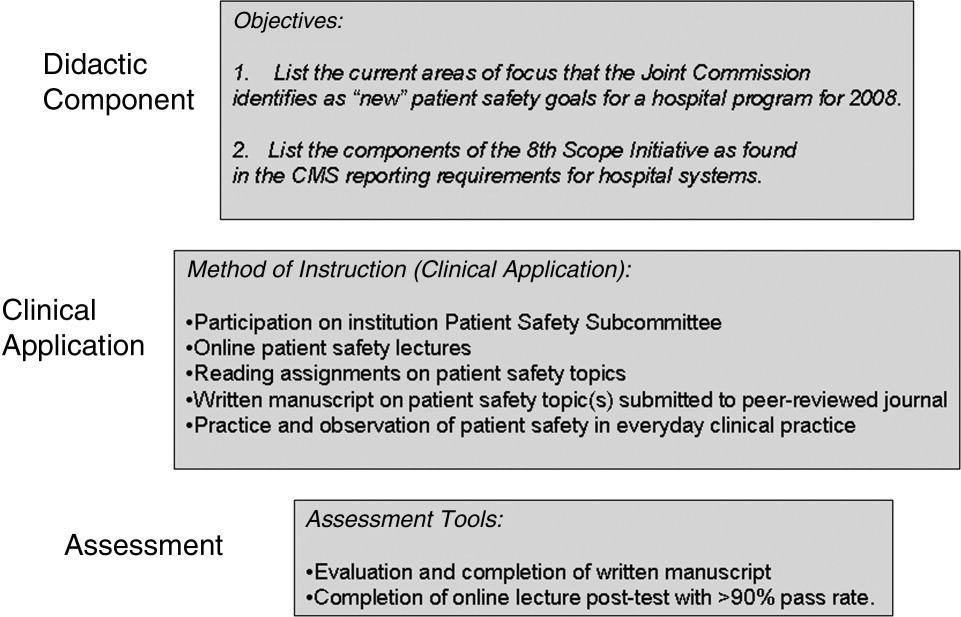
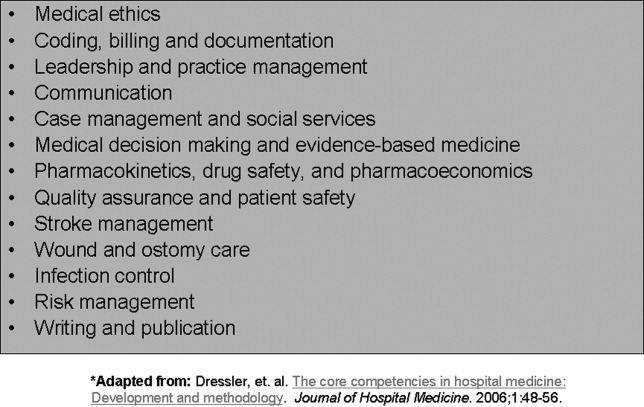
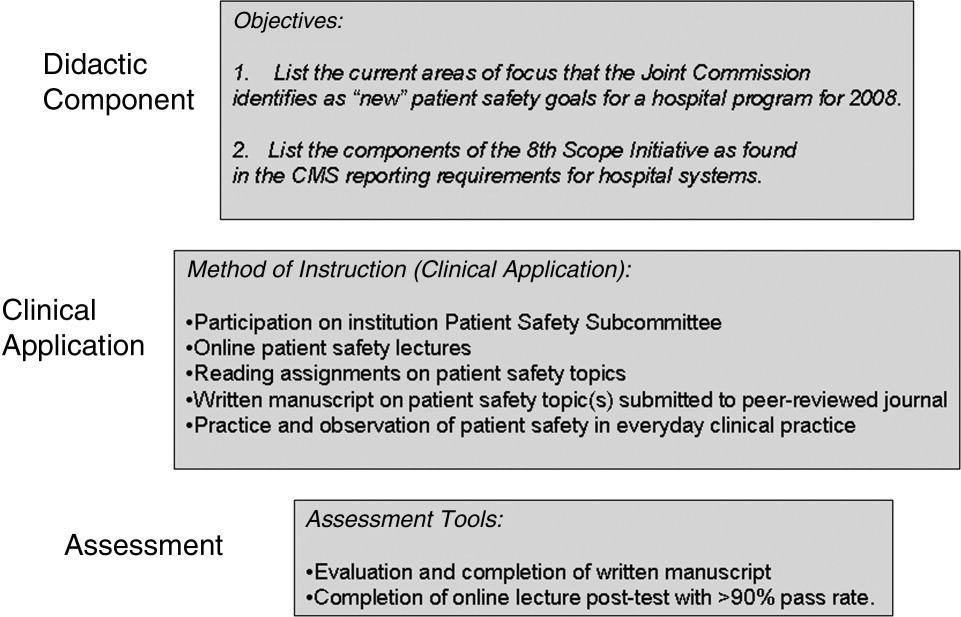
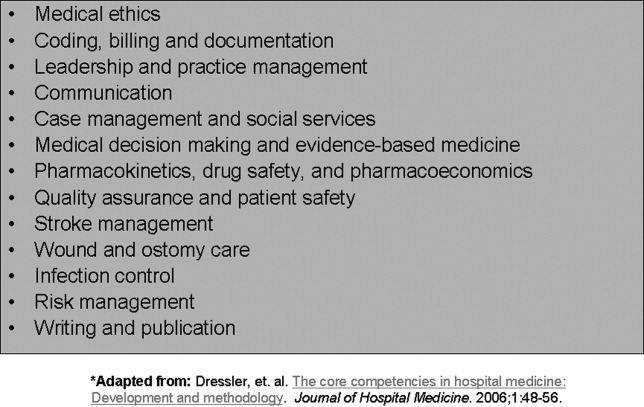
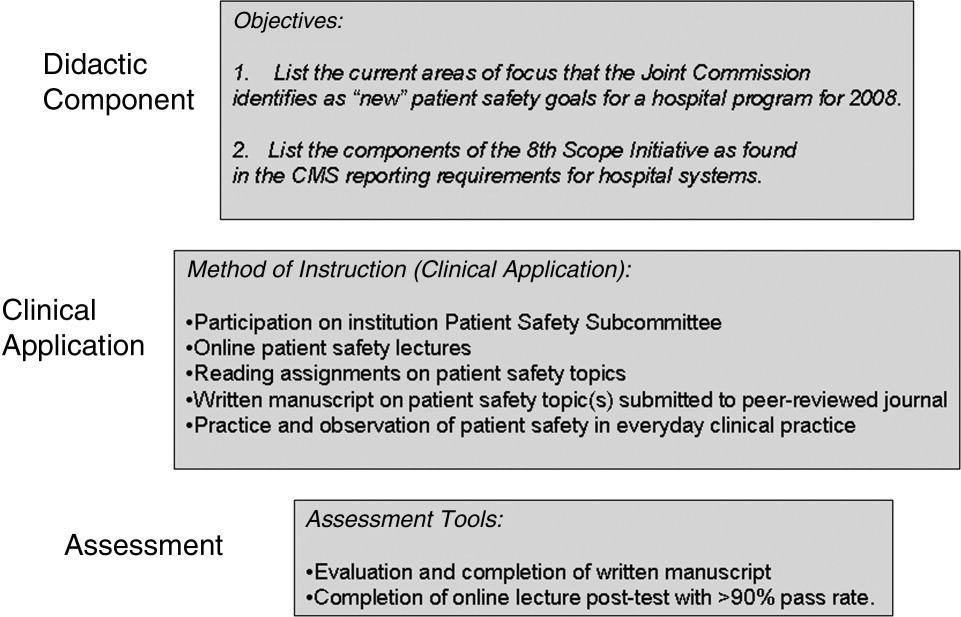
One component of the Hospital Medicine PA fellowship curriculum that may be unique is the concept of teaching modules. While receiving regular didactic instruction and completing their clinical rotations, the PA is also expected to complete self‐directed teaching module assignments. These modules serve to educate the PA fellow on the hospital as a systemthe true essence of hospital medicine. The modules cover a variety of topics not directly addressed during their rotations. These topics are outlined in Figure 3. Each teaching module consists of a didactic component, clinical application, and assessment (Figure 4) and has its own specific objectives and goals. Teaching modules are often taught by the local expert in the hospital in that particular area. For example, for the infectious control teaching module, the PA fellow will rotate with the infection control nursing staff learning about the isolation and infection control policies of the institution.
Assessment Tools
There are several tools utilized to assess both the PA fellow and the fellowship program itself (Figure 5). The assessment tools used include both ongoing and summative assessments. To fulfill the ongoing assessment, each rotation and teaching module contains assessment tools provided by the preceptor, which are reviewed by the program directors. Additionally, during the clinical rotations, skills are assessed using competency checklists that require the preceptor to directly observe the PA fellow perform a specific task or skill‐set and sign off on its successful completion (Supplementary Figures 6, 7).
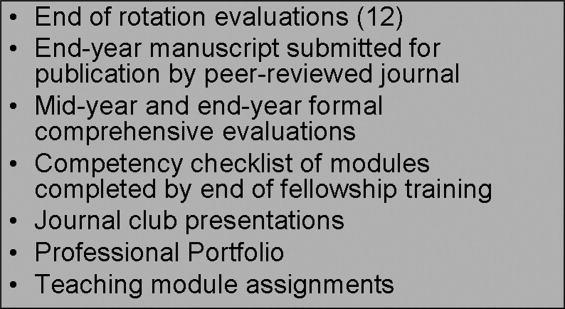
There are 2 forms of summative assessment for the PA fellow. First, to assess the PA fellow's knowledge, comprehensive mid‐year and end‐year examinations are utilized. These multiple‐choice examinations are comprised of questions which align with the didactic lectures/objectives provided by the Hospital Medicine faculty throughout the year. The second form of summative evaluation of the fellow is project‐based and divided into 2 parts. First, the fellow is expected to write a publication‐quality manuscript on a hospital medicine topic by the end of the year. Second, the PA fellow is expected to create a professional portfolio, which is comprised of a collection of all of the rotation/module assessments, the formal program assessments, and documentation of all of the skills obtained by the fellow throughout year (competency checklists). This portfolio can be used by the graduate to demonstrate to future employers what skills they possess and provide documentation of knowledge gained during the fellowship.
The program itself is evaluated by several measures. First, the fellow provides formal feedback during the mid‐year and end‐of‐the‐year assessments, which are used to enhance the experience of future fellows. Second, there is ongoing review by both the division of Hospital Medicine and the institution's Allied Health Education Committee, which ensures that the program maintains the appropriate standards and goals.
Future Goals for the PA Fellowship
The program graduated its first fellow at the end of October 2008 and has enjoyed early success. Integrating the PA fellow onto the hospitalist services augmented the present mid‐level and physician teams. There has been excellent institutional support for the program with extremely positive feedback from the rotation preceptors. There are several futures plans for the program. Our first goal is to seek accreditation from the Accreditation Review Commission for Physician Assistants (ARC‐PA), the organization that accredits entry level PA programs and which began formal, voluntary accreditation of postgraduate programs in early 2008. We plan to begin this process within the next academic year.
Our second long‐term goal for the program is to include NPs in the training program. Because of the desire to seek accreditation, the program directors felt temporarily limiting the fellowship to PAs would aide in the rigorous accreditation process, which can take approximately 1 year to complete. There is an NP on our faculty and the program has received interest from NPs. Once we obtain accreditation, expand the program enrollment, and develop an NP curriculum, we plan to open the fellowship to either PA or NP applicants.
Our third goal is to substantiate our PA Fellowship validity with outcome measures and ultimately publishable data. Thus far, the success of the PA fellowship is qualitative, and with small numbers of graduates it is difficult to quantify. After graduation of many subsequent PA fellows, our goal is to obtain quantifiable data that can be used to improve the quality of the PA fellowship and demonstrate the value of postgraduate training for physician assistants.
Perhaps the most important goal of the program is to eventually accept additional PA/NP fellows per year. While 1 program does not meet the demands of a national shortage of hospitalist providers, it may serve as a model that other institutions can adapt to their own needs. Since the program is based upon the SHM Core Competencies, the curriculum can be applied to a variety of hospitalist programs, and its relatively low operating cost makes it feasible for both academic‐based and community‐based institutions. Importantly, since recruitment and retention of employees is such a challenge for most hospitalist groups, this PA fellowship program may serve as a vehicle for recruitment and long‐term retention of well‐trained employees. This precedent has been set, as our division has hired our first PA fellow, whose transition from PA fellow to PA staff was seamless.
In conclusion, our PA fellowship in Hospital Medicine represents the first reported postgraduate PA program of this kind in the United States offering a certificate of completion. As the need for hospitalists increase so will the need for NPPs, particularly those with additional training in hospital medicine. This program serves as an example of 1 type of training tool for physician assistants looking to work in hospital medicine.
- ,,,.Health care market trends and the evolution of hospitalist use and roles.J Gen Intern Med.2004;20:101–107.
- .Innovations in the management of hospitalized patients. Nurse Pract Spring2006 (suppl):2–3.
- .Hospitalist pay up, productivity steady in SHM's latest survey.Hospitalist.2008;12(5):7,16.
- .Physician assistants: filling the gap in patient care in academic hospitals.Perspect Physician Assist Educ.2003;14(3):158–167.
- ,,, et al.The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs.J Nurs Adm.2006;36(2):79–85.
- ,,, et al.Physician extenders impact trauma systems.J Trauma.2005;58(5):917–920.
- ,,.The role of physician assistants in critical care units.Chest.1991;99:89–91.
- .Alliances: invaluable assistants.Hospitalist.2006;April:32–33.
- ,,.Resource use by physician assistant services versus teaching services.JAAPA.2002;15:33–42.
- ,,,,,.Analyzing the time and value of house staff inpatient work.J Intern Med.1998;13:534–540.
- ,,, et al.Improving resource utilization in a teaching hospital: Development of a nonteaching service for chest pain admissions.Acad Med.2006;81(5):432–435.
- .Midlevels make a rocky entrance into hospital medicine.Todays Hospitalist.2007;5(1):28–32.
- Accreditation Review Commission for Physician Assistant Education.3rd ed. 2005. Available at: http://www.arc‐pa.org/Standards/standards.html. Accessed September2009.
- 22nd Annual Report on Physician Assistant Education in the U.S., 2005–2006. Available at: http://www.paeaonline.org. Accessed September2009.
- Association of Postgraduate Physician Assistant Programs. Available at: http://www.appap.org. Accessed September2009.
- ,,,,.The core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
In recent years, the demand for hospitalists has outstripped the supply, creating a national shortage.1, 2 A recent Society of Hospital Medicine (SHM) survey found that in the last 2 years there has been a 31% mean growth increase in the number of hospitalist groups.3 As hospitalists are becoming more difficult to recruit, many practices are utilizing physician assistants (PAs) and nurse practitioners (NPs), collectively referred to as nonphysician providers (NPPs) to help offset the workload.4 The SHM survey also noted that the number of hospitalist groups utilizing NPPs increased from 29% to 38%.3 The exact number of NPPs working for hospitalist groups is unknown.
Hospitalist NPPs are in demand for reasons other than just physician shortages. NPPs have been utilized to fill the gap in many institutions where the workforce was impacted by the 2002 Accreditation Council for Graduate Medical Education (ACGME) ruling to restrict resident work hours. Several studies have documented NPPs' ability to assist with the compliance of ACCGME resident work‐hour restrictions while maintaining patient continuity of care, improving length of stays, and reducing health care costs on various hospital services.59 Dresselhaus et al.10 found that 56% of medical resident's time on service was delegated to tasks not related to direct patient care. They proposed that these tasks can be delegated to the NPPs, leaving more time for the residents to focus on direct patient care. In a recent study performed at a Pennsylvania hospital, patients presenting to the emergency department with low‐risk chest pain (based upon thrombolysis in myocardial infarction [TIMI] risk score) were admitted to a nonteaching service staffed with NPPs and attending physicians. Simultaneously, a similar group of low‐risk chest pain patients were admitted to a traditional internal medicine resident service. The results demonstrated lower median length of stay and hospital charges on the nonteaching service. This study suggested that NPPs can offset the workload volume for medical residents, allowing them to focus on patients with higher acuity and greater learning value.11
Barriers to Finding Experienced NPPs in Hospital Medicine
Although many hospitalist groups are interested in hiring NPPs, there can be significant obstacles to recruitment. For example, most experienced PAs and NPs have clinical backgrounds in either surgical or medical subspecialties and therefore typically need extensive on‐the‐job training in hospital medicine, which can often take at least 6 to 12 months to acquire the basic skill set.12 Hiring new graduates may require even longer training periods.
The inexperience of new graduates has become an even more pertinent issue due to recent changes in PA education. Traditionally, PA programs attracted older students with prior healthcare experience, who wished to return to school for additional training. However, in 2005 a major shift occurred in PA education: programs began transitioning from graduating trainees with a bachelor's degree to now requiring a master's level degree for completion of the PA program.13 The acquisition of more advanced degrees has changed the demographics of the students matriculating into PA programs, attracting younger students, straight from undergraduate institutions, with less prior healthcare experience.14 As a result, not only are new PA graduates less experienced overall, but they are particularly lacking in exposure to hospital medicine. After PA students complete their first 12 months of PA school in the basic sciences and didactic coursework, they embark on 12 to 15 months of clinical rotations, which are largely rooted in primary care. In fact, many PA programs find it difficult to offer hospital‐based rotations while fulfilling the required rotations in primary care. These factors have resulted in the need for more extensive on‐the‐job training particularly for those new graduates interested in hospital medicine. In light of these challenges, our institution created a 12‐month postgraduate PA fellowship program in Hospital Medicine.
Postgraduate PA Training Programs
Postgraduate PA fellowships, interchangeably called residencies, are voluntary 1‐year training programs that provide both didactic instruction and clinical experience in a medical or surgical subspecialty, thereby lessening the need for on‐the‐job training. These programs are recognized by the Association of Postgraduate Physician Assistant Programs.15 Currently, there are 44 postgraduate training programs in the United States, in a wide range of medical and surgical specialties. At the end of these 1‐year postgraduate PA programs, most graduates receive a certificate of completion. Until now, the only postgraduate education option for PAs interested in Hospital Medicine was a master's completion program only available to PAs who were already employed by a hospitalist group.15 This work reviews the first reported postgraduate hospitalist training program for PAs. Specifically, the program's background, curriculum, anticipated program outcomes, and future plans are discussed.
Background for A Hospitalist Postgraduate PA Fellowship
Mayo Clinic Arizona is a multispecialty private group comprised of both outpatient services and a tertiary care hospital medical center, located in the metropolitan Phoenix, AZ, area. The Mayo Clinic Hospital is a 7‐story facility with 244 licensed beds, 18 operating rooms, and a Level II emergency department. The Mayo Hospitalist group is composed of 15 full time hospitalists and 6 part‐time hospitalists, all of whom are salaried Mayo employees. The group provides 24‐hour in‐house staffing, covering both resident services (teams composed of interns and residents supervised by a staff hospitalist) and nonresident services (staff hospitalists). Over the years there has been steady growth in the number of nonresident services, in part due to resident work‐hour restrictions. To support the physicians working on these nonresident services, the first PA was hired in 2001. Since then, the number of NPPs in our Hospitalist group has increased to 9.35 full‐time equivalents (FTEs), including 1 nurse practitioner. However, one of the greatest challenges in expanding the NPP service was the difficulty finding candidates with experience in hospital internal medicine. This need inspired the creation of a PA fellowship in Hospital Medicine. At the time, there were 2 other postgraduate PA training programs at the Mayo Clinic Arizona in Hepatology and Otolaryngology/Ear, Nose, and Throat (ENT) Surgery.
Program Description
The Mayo Clinic Arizona PA fellowship in Hospital Medicine began in October 2007 and currently accepts 1 fellow per year. Applicants must be graduates of an Accreditation Review Commission in Education for the Physician Assistant (ARC‐PA)‐accredited PA program and be certified through the National Commission on Certification of Physician Assistants (NCCPA). Furthermore, they must be licensed to work as a PA in the state of Arizona. The program is 12 months in duration, and is comprised of both didactic and clinical components. Upon graduation, the fellow earns a certificate of completion from the Mayo Clinic College of Medicine. The program has received recognition with the Association of Postgraduate Physician Assistant Programs (APPAP).
Two physician assistants act as co‐program directors of the PA fellowship in hospital medicine. They are given 0.10 full‐time equivalent (FTE) for management of the program, which includes day‐to‐day operations, curriculum development, and candidate selection. The program also has 2 volunteer physician medical directors, both of whom have previous medical residency experience. The physicians and NPPs in our hospitalist group volunteer their time to serve as faculty for the program, assisting with much of the didactic and clinical education. The program receives a budget of $99,500 per year, which is funded by the organization's foundation through the department of education. This includes the fellow stipend of $44,000 per 12 months and institutional malpractice insurance coverage. The fellow also receives health and dental insurance, 2 weeks of paid vacation, and $500 stipend toward attendance of a continuing medical education (CME) conference.
CURRICULUM
The PA fellowship curriculum is designed in a diverse unique format that strives to accommodate all types of learners. It includes clinical rotations in various medicine/surgical subspecialties, didactic instruction, and teaching modules (Figure 1). The curriculum is based upon the SHM Core Competencies.15
Clinical Rotations
The PA fellow completes 12 to 14 general hospital medicine and medical specialty rotations, each 2 to 4 weeks in duration. The rotation calendar for the current fellow is given in Figure 2. These rotations are all inpatient‐based and are supervised by either the hospitalist or the respective inpatient subspecialists. The PA fellow's specific clinical responsibilities vary from rotation to rotation, and are designed to maximize the fellow's exposure to that particular specialty. Each rotation has specific written objectives created by the program directors and reviewed by the rotation's preceptor(s) (Figure 2). During the clinical rotations, complementary didactic lectures, coursework, and readings are provided to ensure the PA fellow receives a strong foundation. Didactic instruction is designed by the program directors, physician preceptors and staff NPPs, and is coordinated with the clinical rotation specialty. At the end of each rotation the fellow is evaluated by the preceptor and given direct feedback on their performance.
Didactic Instruction
The didactic instruction is organized in a system‐based manner and occurs on a weekly basis during the Hospital Internal Medicine service and Medicine Consults rotations. Hospitalist NPPs and physician faculty are responsible for most of the teaching. This formal didactic instruction is supplemented by journal club presentations given by the PA fellow to faculty in the division of hospital internal medicine. The fellow is also required to attend daily medical resident lunchtime educational lectures, weekly medical grand rounds, and any lectures provided by the medicine subspecialties while the PA is on that particular rotation.
Teaching Modules
One component of the Hospital Medicine PA fellowship curriculum that may be unique is the concept of teaching modules. While receiving regular didactic instruction and completing their clinical rotations, the PA is also expected to complete self‐directed teaching module assignments. These modules serve to educate the PA fellow on the hospital as a systemthe true essence of hospital medicine. The modules cover a variety of topics not directly addressed during their rotations. These topics are outlined in Figure 3. Each teaching module consists of a didactic component, clinical application, and assessment (Figure 4) and has its own specific objectives and goals. Teaching modules are often taught by the local expert in the hospital in that particular area. For example, for the infectious control teaching module, the PA fellow will rotate with the infection control nursing staff learning about the isolation and infection control policies of the institution.
Assessment Tools
There are several tools utilized to assess both the PA fellow and the fellowship program itself (Figure 5). The assessment tools used include both ongoing and summative assessments. To fulfill the ongoing assessment, each rotation and teaching module contains assessment tools provided by the preceptor, which are reviewed by the program directors. Additionally, during the clinical rotations, skills are assessed using competency checklists that require the preceptor to directly observe the PA fellow perform a specific task or skill‐set and sign off on its successful completion (Supplementary Figures 6, 7).
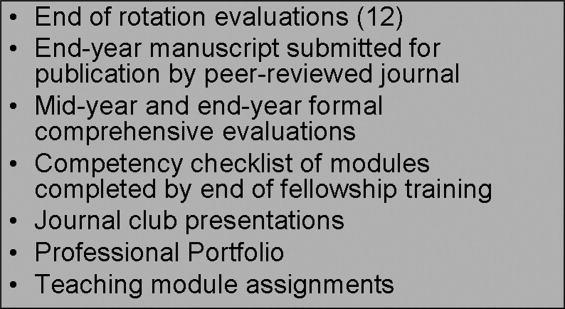
There are 2 forms of summative assessment for the PA fellow. First, to assess the PA fellow's knowledge, comprehensive mid‐year and end‐year examinations are utilized. These multiple‐choice examinations are comprised of questions which align with the didactic lectures/objectives provided by the Hospital Medicine faculty throughout the year. The second form of summative evaluation of the fellow is project‐based and divided into 2 parts. First, the fellow is expected to write a publication‐quality manuscript on a hospital medicine topic by the end of the year. Second, the PA fellow is expected to create a professional portfolio, which is comprised of a collection of all of the rotation/module assessments, the formal program assessments, and documentation of all of the skills obtained by the fellow throughout year (competency checklists). This portfolio can be used by the graduate to demonstrate to future employers what skills they possess and provide documentation of knowledge gained during the fellowship.
The program itself is evaluated by several measures. First, the fellow provides formal feedback during the mid‐year and end‐of‐the‐year assessments, which are used to enhance the experience of future fellows. Second, there is ongoing review by both the division of Hospital Medicine and the institution's Allied Health Education Committee, which ensures that the program maintains the appropriate standards and goals.
Future Goals for the PA Fellowship
The program graduated its first fellow at the end of October 2008 and has enjoyed early success. Integrating the PA fellow onto the hospitalist services augmented the present mid‐level and physician teams. There has been excellent institutional support for the program with extremely positive feedback from the rotation preceptors. There are several futures plans for the program. Our first goal is to seek accreditation from the Accreditation Review Commission for Physician Assistants (ARC‐PA), the organization that accredits entry level PA programs and which began formal, voluntary accreditation of postgraduate programs in early 2008. We plan to begin this process within the next academic year.
Our second long‐term goal for the program is to include NPs in the training program. Because of the desire to seek accreditation, the program directors felt temporarily limiting the fellowship to PAs would aide in the rigorous accreditation process, which can take approximately 1 year to complete. There is an NP on our faculty and the program has received interest from NPs. Once we obtain accreditation, expand the program enrollment, and develop an NP curriculum, we plan to open the fellowship to either PA or NP applicants.
Our third goal is to substantiate our PA Fellowship validity with outcome measures and ultimately publishable data. Thus far, the success of the PA fellowship is qualitative, and with small numbers of graduates it is difficult to quantify. After graduation of many subsequent PA fellows, our goal is to obtain quantifiable data that can be used to improve the quality of the PA fellowship and demonstrate the value of postgraduate training for physician assistants.
Perhaps the most important goal of the program is to eventually accept additional PA/NP fellows per year. While 1 program does not meet the demands of a national shortage of hospitalist providers, it may serve as a model that other institutions can adapt to their own needs. Since the program is based upon the SHM Core Competencies, the curriculum can be applied to a variety of hospitalist programs, and its relatively low operating cost makes it feasible for both academic‐based and community‐based institutions. Importantly, since recruitment and retention of employees is such a challenge for most hospitalist groups, this PA fellowship program may serve as a vehicle for recruitment and long‐term retention of well‐trained employees. This precedent has been set, as our division has hired our first PA fellow, whose transition from PA fellow to PA staff was seamless.
In conclusion, our PA fellowship in Hospital Medicine represents the first reported postgraduate PA program of this kind in the United States offering a certificate of completion. As the need for hospitalists increase so will the need for NPPs, particularly those with additional training in hospital medicine. This program serves as an example of 1 type of training tool for physician assistants looking to work in hospital medicine.
In recent years, the demand for hospitalists has outstripped the supply, creating a national shortage.1, 2 A recent Society of Hospital Medicine (SHM) survey found that in the last 2 years there has been a 31% mean growth increase in the number of hospitalist groups.3 As hospitalists are becoming more difficult to recruit, many practices are utilizing physician assistants (PAs) and nurse practitioners (NPs), collectively referred to as nonphysician providers (NPPs) to help offset the workload.4 The SHM survey also noted that the number of hospitalist groups utilizing NPPs increased from 29% to 38%.3 The exact number of NPPs working for hospitalist groups is unknown.
Hospitalist NPPs are in demand for reasons other than just physician shortages. NPPs have been utilized to fill the gap in many institutions where the workforce was impacted by the 2002 Accreditation Council for Graduate Medical Education (ACGME) ruling to restrict resident work hours. Several studies have documented NPPs' ability to assist with the compliance of ACCGME resident work‐hour restrictions while maintaining patient continuity of care, improving length of stays, and reducing health care costs on various hospital services.59 Dresselhaus et al.10 found that 56% of medical resident's time on service was delegated to tasks not related to direct patient care. They proposed that these tasks can be delegated to the NPPs, leaving more time for the residents to focus on direct patient care. In a recent study performed at a Pennsylvania hospital, patients presenting to the emergency department with low‐risk chest pain (based upon thrombolysis in myocardial infarction [TIMI] risk score) were admitted to a nonteaching service staffed with NPPs and attending physicians. Simultaneously, a similar group of low‐risk chest pain patients were admitted to a traditional internal medicine resident service. The results demonstrated lower median length of stay and hospital charges on the nonteaching service. This study suggested that NPPs can offset the workload volume for medical residents, allowing them to focus on patients with higher acuity and greater learning value.11
Barriers to Finding Experienced NPPs in Hospital Medicine
Although many hospitalist groups are interested in hiring NPPs, there can be significant obstacles to recruitment. For example, most experienced PAs and NPs have clinical backgrounds in either surgical or medical subspecialties and therefore typically need extensive on‐the‐job training in hospital medicine, which can often take at least 6 to 12 months to acquire the basic skill set.12 Hiring new graduates may require even longer training periods.
The inexperience of new graduates has become an even more pertinent issue due to recent changes in PA education. Traditionally, PA programs attracted older students with prior healthcare experience, who wished to return to school for additional training. However, in 2005 a major shift occurred in PA education: programs began transitioning from graduating trainees with a bachelor's degree to now requiring a master's level degree for completion of the PA program.13 The acquisition of more advanced degrees has changed the demographics of the students matriculating into PA programs, attracting younger students, straight from undergraduate institutions, with less prior healthcare experience.14 As a result, not only are new PA graduates less experienced overall, but they are particularly lacking in exposure to hospital medicine. After PA students complete their first 12 months of PA school in the basic sciences and didactic coursework, they embark on 12 to 15 months of clinical rotations, which are largely rooted in primary care. In fact, many PA programs find it difficult to offer hospital‐based rotations while fulfilling the required rotations in primary care. These factors have resulted in the need for more extensive on‐the‐job training particularly for those new graduates interested in hospital medicine. In light of these challenges, our institution created a 12‐month postgraduate PA fellowship program in Hospital Medicine.
Postgraduate PA Training Programs
Postgraduate PA fellowships, interchangeably called residencies, are voluntary 1‐year training programs that provide both didactic instruction and clinical experience in a medical or surgical subspecialty, thereby lessening the need for on‐the‐job training. These programs are recognized by the Association of Postgraduate Physician Assistant Programs.15 Currently, there are 44 postgraduate training programs in the United States, in a wide range of medical and surgical specialties. At the end of these 1‐year postgraduate PA programs, most graduates receive a certificate of completion. Until now, the only postgraduate education option for PAs interested in Hospital Medicine was a master's completion program only available to PAs who were already employed by a hospitalist group.15 This work reviews the first reported postgraduate hospitalist training program for PAs. Specifically, the program's background, curriculum, anticipated program outcomes, and future plans are discussed.
Background for A Hospitalist Postgraduate PA Fellowship
Mayo Clinic Arizona is a multispecialty private group comprised of both outpatient services and a tertiary care hospital medical center, located in the metropolitan Phoenix, AZ, area. The Mayo Clinic Hospital is a 7‐story facility with 244 licensed beds, 18 operating rooms, and a Level II emergency department. The Mayo Hospitalist group is composed of 15 full time hospitalists and 6 part‐time hospitalists, all of whom are salaried Mayo employees. The group provides 24‐hour in‐house staffing, covering both resident services (teams composed of interns and residents supervised by a staff hospitalist) and nonresident services (staff hospitalists). Over the years there has been steady growth in the number of nonresident services, in part due to resident work‐hour restrictions. To support the physicians working on these nonresident services, the first PA was hired in 2001. Since then, the number of NPPs in our Hospitalist group has increased to 9.35 full‐time equivalents (FTEs), including 1 nurse practitioner. However, one of the greatest challenges in expanding the NPP service was the difficulty finding candidates with experience in hospital internal medicine. This need inspired the creation of a PA fellowship in Hospital Medicine. At the time, there were 2 other postgraduate PA training programs at the Mayo Clinic Arizona in Hepatology and Otolaryngology/Ear, Nose, and Throat (ENT) Surgery.
Program Description
The Mayo Clinic Arizona PA fellowship in Hospital Medicine began in October 2007 and currently accepts 1 fellow per year. Applicants must be graduates of an Accreditation Review Commission in Education for the Physician Assistant (ARC‐PA)‐accredited PA program and be certified through the National Commission on Certification of Physician Assistants (NCCPA). Furthermore, they must be licensed to work as a PA in the state of Arizona. The program is 12 months in duration, and is comprised of both didactic and clinical components. Upon graduation, the fellow earns a certificate of completion from the Mayo Clinic College of Medicine. The program has received recognition with the Association of Postgraduate Physician Assistant Programs (APPAP).
Two physician assistants act as co‐program directors of the PA fellowship in hospital medicine. They are given 0.10 full‐time equivalent (FTE) for management of the program, which includes day‐to‐day operations, curriculum development, and candidate selection. The program also has 2 volunteer physician medical directors, both of whom have previous medical residency experience. The physicians and NPPs in our hospitalist group volunteer their time to serve as faculty for the program, assisting with much of the didactic and clinical education. The program receives a budget of $99,500 per year, which is funded by the organization's foundation through the department of education. This includes the fellow stipend of $44,000 per 12 months and institutional malpractice insurance coverage. The fellow also receives health and dental insurance, 2 weeks of paid vacation, and $500 stipend toward attendance of a continuing medical education (CME) conference.
CURRICULUM
The PA fellowship curriculum is designed in a diverse unique format that strives to accommodate all types of learners. It includes clinical rotations in various medicine/surgical subspecialties, didactic instruction, and teaching modules (Figure 1). The curriculum is based upon the SHM Core Competencies.15
Clinical Rotations
The PA fellow completes 12 to 14 general hospital medicine and medical specialty rotations, each 2 to 4 weeks in duration. The rotation calendar for the current fellow is given in Figure 2. These rotations are all inpatient‐based and are supervised by either the hospitalist or the respective inpatient subspecialists. The PA fellow's specific clinical responsibilities vary from rotation to rotation, and are designed to maximize the fellow's exposure to that particular specialty. Each rotation has specific written objectives created by the program directors and reviewed by the rotation's preceptor(s) (Figure 2). During the clinical rotations, complementary didactic lectures, coursework, and readings are provided to ensure the PA fellow receives a strong foundation. Didactic instruction is designed by the program directors, physician preceptors and staff NPPs, and is coordinated with the clinical rotation specialty. At the end of each rotation the fellow is evaluated by the preceptor and given direct feedback on their performance.
Didactic Instruction
The didactic instruction is organized in a system‐based manner and occurs on a weekly basis during the Hospital Internal Medicine service and Medicine Consults rotations. Hospitalist NPPs and physician faculty are responsible for most of the teaching. This formal didactic instruction is supplemented by journal club presentations given by the PA fellow to faculty in the division of hospital internal medicine. The fellow is also required to attend daily medical resident lunchtime educational lectures, weekly medical grand rounds, and any lectures provided by the medicine subspecialties while the PA is on that particular rotation.
Teaching Modules
One component of the Hospital Medicine PA fellowship curriculum that may be unique is the concept of teaching modules. While receiving regular didactic instruction and completing their clinical rotations, the PA is also expected to complete self‐directed teaching module assignments. These modules serve to educate the PA fellow on the hospital as a systemthe true essence of hospital medicine. The modules cover a variety of topics not directly addressed during their rotations. These topics are outlined in Figure 3. Each teaching module consists of a didactic component, clinical application, and assessment (Figure 4) and has its own specific objectives and goals. Teaching modules are often taught by the local expert in the hospital in that particular area. For example, for the infectious control teaching module, the PA fellow will rotate with the infection control nursing staff learning about the isolation and infection control policies of the institution.
Assessment Tools
There are several tools utilized to assess both the PA fellow and the fellowship program itself (Figure 5). The assessment tools used include both ongoing and summative assessments. To fulfill the ongoing assessment, each rotation and teaching module contains assessment tools provided by the preceptor, which are reviewed by the program directors. Additionally, during the clinical rotations, skills are assessed using competency checklists that require the preceptor to directly observe the PA fellow perform a specific task or skill‐set and sign off on its successful completion (Supplementary Figures 6, 7).
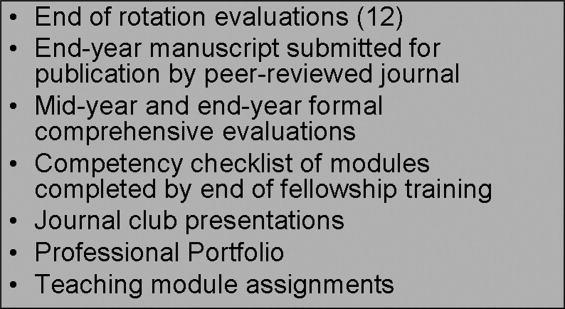
There are 2 forms of summative assessment for the PA fellow. First, to assess the PA fellow's knowledge, comprehensive mid‐year and end‐year examinations are utilized. These multiple‐choice examinations are comprised of questions which align with the didactic lectures/objectives provided by the Hospital Medicine faculty throughout the year. The second form of summative evaluation of the fellow is project‐based and divided into 2 parts. First, the fellow is expected to write a publication‐quality manuscript on a hospital medicine topic by the end of the year. Second, the PA fellow is expected to create a professional portfolio, which is comprised of a collection of all of the rotation/module assessments, the formal program assessments, and documentation of all of the skills obtained by the fellow throughout year (competency checklists). This portfolio can be used by the graduate to demonstrate to future employers what skills they possess and provide documentation of knowledge gained during the fellowship.
The program itself is evaluated by several measures. First, the fellow provides formal feedback during the mid‐year and end‐of‐the‐year assessments, which are used to enhance the experience of future fellows. Second, there is ongoing review by both the division of Hospital Medicine and the institution's Allied Health Education Committee, which ensures that the program maintains the appropriate standards and goals.
Future Goals for the PA Fellowship
The program graduated its first fellow at the end of October 2008 and has enjoyed early success. Integrating the PA fellow onto the hospitalist services augmented the present mid‐level and physician teams. There has been excellent institutional support for the program with extremely positive feedback from the rotation preceptors. There are several futures plans for the program. Our first goal is to seek accreditation from the Accreditation Review Commission for Physician Assistants (ARC‐PA), the organization that accredits entry level PA programs and which began formal, voluntary accreditation of postgraduate programs in early 2008. We plan to begin this process within the next academic year.
Our second long‐term goal for the program is to include NPs in the training program. Because of the desire to seek accreditation, the program directors felt temporarily limiting the fellowship to PAs would aide in the rigorous accreditation process, which can take approximately 1 year to complete. There is an NP on our faculty and the program has received interest from NPs. Once we obtain accreditation, expand the program enrollment, and develop an NP curriculum, we plan to open the fellowship to either PA or NP applicants.
Our third goal is to substantiate our PA Fellowship validity with outcome measures and ultimately publishable data. Thus far, the success of the PA fellowship is qualitative, and with small numbers of graduates it is difficult to quantify. After graduation of many subsequent PA fellows, our goal is to obtain quantifiable data that can be used to improve the quality of the PA fellowship and demonstrate the value of postgraduate training for physician assistants.
Perhaps the most important goal of the program is to eventually accept additional PA/NP fellows per year. While 1 program does not meet the demands of a national shortage of hospitalist providers, it may serve as a model that other institutions can adapt to their own needs. Since the program is based upon the SHM Core Competencies, the curriculum can be applied to a variety of hospitalist programs, and its relatively low operating cost makes it feasible for both academic‐based and community‐based institutions. Importantly, since recruitment and retention of employees is such a challenge for most hospitalist groups, this PA fellowship program may serve as a vehicle for recruitment and long‐term retention of well‐trained employees. This precedent has been set, as our division has hired our first PA fellow, whose transition from PA fellow to PA staff was seamless.
In conclusion, our PA fellowship in Hospital Medicine represents the first reported postgraduate PA program of this kind in the United States offering a certificate of completion. As the need for hospitalists increase so will the need for NPPs, particularly those with additional training in hospital medicine. This program serves as an example of 1 type of training tool for physician assistants looking to work in hospital medicine.
- ,,,.Health care market trends and the evolution of hospitalist use and roles.J Gen Intern Med.2004;20:101–107.
- .Innovations in the management of hospitalized patients. Nurse Pract Spring2006 (suppl):2–3.
- .Hospitalist pay up, productivity steady in SHM's latest survey.Hospitalist.2008;12(5):7,16.
- .Physician assistants: filling the gap in patient care in academic hospitals.Perspect Physician Assist Educ.2003;14(3):158–167.
- ,,, et al.The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs.J Nurs Adm.2006;36(2):79–85.
- ,,, et al.Physician extenders impact trauma systems.J Trauma.2005;58(5):917–920.
- ,,.The role of physician assistants in critical care units.Chest.1991;99:89–91.
- .Alliances: invaluable assistants.Hospitalist.2006;April:32–33.
- ,,.Resource use by physician assistant services versus teaching services.JAAPA.2002;15:33–42.
- ,,,,,.Analyzing the time and value of house staff inpatient work.J Intern Med.1998;13:534–540.
- ,,, et al.Improving resource utilization in a teaching hospital: Development of a nonteaching service for chest pain admissions.Acad Med.2006;81(5):432–435.
- .Midlevels make a rocky entrance into hospital medicine.Todays Hospitalist.2007;5(1):28–32.
- Accreditation Review Commission for Physician Assistant Education.3rd ed. 2005. Available at: http://www.arc‐pa.org/Standards/standards.html. Accessed September2009.
- 22nd Annual Report on Physician Assistant Education in the U.S., 2005–2006. Available at: http://www.paeaonline.org. Accessed September2009.
- Association of Postgraduate Physician Assistant Programs. Available at: http://www.appap.org. Accessed September2009.
- ,,,,.The core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- ,,,.Health care market trends and the evolution of hospitalist use and roles.J Gen Intern Med.2004;20:101–107.
- .Innovations in the management of hospitalized patients. Nurse Pract Spring2006 (suppl):2–3.
- .Hospitalist pay up, productivity steady in SHM's latest survey.Hospitalist.2008;12(5):7,16.
- .Physician assistants: filling the gap in patient care in academic hospitals.Perspect Physician Assist Educ.2003;14(3):158–167.
- ,,, et al.The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs.J Nurs Adm.2006;36(2):79–85.
- ,,, et al.Physician extenders impact trauma systems.J Trauma.2005;58(5):917–920.
- ,,.The role of physician assistants in critical care units.Chest.1991;99:89–91.
- .Alliances: invaluable assistants.Hospitalist.2006;April:32–33.
- ,,.Resource use by physician assistant services versus teaching services.JAAPA.2002;15:33–42.
- ,,,,,.Analyzing the time and value of house staff inpatient work.J Intern Med.1998;13:534–540.
- ,,, et al.Improving resource utilization in a teaching hospital: Development of a nonteaching service for chest pain admissions.Acad Med.2006;81(5):432–435.
- .Midlevels make a rocky entrance into hospital medicine.Todays Hospitalist.2007;5(1):28–32.
- Accreditation Review Commission for Physician Assistant Education.3rd ed. 2005. Available at: http://www.arc‐pa.org/Standards/standards.html. Accessed September2009.
- 22nd Annual Report on Physician Assistant Education in the U.S., 2005–2006. Available at: http://www.paeaonline.org. Accessed September2009.
- Association of Postgraduate Physician Assistant Programs. Available at: http://www.appap.org. Accessed September2009.
- ,,,,.The core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
Copyright © 2010 Society of Hospital Medicine