User login
Inactivity and increased sedentary time are major public health problems, particularly among older adults.1-3 Inactivity increases with age and produces deleterious effects on physical health, mental health, and quality of life and leads to increased health care costs.4 The high prevalence of a sedentary lifestyle among older veterans may be due to multiple factors, including misconceptions about the health benefits of exercise, lack of motivation, or associating exercise with discomfort or pain. Older veterans living in rural areas are at high risk because they are more sedentary than are urban-dwelling veterans.5 Of veterans aged ≥ 65 years who use health care services in VISN 16, 59% live in rural or highly rural areas.
Given the large number of older veterans and their at-risk status, addressing inactivity among this population is critical. Until recently, few programs existed within the VHA that addressed this need. Despite strong evidence that physical activity helps maintain functional independence and avoids institutionalization of frail elderly veterans, the VHA had no established procedures or guidelines for assessment and counseling.
To address this void, a Geriatric Walking Clinic (GWC) was established at the Central Arkansas Veterans Healthcare System (CAVHS) in March 2013. The GWC developed a patient-centric, home-based program that implements a comprehensive approach to assess, educate, motivate, and activate older veterans to commit to, engage in, and adhere to, a long-term program of regular physical activity primarily in the form of walking. The program uses proven strategies, such as motivational counseling, follow-up phone calls from a nurse, and self-monitoring using pedometers.6-8 Funding for the GWC project was provided by the VHA Office of Geriatrics and Extended Care as part of its Transition to the 21st Century (T21) initiative and by the VHA Office of Rural Health.
Methods
Quality improvement (QI) principles were used to develop the program, which received a nonresearch determination status from the local institutional review board. The GWC is staffed by a registered nurse, health technician, and physician. Both the nurse and the health technician were trained on the use of various assessments. Several tactics were developed to promote patient recruitment to the GWC, including systemwide in-services, an easy-to-use consultation request within the electronic medical record, patient and provider brochures, and informational booths and kiosks. Collaborations were developed with various clinical services to promote referrals. Several other services, such as Primary Care, Geriatrics, the Move! Weight Management Program, Cardiology (including Congestive Heart Failure), Hematology/Oncology, and Mental Health referred patients to the GWC.
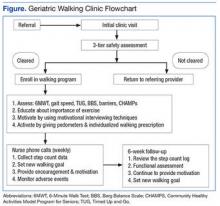
The GWC targets sedentary, community-dwelling veterans aged ≥ 60 years who are able to ambulate in their home without an assistive device, are willing to walk for exercise, and are willing to receive phone calls. All-comers are included in the program. Although most of these veterans have multiple chronic medical problems, only those with absolute contraindications to exercise per the American College of Sports Medicine guidelines and those with any medical condition that is likely to compromise their ability to safely participate in the walking program are excluded (Figure).
First Visit
At the first visit, veterans receive a brief education about GWC, highlighting its potential health benefits. If veterans want to join, they are evaluated using a 3-tier screening assessment to determine the safety of starting a new walking regimen. Veterans who fail the 3-tier safety screening are referred to their primary care physician (PCP) for further assessment (eg, cardiac stress testing) to better define eligibility status. Veterans who pass the screen complete brief tests of physical performance, including gait speed, 6-Minute Walk Test (6MWT), Timed Up and Go test, and Berg Balance Scale.9-12 Participants also complete short surveys that provide useful information about their social support, barriers to exercise, response to physical activity, and usual activity level as measured by Community Healthy Activities Model Program for Seniors.13,14 This information is used to help develop an individualized walking prescription.
After completing the baseline assessments, the GWC staff members help the veteran set realistic goals, using motivational counseling techniques. The veteran receives a walking prescription to walk indoors or outdoors, based on current physical condition, self-identified goals, perceived barriers, and strength of support system; educational material about safe walking; a log for recording daily step count; information on follow-up calls; and an invitation to return for follow-up visits. The veteran also receives a pedometer and is instructed to continue his or her usual routine for the first week. The average daily step count is recorded as the baseline. The veteran is instructed to start the walking program after the baseline week with goals tailored to the personal activity level. For example: Some patients are asked to simply add an extra minute to their walking, whereas others savvy with pedometer numbers are asked to increase their step count.
Follow-up
Veterans are followed closely between their clinic appointments via phone calls from a nurse who provides encouragement and helps set new goals. The nurse collects the step count data to determine progress and set new walking goals. Those unable to adhere to their walking prescription are reassessed for their barriers. The nurse also helps participants identify ways to overcome individual challenges. The PCP is consulted when barriers include medical problems, such as pain or poor blood sugar control.
At the 6-week follow-up visit, the health care provider reviews the pedometer log and repeats all outcome assessments, including the physical performance testing and the participant surveys. Veterans receive feedback from these outcome assessments. To assess participant satisfaction, CAVHS GRECC developed a satisfaction questionnaire, which was given to participants.
Results
A total of 249 older veterans participated in the GWC program. The mean age was 67 (±6) years; 92% were male, 60% were white, and 39% were African American. Most participants lived in a rural location (60%) and were obese (69%); consistent with national standards, obesity was defined as a body mass index (BMI) ≥ 30 kg/m2. Several barriers to exercise were endorsed by the veterans. Most commonly endorsed barriers included bad weather, lack of motivation, feeling tired, and fear of pain. Most participants (93%) were actively engaged via regular phone follow-ups visits; 121 (49%) participants returned to the clinic for the 6-week reassessment. Repeat performance testing at the 6-week visit showed a clinically significant average 14% improvement in the 6MWT, 6% improvement in the Timed Up and Go test, and a 27% improvement in gait speed. Of those veterans who were obese, 64% lost weight. On entry into the program, 32 participants (13%) had poorly controlled diabetes mellitus (DM), defined as hemoglobin A1c (HbA1c) ≥ 8. Among this group, HbA1c improved by an average of 1.5% by the 6-week visit. The GWC program may have contributed to the improved glycemic control as a generally accepted frequency of monitoring HbA1c is at least 3 months.
At the 6-week clinic visit, 94% of those surveyed completed a program evaluation. The GWC scored high on satisfaction; over 80% strongly agreed that they were satisfied with the GWC program as a whole, 80% strongly agreed that the program increased their awareness about need for exercise, 82% strongly agreed that the clinician’s advice was applicable to them, and 77% strongly agreed that the program improved their motivation to walk regularly (Table 1).
Program Economics
An analysis of the clinic costs and benefits was performed to determine whether costs could potentially be offset by the savings realized from improved health outcomes of participating veterans. For this simplified analysis, costs of maintaining the GWC were set equal to the costs of the full-time equivalent employee hours, equipment, and educational materials. Based on the authors’ experience, they projected that for each 1,000 older veterans enrolled in the GWC, there is a requirement for 0.5 medical support assistant (GS-6 pay scale), 1.0 registered nurse grade 2 (RN), 1.0 health science specialist (GS-7), and 0.25 physician. At the host facility, the annual personnel costs are estimated at $205,149. The total annual cost of the GWC, including the equipment and educational materials, is estimated at $240,149.
Although full financial return on investment has yet to be determined, the authors estimated potential cost savings resulting if patients enrolled in a GWC achieved and maintained the types of improvements observed in the first cohort of patients. These estimates were based on identified improvements in 3 patient outcome measures cited in the medical literature that are associated with reductions in subsequent health care costs. These measures include gait speed, weight loss, and HbA1c. It is estimated that the cost savings associated with improvement of gait speed by 0.1 m/s (a clinically relevant change) is $1,200 annually.15
On average, patients enrolled in the GWC program improved their gait speed by 0.22 m/s. Cost savings related to gait speed improvement for 1,000 participants could reach $1,200,000. Conservative estimates of cost savings per 1% reduction of HbA1c is $950/year.16 Among those with poorly controlled DM (ie, HbA1c of ≥ 8), average HbA1c declined by 1.5%. Provided that 13% of the patients have poorly controlled DM, the total cost saving for 1,000 participants could be $209,950 annually.
It also is estimated that a 1% weight loss in obese patients is associated with a $256 decrease in subsequent total health care costs.17 In the GWC, the obese participants lost an average of 1.3% of their baseline weight. Assuming that about 60% of all older veterans participating in the clinic program are obese, annual cost savings per 1,000 participants related to weight loss is estimated to be $199,680. After accounting for the costs of operating the clinic, the total cost savings for a GWC with 1,000 enrolled older veterans is estimated to be as much as $1.4 million annually. Such a favorable cost assessment suggests that the program should be evaluated for widespread dissemination throughout the entire VHA system. Other potential benefits associated with GWC participation, such as improved quality of life and greater functional independence, may be of even greater importance to veterans.
Limitations
Results of this QI project need to be considered in light of its limitations. One of the most important limitations is the design of the project. Since this was a clinical initiative and not a research study, there was no control group or randomization. There were also limitations on data availability. HbA1c tests were not ordered as part of this QI project. Instead, baseline HbA1c was set equal to the most recent of any value obtained clinically within 2 months before the participant’s GWC enrollment; the 6-week follow-up value was set to any HbA1c obtained within 2 months after the 6-week visit. It is also recognized that factors other than the veterans’ participation in the GWC (eg, alterations in their DM medication regimen) may have contributed to the changes noted in some participant’s HbA1c. Although not necessarily a limitation, 140 of the 247 participants (57%) were enrolled in MOVE! as well. MOVE! is a widely popular weight management program in the VA focusing on diet control.18 The authors, however, have no information about the veterans’ adherence to MOVE!
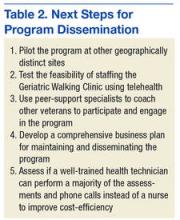
Five immediate next steps to disseminate the program have been identified (Table 2).
Conclusion
The GWC was successfully developed and implemented as a QI project at CAVHS and was met with much satisfaction by older veterans. Participants experienced clinically significant improvements in physical performance and other health indicators, suggesting that these benefits could potentially offset clinic costs.
1. Jefferis BJ, Sartini C, Ash S, et al. Trajectories of objectively measured physical activity in free-living older men. Med Sci Sports Exerc. 2015;47(2):343-349.
2. Sun F, Norman IJ, While AE. Physical activity in older people: a systematic review. BMC Public Health. 2013;13:449.
3. Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181-188.
4. Vogel T, Brechat PH, Lepretre PM, Kaltenbach G, Berthel M, Lonsdorfer J. Health benefits of physical activity in older patients: a review. Int J Clin Pract. 2009;63(2):303-320.
5. Patterson PD, Moore CG, Probst JC, Shinogle JA. Obesity and physical inactivity in rural America. J Rural Health. 2004;20(2):151-159.
6. Dubbert PM, Cooper KM, Kirchner KA, Meydrech EF, Bilbrew D. Effects of nurse counseling on walking for exercise in elderly primary care patients. J Gerontol A Biol Sci Med Sci. 2002;57(11):M733-M740.
7. Dubbert PM, Morey MC, Kirchner KA, Meydrech EF, Grothe K. Counseling for home-based walking and strength exercise in older primary care patients. Arch Intern Med. 2008;168(9):979-986.
8. Newton RL Jr, HH M, Dubbert PM, et al. Pedometer determined physical activity tracks in African American adults: the Jackson Heart Study. Int J Behav Nutr Phys Act. 2012;9:44.
9. Bohannon RW. Comfortable and maximum walking speed of adults aged 20-79 years: reference values and determinants. Age Ageing. 1997;26(1):15-19.
10. Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132(8):919-923.
11. Hiengkaew V, Jitaree K, Chaiyawat P. Minimal detectable changes of the Berg Balance Scale, Fugl-Meyer Assessment Scale, Timed “Up & Go” Test, gait speeds, and 2-minute walk test in individuals with chronic stroke with different degrees of ankle plantarflexor tone. Arch Phys Med Rehabil. 2012;93(7):1201-1208.
12. Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449-459.
13. Clark DO, Nothwehr F. Exercise self-efficacy and its correlates among socioeconomically disadvantaged older adults. Health Educ Behav. 1999;26(4):535-546.
14. Stewart AL, Verboncoeur CJ, McLellan BY, et al. Physical activity outcomes of CHAMPS II: a physical activity promotion program for older adults. J Gerontol A Biol Sci Med Sci. 2001;56(8):M465-M470.
15. Purser JL, Weinberger M, Cohen HJ, et al. Walking speed predicts health status and hospital costs for frail elderly male Veterans. J Rehabil Res Dev. 2005;42(4):535-546.
16. Wagner EH, Sandhu N, Newton KM, McCulloch DK, Ramsey SD, Grothaus LC. Effect of improved glycemic control on health care costs and utilization. JAMA. 2001;285(2):182-189.
17. Yu AP, Wu EQ, Birnbaum HG, et al. Short-term economic impact of body weight change among patients with type 2 diabetes treated with antidiabetic agents: analysis using claims, laboratory, and medical record data. Curr Med Res Opin. 2007;23(9):2157-2169.
18. Romanova M, Liang LJ, Deng ML, Li Z, Heber D. Effectiveness of the MOVE! multidisciplinary weight loss program for veterans in Los Angeles. Prev Chronic Dis. 2013;10:E112.
Inactivity and increased sedentary time are major public health problems, particularly among older adults.1-3 Inactivity increases with age and produces deleterious effects on physical health, mental health, and quality of life and leads to increased health care costs.4 The high prevalence of a sedentary lifestyle among older veterans may be due to multiple factors, including misconceptions about the health benefits of exercise, lack of motivation, or associating exercise with discomfort or pain. Older veterans living in rural areas are at high risk because they are more sedentary than are urban-dwelling veterans.5 Of veterans aged ≥ 65 years who use health care services in VISN 16, 59% live in rural or highly rural areas.
Given the large number of older veterans and their at-risk status, addressing inactivity among this population is critical. Until recently, few programs existed within the VHA that addressed this need. Despite strong evidence that physical activity helps maintain functional independence and avoids institutionalization of frail elderly veterans, the VHA had no established procedures or guidelines for assessment and counseling.
To address this void, a Geriatric Walking Clinic (GWC) was established at the Central Arkansas Veterans Healthcare System (CAVHS) in March 2013. The GWC developed a patient-centric, home-based program that implements a comprehensive approach to assess, educate, motivate, and activate older veterans to commit to, engage in, and adhere to, a long-term program of regular physical activity primarily in the form of walking. The program uses proven strategies, such as motivational counseling, follow-up phone calls from a nurse, and self-monitoring using pedometers.6-8 Funding for the GWC project was provided by the VHA Office of Geriatrics and Extended Care as part of its Transition to the 21st Century (T21) initiative and by the VHA Office of Rural Health.
Methods
Quality improvement (QI) principles were used to develop the program, which received a nonresearch determination status from the local institutional review board. The GWC is staffed by a registered nurse, health technician, and physician. Both the nurse and the health technician were trained on the use of various assessments. Several tactics were developed to promote patient recruitment to the GWC, including systemwide in-services, an easy-to-use consultation request within the electronic medical record, patient and provider brochures, and informational booths and kiosks. Collaborations were developed with various clinical services to promote referrals. Several other services, such as Primary Care, Geriatrics, the Move! Weight Management Program, Cardiology (including Congestive Heart Failure), Hematology/Oncology, and Mental Health referred patients to the GWC.
The GWC targets sedentary, community-dwelling veterans aged ≥ 60 years who are able to ambulate in their home without an assistive device, are willing to walk for exercise, and are willing to receive phone calls. All-comers are included in the program. Although most of these veterans have multiple chronic medical problems, only those with absolute contraindications to exercise per the American College of Sports Medicine guidelines and those with any medical condition that is likely to compromise their ability to safely participate in the walking program are excluded (Figure).
First Visit
At the first visit, veterans receive a brief education about GWC, highlighting its potential health benefits. If veterans want to join, they are evaluated using a 3-tier screening assessment to determine the safety of starting a new walking regimen. Veterans who fail the 3-tier safety screening are referred to their primary care physician (PCP) for further assessment (eg, cardiac stress testing) to better define eligibility status. Veterans who pass the screen complete brief tests of physical performance, including gait speed, 6-Minute Walk Test (6MWT), Timed Up and Go test, and Berg Balance Scale.9-12 Participants also complete short surveys that provide useful information about their social support, barriers to exercise, response to physical activity, and usual activity level as measured by Community Healthy Activities Model Program for Seniors.13,14 This information is used to help develop an individualized walking prescription.
After completing the baseline assessments, the GWC staff members help the veteran set realistic goals, using motivational counseling techniques. The veteran receives a walking prescription to walk indoors or outdoors, based on current physical condition, self-identified goals, perceived barriers, and strength of support system; educational material about safe walking; a log for recording daily step count; information on follow-up calls; and an invitation to return for follow-up visits. The veteran also receives a pedometer and is instructed to continue his or her usual routine for the first week. The average daily step count is recorded as the baseline. The veteran is instructed to start the walking program after the baseline week with goals tailored to the personal activity level. For example: Some patients are asked to simply add an extra minute to their walking, whereas others savvy with pedometer numbers are asked to increase their step count.
Follow-up
Veterans are followed closely between their clinic appointments via phone calls from a nurse who provides encouragement and helps set new goals. The nurse collects the step count data to determine progress and set new walking goals. Those unable to adhere to their walking prescription are reassessed for their barriers. The nurse also helps participants identify ways to overcome individual challenges. The PCP is consulted when barriers include medical problems, such as pain or poor blood sugar control.
At the 6-week follow-up visit, the health care provider reviews the pedometer log and repeats all outcome assessments, including the physical performance testing and the participant surveys. Veterans receive feedback from these outcome assessments. To assess participant satisfaction, CAVHS GRECC developed a satisfaction questionnaire, which was given to participants.
Results
A total of 249 older veterans participated in the GWC program. The mean age was 67 (±6) years; 92% were male, 60% were white, and 39% were African American. Most participants lived in a rural location (60%) and were obese (69%); consistent with national standards, obesity was defined as a body mass index (BMI) ≥ 30 kg/m2. Several barriers to exercise were endorsed by the veterans. Most commonly endorsed barriers included bad weather, lack of motivation, feeling tired, and fear of pain. Most participants (93%) were actively engaged via regular phone follow-ups visits; 121 (49%) participants returned to the clinic for the 6-week reassessment. Repeat performance testing at the 6-week visit showed a clinically significant average 14% improvement in the 6MWT, 6% improvement in the Timed Up and Go test, and a 27% improvement in gait speed. Of those veterans who were obese, 64% lost weight. On entry into the program, 32 participants (13%) had poorly controlled diabetes mellitus (DM), defined as hemoglobin A1c (HbA1c) ≥ 8. Among this group, HbA1c improved by an average of 1.5% by the 6-week visit. The GWC program may have contributed to the improved glycemic control as a generally accepted frequency of monitoring HbA1c is at least 3 months.
At the 6-week clinic visit, 94% of those surveyed completed a program evaluation. The GWC scored high on satisfaction; over 80% strongly agreed that they were satisfied with the GWC program as a whole, 80% strongly agreed that the program increased their awareness about need for exercise, 82% strongly agreed that the clinician’s advice was applicable to them, and 77% strongly agreed that the program improved their motivation to walk regularly (Table 1).
Program Economics
An analysis of the clinic costs and benefits was performed to determine whether costs could potentially be offset by the savings realized from improved health outcomes of participating veterans. For this simplified analysis, costs of maintaining the GWC were set equal to the costs of the full-time equivalent employee hours, equipment, and educational materials. Based on the authors’ experience, they projected that for each 1,000 older veterans enrolled in the GWC, there is a requirement for 0.5 medical support assistant (GS-6 pay scale), 1.0 registered nurse grade 2 (RN), 1.0 health science specialist (GS-7), and 0.25 physician. At the host facility, the annual personnel costs are estimated at $205,149. The total annual cost of the GWC, including the equipment and educational materials, is estimated at $240,149.
Although full financial return on investment has yet to be determined, the authors estimated potential cost savings resulting if patients enrolled in a GWC achieved and maintained the types of improvements observed in the first cohort of patients. These estimates were based on identified improvements in 3 patient outcome measures cited in the medical literature that are associated with reductions in subsequent health care costs. These measures include gait speed, weight loss, and HbA1c. It is estimated that the cost savings associated with improvement of gait speed by 0.1 m/s (a clinically relevant change) is $1,200 annually.15
On average, patients enrolled in the GWC program improved their gait speed by 0.22 m/s. Cost savings related to gait speed improvement for 1,000 participants could reach $1,200,000. Conservative estimates of cost savings per 1% reduction of HbA1c is $950/year.16 Among those with poorly controlled DM (ie, HbA1c of ≥ 8), average HbA1c declined by 1.5%. Provided that 13% of the patients have poorly controlled DM, the total cost saving for 1,000 participants could be $209,950 annually.
It also is estimated that a 1% weight loss in obese patients is associated with a $256 decrease in subsequent total health care costs.17 In the GWC, the obese participants lost an average of 1.3% of their baseline weight. Assuming that about 60% of all older veterans participating in the clinic program are obese, annual cost savings per 1,000 participants related to weight loss is estimated to be $199,680. After accounting for the costs of operating the clinic, the total cost savings for a GWC with 1,000 enrolled older veterans is estimated to be as much as $1.4 million annually. Such a favorable cost assessment suggests that the program should be evaluated for widespread dissemination throughout the entire VHA system. Other potential benefits associated with GWC participation, such as improved quality of life and greater functional independence, may be of even greater importance to veterans.
Limitations
Results of this QI project need to be considered in light of its limitations. One of the most important limitations is the design of the project. Since this was a clinical initiative and not a research study, there was no control group or randomization. There were also limitations on data availability. HbA1c tests were not ordered as part of this QI project. Instead, baseline HbA1c was set equal to the most recent of any value obtained clinically within 2 months before the participant’s GWC enrollment; the 6-week follow-up value was set to any HbA1c obtained within 2 months after the 6-week visit. It is also recognized that factors other than the veterans’ participation in the GWC (eg, alterations in their DM medication regimen) may have contributed to the changes noted in some participant’s HbA1c. Although not necessarily a limitation, 140 of the 247 participants (57%) were enrolled in MOVE! as well. MOVE! is a widely popular weight management program in the VA focusing on diet control.18 The authors, however, have no information about the veterans’ adherence to MOVE!
Five immediate next steps to disseminate the program have been identified (Table 2).
Conclusion
The GWC was successfully developed and implemented as a QI project at CAVHS and was met with much satisfaction by older veterans. Participants experienced clinically significant improvements in physical performance and other health indicators, suggesting that these benefits could potentially offset clinic costs.
Inactivity and increased sedentary time are major public health problems, particularly among older adults.1-3 Inactivity increases with age and produces deleterious effects on physical health, mental health, and quality of life and leads to increased health care costs.4 The high prevalence of a sedentary lifestyle among older veterans may be due to multiple factors, including misconceptions about the health benefits of exercise, lack of motivation, or associating exercise with discomfort or pain. Older veterans living in rural areas are at high risk because they are more sedentary than are urban-dwelling veterans.5 Of veterans aged ≥ 65 years who use health care services in VISN 16, 59% live in rural or highly rural areas.
Given the large number of older veterans and their at-risk status, addressing inactivity among this population is critical. Until recently, few programs existed within the VHA that addressed this need. Despite strong evidence that physical activity helps maintain functional independence and avoids institutionalization of frail elderly veterans, the VHA had no established procedures or guidelines for assessment and counseling.
To address this void, a Geriatric Walking Clinic (GWC) was established at the Central Arkansas Veterans Healthcare System (CAVHS) in March 2013. The GWC developed a patient-centric, home-based program that implements a comprehensive approach to assess, educate, motivate, and activate older veterans to commit to, engage in, and adhere to, a long-term program of regular physical activity primarily in the form of walking. The program uses proven strategies, such as motivational counseling, follow-up phone calls from a nurse, and self-monitoring using pedometers.6-8 Funding for the GWC project was provided by the VHA Office of Geriatrics and Extended Care as part of its Transition to the 21st Century (T21) initiative and by the VHA Office of Rural Health.
Methods
Quality improvement (QI) principles were used to develop the program, which received a nonresearch determination status from the local institutional review board. The GWC is staffed by a registered nurse, health technician, and physician. Both the nurse and the health technician were trained on the use of various assessments. Several tactics were developed to promote patient recruitment to the GWC, including systemwide in-services, an easy-to-use consultation request within the electronic medical record, patient and provider brochures, and informational booths and kiosks. Collaborations were developed with various clinical services to promote referrals. Several other services, such as Primary Care, Geriatrics, the Move! Weight Management Program, Cardiology (including Congestive Heart Failure), Hematology/Oncology, and Mental Health referred patients to the GWC.
The GWC targets sedentary, community-dwelling veterans aged ≥ 60 years who are able to ambulate in their home without an assistive device, are willing to walk for exercise, and are willing to receive phone calls. All-comers are included in the program. Although most of these veterans have multiple chronic medical problems, only those with absolute contraindications to exercise per the American College of Sports Medicine guidelines and those with any medical condition that is likely to compromise their ability to safely participate in the walking program are excluded (Figure).
First Visit
At the first visit, veterans receive a brief education about GWC, highlighting its potential health benefits. If veterans want to join, they are evaluated using a 3-tier screening assessment to determine the safety of starting a new walking regimen. Veterans who fail the 3-tier safety screening are referred to their primary care physician (PCP) for further assessment (eg, cardiac stress testing) to better define eligibility status. Veterans who pass the screen complete brief tests of physical performance, including gait speed, 6-Minute Walk Test (6MWT), Timed Up and Go test, and Berg Balance Scale.9-12 Participants also complete short surveys that provide useful information about their social support, barriers to exercise, response to physical activity, and usual activity level as measured by Community Healthy Activities Model Program for Seniors.13,14 This information is used to help develop an individualized walking prescription.
After completing the baseline assessments, the GWC staff members help the veteran set realistic goals, using motivational counseling techniques. The veteran receives a walking prescription to walk indoors or outdoors, based on current physical condition, self-identified goals, perceived barriers, and strength of support system; educational material about safe walking; a log for recording daily step count; information on follow-up calls; and an invitation to return for follow-up visits. The veteran also receives a pedometer and is instructed to continue his or her usual routine for the first week. The average daily step count is recorded as the baseline. The veteran is instructed to start the walking program after the baseline week with goals tailored to the personal activity level. For example: Some patients are asked to simply add an extra minute to their walking, whereas others savvy with pedometer numbers are asked to increase their step count.
Follow-up
Veterans are followed closely between their clinic appointments via phone calls from a nurse who provides encouragement and helps set new goals. The nurse collects the step count data to determine progress and set new walking goals. Those unable to adhere to their walking prescription are reassessed for their barriers. The nurse also helps participants identify ways to overcome individual challenges. The PCP is consulted when barriers include medical problems, such as pain or poor blood sugar control.
At the 6-week follow-up visit, the health care provider reviews the pedometer log and repeats all outcome assessments, including the physical performance testing and the participant surveys. Veterans receive feedback from these outcome assessments. To assess participant satisfaction, CAVHS GRECC developed a satisfaction questionnaire, which was given to participants.
Results
A total of 249 older veterans participated in the GWC program. The mean age was 67 (±6) years; 92% were male, 60% were white, and 39% were African American. Most participants lived in a rural location (60%) and were obese (69%); consistent with national standards, obesity was defined as a body mass index (BMI) ≥ 30 kg/m2. Several barriers to exercise were endorsed by the veterans. Most commonly endorsed barriers included bad weather, lack of motivation, feeling tired, and fear of pain. Most participants (93%) were actively engaged via regular phone follow-ups visits; 121 (49%) participants returned to the clinic for the 6-week reassessment. Repeat performance testing at the 6-week visit showed a clinically significant average 14% improvement in the 6MWT, 6% improvement in the Timed Up and Go test, and a 27% improvement in gait speed. Of those veterans who were obese, 64% lost weight. On entry into the program, 32 participants (13%) had poorly controlled diabetes mellitus (DM), defined as hemoglobin A1c (HbA1c) ≥ 8. Among this group, HbA1c improved by an average of 1.5% by the 6-week visit. The GWC program may have contributed to the improved glycemic control as a generally accepted frequency of monitoring HbA1c is at least 3 months.
At the 6-week clinic visit, 94% of those surveyed completed a program evaluation. The GWC scored high on satisfaction; over 80% strongly agreed that they were satisfied with the GWC program as a whole, 80% strongly agreed that the program increased their awareness about need for exercise, 82% strongly agreed that the clinician’s advice was applicable to them, and 77% strongly agreed that the program improved their motivation to walk regularly (Table 1).
Program Economics
An analysis of the clinic costs and benefits was performed to determine whether costs could potentially be offset by the savings realized from improved health outcomes of participating veterans. For this simplified analysis, costs of maintaining the GWC were set equal to the costs of the full-time equivalent employee hours, equipment, and educational materials. Based on the authors’ experience, they projected that for each 1,000 older veterans enrolled in the GWC, there is a requirement for 0.5 medical support assistant (GS-6 pay scale), 1.0 registered nurse grade 2 (RN), 1.0 health science specialist (GS-7), and 0.25 physician. At the host facility, the annual personnel costs are estimated at $205,149. The total annual cost of the GWC, including the equipment and educational materials, is estimated at $240,149.
Although full financial return on investment has yet to be determined, the authors estimated potential cost savings resulting if patients enrolled in a GWC achieved and maintained the types of improvements observed in the first cohort of patients. These estimates were based on identified improvements in 3 patient outcome measures cited in the medical literature that are associated with reductions in subsequent health care costs. These measures include gait speed, weight loss, and HbA1c. It is estimated that the cost savings associated with improvement of gait speed by 0.1 m/s (a clinically relevant change) is $1,200 annually.15
On average, patients enrolled in the GWC program improved their gait speed by 0.22 m/s. Cost savings related to gait speed improvement for 1,000 participants could reach $1,200,000. Conservative estimates of cost savings per 1% reduction of HbA1c is $950/year.16 Among those with poorly controlled DM (ie, HbA1c of ≥ 8), average HbA1c declined by 1.5%. Provided that 13% of the patients have poorly controlled DM, the total cost saving for 1,000 participants could be $209,950 annually.
It also is estimated that a 1% weight loss in obese patients is associated with a $256 decrease in subsequent total health care costs.17 In the GWC, the obese participants lost an average of 1.3% of their baseline weight. Assuming that about 60% of all older veterans participating in the clinic program are obese, annual cost savings per 1,000 participants related to weight loss is estimated to be $199,680. After accounting for the costs of operating the clinic, the total cost savings for a GWC with 1,000 enrolled older veterans is estimated to be as much as $1.4 million annually. Such a favorable cost assessment suggests that the program should be evaluated for widespread dissemination throughout the entire VHA system. Other potential benefits associated with GWC participation, such as improved quality of life and greater functional independence, may be of even greater importance to veterans.
Limitations
Results of this QI project need to be considered in light of its limitations. One of the most important limitations is the design of the project. Since this was a clinical initiative and not a research study, there was no control group or randomization. There were also limitations on data availability. HbA1c tests were not ordered as part of this QI project. Instead, baseline HbA1c was set equal to the most recent of any value obtained clinically within 2 months before the participant’s GWC enrollment; the 6-week follow-up value was set to any HbA1c obtained within 2 months after the 6-week visit. It is also recognized that factors other than the veterans’ participation in the GWC (eg, alterations in their DM medication regimen) may have contributed to the changes noted in some participant’s HbA1c. Although not necessarily a limitation, 140 of the 247 participants (57%) were enrolled in MOVE! as well. MOVE! is a widely popular weight management program in the VA focusing on diet control.18 The authors, however, have no information about the veterans’ adherence to MOVE!
Five immediate next steps to disseminate the program have been identified (Table 2).
Conclusion
The GWC was successfully developed and implemented as a QI project at CAVHS and was met with much satisfaction by older veterans. Participants experienced clinically significant improvements in physical performance and other health indicators, suggesting that these benefits could potentially offset clinic costs.
1. Jefferis BJ, Sartini C, Ash S, et al. Trajectories of objectively measured physical activity in free-living older men. Med Sci Sports Exerc. 2015;47(2):343-349.
2. Sun F, Norman IJ, While AE. Physical activity in older people: a systematic review. BMC Public Health. 2013;13:449.
3. Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181-188.
4. Vogel T, Brechat PH, Lepretre PM, Kaltenbach G, Berthel M, Lonsdorfer J. Health benefits of physical activity in older patients: a review. Int J Clin Pract. 2009;63(2):303-320.
5. Patterson PD, Moore CG, Probst JC, Shinogle JA. Obesity and physical inactivity in rural America. J Rural Health. 2004;20(2):151-159.
6. Dubbert PM, Cooper KM, Kirchner KA, Meydrech EF, Bilbrew D. Effects of nurse counseling on walking for exercise in elderly primary care patients. J Gerontol A Biol Sci Med Sci. 2002;57(11):M733-M740.
7. Dubbert PM, Morey MC, Kirchner KA, Meydrech EF, Grothe K. Counseling for home-based walking and strength exercise in older primary care patients. Arch Intern Med. 2008;168(9):979-986.
8. Newton RL Jr, HH M, Dubbert PM, et al. Pedometer determined physical activity tracks in African American adults: the Jackson Heart Study. Int J Behav Nutr Phys Act. 2012;9:44.
9. Bohannon RW. Comfortable and maximum walking speed of adults aged 20-79 years: reference values and determinants. Age Ageing. 1997;26(1):15-19.
10. Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132(8):919-923.
11. Hiengkaew V, Jitaree K, Chaiyawat P. Minimal detectable changes of the Berg Balance Scale, Fugl-Meyer Assessment Scale, Timed “Up & Go” Test, gait speeds, and 2-minute walk test in individuals with chronic stroke with different degrees of ankle plantarflexor tone. Arch Phys Med Rehabil. 2012;93(7):1201-1208.
12. Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449-459.
13. Clark DO, Nothwehr F. Exercise self-efficacy and its correlates among socioeconomically disadvantaged older adults. Health Educ Behav. 1999;26(4):535-546.
14. Stewart AL, Verboncoeur CJ, McLellan BY, et al. Physical activity outcomes of CHAMPS II: a physical activity promotion program for older adults. J Gerontol A Biol Sci Med Sci. 2001;56(8):M465-M470.
15. Purser JL, Weinberger M, Cohen HJ, et al. Walking speed predicts health status and hospital costs for frail elderly male Veterans. J Rehabil Res Dev. 2005;42(4):535-546.
16. Wagner EH, Sandhu N, Newton KM, McCulloch DK, Ramsey SD, Grothaus LC. Effect of improved glycemic control on health care costs and utilization. JAMA. 2001;285(2):182-189.
17. Yu AP, Wu EQ, Birnbaum HG, et al. Short-term economic impact of body weight change among patients with type 2 diabetes treated with antidiabetic agents: analysis using claims, laboratory, and medical record data. Curr Med Res Opin. 2007;23(9):2157-2169.
18. Romanova M, Liang LJ, Deng ML, Li Z, Heber D. Effectiveness of the MOVE! multidisciplinary weight loss program for veterans in Los Angeles. Prev Chronic Dis. 2013;10:E112.
1. Jefferis BJ, Sartini C, Ash S, et al. Trajectories of objectively measured physical activity in free-living older men. Med Sci Sports Exerc. 2015;47(2):343-349.
2. Sun F, Norman IJ, While AE. Physical activity in older people: a systematic review. BMC Public Health. 2013;13:449.
3. Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181-188.
4. Vogel T, Brechat PH, Lepretre PM, Kaltenbach G, Berthel M, Lonsdorfer J. Health benefits of physical activity in older patients: a review. Int J Clin Pract. 2009;63(2):303-320.
5. Patterson PD, Moore CG, Probst JC, Shinogle JA. Obesity and physical inactivity in rural America. J Rural Health. 2004;20(2):151-159.
6. Dubbert PM, Cooper KM, Kirchner KA, Meydrech EF, Bilbrew D. Effects of nurse counseling on walking for exercise in elderly primary care patients. J Gerontol A Biol Sci Med Sci. 2002;57(11):M733-M740.
7. Dubbert PM, Morey MC, Kirchner KA, Meydrech EF, Grothe K. Counseling for home-based walking and strength exercise in older primary care patients. Arch Intern Med. 2008;168(9):979-986.
8. Newton RL Jr, HH M, Dubbert PM, et al. Pedometer determined physical activity tracks in African American adults: the Jackson Heart Study. Int J Behav Nutr Phys Act. 2012;9:44.
9. Bohannon RW. Comfortable and maximum walking speed of adults aged 20-79 years: reference values and determinants. Age Ageing. 1997;26(1):15-19.
10. Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132(8):919-923.
11. Hiengkaew V, Jitaree K, Chaiyawat P. Minimal detectable changes of the Berg Balance Scale, Fugl-Meyer Assessment Scale, Timed “Up & Go” Test, gait speeds, and 2-minute walk test in individuals with chronic stroke with different degrees of ankle plantarflexor tone. Arch Phys Med Rehabil. 2012;93(7):1201-1208.
12. Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449-459.
13. Clark DO, Nothwehr F. Exercise self-efficacy and its correlates among socioeconomically disadvantaged older adults. Health Educ Behav. 1999;26(4):535-546.
14. Stewart AL, Verboncoeur CJ, McLellan BY, et al. Physical activity outcomes of CHAMPS II: a physical activity promotion program for older adults. J Gerontol A Biol Sci Med Sci. 2001;56(8):M465-M470.
15. Purser JL, Weinberger M, Cohen HJ, et al. Walking speed predicts health status and hospital costs for frail elderly male Veterans. J Rehabil Res Dev. 2005;42(4):535-546.
16. Wagner EH, Sandhu N, Newton KM, McCulloch DK, Ramsey SD, Grothaus LC. Effect of improved glycemic control on health care costs and utilization. JAMA. 2001;285(2):182-189.
17. Yu AP, Wu EQ, Birnbaum HG, et al. Short-term economic impact of body weight change among patients with type 2 diabetes treated with antidiabetic agents: analysis using claims, laboratory, and medical record data. Curr Med Res Opin. 2007;23(9):2157-2169.
18. Romanova M, Liang LJ, Deng ML, Li Z, Heber D. Effectiveness of the MOVE! multidisciplinary weight loss program for veterans in Los Angeles. Prev Chronic Dis. 2013;10:E112.