User login
With an increasing demand for mental health services for veterans in rural clinics, telehealth can deliver services to veterans at home or in other nonclinic settings. Telehealth can reduce demands on VA clinic space and staff required for traditional videoconferencing.
Clinic-based telemental health started at the VA in 2003 and has provided access to more than 1 million appointments.1 Despite the great strides in accessibility, logistic barriers limit expansion of clinic-based telehealth appointments. A VA staff member at the patient site must be available to “greet and seat” the veteran; scheduling requires 2 separate appointments (on patient and provider sites); and limited telehealth equipment and clinic space need to be reserved ahead of time.
The first known use of telehealth technologies to deliver mental health services within the VA network information technology system to at-home veterans occurred in 2009 at the VA Portland Health Care System (VAPORHCS) in Oregon. Between 2010 and 2013, the VAPORHCS Home-Based Telemental Health (HBTMH) pilot served about 82 veterans through about 740 appointments. The HBTMH pilot transitioned from a single facility to a regional implementation model under an Office of Innovation Grant Innovation #669: Home-Based Telemental Health (Innovation), which served about 84 veterans from 2013 to 2014.
In 2014, about 4,200 veterans accessed some health care via the national Clinical Video Telehealth–Into the Home (CVT-IH) program, with all 21 VISNs participating (John Peters, e-mail communication, February 2014). In all 3 implementation models (HBTMH pilot, Innovation, and CVT-IH), the veteran can receive health services via videoconferencing in real time, on personal or loaned computers, at home or in another nonclinic setting.
As the VA’s use of telehealth services grows in non-VA settings, technical support remains a significant challenge.2 Increased use of CVT-IH through veterans’ personal computers and devices has generated a corresponding need for technical support. The National Telehealth Technical Help Desk (NTTHD), which supports the national CVT-IH program, does not provide technical support directly to veterans. Instead, recommendations are given to the providers who are expected to transmit and implement the technical solutions with the veterans. Similarly, HBTMH pilot providers were initially responsible for all technical issues for home-based telehealth work, including helping patients with software installation and subsequent troubleshooting.
Providers participating in the HBTMH pilot project encountered veterans with all levels of comfort and skill with the required technology. Some veterans have never used a personal computer, e-mail, and/or webcam. Addressing technical issues often required up to 15 to 20 minutes during an HBTMH pilot session; some cases took hours spread over several days. In VISN 20, providers in Oregon and Washington have reported discontinuation of treatment of veterans enrolled in CVT-IH for technical reasons, including poor connections, lack of timely technical support, and incompatibility of veteran-owned computers with VA-approved third-party software (Anders Goranson, Sara Smucker Barnwell, Kathleen Woodside, e-mail communication, December 2013).
A peer technical consultant (PTC) who directly serves patients and providers may be better positioned to meet the technical needs of everyone involved in a home-based telehealth program. The PTC role was developed for the HBTMH Pilot and expanded during the Innovation program. The authors describe the role of the PTC, outline key responsibilities, and highlight how the PTC can provide effective technical support and improve provider and patient access and engagement with nonclinic-based telehealth services.
Methods
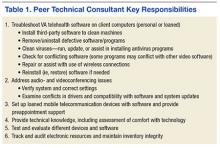
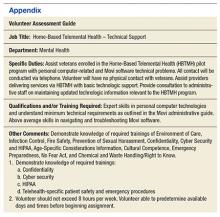
Lessons from the initial phases of the HBTMH pilot strongly suggested that technical barriers had to be reduced. In 2010, a former patient in the HBTMH pilot who had a background in information technology and computer systems and interest in helping other veterans contacted Dr. Peter Shore. They developed the novel role of a PTC, focused on delivering technical support with compassion (Table 1). A functional statement and position description were submitted to volunteer services at the VAPORHCS (Appendix). With the regionwide expansion of the HBTMH pilot into the Innovation program, the PTC was hired as a full-time contract employee to increase the availability of technical support.
The PTC assumed responsibility for installations and troubleshooting for both providers and veterans enrolled in the HBTMH pilot. The PTC, who was based at the VAPORHCS, received referrals, contacted veterans by telephone, addressed technical problems, and reported the result to the provider. No face-to-face contact occurred between the PTC and the veterans. The PTC received regular supervision from the project director. Starting in mid-2012, local providers who were using the national CVT-IH program also requested PTC services. The PTC was able to add technical support for veterans beyond the NTTHD model, allowing for immediate in-session attention in some cases.
For the Innovation program, which loaned devices (netbooks or iPads) and connectivity (mobile broadband Internet access) to veterans who needed them, the role of PTC expanded to become a technology concierge, helping to set up and manage all mobile telecommunication devices. The PTC phoned veterans when they received their device and provided a virtual tour, helped familiarize them with the technology by using test calls, and guided them in the use of relevant mobile applications installed on the device. During treatment, the PTC called enrolled veterans to follow up and to answer additional questions. The PTC also provided assistance to veterans interested in enrolling in the patient online portal My HealtheVet to access health information, communicate with providers, and request medication refills.
The VAPORHCS received institutional review board approval to present HBTMH pilot research data and program evaluation data for Innovation (as a quality improvement project). An initial evaluation of the position was completed through review of PTC workload and productivity, informal feedback from telehealth providers, and veteran and provider surveys during and after treatment.
Results
From March 2010 through April 2012, the PTC logged more than 2,500 hours of volunteer service on behalf of the HBTMH pilot (before the Innovation expansion). The dropout rate due to nonclinical reasons for veterans enrolled in the HBTMH pilot was 11%.3 During the HBTMH pilot, 78% of veterans reported that they had enough technical support (ie, from the volunteer PTC), whereas among veterans receiving clinic-based videoconferencing sessions, 61% reported having adequate technical support (ie, from telehealth clinical technicians employed by the VA).3
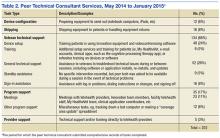
During 2013 to 2014, veterans and providers were surveyed during and after Innovation program treatment. Eighty percent of participants stated that the PTC was prompt in resolving any issues (20% reported “neutral”). One hundred percent of providers indicated that the PTC was able to resolve the technical issues and that they were “very likely” to continue participating in HBTMH if the PTC was involved. Eighty-nine percent of veterans reported they felt there was enough technical support, and 11% responded “neutral” to this question. Table 2 describes typical PTC services provided during the Innovation program.
Informal summary observations from the PTC confirmed that the most frequent interventions were device and software orientation, assessment of audio and/or video disruptions during sessions, and software log-in configuration and support. Common technical issues included audio and video bandwidth limitations and the need to clean up veterans’ personal computers to restore functionality or improve performance (eg, problems due to malware and viruses; e-mail communication, various dates, William Cannon).
Troubleshooting was performed immediately during a session about half the time (vs between sessions) and initiated by veterans about half the time (vs by providers on their behalf) according to informal observations. The average length of a technical support appointment was about 30 minutes for veterans who were comfortable with technology; in contrast, appointments with veterans who were unfamiliar with technology averaged about 90 minutes.
The task logs recorded instances where flexibility and availability were needed for optimal task completion. Although many tasks seemed to be routine, others showed considerable use of the PTC’s time or direct participation during a session.
One PTC noted, “Client called around 9:30 and had me put [provider’s name] info into Jabber. Also Jabber had an issue of being stuck but forced a call and issue cleared up. 15 min. Stayed online with client to ensure appointment connection went well. 5 min.”
Malware, although not the most common issue, seemed to be time consuming. A task that required 4 hours for resolution of multiple issues was described as “requested outside assist due to drivers. Troubleshooting discovered 240 plus malware and numerous Trojan [horses].”
Another time-consuming issue involved software or updates to existing software interfering with the videoconferencing program, with the following example logged for 90 minutes: “Jabber will not store contacts. Updated IOS. Deleted games. Deleted and reinstalled Jabber. Re-updated Jabber. Problem finally resolved” (December 19, 2014). Other patients simply needed more time to familiarize themselves with the technology, as in this example: “2.5 hours of training and using the iPad” (November 25, 2014).
Informal feedback from providers as well as formal feedback from a program audit indicated appreciation for the PTC’s ability to facilitate engagement and surmount technical hurdles. One provider reflected on a particular instance in which the PTC worked with both the veteran and the provider over the phone and webchat to teach them to use the equipment. “[Veteran] and the peer technician developed a friendly rapport and [veteran] expressed gratitude for the team’s efforts to deliver treatment that he would not have had otherwise.” Another provider commented, “The [National] Help Desk is almost too general. You have to explain who you are each time, and never get to explain who [the] veteran is. … They are aware of national problems. Otherwise, they can’t help out much.”
In 2012, the Office of Telehealth Services completed its Conditions of Participation review of all VISN 20 Telehealth programs and in their final report commended the practices of the HBTMH program, highlighting the associated peer-to-peer volunteer program.4
Discussion
The number of technical issues addressed by the PTC demonstrates the versatility and potential impact of this role. In each case, the PTC accommodates the specific needs of the veteran and any factors that might impact their technology use (eg, low cognitive functioning, hyperarousal, slowed processing speed, low frustration tolerance, or paranoia). This model could be expanded within or outside the VA, although due to the limited scope of the evaluation and the unique qualifications of the individual who filled the PTC role, generalizability remains to be established.
By providing direct support, the PTC attempts to meet veterans where they are and helps them become comfortable with the technology so they are not preoccupied with technical problems while receiving health care. In doing so, engagement in telehealth care is enhanced for patients and providers, and dropouts due to technologic problems may be prevented. Initial program evaluation of this role also suggests considerable provider and veteran satisfaction.
The PTC’s interactions help minimize potential frustrations related to technology use for the delivery of mental health care. Frequently, veterans using in-home telehealth have little experience with technology. Moreover, technology use has been found to be lower for rural dwelling adults.5 Other populations (eg, geriatric) may have greater technology challenges and need additional support.6 When patients start CVT services, there is a potential for dropout if there are initial connection problems, particularly among patients who may have low stress tolerance. The PTC can develop an ongoing relationship with veterans who have a history of technologic difficulties and help monitor them.
Technology barriers and limited support are also a documented barrier to provider engagement.7 Given the inherent limitations and reported provider discouragement with the NTTHD model, more directed technical support may enhance provider engagement and efficiency. With the immediate and one-on-one support given by the PTC, this concern has been assertively addressed. In VISN 20 some mental health care providers elected not to use the CVT-IH program technical support system of the and chose instead to work with the Innovation PTC.
Programmatically, the PTC role is consistent with the VA Office of Mental Health Services and the VA Central Office initiative to increase involvement of peer support programs. From a recovery model perspective, the role of the PTC goes beyond technical support in connecting veterans to other veterans who are encouraged to take control of their health care by making self-directed choices. They can experience empowerment through interactions with another veteran who may share some of their experiences. Further investigation into the effects of using a peer technical support system on veterans, providers, and PTCs compared with the existing national VA technical support help desk system might be useful, particularly with regard to rates of initiation of care or dropouts.
Integration of this role should be done in a purposeful and direct manner, defining peer roles and establishing clear policies and practices. Logistically, the transition of the PTC from a volunteer to a contract employee afforded increased credentialing to allow for improved integration with the other HBTMH team members. The PTC was able to effectively coordinate with clinical, support and administrative staff to share information, resolve issues collaboratively, and bridge gaps in technology knowledge.
Conclusion
Between the HBTMH pilot and the Innovation program, the authors have demonstrated the growing need for personalized and attentive technical support for patients enrolled in home-based telehealth services. Under a current call center help desk model, satisfaction and services may be inadequate for some veterans’ needs. The authors contend that the PTC is an effective way to deliver the necessary specialized technical assistance to veterans and providers and encourage further implementation and evaluation of this approach.
There is preliminary evidence suggesting that this support can have a beneficial impact on provider and veteran engagement in telehealth services. The PTC offers much needed support to providers who frequently do not have the time or knowledge to address all the technical issues that arise during telehealth care. Veterans helping veterans is a powerful alternative deserving of national resources and policy change. Although this case developed in a very VA-specific context, peer technical support may be applicable to other organizations as well.
Acknowledgements
Being the first to do anything in the VA takes courage, tenacity, and luck. The following individuals greatly assisted with the HBTMH pilot and the subsequent Innovation: William “Bear” Cannon, David Greaves, Tracy Dekelboum, William Minium, Sean O’Connor, Joe Ronzio, Kit Teague, and Mark Ward. For assistance with data entry and analysis, the authors thank Athalia White. For help with administrative approvals, the authors thank Bradford Felker and Carol Simons.
This article is dedicated to William “Bear” Cannon, who reinvented himself while serving as the PTC and saved his life along the way. His unwavering commitment to serve his fellow veterans is unheralded. May he be the shining light to those who follow him.
1. Darkins A. The growth of telehealth services in the Veterans Health Administration between 1994 and 2014: a study in the diffusion of innovation. Telemed J E Health. 2014;20(9):761-768.
2. Ronzio JL, Tuerk PW, Shore P. Technology and clinical videoconferencing infrastructures: a guide to selecting appropriate system. In: Tuerk PW, Shore P, eds. Clinical Video Teleconferencing: Program Development and Practice. New York, NY: Springer;2015:3-22.
3. Shore P, Goranson A, Ward MF, Lu MW. Meeting veterans where they're @: a VA home-based telemental health (HBTMH) pilot program. Int J Psychiatry Med. 2014;48(1):5-17.
4. U.S. Department of Veterans Affairs, Veterans Health Administration. Telehealth Conditions of Participation: Final Core and Modality-Specific Standards. Washington, DC: Veterans Health Administration; 2014.
5. Calvert JF Jr, Kaye J, Leahy M, Hexem K, Carlson N. Technology use by rural and urban oldest old. Technol Health Care. 2009;17(1):1-11.
6. Kang HG, Mahoney DF, Hoenig H, et al; Center for Integration of Medicine and Innovative Technology Working Group on Advanced Approaches to Physiologic Monitoring for the Aged. In situ monitoring of health in older adults: technologies and issues. J Am Geriatr Soc. 2010;58(8):1579-1586.
7. Brooks E, Turvey C, Augusterfer EF. Provider barriers to telemental health: obstacles overcome, obstacles remain. Telemed J E Health. 2013;19(6):433-437.
With an increasing demand for mental health services for veterans in rural clinics, telehealth can deliver services to veterans at home or in other nonclinic settings. Telehealth can reduce demands on VA clinic space and staff required for traditional videoconferencing.
Clinic-based telemental health started at the VA in 2003 and has provided access to more than 1 million appointments.1 Despite the great strides in accessibility, logistic barriers limit expansion of clinic-based telehealth appointments. A VA staff member at the patient site must be available to “greet and seat” the veteran; scheduling requires 2 separate appointments (on patient and provider sites); and limited telehealth equipment and clinic space need to be reserved ahead of time.
The first known use of telehealth technologies to deliver mental health services within the VA network information technology system to at-home veterans occurred in 2009 at the VA Portland Health Care System (VAPORHCS) in Oregon. Between 2010 and 2013, the VAPORHCS Home-Based Telemental Health (HBTMH) pilot served about 82 veterans through about 740 appointments. The HBTMH pilot transitioned from a single facility to a regional implementation model under an Office of Innovation Grant Innovation #669: Home-Based Telemental Health (Innovation), which served about 84 veterans from 2013 to 2014.
In 2014, about 4,200 veterans accessed some health care via the national Clinical Video Telehealth–Into the Home (CVT-IH) program, with all 21 VISNs participating (John Peters, e-mail communication, February 2014). In all 3 implementation models (HBTMH pilot, Innovation, and CVT-IH), the veteran can receive health services via videoconferencing in real time, on personal or loaned computers, at home or in another nonclinic setting.
As the VA’s use of telehealth services grows in non-VA settings, technical support remains a significant challenge.2 Increased use of CVT-IH through veterans’ personal computers and devices has generated a corresponding need for technical support. The National Telehealth Technical Help Desk (NTTHD), which supports the national CVT-IH program, does not provide technical support directly to veterans. Instead, recommendations are given to the providers who are expected to transmit and implement the technical solutions with the veterans. Similarly, HBTMH pilot providers were initially responsible for all technical issues for home-based telehealth work, including helping patients with software installation and subsequent troubleshooting.
Providers participating in the HBTMH pilot project encountered veterans with all levels of comfort and skill with the required technology. Some veterans have never used a personal computer, e-mail, and/or webcam. Addressing technical issues often required up to 15 to 20 minutes during an HBTMH pilot session; some cases took hours spread over several days. In VISN 20, providers in Oregon and Washington have reported discontinuation of treatment of veterans enrolled in CVT-IH for technical reasons, including poor connections, lack of timely technical support, and incompatibility of veteran-owned computers with VA-approved third-party software (Anders Goranson, Sara Smucker Barnwell, Kathleen Woodside, e-mail communication, December 2013).
A peer technical consultant (PTC) who directly serves patients and providers may be better positioned to meet the technical needs of everyone involved in a home-based telehealth program. The PTC role was developed for the HBTMH Pilot and expanded during the Innovation program. The authors describe the role of the PTC, outline key responsibilities, and highlight how the PTC can provide effective technical support and improve provider and patient access and engagement with nonclinic-based telehealth services.
Methods
Lessons from the initial phases of the HBTMH pilot strongly suggested that technical barriers had to be reduced. In 2010, a former patient in the HBTMH pilot who had a background in information technology and computer systems and interest in helping other veterans contacted Dr. Peter Shore. They developed the novel role of a PTC, focused on delivering technical support with compassion (Table 1). A functional statement and position description were submitted to volunteer services at the VAPORHCS (Appendix). With the regionwide expansion of the HBTMH pilot into the Innovation program, the PTC was hired as a full-time contract employee to increase the availability of technical support.
The PTC assumed responsibility for installations and troubleshooting for both providers and veterans enrolled in the HBTMH pilot. The PTC, who was based at the VAPORHCS, received referrals, contacted veterans by telephone, addressed technical problems, and reported the result to the provider. No face-to-face contact occurred between the PTC and the veterans. The PTC received regular supervision from the project director. Starting in mid-2012, local providers who were using the national CVT-IH program also requested PTC services. The PTC was able to add technical support for veterans beyond the NTTHD model, allowing for immediate in-session attention in some cases.
For the Innovation program, which loaned devices (netbooks or iPads) and connectivity (mobile broadband Internet access) to veterans who needed them, the role of PTC expanded to become a technology concierge, helping to set up and manage all mobile telecommunication devices. The PTC phoned veterans when they received their device and provided a virtual tour, helped familiarize them with the technology by using test calls, and guided them in the use of relevant mobile applications installed on the device. During treatment, the PTC called enrolled veterans to follow up and to answer additional questions. The PTC also provided assistance to veterans interested in enrolling in the patient online portal My HealtheVet to access health information, communicate with providers, and request medication refills.
The VAPORHCS received institutional review board approval to present HBTMH pilot research data and program evaluation data for Innovation (as a quality improvement project). An initial evaluation of the position was completed through review of PTC workload and productivity, informal feedback from telehealth providers, and veteran and provider surveys during and after treatment.
Results
From March 2010 through April 2012, the PTC logged more than 2,500 hours of volunteer service on behalf of the HBTMH pilot (before the Innovation expansion). The dropout rate due to nonclinical reasons for veterans enrolled in the HBTMH pilot was 11%.3 During the HBTMH pilot, 78% of veterans reported that they had enough technical support (ie, from the volunteer PTC), whereas among veterans receiving clinic-based videoconferencing sessions, 61% reported having adequate technical support (ie, from telehealth clinical technicians employed by the VA).3
During 2013 to 2014, veterans and providers were surveyed during and after Innovation program treatment. Eighty percent of participants stated that the PTC was prompt in resolving any issues (20% reported “neutral”). One hundred percent of providers indicated that the PTC was able to resolve the technical issues and that they were “very likely” to continue participating in HBTMH if the PTC was involved. Eighty-nine percent of veterans reported they felt there was enough technical support, and 11% responded “neutral” to this question. Table 2 describes typical PTC services provided during the Innovation program.
Informal summary observations from the PTC confirmed that the most frequent interventions were device and software orientation, assessment of audio and/or video disruptions during sessions, and software log-in configuration and support. Common technical issues included audio and video bandwidth limitations and the need to clean up veterans’ personal computers to restore functionality or improve performance (eg, problems due to malware and viruses; e-mail communication, various dates, William Cannon).
Troubleshooting was performed immediately during a session about half the time (vs between sessions) and initiated by veterans about half the time (vs by providers on their behalf) according to informal observations. The average length of a technical support appointment was about 30 minutes for veterans who were comfortable with technology; in contrast, appointments with veterans who were unfamiliar with technology averaged about 90 minutes.
The task logs recorded instances where flexibility and availability were needed for optimal task completion. Although many tasks seemed to be routine, others showed considerable use of the PTC’s time or direct participation during a session.
One PTC noted, “Client called around 9:30 and had me put [provider’s name] info into Jabber. Also Jabber had an issue of being stuck but forced a call and issue cleared up. 15 min. Stayed online with client to ensure appointment connection went well. 5 min.”
Malware, although not the most common issue, seemed to be time consuming. A task that required 4 hours for resolution of multiple issues was described as “requested outside assist due to drivers. Troubleshooting discovered 240 plus malware and numerous Trojan [horses].”
Another time-consuming issue involved software or updates to existing software interfering with the videoconferencing program, with the following example logged for 90 minutes: “Jabber will not store contacts. Updated IOS. Deleted games. Deleted and reinstalled Jabber. Re-updated Jabber. Problem finally resolved” (December 19, 2014). Other patients simply needed more time to familiarize themselves with the technology, as in this example: “2.5 hours of training and using the iPad” (November 25, 2014).
Informal feedback from providers as well as formal feedback from a program audit indicated appreciation for the PTC’s ability to facilitate engagement and surmount technical hurdles. One provider reflected on a particular instance in which the PTC worked with both the veteran and the provider over the phone and webchat to teach them to use the equipment. “[Veteran] and the peer technician developed a friendly rapport and [veteran] expressed gratitude for the team’s efforts to deliver treatment that he would not have had otherwise.” Another provider commented, “The [National] Help Desk is almost too general. You have to explain who you are each time, and never get to explain who [the] veteran is. … They are aware of national problems. Otherwise, they can’t help out much.”
In 2012, the Office of Telehealth Services completed its Conditions of Participation review of all VISN 20 Telehealth programs and in their final report commended the practices of the HBTMH program, highlighting the associated peer-to-peer volunteer program.4
Discussion
The number of technical issues addressed by the PTC demonstrates the versatility and potential impact of this role. In each case, the PTC accommodates the specific needs of the veteran and any factors that might impact their technology use (eg, low cognitive functioning, hyperarousal, slowed processing speed, low frustration tolerance, or paranoia). This model could be expanded within or outside the VA, although due to the limited scope of the evaluation and the unique qualifications of the individual who filled the PTC role, generalizability remains to be established.
By providing direct support, the PTC attempts to meet veterans where they are and helps them become comfortable with the technology so they are not preoccupied with technical problems while receiving health care. In doing so, engagement in telehealth care is enhanced for patients and providers, and dropouts due to technologic problems may be prevented. Initial program evaluation of this role also suggests considerable provider and veteran satisfaction.
The PTC’s interactions help minimize potential frustrations related to technology use for the delivery of mental health care. Frequently, veterans using in-home telehealth have little experience with technology. Moreover, technology use has been found to be lower for rural dwelling adults.5 Other populations (eg, geriatric) may have greater technology challenges and need additional support.6 When patients start CVT services, there is a potential for dropout if there are initial connection problems, particularly among patients who may have low stress tolerance. The PTC can develop an ongoing relationship with veterans who have a history of technologic difficulties and help monitor them.
Technology barriers and limited support are also a documented barrier to provider engagement.7 Given the inherent limitations and reported provider discouragement with the NTTHD model, more directed technical support may enhance provider engagement and efficiency. With the immediate and one-on-one support given by the PTC, this concern has been assertively addressed. In VISN 20 some mental health care providers elected not to use the CVT-IH program technical support system of the and chose instead to work with the Innovation PTC.
Programmatically, the PTC role is consistent with the VA Office of Mental Health Services and the VA Central Office initiative to increase involvement of peer support programs. From a recovery model perspective, the role of the PTC goes beyond technical support in connecting veterans to other veterans who are encouraged to take control of their health care by making self-directed choices. They can experience empowerment through interactions with another veteran who may share some of their experiences. Further investigation into the effects of using a peer technical support system on veterans, providers, and PTCs compared with the existing national VA technical support help desk system might be useful, particularly with regard to rates of initiation of care or dropouts.
Integration of this role should be done in a purposeful and direct manner, defining peer roles and establishing clear policies and practices. Logistically, the transition of the PTC from a volunteer to a contract employee afforded increased credentialing to allow for improved integration with the other HBTMH team members. The PTC was able to effectively coordinate with clinical, support and administrative staff to share information, resolve issues collaboratively, and bridge gaps in technology knowledge.
Conclusion
Between the HBTMH pilot and the Innovation program, the authors have demonstrated the growing need for personalized and attentive technical support for patients enrolled in home-based telehealth services. Under a current call center help desk model, satisfaction and services may be inadequate for some veterans’ needs. The authors contend that the PTC is an effective way to deliver the necessary specialized technical assistance to veterans and providers and encourage further implementation and evaluation of this approach.
There is preliminary evidence suggesting that this support can have a beneficial impact on provider and veteran engagement in telehealth services. The PTC offers much needed support to providers who frequently do not have the time or knowledge to address all the technical issues that arise during telehealth care. Veterans helping veterans is a powerful alternative deserving of national resources and policy change. Although this case developed in a very VA-specific context, peer technical support may be applicable to other organizations as well.
Acknowledgements
Being the first to do anything in the VA takes courage, tenacity, and luck. The following individuals greatly assisted with the HBTMH pilot and the subsequent Innovation: William “Bear” Cannon, David Greaves, Tracy Dekelboum, William Minium, Sean O’Connor, Joe Ronzio, Kit Teague, and Mark Ward. For assistance with data entry and analysis, the authors thank Athalia White. For help with administrative approvals, the authors thank Bradford Felker and Carol Simons.
This article is dedicated to William “Bear” Cannon, who reinvented himself while serving as the PTC and saved his life along the way. His unwavering commitment to serve his fellow veterans is unheralded. May he be the shining light to those who follow him.
With an increasing demand for mental health services for veterans in rural clinics, telehealth can deliver services to veterans at home or in other nonclinic settings. Telehealth can reduce demands on VA clinic space and staff required for traditional videoconferencing.
Clinic-based telemental health started at the VA in 2003 and has provided access to more than 1 million appointments.1 Despite the great strides in accessibility, logistic barriers limit expansion of clinic-based telehealth appointments. A VA staff member at the patient site must be available to “greet and seat” the veteran; scheduling requires 2 separate appointments (on patient and provider sites); and limited telehealth equipment and clinic space need to be reserved ahead of time.
The first known use of telehealth technologies to deliver mental health services within the VA network information technology system to at-home veterans occurred in 2009 at the VA Portland Health Care System (VAPORHCS) in Oregon. Between 2010 and 2013, the VAPORHCS Home-Based Telemental Health (HBTMH) pilot served about 82 veterans through about 740 appointments. The HBTMH pilot transitioned from a single facility to a regional implementation model under an Office of Innovation Grant Innovation #669: Home-Based Telemental Health (Innovation), which served about 84 veterans from 2013 to 2014.
In 2014, about 4,200 veterans accessed some health care via the national Clinical Video Telehealth–Into the Home (CVT-IH) program, with all 21 VISNs participating (John Peters, e-mail communication, February 2014). In all 3 implementation models (HBTMH pilot, Innovation, and CVT-IH), the veteran can receive health services via videoconferencing in real time, on personal or loaned computers, at home or in another nonclinic setting.
As the VA’s use of telehealth services grows in non-VA settings, technical support remains a significant challenge.2 Increased use of CVT-IH through veterans’ personal computers and devices has generated a corresponding need for technical support. The National Telehealth Technical Help Desk (NTTHD), which supports the national CVT-IH program, does not provide technical support directly to veterans. Instead, recommendations are given to the providers who are expected to transmit and implement the technical solutions with the veterans. Similarly, HBTMH pilot providers were initially responsible for all technical issues for home-based telehealth work, including helping patients with software installation and subsequent troubleshooting.
Providers participating in the HBTMH pilot project encountered veterans with all levels of comfort and skill with the required technology. Some veterans have never used a personal computer, e-mail, and/or webcam. Addressing technical issues often required up to 15 to 20 minutes during an HBTMH pilot session; some cases took hours spread over several days. In VISN 20, providers in Oregon and Washington have reported discontinuation of treatment of veterans enrolled in CVT-IH for technical reasons, including poor connections, lack of timely technical support, and incompatibility of veteran-owned computers with VA-approved third-party software (Anders Goranson, Sara Smucker Barnwell, Kathleen Woodside, e-mail communication, December 2013).
A peer technical consultant (PTC) who directly serves patients and providers may be better positioned to meet the technical needs of everyone involved in a home-based telehealth program. The PTC role was developed for the HBTMH Pilot and expanded during the Innovation program. The authors describe the role of the PTC, outline key responsibilities, and highlight how the PTC can provide effective technical support and improve provider and patient access and engagement with nonclinic-based telehealth services.
Methods
Lessons from the initial phases of the HBTMH pilot strongly suggested that technical barriers had to be reduced. In 2010, a former patient in the HBTMH pilot who had a background in information technology and computer systems and interest in helping other veterans contacted Dr. Peter Shore. They developed the novel role of a PTC, focused on delivering technical support with compassion (Table 1). A functional statement and position description were submitted to volunteer services at the VAPORHCS (Appendix). With the regionwide expansion of the HBTMH pilot into the Innovation program, the PTC was hired as a full-time contract employee to increase the availability of technical support.
The PTC assumed responsibility for installations and troubleshooting for both providers and veterans enrolled in the HBTMH pilot. The PTC, who was based at the VAPORHCS, received referrals, contacted veterans by telephone, addressed technical problems, and reported the result to the provider. No face-to-face contact occurred between the PTC and the veterans. The PTC received regular supervision from the project director. Starting in mid-2012, local providers who were using the national CVT-IH program also requested PTC services. The PTC was able to add technical support for veterans beyond the NTTHD model, allowing for immediate in-session attention in some cases.
For the Innovation program, which loaned devices (netbooks or iPads) and connectivity (mobile broadband Internet access) to veterans who needed them, the role of PTC expanded to become a technology concierge, helping to set up and manage all mobile telecommunication devices. The PTC phoned veterans when they received their device and provided a virtual tour, helped familiarize them with the technology by using test calls, and guided them in the use of relevant mobile applications installed on the device. During treatment, the PTC called enrolled veterans to follow up and to answer additional questions. The PTC also provided assistance to veterans interested in enrolling in the patient online portal My HealtheVet to access health information, communicate with providers, and request medication refills.
The VAPORHCS received institutional review board approval to present HBTMH pilot research data and program evaluation data for Innovation (as a quality improvement project). An initial evaluation of the position was completed through review of PTC workload and productivity, informal feedback from telehealth providers, and veteran and provider surveys during and after treatment.
Results
From March 2010 through April 2012, the PTC logged more than 2,500 hours of volunteer service on behalf of the HBTMH pilot (before the Innovation expansion). The dropout rate due to nonclinical reasons for veterans enrolled in the HBTMH pilot was 11%.3 During the HBTMH pilot, 78% of veterans reported that they had enough technical support (ie, from the volunteer PTC), whereas among veterans receiving clinic-based videoconferencing sessions, 61% reported having adequate technical support (ie, from telehealth clinical technicians employed by the VA).3
During 2013 to 2014, veterans and providers were surveyed during and after Innovation program treatment. Eighty percent of participants stated that the PTC was prompt in resolving any issues (20% reported “neutral”). One hundred percent of providers indicated that the PTC was able to resolve the technical issues and that they were “very likely” to continue participating in HBTMH if the PTC was involved. Eighty-nine percent of veterans reported they felt there was enough technical support, and 11% responded “neutral” to this question. Table 2 describes typical PTC services provided during the Innovation program.
Informal summary observations from the PTC confirmed that the most frequent interventions were device and software orientation, assessment of audio and/or video disruptions during sessions, and software log-in configuration and support. Common technical issues included audio and video bandwidth limitations and the need to clean up veterans’ personal computers to restore functionality or improve performance (eg, problems due to malware and viruses; e-mail communication, various dates, William Cannon).
Troubleshooting was performed immediately during a session about half the time (vs between sessions) and initiated by veterans about half the time (vs by providers on their behalf) according to informal observations. The average length of a technical support appointment was about 30 minutes for veterans who were comfortable with technology; in contrast, appointments with veterans who were unfamiliar with technology averaged about 90 minutes.
The task logs recorded instances where flexibility and availability were needed for optimal task completion. Although many tasks seemed to be routine, others showed considerable use of the PTC’s time or direct participation during a session.
One PTC noted, “Client called around 9:30 and had me put [provider’s name] info into Jabber. Also Jabber had an issue of being stuck but forced a call and issue cleared up. 15 min. Stayed online with client to ensure appointment connection went well. 5 min.”
Malware, although not the most common issue, seemed to be time consuming. A task that required 4 hours for resolution of multiple issues was described as “requested outside assist due to drivers. Troubleshooting discovered 240 plus malware and numerous Trojan [horses].”
Another time-consuming issue involved software or updates to existing software interfering with the videoconferencing program, with the following example logged for 90 minutes: “Jabber will not store contacts. Updated IOS. Deleted games. Deleted and reinstalled Jabber. Re-updated Jabber. Problem finally resolved” (December 19, 2014). Other patients simply needed more time to familiarize themselves with the technology, as in this example: “2.5 hours of training and using the iPad” (November 25, 2014).
Informal feedback from providers as well as formal feedback from a program audit indicated appreciation for the PTC’s ability to facilitate engagement and surmount technical hurdles. One provider reflected on a particular instance in which the PTC worked with both the veteran and the provider over the phone and webchat to teach them to use the equipment. “[Veteran] and the peer technician developed a friendly rapport and [veteran] expressed gratitude for the team’s efforts to deliver treatment that he would not have had otherwise.” Another provider commented, “The [National] Help Desk is almost too general. You have to explain who you are each time, and never get to explain who [the] veteran is. … They are aware of national problems. Otherwise, they can’t help out much.”
In 2012, the Office of Telehealth Services completed its Conditions of Participation review of all VISN 20 Telehealth programs and in their final report commended the practices of the HBTMH program, highlighting the associated peer-to-peer volunteer program.4
Discussion
The number of technical issues addressed by the PTC demonstrates the versatility and potential impact of this role. In each case, the PTC accommodates the specific needs of the veteran and any factors that might impact their technology use (eg, low cognitive functioning, hyperarousal, slowed processing speed, low frustration tolerance, or paranoia). This model could be expanded within or outside the VA, although due to the limited scope of the evaluation and the unique qualifications of the individual who filled the PTC role, generalizability remains to be established.
By providing direct support, the PTC attempts to meet veterans where they are and helps them become comfortable with the technology so they are not preoccupied with technical problems while receiving health care. In doing so, engagement in telehealth care is enhanced for patients and providers, and dropouts due to technologic problems may be prevented. Initial program evaluation of this role also suggests considerable provider and veteran satisfaction.
The PTC’s interactions help minimize potential frustrations related to technology use for the delivery of mental health care. Frequently, veterans using in-home telehealth have little experience with technology. Moreover, technology use has been found to be lower for rural dwelling adults.5 Other populations (eg, geriatric) may have greater technology challenges and need additional support.6 When patients start CVT services, there is a potential for dropout if there are initial connection problems, particularly among patients who may have low stress tolerance. The PTC can develop an ongoing relationship with veterans who have a history of technologic difficulties and help monitor them.
Technology barriers and limited support are also a documented barrier to provider engagement.7 Given the inherent limitations and reported provider discouragement with the NTTHD model, more directed technical support may enhance provider engagement and efficiency. With the immediate and one-on-one support given by the PTC, this concern has been assertively addressed. In VISN 20 some mental health care providers elected not to use the CVT-IH program technical support system of the and chose instead to work with the Innovation PTC.
Programmatically, the PTC role is consistent with the VA Office of Mental Health Services and the VA Central Office initiative to increase involvement of peer support programs. From a recovery model perspective, the role of the PTC goes beyond technical support in connecting veterans to other veterans who are encouraged to take control of their health care by making self-directed choices. They can experience empowerment through interactions with another veteran who may share some of their experiences. Further investigation into the effects of using a peer technical support system on veterans, providers, and PTCs compared with the existing national VA technical support help desk system might be useful, particularly with regard to rates of initiation of care or dropouts.
Integration of this role should be done in a purposeful and direct manner, defining peer roles and establishing clear policies and practices. Logistically, the transition of the PTC from a volunteer to a contract employee afforded increased credentialing to allow for improved integration with the other HBTMH team members. The PTC was able to effectively coordinate with clinical, support and administrative staff to share information, resolve issues collaboratively, and bridge gaps in technology knowledge.
Conclusion
Between the HBTMH pilot and the Innovation program, the authors have demonstrated the growing need for personalized and attentive technical support for patients enrolled in home-based telehealth services. Under a current call center help desk model, satisfaction and services may be inadequate for some veterans’ needs. The authors contend that the PTC is an effective way to deliver the necessary specialized technical assistance to veterans and providers and encourage further implementation and evaluation of this approach.
There is preliminary evidence suggesting that this support can have a beneficial impact on provider and veteran engagement in telehealth services. The PTC offers much needed support to providers who frequently do not have the time or knowledge to address all the technical issues that arise during telehealth care. Veterans helping veterans is a powerful alternative deserving of national resources and policy change. Although this case developed in a very VA-specific context, peer technical support may be applicable to other organizations as well.
Acknowledgements
Being the first to do anything in the VA takes courage, tenacity, and luck. The following individuals greatly assisted with the HBTMH pilot and the subsequent Innovation: William “Bear” Cannon, David Greaves, Tracy Dekelboum, William Minium, Sean O’Connor, Joe Ronzio, Kit Teague, and Mark Ward. For assistance with data entry and analysis, the authors thank Athalia White. For help with administrative approvals, the authors thank Bradford Felker and Carol Simons.
This article is dedicated to William “Bear” Cannon, who reinvented himself while serving as the PTC and saved his life along the way. His unwavering commitment to serve his fellow veterans is unheralded. May he be the shining light to those who follow him.
1. Darkins A. The growth of telehealth services in the Veterans Health Administration between 1994 and 2014: a study in the diffusion of innovation. Telemed J E Health. 2014;20(9):761-768.
2. Ronzio JL, Tuerk PW, Shore P. Technology and clinical videoconferencing infrastructures: a guide to selecting appropriate system. In: Tuerk PW, Shore P, eds. Clinical Video Teleconferencing: Program Development and Practice. New York, NY: Springer;2015:3-22.
3. Shore P, Goranson A, Ward MF, Lu MW. Meeting veterans where they're @: a VA home-based telemental health (HBTMH) pilot program. Int J Psychiatry Med. 2014;48(1):5-17.
4. U.S. Department of Veterans Affairs, Veterans Health Administration. Telehealth Conditions of Participation: Final Core and Modality-Specific Standards. Washington, DC: Veterans Health Administration; 2014.
5. Calvert JF Jr, Kaye J, Leahy M, Hexem K, Carlson N. Technology use by rural and urban oldest old. Technol Health Care. 2009;17(1):1-11.
6. Kang HG, Mahoney DF, Hoenig H, et al; Center for Integration of Medicine and Innovative Technology Working Group on Advanced Approaches to Physiologic Monitoring for the Aged. In situ monitoring of health in older adults: technologies and issues. J Am Geriatr Soc. 2010;58(8):1579-1586.
7. Brooks E, Turvey C, Augusterfer EF. Provider barriers to telemental health: obstacles overcome, obstacles remain. Telemed J E Health. 2013;19(6):433-437.
1. Darkins A. The growth of telehealth services in the Veterans Health Administration between 1994 and 2014: a study in the diffusion of innovation. Telemed J E Health. 2014;20(9):761-768.
2. Ronzio JL, Tuerk PW, Shore P. Technology and clinical videoconferencing infrastructures: a guide to selecting appropriate system. In: Tuerk PW, Shore P, eds. Clinical Video Teleconferencing: Program Development and Practice. New York, NY: Springer;2015:3-22.
3. Shore P, Goranson A, Ward MF, Lu MW. Meeting veterans where they're @: a VA home-based telemental health (HBTMH) pilot program. Int J Psychiatry Med. 2014;48(1):5-17.
4. U.S. Department of Veterans Affairs, Veterans Health Administration. Telehealth Conditions of Participation: Final Core and Modality-Specific Standards. Washington, DC: Veterans Health Administration; 2014.
5. Calvert JF Jr, Kaye J, Leahy M, Hexem K, Carlson N. Technology use by rural and urban oldest old. Technol Health Care. 2009;17(1):1-11.
6. Kang HG, Mahoney DF, Hoenig H, et al; Center for Integration of Medicine and Innovative Technology Working Group on Advanced Approaches to Physiologic Monitoring for the Aged. In situ monitoring of health in older adults: technologies and issues. J Am Geriatr Soc. 2010;58(8):1579-1586.
7. Brooks E, Turvey C, Augusterfer EF. Provider barriers to telemental health: obstacles overcome, obstacles remain. Telemed J E Health. 2013;19(6):433-437.