User login
PACT ICU Model: Interprofessional Case Conferences for High-Risk/High-Need Patients
Physician, nurse practitioner trainees, medical center faculty, and clinic staff develop proactive, team-based, interprofessional care plans to address unmet chronic care needs for high-risk patients.
This article is part of a series that illustrates strategies intended to redesign primary care education at the Veterans Health Administration (VHA), using interprofessional workplace learning. All have been implemented in the VA Centers of Excellence in Primary Care Education (CoEPCE). These models embody visionary transformation of clinical and educational environments that have potential for replication and dissemination throughout VA and other primary care clinical educational environments. For an introduction to the series see Klink K. Transforming primary care clinical learning environments to optimize education, outcomes, and satisfaction. Fed Pract. 2018;35(9):8-10.
Background
In 2011, 5 US Department of Veterans Affairs (VA) medical centers (VAMCs) were selected by the Office of Academic Affiliations (OAA) to establish CoEPCE. Part of the VA New Models of Care initiative, the 5 Centers of Excellence (CoE) in Boise, Idaho; Cleveland, Ohio; San Francisco, California; Seattle, Washington; and West Haven, Connecticut, are utilizing VA primary care settings to develop and test innovative approaches to prepare physician residents and students, advanced practice nurse residents and undergraduate nursing students, and other professions of health trainees (eg, pharmacy, social work, psychology, physician assistants [PAs]) for primary care practice in the 21st century.
The Boise CoE developed and implemented a practice-based learning model. Nurse practitioner (NP) students and residents, physician residents, pharmacy residents, psychology interns, and psychology postdoctoral fellows participate in a comprehensive curriculum and practice together for 1 to 3 years. The goal is to produce providers who are able to lead and practice health care in patient-centered primary care and rural care environments. All core curricula are interprofessionally coauthored and cotaught.1
Methods
In 2015, OAA evaluators reviewed background documents and conducted open-ended interviews with 10 CoE staff, participating trainees, VA faculty, VA facility leadership, and affiliate faculty. In response to questions focused on their experiences, informants described lessons learned, challenges encountered, and benefits for participants, veterans, and the VA. Using a qualitative and quantitative approach, this case study draws on those interviews, surveys of PACT ICU (patient aligned care team interprofessional care update) participants, and analysis of presented patients to examine PACT ICU outcomes.
Interprofessional Education and Care
A key CoEPCE aim is to create more clinical opportunities for CoE trainees from a variety of professions to work as a team in ways that anticipate and address the care needs of veterans. This emphasis on workplace learning is needed since most current health care professional education programs lack settings where trainees from different professions can learn and work together with their clinic partners to provide care for patients. With the emphasis on patient-centered medical homes (PCMH) and team-based care in the Affordable Care Act, there is an imperative to develop new training models that address this gap in the preparation of future health professionals. Along with this imperative, clinicians are increasingly required to optimize the health of complex patients who consequently require a multidisciplinary approach to care, particularly high-risk, high-needs patients inappropriately using services, such as frequent emergency department (ED) use.
Addressing Complex Needs
In 2010, the Boise VA Medical Center (VAMC) phased in patient aligned care teams (PACTs), the VA-mandated version of PCMH that consist of a physician or NP primary care provider (PCP), a registered nurse (RN) care manager, a licensed vocational nurse (LVN), and a medical support assistant (MSA).
The PACT ICU also serves as a venue in which trainees and supervisors from different professions use a patient-centered framework to collaborate on these specific patient cases. The PACT ICU is easily applied to a range of health conditions, such as diabetes mellitus (DM), mental and behavioral health, lack of social support, and delivery system issues, such as ED use. The goals of PACT ICU are to improve the quality and satisfaction of patient care for high-risk patients; encourage appropriate use of health care resources by prioritizing continuity with the PACT team; and enhance interprofessional PACT team function, decreasing PCP and staff stress.
Planning and Implementation
In January 2013, Boise VAMC and the Caldwell, Idaho community-based outpatient clinic (CBOC) implemented PACT ICU. Other nonteaching clinics followed later in the year. Planning and executing PACT ICU took about 10 hours of CoE staff time and required no change in Boise VAMC policy. Program leadership approval was necessary for participation of CoE residents and postdocs. Service-line leadership support was required to protect clinic staff time (nurse care manager, social workers, chaplaincy, and ethics service). At the Caldwell CBOC, the section chief approved the program, and it took about 1 month to initiate a similar version of PACT ICU.
Curriculum
PACT ICU is a workplace clinical activity with roots in the case conference model, specifically the EFECT model (Elicit the narrative of illness, Facilitate a group meeting, Evidence-based gap analysis, Care plan, and Track changes).3 PACT ICU emphasizes a patient-centered approach to developing care plans. Staff review the 5 highest risk patients who are identified by the VA Care Assessment Need (CAN) registry. The CAN is an analytic tool that is available throughout VA and estimates patients’ risk of mortality or hospitalization in the following 90 days. Physician and NP residents choose 1 of the 5 patients to discuss in PACT ICU, while the remaining 4 serve as case-control comparisons to examine long-term patient outcomes. All trainees, faculty, and staff are provided patient data that can be discussed on a secure website.
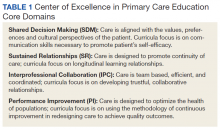
The PACT ICU combines didactic teaching with workplace learning. For example, the patient’s medical issues may lead to a formal presentation about a topic, such as secondary stroke medication prophylaxis. The workplace learning occurs as the trainees observe and participate in the decision making toward a treatment plan. Interprofessional interactions are role-modeled by clinical faculty and staff during these discussions, and the result impact the patients care. PACT ICU embodies the core domains that shape the CoEPCE curriculum: Interprofessional collaboration (IPC), performance improvement (PI), sustained relationships (SR), and shared decision making (SDM) (Table 1).
There have been some changes to the PACT ICU model over time. Initially, conferences took place on a weekly basis, to build momentum among the team and to normalize processes. After about 2 years, this decreased to every other week to reduce the time burden. Additionally, the CoE has strengthened the “tracking changes” component of the EFECT model—trainees now present a 5-minute update on the last patient they presented at the prior PACT ICU case conference. Most recently, psychology postdoctoral candidates have instituted preconference calls with patients to further improve the teams understanding of the patients’ perspective and narrative.
Related: Improving Team-Based Care Coordination Delivery and Documentation in the Health Record
Resources
The CoE faculty participate in an education program concerning facilitation of interprofessional meetings. All faculty are expected to role model collaborative behavior and mentor trainees on the cases they present.
The PACT ICU requires a room large enough to accommodate at least 12 people. One staff member is required to review patient cases prior to the case conferences (usually about 1 hour of preparation per case conference). Another staff person creates and shares a spreadsheet stored with VA-approved information security with data fields to include the site, PACT ICU date, patient identifier, the CAN score, and a checkbox for whether the patient was selected or part of a control group. Logistic support is required for reserving the room and sending information to presenters. A clinic-based RN with training in interprofessional care case management uses an online schedule to facilitate selection and review of patients. The RN care managers can use a secure management tool to track patient care and outreach.
The RN care manager also needs to be available to attend the PACT ICU case conferences. The Boise CoE built a website to share and standardize resources, such as a presenter schedule, PACT ICU worksheet, and provider questionnaire. (Contact Boise CoE staff for access.) For the initial evaluation of impact, PACT ICU utilized staff data support in the form of a data manager and biostatistician to identify, collect, and analyze data. While optional, this was helpful in refining the approach and demonstrating the impact of the project. Other resource-related requirements for exporting PACT ICU include:
- Staff members, usually RN care managers who coordinate meetings with participants and identify appropriate patients using a registry, such as CAN;
- Meeting facilitators who enforce use of the EFECT model and interprofessional participation to ensure that the interprofessional care plan is carried out by the presenting provider; and
- Interprofessional trainees and faculty who participate in PACT ICU and complete surveys after the first conference.
Monitoring and Assessment
The CoE staff have analyzed the evaluation of PACT ICU with participant self-evaluation, consultation referral patterns, and utilization data, combination of ED and episodic care visits along with hospitalizations).4 Pharmacy faculty are exploring the use polypharmacy registries, and psychology will use registries of poor psychosocial function.
Partnerships
Beyond support and engagement from VA CoEPCE and affiliate faculty, PACT ICU has greatly benefited from partnerships with VA facility department and CBOC leadership. The CoEPCE codirector and faculty are in facility committees, such as the PACT Strategic Planning Committee.
Academic affiliates are integral partners who assist with NP student and resident recruitment as well as participate in the planning and refinement of CoEPCE components. PACT ICU supports their mandate to encourage interprofessional teamwork. Faculty members from Gonzaga University (NP affiliate) were involved in the initial discussion on PACT ICU and consider it a “learning laboratory” to work through challenging problems. Gonzaga CoEPCE NP trainees are asked to talk about their PACT ICU experience—its strengths, weaknesses, and challenges—to other Gonzaga students who don’t have exposure to the team experience.
Challenges and Solutions
The demand for direct patient care puts pressure on indirect patient care approaches like PACT ICU, which is a time-intensive process with high impact on only a small number of patients. The argument for deploying strategies such as PACT ICU is that managing chronic conditions and encouraging appropriate use of services will improve outcomes for the highest risk patients and save important system resources in the long-run. However, in the short-term, a strong case must be made for the diversion of resources from usual clinic flow, particularly securing recurring blocks of provider time and clinic staff members. In addition, issues about team communication and understanding of appropriate team-based care can overflow to complex patients not presented in the PACT ICU conference.
Providing a facilitated interprofessional venue to discuss how to appropriately coordinate care improves the participation and perceived value of different team members. This approach has led to improved engagement of the team for patients discussed in the PACT ICU, as well as in general care within the participating clinic. With recent changes, the VA does see a workload benefit, and participants get encounter credit through “Non face-to-face prolonged service” codes (CPT 99358/99359), and other possibilities exist related to clinical team conference codes (CPT 99367-8) and complex chronic care management codes (CPT 99487-89). More information on documentation, scheduling and encountering/billing can be found at boisevacoe.org under Products. Other challenges include logistic challenges of finding appropriate patients and distributing sensitive patient information among the team. Additionally, PACT ICU has to wrestle with staffing shortages and episodic participation by some professions that are chronically understaffed. We have addressed many of these problems by receiving buy-in from both leadership and participants. Leadership have allowed time for participation in clinic staff schedules, and each participant has committed to recruiting a substitute in case of a schedule conflict.
Factors for Success
The commitment from the Boise VAMC facility, primary care clinic leadership and affiliated training programs to support staff and trainee participation also has been critical. Additionally, VA facility leadership commitment to ongoing improvements to PACT implementation was a key facilitating factor. Colocation of trainees and clinic staff on the academic PACT team facilitates communication between PACT ICU case conferences, while also supporting team dynamics and sustained relationships with patients. Many of these patients can and will typically seek care using the interdisciplinary trainees, and trainees were motivated to proactively coordinate warm handoffs and other models of transfer of care. PACT ICU has been successfully replicated and sustained at 4 of the 5 CoEPCE sites. The Caldwell CBOC PACT ICU has been up and running for 2 years, and 2 other nonacademic clinics have piloted PACT ICU managed care conferences thus far. Experience regarding the implementation at other academic sites has been published.5
Accomplishments and Benefits
There is evidence that PACT ICU is achieving its goals of improving trainee learning and patient outcomes. Trainees are using team skills to provide patient-centered care; trainees are strengthening their overall clinical skills by learning how to improve their responses to high-risk patients. There is also evidence of an increase in interprofessional warm handoffs within the clinic, in which “a clinician directly introduces a patient to another clinician at the time of the patient’s visit, and often a brief encounter between the patient and the health care professional occurs.”4,6
Unlike a traditional didactic with classroom case conferences on interprofessional collaboration, PACT ICU is an opportunity for health care professionals to both learn and work together providing care in a clinic. Moreover, colocation of diverse trainee and faculty professions during the case conferences better prepares trainees to work with other professions and supports all participants to work and communicate as a team.
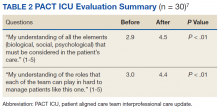
CoE staff have assessed educational outcomes before and after attendance in PACT ICU. On average, trainees (n = 30) said they found the PACT ICU case conferences to be “very helpful” in developing treatment plans.
Interprofessional Collaboration
Team building and colocating trainees, faculty, and clinic staff from different professions are a primary focus of PACT ICU. The case conferences are designed to break down silos and foster a team approach to care. Trainees learn how the team works and the ways other professionals can help them take care of the patient. For example, trainees learn early about the contributions and expertise that the pharmacist and psychologist offer in terms of their scope of practice and referral opportunities. Additionally, the RN care manager increases the integration with the PACT clinical team by sharing pertinent information on individual patients. Based on recent trainee survey findings, the CoE has observed a positive change in the team dynamic and trainee ability to interface between professions. PACT ICU participants were more likely to make referrals to other members within the PACT team, such as a warm handoff during a clinic appointment, while they were less likely to seek a consult outside the team.7
Clinical Performance
The PACT ICU is an opportunity for a trainee to increase clinical expertise. It provides exposure to a variety of patientsand their care needs and serves as an opportunity to present a high-risk, challenging patient to colleagues of various professions. As of June 2018, 96 physician resident and NP residents have presented complex patient cases.
In addition, a structured forum for discussing patients and their care options strengthens team clinical performance, which supports people to work to the full scope of their practice. Trainees learn and apply team skills, such as communication and the warm handoff.
An interprofessional care plan that is delineated during the meeting supports the trainee and is carried out with help from consultants as needed. These consultants often facilitate plans for a covisit or warm handoff at the next clinic visit, a call from the RN care manager, a virtual clinic appointment, or other nontraditional visits. The clinic staff can get information from PCPs about patient’s plan of care, and PCPs get a more complete picture of a patient’s situation (eg, history, communications, and life-style factors). In addition, surveys of PACT ICU participants suggest the curriculum’s effectiveness at encouraging use of PACT principles within the clinic team and improving appropriate referrals to other members of the PACT team, such as pharmacy and behavioral health.
Patients presented at PACT ICU can be particularly challenging, so there may be a psychological benefit to working with a team to develop a new care plan. The PCPs who feel they are overwhelmed and have exhausted every option step back, get input, and look at the patient in a new light.
Related: Interprofessional Education in Patient Aligned Care Team Primary Care-Mental Health Integration
CoEPCE Function
The PACT ICU is flexible and has been adapted to different ambulatory care settings. Currently, PACT ICU case conferences take place at Boise VAMC, the Caldwell CBOCs, and more recently at a smaller CBOC in Burns, Oregon. The PACT ICU structure is slightly different in the clinic settings since the VA primary care clinic has different resources to draw upon, such as hospital and specialty services. The Caldwell CBOC was unable to protect time for PCPs, so it holds a monthly PACT ICU case conference. In addition to continuing expansion in other nonacademic PACT clinics and collaboration with other CoEPCE sites, work is underway to disseminate generalizable principles for interprofessional education, as well as exporting the model for implementation in non-VA settings.
Primary Care Services
The PACT ICU has the potential to create efficiencies in busy clinic settings. It strengthens communication between PCPs and is an opportunity to touch base on the patient, delegate care, and keep track of high-risk patients who might otherwise receive attention only when having an acute problem. Nurses gain a deeper understanding of the patients presented at PACT ICU.
PACT ICU leverages and builds on existing PACT resources in an achievable and sustainable manner benefiting primary care. CoE trainees, who are part of the Silver Team, tap in to the information that team nurses gain from checking in with these high-risk patients biweekly. Moreover, the integration with the Silver Team improves continuity, which helps enhance a patient’s level of trust. The relationship strengthened between primary care and behavioral health at the Caldwell CBOC, providing improved patient access and increased professional sharing.
Patient Outcomes
The PACT ICU provides a forum for input beyond that of the PCP. This feature results in a more robust treatment plan than might be developed by individual PCPs who might not have time to consider options that are outside their scope of practice. Formulating an enriched care plan, informed by multiple professions, has the potential to improve utilization and provide better care.
The Boise VAMC PACT ICU has presented 219 patients as of June 2018. While clinical outcomes data are difficult to collect, the CoE has data on utilization differences on all patients presented at the PACT ICU case conferences. This includes 4 control patients from the same PCP, with similarly high risk based on CAN scores at the time of selection. A single control patient is selected based on gender, closest age, and CAN score; this serves as a comparator for subsequent utilization analysis.
Data from the first 2 years of this study demonstrate that compared with the high-risk control group, there was an increase in contacts with PACT team members, including behavioral health, clinical pharmacists, and nurse care management, persisting up to 6 months following the PACT ICU presentation.4 However, PACT ICU participation did not increase the number of visits with the PCP, indicating better engagement with the entire team. Participation was associated with significantly decreased hospitalizations and a trend toward decreased ED visits. These findings persisted when compared with controls in the PCP’s panel with similar CAN scores, making “regression to the mean” often seen in these studies much less likely.
Analysis of patients early in the project suggests the possibility of improved glycemic control in patients with DM and improved blood pressure control in hypertensive patients presented at the PACT ICU compared with that of non-PACT ICU patients.8 Another potential benefit includes better team-based coordination. Because the patient now has a team focusing on care, this new dynamic results in improving outreach, identifying patients who could receive care by a telephone, and better preparing team members to establish rapport when the patient calls or comes in for a visit.
The Future
In stage 2 of the CoEPCE program, a multi-site trial of PACT ICU was completed to better understand which elements are critical to success, with the goal of facilitating broader exportability.5 The trial focused on 3 intertwined elements: structure, delivery, and evaluation. Using local implementation and the multisite trial, the most effective practices have been documented as part of an implementation kit, available at boisevacoe.org. The goal of the implementation kit is to facilitate step-by-step implementation of PACT ICU to other settings beyond the multisite study. Since the open-ended structure of PACT ICU enables accommodating different professions and specialties beyond the model’s Boise VAMC participants, it could be easily adapted to potentially support a variety of implementations elsewhere (Appendix).
Another opportunity for expansion is increased patient involvement. Currently, PACT ICU patients have the opportunity to review and ask questions about their multidisciplinary care plans before starting.
1. Rugen KW, Watts S, Janson S, et al. Veteran Affairs centers of excellence in primary care education: transforming nurse practitioner education. Nurs Outlook. 2014;62(2):78-88.
2. Billett S. Learning through practice: beyond informal and towards a framework for learning through practice. UNESCO-UNEVOC. https://unevoc.unesco.org/fileadmin/up/2013_epub_revisiting_global_trends_in_tvet_chapter4.pdf. Published 2013. Accessed August 30, 2018.
3. Bitton A, Pereira AG, Smith CS, Babbott SF, Bowen JL. The EFECT framework for interprofessional education in the patient centered medical home. Healthc (Amst). 2013;1(3-4):63-68.
4. Weppner WG, Davis K, Tivis R, et al. Impact of a complex chronic care patient case conference on quality and utilization. Transl Behav Med. 2018;8(3):366-374.
5. King IC, Strewler A, Wipf JE. Translating innovation: exploring dissemination of a unique case conference. J Interprof Educ Pract. 2017;6(1):55-60.
6. Cohen DJ, Balasubramanian BA, Davis M, et al. Understanding care integration from the ground up: five organizing constructs that shape integrated practices. J Am Board Fam Med. 2015;28(suppl 1):S7-S20.
7. Weppner WG, Davis K, Sordahl J, et al. Interprofessional care conferences for high risk primary care patients. Acad Med. 2016;91(6):798-802.
8. Buu J, Fisher A, Weppner W, Mason B. Impact of patient aligned care team interprofessional care updates (ICU) on metabolic parameters. Fed Pract. 2016;33(2):44-48.
Physician, nurse practitioner trainees, medical center faculty, and clinic staff develop proactive, team-based, interprofessional care plans to address unmet chronic care needs for high-risk patients.
Physician, nurse practitioner trainees, medical center faculty, and clinic staff develop proactive, team-based, interprofessional care plans to address unmet chronic care needs for high-risk patients.
This article is part of a series that illustrates strategies intended to redesign primary care education at the Veterans Health Administration (VHA), using interprofessional workplace learning. All have been implemented in the VA Centers of Excellence in Primary Care Education (CoEPCE). These models embody visionary transformation of clinical and educational environments that have potential for replication and dissemination throughout VA and other primary care clinical educational environments. For an introduction to the series see Klink K. Transforming primary care clinical learning environments to optimize education, outcomes, and satisfaction. Fed Pract. 2018;35(9):8-10.
Background
In 2011, 5 US Department of Veterans Affairs (VA) medical centers (VAMCs) were selected by the Office of Academic Affiliations (OAA) to establish CoEPCE. Part of the VA New Models of Care initiative, the 5 Centers of Excellence (CoE) in Boise, Idaho; Cleveland, Ohio; San Francisco, California; Seattle, Washington; and West Haven, Connecticut, are utilizing VA primary care settings to develop and test innovative approaches to prepare physician residents and students, advanced practice nurse residents and undergraduate nursing students, and other professions of health trainees (eg, pharmacy, social work, psychology, physician assistants [PAs]) for primary care practice in the 21st century.
The Boise CoE developed and implemented a practice-based learning model. Nurse practitioner (NP) students and residents, physician residents, pharmacy residents, psychology interns, and psychology postdoctoral fellows participate in a comprehensive curriculum and practice together for 1 to 3 years. The goal is to produce providers who are able to lead and practice health care in patient-centered primary care and rural care environments. All core curricula are interprofessionally coauthored and cotaught.1
Methods
In 2015, OAA evaluators reviewed background documents and conducted open-ended interviews with 10 CoE staff, participating trainees, VA faculty, VA facility leadership, and affiliate faculty. In response to questions focused on their experiences, informants described lessons learned, challenges encountered, and benefits for participants, veterans, and the VA. Using a qualitative and quantitative approach, this case study draws on those interviews, surveys of PACT ICU (patient aligned care team interprofessional care update) participants, and analysis of presented patients to examine PACT ICU outcomes.
Interprofessional Education and Care
A key CoEPCE aim is to create more clinical opportunities for CoE trainees from a variety of professions to work as a team in ways that anticipate and address the care needs of veterans. This emphasis on workplace learning is needed since most current health care professional education programs lack settings where trainees from different professions can learn and work together with their clinic partners to provide care for patients. With the emphasis on patient-centered medical homes (PCMH) and team-based care in the Affordable Care Act, there is an imperative to develop new training models that address this gap in the preparation of future health professionals. Along with this imperative, clinicians are increasingly required to optimize the health of complex patients who consequently require a multidisciplinary approach to care, particularly high-risk, high-needs patients inappropriately using services, such as frequent emergency department (ED) use.
Addressing Complex Needs
In 2010, the Boise VA Medical Center (VAMC) phased in patient aligned care teams (PACTs), the VA-mandated version of PCMH that consist of a physician or NP primary care provider (PCP), a registered nurse (RN) care manager, a licensed vocational nurse (LVN), and a medical support assistant (MSA).
The PACT ICU also serves as a venue in which trainees and supervisors from different professions use a patient-centered framework to collaborate on these specific patient cases. The PACT ICU is easily applied to a range of health conditions, such as diabetes mellitus (DM), mental and behavioral health, lack of social support, and delivery system issues, such as ED use. The goals of PACT ICU are to improve the quality and satisfaction of patient care for high-risk patients; encourage appropriate use of health care resources by prioritizing continuity with the PACT team; and enhance interprofessional PACT team function, decreasing PCP and staff stress.
Planning and Implementation
In January 2013, Boise VAMC and the Caldwell, Idaho community-based outpatient clinic (CBOC) implemented PACT ICU. Other nonteaching clinics followed later in the year. Planning and executing PACT ICU took about 10 hours of CoE staff time and required no change in Boise VAMC policy. Program leadership approval was necessary for participation of CoE residents and postdocs. Service-line leadership support was required to protect clinic staff time (nurse care manager, social workers, chaplaincy, and ethics service). At the Caldwell CBOC, the section chief approved the program, and it took about 1 month to initiate a similar version of PACT ICU.
Curriculum
PACT ICU is a workplace clinical activity with roots in the case conference model, specifically the EFECT model (Elicit the narrative of illness, Facilitate a group meeting, Evidence-based gap analysis, Care plan, and Track changes).3 PACT ICU emphasizes a patient-centered approach to developing care plans. Staff review the 5 highest risk patients who are identified by the VA Care Assessment Need (CAN) registry. The CAN is an analytic tool that is available throughout VA and estimates patients’ risk of mortality or hospitalization in the following 90 days. Physician and NP residents choose 1 of the 5 patients to discuss in PACT ICU, while the remaining 4 serve as case-control comparisons to examine long-term patient outcomes. All trainees, faculty, and staff are provided patient data that can be discussed on a secure website.
The PACT ICU combines didactic teaching with workplace learning. For example, the patient’s medical issues may lead to a formal presentation about a topic, such as secondary stroke medication prophylaxis. The workplace learning occurs as the trainees observe and participate in the decision making toward a treatment plan. Interprofessional interactions are role-modeled by clinical faculty and staff during these discussions, and the result impact the patients care. PACT ICU embodies the core domains that shape the CoEPCE curriculum: Interprofessional collaboration (IPC), performance improvement (PI), sustained relationships (SR), and shared decision making (SDM) (Table 1).
There have been some changes to the PACT ICU model over time. Initially, conferences took place on a weekly basis, to build momentum among the team and to normalize processes. After about 2 years, this decreased to every other week to reduce the time burden. Additionally, the CoE has strengthened the “tracking changes” component of the EFECT model—trainees now present a 5-minute update on the last patient they presented at the prior PACT ICU case conference. Most recently, psychology postdoctoral candidates have instituted preconference calls with patients to further improve the teams understanding of the patients’ perspective and narrative.
Related: Improving Team-Based Care Coordination Delivery and Documentation in the Health Record
Resources
The CoE faculty participate in an education program concerning facilitation of interprofessional meetings. All faculty are expected to role model collaborative behavior and mentor trainees on the cases they present.
The PACT ICU requires a room large enough to accommodate at least 12 people. One staff member is required to review patient cases prior to the case conferences (usually about 1 hour of preparation per case conference). Another staff person creates and shares a spreadsheet stored with VA-approved information security with data fields to include the site, PACT ICU date, patient identifier, the CAN score, and a checkbox for whether the patient was selected or part of a control group. Logistic support is required for reserving the room and sending information to presenters. A clinic-based RN with training in interprofessional care case management uses an online schedule to facilitate selection and review of patients. The RN care managers can use a secure management tool to track patient care and outreach.
The RN care manager also needs to be available to attend the PACT ICU case conferences. The Boise CoE built a website to share and standardize resources, such as a presenter schedule, PACT ICU worksheet, and provider questionnaire. (Contact Boise CoE staff for access.) For the initial evaluation of impact, PACT ICU utilized staff data support in the form of a data manager and biostatistician to identify, collect, and analyze data. While optional, this was helpful in refining the approach and demonstrating the impact of the project. Other resource-related requirements for exporting PACT ICU include:
- Staff members, usually RN care managers who coordinate meetings with participants and identify appropriate patients using a registry, such as CAN;
- Meeting facilitators who enforce use of the EFECT model and interprofessional participation to ensure that the interprofessional care plan is carried out by the presenting provider; and
- Interprofessional trainees and faculty who participate in PACT ICU and complete surveys after the first conference.
Monitoring and Assessment
The CoE staff have analyzed the evaluation of PACT ICU with participant self-evaluation, consultation referral patterns, and utilization data, combination of ED and episodic care visits along with hospitalizations).4 Pharmacy faculty are exploring the use polypharmacy registries, and psychology will use registries of poor psychosocial function.
Partnerships
Beyond support and engagement from VA CoEPCE and affiliate faculty, PACT ICU has greatly benefited from partnerships with VA facility department and CBOC leadership. The CoEPCE codirector and faculty are in facility committees, such as the PACT Strategic Planning Committee.
Academic affiliates are integral partners who assist with NP student and resident recruitment as well as participate in the planning and refinement of CoEPCE components. PACT ICU supports their mandate to encourage interprofessional teamwork. Faculty members from Gonzaga University (NP affiliate) were involved in the initial discussion on PACT ICU and consider it a “learning laboratory” to work through challenging problems. Gonzaga CoEPCE NP trainees are asked to talk about their PACT ICU experience—its strengths, weaknesses, and challenges—to other Gonzaga students who don’t have exposure to the team experience.
Challenges and Solutions
The demand for direct patient care puts pressure on indirect patient care approaches like PACT ICU, which is a time-intensive process with high impact on only a small number of patients. The argument for deploying strategies such as PACT ICU is that managing chronic conditions and encouraging appropriate use of services will improve outcomes for the highest risk patients and save important system resources in the long-run. However, in the short-term, a strong case must be made for the diversion of resources from usual clinic flow, particularly securing recurring blocks of provider time and clinic staff members. In addition, issues about team communication and understanding of appropriate team-based care can overflow to complex patients not presented in the PACT ICU conference.
Providing a facilitated interprofessional venue to discuss how to appropriately coordinate care improves the participation and perceived value of different team members. This approach has led to improved engagement of the team for patients discussed in the PACT ICU, as well as in general care within the participating clinic. With recent changes, the VA does see a workload benefit, and participants get encounter credit through “Non face-to-face prolonged service” codes (CPT 99358/99359), and other possibilities exist related to clinical team conference codes (CPT 99367-8) and complex chronic care management codes (CPT 99487-89). More information on documentation, scheduling and encountering/billing can be found at boisevacoe.org under Products. Other challenges include logistic challenges of finding appropriate patients and distributing sensitive patient information among the team. Additionally, PACT ICU has to wrestle with staffing shortages and episodic participation by some professions that are chronically understaffed. We have addressed many of these problems by receiving buy-in from both leadership and participants. Leadership have allowed time for participation in clinic staff schedules, and each participant has committed to recruiting a substitute in case of a schedule conflict.
Factors for Success
The commitment from the Boise VAMC facility, primary care clinic leadership and affiliated training programs to support staff and trainee participation also has been critical. Additionally, VA facility leadership commitment to ongoing improvements to PACT implementation was a key facilitating factor. Colocation of trainees and clinic staff on the academic PACT team facilitates communication between PACT ICU case conferences, while also supporting team dynamics and sustained relationships with patients. Many of these patients can and will typically seek care using the interdisciplinary trainees, and trainees were motivated to proactively coordinate warm handoffs and other models of transfer of care. PACT ICU has been successfully replicated and sustained at 4 of the 5 CoEPCE sites. The Caldwell CBOC PACT ICU has been up and running for 2 years, and 2 other nonacademic clinics have piloted PACT ICU managed care conferences thus far. Experience regarding the implementation at other academic sites has been published.5
Accomplishments and Benefits
There is evidence that PACT ICU is achieving its goals of improving trainee learning and patient outcomes. Trainees are using team skills to provide patient-centered care; trainees are strengthening their overall clinical skills by learning how to improve their responses to high-risk patients. There is also evidence of an increase in interprofessional warm handoffs within the clinic, in which “a clinician directly introduces a patient to another clinician at the time of the patient’s visit, and often a brief encounter between the patient and the health care professional occurs.”4,6
Unlike a traditional didactic with classroom case conferences on interprofessional collaboration, PACT ICU is an opportunity for health care professionals to both learn and work together providing care in a clinic. Moreover, colocation of diverse trainee and faculty professions during the case conferences better prepares trainees to work with other professions and supports all participants to work and communicate as a team.
CoE staff have assessed educational outcomes before and after attendance in PACT ICU. On average, trainees (n = 30) said they found the PACT ICU case conferences to be “very helpful” in developing treatment plans.
Interprofessional Collaboration
Team building and colocating trainees, faculty, and clinic staff from different professions are a primary focus of PACT ICU. The case conferences are designed to break down silos and foster a team approach to care. Trainees learn how the team works and the ways other professionals can help them take care of the patient. For example, trainees learn early about the contributions and expertise that the pharmacist and psychologist offer in terms of their scope of practice and referral opportunities. Additionally, the RN care manager increases the integration with the PACT clinical team by sharing pertinent information on individual patients. Based on recent trainee survey findings, the CoE has observed a positive change in the team dynamic and trainee ability to interface between professions. PACT ICU participants were more likely to make referrals to other members within the PACT team, such as a warm handoff during a clinic appointment, while they were less likely to seek a consult outside the team.7
Clinical Performance
The PACT ICU is an opportunity for a trainee to increase clinical expertise. It provides exposure to a variety of patientsand their care needs and serves as an opportunity to present a high-risk, challenging patient to colleagues of various professions. As of June 2018, 96 physician resident and NP residents have presented complex patient cases.
In addition, a structured forum for discussing patients and their care options strengthens team clinical performance, which supports people to work to the full scope of their practice. Trainees learn and apply team skills, such as communication and the warm handoff.
An interprofessional care plan that is delineated during the meeting supports the trainee and is carried out with help from consultants as needed. These consultants often facilitate plans for a covisit or warm handoff at the next clinic visit, a call from the RN care manager, a virtual clinic appointment, or other nontraditional visits. The clinic staff can get information from PCPs about patient’s plan of care, and PCPs get a more complete picture of a patient’s situation (eg, history, communications, and life-style factors). In addition, surveys of PACT ICU participants suggest the curriculum’s effectiveness at encouraging use of PACT principles within the clinic team and improving appropriate referrals to other members of the PACT team, such as pharmacy and behavioral health.
Patients presented at PACT ICU can be particularly challenging, so there may be a psychological benefit to working with a team to develop a new care plan. The PCPs who feel they are overwhelmed and have exhausted every option step back, get input, and look at the patient in a new light.
Related: Interprofessional Education in Patient Aligned Care Team Primary Care-Mental Health Integration
CoEPCE Function
The PACT ICU is flexible and has been adapted to different ambulatory care settings. Currently, PACT ICU case conferences take place at Boise VAMC, the Caldwell CBOCs, and more recently at a smaller CBOC in Burns, Oregon. The PACT ICU structure is slightly different in the clinic settings since the VA primary care clinic has different resources to draw upon, such as hospital and specialty services. The Caldwell CBOC was unable to protect time for PCPs, so it holds a monthly PACT ICU case conference. In addition to continuing expansion in other nonacademic PACT clinics and collaboration with other CoEPCE sites, work is underway to disseminate generalizable principles for interprofessional education, as well as exporting the model for implementation in non-VA settings.
Primary Care Services
The PACT ICU has the potential to create efficiencies in busy clinic settings. It strengthens communication between PCPs and is an opportunity to touch base on the patient, delegate care, and keep track of high-risk patients who might otherwise receive attention only when having an acute problem. Nurses gain a deeper understanding of the patients presented at PACT ICU.
PACT ICU leverages and builds on existing PACT resources in an achievable and sustainable manner benefiting primary care. CoE trainees, who are part of the Silver Team, tap in to the information that team nurses gain from checking in with these high-risk patients biweekly. Moreover, the integration with the Silver Team improves continuity, which helps enhance a patient’s level of trust. The relationship strengthened between primary care and behavioral health at the Caldwell CBOC, providing improved patient access and increased professional sharing.
Patient Outcomes
The PACT ICU provides a forum for input beyond that of the PCP. This feature results in a more robust treatment plan than might be developed by individual PCPs who might not have time to consider options that are outside their scope of practice. Formulating an enriched care plan, informed by multiple professions, has the potential to improve utilization and provide better care.
The Boise VAMC PACT ICU has presented 219 patients as of June 2018. While clinical outcomes data are difficult to collect, the CoE has data on utilization differences on all patients presented at the PACT ICU case conferences. This includes 4 control patients from the same PCP, with similarly high risk based on CAN scores at the time of selection. A single control patient is selected based on gender, closest age, and CAN score; this serves as a comparator for subsequent utilization analysis.
Data from the first 2 years of this study demonstrate that compared with the high-risk control group, there was an increase in contacts with PACT team members, including behavioral health, clinical pharmacists, and nurse care management, persisting up to 6 months following the PACT ICU presentation.4 However, PACT ICU participation did not increase the number of visits with the PCP, indicating better engagement with the entire team. Participation was associated with significantly decreased hospitalizations and a trend toward decreased ED visits. These findings persisted when compared with controls in the PCP’s panel with similar CAN scores, making “regression to the mean” often seen in these studies much less likely.
Analysis of patients early in the project suggests the possibility of improved glycemic control in patients with DM and improved blood pressure control in hypertensive patients presented at the PACT ICU compared with that of non-PACT ICU patients.8 Another potential benefit includes better team-based coordination. Because the patient now has a team focusing on care, this new dynamic results in improving outreach, identifying patients who could receive care by a telephone, and better preparing team members to establish rapport when the patient calls or comes in for a visit.
The Future
In stage 2 of the CoEPCE program, a multi-site trial of PACT ICU was completed to better understand which elements are critical to success, with the goal of facilitating broader exportability.5 The trial focused on 3 intertwined elements: structure, delivery, and evaluation. Using local implementation and the multisite trial, the most effective practices have been documented as part of an implementation kit, available at boisevacoe.org. The goal of the implementation kit is to facilitate step-by-step implementation of PACT ICU to other settings beyond the multisite study. Since the open-ended structure of PACT ICU enables accommodating different professions and specialties beyond the model’s Boise VAMC participants, it could be easily adapted to potentially support a variety of implementations elsewhere (Appendix).
Another opportunity for expansion is increased patient involvement. Currently, PACT ICU patients have the opportunity to review and ask questions about their multidisciplinary care plans before starting.
This article is part of a series that illustrates strategies intended to redesign primary care education at the Veterans Health Administration (VHA), using interprofessional workplace learning. All have been implemented in the VA Centers of Excellence in Primary Care Education (CoEPCE). These models embody visionary transformation of clinical and educational environments that have potential for replication and dissemination throughout VA and other primary care clinical educational environments. For an introduction to the series see Klink K. Transforming primary care clinical learning environments to optimize education, outcomes, and satisfaction. Fed Pract. 2018;35(9):8-10.
Background
In 2011, 5 US Department of Veterans Affairs (VA) medical centers (VAMCs) were selected by the Office of Academic Affiliations (OAA) to establish CoEPCE. Part of the VA New Models of Care initiative, the 5 Centers of Excellence (CoE) in Boise, Idaho; Cleveland, Ohio; San Francisco, California; Seattle, Washington; and West Haven, Connecticut, are utilizing VA primary care settings to develop and test innovative approaches to prepare physician residents and students, advanced practice nurse residents and undergraduate nursing students, and other professions of health trainees (eg, pharmacy, social work, psychology, physician assistants [PAs]) for primary care practice in the 21st century.
The Boise CoE developed and implemented a practice-based learning model. Nurse practitioner (NP) students and residents, physician residents, pharmacy residents, psychology interns, and psychology postdoctoral fellows participate in a comprehensive curriculum and practice together for 1 to 3 years. The goal is to produce providers who are able to lead and practice health care in patient-centered primary care and rural care environments. All core curricula are interprofessionally coauthored and cotaught.1
Methods
In 2015, OAA evaluators reviewed background documents and conducted open-ended interviews with 10 CoE staff, participating trainees, VA faculty, VA facility leadership, and affiliate faculty. In response to questions focused on their experiences, informants described lessons learned, challenges encountered, and benefits for participants, veterans, and the VA. Using a qualitative and quantitative approach, this case study draws on those interviews, surveys of PACT ICU (patient aligned care team interprofessional care update) participants, and analysis of presented patients to examine PACT ICU outcomes.
Interprofessional Education and Care
A key CoEPCE aim is to create more clinical opportunities for CoE trainees from a variety of professions to work as a team in ways that anticipate and address the care needs of veterans. This emphasis on workplace learning is needed since most current health care professional education programs lack settings where trainees from different professions can learn and work together with their clinic partners to provide care for patients. With the emphasis on patient-centered medical homes (PCMH) and team-based care in the Affordable Care Act, there is an imperative to develop new training models that address this gap in the preparation of future health professionals. Along with this imperative, clinicians are increasingly required to optimize the health of complex patients who consequently require a multidisciplinary approach to care, particularly high-risk, high-needs patients inappropriately using services, such as frequent emergency department (ED) use.
Addressing Complex Needs
In 2010, the Boise VA Medical Center (VAMC) phased in patient aligned care teams (PACTs), the VA-mandated version of PCMH that consist of a physician or NP primary care provider (PCP), a registered nurse (RN) care manager, a licensed vocational nurse (LVN), and a medical support assistant (MSA).
The PACT ICU also serves as a venue in which trainees and supervisors from different professions use a patient-centered framework to collaborate on these specific patient cases. The PACT ICU is easily applied to a range of health conditions, such as diabetes mellitus (DM), mental and behavioral health, lack of social support, and delivery system issues, such as ED use. The goals of PACT ICU are to improve the quality and satisfaction of patient care for high-risk patients; encourage appropriate use of health care resources by prioritizing continuity with the PACT team; and enhance interprofessional PACT team function, decreasing PCP and staff stress.
Planning and Implementation
In January 2013, Boise VAMC and the Caldwell, Idaho community-based outpatient clinic (CBOC) implemented PACT ICU. Other nonteaching clinics followed later in the year. Planning and executing PACT ICU took about 10 hours of CoE staff time and required no change in Boise VAMC policy. Program leadership approval was necessary for participation of CoE residents and postdocs. Service-line leadership support was required to protect clinic staff time (nurse care manager, social workers, chaplaincy, and ethics service). At the Caldwell CBOC, the section chief approved the program, and it took about 1 month to initiate a similar version of PACT ICU.
Curriculum
PACT ICU is a workplace clinical activity with roots in the case conference model, specifically the EFECT model (Elicit the narrative of illness, Facilitate a group meeting, Evidence-based gap analysis, Care plan, and Track changes).3 PACT ICU emphasizes a patient-centered approach to developing care plans. Staff review the 5 highest risk patients who are identified by the VA Care Assessment Need (CAN) registry. The CAN is an analytic tool that is available throughout VA and estimates patients’ risk of mortality or hospitalization in the following 90 days. Physician and NP residents choose 1 of the 5 patients to discuss in PACT ICU, while the remaining 4 serve as case-control comparisons to examine long-term patient outcomes. All trainees, faculty, and staff are provided patient data that can be discussed on a secure website.
The PACT ICU combines didactic teaching with workplace learning. For example, the patient’s medical issues may lead to a formal presentation about a topic, such as secondary stroke medication prophylaxis. The workplace learning occurs as the trainees observe and participate in the decision making toward a treatment plan. Interprofessional interactions are role-modeled by clinical faculty and staff during these discussions, and the result impact the patients care. PACT ICU embodies the core domains that shape the CoEPCE curriculum: Interprofessional collaboration (IPC), performance improvement (PI), sustained relationships (SR), and shared decision making (SDM) (Table 1).
There have been some changes to the PACT ICU model over time. Initially, conferences took place on a weekly basis, to build momentum among the team and to normalize processes. After about 2 years, this decreased to every other week to reduce the time burden. Additionally, the CoE has strengthened the “tracking changes” component of the EFECT model—trainees now present a 5-minute update on the last patient they presented at the prior PACT ICU case conference. Most recently, psychology postdoctoral candidates have instituted preconference calls with patients to further improve the teams understanding of the patients’ perspective and narrative.
Related: Improving Team-Based Care Coordination Delivery and Documentation in the Health Record
Resources
The CoE faculty participate in an education program concerning facilitation of interprofessional meetings. All faculty are expected to role model collaborative behavior and mentor trainees on the cases they present.
The PACT ICU requires a room large enough to accommodate at least 12 people. One staff member is required to review patient cases prior to the case conferences (usually about 1 hour of preparation per case conference). Another staff person creates and shares a spreadsheet stored with VA-approved information security with data fields to include the site, PACT ICU date, patient identifier, the CAN score, and a checkbox for whether the patient was selected or part of a control group. Logistic support is required for reserving the room and sending information to presenters. A clinic-based RN with training in interprofessional care case management uses an online schedule to facilitate selection and review of patients. The RN care managers can use a secure management tool to track patient care and outreach.
The RN care manager also needs to be available to attend the PACT ICU case conferences. The Boise CoE built a website to share and standardize resources, such as a presenter schedule, PACT ICU worksheet, and provider questionnaire. (Contact Boise CoE staff for access.) For the initial evaluation of impact, PACT ICU utilized staff data support in the form of a data manager and biostatistician to identify, collect, and analyze data. While optional, this was helpful in refining the approach and demonstrating the impact of the project. Other resource-related requirements for exporting PACT ICU include:
- Staff members, usually RN care managers who coordinate meetings with participants and identify appropriate patients using a registry, such as CAN;
- Meeting facilitators who enforce use of the EFECT model and interprofessional participation to ensure that the interprofessional care plan is carried out by the presenting provider; and
- Interprofessional trainees and faculty who participate in PACT ICU and complete surveys after the first conference.
Monitoring and Assessment
The CoE staff have analyzed the evaluation of PACT ICU with participant self-evaluation, consultation referral patterns, and utilization data, combination of ED and episodic care visits along with hospitalizations).4 Pharmacy faculty are exploring the use polypharmacy registries, and psychology will use registries of poor psychosocial function.
Partnerships
Beyond support and engagement from VA CoEPCE and affiliate faculty, PACT ICU has greatly benefited from partnerships with VA facility department and CBOC leadership. The CoEPCE codirector and faculty are in facility committees, such as the PACT Strategic Planning Committee.
Academic affiliates are integral partners who assist with NP student and resident recruitment as well as participate in the planning and refinement of CoEPCE components. PACT ICU supports their mandate to encourage interprofessional teamwork. Faculty members from Gonzaga University (NP affiliate) were involved in the initial discussion on PACT ICU and consider it a “learning laboratory” to work through challenging problems. Gonzaga CoEPCE NP trainees are asked to talk about their PACT ICU experience—its strengths, weaknesses, and challenges—to other Gonzaga students who don’t have exposure to the team experience.
Challenges and Solutions
The demand for direct patient care puts pressure on indirect patient care approaches like PACT ICU, which is a time-intensive process with high impact on only a small number of patients. The argument for deploying strategies such as PACT ICU is that managing chronic conditions and encouraging appropriate use of services will improve outcomes for the highest risk patients and save important system resources in the long-run. However, in the short-term, a strong case must be made for the diversion of resources from usual clinic flow, particularly securing recurring blocks of provider time and clinic staff members. In addition, issues about team communication and understanding of appropriate team-based care can overflow to complex patients not presented in the PACT ICU conference.
Providing a facilitated interprofessional venue to discuss how to appropriately coordinate care improves the participation and perceived value of different team members. This approach has led to improved engagement of the team for patients discussed in the PACT ICU, as well as in general care within the participating clinic. With recent changes, the VA does see a workload benefit, and participants get encounter credit through “Non face-to-face prolonged service” codes (CPT 99358/99359), and other possibilities exist related to clinical team conference codes (CPT 99367-8) and complex chronic care management codes (CPT 99487-89). More information on documentation, scheduling and encountering/billing can be found at boisevacoe.org under Products. Other challenges include logistic challenges of finding appropriate patients and distributing sensitive patient information among the team. Additionally, PACT ICU has to wrestle with staffing shortages and episodic participation by some professions that are chronically understaffed. We have addressed many of these problems by receiving buy-in from both leadership and participants. Leadership have allowed time for participation in clinic staff schedules, and each participant has committed to recruiting a substitute in case of a schedule conflict.
Factors for Success
The commitment from the Boise VAMC facility, primary care clinic leadership and affiliated training programs to support staff and trainee participation also has been critical. Additionally, VA facility leadership commitment to ongoing improvements to PACT implementation was a key facilitating factor. Colocation of trainees and clinic staff on the academic PACT team facilitates communication between PACT ICU case conferences, while also supporting team dynamics and sustained relationships with patients. Many of these patients can and will typically seek care using the interdisciplinary trainees, and trainees were motivated to proactively coordinate warm handoffs and other models of transfer of care. PACT ICU has been successfully replicated and sustained at 4 of the 5 CoEPCE sites. The Caldwell CBOC PACT ICU has been up and running for 2 years, and 2 other nonacademic clinics have piloted PACT ICU managed care conferences thus far. Experience regarding the implementation at other academic sites has been published.5
Accomplishments and Benefits
There is evidence that PACT ICU is achieving its goals of improving trainee learning and patient outcomes. Trainees are using team skills to provide patient-centered care; trainees are strengthening their overall clinical skills by learning how to improve their responses to high-risk patients. There is also evidence of an increase in interprofessional warm handoffs within the clinic, in which “a clinician directly introduces a patient to another clinician at the time of the patient’s visit, and often a brief encounter between the patient and the health care professional occurs.”4,6
Unlike a traditional didactic with classroom case conferences on interprofessional collaboration, PACT ICU is an opportunity for health care professionals to both learn and work together providing care in a clinic. Moreover, colocation of diverse trainee and faculty professions during the case conferences better prepares trainees to work with other professions and supports all participants to work and communicate as a team.
CoE staff have assessed educational outcomes before and after attendance in PACT ICU. On average, trainees (n = 30) said they found the PACT ICU case conferences to be “very helpful” in developing treatment plans.
Interprofessional Collaboration
Team building and colocating trainees, faculty, and clinic staff from different professions are a primary focus of PACT ICU. The case conferences are designed to break down silos and foster a team approach to care. Trainees learn how the team works and the ways other professionals can help them take care of the patient. For example, trainees learn early about the contributions and expertise that the pharmacist and psychologist offer in terms of their scope of practice and referral opportunities. Additionally, the RN care manager increases the integration with the PACT clinical team by sharing pertinent information on individual patients. Based on recent trainee survey findings, the CoE has observed a positive change in the team dynamic and trainee ability to interface between professions. PACT ICU participants were more likely to make referrals to other members within the PACT team, such as a warm handoff during a clinic appointment, while they were less likely to seek a consult outside the team.7
Clinical Performance
The PACT ICU is an opportunity for a trainee to increase clinical expertise. It provides exposure to a variety of patientsand their care needs and serves as an opportunity to present a high-risk, challenging patient to colleagues of various professions. As of June 2018, 96 physician resident and NP residents have presented complex patient cases.
In addition, a structured forum for discussing patients and their care options strengthens team clinical performance, which supports people to work to the full scope of their practice. Trainees learn and apply team skills, such as communication and the warm handoff.
An interprofessional care plan that is delineated during the meeting supports the trainee and is carried out with help from consultants as needed. These consultants often facilitate plans for a covisit or warm handoff at the next clinic visit, a call from the RN care manager, a virtual clinic appointment, or other nontraditional visits. The clinic staff can get information from PCPs about patient’s plan of care, and PCPs get a more complete picture of a patient’s situation (eg, history, communications, and life-style factors). In addition, surveys of PACT ICU participants suggest the curriculum’s effectiveness at encouraging use of PACT principles within the clinic team and improving appropriate referrals to other members of the PACT team, such as pharmacy and behavioral health.
Patients presented at PACT ICU can be particularly challenging, so there may be a psychological benefit to working with a team to develop a new care plan. The PCPs who feel they are overwhelmed and have exhausted every option step back, get input, and look at the patient in a new light.
Related: Interprofessional Education in Patient Aligned Care Team Primary Care-Mental Health Integration
CoEPCE Function
The PACT ICU is flexible and has been adapted to different ambulatory care settings. Currently, PACT ICU case conferences take place at Boise VAMC, the Caldwell CBOCs, and more recently at a smaller CBOC in Burns, Oregon. The PACT ICU structure is slightly different in the clinic settings since the VA primary care clinic has different resources to draw upon, such as hospital and specialty services. The Caldwell CBOC was unable to protect time for PCPs, so it holds a monthly PACT ICU case conference. In addition to continuing expansion in other nonacademic PACT clinics and collaboration with other CoEPCE sites, work is underway to disseminate generalizable principles for interprofessional education, as well as exporting the model for implementation in non-VA settings.
Primary Care Services
The PACT ICU has the potential to create efficiencies in busy clinic settings. It strengthens communication between PCPs and is an opportunity to touch base on the patient, delegate care, and keep track of high-risk patients who might otherwise receive attention only when having an acute problem. Nurses gain a deeper understanding of the patients presented at PACT ICU.
PACT ICU leverages and builds on existing PACT resources in an achievable and sustainable manner benefiting primary care. CoE trainees, who are part of the Silver Team, tap in to the information that team nurses gain from checking in with these high-risk patients biweekly. Moreover, the integration with the Silver Team improves continuity, which helps enhance a patient’s level of trust. The relationship strengthened between primary care and behavioral health at the Caldwell CBOC, providing improved patient access and increased professional sharing.
Patient Outcomes
The PACT ICU provides a forum for input beyond that of the PCP. This feature results in a more robust treatment plan than might be developed by individual PCPs who might not have time to consider options that are outside their scope of practice. Formulating an enriched care plan, informed by multiple professions, has the potential to improve utilization and provide better care.
The Boise VAMC PACT ICU has presented 219 patients as of June 2018. While clinical outcomes data are difficult to collect, the CoE has data on utilization differences on all patients presented at the PACT ICU case conferences. This includes 4 control patients from the same PCP, with similarly high risk based on CAN scores at the time of selection. A single control patient is selected based on gender, closest age, and CAN score; this serves as a comparator for subsequent utilization analysis.
Data from the first 2 years of this study demonstrate that compared with the high-risk control group, there was an increase in contacts with PACT team members, including behavioral health, clinical pharmacists, and nurse care management, persisting up to 6 months following the PACT ICU presentation.4 However, PACT ICU participation did not increase the number of visits with the PCP, indicating better engagement with the entire team. Participation was associated with significantly decreased hospitalizations and a trend toward decreased ED visits. These findings persisted when compared with controls in the PCP’s panel with similar CAN scores, making “regression to the mean” often seen in these studies much less likely.
Analysis of patients early in the project suggests the possibility of improved glycemic control in patients with DM and improved blood pressure control in hypertensive patients presented at the PACT ICU compared with that of non-PACT ICU patients.8 Another potential benefit includes better team-based coordination. Because the patient now has a team focusing on care, this new dynamic results in improving outreach, identifying patients who could receive care by a telephone, and better preparing team members to establish rapport when the patient calls or comes in for a visit.
The Future
In stage 2 of the CoEPCE program, a multi-site trial of PACT ICU was completed to better understand which elements are critical to success, with the goal of facilitating broader exportability.5 The trial focused on 3 intertwined elements: structure, delivery, and evaluation. Using local implementation and the multisite trial, the most effective practices have been documented as part of an implementation kit, available at boisevacoe.org. The goal of the implementation kit is to facilitate step-by-step implementation of PACT ICU to other settings beyond the multisite study. Since the open-ended structure of PACT ICU enables accommodating different professions and specialties beyond the model’s Boise VAMC participants, it could be easily adapted to potentially support a variety of implementations elsewhere (Appendix).
Another opportunity for expansion is increased patient involvement. Currently, PACT ICU patients have the opportunity to review and ask questions about their multidisciplinary care plans before starting.
1. Rugen KW, Watts S, Janson S, et al. Veteran Affairs centers of excellence in primary care education: transforming nurse practitioner education. Nurs Outlook. 2014;62(2):78-88.
2. Billett S. Learning through practice: beyond informal and towards a framework for learning through practice. UNESCO-UNEVOC. https://unevoc.unesco.org/fileadmin/up/2013_epub_revisiting_global_trends_in_tvet_chapter4.pdf. Published 2013. Accessed August 30, 2018.
3. Bitton A, Pereira AG, Smith CS, Babbott SF, Bowen JL. The EFECT framework for interprofessional education in the patient centered medical home. Healthc (Amst). 2013;1(3-4):63-68.
4. Weppner WG, Davis K, Tivis R, et al. Impact of a complex chronic care patient case conference on quality and utilization. Transl Behav Med. 2018;8(3):366-374.
5. King IC, Strewler A, Wipf JE. Translating innovation: exploring dissemination of a unique case conference. J Interprof Educ Pract. 2017;6(1):55-60.
6. Cohen DJ, Balasubramanian BA, Davis M, et al. Understanding care integration from the ground up: five organizing constructs that shape integrated practices. J Am Board Fam Med. 2015;28(suppl 1):S7-S20.
7. Weppner WG, Davis K, Sordahl J, et al. Interprofessional care conferences for high risk primary care patients. Acad Med. 2016;91(6):798-802.
8. Buu J, Fisher A, Weppner W, Mason B. Impact of patient aligned care team interprofessional care updates (ICU) on metabolic parameters. Fed Pract. 2016;33(2):44-48.
1. Rugen KW, Watts S, Janson S, et al. Veteran Affairs centers of excellence in primary care education: transforming nurse practitioner education. Nurs Outlook. 2014;62(2):78-88.
2. Billett S. Learning through practice: beyond informal and towards a framework for learning through practice. UNESCO-UNEVOC. https://unevoc.unesco.org/fileadmin/up/2013_epub_revisiting_global_trends_in_tvet_chapter4.pdf. Published 2013. Accessed August 30, 2018.
3. Bitton A, Pereira AG, Smith CS, Babbott SF, Bowen JL. The EFECT framework for interprofessional education in the patient centered medical home. Healthc (Amst). 2013;1(3-4):63-68.
4. Weppner WG, Davis K, Tivis R, et al. Impact of a complex chronic care patient case conference on quality and utilization. Transl Behav Med. 2018;8(3):366-374.
5. King IC, Strewler A, Wipf JE. Translating innovation: exploring dissemination of a unique case conference. J Interprof Educ Pract. 2017;6(1):55-60.
6. Cohen DJ, Balasubramanian BA, Davis M, et al. Understanding care integration from the ground up: five organizing constructs that shape integrated practices. J Am Board Fam Med. 2015;28(suppl 1):S7-S20.
7. Weppner WG, Davis K, Sordahl J, et al. Interprofessional care conferences for high risk primary care patients. Acad Med. 2016;91(6):798-802.
8. Buu J, Fisher A, Weppner W, Mason B. Impact of patient aligned care team interprofessional care updates (ICU) on metabolic parameters. Fed Pract. 2016;33(2):44-48.
More Than a Mnemonic
A 51‐year‐old man presented to the emergency department after 1 day of progressive dyspnea and increasing confusion.
Acute dyspnea most commonly stems from a cardiac or pulmonary disorder such as heart failure, acute coronary syndrome, pneumonia, pulmonary embolism, or exacerbations of asthma or chronic obstructive pulmonary disease. Less frequent cardiopulmonary considerations include pericardial or pleural effusion, pneumothorax, aspiration, and upper airway obstruction. Dyspnea might also be the initial manifestation of profound anemia or metabolic acidosis.
The presence of confusion suggests either a severe presentation of any of the aforementioned possibilities (with confusion resulting from hypoxia, hypercapnia, or hypotension); a multiorgan illness such as sepsis, malignancy, thromboembolic disease, vasculitis, thyroid dysfunction, or toxic ingestion; or a metabolic derangement related to the underlying cause of dyspnea (for example, hypercalcemia or hyponatremia associated with lung cancer).
Twelve hours prior to presentation, he started to have visual hallucinations. He denied fever, chills, cough, chest discomfort, palpitations, weight gain, headache, neck pain, or weakness.
Visual hallucinations could result from a toxic‐metabolic encephalopathy, such as drug overdose or withdrawal, liver or kidney failure, or hypoxia. A structural brain abnormality may also manifest with visual hallucination. Acute onset at age 51 and the absence of auditory hallucinations argue against a neurodegenerative illness and a primary psychiatric disturbance, respectively.
Episodic hallucinations would support the possibility of seizures, monocular hallucinations would point to a retinal or ocular problem, and a description of yellow‐green hue would suggest a side effect of digoxin.
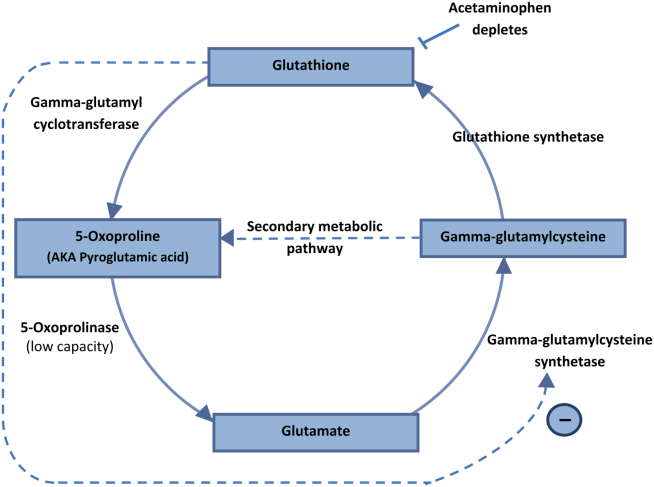
His past medical history was remarkable for diet‐controlled type 2 diabetes mellitus, hypertension, hyperlipidemia, and chronic low back pain. His medications included metoprolol tartrate 25 mg twice daily, omeprazole 40 mg daily, baclofen 15 mg twice daily, oxycodone 30 mg 3 times daily, and hydrocodone 10 mg/acetaminophen 325 mg, 2 tablets 3 times daily as needed for back pain. He was a smoker with a 30 pack‐year history. He had a history of alcohol and cocaine use, but denied any recent substance use. He had no known history of obstructive pulmonary disease.
The patient takes 3 medications well known to cause confusion and hallucinations (oxycodone, hydrocodone, and baclofen), especially when they accumulate due to excessive ingestion or impaired clearance. Although these medications may suppress ventilatory drive, dyspnea would not be a common presenting complaint. He has risk factors for ischemic heart disease and cardiomyopathy, and his smoking history raises the possibility of malignancy.
On exam, the patient's temperature was 94.4C, heart rate 128 beats per minute, respiration rate 28 breaths per minute, blood pressure 155/63 mm Hg, and oxygen saturation 100% while breathing ambient air. The patient was cachectic and appeared in moderate respiratory distress. His pupils were equal and reactive to light, and extraocular movements were intact. He did not have scleral icterus, or cervical or clavicular lymphadenopathy. His oropharynx was negative for erythema, edema, or exudate. His cardiovascular exam revealed a regular tachycardia without rubs or diastolic gallops. There was a 2/6 systolic murmur heard best at left sternal border, without radiation. He did not have jugular venous distention. His pulmonary exam was notable for tachypnea but with normal vesicular breath sounds throughout. He did not have stridor, wheezing, rhonchi, or rales. His abdomen had normal bowel tones and was soft without tenderness, distention, or organomegaly. His extremities were warm, revealed normal pulses, and no edema was present. His joints were cool to palpation, without effusion. On neurologic exam, he was oriented to person and place and able to answer yes/no questions, but unable to provide detailed history. His speech was fluent. His motor exam was without focal deficits. His skin was without any notable lesions.
The constellation of findings does not point to a specific toxidrome. The finding of warm extremities in a hypothermic patient suggests heat loss due to inappropriate peripheral vasodilation. In the absence of vasodilators or features of aortic insufficiency, sepsis becomes a leading consideration. Infection could result in hypothermia and altered sensorium, and accompanying lactic acidosis could trigger tachypnea.
Shortly after admission, he became more somnolent and developed progressive respiratory distress, requiring intubation. Arterial blood gas revealed a pH of 6.93, PaCO2<20 mm Hg, PaO2 127 mm Hg, and HCO3<5 mEq/L. Other laboratory results included a lactate of 4.1 mmol/L, blood urea nitrogen 49 mg/dL, creatinine 2.3 mg/dL (0.8 at 1 month prior), sodium level of 143 mmol/L, chloride of 106 mmol/L, and bicarbonate level of <5 mg/dL. His aspartate aminotransferase was 34 IU/L, alanine transaminase was 28 IU/L, total bilirubin was 0.6 mg/dL, International Normalized Ratio was 1.3. A complete blood count revealed a white blood cell count of 23,000/L, hemoglobin of 10.6 g/dL, and platelet count of 454,000/L. A urinalysis was unremarkable. Cultures of blood, urine, and sputum were collected. Head computed tomography was negative.
This patient has a combined anion gap and nongap metabolic acidosis, as well as respiratory alkalosis. Although his acute kidney failure could produce these 2 types of metabolic acidosis, the modest elevation of the serum creatinine is not commensurate with such profound acidosis. Similarly, sepsis without hypotension or more striking elevation in lactate levels would not account for the entirety of the acidosis. Severe diabetic ketoacidosis can result in profound metabolic acidosis, and marked hyperglycemia or hyperosmolarity could result in somnolence; however, his diabetes has been controlled without medication and there is no obvious precipitant for an episode of ketoacidosis.
Remaining causes of anion gap acidosis include ingestion of methanol, ethylene glycol, ethanol, or salicylates. A careful history of ingestions and medications from witnesses including any prehospital personnel might suggest a source of intoxication. Absent this information, the hypothermia favors an ingestion of an alcohol over salicylates, and the lack of urine crystals and the presence of prominent visual hallucinations would point more toward methanol poisoning than ethylene glycol. A serum osmolarity measurement would allow determination of the osmolar gap, which would be elevated in the setting of methanol or ethylene glycol poisoning. If he were this ill from ethanol, I would have expected to see evidence of hepatotoxicity.
I would administer sodium bicarbonate to reverse the acidosis and to promote renal clearance of salicylates, methanol, ethylene glycol, and their metabolites. Orogastric decontamination with activated charcoal should be considered. If the osmolar gap is elevated, I would also administer intravenous fomepizole to attempt to reverse methanol or ethylene glycol poisoning. I would not delay treatment while waiting for these serum levels to return.
Initial serologic toxicology performed in the emergency department revealed negative ethanol, salicylates, and ketones. His osmolar gap was 13 mOsm/kg. His acetaminophen level was 69 g/mL (normal <120 g/mL). A creatinine phosphokinase was 84 IU/L and myoglobin was 93 ng/mL. His subsequent serum toxicology screen was negative for methanol, ethylene glycol, isopropranol, and hippuric acid. Urine toxicology was positive for opiates, but negative for amphetamine, benzodiazepine, cannabinoid, and cocaine.
Serum and urine ketone assays typically involve the nitroprusside reaction and detect acetoacetate, but not ‐hydroxybutyrate, and can lead to negative test results early in diabetic or alcoholic ketoacidosis. However, the normal ethanol level argues against alcoholic ketoacidosis. Rare causes of elevated anion gap acidosis include toluene toxicity, acetaminophen poisoning, and ingestion of other alcohols. Toluene is metabolized to hippuric acid, and acetaminophen toxicity and associated glutathione depletion can lead to 5‐oxoproline accumulation, producing an anion gap. Patients who abuse alcohol are at risk for acetaminophen toxicity even at doses considered normal. However, this degree of encephalopathy would be unusual for acetaminophen toxicity unless liver failure had developed or unless there was another ingestion that might alter sensorium. Furthermore, the elevated osmolar gap is not a feature of acetaminophen poisoning. I would monitor liver enzyme tests and consider a serum ammonia level, but would not attribute the entire picture to acetaminophen.
The combination of elevated anion gap with an elevated osmolar gap narrows the diagnostic possibilities. Ingestion of several alcohols (ethanol, methanol, ethylene glycol, diethylene glycol) or toluene could produce these abnormalities. Of note, the osmolar gap is typically most markedly elevated early in methanol and ethylene glycol ingestions, and then as the parent compound is metabolized, the osmolar gap closes and the accumulation of metabolites produces the anion gap. Hallucinations are more common with methanol and toluene, and renal failure is more typical of ethylene glycol or toluene. The lack of oxalate crystalluria does not exclude ethylene glycol poisoning. Unfortunately, urine testing for oxalate crystals or fluorescein examination are neither sensitive nor specific enough to diagnosis ethylene glycol toxicity reliably. In most hospitals, assays used for serum testing for alcohols are insensitive, and require confirmation with gas chromatography performed at a specialty lab.
Additional history might reveal the likely culprit or culprits. Inhalant abuse including huffing would point to toluene or organic acid exposure. Solvent ingestion (eg, antifreeze, brake fluid) would suggest methanol or ethylene glycol. Absent this history, I remain suspicious for poisoning with methanol or ethylene glycol and would consider empiric treatment after urgent consultation with a medical toxicologist. A careful ophthalmologic exam might demonstrate characteristic features of methanol poisoning. Serum samples should be sent to a regional lab for analysis for alcohols and organic acids.
He was admitted to the intensive care unit, and empiric antibiotics started. He was empirically started on N‐acetylcysteine and sodium bicarbonate drips. However, his acidemia persisted and he required hemodialysis, which was initiated 12 hours after initial presentation. His acidemia and mental status quickly improved after hemodialysis. He was extubated on hospital day 2 and no longer required hemodialysis.
The differential diagnosis at this point consists of 3 main possibilities: ingestion of methanol, ethylene glycol, or inhalant abuse such as from toluene. The normal hippuric acid level points away from toluene, whereas serum levels can be misleading in the alcohol poisonings. Other discriminating features to consider include exposure history and unique clinical aspects. In this patient, an exposure history is lacking, but 4 clinical features stand out: visual hallucinations, acute kidney injury, mild lactic acidosis, and rapid improvement with hemodialysis. Both ethylene glycol and methanol toxicity may produce a mild lactic acidosis by increasing hepatic metabolism of pyruvate to lactate, and both are rapidly cleared by dialysis. Although it is tempting to place methanol at the top of the list of possibilities due to the report of visual hallucinations, the subjective visual complaints without objective exam corollaries (loss of visual acuity, abnormal pupillary reflexes, or optic disc hyperemia) are nonspecific and might be provoked by alcohol or an inhalant. Furthermore, the acute renal failure is much more typical of ethylene glycol, and thus I would consider ethylene glycol as being the more likely of the ingestions. Coingestion of multiple alcohols is a possibility, but it would be statistically less likely. Confirmation of ethylene glycol poisoning would consist of further insight into his exposures and measurement of levels using gas chromatography.
A urine sample from his emergency department presentation was sent to an outside lab for organic acid levels. Based on high clinical suspicion for 5‐oxoprolinemia (pyroglutamic acidemia) the patient was counseled to avoid any acetaminophen. His primary care provider was informed of this and acetaminophen was added as an adverse drug reaction. The patient left against medical advice soon after extubation. Following discharge, his 5‐oxoproline (pyroglutamic acid) level returned markedly elevated at greater than 10,000 mmol/mol creatinine (200 times the upper limit of normal).
Elevations in 5‐oxoproline levels in this patient most likely stem from glutathione depletion related to chronic acetaminophen use. Alcohol use and malnutrition may have heightened this patient's susceptibility. Despite the common occurrence of acetaminophen use in alcohol abusers or the malnourished, the rarity of severe 5‐oxoproline toxicity suggests unknown factors may be present in predisposed individuals, or under‐recognition. Although acetaminophen‐induced hepatotoxicity may occur along with 5‐oxoprolinemia, this does not always occur.
Several features led me away from this syndrome. First, its rarity lowered my pretest probability. Second, the lack of exposure history and details about the serum assays, specifically whether the measurements were confirmed by gas chromatography, reduced my confidence in eliminating more common ingestions. Third, several aspects proved to be less useful discriminating features: the mild elevation in osmolar gap, renal failure, and hallucinations, which in retrospect proved to be nonspecific.
The patient admitted that he had a longstanding use of acetaminophen in addition to using his girlfriend's acetaminophen‐hydrocodone. He had significant weight loss of over 50 pounds over the previous year, which he attributed to poor appetite. On further chart review, he had been admitted 3 times with a similar clinical presentation and recovered quickly with intensive and supportive care, with no etiology found at those times. He had 2 subsequent hospital admissions for altered mental status and respiratory failure, and his final hospitalization resulted in cardiac arrest and death.
DISCUSSION
5‐Oxoprolinemia is a rare, but potentially lethal cause of severe anion gap metabolic acidosis.[1, 2] The mechanism is thought to be impairment of glutathione metabolism, in the context of other predisposing factors. This can be a congenital error of metabolism, or can be acquired and exacerbated by acetaminophen use. Ingestion of acetaminophen leads to glutathione depletion, which in turn may precipitate accumulation of pyroglutamic acid and subsequent anion gap metabolic acidosis (Figure 1). Additional risk factors that may predispose patients to this condition include malnutrition, renal insufficiency, concurrent infection, and female gender.[1, 2, 3]
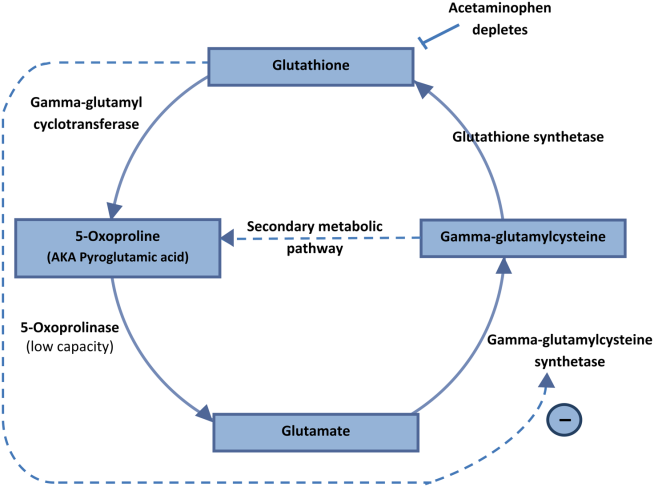
The diagnosis of 5‐oxoprolinemia is made via urine or serum organic acid analysis, testing routinely performed in pediatric populations when screening for congenital metabolic disorders. The pathophysiology suggests that obtaining a urine sample early in presentation, when acidosis is greatest, would lead to the highest 5‐oxoproline levels and best chance for diagnosis. Case patients have had normal levels prior to and in convalescent phases after the acute episode.[4] Given the long turnaround time for lab testing, presumptive diagnosis and treatment may be necessary.
Treatment of 5‐oxoprolinemia is primarily supportive, aimed at the metabolic acidosis. Fluid resuscitation and bicarbonate therapy are reasonable temporizing measures. Hemodialysis can clear 5‐oxoproline and may be indicated in severe acidosis.[5] Furthermore, the proposed pathophysiology suggests that administration of N‐acetylcysteine (NAC) may help to address the underlying process, but there are no trials to support a specific dosing regimen. However, given the fulminant presentation and common competing concern for acetaminophen toxicity, it is reasonable to initiate NAC aimed at treatment for possible acetaminophen overdose. Prevention of recurrence includes avoidance of acetaminophen, and counseling the patient to avoid acetaminophen in prescription combination medications and over‐the‐counter preparations.
Recent regulatory changes regarding acetaminophen/opioid combinations may reduce the incidence of 5‐oxoprolinemia. The US Food and Drug Administration has taken action to reduce adverse effects from acetaminophen exposure by limiting the amount of acetaminophen in opioid combination pills from 500 mg to a maximum of 325 mg per pill. This is aimed at preventing hepatotoxicity from ingestion of higher‐than‐recommended doses. However, clinicians should remember that 5‐oxoprolinemia can result from ingestion of acetaminophen at therapeutic levels.
Given its rare incidence, low clinical suspicion, and transient nature of confirmatory testing, it is likely this remains an underdiagnosed syndrome. In the case discussed, subsequent chart review demonstrated 5 previous admissions in multiple hospitals for severe transient anion gap acidosis. The likelihood that 5‐oxoprolinemia was missed in each of these cases supports a lack of awareness of this syndrome. In this patient, the discussant appropriately identified the possibility of 5‐oxoproline toxicity, but felt ethylene glycol ingestion was more likely. As this case underscores, a cornerstone in the management of suspected ingestions is empiric treatment for the most likely etiologies. Here, treatment for acetaminophen overdose and for methanol or ethylene glycol were warranted, and fortunately also addressed the rarer possibility of 5‐oxoproline toxicity.
The mnemonic MUDPILES is commonly used to identify possible causes of life‐threatening anion gap metabolic acidosis, as such heuristics have benefits in rapidly generating a differential diagnosis to guide initial evaluation. Given the fact that the traditional letter P (paraldehyde) in MUDPILES is no longer clinically utilized, some authors have suggested replacing this with pyroglutamic acid (a synonym of 5‐oxoproline). Such a change may help providers who have ruled out other causes of a high anion gap metabolic acidosis, facilitating diagnosis of this life‐threatening syndrome. In any case, clinicians must be mindful that simple memory aids may mislead clinicians, and a complete differential diagnosis may require more than a mnemonic.
TEACHING POINTS
- Acetaminophen use, even at therapeutic levels, can lead to 5‐oxoprolinemia, a potentially lethal anion gap metabolic acidosis.
- 5‐oxoprolinemia is likely related to glutathione depletion, worsened by acetaminophen, malnutrition, renal insufficiency, female gender, and infection. This implies theoretical benefit from administration of NAC for glutathione repletion.
- Mnemonics can be useful, but have limitations by way of oversimplification. This case suggests that changing the letter P in MUDPILES from paraldehyde to pyroglutamic acid could reduce underdiagnosis.
Disclosure: Nothing to report.
- , , , , . 5‐oxoprolinemia causing elevated anion gap metabolic acidosis in the setting of acetaminophen use. J Emerg Med. 2012;43(1):54–57.
- , , , . What is the clinical significance of 5‐oxoproline (pyroglutamic acid) in high anion gap metabolic acidosis following paracetamol (acetaminophen) exposure? Clin Toxicol (Phila). 2013;51(9):817–827.
- , , , , . Increased anion gap metabolic acidosis as a result of 5‐oxoproline (pyroglutamic acid): a role for acetaminophen. Clin J Am Soc Nephrol. 2006;1(3):441–447.
- , , , et al. Recurrent high anion gap metabolic acidosis secondary to 5‐oxoproline (pyroglutamic acid). Am J Kidney Dis. 2005;46(1):e4–e10.
- , , . Profound metabolic acidosis from pyroglutamic acidemia: an underappreciated cause of high anion gap metabolic acidosis. CJEM. 2010;12(5):449–452.
A 51‐year‐old man presented to the emergency department after 1 day of progressive dyspnea and increasing confusion.
Acute dyspnea most commonly stems from a cardiac or pulmonary disorder such as heart failure, acute coronary syndrome, pneumonia, pulmonary embolism, or exacerbations of asthma or chronic obstructive pulmonary disease. Less frequent cardiopulmonary considerations include pericardial or pleural effusion, pneumothorax, aspiration, and upper airway obstruction. Dyspnea might also be the initial manifestation of profound anemia or metabolic acidosis.
The presence of confusion suggests either a severe presentation of any of the aforementioned possibilities (with confusion resulting from hypoxia, hypercapnia, or hypotension); a multiorgan illness such as sepsis, malignancy, thromboembolic disease, vasculitis, thyroid dysfunction, or toxic ingestion; or a metabolic derangement related to the underlying cause of dyspnea (for example, hypercalcemia or hyponatremia associated with lung cancer).
Twelve hours prior to presentation, he started to have visual hallucinations. He denied fever, chills, cough, chest discomfort, palpitations, weight gain, headache, neck pain, or weakness.
Visual hallucinations could result from a toxic‐metabolic encephalopathy, such as drug overdose or withdrawal, liver or kidney failure, or hypoxia. A structural brain abnormality may also manifest with visual hallucination. Acute onset at age 51 and the absence of auditory hallucinations argue against a neurodegenerative illness and a primary psychiatric disturbance, respectively.
Episodic hallucinations would support the possibility of seizures, monocular hallucinations would point to a retinal or ocular problem, and a description of yellow‐green hue would suggest a side effect of digoxin.
His past medical history was remarkable for diet‐controlled type 2 diabetes mellitus, hypertension, hyperlipidemia, and chronic low back pain. His medications included metoprolol tartrate 25 mg twice daily, omeprazole 40 mg daily, baclofen 15 mg twice daily, oxycodone 30 mg 3 times daily, and hydrocodone 10 mg/acetaminophen 325 mg, 2 tablets 3 times daily as needed for back pain. He was a smoker with a 30 pack‐year history. He had a history of alcohol and cocaine use, but denied any recent substance use. He had no known history of obstructive pulmonary disease.
The patient takes 3 medications well known to cause confusion and hallucinations (oxycodone, hydrocodone, and baclofen), especially when they accumulate due to excessive ingestion or impaired clearance. Although these medications may suppress ventilatory drive, dyspnea would not be a common presenting complaint. He has risk factors for ischemic heart disease and cardiomyopathy, and his smoking history raises the possibility of malignancy.
On exam, the patient's temperature was 94.4C, heart rate 128 beats per minute, respiration rate 28 breaths per minute, blood pressure 155/63 mm Hg, and oxygen saturation 100% while breathing ambient air. The patient was cachectic and appeared in moderate respiratory distress. His pupils were equal and reactive to light, and extraocular movements were intact. He did not have scleral icterus, or cervical or clavicular lymphadenopathy. His oropharynx was negative for erythema, edema, or exudate. His cardiovascular exam revealed a regular tachycardia without rubs or diastolic gallops. There was a 2/6 systolic murmur heard best at left sternal border, without radiation. He did not have jugular venous distention. His pulmonary exam was notable for tachypnea but with normal vesicular breath sounds throughout. He did not have stridor, wheezing, rhonchi, or rales. His abdomen had normal bowel tones and was soft without tenderness, distention, or organomegaly. His extremities were warm, revealed normal pulses, and no edema was present. His joints were cool to palpation, without effusion. On neurologic exam, he was oriented to person and place and able to answer yes/no questions, but unable to provide detailed history. His speech was fluent. His motor exam was without focal deficits. His skin was without any notable lesions.
The constellation of findings does not point to a specific toxidrome. The finding of warm extremities in a hypothermic patient suggests heat loss due to inappropriate peripheral vasodilation. In the absence of vasodilators or features of aortic insufficiency, sepsis becomes a leading consideration. Infection could result in hypothermia and altered sensorium, and accompanying lactic acidosis could trigger tachypnea.
Shortly after admission, he became more somnolent and developed progressive respiratory distress, requiring intubation. Arterial blood gas revealed a pH of 6.93, PaCO2<20 mm Hg, PaO2 127 mm Hg, and HCO3<5 mEq/L. Other laboratory results included a lactate of 4.1 mmol/L, blood urea nitrogen 49 mg/dL, creatinine 2.3 mg/dL (0.8 at 1 month prior), sodium level of 143 mmol/L, chloride of 106 mmol/L, and bicarbonate level of <5 mg/dL. His aspartate aminotransferase was 34 IU/L, alanine transaminase was 28 IU/L, total bilirubin was 0.6 mg/dL, International Normalized Ratio was 1.3. A complete blood count revealed a white blood cell count of 23,000/L, hemoglobin of 10.6 g/dL, and platelet count of 454,000/L. A urinalysis was unremarkable. Cultures of blood, urine, and sputum were collected. Head computed tomography was negative.
This patient has a combined anion gap and nongap metabolic acidosis, as well as respiratory alkalosis. Although his acute kidney failure could produce these 2 types of metabolic acidosis, the modest elevation of the serum creatinine is not commensurate with such profound acidosis. Similarly, sepsis without hypotension or more striking elevation in lactate levels would not account for the entirety of the acidosis. Severe diabetic ketoacidosis can result in profound metabolic acidosis, and marked hyperglycemia or hyperosmolarity could result in somnolence; however, his diabetes has been controlled without medication and there is no obvious precipitant for an episode of ketoacidosis.
Remaining causes of anion gap acidosis include ingestion of methanol, ethylene glycol, ethanol, or salicylates. A careful history of ingestions and medications from witnesses including any prehospital personnel might suggest a source of intoxication. Absent this information, the hypothermia favors an ingestion of an alcohol over salicylates, and the lack of urine crystals and the presence of prominent visual hallucinations would point more toward methanol poisoning than ethylene glycol. A serum osmolarity measurement would allow determination of the osmolar gap, which would be elevated in the setting of methanol or ethylene glycol poisoning. If he were this ill from ethanol, I would have expected to see evidence of hepatotoxicity.
I would administer sodium bicarbonate to reverse the acidosis and to promote renal clearance of salicylates, methanol, ethylene glycol, and their metabolites. Orogastric decontamination with activated charcoal should be considered. If the osmolar gap is elevated, I would also administer intravenous fomepizole to attempt to reverse methanol or ethylene glycol poisoning. I would not delay treatment while waiting for these serum levels to return.
Initial serologic toxicology performed in the emergency department revealed negative ethanol, salicylates, and ketones. His osmolar gap was 13 mOsm/kg. His acetaminophen level was 69 g/mL (normal <120 g/mL). A creatinine phosphokinase was 84 IU/L and myoglobin was 93 ng/mL. His subsequent serum toxicology screen was negative for methanol, ethylene glycol, isopropranol, and hippuric acid. Urine toxicology was positive for opiates, but negative for amphetamine, benzodiazepine, cannabinoid, and cocaine.
Serum and urine ketone assays typically involve the nitroprusside reaction and detect acetoacetate, but not ‐hydroxybutyrate, and can lead to negative test results early in diabetic or alcoholic ketoacidosis. However, the normal ethanol level argues against alcoholic ketoacidosis. Rare causes of elevated anion gap acidosis include toluene toxicity, acetaminophen poisoning, and ingestion of other alcohols. Toluene is metabolized to hippuric acid, and acetaminophen toxicity and associated glutathione depletion can lead to 5‐oxoproline accumulation, producing an anion gap. Patients who abuse alcohol are at risk for acetaminophen toxicity even at doses considered normal. However, this degree of encephalopathy would be unusual for acetaminophen toxicity unless liver failure had developed or unless there was another ingestion that might alter sensorium. Furthermore, the elevated osmolar gap is not a feature of acetaminophen poisoning. I would monitor liver enzyme tests and consider a serum ammonia level, but would not attribute the entire picture to acetaminophen.
The combination of elevated anion gap with an elevated osmolar gap narrows the diagnostic possibilities. Ingestion of several alcohols (ethanol, methanol, ethylene glycol, diethylene glycol) or toluene could produce these abnormalities. Of note, the osmolar gap is typically most markedly elevated early in methanol and ethylene glycol ingestions, and then as the parent compound is metabolized, the osmolar gap closes and the accumulation of metabolites produces the anion gap. Hallucinations are more common with methanol and toluene, and renal failure is more typical of ethylene glycol or toluene. The lack of oxalate crystalluria does not exclude ethylene glycol poisoning. Unfortunately, urine testing for oxalate crystals or fluorescein examination are neither sensitive nor specific enough to diagnosis ethylene glycol toxicity reliably. In most hospitals, assays used for serum testing for alcohols are insensitive, and require confirmation with gas chromatography performed at a specialty lab.
Additional history might reveal the likely culprit or culprits. Inhalant abuse including huffing would point to toluene or organic acid exposure. Solvent ingestion (eg, antifreeze, brake fluid) would suggest methanol or ethylene glycol. Absent this history, I remain suspicious for poisoning with methanol or ethylene glycol and would consider empiric treatment after urgent consultation with a medical toxicologist. A careful ophthalmologic exam might demonstrate characteristic features of methanol poisoning. Serum samples should be sent to a regional lab for analysis for alcohols and organic acids.
He was admitted to the intensive care unit, and empiric antibiotics started. He was empirically started on N‐acetylcysteine and sodium bicarbonate drips. However, his acidemia persisted and he required hemodialysis, which was initiated 12 hours after initial presentation. His acidemia and mental status quickly improved after hemodialysis. He was extubated on hospital day 2 and no longer required hemodialysis.
The differential diagnosis at this point consists of 3 main possibilities: ingestion of methanol, ethylene glycol, or inhalant abuse such as from toluene. The normal hippuric acid level points away from toluene, whereas serum levels can be misleading in the alcohol poisonings. Other discriminating features to consider include exposure history and unique clinical aspects. In this patient, an exposure history is lacking, but 4 clinical features stand out: visual hallucinations, acute kidney injury, mild lactic acidosis, and rapid improvement with hemodialysis. Both ethylene glycol and methanol toxicity may produce a mild lactic acidosis by increasing hepatic metabolism of pyruvate to lactate, and both are rapidly cleared by dialysis. Although it is tempting to place methanol at the top of the list of possibilities due to the report of visual hallucinations, the subjective visual complaints without objective exam corollaries (loss of visual acuity, abnormal pupillary reflexes, or optic disc hyperemia) are nonspecific and might be provoked by alcohol or an inhalant. Furthermore, the acute renal failure is much more typical of ethylene glycol, and thus I would consider ethylene glycol as being the more likely of the ingestions. Coingestion of multiple alcohols is a possibility, but it would be statistically less likely. Confirmation of ethylene glycol poisoning would consist of further insight into his exposures and measurement of levels using gas chromatography.
A urine sample from his emergency department presentation was sent to an outside lab for organic acid levels. Based on high clinical suspicion for 5‐oxoprolinemia (pyroglutamic acidemia) the patient was counseled to avoid any acetaminophen. His primary care provider was informed of this and acetaminophen was added as an adverse drug reaction. The patient left against medical advice soon after extubation. Following discharge, his 5‐oxoproline (pyroglutamic acid) level returned markedly elevated at greater than 10,000 mmol/mol creatinine (200 times the upper limit of normal).
Elevations in 5‐oxoproline levels in this patient most likely stem from glutathione depletion related to chronic acetaminophen use. Alcohol use and malnutrition may have heightened this patient's susceptibility. Despite the common occurrence of acetaminophen use in alcohol abusers or the malnourished, the rarity of severe 5‐oxoproline toxicity suggests unknown factors may be present in predisposed individuals, or under‐recognition. Although acetaminophen‐induced hepatotoxicity may occur along with 5‐oxoprolinemia, this does not always occur.
Several features led me away from this syndrome. First, its rarity lowered my pretest probability. Second, the lack of exposure history and details about the serum assays, specifically whether the measurements were confirmed by gas chromatography, reduced my confidence in eliminating more common ingestions. Third, several aspects proved to be less useful discriminating features: the mild elevation in osmolar gap, renal failure, and hallucinations, which in retrospect proved to be nonspecific.
The patient admitted that he had a longstanding use of acetaminophen in addition to using his girlfriend's acetaminophen‐hydrocodone. He had significant weight loss of over 50 pounds over the previous year, which he attributed to poor appetite. On further chart review, he had been admitted 3 times with a similar clinical presentation and recovered quickly with intensive and supportive care, with no etiology found at those times. He had 2 subsequent hospital admissions for altered mental status and respiratory failure, and his final hospitalization resulted in cardiac arrest and death.
DISCUSSION
5‐Oxoprolinemia is a rare, but potentially lethal cause of severe anion gap metabolic acidosis.[1, 2] The mechanism is thought to be impairment of glutathione metabolism, in the context of other predisposing factors. This can be a congenital error of metabolism, or can be acquired and exacerbated by acetaminophen use. Ingestion of acetaminophen leads to glutathione depletion, which in turn may precipitate accumulation of pyroglutamic acid and subsequent anion gap metabolic acidosis (Figure 1). Additional risk factors that may predispose patients to this condition include malnutrition, renal insufficiency, concurrent infection, and female gender.[1, 2, 3]
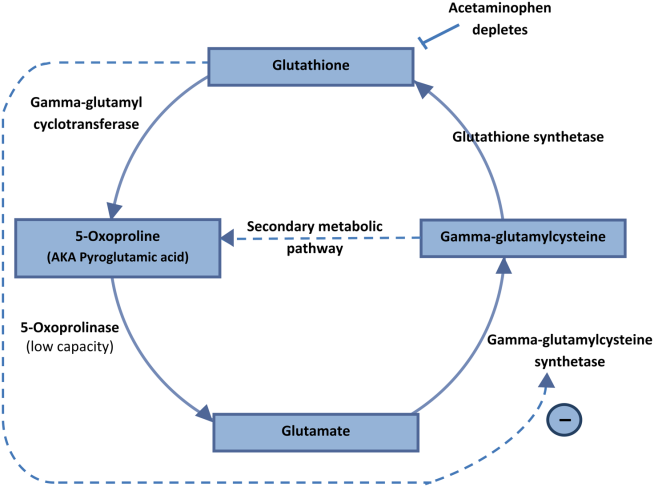
The diagnosis of 5‐oxoprolinemia is made via urine or serum organic acid analysis, testing routinely performed in pediatric populations when screening for congenital metabolic disorders. The pathophysiology suggests that obtaining a urine sample early in presentation, when acidosis is greatest, would lead to the highest 5‐oxoproline levels and best chance for diagnosis. Case patients have had normal levels prior to and in convalescent phases after the acute episode.[4] Given the long turnaround time for lab testing, presumptive diagnosis and treatment may be necessary.
Treatment of 5‐oxoprolinemia is primarily supportive, aimed at the metabolic acidosis. Fluid resuscitation and bicarbonate therapy are reasonable temporizing measures. Hemodialysis can clear 5‐oxoproline and may be indicated in severe acidosis.[5] Furthermore, the proposed pathophysiology suggests that administration of N‐acetylcysteine (NAC) may help to address the underlying process, but there are no trials to support a specific dosing regimen. However, given the fulminant presentation and common competing concern for acetaminophen toxicity, it is reasonable to initiate NAC aimed at treatment for possible acetaminophen overdose. Prevention of recurrence includes avoidance of acetaminophen, and counseling the patient to avoid acetaminophen in prescription combination medications and over‐the‐counter preparations.
Recent regulatory changes regarding acetaminophen/opioid combinations may reduce the incidence of 5‐oxoprolinemia. The US Food and Drug Administration has taken action to reduce adverse effects from acetaminophen exposure by limiting the amount of acetaminophen in opioid combination pills from 500 mg to a maximum of 325 mg per pill. This is aimed at preventing hepatotoxicity from ingestion of higher‐than‐recommended doses. However, clinicians should remember that 5‐oxoprolinemia can result from ingestion of acetaminophen at therapeutic levels.
Given its rare incidence, low clinical suspicion, and transient nature of confirmatory testing, it is likely this remains an underdiagnosed syndrome. In the case discussed, subsequent chart review demonstrated 5 previous admissions in multiple hospitals for severe transient anion gap acidosis. The likelihood that 5‐oxoprolinemia was missed in each of these cases supports a lack of awareness of this syndrome. In this patient, the discussant appropriately identified the possibility of 5‐oxoproline toxicity, but felt ethylene glycol ingestion was more likely. As this case underscores, a cornerstone in the management of suspected ingestions is empiric treatment for the most likely etiologies. Here, treatment for acetaminophen overdose and for methanol or ethylene glycol were warranted, and fortunately also addressed the rarer possibility of 5‐oxoproline toxicity.
The mnemonic MUDPILES is commonly used to identify possible causes of life‐threatening anion gap metabolic acidosis, as such heuristics have benefits in rapidly generating a differential diagnosis to guide initial evaluation. Given the fact that the traditional letter P (paraldehyde) in MUDPILES is no longer clinically utilized, some authors have suggested replacing this with pyroglutamic acid (a synonym of 5‐oxoproline). Such a change may help providers who have ruled out other causes of a high anion gap metabolic acidosis, facilitating diagnosis of this life‐threatening syndrome. In any case, clinicians must be mindful that simple memory aids may mislead clinicians, and a complete differential diagnosis may require more than a mnemonic.
TEACHING POINTS
- Acetaminophen use, even at therapeutic levels, can lead to 5‐oxoprolinemia, a potentially lethal anion gap metabolic acidosis.
- 5‐oxoprolinemia is likely related to glutathione depletion, worsened by acetaminophen, malnutrition, renal insufficiency, female gender, and infection. This implies theoretical benefit from administration of NAC for glutathione repletion.
- Mnemonics can be useful, but have limitations by way of oversimplification. This case suggests that changing the letter P in MUDPILES from paraldehyde to pyroglutamic acid could reduce underdiagnosis.
Disclosure: Nothing to report.
A 51‐year‐old man presented to the emergency department after 1 day of progressive dyspnea and increasing confusion.
Acute dyspnea most commonly stems from a cardiac or pulmonary disorder such as heart failure, acute coronary syndrome, pneumonia, pulmonary embolism, or exacerbations of asthma or chronic obstructive pulmonary disease. Less frequent cardiopulmonary considerations include pericardial or pleural effusion, pneumothorax, aspiration, and upper airway obstruction. Dyspnea might also be the initial manifestation of profound anemia or metabolic acidosis.
The presence of confusion suggests either a severe presentation of any of the aforementioned possibilities (with confusion resulting from hypoxia, hypercapnia, or hypotension); a multiorgan illness such as sepsis, malignancy, thromboembolic disease, vasculitis, thyroid dysfunction, or toxic ingestion; or a metabolic derangement related to the underlying cause of dyspnea (for example, hypercalcemia or hyponatremia associated with lung cancer).
Twelve hours prior to presentation, he started to have visual hallucinations. He denied fever, chills, cough, chest discomfort, palpitations, weight gain, headache, neck pain, or weakness.
Visual hallucinations could result from a toxic‐metabolic encephalopathy, such as drug overdose or withdrawal, liver or kidney failure, or hypoxia. A structural brain abnormality may also manifest with visual hallucination. Acute onset at age 51 and the absence of auditory hallucinations argue against a neurodegenerative illness and a primary psychiatric disturbance, respectively.
Episodic hallucinations would support the possibility of seizures, monocular hallucinations would point to a retinal or ocular problem, and a description of yellow‐green hue would suggest a side effect of digoxin.
His past medical history was remarkable for diet‐controlled type 2 diabetes mellitus, hypertension, hyperlipidemia, and chronic low back pain. His medications included metoprolol tartrate 25 mg twice daily, omeprazole 40 mg daily, baclofen 15 mg twice daily, oxycodone 30 mg 3 times daily, and hydrocodone 10 mg/acetaminophen 325 mg, 2 tablets 3 times daily as needed for back pain. He was a smoker with a 30 pack‐year history. He had a history of alcohol and cocaine use, but denied any recent substance use. He had no known history of obstructive pulmonary disease.
The patient takes 3 medications well known to cause confusion and hallucinations (oxycodone, hydrocodone, and baclofen), especially when they accumulate due to excessive ingestion or impaired clearance. Although these medications may suppress ventilatory drive, dyspnea would not be a common presenting complaint. He has risk factors for ischemic heart disease and cardiomyopathy, and his smoking history raises the possibility of malignancy.
On exam, the patient's temperature was 94.4C, heart rate 128 beats per minute, respiration rate 28 breaths per minute, blood pressure 155/63 mm Hg, and oxygen saturation 100% while breathing ambient air. The patient was cachectic and appeared in moderate respiratory distress. His pupils were equal and reactive to light, and extraocular movements were intact. He did not have scleral icterus, or cervical or clavicular lymphadenopathy. His oropharynx was negative for erythema, edema, or exudate. His cardiovascular exam revealed a regular tachycardia without rubs or diastolic gallops. There was a 2/6 systolic murmur heard best at left sternal border, without radiation. He did not have jugular venous distention. His pulmonary exam was notable for tachypnea but with normal vesicular breath sounds throughout. He did not have stridor, wheezing, rhonchi, or rales. His abdomen had normal bowel tones and was soft without tenderness, distention, or organomegaly. His extremities were warm, revealed normal pulses, and no edema was present. His joints were cool to palpation, without effusion. On neurologic exam, he was oriented to person and place and able to answer yes/no questions, but unable to provide detailed history. His speech was fluent. His motor exam was without focal deficits. His skin was without any notable lesions.
The constellation of findings does not point to a specific toxidrome. The finding of warm extremities in a hypothermic patient suggests heat loss due to inappropriate peripheral vasodilation. In the absence of vasodilators or features of aortic insufficiency, sepsis becomes a leading consideration. Infection could result in hypothermia and altered sensorium, and accompanying lactic acidosis could trigger tachypnea.
Shortly after admission, he became more somnolent and developed progressive respiratory distress, requiring intubation. Arterial blood gas revealed a pH of 6.93, PaCO2<20 mm Hg, PaO2 127 mm Hg, and HCO3<5 mEq/L. Other laboratory results included a lactate of 4.1 mmol/L, blood urea nitrogen 49 mg/dL, creatinine 2.3 mg/dL (0.8 at 1 month prior), sodium level of 143 mmol/L, chloride of 106 mmol/L, and bicarbonate level of <5 mg/dL. His aspartate aminotransferase was 34 IU/L, alanine transaminase was 28 IU/L, total bilirubin was 0.6 mg/dL, International Normalized Ratio was 1.3. A complete blood count revealed a white blood cell count of 23,000/L, hemoglobin of 10.6 g/dL, and platelet count of 454,000/L. A urinalysis was unremarkable. Cultures of blood, urine, and sputum were collected. Head computed tomography was negative.
This patient has a combined anion gap and nongap metabolic acidosis, as well as respiratory alkalosis. Although his acute kidney failure could produce these 2 types of metabolic acidosis, the modest elevation of the serum creatinine is not commensurate with such profound acidosis. Similarly, sepsis without hypotension or more striking elevation in lactate levels would not account for the entirety of the acidosis. Severe diabetic ketoacidosis can result in profound metabolic acidosis, and marked hyperglycemia or hyperosmolarity could result in somnolence; however, his diabetes has been controlled without medication and there is no obvious precipitant for an episode of ketoacidosis.
Remaining causes of anion gap acidosis include ingestion of methanol, ethylene glycol, ethanol, or salicylates. A careful history of ingestions and medications from witnesses including any prehospital personnel might suggest a source of intoxication. Absent this information, the hypothermia favors an ingestion of an alcohol over salicylates, and the lack of urine crystals and the presence of prominent visual hallucinations would point more toward methanol poisoning than ethylene glycol. A serum osmolarity measurement would allow determination of the osmolar gap, which would be elevated in the setting of methanol or ethylene glycol poisoning. If he were this ill from ethanol, I would have expected to see evidence of hepatotoxicity.
I would administer sodium bicarbonate to reverse the acidosis and to promote renal clearance of salicylates, methanol, ethylene glycol, and their metabolites. Orogastric decontamination with activated charcoal should be considered. If the osmolar gap is elevated, I would also administer intravenous fomepizole to attempt to reverse methanol or ethylene glycol poisoning. I would not delay treatment while waiting for these serum levels to return.
Initial serologic toxicology performed in the emergency department revealed negative ethanol, salicylates, and ketones. His osmolar gap was 13 mOsm/kg. His acetaminophen level was 69 g/mL (normal <120 g/mL). A creatinine phosphokinase was 84 IU/L and myoglobin was 93 ng/mL. His subsequent serum toxicology screen was negative for methanol, ethylene glycol, isopropranol, and hippuric acid. Urine toxicology was positive for opiates, but negative for amphetamine, benzodiazepine, cannabinoid, and cocaine.
Serum and urine ketone assays typically involve the nitroprusside reaction and detect acetoacetate, but not ‐hydroxybutyrate, and can lead to negative test results early in diabetic or alcoholic ketoacidosis. However, the normal ethanol level argues against alcoholic ketoacidosis. Rare causes of elevated anion gap acidosis include toluene toxicity, acetaminophen poisoning, and ingestion of other alcohols. Toluene is metabolized to hippuric acid, and acetaminophen toxicity and associated glutathione depletion can lead to 5‐oxoproline accumulation, producing an anion gap. Patients who abuse alcohol are at risk for acetaminophen toxicity even at doses considered normal. However, this degree of encephalopathy would be unusual for acetaminophen toxicity unless liver failure had developed or unless there was another ingestion that might alter sensorium. Furthermore, the elevated osmolar gap is not a feature of acetaminophen poisoning. I would monitor liver enzyme tests and consider a serum ammonia level, but would not attribute the entire picture to acetaminophen.
The combination of elevated anion gap with an elevated osmolar gap narrows the diagnostic possibilities. Ingestion of several alcohols (ethanol, methanol, ethylene glycol, diethylene glycol) or toluene could produce these abnormalities. Of note, the osmolar gap is typically most markedly elevated early in methanol and ethylene glycol ingestions, and then as the parent compound is metabolized, the osmolar gap closes and the accumulation of metabolites produces the anion gap. Hallucinations are more common with methanol and toluene, and renal failure is more typical of ethylene glycol or toluene. The lack of oxalate crystalluria does not exclude ethylene glycol poisoning. Unfortunately, urine testing for oxalate crystals or fluorescein examination are neither sensitive nor specific enough to diagnosis ethylene glycol toxicity reliably. In most hospitals, assays used for serum testing for alcohols are insensitive, and require confirmation with gas chromatography performed at a specialty lab.
Additional history might reveal the likely culprit or culprits. Inhalant abuse including huffing would point to toluene or organic acid exposure. Solvent ingestion (eg, antifreeze, brake fluid) would suggest methanol or ethylene glycol. Absent this history, I remain suspicious for poisoning with methanol or ethylene glycol and would consider empiric treatment after urgent consultation with a medical toxicologist. A careful ophthalmologic exam might demonstrate characteristic features of methanol poisoning. Serum samples should be sent to a regional lab for analysis for alcohols and organic acids.
He was admitted to the intensive care unit, and empiric antibiotics started. He was empirically started on N‐acetylcysteine and sodium bicarbonate drips. However, his acidemia persisted and he required hemodialysis, which was initiated 12 hours after initial presentation. His acidemia and mental status quickly improved after hemodialysis. He was extubated on hospital day 2 and no longer required hemodialysis.
The differential diagnosis at this point consists of 3 main possibilities: ingestion of methanol, ethylene glycol, or inhalant abuse such as from toluene. The normal hippuric acid level points away from toluene, whereas serum levels can be misleading in the alcohol poisonings. Other discriminating features to consider include exposure history and unique clinical aspects. In this patient, an exposure history is lacking, but 4 clinical features stand out: visual hallucinations, acute kidney injury, mild lactic acidosis, and rapid improvement with hemodialysis. Both ethylene glycol and methanol toxicity may produce a mild lactic acidosis by increasing hepatic metabolism of pyruvate to lactate, and both are rapidly cleared by dialysis. Although it is tempting to place methanol at the top of the list of possibilities due to the report of visual hallucinations, the subjective visual complaints without objective exam corollaries (loss of visual acuity, abnormal pupillary reflexes, or optic disc hyperemia) are nonspecific and might be provoked by alcohol or an inhalant. Furthermore, the acute renal failure is much more typical of ethylene glycol, and thus I would consider ethylene glycol as being the more likely of the ingestions. Coingestion of multiple alcohols is a possibility, but it would be statistically less likely. Confirmation of ethylene glycol poisoning would consist of further insight into his exposures and measurement of levels using gas chromatography.
A urine sample from his emergency department presentation was sent to an outside lab for organic acid levels. Based on high clinical suspicion for 5‐oxoprolinemia (pyroglutamic acidemia) the patient was counseled to avoid any acetaminophen. His primary care provider was informed of this and acetaminophen was added as an adverse drug reaction. The patient left against medical advice soon after extubation. Following discharge, his 5‐oxoproline (pyroglutamic acid) level returned markedly elevated at greater than 10,000 mmol/mol creatinine (200 times the upper limit of normal).
Elevations in 5‐oxoproline levels in this patient most likely stem from glutathione depletion related to chronic acetaminophen use. Alcohol use and malnutrition may have heightened this patient's susceptibility. Despite the common occurrence of acetaminophen use in alcohol abusers or the malnourished, the rarity of severe 5‐oxoproline toxicity suggests unknown factors may be present in predisposed individuals, or under‐recognition. Although acetaminophen‐induced hepatotoxicity may occur along with 5‐oxoprolinemia, this does not always occur.
Several features led me away from this syndrome. First, its rarity lowered my pretest probability. Second, the lack of exposure history and details about the serum assays, specifically whether the measurements were confirmed by gas chromatography, reduced my confidence in eliminating more common ingestions. Third, several aspects proved to be less useful discriminating features: the mild elevation in osmolar gap, renal failure, and hallucinations, which in retrospect proved to be nonspecific.
The patient admitted that he had a longstanding use of acetaminophen in addition to using his girlfriend's acetaminophen‐hydrocodone. He had significant weight loss of over 50 pounds over the previous year, which he attributed to poor appetite. On further chart review, he had been admitted 3 times with a similar clinical presentation and recovered quickly with intensive and supportive care, with no etiology found at those times. He had 2 subsequent hospital admissions for altered mental status and respiratory failure, and his final hospitalization resulted in cardiac arrest and death.
DISCUSSION
5‐Oxoprolinemia is a rare, but potentially lethal cause of severe anion gap metabolic acidosis.[1, 2] The mechanism is thought to be impairment of glutathione metabolism, in the context of other predisposing factors. This can be a congenital error of metabolism, or can be acquired and exacerbated by acetaminophen use. Ingestion of acetaminophen leads to glutathione depletion, which in turn may precipitate accumulation of pyroglutamic acid and subsequent anion gap metabolic acidosis (Figure 1). Additional risk factors that may predispose patients to this condition include malnutrition, renal insufficiency, concurrent infection, and female gender.[1, 2, 3]
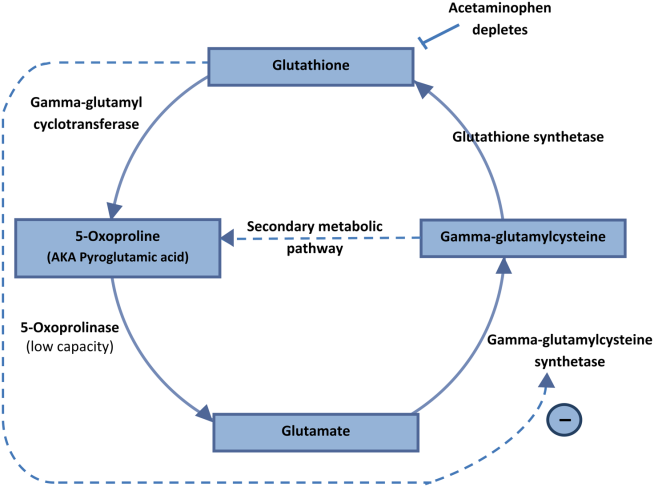
The diagnosis of 5‐oxoprolinemia is made via urine or serum organic acid analysis, testing routinely performed in pediatric populations when screening for congenital metabolic disorders. The pathophysiology suggests that obtaining a urine sample early in presentation, when acidosis is greatest, would lead to the highest 5‐oxoproline levels and best chance for diagnosis. Case patients have had normal levels prior to and in convalescent phases after the acute episode.[4] Given the long turnaround time for lab testing, presumptive diagnosis and treatment may be necessary.
Treatment of 5‐oxoprolinemia is primarily supportive, aimed at the metabolic acidosis. Fluid resuscitation and bicarbonate therapy are reasonable temporizing measures. Hemodialysis can clear 5‐oxoproline and may be indicated in severe acidosis.[5] Furthermore, the proposed pathophysiology suggests that administration of N‐acetylcysteine (NAC) may help to address the underlying process, but there are no trials to support a specific dosing regimen. However, given the fulminant presentation and common competing concern for acetaminophen toxicity, it is reasonable to initiate NAC aimed at treatment for possible acetaminophen overdose. Prevention of recurrence includes avoidance of acetaminophen, and counseling the patient to avoid acetaminophen in prescription combination medications and over‐the‐counter preparations.
Recent regulatory changes regarding acetaminophen/opioid combinations may reduce the incidence of 5‐oxoprolinemia. The US Food and Drug Administration has taken action to reduce adverse effects from acetaminophen exposure by limiting the amount of acetaminophen in opioid combination pills from 500 mg to a maximum of 325 mg per pill. This is aimed at preventing hepatotoxicity from ingestion of higher‐than‐recommended doses. However, clinicians should remember that 5‐oxoprolinemia can result from ingestion of acetaminophen at therapeutic levels.
Given its rare incidence, low clinical suspicion, and transient nature of confirmatory testing, it is likely this remains an underdiagnosed syndrome. In the case discussed, subsequent chart review demonstrated 5 previous admissions in multiple hospitals for severe transient anion gap acidosis. The likelihood that 5‐oxoprolinemia was missed in each of these cases supports a lack of awareness of this syndrome. In this patient, the discussant appropriately identified the possibility of 5‐oxoproline toxicity, but felt ethylene glycol ingestion was more likely. As this case underscores, a cornerstone in the management of suspected ingestions is empiric treatment for the most likely etiologies. Here, treatment for acetaminophen overdose and for methanol or ethylene glycol were warranted, and fortunately also addressed the rarer possibility of 5‐oxoproline toxicity.
The mnemonic MUDPILES is commonly used to identify possible causes of life‐threatening anion gap metabolic acidosis, as such heuristics have benefits in rapidly generating a differential diagnosis to guide initial evaluation. Given the fact that the traditional letter P (paraldehyde) in MUDPILES is no longer clinically utilized, some authors have suggested replacing this with pyroglutamic acid (a synonym of 5‐oxoproline). Such a change may help providers who have ruled out other causes of a high anion gap metabolic acidosis, facilitating diagnosis of this life‐threatening syndrome. In any case, clinicians must be mindful that simple memory aids may mislead clinicians, and a complete differential diagnosis may require more than a mnemonic.
TEACHING POINTS
- Acetaminophen use, even at therapeutic levels, can lead to 5‐oxoprolinemia, a potentially lethal anion gap metabolic acidosis.
- 5‐oxoprolinemia is likely related to glutathione depletion, worsened by acetaminophen, malnutrition, renal insufficiency, female gender, and infection. This implies theoretical benefit from administration of NAC for glutathione repletion.
- Mnemonics can be useful, but have limitations by way of oversimplification. This case suggests that changing the letter P in MUDPILES from paraldehyde to pyroglutamic acid could reduce underdiagnosis.
Disclosure: Nothing to report.
- , , , , . 5‐oxoprolinemia causing elevated anion gap metabolic acidosis in the setting of acetaminophen use. J Emerg Med. 2012;43(1):54–57.
- , , , . What is the clinical significance of 5‐oxoproline (pyroglutamic acid) in high anion gap metabolic acidosis following paracetamol (acetaminophen) exposure? Clin Toxicol (Phila). 2013;51(9):817–827.
- , , , , . Increased anion gap metabolic acidosis as a result of 5‐oxoproline (pyroglutamic acid): a role for acetaminophen. Clin J Am Soc Nephrol. 2006;1(3):441–447.
- , , , et al. Recurrent high anion gap metabolic acidosis secondary to 5‐oxoproline (pyroglutamic acid). Am J Kidney Dis. 2005;46(1):e4–e10.
- , , . Profound metabolic acidosis from pyroglutamic acidemia: an underappreciated cause of high anion gap metabolic acidosis. CJEM. 2010;12(5):449–452.
- , , , , . 5‐oxoprolinemia causing elevated anion gap metabolic acidosis in the setting of acetaminophen use. J Emerg Med. 2012;43(1):54–57.
- , , , . What is the clinical significance of 5‐oxoproline (pyroglutamic acid) in high anion gap metabolic acidosis following paracetamol (acetaminophen) exposure? Clin Toxicol (Phila). 2013;51(9):817–827.
- , , , , . Increased anion gap metabolic acidosis as a result of 5‐oxoproline (pyroglutamic acid): a role for acetaminophen. Clin J Am Soc Nephrol. 2006;1(3):441–447.
- , , , et al. Recurrent high anion gap metabolic acidosis secondary to 5‐oxoproline (pyroglutamic acid). Am J Kidney Dis. 2005;46(1):e4–e10.
- , , . Profound metabolic acidosis from pyroglutamic acidemia: an underappreciated cause of high anion gap metabolic acidosis. CJEM. 2010;12(5):449–452.