User login
VIDEO: Don’t miss reactions to these up and coming allergens
SONOMA, CALIF. – Skin reactions to components of baby wipes, cosmetics, leather, and even artificial hips or knees top an informal list of dermatoses caused by newer allergens for dermatologists to consider, Dr. Joseph F. Fowler Jr. said at the annual Coastal Dermatology Symposium.
He described some of these new allergens in a video interview at the symposium, jointly presented by the University of Louisville, Kentucky, and the Global Academy for Medical Education.
A relatively new preservative found in baby wipes and hair and skin products is one of the main culprits – methylisothiazolinone, said Dr. Fowler of the university. Bee glue (also called propolis) is another problematic material, found in some lip moisturizers and other personal-care products.
Shellac (the same shellac that’s often used as a furniture coating) in mascara and nail products can cause skin reactions, too.
Leather can cause dermatoses because of the chromium used in leather processing, but recent reports also point to cobalt, another product used in leather processing, as an allergen source, Dr. Fowler said.
Also, in rare cases, components of orthopedic implants are causing allergic reactions that sometimes necessitate removal of the implant, he added.
Dr. Fowler reported financial associations with Bayer, Valeant, Amgen, AbbVie, Allergan, Celgene, Galderma, Novartis, and Lilly. This publication and the Global Academy for Medical Education are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SONOMA, CALIF. – Skin reactions to components of baby wipes, cosmetics, leather, and even artificial hips or knees top an informal list of dermatoses caused by newer allergens for dermatologists to consider, Dr. Joseph F. Fowler Jr. said at the annual Coastal Dermatology Symposium.
He described some of these new allergens in a video interview at the symposium, jointly presented by the University of Louisville, Kentucky, and the Global Academy for Medical Education.
A relatively new preservative found in baby wipes and hair and skin products is one of the main culprits – methylisothiazolinone, said Dr. Fowler of the university. Bee glue (also called propolis) is another problematic material, found in some lip moisturizers and other personal-care products.
Shellac (the same shellac that’s often used as a furniture coating) in mascara and nail products can cause skin reactions, too.
Leather can cause dermatoses because of the chromium used in leather processing, but recent reports also point to cobalt, another product used in leather processing, as an allergen source, Dr. Fowler said.
Also, in rare cases, components of orthopedic implants are causing allergic reactions that sometimes necessitate removal of the implant, he added.
Dr. Fowler reported financial associations with Bayer, Valeant, Amgen, AbbVie, Allergan, Celgene, Galderma, Novartis, and Lilly. This publication and the Global Academy for Medical Education are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SONOMA, CALIF. – Skin reactions to components of baby wipes, cosmetics, leather, and even artificial hips or knees top an informal list of dermatoses caused by newer allergens for dermatologists to consider, Dr. Joseph F. Fowler Jr. said at the annual Coastal Dermatology Symposium.
He described some of these new allergens in a video interview at the symposium, jointly presented by the University of Louisville, Kentucky, and the Global Academy for Medical Education.
A relatively new preservative found in baby wipes and hair and skin products is one of the main culprits – methylisothiazolinone, said Dr. Fowler of the university. Bee glue (also called propolis) is another problematic material, found in some lip moisturizers and other personal-care products.
Shellac (the same shellac that’s often used as a furniture coating) in mascara and nail products can cause skin reactions, too.
Leather can cause dermatoses because of the chromium used in leather processing, but recent reports also point to cobalt, another product used in leather processing, as an allergen source, Dr. Fowler said.
Also, in rare cases, components of orthopedic implants are causing allergic reactions that sometimes necessitate removal of the implant, he added.
Dr. Fowler reported financial associations with Bayer, Valeant, Amgen, AbbVie, Allergan, Celgene, Galderma, Novartis, and Lilly. This publication and the Global Academy for Medical Education are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT THE COASTAL DERMATOLOGY SYMPOSIUM
VIDEO: Mayo Clinic app shortened hospitalizations
The Mayo Clinic handed iPads with an app called “myCare” to patients scheduled for surgery and showed that its use significantly reduced postsurgical length of stay, the total cost of care, and the need for home health care or skilled nursing care at discharge.
A study of 150 patients was so successful that the software, developed initially as an external software program for testing, is now being rebuilt into the institution’s systems so that it has a home in clinicians’ workflow, Dr. David J. Cook said at the Health 2.0 fall conference.
Dr. Cook, chair of cardiovascular anesthesiology at the Mayo Clinic, Rochester, Minn., describes the app in detail in this video interview. The app provides patients a customized plan of care including what they can expect daily, just-in-time education, self-assessment tools, and more. Results are transmitted wirelessly to a dashboard, where clinicians can track a patient’s progress, facilitating earlier intervention when needed.
Other investigators at the Mayo Clinic developed a separate online and smartphone-based app to help with rehabilitation of patients hospitalized after a heart attack and stent placement. The app functioned as a self-monitoring system that allowed patients to enter vital signs and to access educational content about steps they could take to reduce their risk of another heart attack.
During a 90-day study, 20% of 25 patients using the app were rehospitalized or admitted to an emergency department, compared with 60% of 19 patients in a control group who received conventional cardiac rehabilitation care without the app. The investigators reported the data at the American College of Cardiology earlier this year.
“We hope a tool like this will help us extend the reach of cardiac rehabilitation to all heart patients, but in particular, it could help patients in rural and underserved populations who might not be able to attend cardiac rehabilitation sessions,” Dr. R. Jay Widmer said in a statement released by the Mayo Clinic.
These and dozens of other apps and technological tools are being developed and tested is a systematic fashion through the Mayo Clinic’s Center for Innovation. In the video, Dr. Cook also describes the Center’s activities and previews another innovative tool in development.
Dr. Cook reported having no financial disclosures.
On Twitter @sherryboschert
The Mayo Clinic handed iPads with an app called “myCare” to patients scheduled for surgery and showed that its use significantly reduced postsurgical length of stay, the total cost of care, and the need for home health care or skilled nursing care at discharge.
A study of 150 patients was so successful that the software, developed initially as an external software program for testing, is now being rebuilt into the institution’s systems so that it has a home in clinicians’ workflow, Dr. David J. Cook said at the Health 2.0 fall conference.
Dr. Cook, chair of cardiovascular anesthesiology at the Mayo Clinic, Rochester, Minn., describes the app in detail in this video interview. The app provides patients a customized plan of care including what they can expect daily, just-in-time education, self-assessment tools, and more. Results are transmitted wirelessly to a dashboard, where clinicians can track a patient’s progress, facilitating earlier intervention when needed.
Other investigators at the Mayo Clinic developed a separate online and smartphone-based app to help with rehabilitation of patients hospitalized after a heart attack and stent placement. The app functioned as a self-monitoring system that allowed patients to enter vital signs and to access educational content about steps they could take to reduce their risk of another heart attack.
During a 90-day study, 20% of 25 patients using the app were rehospitalized or admitted to an emergency department, compared with 60% of 19 patients in a control group who received conventional cardiac rehabilitation care without the app. The investigators reported the data at the American College of Cardiology earlier this year.
“We hope a tool like this will help us extend the reach of cardiac rehabilitation to all heart patients, but in particular, it could help patients in rural and underserved populations who might not be able to attend cardiac rehabilitation sessions,” Dr. R. Jay Widmer said in a statement released by the Mayo Clinic.
These and dozens of other apps and technological tools are being developed and tested is a systematic fashion through the Mayo Clinic’s Center for Innovation. In the video, Dr. Cook also describes the Center’s activities and previews another innovative tool in development.
Dr. Cook reported having no financial disclosures.
On Twitter @sherryboschert
The Mayo Clinic handed iPads with an app called “myCare” to patients scheduled for surgery and showed that its use significantly reduced postsurgical length of stay, the total cost of care, and the need for home health care or skilled nursing care at discharge.
A study of 150 patients was so successful that the software, developed initially as an external software program for testing, is now being rebuilt into the institution’s systems so that it has a home in clinicians’ workflow, Dr. David J. Cook said at the Health 2.0 fall conference.
Dr. Cook, chair of cardiovascular anesthesiology at the Mayo Clinic, Rochester, Minn., describes the app in detail in this video interview. The app provides patients a customized plan of care including what they can expect daily, just-in-time education, self-assessment tools, and more. Results are transmitted wirelessly to a dashboard, where clinicians can track a patient’s progress, facilitating earlier intervention when needed.
Other investigators at the Mayo Clinic developed a separate online and smartphone-based app to help with rehabilitation of patients hospitalized after a heart attack and stent placement. The app functioned as a self-monitoring system that allowed patients to enter vital signs and to access educational content about steps they could take to reduce their risk of another heart attack.
During a 90-day study, 20% of 25 patients using the app were rehospitalized or admitted to an emergency department, compared with 60% of 19 patients in a control group who received conventional cardiac rehabilitation care without the app. The investigators reported the data at the American College of Cardiology earlier this year.
“We hope a tool like this will help us extend the reach of cardiac rehabilitation to all heart patients, but in particular, it could help patients in rural and underserved populations who might not be able to attend cardiac rehabilitation sessions,” Dr. R. Jay Widmer said in a statement released by the Mayo Clinic.
These and dozens of other apps and technological tools are being developed and tested is a systematic fashion through the Mayo Clinic’s Center for Innovation. In the video, Dr. Cook also describes the Center’s activities and previews another innovative tool in development.
Dr. Cook reported having no financial disclosures.
On Twitter @sherryboschert
AT HEALTH 2.0
Smartphone device detects atrial fibrillation
The Food and Drug Administration cleared an algorithm for use by patients on a device that attaches to a smartphone to screen for atrial fibrillation instantly.
The AliveCor Heart Monitor attaches to the back of iPhones or Android-based smartphones. Users place fingers on the device and see information on the phone’s screen. They can log their symptoms, and the ECG reading is sent to the company’s server, so data can be accessed later.
The FDA approved the AliveCor Heart Monitor in 2013, and patients have used it since March 2014, with the device sending the ECG reading to a cardiologist or cardiac technician who would send a reply within 24 hours. In August 2014, the FDA cleared an algorithm to be used in a new, free app on the device that allows patients to get an immediate result showing whether or not they are likely to have atrial fibrillation. The company launched the app on the marketplace at the Health 2.0 fall conference in Santa Clara, Calif.
Validation trials have shown that the single-lead AliveCor Heart Monitor system is comparable to a conventional 12-lead ECG, Dr. Omar Dawood said in an interview at the conference. He is a clinical adviser to AliveCor, a surgeon by training who now works with technology companies. And results of two small Australian trials in clinical settings suggest that the AliveCor system is easily used on patients by pharmacists or nurses and is cost-effective.
In one study, pharmacists screened 1,000 pharmacy customers aged 65 years or older using the AliveCor system. A cardiologist read the results, and patients with suspected new atrial fibrillation were referred to general practitioners for conventional 12-lead ECG.
The AliveCor screening identified new cases of atrial fibrillation in 1.5% of patients and a 6.7% prevalence of atrial fibrillation in the cohort. The automated AliveCor algorithm was 98.5% sensitive and 91.4% specific for atrial fibrillation, reported Nicole Lowres of the University of Sydney, and her associates (Thromb. Haemost. 2014;111:1167-76). The investigators also estimated the incremental cost-effectiveness if AliveCor screening were extended into the community, with some patients receiving prescriptions for warfarin and 55% of those adhering to the medication regimen. They calculated a cost in U.S. dollars of $4,066 per quality-adjusted life-year gained and $20,695 to prevent one stroke.
Screening with the AliveCor Heart Monitor “in pharmacies with an automated algorithm is both feasible and cost-effective,” the investigators concluded.
In a separate pilot study, 88 patients seen in three general practices in Sydney were screened by a receptionist or a nurse using AliveCor before seeing the physician. The AliveCor results were transmitted to a secure website where the physician could see them during the patient’s consultation during the same visit.
The device found active atrial fibrillation in 17 patients (19%), all previously diagnosed. The general practitioners and nurses liked the system and its immediate results, but the receptionists felt uneasy doing the screening, reported Jessica Orchard, also of the university, and her associates.
“Atrial fibrillation screening in general practice is feasible,” the investigators concluded (Aust. Fam. Physician 2014;43:315-9). The AliveCor sells for $60-$199, depending on the model of smartphone.
For more on AliveCor, see our video interview with Dr. Dawood at the Health 2.0 fall conference.
AliveCor provided free devices for the studies, which were funded by scholarships from the National Heart Foundation of Australia. The investigators reported having no other financial associations with AliveCor. Some reported financial associations with BMS/Pfizer, Boehringer Ingelheim, Bayer, Servier, and AstraZeneca.
On Twitter @sherryboschert
The Food and Drug Administration cleared an algorithm for use by patients on a device that attaches to a smartphone to screen for atrial fibrillation instantly.
The AliveCor Heart Monitor attaches to the back of iPhones or Android-based smartphones. Users place fingers on the device and see information on the phone’s screen. They can log their symptoms, and the ECG reading is sent to the company’s server, so data can be accessed later.
The FDA approved the AliveCor Heart Monitor in 2013, and patients have used it since March 2014, with the device sending the ECG reading to a cardiologist or cardiac technician who would send a reply within 24 hours. In August 2014, the FDA cleared an algorithm to be used in a new, free app on the device that allows patients to get an immediate result showing whether or not they are likely to have atrial fibrillation. The company launched the app on the marketplace at the Health 2.0 fall conference in Santa Clara, Calif.
Validation trials have shown that the single-lead AliveCor Heart Monitor system is comparable to a conventional 12-lead ECG, Dr. Omar Dawood said in an interview at the conference. He is a clinical adviser to AliveCor, a surgeon by training who now works with technology companies. And results of two small Australian trials in clinical settings suggest that the AliveCor system is easily used on patients by pharmacists or nurses and is cost-effective.
In one study, pharmacists screened 1,000 pharmacy customers aged 65 years or older using the AliveCor system. A cardiologist read the results, and patients with suspected new atrial fibrillation were referred to general practitioners for conventional 12-lead ECG.
The AliveCor screening identified new cases of atrial fibrillation in 1.5% of patients and a 6.7% prevalence of atrial fibrillation in the cohort. The automated AliveCor algorithm was 98.5% sensitive and 91.4% specific for atrial fibrillation, reported Nicole Lowres of the University of Sydney, and her associates (Thromb. Haemost. 2014;111:1167-76). The investigators also estimated the incremental cost-effectiveness if AliveCor screening were extended into the community, with some patients receiving prescriptions for warfarin and 55% of those adhering to the medication regimen. They calculated a cost in U.S. dollars of $4,066 per quality-adjusted life-year gained and $20,695 to prevent one stroke.
Screening with the AliveCor Heart Monitor “in pharmacies with an automated algorithm is both feasible and cost-effective,” the investigators concluded.
In a separate pilot study, 88 patients seen in three general practices in Sydney were screened by a receptionist or a nurse using AliveCor before seeing the physician. The AliveCor results were transmitted to a secure website where the physician could see them during the patient’s consultation during the same visit.
The device found active atrial fibrillation in 17 patients (19%), all previously diagnosed. The general practitioners and nurses liked the system and its immediate results, but the receptionists felt uneasy doing the screening, reported Jessica Orchard, also of the university, and her associates.
“Atrial fibrillation screening in general practice is feasible,” the investigators concluded (Aust. Fam. Physician 2014;43:315-9). The AliveCor sells for $60-$199, depending on the model of smartphone.
For more on AliveCor, see our video interview with Dr. Dawood at the Health 2.0 fall conference.
AliveCor provided free devices for the studies, which were funded by scholarships from the National Heart Foundation of Australia. The investigators reported having no other financial associations with AliveCor. Some reported financial associations with BMS/Pfizer, Boehringer Ingelheim, Bayer, Servier, and AstraZeneca.
On Twitter @sherryboschert
The Food and Drug Administration cleared an algorithm for use by patients on a device that attaches to a smartphone to screen for atrial fibrillation instantly.
The AliveCor Heart Monitor attaches to the back of iPhones or Android-based smartphones. Users place fingers on the device and see information on the phone’s screen. They can log their symptoms, and the ECG reading is sent to the company’s server, so data can be accessed later.
The FDA approved the AliveCor Heart Monitor in 2013, and patients have used it since March 2014, with the device sending the ECG reading to a cardiologist or cardiac technician who would send a reply within 24 hours. In August 2014, the FDA cleared an algorithm to be used in a new, free app on the device that allows patients to get an immediate result showing whether or not they are likely to have atrial fibrillation. The company launched the app on the marketplace at the Health 2.0 fall conference in Santa Clara, Calif.
Validation trials have shown that the single-lead AliveCor Heart Monitor system is comparable to a conventional 12-lead ECG, Dr. Omar Dawood said in an interview at the conference. He is a clinical adviser to AliveCor, a surgeon by training who now works with technology companies. And results of two small Australian trials in clinical settings suggest that the AliveCor system is easily used on patients by pharmacists or nurses and is cost-effective.
In one study, pharmacists screened 1,000 pharmacy customers aged 65 years or older using the AliveCor system. A cardiologist read the results, and patients with suspected new atrial fibrillation were referred to general practitioners for conventional 12-lead ECG.
The AliveCor screening identified new cases of atrial fibrillation in 1.5% of patients and a 6.7% prevalence of atrial fibrillation in the cohort. The automated AliveCor algorithm was 98.5% sensitive and 91.4% specific for atrial fibrillation, reported Nicole Lowres of the University of Sydney, and her associates (Thromb. Haemost. 2014;111:1167-76). The investigators also estimated the incremental cost-effectiveness if AliveCor screening were extended into the community, with some patients receiving prescriptions for warfarin and 55% of those adhering to the medication regimen. They calculated a cost in U.S. dollars of $4,066 per quality-adjusted life-year gained and $20,695 to prevent one stroke.
Screening with the AliveCor Heart Monitor “in pharmacies with an automated algorithm is both feasible and cost-effective,” the investigators concluded.
In a separate pilot study, 88 patients seen in three general practices in Sydney were screened by a receptionist or a nurse using AliveCor before seeing the physician. The AliveCor results were transmitted to a secure website where the physician could see them during the patient’s consultation during the same visit.
The device found active atrial fibrillation in 17 patients (19%), all previously diagnosed. The general practitioners and nurses liked the system and its immediate results, but the receptionists felt uneasy doing the screening, reported Jessica Orchard, also of the university, and her associates.
“Atrial fibrillation screening in general practice is feasible,” the investigators concluded (Aust. Fam. Physician 2014;43:315-9). The AliveCor sells for $60-$199, depending on the model of smartphone.
For more on AliveCor, see our video interview with Dr. Dawood at the Health 2.0 fall conference.
AliveCor provided free devices for the studies, which were funded by scholarships from the National Heart Foundation of Australia. The investigators reported having no other financial associations with AliveCor. Some reported financial associations with BMS/Pfizer, Boehringer Ingelheim, Bayer, Servier, and AstraZeneca.
On Twitter @sherryboschert
VIDEO: Smartphone ECG detects atrial fibrillation
SANTA CLARA, CALIF. – When Dr. Omar Dawood demonstrated the AliveCor Heart Monitor with a new app and algorithm for detecting atrial fibrillation on stage at the Health 2.0 fall conference 2014, it showed that his heart was in normal sinus rhythm – but he had a heart rate of 135 beats per minute.
Chalk it up to the excitement of speaking before an audience of physicians and technologists about this new mobile ECG tool, Dr. Dawood said. “I’m not always that anxious.”
The AliveCor device attaches to the back of iPhones or Android-based smartphones and sells for $60-$199, depending on the model of smartphone. The Food and Drug Administration approved it in 2013, and patients have used it since March 2014. The device sends an ECG reading to a cardiologist or cardiac technician, who sends a reply within 24 hours.
With the new, free app, however, patients get an immediate result from the device showing whether or not they are likely to have atrial fibrillation. The FDA cleared the algorithm for the app in August 2014, and the company launched it on the marketplace at the Health 2.0 conference.
Validation studies have shown that the AliveCor system performs comparably to a traditional 12-lead ECG, Dr. Dawood said in a video interview.
For other recent news on studies of AliveCor in clinical settings, see our Evidence-Based Apps column.
Dr. Dawood, a surgeon by training, is a clinical adviser at AliveCor and also works for a separate technology company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SANTA CLARA, CALIF. – When Dr. Omar Dawood demonstrated the AliveCor Heart Monitor with a new app and algorithm for detecting atrial fibrillation on stage at the Health 2.0 fall conference 2014, it showed that his heart was in normal sinus rhythm – but he had a heart rate of 135 beats per minute.
Chalk it up to the excitement of speaking before an audience of physicians and technologists about this new mobile ECG tool, Dr. Dawood said. “I’m not always that anxious.”
The AliveCor device attaches to the back of iPhones or Android-based smartphones and sells for $60-$199, depending on the model of smartphone. The Food and Drug Administration approved it in 2013, and patients have used it since March 2014. The device sends an ECG reading to a cardiologist or cardiac technician, who sends a reply within 24 hours.
With the new, free app, however, patients get an immediate result from the device showing whether or not they are likely to have atrial fibrillation. The FDA cleared the algorithm for the app in August 2014, and the company launched it on the marketplace at the Health 2.0 conference.
Validation studies have shown that the AliveCor system performs comparably to a traditional 12-lead ECG, Dr. Dawood said in a video interview.
For other recent news on studies of AliveCor in clinical settings, see our Evidence-Based Apps column.
Dr. Dawood, a surgeon by training, is a clinical adviser at AliveCor and also works for a separate technology company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SANTA CLARA, CALIF. – When Dr. Omar Dawood demonstrated the AliveCor Heart Monitor with a new app and algorithm for detecting atrial fibrillation on stage at the Health 2.0 fall conference 2014, it showed that his heart was in normal sinus rhythm – but he had a heart rate of 135 beats per minute.
Chalk it up to the excitement of speaking before an audience of physicians and technologists about this new mobile ECG tool, Dr. Dawood said. “I’m not always that anxious.”
The AliveCor device attaches to the back of iPhones or Android-based smartphones and sells for $60-$199, depending on the model of smartphone. The Food and Drug Administration approved it in 2013, and patients have used it since March 2014. The device sends an ECG reading to a cardiologist or cardiac technician, who sends a reply within 24 hours.
With the new, free app, however, patients get an immediate result from the device showing whether or not they are likely to have atrial fibrillation. The FDA cleared the algorithm for the app in August 2014, and the company launched it on the marketplace at the Health 2.0 conference.
Validation studies have shown that the AliveCor system performs comparably to a traditional 12-lead ECG, Dr. Dawood said in a video interview.
For other recent news on studies of AliveCor in clinical settings, see our Evidence-Based Apps column.
Dr. Dawood, a surgeon by training, is a clinical adviser at AliveCor and also works for a separate technology company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
Blood biomarkers may diagnose depression
Analyses of blood RNA in a study of 64 patients with or without major depression showed significant differences in gene transcript levels between groups, in ways that suggest blood transcriptomic markers may provide an objective way to diagnose depression, predict response to cognitive-behavioral therapy, and identify people with a predisposition to depression.
As a secondary part of a randomized study comparing the efficacy of 18 weeks of live versus telephone-based cognitive-behavioral therapy (CBT), investigators studied a panel of blood transcriptomic markers before treatment in 32 patients with major depressive disorder and 32 matched controls without depression, and in 22 patients in each group after treatment.
The abundance of nine transcripts differed significantly between groups at baseline, suggesting that a panel of transcriptomic markers could be diagnostic in a clinical population, Eva E. Redei, Ph.D., and her associates reported (Transl. Psychiatry 2014 Aug. 16 [doi:10.1038/tp.2014.66]).
These markers include adenylate cyclase 3 (ADCY3); diacylglycerol kinase, alpha (DGKA); family with sequence similarity 46, member A (FAM46A); immunoglobulin superfamily, member 4 (IGSF4), which also is known as cell adhesion molecule 1 (CADM1); KIAA1539; myristoylated alanine-rich protein kinase C substrate (MARCKS); proteasome activator subunit 1 (PSME1); Ras association and pleckstrin homology domains 1, also known as LPD (RAPH1); and intracellular Toll-like receptor 7 (TLR7).
After CBT, the abundance of five transcripts – DGKA, IGSF4A/CADM1, KIAA1539, MARCKS, and RAPH1 – remained significantly different between the two patient groups.
Receiver-operating characteristic (ROC) analyses of blood transcript levels showed that RAPH1, KIAA1539, and DGKA also had significant areas under the curve (AUC) in the depressed patients after cognitive-behavioral therapy both in the nine patients who achieved a full remission of disease and in the 13 patients who did not. “These markers come closest to the ultimate goal of identifying predisposition to depression, even in the absence of a current depressive episode,” reported Dr. Redei, professor in psychiatry and behavioral sciences, and physiology at Northwestern University, Chicago.
In addition, coexpression patterns of transcripts might help predict remission or persistence of clinical depression after CBT. Patients whose depression remitted had 11 “hubs” of coexpressed gene-pairs that correlated significantly with three or more transcripts, compared with five hubs in patients who did not achieve remission. Transcript levels of ADCY3, DGKA, IGSF4A/CADM1, PSME1, and RAPH1 significantly correlated in their expression at baseline in patients whose disease remitted after treatment but not in patients who remained clinically depressed after treatment.
Subjects in the control group were matched to patients with depression by age, sex, and race. Most patients in the depressed group were on medication, including those who did not achieve remission, so it was thought that the medications did not interfere with the blood marker measurements.
The results support findings from previous studies using animal models of depression, and from a pilot study of teenagers with and without major depressive disorder, which showed differences between groups in the abundance of some transcriptomic markers, Dr. Redei said. Unlike the current study, which accepted a wide range of ages (23-83 years) and concurrent medical therapy, the study of adolescents required participants to be 15-19 years of age and medication free. Blood levels of three transcripts – PSME1, RAPH1, and IGSF4A – differed significantly in the teens with depression, compared with nondepressed controls (Transl. Psychiatry 2012 April 17 [doi:10.1038/tp.2012.26]).
At least one separate pilot study previously has proposed using serum levels of nine biomarkers and a proprietary algorithm to diagnose major depressive disorder, Dr. Redei noted (Mol. Psychiatry 2013;18:332-9).
Future validation studies should include more patients and try to assess the usefulness of a panel of blood transcriptomic markers in patients with other psychiatric illnesses, the investigators suggested.
Dr. Redei is named as an inventor on two pending patent applications. She and her associates reported having no other financial disclosures. The National Institute of Mental Health and the Davee Foundation funded the study.
On Twitter @sherryboschert
Analyses of blood RNA in a study of 64 patients with or without major depression showed significant differences in gene transcript levels between groups, in ways that suggest blood transcriptomic markers may provide an objective way to diagnose depression, predict response to cognitive-behavioral therapy, and identify people with a predisposition to depression.
As a secondary part of a randomized study comparing the efficacy of 18 weeks of live versus telephone-based cognitive-behavioral therapy (CBT), investigators studied a panel of blood transcriptomic markers before treatment in 32 patients with major depressive disorder and 32 matched controls without depression, and in 22 patients in each group after treatment.
The abundance of nine transcripts differed significantly between groups at baseline, suggesting that a panel of transcriptomic markers could be diagnostic in a clinical population, Eva E. Redei, Ph.D., and her associates reported (Transl. Psychiatry 2014 Aug. 16 [doi:10.1038/tp.2014.66]).
These markers include adenylate cyclase 3 (ADCY3); diacylglycerol kinase, alpha (DGKA); family with sequence similarity 46, member A (FAM46A); immunoglobulin superfamily, member 4 (IGSF4), which also is known as cell adhesion molecule 1 (CADM1); KIAA1539; myristoylated alanine-rich protein kinase C substrate (MARCKS); proteasome activator subunit 1 (PSME1); Ras association and pleckstrin homology domains 1, also known as LPD (RAPH1); and intracellular Toll-like receptor 7 (TLR7).
After CBT, the abundance of five transcripts – DGKA, IGSF4A/CADM1, KIAA1539, MARCKS, and RAPH1 – remained significantly different between the two patient groups.
Receiver-operating characteristic (ROC) analyses of blood transcript levels showed that RAPH1, KIAA1539, and DGKA also had significant areas under the curve (AUC) in the depressed patients after cognitive-behavioral therapy both in the nine patients who achieved a full remission of disease and in the 13 patients who did not. “These markers come closest to the ultimate goal of identifying predisposition to depression, even in the absence of a current depressive episode,” reported Dr. Redei, professor in psychiatry and behavioral sciences, and physiology at Northwestern University, Chicago.
In addition, coexpression patterns of transcripts might help predict remission or persistence of clinical depression after CBT. Patients whose depression remitted had 11 “hubs” of coexpressed gene-pairs that correlated significantly with three or more transcripts, compared with five hubs in patients who did not achieve remission. Transcript levels of ADCY3, DGKA, IGSF4A/CADM1, PSME1, and RAPH1 significantly correlated in their expression at baseline in patients whose disease remitted after treatment but not in patients who remained clinically depressed after treatment.
Subjects in the control group were matched to patients with depression by age, sex, and race. Most patients in the depressed group were on medication, including those who did not achieve remission, so it was thought that the medications did not interfere with the blood marker measurements.
The results support findings from previous studies using animal models of depression, and from a pilot study of teenagers with and without major depressive disorder, which showed differences between groups in the abundance of some transcriptomic markers, Dr. Redei said. Unlike the current study, which accepted a wide range of ages (23-83 years) and concurrent medical therapy, the study of adolescents required participants to be 15-19 years of age and medication free. Blood levels of three transcripts – PSME1, RAPH1, and IGSF4A – differed significantly in the teens with depression, compared with nondepressed controls (Transl. Psychiatry 2012 April 17 [doi:10.1038/tp.2012.26]).
At least one separate pilot study previously has proposed using serum levels of nine biomarkers and a proprietary algorithm to diagnose major depressive disorder, Dr. Redei noted (Mol. Psychiatry 2013;18:332-9).
Future validation studies should include more patients and try to assess the usefulness of a panel of blood transcriptomic markers in patients with other psychiatric illnesses, the investigators suggested.
Dr. Redei is named as an inventor on two pending patent applications. She and her associates reported having no other financial disclosures. The National Institute of Mental Health and the Davee Foundation funded the study.
On Twitter @sherryboschert
Analyses of blood RNA in a study of 64 patients with or without major depression showed significant differences in gene transcript levels between groups, in ways that suggest blood transcriptomic markers may provide an objective way to diagnose depression, predict response to cognitive-behavioral therapy, and identify people with a predisposition to depression.
As a secondary part of a randomized study comparing the efficacy of 18 weeks of live versus telephone-based cognitive-behavioral therapy (CBT), investigators studied a panel of blood transcriptomic markers before treatment in 32 patients with major depressive disorder and 32 matched controls without depression, and in 22 patients in each group after treatment.
The abundance of nine transcripts differed significantly between groups at baseline, suggesting that a panel of transcriptomic markers could be diagnostic in a clinical population, Eva E. Redei, Ph.D., and her associates reported (Transl. Psychiatry 2014 Aug. 16 [doi:10.1038/tp.2014.66]).
These markers include adenylate cyclase 3 (ADCY3); diacylglycerol kinase, alpha (DGKA); family with sequence similarity 46, member A (FAM46A); immunoglobulin superfamily, member 4 (IGSF4), which also is known as cell adhesion molecule 1 (CADM1); KIAA1539; myristoylated alanine-rich protein kinase C substrate (MARCKS); proteasome activator subunit 1 (PSME1); Ras association and pleckstrin homology domains 1, also known as LPD (RAPH1); and intracellular Toll-like receptor 7 (TLR7).
After CBT, the abundance of five transcripts – DGKA, IGSF4A/CADM1, KIAA1539, MARCKS, and RAPH1 – remained significantly different between the two patient groups.
Receiver-operating characteristic (ROC) analyses of blood transcript levels showed that RAPH1, KIAA1539, and DGKA also had significant areas under the curve (AUC) in the depressed patients after cognitive-behavioral therapy both in the nine patients who achieved a full remission of disease and in the 13 patients who did not. “These markers come closest to the ultimate goal of identifying predisposition to depression, even in the absence of a current depressive episode,” reported Dr. Redei, professor in psychiatry and behavioral sciences, and physiology at Northwestern University, Chicago.
In addition, coexpression patterns of transcripts might help predict remission or persistence of clinical depression after CBT. Patients whose depression remitted had 11 “hubs” of coexpressed gene-pairs that correlated significantly with three or more transcripts, compared with five hubs in patients who did not achieve remission. Transcript levels of ADCY3, DGKA, IGSF4A/CADM1, PSME1, and RAPH1 significantly correlated in their expression at baseline in patients whose disease remitted after treatment but not in patients who remained clinically depressed after treatment.
Subjects in the control group were matched to patients with depression by age, sex, and race. Most patients in the depressed group were on medication, including those who did not achieve remission, so it was thought that the medications did not interfere with the blood marker measurements.
The results support findings from previous studies using animal models of depression, and from a pilot study of teenagers with and without major depressive disorder, which showed differences between groups in the abundance of some transcriptomic markers, Dr. Redei said. Unlike the current study, which accepted a wide range of ages (23-83 years) and concurrent medical therapy, the study of adolescents required participants to be 15-19 years of age and medication free. Blood levels of three transcripts – PSME1, RAPH1, and IGSF4A – differed significantly in the teens with depression, compared with nondepressed controls (Transl. Psychiatry 2012 April 17 [doi:10.1038/tp.2012.26]).
At least one separate pilot study previously has proposed using serum levels of nine biomarkers and a proprietary algorithm to diagnose major depressive disorder, Dr. Redei noted (Mol. Psychiatry 2013;18:332-9).
Future validation studies should include more patients and try to assess the usefulness of a panel of blood transcriptomic markers in patients with other psychiatric illnesses, the investigators suggested.
Dr. Redei is named as an inventor on two pending patent applications. She and her associates reported having no other financial disclosures. The National Institute of Mental Health and the Davee Foundation funded the study.
On Twitter @sherryboschert
FROM TRANSLATIONAL PSYCHIATRY
Key clinical point: Blood levels of transcript panels differentiated depressed patients from controls.
Major finding: Blood transcript levels of nine markers differed significantly between groups.
Data source: Secondary analyses from a study of 32 depressed patients and 32 nondepressed subjects.
Disclosures: Dr. Redei is named as an inventor on two pending patent applications. She and her associates reported having no other financial disclosures. The National Institute of Mental Health and the Davee Foundation funded the study.
VIDEO: Waiting for long-term data on pCR could be disservice to some breast cancer patients, expert says
SAN FRANCISCO – Only a fraction of patients with breast cancer who are eligible for neoadjuvant therapy are getting it, partly because of confusion around the significance of achieving a pathologic complete response, Dr. William M. Sikov said in an interview at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
Dr. Sikov of Brown University, Providence, R.I., explained why it’s been difficult for researchers to show improved outcomes even after a pathologic complete response (pCR) is obtained, but argued that waiting for long-term outcomes data for neoadjuvant therapy could be a disservice to some patients with breast cancer.
Breast cancer surgeons at his own institution have become converts in favor of neoadjuvant therapy, and Dr. Sikov explained why in this video report.
He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Only a fraction of patients with breast cancer who are eligible for neoadjuvant therapy are getting it, partly because of confusion around the significance of achieving a pathologic complete response, Dr. William M. Sikov said in an interview at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
Dr. Sikov of Brown University, Providence, R.I., explained why it’s been difficult for researchers to show improved outcomes even after a pathologic complete response (pCR) is obtained, but argued that waiting for long-term outcomes data for neoadjuvant therapy could be a disservice to some patients with breast cancer.
Breast cancer surgeons at his own institution have become converts in favor of neoadjuvant therapy, and Dr. Sikov explained why in this video report.
He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Only a fraction of patients with breast cancer who are eligible for neoadjuvant therapy are getting it, partly because of confusion around the significance of achieving a pathologic complete response, Dr. William M. Sikov said in an interview at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
Dr. Sikov of Brown University, Providence, R.I., explained why it’s been difficult for researchers to show improved outcomes even after a pathologic complete response (pCR) is obtained, but argued that waiting for long-term outcomes data for neoadjuvant therapy could be a disservice to some patients with breast cancer.
Breast cancer surgeons at his own institution have become converts in favor of neoadjuvant therapy, and Dr. Sikov explained why in this video report.
He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT THE ASCO BREAST CANCER SYMPOSIUM
VIDEO: Unclear if altering lifestyle affects breast cancer
SAN FRANCISCO – Physicians have multiple good reasons to suggest lifestyle changes to many patients with breast cancer, but affecting the cancer itself may not be one of them, Dr. Pamela J. Goodwin said at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
In this video interview, Dr. Goodwin summarizes the ongoing research on how changes in lifestyle such as weight loss, diet, physical activity, and drinking may or may not alter outcomes in patients with breast cancer.
The good news: A drink or two a day probably doesn’t hurt, said Dr. Goodwin, professor of medicine at the University of Toronto’s Mount Sinai Hospital.
She reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Physicians have multiple good reasons to suggest lifestyle changes to many patients with breast cancer, but affecting the cancer itself may not be one of them, Dr. Pamela J. Goodwin said at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
In this video interview, Dr. Goodwin summarizes the ongoing research on how changes in lifestyle such as weight loss, diet, physical activity, and drinking may or may not alter outcomes in patients with breast cancer.
The good news: A drink or two a day probably doesn’t hurt, said Dr. Goodwin, professor of medicine at the University of Toronto’s Mount Sinai Hospital.
She reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Physicians have multiple good reasons to suggest lifestyle changes to many patients with breast cancer, but affecting the cancer itself may not be one of them, Dr. Pamela J. Goodwin said at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
In this video interview, Dr. Goodwin summarizes the ongoing research on how changes in lifestyle such as weight loss, diet, physical activity, and drinking may or may not alter outcomes in patients with breast cancer.
The good news: A drink or two a day probably doesn’t hurt, said Dr. Goodwin, professor of medicine at the University of Toronto’s Mount Sinai Hospital.
She reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT THE 2014 ASCO BREAST CANCER SYMPOSIUM
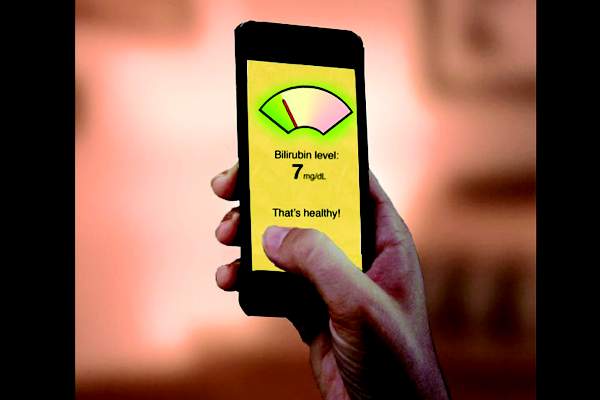
Newborn jaundice app shows promise
An investigational smartphone app performed similarly to a transcutaneous bilirubinometer to screen for newborn jaundice in a pilot study of 100 babies. Measurements from the BiliCam app yielded a rank order correlation of 0.85 with the gold standard blood test to measure total serum bilirubin levels. Transcutaneous bilirubinometer readings had a rank order correlation of 0.92 with total serum bilirubin levels, according to data presented by investigators from the University of Washington, Seattle, at the Association for Computing Machinery’s International Joint Conference on Pervasive and Ubiquitous Computing (UbiComp2014).
The BiliCam had a mean error of 2 mg/dL and transcutaneous bilirubinometer readings had a mean error of 1.5 mg/dL, compared with total serum bilirubin levels, Dr. James W. Stout said in an interview.
The BiliCam “compared favorably” with transcutaneous bilirubinometry, according to the investigators, Dr. Stout and Dr. James A. Taylor, both professors of pediatrics at the university.
“Where we’re at now is very much a work in progress. It will almost certainly perform better as the data set grows” to 400-500 and eventually 1,000 babies, Dr. Stout said. “The way it performs now is more than anything a promising signal about how we think it can perform.”
Getting the BiliCam into the hands of clinicians in general within a year is an “optimistic” goal, and “I feel pretty confident we can have this out in the world in 2 years,” he said. Food and Drug Administration approval would be needed before parents could use the BiliCam at home, he added.
If it pans out, the BiliCam could be more accessible and less expensive than transcutaneous bilirubinometers, which cost $7,000-$8,000, he said. The expensive devices usually aren’t found in general pediatric offices and certainly aren’t used by many parents at home.
In the study, users downloaded the app to an iPhone 4, placed a business card–size color-calibration card on the baby’s belly, and triggered the app to take photos with the card in view. The app sent the data to the Cloud for analysis by algorithms, and a report on the newborn’s bilirubin levels was sent almost instantly to the user’s phone. All babies were tested between 2-5 days of age using the BiliCam, a transcutaneous bilirubinometer, and serum testing.
Although an estimated 84% of newborns develop jaundice, only approximately 20 U.S. babies per year develop kernicterus from severe jaundice, Dr. Stout said. Visual assessment, even by experienced clinicians, has been shown to be only moderately accurate, at best, for estimating the severity of jaundice, leading many parents to return to clinics with “yellow babies” who are not really at risk but may undergo blood draws, he said. “We want to reduce the churn.”
More importantly, the investigators hope that the BiliCam eventually will prove useful in resource-poor nations where kernicterus causes many newborn deaths, he added. Before that can happen, the BiliCam must be tested on more racially diverse populations so that the algorithms can extract the relevant wavelengths to incorporate into the app. “We don’t know yet that we can do that in really dark babies,” he said.
Other testing should begin within the year to adapt the BiliCam to other types of phones beyond iPhones. The investigator are exploring infrastructures for national and international trials.
Grants from the Coulter Foundation and the National Science Foundation funded the research. The investigators and the university have filed a patent on BiliCam, which is expected to generate future revenue from fees for the app or for processing photos, or from coverage by insurers or some other commercial model.
On Twitter @sherryboschert
An investigational smartphone app performed similarly to a transcutaneous bilirubinometer to screen for newborn jaundice in a pilot study of 100 babies. Measurements from the BiliCam app yielded a rank order correlation of 0.85 with the gold standard blood test to measure total serum bilirubin levels. Transcutaneous bilirubinometer readings had a rank order correlation of 0.92 with total serum bilirubin levels, according to data presented by investigators from the University of Washington, Seattle, at the Association for Computing Machinery’s International Joint Conference on Pervasive and Ubiquitous Computing (UbiComp2014).
The BiliCam had a mean error of 2 mg/dL and transcutaneous bilirubinometer readings had a mean error of 1.5 mg/dL, compared with total serum bilirubin levels, Dr. James W. Stout said in an interview.
The BiliCam “compared favorably” with transcutaneous bilirubinometry, according to the investigators, Dr. Stout and Dr. James A. Taylor, both professors of pediatrics at the university.
“Where we’re at now is very much a work in progress. It will almost certainly perform better as the data set grows” to 400-500 and eventually 1,000 babies, Dr. Stout said. “The way it performs now is more than anything a promising signal about how we think it can perform.”
Getting the BiliCam into the hands of clinicians in general within a year is an “optimistic” goal, and “I feel pretty confident we can have this out in the world in 2 years,” he said. Food and Drug Administration approval would be needed before parents could use the BiliCam at home, he added.
If it pans out, the BiliCam could be more accessible and less expensive than transcutaneous bilirubinometers, which cost $7,000-$8,000, he said. The expensive devices usually aren’t found in general pediatric offices and certainly aren’t used by many parents at home.
In the study, users downloaded the app to an iPhone 4, placed a business card–size color-calibration card on the baby’s belly, and triggered the app to take photos with the card in view. The app sent the data to the Cloud for analysis by algorithms, and a report on the newborn’s bilirubin levels was sent almost instantly to the user’s phone. All babies were tested between 2-5 days of age using the BiliCam, a transcutaneous bilirubinometer, and serum testing.
Although an estimated 84% of newborns develop jaundice, only approximately 20 U.S. babies per year develop kernicterus from severe jaundice, Dr. Stout said. Visual assessment, even by experienced clinicians, has been shown to be only moderately accurate, at best, for estimating the severity of jaundice, leading many parents to return to clinics with “yellow babies” who are not really at risk but may undergo blood draws, he said. “We want to reduce the churn.”
More importantly, the investigators hope that the BiliCam eventually will prove useful in resource-poor nations where kernicterus causes many newborn deaths, he added. Before that can happen, the BiliCam must be tested on more racially diverse populations so that the algorithms can extract the relevant wavelengths to incorporate into the app. “We don’t know yet that we can do that in really dark babies,” he said.
Other testing should begin within the year to adapt the BiliCam to other types of phones beyond iPhones. The investigator are exploring infrastructures for national and international trials.
Grants from the Coulter Foundation and the National Science Foundation funded the research. The investigators and the university have filed a patent on BiliCam, which is expected to generate future revenue from fees for the app or for processing photos, or from coverage by insurers or some other commercial model.
On Twitter @sherryboschert
An investigational smartphone app performed similarly to a transcutaneous bilirubinometer to screen for newborn jaundice in a pilot study of 100 babies. Measurements from the BiliCam app yielded a rank order correlation of 0.85 with the gold standard blood test to measure total serum bilirubin levels. Transcutaneous bilirubinometer readings had a rank order correlation of 0.92 with total serum bilirubin levels, according to data presented by investigators from the University of Washington, Seattle, at the Association for Computing Machinery’s International Joint Conference on Pervasive and Ubiquitous Computing (UbiComp2014).
The BiliCam had a mean error of 2 mg/dL and transcutaneous bilirubinometer readings had a mean error of 1.5 mg/dL, compared with total serum bilirubin levels, Dr. James W. Stout said in an interview.
The BiliCam “compared favorably” with transcutaneous bilirubinometry, according to the investigators, Dr. Stout and Dr. James A. Taylor, both professors of pediatrics at the university.
“Where we’re at now is very much a work in progress. It will almost certainly perform better as the data set grows” to 400-500 and eventually 1,000 babies, Dr. Stout said. “The way it performs now is more than anything a promising signal about how we think it can perform.”
Getting the BiliCam into the hands of clinicians in general within a year is an “optimistic” goal, and “I feel pretty confident we can have this out in the world in 2 years,” he said. Food and Drug Administration approval would be needed before parents could use the BiliCam at home, he added.
If it pans out, the BiliCam could be more accessible and less expensive than transcutaneous bilirubinometers, which cost $7,000-$8,000, he said. The expensive devices usually aren’t found in general pediatric offices and certainly aren’t used by many parents at home.
In the study, users downloaded the app to an iPhone 4, placed a business card–size color-calibration card on the baby’s belly, and triggered the app to take photos with the card in view. The app sent the data to the Cloud for analysis by algorithms, and a report on the newborn’s bilirubin levels was sent almost instantly to the user’s phone. All babies were tested between 2-5 days of age using the BiliCam, a transcutaneous bilirubinometer, and serum testing.
Although an estimated 84% of newborns develop jaundice, only approximately 20 U.S. babies per year develop kernicterus from severe jaundice, Dr. Stout said. Visual assessment, even by experienced clinicians, has been shown to be only moderately accurate, at best, for estimating the severity of jaundice, leading many parents to return to clinics with “yellow babies” who are not really at risk but may undergo blood draws, he said. “We want to reduce the churn.”
More importantly, the investigators hope that the BiliCam eventually will prove useful in resource-poor nations where kernicterus causes many newborn deaths, he added. Before that can happen, the BiliCam must be tested on more racially diverse populations so that the algorithms can extract the relevant wavelengths to incorporate into the app. “We don’t know yet that we can do that in really dark babies,” he said.
Other testing should begin within the year to adapt the BiliCam to other types of phones beyond iPhones. The investigator are exploring infrastructures for national and international trials.
Grants from the Coulter Foundation and the National Science Foundation funded the research. The investigators and the university have filed a patent on BiliCam, which is expected to generate future revenue from fees for the app or for processing photos, or from coverage by insurers or some other commercial model.
On Twitter @sherryboschert
Markers predict hypoglycemia on intensive glycemic therapy
SAN FRANCISCO – Patients with type 2 diabetes who were insulin deficient were 36 times more likely to develop severe hypoglycemia on treatment and to fail to get hemoglobin A1c levels below 6% after starting intensive therapy in a retrospective analysis of data on 1,401 patients.
In addition, patients with any of four antibodies against islet cells at baseline were 4-12 times more likely to develop severe hypoglycemia and fail to reach the glycemic target on intensive therapy, compared with patients without those biomarkers, Dr. Lisa Chow reported at the annual scientific sessions of the American Diabetes Association.
The study defined insulin deficiency as a fasting C-peptide level no higher than 0.45 ng/mL. Investigators measured levels of three of the autoantibodies and considered the fourth – insulin autoantibody (IAA) – to be present if the patient used insulin at baseline.
In unadjusted analyses, the likelihood of severe hypoglycemia and failure to reach the glycemic target was four times higher in patients with IAA or antibodies against glutamic acid decarboxylase (GAD) or zinc transporter 8 (ZnT8), compared with patients without those autoantibodies. Severe hypoglycemia and failure to get hemoglobin A1c (HbA1c) below 6% were 11 times more likely in patients with antibodies against tyrosine phosphatase–related islet antigen 2 (IA-2), reported Dr. Chow, an endocrinologist at the University of Minnesota, Minneapolis.
She and her associates studied data on 1,401 patients who were randomized to the intensive glycemic control arm of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. They compared 326 patients ("cases") who developed severe hypoglycemia and whose HbA1c levels did not reach the target of less than 6% with 1,075 control patients (matched 4:1 by age, race, and body mass index) who did not have severe hypoglycemia and who reached the HbA1c target.
Overall, 17% of cases and 1% of controls were insulin deficient. Excluding IAA (present in 62% of cases and 26% of controls), the most common islet antibody was GAD, in 17% of cases and 6% of controls. IA-2 was present in 4% of cases and 0.4% of controls, and ZnT8 was present in 2% of cases and 0.7% of controls.
"We propose that measuring C-peptide and GAD antibodies in patients with type 2 diabetes may serve as a biomarker to help tailor and individualize therapy" by predicting which patients are more likely to have adverse outcomes on intensive glycemic treatment, Dr. Chow said.
At baseline, the case group was significantly more likely to use insulin, compared with controls (89% and 24%, respectively) and less likely to be male (50% vs. 59%). The case patients had a higher HbA1c at baseline, compared with controls (8.54% vs. 8.08%, respectively) and a longer duration of diabetes (15 vs. 9 years).
After adjusting for the effects of age and body mass index, the combined outcome of severe hypoglycemia and failure to reach the glycemic target was 32 times more likely in patients with insulin deficiency at baseline, 3 times more likely in patients with GAD or ZnT8, 5 times more likely in patients with IAA, and 9 times more likely in patients with IA-2, compared with patients without those markers, Dr. Chow said.
A third analysis removed data for any case patients who died and their associated controls and found that severe hypoglycemia and failure to reach the glycemic target was 30 times more likely in patients with insulin deficiency at baseline, 4 times more likely in patients with GAD or ZnT8, 5 times more likely in patients with IAA, and 12 times more likely in patients with IA-2, compared with patients without those markers.
The study defined severe hypoglycemia as any hypoglycemia requiring assistance. Patients who developed severe hypoglycemia were four times less likely to get their HbA1c levels below 6%.
Dr. Chow reported having no financial disclosures. The National Institutes of Health funded the study.
I don’t think this study means that we automatically should test everybody with type 2 diabetes for their insulin levels and their autoantibodies because we would need a study to show that if you did that, versus not doing that, people actually do better.
 |
|
I think what this study tells us is that there is a fair amount of slow-burn type 1 diabetes amongst people who we think have type 2 diabetes. Perhaps unsurprisingly, those people tend to have more hypoglycemia and trouble.
The study defined poor glycemic control as not being able to get an HbA1c of less than 6%. To be fair, that’s what the ACCORD trial said. Clinically, nobody would consider someone with an HbA1c of 6.2% to have poor glycemic control.
One take-home message might be that if your patient has poor glycemic control and severe hypoglycemia, consider checking for autoantibodies.
Dr. Amanda Adler is consultant physician at Cambridge University’s Addenbrooke’s Hospital and chair of the technology appraisals committee for the National Institute for Health and Clinical Excellence, England. She gave these comments in an interview at the meeting.
I don’t think this study means that we automatically should test everybody with type 2 diabetes for their insulin levels and their autoantibodies because we would need a study to show that if you did that, versus not doing that, people actually do better.
 |
|
I think what this study tells us is that there is a fair amount of slow-burn type 1 diabetes amongst people who we think have type 2 diabetes. Perhaps unsurprisingly, those people tend to have more hypoglycemia and trouble.
The study defined poor glycemic control as not being able to get an HbA1c of less than 6%. To be fair, that’s what the ACCORD trial said. Clinically, nobody would consider someone with an HbA1c of 6.2% to have poor glycemic control.
One take-home message might be that if your patient has poor glycemic control and severe hypoglycemia, consider checking for autoantibodies.
Dr. Amanda Adler is consultant physician at Cambridge University’s Addenbrooke’s Hospital and chair of the technology appraisals committee for the National Institute for Health and Clinical Excellence, England. She gave these comments in an interview at the meeting.
I don’t think this study means that we automatically should test everybody with type 2 diabetes for their insulin levels and their autoantibodies because we would need a study to show that if you did that, versus not doing that, people actually do better.
 |
|
I think what this study tells us is that there is a fair amount of slow-burn type 1 diabetes amongst people who we think have type 2 diabetes. Perhaps unsurprisingly, those people tend to have more hypoglycemia and trouble.
The study defined poor glycemic control as not being able to get an HbA1c of less than 6%. To be fair, that’s what the ACCORD trial said. Clinically, nobody would consider someone with an HbA1c of 6.2% to have poor glycemic control.
One take-home message might be that if your patient has poor glycemic control and severe hypoglycemia, consider checking for autoantibodies.
Dr. Amanda Adler is consultant physician at Cambridge University’s Addenbrooke’s Hospital and chair of the technology appraisals committee for the National Institute for Health and Clinical Excellence, England. She gave these comments in an interview at the meeting.
SAN FRANCISCO – Patients with type 2 diabetes who were insulin deficient were 36 times more likely to develop severe hypoglycemia on treatment and to fail to get hemoglobin A1c levels below 6% after starting intensive therapy in a retrospective analysis of data on 1,401 patients.
In addition, patients with any of four antibodies against islet cells at baseline were 4-12 times more likely to develop severe hypoglycemia and fail to reach the glycemic target on intensive therapy, compared with patients without those biomarkers, Dr. Lisa Chow reported at the annual scientific sessions of the American Diabetes Association.
The study defined insulin deficiency as a fasting C-peptide level no higher than 0.45 ng/mL. Investigators measured levels of three of the autoantibodies and considered the fourth – insulin autoantibody (IAA) – to be present if the patient used insulin at baseline.
In unadjusted analyses, the likelihood of severe hypoglycemia and failure to reach the glycemic target was four times higher in patients with IAA or antibodies against glutamic acid decarboxylase (GAD) or zinc transporter 8 (ZnT8), compared with patients without those autoantibodies. Severe hypoglycemia and failure to get hemoglobin A1c (HbA1c) below 6% were 11 times more likely in patients with antibodies against tyrosine phosphatase–related islet antigen 2 (IA-2), reported Dr. Chow, an endocrinologist at the University of Minnesota, Minneapolis.
She and her associates studied data on 1,401 patients who were randomized to the intensive glycemic control arm of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. They compared 326 patients ("cases") who developed severe hypoglycemia and whose HbA1c levels did not reach the target of less than 6% with 1,075 control patients (matched 4:1 by age, race, and body mass index) who did not have severe hypoglycemia and who reached the HbA1c target.
Overall, 17% of cases and 1% of controls were insulin deficient. Excluding IAA (present in 62% of cases and 26% of controls), the most common islet antibody was GAD, in 17% of cases and 6% of controls. IA-2 was present in 4% of cases and 0.4% of controls, and ZnT8 was present in 2% of cases and 0.7% of controls.
"We propose that measuring C-peptide and GAD antibodies in patients with type 2 diabetes may serve as a biomarker to help tailor and individualize therapy" by predicting which patients are more likely to have adverse outcomes on intensive glycemic treatment, Dr. Chow said.
At baseline, the case group was significantly more likely to use insulin, compared with controls (89% and 24%, respectively) and less likely to be male (50% vs. 59%). The case patients had a higher HbA1c at baseline, compared with controls (8.54% vs. 8.08%, respectively) and a longer duration of diabetes (15 vs. 9 years).
After adjusting for the effects of age and body mass index, the combined outcome of severe hypoglycemia and failure to reach the glycemic target was 32 times more likely in patients with insulin deficiency at baseline, 3 times more likely in patients with GAD or ZnT8, 5 times more likely in patients with IAA, and 9 times more likely in patients with IA-2, compared with patients without those markers, Dr. Chow said.
A third analysis removed data for any case patients who died and their associated controls and found that severe hypoglycemia and failure to reach the glycemic target was 30 times more likely in patients with insulin deficiency at baseline, 4 times more likely in patients with GAD or ZnT8, 5 times more likely in patients with IAA, and 12 times more likely in patients with IA-2, compared with patients without those markers.
The study defined severe hypoglycemia as any hypoglycemia requiring assistance. Patients who developed severe hypoglycemia were four times less likely to get their HbA1c levels below 6%.
Dr. Chow reported having no financial disclosures. The National Institutes of Health funded the study.
SAN FRANCISCO – Patients with type 2 diabetes who were insulin deficient were 36 times more likely to develop severe hypoglycemia on treatment and to fail to get hemoglobin A1c levels below 6% after starting intensive therapy in a retrospective analysis of data on 1,401 patients.
In addition, patients with any of four antibodies against islet cells at baseline were 4-12 times more likely to develop severe hypoglycemia and fail to reach the glycemic target on intensive therapy, compared with patients without those biomarkers, Dr. Lisa Chow reported at the annual scientific sessions of the American Diabetes Association.
The study defined insulin deficiency as a fasting C-peptide level no higher than 0.45 ng/mL. Investigators measured levels of three of the autoantibodies and considered the fourth – insulin autoantibody (IAA) – to be present if the patient used insulin at baseline.
In unadjusted analyses, the likelihood of severe hypoglycemia and failure to reach the glycemic target was four times higher in patients with IAA or antibodies against glutamic acid decarboxylase (GAD) or zinc transporter 8 (ZnT8), compared with patients without those autoantibodies. Severe hypoglycemia and failure to get hemoglobin A1c (HbA1c) below 6% were 11 times more likely in patients with antibodies against tyrosine phosphatase–related islet antigen 2 (IA-2), reported Dr. Chow, an endocrinologist at the University of Minnesota, Minneapolis.
She and her associates studied data on 1,401 patients who were randomized to the intensive glycemic control arm of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. They compared 326 patients ("cases") who developed severe hypoglycemia and whose HbA1c levels did not reach the target of less than 6% with 1,075 control patients (matched 4:1 by age, race, and body mass index) who did not have severe hypoglycemia and who reached the HbA1c target.
Overall, 17% of cases and 1% of controls were insulin deficient. Excluding IAA (present in 62% of cases and 26% of controls), the most common islet antibody was GAD, in 17% of cases and 6% of controls. IA-2 was present in 4% of cases and 0.4% of controls, and ZnT8 was present in 2% of cases and 0.7% of controls.
"We propose that measuring C-peptide and GAD antibodies in patients with type 2 diabetes may serve as a biomarker to help tailor and individualize therapy" by predicting which patients are more likely to have adverse outcomes on intensive glycemic treatment, Dr. Chow said.
At baseline, the case group was significantly more likely to use insulin, compared with controls (89% and 24%, respectively) and less likely to be male (50% vs. 59%). The case patients had a higher HbA1c at baseline, compared with controls (8.54% vs. 8.08%, respectively) and a longer duration of diabetes (15 vs. 9 years).
After adjusting for the effects of age and body mass index, the combined outcome of severe hypoglycemia and failure to reach the glycemic target was 32 times more likely in patients with insulin deficiency at baseline, 3 times more likely in patients with GAD or ZnT8, 5 times more likely in patients with IAA, and 9 times more likely in patients with IA-2, compared with patients without those markers, Dr. Chow said.
A third analysis removed data for any case patients who died and their associated controls and found that severe hypoglycemia and failure to reach the glycemic target was 30 times more likely in patients with insulin deficiency at baseline, 4 times more likely in patients with GAD or ZnT8, 5 times more likely in patients with IAA, and 12 times more likely in patients with IA-2, compared with patients without those markers.
The study defined severe hypoglycemia as any hypoglycemia requiring assistance. Patients who developed severe hypoglycemia were four times less likely to get their HbA1c levels below 6%.
Dr. Chow reported having no financial disclosures. The National Institutes of Health funded the study.
AT THE ADA ANNUAL SCIENTIFIC SESSION
VIDEO: Low recurrence with high HER2 expression and a GP2 peptide vaccine
SAN FRANCISCO – A GP2 peptide vaccine to prevent breast cancer recurrence appears most effective in women whose tumors had the highest HER2 overexpression. In a video interview, Dr. Erika J. Schneble of the San Antonio (Tex.) Military Medical Center describes the phase II adjuvant vaccine study she presented at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
Results of an intent-to-treat analysis of all patients showed that 88% of 89 vaccinated women and 81% of 91 patients in the control group remained disease free after a median follow-up of 34 months (P = .43). Among patients who completed treatment, disease-free survival rates were 94% among 83 patients in the vaccine group and 85% among 87 patients in the control group, the investigators reported (P = .17).
In prespecified subgroup analyses based on the level of expression of human epidermal growth factor receptor 2 (HER2), the greatest potential effect was seen in those with the highest HER2 overexpression. In this subgroup, disease-free survival rates were 94% in 51 patients in the vaccine group and 89% in 50 patients in the control group, in an intent-to-treat analysis (P = .86). Excluding two of these patients who developed early recurrences during the primary vaccine series and one patient who developed a non-breast malignancy, however, no recurrences were seen in the vaccine group. Disease-free survival rates were 100% in 48 women in the vaccine group and 89% in 50 women in the control group (P = .08).
Dr. Schneble conducted the 180-patient trial with primary investigator Dr. Elizabeth A. Mittendorf, a surgical oncologist at the University of Texas MD Anderson Cancer Center, Houston, and her associates.
Also in the video, Dr. Hope S. Rugo, director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco, gives her perspective on the study findings. She was not involved with the trial.
Dr. Schneble reporting having no financial disclosures. Dr. Mittendorf’s institution receives per-patient support to enroll patients in vaccine trials sponsored by Galena Biopharma, Antigen Express, and Norwell. One of their coinvestigators has partial inventor rights to GP2. Dr. Rugo disclosed financial associations with Genomic Health, Plexxikon, Merck, and Novartis. She is on the scientific advisory board of Galena Biopharma.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – A GP2 peptide vaccine to prevent breast cancer recurrence appears most effective in women whose tumors had the highest HER2 overexpression. In a video interview, Dr. Erika J. Schneble of the San Antonio (Tex.) Military Medical Center describes the phase II adjuvant vaccine study she presented at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
Results of an intent-to-treat analysis of all patients showed that 88% of 89 vaccinated women and 81% of 91 patients in the control group remained disease free after a median follow-up of 34 months (P = .43). Among patients who completed treatment, disease-free survival rates were 94% among 83 patients in the vaccine group and 85% among 87 patients in the control group, the investigators reported (P = .17).
In prespecified subgroup analyses based on the level of expression of human epidermal growth factor receptor 2 (HER2), the greatest potential effect was seen in those with the highest HER2 overexpression. In this subgroup, disease-free survival rates were 94% in 51 patients in the vaccine group and 89% in 50 patients in the control group, in an intent-to-treat analysis (P = .86). Excluding two of these patients who developed early recurrences during the primary vaccine series and one patient who developed a non-breast malignancy, however, no recurrences were seen in the vaccine group. Disease-free survival rates were 100% in 48 women in the vaccine group and 89% in 50 women in the control group (P = .08).
Dr. Schneble conducted the 180-patient trial with primary investigator Dr. Elizabeth A. Mittendorf, a surgical oncologist at the University of Texas MD Anderson Cancer Center, Houston, and her associates.
Also in the video, Dr. Hope S. Rugo, director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco, gives her perspective on the study findings. She was not involved with the trial.
Dr. Schneble reporting having no financial disclosures. Dr. Mittendorf’s institution receives per-patient support to enroll patients in vaccine trials sponsored by Galena Biopharma, Antigen Express, and Norwell. One of their coinvestigators has partial inventor rights to GP2. Dr. Rugo disclosed financial associations with Genomic Health, Plexxikon, Merck, and Novartis. She is on the scientific advisory board of Galena Biopharma.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – A GP2 peptide vaccine to prevent breast cancer recurrence appears most effective in women whose tumors had the highest HER2 overexpression. In a video interview, Dr. Erika J. Schneble of the San Antonio (Tex.) Military Medical Center describes the phase II adjuvant vaccine study she presented at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
Results of an intent-to-treat analysis of all patients showed that 88% of 89 vaccinated women and 81% of 91 patients in the control group remained disease free after a median follow-up of 34 months (P = .43). Among patients who completed treatment, disease-free survival rates were 94% among 83 patients in the vaccine group and 85% among 87 patients in the control group, the investigators reported (P = .17).
In prespecified subgroup analyses based on the level of expression of human epidermal growth factor receptor 2 (HER2), the greatest potential effect was seen in those with the highest HER2 overexpression. In this subgroup, disease-free survival rates were 94% in 51 patients in the vaccine group and 89% in 50 patients in the control group, in an intent-to-treat analysis (P = .86). Excluding two of these patients who developed early recurrences during the primary vaccine series and one patient who developed a non-breast malignancy, however, no recurrences were seen in the vaccine group. Disease-free survival rates were 100% in 48 women in the vaccine group and 89% in 50 women in the control group (P = .08).
Dr. Schneble conducted the 180-patient trial with primary investigator Dr. Elizabeth A. Mittendorf, a surgical oncologist at the University of Texas MD Anderson Cancer Center, Houston, and her associates.
Also in the video, Dr. Hope S. Rugo, director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco, gives her perspective on the study findings. She was not involved with the trial.
Dr. Schneble reporting having no financial disclosures. Dr. Mittendorf’s institution receives per-patient support to enroll patients in vaccine trials sponsored by Galena Biopharma, Antigen Express, and Norwell. One of their coinvestigators has partial inventor rights to GP2. Dr. Rugo disclosed financial associations with Genomic Health, Plexxikon, Merck, and Novartis. She is on the scientific advisory board of Galena Biopharma.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT THE ASCO BREAST CANCER SYMPOSIUM