User login
In the Literature: Research You Need to Know
Clinical question: What is the relationship between well-being and demographic factors, educational debt, and medical knowledge in internal-medicine residents?
Background: Physician distress during training is common and can negatively impact patient care. There has never been a study of internal-medicine residents nationally that examined the patterns of distress across demographic factors or the association of these factors with medical knowledge.
Study design: Cross-sectional study.
Setting: U.S. internal-medicine residency programs.
Synopsis: Of the 21,208 U.S. internal-medicine residents who completed the 2008 in-training examination, 77.3% had both survey and demographic data available for analysis. Nearly 15% of these 16,394 residents rated quality of life “as bad as it can be” or “somewhat bad,” and 32.9% felt somewhat or very dissatisfied with work-life balance.
Overall burnout, high levels of weekly emotional exhaustion, and weekly depersonalization were reported by 51.5%, 45.8%, and 28.9% of residents, respectively. Symptoms of emotional exhaustion decreased as training increased, while depersonalization increased after the first postgraduate year. Residents reporting quality of life “as bad as it can be,” emotional exhaustion, or debt greater than $200,000 had mean exam scores 2.7, 4.2, and 5 points, respectively, lower than others surveyed.
Although unlikely given the study design, nonresponse bias could affect these results. Not all demographic variables or domains of well-being were studied, and self-reported educational debt could have been misclassified. Nonetheless, findings suggest that distress remains among residents despite the changes made to duty-hour regulations in 2003.
Bottom line: Suboptimal quality of life and burnout were common among internal-medicine residents nationally; symptoms of burnout were associated with higher debt and lower exam scores.
Citation: West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306:952-960.
Visit our website for more physician reviews of HM-related research.
Clinical question: What is the relationship between well-being and demographic factors, educational debt, and medical knowledge in internal-medicine residents?
Background: Physician distress during training is common and can negatively impact patient care. There has never been a study of internal-medicine residents nationally that examined the patterns of distress across demographic factors or the association of these factors with medical knowledge.
Study design: Cross-sectional study.
Setting: U.S. internal-medicine residency programs.
Synopsis: Of the 21,208 U.S. internal-medicine residents who completed the 2008 in-training examination, 77.3% had both survey and demographic data available for analysis. Nearly 15% of these 16,394 residents rated quality of life “as bad as it can be” or “somewhat bad,” and 32.9% felt somewhat or very dissatisfied with work-life balance.
Overall burnout, high levels of weekly emotional exhaustion, and weekly depersonalization were reported by 51.5%, 45.8%, and 28.9% of residents, respectively. Symptoms of emotional exhaustion decreased as training increased, while depersonalization increased after the first postgraduate year. Residents reporting quality of life “as bad as it can be,” emotional exhaustion, or debt greater than $200,000 had mean exam scores 2.7, 4.2, and 5 points, respectively, lower than others surveyed.
Although unlikely given the study design, nonresponse bias could affect these results. Not all demographic variables or domains of well-being were studied, and self-reported educational debt could have been misclassified. Nonetheless, findings suggest that distress remains among residents despite the changes made to duty-hour regulations in 2003.
Bottom line: Suboptimal quality of life and burnout were common among internal-medicine residents nationally; symptoms of burnout were associated with higher debt and lower exam scores.
Citation: West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306:952-960.
Visit our website for more physician reviews of HM-related research.
Clinical question: What is the relationship between well-being and demographic factors, educational debt, and medical knowledge in internal-medicine residents?
Background: Physician distress during training is common and can negatively impact patient care. There has never been a study of internal-medicine residents nationally that examined the patterns of distress across demographic factors or the association of these factors with medical knowledge.
Study design: Cross-sectional study.
Setting: U.S. internal-medicine residency programs.
Synopsis: Of the 21,208 U.S. internal-medicine residents who completed the 2008 in-training examination, 77.3% had both survey and demographic data available for analysis. Nearly 15% of these 16,394 residents rated quality of life “as bad as it can be” or “somewhat bad,” and 32.9% felt somewhat or very dissatisfied with work-life balance.
Overall burnout, high levels of weekly emotional exhaustion, and weekly depersonalization were reported by 51.5%, 45.8%, and 28.9% of residents, respectively. Symptoms of emotional exhaustion decreased as training increased, while depersonalization increased after the first postgraduate year. Residents reporting quality of life “as bad as it can be,” emotional exhaustion, or debt greater than $200,000 had mean exam scores 2.7, 4.2, and 5 points, respectively, lower than others surveyed.
Although unlikely given the study design, nonresponse bias could affect these results. Not all demographic variables or domains of well-being were studied, and self-reported educational debt could have been misclassified. Nonetheless, findings suggest that distress remains among residents despite the changes made to duty-hour regulations in 2003.
Bottom line: Suboptimal quality of life and burnout were common among internal-medicine residents nationally; symptoms of burnout were associated with higher debt and lower exam scores.
Citation: West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306:952-960.
Visit our website for more physician reviews of HM-related research.
In the Literature: Research You Need to Know
Clinical question: To what extent does diagnostic phlebotomy contribute to hospital-acquired anemia (HAA) during acute myocardial infarction (AMI)?
Background: During AMI, hospital-acquired HAA is associated with higher mortality and poorer health status. Moderate to severe HAA (nadir hemoglobin level <11 g/dL) has been shown to be prognostically important. The contribution of diagnostic phlebotomy blood loss on HAA is unknown and is a potentially modifiable factor.
Study design: Retrospective observational cohort study.
Setting: Fifty-seven U.S. hospitals.
Synopsis: Using Cerner Corp.'s Health Facts database, information was collected on 17,676 patients with AMI. Moderate to severe HAA developed in 3,551 (20%) patients who were not anemic upon admission. The diagnostic blood loss was estimated by assuming minimal blood volume per adult tube required to perform the lab work obtained. The mean phlebotomy volume was higher in patients with HAA compared with patients without HAA (173.8 mL vs. 83.5 mL; P<0.001). There was significant variation of diagnostic blood loss between hospitals. The risk of HAA increased by 18% (RR 1.18; 95% CI, 1.13-1.22) for every 50 mL of diagnostic blood loss.
Patients with HAA were noted to have greater disease severity and comorbidities. No causal inference can be made given the observational nature of the study. Randomized trials are needed to evaluate if strategies to reduce diagnostic blood loss can reduce HAA and improve clinical outcomes for patients with AMI.
Bottom line: Diagnostic blood loss is associated with development of hospital-acquired anemia in patients with acute myocardial infarction.
Citation: Salisbury AC, Reid KJ, Alexander KP, et al. Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171:1646-1653.
For more physician reviews of HM-relevant research, visit our website.
Clinical question: To what extent does diagnostic phlebotomy contribute to hospital-acquired anemia (HAA) during acute myocardial infarction (AMI)?
Background: During AMI, hospital-acquired HAA is associated with higher mortality and poorer health status. Moderate to severe HAA (nadir hemoglobin level <11 g/dL) has been shown to be prognostically important. The contribution of diagnostic phlebotomy blood loss on HAA is unknown and is a potentially modifiable factor.
Study design: Retrospective observational cohort study.
Setting: Fifty-seven U.S. hospitals.
Synopsis: Using Cerner Corp.'s Health Facts database, information was collected on 17,676 patients with AMI. Moderate to severe HAA developed in 3,551 (20%) patients who were not anemic upon admission. The diagnostic blood loss was estimated by assuming minimal blood volume per adult tube required to perform the lab work obtained. The mean phlebotomy volume was higher in patients with HAA compared with patients without HAA (173.8 mL vs. 83.5 mL; P<0.001). There was significant variation of diagnostic blood loss between hospitals. The risk of HAA increased by 18% (RR 1.18; 95% CI, 1.13-1.22) for every 50 mL of diagnostic blood loss.
Patients with HAA were noted to have greater disease severity and comorbidities. No causal inference can be made given the observational nature of the study. Randomized trials are needed to evaluate if strategies to reduce diagnostic blood loss can reduce HAA and improve clinical outcomes for patients with AMI.
Bottom line: Diagnostic blood loss is associated with development of hospital-acquired anemia in patients with acute myocardial infarction.
Citation: Salisbury AC, Reid KJ, Alexander KP, et al. Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171:1646-1653.
For more physician reviews of HM-relevant research, visit our website.
Clinical question: To what extent does diagnostic phlebotomy contribute to hospital-acquired anemia (HAA) during acute myocardial infarction (AMI)?
Background: During AMI, hospital-acquired HAA is associated with higher mortality and poorer health status. Moderate to severe HAA (nadir hemoglobin level <11 g/dL) has been shown to be prognostically important. The contribution of diagnostic phlebotomy blood loss on HAA is unknown and is a potentially modifiable factor.
Study design: Retrospective observational cohort study.
Setting: Fifty-seven U.S. hospitals.
Synopsis: Using Cerner Corp.'s Health Facts database, information was collected on 17,676 patients with AMI. Moderate to severe HAA developed in 3,551 (20%) patients who were not anemic upon admission. The diagnostic blood loss was estimated by assuming minimal blood volume per adult tube required to perform the lab work obtained. The mean phlebotomy volume was higher in patients with HAA compared with patients without HAA (173.8 mL vs. 83.5 mL; P<0.001). There was significant variation of diagnostic blood loss between hospitals. The risk of HAA increased by 18% (RR 1.18; 95% CI, 1.13-1.22) for every 50 mL of diagnostic blood loss.
Patients with HAA were noted to have greater disease severity and comorbidities. No causal inference can be made given the observational nature of the study. Randomized trials are needed to evaluate if strategies to reduce diagnostic blood loss can reduce HAA and improve clinical outcomes for patients with AMI.
Bottom line: Diagnostic blood loss is associated with development of hospital-acquired anemia in patients with acute myocardial infarction.
Citation: Salisbury AC, Reid KJ, Alexander KP, et al. Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171:1646-1653.
For more physician reviews of HM-relevant research, visit our website.
In the Literature: Research You Need to Know
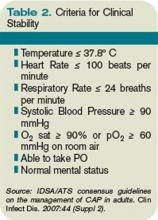
Clinical question: What is the association between time to clinical stability (TCS) and post-discharge death or readmission in patients hospitalized with community-acquired pneumonia (CAP)?
Background: In patients with CAP, inflammatory response during hospitalization might be associated with adverse outcomes after discharge. Studies have not evaluated if time to clinical stability, a reflection of inflammatory response, can be used to identify patients at high risk of adverse outcomes after discharge.
Study design: Retrospective cohort study.
Setting: Veterans Hospital, Louisville, Ky.
Synopsis: Of 464 hospitalized patients with CAP, those with TCS >3 days had a higher rate of readmission or death within 30 days after discharge compared with those who had a TCS =3 days (26% versus 15%; OR 1.98; 95% CI, 1.19-3.3; P=0.008). Longer TCS during hospitalization was associated with a significantly increased risk of adverse outcomes (adjusted OR 1.06, 1.54, 2.40, 10.53 if TCS was reached at days 2, 3, 4, 5 versus Day 1, respectively). The authors proposed that patients with delays in reaching clinical stability should receive a special discharge management approach to decrease the risk of morbidity and mortality after discharge; this may include close observation, home visits, and a follow-up clinic appointment within 10 days.
As a retrospective cohort study, unaccounted-for confounders might exist between TCS and adverse outcomes. The small sample size precluded development of a fully predictive model. Additionally, the population studied was elderly men in a single hospital, which might limit generalizability.
Bottom line: Hospitalized patients with community-acquired pneumonia whose time to clinical stability was greater than three days had a higher risk of readmission or death within 30 days after discharge.
Citation: Aliberti S, Peyrani P, Filardo G, et al. Association between time to clinical stability and outcomes after discharge in hospitalized patients with community-acquired pneumonia. Chest. 2011;140:482-488.
For more physician reviews of HM-relevant research, visit our website.
Clinical question: What is the association between time to clinical stability (TCS) and post-discharge death or readmission in patients hospitalized with community-acquired pneumonia (CAP)?
Background: In patients with CAP, inflammatory response during hospitalization might be associated with adverse outcomes after discharge. Studies have not evaluated if time to clinical stability, a reflection of inflammatory response, can be used to identify patients at high risk of adverse outcomes after discharge.
Study design: Retrospective cohort study.
Setting: Veterans Hospital, Louisville, Ky.
Synopsis: Of 464 hospitalized patients with CAP, those with TCS >3 days had a higher rate of readmission or death within 30 days after discharge compared with those who had a TCS =3 days (26% versus 15%; OR 1.98; 95% CI, 1.19-3.3; P=0.008). Longer TCS during hospitalization was associated with a significantly increased risk of adverse outcomes (adjusted OR 1.06, 1.54, 2.40, 10.53 if TCS was reached at days 2, 3, 4, 5 versus Day 1, respectively). The authors proposed that patients with delays in reaching clinical stability should receive a special discharge management approach to decrease the risk of morbidity and mortality after discharge; this may include close observation, home visits, and a follow-up clinic appointment within 10 days.
As a retrospective cohort study, unaccounted-for confounders might exist between TCS and adverse outcomes. The small sample size precluded development of a fully predictive model. Additionally, the population studied was elderly men in a single hospital, which might limit generalizability.
Bottom line: Hospitalized patients with community-acquired pneumonia whose time to clinical stability was greater than three days had a higher risk of readmission or death within 30 days after discharge.
Citation: Aliberti S, Peyrani P, Filardo G, et al. Association between time to clinical stability and outcomes after discharge in hospitalized patients with community-acquired pneumonia. Chest. 2011;140:482-488.
For more physician reviews of HM-relevant research, visit our website.
Clinical question: What is the association between time to clinical stability (TCS) and post-discharge death or readmission in patients hospitalized with community-acquired pneumonia (CAP)?
Background: In patients with CAP, inflammatory response during hospitalization might be associated with adverse outcomes after discharge. Studies have not evaluated if time to clinical stability, a reflection of inflammatory response, can be used to identify patients at high risk of adverse outcomes after discharge.
Study design: Retrospective cohort study.
Setting: Veterans Hospital, Louisville, Ky.
Synopsis: Of 464 hospitalized patients with CAP, those with TCS >3 days had a higher rate of readmission or death within 30 days after discharge compared with those who had a TCS =3 days (26% versus 15%; OR 1.98; 95% CI, 1.19-3.3; P=0.008). Longer TCS during hospitalization was associated with a significantly increased risk of adverse outcomes (adjusted OR 1.06, 1.54, 2.40, 10.53 if TCS was reached at days 2, 3, 4, 5 versus Day 1, respectively). The authors proposed that patients with delays in reaching clinical stability should receive a special discharge management approach to decrease the risk of morbidity and mortality after discharge; this may include close observation, home visits, and a follow-up clinic appointment within 10 days.
As a retrospective cohort study, unaccounted-for confounders might exist between TCS and adverse outcomes. The small sample size precluded development of a fully predictive model. Additionally, the population studied was elderly men in a single hospital, which might limit generalizability.
Bottom line: Hospitalized patients with community-acquired pneumonia whose time to clinical stability was greater than three days had a higher risk of readmission or death within 30 days after discharge.
Citation: Aliberti S, Peyrani P, Filardo G, et al. Association between time to clinical stability and outcomes after discharge in hospitalized patients with community-acquired pneumonia. Chest. 2011;140:482-488.
For more physician reviews of HM-relevant research, visit our website.
In the Literature: The latest research you need to know
In This Edition
Literature At A Glance
A guide to this month’s studies
- Procalcitonin to guide antimicrobial use in ICU patients
- Platelet reactivity and event rates after PCI
- Conservative treatment of necrotizing pancreatitis
- Use of MRI to diagnose Takotsubo cardiomyopathy
- Rates of inadvertent medication discontinuation after hospitalization
- Role of history and physical exam in diagnosing medical illness
- Red-cell distribution width and rates of mortality
Procalcitonin-Guided Therapy Decreases Antimicrobial Duration in ICU Patients
Clinical question: Can utilization of serum procalcitonin (PCT) levels safely reduce antimicrobial exposure in ICU patients?
Background: Serum PCT levels are elevated in bacterial infections and sepsis and have been used in some settings to guide antimicrobial therapy. Randomized controlled trials have demonstrated reduction of antibiotic use with PCT measurement. This systematic review assessed the safety and effectiveness of PCT measurements in reducing antimicrobial exposure in ICU patients.
Study design: Systematic review.
Setting: Adult medical and surgical ICUs.
Synopsis: A search of MEDLINE and EMBASE yielded 1,018 publications related to PCT, critically ill patients, and antimicrobial therapy. Six randomized controlled trials involving 1,476 patients were reviewed. The duration of antimicrobial use was significantly decreased in all five studies that evaluated treatment duration. The remaining study only assessed the impact of PCT on initiation of antimicrobial therapy and did not demonstrate decreased antimicrobial exposure. Compared with the control group, patients randomized to PCT-guided therapy had relative reductions in duration of first antibiotic course by 21%, down to 38%, and decreases in days of antimicrobial therapy per 1,000 ICU patient days by 20%, down to 23%. PCT intervention also was associated with a 23% to 37% increase in days alive without antimicrobial therapy during the first 28 days. The length of ICU stay was significantly decreased in two studies but was not significantly different in the other studies. There were no significant differences in rates of mortality, infection relapse, or days free of mechanical ventilation.
Bottom line: PCT guidance reduced antimicrobial exposure of ICU patients without increasing rates of mortality or infection relapse.
Citation: Agarwal R, Schwartz DN. Procalcitonin to guide duration of antimicrobial therapy in intensive care units: a systematic review. Clin Infect Dis. 2011;53:379-387.
High Residual Platelet Reactivity Increases Risk of Cardiovascular Events among Patients with Acute Coronary Syndromes Undergoing PCI
Clinical question: Is high residual platelet reactivity (HRPR) in patients receiving clopidogrel associated with increased risk of ischemic events after percutaneous coronary intervention (PCI)?
Background: Studies have demonstrated an increased risk of cardiovascular events associated with HRPR in patients receiving clopidogrel while undergoing PCI. However, these studies have used a variety of platelet function tests, and thresholds for positive tests have not been established. In addition, these studies have enrolled heterogeneous populations with short-term follow-up and few have included patients with acute coronary syndromes (ACSs).
Study design: Prospective cohort study.
Setting: Cardiology service of a referral center in Italy.
Synopsis: This study included 1,789 consecutive patients with ACS undergoing PCI. Patients were given 325 mg aspirin and a 600-mg loading dose of clopidogrel on admission, followed by a daily maintenance dose of aspirin 325 mg and clopidogrel 75 mg for at least six months. Platelet reactivity was measured using adenosine diphosphate (ADP) testing, and those with HRPR (≥70% platelet aggregation) were given increased dosing of clopidogrel or switched to ticlopidine using ADP test guidance. At two-year follow-up, patients with HRPR experienced an increased composite endpoint of cardiac death, myocardial infarction, urgent coronary revascularization, and stroke with a combined event rate of 14.6% in patients with HRPR and 8.7% in patients with low residual platelet reactivity (95% CI, 1.6%-11.1%; P=0.003). Stent thrombosis was also higher in HRPR patients (absolute risk increase 3.2%; 95% CI, 0.4%-6.7%; P=0.01).
This study is nonrandomized, and residual unmeasured confounding cannot be excluded. In addition, use of non-antiplatelet drugs and adherence to recommended drugs might have influenced outcomes.
Bottom line: HRPR is associated with increased risk of ischemic events in patients with ACS receiving antiplatelet agents after PCI.
Citation: Parodi G, Marcucci R, Valenti R, et al. High residual platelet reactivity after clopidogrel loading and long-term cardiovascular events among patients with acute coronary syndromes undergoing PCI. JAMA. 2011;306:1215-1223.
Conservative Treatment of Necrotizing Pancreatitis Is Associated with Improved Outcomes
Clinical question: What are the outcomes of conservative and interventional management of necrotizing pancreatitis?
Background: Open necrosectomy was historically the treatment of choice for necrotizing pancreatitis, but, currently, pancreatic necrosis is only managed invasively when complicated by infection. Other changes in management over time have included a shift in the timing of intervention and the use of minimally invasive techniques. Existing studies do not reflect these changes in practice patterns and have been limited by small sample sizes or the exclusion of important subgroups of patients.
Study design: Prospective cohort study.
Setting: Twenty-one Dutch hospitals.
Synopsis: This study included 639 patients with acute necrotizing pancreatitis confirmed by imaging. Overall mortality was 15%. Conservative treatment was performed in 62% of the patients with a mortality of 7%; however, patients with organ failure (pulmonary, circulatory, and/or renal) who received conservative therapy had a mortality rate of 37%. Intervention (percutaneous drainage, video-assisted retroperitoneal debridement, endoscopic transluminal necrosectomy, laparotomy) in patients with suspected or confirmed infected pancreatic necrosis was performed on 38% of the patients with associated mortality of 27%. Interventions performed within the first 14 days of hospitalization resulted in a 56% mortality rate, whereas interventions performed after Day 29 resulted in a 15% mortality rate (P<0.001). Patients with organ failure experienced significantly greater mortality compared with patients with no organ failure (35% vs. 2%; P<0.001). Primary percutaneous drainage was associated with fewer complications than was primary necrosectomy (42% vs. 64%; P=0.003).
This study was nonrandomized, and final decisions regarding management were left to the treating physician. Notably, while there was no significant difference in APACHE II scores between the conservative and intervention groups, intervention patients had more severe pancreatic disease and scored higher on other measures of disease severity.
Bottom line: Patients with necrotizing pancreatitis can frequently be managed conservatively, though the presence of organ failure and parenchymal necrosis confer poorer prognosis. When intervention is indicated, postponing intervention and utilizing minimally invasive techniques decrease morbidity and mortality.
Citation: Van Santvoort HC, Bakker OJ, Bollen TL, et al. A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology. 2011;141:1254-1263.
Cardiac MRI Complements Clinical Findings in Diagnosis of Stress Cardiomyopathy
Clinical question: What are the clinical features and cardiovascular MRI findings in patients with stress (Takotsubo) cardiomyopathy?
Background: Stress cardiomyopathy (SC) is characterized by acute and profound reversible left ventricular dysfunction that is thought to result from increased sympathetic activity related to emotional and/or physical stress. Prior studies evaluating the clinical features of SC were limited by small sample sizes and single-center enrollment, and cardiac MRI use in SC has not been well studied.
Study design: Prospective cohort study.
Setting: Seven North American and European tertiary-care centers.
Synopsis: This study enrolled 256 patients who met diagnostic criteria for SC according to Mayo criteria. Postmenopausal women were most commonly affected; only 11% of participants were men and 8% were women younger than 50 years old. An identifiable stressor was found in 71% of the patients. Clinical presentation was notable for symptoms of acute coronary syndrome (ACS) in 88% of patients, abnormal electrocardiogram in 87%, and elevated troponin T in 90%. Coronary angiography was normal in three-fourths of patients, and no patients had features of acute plaque rupture. Typical apical ballooning was seen on left ventriculography in 82% of patients.
Cardiac MRI findings included severe left ventricular dysfunction in a noncoronary distribution, myocardial edema in areas of regional wall abnormalities, absence of high signal areas in late gadolinium enhancement (e.g., absence of necrosis/fibrosis), and increased early gadolinium uptake (i.e. early inflammation). Repeat cardiac MRI four weeks after initial diagnosis showed near or complete resolution of imaging findings.
Bottom line: Stress cardiomyopathy typically presents like ACS, usually affects postmenopausal women, is often preceded by a stressful event, and is characterized by cardiac MRI findings of regional wall motion abnormalities, reversible myocardial injury, and the absence of fibrosis. Cardiac MRI may be valuable in diagnosing SC in patients who present without the classic clinical features.
Citation: Eitel I, von Knobelsdorff-Brenkenhoff F, Bernhardt P, et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (Takotsubo) cardiomyopathy. JAMA. 2011;306:277-286.
Increased Risk of Potentially Inadvertent Medication Discontinuation Following Acute-Care Hospitalization
Clinical question: Are medications for chronic diseases inadvertently discontinued after acute-care hospitalization, and is this risk increased in patients who had an ICU stay?
Background: Transitions of care are associated with medical errors. Two such transitions are a shift from the ICU to floor setting and from the inpatient to outpatient setting. Medications for chronic diseases might be held during hospitalization for a variety of reasons, and medication errors may occur if these drugs are not restarted when the acute problem resolves or the patient is discharged from the hospital.
Study design: Population-based cohort study.
Setting: Ontario, Canada.
Synopsis: Using four separate databases, administrative records were reviewed for 396,380 patients aged >65 years who were continuous users of at least one of five evidence-based medication groups for common chronic diseases. Medications included statins, antiplatelet/anticoagulant agents, levothyroxine, respiratory inhalers, and gastric acid suppressants. The primary outcome was potentially unintentional medication discontinuation (measured by failure to renew the prescription at 90 days) for hospitalized versus nonhospitalized patients. All medication groups had statistically significant adjusted odds ratios ranging from 1.18 (95% CI, 1.14-1.23) for discontinuation of levothyroxine to 1.86 (95% CI, 1.77-1.97) for discontinuation of antiplatelet/anticoagulant medications. Treatment in an ICU further increased this risk compared with nonhospitalized patients, and increased the risk for medication discontinuation in four of the five medication groups when compared with patients hospitalized without ICU treatment.
Important study limitations include the lack of appropriate clinical details to classify medication discontinuation as unintentional and the inability of administrative data to prove causality. This study highlights the importance of medication reconciliation and calls attention to inadvertent medication discontinuation during care transitions (see “Reconciliation Act,”).
Bottom line: Patients discharged from the hospital, particularly after ICU treatment, have a higher risk of discontinuation of long-term medications for chronic medical problems when compared with nonhospitalized patients.
Citation: Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306:840-847.
Clinical Exam Remains Valuable in the Diagnosis of Patients Admitted to a Medicine Service
Clinical question: Is a clinical exam useful in the diagnosis of newly admitted patients to a general medicine service?
Background: The clinical exam, which comprises the history and physical examination, has long been described as essential to the diagnosis of illness. However, the literature supporting this claim is limited to the ambulatory setting. There has not been evaluation of the clinical exam as a diagnostic tool in the hospital setting, where more advanced testing is readily available.
Study design: Retrospective chart review.
Setting: Urban academic medical center.
Synopsis: The study included 442 adult patients consecutively admitted from the emergency department to the general medicine service who were separately assessed by one senior resident (SR) and one experienced hospital physician (HP) not involved with the case. The SR and HP each made an initial diagnosis and documented the most helpful component(s) in arriving at that diagnosis. Outcomes included comparison of the SR and HP’s admission diagnosis with the discharge diagnosis, and the diagnostic value of the various components of the clinical exam and initial studies.
Compared with the discharge diagnosis, the SR’s initial diagnosis was correct in 80.1% of cases, while the HP was correct in 84.4%. The patient’s history was the most important element in the initial assessment, independently influencing approximately 20% of the correct diagnoses for both physicians. Approximately 60% of correct diagnoses were established using the history and/or physical, and more than 90% were made using a combination of history, physical exam, and/or basic tests (admission labs, electrocardiogram, chest X-ray).
The generalizability of these results is limited by the retrospective, single-center study design, involvement of only one resident physician, and the lack of information regarding number of experienced clinicians and types of diagnoses.
Bottom line: Among patients admitted to a general medicine service, the most powerful tool in obtaining an accurate diagnosis was the combination of a patient’s history and a physical exam.
Citation: Paley L, Zornitzki T, Cohen J, et al. Utility of clinical examination in the diagnosis of emergency department patients admitted to the department of medicine of an academic hospital. Arch Intern Med. 2011;171:1394-1396.
RDW Predicts All-Cause Mortality and Bloodstream Infection in ICU Patients
Clinical question: Among patients admitted to the ICU, is red blood cell distribution width (RDW) a reliable indicator of mortality?
Background: The RDW is an inexpensive test that is commonly included in routine laboratory studies. It has been associated with multiple disease processes and found to be a strong predictor of mortality in the general adult population. However, there has been limited study of the association between RDW and outcomes in critically ill patients.
Study design: Observational cohort study.
Setting: Urban tertiary-care academic medical center.
Synopsis: Data from 51,413 adult patients who received critical care between 1997 and 2007 were obtained from a computerized registry and evaluated for the primary outcome of 30-day mortality after critical-care initiation. Secondary outcomes included 90-day, 365-day, and in-hospital mortality, as well as bloodstream infection. Logistic regression examined both primary and secondary outcomes in association with pre-established RDW quintiles. After multivariable adjustment, RDW was found to be associated with mortality at 30, 90, and 365 days, in addition to in-hospital mortality. The highest RDW quintile (RDW >15.8%) had an adjusted OR of 2.61 (95% CI, 2.37-2.86; P<0.001) for the primary outcome, with similar risk for secondary outcomes of mortality. A subgroup of 18,525 patients with blood culture data was analyzed and an adjusted OR of 1.44 was found in the highest RDW quintile for the secondary outcome of bloodstream infection.
Bottom line: Red blood cell distribution width is a strong independent predictor of all-cause mortality and bloodstream infection in patients receiving intensive care.
Citation: Bazick HS, Chang D, Mahadevappa K, Gibbons FK, Christopher KB. Red cell distribution width and all-cause mortality in critically ill patients. Crit Care Med. 2011;39:1913-1921.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Procalcitonin to guide antimicrobial use in ICU patients
- Platelet reactivity and event rates after PCI
- Conservative treatment of necrotizing pancreatitis
- Use of MRI to diagnose Takotsubo cardiomyopathy
- Rates of inadvertent medication discontinuation after hospitalization
- Role of history and physical exam in diagnosing medical illness
- Red-cell distribution width and rates of mortality
Procalcitonin-Guided Therapy Decreases Antimicrobial Duration in ICU Patients
Clinical question: Can utilization of serum procalcitonin (PCT) levels safely reduce antimicrobial exposure in ICU patients?
Background: Serum PCT levels are elevated in bacterial infections and sepsis and have been used in some settings to guide antimicrobial therapy. Randomized controlled trials have demonstrated reduction of antibiotic use with PCT measurement. This systematic review assessed the safety and effectiveness of PCT measurements in reducing antimicrobial exposure in ICU patients.
Study design: Systematic review.
Setting: Adult medical and surgical ICUs.
Synopsis: A search of MEDLINE and EMBASE yielded 1,018 publications related to PCT, critically ill patients, and antimicrobial therapy. Six randomized controlled trials involving 1,476 patients were reviewed. The duration of antimicrobial use was significantly decreased in all five studies that evaluated treatment duration. The remaining study only assessed the impact of PCT on initiation of antimicrobial therapy and did not demonstrate decreased antimicrobial exposure. Compared with the control group, patients randomized to PCT-guided therapy had relative reductions in duration of first antibiotic course by 21%, down to 38%, and decreases in days of antimicrobial therapy per 1,000 ICU patient days by 20%, down to 23%. PCT intervention also was associated with a 23% to 37% increase in days alive without antimicrobial therapy during the first 28 days. The length of ICU stay was significantly decreased in two studies but was not significantly different in the other studies. There were no significant differences in rates of mortality, infection relapse, or days free of mechanical ventilation.
Bottom line: PCT guidance reduced antimicrobial exposure of ICU patients without increasing rates of mortality or infection relapse.
Citation: Agarwal R, Schwartz DN. Procalcitonin to guide duration of antimicrobial therapy in intensive care units: a systematic review. Clin Infect Dis. 2011;53:379-387.
High Residual Platelet Reactivity Increases Risk of Cardiovascular Events among Patients with Acute Coronary Syndromes Undergoing PCI
Clinical question: Is high residual platelet reactivity (HRPR) in patients receiving clopidogrel associated with increased risk of ischemic events after percutaneous coronary intervention (PCI)?
Background: Studies have demonstrated an increased risk of cardiovascular events associated with HRPR in patients receiving clopidogrel while undergoing PCI. However, these studies have used a variety of platelet function tests, and thresholds for positive tests have not been established. In addition, these studies have enrolled heterogeneous populations with short-term follow-up and few have included patients with acute coronary syndromes (ACSs).
Study design: Prospective cohort study.
Setting: Cardiology service of a referral center in Italy.
Synopsis: This study included 1,789 consecutive patients with ACS undergoing PCI. Patients were given 325 mg aspirin and a 600-mg loading dose of clopidogrel on admission, followed by a daily maintenance dose of aspirin 325 mg and clopidogrel 75 mg for at least six months. Platelet reactivity was measured using adenosine diphosphate (ADP) testing, and those with HRPR (≥70% platelet aggregation) were given increased dosing of clopidogrel or switched to ticlopidine using ADP test guidance. At two-year follow-up, patients with HRPR experienced an increased composite endpoint of cardiac death, myocardial infarction, urgent coronary revascularization, and stroke with a combined event rate of 14.6% in patients with HRPR and 8.7% in patients with low residual platelet reactivity (95% CI, 1.6%-11.1%; P=0.003). Stent thrombosis was also higher in HRPR patients (absolute risk increase 3.2%; 95% CI, 0.4%-6.7%; P=0.01).
This study is nonrandomized, and residual unmeasured confounding cannot be excluded. In addition, use of non-antiplatelet drugs and adherence to recommended drugs might have influenced outcomes.
Bottom line: HRPR is associated with increased risk of ischemic events in patients with ACS receiving antiplatelet agents after PCI.
Citation: Parodi G, Marcucci R, Valenti R, et al. High residual platelet reactivity after clopidogrel loading and long-term cardiovascular events among patients with acute coronary syndromes undergoing PCI. JAMA. 2011;306:1215-1223.
Conservative Treatment of Necrotizing Pancreatitis Is Associated with Improved Outcomes
Clinical question: What are the outcomes of conservative and interventional management of necrotizing pancreatitis?
Background: Open necrosectomy was historically the treatment of choice for necrotizing pancreatitis, but, currently, pancreatic necrosis is only managed invasively when complicated by infection. Other changes in management over time have included a shift in the timing of intervention and the use of minimally invasive techniques. Existing studies do not reflect these changes in practice patterns and have been limited by small sample sizes or the exclusion of important subgroups of patients.
Study design: Prospective cohort study.
Setting: Twenty-one Dutch hospitals.
Synopsis: This study included 639 patients with acute necrotizing pancreatitis confirmed by imaging. Overall mortality was 15%. Conservative treatment was performed in 62% of the patients with a mortality of 7%; however, patients with organ failure (pulmonary, circulatory, and/or renal) who received conservative therapy had a mortality rate of 37%. Intervention (percutaneous drainage, video-assisted retroperitoneal debridement, endoscopic transluminal necrosectomy, laparotomy) in patients with suspected or confirmed infected pancreatic necrosis was performed on 38% of the patients with associated mortality of 27%. Interventions performed within the first 14 days of hospitalization resulted in a 56% mortality rate, whereas interventions performed after Day 29 resulted in a 15% mortality rate (P<0.001). Patients with organ failure experienced significantly greater mortality compared with patients with no organ failure (35% vs. 2%; P<0.001). Primary percutaneous drainage was associated with fewer complications than was primary necrosectomy (42% vs. 64%; P=0.003).
This study was nonrandomized, and final decisions regarding management were left to the treating physician. Notably, while there was no significant difference in APACHE II scores between the conservative and intervention groups, intervention patients had more severe pancreatic disease and scored higher on other measures of disease severity.
Bottom line: Patients with necrotizing pancreatitis can frequently be managed conservatively, though the presence of organ failure and parenchymal necrosis confer poorer prognosis. When intervention is indicated, postponing intervention and utilizing minimally invasive techniques decrease morbidity and mortality.
Citation: Van Santvoort HC, Bakker OJ, Bollen TL, et al. A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology. 2011;141:1254-1263.
Cardiac MRI Complements Clinical Findings in Diagnosis of Stress Cardiomyopathy
Clinical question: What are the clinical features and cardiovascular MRI findings in patients with stress (Takotsubo) cardiomyopathy?
Background: Stress cardiomyopathy (SC) is characterized by acute and profound reversible left ventricular dysfunction that is thought to result from increased sympathetic activity related to emotional and/or physical stress. Prior studies evaluating the clinical features of SC were limited by small sample sizes and single-center enrollment, and cardiac MRI use in SC has not been well studied.
Study design: Prospective cohort study.
Setting: Seven North American and European tertiary-care centers.
Synopsis: This study enrolled 256 patients who met diagnostic criteria for SC according to Mayo criteria. Postmenopausal women were most commonly affected; only 11% of participants were men and 8% were women younger than 50 years old. An identifiable stressor was found in 71% of the patients. Clinical presentation was notable for symptoms of acute coronary syndrome (ACS) in 88% of patients, abnormal electrocardiogram in 87%, and elevated troponin T in 90%. Coronary angiography was normal in three-fourths of patients, and no patients had features of acute plaque rupture. Typical apical ballooning was seen on left ventriculography in 82% of patients.
Cardiac MRI findings included severe left ventricular dysfunction in a noncoronary distribution, myocardial edema in areas of regional wall abnormalities, absence of high signal areas in late gadolinium enhancement (e.g., absence of necrosis/fibrosis), and increased early gadolinium uptake (i.e. early inflammation). Repeat cardiac MRI four weeks after initial diagnosis showed near or complete resolution of imaging findings.
Bottom line: Stress cardiomyopathy typically presents like ACS, usually affects postmenopausal women, is often preceded by a stressful event, and is characterized by cardiac MRI findings of regional wall motion abnormalities, reversible myocardial injury, and the absence of fibrosis. Cardiac MRI may be valuable in diagnosing SC in patients who present without the classic clinical features.
Citation: Eitel I, von Knobelsdorff-Brenkenhoff F, Bernhardt P, et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (Takotsubo) cardiomyopathy. JAMA. 2011;306:277-286.
Increased Risk of Potentially Inadvertent Medication Discontinuation Following Acute-Care Hospitalization
Clinical question: Are medications for chronic diseases inadvertently discontinued after acute-care hospitalization, and is this risk increased in patients who had an ICU stay?
Background: Transitions of care are associated with medical errors. Two such transitions are a shift from the ICU to floor setting and from the inpatient to outpatient setting. Medications for chronic diseases might be held during hospitalization for a variety of reasons, and medication errors may occur if these drugs are not restarted when the acute problem resolves or the patient is discharged from the hospital.
Study design: Population-based cohort study.
Setting: Ontario, Canada.
Synopsis: Using four separate databases, administrative records were reviewed for 396,380 patients aged >65 years who were continuous users of at least one of five evidence-based medication groups for common chronic diseases. Medications included statins, antiplatelet/anticoagulant agents, levothyroxine, respiratory inhalers, and gastric acid suppressants. The primary outcome was potentially unintentional medication discontinuation (measured by failure to renew the prescription at 90 days) for hospitalized versus nonhospitalized patients. All medication groups had statistically significant adjusted odds ratios ranging from 1.18 (95% CI, 1.14-1.23) for discontinuation of levothyroxine to 1.86 (95% CI, 1.77-1.97) for discontinuation of antiplatelet/anticoagulant medications. Treatment in an ICU further increased this risk compared with nonhospitalized patients, and increased the risk for medication discontinuation in four of the five medication groups when compared with patients hospitalized without ICU treatment.
Important study limitations include the lack of appropriate clinical details to classify medication discontinuation as unintentional and the inability of administrative data to prove causality. This study highlights the importance of medication reconciliation and calls attention to inadvertent medication discontinuation during care transitions (see “Reconciliation Act,”).
Bottom line: Patients discharged from the hospital, particularly after ICU treatment, have a higher risk of discontinuation of long-term medications for chronic medical problems when compared with nonhospitalized patients.
Citation: Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306:840-847.
Clinical Exam Remains Valuable in the Diagnosis of Patients Admitted to a Medicine Service
Clinical question: Is a clinical exam useful in the diagnosis of newly admitted patients to a general medicine service?
Background: The clinical exam, which comprises the history and physical examination, has long been described as essential to the diagnosis of illness. However, the literature supporting this claim is limited to the ambulatory setting. There has not been evaluation of the clinical exam as a diagnostic tool in the hospital setting, where more advanced testing is readily available.
Study design: Retrospective chart review.
Setting: Urban academic medical center.
Synopsis: The study included 442 adult patients consecutively admitted from the emergency department to the general medicine service who were separately assessed by one senior resident (SR) and one experienced hospital physician (HP) not involved with the case. The SR and HP each made an initial diagnosis and documented the most helpful component(s) in arriving at that diagnosis. Outcomes included comparison of the SR and HP’s admission diagnosis with the discharge diagnosis, and the diagnostic value of the various components of the clinical exam and initial studies.
Compared with the discharge diagnosis, the SR’s initial diagnosis was correct in 80.1% of cases, while the HP was correct in 84.4%. The patient’s history was the most important element in the initial assessment, independently influencing approximately 20% of the correct diagnoses for both physicians. Approximately 60% of correct diagnoses were established using the history and/or physical, and more than 90% were made using a combination of history, physical exam, and/or basic tests (admission labs, electrocardiogram, chest X-ray).
The generalizability of these results is limited by the retrospective, single-center study design, involvement of only one resident physician, and the lack of information regarding number of experienced clinicians and types of diagnoses.
Bottom line: Among patients admitted to a general medicine service, the most powerful tool in obtaining an accurate diagnosis was the combination of a patient’s history and a physical exam.
Citation: Paley L, Zornitzki T, Cohen J, et al. Utility of clinical examination in the diagnosis of emergency department patients admitted to the department of medicine of an academic hospital. Arch Intern Med. 2011;171:1394-1396.
RDW Predicts All-Cause Mortality and Bloodstream Infection in ICU Patients
Clinical question: Among patients admitted to the ICU, is red blood cell distribution width (RDW) a reliable indicator of mortality?
Background: The RDW is an inexpensive test that is commonly included in routine laboratory studies. It has been associated with multiple disease processes and found to be a strong predictor of mortality in the general adult population. However, there has been limited study of the association between RDW and outcomes in critically ill patients.
Study design: Observational cohort study.
Setting: Urban tertiary-care academic medical center.
Synopsis: Data from 51,413 adult patients who received critical care between 1997 and 2007 were obtained from a computerized registry and evaluated for the primary outcome of 30-day mortality after critical-care initiation. Secondary outcomes included 90-day, 365-day, and in-hospital mortality, as well as bloodstream infection. Logistic regression examined both primary and secondary outcomes in association with pre-established RDW quintiles. After multivariable adjustment, RDW was found to be associated with mortality at 30, 90, and 365 days, in addition to in-hospital mortality. The highest RDW quintile (RDW >15.8%) had an adjusted OR of 2.61 (95% CI, 2.37-2.86; P<0.001) for the primary outcome, with similar risk for secondary outcomes of mortality. A subgroup of 18,525 patients with blood culture data was analyzed and an adjusted OR of 1.44 was found in the highest RDW quintile for the secondary outcome of bloodstream infection.
Bottom line: Red blood cell distribution width is a strong independent predictor of all-cause mortality and bloodstream infection in patients receiving intensive care.
Citation: Bazick HS, Chang D, Mahadevappa K, Gibbons FK, Christopher KB. Red cell distribution width and all-cause mortality in critically ill patients. Crit Care Med. 2011;39:1913-1921.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Procalcitonin to guide antimicrobial use in ICU patients
- Platelet reactivity and event rates after PCI
- Conservative treatment of necrotizing pancreatitis
- Use of MRI to diagnose Takotsubo cardiomyopathy
- Rates of inadvertent medication discontinuation after hospitalization
- Role of history and physical exam in diagnosing medical illness
- Red-cell distribution width and rates of mortality
Procalcitonin-Guided Therapy Decreases Antimicrobial Duration in ICU Patients
Clinical question: Can utilization of serum procalcitonin (PCT) levels safely reduce antimicrobial exposure in ICU patients?
Background: Serum PCT levels are elevated in bacterial infections and sepsis and have been used in some settings to guide antimicrobial therapy. Randomized controlled trials have demonstrated reduction of antibiotic use with PCT measurement. This systematic review assessed the safety and effectiveness of PCT measurements in reducing antimicrobial exposure in ICU patients.
Study design: Systematic review.
Setting: Adult medical and surgical ICUs.
Synopsis: A search of MEDLINE and EMBASE yielded 1,018 publications related to PCT, critically ill patients, and antimicrobial therapy. Six randomized controlled trials involving 1,476 patients were reviewed. The duration of antimicrobial use was significantly decreased in all five studies that evaluated treatment duration. The remaining study only assessed the impact of PCT on initiation of antimicrobial therapy and did not demonstrate decreased antimicrobial exposure. Compared with the control group, patients randomized to PCT-guided therapy had relative reductions in duration of first antibiotic course by 21%, down to 38%, and decreases in days of antimicrobial therapy per 1,000 ICU patient days by 20%, down to 23%. PCT intervention also was associated with a 23% to 37% increase in days alive without antimicrobial therapy during the first 28 days. The length of ICU stay was significantly decreased in two studies but was not significantly different in the other studies. There were no significant differences in rates of mortality, infection relapse, or days free of mechanical ventilation.
Bottom line: PCT guidance reduced antimicrobial exposure of ICU patients without increasing rates of mortality or infection relapse.
Citation: Agarwal R, Schwartz DN. Procalcitonin to guide duration of antimicrobial therapy in intensive care units: a systematic review. Clin Infect Dis. 2011;53:379-387.
High Residual Platelet Reactivity Increases Risk of Cardiovascular Events among Patients with Acute Coronary Syndromes Undergoing PCI
Clinical question: Is high residual platelet reactivity (HRPR) in patients receiving clopidogrel associated with increased risk of ischemic events after percutaneous coronary intervention (PCI)?
Background: Studies have demonstrated an increased risk of cardiovascular events associated with HRPR in patients receiving clopidogrel while undergoing PCI. However, these studies have used a variety of platelet function tests, and thresholds for positive tests have not been established. In addition, these studies have enrolled heterogeneous populations with short-term follow-up and few have included patients with acute coronary syndromes (ACSs).
Study design: Prospective cohort study.
Setting: Cardiology service of a referral center in Italy.
Synopsis: This study included 1,789 consecutive patients with ACS undergoing PCI. Patients were given 325 mg aspirin and a 600-mg loading dose of clopidogrel on admission, followed by a daily maintenance dose of aspirin 325 mg and clopidogrel 75 mg for at least six months. Platelet reactivity was measured using adenosine diphosphate (ADP) testing, and those with HRPR (≥70% platelet aggregation) were given increased dosing of clopidogrel or switched to ticlopidine using ADP test guidance. At two-year follow-up, patients with HRPR experienced an increased composite endpoint of cardiac death, myocardial infarction, urgent coronary revascularization, and stroke with a combined event rate of 14.6% in patients with HRPR and 8.7% in patients with low residual platelet reactivity (95% CI, 1.6%-11.1%; P=0.003). Stent thrombosis was also higher in HRPR patients (absolute risk increase 3.2%; 95% CI, 0.4%-6.7%; P=0.01).
This study is nonrandomized, and residual unmeasured confounding cannot be excluded. In addition, use of non-antiplatelet drugs and adherence to recommended drugs might have influenced outcomes.
Bottom line: HRPR is associated with increased risk of ischemic events in patients with ACS receiving antiplatelet agents after PCI.
Citation: Parodi G, Marcucci R, Valenti R, et al. High residual platelet reactivity after clopidogrel loading and long-term cardiovascular events among patients with acute coronary syndromes undergoing PCI. JAMA. 2011;306:1215-1223.
Conservative Treatment of Necrotizing Pancreatitis Is Associated with Improved Outcomes
Clinical question: What are the outcomes of conservative and interventional management of necrotizing pancreatitis?
Background: Open necrosectomy was historically the treatment of choice for necrotizing pancreatitis, but, currently, pancreatic necrosis is only managed invasively when complicated by infection. Other changes in management over time have included a shift in the timing of intervention and the use of minimally invasive techniques. Existing studies do not reflect these changes in practice patterns and have been limited by small sample sizes or the exclusion of important subgroups of patients.
Study design: Prospective cohort study.
Setting: Twenty-one Dutch hospitals.
Synopsis: This study included 639 patients with acute necrotizing pancreatitis confirmed by imaging. Overall mortality was 15%. Conservative treatment was performed in 62% of the patients with a mortality of 7%; however, patients with organ failure (pulmonary, circulatory, and/or renal) who received conservative therapy had a mortality rate of 37%. Intervention (percutaneous drainage, video-assisted retroperitoneal debridement, endoscopic transluminal necrosectomy, laparotomy) in patients with suspected or confirmed infected pancreatic necrosis was performed on 38% of the patients with associated mortality of 27%. Interventions performed within the first 14 days of hospitalization resulted in a 56% mortality rate, whereas interventions performed after Day 29 resulted in a 15% mortality rate (P<0.001). Patients with organ failure experienced significantly greater mortality compared with patients with no organ failure (35% vs. 2%; P<0.001). Primary percutaneous drainage was associated with fewer complications than was primary necrosectomy (42% vs. 64%; P=0.003).
This study was nonrandomized, and final decisions regarding management were left to the treating physician. Notably, while there was no significant difference in APACHE II scores between the conservative and intervention groups, intervention patients had more severe pancreatic disease and scored higher on other measures of disease severity.
Bottom line: Patients with necrotizing pancreatitis can frequently be managed conservatively, though the presence of organ failure and parenchymal necrosis confer poorer prognosis. When intervention is indicated, postponing intervention and utilizing minimally invasive techniques decrease morbidity and mortality.
Citation: Van Santvoort HC, Bakker OJ, Bollen TL, et al. A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology. 2011;141:1254-1263.
Cardiac MRI Complements Clinical Findings in Diagnosis of Stress Cardiomyopathy
Clinical question: What are the clinical features and cardiovascular MRI findings in patients with stress (Takotsubo) cardiomyopathy?
Background: Stress cardiomyopathy (SC) is characterized by acute and profound reversible left ventricular dysfunction that is thought to result from increased sympathetic activity related to emotional and/or physical stress. Prior studies evaluating the clinical features of SC were limited by small sample sizes and single-center enrollment, and cardiac MRI use in SC has not been well studied.
Study design: Prospective cohort study.
Setting: Seven North American and European tertiary-care centers.
Synopsis: This study enrolled 256 patients who met diagnostic criteria for SC according to Mayo criteria. Postmenopausal women were most commonly affected; only 11% of participants were men and 8% were women younger than 50 years old. An identifiable stressor was found in 71% of the patients. Clinical presentation was notable for symptoms of acute coronary syndrome (ACS) in 88% of patients, abnormal electrocardiogram in 87%, and elevated troponin T in 90%. Coronary angiography was normal in three-fourths of patients, and no patients had features of acute plaque rupture. Typical apical ballooning was seen on left ventriculography in 82% of patients.
Cardiac MRI findings included severe left ventricular dysfunction in a noncoronary distribution, myocardial edema in areas of regional wall abnormalities, absence of high signal areas in late gadolinium enhancement (e.g., absence of necrosis/fibrosis), and increased early gadolinium uptake (i.e. early inflammation). Repeat cardiac MRI four weeks after initial diagnosis showed near or complete resolution of imaging findings.
Bottom line: Stress cardiomyopathy typically presents like ACS, usually affects postmenopausal women, is often preceded by a stressful event, and is characterized by cardiac MRI findings of regional wall motion abnormalities, reversible myocardial injury, and the absence of fibrosis. Cardiac MRI may be valuable in diagnosing SC in patients who present without the classic clinical features.
Citation: Eitel I, von Knobelsdorff-Brenkenhoff F, Bernhardt P, et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (Takotsubo) cardiomyopathy. JAMA. 2011;306:277-286.
Increased Risk of Potentially Inadvertent Medication Discontinuation Following Acute-Care Hospitalization
Clinical question: Are medications for chronic diseases inadvertently discontinued after acute-care hospitalization, and is this risk increased in patients who had an ICU stay?
Background: Transitions of care are associated with medical errors. Two such transitions are a shift from the ICU to floor setting and from the inpatient to outpatient setting. Medications for chronic diseases might be held during hospitalization for a variety of reasons, and medication errors may occur if these drugs are not restarted when the acute problem resolves or the patient is discharged from the hospital.
Study design: Population-based cohort study.
Setting: Ontario, Canada.
Synopsis: Using four separate databases, administrative records were reviewed for 396,380 patients aged >65 years who were continuous users of at least one of five evidence-based medication groups for common chronic diseases. Medications included statins, antiplatelet/anticoagulant agents, levothyroxine, respiratory inhalers, and gastric acid suppressants. The primary outcome was potentially unintentional medication discontinuation (measured by failure to renew the prescription at 90 days) for hospitalized versus nonhospitalized patients. All medication groups had statistically significant adjusted odds ratios ranging from 1.18 (95% CI, 1.14-1.23) for discontinuation of levothyroxine to 1.86 (95% CI, 1.77-1.97) for discontinuation of antiplatelet/anticoagulant medications. Treatment in an ICU further increased this risk compared with nonhospitalized patients, and increased the risk for medication discontinuation in four of the five medication groups when compared with patients hospitalized without ICU treatment.
Important study limitations include the lack of appropriate clinical details to classify medication discontinuation as unintentional and the inability of administrative data to prove causality. This study highlights the importance of medication reconciliation and calls attention to inadvertent medication discontinuation during care transitions (see “Reconciliation Act,”).
Bottom line: Patients discharged from the hospital, particularly after ICU treatment, have a higher risk of discontinuation of long-term medications for chronic medical problems when compared with nonhospitalized patients.
Citation: Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306:840-847.
Clinical Exam Remains Valuable in the Diagnosis of Patients Admitted to a Medicine Service
Clinical question: Is a clinical exam useful in the diagnosis of newly admitted patients to a general medicine service?
Background: The clinical exam, which comprises the history and physical examination, has long been described as essential to the diagnosis of illness. However, the literature supporting this claim is limited to the ambulatory setting. There has not been evaluation of the clinical exam as a diagnostic tool in the hospital setting, where more advanced testing is readily available.
Study design: Retrospective chart review.
Setting: Urban academic medical center.
Synopsis: The study included 442 adult patients consecutively admitted from the emergency department to the general medicine service who were separately assessed by one senior resident (SR) and one experienced hospital physician (HP) not involved with the case. The SR and HP each made an initial diagnosis and documented the most helpful component(s) in arriving at that diagnosis. Outcomes included comparison of the SR and HP’s admission diagnosis with the discharge diagnosis, and the diagnostic value of the various components of the clinical exam and initial studies.
Compared with the discharge diagnosis, the SR’s initial diagnosis was correct in 80.1% of cases, while the HP was correct in 84.4%. The patient’s history was the most important element in the initial assessment, independently influencing approximately 20% of the correct diagnoses for both physicians. Approximately 60% of correct diagnoses were established using the history and/or physical, and more than 90% were made using a combination of history, physical exam, and/or basic tests (admission labs, electrocardiogram, chest X-ray).
The generalizability of these results is limited by the retrospective, single-center study design, involvement of only one resident physician, and the lack of information regarding number of experienced clinicians and types of diagnoses.
Bottom line: Among patients admitted to a general medicine service, the most powerful tool in obtaining an accurate diagnosis was the combination of a patient’s history and a physical exam.
Citation: Paley L, Zornitzki T, Cohen J, et al. Utility of clinical examination in the diagnosis of emergency department patients admitted to the department of medicine of an academic hospital. Arch Intern Med. 2011;171:1394-1396.
RDW Predicts All-Cause Mortality and Bloodstream Infection in ICU Patients
Clinical question: Among patients admitted to the ICU, is red blood cell distribution width (RDW) a reliable indicator of mortality?
Background: The RDW is an inexpensive test that is commonly included in routine laboratory studies. It has been associated with multiple disease processes and found to be a strong predictor of mortality in the general adult population. However, there has been limited study of the association between RDW and outcomes in critically ill patients.
Study design: Observational cohort study.
Setting: Urban tertiary-care academic medical center.
Synopsis: Data from 51,413 adult patients who received critical care between 1997 and 2007 were obtained from a computerized registry and evaluated for the primary outcome of 30-day mortality after critical-care initiation. Secondary outcomes included 90-day, 365-day, and in-hospital mortality, as well as bloodstream infection. Logistic regression examined both primary and secondary outcomes in association with pre-established RDW quintiles. After multivariable adjustment, RDW was found to be associated with mortality at 30, 90, and 365 days, in addition to in-hospital mortality. The highest RDW quintile (RDW >15.8%) had an adjusted OR of 2.61 (95% CI, 2.37-2.86; P<0.001) for the primary outcome, with similar risk for secondary outcomes of mortality. A subgroup of 18,525 patients with blood culture data was analyzed and an adjusted OR of 1.44 was found in the highest RDW quintile for the secondary outcome of bloodstream infection.
Bottom line: Red blood cell distribution width is a strong independent predictor of all-cause mortality and bloodstream infection in patients receiving intensive care.
Citation: Bazick HS, Chang D, Mahadevappa K, Gibbons FK, Christopher KB. Red cell distribution width and all-cause mortality in critically ill patients. Crit Care Med. 2011;39:1913-1921.
In the Literature: HM-Related Research You Need to Know
In This Edition
Literature at a Glance
A guide to this month’s studies
- Continuous insulin infusion in non-ICU patients
- How hospitalists spend their day
- Outcomes of patients leaving against medical advice
- Prediction rule for readmission
- Effects of high- vs. low-dose PPIs for peptic ulcer
- Hospital utilization by generalists before hospitalists
- Effect of hospitalist fragmentation on length of stay
- Medication errors at admissions in older patients
Continuous Insulin Infusion Provides Effective Glycemic Control in Non-ICU Patients
Clinical question: Is continuous insulin infusion (CII) a safe and effective option in the management of hyperglycemia in non-ICU patients?
Background: Hyperglycemia has been associated with worse outcomes in hospitalized patients. Prior research has demonstrated the benefit of CII in managing hyperglycemia in the ICU setting. However, outcomes have not been evaluated in the general medical (non-ICU) setting, where hyperglycemia is often inadequately addressed.
Study design: Retrospective chart review.
Setting: Urban tertiary-care medical center.
Synopsis: Charts of 200 adult patients treated with CII in non-ICU areas were reviewed with the primary outcomes including mean daily blood glucose (BG) levels and number of hyper- and hypoglycemic events occurring on CII. Mean BG dropped from 323 mg/dL to 182 mg/dL by day one, with a BG≤of 150 achieved in 67% of patients by day two of therapy. Twenty-two percent of patients suffered a hypoglycemic event (BG<60), reportedly similar to prior studies of insulin use in ICU and non-ICU settings. Eighty-two percent of patients received some form of nutritional support while on CII. In multivariate analyses, receiving oral nutrition (either a solid or liquid diet) was the only factor associated with increased risk of hyperglycemia and hypoglycemia.
This study was limited by its retrospective analysis in a single center. No comparison was made with basal-bolus or sliding-scale insulin therapy regarding efficacy or safety.
Bottom line: Non-ICU patients with hyperglycemia who received CII were able to achieve effective glycemic control within 48 hours of initiation, with rates of hypoglycemia comparable to those observed in ICU settings.
Citation: Smiley D, Rhee M, Peng L, et al. Safety and efficacy of continuous insulin infusion in noncritical care settings. J Hosp Med. 2010;5(4):212-217.
Hospitalists Spend More Time on Indirect, Rather Than Direct, Patient Care
Clinical question: What are the components of the daily workflow of hospitalists working on a non-housestaff service?
Background: The use of hospitalists is associated with increased efficiency in the hospital setting. However, it is not known how this efficiency is achieved. Prior literature has attempted to address this question, but with increasing demands and patient census, the representativeness of existing data is unclear.
Study design: Observational time-motion study.
Setting: Urban tertiary-care academic medical center.
Synopsis: Twenty-four hospitalists were directly observed for two weekday shifts. An electronic collection tool was developed using initial data on hospitalist activities and piloted prior to formal study data collection. Direct patient care was defined as involving face-to-face interaction between hospitalist and patient, while indirect patient care involved activities relevant to patient care but not performed in the patient’s presence.
Approximately 500 hours of observation were collected. Direct patient care comprised only a mean of 17.4% of the hospitalists’ daily workflow, while more was spent on indirect care, mainly electronic health record (EHR) documentation (mean 34.1%) and communication activities (mean 25.9%). Multitasking occurred 16% of the time, typically during communication or “critical documentation activities” (e.g. writing prescriptions). As patient volume increased, less time was spent in communication, and documentation was deferred to after hours.
These results were consistent with prior observational studies but were limited to a single center and might not represent the workflow of hospitalists in other settings, such as community hospitals, or nocturnists.
Bottom line: Hospitalists on non-housestaff services spend most of their time on indirect patient care and, with increasing patient census, communication is sacrificed. Multitasking is common during periods of communication and critical documentation.
Citation: Tipping MD, Forth VE, O’Leary KJ, et al. Where did the day go?—a time-motion study of hospitalists. J Hosp Med. 2010;5(6):323-328.
Patients Who Leave Against Medical Advice Have Higher Readmission, Mortality Rates
Clinical question: What are the 30-day hospital readmission and mortality rates for Veterans Administration (VA) patients discharged against medical advice (AMA) compared with those appropriately discharged from the hospital?
Background: Patients discharged AMA might be at increased risk of experiencing worse outcomes. Small studies have demonstrated that patients with asthma and acute myocardial infarction (MI) discharged AMA have increased risk of readmission and death. However, it is unclear whether these risks are generalizable to a wider medical population.
Study design: Five-year retrospective cohort study.
Setting: One hundred twenty-nine VA acute-care hospitals.
Synopsis: Of the nearly 2 million patients admitted to the VA from 2004 to 2008, 1.7% were discharged AMA. Patients discharged AMA generally were younger, had lower incomes, and were more likely to be black. Furthermore, patients discharged AMA had statistically significant higher rates of 30-day readmission (17.7% vs. 11%, P<0.001) and higher 30-day mortality rates (0.75% vs. 0.61%, P=0.001) compared with those who had been appropriately discharged. In hazard models, discharge AMA was a significant predictor of 30-day readmission and conferred a nonstatistically significant increase in 30-day mortality.
Because all patients were seen in VA facilities, the results might not be generalizable to other acute-care settings. Although VA patients differ from the general medical population, the characteristics of patients discharged AMA are similar to those in previously published studies. The study utilized administrative data, which are very reliable but limited by little information on clinical factors that could contribute to AMA discharges.
Bottom line: Patients discharged AMA are at increased risk of worse post-hospitalization outcomes, including hospital readmission and death.
Citation: Glasgow JM, Vaughn-Sarrazin M, Kaboli PJ. Leaving against medical advice (AMA): risk of 30-day mortality and hospital readmission. J Gen Intern Med. 2010;25(9): 926-929.
Simple Model Predicts Hospital Readmission
Clinical question: Which patient-level factors can be used in a simple model to predict hospital readmission of medicine patients?
Background: Hospital readmissions are common and costly. Previously published readmission prediction models have had limited utility because they focused on a specific condition, setting, or population, or were too cumbersome for practical use.
Study design: Prospective observational cohort study.
Setting: Six academic medical centers.
Synopsis: Data from nearly 11,000 general medicine patients were included in the analysis. Overall, almost 18% of patients were readmitted within 30 days of discharge.
In the prediction model derived and validated from the data, seven factors were significant predictors of readmission within 30 days of discharge: insurance status, marital status, having a regular healthcare provider, Charlson comorbidity index, SF 12 physical component score, one or more admissions within the last year, and current length of stay greater than two days. Points assigned from each significant predictor were used to create a risk score. The 5% of patients with risk scores of 25 and higher had 30-day readmission rates of approximately 30%, compared to readmission rates of approximately 16% in patients with scores of less than 25.
These results might not be generalizable to small, rural, nonacademic settings. Planned admissions could not be excluded from the data, and readmissions to nonstudy hospitals could not be ascertained. Despite these limitations, this model is easier to use than prior models and relevant to a broad population of patients.
Bottom line: A simple prediction model using patient-level factors can be used to identify patients at higher risk of readmission within 30 days of discharge to home.
Citation: Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25(3):211-219.
No Difference in Outcomes Between High- and Non-High-Dose Proton Pump Inhibitors in Bleeding Peptic Ulcers
Clinical question: Do high-dose proton pump inhibitors (PPIs) decrease the rate of rebleeding, surgical intervention, or mortality in patients with bleeding peptic ulcers who have undergone endoscopic treatment?
Background: Previous studies have demonstrated superiority of both high- and low-dose PPIs to H2 receptor antagonists and placebo in reducing rebleeding rates in patients with peptic ulcers. However, no clear evidence is available to suggest that high-dose PPIs are more effective than non-high-dose PPIs for treatment of bleeding peptic ulcers.
Study design: Systematic review and meta-analysis.
Setting: Multicenter and single-site studies conducted in several countries.
Synopsis: Studies were included if they were randomized controlled trials, compared high- versus non-high-dose PPIs, evaluated endoscopically confirmed bleeding ulcers, gave PPIs after endoscopy, and documented outcomes regarding rates of rebleeding, surgical intervention, or mortality. High-dose PPIs were defined as equivalent to omeprazole 80 mg intravenous bolus followed by continuous intravenous infusion at 8 mg/hr for 72 hours.
Seven studies met inclusion criteria. The pooled odds ratios for rebleeding, surgical intervention, and mortality were 1.30 (95% CI, 0.88-1.91), 1.49 (95% CI, 0.66-3.37), and 0.89 (95% CI, 0.37-2.13), respectively, for high-dose versus non-high-dose PPIs. The authors concluded that high-dose PPIs were not superior to non-high-dose PPIs in reducing the rates of these adverse outcomes after endoscopic treatment of bleeding ulcers. Considering the cost of high-dose PPIs, further studies are indicated to help guide PPI dosing for patients with peptic ulcers.
Major limitations of this study were the small number of studies (1,157 patients in total) and their heterogeneity, and the lack of intention-to-treat analysis. The studies also included a high Asian predominance, and it has been shown that Asian populations have an enhanced PPI effect.
Bottom line: High-dose PPIs did not demonstrate reduced rates of ulcer rebleeding, surgical intervention, or mortality compared with non-high-dose PPIs in this meta-analysis, which included a small number of studies and patients.
Citation: Wang CH, Ma MH, Chou HC, et al. High-dose vs. non-high-dose proton pump inhibitors after endoscopic treatment in patients with bleeding peptic ulcer: a systematic review and meta-analysis of randomized controlled trials. Arch Intern Med. 2010;170(9):751-758.
Hospital Utilization by Practicing Generalists Declined before the Emergence of Hospitalists
Clinical question: What has been the pattern of hospital utilization by generalists before and after the emergence of hospitalists?
Background: It has been proposed that the emergence of hospitalists has “crowded out” generalist physicians from the U.S. hospital setting. This study evaluated the trends of inpatient practice by generalists both before and after the emergence of hospitalists.
Study design: Retrospective analysis of national databases.
Setting: U.S. data from 1980 to 2005.
Synopsis: Utilizing the National Hospital Discharge Survey and the American Medical Association’s Physician Characteristics and Distribution in the U.S., information was extracted to evaluate the average number of annual inpatient encounters relative to generalist workforce from 1980 to 2005. Total inpatient encounters for each year were calculated by multiplying the total number of hospital admissions by the average hospital length of stay. The emergence of hospitalists was defined as beginning in 1994.
Total inpatient encounters by generalists declined by 35% in the pre-hospitalist era but remained essentially unchanged in the hospitalist era. During the pre-hospitalist period, the number of generalists doubled, to more than 200,000 from approximately 100,000, while the number of hospital discharges remained relatively stable and the length of stay declined by a third. The decrease in average inpatient encounters in the pre-hospitalist era is thought to have been secondary to decreased length of stay and increased workforce.
Bottom line: Hospital utilization relative to generalist physician workforce was decreasing prior to the emergence of hospitalists mainly due to decreased length of hospital stay and increased numbers of physicians.
Citation: Meltzer DO, Chung JW. U.S. trends in hospitalization and generalist physician workforce and the emergence of hospitalists. J Gen Intern Med. 2010;25(5):453-459.
Fragmentation of Hospitalist Care Is Associated with Increased Length of Stay
Clinical question: Does fragmentation of care (FOC) by hospitalists affect length of stay (LOS)?
Background: Previous investigations have explored the impact of FOC provided by residency programs on LOS and quality of care. Results of these studies have been mixed. However, there have been no prior studies on the impact of the fragmentation of hospitalist care on LOS.
Study design: Concurrent control study.
Setting: Hospitalist practices all over the country managed by IPC: The Hospitalist Company.
Synopsis: Investigators looked at 10,977 patients admitted with diagnoses of pneumonia or heart failure. The primary endpoint was LOS. The independent variable of interest was a measure of FOC. The FOC was calculated as a quantitative index, by determining the percentage of hospitalist care delivered by a physician other than the primary hospitalist.
Multivariable analyses revealed a statistically significant increase in LOS of 0.39 days for each 10% increase in fragmentation level for pneumonia admissions. Similarly, for patients with heart failure, there was a significant increase in LOS of 0.30 days for each 10% increase in fragmentation level.
The study is a concurrent control study, so conclusions cannot be drawn about causality. Additionally, there are likely unmeasured differences between every hospital and hospitalist practice, which could further confound the relationships between hospitalist care and LOS.
Bottom line: Fragmentation of care provided by hospitalists is associated with an increased LOS in patients hospitalized for pneumonia or heart failure.
Citation: Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-338.
Admission Medication Errors Are Common and Most Harmful in Older Patients Taking Many Medications
Clinical question: What are the risk factors and potential harm associated with medication errors at hospital admission?
Background: Obtaining a medication history from a hospitalized patient is an error-prone process. Several variables can affect the completeness and quality of medication histories, but existing data are limited regarding patient or medication risk factors associated with medication errors at admission.
Study design: Prospective cohort study.
Setting: Academic hospital in Chicago.
Synopsis: Pharmacist and admitting physician medication histories were compared with admission medication orders to identify any unexplained discrepancies. Discrepancies resulting in order changes were defined as medication errors.
Of the 651 adult medical inpatients studied, 234 (35.9%) had medication order errors identified at admission. Errors originated in the medication histories for 85% of these patients. The most frequent type of error was an omission (48.9%). An age of 65 or older (odds ratio [OR]=2.17, 95% confidence interval [CI], 1.09-4.30) and increased number of medications (OR=1.21, 95% CI, 1.14-1.29) were the only risk factors identified by multivariate analysis to be independently associated with increased risk of medication order errors potentially causing harm or requiring monitoring or intervention. Presenting a medication list upon admission was a significant protective factor (OR=0.35, 95% CI, 0.19-0.63).
Though this is the largest study to date evaluating admission medication errors in hospitalized medical patients, it remains limited by its single hospital site. Because the authors were unable to interview patients who were too ill or unwilling to participate and had no caregiver present, they might have underestimated the number of admission errors. Further, the harm assessment was based on potential and not actual harm.
Bottom line: Admission medication order errors are frequent, most commonly originate in the medication histories, and have increased potential to cause adverse outcomes in older patients and those taking higher numbers of medications.
Citation: Gleason KM, McDaniel MR, Feinglass J, et al. Results of the Medications At Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25(5):441-447.
In This Edition
Literature at a Glance
A guide to this month’s studies
- Continuous insulin infusion in non-ICU patients
- How hospitalists spend their day
- Outcomes of patients leaving against medical advice
- Prediction rule for readmission
- Effects of high- vs. low-dose PPIs for peptic ulcer
- Hospital utilization by generalists before hospitalists
- Effect of hospitalist fragmentation on length of stay
- Medication errors at admissions in older patients
Continuous Insulin Infusion Provides Effective Glycemic Control in Non-ICU Patients
Clinical question: Is continuous insulin infusion (CII) a safe and effective option in the management of hyperglycemia in non-ICU patients?
Background: Hyperglycemia has been associated with worse outcomes in hospitalized patients. Prior research has demonstrated the benefit of CII in managing hyperglycemia in the ICU setting. However, outcomes have not been evaluated in the general medical (non-ICU) setting, where hyperglycemia is often inadequately addressed.
Study design: Retrospective chart review.
Setting: Urban tertiary-care medical center.
Synopsis: Charts of 200 adult patients treated with CII in non-ICU areas were reviewed with the primary outcomes including mean daily blood glucose (BG) levels and number of hyper- and hypoglycemic events occurring on CII. Mean BG dropped from 323 mg/dL to 182 mg/dL by day one, with a BG≤of 150 achieved in 67% of patients by day two of therapy. Twenty-two percent of patients suffered a hypoglycemic event (BG<60), reportedly similar to prior studies of insulin use in ICU and non-ICU settings. Eighty-two percent of patients received some form of nutritional support while on CII. In multivariate analyses, receiving oral nutrition (either a solid or liquid diet) was the only factor associated with increased risk of hyperglycemia and hypoglycemia.
This study was limited by its retrospective analysis in a single center. No comparison was made with basal-bolus or sliding-scale insulin therapy regarding efficacy or safety.
Bottom line: Non-ICU patients with hyperglycemia who received CII were able to achieve effective glycemic control within 48 hours of initiation, with rates of hypoglycemia comparable to those observed in ICU settings.
Citation: Smiley D, Rhee M, Peng L, et al. Safety and efficacy of continuous insulin infusion in noncritical care settings. J Hosp Med. 2010;5(4):212-217.
Hospitalists Spend More Time on Indirect, Rather Than Direct, Patient Care
Clinical question: What are the components of the daily workflow of hospitalists working on a non-housestaff service?
Background: The use of hospitalists is associated with increased efficiency in the hospital setting. However, it is not known how this efficiency is achieved. Prior literature has attempted to address this question, but with increasing demands and patient census, the representativeness of existing data is unclear.
Study design: Observational time-motion study.
Setting: Urban tertiary-care academic medical center.
Synopsis: Twenty-four hospitalists were directly observed for two weekday shifts. An electronic collection tool was developed using initial data on hospitalist activities and piloted prior to formal study data collection. Direct patient care was defined as involving face-to-face interaction between hospitalist and patient, while indirect patient care involved activities relevant to patient care but not performed in the patient’s presence.
Approximately 500 hours of observation were collected. Direct patient care comprised only a mean of 17.4% of the hospitalists’ daily workflow, while more was spent on indirect care, mainly electronic health record (EHR) documentation (mean 34.1%) and communication activities (mean 25.9%). Multitasking occurred 16% of the time, typically during communication or “critical documentation activities” (e.g. writing prescriptions). As patient volume increased, less time was spent in communication, and documentation was deferred to after hours.
These results were consistent with prior observational studies but were limited to a single center and might not represent the workflow of hospitalists in other settings, such as community hospitals, or nocturnists.
Bottom line: Hospitalists on non-housestaff services spend most of their time on indirect patient care and, with increasing patient census, communication is sacrificed. Multitasking is common during periods of communication and critical documentation.
Citation: Tipping MD, Forth VE, O’Leary KJ, et al. Where did the day go?—a time-motion study of hospitalists. J Hosp Med. 2010;5(6):323-328.
Patients Who Leave Against Medical Advice Have Higher Readmission, Mortality Rates
Clinical question: What are the 30-day hospital readmission and mortality rates for Veterans Administration (VA) patients discharged against medical advice (AMA) compared with those appropriately discharged from the hospital?
Background: Patients discharged AMA might be at increased risk of experiencing worse outcomes. Small studies have demonstrated that patients with asthma and acute myocardial infarction (MI) discharged AMA have increased risk of readmission and death. However, it is unclear whether these risks are generalizable to a wider medical population.
Study design: Five-year retrospective cohort study.
Setting: One hundred twenty-nine VA acute-care hospitals.
Synopsis: Of the nearly 2 million patients admitted to the VA from 2004 to 2008, 1.7% were discharged AMA. Patients discharged AMA generally were younger, had lower incomes, and were more likely to be black. Furthermore, patients discharged AMA had statistically significant higher rates of 30-day readmission (17.7% vs. 11%, P<0.001) and higher 30-day mortality rates (0.75% vs. 0.61%, P=0.001) compared with those who had been appropriately discharged. In hazard models, discharge AMA was a significant predictor of 30-day readmission and conferred a nonstatistically significant increase in 30-day mortality.
Because all patients were seen in VA facilities, the results might not be generalizable to other acute-care settings. Although VA patients differ from the general medical population, the characteristics of patients discharged AMA are similar to those in previously published studies. The study utilized administrative data, which are very reliable but limited by little information on clinical factors that could contribute to AMA discharges.
Bottom line: Patients discharged AMA are at increased risk of worse post-hospitalization outcomes, including hospital readmission and death.
Citation: Glasgow JM, Vaughn-Sarrazin M, Kaboli PJ. Leaving against medical advice (AMA): risk of 30-day mortality and hospital readmission. J Gen Intern Med. 2010;25(9): 926-929.
Simple Model Predicts Hospital Readmission
Clinical question: Which patient-level factors can be used in a simple model to predict hospital readmission of medicine patients?
Background: Hospital readmissions are common and costly. Previously published readmission prediction models have had limited utility because they focused on a specific condition, setting, or population, or were too cumbersome for practical use.
Study design: Prospective observational cohort study.
Setting: Six academic medical centers.
Synopsis: Data from nearly 11,000 general medicine patients were included in the analysis. Overall, almost 18% of patients were readmitted within 30 days of discharge.
In the prediction model derived and validated from the data, seven factors were significant predictors of readmission within 30 days of discharge: insurance status, marital status, having a regular healthcare provider, Charlson comorbidity index, SF 12 physical component score, one or more admissions within the last year, and current length of stay greater than two days. Points assigned from each significant predictor were used to create a risk score. The 5% of patients with risk scores of 25 and higher had 30-day readmission rates of approximately 30%, compared to readmission rates of approximately 16% in patients with scores of less than 25.
These results might not be generalizable to small, rural, nonacademic settings. Planned admissions could not be excluded from the data, and readmissions to nonstudy hospitals could not be ascertained. Despite these limitations, this model is easier to use than prior models and relevant to a broad population of patients.
Bottom line: A simple prediction model using patient-level factors can be used to identify patients at higher risk of readmission within 30 days of discharge to home.
Citation: Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25(3):211-219.
No Difference in Outcomes Between High- and Non-High-Dose Proton Pump Inhibitors in Bleeding Peptic Ulcers
Clinical question: Do high-dose proton pump inhibitors (PPIs) decrease the rate of rebleeding, surgical intervention, or mortality in patients with bleeding peptic ulcers who have undergone endoscopic treatment?
Background: Previous studies have demonstrated superiority of both high- and low-dose PPIs to H2 receptor antagonists and placebo in reducing rebleeding rates in patients with peptic ulcers. However, no clear evidence is available to suggest that high-dose PPIs are more effective than non-high-dose PPIs for treatment of bleeding peptic ulcers.
Study design: Systematic review and meta-analysis.
Setting: Multicenter and single-site studies conducted in several countries.
Synopsis: Studies were included if they were randomized controlled trials, compared high- versus non-high-dose PPIs, evaluated endoscopically confirmed bleeding ulcers, gave PPIs after endoscopy, and documented outcomes regarding rates of rebleeding, surgical intervention, or mortality. High-dose PPIs were defined as equivalent to omeprazole 80 mg intravenous bolus followed by continuous intravenous infusion at 8 mg/hr for 72 hours.
Seven studies met inclusion criteria. The pooled odds ratios for rebleeding, surgical intervention, and mortality were 1.30 (95% CI, 0.88-1.91), 1.49 (95% CI, 0.66-3.37), and 0.89 (95% CI, 0.37-2.13), respectively, for high-dose versus non-high-dose PPIs. The authors concluded that high-dose PPIs were not superior to non-high-dose PPIs in reducing the rates of these adverse outcomes after endoscopic treatment of bleeding ulcers. Considering the cost of high-dose PPIs, further studies are indicated to help guide PPI dosing for patients with peptic ulcers.
Major limitations of this study were the small number of studies (1,157 patients in total) and their heterogeneity, and the lack of intention-to-treat analysis. The studies also included a high Asian predominance, and it has been shown that Asian populations have an enhanced PPI effect.
Bottom line: High-dose PPIs did not demonstrate reduced rates of ulcer rebleeding, surgical intervention, or mortality compared with non-high-dose PPIs in this meta-analysis, which included a small number of studies and patients.
Citation: Wang CH, Ma MH, Chou HC, et al. High-dose vs. non-high-dose proton pump inhibitors after endoscopic treatment in patients with bleeding peptic ulcer: a systematic review and meta-analysis of randomized controlled trials. Arch Intern Med. 2010;170(9):751-758.
Hospital Utilization by Practicing Generalists Declined before the Emergence of Hospitalists
Clinical question: What has been the pattern of hospital utilization by generalists before and after the emergence of hospitalists?
Background: It has been proposed that the emergence of hospitalists has “crowded out” generalist physicians from the U.S. hospital setting. This study evaluated the trends of inpatient practice by generalists both before and after the emergence of hospitalists.
Study design: Retrospective analysis of national databases.
Setting: U.S. data from 1980 to 2005.
Synopsis: Utilizing the National Hospital Discharge Survey and the American Medical Association’s Physician Characteristics and Distribution in the U.S., information was extracted to evaluate the average number of annual inpatient encounters relative to generalist workforce from 1980 to 2005. Total inpatient encounters for each year were calculated by multiplying the total number of hospital admissions by the average hospital length of stay. The emergence of hospitalists was defined as beginning in 1994.
Total inpatient encounters by generalists declined by 35% in the pre-hospitalist era but remained essentially unchanged in the hospitalist era. During the pre-hospitalist period, the number of generalists doubled, to more than 200,000 from approximately 100,000, while the number of hospital discharges remained relatively stable and the length of stay declined by a third. The decrease in average inpatient encounters in the pre-hospitalist era is thought to have been secondary to decreased length of stay and increased workforce.
Bottom line: Hospital utilization relative to generalist physician workforce was decreasing prior to the emergence of hospitalists mainly due to decreased length of hospital stay and increased numbers of physicians.
Citation: Meltzer DO, Chung JW. U.S. trends in hospitalization and generalist physician workforce and the emergence of hospitalists. J Gen Intern Med. 2010;25(5):453-459.
Fragmentation of Hospitalist Care Is Associated with Increased Length of Stay
Clinical question: Does fragmentation of care (FOC) by hospitalists affect length of stay (LOS)?
Background: Previous investigations have explored the impact of FOC provided by residency programs on LOS and quality of care. Results of these studies have been mixed. However, there have been no prior studies on the impact of the fragmentation of hospitalist care on LOS.
Study design: Concurrent control study.
Setting: Hospitalist practices all over the country managed by IPC: The Hospitalist Company.
Synopsis: Investigators looked at 10,977 patients admitted with diagnoses of pneumonia or heart failure. The primary endpoint was LOS. The independent variable of interest was a measure of FOC. The FOC was calculated as a quantitative index, by determining the percentage of hospitalist care delivered by a physician other than the primary hospitalist.
Multivariable analyses revealed a statistically significant increase in LOS of 0.39 days for each 10% increase in fragmentation level for pneumonia admissions. Similarly, for patients with heart failure, there was a significant increase in LOS of 0.30 days for each 10% increase in fragmentation level.
The study is a concurrent control study, so conclusions cannot be drawn about causality. Additionally, there are likely unmeasured differences between every hospital and hospitalist practice, which could further confound the relationships between hospitalist care and LOS.
Bottom line: Fragmentation of care provided by hospitalists is associated with an increased LOS in patients hospitalized for pneumonia or heart failure.
Citation: Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-338.
Admission Medication Errors Are Common and Most Harmful in Older Patients Taking Many Medications
Clinical question: What are the risk factors and potential harm associated with medication errors at hospital admission?
Background: Obtaining a medication history from a hospitalized patient is an error-prone process. Several variables can affect the completeness and quality of medication histories, but existing data are limited regarding patient or medication risk factors associated with medication errors at admission.
Study design: Prospective cohort study.
Setting: Academic hospital in Chicago.
Synopsis: Pharmacist and admitting physician medication histories were compared with admission medication orders to identify any unexplained discrepancies. Discrepancies resulting in order changes were defined as medication errors.
Of the 651 adult medical inpatients studied, 234 (35.9%) had medication order errors identified at admission. Errors originated in the medication histories for 85% of these patients. The most frequent type of error was an omission (48.9%). An age of 65 or older (odds ratio [OR]=2.17, 95% confidence interval [CI], 1.09-4.30) and increased number of medications (OR=1.21, 95% CI, 1.14-1.29) were the only risk factors identified by multivariate analysis to be independently associated with increased risk of medication order errors potentially causing harm or requiring monitoring or intervention. Presenting a medication list upon admission was a significant protective factor (OR=0.35, 95% CI, 0.19-0.63).
Though this is the largest study to date evaluating admission medication errors in hospitalized medical patients, it remains limited by its single hospital site. Because the authors were unable to interview patients who were too ill or unwilling to participate and had no caregiver present, they might have underestimated the number of admission errors. Further, the harm assessment was based on potential and not actual harm.
Bottom line: Admission medication order errors are frequent, most commonly originate in the medication histories, and have increased potential to cause adverse outcomes in older patients and those taking higher numbers of medications.
Citation: Gleason KM, McDaniel MR, Feinglass J, et al. Results of the Medications At Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25(5):441-447.
In This Edition
Literature at a Glance
A guide to this month’s studies
- Continuous insulin infusion in non-ICU patients
- How hospitalists spend their day
- Outcomes of patients leaving against medical advice
- Prediction rule for readmission
- Effects of high- vs. low-dose PPIs for peptic ulcer
- Hospital utilization by generalists before hospitalists
- Effect of hospitalist fragmentation on length of stay
- Medication errors at admissions in older patients
Continuous Insulin Infusion Provides Effective Glycemic Control in Non-ICU Patients
Clinical question: Is continuous insulin infusion (CII) a safe and effective option in the management of hyperglycemia in non-ICU patients?
Background: Hyperglycemia has been associated with worse outcomes in hospitalized patients. Prior research has demonstrated the benefit of CII in managing hyperglycemia in the ICU setting. However, outcomes have not been evaluated in the general medical (non-ICU) setting, where hyperglycemia is often inadequately addressed.
Study design: Retrospective chart review.
Setting: Urban tertiary-care medical center.
Synopsis: Charts of 200 adult patients treated with CII in non-ICU areas were reviewed with the primary outcomes including mean daily blood glucose (BG) levels and number of hyper- and hypoglycemic events occurring on CII. Mean BG dropped from 323 mg/dL to 182 mg/dL by day one, with a BG≤of 150 achieved in 67% of patients by day two of therapy. Twenty-two percent of patients suffered a hypoglycemic event (BG<60), reportedly similar to prior studies of insulin use in ICU and non-ICU settings. Eighty-two percent of patients received some form of nutritional support while on CII. In multivariate analyses, receiving oral nutrition (either a solid or liquid diet) was the only factor associated with increased risk of hyperglycemia and hypoglycemia.
This study was limited by its retrospective analysis in a single center. No comparison was made with basal-bolus or sliding-scale insulin therapy regarding efficacy or safety.
Bottom line: Non-ICU patients with hyperglycemia who received CII were able to achieve effective glycemic control within 48 hours of initiation, with rates of hypoglycemia comparable to those observed in ICU settings.
Citation: Smiley D, Rhee M, Peng L, et al. Safety and efficacy of continuous insulin infusion in noncritical care settings. J Hosp Med. 2010;5(4):212-217.
Hospitalists Spend More Time on Indirect, Rather Than Direct, Patient Care
Clinical question: What are the components of the daily workflow of hospitalists working on a non-housestaff service?
Background: The use of hospitalists is associated with increased efficiency in the hospital setting. However, it is not known how this efficiency is achieved. Prior literature has attempted to address this question, but with increasing demands and patient census, the representativeness of existing data is unclear.
Study design: Observational time-motion study.
Setting: Urban tertiary-care academic medical center.
Synopsis: Twenty-four hospitalists were directly observed for two weekday shifts. An electronic collection tool was developed using initial data on hospitalist activities and piloted prior to formal study data collection. Direct patient care was defined as involving face-to-face interaction between hospitalist and patient, while indirect patient care involved activities relevant to patient care but not performed in the patient’s presence.
Approximately 500 hours of observation were collected. Direct patient care comprised only a mean of 17.4% of the hospitalists’ daily workflow, while more was spent on indirect care, mainly electronic health record (EHR) documentation (mean 34.1%) and communication activities (mean 25.9%). Multitasking occurred 16% of the time, typically during communication or “critical documentation activities” (e.g. writing prescriptions). As patient volume increased, less time was spent in communication, and documentation was deferred to after hours.
These results were consistent with prior observational studies but were limited to a single center and might not represent the workflow of hospitalists in other settings, such as community hospitals, or nocturnists.
Bottom line: Hospitalists on non-housestaff services spend most of their time on indirect patient care and, with increasing patient census, communication is sacrificed. Multitasking is common during periods of communication and critical documentation.
Citation: Tipping MD, Forth VE, O’Leary KJ, et al. Where did the day go?—a time-motion study of hospitalists. J Hosp Med. 2010;5(6):323-328.
Patients Who Leave Against Medical Advice Have Higher Readmission, Mortality Rates
Clinical question: What are the 30-day hospital readmission and mortality rates for Veterans Administration (VA) patients discharged against medical advice (AMA) compared with those appropriately discharged from the hospital?
Background: Patients discharged AMA might be at increased risk of experiencing worse outcomes. Small studies have demonstrated that patients with asthma and acute myocardial infarction (MI) discharged AMA have increased risk of readmission and death. However, it is unclear whether these risks are generalizable to a wider medical population.
Study design: Five-year retrospective cohort study.
Setting: One hundred twenty-nine VA acute-care hospitals.
Synopsis: Of the nearly 2 million patients admitted to the VA from 2004 to 2008, 1.7% were discharged AMA. Patients discharged AMA generally were younger, had lower incomes, and were more likely to be black. Furthermore, patients discharged AMA had statistically significant higher rates of 30-day readmission (17.7% vs. 11%, P<0.001) and higher 30-day mortality rates (0.75% vs. 0.61%, P=0.001) compared with those who had been appropriately discharged. In hazard models, discharge AMA was a significant predictor of 30-day readmission and conferred a nonstatistically significant increase in 30-day mortality.
Because all patients were seen in VA facilities, the results might not be generalizable to other acute-care settings. Although VA patients differ from the general medical population, the characteristics of patients discharged AMA are similar to those in previously published studies. The study utilized administrative data, which are very reliable but limited by little information on clinical factors that could contribute to AMA discharges.
Bottom line: Patients discharged AMA are at increased risk of worse post-hospitalization outcomes, including hospital readmission and death.
Citation: Glasgow JM, Vaughn-Sarrazin M, Kaboli PJ. Leaving against medical advice (AMA): risk of 30-day mortality and hospital readmission. J Gen Intern Med. 2010;25(9): 926-929.
Simple Model Predicts Hospital Readmission
Clinical question: Which patient-level factors can be used in a simple model to predict hospital readmission of medicine patients?
Background: Hospital readmissions are common and costly. Previously published readmission prediction models have had limited utility because they focused on a specific condition, setting, or population, or were too cumbersome for practical use.
Study design: Prospective observational cohort study.
Setting: Six academic medical centers.
Synopsis: Data from nearly 11,000 general medicine patients were included in the analysis. Overall, almost 18% of patients were readmitted within 30 days of discharge.
In the prediction model derived and validated from the data, seven factors were significant predictors of readmission within 30 days of discharge: insurance status, marital status, having a regular healthcare provider, Charlson comorbidity index, SF 12 physical component score, one or more admissions within the last year, and current length of stay greater than two days. Points assigned from each significant predictor were used to create a risk score. The 5% of patients with risk scores of 25 and higher had 30-day readmission rates of approximately 30%, compared to readmission rates of approximately 16% in patients with scores of less than 25.
These results might not be generalizable to small, rural, nonacademic settings. Planned admissions could not be excluded from the data, and readmissions to nonstudy hospitals could not be ascertained. Despite these limitations, this model is easier to use than prior models and relevant to a broad population of patients.
Bottom line: A simple prediction model using patient-level factors can be used to identify patients at higher risk of readmission within 30 days of discharge to home.
Citation: Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25(3):211-219.
No Difference in Outcomes Between High- and Non-High-Dose Proton Pump Inhibitors in Bleeding Peptic Ulcers
Clinical question: Do high-dose proton pump inhibitors (PPIs) decrease the rate of rebleeding, surgical intervention, or mortality in patients with bleeding peptic ulcers who have undergone endoscopic treatment?
Background: Previous studies have demonstrated superiority of both high- and low-dose PPIs to H2 receptor antagonists and placebo in reducing rebleeding rates in patients with peptic ulcers. However, no clear evidence is available to suggest that high-dose PPIs are more effective than non-high-dose PPIs for treatment of bleeding peptic ulcers.
Study design: Systematic review and meta-analysis.
Setting: Multicenter and single-site studies conducted in several countries.
Synopsis: Studies were included if they were randomized controlled trials, compared high- versus non-high-dose PPIs, evaluated endoscopically confirmed bleeding ulcers, gave PPIs after endoscopy, and documented outcomes regarding rates of rebleeding, surgical intervention, or mortality. High-dose PPIs were defined as equivalent to omeprazole 80 mg intravenous bolus followed by continuous intravenous infusion at 8 mg/hr for 72 hours.
Seven studies met inclusion criteria. The pooled odds ratios for rebleeding, surgical intervention, and mortality were 1.30 (95% CI, 0.88-1.91), 1.49 (95% CI, 0.66-3.37), and 0.89 (95% CI, 0.37-2.13), respectively, for high-dose versus non-high-dose PPIs. The authors concluded that high-dose PPIs were not superior to non-high-dose PPIs in reducing the rates of these adverse outcomes after endoscopic treatment of bleeding ulcers. Considering the cost of high-dose PPIs, further studies are indicated to help guide PPI dosing for patients with peptic ulcers.
Major limitations of this study were the small number of studies (1,157 patients in total) and their heterogeneity, and the lack of intention-to-treat analysis. The studies also included a high Asian predominance, and it has been shown that Asian populations have an enhanced PPI effect.
Bottom line: High-dose PPIs did not demonstrate reduced rates of ulcer rebleeding, surgical intervention, or mortality compared with non-high-dose PPIs in this meta-analysis, which included a small number of studies and patients.
Citation: Wang CH, Ma MH, Chou HC, et al. High-dose vs. non-high-dose proton pump inhibitors after endoscopic treatment in patients with bleeding peptic ulcer: a systematic review and meta-analysis of randomized controlled trials. Arch Intern Med. 2010;170(9):751-758.
Hospital Utilization by Practicing Generalists Declined before the Emergence of Hospitalists
Clinical question: What has been the pattern of hospital utilization by generalists before and after the emergence of hospitalists?
Background: It has been proposed that the emergence of hospitalists has “crowded out” generalist physicians from the U.S. hospital setting. This study evaluated the trends of inpatient practice by generalists both before and after the emergence of hospitalists.
Study design: Retrospective analysis of national databases.
Setting: U.S. data from 1980 to 2005.
Synopsis: Utilizing the National Hospital Discharge Survey and the American Medical Association’s Physician Characteristics and Distribution in the U.S., information was extracted to evaluate the average number of annual inpatient encounters relative to generalist workforce from 1980 to 2005. Total inpatient encounters for each year were calculated by multiplying the total number of hospital admissions by the average hospital length of stay. The emergence of hospitalists was defined as beginning in 1994.
Total inpatient encounters by generalists declined by 35% in the pre-hospitalist era but remained essentially unchanged in the hospitalist era. During the pre-hospitalist period, the number of generalists doubled, to more than 200,000 from approximately 100,000, while the number of hospital discharges remained relatively stable and the length of stay declined by a third. The decrease in average inpatient encounters in the pre-hospitalist era is thought to have been secondary to decreased length of stay and increased workforce.
Bottom line: Hospital utilization relative to generalist physician workforce was decreasing prior to the emergence of hospitalists mainly due to decreased length of hospital stay and increased numbers of physicians.
Citation: Meltzer DO, Chung JW. U.S. trends in hospitalization and generalist physician workforce and the emergence of hospitalists. J Gen Intern Med. 2010;25(5):453-459.
Fragmentation of Hospitalist Care Is Associated with Increased Length of Stay
Clinical question: Does fragmentation of care (FOC) by hospitalists affect length of stay (LOS)?
Background: Previous investigations have explored the impact of FOC provided by residency programs on LOS and quality of care. Results of these studies have been mixed. However, there have been no prior studies on the impact of the fragmentation of hospitalist care on LOS.
Study design: Concurrent control study.
Setting: Hospitalist practices all over the country managed by IPC: The Hospitalist Company.
Synopsis: Investigators looked at 10,977 patients admitted with diagnoses of pneumonia or heart failure. The primary endpoint was LOS. The independent variable of interest was a measure of FOC. The FOC was calculated as a quantitative index, by determining the percentage of hospitalist care delivered by a physician other than the primary hospitalist.
Multivariable analyses revealed a statistically significant increase in LOS of 0.39 days for each 10% increase in fragmentation level for pneumonia admissions. Similarly, for patients with heart failure, there was a significant increase in LOS of 0.30 days for each 10% increase in fragmentation level.
The study is a concurrent control study, so conclusions cannot be drawn about causality. Additionally, there are likely unmeasured differences between every hospital and hospitalist practice, which could further confound the relationships between hospitalist care and LOS.
Bottom line: Fragmentation of care provided by hospitalists is associated with an increased LOS in patients hospitalized for pneumonia or heart failure.
Citation: Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-338.
Admission Medication Errors Are Common and Most Harmful in Older Patients Taking Many Medications
Clinical question: What are the risk factors and potential harm associated with medication errors at hospital admission?
Background: Obtaining a medication history from a hospitalized patient is an error-prone process. Several variables can affect the completeness and quality of medication histories, but existing data are limited regarding patient or medication risk factors associated with medication errors at admission.
Study design: Prospective cohort study.
Setting: Academic hospital in Chicago.
Synopsis: Pharmacist and admitting physician medication histories were compared with admission medication orders to identify any unexplained discrepancies. Discrepancies resulting in order changes were defined as medication errors.
Of the 651 adult medical inpatients studied, 234 (35.9%) had medication order errors identified at admission. Errors originated in the medication histories for 85% of these patients. The most frequent type of error was an omission (48.9%). An age of 65 or older (odds ratio [OR]=2.17, 95% confidence interval [CI], 1.09-4.30) and increased number of medications (OR=1.21, 95% CI, 1.14-1.29) were the only risk factors identified by multivariate analysis to be independently associated with increased risk of medication order errors potentially causing harm or requiring monitoring or intervention. Presenting a medication list upon admission was a significant protective factor (OR=0.35, 95% CI, 0.19-0.63).
Though this is the largest study to date evaluating admission medication errors in hospitalized medical patients, it remains limited by its single hospital site. Because the authors were unable to interview patients who were too ill or unwilling to participate and had no caregiver present, they might have underestimated the number of admission errors. Further, the harm assessment was based on potential and not actual harm.
Bottom line: Admission medication order errors are frequent, most commonly originate in the medication histories, and have increased potential to cause adverse outcomes in older patients and those taking higher numbers of medications.
Citation: Gleason KM, McDaniel MR, Feinglass J, et al. Results of the Medications At Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25(5):441-447.
In the Literature
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk of VTE with travel
- Hyponatremia and mortality
- Clopidogrel and aspirin for atrial fibrillation
- Cost-effective evaluation of syncope
- Early vs. delayed intervention in STEMI patients receiving fibrinolytics
- Predictors of prolonged SSU length of stay
- Rates of survival for in-hospital CPR
- Hospitalists and hospital quality measures
Travel Increases Risk for Venous Thromboembolism in a Dose-Response Relationship
Clinical question: What is the association between travel and the risk of venous thromboembolism (VTE)?
Background: Previous studies evaluating the relationship between long-distance travel and VTE have been heterogeneous and inconclusive. Though a relationship is often discussed, only about half of prior investigations have identified an elevated VTE risk in those who travel, and the impact of duration on VTE risk is unclear.
Study design: Meta-analysis.
Setting: Western countries.
Synopsis: Studies were included if they investigated the association between travel and VTE for persons using any mode of transportation and if nontraveling persons were included for comparison. Fourteen studies met the criteria, and included 4,055 patients with VTE. Compared with nontravelers, the overall pooled relative risk for VTE in travelers was 2.0 (95% CI, 1.5-2.7).
Significant heterogeneity was present among these 14 studies, specifically with regard to the method used for selecting control participants. Six case-control studies used control patients who had been referred for VTE evaluation. When these studies were excluded, the pooled relative risk for VTE in travelers was 2.8 (95% CI, 2.2-3.7).
A dose-response relationship was identified. There was an 18% higher risk for VTE for each two-hour increase in duration of travel among all modes of transportation (P=0.010). When studies evaluating only air travel were analyzed, a 26% higher risk was found for every two-hour increase in air travel (P=0.005).
Bottom line: Travel is associated with a three-fold increase in the risk for VTE, and for each two-hour increase in travel duration, the risk increases approximately 18%.
Citation: Chandra D, Parisini E, Mozaffarian D. Meta-analysis: travel and risk for venous thromboembolism. Ann Intern Med. 2009;151(3):180-190.
Hyponatremia in Hospitalized Patients is Associated with Increased Mortality
Clinical question: Is hyponatremia in hospitalized patients associated with increased mortality?
Background: Hyponatremia is the most common electrolyte abnormality in hospitalized patients. Patients admitted with hyponatremia have increased in-hospital mortality. Long-term mortality in hospitalized patients with hyponatremia is not known. Further, the effects of the degree of hyponatremia on mortality are not known.
Study design: Prospective cohort.
Setting: Two teaching hospitals in Boston.
Synopsis: The study identified 14,290 patients with hyponatremia (serum sodium <135 mEq/L) at admission (14.5%) and an additional 5,093 patients (19,383 total patients, or 19.7% of the 98,411 study patients) with hyponatremia at some point during their hospital stay. After multivariable adjustments and correction for hyperglycemia, patients with hyponatremia had increased mortality in the hospital (OR 1.47, 95% CI, 1.33-1.62), at one year (HR 1.38, 95% CI, 1.32-1.46), and at five years (HR 1.25, 95% CI, 1.21-1.30) compared with normonatremic patients. These mortality differences were seen in patients with mild, moderate, and moderately severe hyponatremia (serum sodium concentrations 130-134, 125-129, and 120-124 mEq/L, respectively), but not in patients with severe hyponatremia (serum sodium <120 mEq/L).
This study is limited by its post-hoc identification and classification of patients using ICD-9-CM codes, which could have resulted in some misclassification. Also, this study includes only two teaching hospitals in an urban setting; the prevalence of hyponatremia might differ in other settings. Causality cannot be determined based on these results.
Bottom line: Hospitalized patients with hyponatremia have increased in-hospital and long-term mortality.
Citation: Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med. 2009;122(9):857-865.
Clopidogrel Plus Aspirin in Patients with Atrial Fibrillation Reduces Risk of Major Vascular Events
Clinical question: Does the addition of clopidogrel to aspirin therapy reduce the risk of major vascular events in patients with atrial fibrillation for whom vitamin K antagonists (VKAs) are unsuitable?
Background: Although VKAs reduce the risk of stroke in atrial fibrillation, many patients are unable to use VKAs and are treated with aspirin instead. The potential benefits of adding clopidogrel to aspirin therapy in this population are unknown.
Study design: Randomized controlled trial.
Setting: Five hundred eighty medical centers in 33 countries.
Synopsis: More than 7,500 patients with atrial fibrillation who were also at high risk for stroke were randomly assigned to receive either clopidogrel or placebo once daily. All patients also received aspirin at a dose of 75 mg to 100 mg daily. A major vascular event occurred in 6.8% of patients per year who received clopidogrel and in 7.6% of patients per year who received placebo (RR 0.89, 95% CI, 0.89-0.98, P=0.01). This reduction primarily was due to a reduction in stroke, which occurred in 2.4% of patients per year who received clopidogrel, compared with 3.3% of patients per year who received placebo (RR 0.72, 95% CI, 0.62-0.83, P<0.001).
Major bleeding occurred in 2% of patients per year who received clopidogrel and in 1.3% of patients per year who received placebo (RR 1.57, 95% CI, 1.29-1.92, P<0.001).
Bottom line: Adding clopidogrel to aspirin in patients with atrial fibrillation who are not eligible for VKAs decreases the risk of major vascular events, including stroke, but increases risk of major hemorrhage compared with aspirin alone.
Citation: ACTIVE Investigators, Connolly SJ, Pogue J, et al. Effect of clopidogrel added to aspirin in patients with atrial fibrillation. N Engl J Med. 2009;360(20):2066-2078.
Prioritize Syncope Testing by Diagnostic Yield and Cost Effectiveness
Clinical question: What are the utilization, yield, and cost effectiveness of tests used for evaluation of syncope in older patients?
Background: Clinicians utilize multiple diagnostic tests to help delineate the cause of syncope, but the yield and cost effectiveness of many of these tests are unclear. Further, it is unknown if considering patient characteristics, as in the San Francisco syncope rule (SFSR), can improve the yield of diagnostic tests.
Study design: Retrospective cohort.
Setting: Single acute-care hospital.
Synopsis: Review of 2,106 admissions in patients 65 and older with syncope revealed that the most common tests were electrocardiogram (99%), telemetry (95%), cardiac enzymes (95%), and head computed tomography (CT) scan (63%). The majority of tests did not affect diagnosis or management.
Postural blood pressure (BP) reading was infrequently recorded (38%) but had the highest yield. BP influenced diagnosis at least 18% of the time and management at least 25% of the time. Tests with the lowest likelihood of affecting diagnosis and management were head CT, carotid ultrasound, electroencephalography (EEG), and cardiac enzymes.
EEG had the highest cost per test affecting the diagnosis or management ($32,973), followed by head CT. The cost per test affecting diagnosis or management for postural BP was $17. Cardiac testing, including telemetry, echocardiogram, and cardiac enzymes, had significantly better yield in patients who met SFSR criteria.
Bottom line: In patients with syncope, the history and exam should guide evaluation, and tests with high yield and low cost per test, such as postural BP, should be prioritized.
Citation: Mendu ML, McAvay G, Lampert R, Stoehr J, Tinetti ME. Yield of diagnostic tests in evaluating syncopal episodes in older patients. Arch Intern Med. 2009;169(14): 1299-1305.
Early PCI is Superior to Delayed Intervention in Patients with STEMI Receiving Fibrinolytic Therapy
Clinical question: Does early percutaneous coronary intervention (PCI) improve clinical outcomes compared with standard management in patients with ST elevation myocardial infarction (STEMI) who receive fibrinolysis?
Background: Prior research has demonstrated the benefit of timely PCI in the management of acute coronary syndrome, specifically with ST elevation. However, many hospitals do not have this capability and utilize fibrinolysis as a standard alternative. The optimal timing of subsequent invasive intervention following fibrinolysis has not been established.
Study design: Multicenter randomized trial.
Setting: Fifty-two sites in three provinces in Canada.
Synopsis: This study randomized 1,059 patients presenting with STEMI and receiving fibrinolysis to early intervention (immediate transfer to another hospital with PCI less than six hours after fibrinolysis) versus standard intervention (rescue PCI if needed, or delayed angiography at more than 24 hours). The primary outcome was the composite of death, reinfarction, recurrent ischemia, new or worsening congestive heart failure, or cardiogenic shock within 30 days.
The primary outcome occurred in 11% of patients in the early intervention group, compared with 17.2% of patients randomized to standard intervention (RR 0.64, 95% CI, 0.47-0.87, P=0.004). Urgent catheterization was performed within 12 hours of fibrinolysis in 34.9% of patients randomized to the standard treatment group.
This study was not powered to detect differences in mortality and other individual components of the primary endpoint.
Bottom line: STEMI patients who received fibrinolysis had a lower risk of adverse outcomes when receiving transfer and PCI within six hours, compared with standard delayed intervention.
Citation: Cantor WJ, Fitchett D, Borgundvaag B, et al. Routine early angioplasty after fibrinolysis for acute myocardial infarction. N Engl J Med. 2009;360(26):2705-2718.
Specialty Consultation and Limited Access Tests Predict Unsuccessful SSU Admissions
Clinical question: In patients admitted to short-stay units (SSUs), what characteristics are associated with unsuccessful SSU admission?
Background: Short-stay units have become prevalent in U.S. hospitals, but it is unclear which patient populations are best served by SSUs.
Study design: Prospective cohort.
Setting: Fourteen-bed SSU in a 500-bed public teaching hospital in Chicago.
Synopsis: More than 700 patients admitted to the Cook County Hospital SSU over a four-month period were interviewed and examined, and their ED and inpatient records were reviewed. An SSU admission was defined as “successful” if the length of stay (LOS) was less than 72 hours and the patient was discharged directly from the SSU.
Overall, 79% of patients had a successful SSU admission. In multivariate analysis, the strongest predictors of an unsuccessful SSU stay were subspecialty consultation (OR 8.1, P<0.001), a provisional diagnosis of heart failure (OR 1.9, P=0.02), and limited availability of a diagnostic test (OR 2.5, P<0.001).
The study was limited primarily to patients with cardiovascular diagnoses.
Bottom line: Patients admitted to SSUs who receive specialty consultation, carry a diagnosis of heart failure, or require diagnostic testing that is not readily available might have a longer LOS or eventual inpatient admission.
Citation: Lucas BP, Kumapley R, Mba B, et al. A hospitalist-run short-stay unit: features that predict length-of-stay and eventual admission to traditional inpatient services. J Hosp Med. 2009;4(5):276-284.
Lack of Significant Gains in Survival Rates Following In-Hospital CPR
Clinical question: Is survival after in-hospital CPR improving over time, and what are the factors associated with survival?
Background: Advances in out-of-hospital CPR have improved outcomes. However, it is unknown whether the survival rate after in-hospital CPR is improving over time, and it is unclear which patient and/or hospital characteristics predict post-CPR survival.
Study design: Retrospective cohort.
Setting: Inpatient Medicare beneficiaries from 1992 to 2005.
Synopsis: The study examined more than 150 million Medicare admissions, 433,985 of which underwent in-hospital CPR. Survival to discharge occurred in 18.3% of CPR events and did not change significantly from 1992 to 2005. The cumulative incidence of in-hospital CPR events was 2.73 per 1,000 admissions; it did not change substantially over time.
The survival rate was lower among black patients (OR 0.76, 95% CI, 0.74-0.79), which is partially explained due to the fact they tended to receive CPR at hospitals with lower post-CPR survival. Gender (specifically male), older age, race (specifically other nonwhite patients), higher burden of chronic illness, and admission from a skilled nursing facility were significantly associated with decreased survival to hospital discharge following CPR.
Limitations of this study included the identification of CPR by ICD-9 codes, which have not been validated for this purpose and could vary among hospitals. Other factors that might explain variations in survival were not available, including severity of acute illness and the presence (or absence) of a shockable rhythm at initial presentation.
Bottom line: Rates of survival to hospital discharge among Medicare beneficiaries receiving in-hospital CPR have remained constant over time, with poorer survival rates among blacks and other nonwhite patients.
Citation: Ehlenbach WJ, Barnato AE, Curtis JR, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009;361(1):22-31.
Hospitalists Are Associated with Improved Performance on Quality Metrics
Clinical question: Is the presence of hospitalist physicians associated with improved performance on standard quality measures for acute myocardial infarction (AMI), congestive heart failure (CHF), and pneumonia?
Background: Previous investigations have demonstrated significant improvements in cost and LOS for patients under the care of hospitalists compared with other inpatient providers. The association between hospitalist prevalence and quality of care, as measured by standard quality process measures, is unknown.
Study design: Cross-sectional.
Setting: More than 3,600 hospitals participating in the Health Quality Alliance (HQA) program.
Synopsis: Investigators looked at a large sample of HQA hospitals in the American Hospital Association survey, and identified facilities with hospitalist services and those without. The primary endpoint was the adherence to composites of standard quality process measures across three disease categories (AMI, CHF, and pneumonia) and two domains of care (disease treatment/diagnosis and counseling/prevention).
Multivariable analyses revealed a statistically significant association between the presence of hospitalists and adherence to composite quality measures for AMI and pneumonia. This association was demonstrated for both treatment and counseling domains.
The study is cross-sectional, so conclusions cannot be drawn about causality. Also, there are likely unmeasured differences between hospitals that utilize hospitalists compared with those that do not, which could further confound the relationship between the presence of hospitalists and adherence to quality measures.
Finally, this study only evaluated hospital-level performance, and it cannot offer insight on the quality of individual patient care by hospitalist providers.
Bottom line: The presence of hospitalists is associated with improvement in adherence to quality measures for both AMI and pneumonia, and across clinical domains of treatment and counseling.
Citation: López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk of VTE with travel
- Hyponatremia and mortality
- Clopidogrel and aspirin for atrial fibrillation
- Cost-effective evaluation of syncope
- Early vs. delayed intervention in STEMI patients receiving fibrinolytics
- Predictors of prolonged SSU length of stay
- Rates of survival for in-hospital CPR
- Hospitalists and hospital quality measures
Travel Increases Risk for Venous Thromboembolism in a Dose-Response Relationship
Clinical question: What is the association between travel and the risk of venous thromboembolism (VTE)?
Background: Previous studies evaluating the relationship between long-distance travel and VTE have been heterogeneous and inconclusive. Though a relationship is often discussed, only about half of prior investigations have identified an elevated VTE risk in those who travel, and the impact of duration on VTE risk is unclear.
Study design: Meta-analysis.
Setting: Western countries.
Synopsis: Studies were included if they investigated the association between travel and VTE for persons using any mode of transportation and if nontraveling persons were included for comparison. Fourteen studies met the criteria, and included 4,055 patients with VTE. Compared with nontravelers, the overall pooled relative risk for VTE in travelers was 2.0 (95% CI, 1.5-2.7).
Significant heterogeneity was present among these 14 studies, specifically with regard to the method used for selecting control participants. Six case-control studies used control patients who had been referred for VTE evaluation. When these studies were excluded, the pooled relative risk for VTE in travelers was 2.8 (95% CI, 2.2-3.7).
A dose-response relationship was identified. There was an 18% higher risk for VTE for each two-hour increase in duration of travel among all modes of transportation (P=0.010). When studies evaluating only air travel were analyzed, a 26% higher risk was found for every two-hour increase in air travel (P=0.005).
Bottom line: Travel is associated with a three-fold increase in the risk for VTE, and for each two-hour increase in travel duration, the risk increases approximately 18%.
Citation: Chandra D, Parisini E, Mozaffarian D. Meta-analysis: travel and risk for venous thromboembolism. Ann Intern Med. 2009;151(3):180-190.
Hyponatremia in Hospitalized Patients is Associated with Increased Mortality
Clinical question: Is hyponatremia in hospitalized patients associated with increased mortality?
Background: Hyponatremia is the most common electrolyte abnormality in hospitalized patients. Patients admitted with hyponatremia have increased in-hospital mortality. Long-term mortality in hospitalized patients with hyponatremia is not known. Further, the effects of the degree of hyponatremia on mortality are not known.
Study design: Prospective cohort.
Setting: Two teaching hospitals in Boston.
Synopsis: The study identified 14,290 patients with hyponatremia (serum sodium <135 mEq/L) at admission (14.5%) and an additional 5,093 patients (19,383 total patients, or 19.7% of the 98,411 study patients) with hyponatremia at some point during their hospital stay. After multivariable adjustments and correction for hyperglycemia, patients with hyponatremia had increased mortality in the hospital (OR 1.47, 95% CI, 1.33-1.62), at one year (HR 1.38, 95% CI, 1.32-1.46), and at five years (HR 1.25, 95% CI, 1.21-1.30) compared with normonatremic patients. These mortality differences were seen in patients with mild, moderate, and moderately severe hyponatremia (serum sodium concentrations 130-134, 125-129, and 120-124 mEq/L, respectively), but not in patients with severe hyponatremia (serum sodium <120 mEq/L).
This study is limited by its post-hoc identification and classification of patients using ICD-9-CM codes, which could have resulted in some misclassification. Also, this study includes only two teaching hospitals in an urban setting; the prevalence of hyponatremia might differ in other settings. Causality cannot be determined based on these results.
Bottom line: Hospitalized patients with hyponatremia have increased in-hospital and long-term mortality.
Citation: Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med. 2009;122(9):857-865.
Clopidogrel Plus Aspirin in Patients with Atrial Fibrillation Reduces Risk of Major Vascular Events
Clinical question: Does the addition of clopidogrel to aspirin therapy reduce the risk of major vascular events in patients with atrial fibrillation for whom vitamin K antagonists (VKAs) are unsuitable?
Background: Although VKAs reduce the risk of stroke in atrial fibrillation, many patients are unable to use VKAs and are treated with aspirin instead. The potential benefits of adding clopidogrel to aspirin therapy in this population are unknown.
Study design: Randomized controlled trial.
Setting: Five hundred eighty medical centers in 33 countries.
Synopsis: More than 7,500 patients with atrial fibrillation who were also at high risk for stroke were randomly assigned to receive either clopidogrel or placebo once daily. All patients also received aspirin at a dose of 75 mg to 100 mg daily. A major vascular event occurred in 6.8% of patients per year who received clopidogrel and in 7.6% of patients per year who received placebo (RR 0.89, 95% CI, 0.89-0.98, P=0.01). This reduction primarily was due to a reduction in stroke, which occurred in 2.4% of patients per year who received clopidogrel, compared with 3.3% of patients per year who received placebo (RR 0.72, 95% CI, 0.62-0.83, P<0.001).
Major bleeding occurred in 2% of patients per year who received clopidogrel and in 1.3% of patients per year who received placebo (RR 1.57, 95% CI, 1.29-1.92, P<0.001).
Bottom line: Adding clopidogrel to aspirin in patients with atrial fibrillation who are not eligible for VKAs decreases the risk of major vascular events, including stroke, but increases risk of major hemorrhage compared with aspirin alone.
Citation: ACTIVE Investigators, Connolly SJ, Pogue J, et al. Effect of clopidogrel added to aspirin in patients with atrial fibrillation. N Engl J Med. 2009;360(20):2066-2078.
Prioritize Syncope Testing by Diagnostic Yield and Cost Effectiveness
Clinical question: What are the utilization, yield, and cost effectiveness of tests used for evaluation of syncope in older patients?
Background: Clinicians utilize multiple diagnostic tests to help delineate the cause of syncope, but the yield and cost effectiveness of many of these tests are unclear. Further, it is unknown if considering patient characteristics, as in the San Francisco syncope rule (SFSR), can improve the yield of diagnostic tests.
Study design: Retrospective cohort.
Setting: Single acute-care hospital.
Synopsis: Review of 2,106 admissions in patients 65 and older with syncope revealed that the most common tests were electrocardiogram (99%), telemetry (95%), cardiac enzymes (95%), and head computed tomography (CT) scan (63%). The majority of tests did not affect diagnosis or management.
Postural blood pressure (BP) reading was infrequently recorded (38%) but had the highest yield. BP influenced diagnosis at least 18% of the time and management at least 25% of the time. Tests with the lowest likelihood of affecting diagnosis and management were head CT, carotid ultrasound, electroencephalography (EEG), and cardiac enzymes.
EEG had the highest cost per test affecting the diagnosis or management ($32,973), followed by head CT. The cost per test affecting diagnosis or management for postural BP was $17. Cardiac testing, including telemetry, echocardiogram, and cardiac enzymes, had significantly better yield in patients who met SFSR criteria.
Bottom line: In patients with syncope, the history and exam should guide evaluation, and tests with high yield and low cost per test, such as postural BP, should be prioritized.
Citation: Mendu ML, McAvay G, Lampert R, Stoehr J, Tinetti ME. Yield of diagnostic tests in evaluating syncopal episodes in older patients. Arch Intern Med. 2009;169(14): 1299-1305.
Early PCI is Superior to Delayed Intervention in Patients with STEMI Receiving Fibrinolytic Therapy
Clinical question: Does early percutaneous coronary intervention (PCI) improve clinical outcomes compared with standard management in patients with ST elevation myocardial infarction (STEMI) who receive fibrinolysis?
Background: Prior research has demonstrated the benefit of timely PCI in the management of acute coronary syndrome, specifically with ST elevation. However, many hospitals do not have this capability and utilize fibrinolysis as a standard alternative. The optimal timing of subsequent invasive intervention following fibrinolysis has not been established.
Study design: Multicenter randomized trial.
Setting: Fifty-two sites in three provinces in Canada.
Synopsis: This study randomized 1,059 patients presenting with STEMI and receiving fibrinolysis to early intervention (immediate transfer to another hospital with PCI less than six hours after fibrinolysis) versus standard intervention (rescue PCI if needed, or delayed angiography at more than 24 hours). The primary outcome was the composite of death, reinfarction, recurrent ischemia, new or worsening congestive heart failure, or cardiogenic shock within 30 days.
The primary outcome occurred in 11% of patients in the early intervention group, compared with 17.2% of patients randomized to standard intervention (RR 0.64, 95% CI, 0.47-0.87, P=0.004). Urgent catheterization was performed within 12 hours of fibrinolysis in 34.9% of patients randomized to the standard treatment group.
This study was not powered to detect differences in mortality and other individual components of the primary endpoint.
Bottom line: STEMI patients who received fibrinolysis had a lower risk of adverse outcomes when receiving transfer and PCI within six hours, compared with standard delayed intervention.
Citation: Cantor WJ, Fitchett D, Borgundvaag B, et al. Routine early angioplasty after fibrinolysis for acute myocardial infarction. N Engl J Med. 2009;360(26):2705-2718.
Specialty Consultation and Limited Access Tests Predict Unsuccessful SSU Admissions
Clinical question: In patients admitted to short-stay units (SSUs), what characteristics are associated with unsuccessful SSU admission?
Background: Short-stay units have become prevalent in U.S. hospitals, but it is unclear which patient populations are best served by SSUs.
Study design: Prospective cohort.
Setting: Fourteen-bed SSU in a 500-bed public teaching hospital in Chicago.
Synopsis: More than 700 patients admitted to the Cook County Hospital SSU over a four-month period were interviewed and examined, and their ED and inpatient records were reviewed. An SSU admission was defined as “successful” if the length of stay (LOS) was less than 72 hours and the patient was discharged directly from the SSU.
Overall, 79% of patients had a successful SSU admission. In multivariate analysis, the strongest predictors of an unsuccessful SSU stay were subspecialty consultation (OR 8.1, P<0.001), a provisional diagnosis of heart failure (OR 1.9, P=0.02), and limited availability of a diagnostic test (OR 2.5, P<0.001).
The study was limited primarily to patients with cardiovascular diagnoses.
Bottom line: Patients admitted to SSUs who receive specialty consultation, carry a diagnosis of heart failure, or require diagnostic testing that is not readily available might have a longer LOS or eventual inpatient admission.
Citation: Lucas BP, Kumapley R, Mba B, et al. A hospitalist-run short-stay unit: features that predict length-of-stay and eventual admission to traditional inpatient services. J Hosp Med. 2009;4(5):276-284.
Lack of Significant Gains in Survival Rates Following In-Hospital CPR
Clinical question: Is survival after in-hospital CPR improving over time, and what are the factors associated with survival?
Background: Advances in out-of-hospital CPR have improved outcomes. However, it is unknown whether the survival rate after in-hospital CPR is improving over time, and it is unclear which patient and/or hospital characteristics predict post-CPR survival.
Study design: Retrospective cohort.
Setting: Inpatient Medicare beneficiaries from 1992 to 2005.
Synopsis: The study examined more than 150 million Medicare admissions, 433,985 of which underwent in-hospital CPR. Survival to discharge occurred in 18.3% of CPR events and did not change significantly from 1992 to 2005. The cumulative incidence of in-hospital CPR events was 2.73 per 1,000 admissions; it did not change substantially over time.
The survival rate was lower among black patients (OR 0.76, 95% CI, 0.74-0.79), which is partially explained due to the fact they tended to receive CPR at hospitals with lower post-CPR survival. Gender (specifically male), older age, race (specifically other nonwhite patients), higher burden of chronic illness, and admission from a skilled nursing facility were significantly associated with decreased survival to hospital discharge following CPR.
Limitations of this study included the identification of CPR by ICD-9 codes, which have not been validated for this purpose and could vary among hospitals. Other factors that might explain variations in survival were not available, including severity of acute illness and the presence (or absence) of a shockable rhythm at initial presentation.
Bottom line: Rates of survival to hospital discharge among Medicare beneficiaries receiving in-hospital CPR have remained constant over time, with poorer survival rates among blacks and other nonwhite patients.
Citation: Ehlenbach WJ, Barnato AE, Curtis JR, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009;361(1):22-31.
Hospitalists Are Associated with Improved Performance on Quality Metrics
Clinical question: Is the presence of hospitalist physicians associated with improved performance on standard quality measures for acute myocardial infarction (AMI), congestive heart failure (CHF), and pneumonia?
Background: Previous investigations have demonstrated significant improvements in cost and LOS for patients under the care of hospitalists compared with other inpatient providers. The association between hospitalist prevalence and quality of care, as measured by standard quality process measures, is unknown.
Study design: Cross-sectional.
Setting: More than 3,600 hospitals participating in the Health Quality Alliance (HQA) program.
Synopsis: Investigators looked at a large sample of HQA hospitals in the American Hospital Association survey, and identified facilities with hospitalist services and those without. The primary endpoint was the adherence to composites of standard quality process measures across three disease categories (AMI, CHF, and pneumonia) and two domains of care (disease treatment/diagnosis and counseling/prevention).
Multivariable analyses revealed a statistically significant association between the presence of hospitalists and adherence to composite quality measures for AMI and pneumonia. This association was demonstrated for both treatment and counseling domains.
The study is cross-sectional, so conclusions cannot be drawn about causality. Also, there are likely unmeasured differences between hospitals that utilize hospitalists compared with those that do not, which could further confound the relationship between the presence of hospitalists and adherence to quality measures.
Finally, this study only evaluated hospital-level performance, and it cannot offer insight on the quality of individual patient care by hospitalist providers.
Bottom line: The presence of hospitalists is associated with improvement in adherence to quality measures for both AMI and pneumonia, and across clinical domains of treatment and counseling.
Citation: López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk of VTE with travel
- Hyponatremia and mortality
- Clopidogrel and aspirin for atrial fibrillation
- Cost-effective evaluation of syncope
- Early vs. delayed intervention in STEMI patients receiving fibrinolytics
- Predictors of prolonged SSU length of stay
- Rates of survival for in-hospital CPR
- Hospitalists and hospital quality measures
Travel Increases Risk for Venous Thromboembolism in a Dose-Response Relationship
Clinical question: What is the association between travel and the risk of venous thromboembolism (VTE)?
Background: Previous studies evaluating the relationship between long-distance travel and VTE have been heterogeneous and inconclusive. Though a relationship is often discussed, only about half of prior investigations have identified an elevated VTE risk in those who travel, and the impact of duration on VTE risk is unclear.
Study design: Meta-analysis.
Setting: Western countries.
Synopsis: Studies were included if they investigated the association between travel and VTE for persons using any mode of transportation and if nontraveling persons were included for comparison. Fourteen studies met the criteria, and included 4,055 patients with VTE. Compared with nontravelers, the overall pooled relative risk for VTE in travelers was 2.0 (95% CI, 1.5-2.7).
Significant heterogeneity was present among these 14 studies, specifically with regard to the method used for selecting control participants. Six case-control studies used control patients who had been referred for VTE evaluation. When these studies were excluded, the pooled relative risk for VTE in travelers was 2.8 (95% CI, 2.2-3.7).
A dose-response relationship was identified. There was an 18% higher risk for VTE for each two-hour increase in duration of travel among all modes of transportation (P=0.010). When studies evaluating only air travel were analyzed, a 26% higher risk was found for every two-hour increase in air travel (P=0.005).
Bottom line: Travel is associated with a three-fold increase in the risk for VTE, and for each two-hour increase in travel duration, the risk increases approximately 18%.
Citation: Chandra D, Parisini E, Mozaffarian D. Meta-analysis: travel and risk for venous thromboembolism. Ann Intern Med. 2009;151(3):180-190.
Hyponatremia in Hospitalized Patients is Associated with Increased Mortality
Clinical question: Is hyponatremia in hospitalized patients associated with increased mortality?
Background: Hyponatremia is the most common electrolyte abnormality in hospitalized patients. Patients admitted with hyponatremia have increased in-hospital mortality. Long-term mortality in hospitalized patients with hyponatremia is not known. Further, the effects of the degree of hyponatremia on mortality are not known.
Study design: Prospective cohort.
Setting: Two teaching hospitals in Boston.
Synopsis: The study identified 14,290 patients with hyponatremia (serum sodium <135 mEq/L) at admission (14.5%) and an additional 5,093 patients (19,383 total patients, or 19.7% of the 98,411 study patients) with hyponatremia at some point during their hospital stay. After multivariable adjustments and correction for hyperglycemia, patients with hyponatremia had increased mortality in the hospital (OR 1.47, 95% CI, 1.33-1.62), at one year (HR 1.38, 95% CI, 1.32-1.46), and at five years (HR 1.25, 95% CI, 1.21-1.30) compared with normonatremic patients. These mortality differences were seen in patients with mild, moderate, and moderately severe hyponatremia (serum sodium concentrations 130-134, 125-129, and 120-124 mEq/L, respectively), but not in patients with severe hyponatremia (serum sodium <120 mEq/L).
This study is limited by its post-hoc identification and classification of patients using ICD-9-CM codes, which could have resulted in some misclassification. Also, this study includes only two teaching hospitals in an urban setting; the prevalence of hyponatremia might differ in other settings. Causality cannot be determined based on these results.
Bottom line: Hospitalized patients with hyponatremia have increased in-hospital and long-term mortality.
Citation: Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med. 2009;122(9):857-865.
Clopidogrel Plus Aspirin in Patients with Atrial Fibrillation Reduces Risk of Major Vascular Events
Clinical question: Does the addition of clopidogrel to aspirin therapy reduce the risk of major vascular events in patients with atrial fibrillation for whom vitamin K antagonists (VKAs) are unsuitable?
Background: Although VKAs reduce the risk of stroke in atrial fibrillation, many patients are unable to use VKAs and are treated with aspirin instead. The potential benefits of adding clopidogrel to aspirin therapy in this population are unknown.
Study design: Randomized controlled trial.
Setting: Five hundred eighty medical centers in 33 countries.
Synopsis: More than 7,500 patients with atrial fibrillation who were also at high risk for stroke were randomly assigned to receive either clopidogrel or placebo once daily. All patients also received aspirin at a dose of 75 mg to 100 mg daily. A major vascular event occurred in 6.8% of patients per year who received clopidogrel and in 7.6% of patients per year who received placebo (RR 0.89, 95% CI, 0.89-0.98, P=0.01). This reduction primarily was due to a reduction in stroke, which occurred in 2.4% of patients per year who received clopidogrel, compared with 3.3% of patients per year who received placebo (RR 0.72, 95% CI, 0.62-0.83, P<0.001).
Major bleeding occurred in 2% of patients per year who received clopidogrel and in 1.3% of patients per year who received placebo (RR 1.57, 95% CI, 1.29-1.92, P<0.001).
Bottom line: Adding clopidogrel to aspirin in patients with atrial fibrillation who are not eligible for VKAs decreases the risk of major vascular events, including stroke, but increases risk of major hemorrhage compared with aspirin alone.
Citation: ACTIVE Investigators, Connolly SJ, Pogue J, et al. Effect of clopidogrel added to aspirin in patients with atrial fibrillation. N Engl J Med. 2009;360(20):2066-2078.
Prioritize Syncope Testing by Diagnostic Yield and Cost Effectiveness
Clinical question: What are the utilization, yield, and cost effectiveness of tests used for evaluation of syncope in older patients?
Background: Clinicians utilize multiple diagnostic tests to help delineate the cause of syncope, but the yield and cost effectiveness of many of these tests are unclear. Further, it is unknown if considering patient characteristics, as in the San Francisco syncope rule (SFSR), can improve the yield of diagnostic tests.
Study design: Retrospective cohort.
Setting: Single acute-care hospital.
Synopsis: Review of 2,106 admissions in patients 65 and older with syncope revealed that the most common tests were electrocardiogram (99%), telemetry (95%), cardiac enzymes (95%), and head computed tomography (CT) scan (63%). The majority of tests did not affect diagnosis or management.
Postural blood pressure (BP) reading was infrequently recorded (38%) but had the highest yield. BP influenced diagnosis at least 18% of the time and management at least 25% of the time. Tests with the lowest likelihood of affecting diagnosis and management were head CT, carotid ultrasound, electroencephalography (EEG), and cardiac enzymes.
EEG had the highest cost per test affecting the diagnosis or management ($32,973), followed by head CT. The cost per test affecting diagnosis or management for postural BP was $17. Cardiac testing, including telemetry, echocardiogram, and cardiac enzymes, had significantly better yield in patients who met SFSR criteria.
Bottom line: In patients with syncope, the history and exam should guide evaluation, and tests with high yield and low cost per test, such as postural BP, should be prioritized.
Citation: Mendu ML, McAvay G, Lampert R, Stoehr J, Tinetti ME. Yield of diagnostic tests in evaluating syncopal episodes in older patients. Arch Intern Med. 2009;169(14): 1299-1305.
Early PCI is Superior to Delayed Intervention in Patients with STEMI Receiving Fibrinolytic Therapy
Clinical question: Does early percutaneous coronary intervention (PCI) improve clinical outcomes compared with standard management in patients with ST elevation myocardial infarction (STEMI) who receive fibrinolysis?
Background: Prior research has demonstrated the benefit of timely PCI in the management of acute coronary syndrome, specifically with ST elevation. However, many hospitals do not have this capability and utilize fibrinolysis as a standard alternative. The optimal timing of subsequent invasive intervention following fibrinolysis has not been established.
Study design: Multicenter randomized trial.
Setting: Fifty-two sites in three provinces in Canada.
Synopsis: This study randomized 1,059 patients presenting with STEMI and receiving fibrinolysis to early intervention (immediate transfer to another hospital with PCI less than six hours after fibrinolysis) versus standard intervention (rescue PCI if needed, or delayed angiography at more than 24 hours). The primary outcome was the composite of death, reinfarction, recurrent ischemia, new or worsening congestive heart failure, or cardiogenic shock within 30 days.
The primary outcome occurred in 11% of patients in the early intervention group, compared with 17.2% of patients randomized to standard intervention (RR 0.64, 95% CI, 0.47-0.87, P=0.004). Urgent catheterization was performed within 12 hours of fibrinolysis in 34.9% of patients randomized to the standard treatment group.
This study was not powered to detect differences in mortality and other individual components of the primary endpoint.
Bottom line: STEMI patients who received fibrinolysis had a lower risk of adverse outcomes when receiving transfer and PCI within six hours, compared with standard delayed intervention.
Citation: Cantor WJ, Fitchett D, Borgundvaag B, et al. Routine early angioplasty after fibrinolysis for acute myocardial infarction. N Engl J Med. 2009;360(26):2705-2718.
Specialty Consultation and Limited Access Tests Predict Unsuccessful SSU Admissions
Clinical question: In patients admitted to short-stay units (SSUs), what characteristics are associated with unsuccessful SSU admission?
Background: Short-stay units have become prevalent in U.S. hospitals, but it is unclear which patient populations are best served by SSUs.
Study design: Prospective cohort.
Setting: Fourteen-bed SSU in a 500-bed public teaching hospital in Chicago.
Synopsis: More than 700 patients admitted to the Cook County Hospital SSU over a four-month period were interviewed and examined, and their ED and inpatient records were reviewed. An SSU admission was defined as “successful” if the length of stay (LOS) was less than 72 hours and the patient was discharged directly from the SSU.
Overall, 79% of patients had a successful SSU admission. In multivariate analysis, the strongest predictors of an unsuccessful SSU stay were subspecialty consultation (OR 8.1, P<0.001), a provisional diagnosis of heart failure (OR 1.9, P=0.02), and limited availability of a diagnostic test (OR 2.5, P<0.001).
The study was limited primarily to patients with cardiovascular diagnoses.
Bottom line: Patients admitted to SSUs who receive specialty consultation, carry a diagnosis of heart failure, or require diagnostic testing that is not readily available might have a longer LOS or eventual inpatient admission.
Citation: Lucas BP, Kumapley R, Mba B, et al. A hospitalist-run short-stay unit: features that predict length-of-stay and eventual admission to traditional inpatient services. J Hosp Med. 2009;4(5):276-284.
Lack of Significant Gains in Survival Rates Following In-Hospital CPR
Clinical question: Is survival after in-hospital CPR improving over time, and what are the factors associated with survival?
Background: Advances in out-of-hospital CPR have improved outcomes. However, it is unknown whether the survival rate after in-hospital CPR is improving over time, and it is unclear which patient and/or hospital characteristics predict post-CPR survival.
Study design: Retrospective cohort.
Setting: Inpatient Medicare beneficiaries from 1992 to 2005.
Synopsis: The study examined more than 150 million Medicare admissions, 433,985 of which underwent in-hospital CPR. Survival to discharge occurred in 18.3% of CPR events and did not change significantly from 1992 to 2005. The cumulative incidence of in-hospital CPR events was 2.73 per 1,000 admissions; it did not change substantially over time.
The survival rate was lower among black patients (OR 0.76, 95% CI, 0.74-0.79), which is partially explained due to the fact they tended to receive CPR at hospitals with lower post-CPR survival. Gender (specifically male), older age, race (specifically other nonwhite patients), higher burden of chronic illness, and admission from a skilled nursing facility were significantly associated with decreased survival to hospital discharge following CPR.
Limitations of this study included the identification of CPR by ICD-9 codes, which have not been validated for this purpose and could vary among hospitals. Other factors that might explain variations in survival were not available, including severity of acute illness and the presence (or absence) of a shockable rhythm at initial presentation.
Bottom line: Rates of survival to hospital discharge among Medicare beneficiaries receiving in-hospital CPR have remained constant over time, with poorer survival rates among blacks and other nonwhite patients.
Citation: Ehlenbach WJ, Barnato AE, Curtis JR, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009;361(1):22-31.
Hospitalists Are Associated with Improved Performance on Quality Metrics
Clinical question: Is the presence of hospitalist physicians associated with improved performance on standard quality measures for acute myocardial infarction (AMI), congestive heart failure (CHF), and pneumonia?
Background: Previous investigations have demonstrated significant improvements in cost and LOS for patients under the care of hospitalists compared with other inpatient providers. The association between hospitalist prevalence and quality of care, as measured by standard quality process measures, is unknown.
Study design: Cross-sectional.
Setting: More than 3,600 hospitals participating in the Health Quality Alliance (HQA) program.
Synopsis: Investigators looked at a large sample of HQA hospitals in the American Hospital Association survey, and identified facilities with hospitalist services and those without. The primary endpoint was the adherence to composites of standard quality process measures across three disease categories (AMI, CHF, and pneumonia) and two domains of care (disease treatment/diagnosis and counseling/prevention).
Multivariable analyses revealed a statistically significant association between the presence of hospitalists and adherence to composite quality measures for AMI and pneumonia. This association was demonstrated for both treatment and counseling domains.
The study is cross-sectional, so conclusions cannot be drawn about causality. Also, there are likely unmeasured differences between hospitals that utilize hospitalists compared with those that do not, which could further confound the relationship between the presence of hospitalists and adherence to quality measures.
Finally, this study only evaluated hospital-level performance, and it cannot offer insight on the quality of individual patient care by hospitalist providers.
Bottom line: The presence of hospitalists is associated with improvement in adherence to quality measures for both AMI and pneumonia, and across clinical domains of treatment and counseling.
Citation: López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394. TH
What is the proper duration of antibiotic treatment in adults hospitalized with community-acquired pneumonia?
Case
An 83-year-old male with hypertension, coronary artery disease, and obstructive sleep apnea presents with progressive shortness of breath, a productive cough, wheezing, and tachypnea. His blood pressure is 158/70 mm/Hg; temperature is 101.8; respirations are 26 breaths per minute; and oxygen saturation is 87% on room air. He has coarse breath sounds bilaterally, and decreased breath sounds over the right lower lung fields. His chest X-ray reveals a right lower lobe infiltrate. He is admitted to the hospital with a diagnosis of community-acquired pneumonia (CAP), and medical therapy is started. How should his antibiotic treatment be managed?
Overview
Community-acquired pneumonia is the most common infection-related cause of death in the U.S., and the eighth-leading cause of mortality overall.1 According to a 2006 survey, CAP results in more than 1.2 million hospital admissions annually, with an average length of stay of 5.1 days.2 Though less than 20% of CAP patients require hospitalization, cases necessitating admission contribute to more than 90% of the overall cost of pneumonia care.3
During the past several years, the availability of new antibiotics and the evolution of microbial resistance patterns have changed CAP treatment strategies. Furthermore, the development of prognostic scoring systems and increasing pressure to streamline resource utilization while improving quality of care have led to new treatment considerations, such as managing low-risk cases as outpatients.
More recently, attention has been directed to the optimal duration of antibiotic treatment, with a focus on shortening the duration of therapy. Historically, CAP treatment duration has been variable and not evidence-based. Shortening the course of antibiotics might limit antibiotic resistance, decrease costs, and improve patient adherence and tolerability.4 However, before defining the appropriate antibiotic duration for a patient hospitalized with CAP, other factors must be considered, such as the choice of empiric antibiotics, the patient’s initial response to treatment, severity of the disease, and presence of co-morbidities.
Review of the Data
Antibiotic choice. The most widely referenced practice guidelines for the management of CAP patients were published in 2007 by representatives of the Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS).5 Table 1 (above, right) summarizes the recommendations for empiric antibiotics for patients requiring inpatient treatment.
Time to clinical stability. A patient’s clinical response to empiric antibiotic therapy contributes heavily to the decision regarding treatment course and duration. The IDSA/ATS guidelines recommend patients be afebrile for 48 to 72 hours and have no more than one CAP-associated sign of clinical instability before discontinuation of therapy. Although studies have used different definitions of clinical stability, the consensus guidelines refer to six parameters, which are summarized in Table 2 (right).
With appropriate antibiotic therapy, most patients hospitalized with CAP achieve clinical stability in approximately three days.6,7 Providers should expect to see some improvement in vital signs within 48 to 72 hours of admission. Should a patient fail to demonstrate objective improvement during that time, providers should look for unusual pathogens, resistant organisms, nosocomial superinfections, or noninfectious conditions.5 Certain patients, such as those with multilobar pneumonia, associated pleural effusion, or higher pneumonia-severity index scores, also take longer to reach clinical stability.8
Switch to oral therapy. The ability to achieve clinical stability has important implications for hospital length of stay. Most patients hospitalized with CAP initially are treated with intravenous (IV) antibiotics and require transition to oral therapy in anticipation of discharge. Several studies have found there is no advantage to continuing IV medication once a patient is deemed clinically stable and is able to tolerate oral medication.9,10 There are no specific guidelines regarding choice of oral antibiotics, but it is common practice, supported by the IDSA/ATS recommendations, to use the same agent as the IV antibiotic or a medication in the same drug class. For patients started on β-lactam and macrolide combination therapy, it usually is appropriate to switch to a macrolide alone.5 In cases in which a pathogen has been identified, antibiotic selection should be based on the susceptibility profile.
Once patients are switched to oral antibiotics, it is not necessary for them to remain in the hospital for further observation, provided they have no other active medical problems or social needs. A retrospective analysis of 39,232 patients hospitalized with CAP compared those who were observed overnight after switching to oral antibiotics with those who were not and found no difference in 14-day readmission rate or 30-day mortality rate.11 These findings, in conjunction with the strategy of an early switch to oral therapy, suggest hospital length of stay may be safely reduced for many patients with uncomplicated CAP.
Duration of therapy. After a patient becomes clinically stable and a decision is made to switch to oral medication and a plan for hospital discharge, the question becomes how long to continue the course of antibiotics. Historically, clinical practice has extended treatment for up to two weeks, despite lack of evidence for this duration of therapy. The IDSA/ATS guidelines offer some general recommendations, noting patients should be treated for a minimum of five days, in addition to being afebrile for 48 to 72 hours and meet other criteria for clinical stability.5
Li and colleagues conducted a systematic review evaluating 15 randomized controlled trials comparing short-course (less than seven days) with extended (more than seven days) monotherapy for CAP in adults.4 Overall, the authors found no difference in the risk of treatment failure between short-course and extended-course antibiotic therapy, and they found no difference in bacteriologic eradication or mortality. It is important to note the studies included in this analysis enrolled patients with mild to moderate CAP, including those treated as outpatients, which limits the ability to extrapolate to exclusively inpatient populations and more severely ill patients.
Another meta-analysis, published shortly thereafter, examined randomized controlled trials in outpatients and inpatients not requiring intensive care. It compared different durations of treatment with the same agent in the same dosage. The authors similarly found no difference in effectiveness or safety of short (less than seven days) versus longer (at least two additional days of therapy) courses.12 Table 3 (above) reviews selected trials of short courses of antibiotics, which have been studied in inpatient populations.
The trials summarized in these meta-analyses examined monotherapy with levofloxacin for five days; gemifloxacin for seven days, azithromycin for three to five days; ceftriaxone for five days; cefuroxime for seven days; amoxicillin for three days; or telithromycin for five to seven days. The variety of antibiotics in these studies contrasts the IDSA/ATS guidelines, which recommend only fluoroquinolones as monotherapy for inpatient CAP.
One important randomized, double-blind study of fluoroquinolones compared a five-day course of levofloxacin 750 mg daily, with a 10-day course of levofloxacin, 500 mg daily, in 528 patients with mild to severe CAP.13 The authors found no difference in clinical success or microbiologic eradication between the two groups, concluding high-dose levofloxacin for five days is an effective and well-tolerated alternative to a longer course of a lower dose, likely related to the drug’s concentration-dependent properties.
Azithromycin also offers potential for short courses of therapy, as pulmonary concentrations of azithromycin remain elevated for as many as five days following a single oral dose.14 Several small studies have demonstrated the safety, efficacy, and cost-effectiveness of three to five days of azithromycin, as summarized in a meta-analysis by Contopoulos-Ioannidis and colleagues.15 Most of these trials, however, were limited to outpatients or inpatients with mild disease or confirmed atypical pneumonia. One randomized trial of 40 inpatients with mild to moderately severe CAP found comparable clinical outcomes with a three-day course of oral azithromycin 500 mg daily versus clarithromycin for at least eight days.16 Larger studies in more severely ill patients must be completed before routinely recommending this approach in hospitalized patients. Furthermore, due to the rising prevalence of macrolide resistance, empiric therapy with a macrolide alone can only be used for the treatment of carefully selected hospitalized patients with nonsevere diseases and without risk factors for drug-resistant Streptococcus pneumoniae.5
Telithromycin is a ketolide antibiotic, which has been studied in mild to moderate CAP, including multidrug-resistant strains of S. pneumoniae, in courses of five to seven days.17 However, severe adverse reactions, including hepatotoxicity, have been reported. At the time of the 2007 guidelines, the IDSA/ATS committee waited for additional safety data before making any recommendations on its use.
One additional study of note was a trial of amoxicillin in adult inpatients with mild to moderately severe CAP.18 One hundred twenty-one patients who clinically improved (based on a composite score of pulmonary symptoms and general improvement) following three days of IV amoxicillin were randomized to oral amoxicillin for an additional five days or given a placebo. At days 10 and 28, there was no difference in clinical success between the two groups. The authors concluded that a total of three days of treatment was not inferior to eight days in patients who substantially improved after the first 72 hours of empiric treatment. This trial was conducted in the Netherlands, where amoxicillin is the preferred empiric antibiotic for CAP and patterns of antimicrobial resistance differ greatly from those found in the U.S.
Other considerations. While some evidence supports shorter courses of antibiotics, many of the existing studies are limited by their inclusion of outpatients, adults with mild to moderate CAP, or small sample size. Hence, clinical judgment continues to play an important role in determining the appropriate duration of therapy. Factors such as pre-existing co-morbidities, severity of illness, and occurrence of complications should be considered. Data is limited on the appropriate duration of antibiotics in CAP patients requiring intensive care. It also is important to note the IDSA/ATS recommendations and most of the studies reviewed exclude patients with human immunodeficiency virus (HIV), and it is unknown whether these shorter courses of antibiotics are appropriate in the HIV population.
Lastly, the IDSA/ATS guidelines note longer durations of treatment may be required if the initial therapy was not active against the identified pathogen, or in cases complicated by extrapulmonary infections, such as endocarditis or meningitis.
Back to the Case
Our patient with moderately severe CAP was hospitalized based on his age and hypoxia. He was immediately treated with supplemental oxygen by nasal cannula, IV fluids, and a dose of IV levofloxacin 750 mg. Within 48 hours he met criteria for clinical stability, including defervescence, a decline in his respiratory rate to 19 breaths per minute, and improvement in oxygen saturation to 95% on room air. At this point, he was changed from IV to oral antibiotics. He continued on levofloxacin 750 mg daily and later that day was discharged home in good condition to complete a five-day course.
Bottom Line
For hospitalized adults with mild to moderately severe CAP, five to seven days of treatment, depending on the antibiotic selected, appears to be effective in most cases. Patients should be afebrile for 48 to 72 hours and demonstrate signs of clinical stability before therapy is discontinued. TH
Kelly Cunningham, MD, and Shelley Ellis, MD, MPH, are members of the Section of Hospital Medicine at Vanderbilt University in Nashville, Tenn. Sunil Kripalani, MD, MSc, serves as the section chief.
References
1. Kung HC, Hoyert DL, Xu J, Murphy SL. Deaths: final data for 2005. Natl Vital Stat Rep. 2008;56.
2. DeFrances CJ, Lucas CA, Buie VC, Golosinskiy A. 2006 National Hospital Discharge Survey. Natl Health Stat Report. 2008;5.
3. Niederman MS. Recent advances in community-acquired pneumonia: inpatient and outpatient. Chest. 2007;131:1205-1215.
4. Li JZ, Winston LG, Moore DH, Bent S. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med. 2007;120:783-790.
5. Mandell LA, Wunderink RG, Anzueto A et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27-72.
6. Ramirez JA, Bordon J. Early switch from intravenous to oral antibiotics in hospitalized patients with bacteremic community-acquired Streptococcus pneumoniae pneumonia. Arch Intern Med. 2001;161:848-850.
7. Halm EA, Fine MJ, Marrie TJ et al. Time to clinical stability in patients hospitalized with community-acquired pneumonia: implications for practice guidelines. JAMA. 1998;279:1452-1457.
8. Menendez R, Torres A, Rodriguez de Castro F et al. Reaching stability in community-acquired pneumonia: the effects of the severity of disease, treatment, and the characteristics of patients. Clin Infect Dis. 2004;39:1783-1790.
9. Siegal RE, Halpern NA, Almenoff PL et al. A prospective randomised study of inpatient IV antibiotics for community-acquired pneumonia: the optimal duration of therapy. Chest. 1996;110:965-971.
10. Oosterheert JJ, Bonten MJ, Schneider MM et al. Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia: multicentre randomized trial. BMJ. 2006;333:1193-1197.
11. Nathan RV, Rhew DC, Murray C et al. In-hospital observation after antibiotic switch in pneumonia: a national evaluation. Am J Med. 2006;119:512-518.
12. Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, et al. Short- versus long-course antibacterial therapy for community-acquired pneumonia: a meta-analysis. Drugs. 2008;68:1841-1854.
13. Dunbar LM, Wunderink RG, Habib MP et al. High-dose, short-course levofloxacin for community-acquired pneumonia: a new treatment paradigm. Clin Infect Dis. 2003;37:752-760.
14. Morris DL, De Souza A, Jones JA, Morgan WE. High and prolonged pulmonary tissue concentrations of azithromycin following a single oral dose. Eur J Clin Microbiol Infect Dis. 1991;10:859-861.
15. Contopoulos-Ioannidis DG, Ioannidis JPA, Chew P, Lau J. Meta-analysis of randomized controlled trials on the comparative efficacy and safety of azithromycin against other antibiotics for lower respiratory tract infections. J Antimicrob Chemother. 2001;48:691-703.
16. Rizzato G, Montemurro L, Fraioli P et al. Efficacy of a three-day course of azithromycin in moderately severe community-acquired pneumonia. Eur Respir J. 1995;8:398-402.
17. Tellier G, Niederman MS, Nusrat R et al. Clinical and bacteriological efficacy and safety of 5- and 7-day regimens of telithromycin once daily compared with a 10-day regimen of clarithromycin twice daily in patients with mild to moderate community-acquired pneumonia. J Antimicrob Chemother. 2004;54:515.
18. El Moussaoui R, de Borgie CA, van den Broek P et al. Effectiveness of discontinuing antibiotic treatment after three days versus eight days in mild to moderate-severe community acquired pneumonia: randomised, double blind study. BMJ. 2006;332:1355-1361.
19. Siegel RE, Alicea M, Lee A, Blaiklock R. Comparison of 7 versus 10 days of antibiotic therapy for hospitalized patients with uncomplicated community-acquired pneumonia: a prospective, randomized double-blind study. Am J Ther. 1999;6:217-222.
Case
An 83-year-old male with hypertension, coronary artery disease, and obstructive sleep apnea presents with progressive shortness of breath, a productive cough, wheezing, and tachypnea. His blood pressure is 158/70 mm/Hg; temperature is 101.8; respirations are 26 breaths per minute; and oxygen saturation is 87% on room air. He has coarse breath sounds bilaterally, and decreased breath sounds over the right lower lung fields. His chest X-ray reveals a right lower lobe infiltrate. He is admitted to the hospital with a diagnosis of community-acquired pneumonia (CAP), and medical therapy is started. How should his antibiotic treatment be managed?
Overview
Community-acquired pneumonia is the most common infection-related cause of death in the U.S., and the eighth-leading cause of mortality overall.1 According to a 2006 survey, CAP results in more than 1.2 million hospital admissions annually, with an average length of stay of 5.1 days.2 Though less than 20% of CAP patients require hospitalization, cases necessitating admission contribute to more than 90% of the overall cost of pneumonia care.3
During the past several years, the availability of new antibiotics and the evolution of microbial resistance patterns have changed CAP treatment strategies. Furthermore, the development of prognostic scoring systems and increasing pressure to streamline resource utilization while improving quality of care have led to new treatment considerations, such as managing low-risk cases as outpatients.
More recently, attention has been directed to the optimal duration of antibiotic treatment, with a focus on shortening the duration of therapy. Historically, CAP treatment duration has been variable and not evidence-based. Shortening the course of antibiotics might limit antibiotic resistance, decrease costs, and improve patient adherence and tolerability.4 However, before defining the appropriate antibiotic duration for a patient hospitalized with CAP, other factors must be considered, such as the choice of empiric antibiotics, the patient’s initial response to treatment, severity of the disease, and presence of co-morbidities.
Review of the Data
Antibiotic choice. The most widely referenced practice guidelines for the management of CAP patients were published in 2007 by representatives of the Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS).5 Table 1 (above, right) summarizes the recommendations for empiric antibiotics for patients requiring inpatient treatment.
Time to clinical stability. A patient’s clinical response to empiric antibiotic therapy contributes heavily to the decision regarding treatment course and duration. The IDSA/ATS guidelines recommend patients be afebrile for 48 to 72 hours and have no more than one CAP-associated sign of clinical instability before discontinuation of therapy. Although studies have used different definitions of clinical stability, the consensus guidelines refer to six parameters, which are summarized in Table 2 (right).
With appropriate antibiotic therapy, most patients hospitalized with CAP achieve clinical stability in approximately three days.6,7 Providers should expect to see some improvement in vital signs within 48 to 72 hours of admission. Should a patient fail to demonstrate objective improvement during that time, providers should look for unusual pathogens, resistant organisms, nosocomial superinfections, or noninfectious conditions.5 Certain patients, such as those with multilobar pneumonia, associated pleural effusion, or higher pneumonia-severity index scores, also take longer to reach clinical stability.8
Switch to oral therapy. The ability to achieve clinical stability has important implications for hospital length of stay. Most patients hospitalized with CAP initially are treated with intravenous (IV) antibiotics and require transition to oral therapy in anticipation of discharge. Several studies have found there is no advantage to continuing IV medication once a patient is deemed clinically stable and is able to tolerate oral medication.9,10 There are no specific guidelines regarding choice of oral antibiotics, but it is common practice, supported by the IDSA/ATS recommendations, to use the same agent as the IV antibiotic or a medication in the same drug class. For patients started on β-lactam and macrolide combination therapy, it usually is appropriate to switch to a macrolide alone.5 In cases in which a pathogen has been identified, antibiotic selection should be based on the susceptibility profile.
Once patients are switched to oral antibiotics, it is not necessary for them to remain in the hospital for further observation, provided they have no other active medical problems or social needs. A retrospective analysis of 39,232 patients hospitalized with CAP compared those who were observed overnight after switching to oral antibiotics with those who were not and found no difference in 14-day readmission rate or 30-day mortality rate.11 These findings, in conjunction with the strategy of an early switch to oral therapy, suggest hospital length of stay may be safely reduced for many patients with uncomplicated CAP.
Duration of therapy. After a patient becomes clinically stable and a decision is made to switch to oral medication and a plan for hospital discharge, the question becomes how long to continue the course of antibiotics. Historically, clinical practice has extended treatment for up to two weeks, despite lack of evidence for this duration of therapy. The IDSA/ATS guidelines offer some general recommendations, noting patients should be treated for a minimum of five days, in addition to being afebrile for 48 to 72 hours and meet other criteria for clinical stability.5
Li and colleagues conducted a systematic review evaluating 15 randomized controlled trials comparing short-course (less than seven days) with extended (more than seven days) monotherapy for CAP in adults.4 Overall, the authors found no difference in the risk of treatment failure between short-course and extended-course antibiotic therapy, and they found no difference in bacteriologic eradication or mortality. It is important to note the studies included in this analysis enrolled patients with mild to moderate CAP, including those treated as outpatients, which limits the ability to extrapolate to exclusively inpatient populations and more severely ill patients.
Another meta-analysis, published shortly thereafter, examined randomized controlled trials in outpatients and inpatients not requiring intensive care. It compared different durations of treatment with the same agent in the same dosage. The authors similarly found no difference in effectiveness or safety of short (less than seven days) versus longer (at least two additional days of therapy) courses.12 Table 3 (above) reviews selected trials of short courses of antibiotics, which have been studied in inpatient populations.
The trials summarized in these meta-analyses examined monotherapy with levofloxacin for five days; gemifloxacin for seven days, azithromycin for three to five days; ceftriaxone for five days; cefuroxime for seven days; amoxicillin for three days; or telithromycin for five to seven days. The variety of antibiotics in these studies contrasts the IDSA/ATS guidelines, which recommend only fluoroquinolones as monotherapy for inpatient CAP.
One important randomized, double-blind study of fluoroquinolones compared a five-day course of levofloxacin 750 mg daily, with a 10-day course of levofloxacin, 500 mg daily, in 528 patients with mild to severe CAP.13 The authors found no difference in clinical success or microbiologic eradication between the two groups, concluding high-dose levofloxacin for five days is an effective and well-tolerated alternative to a longer course of a lower dose, likely related to the drug’s concentration-dependent properties.
Azithromycin also offers potential for short courses of therapy, as pulmonary concentrations of azithromycin remain elevated for as many as five days following a single oral dose.14 Several small studies have demonstrated the safety, efficacy, and cost-effectiveness of three to five days of azithromycin, as summarized in a meta-analysis by Contopoulos-Ioannidis and colleagues.15 Most of these trials, however, were limited to outpatients or inpatients with mild disease or confirmed atypical pneumonia. One randomized trial of 40 inpatients with mild to moderately severe CAP found comparable clinical outcomes with a three-day course of oral azithromycin 500 mg daily versus clarithromycin for at least eight days.16 Larger studies in more severely ill patients must be completed before routinely recommending this approach in hospitalized patients. Furthermore, due to the rising prevalence of macrolide resistance, empiric therapy with a macrolide alone can only be used for the treatment of carefully selected hospitalized patients with nonsevere diseases and without risk factors for drug-resistant Streptococcus pneumoniae.5
Telithromycin is a ketolide antibiotic, which has been studied in mild to moderate CAP, including multidrug-resistant strains of S. pneumoniae, in courses of five to seven days.17 However, severe adverse reactions, including hepatotoxicity, have been reported. At the time of the 2007 guidelines, the IDSA/ATS committee waited for additional safety data before making any recommendations on its use.
One additional study of note was a trial of amoxicillin in adult inpatients with mild to moderately severe CAP.18 One hundred twenty-one patients who clinically improved (based on a composite score of pulmonary symptoms and general improvement) following three days of IV amoxicillin were randomized to oral amoxicillin for an additional five days or given a placebo. At days 10 and 28, there was no difference in clinical success between the two groups. The authors concluded that a total of three days of treatment was not inferior to eight days in patients who substantially improved after the first 72 hours of empiric treatment. This trial was conducted in the Netherlands, where amoxicillin is the preferred empiric antibiotic for CAP and patterns of antimicrobial resistance differ greatly from those found in the U.S.
Other considerations. While some evidence supports shorter courses of antibiotics, many of the existing studies are limited by their inclusion of outpatients, adults with mild to moderate CAP, or small sample size. Hence, clinical judgment continues to play an important role in determining the appropriate duration of therapy. Factors such as pre-existing co-morbidities, severity of illness, and occurrence of complications should be considered. Data is limited on the appropriate duration of antibiotics in CAP patients requiring intensive care. It also is important to note the IDSA/ATS recommendations and most of the studies reviewed exclude patients with human immunodeficiency virus (HIV), and it is unknown whether these shorter courses of antibiotics are appropriate in the HIV population.
Lastly, the IDSA/ATS guidelines note longer durations of treatment may be required if the initial therapy was not active against the identified pathogen, or in cases complicated by extrapulmonary infections, such as endocarditis or meningitis.
Back to the Case
Our patient with moderately severe CAP was hospitalized based on his age and hypoxia. He was immediately treated with supplemental oxygen by nasal cannula, IV fluids, and a dose of IV levofloxacin 750 mg. Within 48 hours he met criteria for clinical stability, including defervescence, a decline in his respiratory rate to 19 breaths per minute, and improvement in oxygen saturation to 95% on room air. At this point, he was changed from IV to oral antibiotics. He continued on levofloxacin 750 mg daily and later that day was discharged home in good condition to complete a five-day course.
Bottom Line
For hospitalized adults with mild to moderately severe CAP, five to seven days of treatment, depending on the antibiotic selected, appears to be effective in most cases. Patients should be afebrile for 48 to 72 hours and demonstrate signs of clinical stability before therapy is discontinued. TH
Kelly Cunningham, MD, and Shelley Ellis, MD, MPH, are members of the Section of Hospital Medicine at Vanderbilt University in Nashville, Tenn. Sunil Kripalani, MD, MSc, serves as the section chief.
References
1. Kung HC, Hoyert DL, Xu J, Murphy SL. Deaths: final data for 2005. Natl Vital Stat Rep. 2008;56.
2. DeFrances CJ, Lucas CA, Buie VC, Golosinskiy A. 2006 National Hospital Discharge Survey. Natl Health Stat Report. 2008;5.
3. Niederman MS. Recent advances in community-acquired pneumonia: inpatient and outpatient. Chest. 2007;131:1205-1215.
4. Li JZ, Winston LG, Moore DH, Bent S. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med. 2007;120:783-790.
5. Mandell LA, Wunderink RG, Anzueto A et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27-72.
6. Ramirez JA, Bordon J. Early switch from intravenous to oral antibiotics in hospitalized patients with bacteremic community-acquired Streptococcus pneumoniae pneumonia. Arch Intern Med. 2001;161:848-850.
7. Halm EA, Fine MJ, Marrie TJ et al. Time to clinical stability in patients hospitalized with community-acquired pneumonia: implications for practice guidelines. JAMA. 1998;279:1452-1457.
8. Menendez R, Torres A, Rodriguez de Castro F et al. Reaching stability in community-acquired pneumonia: the effects of the severity of disease, treatment, and the characteristics of patients. Clin Infect Dis. 2004;39:1783-1790.
9. Siegal RE, Halpern NA, Almenoff PL et al. A prospective randomised study of inpatient IV antibiotics for community-acquired pneumonia: the optimal duration of therapy. Chest. 1996;110:965-971.
10. Oosterheert JJ, Bonten MJ, Schneider MM et al. Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia: multicentre randomized trial. BMJ. 2006;333:1193-1197.
11. Nathan RV, Rhew DC, Murray C et al. In-hospital observation after antibiotic switch in pneumonia: a national evaluation. Am J Med. 2006;119:512-518.
12. Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, et al. Short- versus long-course antibacterial therapy for community-acquired pneumonia: a meta-analysis. Drugs. 2008;68:1841-1854.
13. Dunbar LM, Wunderink RG, Habib MP et al. High-dose, short-course levofloxacin for community-acquired pneumonia: a new treatment paradigm. Clin Infect Dis. 2003;37:752-760.
14. Morris DL, De Souza A, Jones JA, Morgan WE. High and prolonged pulmonary tissue concentrations of azithromycin following a single oral dose. Eur J Clin Microbiol Infect Dis. 1991;10:859-861.
15. Contopoulos-Ioannidis DG, Ioannidis JPA, Chew P, Lau J. Meta-analysis of randomized controlled trials on the comparative efficacy and safety of azithromycin against other antibiotics for lower respiratory tract infections. J Antimicrob Chemother. 2001;48:691-703.
16. Rizzato G, Montemurro L, Fraioli P et al. Efficacy of a three-day course of azithromycin in moderately severe community-acquired pneumonia. Eur Respir J. 1995;8:398-402.
17. Tellier G, Niederman MS, Nusrat R et al. Clinical and bacteriological efficacy and safety of 5- and 7-day regimens of telithromycin once daily compared with a 10-day regimen of clarithromycin twice daily in patients with mild to moderate community-acquired pneumonia. J Antimicrob Chemother. 2004;54:515.
18. El Moussaoui R, de Borgie CA, van den Broek P et al. Effectiveness of discontinuing antibiotic treatment after three days versus eight days in mild to moderate-severe community acquired pneumonia: randomised, double blind study. BMJ. 2006;332:1355-1361.
19. Siegel RE, Alicea M, Lee A, Blaiklock R. Comparison of 7 versus 10 days of antibiotic therapy for hospitalized patients with uncomplicated community-acquired pneumonia: a prospective, randomized double-blind study. Am J Ther. 1999;6:217-222.
Case
An 83-year-old male with hypertension, coronary artery disease, and obstructive sleep apnea presents with progressive shortness of breath, a productive cough, wheezing, and tachypnea. His blood pressure is 158/70 mm/Hg; temperature is 101.8; respirations are 26 breaths per minute; and oxygen saturation is 87% on room air. He has coarse breath sounds bilaterally, and decreased breath sounds over the right lower lung fields. His chest X-ray reveals a right lower lobe infiltrate. He is admitted to the hospital with a diagnosis of community-acquired pneumonia (CAP), and medical therapy is started. How should his antibiotic treatment be managed?
Overview
Community-acquired pneumonia is the most common infection-related cause of death in the U.S., and the eighth-leading cause of mortality overall.1 According to a 2006 survey, CAP results in more than 1.2 million hospital admissions annually, with an average length of stay of 5.1 days.2 Though less than 20% of CAP patients require hospitalization, cases necessitating admission contribute to more than 90% of the overall cost of pneumonia care.3
During the past several years, the availability of new antibiotics and the evolution of microbial resistance patterns have changed CAP treatment strategies. Furthermore, the development of prognostic scoring systems and increasing pressure to streamline resource utilization while improving quality of care have led to new treatment considerations, such as managing low-risk cases as outpatients.
More recently, attention has been directed to the optimal duration of antibiotic treatment, with a focus on shortening the duration of therapy. Historically, CAP treatment duration has been variable and not evidence-based. Shortening the course of antibiotics might limit antibiotic resistance, decrease costs, and improve patient adherence and tolerability.4 However, before defining the appropriate antibiotic duration for a patient hospitalized with CAP, other factors must be considered, such as the choice of empiric antibiotics, the patient’s initial response to treatment, severity of the disease, and presence of co-morbidities.
Review of the Data
Antibiotic choice. The most widely referenced practice guidelines for the management of CAP patients were published in 2007 by representatives of the Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS).5 Table 1 (above, right) summarizes the recommendations for empiric antibiotics for patients requiring inpatient treatment.
Time to clinical stability. A patient’s clinical response to empiric antibiotic therapy contributes heavily to the decision regarding treatment course and duration. The IDSA/ATS guidelines recommend patients be afebrile for 48 to 72 hours and have no more than one CAP-associated sign of clinical instability before discontinuation of therapy. Although studies have used different definitions of clinical stability, the consensus guidelines refer to six parameters, which are summarized in Table 2 (right).
With appropriate antibiotic therapy, most patients hospitalized with CAP achieve clinical stability in approximately three days.6,7 Providers should expect to see some improvement in vital signs within 48 to 72 hours of admission. Should a patient fail to demonstrate objective improvement during that time, providers should look for unusual pathogens, resistant organisms, nosocomial superinfections, or noninfectious conditions.5 Certain patients, such as those with multilobar pneumonia, associated pleural effusion, or higher pneumonia-severity index scores, also take longer to reach clinical stability.8
Switch to oral therapy. The ability to achieve clinical stability has important implications for hospital length of stay. Most patients hospitalized with CAP initially are treated with intravenous (IV) antibiotics and require transition to oral therapy in anticipation of discharge. Several studies have found there is no advantage to continuing IV medication once a patient is deemed clinically stable and is able to tolerate oral medication.9,10 There are no specific guidelines regarding choice of oral antibiotics, but it is common practice, supported by the IDSA/ATS recommendations, to use the same agent as the IV antibiotic or a medication in the same drug class. For patients started on β-lactam and macrolide combination therapy, it usually is appropriate to switch to a macrolide alone.5 In cases in which a pathogen has been identified, antibiotic selection should be based on the susceptibility profile.
Once patients are switched to oral antibiotics, it is not necessary for them to remain in the hospital for further observation, provided they have no other active medical problems or social needs. A retrospective analysis of 39,232 patients hospitalized with CAP compared those who were observed overnight after switching to oral antibiotics with those who were not and found no difference in 14-day readmission rate or 30-day mortality rate.11 These findings, in conjunction with the strategy of an early switch to oral therapy, suggest hospital length of stay may be safely reduced for many patients with uncomplicated CAP.
Duration of therapy. After a patient becomes clinically stable and a decision is made to switch to oral medication and a plan for hospital discharge, the question becomes how long to continue the course of antibiotics. Historically, clinical practice has extended treatment for up to two weeks, despite lack of evidence for this duration of therapy. The IDSA/ATS guidelines offer some general recommendations, noting patients should be treated for a minimum of five days, in addition to being afebrile for 48 to 72 hours and meet other criteria for clinical stability.5
Li and colleagues conducted a systematic review evaluating 15 randomized controlled trials comparing short-course (less than seven days) with extended (more than seven days) monotherapy for CAP in adults.4 Overall, the authors found no difference in the risk of treatment failure between short-course and extended-course antibiotic therapy, and they found no difference in bacteriologic eradication or mortality. It is important to note the studies included in this analysis enrolled patients with mild to moderate CAP, including those treated as outpatients, which limits the ability to extrapolate to exclusively inpatient populations and more severely ill patients.
Another meta-analysis, published shortly thereafter, examined randomized controlled trials in outpatients and inpatients not requiring intensive care. It compared different durations of treatment with the same agent in the same dosage. The authors similarly found no difference in effectiveness or safety of short (less than seven days) versus longer (at least two additional days of therapy) courses.12 Table 3 (above) reviews selected trials of short courses of antibiotics, which have been studied in inpatient populations.
The trials summarized in these meta-analyses examined monotherapy with levofloxacin for five days; gemifloxacin for seven days, azithromycin for three to five days; ceftriaxone for five days; cefuroxime for seven days; amoxicillin for three days; or telithromycin for five to seven days. The variety of antibiotics in these studies contrasts the IDSA/ATS guidelines, which recommend only fluoroquinolones as monotherapy for inpatient CAP.
One important randomized, double-blind study of fluoroquinolones compared a five-day course of levofloxacin 750 mg daily, with a 10-day course of levofloxacin, 500 mg daily, in 528 patients with mild to severe CAP.13 The authors found no difference in clinical success or microbiologic eradication between the two groups, concluding high-dose levofloxacin for five days is an effective and well-tolerated alternative to a longer course of a lower dose, likely related to the drug’s concentration-dependent properties.
Azithromycin also offers potential for short courses of therapy, as pulmonary concentrations of azithromycin remain elevated for as many as five days following a single oral dose.14 Several small studies have demonstrated the safety, efficacy, and cost-effectiveness of three to five days of azithromycin, as summarized in a meta-analysis by Contopoulos-Ioannidis and colleagues.15 Most of these trials, however, were limited to outpatients or inpatients with mild disease or confirmed atypical pneumonia. One randomized trial of 40 inpatients with mild to moderately severe CAP found comparable clinical outcomes with a three-day course of oral azithromycin 500 mg daily versus clarithromycin for at least eight days.16 Larger studies in more severely ill patients must be completed before routinely recommending this approach in hospitalized patients. Furthermore, due to the rising prevalence of macrolide resistance, empiric therapy with a macrolide alone can only be used for the treatment of carefully selected hospitalized patients with nonsevere diseases and without risk factors for drug-resistant Streptococcus pneumoniae.5
Telithromycin is a ketolide antibiotic, which has been studied in mild to moderate CAP, including multidrug-resistant strains of S. pneumoniae, in courses of five to seven days.17 However, severe adverse reactions, including hepatotoxicity, have been reported. At the time of the 2007 guidelines, the IDSA/ATS committee waited for additional safety data before making any recommendations on its use.
One additional study of note was a trial of amoxicillin in adult inpatients with mild to moderately severe CAP.18 One hundred twenty-one patients who clinically improved (based on a composite score of pulmonary symptoms and general improvement) following three days of IV amoxicillin were randomized to oral amoxicillin for an additional five days or given a placebo. At days 10 and 28, there was no difference in clinical success between the two groups. The authors concluded that a total of three days of treatment was not inferior to eight days in patients who substantially improved after the first 72 hours of empiric treatment. This trial was conducted in the Netherlands, where amoxicillin is the preferred empiric antibiotic for CAP and patterns of antimicrobial resistance differ greatly from those found in the U.S.
Other considerations. While some evidence supports shorter courses of antibiotics, many of the existing studies are limited by their inclusion of outpatients, adults with mild to moderate CAP, or small sample size. Hence, clinical judgment continues to play an important role in determining the appropriate duration of therapy. Factors such as pre-existing co-morbidities, severity of illness, and occurrence of complications should be considered. Data is limited on the appropriate duration of antibiotics in CAP patients requiring intensive care. It also is important to note the IDSA/ATS recommendations and most of the studies reviewed exclude patients with human immunodeficiency virus (HIV), and it is unknown whether these shorter courses of antibiotics are appropriate in the HIV population.
Lastly, the IDSA/ATS guidelines note longer durations of treatment may be required if the initial therapy was not active against the identified pathogen, or in cases complicated by extrapulmonary infections, such as endocarditis or meningitis.
Back to the Case
Our patient with moderately severe CAP was hospitalized based on his age and hypoxia. He was immediately treated with supplemental oxygen by nasal cannula, IV fluids, and a dose of IV levofloxacin 750 mg. Within 48 hours he met criteria for clinical stability, including defervescence, a decline in his respiratory rate to 19 breaths per minute, and improvement in oxygen saturation to 95% on room air. At this point, he was changed from IV to oral antibiotics. He continued on levofloxacin 750 mg daily and later that day was discharged home in good condition to complete a five-day course.
Bottom Line
For hospitalized adults with mild to moderately severe CAP, five to seven days of treatment, depending on the antibiotic selected, appears to be effective in most cases. Patients should be afebrile for 48 to 72 hours and demonstrate signs of clinical stability before therapy is discontinued. TH
Kelly Cunningham, MD, and Shelley Ellis, MD, MPH, are members of the Section of Hospital Medicine at Vanderbilt University in Nashville, Tenn. Sunil Kripalani, MD, MSc, serves as the section chief.
References
1. Kung HC, Hoyert DL, Xu J, Murphy SL. Deaths: final data for 2005. Natl Vital Stat Rep. 2008;56.
2. DeFrances CJ, Lucas CA, Buie VC, Golosinskiy A. 2006 National Hospital Discharge Survey. Natl Health Stat Report. 2008;5.
3. Niederman MS. Recent advances in community-acquired pneumonia: inpatient and outpatient. Chest. 2007;131:1205-1215.
4. Li JZ, Winston LG, Moore DH, Bent S. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med. 2007;120:783-790.
5. Mandell LA, Wunderink RG, Anzueto A et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27-72.
6. Ramirez JA, Bordon J. Early switch from intravenous to oral antibiotics in hospitalized patients with bacteremic community-acquired Streptococcus pneumoniae pneumonia. Arch Intern Med. 2001;161:848-850.
7. Halm EA, Fine MJ, Marrie TJ et al. Time to clinical stability in patients hospitalized with community-acquired pneumonia: implications for practice guidelines. JAMA. 1998;279:1452-1457.
8. Menendez R, Torres A, Rodriguez de Castro F et al. Reaching stability in community-acquired pneumonia: the effects of the severity of disease, treatment, and the characteristics of patients. Clin Infect Dis. 2004;39:1783-1790.
9. Siegal RE, Halpern NA, Almenoff PL et al. A prospective randomised study of inpatient IV antibiotics for community-acquired pneumonia: the optimal duration of therapy. Chest. 1996;110:965-971.
10. Oosterheert JJ, Bonten MJ, Schneider MM et al. Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia: multicentre randomized trial. BMJ. 2006;333:1193-1197.
11. Nathan RV, Rhew DC, Murray C et al. In-hospital observation after antibiotic switch in pneumonia: a national evaluation. Am J Med. 2006;119:512-518.
12. Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, et al. Short- versus long-course antibacterial therapy for community-acquired pneumonia: a meta-analysis. Drugs. 2008;68:1841-1854.
13. Dunbar LM, Wunderink RG, Habib MP et al. High-dose, short-course levofloxacin for community-acquired pneumonia: a new treatment paradigm. Clin Infect Dis. 2003;37:752-760.
14. Morris DL, De Souza A, Jones JA, Morgan WE. High and prolonged pulmonary tissue concentrations of azithromycin following a single oral dose. Eur J Clin Microbiol Infect Dis. 1991;10:859-861.
15. Contopoulos-Ioannidis DG, Ioannidis JPA, Chew P, Lau J. Meta-analysis of randomized controlled trials on the comparative efficacy and safety of azithromycin against other antibiotics for lower respiratory tract infections. J Antimicrob Chemother. 2001;48:691-703.
16. Rizzato G, Montemurro L, Fraioli P et al. Efficacy of a three-day course of azithromycin in moderately severe community-acquired pneumonia. Eur Respir J. 1995;8:398-402.
17. Tellier G, Niederman MS, Nusrat R et al. Clinical and bacteriological efficacy and safety of 5- and 7-day regimens of telithromycin once daily compared with a 10-day regimen of clarithromycin twice daily in patients with mild to moderate community-acquired pneumonia. J Antimicrob Chemother. 2004;54:515.
18. El Moussaoui R, de Borgie CA, van den Broek P et al. Effectiveness of discontinuing antibiotic treatment after three days versus eight days in mild to moderate-severe community acquired pneumonia: randomised, double blind study. BMJ. 2006;332:1355-1361.
19. Siegel RE, Alicea M, Lee A, Blaiklock R. Comparison of 7 versus 10 days of antibiotic therapy for hospitalized patients with uncomplicated community-acquired pneumonia: a prospective, randomized double-blind study. Am J Ther. 1999;6:217-222.
In the Literature
Literature at a Glance
A guide to this month’s studies.
- Adverse events are common after stopping clopidogrel following acute coronary syndrome.
- Treatment intensification with insulin improves inpatient glucose control.
- Pressure for early antibiotic administration leads to inaccuracy of pneumonia diagnosis.
- Multifaceted ventilation strategy no better than low-tidal-volume protocol.
- Higher PEEP ventilation strategy reduces duration of ventilation but not mortality.
- N-acetylcysteine reduces contrast-induced nephropathy.
- Vasopressin is no better than norepinephrine in patients with septic shock.
- Hospital patients desire greater participation in decision-making.
- Outcomes of patients with upper- or lower-extremity DVT are similar.
- Oral and IV steroids may be equally effective in COPD exacerbation.
What is Frequency, Timing of Adverse Events After Stopping Clopidogrel in ACS Patients?
Background: Clopidogrel is recommended in treatment of acute coronary syndrome (ACS) with or without stent placement. A rebound hypercoagulable state may occur following clopidogrel cessation, but this has not been investigated previously.
Study design: Retrospective cohort.
Setting: 127 VA medical centers.
Synopsis: Data were collected as part of the Veterans Health Administration Cardiac Care Follow-up Clinical Study from October 2003 through March 2005 on all patients with acute myocardial infarction (MI) or unstable angina who were discharged with clopidogrel treatment (3,137 patients). The analysis assessed the incidence and timing of adverse events after stopping clopidogrel among medically treated patients and among those treated with percutaneous coronary intervention (PCI).
In adjusted analyses among medically treated patients, the risk of death or acute MI in the first 90 days after clopidogrel cessation was 1.98 times higher, compared with the interval from 91-180 days. Among patients who received PCI (usually with a bare-metal stent), the risk was 1.82 times higher in the first 90 days. The clustering of events shortly after clopidogrel cessation support the possibility of a rebound hypercoagulable state.
Bottom line: In patients with ACS who received medical management or PCI, there was a higher rate of adverse events in the first 90 days after clopidogrel cessation.
Citation: Ho PM, Peterson ED, Wang L, et al. Incidence of death and acute myocardial infarction associated with stopping clopidorel after acute coronary syndrome. JAMA 2008;299(5):532-539.
What is the Relationship Between Treatment Intensification, Blood Pressure Changes in Diabetes Patients?
Background: Hyperglycemia is common in hospitalized patients with diabetes and associated with poor outcomes. Prior research on treatment intensification has focused on the intensive care unit or outpatient setting. The effect of treatment intensification in the inpatient (non-ICU) setting is not known.
Study design: Retrospective cohort.
Setting: 734-bed teaching hospital in Boston.
Synopsis: Between January 2003 and August 2004, data on blood glucose and daily pharmacologic management were gathered from electronic sources on 3,613 inpatients with diabetes. Inpatient hyperglycemia (glucose more than 180 mg/dL) occurred at least once in 2,980 (82.5%) hospitalizations.
Intensification of antihyperglycemic therapy occurred after only 22% of hospital days with hyperglycemia. Intensification included scheduled insulin, sliding scale insulin, and oral antihyperglycemic medications. Intensification of sliding scale insulin, as well as scheduled insulin, but not oral medications, was associated with a significant (12.2 mg/dL and 11.1 mg/dL respectively) average daily reduction in bedside glucose. Hypoglycemia was documented in 2.2% of days after intensification of antihyperglycemic treatment.
Bottom line: Inpatient hyperglycemia is common, and treatment intensification should be considered more often among hospitalized patients with diabetes.
Citation: Matheny ME, Shubina M, Kimmel ZM, Pendergrass ML, Turchin A. Treatment intensification and blood glucose control among hospitalized diabetic patients. J Gen Intern Med. 2008;23(2):184-189.
Does Four-Hour Antibiotic Goal Negatively Affect Accuracy of CAP Diagnosis?
Background: A period of less than our hour from emergency department presentation to first antibiotic dose is a core quality measure for community-acquired pneumonia (CAP). Time pressures might reduce the accuracy of pneumonia diagnosis and lead to unnecessary antibiotic administration.
Study design: Retrospective cohort.
Setting: 365-bed university-affiliated community hospital in Baltimore.
Synopsis: Patients admitted with an initial diagnosis of CAP were studied when the time to first antibiotic dose (TFAD) quality standard was eight hours (n=255) and later when the goal TFAD was four hours (n=293).
At admission, under the eight-hour goal, 45.9% of patients met prespecified diagnostic criteria for CAP, compared with 33.8% of patients under the four-hour goal (odds ratio [OR]=0.61, p=0.004). At discharge, 74.5% of patients had a diagnosis of pneumonia with an eight-hour TFAD standard, vs. 66.9% with a four-hour standard (p=0.05). The most common alternate diagnoses were acute bronchitis, heart failure, and COPD exacerbation.
No significant difference in antibiotic-associated adverse drug events, morbidity, or mortality were detected. Importantly, the goal TFAD reduction did not significantly increase the percentage of patients who received antibiotics within four hours (81.6% when the goal was within eight hours, vs. 85.3% when the goal was within four hours, p=0.21). The study is limited by its retrospective nature and the absence of gold standards for the diagnosis of CAP.
Bottom line: Greater pressure to administer antibiotics early in suspected cases of CAP may decrease diagnostic accuracy, without substantially improving antibiotic administration time.
Citation: Welker JA, Huston M, McCue JD. Antibiotic timing and errors in diagnosing pneumonia. Arch Intern Med. 2008;168(4):351-356.
Do Recruitment Maneuvers and High PEEP Reduce All-cause Hospital Mortality in Acute Lung Injury, ARDS?
Background: Low-tidal-volume ventilation reduces mortality in acute lung injury and acute respiratory distress syndrome (ARDS). Adding methods to open collapsed lung, such as employing recruitment maneuvers or using higher positive end-expiratory pressures (PEEP), may further reduce mortality.
Study design: Randomized controlled trial with blinded analysis. Patients were randomized to ventilation using the ARDS Network protocol (tidal volume of 6 ml/kg predicted body weight, assist control ventilation, low PEEP) vs. a higher PEEP intervention algorithm (using pressure control ventilation but still using 6 ml/kg tidal volume).
Setting: 30 intensive-care units in Canada, Australia, and Saudi Arabia.
Synopsis: Despite higher PEEP in the experimental group (14.6 cm H2O, SD 3.4) vs. the control group (9.8 cm H2O, SD 2.7) during the first 72 hours (p<0.001), there was no difference in all-cause hospital mortality or barotrauma between the two groups. The experimental group did, however, have a lower frequency of refractory hypoxemia (4.6% vs. 10.2%, 95% confidence interval [CI] 0.34-0.86, p=0.01).
At the end of the trial, a difference in the number of patients allocated to each group was noted. Investigation uncovered a programming error that disrupted the specified randomization blocks. Sensitivity analyses, which were not described, indicated that this error did not undermine randomization.
Bottom line: The addition of recruitment maneuvers and high PEEP to low-tidal-volume ventilation in acute lung injury and acute respiratory distress syndrome improved oxygenation but did not lower mortality.
Citation: Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome. A randomized controlled trial. JAMA 2008;299(6):637-645.
Does a Ventilation Strategy Setting PEEP to Increase Alveolar Recruitment, Limit Hyperinflation Improve 28-day Mortality in Acute Lung Injury, ARDS?
Background: The need for lung protection in patients with acute lung injury or acute respiratory distress syndrome (ARDS) is accepted. The optimal level of positive end-expiratory pressure (PEEP) to provide protection yet allow alveolar expansion is debated
Study design: Unblinded, randomized controlled trial. Patients were randomized to standard low tidal volume ventilation with low PEEP or low tidal volume ventilation with higher PEEP (intervention group). PEEP was increased in the intervention group to attain a plateau pressure of 28-30 cm H2O
Setting: 37 intensive care units in France.
Synopsis: Though PEEP, total PEEP, and plateau pressure were considerably higher in the experimental group, there was no difference in 28-day mortality compared with the control group, 27.8% vs. 31.2% (95% CI 0.90-1.40, p=0.31). There was, however, an increase in the number of ventilator-free days (seven vs. three, p=0.04) and organ-failure-free days (six vs. two, p=0.04) in the experimental group compared with the control group. Criteria were used to evaluate patients for readiness for extubation, but the differential application of PEEP between arms may have altered the timing of these evaluations in the two arms and may be at least partly responsible for the difference in ventilator-free days.
Throughout patient recruitment, the primary end point was monitored, resulting in 18 interim analyses of the data. No statistical adjustments were made for these frequent examinations of the data.
Bottom line: The use of higher PEEP and maximum plateau pressure to increase alveolar recruitment while limiting hyperinflation results in more ventilator-free and organ failure-free days in patients with acute lung injury and ARDS. These maneuvers do not, however, alter mortality.
Citation: Mercat A, Richard JCM, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome. A randomized controlled trial. JAMA 2008;299(6):646-655.
What are the Effects of N-acetylcysteine, Theophylline, Other Agents on Preventing Contrast-induced Nephropathy
Background: Contrast-induced nephropathy is the third-most common cause of new acute renal failure in hospitalized patients, occurring in up to 25% of patients with renal impairment, diabetes, heart failure, advanced age, or concurrent use of nephrotoxic drugs. Clinicians use different agents to reduce the risk, including intravenous hydration, N-acetylcysteine, theophylline, fenoldopam, dopamine, furosemide, mannitol, and bicarbonate.
Study design: Meta-analysis of randomized controlled trials.
Setting: 41 studies involving 6,379 patients, published internationally between 1994 and 2006.
Synopsis: All but one study evaluated patients undergoing cardiac catheterization, and 34 trials evaluated patients with impaired renal function. N-acetylcysteine significantly reduced the risk of contrast-induced nephropathy more than saline hydration alone (risk ratio [RR]=0.62, 95% CI 0.44 to 0.88). Theophylline may have renoprotective effects but the findings were not statistically significant (RR=0.49, 95% CI 0.23 to 1.06). Ascorbic acid and bicarbonate significantly reduced nephropathy, though only one study was found for each. The other agents evaluated did not significantly reduce risk. Furosemide increased the risk (RR=3.27, 95% CI 1.48 to 7.26).
Bottom line: N-acetylcycteine is an effective agent for prevention of contrast-induced nephropathy, and it has the added benefits of low cost, few side effects, and rare drug interactions.
Citation: Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC. Meta-analysis: effectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med. 2008;148(4):284-294.
Compared With Norepinephrine, Does Vasopressin Infusion Improve Mortality in Septic Shock Patients?
Background: Vasopressin is commonly used to support blood pressure in patients with septic shock. It has been shown to restore vascular tone, maintain blood pressure, and decrease catecholamine requirements, but its effect on mortality is uncertain.
Study design: Randomized, double-blind trial.
Setting: 27 centers in Canada, Australia, and the United States.
Synopsis: Patients with septic shock who required at least 5 mcg/min of norepinephrine were randomized to receive either low-dose vasopressin infusion (0.01 to 0.03 U/min) or norepinephrine (5 to 15 mcg/min). There was no significant difference in mortality at 28 days (35.4% for vasopressin vs. 39.3% for norepinephrine, p=0.26) or at 90 days (43.9% vs. 49.6%, p=0.11). The vasopressin group had lower heart rate and norepinephrine requirements. There were no significant differences in the frequency of adverse events.
However, since mean blood pressure at baseline was 72-73 mmHg, study patients did not necessarily have catecholamine unresponsive shock. Also, the mean time from meeting criteria for study entry to infusion of the drug was 12 hours, longer than the six-hour time period identified as important in studies of early goal-directed therapy. This may have limited the effectiveness of vasopressin infusion.
Bottom line: Low-dose vasopressin as compared with norepinephrine did not improve mortality in patients with septic shock.
Citation: Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358(9):877-887.
How Much do Hospitalized Patients Want to Participate in Decisions on Therapies of Varying Risk, Benefit?
Background: Obtaining informed consent is required for invasive procedures, but most non-invasive medical treatments are performed without discussing the risks, benefits, and alternatives with patients.
Study design: Questionnaire with four scenarios.
Setting: Medical wards in a Connecticut hospital.
Synopsis: Among the 210 patients studied, about one-fourth wanted physicians to obtain their permission “no matter what” even for mundane therapies like potassium supplementation (24%) or diuretic administration (28%). When presented with a higher risk scenario, such as thrombolysis with a greater than 20% chance of hemorrhage, 40.8% of patients definitely wanted to participate in decision-making.
Younger patients (age 65 or younger) were more likely to want to participate in decision-making. For each scenario, at least 85% of patients noted they would like to be consulted about the decision “no matter what” or if time allowed. Importantly, patients expressed these preferences in response to written scenarios that did not provide detailed information about the risks and benefits. Further, patients did not receive explanations of the logistical hurdles of trying to obtain patient input for each decision.
Bottom line: The great majority of patients in this study wished to participate in decision making for hypothetical medical treatments, especially if time allowed. At least 24% always wanted to be consulted, even about mundane therapies like potassium supplementation.
Citation: Upadhyay S, Beck A, Rishi A, Amoateng-Adjepong Y, Manthous CA. Patients’ predilections regarding informed consent for hospital treatments. J Hosp Med. 2008; 3(1):6-11.
What are the Clinical Characteristics, Treatments, and Three-month Outcomes of Patients With Upper-extremity DVT
Background: Anticoagulation is the treatment of choice for upper-extremity deep venous thrombosis (DVT). However, no large studies have characterized the nature, management, and prognosis of upper-extremity DVT.
Study design: Prospective registry of consecutive patients (RIETE registry).
Setting: International multicenter study (124 centers in Spain, France, Italy, Israel, and Argentina).
Synopsis: Among the 11,564 registry patients with acute DVT, 512 (4.4%) were noted to have upper-extremity DVT. Cancer was more common and immobility was less common with upper-extremity DVT. Initially, most patients (91%) were treated with low-molecular-weight heparin (LMWH). For long-term therapy, 75% of patients with cancer received LMWH, and 76% of patients without cancer were given oral vitamin K antagonists. At diagnosis, only 9% of patients with upper-extremity DVT had clinically apparent pulmonary embolism (PE) versus 29% of those with lower-extremity DVT. During the three-month follow-up, the incidence of PE, fatal PE, recurrent DVT, and bleeding was similar for upper- and lower-extremity DVT. Mortality was higher in patients with upper-extremity DVT, which in multivariable analyses, was explained by the higher prevalence of cancer in that group.
Bottom line: Because the incidence of recurrent DVT/PE, fatal PE, or major bleeding is similar between upper and lower extremity DVT, therapy should not differ.
Citation: Muñoz FJ, Mismetti P, Poggio R, et al. Clinical outcome of patients with upper-extremity deep vein thrombosis. Chest 2008;133(1):143-148.
Are Oral Steroids as Effective as IV Steroids in Patients With COPD Exacerbation?
Background: Oral prednisolone has near 100% bioavailability following oral administration. Although current guidelines suggest using oral steroids in the treatment of COPD exacerbation, the optimal route of administration has not been studied rigorously.
Study design: Non-inferiority, double-blinded, randomized controlled trial.
Setting: Single hospital in the Netherlands.
Synopsis: Patients were randomized to receive either a five-day course of IV or oral prednisolone 60 mg, followed by an oral prednisolone taper. All received nebulized ipratropium and albuterol four times daily, as well as oral amoxicillin/clavulanate (or doxycycline if allergic). The primary outcome was treatment failure, which included death, ICU admission, hospital readmission for COPD, or treatment intensification during 90-day follow-up.
Non-inferiority was defined as a treatment failure rate for oral steroids not more than 15% worse than the treatment failure rate for IV steroids. The study design called for 256 patients to provide adequate (80%) power for the primary analysis. However, only 210 were enrolled due to slow recruitment, and 17 withdrew consent or did not meet study entry criteria.
The intention-to-treat analysis showed no significant difference between oral and IV steroids in the treatment failure rate (56.3% vs. 61.7%, respectively). Results of the per-protocol analysis were similar. However, insufficient power and poor patient accounting raise questions about the validity of the results.
Bottom line: Oral steroids appeared no worse than IV steroids in the treatment of COPD exacerbation, but the study was underpowered, which prevents definitive conclusions.
Citation: De Jong YP, Uil SM, Grotjohan HP, et al. Oral or IV prednisolone in the treatment of COPD exacerbations. A randomized, controlled, double-blind study. Chest 2007;132(6):1741-1747. TH
Literature at a Glance
A guide to this month’s studies.
- Adverse events are common after stopping clopidogrel following acute coronary syndrome.
- Treatment intensification with insulin improves inpatient glucose control.
- Pressure for early antibiotic administration leads to inaccuracy of pneumonia diagnosis.
- Multifaceted ventilation strategy no better than low-tidal-volume protocol.
- Higher PEEP ventilation strategy reduces duration of ventilation but not mortality.
- N-acetylcysteine reduces contrast-induced nephropathy.
- Vasopressin is no better than norepinephrine in patients with septic shock.
- Hospital patients desire greater participation in decision-making.
- Outcomes of patients with upper- or lower-extremity DVT are similar.
- Oral and IV steroids may be equally effective in COPD exacerbation.
What is Frequency, Timing of Adverse Events After Stopping Clopidogrel in ACS Patients?
Background: Clopidogrel is recommended in treatment of acute coronary syndrome (ACS) with or without stent placement. A rebound hypercoagulable state may occur following clopidogrel cessation, but this has not been investigated previously.
Study design: Retrospective cohort.
Setting: 127 VA medical centers.
Synopsis: Data were collected as part of the Veterans Health Administration Cardiac Care Follow-up Clinical Study from October 2003 through March 2005 on all patients with acute myocardial infarction (MI) or unstable angina who were discharged with clopidogrel treatment (3,137 patients). The analysis assessed the incidence and timing of adverse events after stopping clopidogrel among medically treated patients and among those treated with percutaneous coronary intervention (PCI).
In adjusted analyses among medically treated patients, the risk of death or acute MI in the first 90 days after clopidogrel cessation was 1.98 times higher, compared with the interval from 91-180 days. Among patients who received PCI (usually with a bare-metal stent), the risk was 1.82 times higher in the first 90 days. The clustering of events shortly after clopidogrel cessation support the possibility of a rebound hypercoagulable state.
Bottom line: In patients with ACS who received medical management or PCI, there was a higher rate of adverse events in the first 90 days after clopidogrel cessation.
Citation: Ho PM, Peterson ED, Wang L, et al. Incidence of death and acute myocardial infarction associated with stopping clopidorel after acute coronary syndrome. JAMA 2008;299(5):532-539.
What is the Relationship Between Treatment Intensification, Blood Pressure Changes in Diabetes Patients?
Background: Hyperglycemia is common in hospitalized patients with diabetes and associated with poor outcomes. Prior research on treatment intensification has focused on the intensive care unit or outpatient setting. The effect of treatment intensification in the inpatient (non-ICU) setting is not known.
Study design: Retrospective cohort.
Setting: 734-bed teaching hospital in Boston.
Synopsis: Between January 2003 and August 2004, data on blood glucose and daily pharmacologic management were gathered from electronic sources on 3,613 inpatients with diabetes. Inpatient hyperglycemia (glucose more than 180 mg/dL) occurred at least once in 2,980 (82.5%) hospitalizations.
Intensification of antihyperglycemic therapy occurred after only 22% of hospital days with hyperglycemia. Intensification included scheduled insulin, sliding scale insulin, and oral antihyperglycemic medications. Intensification of sliding scale insulin, as well as scheduled insulin, but not oral medications, was associated with a significant (12.2 mg/dL and 11.1 mg/dL respectively) average daily reduction in bedside glucose. Hypoglycemia was documented in 2.2% of days after intensification of antihyperglycemic treatment.
Bottom line: Inpatient hyperglycemia is common, and treatment intensification should be considered more often among hospitalized patients with diabetes.
Citation: Matheny ME, Shubina M, Kimmel ZM, Pendergrass ML, Turchin A. Treatment intensification and blood glucose control among hospitalized diabetic patients. J Gen Intern Med. 2008;23(2):184-189.
Does Four-Hour Antibiotic Goal Negatively Affect Accuracy of CAP Diagnosis?
Background: A period of less than our hour from emergency department presentation to first antibiotic dose is a core quality measure for community-acquired pneumonia (CAP). Time pressures might reduce the accuracy of pneumonia diagnosis and lead to unnecessary antibiotic administration.
Study design: Retrospective cohort.
Setting: 365-bed university-affiliated community hospital in Baltimore.
Synopsis: Patients admitted with an initial diagnosis of CAP were studied when the time to first antibiotic dose (TFAD) quality standard was eight hours (n=255) and later when the goal TFAD was four hours (n=293).
At admission, under the eight-hour goal, 45.9% of patients met prespecified diagnostic criteria for CAP, compared with 33.8% of patients under the four-hour goal (odds ratio [OR]=0.61, p=0.004). At discharge, 74.5% of patients had a diagnosis of pneumonia with an eight-hour TFAD standard, vs. 66.9% with a four-hour standard (p=0.05). The most common alternate diagnoses were acute bronchitis, heart failure, and COPD exacerbation.
No significant difference in antibiotic-associated adverse drug events, morbidity, or mortality were detected. Importantly, the goal TFAD reduction did not significantly increase the percentage of patients who received antibiotics within four hours (81.6% when the goal was within eight hours, vs. 85.3% when the goal was within four hours, p=0.21). The study is limited by its retrospective nature and the absence of gold standards for the diagnosis of CAP.
Bottom line: Greater pressure to administer antibiotics early in suspected cases of CAP may decrease diagnostic accuracy, without substantially improving antibiotic administration time.
Citation: Welker JA, Huston M, McCue JD. Antibiotic timing and errors in diagnosing pneumonia. Arch Intern Med. 2008;168(4):351-356.
Do Recruitment Maneuvers and High PEEP Reduce All-cause Hospital Mortality in Acute Lung Injury, ARDS?
Background: Low-tidal-volume ventilation reduces mortality in acute lung injury and acute respiratory distress syndrome (ARDS). Adding methods to open collapsed lung, such as employing recruitment maneuvers or using higher positive end-expiratory pressures (PEEP), may further reduce mortality.
Study design: Randomized controlled trial with blinded analysis. Patients were randomized to ventilation using the ARDS Network protocol (tidal volume of 6 ml/kg predicted body weight, assist control ventilation, low PEEP) vs. a higher PEEP intervention algorithm (using pressure control ventilation but still using 6 ml/kg tidal volume).
Setting: 30 intensive-care units in Canada, Australia, and Saudi Arabia.
Synopsis: Despite higher PEEP in the experimental group (14.6 cm H2O, SD 3.4) vs. the control group (9.8 cm H2O, SD 2.7) during the first 72 hours (p<0.001), there was no difference in all-cause hospital mortality or barotrauma between the two groups. The experimental group did, however, have a lower frequency of refractory hypoxemia (4.6% vs. 10.2%, 95% confidence interval [CI] 0.34-0.86, p=0.01).
At the end of the trial, a difference in the number of patients allocated to each group was noted. Investigation uncovered a programming error that disrupted the specified randomization blocks. Sensitivity analyses, which were not described, indicated that this error did not undermine randomization.
Bottom line: The addition of recruitment maneuvers and high PEEP to low-tidal-volume ventilation in acute lung injury and acute respiratory distress syndrome improved oxygenation but did not lower mortality.
Citation: Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome. A randomized controlled trial. JAMA 2008;299(6):637-645.
Does a Ventilation Strategy Setting PEEP to Increase Alveolar Recruitment, Limit Hyperinflation Improve 28-day Mortality in Acute Lung Injury, ARDS?
Background: The need for lung protection in patients with acute lung injury or acute respiratory distress syndrome (ARDS) is accepted. The optimal level of positive end-expiratory pressure (PEEP) to provide protection yet allow alveolar expansion is debated
Study design: Unblinded, randomized controlled trial. Patients were randomized to standard low tidal volume ventilation with low PEEP or low tidal volume ventilation with higher PEEP (intervention group). PEEP was increased in the intervention group to attain a plateau pressure of 28-30 cm H2O
Setting: 37 intensive care units in France.
Synopsis: Though PEEP, total PEEP, and plateau pressure were considerably higher in the experimental group, there was no difference in 28-day mortality compared with the control group, 27.8% vs. 31.2% (95% CI 0.90-1.40, p=0.31). There was, however, an increase in the number of ventilator-free days (seven vs. three, p=0.04) and organ-failure-free days (six vs. two, p=0.04) in the experimental group compared with the control group. Criteria were used to evaluate patients for readiness for extubation, but the differential application of PEEP between arms may have altered the timing of these evaluations in the two arms and may be at least partly responsible for the difference in ventilator-free days.
Throughout patient recruitment, the primary end point was monitored, resulting in 18 interim analyses of the data. No statistical adjustments were made for these frequent examinations of the data.
Bottom line: The use of higher PEEP and maximum plateau pressure to increase alveolar recruitment while limiting hyperinflation results in more ventilator-free and organ failure-free days in patients with acute lung injury and ARDS. These maneuvers do not, however, alter mortality.
Citation: Mercat A, Richard JCM, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome. A randomized controlled trial. JAMA 2008;299(6):646-655.
What are the Effects of N-acetylcysteine, Theophylline, Other Agents on Preventing Contrast-induced Nephropathy
Background: Contrast-induced nephropathy is the third-most common cause of new acute renal failure in hospitalized patients, occurring in up to 25% of patients with renal impairment, diabetes, heart failure, advanced age, or concurrent use of nephrotoxic drugs. Clinicians use different agents to reduce the risk, including intravenous hydration, N-acetylcysteine, theophylline, fenoldopam, dopamine, furosemide, mannitol, and bicarbonate.
Study design: Meta-analysis of randomized controlled trials.
Setting: 41 studies involving 6,379 patients, published internationally between 1994 and 2006.
Synopsis: All but one study evaluated patients undergoing cardiac catheterization, and 34 trials evaluated patients with impaired renal function. N-acetylcysteine significantly reduced the risk of contrast-induced nephropathy more than saline hydration alone (risk ratio [RR]=0.62, 95% CI 0.44 to 0.88). Theophylline may have renoprotective effects but the findings were not statistically significant (RR=0.49, 95% CI 0.23 to 1.06). Ascorbic acid and bicarbonate significantly reduced nephropathy, though only one study was found for each. The other agents evaluated did not significantly reduce risk. Furosemide increased the risk (RR=3.27, 95% CI 1.48 to 7.26).
Bottom line: N-acetylcycteine is an effective agent for prevention of contrast-induced nephropathy, and it has the added benefits of low cost, few side effects, and rare drug interactions.
Citation: Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC. Meta-analysis: effectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med. 2008;148(4):284-294.
Compared With Norepinephrine, Does Vasopressin Infusion Improve Mortality in Septic Shock Patients?
Background: Vasopressin is commonly used to support blood pressure in patients with septic shock. It has been shown to restore vascular tone, maintain blood pressure, and decrease catecholamine requirements, but its effect on mortality is uncertain.
Study design: Randomized, double-blind trial.
Setting: 27 centers in Canada, Australia, and the United States.
Synopsis: Patients with septic shock who required at least 5 mcg/min of norepinephrine were randomized to receive either low-dose vasopressin infusion (0.01 to 0.03 U/min) or norepinephrine (5 to 15 mcg/min). There was no significant difference in mortality at 28 days (35.4% for vasopressin vs. 39.3% for norepinephrine, p=0.26) or at 90 days (43.9% vs. 49.6%, p=0.11). The vasopressin group had lower heart rate and norepinephrine requirements. There were no significant differences in the frequency of adverse events.
However, since mean blood pressure at baseline was 72-73 mmHg, study patients did not necessarily have catecholamine unresponsive shock. Also, the mean time from meeting criteria for study entry to infusion of the drug was 12 hours, longer than the six-hour time period identified as important in studies of early goal-directed therapy. This may have limited the effectiveness of vasopressin infusion.
Bottom line: Low-dose vasopressin as compared with norepinephrine did not improve mortality in patients with septic shock.
Citation: Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358(9):877-887.
How Much do Hospitalized Patients Want to Participate in Decisions on Therapies of Varying Risk, Benefit?
Background: Obtaining informed consent is required for invasive procedures, but most non-invasive medical treatments are performed without discussing the risks, benefits, and alternatives with patients.
Study design: Questionnaire with four scenarios.
Setting: Medical wards in a Connecticut hospital.
Synopsis: Among the 210 patients studied, about one-fourth wanted physicians to obtain their permission “no matter what” even for mundane therapies like potassium supplementation (24%) or diuretic administration (28%). When presented with a higher risk scenario, such as thrombolysis with a greater than 20% chance of hemorrhage, 40.8% of patients definitely wanted to participate in decision-making.
Younger patients (age 65 or younger) were more likely to want to participate in decision-making. For each scenario, at least 85% of patients noted they would like to be consulted about the decision “no matter what” or if time allowed. Importantly, patients expressed these preferences in response to written scenarios that did not provide detailed information about the risks and benefits. Further, patients did not receive explanations of the logistical hurdles of trying to obtain patient input for each decision.
Bottom line: The great majority of patients in this study wished to participate in decision making for hypothetical medical treatments, especially if time allowed. At least 24% always wanted to be consulted, even about mundane therapies like potassium supplementation.
Citation: Upadhyay S, Beck A, Rishi A, Amoateng-Adjepong Y, Manthous CA. Patients’ predilections regarding informed consent for hospital treatments. J Hosp Med. 2008; 3(1):6-11.
What are the Clinical Characteristics, Treatments, and Three-month Outcomes of Patients With Upper-extremity DVT
Background: Anticoagulation is the treatment of choice for upper-extremity deep venous thrombosis (DVT). However, no large studies have characterized the nature, management, and prognosis of upper-extremity DVT.
Study design: Prospective registry of consecutive patients (RIETE registry).
Setting: International multicenter study (124 centers in Spain, France, Italy, Israel, and Argentina).
Synopsis: Among the 11,564 registry patients with acute DVT, 512 (4.4%) were noted to have upper-extremity DVT. Cancer was more common and immobility was less common with upper-extremity DVT. Initially, most patients (91%) were treated with low-molecular-weight heparin (LMWH). For long-term therapy, 75% of patients with cancer received LMWH, and 76% of patients without cancer were given oral vitamin K antagonists. At diagnosis, only 9% of patients with upper-extremity DVT had clinically apparent pulmonary embolism (PE) versus 29% of those with lower-extremity DVT. During the three-month follow-up, the incidence of PE, fatal PE, recurrent DVT, and bleeding was similar for upper- and lower-extremity DVT. Mortality was higher in patients with upper-extremity DVT, which in multivariable analyses, was explained by the higher prevalence of cancer in that group.
Bottom line: Because the incidence of recurrent DVT/PE, fatal PE, or major bleeding is similar between upper and lower extremity DVT, therapy should not differ.
Citation: Muñoz FJ, Mismetti P, Poggio R, et al. Clinical outcome of patients with upper-extremity deep vein thrombosis. Chest 2008;133(1):143-148.
Are Oral Steroids as Effective as IV Steroids in Patients With COPD Exacerbation?
Background: Oral prednisolone has near 100% bioavailability following oral administration. Although current guidelines suggest using oral steroids in the treatment of COPD exacerbation, the optimal route of administration has not been studied rigorously.
Study design: Non-inferiority, double-blinded, randomized controlled trial.
Setting: Single hospital in the Netherlands.
Synopsis: Patients were randomized to receive either a five-day course of IV or oral prednisolone 60 mg, followed by an oral prednisolone taper. All received nebulized ipratropium and albuterol four times daily, as well as oral amoxicillin/clavulanate (or doxycycline if allergic). The primary outcome was treatment failure, which included death, ICU admission, hospital readmission for COPD, or treatment intensification during 90-day follow-up.
Non-inferiority was defined as a treatment failure rate for oral steroids not more than 15% worse than the treatment failure rate for IV steroids. The study design called for 256 patients to provide adequate (80%) power for the primary analysis. However, only 210 were enrolled due to slow recruitment, and 17 withdrew consent or did not meet study entry criteria.
The intention-to-treat analysis showed no significant difference between oral and IV steroids in the treatment failure rate (56.3% vs. 61.7%, respectively). Results of the per-protocol analysis were similar. However, insufficient power and poor patient accounting raise questions about the validity of the results.
Bottom line: Oral steroids appeared no worse than IV steroids in the treatment of COPD exacerbation, but the study was underpowered, which prevents definitive conclusions.
Citation: De Jong YP, Uil SM, Grotjohan HP, et al. Oral or IV prednisolone in the treatment of COPD exacerbations. A randomized, controlled, double-blind study. Chest 2007;132(6):1741-1747. TH
Literature at a Glance
A guide to this month’s studies.
- Adverse events are common after stopping clopidogrel following acute coronary syndrome.
- Treatment intensification with insulin improves inpatient glucose control.
- Pressure for early antibiotic administration leads to inaccuracy of pneumonia diagnosis.
- Multifaceted ventilation strategy no better than low-tidal-volume protocol.
- Higher PEEP ventilation strategy reduces duration of ventilation but not mortality.
- N-acetylcysteine reduces contrast-induced nephropathy.
- Vasopressin is no better than norepinephrine in patients with septic shock.
- Hospital patients desire greater participation in decision-making.
- Outcomes of patients with upper- or lower-extremity DVT are similar.
- Oral and IV steroids may be equally effective in COPD exacerbation.
What is Frequency, Timing of Adverse Events After Stopping Clopidogrel in ACS Patients?
Background: Clopidogrel is recommended in treatment of acute coronary syndrome (ACS) with or without stent placement. A rebound hypercoagulable state may occur following clopidogrel cessation, but this has not been investigated previously.
Study design: Retrospective cohort.
Setting: 127 VA medical centers.
Synopsis: Data were collected as part of the Veterans Health Administration Cardiac Care Follow-up Clinical Study from October 2003 through March 2005 on all patients with acute myocardial infarction (MI) or unstable angina who were discharged with clopidogrel treatment (3,137 patients). The analysis assessed the incidence and timing of adverse events after stopping clopidogrel among medically treated patients and among those treated with percutaneous coronary intervention (PCI).
In adjusted analyses among medically treated patients, the risk of death or acute MI in the first 90 days after clopidogrel cessation was 1.98 times higher, compared with the interval from 91-180 days. Among patients who received PCI (usually with a bare-metal stent), the risk was 1.82 times higher in the first 90 days. The clustering of events shortly after clopidogrel cessation support the possibility of a rebound hypercoagulable state.
Bottom line: In patients with ACS who received medical management or PCI, there was a higher rate of adverse events in the first 90 days after clopidogrel cessation.
Citation: Ho PM, Peterson ED, Wang L, et al. Incidence of death and acute myocardial infarction associated with stopping clopidorel after acute coronary syndrome. JAMA 2008;299(5):532-539.
What is the Relationship Between Treatment Intensification, Blood Pressure Changes in Diabetes Patients?
Background: Hyperglycemia is common in hospitalized patients with diabetes and associated with poor outcomes. Prior research on treatment intensification has focused on the intensive care unit or outpatient setting. The effect of treatment intensification in the inpatient (non-ICU) setting is not known.
Study design: Retrospective cohort.
Setting: 734-bed teaching hospital in Boston.
Synopsis: Between January 2003 and August 2004, data on blood glucose and daily pharmacologic management were gathered from electronic sources on 3,613 inpatients with diabetes. Inpatient hyperglycemia (glucose more than 180 mg/dL) occurred at least once in 2,980 (82.5%) hospitalizations.
Intensification of antihyperglycemic therapy occurred after only 22% of hospital days with hyperglycemia. Intensification included scheduled insulin, sliding scale insulin, and oral antihyperglycemic medications. Intensification of sliding scale insulin, as well as scheduled insulin, but not oral medications, was associated with a significant (12.2 mg/dL and 11.1 mg/dL respectively) average daily reduction in bedside glucose. Hypoglycemia was documented in 2.2% of days after intensification of antihyperglycemic treatment.
Bottom line: Inpatient hyperglycemia is common, and treatment intensification should be considered more often among hospitalized patients with diabetes.
Citation: Matheny ME, Shubina M, Kimmel ZM, Pendergrass ML, Turchin A. Treatment intensification and blood glucose control among hospitalized diabetic patients. J Gen Intern Med. 2008;23(2):184-189.
Does Four-Hour Antibiotic Goal Negatively Affect Accuracy of CAP Diagnosis?
Background: A period of less than our hour from emergency department presentation to first antibiotic dose is a core quality measure for community-acquired pneumonia (CAP). Time pressures might reduce the accuracy of pneumonia diagnosis and lead to unnecessary antibiotic administration.
Study design: Retrospective cohort.
Setting: 365-bed university-affiliated community hospital in Baltimore.
Synopsis: Patients admitted with an initial diagnosis of CAP were studied when the time to first antibiotic dose (TFAD) quality standard was eight hours (n=255) and later when the goal TFAD was four hours (n=293).
At admission, under the eight-hour goal, 45.9% of patients met prespecified diagnostic criteria for CAP, compared with 33.8% of patients under the four-hour goal (odds ratio [OR]=0.61, p=0.004). At discharge, 74.5% of patients had a diagnosis of pneumonia with an eight-hour TFAD standard, vs. 66.9% with a four-hour standard (p=0.05). The most common alternate diagnoses were acute bronchitis, heart failure, and COPD exacerbation.
No significant difference in antibiotic-associated adverse drug events, morbidity, or mortality were detected. Importantly, the goal TFAD reduction did not significantly increase the percentage of patients who received antibiotics within four hours (81.6% when the goal was within eight hours, vs. 85.3% when the goal was within four hours, p=0.21). The study is limited by its retrospective nature and the absence of gold standards for the diagnosis of CAP.
Bottom line: Greater pressure to administer antibiotics early in suspected cases of CAP may decrease diagnostic accuracy, without substantially improving antibiotic administration time.
Citation: Welker JA, Huston M, McCue JD. Antibiotic timing and errors in diagnosing pneumonia. Arch Intern Med. 2008;168(4):351-356.
Do Recruitment Maneuvers and High PEEP Reduce All-cause Hospital Mortality in Acute Lung Injury, ARDS?
Background: Low-tidal-volume ventilation reduces mortality in acute lung injury and acute respiratory distress syndrome (ARDS). Adding methods to open collapsed lung, such as employing recruitment maneuvers or using higher positive end-expiratory pressures (PEEP), may further reduce mortality.
Study design: Randomized controlled trial with blinded analysis. Patients were randomized to ventilation using the ARDS Network protocol (tidal volume of 6 ml/kg predicted body weight, assist control ventilation, low PEEP) vs. a higher PEEP intervention algorithm (using pressure control ventilation but still using 6 ml/kg tidal volume).
Setting: 30 intensive-care units in Canada, Australia, and Saudi Arabia.
Synopsis: Despite higher PEEP in the experimental group (14.6 cm H2O, SD 3.4) vs. the control group (9.8 cm H2O, SD 2.7) during the first 72 hours (p<0.001), there was no difference in all-cause hospital mortality or barotrauma between the two groups. The experimental group did, however, have a lower frequency of refractory hypoxemia (4.6% vs. 10.2%, 95% confidence interval [CI] 0.34-0.86, p=0.01).
At the end of the trial, a difference in the number of patients allocated to each group was noted. Investigation uncovered a programming error that disrupted the specified randomization blocks. Sensitivity analyses, which were not described, indicated that this error did not undermine randomization.
Bottom line: The addition of recruitment maneuvers and high PEEP to low-tidal-volume ventilation in acute lung injury and acute respiratory distress syndrome improved oxygenation but did not lower mortality.
Citation: Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome. A randomized controlled trial. JAMA 2008;299(6):637-645.
Does a Ventilation Strategy Setting PEEP to Increase Alveolar Recruitment, Limit Hyperinflation Improve 28-day Mortality in Acute Lung Injury, ARDS?
Background: The need for lung protection in patients with acute lung injury or acute respiratory distress syndrome (ARDS) is accepted. The optimal level of positive end-expiratory pressure (PEEP) to provide protection yet allow alveolar expansion is debated
Study design: Unblinded, randomized controlled trial. Patients were randomized to standard low tidal volume ventilation with low PEEP or low tidal volume ventilation with higher PEEP (intervention group). PEEP was increased in the intervention group to attain a plateau pressure of 28-30 cm H2O
Setting: 37 intensive care units in France.
Synopsis: Though PEEP, total PEEP, and plateau pressure were considerably higher in the experimental group, there was no difference in 28-day mortality compared with the control group, 27.8% vs. 31.2% (95% CI 0.90-1.40, p=0.31). There was, however, an increase in the number of ventilator-free days (seven vs. three, p=0.04) and organ-failure-free days (six vs. two, p=0.04) in the experimental group compared with the control group. Criteria were used to evaluate patients for readiness for extubation, but the differential application of PEEP between arms may have altered the timing of these evaluations in the two arms and may be at least partly responsible for the difference in ventilator-free days.
Throughout patient recruitment, the primary end point was monitored, resulting in 18 interim analyses of the data. No statistical adjustments were made for these frequent examinations of the data.
Bottom line: The use of higher PEEP and maximum plateau pressure to increase alveolar recruitment while limiting hyperinflation results in more ventilator-free and organ failure-free days in patients with acute lung injury and ARDS. These maneuvers do not, however, alter mortality.
Citation: Mercat A, Richard JCM, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome. A randomized controlled trial. JAMA 2008;299(6):646-655.
What are the Effects of N-acetylcysteine, Theophylline, Other Agents on Preventing Contrast-induced Nephropathy
Background: Contrast-induced nephropathy is the third-most common cause of new acute renal failure in hospitalized patients, occurring in up to 25% of patients with renal impairment, diabetes, heart failure, advanced age, or concurrent use of nephrotoxic drugs. Clinicians use different agents to reduce the risk, including intravenous hydration, N-acetylcysteine, theophylline, fenoldopam, dopamine, furosemide, mannitol, and bicarbonate.
Study design: Meta-analysis of randomized controlled trials.
Setting: 41 studies involving 6,379 patients, published internationally between 1994 and 2006.
Synopsis: All but one study evaluated patients undergoing cardiac catheterization, and 34 trials evaluated patients with impaired renal function. N-acetylcysteine significantly reduced the risk of contrast-induced nephropathy more than saline hydration alone (risk ratio [RR]=0.62, 95% CI 0.44 to 0.88). Theophylline may have renoprotective effects but the findings were not statistically significant (RR=0.49, 95% CI 0.23 to 1.06). Ascorbic acid and bicarbonate significantly reduced nephropathy, though only one study was found for each. The other agents evaluated did not significantly reduce risk. Furosemide increased the risk (RR=3.27, 95% CI 1.48 to 7.26).
Bottom line: N-acetylcycteine is an effective agent for prevention of contrast-induced nephropathy, and it has the added benefits of low cost, few side effects, and rare drug interactions.
Citation: Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC. Meta-analysis: effectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med. 2008;148(4):284-294.
Compared With Norepinephrine, Does Vasopressin Infusion Improve Mortality in Septic Shock Patients?
Background: Vasopressin is commonly used to support blood pressure in patients with septic shock. It has been shown to restore vascular tone, maintain blood pressure, and decrease catecholamine requirements, but its effect on mortality is uncertain.
Study design: Randomized, double-blind trial.
Setting: 27 centers in Canada, Australia, and the United States.
Synopsis: Patients with septic shock who required at least 5 mcg/min of norepinephrine were randomized to receive either low-dose vasopressin infusion (0.01 to 0.03 U/min) or norepinephrine (5 to 15 mcg/min). There was no significant difference in mortality at 28 days (35.4% for vasopressin vs. 39.3% for norepinephrine, p=0.26) or at 90 days (43.9% vs. 49.6%, p=0.11). The vasopressin group had lower heart rate and norepinephrine requirements. There were no significant differences in the frequency of adverse events.
However, since mean blood pressure at baseline was 72-73 mmHg, study patients did not necessarily have catecholamine unresponsive shock. Also, the mean time from meeting criteria for study entry to infusion of the drug was 12 hours, longer than the six-hour time period identified as important in studies of early goal-directed therapy. This may have limited the effectiveness of vasopressin infusion.
Bottom line: Low-dose vasopressin as compared with norepinephrine did not improve mortality in patients with septic shock.
Citation: Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358(9):877-887.
How Much do Hospitalized Patients Want to Participate in Decisions on Therapies of Varying Risk, Benefit?
Background: Obtaining informed consent is required for invasive procedures, but most non-invasive medical treatments are performed without discussing the risks, benefits, and alternatives with patients.
Study design: Questionnaire with four scenarios.
Setting: Medical wards in a Connecticut hospital.
Synopsis: Among the 210 patients studied, about one-fourth wanted physicians to obtain their permission “no matter what” even for mundane therapies like potassium supplementation (24%) or diuretic administration (28%). When presented with a higher risk scenario, such as thrombolysis with a greater than 20% chance of hemorrhage, 40.8% of patients definitely wanted to participate in decision-making.
Younger patients (age 65 or younger) were more likely to want to participate in decision-making. For each scenario, at least 85% of patients noted they would like to be consulted about the decision “no matter what” or if time allowed. Importantly, patients expressed these preferences in response to written scenarios that did not provide detailed information about the risks and benefits. Further, patients did not receive explanations of the logistical hurdles of trying to obtain patient input for each decision.
Bottom line: The great majority of patients in this study wished to participate in decision making for hypothetical medical treatments, especially if time allowed. At least 24% always wanted to be consulted, even about mundane therapies like potassium supplementation.
Citation: Upadhyay S, Beck A, Rishi A, Amoateng-Adjepong Y, Manthous CA. Patients’ predilections regarding informed consent for hospital treatments. J Hosp Med. 2008; 3(1):6-11.
What are the Clinical Characteristics, Treatments, and Three-month Outcomes of Patients With Upper-extremity DVT
Background: Anticoagulation is the treatment of choice for upper-extremity deep venous thrombosis (DVT). However, no large studies have characterized the nature, management, and prognosis of upper-extremity DVT.
Study design: Prospective registry of consecutive patients (RIETE registry).
Setting: International multicenter study (124 centers in Spain, France, Italy, Israel, and Argentina).
Synopsis: Among the 11,564 registry patients with acute DVT, 512 (4.4%) were noted to have upper-extremity DVT. Cancer was more common and immobility was less common with upper-extremity DVT. Initially, most patients (91%) were treated with low-molecular-weight heparin (LMWH). For long-term therapy, 75% of patients with cancer received LMWH, and 76% of patients without cancer were given oral vitamin K antagonists. At diagnosis, only 9% of patients with upper-extremity DVT had clinically apparent pulmonary embolism (PE) versus 29% of those with lower-extremity DVT. During the three-month follow-up, the incidence of PE, fatal PE, recurrent DVT, and bleeding was similar for upper- and lower-extremity DVT. Mortality was higher in patients with upper-extremity DVT, which in multivariable analyses, was explained by the higher prevalence of cancer in that group.
Bottom line: Because the incidence of recurrent DVT/PE, fatal PE, or major bleeding is similar between upper and lower extremity DVT, therapy should not differ.
Citation: Muñoz FJ, Mismetti P, Poggio R, et al. Clinical outcome of patients with upper-extremity deep vein thrombosis. Chest 2008;133(1):143-148.
Are Oral Steroids as Effective as IV Steroids in Patients With COPD Exacerbation?
Background: Oral prednisolone has near 100% bioavailability following oral administration. Although current guidelines suggest using oral steroids in the treatment of COPD exacerbation, the optimal route of administration has not been studied rigorously.
Study design: Non-inferiority, double-blinded, randomized controlled trial.
Setting: Single hospital in the Netherlands.
Synopsis: Patients were randomized to receive either a five-day course of IV or oral prednisolone 60 mg, followed by an oral prednisolone taper. All received nebulized ipratropium and albuterol four times daily, as well as oral amoxicillin/clavulanate (or doxycycline if allergic). The primary outcome was treatment failure, which included death, ICU admission, hospital readmission for COPD, or treatment intensification during 90-day follow-up.
Non-inferiority was defined as a treatment failure rate for oral steroids not more than 15% worse than the treatment failure rate for IV steroids. The study design called for 256 patients to provide adequate (80%) power for the primary analysis. However, only 210 were enrolled due to slow recruitment, and 17 withdrew consent or did not meet study entry criteria.
The intention-to-treat analysis showed no significant difference between oral and IV steroids in the treatment failure rate (56.3% vs. 61.7%, respectively). Results of the per-protocol analysis were similar. However, insufficient power and poor patient accounting raise questions about the validity of the results.
Bottom line: Oral steroids appeared no worse than IV steroids in the treatment of COPD exacerbation, but the study was underpowered, which prevents definitive conclusions.
Citation: De Jong YP, Uil SM, Grotjohan HP, et al. Oral or IV prednisolone in the treatment of COPD exacerbations. A randomized, controlled, double-blind study. Chest 2007;132(6):1741-1747. TH