User login
Losing a patient to suicide: Navigating the aftermath
At some point during their career, many mental health professionals will lose a patient to suicide, but few will be prepared for the experience and its aftermath. As I described in Part 1 of this article (
A chance for growth
Traumatic experiences such as a suicide loss can paradoxically present a multitude of opportunities for new growth and profound personal transformation.1 Such transformation is primarily fostered by social support in the aftermath of the trauma.2
Virtually all of the models of the clinician’s suicide grief trajectory I described in Part 1 not only assume the eventual resolution of the distressing reactions accompanying the original loss, but also suggest that mastery of these reactions can be a catalyst for both personal and professional growth. Clearly, not everyone who experiences such a loss will experience subsequent growth; there are many reports of clinicians leaving the field3 or becoming “burned out” after this occurs. Yet most clinicians who have described this loss in the literature and in discussion groups (including those I’ve conducted) have reported more positive eventual outcomes. It is difficult to establish whether this is due to a cohort effect—clinicians who are most likely to write about their experiences, be interviewed for research studies, and/or to seek out and participate in discussion/support groups may be more prone to find benefits in this experience, either by virtue of their nature or through the subsequent process of sharing these experiences in a supportive atmosphere.
The literature on patient suicide loss, as well as anecdotal reports, confirms that clinicians who experience optimal support are able to identify many retrospective benefits of their experience.4-6 Clinicians generally report that they are better able to identify potential risk and protective factors for suicide, and are more knowledgeable about optimal interventions with individuals who are suicidal. They also describe an increased sensitivity towards patients who are suicidal and those bereaved by suicide. In addition, clinicians report a reduction in therapeutic grandiosity/omnipotence, and more realistic appraisals and expectations in relation to their clinical competence. In their effort to understand the “whys” of their patient’s suicide, they are likely to retrospectively identify errors in treatment, “missed cues,” or things they might subsequently do differently,7 and to learn from these mistakes. Optimally, clinicians become more aware of their own therapeutic limitations, both in the short- and the long-term, and can use this knowledge to better determine how they will continue their clinical work. They also become much more aware of the issues involved in the aftermath of a patient suicide, including perceived gaps in the clinical and institutional systems that could optimally offer support to families and clinicians.
In addition to the positive changes related to knowledge and clinical skills, many clinicians also note deeper personal changes subsequent to their patient’s suicide, consistent with the literature on posttraumatic growth.1 Munson8 explored internal changes in clinicians following a patient suicide and found that in the aftermath, clinicians experienced both posttraumatic growth and compassion fatigue. He also found that the amount of time that elapsed since the patient’s suicide predicted posttraumatic growth, and the seemingly counterintuitive result that the number of years of clinical experience prior to the suicide was negatively correlated with posttraumatic growth.
Huhra et al4 described some of the existential issues that a clinician is likely to confront following a patient suicide. A clinician’s attempt to find a way to meaningfully understand the circumstances around this loss often prompts reflection on mortality, freedom, choice and personal autonomy, and the scope and limits of one’s responsibility toward others. The suicide challenges one’s previous conceptions and expectations around these professional issues, and the clinician must construct new paradigms that serve to integrate these new experiences and perspectives in a coherent way.
One of the most notable sequelae of this (and to other traumatic) experience is a subsequent desire to make use of the learning inherent in these experiences and to “give back.” Once they feel that they have resolved their own grief process, many clinicians express the desire to support others with similar experiences. Even when their experiences have been quite distressing, many clinicians are able to view the suicide as an opportunity to learn about ongoing limitations in the systems of support, and to work toward changing these in a way that ensures that future clinician-survivors will have more supportive experiences. Many view these new perspectives, and their consequent ability to be more helpful, as “unexpected gifts.” They often express gratitude toward the people and resources that have allowed them to make these transformations. Jones5 noted “the tragedy of patient suicide can also be an opportunity for us as therapists to grow in our skills at assessing and intervening in a suicidal crisis, to broaden and deepen the support we give and receive, to grow in our appreciation of the precious gift that life is, and to help each other live it more fully.”
Continue to: Guidelines for postvention
Guidelines for postvention
When a patient suicide occurs in the context of an agency setting, Grad9 recommends prompt responses on 4 levels:
- administrative
- institutional
- educational
- emotional.
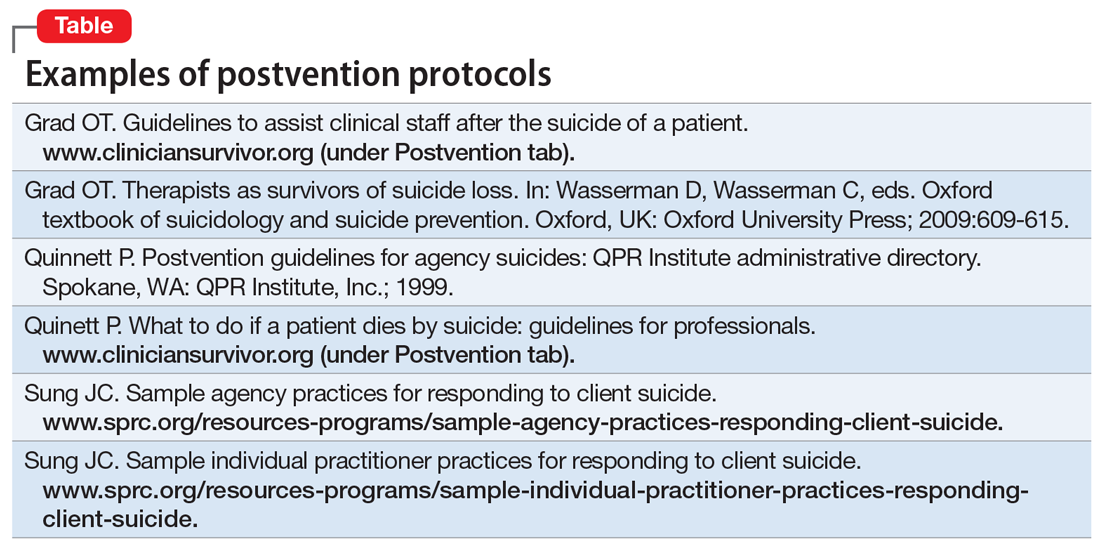
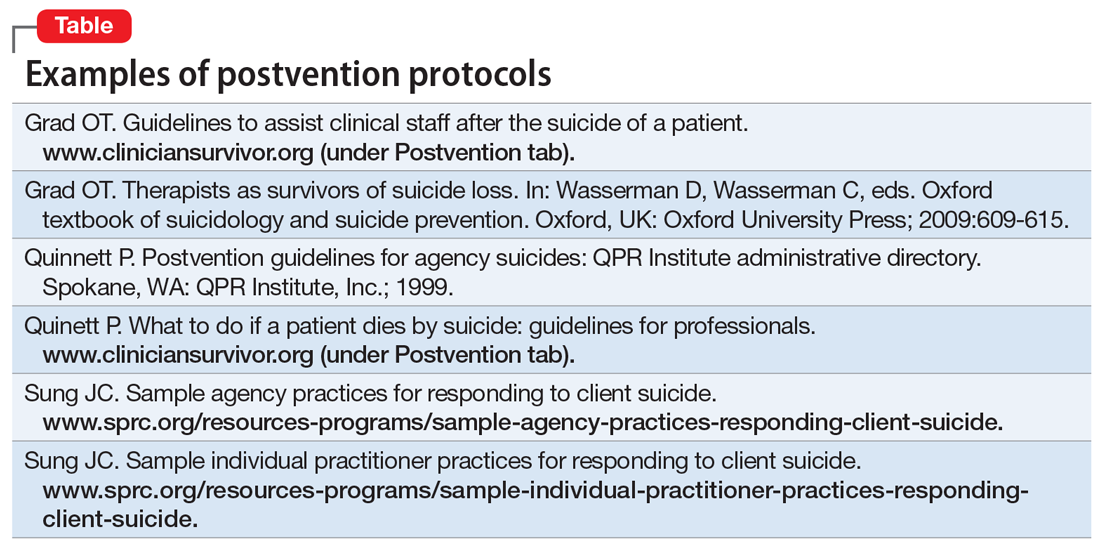
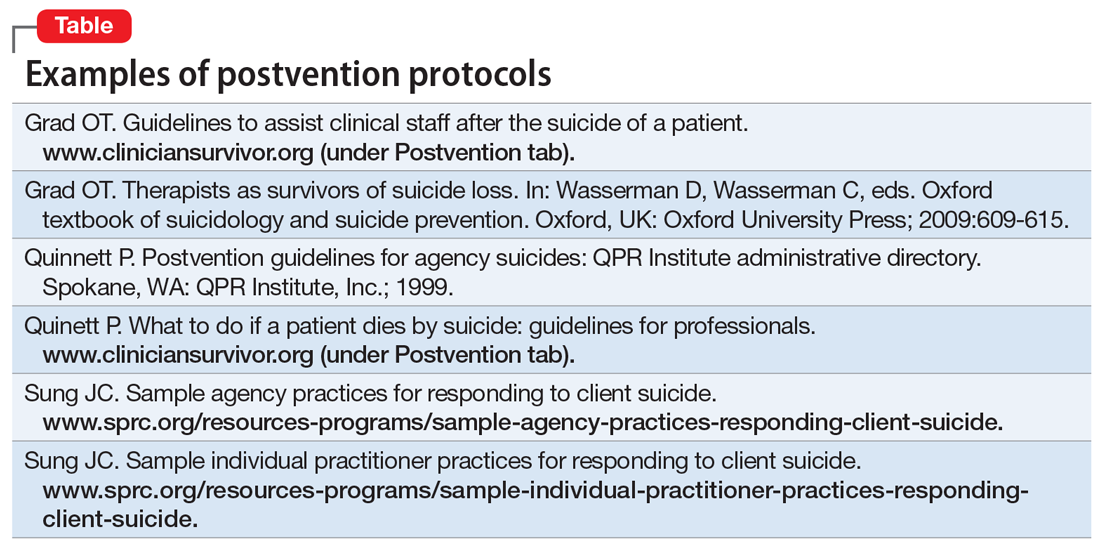
Numerous authors5,10-21 have developed suggestions, guidelines, and detailed postvention protocols to help agencies and clinicians in various mental health settings navigate the often-complicated sequelae to a patient’s suicide. The Table highlights a few of these. Most emphasize that information about suicide loss, including both its statistical likelihood and its potential aftermath, should integrated into clinicians’ general education and training. They also suggest that suicide postvention policies and protocols be in place from the outset, and that such information be incorporated into institutional policy and procedure manuals. In addition, they stress that legal, institutional, and administrative needs be balanced with the emotional needs of affected clinicians and staff, as well as those of the surviving family.
Institutional and administrative procedures
The following are some of the recommended procedures that should take place following a suicide loss. The postvention protocols listed in the Table provide more detailed recommendations.
Legal/ethical. It is essential to consult with a legal representative/risk management specialist associated with the affected agency (ideally, one with specific expertise in suicide litigation.). It is also crucial to clarify who holds privilege after a patient’s death (varies by state), what may and may not be shared under the restrictions of confidentiality and Health Insurance Portability and Accountability Act (HIPAA) laws, and to clarify procedures for chart completion and review. It is also important to clarify the specific information to be shared both within and outside of the agency, and how to address the needs of current patients in the agency settings.
Case review. The optimal purpose of the case review (also known as a psychological autopsy) is to facilitate learning, identify gaps in agency procedures and training, improve pre- and postvention procedures, and help clinicians cope with the loss.22 Again, the legal and administrative needs of the agency need to be balanced with the attention to the emotional impact on the treating clinician.17 Ellis and Patel18 recommend delaying this procedure until the treating clinician is no longer in the “shock” phase of the loss, and is able to think and process events more objectively.
Continue to: Family contact
Family contact. Most authors have recommended that clinicians and/or agencies reach out to surviving families. Although some legal representatives will advise against this, experts in the field of suicide litigation have noted that compassionate family contact reduces liability and facilitates healing for both parties. In a personal communication (May 2008), Eric Harris, of the American Psychological Association Trust, recommended “compassion over caution” when considering these issues. Again, it is important to clarify who holds privilege after a patient’s death in determining when and with whom the patient’s confidential information may be shared. When confidentiality may be broken, clinical judgment should be used to determine how best to present the information to grieving family members.
Even if surviving family members do not hold privilege, there are many things that clinicians can do to be helpful.23 Inevitably, families will want any information that will help them make sense of the loss, and general psychoeducation about mental illness and suicide can be helpful in this regard. In addition, providing information about “Survivors After Suicide” support groups, reading materials, etc., can be helpful. Both support groups and survivor-related bibliographies are available on the web sites of the American Association of Suicidology (www.suicidology.org) and The American Foundation for Suicide Prevention (www.afsp.org).
In addition, clinicians should ask the family if it would be helpful if they were to attend the funeral/memorial services, and how to introduce themselves if asked by other attendees.
Patients in clinics/hospitals. When a patient suicide occurs in a clinic or hospital setting, it is likely to impact other patients in that setting to the extent that they have heard, about the event, even from outside sources.According to Hodgkinson,24 in addition to being overwhelmed with intense feelings about the suicide loss (particularly if they had known the patient), affected patients are likely to be at increased risk for suicidal behaviors. This is consistent with the considerable literature on suicide contagion.
Thus, it is important to clarify information to be shared with patients; however, avoid describing details of the method, because this can foster contagion and “copycat” suicides. In addition, Kaye and Soreff22 noted that these patients may now be concerned about the staff’s ability to be helpful to them, because they were unable to help the deceased. In light of this, take extra care to attend to the impact of the suicide on current patients, and to monitor both pre-existing and new suicidality.
Continue to: Helping affected clinicians
Helping affected clinicians
Suggestions for optimally supporting affected clinicians include:
- clear communication about the nature of upcoming administrative procedures (including chart and institutional reviews)
- consultation from supervisors and/or colleagues that is supportive and reassuring, rather than blaming
- opportunities for the clinician to talk openly about the experience of the loss, either individually or in group settings, without fear of judgment or censure
- recognition that the loss is likely to impact clinical work, support in monitoring this impact, and the provision of medical leaves and/or modified caseloads (ie, fewer high-risk patients) as necessary.
Box 1
Frank Jones and Judy Meade founded the Clinical Survivor Task Force (CSTF) of the American Association of Suicidology (AAS) in 1987. As Jones noted, “clinicians who have lost patients to suicide need a place to acknowledge and carry forward their personal loss…to benefit both personally and professionally from the opportunity to talk with other therapists who have survived the loss of a patient through suicide.”7 Nina Gutin, PhD, and Vanessa McGann, PhD, have co-chaired the CSTF since 2003. It supports clinicians who have lost patients and/or loved ones, with the recognition that both types of losses carry implications within clinical and professional domains. The CSTF provides a listserve, opportunities to participate in video support groups, and a web site (www.cliniciansurvivor.org) that provides information about the clinician-survivor experience, the opportunity to read and post narratives about one’s experience with suicide loss, an updated bibliography maintained by John McIntosh, PhD, a list of clinical contacts, and links to several excellent postvention protocols. In addition, Drs. Gutin and McGann conduct clinician-survivor support activities at the annual AAS conference, and in their respective geographic areas.
Both researchers and clinician-survivors in my practice and support groups have noted that speaking with other clinicians who have experienced suicide loss can be particularly reassuring and validating. If none are available on staff, the listserve and online support groups of the American Association of Suicidology’s Clinician Survivor Task Force may be helpful (Box 17). In addition, the film “Collateral Damages: The Impact of Patient Suicide on the Physician” features physicians describing their experience of losing a patient to suicide (Box 2).
Box 2
“Collateral Damages: The Impact of Patient Suicide on the Physician” is a film that features several physicians speaking about their experience of losing a patient to suicide, as well as a group discussion. Psychiatrists in this educational film include Drs. Glen Gabbard, Sidney Zisook, and Jim Lomax. This resource can be used to facilitate an educational session for physicians, psychologists, residents, or other trainees. Please contact education@afsp.org to request a DVD of this film and a copy of a related article, Prabhakar D, Anzia JM, Balon R, et al. “Collateral damages”: preparing residents for coping with patient suicide. Acad Psychiatry. 2013;37(6):429-430.
Schultz14 offered suggestions for staff in supervisory positions, noting that they may bear at least some clinical and legal responsibility for the treatments that they supervise. She encouraged supervisors to take an active stance in advocating for trainees, to encourage colleagues to express their support, and to discourage rumors and other stigmatizing reactions. Schultz also urges supervisors to14:
- allow extra time for the clinician to engage in the normative exploration of the “whys” that are unique to suicide survivors
- use education about suicide to help the clinician gain a more realistic perspective on their relative culpability
- become aware of and provide education about normative grief reactions following a suicide.
Continue to: Because a suicide loss...
Because a suicide loss is likely to affect a clinician’s subsequent clinical activity, Schultz encourages supervisors to help clinicians monitor this impact on their work.14
A supportive environment is key
Losing a patient to suicide is a complicated, potentially traumatic process that many mental health clinicians will face. Yet with comprehensive and supportive postvention policies in place, clinicians who are impacted are more likely to experience healing and posttraumatic growth in both personal and professional domains.
Bottom Line
Although often traumatic, losing a patient to suicide presents clinicians with an opportunity for personal and professional growth. Following established postvention protocols can help ensure that legal, institutional, and administrative needs are balanced with the emotional needs of affected clinicians and staff, as well as those of the surviving family.
Related Resources
- American Association of Suicidology Clinician Survivor Task Force. www.cliniciansurvivor.org.
- Dotinga R. Coping when a patient commits suicide. July 21, 2017. www.mdedge.com/psychiatry/article/142975/depression/coping-when-patient-commits-suicide.
- Gutin N. Losing a patent to suicide: What we know. Part 1. 2019;18(10):14-16,19-22,30-32.
1. Tedeschi RG, Calhoun LG. Beyond the concept of recovery: Growth and the experience of loss. Death Stud. 2008;32(1):27-39.
2. Fuentes MA, Cruz D. Posttraumatic growth: positive psychological changes after trauma. Mental Health News. 2009;11(1):31,37.
3. Gitlin M. Aftermath of a tragedy: reaction of psychiatrists to patient suicides. Psychiatr Ann. 2007;37(10):684-687.
4. Huhra R, Hunka N, Rogers J, et al. Finding meaning: theoretical perspectives on patient suicide. Paper presented at: 2004 Annual Conference of the American Association of Suicidology; April 2004; Miami, FL.
5. Jones FA Jr. Therapists as survivors of patient suicide. In: Dunne EJ, McIntosh JL, Dunne-Maxim K, eds. Suicide and its aftermath: understanding and counseling the survivors. New York, NY: W.W. Norton; 1987;126-141.
6. Gutin N, McGann VM, Jordan JR. The impact of suicide on professional caregivers. In: Jordan J, McIntosh J, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge; 2011:93-111.
7. Hendin H, Lipschitz A, Maltsberger JT, et al. Therapists’ reactions to patients’ suicides. Am J Psychiatry. 2000;157(12):2022-2027.
8. Munson JS. Impact of client suicide on practitioner posttraumatic growth [dissertation]. Gainesville, Florida: University of Florida; 2009.
9. Grad OT. Therapists as survivors of suicide loss. In: Wasserman D, Wasserman C, eds. Oxford textbook of suicidology and suicide prevention. Oxford, UK: Oxford University Press; 2009:609-615.
10. Douglas J, Brown HN. Suicide: understanding and responding: Harvard Medical School perspectives. Madison, CT: International Universities Press; 1989.
11. Farberow NL. The mental health professional as suicide survivor. Clin Neuropsychiatry. 2005;2(1):13-20.
12. Plakun EM, Tillman JG. Responding to clinicians after loss of a patient to suicide. Dir Psychiatry. 2005;25:301-310.
13. Quinnett P. QPR: for suicide prevention. QPR Institute, Inc. www.cliniciansurvivor.org (under Postvention tab). Published September 21, 2009. Accessed August 26, 2019.
14. Schultz, D. Suggestions for supervisors when a therapist experiences a client’s suicide. Women Ther. 2005;28(1):59-69.
15. Spiegelman JS Jr, Werth JL Jr. Don’t forget about me: the experiences of therapists-in-training after a patient has attempted or died by suicide. Women Ther. 2005;28(1):35-57.
16. American Association of Suicidology. Clinician Survivor Task Force. Clinicians as survivors of suicide: postvention information. http://cliniciansurvivor.org. Published May 16, 2016. Accessed January 13, 2019.
17. Whitmore CA, Cook J, Salg L. Supporting residents in the wake of patient suicide. The American Journal of Psychiatry Residents’ Journal. 2017;12(1):5-7.
18. Ellis TE, Patel AB. Client suicide: what now? Cogn Behav Pract. 2012;19(2):277-287.
19. Figueroa S, Dalack GW. Exploring the impact of suicide on clinicians: a multidisciplinary retreat model. J Psychiatr Pract. 2013;19(1):72-77.
20. Lerner U, Brooks, K, McNeil DE, et al. Coping with a patient’s suicide: a curriculum for psychiatry residency training programs. Acad Psychiatry. 2012;36(1):29-33.
21. Prabhakar D, Balon R, Anzia J, et al. Helping psychiatry residents cope with patient suicide. Acad Psychiatry. 2014;38(5):593-597.
22. Kaye NS, Soreff SM. The psychiatrist’s role, responses, and responsibilities when a patient commits suicide. Am J Psychiatry. 1991;148(6):739-743.
23. McGann VL, Gutin N, Jordan JR. Guidelines for postvention care with survivor families after the suicide of a client. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge; 2011:133-155.
24. Hodgkinson PE. Responding to in-patient suicide. Br J Med Psychol. 1987;60(4):387-392.
At some point during their career, many mental health professionals will lose a patient to suicide, but few will be prepared for the experience and its aftermath. As I described in Part 1 of this article (
A chance for growth
Traumatic experiences such as a suicide loss can paradoxically present a multitude of opportunities for new growth and profound personal transformation.1 Such transformation is primarily fostered by social support in the aftermath of the trauma.2
Virtually all of the models of the clinician’s suicide grief trajectory I described in Part 1 not only assume the eventual resolution of the distressing reactions accompanying the original loss, but also suggest that mastery of these reactions can be a catalyst for both personal and professional growth. Clearly, not everyone who experiences such a loss will experience subsequent growth; there are many reports of clinicians leaving the field3 or becoming “burned out” after this occurs. Yet most clinicians who have described this loss in the literature and in discussion groups (including those I’ve conducted) have reported more positive eventual outcomes. It is difficult to establish whether this is due to a cohort effect—clinicians who are most likely to write about their experiences, be interviewed for research studies, and/or to seek out and participate in discussion/support groups may be more prone to find benefits in this experience, either by virtue of their nature or through the subsequent process of sharing these experiences in a supportive atmosphere.
The literature on patient suicide loss, as well as anecdotal reports, confirms that clinicians who experience optimal support are able to identify many retrospective benefits of their experience.4-6 Clinicians generally report that they are better able to identify potential risk and protective factors for suicide, and are more knowledgeable about optimal interventions with individuals who are suicidal. They also describe an increased sensitivity towards patients who are suicidal and those bereaved by suicide. In addition, clinicians report a reduction in therapeutic grandiosity/omnipotence, and more realistic appraisals and expectations in relation to their clinical competence. In their effort to understand the “whys” of their patient’s suicide, they are likely to retrospectively identify errors in treatment, “missed cues,” or things they might subsequently do differently,7 and to learn from these mistakes. Optimally, clinicians become more aware of their own therapeutic limitations, both in the short- and the long-term, and can use this knowledge to better determine how they will continue their clinical work. They also become much more aware of the issues involved in the aftermath of a patient suicide, including perceived gaps in the clinical and institutional systems that could optimally offer support to families and clinicians.
In addition to the positive changes related to knowledge and clinical skills, many clinicians also note deeper personal changes subsequent to their patient’s suicide, consistent with the literature on posttraumatic growth.1 Munson8 explored internal changes in clinicians following a patient suicide and found that in the aftermath, clinicians experienced both posttraumatic growth and compassion fatigue. He also found that the amount of time that elapsed since the patient’s suicide predicted posttraumatic growth, and the seemingly counterintuitive result that the number of years of clinical experience prior to the suicide was negatively correlated with posttraumatic growth.
Huhra et al4 described some of the existential issues that a clinician is likely to confront following a patient suicide. A clinician’s attempt to find a way to meaningfully understand the circumstances around this loss often prompts reflection on mortality, freedom, choice and personal autonomy, and the scope and limits of one’s responsibility toward others. The suicide challenges one’s previous conceptions and expectations around these professional issues, and the clinician must construct new paradigms that serve to integrate these new experiences and perspectives in a coherent way.
One of the most notable sequelae of this (and to other traumatic) experience is a subsequent desire to make use of the learning inherent in these experiences and to “give back.” Once they feel that they have resolved their own grief process, many clinicians express the desire to support others with similar experiences. Even when their experiences have been quite distressing, many clinicians are able to view the suicide as an opportunity to learn about ongoing limitations in the systems of support, and to work toward changing these in a way that ensures that future clinician-survivors will have more supportive experiences. Many view these new perspectives, and their consequent ability to be more helpful, as “unexpected gifts.” They often express gratitude toward the people and resources that have allowed them to make these transformations. Jones5 noted “the tragedy of patient suicide can also be an opportunity for us as therapists to grow in our skills at assessing and intervening in a suicidal crisis, to broaden and deepen the support we give and receive, to grow in our appreciation of the precious gift that life is, and to help each other live it more fully.”
Continue to: Guidelines for postvention
Guidelines for postvention
When a patient suicide occurs in the context of an agency setting, Grad9 recommends prompt responses on 4 levels:
- administrative
- institutional
- educational
- emotional.
Numerous authors5,10-21 have developed suggestions, guidelines, and detailed postvention protocols to help agencies and clinicians in various mental health settings navigate the often-complicated sequelae to a patient’s suicide. The Table highlights a few of these. Most emphasize that information about suicide loss, including both its statistical likelihood and its potential aftermath, should integrated into clinicians’ general education and training. They also suggest that suicide postvention policies and protocols be in place from the outset, and that such information be incorporated into institutional policy and procedure manuals. In addition, they stress that legal, institutional, and administrative needs be balanced with the emotional needs of affected clinicians and staff, as well as those of the surviving family.
Institutional and administrative procedures
The following are some of the recommended procedures that should take place following a suicide loss. The postvention protocols listed in the Table provide more detailed recommendations.
Legal/ethical. It is essential to consult with a legal representative/risk management specialist associated with the affected agency (ideally, one with specific expertise in suicide litigation.). It is also crucial to clarify who holds privilege after a patient’s death (varies by state), what may and may not be shared under the restrictions of confidentiality and Health Insurance Portability and Accountability Act (HIPAA) laws, and to clarify procedures for chart completion and review. It is also important to clarify the specific information to be shared both within and outside of the agency, and how to address the needs of current patients in the agency settings.
Case review. The optimal purpose of the case review (also known as a psychological autopsy) is to facilitate learning, identify gaps in agency procedures and training, improve pre- and postvention procedures, and help clinicians cope with the loss.22 Again, the legal and administrative needs of the agency need to be balanced with the attention to the emotional impact on the treating clinician.17 Ellis and Patel18 recommend delaying this procedure until the treating clinician is no longer in the “shock” phase of the loss, and is able to think and process events more objectively.
Continue to: Family contact
Family contact. Most authors have recommended that clinicians and/or agencies reach out to surviving families. Although some legal representatives will advise against this, experts in the field of suicide litigation have noted that compassionate family contact reduces liability and facilitates healing for both parties. In a personal communication (May 2008), Eric Harris, of the American Psychological Association Trust, recommended “compassion over caution” when considering these issues. Again, it is important to clarify who holds privilege after a patient’s death in determining when and with whom the patient’s confidential information may be shared. When confidentiality may be broken, clinical judgment should be used to determine how best to present the information to grieving family members.
Even if surviving family members do not hold privilege, there are many things that clinicians can do to be helpful.23 Inevitably, families will want any information that will help them make sense of the loss, and general psychoeducation about mental illness and suicide can be helpful in this regard. In addition, providing information about “Survivors After Suicide” support groups, reading materials, etc., can be helpful. Both support groups and survivor-related bibliographies are available on the web sites of the American Association of Suicidology (www.suicidology.org) and The American Foundation for Suicide Prevention (www.afsp.org).
In addition, clinicians should ask the family if it would be helpful if they were to attend the funeral/memorial services, and how to introduce themselves if asked by other attendees.
Patients in clinics/hospitals. When a patient suicide occurs in a clinic or hospital setting, it is likely to impact other patients in that setting to the extent that they have heard, about the event, even from outside sources.According to Hodgkinson,24 in addition to being overwhelmed with intense feelings about the suicide loss (particularly if they had known the patient), affected patients are likely to be at increased risk for suicidal behaviors. This is consistent with the considerable literature on suicide contagion.
Thus, it is important to clarify information to be shared with patients; however, avoid describing details of the method, because this can foster contagion and “copycat” suicides. In addition, Kaye and Soreff22 noted that these patients may now be concerned about the staff’s ability to be helpful to them, because they were unable to help the deceased. In light of this, take extra care to attend to the impact of the suicide on current patients, and to monitor both pre-existing and new suicidality.
Continue to: Helping affected clinicians
Helping affected clinicians
Suggestions for optimally supporting affected clinicians include:
- clear communication about the nature of upcoming administrative procedures (including chart and institutional reviews)
- consultation from supervisors and/or colleagues that is supportive and reassuring, rather than blaming
- opportunities for the clinician to talk openly about the experience of the loss, either individually or in group settings, without fear of judgment or censure
- recognition that the loss is likely to impact clinical work, support in monitoring this impact, and the provision of medical leaves and/or modified caseloads (ie, fewer high-risk patients) as necessary.
Box 1
Frank Jones and Judy Meade founded the Clinical Survivor Task Force (CSTF) of the American Association of Suicidology (AAS) in 1987. As Jones noted, “clinicians who have lost patients to suicide need a place to acknowledge and carry forward their personal loss…to benefit both personally and professionally from the opportunity to talk with other therapists who have survived the loss of a patient through suicide.”7 Nina Gutin, PhD, and Vanessa McGann, PhD, have co-chaired the CSTF since 2003. It supports clinicians who have lost patients and/or loved ones, with the recognition that both types of losses carry implications within clinical and professional domains. The CSTF provides a listserve, opportunities to participate in video support groups, and a web site (www.cliniciansurvivor.org) that provides information about the clinician-survivor experience, the opportunity to read and post narratives about one’s experience with suicide loss, an updated bibliography maintained by John McIntosh, PhD, a list of clinical contacts, and links to several excellent postvention protocols. In addition, Drs. Gutin and McGann conduct clinician-survivor support activities at the annual AAS conference, and in their respective geographic areas.
Both researchers and clinician-survivors in my practice and support groups have noted that speaking with other clinicians who have experienced suicide loss can be particularly reassuring and validating. If none are available on staff, the listserve and online support groups of the American Association of Suicidology’s Clinician Survivor Task Force may be helpful (Box 17). In addition, the film “Collateral Damages: The Impact of Patient Suicide on the Physician” features physicians describing their experience of losing a patient to suicide (Box 2).
Box 2
“Collateral Damages: The Impact of Patient Suicide on the Physician” is a film that features several physicians speaking about their experience of losing a patient to suicide, as well as a group discussion. Psychiatrists in this educational film include Drs. Glen Gabbard, Sidney Zisook, and Jim Lomax. This resource can be used to facilitate an educational session for physicians, psychologists, residents, or other trainees. Please contact education@afsp.org to request a DVD of this film and a copy of a related article, Prabhakar D, Anzia JM, Balon R, et al. “Collateral damages”: preparing residents for coping with patient suicide. Acad Psychiatry. 2013;37(6):429-430.
Schultz14 offered suggestions for staff in supervisory positions, noting that they may bear at least some clinical and legal responsibility for the treatments that they supervise. She encouraged supervisors to take an active stance in advocating for trainees, to encourage colleagues to express their support, and to discourage rumors and other stigmatizing reactions. Schultz also urges supervisors to14:
- allow extra time for the clinician to engage in the normative exploration of the “whys” that are unique to suicide survivors
- use education about suicide to help the clinician gain a more realistic perspective on their relative culpability
- become aware of and provide education about normative grief reactions following a suicide.
Continue to: Because a suicide loss...
Because a suicide loss is likely to affect a clinician’s subsequent clinical activity, Schultz encourages supervisors to help clinicians monitor this impact on their work.14
A supportive environment is key
Losing a patient to suicide is a complicated, potentially traumatic process that many mental health clinicians will face. Yet with comprehensive and supportive postvention policies in place, clinicians who are impacted are more likely to experience healing and posttraumatic growth in both personal and professional domains.
Bottom Line
Although often traumatic, losing a patient to suicide presents clinicians with an opportunity for personal and professional growth. Following established postvention protocols can help ensure that legal, institutional, and administrative needs are balanced with the emotional needs of affected clinicians and staff, as well as those of the surviving family.
Related Resources
- American Association of Suicidology Clinician Survivor Task Force. www.cliniciansurvivor.org.
- Dotinga R. Coping when a patient commits suicide. July 21, 2017. www.mdedge.com/psychiatry/article/142975/depression/coping-when-patient-commits-suicide.
- Gutin N. Losing a patent to suicide: What we know. Part 1. 2019;18(10):14-16,19-22,30-32.
At some point during their career, many mental health professionals will lose a patient to suicide, but few will be prepared for the experience and its aftermath. As I described in Part 1 of this article (
A chance for growth
Traumatic experiences such as a suicide loss can paradoxically present a multitude of opportunities for new growth and profound personal transformation.1 Such transformation is primarily fostered by social support in the aftermath of the trauma.2
Virtually all of the models of the clinician’s suicide grief trajectory I described in Part 1 not only assume the eventual resolution of the distressing reactions accompanying the original loss, but also suggest that mastery of these reactions can be a catalyst for both personal and professional growth. Clearly, not everyone who experiences such a loss will experience subsequent growth; there are many reports of clinicians leaving the field3 or becoming “burned out” after this occurs. Yet most clinicians who have described this loss in the literature and in discussion groups (including those I’ve conducted) have reported more positive eventual outcomes. It is difficult to establish whether this is due to a cohort effect—clinicians who are most likely to write about their experiences, be interviewed for research studies, and/or to seek out and participate in discussion/support groups may be more prone to find benefits in this experience, either by virtue of their nature or through the subsequent process of sharing these experiences in a supportive atmosphere.
The literature on patient suicide loss, as well as anecdotal reports, confirms that clinicians who experience optimal support are able to identify many retrospective benefits of their experience.4-6 Clinicians generally report that they are better able to identify potential risk and protective factors for suicide, and are more knowledgeable about optimal interventions with individuals who are suicidal. They also describe an increased sensitivity towards patients who are suicidal and those bereaved by suicide. In addition, clinicians report a reduction in therapeutic grandiosity/omnipotence, and more realistic appraisals and expectations in relation to their clinical competence. In their effort to understand the “whys” of their patient’s suicide, they are likely to retrospectively identify errors in treatment, “missed cues,” or things they might subsequently do differently,7 and to learn from these mistakes. Optimally, clinicians become more aware of their own therapeutic limitations, both in the short- and the long-term, and can use this knowledge to better determine how they will continue their clinical work. They also become much more aware of the issues involved in the aftermath of a patient suicide, including perceived gaps in the clinical and institutional systems that could optimally offer support to families and clinicians.
In addition to the positive changes related to knowledge and clinical skills, many clinicians also note deeper personal changes subsequent to their patient’s suicide, consistent with the literature on posttraumatic growth.1 Munson8 explored internal changes in clinicians following a patient suicide and found that in the aftermath, clinicians experienced both posttraumatic growth and compassion fatigue. He also found that the amount of time that elapsed since the patient’s suicide predicted posttraumatic growth, and the seemingly counterintuitive result that the number of years of clinical experience prior to the suicide was negatively correlated with posttraumatic growth.
Huhra et al4 described some of the existential issues that a clinician is likely to confront following a patient suicide. A clinician’s attempt to find a way to meaningfully understand the circumstances around this loss often prompts reflection on mortality, freedom, choice and personal autonomy, and the scope and limits of one’s responsibility toward others. The suicide challenges one’s previous conceptions and expectations around these professional issues, and the clinician must construct new paradigms that serve to integrate these new experiences and perspectives in a coherent way.
One of the most notable sequelae of this (and to other traumatic) experience is a subsequent desire to make use of the learning inherent in these experiences and to “give back.” Once they feel that they have resolved their own grief process, many clinicians express the desire to support others with similar experiences. Even when their experiences have been quite distressing, many clinicians are able to view the suicide as an opportunity to learn about ongoing limitations in the systems of support, and to work toward changing these in a way that ensures that future clinician-survivors will have more supportive experiences. Many view these new perspectives, and their consequent ability to be more helpful, as “unexpected gifts.” They often express gratitude toward the people and resources that have allowed them to make these transformations. Jones5 noted “the tragedy of patient suicide can also be an opportunity for us as therapists to grow in our skills at assessing and intervening in a suicidal crisis, to broaden and deepen the support we give and receive, to grow in our appreciation of the precious gift that life is, and to help each other live it more fully.”
Continue to: Guidelines for postvention
Guidelines for postvention
When a patient suicide occurs in the context of an agency setting, Grad9 recommends prompt responses on 4 levels:
- administrative
- institutional
- educational
- emotional.
Numerous authors5,10-21 have developed suggestions, guidelines, and detailed postvention protocols to help agencies and clinicians in various mental health settings navigate the often-complicated sequelae to a patient’s suicide. The Table highlights a few of these. Most emphasize that information about suicide loss, including both its statistical likelihood and its potential aftermath, should integrated into clinicians’ general education and training. They also suggest that suicide postvention policies and protocols be in place from the outset, and that such information be incorporated into institutional policy and procedure manuals. In addition, they stress that legal, institutional, and administrative needs be balanced with the emotional needs of affected clinicians and staff, as well as those of the surviving family.
Institutional and administrative procedures
The following are some of the recommended procedures that should take place following a suicide loss. The postvention protocols listed in the Table provide more detailed recommendations.
Legal/ethical. It is essential to consult with a legal representative/risk management specialist associated with the affected agency (ideally, one with specific expertise in suicide litigation.). It is also crucial to clarify who holds privilege after a patient’s death (varies by state), what may and may not be shared under the restrictions of confidentiality and Health Insurance Portability and Accountability Act (HIPAA) laws, and to clarify procedures for chart completion and review. It is also important to clarify the specific information to be shared both within and outside of the agency, and how to address the needs of current patients in the agency settings.
Case review. The optimal purpose of the case review (also known as a psychological autopsy) is to facilitate learning, identify gaps in agency procedures and training, improve pre- and postvention procedures, and help clinicians cope with the loss.22 Again, the legal and administrative needs of the agency need to be balanced with the attention to the emotional impact on the treating clinician.17 Ellis and Patel18 recommend delaying this procedure until the treating clinician is no longer in the “shock” phase of the loss, and is able to think and process events more objectively.
Continue to: Family contact
Family contact. Most authors have recommended that clinicians and/or agencies reach out to surviving families. Although some legal representatives will advise against this, experts in the field of suicide litigation have noted that compassionate family contact reduces liability and facilitates healing for both parties. In a personal communication (May 2008), Eric Harris, of the American Psychological Association Trust, recommended “compassion over caution” when considering these issues. Again, it is important to clarify who holds privilege after a patient’s death in determining when and with whom the patient’s confidential information may be shared. When confidentiality may be broken, clinical judgment should be used to determine how best to present the information to grieving family members.
Even if surviving family members do not hold privilege, there are many things that clinicians can do to be helpful.23 Inevitably, families will want any information that will help them make sense of the loss, and general psychoeducation about mental illness and suicide can be helpful in this regard. In addition, providing information about “Survivors After Suicide” support groups, reading materials, etc., can be helpful. Both support groups and survivor-related bibliographies are available on the web sites of the American Association of Suicidology (www.suicidology.org) and The American Foundation for Suicide Prevention (www.afsp.org).
In addition, clinicians should ask the family if it would be helpful if they were to attend the funeral/memorial services, and how to introduce themselves if asked by other attendees.
Patients in clinics/hospitals. When a patient suicide occurs in a clinic or hospital setting, it is likely to impact other patients in that setting to the extent that they have heard, about the event, even from outside sources.According to Hodgkinson,24 in addition to being overwhelmed with intense feelings about the suicide loss (particularly if they had known the patient), affected patients are likely to be at increased risk for suicidal behaviors. This is consistent with the considerable literature on suicide contagion.
Thus, it is important to clarify information to be shared with patients; however, avoid describing details of the method, because this can foster contagion and “copycat” suicides. In addition, Kaye and Soreff22 noted that these patients may now be concerned about the staff’s ability to be helpful to them, because they were unable to help the deceased. In light of this, take extra care to attend to the impact of the suicide on current patients, and to monitor both pre-existing and new suicidality.
Continue to: Helping affected clinicians
Helping affected clinicians
Suggestions for optimally supporting affected clinicians include:
- clear communication about the nature of upcoming administrative procedures (including chart and institutional reviews)
- consultation from supervisors and/or colleagues that is supportive and reassuring, rather than blaming
- opportunities for the clinician to talk openly about the experience of the loss, either individually or in group settings, without fear of judgment or censure
- recognition that the loss is likely to impact clinical work, support in monitoring this impact, and the provision of medical leaves and/or modified caseloads (ie, fewer high-risk patients) as necessary.
Box 1
Frank Jones and Judy Meade founded the Clinical Survivor Task Force (CSTF) of the American Association of Suicidology (AAS) in 1987. As Jones noted, “clinicians who have lost patients to suicide need a place to acknowledge and carry forward their personal loss…to benefit both personally and professionally from the opportunity to talk with other therapists who have survived the loss of a patient through suicide.”7 Nina Gutin, PhD, and Vanessa McGann, PhD, have co-chaired the CSTF since 2003. It supports clinicians who have lost patients and/or loved ones, with the recognition that both types of losses carry implications within clinical and professional domains. The CSTF provides a listserve, opportunities to participate in video support groups, and a web site (www.cliniciansurvivor.org) that provides information about the clinician-survivor experience, the opportunity to read and post narratives about one’s experience with suicide loss, an updated bibliography maintained by John McIntosh, PhD, a list of clinical contacts, and links to several excellent postvention protocols. In addition, Drs. Gutin and McGann conduct clinician-survivor support activities at the annual AAS conference, and in their respective geographic areas.
Both researchers and clinician-survivors in my practice and support groups have noted that speaking with other clinicians who have experienced suicide loss can be particularly reassuring and validating. If none are available on staff, the listserve and online support groups of the American Association of Suicidology’s Clinician Survivor Task Force may be helpful (Box 17). In addition, the film “Collateral Damages: The Impact of Patient Suicide on the Physician” features physicians describing their experience of losing a patient to suicide (Box 2).
Box 2
“Collateral Damages: The Impact of Patient Suicide on the Physician” is a film that features several physicians speaking about their experience of losing a patient to suicide, as well as a group discussion. Psychiatrists in this educational film include Drs. Glen Gabbard, Sidney Zisook, and Jim Lomax. This resource can be used to facilitate an educational session for physicians, psychologists, residents, or other trainees. Please contact education@afsp.org to request a DVD of this film and a copy of a related article, Prabhakar D, Anzia JM, Balon R, et al. “Collateral damages”: preparing residents for coping with patient suicide. Acad Psychiatry. 2013;37(6):429-430.
Schultz14 offered suggestions for staff in supervisory positions, noting that they may bear at least some clinical and legal responsibility for the treatments that they supervise. She encouraged supervisors to take an active stance in advocating for trainees, to encourage colleagues to express their support, and to discourage rumors and other stigmatizing reactions. Schultz also urges supervisors to14:
- allow extra time for the clinician to engage in the normative exploration of the “whys” that are unique to suicide survivors
- use education about suicide to help the clinician gain a more realistic perspective on their relative culpability
- become aware of and provide education about normative grief reactions following a suicide.
Continue to: Because a suicide loss...
Because a suicide loss is likely to affect a clinician’s subsequent clinical activity, Schultz encourages supervisors to help clinicians monitor this impact on their work.14
A supportive environment is key
Losing a patient to suicide is a complicated, potentially traumatic process that many mental health clinicians will face. Yet with comprehensive and supportive postvention policies in place, clinicians who are impacted are more likely to experience healing and posttraumatic growth in both personal and professional domains.
Bottom Line
Although often traumatic, losing a patient to suicide presents clinicians with an opportunity for personal and professional growth. Following established postvention protocols can help ensure that legal, institutional, and administrative needs are balanced with the emotional needs of affected clinicians and staff, as well as those of the surviving family.
Related Resources
- American Association of Suicidology Clinician Survivor Task Force. www.cliniciansurvivor.org.
- Dotinga R. Coping when a patient commits suicide. July 21, 2017. www.mdedge.com/psychiatry/article/142975/depression/coping-when-patient-commits-suicide.
- Gutin N. Losing a patent to suicide: What we know. Part 1. 2019;18(10):14-16,19-22,30-32.
1. Tedeschi RG, Calhoun LG. Beyond the concept of recovery: Growth and the experience of loss. Death Stud. 2008;32(1):27-39.
2. Fuentes MA, Cruz D. Posttraumatic growth: positive psychological changes after trauma. Mental Health News. 2009;11(1):31,37.
3. Gitlin M. Aftermath of a tragedy: reaction of psychiatrists to patient suicides. Psychiatr Ann. 2007;37(10):684-687.
4. Huhra R, Hunka N, Rogers J, et al. Finding meaning: theoretical perspectives on patient suicide. Paper presented at: 2004 Annual Conference of the American Association of Suicidology; April 2004; Miami, FL.
5. Jones FA Jr. Therapists as survivors of patient suicide. In: Dunne EJ, McIntosh JL, Dunne-Maxim K, eds. Suicide and its aftermath: understanding and counseling the survivors. New York, NY: W.W. Norton; 1987;126-141.
6. Gutin N, McGann VM, Jordan JR. The impact of suicide on professional caregivers. In: Jordan J, McIntosh J, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge; 2011:93-111.
7. Hendin H, Lipschitz A, Maltsberger JT, et al. Therapists’ reactions to patients’ suicides. Am J Psychiatry. 2000;157(12):2022-2027.
8. Munson JS. Impact of client suicide on practitioner posttraumatic growth [dissertation]. Gainesville, Florida: University of Florida; 2009.
9. Grad OT. Therapists as survivors of suicide loss. In: Wasserman D, Wasserman C, eds. Oxford textbook of suicidology and suicide prevention. Oxford, UK: Oxford University Press; 2009:609-615.
10. Douglas J, Brown HN. Suicide: understanding and responding: Harvard Medical School perspectives. Madison, CT: International Universities Press; 1989.
11. Farberow NL. The mental health professional as suicide survivor. Clin Neuropsychiatry. 2005;2(1):13-20.
12. Plakun EM, Tillman JG. Responding to clinicians after loss of a patient to suicide. Dir Psychiatry. 2005;25:301-310.
13. Quinnett P. QPR: for suicide prevention. QPR Institute, Inc. www.cliniciansurvivor.org (under Postvention tab). Published September 21, 2009. Accessed August 26, 2019.
14. Schultz, D. Suggestions for supervisors when a therapist experiences a client’s suicide. Women Ther. 2005;28(1):59-69.
15. Spiegelman JS Jr, Werth JL Jr. Don’t forget about me: the experiences of therapists-in-training after a patient has attempted or died by suicide. Women Ther. 2005;28(1):35-57.
16. American Association of Suicidology. Clinician Survivor Task Force. Clinicians as survivors of suicide: postvention information. http://cliniciansurvivor.org. Published May 16, 2016. Accessed January 13, 2019.
17. Whitmore CA, Cook J, Salg L. Supporting residents in the wake of patient suicide. The American Journal of Psychiatry Residents’ Journal. 2017;12(1):5-7.
18. Ellis TE, Patel AB. Client suicide: what now? Cogn Behav Pract. 2012;19(2):277-287.
19. Figueroa S, Dalack GW. Exploring the impact of suicide on clinicians: a multidisciplinary retreat model. J Psychiatr Pract. 2013;19(1):72-77.
20. Lerner U, Brooks, K, McNeil DE, et al. Coping with a patient’s suicide: a curriculum for psychiatry residency training programs. Acad Psychiatry. 2012;36(1):29-33.
21. Prabhakar D, Balon R, Anzia J, et al. Helping psychiatry residents cope with patient suicide. Acad Psychiatry. 2014;38(5):593-597.
22. Kaye NS, Soreff SM. The psychiatrist’s role, responses, and responsibilities when a patient commits suicide. Am J Psychiatry. 1991;148(6):739-743.
23. McGann VL, Gutin N, Jordan JR. Guidelines for postvention care with survivor families after the suicide of a client. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge; 2011:133-155.
24. Hodgkinson PE. Responding to in-patient suicide. Br J Med Psychol. 1987;60(4):387-392.
1. Tedeschi RG, Calhoun LG. Beyond the concept of recovery: Growth and the experience of loss. Death Stud. 2008;32(1):27-39.
2. Fuentes MA, Cruz D. Posttraumatic growth: positive psychological changes after trauma. Mental Health News. 2009;11(1):31,37.
3. Gitlin M. Aftermath of a tragedy: reaction of psychiatrists to patient suicides. Psychiatr Ann. 2007;37(10):684-687.
4. Huhra R, Hunka N, Rogers J, et al. Finding meaning: theoretical perspectives on patient suicide. Paper presented at: 2004 Annual Conference of the American Association of Suicidology; April 2004; Miami, FL.
5. Jones FA Jr. Therapists as survivors of patient suicide. In: Dunne EJ, McIntosh JL, Dunne-Maxim K, eds. Suicide and its aftermath: understanding and counseling the survivors. New York, NY: W.W. Norton; 1987;126-141.
6. Gutin N, McGann VM, Jordan JR. The impact of suicide on professional caregivers. In: Jordan J, McIntosh J, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge; 2011:93-111.
7. Hendin H, Lipschitz A, Maltsberger JT, et al. Therapists’ reactions to patients’ suicides. Am J Psychiatry. 2000;157(12):2022-2027.
8. Munson JS. Impact of client suicide on practitioner posttraumatic growth [dissertation]. Gainesville, Florida: University of Florida; 2009.
9. Grad OT. Therapists as survivors of suicide loss. In: Wasserman D, Wasserman C, eds. Oxford textbook of suicidology and suicide prevention. Oxford, UK: Oxford University Press; 2009:609-615.
10. Douglas J, Brown HN. Suicide: understanding and responding: Harvard Medical School perspectives. Madison, CT: International Universities Press; 1989.
11. Farberow NL. The mental health professional as suicide survivor. Clin Neuropsychiatry. 2005;2(1):13-20.
12. Plakun EM, Tillman JG. Responding to clinicians after loss of a patient to suicide. Dir Psychiatry. 2005;25:301-310.
13. Quinnett P. QPR: for suicide prevention. QPR Institute, Inc. www.cliniciansurvivor.org (under Postvention tab). Published September 21, 2009. Accessed August 26, 2019.
14. Schultz, D. Suggestions for supervisors when a therapist experiences a client’s suicide. Women Ther. 2005;28(1):59-69.
15. Spiegelman JS Jr, Werth JL Jr. Don’t forget about me: the experiences of therapists-in-training after a patient has attempted or died by suicide. Women Ther. 2005;28(1):35-57.
16. American Association of Suicidology. Clinician Survivor Task Force. Clinicians as survivors of suicide: postvention information. http://cliniciansurvivor.org. Published May 16, 2016. Accessed January 13, 2019.
17. Whitmore CA, Cook J, Salg L. Supporting residents in the wake of patient suicide. The American Journal of Psychiatry Residents’ Journal. 2017;12(1):5-7.
18. Ellis TE, Patel AB. Client suicide: what now? Cogn Behav Pract. 2012;19(2):277-287.
19. Figueroa S, Dalack GW. Exploring the impact of suicide on clinicians: a multidisciplinary retreat model. J Psychiatr Pract. 2013;19(1):72-77.
20. Lerner U, Brooks, K, McNeil DE, et al. Coping with a patient’s suicide: a curriculum for psychiatry residency training programs. Acad Psychiatry. 2012;36(1):29-33.
21. Prabhakar D, Balon R, Anzia J, et al. Helping psychiatry residents cope with patient suicide. Acad Psychiatry. 2014;38(5):593-597.
22. Kaye NS, Soreff SM. The psychiatrist’s role, responses, and responsibilities when a patient commits suicide. Am J Psychiatry. 1991;148(6):739-743.
23. McGann VL, Gutin N, Jordan JR. Guidelines for postvention care with survivor families after the suicide of a client. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge; 2011:133-155.
24. Hodgkinson PE. Responding to in-patient suicide. Br J Med Psychol. 1987;60(4):387-392.
Losing a patient to suicide: What we know
Studies have found that 1 in 2 psychiatrists,1-4 and 1 in 5 psychologists, clinical social workers, and other mental health professionals,5 will lose a patient to suicide in the course of their career. This statistic suggests that losing a patient to suicide constitutes a clear occupational hazard.6,7 Despite this, most mental health professionals continue to view suicide loss as an aberration. Consequently, there is often a lack of preparedness for such an event when it does occur.
This 2-part article summarizes what is currently known about the unique personal and professional issues experienced by clinician-survivors (clinicians who have lost patients and/or loved ones to suicide). In Part 1, I cover:
- the impact of losing a patient to suicide
- confidentiality-related constraints on the ability to discuss and process the loss
- legal and ethical issues
- colleagues’ reactions and stigma
- the effects of a suicide loss on one’s clinical work.
Part 2 will discuss the opportunities for personal growth that can result from experiencing a suicide loss, guidelines for optimal postventions, and steps clinicians can take to help support colleagues who have lost a patient to suicide.
A neglected topic
For psychiatrists and other mental health professionals, the loss of a patient to suicide is certainly not uncommon.1-5 Despite this, coping with a patient’s suicide is a “neglected topic”8 in residency and general mental health training.
There are many published articles on clinicians experiencing suicide loss (for a comprehensive bibliography, see McIntosh9), and several authors10-19 have developed suggestions, guidelines, and detailed postvention protocols to help clinicians navigate the often-complicated sequelae to such a loss. However, these resources have generally not been integrated into clinical training, and tend to be poorly disseminated. In a national survey of chief residents, Melton and Coverdale20 found that only 25% of residency training programs covered topics related to postvention, and 72% of chief residents felt this topic needed more attention. Thus, despite the existence of guidelines for optimal postvention and support, clinicians are often left to cope with the consequences of this difficult loss on their own, and under less-than-optimal conditions.
A patient’s suicide typically affects clinicians on multiple levels, both personally and professionally. In this article, I highlight the range of normative responses, as well as the factors that may facilitate or inhibit subsequent healing and growth, with the hope that this knowledge may be utilized to help current and future generations of clinician-survivors obtain optimal support, and that institutions who treat potentially suicidal individuals will develop optimal postvention responses following a suicide loss. Many aspects of what this article discusses also apply to clinicians who have experienced a suicide loss in their personal or family life, as this also tends to “spill over” into one’s professional roles and identity.
Grief and other emotional effects
In many ways, clinicians’ responses after a patient’s suicide are similar to those of other survivors after the loss of a loved one to suicide.21 Chemtob et al2 found that approximately one-half of psychiatrists who lost a patient to suicide had scores on the Impact of an Event Scale that were comparable to those of a clinical population seeking treatment after the death of a parent.
Continue to: Jordan and McIntosh have detailed...
Jordan and McIntosh22 have detailed several elements and themes that differentiate suicide loss and its associated reactions from other types of loss and grief. In general, suicide loss is considered traumatic, and is often accompanied by intense confusion and existential questioning, reflecting a negative impact on one’s core beliefs and assumptive world. The subsequent need to address the myriad of “why” questions left in its wake are often tinted with what Jordan and Baugher23 term the “tyranny of hindsight,” and take the form of implicit guilt for “sins of omission or commission” in relation to the lost individual.
Responses to suicide loss typically include initial shock, denial and numbness, intense sadness, anxiety, anger, and intense distress. Consistent with the traumatic nature of the loss, survivors are also likely to experience posttraumatic stress disorder symptoms such as intrusive thoughts, avoidance, and dissociation. Survivors also commonly experience significant guilt and shame, and this is likely to be socially reinforced by the general stigma associated with suicide as well as the actual blaming and avoidance responses of others.24-27
Clinicians’ unique reactions
For clinicians, there are additional components that may further complicate or exacerbate these reactions and extend their duration. First and foremost, such a loss affects clinicians on both personal and professional levels, a phenomenon that Plakun and Tillman13 have termed a “twin bereavement.” Thus, in addition to the personal grief and trauma reactions entailed in losing a patient to suicide, this loss is likely to impact clinicians’ professional identities, their relationships with colleagues, and their clinical work.
Clinicians’ professional identities are often predicated on generally shared assumptions and beliefs that, as trained professionals, they should have the power, aptitude, and competence to heal, or at least improve, the lives of patients, to reduce their distress, and to provide safety. In addition, such assumptions about clinicians’ responsibility and ability to prevent suicide are often reinforced in the clinical literature.28,29
These assumptions are often challenged, if not shattered, when patients take their own lives. A clinician’s sense of professional responsibility, the guilt and self-blame that may accompany this, self-doubts about one’s skills and clinical competence, the fear of (and actual) blame of colleagues and family members, and the real or imagined threat of litigation may all greatly exacerbate a clinician’s distress.11
Continue to: Hendin et al found...
Hendin et al30 found that mental health therapists have described losing a patient as “the most profoundly disturbing event of their professional careers,” noting that one-third of these clinicians experienced severe distress that lasted at least 1 year beyond the initial loss. In a 2004 study, Ruskin et al4 similarly found that one-quarter of psychiatrists and psychiatric trainees noted that losing a patient had a “profound and enduring effect on them.” In her article on surviving a patient’s suicide, Rycroft31 describes a “professional void” following the loss of her patient, in which “the world had changed, nothing was predictable any more, and it was no longer safe to assume anything.” Additionally, many clinicians experience an “acute sense of aloneness and isolation” subsequent to the loss.32
Many clinicians have noted that they considered leaving the field after such a loss,33,34 and it is hypothesized that many may have done so.35-37 Others have noted that, at least temporarily, they stopped treating patients who were potentially suicidal.29,35
Box 1
Several authors have proposed general models for describing the suicide grief trajectories of clinicians after a suicide loss. Tillman38 identified distinct groups of responses to this event: traumatic, affective, those related to the treatment, those related to interactions with colleagues, liability concerns, and the impact on one’s professional philosophy. She also found that Erikson’s stages of identity39 provided an uncannily similar trajectory to the ways in which those who participated in her research—clinicians at a mental hospital—had attempted to cope with their patients’ deaths, noting that the “suicide of a patient may provoke a revisiting of Erikson’s psychosocial crises in a telescoped and accelerated fashion.”38
Maltsberger40 offered a detailed psychoanalytic analysis of the responses clinicians may manifest in relation to a suicide loss, including the initial narcissistic injury sustained in relation to their patient’s actions; the subsequent potential for melancholic, atonement, or avoidance reactions; and the eventual capacity for the resolution of these reactions.
Al-Mateen et al33 described 3 phases of the clinician’s reaction after losing a patient who was a child to suicide:
- initial, which includes trauma and shock
- turmoil, which includes emotional flooding and functional impairments
- new growth, in which clinicians are able to reflect on their experiences and implications for training and policy.
For each phase, they also described staff activities that would foster forward movement through the trajectory.
In a 1981 study, Bissell41 found that psychiatric nurses who had experienced patient completed suicides progressed through several developmental stages (naïveté, recognition, responsibility, individual choice) that enabled them to come to terms with their personal reactions and place the ultimate responsibility for the suicide with the patient.
After losing a patient to suicide, a clinician may experience grief that proceeds through specific stages (Box 133,38-41). Box 22-4,6,16,24,29,30,33,34,40,42-45 describes a wide range of factors that affect each clinician’s unique response to losing a patient to suicide.
Box 2
There are many factors that make the experience of losing a patient to suicide unique and variable for individual clinicians. These include the amount of a clinician’s professional training and experience, both in general and in working with potentially suicidal individuals. Chemtob et al2 found that trainees were more likely to experience patient suicide loss than more seasoned clinicians, and to experience more distress.4,30,42 Brown24 noted that many training programs were likely to assign the most “extraordinarily sick patients to inexperienced trainees.” He noted that because the skill level of trainees has not yet tempered their personal aspirations, they are likely to experience a patient’s suicide as a personal failure. However, in contrast to the findings of Kleespies,42 Hendin,30 Ruskin et al,4 and Brown24 suggested that the overall impact of a patient’s suicide may be greater for seasoned clinicians, when the “protective advantage” or “explanation” of being in training is no longer applicable. This appears consistent with Munson’s study,43 which found that a greater number of years of clinical experience prior to a suicide loss was negatively correlated with posttraumatic growth.
Other factors affecting a clinician’s grief response include the context in which the treatment occurred, such as inpatient, outpatient, clinic, private practice, etc.44; the presence and involvement of supportive mentors or supervisors16; the length and intensity of the clinical relationship6,29; countertransference issues40; whether the patient was a child33; and the time elapsed since the suicide occurred.
In addition, each clinician’s set of personal and life experiences can affect the way he/ she moves through the grieving process. Any previous trauma or losses, particularly prior exposure to suicide, will likely impact a clinician’s reaction to his/her current loss, as will any susceptibility to anxiety or depression. Gorkin45 has suggested that the degree of omnipotence in the clinician’s therapeutic strivings will affect his/her ability to accept the inherent ambiguity involved in suicide loss. Gender may also play a role: Henry et al34 found that female clinicians had higher levels of stress reactions, and Grad et al3 found that female clinicians felt more shame and guilt and professed more doubts about their professional competence than male clinicians, and were more than twice as likely as men to identify talking with colleagues as an effective coping strategy.
Continue to: Implications of confidentiality restrictions
Implications of confidentiality restrictions
Confidentiality issues, as well as advice from attorneys to limit the disclosure of information about a patient, are likely to preclude a clinician’s ability to talk freely about the patient, the therapeutic relationship, and his/her reactions to the loss, all of which are known to facilitate movement through the grief process.46
The development of trust and the sharing of pain are just 2 factors that can make the clinical encounter an intense emotional experience for both parties. Recent trends in the psychodynamic literature acknowledge the profundity and depth of the personal impact that patients have on the clinician, an impact that is neither pathological nor an indication of poor boundaries in the therapy dyad, but instead a recognition of how all aspects of the clinician’s person, whether consciously or not, are used within the context of a therapeutic relationship. Yet when clinicians lose a patient, confidentiality restrictions often leave them wondering if and where any aspects of their experiences can be shared. Legal counsel may advise a clinician against speaking to consultants or supervisors or even surviving family members for fear that these non-privileged communications are subject to discovery should any legal proceedings ensue. Furthermore, the usual grief rituals that facilitate the healing of loss and the processing of grief (eg, gathering with others who knew the deceased, sharing feelings and memories, attending memorials) are usually denied to the clinician, and are often compounded by the reactions of one’s professional colleagues, who tend not to view the therapist’s grief as “legitimate.” Thus, clinician-survivors, despite having experienced a profound and traumatic loss, have very few places where this may be processed or even validated. As one clinician in a clinician-survivors support group stated, “I felt like I was grieving in a vacuum, that I wasn’t allowed to talk about how much my patient meant to me or how I’m feeling about it.” The isolation of grieving alone is likely to be compounded by the general lack of resources for supporting clinicians after such a loss. In contrast to the general suicide “survivor” network of support groups for family members who have experienced a suicide loss, there is an almost complete lack of supportive resources for clinicians following such a loss, and most clinicians are not aware of the resources that are available, such as the Clinician Survivor Task Force of the American Association of Suicidology (Box 312).
Box 3
Frank Jones and Judy Meade founded the Clinician Survivor Task Force (CSTF) of the American Association of Suicidology (AAS) in 1987. As Jones noted, “clinicians who have lost patients to suicide need a place to acknowledge and carry forward their personal loss … to benefit both personally and professionally from the opportunity to talk with other therapists who have survived the loss of a patient through suicide.”12
Nina Gutin, PhD, and Vanessa McGann, PhD, have co-chaired the CSTF since 2003. It now supports clinicians who have lost patients and/or loved ones, with the recognition that both types of losses carry implications within clinical and professional domains. The CSTF provides a listserve, opportunities to participate in video support groups, and a web site (www. cliniciansurvivor.org) that provides information about the clinician-survivor experience, the opportunity to read and post narratives about one’s experience with suicide loss, an updated bibliography maintained by John McIntosh, PhD, a list of clinical contacts, and a link to several excellent postvention protocols. In addition, Drs. Gutin and McGann conduct clinician-survivor support activities at the annual AAS conference, and in their respective geographic areas.
Continue to: Doka has described...
Doka47 has described “disenfranchised grief” in which the bereaved person does not receive the type and quality of support accorded to other bereaved persons, and thus is likely to internalize the view that his/her grief is not legitimate, and to believe that sharing related distress is a shame-ridden liability. This clearly relates to the sense of profound isolation and distress often described by clinician-survivors.
Other legal/ethical issues
The clinician-survivor’s concern about litigation, or an actual lawsuit, is likely to produce intense anxiety. This common fear is both understandable and credible. According to Bongar,48 the most common malpractice lawsuits filed against clinicians are those that involve a patient’s suicide. Peterson et al49 found that 34% of surviving family members considered bringing a lawsuit against the clinician, and of these, 57% consulted a lawyer.
In addition, an institution’s concern about protecting itself from liability may compromise its ability to support the clinician or trainee who sustained the loss. As noted above, the potential prohibitions around discussing the case can compromise the grief process. Additionally, the fear of (or actual) legal reprisals against supervisors and the larger institution may engender angry and blaming responses toward the treating clinician. In a personal communication (April 2008), Quinnett described an incident in which a supervising psychologist stomped into the grieving therapist’s office unannounced and shouted, “Now look what you’ve done! You’re going to get me sued!”
Other studies29,50,51 note that clinician-survivors fear losing their job, and that their colleagues and supervisors will be reluctant to assign new patients to them. Spiegleman and Werth17 also note that trainees grapple with additional concerns over negative evaluations, suspension or termination from clinical sites or training programs, and a potential interruption of obtaining a degree. Such supervisory and institutional reactions are likely to intensify a clinician’s sense of shame and distress, and are antithetical to postvention responses that promote optimal personal and professional growth. Such negative reactions are also likely to contribute to a clinician or trainee’s subsequent reluctance to work with suicidal individuals, or their decision to discontinue their clinical work altogether. Lastly, other ethical issues, such as contact with the patient’s family following the suicide, attending the funeral, etc., are likely to be a source of additional anxiety and distress, particularly if the clinician needs to address these issues in isolation.
Professional relationships/colleagues’ reactions
Many clinician-survivors have described reactions from colleagues and supervisors that are hurtful and unsupportive. According to Jobes and Maltsberger,52 “the suicide death of a patient in active treatment is commonly taken as prima facie evidence that the therapist, somehow or another, has mismanaged the case,” and thus the clinician often faces unwarranted blame and censure from colleagues and supervisors. Hendin et al30 noted that many trainees found reactions by their institutions to be insensitive and unsupportive, one noting that the department’s review of the case “felt more like a tribunal or inquest.” In a personal communication (April 2008), Quinnett noted that many clinicians he interviewed following a suicide loss reported a pattern of isolation and interpersonal discomfort with their colleagues, who implicitly or explicitly expressed concerns about their competence. He described how a respected colleague received “no understanding, no support, only abuse” from her supervisors. Such responses, while perhaps surprising from mental health professionals, probably reflect the long-standing cultural attitude of social condemnation of suicide, and of those who are associated with it.
Continue to: Negative reactions from professional colleagues...
Negative reactions from professional colleagues are most likely to occur immediately after the suicide loss and/or during the course of a subsequent investigation or psychological autopsy. Castelli-Dransart et al53 found that the lack of institutional support after a clinician experiences a suicide loss contributed to significantly higher stress responses for impacted clinicians, and may lead to a well-founded ambivalence about disclosure to colleagues, and consequent resistance to seeking out optimal supervision/consultation or even personal therapy that could help the clinician gain clarity on the effects of these issues. Many mental health professionals have described how, after the distressing experience of losing a patient to suicide, they moved through this process in relative isolation and loneliness, feeling abandoned by their colleagues and by their own hopes and expectations for support.
Stigmatization. In clinical settings, when a patient in treatment completes suicide, the treating clinician becomes an easy scapegoat for family members and colleagues. To the extent that mental health professionals are not immune from the effects and imposition of stigma, this might also affect their previously mentioned tendency to project judgment, overtly or covertly, onto the treating clinician.
Stigma around suicide is well documented.25 In The Surgeon General’s Call to Action to Prevent Suicide,54 former Surgeon General David Satcher specifically described stigma around suicide as one of the biggest barriers to prevention. Studies have shown that individuals bereaved by suicide are also stigmatized, and that those who were in caregiving roles (parents, clinicians) are believed to be more psychologically disturbed, less likable, more blameworthy, and less worthy of receiving support than other bereaved individuals.25,55-63 These judgments often mirror survivors’ self-punitive assessments, which then become exacerbated by and intertwined with both externally imposed and internalized stigma. Hence, it is not uncommon for suicide survivors to question their own right to grieve, to report low expectations of social support, and to feel compelled to deny or hide the mode of death. Feigelman et al26 found that stigmatization after a suicide loss was specifically associated with ongoing grief difficulties, depression, and suicidal thinking.
In my long-term work with clinician-survivors, I’ve come to believe that in addition to stigma around suicide, there may also be stigma projected by colleagues in relation to a clinician’s perceived emotional vulnerability. A traumatized clinician potentially challenges the notion of the implicit dichotomy/power imbalance between professionals and the patients we treat: “Us”—the professional, competent, healthy, and benevolent clinicians who have the care to offer, and “Them”—our patients, being needy, pathological, looking to us for care. This “us/them” distinction may serve to bolster a clinician’s professional esteem and identity. But when one of “us” becomes one of “them”—when a professional colleague is perceived as being emotionally vulnerable—this can be threatening to the predicates of this distinction, leading to the need to put the affected clinician firmly into the “them” camp. Thus, unwarranted condemnations of the clinician-survivor’s handling of the case, and/or the pathologizing of their normative grief reactions after the suicide loss, can seem justified.
Stigma associated both with suicide and with professional vulnerability is likely to be internalized and to have a profound effect on the clinician’s decisions about disclosure, asking for support, and ultimately on one’s ability to integrate the loss. When this occurs, it is likely to lead to even more isolation, shame, and self-blame. It is not surprising that many clinicians consider leaving the profession after this type of experience.
Continue to: Effects on clinical work
Effects on clinical work
A suicide loss is also likely to affect a clinician’s therapeutic work. Many authors12,52,64-67 have found that this commonly leads therapists to question their abilities as clinicians, and to experience a sharp loss of confidence in their work with patients. The shattered beliefs and assumptions around the efficacy of the therapeutic process, a sense of guilt or self-blame, and any perceived or actual negative judgment from colleagues can dramatically compromise a clinician’s sense of competence. Hendin et al30 noted that even the most experienced therapists expressed difficulty in trusting their own clinical judgment, or accurately assessing risk after a suicide loss.
In addition, the common grief and trauma-related responses to a suicide loss (including shock, numbness, sadness, anxiety, and generalized distress) are likely to result in at least some temporary disruption of a clinician’s optimal functioning. If trauma-related symptoms are more pronounced, the effect and longevity of such impairment may be exacerbated, and are likely to “impair clinical response and therapeutic judgment.”15 In addition, because such symptoms and states may be triggered by exposure to other potentially suicidal patients, they are more likely to impact clinical functioning when the clinician works with suicidal individuals. Thus, the normative responses to a suicide loss are likely to impact a clinician’s work, just as they are likely to impact the personal and occupational functioning of any survivor of suicide loss.
In clinician-survivor discussions and support groups I’ve led, participants have identified many common areas of clinical impact. Perhaps one of the most common early responses reported by clinician-survivors who continued to work with potentially suicidal individuals was to become hypervigilant in relation to any perceived suicide risk, to interpret such risk in such a way as to warrant more conservative interventions than are necessary, and to consequently minimize the patient’s own capacities for self-care.68 Conversely, others reported a tendency to minimize or deny suicidal potential by, for example, avoiding asking patients directly about suicidal ideation, even when they later realized that such questioning was indicated.69
Suicide loss may also lead to more subtle clinical reactions that have been observed not only with suicidal patients, but also in relation to patients who struggle with loss or grief. These include avoidant or even dissociative reactions in relation to their patient’s pain, which in turn can impact the clinician’s ability to “be fully present” or empathic in clinical encounters.50,69 Still, other clinicians noted that they tended to project residual feelings of anger onto their current suicidal patients, or envied patients who seemed to have mastered their grief. Consistent with Maltsberger’s description of “atonement reactions,”40 some clinicians found themselves doing more than should be expected for their patients, even losing their sense of professional boundaries in the process. Anderson70 noted that in pushing herself beyond what she knew were her optimal clinical boundaries, she was “punishing herself” for failing to prevent her patient’s suicide because, as she realized, “doing ‘penance’ was better than feeling helpless and powerless.” And Schultz16 described how therapists may have subsequent difficulty in trusting other patients, especially if patients who completed suicide did not disclose or denied their suicidal intent.
Working toward a supportive solution
In summary, unless clinicians who lose a patient to suicide have more supportive experiences, the combination of confidentiality-related restrictions, confusion about legal/ethical repercussions, unsupportive reactions from colleagues, and unexpected impairments in clinical work are likely to lead to intensified distress, isolation, the perceived need to “hide” the impact in professional settings, and consideration of leaving the profession. However, as I will describe in Part 2 (
Bottom Line
For mental health clinicians, losing a patient to suicide is a clear occupational hazard. After a suicide loss, clinicians often experience unique personal and professional challenges, including the impact of the loss on clinical work and professional identity, legal/ethical issues, and confidentiality-related constraints on the ability to discuss and process the loss.
Related Resources
- American Association of Suicidology Clinician Survivor Task Force. www.cliniciansurvivor.org.
- Gutin N. Helping survivors in the aftermath of suicide loss. Current Psychiatry. 2018;17(8):27-33.
1. Alexander D, Klein S, Gray NM, et al. Suicide by patients: questionnaire study of its effect on consultant psychiatrists. BMJ. 2000;320(7249):1571-1574.
2. Chemtob CM, Hamada RS, Bauer G, et al. Patients’ suicides: frequency and impact on psychiatrists. Am J Psychiatry. 1988;145(2):224-228.
3. Grad OT, Zavasnik A, Groleger U. Suicide of a patient: gender differences in bereavement reactions of therapists. Suicide Life Threat Behav. 1997;27(4):379-386.
4. Ruskin R, Sakinofsky I, Bagby RM, et al. Impact of patient suicide on psychiatrists and psychiatric trainees. Acad Psychiatry. 2004;28(2):104-110.
5. Bersoff DN. Ethical conflicts in psychology, 2nd ed. Washington, DC: American Psychological Association; 1999.
6. Chemtob CM, Bauer GB, Hamada RS, et al. Patient suicide: occupational hazard for psychologists and psychiatrists. Prof Psychol Res Pr. 1989;20(5):294-300.
7. Rubin HL. Surviving a suicide in your practice. In: Blumenthal SJ, Kupfer DJ, eds. Suicide over the life cycle: risk factors, assessment, and treatment of suicidal patients. Washington, DC: American Psychiatric Press; 1990:619-636.
8. Kaye NS, Soreff SM. The psychiatrist’s role, responses, and responsibilities when a patient commits suicide. Am J Psychiatry. 1991;148(6):739-743.
9. McIntosh JL. Clinicians as survivors of suicide: bibliography. American Association of Suicidology Clinician Survivor Task Force. http://pages.iu.edu/~jmcintos/Surv.Ther.bib.htm. Updated May 19, 2019. Accessed August 26, 2019.
10. Douglas J, Brown HN. Suicide: understanding and responding: Harvard Medical School perspectives. Madison, CT: International Universities Press; 1989.
11. Farberow NL. The mental health professional as suicide survivor. Clin Neuropsychiatry. 2005;2(1):13-20.
12. Jones FA Jr. Therapists as survivors of patient suicide. In: Dunne EJ, McIntosh JL, Dunne-Maxim K, eds. Suicide and its aftermath: understanding and counseling the survivors. New York, NY: W.W. Norton; 1987;126-141.
13. Plakun EM, Tillman JG. Responding to clinicians after loss of a patient to suicide. Dir Psychiatry. 2005;25:301-310.
14. Prabhakar D, Anzia JM, Balon R, et al. “Collateral damages”: preparing residents for coping with patient suicide. Acad Psychiatry. 2013;37(6):429-30.
15. Quinnett P. QPR: for suicide prevention. QPR Institute, Inc. http://pages.iu.edu/~jmcintos/postvention.htm. Published September 21, 2009. Accessed August 26, 2019.
16. Schultz, D. Suggestions for supervisors when a therapist experiences a client’s suicide. Women Ther. 2005;28(1):59-69.
17. Spiegelman JS Jr, Werth JL Jr. Don’t forget about me: the experiences of therapists-in-training after a patient has attempted or died by suicide. Women Ther. 2005;28(1):35-57.
18. American Association of Suicidology. Clinician Survivor Task Force. Clinicians as survivors of suicide: postvention information.
19. Whitmore CA, Cook J, Salg L. Supporting residents in the wake of patient suicide. The American Journal of Psychiatry Residents’ Journal. 2017;12(1):5-7.
20. Melton B, Coverdale J. What do we teach psychiatric residents about suicide? A national survey of chief residents. Acad Psychiatry. 2009;33(1):47-50.
21. Valente SM. Psychotherapist reactions to the suicide of a patient. Am J Orthopsychiatry. 1994;64(4):614-621.
22. Jordan JR, McIntosh JL. Is suicide bereavement different? A framework for rethinking the question. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge; 2011:19-42.
23. Jordan JR, Baugher B. After suicide loss: coping with your grief, 2nd ed. Newcastle, WA: Caring People Press; 2016.
24. Brown HB. The impact of suicide on therapists in training. Compr Psychiatry. 1987;28(2):101-112.
25. Cvinar JG. Do suicide survivors suffer social stigma: a review of the literature. Perspect Psychiatr Care. 2005;41(1):14-21.
26. Feigelman W, Gorman BS, Jordan JR. Stigmatization and suicide bereavement. Death Stud. 2009;33(7):591-608.
27. Goffman E. Stigma: notes on the management of spoiled identity. New York, NY: Simon & Schuster; 1963.
28. Goldney RD. The privilege and responsibility of suicide prevention. Crisis. 2000;21(1):8-15.
29. Litman RE. When patients commit suicide. Am J Psychother. 1965;19(4):570-576.
30. Hendin H, Lipschitz A, Maltsberger JT, et al. Therapists’ reactions to patients’ suicides. Am J Psychiatry. 2000;157(12):2022-2027.
31. Rycroft P. Touching the heart and soul of therapy: surviving client suicide. Women Ther. 2004;28(1):83-94.
32. Ellis TE, Patel AB. Client suicide: what now? Cogn Behav Pract. 2012;19(2):277-287.
33. Al-Mateen CS, Jones K, Linker J, et al. Clinician response to a child who completes suicide. Child Adolesc Psychiatric Clin N Am. 2018;27(4):621-635.
34. Henry M, Séguin M, Drouin M-S. Mental health professionals’ response to the suicide of their patients [in French]. Revue Québécoise de Psychologie. 2004;25:241-257.
35. Carter RE. Some effects of client suicide on the therapist. Psychother Theory Res Practice. 1971;8(4):287-289.
36. Dewar I, Eagles J, Klein S, et al. Psychiatric trainees’ experiences of, and reactions to, patient suicide. Psychiatr Bull. 2000;24(1):20-23.
37. Gitlin M. Aftermath of a tragedy: reaction of psychiatrists to patient suicides. Psychiatr Ann. 2007;37(10):684-687.
38. Tillman JG. When a patient commits suicide: an empirical study of psychoanalytic clinicians. Inter J Psychoanal. 2006;87(1):159-177.
39. Erikson EH. Identity and the life cycle. New York, NY: International Universities Press, Inc.; 1959.
40. Maltsberger JT. The implications of patient suicide for the surviving psychotherapist. In: Jacobs D, ed. Suicide and clinical practice. Washington, DC: American Psychiatric Press; 1992:169-182.
41. Bissell BPH. The experience of the nurse therapist working with suicidal cases: a developmental study [dissertation]. Boston, MA: Boston University School of Education; 1981.
42. Kleespies PM. The stress of patient suicidal behavior: Implications for interns and training programs in psychology. Prof Psychol Res Pract. 1993;24(4):477-482.
43. Munson JS. Impact of client suicide on practitioner posttraumatic growth [dissertation]. Gainsville, Florida: University of Florida; 2009.
44. Hodgkinson PE. Responding to in-patient suicide. Br J Med Psychol. 1987;60(4):387-392.
45. Gorkin M. On the suicide of one’s patient. Bull Menninger Clin. 1985;49(1):1-9.
46. Fuentes MA, Cruz D. Posttraumatic growth: positive psychological changes after trauma. Mental Health News. 2009;11(1):31,37.
47. Doka KJ. Disenfranchised grief: new Directions, challenges, and strategies for practice. Champaign, IL: Research Press; 2002.
48. Bongar B. The suicidal patient: clinical and legal standards of care, 2nd ed. Washington, DC: American Psychological Association; 2002.
49. Peterson EM, Luoma JB, Dunne E. Suicide survivors’ perceptions of the treating clinician. Suicide Life Threat Behav. 2002;32(2):158-166.
50. Kolodny S, Binder RL, Bronstein AA, et al. The working through of patients’ suicides by four therapists. Suicide Life Threat Behav. 1979;9(1):33-46.
51. Marshall KA. When a patient commits suicide. Suicide Life Threat Behav. 1980;10(1):29-40.
52. Jobes DA, Maltsberger JT. The hazards of treating suicidal patients. In: Sussman MB, ed. A perilous calling: the hazards of psychotherapy practice. New York, NY: Wiley & Sons; 1995:200-214.
53. Castelli-Dransart DA, Gutjahr E, Gulfi A, et al. Patient suicide in institutions: emotional responses and traumatic impact on Swiss mental health professionals. Death Stud. 2014;38(1-5):315-321.
54. US Public Health Service. The Surgeon General’s call to action to prevent suicide. Washington, DC: Department of Health and Human Services; 1999.
55. Armour M. Violent death: understanding the context of traumatic and stigmatized grief. J Hum Behav Soc Environ. 2006;14(4):53-90.
56. Calhoun, LG, Allen BG. Social reactions to the survivor of a suicide in the family: a review of the literature. Omega (Westport). 1991;23(2):95-107.
57. Dunne EJ, McIntosh JL, Dunne-Maxim K, eds. Suicide and its aftermath: understanding and counseling the survivors. New York, NY: WW Norton & Co; 1987.
58. Harwood D, Hawton K, Hope J, et al. The grief experiences and needs of bereaved relatives and friends of older people dying through suicide: a descriptive and case-control study. J Affect Disord. 2002;72(2):185-194.
59. Jordan JR. Is suicide bereavement different? A reassessment of the literature. Suicide Life Threat Behav. 2001;31(1):91-102.
60. McIntosh JL. Control group studies of suicide survivors: a review and critique. Suicide Life Threat Behav. 2003;23(2):146-161.
61. Range LM. When a loss is due to suicide: unique aspects of bereavement. In: Harvey JH, ed. Perspectives on loss: a sourcebook. Philadelphia, PA: Brunner/Mazel; 1998:213-220.
62. Sveen CA, Walby FA. Suicide survivors’ mental health and grief reactions: a systematic review of controlled studies. Suicide Life Threat Behav. 2008;38(1):13-29.
63. Van Dongen CJ. Social context of postsuicide bereavement. Death Stud. 1993;17(2):125-141.
64. Bultema JK. The healing process for the multidisciplinary team: recovering post-inpatient suicide. J Psychosoc Nurs. 1994;32(2):19-24.
65. Cooper C. Patient suicide and assault: their impact on psychiatric hospital staff. J Psychosoc Nurs Ment Health Serv. 1995;33(6):26-29.
66. Foster VA, McAdams CR III. The impact of client suicide in counselor training: Implications for counselor education and supervision. Counselor Educ Supervision. 1999;39(1):22-33.
67. Little JD. Staff response to inpatient and outpatient suicide: what happened and what do we do? Aust N Z J Psychiatry. 1992;26(2):162-167.
68. Horn PJ. Therapists’ psychological adaptation to client suicidal behavior. Chicago, IL: Loyola University of Chicago; 1995.
69. Gutin N, McGann VM, Jordan JR. The impact of suicide on professional caregivers. In: Jordan J, McIntosh J, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge; 2011:93-111.
70. Anderson GO. Who, what, when, where, how, and mostly why? A therapist’s grief over the suicide of a client. Women Ther. 2004;28(1):25-34.
Studies have found that 1 in 2 psychiatrists,1-4 and 1 in 5 psychologists, clinical social workers, and other mental health professionals,5 will lose a patient to suicide in the course of their career. This statistic suggests that losing a patient to suicide constitutes a clear occupational hazard.6,7 Despite this, most mental health professionals continue to view suicide loss as an aberration. Consequently, there is often a lack of preparedness for such an event when it does occur.
This 2-part article summarizes what is currently known about the unique personal and professional issues experienced by clinician-survivors (clinicians who have lost patients and/or loved ones to suicide). In Part 1, I cover:
- the impact of losing a patient to suicide
- confidentiality-related constraints on the ability to discuss and process the loss
- legal and ethical issues
- colleagues’ reactions and stigma
- the effects of a suicide loss on one’s clinical work.
Part 2 will discuss the opportunities for personal growth that can result from experiencing a suicide loss, guidelines for optimal postventions, and steps clinicians can take to help support colleagues who have lost a patient to suicide.
A neglected topic
For psychiatrists and other mental health professionals, the loss of a patient to suicide is certainly not uncommon.1-5 Despite this, coping with a patient’s suicide is a “neglected topic”8 in residency and general mental health training.
There are many published articles on clinicians experiencing suicide loss (for a comprehensive bibliography, see McIntosh9), and several authors10-19 have developed suggestions, guidelines, and detailed postvention protocols to help clinicians navigate the often-complicated sequelae to such a loss. However, these resources have generally not been integrated into clinical training, and tend to be poorly disseminated. In a national survey of chief residents, Melton and Coverdale20 found that only 25% of residency training programs covered topics related to postvention, and 72% of chief residents felt this topic needed more attention. Thus, despite the existence of guidelines for optimal postvention and support, clinicians are often left to cope with the consequences of this difficult loss on their own, and under less-than-optimal conditions.
A patient’s suicide typically affects clinicians on multiple levels, both personally and professionally. In this article, I highlight the range of normative responses, as well as the factors that may facilitate or inhibit subsequent healing and growth, with the hope that this knowledge may be utilized to help current and future generations of clinician-survivors obtain optimal support, and that institutions who treat potentially suicidal individuals will develop optimal postvention responses following a suicide loss. Many aspects of what this article discusses also apply to clinicians who have experienced a suicide loss in their personal or family life, as this also tends to “spill over” into one’s professional roles and identity.
Grief and other emotional effects
In many ways, clinicians’ responses after a patient’s suicide are similar to those of other survivors after the loss of a loved one to suicide.21 Chemtob et al2 found that approximately one-half of psychiatrists who lost a patient to suicide had scores on the Impact of an Event Scale that were comparable to those of a clinical population seeking treatment after the death of a parent.
Continue to: Jordan and McIntosh have detailed...
Jordan and McIntosh22 have detailed several elements and themes that differentiate suicide loss and its associated reactions from other types of loss and grief. In general, suicide loss is considered traumatic, and is often accompanied by intense confusion and existential questioning, reflecting a negative impact on one’s core beliefs and assumptive world. The subsequent need to address the myriad of “why” questions left in its wake are often tinted with what Jordan and Baugher23 term the “tyranny of hindsight,” and take the form of implicit guilt for “sins of omission or commission” in relation to the lost individual.
Responses to suicide loss typically include initial shock, denial and numbness, intense sadness, anxiety, anger, and intense distress. Consistent with the traumatic nature of the loss, survivors are also likely to experience posttraumatic stress disorder symptoms such as intrusive thoughts, avoidance, and dissociation. Survivors also commonly experience significant guilt and shame, and this is likely to be socially reinforced by the general stigma associated with suicide as well as the actual blaming and avoidance responses of others.24-27
Clinicians’ unique reactions
For clinicians, there are additional components that may further complicate or exacerbate these reactions and extend their duration. First and foremost, such a loss affects clinicians on both personal and professional levels, a phenomenon that Plakun and Tillman13 have termed a “twin bereavement.” Thus, in addition to the personal grief and trauma reactions entailed in losing a patient to suicide, this loss is likely to impact clinicians’ professional identities, their relationships with colleagues, and their clinical work.
Clinicians’ professional identities are often predicated on generally shared assumptions and beliefs that, as trained professionals, they should have the power, aptitude, and competence to heal, or at least improve, the lives of patients, to reduce their distress, and to provide safety. In addition, such assumptions about clinicians’ responsibility and ability to prevent suicide are often reinforced in the clinical literature.28,29
These assumptions are often challenged, if not shattered, when patients take their own lives. A clinician’s sense of professional responsibility, the guilt and self-blame that may accompany this, self-doubts about one’s skills and clinical competence, the fear of (and actual) blame of colleagues and family members, and the real or imagined threat of litigation may all greatly exacerbate a clinician’s distress.11
Continue to: Hendin et al found...
Hendin et al30 found that mental health therapists have described losing a patient as “the most profoundly disturbing event of their professional careers,” noting that one-third of these clinicians experienced severe distress that lasted at least 1 year beyond the initial loss. In a 2004 study, Ruskin et al4 similarly found that one-quarter of psychiatrists and psychiatric trainees noted that losing a patient had a “profound and enduring effect on them.” In her article on surviving a patient’s suicide, Rycroft31 describes a “professional void” following the loss of her patient, in which “the world had changed, nothing was predictable any more, and it was no longer safe to assume anything.” Additionally, many clinicians experience an “acute sense of aloneness and isolation” subsequent to the loss.32
Many clinicians have noted that they considered leaving the field after such a loss,33,34 and it is hypothesized that many may have done so.35-37 Others have noted that, at least temporarily, they stopped treating patients who were potentially suicidal.29,35
Box 1
Several authors have proposed general models for describing the suicide grief trajectories of clinicians after a suicide loss. Tillman38 identified distinct groups of responses to this event: traumatic, affective, those related to the treatment, those related to interactions with colleagues, liability concerns, and the impact on one’s professional philosophy. She also found that Erikson’s stages of identity39 provided an uncannily similar trajectory to the ways in which those who participated in her research—clinicians at a mental hospital—had attempted to cope with their patients’ deaths, noting that the “suicide of a patient may provoke a revisiting of Erikson’s psychosocial crises in a telescoped and accelerated fashion.”38
Maltsberger40 offered a detailed psychoanalytic analysis of the responses clinicians may manifest in relation to a suicide loss, including the initial narcissistic injury sustained in relation to their patient’s actions; the subsequent potential for melancholic, atonement, or avoidance reactions; and the eventual capacity for the resolution of these reactions.
Al-Mateen et al33 described 3 phases of the clinician’s reaction after losing a patient who was a child to suicide:
- initial, which includes trauma and shock
- turmoil, which includes emotional flooding and functional impairments
- new growth, in which clinicians are able to reflect on their experiences and implications for training and policy.
For each phase, they also described staff activities that would foster forward movement through the trajectory.
In a 1981 study, Bissell41 found that psychiatric nurses who had experienced patient completed suicides progressed through several developmental stages (naïveté, recognition, responsibility, individual choice) that enabled them to come to terms with their personal reactions and place the ultimate responsibility for the suicide with the patient.
After losing a patient to suicide, a clinician may experience grief that proceeds through specific stages (Box 133,38-41). Box 22-4,6,16,24,29,30,33,34,40,42-45 describes a wide range of factors that affect each clinician’s unique response to losing a patient to suicide.
Box 2
There are many factors that make the experience of losing a patient to suicide unique and variable for individual clinicians. These include the amount of a clinician’s professional training and experience, both in general and in working with potentially suicidal individuals. Chemtob et al2 found that trainees were more likely to experience patient suicide loss than more seasoned clinicians, and to experience more distress.4,30,42 Brown24 noted that many training programs were likely to assign the most “extraordinarily sick patients to inexperienced trainees.” He noted that because the skill level of trainees has not yet tempered their personal aspirations, they are likely to experience a patient’s suicide as a personal failure. However, in contrast to the findings of Kleespies,42 Hendin,30 Ruskin et al,4 and Brown24 suggested that the overall impact of a patient’s suicide may be greater for seasoned clinicians, when the “protective advantage” or “explanation” of being in training is no longer applicable. This appears consistent with Munson’s study,43 which found that a greater number of years of clinical experience prior to a suicide loss was negatively correlated with posttraumatic growth.
Other factors affecting a clinician’s grief response include the context in which the treatment occurred, such as inpatient, outpatient, clinic, private practice, etc.44; the presence and involvement of supportive mentors or supervisors16; the length and intensity of the clinical relationship6,29; countertransference issues40; whether the patient was a child33; and the time elapsed since the suicide occurred.
In addition, each clinician’s set of personal and life experiences can affect the way he/ she moves through the grieving process. Any previous trauma or losses, particularly prior exposure to suicide, will likely impact a clinician’s reaction to his/her current loss, as will any susceptibility to anxiety or depression. Gorkin45 has suggested that the degree of omnipotence in the clinician’s therapeutic strivings will affect his/her ability to accept the inherent ambiguity involved in suicide loss. Gender may also play a role: Henry et al34 found that female clinicians had higher levels of stress reactions, and Grad et al3 found that female clinicians felt more shame and guilt and professed more doubts about their professional competence than male clinicians, and were more than twice as likely as men to identify talking with colleagues as an effective coping strategy.
Continue to: Implications of confidentiality restrictions
Implications of confidentiality restrictions
Confidentiality issues, as well as advice from attorneys to limit the disclosure of information about a patient, are likely to preclude a clinician’s ability to talk freely about the patient, the therapeutic relationship, and his/her reactions to the loss, all of which are known to facilitate movement through the grief process.46
The development of trust and the sharing of pain are just 2 factors that can make the clinical encounter an intense emotional experience for both parties. Recent trends in the psychodynamic literature acknowledge the profundity and depth of the personal impact that patients have on the clinician, an impact that is neither pathological nor an indication of poor boundaries in the therapy dyad, but instead a recognition of how all aspects of the clinician’s person, whether consciously or not, are used within the context of a therapeutic relationship. Yet when clinicians lose a patient, confidentiality restrictions often leave them wondering if and where any aspects of their experiences can be shared. Legal counsel may advise a clinician against speaking to consultants or supervisors or even surviving family members for fear that these non-privileged communications are subject to discovery should any legal proceedings ensue. Furthermore, the usual grief rituals that facilitate the healing of loss and the processing of grief (eg, gathering with others who knew the deceased, sharing feelings and memories, attending memorials) are usually denied to the clinician, and are often compounded by the reactions of one’s professional colleagues, who tend not to view the therapist’s grief as “legitimate.” Thus, clinician-survivors, despite having experienced a profound and traumatic loss, have very few places where this may be processed or even validated. As one clinician in a clinician-survivors support group stated, “I felt like I was grieving in a vacuum, that I wasn’t allowed to talk about how much my patient meant to me or how I’m feeling about it.” The isolation of grieving alone is likely to be compounded by the general lack of resources for supporting clinicians after such a loss. In contrast to the general suicide “survivor” network of support groups for family members who have experienced a suicide loss, there is an almost complete lack of supportive resources for clinicians following such a loss, and most clinicians are not aware of the resources that are available, such as the Clinician Survivor Task Force of the American Association of Suicidology (Box 312).
Box 3
Frank Jones and Judy Meade founded the Clinician Survivor Task Force (CSTF) of the American Association of Suicidology (AAS) in 1987. As Jones noted, “clinicians who have lost patients to suicide need a place to acknowledge and carry forward their personal loss … to benefit both personally and professionally from the opportunity to talk with other therapists who have survived the loss of a patient through suicide.”12
Nina Gutin, PhD, and Vanessa McGann, PhD, have co-chaired the CSTF since 2003. It now supports clinicians who have lost patients and/or loved ones, with the recognition that both types of losses carry implications within clinical and professional domains. The CSTF provides a listserve, opportunities to participate in video support groups, and a web site (www. cliniciansurvivor.org) that provides information about the clinician-survivor experience, the opportunity to read and post narratives about one’s experience with suicide loss, an updated bibliography maintained by John McIntosh, PhD, a list of clinical contacts, and a link to several excellent postvention protocols. In addition, Drs. Gutin and McGann conduct clinician-survivor support activities at the annual AAS conference, and in their respective geographic areas.
Continue to: Doka has described...
Doka47 has described “disenfranchised grief” in which the bereaved person does not receive the type and quality of support accorded to other bereaved persons, and thus is likely to internalize the view that his/her grief is not legitimate, and to believe that sharing related distress is a shame-ridden liability. This clearly relates to the sense of profound isolation and distress often described by clinician-survivors.
Other legal/ethical issues
The clinician-survivor’s concern about litigation, or an actual lawsuit, is likely to produce intense anxiety. This common fear is both understandable and credible. According to Bongar,48 the most common malpractice lawsuits filed against clinicians are those that involve a patient’s suicide. Peterson et al49 found that 34% of surviving family members considered bringing a lawsuit against the clinician, and of these, 57% consulted a lawyer.
In addition, an institution’s concern about protecting itself from liability may compromise its ability to support the clinician or trainee who sustained the loss. As noted above, the potential prohibitions around discussing the case can compromise the grief process. Additionally, the fear of (or actual) legal reprisals against supervisors and the larger institution may engender angry and blaming responses toward the treating clinician. In a personal communication (April 2008), Quinnett described an incident in which a supervising psychologist stomped into the grieving therapist’s office unannounced and shouted, “Now look what you’ve done! You’re going to get me sued!”
Other studies29,50,51 note that clinician-survivors fear losing their job, and that their colleagues and supervisors will be reluctant to assign new patients to them. Spiegleman and Werth17 also note that trainees grapple with additional concerns over negative evaluations, suspension or termination from clinical sites or training programs, and a potential interruption of obtaining a degree. Such supervisory and institutional reactions are likely to intensify a clinician’s sense of shame and distress, and are antithetical to postvention responses that promote optimal personal and professional growth. Such negative reactions are also likely to contribute to a clinician or trainee’s subsequent reluctance to work with suicidal individuals, or their decision to discontinue their clinical work altogether. Lastly, other ethical issues, such as contact with the patient’s family following the suicide, attending the funeral, etc., are likely to be a source of additional anxiety and distress, particularly if the clinician needs to address these issues in isolation.
Professional relationships/colleagues’ reactions
Many clinician-survivors have described reactions from colleagues and supervisors that are hurtful and unsupportive. According to Jobes and Maltsberger,52 “the suicide death of a patient in active treatment is commonly taken as prima facie evidence that the therapist, somehow or another, has mismanaged the case,” and thus the clinician often faces unwarranted blame and censure from colleagues and supervisors. Hendin et al30 noted that many trainees found reactions by their institutions to be insensitive and unsupportive, one noting that the department’s review of the case “felt more like a tribunal or inquest.” In a personal communication (April 2008), Quinnett noted that many clinicians he interviewed following a suicide loss reported a pattern of isolation and interpersonal discomfort with their colleagues, who implicitly or explicitly expressed concerns about their competence. He described how a respected colleague received “no understanding, no support, only abuse” from her supervisors. Such responses, while perhaps surprising from mental health professionals, probably reflect the long-standing cultural attitude of social condemnation of suicide, and of those who are associated with it.
Continue to: Negative reactions from professional colleagues...
Negative reactions from professional colleagues are most likely to occur immediately after the suicide loss and/or during the course of a subsequent investigation or psychological autopsy. Castelli-Dransart et al53 found that the lack of institutional support after a clinician experiences a suicide loss contributed to significantly higher stress responses for impacted clinicians, and may lead to a well-founded ambivalence about disclosure to colleagues, and consequent resistance to seeking out optimal supervision/consultation or even personal therapy that could help the clinician gain clarity on the effects of these issues. Many mental health professionals have described how, after the distressing experience of losing a patient to suicide, they moved through this process in relative isolation and loneliness, feeling abandoned by their colleagues and by their own hopes and expectations for support.
Stigmatization. In clinical settings, when a patient in treatment completes suicide, the treating clinician becomes an easy scapegoat for family members and colleagues. To the extent that mental health professionals are not immune from the effects and imposition of stigma, this might also affect their previously mentioned tendency to project judgment, overtly or covertly, onto the treating clinician.
Stigma around suicide is well documented.25 In The Surgeon General’s Call to Action to Prevent Suicide,54 former Surgeon General David Satcher specifically described stigma around suicide as one of the biggest barriers to prevention. Studies have shown that individuals bereaved by suicide are also stigmatized, and that those who were in caregiving roles (parents, clinicians) are believed to be more psychologically disturbed, less likable, more blameworthy, and less worthy of receiving support than other bereaved individuals.25,55-63 These judgments often mirror survivors’ self-punitive assessments, which then become exacerbated by and intertwined with both externally imposed and internalized stigma. Hence, it is not uncommon for suicide survivors to question their own right to grieve, to report low expectations of social support, and to feel compelled to deny or hide the mode of death. Feigelman et al26 found that stigmatization after a suicide loss was specifically associated with ongoing grief difficulties, depression, and suicidal thinking.
In my long-term work with clinician-survivors, I’ve come to believe that in addition to stigma around suicide, there may also be stigma projected by colleagues in relation to a clinician’s perceived emotional vulnerability. A traumatized clinician potentially challenges the notion of the implicit dichotomy/power imbalance between professionals and the patients we treat: “Us”—the professional, competent, healthy, and benevolent clinicians who have the care to offer, and “Them”—our patients, being needy, pathological, looking to us for care. This “us/them” distinction may serve to bolster a clinician’s professional esteem and identity. But when one of “us” becomes one of “them”—when a professional colleague is perceived as being emotionally vulnerable—this can be threatening to the predicates of this distinction, leading to the need to put the affected clinician firmly into the “them” camp. Thus, unwarranted condemnations of the clinician-survivor’s handling of the case, and/or the pathologizing of their normative grief reactions after the suicide loss, can seem justified.
Stigma associated both with suicide and with professional vulnerability is likely to be internalized and to have a profound effect on the clinician’s decisions about disclosure, asking for support, and ultimately on one’s ability to integrate the loss. When this occurs, it is likely to lead to even more isolation, shame, and self-blame. It is not surprising that many clinicians consider leaving the profession after this type of experience.
Continue to: Effects on clinical work
Effects on clinical work
A suicide loss is also likely to affect a clinician’s therapeutic work. Many authors12,52,64-67 have found that this commonly leads therapists to question their abilities as clinicians, and to experience a sharp loss of confidence in their work with patients. The shattered beliefs and assumptions around the efficacy of the therapeutic process, a sense of guilt or self-blame, and any perceived or actual negative judgment from colleagues can dramatically compromise a clinician’s sense of competence. Hendin et al30 noted that even the most experienced therapists expressed difficulty in trusting their own clinical judgment, or accurately assessing risk after a suicide loss.
In addition, the common grief and trauma-related responses to a suicide loss (including shock, numbness, sadness, anxiety, and generalized distress) are likely to result in at least some temporary disruption of a clinician’s optimal functioning. If trauma-related symptoms are more pronounced, the effect and longevity of such impairment may be exacerbated, and are likely to “impair clinical response and therapeutic judgment.”15 In addition, because such symptoms and states may be triggered by exposure to other potentially suicidal patients, they are more likely to impact clinical functioning when the clinician works with suicidal individuals. Thus, the normative responses to a suicide loss are likely to impact a clinician’s work, just as they are likely to impact the personal and occupational functioning of any survivor of suicide loss.
In clinician-survivor discussions and support groups I’ve led, participants have identified many common areas of clinical impact. Perhaps one of the most common early responses reported by clinician-survivors who continued to work with potentially suicidal individuals was to become hypervigilant in relation to any perceived suicide risk, to interpret such risk in such a way as to warrant more conservative interventions than are necessary, and to consequently minimize the patient’s own capacities for self-care.68 Conversely, others reported a tendency to minimize or deny suicidal potential by, for example, avoiding asking patients directly about suicidal ideation, even when they later realized that such questioning was indicated.69
Suicide loss may also lead to more subtle clinical reactions that have been observed not only with suicidal patients, but also in relation to patients who struggle with loss or grief. These include avoidant or even dissociative reactions in relation to their patient’s pain, which in turn can impact the clinician’s ability to “be fully present” or empathic in clinical encounters.50,69 Still, other clinicians noted that they tended to project residual feelings of anger onto their current suicidal patients, or envied patients who seemed to have mastered their grief. Consistent with Maltsberger’s description of “atonement reactions,”40 some clinicians found themselves doing more than should be expected for their patients, even losing their sense of professional boundaries in the process. Anderson70 noted that in pushing herself beyond what she knew were her optimal clinical boundaries, she was “punishing herself” for failing to prevent her patient’s suicide because, as she realized, “doing ‘penance’ was better than feeling helpless and powerless.” And Schultz16 described how therapists may have subsequent difficulty in trusting other patients, especially if patients who completed suicide did not disclose or denied their suicidal intent.
Working toward a supportive solution
In summary, unless clinicians who lose a patient to suicide have more supportive experiences, the combination of confidentiality-related restrictions, confusion about legal/ethical repercussions, unsupportive reactions from colleagues, and unexpected impairments in clinical work are likely to lead to intensified distress, isolation, the perceived need to “hide” the impact in professional settings, and consideration of leaving the profession. However, as I will describe in Part 2 (
Bottom Line
For mental health clinicians, losing a patient to suicide is a clear occupational hazard. After a suicide loss, clinicians often experience unique personal and professional challenges, including the impact of the loss on clinical work and professional identity, legal/ethical issues, and confidentiality-related constraints on the ability to discuss and process the loss.
Related Resources
- American Association of Suicidology Clinician Survivor Task Force. www.cliniciansurvivor.org.
- Gutin N. Helping survivors in the aftermath of suicide loss. Current Psychiatry. 2018;17(8):27-33.
Studies have found that 1 in 2 psychiatrists,1-4 and 1 in 5 psychologists, clinical social workers, and other mental health professionals,5 will lose a patient to suicide in the course of their career. This statistic suggests that losing a patient to suicide constitutes a clear occupational hazard.6,7 Despite this, most mental health professionals continue to view suicide loss as an aberration. Consequently, there is often a lack of preparedness for such an event when it does occur.
This 2-part article summarizes what is currently known about the unique personal and professional issues experienced by clinician-survivors (clinicians who have lost patients and/or loved ones to suicide). In Part 1, I cover:
- the impact of losing a patient to suicide
- confidentiality-related constraints on the ability to discuss and process the loss
- legal and ethical issues
- colleagues’ reactions and stigma
- the effects of a suicide loss on one’s clinical work.
Part 2 will discuss the opportunities for personal growth that can result from experiencing a suicide loss, guidelines for optimal postventions, and steps clinicians can take to help support colleagues who have lost a patient to suicide.
A neglected topic
For psychiatrists and other mental health professionals, the loss of a patient to suicide is certainly not uncommon.1-5 Despite this, coping with a patient’s suicide is a “neglected topic”8 in residency and general mental health training.
There are many published articles on clinicians experiencing suicide loss (for a comprehensive bibliography, see McIntosh9), and several authors10-19 have developed suggestions, guidelines, and detailed postvention protocols to help clinicians navigate the often-complicated sequelae to such a loss. However, these resources have generally not been integrated into clinical training, and tend to be poorly disseminated. In a national survey of chief residents, Melton and Coverdale20 found that only 25% of residency training programs covered topics related to postvention, and 72% of chief residents felt this topic needed more attention. Thus, despite the existence of guidelines for optimal postvention and support, clinicians are often left to cope with the consequences of this difficult loss on their own, and under less-than-optimal conditions.
A patient’s suicide typically affects clinicians on multiple levels, both personally and professionally. In this article, I highlight the range of normative responses, as well as the factors that may facilitate or inhibit subsequent healing and growth, with the hope that this knowledge may be utilized to help current and future generations of clinician-survivors obtain optimal support, and that institutions who treat potentially suicidal individuals will develop optimal postvention responses following a suicide loss. Many aspects of what this article discusses also apply to clinicians who have experienced a suicide loss in their personal or family life, as this also tends to “spill over” into one’s professional roles and identity.
Grief and other emotional effects
In many ways, clinicians’ responses after a patient’s suicide are similar to those of other survivors after the loss of a loved one to suicide.21 Chemtob et al2 found that approximately one-half of psychiatrists who lost a patient to suicide had scores on the Impact of an Event Scale that were comparable to those of a clinical population seeking treatment after the death of a parent.
Continue to: Jordan and McIntosh have detailed...
Jordan and McIntosh22 have detailed several elements and themes that differentiate suicide loss and its associated reactions from other types of loss and grief. In general, suicide loss is considered traumatic, and is often accompanied by intense confusion and existential questioning, reflecting a negative impact on one’s core beliefs and assumptive world. The subsequent need to address the myriad of “why” questions left in its wake are often tinted with what Jordan and Baugher23 term the “tyranny of hindsight,” and take the form of implicit guilt for “sins of omission or commission” in relation to the lost individual.
Responses to suicide loss typically include initial shock, denial and numbness, intense sadness, anxiety, anger, and intense distress. Consistent with the traumatic nature of the loss, survivors are also likely to experience posttraumatic stress disorder symptoms such as intrusive thoughts, avoidance, and dissociation. Survivors also commonly experience significant guilt and shame, and this is likely to be socially reinforced by the general stigma associated with suicide as well as the actual blaming and avoidance responses of others.24-27
Clinicians’ unique reactions
For clinicians, there are additional components that may further complicate or exacerbate these reactions and extend their duration. First and foremost, such a loss affects clinicians on both personal and professional levels, a phenomenon that Plakun and Tillman13 have termed a “twin bereavement.” Thus, in addition to the personal grief and trauma reactions entailed in losing a patient to suicide, this loss is likely to impact clinicians’ professional identities, their relationships with colleagues, and their clinical work.
Clinicians’ professional identities are often predicated on generally shared assumptions and beliefs that, as trained professionals, they should have the power, aptitude, and competence to heal, or at least improve, the lives of patients, to reduce their distress, and to provide safety. In addition, such assumptions about clinicians’ responsibility and ability to prevent suicide are often reinforced in the clinical literature.28,29
These assumptions are often challenged, if not shattered, when patients take their own lives. A clinician’s sense of professional responsibility, the guilt and self-blame that may accompany this, self-doubts about one’s skills and clinical competence, the fear of (and actual) blame of colleagues and family members, and the real or imagined threat of litigation may all greatly exacerbate a clinician’s distress.11
Continue to: Hendin et al found...
Hendin et al30 found that mental health therapists have described losing a patient as “the most profoundly disturbing event of their professional careers,” noting that one-third of these clinicians experienced severe distress that lasted at least 1 year beyond the initial loss. In a 2004 study, Ruskin et al4 similarly found that one-quarter of psychiatrists and psychiatric trainees noted that losing a patient had a “profound and enduring effect on them.” In her article on surviving a patient’s suicide, Rycroft31 describes a “professional void” following the loss of her patient, in which “the world had changed, nothing was predictable any more, and it was no longer safe to assume anything.” Additionally, many clinicians experience an “acute sense of aloneness and isolation” subsequent to the loss.32
Many clinicians have noted that they considered leaving the field after such a loss,33,34 and it is hypothesized that many may have done so.35-37 Others have noted that, at least temporarily, they stopped treating patients who were potentially suicidal.29,35
Box 1
Several authors have proposed general models for describing the suicide grief trajectories of clinicians after a suicide loss. Tillman38 identified distinct groups of responses to this event: traumatic, affective, those related to the treatment, those related to interactions with colleagues, liability concerns, and the impact on one’s professional philosophy. She also found that Erikson’s stages of identity39 provided an uncannily similar trajectory to the ways in which those who participated in her research—clinicians at a mental hospital—had attempted to cope with their patients’ deaths, noting that the “suicide of a patient may provoke a revisiting of Erikson’s psychosocial crises in a telescoped and accelerated fashion.”38
Maltsberger40 offered a detailed psychoanalytic analysis of the responses clinicians may manifest in relation to a suicide loss, including the initial narcissistic injury sustained in relation to their patient’s actions; the subsequent potential for melancholic, atonement, or avoidance reactions; and the eventual capacity for the resolution of these reactions.
Al-Mateen et al33 described 3 phases of the clinician’s reaction after losing a patient who was a child to suicide:
- initial, which includes trauma and shock
- turmoil, which includes emotional flooding and functional impairments
- new growth, in which clinicians are able to reflect on their experiences and implications for training and policy.
For each phase, they also described staff activities that would foster forward movement through the trajectory.
In a 1981 study, Bissell41 found that psychiatric nurses who had experienced patient completed suicides progressed through several developmental stages (naïveté, recognition, responsibility, individual choice) that enabled them to come to terms with their personal reactions and place the ultimate responsibility for the suicide with the patient.
After losing a patient to suicide, a clinician may experience grief that proceeds through specific stages (Box 133,38-41). Box 22-4,6,16,24,29,30,33,34,40,42-45 describes a wide range of factors that affect each clinician’s unique response to losing a patient to suicide.
Box 2
There are many factors that make the experience of losing a patient to suicide unique and variable for individual clinicians. These include the amount of a clinician’s professional training and experience, both in general and in working with potentially suicidal individuals. Chemtob et al2 found that trainees were more likely to experience patient suicide loss than more seasoned clinicians, and to experience more distress.4,30,42 Brown24 noted that many training programs were likely to assign the most “extraordinarily sick patients to inexperienced trainees.” He noted that because the skill level of trainees has not yet tempered their personal aspirations, they are likely to experience a patient’s suicide as a personal failure. However, in contrast to the findings of Kleespies,42 Hendin,30 Ruskin et al,4 and Brown24 suggested that the overall impact of a patient’s suicide may be greater for seasoned clinicians, when the “protective advantage” or “explanation” of being in training is no longer applicable. This appears consistent with Munson’s study,43 which found that a greater number of years of clinical experience prior to a suicide loss was negatively correlated with posttraumatic growth.
Other factors affecting a clinician’s grief response include the context in which the treatment occurred, such as inpatient, outpatient, clinic, private practice, etc.44; the presence and involvement of supportive mentors or supervisors16; the length and intensity of the clinical relationship6,29; countertransference issues40; whether the patient was a child33; and the time elapsed since the suicide occurred.
In addition, each clinician’s set of personal and life experiences can affect the way he/ she moves through the grieving process. Any previous trauma or losses, particularly prior exposure to suicide, will likely impact a clinician’s reaction to his/her current loss, as will any susceptibility to anxiety or depression. Gorkin45 has suggested that the degree of omnipotence in the clinician’s therapeutic strivings will affect his/her ability to accept the inherent ambiguity involved in suicide loss. Gender may also play a role: Henry et al34 found that female clinicians had higher levels of stress reactions, and Grad et al3 found that female clinicians felt more shame and guilt and professed more doubts about their professional competence than male clinicians, and were more than twice as likely as men to identify talking with colleagues as an effective coping strategy.
Continue to: Implications of confidentiality restrictions
Implications of confidentiality restrictions
Confidentiality issues, as well as advice from attorneys to limit the disclosure of information about a patient, are likely to preclude a clinician’s ability to talk freely about the patient, the therapeutic relationship, and his/her reactions to the loss, all of which are known to facilitate movement through the grief process.46
The development of trust and the sharing of pain are just 2 factors that can make the clinical encounter an intense emotional experience for both parties. Recent trends in the psychodynamic literature acknowledge the profundity and depth of the personal impact that patients have on the clinician, an impact that is neither pathological nor an indication of poor boundaries in the therapy dyad, but instead a recognition of how all aspects of the clinician’s person, whether consciously or not, are used within the context of a therapeutic relationship. Yet when clinicians lose a patient, confidentiality restrictions often leave them wondering if and where any aspects of their experiences can be shared. Legal counsel may advise a clinician against speaking to consultants or supervisors or even surviving family members for fear that these non-privileged communications are subject to discovery should any legal proceedings ensue. Furthermore, the usual grief rituals that facilitate the healing of loss and the processing of grief (eg, gathering with others who knew the deceased, sharing feelings and memories, attending memorials) are usually denied to the clinician, and are often compounded by the reactions of one’s professional colleagues, who tend not to view the therapist’s grief as “legitimate.” Thus, clinician-survivors, despite having experienced a profound and traumatic loss, have very few places where this may be processed or even validated. As one clinician in a clinician-survivors support group stated, “I felt like I was grieving in a vacuum, that I wasn’t allowed to talk about how much my patient meant to me or how I’m feeling about it.” The isolation of grieving alone is likely to be compounded by the general lack of resources for supporting clinicians after such a loss. In contrast to the general suicide “survivor” network of support groups for family members who have experienced a suicide loss, there is an almost complete lack of supportive resources for clinicians following such a loss, and most clinicians are not aware of the resources that are available, such as the Clinician Survivor Task Force of the American Association of Suicidology (Box 312).
Box 3
Frank Jones and Judy Meade founded the Clinician Survivor Task Force (CSTF) of the American Association of Suicidology (AAS) in 1987. As Jones noted, “clinicians who have lost patients to suicide need a place to acknowledge and carry forward their personal loss … to benefit both personally and professionally from the opportunity to talk with other therapists who have survived the loss of a patient through suicide.”12
Nina Gutin, PhD, and Vanessa McGann, PhD, have co-chaired the CSTF since 2003. It now supports clinicians who have lost patients and/or loved ones, with the recognition that both types of losses carry implications within clinical and professional domains. The CSTF provides a listserve, opportunities to participate in video support groups, and a web site (www. cliniciansurvivor.org) that provides information about the clinician-survivor experience, the opportunity to read and post narratives about one’s experience with suicide loss, an updated bibliography maintained by John McIntosh, PhD, a list of clinical contacts, and a link to several excellent postvention protocols. In addition, Drs. Gutin and McGann conduct clinician-survivor support activities at the annual AAS conference, and in their respective geographic areas.
Continue to: Doka has described...
Doka47 has described “disenfranchised grief” in which the bereaved person does not receive the type and quality of support accorded to other bereaved persons, and thus is likely to internalize the view that his/her grief is not legitimate, and to believe that sharing related distress is a shame-ridden liability. This clearly relates to the sense of profound isolation and distress often described by clinician-survivors.
Other legal/ethical issues
The clinician-survivor’s concern about litigation, or an actual lawsuit, is likely to produce intense anxiety. This common fear is both understandable and credible. According to Bongar,48 the most common malpractice lawsuits filed against clinicians are those that involve a patient’s suicide. Peterson et al49 found that 34% of surviving family members considered bringing a lawsuit against the clinician, and of these, 57% consulted a lawyer.
In addition, an institution’s concern about protecting itself from liability may compromise its ability to support the clinician or trainee who sustained the loss. As noted above, the potential prohibitions around discussing the case can compromise the grief process. Additionally, the fear of (or actual) legal reprisals against supervisors and the larger institution may engender angry and blaming responses toward the treating clinician. In a personal communication (April 2008), Quinnett described an incident in which a supervising psychologist stomped into the grieving therapist’s office unannounced and shouted, “Now look what you’ve done! You’re going to get me sued!”
Other studies29,50,51 note that clinician-survivors fear losing their job, and that their colleagues and supervisors will be reluctant to assign new patients to them. Spiegleman and Werth17 also note that trainees grapple with additional concerns over negative evaluations, suspension or termination from clinical sites or training programs, and a potential interruption of obtaining a degree. Such supervisory and institutional reactions are likely to intensify a clinician’s sense of shame and distress, and are antithetical to postvention responses that promote optimal personal and professional growth. Such negative reactions are also likely to contribute to a clinician or trainee’s subsequent reluctance to work with suicidal individuals, or their decision to discontinue their clinical work altogether. Lastly, other ethical issues, such as contact with the patient’s family following the suicide, attending the funeral, etc., are likely to be a source of additional anxiety and distress, particularly if the clinician needs to address these issues in isolation.
Professional relationships/colleagues’ reactions
Many clinician-survivors have described reactions from colleagues and supervisors that are hurtful and unsupportive. According to Jobes and Maltsberger,52 “the suicide death of a patient in active treatment is commonly taken as prima facie evidence that the therapist, somehow or another, has mismanaged the case,” and thus the clinician often faces unwarranted blame and censure from colleagues and supervisors. Hendin et al30 noted that many trainees found reactions by their institutions to be insensitive and unsupportive, one noting that the department’s review of the case “felt more like a tribunal or inquest.” In a personal communication (April 2008), Quinnett noted that many clinicians he interviewed following a suicide loss reported a pattern of isolation and interpersonal discomfort with their colleagues, who implicitly or explicitly expressed concerns about their competence. He described how a respected colleague received “no understanding, no support, only abuse” from her supervisors. Such responses, while perhaps surprising from mental health professionals, probably reflect the long-standing cultural attitude of social condemnation of suicide, and of those who are associated with it.
Continue to: Negative reactions from professional colleagues...
Negative reactions from professional colleagues are most likely to occur immediately after the suicide loss and/or during the course of a subsequent investigation or psychological autopsy. Castelli-Dransart et al53 found that the lack of institutional support after a clinician experiences a suicide loss contributed to significantly higher stress responses for impacted clinicians, and may lead to a well-founded ambivalence about disclosure to colleagues, and consequent resistance to seeking out optimal supervision/consultation or even personal therapy that could help the clinician gain clarity on the effects of these issues. Many mental health professionals have described how, after the distressing experience of losing a patient to suicide, they moved through this process in relative isolation and loneliness, feeling abandoned by their colleagues and by their own hopes and expectations for support.
Stigmatization. In clinical settings, when a patient in treatment completes suicide, the treating clinician becomes an easy scapegoat for family members and colleagues. To the extent that mental health professionals are not immune from the effects and imposition of stigma, this might also affect their previously mentioned tendency to project judgment, overtly or covertly, onto the treating clinician.
Stigma around suicide is well documented.25 In The Surgeon General’s Call to Action to Prevent Suicide,54 former Surgeon General David Satcher specifically described stigma around suicide as one of the biggest barriers to prevention. Studies have shown that individuals bereaved by suicide are also stigmatized, and that those who were in caregiving roles (parents, clinicians) are believed to be more psychologically disturbed, less likable, more blameworthy, and less worthy of receiving support than other bereaved individuals.25,55-63 These judgments often mirror survivors’ self-punitive assessments, which then become exacerbated by and intertwined with both externally imposed and internalized stigma. Hence, it is not uncommon for suicide survivors to question their own right to grieve, to report low expectations of social support, and to feel compelled to deny or hide the mode of death. Feigelman et al26 found that stigmatization after a suicide loss was specifically associated with ongoing grief difficulties, depression, and suicidal thinking.
In my long-term work with clinician-survivors, I’ve come to believe that in addition to stigma around suicide, there may also be stigma projected by colleagues in relation to a clinician’s perceived emotional vulnerability. A traumatized clinician potentially challenges the notion of the implicit dichotomy/power imbalance between professionals and the patients we treat: “Us”—the professional, competent, healthy, and benevolent clinicians who have the care to offer, and “Them”—our patients, being needy, pathological, looking to us for care. This “us/them” distinction may serve to bolster a clinician’s professional esteem and identity. But when one of “us” becomes one of “them”—when a professional colleague is perceived as being emotionally vulnerable—this can be threatening to the predicates of this distinction, leading to the need to put the affected clinician firmly into the “them” camp. Thus, unwarranted condemnations of the clinician-survivor’s handling of the case, and/or the pathologizing of their normative grief reactions after the suicide loss, can seem justified.
Stigma associated both with suicide and with professional vulnerability is likely to be internalized and to have a profound effect on the clinician’s decisions about disclosure, asking for support, and ultimately on one’s ability to integrate the loss. When this occurs, it is likely to lead to even more isolation, shame, and self-blame. It is not surprising that many clinicians consider leaving the profession after this type of experience.
Continue to: Effects on clinical work
Effects on clinical work
A suicide loss is also likely to affect a clinician’s therapeutic work. Many authors12,52,64-67 have found that this commonly leads therapists to question their abilities as clinicians, and to experience a sharp loss of confidence in their work with patients. The shattered beliefs and assumptions around the efficacy of the therapeutic process, a sense of guilt or self-blame, and any perceived or actual negative judgment from colleagues can dramatically compromise a clinician’s sense of competence. Hendin et al30 noted that even the most experienced therapists expressed difficulty in trusting their own clinical judgment, or accurately assessing risk after a suicide loss.
In addition, the common grief and trauma-related responses to a suicide loss (including shock, numbness, sadness, anxiety, and generalized distress) are likely to result in at least some temporary disruption of a clinician’s optimal functioning. If trauma-related symptoms are more pronounced, the effect and longevity of such impairment may be exacerbated, and are likely to “impair clinical response and therapeutic judgment.”15 In addition, because such symptoms and states may be triggered by exposure to other potentially suicidal patients, they are more likely to impact clinical functioning when the clinician works with suicidal individuals. Thus, the normative responses to a suicide loss are likely to impact a clinician’s work, just as they are likely to impact the personal and occupational functioning of any survivor of suicide loss.
In clinician-survivor discussions and support groups I’ve led, participants have identified many common areas of clinical impact. Perhaps one of the most common early responses reported by clinician-survivors who continued to work with potentially suicidal individuals was to become hypervigilant in relation to any perceived suicide risk, to interpret such risk in such a way as to warrant more conservative interventions than are necessary, and to consequently minimize the patient’s own capacities for self-care.68 Conversely, others reported a tendency to minimize or deny suicidal potential by, for example, avoiding asking patients directly about suicidal ideation, even when they later realized that such questioning was indicated.69
Suicide loss may also lead to more subtle clinical reactions that have been observed not only with suicidal patients, but also in relation to patients who struggle with loss or grief. These include avoidant or even dissociative reactions in relation to their patient’s pain, which in turn can impact the clinician’s ability to “be fully present” or empathic in clinical encounters.50,69 Still, other clinicians noted that they tended to project residual feelings of anger onto their current suicidal patients, or envied patients who seemed to have mastered their grief. Consistent with Maltsberger’s description of “atonement reactions,”40 some clinicians found themselves doing more than should be expected for their patients, even losing their sense of professional boundaries in the process. Anderson70 noted that in pushing herself beyond what she knew were her optimal clinical boundaries, she was “punishing herself” for failing to prevent her patient’s suicide because, as she realized, “doing ‘penance’ was better than feeling helpless and powerless.” And Schultz16 described how therapists may have subsequent difficulty in trusting other patients, especially if patients who completed suicide did not disclose or denied their suicidal intent.
Working toward a supportive solution
In summary, unless clinicians who lose a patient to suicide have more supportive experiences, the combination of confidentiality-related restrictions, confusion about legal/ethical repercussions, unsupportive reactions from colleagues, and unexpected impairments in clinical work are likely to lead to intensified distress, isolation, the perceived need to “hide” the impact in professional settings, and consideration of leaving the profession. However, as I will describe in Part 2 (
Bottom Line
For mental health clinicians, losing a patient to suicide is a clear occupational hazard. After a suicide loss, clinicians often experience unique personal and professional challenges, including the impact of the loss on clinical work and professional identity, legal/ethical issues, and confidentiality-related constraints on the ability to discuss and process the loss.
Related Resources
- American Association of Suicidology Clinician Survivor Task Force. www.cliniciansurvivor.org.
- Gutin N. Helping survivors in the aftermath of suicide loss. Current Psychiatry. 2018;17(8):27-33.
1. Alexander D, Klein S, Gray NM, et al. Suicide by patients: questionnaire study of its effect on consultant psychiatrists. BMJ. 2000;320(7249):1571-1574.
2. Chemtob CM, Hamada RS, Bauer G, et al. Patients’ suicides: frequency and impact on psychiatrists. Am J Psychiatry. 1988;145(2):224-228.
3. Grad OT, Zavasnik A, Groleger U. Suicide of a patient: gender differences in bereavement reactions of therapists. Suicide Life Threat Behav. 1997;27(4):379-386.
4. Ruskin R, Sakinofsky I, Bagby RM, et al. Impact of patient suicide on psychiatrists and psychiatric trainees. Acad Psychiatry. 2004;28(2):104-110.
5. Bersoff DN. Ethical conflicts in psychology, 2nd ed. Washington, DC: American Psychological Association; 1999.
6. Chemtob CM, Bauer GB, Hamada RS, et al. Patient suicide: occupational hazard for psychologists and psychiatrists. Prof Psychol Res Pr. 1989;20(5):294-300.
7. Rubin HL. Surviving a suicide in your practice. In: Blumenthal SJ, Kupfer DJ, eds. Suicide over the life cycle: risk factors, assessment, and treatment of suicidal patients. Washington, DC: American Psychiatric Press; 1990:619-636.
8. Kaye NS, Soreff SM. The psychiatrist’s role, responses, and responsibilities when a patient commits suicide. Am J Psychiatry. 1991;148(6):739-743.
9. McIntosh JL. Clinicians as survivors of suicide: bibliography. American Association of Suicidology Clinician Survivor Task Force. http://pages.iu.edu/~jmcintos/Surv.Ther.bib.htm. Updated May 19, 2019. Accessed August 26, 2019.
10. Douglas J, Brown HN. Suicide: understanding and responding: Harvard Medical School perspectives. Madison, CT: International Universities Press; 1989.
11. Farberow NL. The mental health professional as suicide survivor. Clin Neuropsychiatry. 2005;2(1):13-20.
12. Jones FA Jr. Therapists as survivors of patient suicide. In: Dunne EJ, McIntosh JL, Dunne-Maxim K, eds. Suicide and its aftermath: understanding and counseling the survivors. New York, NY: W.W. Norton; 1987;126-141.
13. Plakun EM, Tillman JG. Responding to clinicians after loss of a patient to suicide. Dir Psychiatry. 2005;25:301-310.
14. Prabhakar D, Anzia JM, Balon R, et al. “Collateral damages”: preparing residents for coping with patient suicide. Acad Psychiatry. 2013;37(6):429-30.
15. Quinnett P. QPR: for suicide prevention. QPR Institute, Inc. http://pages.iu.edu/~jmcintos/postvention.htm. Published September 21, 2009. Accessed August 26, 2019.
16. Schultz, D. Suggestions for supervisors when a therapist experiences a client’s suicide. Women Ther. 2005;28(1):59-69.
17. Spiegelman JS Jr, Werth JL Jr. Don’t forget about me: the experiences of therapists-in-training after a patient has attempted or died by suicide. Women Ther. 2005;28(1):35-57.
18. American Association of Suicidology. Clinician Survivor Task Force. Clinicians as survivors of suicide: postvention information.
19. Whitmore CA, Cook J, Salg L. Supporting residents in the wake of patient suicide. The American Journal of Psychiatry Residents’ Journal. 2017;12(1):5-7.
20. Melton B, Coverdale J. What do we teach psychiatric residents about suicide? A national survey of chief residents. Acad Psychiatry. 2009;33(1):47-50.
21. Valente SM. Psychotherapist reactions to the suicide of a patient. Am J Orthopsychiatry. 1994;64(4):614-621.
22. Jordan JR, McIntosh JL. Is suicide bereavement different? A framework for rethinking the question. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge; 2011:19-42.
23. Jordan JR, Baugher B. After suicide loss: coping with your grief, 2nd ed. Newcastle, WA: Caring People Press; 2016.
24. Brown HB. The impact of suicide on therapists in training. Compr Psychiatry. 1987;28(2):101-112.
25. Cvinar JG. Do suicide survivors suffer social stigma: a review of the literature. Perspect Psychiatr Care. 2005;41(1):14-21.
26. Feigelman W, Gorman BS, Jordan JR. Stigmatization and suicide bereavement. Death Stud. 2009;33(7):591-608.
27. Goffman E. Stigma: notes on the management of spoiled identity. New York, NY: Simon & Schuster; 1963.
28. Goldney RD. The privilege and responsibility of suicide prevention. Crisis. 2000;21(1):8-15.
29. Litman RE. When patients commit suicide. Am J Psychother. 1965;19(4):570-576.
30. Hendin H, Lipschitz A, Maltsberger JT, et al. Therapists’ reactions to patients’ suicides. Am J Psychiatry. 2000;157(12):2022-2027.
31. Rycroft P. Touching the heart and soul of therapy: surviving client suicide. Women Ther. 2004;28(1):83-94.
32. Ellis TE, Patel AB. Client suicide: what now? Cogn Behav Pract. 2012;19(2):277-287.
33. Al-Mateen CS, Jones K, Linker J, et al. Clinician response to a child who completes suicide. Child Adolesc Psychiatric Clin N Am. 2018;27(4):621-635.
34. Henry M, Séguin M, Drouin M-S. Mental health professionals’ response to the suicide of their patients [in French]. Revue Québécoise de Psychologie. 2004;25:241-257.
35. Carter RE. Some effects of client suicide on the therapist. Psychother Theory Res Practice. 1971;8(4):287-289.
36. Dewar I, Eagles J, Klein S, et al. Psychiatric trainees’ experiences of, and reactions to, patient suicide. Psychiatr Bull. 2000;24(1):20-23.
37. Gitlin M. Aftermath of a tragedy: reaction of psychiatrists to patient suicides. Psychiatr Ann. 2007;37(10):684-687.
38. Tillman JG. When a patient commits suicide: an empirical study of psychoanalytic clinicians. Inter J Psychoanal. 2006;87(1):159-177.
39. Erikson EH. Identity and the life cycle. New York, NY: International Universities Press, Inc.; 1959.
40. Maltsberger JT. The implications of patient suicide for the surviving psychotherapist. In: Jacobs D, ed. Suicide and clinical practice. Washington, DC: American Psychiatric Press; 1992:169-182.
41. Bissell BPH. The experience of the nurse therapist working with suicidal cases: a developmental study [dissertation]. Boston, MA: Boston University School of Education; 1981.
42. Kleespies PM. The stress of patient suicidal behavior: Implications for interns and training programs in psychology. Prof Psychol Res Pract. 1993;24(4):477-482.
43. Munson JS. Impact of client suicide on practitioner posttraumatic growth [dissertation]. Gainsville, Florida: University of Florida; 2009.
44. Hodgkinson PE. Responding to in-patient suicide. Br J Med Psychol. 1987;60(4):387-392.
45. Gorkin M. On the suicide of one’s patient. Bull Menninger Clin. 1985;49(1):1-9.
46. Fuentes MA, Cruz D. Posttraumatic growth: positive psychological changes after trauma. Mental Health News. 2009;11(1):31,37.
47. Doka KJ. Disenfranchised grief: new Directions, challenges, and strategies for practice. Champaign, IL: Research Press; 2002.
48. Bongar B. The suicidal patient: clinical and legal standards of care, 2nd ed. Washington, DC: American Psychological Association; 2002.
49. Peterson EM, Luoma JB, Dunne E. Suicide survivors’ perceptions of the treating clinician. Suicide Life Threat Behav. 2002;32(2):158-166.
50. Kolodny S, Binder RL, Bronstein AA, et al. The working through of patients’ suicides by four therapists. Suicide Life Threat Behav. 1979;9(1):33-46.
51. Marshall KA. When a patient commits suicide. Suicide Life Threat Behav. 1980;10(1):29-40.
52. Jobes DA, Maltsberger JT. The hazards of treating suicidal patients. In: Sussman MB, ed. A perilous calling: the hazards of psychotherapy practice. New York, NY: Wiley & Sons; 1995:200-214.
53. Castelli-Dransart DA, Gutjahr E, Gulfi A, et al. Patient suicide in institutions: emotional responses and traumatic impact on Swiss mental health professionals. Death Stud. 2014;38(1-5):315-321.
54. US Public Health Service. The Surgeon General’s call to action to prevent suicide. Washington, DC: Department of Health and Human Services; 1999.
55. Armour M. Violent death: understanding the context of traumatic and stigmatized grief. J Hum Behav Soc Environ. 2006;14(4):53-90.
56. Calhoun, LG, Allen BG. Social reactions to the survivor of a suicide in the family: a review of the literature. Omega (Westport). 1991;23(2):95-107.
57. Dunne EJ, McIntosh JL, Dunne-Maxim K, eds. Suicide and its aftermath: understanding and counseling the survivors. New York, NY: WW Norton & Co; 1987.
58. Harwood D, Hawton K, Hope J, et al. The grief experiences and needs of bereaved relatives and friends of older people dying through suicide: a descriptive and case-control study. J Affect Disord. 2002;72(2):185-194.
59. Jordan JR. Is suicide bereavement different? A reassessment of the literature. Suicide Life Threat Behav. 2001;31(1):91-102.
60. McIntosh JL. Control group studies of suicide survivors: a review and critique. Suicide Life Threat Behav. 2003;23(2):146-161.
61. Range LM. When a loss is due to suicide: unique aspects of bereavement. In: Harvey JH, ed. Perspectives on loss: a sourcebook. Philadelphia, PA: Brunner/Mazel; 1998:213-220.
62. Sveen CA, Walby FA. Suicide survivors’ mental health and grief reactions: a systematic review of controlled studies. Suicide Life Threat Behav. 2008;38(1):13-29.
63. Van Dongen CJ. Social context of postsuicide bereavement. Death Stud. 1993;17(2):125-141.
64. Bultema JK. The healing process for the multidisciplinary team: recovering post-inpatient suicide. J Psychosoc Nurs. 1994;32(2):19-24.
65. Cooper C. Patient suicide and assault: their impact on psychiatric hospital staff. J Psychosoc Nurs Ment Health Serv. 1995;33(6):26-29.
66. Foster VA, McAdams CR III. The impact of client suicide in counselor training: Implications for counselor education and supervision. Counselor Educ Supervision. 1999;39(1):22-33.
67. Little JD. Staff response to inpatient and outpatient suicide: what happened and what do we do? Aust N Z J Psychiatry. 1992;26(2):162-167.
68. Horn PJ. Therapists’ psychological adaptation to client suicidal behavior. Chicago, IL: Loyola University of Chicago; 1995.
69. Gutin N, McGann VM, Jordan JR. The impact of suicide on professional caregivers. In: Jordan J, McIntosh J, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge; 2011:93-111.
70. Anderson GO. Who, what, when, where, how, and mostly why? A therapist’s grief over the suicide of a client. Women Ther. 2004;28(1):25-34.
1. Alexander D, Klein S, Gray NM, et al. Suicide by patients: questionnaire study of its effect on consultant psychiatrists. BMJ. 2000;320(7249):1571-1574.
2. Chemtob CM, Hamada RS, Bauer G, et al. Patients’ suicides: frequency and impact on psychiatrists. Am J Psychiatry. 1988;145(2):224-228.
3. Grad OT, Zavasnik A, Groleger U. Suicide of a patient: gender differences in bereavement reactions of therapists. Suicide Life Threat Behav. 1997;27(4):379-386.
4. Ruskin R, Sakinofsky I, Bagby RM, et al. Impact of patient suicide on psychiatrists and psychiatric trainees. Acad Psychiatry. 2004;28(2):104-110.
5. Bersoff DN. Ethical conflicts in psychology, 2nd ed. Washington, DC: American Psychological Association; 1999.
6. Chemtob CM, Bauer GB, Hamada RS, et al. Patient suicide: occupational hazard for psychologists and psychiatrists. Prof Psychol Res Pr. 1989;20(5):294-300.
7. Rubin HL. Surviving a suicide in your practice. In: Blumenthal SJ, Kupfer DJ, eds. Suicide over the life cycle: risk factors, assessment, and treatment of suicidal patients. Washington, DC: American Psychiatric Press; 1990:619-636.
8. Kaye NS, Soreff SM. The psychiatrist’s role, responses, and responsibilities when a patient commits suicide. Am J Psychiatry. 1991;148(6):739-743.
9. McIntosh JL. Clinicians as survivors of suicide: bibliography. American Association of Suicidology Clinician Survivor Task Force. http://pages.iu.edu/~jmcintos/Surv.Ther.bib.htm. Updated May 19, 2019. Accessed August 26, 2019.
10. Douglas J, Brown HN. Suicide: understanding and responding: Harvard Medical School perspectives. Madison, CT: International Universities Press; 1989.
11. Farberow NL. The mental health professional as suicide survivor. Clin Neuropsychiatry. 2005;2(1):13-20.
12. Jones FA Jr. Therapists as survivors of patient suicide. In: Dunne EJ, McIntosh JL, Dunne-Maxim K, eds. Suicide and its aftermath: understanding and counseling the survivors. New York, NY: W.W. Norton; 1987;126-141.
13. Plakun EM, Tillman JG. Responding to clinicians after loss of a patient to suicide. Dir Psychiatry. 2005;25:301-310.
14. Prabhakar D, Anzia JM, Balon R, et al. “Collateral damages”: preparing residents for coping with patient suicide. Acad Psychiatry. 2013;37(6):429-30.
15. Quinnett P. QPR: for suicide prevention. QPR Institute, Inc. http://pages.iu.edu/~jmcintos/postvention.htm. Published September 21, 2009. Accessed August 26, 2019.
16. Schultz, D. Suggestions for supervisors when a therapist experiences a client’s suicide. Women Ther. 2005;28(1):59-69.
17. Spiegelman JS Jr, Werth JL Jr. Don’t forget about me: the experiences of therapists-in-training after a patient has attempted or died by suicide. Women Ther. 2005;28(1):35-57.
18. American Association of Suicidology. Clinician Survivor Task Force. Clinicians as survivors of suicide: postvention information.
19. Whitmore CA, Cook J, Salg L. Supporting residents in the wake of patient suicide. The American Journal of Psychiatry Residents’ Journal. 2017;12(1):5-7.
20. Melton B, Coverdale J. What do we teach psychiatric residents about suicide? A national survey of chief residents. Acad Psychiatry. 2009;33(1):47-50.
21. Valente SM. Psychotherapist reactions to the suicide of a patient. Am J Orthopsychiatry. 1994;64(4):614-621.
22. Jordan JR, McIntosh JL. Is suicide bereavement different? A framework for rethinking the question. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge; 2011:19-42.
23. Jordan JR, Baugher B. After suicide loss: coping with your grief, 2nd ed. Newcastle, WA: Caring People Press; 2016.
24. Brown HB. The impact of suicide on therapists in training. Compr Psychiatry. 1987;28(2):101-112.
25. Cvinar JG. Do suicide survivors suffer social stigma: a review of the literature. Perspect Psychiatr Care. 2005;41(1):14-21.
26. Feigelman W, Gorman BS, Jordan JR. Stigmatization and suicide bereavement. Death Stud. 2009;33(7):591-608.
27. Goffman E. Stigma: notes on the management of spoiled identity. New York, NY: Simon & Schuster; 1963.
28. Goldney RD. The privilege and responsibility of suicide prevention. Crisis. 2000;21(1):8-15.
29. Litman RE. When patients commit suicide. Am J Psychother. 1965;19(4):570-576.
30. Hendin H, Lipschitz A, Maltsberger JT, et al. Therapists’ reactions to patients’ suicides. Am J Psychiatry. 2000;157(12):2022-2027.
31. Rycroft P. Touching the heart and soul of therapy: surviving client suicide. Women Ther. 2004;28(1):83-94.
32. Ellis TE, Patel AB. Client suicide: what now? Cogn Behav Pract. 2012;19(2):277-287.
33. Al-Mateen CS, Jones K, Linker J, et al. Clinician response to a child who completes suicide. Child Adolesc Psychiatric Clin N Am. 2018;27(4):621-635.
34. Henry M, Séguin M, Drouin M-S. Mental health professionals’ response to the suicide of their patients [in French]. Revue Québécoise de Psychologie. 2004;25:241-257.
35. Carter RE. Some effects of client suicide on the therapist. Psychother Theory Res Practice. 1971;8(4):287-289.
36. Dewar I, Eagles J, Klein S, et al. Psychiatric trainees’ experiences of, and reactions to, patient suicide. Psychiatr Bull. 2000;24(1):20-23.
37. Gitlin M. Aftermath of a tragedy: reaction of psychiatrists to patient suicides. Psychiatr Ann. 2007;37(10):684-687.
38. Tillman JG. When a patient commits suicide: an empirical study of psychoanalytic clinicians. Inter J Psychoanal. 2006;87(1):159-177.
39. Erikson EH. Identity and the life cycle. New York, NY: International Universities Press, Inc.; 1959.
40. Maltsberger JT. The implications of patient suicide for the surviving psychotherapist. In: Jacobs D, ed. Suicide and clinical practice. Washington, DC: American Psychiatric Press; 1992:169-182.
41. Bissell BPH. The experience of the nurse therapist working with suicidal cases: a developmental study [dissertation]. Boston, MA: Boston University School of Education; 1981.
42. Kleespies PM. The stress of patient suicidal behavior: Implications for interns and training programs in psychology. Prof Psychol Res Pract. 1993;24(4):477-482.
43. Munson JS. Impact of client suicide on practitioner posttraumatic growth [dissertation]. Gainsville, Florida: University of Florida; 2009.
44. Hodgkinson PE. Responding to in-patient suicide. Br J Med Psychol. 1987;60(4):387-392.
45. Gorkin M. On the suicide of one’s patient. Bull Menninger Clin. 1985;49(1):1-9.
46. Fuentes MA, Cruz D. Posttraumatic growth: positive psychological changes after trauma. Mental Health News. 2009;11(1):31,37.
47. Doka KJ. Disenfranchised grief: new Directions, challenges, and strategies for practice. Champaign, IL: Research Press; 2002.
48. Bongar B. The suicidal patient: clinical and legal standards of care, 2nd ed. Washington, DC: American Psychological Association; 2002.
49. Peterson EM, Luoma JB, Dunne E. Suicide survivors’ perceptions of the treating clinician. Suicide Life Threat Behav. 2002;32(2):158-166.
50. Kolodny S, Binder RL, Bronstein AA, et al. The working through of patients’ suicides by four therapists. Suicide Life Threat Behav. 1979;9(1):33-46.
51. Marshall KA. When a patient commits suicide. Suicide Life Threat Behav. 1980;10(1):29-40.
52. Jobes DA, Maltsberger JT. The hazards of treating suicidal patients. In: Sussman MB, ed. A perilous calling: the hazards of psychotherapy practice. New York, NY: Wiley & Sons; 1995:200-214.
53. Castelli-Dransart DA, Gutjahr E, Gulfi A, et al. Patient suicide in institutions: emotional responses and traumatic impact on Swiss mental health professionals. Death Stud. 2014;38(1-5):315-321.
54. US Public Health Service. The Surgeon General’s call to action to prevent suicide. Washington, DC: Department of Health and Human Services; 1999.
55. Armour M. Violent death: understanding the context of traumatic and stigmatized grief. J Hum Behav Soc Environ. 2006;14(4):53-90.
56. Calhoun, LG, Allen BG. Social reactions to the survivor of a suicide in the family: a review of the literature. Omega (Westport). 1991;23(2):95-107.
57. Dunne EJ, McIntosh JL, Dunne-Maxim K, eds. Suicide and its aftermath: understanding and counseling the survivors. New York, NY: WW Norton & Co; 1987.
58. Harwood D, Hawton K, Hope J, et al. The grief experiences and needs of bereaved relatives and friends of older people dying through suicide: a descriptive and case-control study. J Affect Disord. 2002;72(2):185-194.
59. Jordan JR. Is suicide bereavement different? A reassessment of the literature. Suicide Life Threat Behav. 2001;31(1):91-102.
60. McIntosh JL. Control group studies of suicide survivors: a review and critique. Suicide Life Threat Behav. 2003;23(2):146-161.
61. Range LM. When a loss is due to suicide: unique aspects of bereavement. In: Harvey JH, ed. Perspectives on loss: a sourcebook. Philadelphia, PA: Brunner/Mazel; 1998:213-220.
62. Sveen CA, Walby FA. Suicide survivors’ mental health and grief reactions: a systematic review of controlled studies. Suicide Life Threat Behav. 2008;38(1):13-29.
63. Van Dongen CJ. Social context of postsuicide bereavement. Death Stud. 1993;17(2):125-141.
64. Bultema JK. The healing process for the multidisciplinary team: recovering post-inpatient suicide. J Psychosoc Nurs. 1994;32(2):19-24.
65. Cooper C. Patient suicide and assault: their impact on psychiatric hospital staff. J Psychosoc Nurs Ment Health Serv. 1995;33(6):26-29.
66. Foster VA, McAdams CR III. The impact of client suicide in counselor training: Implications for counselor education and supervision. Counselor Educ Supervision. 1999;39(1):22-33.
67. Little JD. Staff response to inpatient and outpatient suicide: what happened and what do we do? Aust N Z J Psychiatry. 1992;26(2):162-167.
68. Horn PJ. Therapists’ psychological adaptation to client suicidal behavior. Chicago, IL: Loyola University of Chicago; 1995.
69. Gutin N, McGann VM, Jordan JR. The impact of suicide on professional caregivers. In: Jordan J, McIntosh J, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge; 2011:93-111.
70. Anderson GO. Who, what, when, where, how, and mostly why? A therapist’s grief over the suicide of a client. Women Ther. 2004;28(1):25-34.
Helping survivors in the aftermath of suicide loss
The loss of a loved one to suicide is often experienced as “devastating.”1 While survivors of suicide loss may be able to move through the grief process without clinical support,2 the traumatic and stigmatizing nature of suicide is likely to make its aftermath more challenging to navigate than other types of loss. Sanford et al3 found that more than two-thirds of suicide loss survivors sought therapy after their loss. Further, when individuals facing these challenges present for treatment, clinicians often face challenges of their own.
Very few clinicians are trained in general grief processes,4 and even those specifically trained in grief and loss have been shown to “miss” several of the common clinical features that are unique to suicide loss.3 In my professional experience, the intensity and duration of suicide grief are often greater than they are for other losses, and many survivors of suicide loss have reported that others, including clinicians, have “pathologized” this, rather than having understood it as normative under the circumstances.
Although there is extensive literature on the aftermath of suicide for surviving loved ones, very few controlled studies have assessed interventions specifically for this population. Yet the U.S. Guidelines for Suicide Postvention5 explicitly call for improved training for those who work with suicide loss survivors, as well as research on these interventions. Jordan and McGann6 noted, “Without a full knowledge of suicide and its aftermath, it is very possible to make clinical errors which can hamper treatment.” This article summarizes what is currently known about the general experience of suicide bereavement and optimal interventions in treatment.
What makes suicide loss unique?
Suicide bereavement is distinct from other types of loss in 3 significant ways7:
- the thematic content of the grief
- the social processes surrounding the survivor
- the impact that suicide has on family systems.
Additionally, the perceived intentionality and preventability of a suicide death, as well as its stigmatized and traumatic nature, differentiate it from other types of traumatic loss.7 These elements are all likely to affect the nature, intensity, and duration of the grief.
Stigma and suicide. Stigma associated with suicide is well documented.8 Former U.S. Surgeon General David Satcher9 specifically described stigma toward suicide as one of the biggest barriers to prevention. In addition, researchers have found that the stigma associated with suicide “spills over” to the bereaved family members. Doka10,11 refers to “disenfranchised grief,” in which bereaved individuals receive the message that their grief is not legitimate, and as a result, they are likely to internalize this view. Studies have shown that individuals bereaved by suicide are also stigmatized, and are believed to be more psychologically disturbed, less likable, more blameworthy, more ashamed, and more in need of professional help than other bereaved individuals.8,12-20
These judgments often mirror suicide loss survivors’ self-punitive assessments, which then become exacerbated by and intertwined with both externally imposed and internalized stigma. Thus, it is not uncommon for survivors of suicide loss to question their own right to grieve, to report low expectations of social support, and to feel compelled to deny or hide the mode of death. To the extent that they are actively grieving, survivors of suicide loss often feel that they must do so in isolation. Thus, the perception of stigma, whether external or internalized, can have a profound effect on decisions about disclosure, requesting support, and ultimately on one’s ability to integrate the loss. Indeed, Feigelman et al21 found that stigmatization after suicide was specifically associated with ongoing grief difficulties, depression, and suicidal ideation.
Continue to: Traumatic nature of suicide
Traumatic nature of suicide. Suicide loss is also quite traumatic, and posttraumatic stress disorder (PTSD) symptoms such as shock, horror, disbelief, and intrusive/perseverative thoughts and questions, particularly in the earlier stages of grief, are common. Sanford et al3 found that the higher the level of “perceived closeness” to the deceased, the more likely that survivors of suicide loss would experience PTSD symptoms. In addition, the dramatic loss of social support following a suicide loss may itself be traumatic, which can serve to compound these difficulties. Notably, Sanford et al3 found that even for those survivors of suicide loss in treatment who endorsed PTSD symptoms, many of their treating clinicians did not assess or diagnose this disorder, thus missing an important component for treatment.
Increased risk for suicidality. Studies have shown that individuals who have lost a loved one to suicide are themselves at heightened risk for suicidal ideation and behaviors.22-27 Therefore, an assessment for suicide risk is always advisable. However, it is important to note that suicidal ideation is not uncommon and can serve different functions for survivors of suicide loss without necessarily progressing to a plan for acting on such ideations. Survivors of suicide loss may wish to “join” their loved one; to understand or identify with the mental state of the deceased; to punish themselves for failing to prevent the suicide; or to end their own pain through death. Therefore, it is crucial to assess the nature and function of expressed ideation (in addition to the presence or absence of plans) before assigning the level of risk.
Elements of suicide grief
After the loss of a loved one to suicide, the path to healing is often complex, with survivors of suicide loss enduring the following challenges:
Existential assumptions are shattered. Several authors28-30 have found that suicide loss is also likely to shatter survivors’ existential assumptions regarding their worldviews, roles, and identities, as well as religious and spiritual beliefs. As one survivor of suicide loss in my practice noted, “The world is gone, nothing is predictable anymore, and it’s no longer safe to assume anything.” Others have described feeling “fragmented” in ways they had never before experienced, and many have reported difficulties in “trusting” their own judgment, the stability of the world, and relationships. “Why?” becomes an emergent and insistent question in the survivor’s efforts to understand the suicide and (ideally) reassemble a coherent narrative around the loss.
Increased duration and intensity of grief. The duration of the grief process is likely to be affected by the traumatic nature of suicide loss, the differential social support accorded to its survivors, and the difficulty in finding systems that can validate and normalize the unique elements in suicide bereavement. The stigmatized reactions of others, particularly when internalized, can present barriers to the processing of grief. In addition, the intensity of the trauma and existential impact, as well as the perseverative nature of several of the unique themes (Box 1), can also prolong the processing and increase the intensity of suicide grief. Clinicians would do well to recognize the relatively “normative” nature of the increased duration and intensity, rather than seeing it as immediately indicative of a DSM diagnosis of complicated/prolonged grief disorder.
Box 1
Common themes in the suicide grief process
Several common themes are likely to emerge during the suicide grief process. Guilt and a sense of failure—around what one did and did not do—can be pervasive and persistent, and are often present even when not objectively warranted.
Anger and blame directed towards the deceased, other family members, and clinicians who had been treating the deceased may also be present, and may be used in efforts to deflect guilt. Any of these themes may be enlisted to create a deceptively simple narrative for understanding the reasons for the suicide.
Shame is often present, and certainly exacerbated by both external and internalized stigma. Feelings of rejection, betrayal, and abandonment by the deceased are also common, as well as fear/hypervigilance regarding the possibility of losing others to suicide. Given the intensity of suicide grief, it has been my observation that there may also be fear in relation to one's own mental status, as many otherwise healthy survivors of suicide loss have described feeling like they're "going crazy." Finally, there may also be relief, particularly if the deceased had been suffering from chronic psychiatric distress or had been cruel or abusive.
Continue to: Family disruption
Family disruption. It is not uncommon for a suicide loss to result in family disruption.6,31-32 This may manifest in the blaming of family members for “sins of omission or commission,”6 conflicts around the disclosure of the suicide both within and outside of the family, discordant grieving styles, and difficulties in understanding and attending to the needs of one’s children while grieving oneself.
Despite the common elements often seen in suicide grief, it is crucial to recognize that this process is not “one size fits all.” Not only are there individual variants, but Grad et al33 found gender-based differences in grieving styles, and cultural issues such as the “meanings” assigned to suicide, and culturally sanctioned grief rituals and behaviors that are also likely to affect how grief is experienced and expressed. In addition, personal variants such as closeness/conflicts with the deceased, histories of previous trauma or loss, pre-existing psychiatric disorders, and attachment orientation34 are likely to impact the grief process.
Losing close friends and colleagues may be similarly traumatic, but these survivors of suicide loss often receive even less social support than those who have kinship losses. Finally, when a suicide loss occurs in a professional capacity (such as the loss of a patient), this is likely to have many additional implications for one’s professional functions and identity.35
Interventions to help survivors
Several goals and “tasks” are involved in the suicide bereavement process (Box 21,6,30,36-40). These can be achieved through the following interventions: Support groups. Many survivors find that support groups that focus on suicide loss are extremely helpful, and research has supported this.1,4,41-44 Interactions with other suicide loss survivors provide hope, connection, and an “antidote” to stigma and shame. Optimally, group facilitators provide education, validation and normalization of the grief trajectory, and facilitate the sharing of both loss experiences and current functioning between group members. As a result, group participants often report renewed connections, increased efficacy in giving and accepting support, and decreased distress (including reductions in PTSD and depressive symptoms). The American Association of Suicidology (www.suicidology.org) and American Foundation of Suicide Prevention (www.afsp.org) provide contact information for suicide loss survivor groups (by geographical area) as well as information about online support groups.
Box 2
Goals and 'tasks' in suicide bereavement
The following goals and "tasks" should be part of the process of suicide bereavement:
- Reduce symptoms of posttraumatic stress disorder and other psychiatric disorders. Given the traumatic nature of the loss, an important goal is to understand and reduce posttraumatic stress disorder and other psychiatric symptoms, and incrementally improving functionality in relation to these.
- Integrate the loss. Recent authors36-38 have highlighted the need for survivors of suicide loss to "bear" and integrate the loss, as opposed to the concept of "getting over it." In these paradigms, the loss becomes an important part of one's identity, and eventually ceases to define it. Optimally, the "whole person" is remembered, not just the suicide. Part of this involves a reinvestment in life, with the acceptance of a "new normal" that takes the loss into account. It is not unusual for survivors of suicide loss to report some guilt in "moving on" and/or experiencing pleasure; often this is felt as a "betrayal" of the deceased.
- Create meaning from the loss. A major goal for those who have lost a loved one to suicide is the ability to find and/or create meaning from the loss. This would include the creation of a loss narrative39 that incorporates both ambiguity and complexity, as well as a regained/renewed sense of purpose in ongoing life.
- Develop ambiguity tolerance. A related "task" in suicide grief is the development of ambiguity tolerance, which generally includes an understanding of the complexity underlying suicide, the ability to offer oneself a "fair trial"30 in relation to one's realistic degree of responsibility, and the acceptance that many questions may remain unanswerable. In addition, in concert with the current understanding of "continuing bonds,"40 survivors should attempt to attend to the ongoing relationship with the deceased, including any "unfinished business."6
- Develop skills to manage stigmatized social responses and/or changes in family and social relationships.
- Memorialize and honor the deceased. Healing for survivors is facilitated by memorializations, which both validate the mourning process itself while also paying tribute to the richness of the deceased person's life.
- Post-traumatic growth. The relatively new understanding of "post-traumatic" growth is certainly applicable to the "unexpected gifts" many survivors of suicide loss report after they have moved through suicide grief. This includes greater understanding toward oneself, other survivors of suicide loss, and suicidal individuals; gratitude toward those who have provided support; and a desire to "use" their newfound understanding of suicide and suicide grief in ways to honor the deceased and benefit others. Feigelman et al1 found that many longer-term survivors of suicide loss engaged in both direct service and social activism around suicide pre- and postvention.
Individual treatment. The limited research on individual treatment for suicide loss survivors suggests that while most participants find it generally helpful, a significant number of others report that their therapists lack knowledge of suicide grief and endorse stigmatizing attitudes toward suicide and suicide loss survivors.45-46 In addition, Sanford et al3 found that survivors of suicide loss who endorsed PTSD symptoms were not assessed, diagnosed, or treated for these symptoms.
Continue to: This speaks to the importance of understanding what is...
This speaks to the importance of understanding what is “normative” for survivors of suicide loss. In general, “normalization” and psychoeducation about the suicide grief trajectory can play an important role in work with survivors of suicide loss, even in the presence of diagnosable disorders. While PTSD, depressive symptoms, and suicidal ideation are not uncommon in suicide loss survivors, and certainly may warrant clinical assessment and treatment, it can be helpful (and less stigmatizing) for your patients to know that these diagnoses are relatively common and understandable in the context of this devastating experience. For instance, survivors of suicide loss often report feeling relieved when clinicians explain the connections between traumatic loss and PTSD and/or depressive symptoms, and this can also help to relieve secondary anxiety about “going crazy.” Many survivors of suicide loss also describe feeling as though they are functioning on “autopilot” in the earlier stages of grief; it can help them understand the “function” of compartmentalization as potentially adaptive in the short run.
Suicide loss survivors may also find it helpful to learn about suicidal states of mind and their relationships to any types of mental illness their loved ones had struggled with.47
Your role: Help survivors integrate the loss
Before beginning treatment with an individual who has lost a loved one to suicide, clinicians should thoroughly explore their own understanding of and experience with suicide, including assumptions around causation, internalized stigma about suicidal individuals and survivors of suicide loss, their own history of suicide loss or suicidality, cultural/religious attitudes, and anxiety/defenses associated with the topic of suicide. These factors, particularly when unexamined, are likely to impact the treatment relationship and one’s clinical efficacy.
In concert with the existing literature, consider the potential goals and tasks involved in the integration of the individual’s suicide loss, along with any individual factors/variants that may impact the grief trajectory. Kosminsky and Jordon34 described the role of the clinician in this situation as a “transitional attachment figure” who facilitates the management and integration of the loss into the creation of what survivors of suicide loss have termed a “new normal.”
Because suicide loss is often associated with PTSD and other psychiatric illnesses (eg, depression, suicidality, substance abuse), it is essential to balance the assessment and treatment of these issues with attention to grief issues as needed. Again, to the extent that such issues have arisen primarily in the wake of the suicide loss, it can be helpful for patients to understand their connection to the context of the loss.
Continue to: Ideally, the clinician should...
Ideally, the clinician should be “present” with the patient’s pain, normative guilt, and rumination, without attempting to quickly eliminate or “fix” it or provide premature reassurance that the survivor of suicide loss “did nothing wrong.” Rather, as Jordan6 suggests, the clinician should act to promote a “fair trial” with respect to the patient’s guilt and blame, with an understanding of the “tyranny of hindsight.” The promotion of ambiguity tolerance should also play a role in coming to terms with many questions that may remain unanswered.
Optimally, clinicians should encourage patients to attend to their ongoing relationship with the deceased, particularly in the service of resolving “unfinished business,” ultimately integrating the loss into memories of the whole person. In line with this, survivors of suicide loss may be encouraged to create a narrative of the loss that incorporates both complexity and ambiguity. In the service of supporting the suicide loss survivor’s reinvestment in life, it is often helpful to facilitate their ability to anticipate and cope with triggers, such as anniversaries, birthdays, or holidays, as well as to develop and use skills for managing difficult or stigmatizing social or cultural reactions.
Any disruptions in family functioning should also be addressed. Psychoeducation about discordant grieving styles (particularly around gender) and the support of children’s grief may be helpful, and referrals to family or couples therapists should be considered as needed. Finally, the facilitation of suicide loss survivors’ creation of memorializations or rituals can help promote healing and make their loss meaningful.
Bottom Line
Losing a loved one to suicide is often a devastating and traumatic experience, but with optimal support, most survivors are ultimately able to integrate the loss and grow as a result. Understanding the suicide grief trajectory, as well as general guidelines for treatment, will facilitate healing and growth in the aftermath of suicide loss.
Related Resources
- Jordan JR, McIntosh JL. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011.
- American Association of Suicidology. http://www.suicidology.org/.
- American Foundation for Suicide Prevention. https://afsp.org/.
1. Feigelman W, Jordan JR, McIntosh JL, et al. Devastating losses: how parents cope with the death of a child to suicide or drugs. New York, NY: Springer; 2012.
2. McIntosh JL. Research on survivors of suicide. In: Stimming MT, Stimming M, eds. Before their time: adult children’s experiences of parental suicide. Philadelphia, PA: Temple University Press; 1999:157-180.
3. Sanford RL, Cerel J, McGann VL, et al. Suicide loss survivors’ experiences with therapy: Implications for clinical practice. Community Ment Health J. 2016;5(2):551-558.
4. Jordan JR, McMenamy J. Interventions for suicide survivors: a review of the literature. Suicide Life Threat Behav. 2004;34(4):337-349.
5. Survivors of Suicide Loss Task Force. Responding to grief, trauma, & distress after a suicide: U.S. national guidelines. Washington, DC: National Action Alliance for Suicide Prevention; 2015.
6. Jordan JR, McGann V. Clinical work with suicide loss survivors: implications of the U.S. postvention guidelines. Death Stud. 2017;41(10):659-672.
7. Jordan JR. Is suicide bereavement different? A reassessment of the literature. Suicide Life Threat Behav. 2001;31(1):91-102.
8. Cvinar JG. Do suicide survivors suffer social stigma: a review of the literature. Perspect Psychiatr Care. 2005;41(1):14-21.
9. U.S. Public Health Service. The Surgeon General’s call to action to prevent suicide. Washington, DC: Department of Health and Human Services; 1999.
10. Doka KJ. Disenfranchised grief: recognizing hidden sorrow. Lexington, MA: Lexington; 1989.
11. Doka KJ. Disenfranchised grief: new directions, challenges, and strategies for practice. Champaign, IL: Research Press; 2002.
12. McIntosh JL. Suicide survivors: the aftermath of suicide and suicidal behavior. In: Bryant CD, ed. Handbook of death & dying. Vol. 1. Thousand Oaks, CA: SAGE Publications; 2003:339-350.
13. Jordan, JR, McIntosh, JL. Is suicide bereavement different? A framework for rethinking the question. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:19-42.
14. Dunne EJ, McIntosh JL, Dunne-Maxim K, eds. Suicide and its aftermath: understanding and counseling the survivors. New York, NY: W.W. Norton & Co.; 1987.
15. Harwood D, Hawton K, Hope T, et al. The grief experiences and needs of bereaved relatives and friends of older people dying through suicide: a descriptive and case-control study. J Affect Disord. 2002;72(2):185-194.
16. Armour, M. Violent death: understanding the context of traumatic and stigmatized grief. J Hum Behav Soc Environ. 2006;14(4):53-90.
17. Van Dongen CJ. Social context of postsuicide bereavement. Death Stud. 1993;17(2):125-141.
18. Calhoun LG, Allen BG. Social reactions to the survivor of a suicide in the family: A review of the literature. Omega – Journal of Death and Dying. 1991;23(2):95-107.
19. Range LM. When a loss is due to suicide: unique aspects of bereavement. In: Harvey JH, ed. Perspectives on loss: a sourcebook. Philadelphia, PA: Brunner/Mazel; 1998:213-220.
20. Sveen CA, Walby FA. Suicide survivors’ mental health and grief reactions: a systematic review of controlled studies. Suicide Life Threat Behav. 2008;38(1):13-29.
21. Feigelman W, Gorman BS, Jordan JR. Stigmatization and suicide bereavement. Death Stud. 2009;33(7):591-608.
22. Shneidman ES. Foreword. In: Cain AC, ed. Survivors of suicide. Springfield, IL: Charles C. Thomas; 1972:ix-xi.
23. Jordan JR, McIntosh, JL. Suicide bereavement: Why study survivors of suicide loss? In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:3-18.
24. Agerbo E. Midlife suicide risk, partner’s psychiatric illness, spouse and child bereavement by suicide or other modes of death: a gender specific study. J Epidemiol Community Health. 2005;59(5):407-412.
25. Hedström P, Liu KY, Nordvik MK. Interaction domains and suicide: a population-based panel study of suicides in Stockholm, 1991-1999. Soc Forces. 2008;87(2):713-740.
26. Qin P, Agerbo E, Mortensen PB. Suicide risk in relation to family history of completed suicide and psychiatric disorders: a nested case-control study based on longitudinal registers. Lancet. 2002;360(9340):1126-1130.
27. Qin P, Mortensen PB. The impact of parental status on the risk of completed suicide. Arch Gen Psychiatry. 2003;60(8):797-802.
28. Neimeyer RA, Sands D. Suicide loss and the quest for meaning. In: Andriessen K, Krysinska K, Grad OT, eds. Postvention in action: the international handbook of suicide bereavement support. Cambridge, MA: Hogrefe; 2017:71-84.
29. Sands DC, Jordan JR, Neimeyer RA. The meanings of suicide: A narrative approach to healing. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:249-282.
30. Jordan JR. Principles of grief counseling with adult survivors. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:179-224.
31. Cerel J, Jordan JR, Duberstein PR. The impact of suicide on the family. Crisis. 2008;29:38-44.
32. Kaslow NJ, Samples TC, Rhodes M, et al. A family-oriented and culturally sensitive postvention approach with suicide survivors. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:301-323.
33. Grad OT, Treven M, Krysinska K. Suicide bereavement and gender. In: Andriessen K, Krysinska K, Grad OT, eds. Postvention in action: the international handbook of suicide bereavement support. Cambridge, MA: Hogrefe; 2017:39-49.
34. Kosminsky PS, Jordan JR. Attachment-informed grief therapy: the clinician’s guide to foundations and applications. New York, NY: Routledge; 2016.
35. Gutin N, McGann VL, Jordan JR. The impact of suicide on professional caregivers. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:93-111.
36. Jordan JR. Bereavement after suicide. Psychiatr Ann. 2008;38(10):679-685.
37. Jordan JR. After suicide: clinical work with survivors. Grief Matters. 2009;12(1):4-9.
38. Neimeyer, RA. Traumatic loss and the reconstruction of meaning. J Palliat Med. 2002;5(6):935-942; discussion 942-943.
39. Neimeyer R, ed. Meaning reconstruction & the experience of loss. Washington, DC: American Psychological Association; 2001.
40. Klass, D. Sorrow and solace: Neglected areas in bereavement research. Death Stud. 2013;37(7):597-616.
41. Farberow NL. The Los Angeles Survivors-After-Suicide program: an evaluation. Crisis. 1992;13(1):23-34.
42. McDaid C, Trowman R, Golder S, et al. Interventions for people bereaved through suicide: systematic review. Br J Psychiatry. 2008;193(6):438-443.
43. Groos AD, Shakespeare-Finch J. Positive experiences for participants in suicide bereavement groups: a grounded theory model. Death Stud. 2013;37(1):1-24.
44. Jordan JR. Group work with suicide survivors. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:283-300.
45. Wilson A, Marshall A. The support needs and experiences of suicidally bereaved family and friends. Death Stud. 2010;34(7):625-640.
46. McKinnon JM, Chonody J. Exploring the formal supports used by people bereaved through suicide: a qualitative study. Soc Work Ment Health. 2014;12(3):231-248.
47. Myers MF, Fine C. Touched by suicide: hope and healing after loss. New York, NY: Gotham Books; 2006.
The loss of a loved one to suicide is often experienced as “devastating.”1 While survivors of suicide loss may be able to move through the grief process without clinical support,2 the traumatic and stigmatizing nature of suicide is likely to make its aftermath more challenging to navigate than other types of loss. Sanford et al3 found that more than two-thirds of suicide loss survivors sought therapy after their loss. Further, when individuals facing these challenges present for treatment, clinicians often face challenges of their own.
Very few clinicians are trained in general grief processes,4 and even those specifically trained in grief and loss have been shown to “miss” several of the common clinical features that are unique to suicide loss.3 In my professional experience, the intensity and duration of suicide grief are often greater than they are for other losses, and many survivors of suicide loss have reported that others, including clinicians, have “pathologized” this, rather than having understood it as normative under the circumstances.
Although there is extensive literature on the aftermath of suicide for surviving loved ones, very few controlled studies have assessed interventions specifically for this population. Yet the U.S. Guidelines for Suicide Postvention5 explicitly call for improved training for those who work with suicide loss survivors, as well as research on these interventions. Jordan and McGann6 noted, “Without a full knowledge of suicide and its aftermath, it is very possible to make clinical errors which can hamper treatment.” This article summarizes what is currently known about the general experience of suicide bereavement and optimal interventions in treatment.
What makes suicide loss unique?
Suicide bereavement is distinct from other types of loss in 3 significant ways7:
- the thematic content of the grief
- the social processes surrounding the survivor
- the impact that suicide has on family systems.
Additionally, the perceived intentionality and preventability of a suicide death, as well as its stigmatized and traumatic nature, differentiate it from other types of traumatic loss.7 These elements are all likely to affect the nature, intensity, and duration of the grief.
Stigma and suicide. Stigma associated with suicide is well documented.8 Former U.S. Surgeon General David Satcher9 specifically described stigma toward suicide as one of the biggest barriers to prevention. In addition, researchers have found that the stigma associated with suicide “spills over” to the bereaved family members. Doka10,11 refers to “disenfranchised grief,” in which bereaved individuals receive the message that their grief is not legitimate, and as a result, they are likely to internalize this view. Studies have shown that individuals bereaved by suicide are also stigmatized, and are believed to be more psychologically disturbed, less likable, more blameworthy, more ashamed, and more in need of professional help than other bereaved individuals.8,12-20
These judgments often mirror suicide loss survivors’ self-punitive assessments, which then become exacerbated by and intertwined with both externally imposed and internalized stigma. Thus, it is not uncommon for survivors of suicide loss to question their own right to grieve, to report low expectations of social support, and to feel compelled to deny or hide the mode of death. To the extent that they are actively grieving, survivors of suicide loss often feel that they must do so in isolation. Thus, the perception of stigma, whether external or internalized, can have a profound effect on decisions about disclosure, requesting support, and ultimately on one’s ability to integrate the loss. Indeed, Feigelman et al21 found that stigmatization after suicide was specifically associated with ongoing grief difficulties, depression, and suicidal ideation.
Continue to: Traumatic nature of suicide
Traumatic nature of suicide. Suicide loss is also quite traumatic, and posttraumatic stress disorder (PTSD) symptoms such as shock, horror, disbelief, and intrusive/perseverative thoughts and questions, particularly in the earlier stages of grief, are common. Sanford et al3 found that the higher the level of “perceived closeness” to the deceased, the more likely that survivors of suicide loss would experience PTSD symptoms. In addition, the dramatic loss of social support following a suicide loss may itself be traumatic, which can serve to compound these difficulties. Notably, Sanford et al3 found that even for those survivors of suicide loss in treatment who endorsed PTSD symptoms, many of their treating clinicians did not assess or diagnose this disorder, thus missing an important component for treatment.
Increased risk for suicidality. Studies have shown that individuals who have lost a loved one to suicide are themselves at heightened risk for suicidal ideation and behaviors.22-27 Therefore, an assessment for suicide risk is always advisable. However, it is important to note that suicidal ideation is not uncommon and can serve different functions for survivors of suicide loss without necessarily progressing to a plan for acting on such ideations. Survivors of suicide loss may wish to “join” their loved one; to understand or identify with the mental state of the deceased; to punish themselves for failing to prevent the suicide; or to end their own pain through death. Therefore, it is crucial to assess the nature and function of expressed ideation (in addition to the presence or absence of plans) before assigning the level of risk.
Elements of suicide grief
After the loss of a loved one to suicide, the path to healing is often complex, with survivors of suicide loss enduring the following challenges:
Existential assumptions are shattered. Several authors28-30 have found that suicide loss is also likely to shatter survivors’ existential assumptions regarding their worldviews, roles, and identities, as well as religious and spiritual beliefs. As one survivor of suicide loss in my practice noted, “The world is gone, nothing is predictable anymore, and it’s no longer safe to assume anything.” Others have described feeling “fragmented” in ways they had never before experienced, and many have reported difficulties in “trusting” their own judgment, the stability of the world, and relationships. “Why?” becomes an emergent and insistent question in the survivor’s efforts to understand the suicide and (ideally) reassemble a coherent narrative around the loss.
Increased duration and intensity of grief. The duration of the grief process is likely to be affected by the traumatic nature of suicide loss, the differential social support accorded to its survivors, and the difficulty in finding systems that can validate and normalize the unique elements in suicide bereavement. The stigmatized reactions of others, particularly when internalized, can present barriers to the processing of grief. In addition, the intensity of the trauma and existential impact, as well as the perseverative nature of several of the unique themes (Box 1), can also prolong the processing and increase the intensity of suicide grief. Clinicians would do well to recognize the relatively “normative” nature of the increased duration and intensity, rather than seeing it as immediately indicative of a DSM diagnosis of complicated/prolonged grief disorder.
Box 1
Common themes in the suicide grief process
Several common themes are likely to emerge during the suicide grief process. Guilt and a sense of failure—around what one did and did not do—can be pervasive and persistent, and are often present even when not objectively warranted.
Anger and blame directed towards the deceased, other family members, and clinicians who had been treating the deceased may also be present, and may be used in efforts to deflect guilt. Any of these themes may be enlisted to create a deceptively simple narrative for understanding the reasons for the suicide.
Shame is often present, and certainly exacerbated by both external and internalized stigma. Feelings of rejection, betrayal, and abandonment by the deceased are also common, as well as fear/hypervigilance regarding the possibility of losing others to suicide. Given the intensity of suicide grief, it has been my observation that there may also be fear in relation to one's own mental status, as many otherwise healthy survivors of suicide loss have described feeling like they're "going crazy." Finally, there may also be relief, particularly if the deceased had been suffering from chronic psychiatric distress or had been cruel or abusive.
Continue to: Family disruption
Family disruption. It is not uncommon for a suicide loss to result in family disruption.6,31-32 This may manifest in the blaming of family members for “sins of omission or commission,”6 conflicts around the disclosure of the suicide both within and outside of the family, discordant grieving styles, and difficulties in understanding and attending to the needs of one’s children while grieving oneself.
Despite the common elements often seen in suicide grief, it is crucial to recognize that this process is not “one size fits all.” Not only are there individual variants, but Grad et al33 found gender-based differences in grieving styles, and cultural issues such as the “meanings” assigned to suicide, and culturally sanctioned grief rituals and behaviors that are also likely to affect how grief is experienced and expressed. In addition, personal variants such as closeness/conflicts with the deceased, histories of previous trauma or loss, pre-existing psychiatric disorders, and attachment orientation34 are likely to impact the grief process.
Losing close friends and colleagues may be similarly traumatic, but these survivors of suicide loss often receive even less social support than those who have kinship losses. Finally, when a suicide loss occurs in a professional capacity (such as the loss of a patient), this is likely to have many additional implications for one’s professional functions and identity.35
Interventions to help survivors
Several goals and “tasks” are involved in the suicide bereavement process (Box 21,6,30,36-40). These can be achieved through the following interventions: Support groups. Many survivors find that support groups that focus on suicide loss are extremely helpful, and research has supported this.1,4,41-44 Interactions with other suicide loss survivors provide hope, connection, and an “antidote” to stigma and shame. Optimally, group facilitators provide education, validation and normalization of the grief trajectory, and facilitate the sharing of both loss experiences and current functioning between group members. As a result, group participants often report renewed connections, increased efficacy in giving and accepting support, and decreased distress (including reductions in PTSD and depressive symptoms). The American Association of Suicidology (www.suicidology.org) and American Foundation of Suicide Prevention (www.afsp.org) provide contact information for suicide loss survivor groups (by geographical area) as well as information about online support groups.
Box 2
Goals and 'tasks' in suicide bereavement
The following goals and "tasks" should be part of the process of suicide bereavement:
- Reduce symptoms of posttraumatic stress disorder and other psychiatric disorders. Given the traumatic nature of the loss, an important goal is to understand and reduce posttraumatic stress disorder and other psychiatric symptoms, and incrementally improving functionality in relation to these.
- Integrate the loss. Recent authors36-38 have highlighted the need for survivors of suicide loss to "bear" and integrate the loss, as opposed to the concept of "getting over it." In these paradigms, the loss becomes an important part of one's identity, and eventually ceases to define it. Optimally, the "whole person" is remembered, not just the suicide. Part of this involves a reinvestment in life, with the acceptance of a "new normal" that takes the loss into account. It is not unusual for survivors of suicide loss to report some guilt in "moving on" and/or experiencing pleasure; often this is felt as a "betrayal" of the deceased.
- Create meaning from the loss. A major goal for those who have lost a loved one to suicide is the ability to find and/or create meaning from the loss. This would include the creation of a loss narrative39 that incorporates both ambiguity and complexity, as well as a regained/renewed sense of purpose in ongoing life.
- Develop ambiguity tolerance. A related "task" in suicide grief is the development of ambiguity tolerance, which generally includes an understanding of the complexity underlying suicide, the ability to offer oneself a "fair trial"30 in relation to one's realistic degree of responsibility, and the acceptance that many questions may remain unanswerable. In addition, in concert with the current understanding of "continuing bonds,"40 survivors should attempt to attend to the ongoing relationship with the deceased, including any "unfinished business."6
- Develop skills to manage stigmatized social responses and/or changes in family and social relationships.
- Memorialize and honor the deceased. Healing for survivors is facilitated by memorializations, which both validate the mourning process itself while also paying tribute to the richness of the deceased person's life.
- Post-traumatic growth. The relatively new understanding of "post-traumatic" growth is certainly applicable to the "unexpected gifts" many survivors of suicide loss report after they have moved through suicide grief. This includes greater understanding toward oneself, other survivors of suicide loss, and suicidal individuals; gratitude toward those who have provided support; and a desire to "use" their newfound understanding of suicide and suicide grief in ways to honor the deceased and benefit others. Feigelman et al1 found that many longer-term survivors of suicide loss engaged in both direct service and social activism around suicide pre- and postvention.
Individual treatment. The limited research on individual treatment for suicide loss survivors suggests that while most participants find it generally helpful, a significant number of others report that their therapists lack knowledge of suicide grief and endorse stigmatizing attitudes toward suicide and suicide loss survivors.45-46 In addition, Sanford et al3 found that survivors of suicide loss who endorsed PTSD symptoms were not assessed, diagnosed, or treated for these symptoms.
Continue to: This speaks to the importance of understanding what is...
This speaks to the importance of understanding what is “normative” for survivors of suicide loss. In general, “normalization” and psychoeducation about the suicide grief trajectory can play an important role in work with survivors of suicide loss, even in the presence of diagnosable disorders. While PTSD, depressive symptoms, and suicidal ideation are not uncommon in suicide loss survivors, and certainly may warrant clinical assessment and treatment, it can be helpful (and less stigmatizing) for your patients to know that these diagnoses are relatively common and understandable in the context of this devastating experience. For instance, survivors of suicide loss often report feeling relieved when clinicians explain the connections between traumatic loss and PTSD and/or depressive symptoms, and this can also help to relieve secondary anxiety about “going crazy.” Many survivors of suicide loss also describe feeling as though they are functioning on “autopilot” in the earlier stages of grief; it can help them understand the “function” of compartmentalization as potentially adaptive in the short run.
Suicide loss survivors may also find it helpful to learn about suicidal states of mind and their relationships to any types of mental illness their loved ones had struggled with.47
Your role: Help survivors integrate the loss
Before beginning treatment with an individual who has lost a loved one to suicide, clinicians should thoroughly explore their own understanding of and experience with suicide, including assumptions around causation, internalized stigma about suicidal individuals and survivors of suicide loss, their own history of suicide loss or suicidality, cultural/religious attitudes, and anxiety/defenses associated with the topic of suicide. These factors, particularly when unexamined, are likely to impact the treatment relationship and one’s clinical efficacy.
In concert with the existing literature, consider the potential goals and tasks involved in the integration of the individual’s suicide loss, along with any individual factors/variants that may impact the grief trajectory. Kosminsky and Jordon34 described the role of the clinician in this situation as a “transitional attachment figure” who facilitates the management and integration of the loss into the creation of what survivors of suicide loss have termed a “new normal.”
Because suicide loss is often associated with PTSD and other psychiatric illnesses (eg, depression, suicidality, substance abuse), it is essential to balance the assessment and treatment of these issues with attention to grief issues as needed. Again, to the extent that such issues have arisen primarily in the wake of the suicide loss, it can be helpful for patients to understand their connection to the context of the loss.
Continue to: Ideally, the clinician should...
Ideally, the clinician should be “present” with the patient’s pain, normative guilt, and rumination, without attempting to quickly eliminate or “fix” it or provide premature reassurance that the survivor of suicide loss “did nothing wrong.” Rather, as Jordan6 suggests, the clinician should act to promote a “fair trial” with respect to the patient’s guilt and blame, with an understanding of the “tyranny of hindsight.” The promotion of ambiguity tolerance should also play a role in coming to terms with many questions that may remain unanswered.
Optimally, clinicians should encourage patients to attend to their ongoing relationship with the deceased, particularly in the service of resolving “unfinished business,” ultimately integrating the loss into memories of the whole person. In line with this, survivors of suicide loss may be encouraged to create a narrative of the loss that incorporates both complexity and ambiguity. In the service of supporting the suicide loss survivor’s reinvestment in life, it is often helpful to facilitate their ability to anticipate and cope with triggers, such as anniversaries, birthdays, or holidays, as well as to develop and use skills for managing difficult or stigmatizing social or cultural reactions.
Any disruptions in family functioning should also be addressed. Psychoeducation about discordant grieving styles (particularly around gender) and the support of children’s grief may be helpful, and referrals to family or couples therapists should be considered as needed. Finally, the facilitation of suicide loss survivors’ creation of memorializations or rituals can help promote healing and make their loss meaningful.
Bottom Line
Losing a loved one to suicide is often a devastating and traumatic experience, but with optimal support, most survivors are ultimately able to integrate the loss and grow as a result. Understanding the suicide grief trajectory, as well as general guidelines for treatment, will facilitate healing and growth in the aftermath of suicide loss.
Related Resources
- Jordan JR, McIntosh JL. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011.
- American Association of Suicidology. http://www.suicidology.org/.
- American Foundation for Suicide Prevention. https://afsp.org/.
The loss of a loved one to suicide is often experienced as “devastating.”1 While survivors of suicide loss may be able to move through the grief process without clinical support,2 the traumatic and stigmatizing nature of suicide is likely to make its aftermath more challenging to navigate than other types of loss. Sanford et al3 found that more than two-thirds of suicide loss survivors sought therapy after their loss. Further, when individuals facing these challenges present for treatment, clinicians often face challenges of their own.
Very few clinicians are trained in general grief processes,4 and even those specifically trained in grief and loss have been shown to “miss” several of the common clinical features that are unique to suicide loss.3 In my professional experience, the intensity and duration of suicide grief are often greater than they are for other losses, and many survivors of suicide loss have reported that others, including clinicians, have “pathologized” this, rather than having understood it as normative under the circumstances.
Although there is extensive literature on the aftermath of suicide for surviving loved ones, very few controlled studies have assessed interventions specifically for this population. Yet the U.S. Guidelines for Suicide Postvention5 explicitly call for improved training for those who work with suicide loss survivors, as well as research on these interventions. Jordan and McGann6 noted, “Without a full knowledge of suicide and its aftermath, it is very possible to make clinical errors which can hamper treatment.” This article summarizes what is currently known about the general experience of suicide bereavement and optimal interventions in treatment.
What makes suicide loss unique?
Suicide bereavement is distinct from other types of loss in 3 significant ways7:
- the thematic content of the grief
- the social processes surrounding the survivor
- the impact that suicide has on family systems.
Additionally, the perceived intentionality and preventability of a suicide death, as well as its stigmatized and traumatic nature, differentiate it from other types of traumatic loss.7 These elements are all likely to affect the nature, intensity, and duration of the grief.
Stigma and suicide. Stigma associated with suicide is well documented.8 Former U.S. Surgeon General David Satcher9 specifically described stigma toward suicide as one of the biggest barriers to prevention. In addition, researchers have found that the stigma associated with suicide “spills over” to the bereaved family members. Doka10,11 refers to “disenfranchised grief,” in which bereaved individuals receive the message that their grief is not legitimate, and as a result, they are likely to internalize this view. Studies have shown that individuals bereaved by suicide are also stigmatized, and are believed to be more psychologically disturbed, less likable, more blameworthy, more ashamed, and more in need of professional help than other bereaved individuals.8,12-20
These judgments often mirror suicide loss survivors’ self-punitive assessments, which then become exacerbated by and intertwined with both externally imposed and internalized stigma. Thus, it is not uncommon for survivors of suicide loss to question their own right to grieve, to report low expectations of social support, and to feel compelled to deny or hide the mode of death. To the extent that they are actively grieving, survivors of suicide loss often feel that they must do so in isolation. Thus, the perception of stigma, whether external or internalized, can have a profound effect on decisions about disclosure, requesting support, and ultimately on one’s ability to integrate the loss. Indeed, Feigelman et al21 found that stigmatization after suicide was specifically associated with ongoing grief difficulties, depression, and suicidal ideation.
Continue to: Traumatic nature of suicide
Traumatic nature of suicide. Suicide loss is also quite traumatic, and posttraumatic stress disorder (PTSD) symptoms such as shock, horror, disbelief, and intrusive/perseverative thoughts and questions, particularly in the earlier stages of grief, are common. Sanford et al3 found that the higher the level of “perceived closeness” to the deceased, the more likely that survivors of suicide loss would experience PTSD symptoms. In addition, the dramatic loss of social support following a suicide loss may itself be traumatic, which can serve to compound these difficulties. Notably, Sanford et al3 found that even for those survivors of suicide loss in treatment who endorsed PTSD symptoms, many of their treating clinicians did not assess or diagnose this disorder, thus missing an important component for treatment.
Increased risk for suicidality. Studies have shown that individuals who have lost a loved one to suicide are themselves at heightened risk for suicidal ideation and behaviors.22-27 Therefore, an assessment for suicide risk is always advisable. However, it is important to note that suicidal ideation is not uncommon and can serve different functions for survivors of suicide loss without necessarily progressing to a plan for acting on such ideations. Survivors of suicide loss may wish to “join” their loved one; to understand or identify with the mental state of the deceased; to punish themselves for failing to prevent the suicide; or to end their own pain through death. Therefore, it is crucial to assess the nature and function of expressed ideation (in addition to the presence or absence of plans) before assigning the level of risk.
Elements of suicide grief
After the loss of a loved one to suicide, the path to healing is often complex, with survivors of suicide loss enduring the following challenges:
Existential assumptions are shattered. Several authors28-30 have found that suicide loss is also likely to shatter survivors’ existential assumptions regarding their worldviews, roles, and identities, as well as religious and spiritual beliefs. As one survivor of suicide loss in my practice noted, “The world is gone, nothing is predictable anymore, and it’s no longer safe to assume anything.” Others have described feeling “fragmented” in ways they had never before experienced, and many have reported difficulties in “trusting” their own judgment, the stability of the world, and relationships. “Why?” becomes an emergent and insistent question in the survivor’s efforts to understand the suicide and (ideally) reassemble a coherent narrative around the loss.
Increased duration and intensity of grief. The duration of the grief process is likely to be affected by the traumatic nature of suicide loss, the differential social support accorded to its survivors, and the difficulty in finding systems that can validate and normalize the unique elements in suicide bereavement. The stigmatized reactions of others, particularly when internalized, can present barriers to the processing of grief. In addition, the intensity of the trauma and existential impact, as well as the perseverative nature of several of the unique themes (Box 1), can also prolong the processing and increase the intensity of suicide grief. Clinicians would do well to recognize the relatively “normative” nature of the increased duration and intensity, rather than seeing it as immediately indicative of a DSM diagnosis of complicated/prolonged grief disorder.
Box 1
Common themes in the suicide grief process
Several common themes are likely to emerge during the suicide grief process. Guilt and a sense of failure—around what one did and did not do—can be pervasive and persistent, and are often present even when not objectively warranted.
Anger and blame directed towards the deceased, other family members, and clinicians who had been treating the deceased may also be present, and may be used in efforts to deflect guilt. Any of these themes may be enlisted to create a deceptively simple narrative for understanding the reasons for the suicide.
Shame is often present, and certainly exacerbated by both external and internalized stigma. Feelings of rejection, betrayal, and abandonment by the deceased are also common, as well as fear/hypervigilance regarding the possibility of losing others to suicide. Given the intensity of suicide grief, it has been my observation that there may also be fear in relation to one's own mental status, as many otherwise healthy survivors of suicide loss have described feeling like they're "going crazy." Finally, there may also be relief, particularly if the deceased had been suffering from chronic psychiatric distress or had been cruel or abusive.
Continue to: Family disruption
Family disruption. It is not uncommon for a suicide loss to result in family disruption.6,31-32 This may manifest in the blaming of family members for “sins of omission or commission,”6 conflicts around the disclosure of the suicide both within and outside of the family, discordant grieving styles, and difficulties in understanding and attending to the needs of one’s children while grieving oneself.
Despite the common elements often seen in suicide grief, it is crucial to recognize that this process is not “one size fits all.” Not only are there individual variants, but Grad et al33 found gender-based differences in grieving styles, and cultural issues such as the “meanings” assigned to suicide, and culturally sanctioned grief rituals and behaviors that are also likely to affect how grief is experienced and expressed. In addition, personal variants such as closeness/conflicts with the deceased, histories of previous trauma or loss, pre-existing psychiatric disorders, and attachment orientation34 are likely to impact the grief process.
Losing close friends and colleagues may be similarly traumatic, but these survivors of suicide loss often receive even less social support than those who have kinship losses. Finally, when a suicide loss occurs in a professional capacity (such as the loss of a patient), this is likely to have many additional implications for one’s professional functions and identity.35
Interventions to help survivors
Several goals and “tasks” are involved in the suicide bereavement process (Box 21,6,30,36-40). These can be achieved through the following interventions: Support groups. Many survivors find that support groups that focus on suicide loss are extremely helpful, and research has supported this.1,4,41-44 Interactions with other suicide loss survivors provide hope, connection, and an “antidote” to stigma and shame. Optimally, group facilitators provide education, validation and normalization of the grief trajectory, and facilitate the sharing of both loss experiences and current functioning between group members. As a result, group participants often report renewed connections, increased efficacy in giving and accepting support, and decreased distress (including reductions in PTSD and depressive symptoms). The American Association of Suicidology (www.suicidology.org) and American Foundation of Suicide Prevention (www.afsp.org) provide contact information for suicide loss survivor groups (by geographical area) as well as information about online support groups.
Box 2
Goals and 'tasks' in suicide bereavement
The following goals and "tasks" should be part of the process of suicide bereavement:
- Reduce symptoms of posttraumatic stress disorder and other psychiatric disorders. Given the traumatic nature of the loss, an important goal is to understand and reduce posttraumatic stress disorder and other psychiatric symptoms, and incrementally improving functionality in relation to these.
- Integrate the loss. Recent authors36-38 have highlighted the need for survivors of suicide loss to "bear" and integrate the loss, as opposed to the concept of "getting over it." In these paradigms, the loss becomes an important part of one's identity, and eventually ceases to define it. Optimally, the "whole person" is remembered, not just the suicide. Part of this involves a reinvestment in life, with the acceptance of a "new normal" that takes the loss into account. It is not unusual for survivors of suicide loss to report some guilt in "moving on" and/or experiencing pleasure; often this is felt as a "betrayal" of the deceased.
- Create meaning from the loss. A major goal for those who have lost a loved one to suicide is the ability to find and/or create meaning from the loss. This would include the creation of a loss narrative39 that incorporates both ambiguity and complexity, as well as a regained/renewed sense of purpose in ongoing life.
- Develop ambiguity tolerance. A related "task" in suicide grief is the development of ambiguity tolerance, which generally includes an understanding of the complexity underlying suicide, the ability to offer oneself a "fair trial"30 in relation to one's realistic degree of responsibility, and the acceptance that many questions may remain unanswerable. In addition, in concert with the current understanding of "continuing bonds,"40 survivors should attempt to attend to the ongoing relationship with the deceased, including any "unfinished business."6
- Develop skills to manage stigmatized social responses and/or changes in family and social relationships.
- Memorialize and honor the deceased. Healing for survivors is facilitated by memorializations, which both validate the mourning process itself while also paying tribute to the richness of the deceased person's life.
- Post-traumatic growth. The relatively new understanding of "post-traumatic" growth is certainly applicable to the "unexpected gifts" many survivors of suicide loss report after they have moved through suicide grief. This includes greater understanding toward oneself, other survivors of suicide loss, and suicidal individuals; gratitude toward those who have provided support; and a desire to "use" their newfound understanding of suicide and suicide grief in ways to honor the deceased and benefit others. Feigelman et al1 found that many longer-term survivors of suicide loss engaged in both direct service and social activism around suicide pre- and postvention.
Individual treatment. The limited research on individual treatment for suicide loss survivors suggests that while most participants find it generally helpful, a significant number of others report that their therapists lack knowledge of suicide grief and endorse stigmatizing attitudes toward suicide and suicide loss survivors.45-46 In addition, Sanford et al3 found that survivors of suicide loss who endorsed PTSD symptoms were not assessed, diagnosed, or treated for these symptoms.
Continue to: This speaks to the importance of understanding what is...
This speaks to the importance of understanding what is “normative” for survivors of suicide loss. In general, “normalization” and psychoeducation about the suicide grief trajectory can play an important role in work with survivors of suicide loss, even in the presence of diagnosable disorders. While PTSD, depressive symptoms, and suicidal ideation are not uncommon in suicide loss survivors, and certainly may warrant clinical assessment and treatment, it can be helpful (and less stigmatizing) for your patients to know that these diagnoses are relatively common and understandable in the context of this devastating experience. For instance, survivors of suicide loss often report feeling relieved when clinicians explain the connections between traumatic loss and PTSD and/or depressive symptoms, and this can also help to relieve secondary anxiety about “going crazy.” Many survivors of suicide loss also describe feeling as though they are functioning on “autopilot” in the earlier stages of grief; it can help them understand the “function” of compartmentalization as potentially adaptive in the short run.
Suicide loss survivors may also find it helpful to learn about suicidal states of mind and their relationships to any types of mental illness their loved ones had struggled with.47
Your role: Help survivors integrate the loss
Before beginning treatment with an individual who has lost a loved one to suicide, clinicians should thoroughly explore their own understanding of and experience with suicide, including assumptions around causation, internalized stigma about suicidal individuals and survivors of suicide loss, their own history of suicide loss or suicidality, cultural/religious attitudes, and anxiety/defenses associated with the topic of suicide. These factors, particularly when unexamined, are likely to impact the treatment relationship and one’s clinical efficacy.
In concert with the existing literature, consider the potential goals and tasks involved in the integration of the individual’s suicide loss, along with any individual factors/variants that may impact the grief trajectory. Kosminsky and Jordon34 described the role of the clinician in this situation as a “transitional attachment figure” who facilitates the management and integration of the loss into the creation of what survivors of suicide loss have termed a “new normal.”
Because suicide loss is often associated with PTSD and other psychiatric illnesses (eg, depression, suicidality, substance abuse), it is essential to balance the assessment and treatment of these issues with attention to grief issues as needed. Again, to the extent that such issues have arisen primarily in the wake of the suicide loss, it can be helpful for patients to understand their connection to the context of the loss.
Continue to: Ideally, the clinician should...
Ideally, the clinician should be “present” with the patient’s pain, normative guilt, and rumination, without attempting to quickly eliminate or “fix” it or provide premature reassurance that the survivor of suicide loss “did nothing wrong.” Rather, as Jordan6 suggests, the clinician should act to promote a “fair trial” with respect to the patient’s guilt and blame, with an understanding of the “tyranny of hindsight.” The promotion of ambiguity tolerance should also play a role in coming to terms with many questions that may remain unanswered.
Optimally, clinicians should encourage patients to attend to their ongoing relationship with the deceased, particularly in the service of resolving “unfinished business,” ultimately integrating the loss into memories of the whole person. In line with this, survivors of suicide loss may be encouraged to create a narrative of the loss that incorporates both complexity and ambiguity. In the service of supporting the suicide loss survivor’s reinvestment in life, it is often helpful to facilitate their ability to anticipate and cope with triggers, such as anniversaries, birthdays, or holidays, as well as to develop and use skills for managing difficult or stigmatizing social or cultural reactions.
Any disruptions in family functioning should also be addressed. Psychoeducation about discordant grieving styles (particularly around gender) and the support of children’s grief may be helpful, and referrals to family or couples therapists should be considered as needed. Finally, the facilitation of suicide loss survivors’ creation of memorializations or rituals can help promote healing and make their loss meaningful.
Bottom Line
Losing a loved one to suicide is often a devastating and traumatic experience, but with optimal support, most survivors are ultimately able to integrate the loss and grow as a result. Understanding the suicide grief trajectory, as well as general guidelines for treatment, will facilitate healing and growth in the aftermath of suicide loss.
Related Resources
- Jordan JR, McIntosh JL. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011.
- American Association of Suicidology. http://www.suicidology.org/.
- American Foundation for Suicide Prevention. https://afsp.org/.
1. Feigelman W, Jordan JR, McIntosh JL, et al. Devastating losses: how parents cope with the death of a child to suicide or drugs. New York, NY: Springer; 2012.
2. McIntosh JL. Research on survivors of suicide. In: Stimming MT, Stimming M, eds. Before their time: adult children’s experiences of parental suicide. Philadelphia, PA: Temple University Press; 1999:157-180.
3. Sanford RL, Cerel J, McGann VL, et al. Suicide loss survivors’ experiences with therapy: Implications for clinical practice. Community Ment Health J. 2016;5(2):551-558.
4. Jordan JR, McMenamy J. Interventions for suicide survivors: a review of the literature. Suicide Life Threat Behav. 2004;34(4):337-349.
5. Survivors of Suicide Loss Task Force. Responding to grief, trauma, & distress after a suicide: U.S. national guidelines. Washington, DC: National Action Alliance for Suicide Prevention; 2015.
6. Jordan JR, McGann V. Clinical work with suicide loss survivors: implications of the U.S. postvention guidelines. Death Stud. 2017;41(10):659-672.
7. Jordan JR. Is suicide bereavement different? A reassessment of the literature. Suicide Life Threat Behav. 2001;31(1):91-102.
8. Cvinar JG. Do suicide survivors suffer social stigma: a review of the literature. Perspect Psychiatr Care. 2005;41(1):14-21.
9. U.S. Public Health Service. The Surgeon General’s call to action to prevent suicide. Washington, DC: Department of Health and Human Services; 1999.
10. Doka KJ. Disenfranchised grief: recognizing hidden sorrow. Lexington, MA: Lexington; 1989.
11. Doka KJ. Disenfranchised grief: new directions, challenges, and strategies for practice. Champaign, IL: Research Press; 2002.
12. McIntosh JL. Suicide survivors: the aftermath of suicide and suicidal behavior. In: Bryant CD, ed. Handbook of death & dying. Vol. 1. Thousand Oaks, CA: SAGE Publications; 2003:339-350.
13. Jordan, JR, McIntosh, JL. Is suicide bereavement different? A framework for rethinking the question. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:19-42.
14. Dunne EJ, McIntosh JL, Dunne-Maxim K, eds. Suicide and its aftermath: understanding and counseling the survivors. New York, NY: W.W. Norton & Co.; 1987.
15. Harwood D, Hawton K, Hope T, et al. The grief experiences and needs of bereaved relatives and friends of older people dying through suicide: a descriptive and case-control study. J Affect Disord. 2002;72(2):185-194.
16. Armour, M. Violent death: understanding the context of traumatic and stigmatized grief. J Hum Behav Soc Environ. 2006;14(4):53-90.
17. Van Dongen CJ. Social context of postsuicide bereavement. Death Stud. 1993;17(2):125-141.
18. Calhoun LG, Allen BG. Social reactions to the survivor of a suicide in the family: A review of the literature. Omega – Journal of Death and Dying. 1991;23(2):95-107.
19. Range LM. When a loss is due to suicide: unique aspects of bereavement. In: Harvey JH, ed. Perspectives on loss: a sourcebook. Philadelphia, PA: Brunner/Mazel; 1998:213-220.
20. Sveen CA, Walby FA. Suicide survivors’ mental health and grief reactions: a systematic review of controlled studies. Suicide Life Threat Behav. 2008;38(1):13-29.
21. Feigelman W, Gorman BS, Jordan JR. Stigmatization and suicide bereavement. Death Stud. 2009;33(7):591-608.
22. Shneidman ES. Foreword. In: Cain AC, ed. Survivors of suicide. Springfield, IL: Charles C. Thomas; 1972:ix-xi.
23. Jordan JR, McIntosh, JL. Suicide bereavement: Why study survivors of suicide loss? In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:3-18.
24. Agerbo E. Midlife suicide risk, partner’s psychiatric illness, spouse and child bereavement by suicide or other modes of death: a gender specific study. J Epidemiol Community Health. 2005;59(5):407-412.
25. Hedström P, Liu KY, Nordvik MK. Interaction domains and suicide: a population-based panel study of suicides in Stockholm, 1991-1999. Soc Forces. 2008;87(2):713-740.
26. Qin P, Agerbo E, Mortensen PB. Suicide risk in relation to family history of completed suicide and psychiatric disorders: a nested case-control study based on longitudinal registers. Lancet. 2002;360(9340):1126-1130.
27. Qin P, Mortensen PB. The impact of parental status on the risk of completed suicide. Arch Gen Psychiatry. 2003;60(8):797-802.
28. Neimeyer RA, Sands D. Suicide loss and the quest for meaning. In: Andriessen K, Krysinska K, Grad OT, eds. Postvention in action: the international handbook of suicide bereavement support. Cambridge, MA: Hogrefe; 2017:71-84.
29. Sands DC, Jordan JR, Neimeyer RA. The meanings of suicide: A narrative approach to healing. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:249-282.
30. Jordan JR. Principles of grief counseling with adult survivors. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:179-224.
31. Cerel J, Jordan JR, Duberstein PR. The impact of suicide on the family. Crisis. 2008;29:38-44.
32. Kaslow NJ, Samples TC, Rhodes M, et al. A family-oriented and culturally sensitive postvention approach with suicide survivors. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:301-323.
33. Grad OT, Treven M, Krysinska K. Suicide bereavement and gender. In: Andriessen K, Krysinska K, Grad OT, eds. Postvention in action: the international handbook of suicide bereavement support. Cambridge, MA: Hogrefe; 2017:39-49.
34. Kosminsky PS, Jordan JR. Attachment-informed grief therapy: the clinician’s guide to foundations and applications. New York, NY: Routledge; 2016.
35. Gutin N, McGann VL, Jordan JR. The impact of suicide on professional caregivers. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:93-111.
36. Jordan JR. Bereavement after suicide. Psychiatr Ann. 2008;38(10):679-685.
37. Jordan JR. After suicide: clinical work with survivors. Grief Matters. 2009;12(1):4-9.
38. Neimeyer, RA. Traumatic loss and the reconstruction of meaning. J Palliat Med. 2002;5(6):935-942; discussion 942-943.
39. Neimeyer R, ed. Meaning reconstruction & the experience of loss. Washington, DC: American Psychological Association; 2001.
40. Klass, D. Sorrow and solace: Neglected areas in bereavement research. Death Stud. 2013;37(7):597-616.
41. Farberow NL. The Los Angeles Survivors-After-Suicide program: an evaluation. Crisis. 1992;13(1):23-34.
42. McDaid C, Trowman R, Golder S, et al. Interventions for people bereaved through suicide: systematic review. Br J Psychiatry. 2008;193(6):438-443.
43. Groos AD, Shakespeare-Finch J. Positive experiences for participants in suicide bereavement groups: a grounded theory model. Death Stud. 2013;37(1):1-24.
44. Jordan JR. Group work with suicide survivors. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:283-300.
45. Wilson A, Marshall A. The support needs and experiences of suicidally bereaved family and friends. Death Stud. 2010;34(7):625-640.
46. McKinnon JM, Chonody J. Exploring the formal supports used by people bereaved through suicide: a qualitative study. Soc Work Ment Health. 2014;12(3):231-248.
47. Myers MF, Fine C. Touched by suicide: hope and healing after loss. New York, NY: Gotham Books; 2006.
1. Feigelman W, Jordan JR, McIntosh JL, et al. Devastating losses: how parents cope with the death of a child to suicide or drugs. New York, NY: Springer; 2012.
2. McIntosh JL. Research on survivors of suicide. In: Stimming MT, Stimming M, eds. Before their time: adult children’s experiences of parental suicide. Philadelphia, PA: Temple University Press; 1999:157-180.
3. Sanford RL, Cerel J, McGann VL, et al. Suicide loss survivors’ experiences with therapy: Implications for clinical practice. Community Ment Health J. 2016;5(2):551-558.
4. Jordan JR, McMenamy J. Interventions for suicide survivors: a review of the literature. Suicide Life Threat Behav. 2004;34(4):337-349.
5. Survivors of Suicide Loss Task Force. Responding to grief, trauma, & distress after a suicide: U.S. national guidelines. Washington, DC: National Action Alliance for Suicide Prevention; 2015.
6. Jordan JR, McGann V. Clinical work with suicide loss survivors: implications of the U.S. postvention guidelines. Death Stud. 2017;41(10):659-672.
7. Jordan JR. Is suicide bereavement different? A reassessment of the literature. Suicide Life Threat Behav. 2001;31(1):91-102.
8. Cvinar JG. Do suicide survivors suffer social stigma: a review of the literature. Perspect Psychiatr Care. 2005;41(1):14-21.
9. U.S. Public Health Service. The Surgeon General’s call to action to prevent suicide. Washington, DC: Department of Health and Human Services; 1999.
10. Doka KJ. Disenfranchised grief: recognizing hidden sorrow. Lexington, MA: Lexington; 1989.
11. Doka KJ. Disenfranchised grief: new directions, challenges, and strategies for practice. Champaign, IL: Research Press; 2002.
12. McIntosh JL. Suicide survivors: the aftermath of suicide and suicidal behavior. In: Bryant CD, ed. Handbook of death & dying. Vol. 1. Thousand Oaks, CA: SAGE Publications; 2003:339-350.
13. Jordan, JR, McIntosh, JL. Is suicide bereavement different? A framework for rethinking the question. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:19-42.
14. Dunne EJ, McIntosh JL, Dunne-Maxim K, eds. Suicide and its aftermath: understanding and counseling the survivors. New York, NY: W.W. Norton & Co.; 1987.
15. Harwood D, Hawton K, Hope T, et al. The grief experiences and needs of bereaved relatives and friends of older people dying through suicide: a descriptive and case-control study. J Affect Disord. 2002;72(2):185-194.
16. Armour, M. Violent death: understanding the context of traumatic and stigmatized grief. J Hum Behav Soc Environ. 2006;14(4):53-90.
17. Van Dongen CJ. Social context of postsuicide bereavement. Death Stud. 1993;17(2):125-141.
18. Calhoun LG, Allen BG. Social reactions to the survivor of a suicide in the family: A review of the literature. Omega – Journal of Death and Dying. 1991;23(2):95-107.
19. Range LM. When a loss is due to suicide: unique aspects of bereavement. In: Harvey JH, ed. Perspectives on loss: a sourcebook. Philadelphia, PA: Brunner/Mazel; 1998:213-220.
20. Sveen CA, Walby FA. Suicide survivors’ mental health and grief reactions: a systematic review of controlled studies. Suicide Life Threat Behav. 2008;38(1):13-29.
21. Feigelman W, Gorman BS, Jordan JR. Stigmatization and suicide bereavement. Death Stud. 2009;33(7):591-608.
22. Shneidman ES. Foreword. In: Cain AC, ed. Survivors of suicide. Springfield, IL: Charles C. Thomas; 1972:ix-xi.
23. Jordan JR, McIntosh, JL. Suicide bereavement: Why study survivors of suicide loss? In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:3-18.
24. Agerbo E. Midlife suicide risk, partner’s psychiatric illness, spouse and child bereavement by suicide or other modes of death: a gender specific study. J Epidemiol Community Health. 2005;59(5):407-412.
25. Hedström P, Liu KY, Nordvik MK. Interaction domains and suicide: a population-based panel study of suicides in Stockholm, 1991-1999. Soc Forces. 2008;87(2):713-740.
26. Qin P, Agerbo E, Mortensen PB. Suicide risk in relation to family history of completed suicide and psychiatric disorders: a nested case-control study based on longitudinal registers. Lancet. 2002;360(9340):1126-1130.
27. Qin P, Mortensen PB. The impact of parental status on the risk of completed suicide. Arch Gen Psychiatry. 2003;60(8):797-802.
28. Neimeyer RA, Sands D. Suicide loss and the quest for meaning. In: Andriessen K, Krysinska K, Grad OT, eds. Postvention in action: the international handbook of suicide bereavement support. Cambridge, MA: Hogrefe; 2017:71-84.
29. Sands DC, Jordan JR, Neimeyer RA. The meanings of suicide: A narrative approach to healing. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:249-282.
30. Jordan JR. Principles of grief counseling with adult survivors. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:179-224.
31. Cerel J, Jordan JR, Duberstein PR. The impact of suicide on the family. Crisis. 2008;29:38-44.
32. Kaslow NJ, Samples TC, Rhodes M, et al. A family-oriented and culturally sensitive postvention approach with suicide survivors. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:301-323.
33. Grad OT, Treven M, Krysinska K. Suicide bereavement and gender. In: Andriessen K, Krysinska K, Grad OT, eds. Postvention in action: the international handbook of suicide bereavement support. Cambridge, MA: Hogrefe; 2017:39-49.
34. Kosminsky PS, Jordan JR. Attachment-informed grief therapy: the clinician’s guide to foundations and applications. New York, NY: Routledge; 2016.
35. Gutin N, McGann VL, Jordan JR. The impact of suicide on professional caregivers. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:93-111.
36. Jordan JR. Bereavement after suicide. Psychiatr Ann. 2008;38(10):679-685.
37. Jordan JR. After suicide: clinical work with survivors. Grief Matters. 2009;12(1):4-9.
38. Neimeyer, RA. Traumatic loss and the reconstruction of meaning. J Palliat Med. 2002;5(6):935-942; discussion 942-943.
39. Neimeyer R, ed. Meaning reconstruction & the experience of loss. Washington, DC: American Psychological Association; 2001.
40. Klass, D. Sorrow and solace: Neglected areas in bereavement research. Death Stud. 2013;37(7):597-616.
41. Farberow NL. The Los Angeles Survivors-After-Suicide program: an evaluation. Crisis. 1992;13(1):23-34.
42. McDaid C, Trowman R, Golder S, et al. Interventions for people bereaved through suicide: systematic review. Br J Psychiatry. 2008;193(6):438-443.
43. Groos AD, Shakespeare-Finch J. Positive experiences for participants in suicide bereavement groups: a grounded theory model. Death Stud. 2013;37(1):1-24.
44. Jordan JR. Group work with suicide survivors. In: Jordan JR, McIntosh JL, eds. Grief after suicide: understanding the consequences and caring for the survivors. New York, NY: Routledge/Taylor & Francis Group; 2011:283-300.
45. Wilson A, Marshall A. The support needs and experiences of suicidally bereaved family and friends. Death Stud. 2010;34(7):625-640.
46. McKinnon JM, Chonody J. Exploring the formal supports used by people bereaved through suicide: a qualitative study. Soc Work Ment Health. 2014;12(3):231-248.
47. Myers MF, Fine C. Touched by suicide: hope and healing after loss. New York, NY: Gotham Books; 2006.


