User login
Precepting: Holding Students and Programs Accountable
Randy Danielsen’s editorial on the topic of precepting (April 2016) elicited a flurry of responses from our NP readers.1 The influx of feedback prompted me as an educator, an NP, and a former preceptor to wonder: Why the paucity of preceptors? Are there too many programs and too many students? And are we dropping the ball when it comes to engendering professional responsibility as a “social contract”?1
Let me start with a query: Are we requiring students to uphold their social contracts? That is, are they engaged in professional networking to enrich their own clinical experiences? Are they responsible for establishing relationships with providers in their communities in preparation for clinical rotations? Aren’t these all components of their social contracts as students?
In my PNP program, we found our own preceptors (there were no clinical coordinators “back in the day”). As a component of that, we often had to educate our preceptors on the role of the NP. Thankfully, the pediatric community was aware of the NP; in the Boston area, at least, many settings already had NPs (and PAs) as providers. Still, when I reflect back, the experience of finding a preceptor augmented my professional education. It also instilled in me responsibility for my own professional development.
When it was my turn, I agreed to precept as my contribution to the profession. However, my first foray into precepting was not a pleasant one. As some of our email authors attested to experiencing, my student was completely unprepared for her clinical rotation. I found myself teaching basic assessment skills (to a student in her final semester!), which takes considerable time in the office setting. Subsequently, I required students to have at least three years of RN experience and demonstrate a full H&P prior to acceptance. This proviso raised some eyebrows among my colleagues, but as I saw it, my role as a preceptor was to help students to improve their skills—not teach them the basics. The result: a happy preceptor and long-standing relationships with the precepted students.
Even so, like many of the clinicians who responded to Dr. Danielsen’s editorial, I must admit I eventually stopped precepting. My decision was based on several factors, but the primary reason was that the students and faculty recruiting me were somewhat cavalier in their responsibility for preparedness to practice.
Among the readers who shared their precepting experiences, many cited inexperience in the RN role as a significant issue, as well as the rapidity with which students progress through their NP programs. Some commented that there is too much material to understand and process and not enough time to master the skills. These observations lead me back to the idea of “too many programs and students.” I know I risk offending my colleagues in academia with that statement. But I also know, from conversations with colleagues and the volume of emails we received on this topic, that many preceptors are frustrated by some students’ lack of responsibility, motivation, and preparation for their clinical rotations.
Some chalk up this shortcoming to being “millennials.” Others suggest that online programs do not hold students accountable for the “real world” demands of the job. On the latter point, I would submit that the “brick and mortar” programs have similar issues with students. And while both of these points have some validity, I think the problem is more complicated.
We face a perfect storm in NP education: The demand for NPs has increased as a result of the implementation of the ACA. In response to this demand, the number of NP programs has grown, and so has the need for NP preceptors. Yet, at this critical time, the number of preceptors is dwindling (in volume, yes, but also in willingness).
To resolve this conundrum, we must take a closer look at ways we can reverse the declining interest in preceptorship. Increasing the number of available preceptors requires overcoming perceived barriers. One of these, as noted by Barker and Pittman, is the detrimental effect precepting has on productivity.2 To illustrate this, they presented findings from a study of community physicians that documented an increase in the time taken to see patients and a decrease in the number of patients seen when the physician was precepting students.3 Additional time and reduced productivity are not tolerated in today’s work environment, and patients, who increasingly see themselves as health care consumers (who can take their “business” elsewhere), don’t appreciate waiting to see their health care provider when they have an appointment.
In their research, Logan, Kovacs, and Barry also found that productivity expectations (or should I say, the expectation of reduced productivity) impeded willingness to precept.4 They identified lack of time in the workday as a major barrier. This point is difficult to counter, I admit. But they also presented two other deterrents that, conversely, I view as potential opportunities for increasing the number of willing preceptors:
Lack of training for preceptors. Preceptors must learn how to fulfill this role on their own, without any training or support. This is a significant problem, not only for nascent preceptors but also for seasoned ones, who often precept students from different programs with a variety of requirements and expectations (and paperwork!). In an editorial, a new preceptor expressed concern about her ability to “get it right” and give her student what was needed to accomplish the goals for the rotation.5 Training and supportive testimonies are essential for successful precepting. A simple approach would be for program faculty to “mentor” new preceptors: Spend time orienting them to the expectations of the program and explaining how to evaluate students. Be proactive—establish weekly conference calls and share both strategies for successful precepting relationships and the “pitfalls to avoid.”
Student preparation. The other problem discussed by Logan, Kovacs, and Barry—and attested to by many of our readers—was the skill level and readiness of students on the first day of their clinical experience. While this responsibility lies with the student (rightfully so), I believe awareness of this problem, and understanding of how it affects practitioners’ willingness to precept, offers an opportunity for our education programs. Students may not know what they don’t know, or some may be too timid to speak up if they feel unprepared to step into a clinical arena (not to confuse that unease with “first-day jitters”). It is incumbent on the program faculty to ensure their students—who are representatives of that program and the faculty—are ready for clinical rotations. What do they need to do? Conduct an assessment of skills and readiness, which would assist all parties—the student, the preceptor, and the faculty—in gauging the progress of skill improvement and student competency and capability as a provider. It is also imperative that any remediation be provided by the program (prior to the student’s entrance into the clinical setting) and not the preceptor.
The bottom line is that precepting is a partnership between the skilled practitioner, the NP faculty, and the focused student.2 The responsibility for a mutually enjoyable and rewarding experience lies with all parties involved. As seasoned NPs, we must be active participants in preparing the next generation of our colleagues. That is our professional responsibility—our fulfillment of the “social contract.” We owe it to them, we owe it to our patients, and we owe it to ourselves—because someday, down the road, these clinicians will be taking care of us!
When a topic merits two editorials, there is clearly much to discuss. What steps do you suggest we undertake to mitigate this conundrum? Share your ideas by writing to me at NPEditor@frontlinemedcom.com.
References
1. Danielsen RD. The death of altruism, or, can I get a preceptor please? Clin Rev. 2016;26(4):10,13-14.
2. Barker ER, Pittman O. Becoming a super preceptor: a practical guide to preceptorship in today’s clinical climate. J Am Acad Nurse Pract. 2010;22(3):144-149.
3. Levy BT, Gjerde CL, Albrecht LA. The effects of precepting on and the support desired by community-based preceptors in Iowa. Acad Med. 1997;72(5):382-384.
4. Logan BL, Kovacs KA, Barry TL. Precepting nurse practitioner students: one medical center’s efforts to improve the precepting process. J Am Assoc Nurse Pract. 2015;27(12):676-682.
5. Aktan NM. Clinical preceptoring: what’s in it for me? J Nurse Pract. 2010;6(2):159-160.
Randy Danielsen’s editorial on the topic of precepting (April 2016) elicited a flurry of responses from our NP readers.1 The influx of feedback prompted me as an educator, an NP, and a former preceptor to wonder: Why the paucity of preceptors? Are there too many programs and too many students? And are we dropping the ball when it comes to engendering professional responsibility as a “social contract”?1
Let me start with a query: Are we requiring students to uphold their social contracts? That is, are they engaged in professional networking to enrich their own clinical experiences? Are they responsible for establishing relationships with providers in their communities in preparation for clinical rotations? Aren’t these all components of their social contracts as students?
In my PNP program, we found our own preceptors (there were no clinical coordinators “back in the day”). As a component of that, we often had to educate our preceptors on the role of the NP. Thankfully, the pediatric community was aware of the NP; in the Boston area, at least, many settings already had NPs (and PAs) as providers. Still, when I reflect back, the experience of finding a preceptor augmented my professional education. It also instilled in me responsibility for my own professional development.
When it was my turn, I agreed to precept as my contribution to the profession. However, my first foray into precepting was not a pleasant one. As some of our email authors attested to experiencing, my student was completely unprepared for her clinical rotation. I found myself teaching basic assessment skills (to a student in her final semester!), which takes considerable time in the office setting. Subsequently, I required students to have at least three years of RN experience and demonstrate a full H&P prior to acceptance. This proviso raised some eyebrows among my colleagues, but as I saw it, my role as a preceptor was to help students to improve their skills—not teach them the basics. The result: a happy preceptor and long-standing relationships with the precepted students.
Even so, like many of the clinicians who responded to Dr. Danielsen’s editorial, I must admit I eventually stopped precepting. My decision was based on several factors, but the primary reason was that the students and faculty recruiting me were somewhat cavalier in their responsibility for preparedness to practice.
Among the readers who shared their precepting experiences, many cited inexperience in the RN role as a significant issue, as well as the rapidity with which students progress through their NP programs. Some commented that there is too much material to understand and process and not enough time to master the skills. These observations lead me back to the idea of “too many programs and students.” I know I risk offending my colleagues in academia with that statement. But I also know, from conversations with colleagues and the volume of emails we received on this topic, that many preceptors are frustrated by some students’ lack of responsibility, motivation, and preparation for their clinical rotations.
Some chalk up this shortcoming to being “millennials.” Others suggest that online programs do not hold students accountable for the “real world” demands of the job. On the latter point, I would submit that the “brick and mortar” programs have similar issues with students. And while both of these points have some validity, I think the problem is more complicated.
We face a perfect storm in NP education: The demand for NPs has increased as a result of the implementation of the ACA. In response to this demand, the number of NP programs has grown, and so has the need for NP preceptors. Yet, at this critical time, the number of preceptors is dwindling (in volume, yes, but also in willingness).
To resolve this conundrum, we must take a closer look at ways we can reverse the declining interest in preceptorship. Increasing the number of available preceptors requires overcoming perceived barriers. One of these, as noted by Barker and Pittman, is the detrimental effect precepting has on productivity.2 To illustrate this, they presented findings from a study of community physicians that documented an increase in the time taken to see patients and a decrease in the number of patients seen when the physician was precepting students.3 Additional time and reduced productivity are not tolerated in today’s work environment, and patients, who increasingly see themselves as health care consumers (who can take their “business” elsewhere), don’t appreciate waiting to see their health care provider when they have an appointment.
In their research, Logan, Kovacs, and Barry also found that productivity expectations (or should I say, the expectation of reduced productivity) impeded willingness to precept.4 They identified lack of time in the workday as a major barrier. This point is difficult to counter, I admit. But they also presented two other deterrents that, conversely, I view as potential opportunities for increasing the number of willing preceptors:
Lack of training for preceptors. Preceptors must learn how to fulfill this role on their own, without any training or support. This is a significant problem, not only for nascent preceptors but also for seasoned ones, who often precept students from different programs with a variety of requirements and expectations (and paperwork!). In an editorial, a new preceptor expressed concern about her ability to “get it right” and give her student what was needed to accomplish the goals for the rotation.5 Training and supportive testimonies are essential for successful precepting. A simple approach would be for program faculty to “mentor” new preceptors: Spend time orienting them to the expectations of the program and explaining how to evaluate students. Be proactive—establish weekly conference calls and share both strategies for successful precepting relationships and the “pitfalls to avoid.”
Student preparation. The other problem discussed by Logan, Kovacs, and Barry—and attested to by many of our readers—was the skill level and readiness of students on the first day of their clinical experience. While this responsibility lies with the student (rightfully so), I believe awareness of this problem, and understanding of how it affects practitioners’ willingness to precept, offers an opportunity for our education programs. Students may not know what they don’t know, or some may be too timid to speak up if they feel unprepared to step into a clinical arena (not to confuse that unease with “first-day jitters”). It is incumbent on the program faculty to ensure their students—who are representatives of that program and the faculty—are ready for clinical rotations. What do they need to do? Conduct an assessment of skills and readiness, which would assist all parties—the student, the preceptor, and the faculty—in gauging the progress of skill improvement and student competency and capability as a provider. It is also imperative that any remediation be provided by the program (prior to the student’s entrance into the clinical setting) and not the preceptor.
The bottom line is that precepting is a partnership between the skilled practitioner, the NP faculty, and the focused student.2 The responsibility for a mutually enjoyable and rewarding experience lies with all parties involved. As seasoned NPs, we must be active participants in preparing the next generation of our colleagues. That is our professional responsibility—our fulfillment of the “social contract.” We owe it to them, we owe it to our patients, and we owe it to ourselves—because someday, down the road, these clinicians will be taking care of us!
When a topic merits two editorials, there is clearly much to discuss. What steps do you suggest we undertake to mitigate this conundrum? Share your ideas by writing to me at NPEditor@frontlinemedcom.com.
References
1. Danielsen RD. The death of altruism, or, can I get a preceptor please? Clin Rev. 2016;26(4):10,13-14.
2. Barker ER, Pittman O. Becoming a super preceptor: a practical guide to preceptorship in today’s clinical climate. J Am Acad Nurse Pract. 2010;22(3):144-149.
3. Levy BT, Gjerde CL, Albrecht LA. The effects of precepting on and the support desired by community-based preceptors in Iowa. Acad Med. 1997;72(5):382-384.
4. Logan BL, Kovacs KA, Barry TL. Precepting nurse practitioner students: one medical center’s efforts to improve the precepting process. J Am Assoc Nurse Pract. 2015;27(12):676-682.
5. Aktan NM. Clinical preceptoring: what’s in it for me? J Nurse Pract. 2010;6(2):159-160.
Randy Danielsen’s editorial on the topic of precepting (April 2016) elicited a flurry of responses from our NP readers.1 The influx of feedback prompted me as an educator, an NP, and a former preceptor to wonder: Why the paucity of preceptors? Are there too many programs and too many students? And are we dropping the ball when it comes to engendering professional responsibility as a “social contract”?1
Let me start with a query: Are we requiring students to uphold their social contracts? That is, are they engaged in professional networking to enrich their own clinical experiences? Are they responsible for establishing relationships with providers in their communities in preparation for clinical rotations? Aren’t these all components of their social contracts as students?
In my PNP program, we found our own preceptors (there were no clinical coordinators “back in the day”). As a component of that, we often had to educate our preceptors on the role of the NP. Thankfully, the pediatric community was aware of the NP; in the Boston area, at least, many settings already had NPs (and PAs) as providers. Still, when I reflect back, the experience of finding a preceptor augmented my professional education. It also instilled in me responsibility for my own professional development.
When it was my turn, I agreed to precept as my contribution to the profession. However, my first foray into precepting was not a pleasant one. As some of our email authors attested to experiencing, my student was completely unprepared for her clinical rotation. I found myself teaching basic assessment skills (to a student in her final semester!), which takes considerable time in the office setting. Subsequently, I required students to have at least three years of RN experience and demonstrate a full H&P prior to acceptance. This proviso raised some eyebrows among my colleagues, but as I saw it, my role as a preceptor was to help students to improve their skills—not teach them the basics. The result: a happy preceptor and long-standing relationships with the precepted students.
Even so, like many of the clinicians who responded to Dr. Danielsen’s editorial, I must admit I eventually stopped precepting. My decision was based on several factors, but the primary reason was that the students and faculty recruiting me were somewhat cavalier in their responsibility for preparedness to practice.
Among the readers who shared their precepting experiences, many cited inexperience in the RN role as a significant issue, as well as the rapidity with which students progress through their NP programs. Some commented that there is too much material to understand and process and not enough time to master the skills. These observations lead me back to the idea of “too many programs and students.” I know I risk offending my colleagues in academia with that statement. But I also know, from conversations with colleagues and the volume of emails we received on this topic, that many preceptors are frustrated by some students’ lack of responsibility, motivation, and preparation for their clinical rotations.
Some chalk up this shortcoming to being “millennials.” Others suggest that online programs do not hold students accountable for the “real world” demands of the job. On the latter point, I would submit that the “brick and mortar” programs have similar issues with students. And while both of these points have some validity, I think the problem is more complicated.
We face a perfect storm in NP education: The demand for NPs has increased as a result of the implementation of the ACA. In response to this demand, the number of NP programs has grown, and so has the need for NP preceptors. Yet, at this critical time, the number of preceptors is dwindling (in volume, yes, but also in willingness).
To resolve this conundrum, we must take a closer look at ways we can reverse the declining interest in preceptorship. Increasing the number of available preceptors requires overcoming perceived barriers. One of these, as noted by Barker and Pittman, is the detrimental effect precepting has on productivity.2 To illustrate this, they presented findings from a study of community physicians that documented an increase in the time taken to see patients and a decrease in the number of patients seen when the physician was precepting students.3 Additional time and reduced productivity are not tolerated in today’s work environment, and patients, who increasingly see themselves as health care consumers (who can take their “business” elsewhere), don’t appreciate waiting to see their health care provider when they have an appointment.
In their research, Logan, Kovacs, and Barry also found that productivity expectations (or should I say, the expectation of reduced productivity) impeded willingness to precept.4 They identified lack of time in the workday as a major barrier. This point is difficult to counter, I admit. But they also presented two other deterrents that, conversely, I view as potential opportunities for increasing the number of willing preceptors:
Lack of training for preceptors. Preceptors must learn how to fulfill this role on their own, without any training or support. This is a significant problem, not only for nascent preceptors but also for seasoned ones, who often precept students from different programs with a variety of requirements and expectations (and paperwork!). In an editorial, a new preceptor expressed concern about her ability to “get it right” and give her student what was needed to accomplish the goals for the rotation.5 Training and supportive testimonies are essential for successful precepting. A simple approach would be for program faculty to “mentor” new preceptors: Spend time orienting them to the expectations of the program and explaining how to evaluate students. Be proactive—establish weekly conference calls and share both strategies for successful precepting relationships and the “pitfalls to avoid.”
Student preparation. The other problem discussed by Logan, Kovacs, and Barry—and attested to by many of our readers—was the skill level and readiness of students on the first day of their clinical experience. While this responsibility lies with the student (rightfully so), I believe awareness of this problem, and understanding of how it affects practitioners’ willingness to precept, offers an opportunity for our education programs. Students may not know what they don’t know, or some may be too timid to speak up if they feel unprepared to step into a clinical arena (not to confuse that unease with “first-day jitters”). It is incumbent on the program faculty to ensure their students—who are representatives of that program and the faculty—are ready for clinical rotations. What do they need to do? Conduct an assessment of skills and readiness, which would assist all parties—the student, the preceptor, and the faculty—in gauging the progress of skill improvement and student competency and capability as a provider. It is also imperative that any remediation be provided by the program (prior to the student’s entrance into the clinical setting) and not the preceptor.
The bottom line is that precepting is a partnership between the skilled practitioner, the NP faculty, and the focused student.2 The responsibility for a mutually enjoyable and rewarding experience lies with all parties involved. As seasoned NPs, we must be active participants in preparing the next generation of our colleagues. That is our professional responsibility—our fulfillment of the “social contract.” We owe it to them, we owe it to our patients, and we owe it to ourselves—because someday, down the road, these clinicians will be taking care of us!
When a topic merits two editorials, there is clearly much to discuss. What steps do you suggest we undertake to mitigate this conundrum? Share your ideas by writing to me at NPEditor@frontlinemedcom.com.
References
1. Danielsen RD. The death of altruism, or, can I get a preceptor please? Clin Rev. 2016;26(4):10,13-14.
2. Barker ER, Pittman O. Becoming a super preceptor: a practical guide to preceptorship in today’s clinical climate. J Am Acad Nurse Pract. 2010;22(3):144-149.
3. Levy BT, Gjerde CL, Albrecht LA. The effects of precepting on and the support desired by community-based preceptors in Iowa. Acad Med. 1997;72(5):382-384.
4. Logan BL, Kovacs KA, Barry TL. Precepting nurse practitioner students: one medical center’s efforts to improve the precepting process. J Am Assoc Nurse Pract. 2015;27(12):676-682.
5. Aktan NM. Clinical preceptoring: what’s in it for me? J Nurse Pract. 2010;6(2):159-160.
The ACA, Six Years Later …
On March 23, 2016, we recognized the sixth anniversary of the signing of the Patient Protection and Affordable Care Act (ACA), a law designed to increase the number of Americans covered by health insurance and decrease the cost of health care. Prior to and since its passage, many have criticized the ACA as too costly and too quickly implemented (indeed, some would say, implemented without much planning or thought). Others have denigrated it as a step toward “socialized medicine” or as “big government”—a historically distrusted approach to solving problems.
As a student of health policy, I have watched the yarn of attempts to enact a comprehensive health insurance system ravel and unravel with each administration. Yes, for decades, political parties have staunchly opposed this type of program to reform our ailing system. But why is there such resistance to government involvement in health care reform?
This hasn’t been limited to insurance. Since the mid-1800s, despite the known dangers (including death) of various contagious diseases (eg, smallpox, malaria), people have resisted, even vehemently opposed, government-initiated regulations intended to combat such illnesses.1 Yet, today, we recognize that many improvements in the health of our communities and ourselves are founded on the infrastructure of the public health system. In most cities and states, the public health department responds to everyday health threats and emergencies through programs and initiatives that are government sponsored and funded—and accepted (one might even say expected) by most of us. Dare I point out that these are part of a “social insurance” program?
The idea of a comprehensive approach to health care coverage is not new. One of the earliest government interventions toward social insurance was the 1921 Sheppard-Towner Act, which provided matching funds to states for prenatal and child health centers. Regrettably, it was viewed by the AMA as “excessive federal interference in local health concerns” and discontinued a mere six years later.1
A later intervention, the Hill-Burton Act (passed in 1946) provided hospitals, nursing homes, and other health facilities with grants and loans for construction and modernization.2 An obligation tied to receiving funds was the requirement that administrators of the facilities “provide a reasonable volume of services to persons unable to pay and to make their services available to all persons residing in the facility’s area.”2 One could posit that these two policies influenced the movement toward national insurance in the United States.
We have a patchwork quilt of a health insurance system that includes social insurance programs: Social Security and Medicare. Generations of Americans have contributed to those programs through taxes and expect to benefit from them. And for generations—actually a century—there have been attempts to establish national health insurance (NHI) in the US. In the early 1900s, after Germany and England established health insurance for industrial workers, progressive social reformers attempted to secure similar protection for American workers but were unsuccessful.3 Repeated efforts in 1948, 1965, 1974, 1978, and 1994 also failed to institute an NHI program.
But why? There has been public support for some form of comprehensive NHI since the 1930s. The percentage of Americans expressing support for more government intervention on health care delivery has not fallen below 60% since 1937.4 This disconnect between the people’s desires and politics has been analyzed extensively and written about in many health policy texts.
So when did the idea of NHI become palatable? The notion came closer to reality during the Clinton administration. As the political parties began to fragment, they lost their power over health care politics. With more than 30 million Americans either without health insurance, or in jeopardy of losing what they had, the push for reform was stronger than ever before. We came close, but the scare tactics by NHI opponents about cost, decreased benefits, and increased risk (remember the Harry and Louise commercials?) quickly put the kibosh on that attempt at reform.
Continue forward to 2009 >>
Fast forward to 2009: Barack Obama is elected president and upholds his stance on health care reform, with a vow to institute a universal or near-universal health insurance program during his administration. As he said in his remarks to Congress, “I am not the first President to take up this cause [the issue of health care], but I am determined to be the last.”5 Hearing that an NHI program would cost $900 billion over 10 years was a bitter pill to swallow for some.5 But we couldn’t afford not to undertake it.
Since the enactment of the ACA, 18 million uninsured people have gained health coverage.6 The law has also improved access to health care services provided by NPs and PAs, evidenced by the nondiscrimination provision acknowledging us as primary care providers. The shortage of physicians and the increase in the number of newly insured persons seeking health care created an unprecedented opportunity to increase the utilization of NPs and PAs throughout the health care system.
Reflecting on the cost of the ACA, I have always maintained two positions: First, we pay for health care at often the most expensive place (the ED) or time (end-stage disease) … so it is a case of “pay me now or pay me later.” Second, we must gain control over the overall cost of health care. Providing access to primary care services for everyone is a step toward getting that control.
I have been a supporter of an NHI system all my adult life. I consider myself lucky to have had continuous access to health care. But I have cared for many who have not been so fortunate, and I have seen a minor illness become a major event because the family has no access to care. Without universal access to care, these cases increase—and with them, the cost of care.
Is the ACA the perfect solution? Even six years later, I think the jury is still out. But what I know for sure is that it was the first step in the right direction. You no doubt have opinions on this topic; please share them with me at NPEditor@frontlinemedcom.com.
References
1. Heinrich J. Organization and delivery of health care in the United States: the health care system that isn’t. In: Mason DJ, Leavitt JK, eds. Policy and Politics in Nursing and Health Care. 3rd ed. Philadelphia: Saunders; 1998:59-79.
2. US Department of Health and Human Services, Health Resources and Services Administration. Hill-Burton Program (July 2010). www.hrsa.gov/gethealthcare/affordable/hillburton/hillburton.pdf. Accessed April 11, 2016.
3. Altman S, Schactman D. Power, Politics, and Universal Health Care: The Inside Story of a Century-long Battle. Amherst, NY: Prometheus Books; 2011.
4. Steinmo S, Watts J. It’s the institutions, stupid: why comprehensive national health insurance always fails in America. In: Harrington C, Estes CL, eds. Health Policy: Crisis and Reform in the US Health Care Delivery System. 5th ed. Burlington, MA: Jones and Bartlett; 2008:30-36.
5. White House Office of the Press Secretary. Remarks by the President to a Joint Session of Congress on Health Care, September 9, 2009. www.whitehouse.gov/the-press-office/remarks-president-a-joint-session-congress-health-care. Accessed April 11, 2016.
6. US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. Health insurance coverage and the Affordable Care Act, September 2015. https://aspe.hhs.gov/pdf-report/health-insurance-coverage-and-affordable-care-act-september-2015. Accessed April 11, 2016.
On March 23, 2016, we recognized the sixth anniversary of the signing of the Patient Protection and Affordable Care Act (ACA), a law designed to increase the number of Americans covered by health insurance and decrease the cost of health care. Prior to and since its passage, many have criticized the ACA as too costly and too quickly implemented (indeed, some would say, implemented without much planning or thought). Others have denigrated it as a step toward “socialized medicine” or as “big government”—a historically distrusted approach to solving problems.
As a student of health policy, I have watched the yarn of attempts to enact a comprehensive health insurance system ravel and unravel with each administration. Yes, for decades, political parties have staunchly opposed this type of program to reform our ailing system. But why is there such resistance to government involvement in health care reform?
This hasn’t been limited to insurance. Since the mid-1800s, despite the known dangers (including death) of various contagious diseases (eg, smallpox, malaria), people have resisted, even vehemently opposed, government-initiated regulations intended to combat such illnesses.1 Yet, today, we recognize that many improvements in the health of our communities and ourselves are founded on the infrastructure of the public health system. In most cities and states, the public health department responds to everyday health threats and emergencies through programs and initiatives that are government sponsored and funded—and accepted (one might even say expected) by most of us. Dare I point out that these are part of a “social insurance” program?
The idea of a comprehensive approach to health care coverage is not new. One of the earliest government interventions toward social insurance was the 1921 Sheppard-Towner Act, which provided matching funds to states for prenatal and child health centers. Regrettably, it was viewed by the AMA as “excessive federal interference in local health concerns” and discontinued a mere six years later.1
A later intervention, the Hill-Burton Act (passed in 1946) provided hospitals, nursing homes, and other health facilities with grants and loans for construction and modernization.2 An obligation tied to receiving funds was the requirement that administrators of the facilities “provide a reasonable volume of services to persons unable to pay and to make their services available to all persons residing in the facility’s area.”2 One could posit that these two policies influenced the movement toward national insurance in the United States.
We have a patchwork quilt of a health insurance system that includes social insurance programs: Social Security and Medicare. Generations of Americans have contributed to those programs through taxes and expect to benefit from them. And for generations—actually a century—there have been attempts to establish national health insurance (NHI) in the US. In the early 1900s, after Germany and England established health insurance for industrial workers, progressive social reformers attempted to secure similar protection for American workers but were unsuccessful.3 Repeated efforts in 1948, 1965, 1974, 1978, and 1994 also failed to institute an NHI program.
But why? There has been public support for some form of comprehensive NHI since the 1930s. The percentage of Americans expressing support for more government intervention on health care delivery has not fallen below 60% since 1937.4 This disconnect between the people’s desires and politics has been analyzed extensively and written about in many health policy texts.
So when did the idea of NHI become palatable? The notion came closer to reality during the Clinton administration. As the political parties began to fragment, they lost their power over health care politics. With more than 30 million Americans either without health insurance, or in jeopardy of losing what they had, the push for reform was stronger than ever before. We came close, but the scare tactics by NHI opponents about cost, decreased benefits, and increased risk (remember the Harry and Louise commercials?) quickly put the kibosh on that attempt at reform.
Continue forward to 2009 >>
Fast forward to 2009: Barack Obama is elected president and upholds his stance on health care reform, with a vow to institute a universal or near-universal health insurance program during his administration. As he said in his remarks to Congress, “I am not the first President to take up this cause [the issue of health care], but I am determined to be the last.”5 Hearing that an NHI program would cost $900 billion over 10 years was a bitter pill to swallow for some.5 But we couldn’t afford not to undertake it.
Since the enactment of the ACA, 18 million uninsured people have gained health coverage.6 The law has also improved access to health care services provided by NPs and PAs, evidenced by the nondiscrimination provision acknowledging us as primary care providers. The shortage of physicians and the increase in the number of newly insured persons seeking health care created an unprecedented opportunity to increase the utilization of NPs and PAs throughout the health care system.
Reflecting on the cost of the ACA, I have always maintained two positions: First, we pay for health care at often the most expensive place (the ED) or time (end-stage disease) … so it is a case of “pay me now or pay me later.” Second, we must gain control over the overall cost of health care. Providing access to primary care services for everyone is a step toward getting that control.
I have been a supporter of an NHI system all my adult life. I consider myself lucky to have had continuous access to health care. But I have cared for many who have not been so fortunate, and I have seen a minor illness become a major event because the family has no access to care. Without universal access to care, these cases increase—and with them, the cost of care.
Is the ACA the perfect solution? Even six years later, I think the jury is still out. But what I know for sure is that it was the first step in the right direction. You no doubt have opinions on this topic; please share them with me at NPEditor@frontlinemedcom.com.
References
1. Heinrich J. Organization and delivery of health care in the United States: the health care system that isn’t. In: Mason DJ, Leavitt JK, eds. Policy and Politics in Nursing and Health Care. 3rd ed. Philadelphia: Saunders; 1998:59-79.
2. US Department of Health and Human Services, Health Resources and Services Administration. Hill-Burton Program (July 2010). www.hrsa.gov/gethealthcare/affordable/hillburton/hillburton.pdf. Accessed April 11, 2016.
3. Altman S, Schactman D. Power, Politics, and Universal Health Care: The Inside Story of a Century-long Battle. Amherst, NY: Prometheus Books; 2011.
4. Steinmo S, Watts J. It’s the institutions, stupid: why comprehensive national health insurance always fails in America. In: Harrington C, Estes CL, eds. Health Policy: Crisis and Reform in the US Health Care Delivery System. 5th ed. Burlington, MA: Jones and Bartlett; 2008:30-36.
5. White House Office of the Press Secretary. Remarks by the President to a Joint Session of Congress on Health Care, September 9, 2009. www.whitehouse.gov/the-press-office/remarks-president-a-joint-session-congress-health-care. Accessed April 11, 2016.
6. US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. Health insurance coverage and the Affordable Care Act, September 2015. https://aspe.hhs.gov/pdf-report/health-insurance-coverage-and-affordable-care-act-september-2015. Accessed April 11, 2016.
On March 23, 2016, we recognized the sixth anniversary of the signing of the Patient Protection and Affordable Care Act (ACA), a law designed to increase the number of Americans covered by health insurance and decrease the cost of health care. Prior to and since its passage, many have criticized the ACA as too costly and too quickly implemented (indeed, some would say, implemented without much planning or thought). Others have denigrated it as a step toward “socialized medicine” or as “big government”—a historically distrusted approach to solving problems.
As a student of health policy, I have watched the yarn of attempts to enact a comprehensive health insurance system ravel and unravel with each administration. Yes, for decades, political parties have staunchly opposed this type of program to reform our ailing system. But why is there such resistance to government involvement in health care reform?
This hasn’t been limited to insurance. Since the mid-1800s, despite the known dangers (including death) of various contagious diseases (eg, smallpox, malaria), people have resisted, even vehemently opposed, government-initiated regulations intended to combat such illnesses.1 Yet, today, we recognize that many improvements in the health of our communities and ourselves are founded on the infrastructure of the public health system. In most cities and states, the public health department responds to everyday health threats and emergencies through programs and initiatives that are government sponsored and funded—and accepted (one might even say expected) by most of us. Dare I point out that these are part of a “social insurance” program?
The idea of a comprehensive approach to health care coverage is not new. One of the earliest government interventions toward social insurance was the 1921 Sheppard-Towner Act, which provided matching funds to states for prenatal and child health centers. Regrettably, it was viewed by the AMA as “excessive federal interference in local health concerns” and discontinued a mere six years later.1
A later intervention, the Hill-Burton Act (passed in 1946) provided hospitals, nursing homes, and other health facilities with grants and loans for construction and modernization.2 An obligation tied to receiving funds was the requirement that administrators of the facilities “provide a reasonable volume of services to persons unable to pay and to make their services available to all persons residing in the facility’s area.”2 One could posit that these two policies influenced the movement toward national insurance in the United States.
We have a patchwork quilt of a health insurance system that includes social insurance programs: Social Security and Medicare. Generations of Americans have contributed to those programs through taxes and expect to benefit from them. And for generations—actually a century—there have been attempts to establish national health insurance (NHI) in the US. In the early 1900s, after Germany and England established health insurance for industrial workers, progressive social reformers attempted to secure similar protection for American workers but were unsuccessful.3 Repeated efforts in 1948, 1965, 1974, 1978, and 1994 also failed to institute an NHI program.
But why? There has been public support for some form of comprehensive NHI since the 1930s. The percentage of Americans expressing support for more government intervention on health care delivery has not fallen below 60% since 1937.4 This disconnect between the people’s desires and politics has been analyzed extensively and written about in many health policy texts.
So when did the idea of NHI become palatable? The notion came closer to reality during the Clinton administration. As the political parties began to fragment, they lost their power over health care politics. With more than 30 million Americans either without health insurance, or in jeopardy of losing what they had, the push for reform was stronger than ever before. We came close, but the scare tactics by NHI opponents about cost, decreased benefits, and increased risk (remember the Harry and Louise commercials?) quickly put the kibosh on that attempt at reform.
Continue forward to 2009 >>
Fast forward to 2009: Barack Obama is elected president and upholds his stance on health care reform, with a vow to institute a universal or near-universal health insurance program during his administration. As he said in his remarks to Congress, “I am not the first President to take up this cause [the issue of health care], but I am determined to be the last.”5 Hearing that an NHI program would cost $900 billion over 10 years was a bitter pill to swallow for some.5 But we couldn’t afford not to undertake it.
Since the enactment of the ACA, 18 million uninsured people have gained health coverage.6 The law has also improved access to health care services provided by NPs and PAs, evidenced by the nondiscrimination provision acknowledging us as primary care providers. The shortage of physicians and the increase in the number of newly insured persons seeking health care created an unprecedented opportunity to increase the utilization of NPs and PAs throughout the health care system.
Reflecting on the cost of the ACA, I have always maintained two positions: First, we pay for health care at often the most expensive place (the ED) or time (end-stage disease) … so it is a case of “pay me now or pay me later.” Second, we must gain control over the overall cost of health care. Providing access to primary care services for everyone is a step toward getting that control.
I have been a supporter of an NHI system all my adult life. I consider myself lucky to have had continuous access to health care. But I have cared for many who have not been so fortunate, and I have seen a minor illness become a major event because the family has no access to care. Without universal access to care, these cases increase—and with them, the cost of care.
Is the ACA the perfect solution? Even six years later, I think the jury is still out. But what I know for sure is that it was the first step in the right direction. You no doubt have opinions on this topic; please share them with me at NPEditor@frontlinemedcom.com.
References
1. Heinrich J. Organization and delivery of health care in the United States: the health care system that isn’t. In: Mason DJ, Leavitt JK, eds. Policy and Politics in Nursing and Health Care. 3rd ed. Philadelphia: Saunders; 1998:59-79.
2. US Department of Health and Human Services, Health Resources and Services Administration. Hill-Burton Program (July 2010). www.hrsa.gov/gethealthcare/affordable/hillburton/hillburton.pdf. Accessed April 11, 2016.
3. Altman S, Schactman D. Power, Politics, and Universal Health Care: The Inside Story of a Century-long Battle. Amherst, NY: Prometheus Books; 2011.
4. Steinmo S, Watts J. It’s the institutions, stupid: why comprehensive national health insurance always fails in America. In: Harrington C, Estes CL, eds. Health Policy: Crisis and Reform in the US Health Care Delivery System. 5th ed. Burlington, MA: Jones and Bartlett; 2008:30-36.
5. White House Office of the Press Secretary. Remarks by the President to a Joint Session of Congress on Health Care, September 9, 2009. www.whitehouse.gov/the-press-office/remarks-president-a-joint-session-congress-health-care. Accessed April 11, 2016.
6. US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. Health insurance coverage and the Affordable Care Act, September 2015. https://aspe.hhs.gov/pdf-report/health-insurance-coverage-and-affordable-care-act-september-2015. Accessed April 11, 2016.
Scholars in Solitude
Recently, six faculty colleagues and I were discussing socialization of students in distance-learning programs. Each of us shared concerns that had been voiced by students regarding the periods of isolation they frequently feel while studying or completing course assignments. The common theme was expressed as “not feeling connected” and “no real camaraderie” with fellow students. One of us also raised the issue of internal conflict; a student had described herself as enjoying the freedom to listen to lectures on her own schedule and not be obligated to attend class on a specific day at a specific time but simultaneously missing seeing her classmates on a weekly basis.
For the most part, my colleagues and I were all “bricks and mortar” students, tied to required attendance during scheduled classes. We collectively agreed that this was frequently a bother, but we recognized the advantage of being able to sit together before or after class to discuss assignments, bring clarity to confusion, or simply commiserate on the difficulties of balancing family, school, and work obligations. In my own doctoral studies, week-to-week support and encouragement kept us a close-knit group, seeing us through to completed dissertations.
As our conversation continued, we began to lament our own lack of connectedness, not to our students (we communicate with them at least, if not more than, once a week) but to our faculty colleagues. Our consensus was that the focus on student-to-faculty contact left faculty-to-faculty contact seemingly an afterthought—or not a thought at all. I consider myself lucky that most of “my faculty” were friends or professional colleagues prior to our academic postings. Thus, we had established relationships outside our faculty roles.
But this whole idea of the socialization of faculty in distance education got me wondering: Are there criteria or guidelines for communication among faculty? I don’t mean the required staff meetings; I mean something similar to the requirements for type, and frequency, of interactions with the students, which are set forth by credentialing entities. I wondered what I could find in the literature or educational texts about faculty “connectedness.” And so my search began.
Continue for where my search began >>
I started with Keating’s text,1 the table of contents of which listed a chapter on Distance Education. Hmm, I thought, there must be something there. Several sections were enlightening and could very easily provide guidance for faculty-student interactions, but not so much for faculty to faculty. Granted, the basis for the text is curriculum development, so I am not denigrating the work; I just hoped a chapter on program development would include something on developing faculty networks.
As my search continued, I found the Online Journal of Distance Learning Administration. Notable was research presented by Bower,2 who described findings of an American Faculty Poll conducted in 2000 noting that “direct engagement with the students is one of the most important factors” in an educator’s decision to pursue an academic career.3 In this poll, a flexible work schedule was viewed as very important by 60% of those surveyed; those of us who are engaged in distance education have the most control (I would submit) over our schedules. But there was no evidence that faculty who taught online were represented in that survey—and no discussion of faculty-to-faculty connections.
Despite repeated searches, I found a paucity of research regarding socialization (or lack thereof) among faculty teaching in the online environment. In her dissertation, Heilman4 addressed perceptions of satisfaction with online teaching. One element she researched was faculty/peer relationships. Her participants noted that “networking and sharing with other online faculty members who work in another location” enhanced their satisfaction, but several noted that “lack of interactions or feeling isolated from their peers” diminished their satisfaction with online teaching. In reading their comments, I formed the impression that the interactions were initiated by the individual faculty, rather than facilitated by the institution.
Recently, I have seen blog posts addressing the issue of transforming clinicians to academics. There is a universal understanding that being an expert clinician does not necessarily mean you are a proficient educator. Moreover, transitioning from a face-to-face system to an online environment can be intimidating. Faculty, especially those new to the role, may need additional support.
Having an internal social network for online faculty is a means to achieving a supportive community and building a mentoring culture within an institution. A faculty member who has a sense of connectedness to other faculty (onsite and online) is as important to the successful online environment as is the development of a sense of community for students. The community must serve to enhance learning and teaching for both groups.
There are several published guidelines for successful online teaching—that is, what faculty can do for students. I have taken those principles, modified them, and applied them as suggestions for improving the socialization of faculty. With recognition of those who devised them5,6 and acknowledgement of the poetic license applied, here they are:
• Encourage faculty-to-faculty contact outside mandatory meetings
• Encourage faculty collaboration beyond course/institutional requirements
• Provide for live, interactive events that are fun.
With the ever-increasing number of educational institutions providing online programs (now at about 89%7), it is imperative that we as faculty and program administrators include socialization as a component of faculty orientation and training. What better than a connected faculty to enhance student achievement?
When we’re on site, my faculty colleagues and I plan dinner together. During commencement week, laughter and camaraderie from “unofficial” social activities allow us to relax, celebrate another successful class, and form memories that we carry with us throughout the year. What about your institutions? Please share your ideas about “staying connected” to colleagues in a digital environment by writing to NPEditor@frontlinemedcom.com.
References
1. Keating SB. Curriculum Development and Evaluation in Nursing. Philadelphia, PA: Lippincott Williams and Wilkins; 2006.
2. Bower BL. Distance education: facing the faculty challenge. Online J Distance Learning Admin. 2001;4(2).
3. Sanderson A, Phua VC, Herda D. The American Faculty Poll. Chicago: National Opinion Research Center; 2000.
4. Heilman JG. Higher education faculty satisfaction with online teaching [dissertation]. 2007. http://hdl.handle.net/2152/3796. Accessed February 15, 2016.
5. Koeckeritz J, Malkiewicz J, Henderson A. The seven principles of good practice: applications for online education in nursing. Nurse Educ. 2002;27(6):283-287.
6. Chickering AW, Gamson ZF. Seven principles for good practice in undergraduate education. AAHE Bulletin. 1987;39(7):3-7.
7. Parker K, Lenhart A, Moore K. The Digital Revolution and Higher Education: College Presidents, Public Differ on Value of Online Learning. Washington, DC: Pew Research Center; 2011.
Recently, six faculty colleagues and I were discussing socialization of students in distance-learning programs. Each of us shared concerns that had been voiced by students regarding the periods of isolation they frequently feel while studying or completing course assignments. The common theme was expressed as “not feeling connected” and “no real camaraderie” with fellow students. One of us also raised the issue of internal conflict; a student had described herself as enjoying the freedom to listen to lectures on her own schedule and not be obligated to attend class on a specific day at a specific time but simultaneously missing seeing her classmates on a weekly basis.
For the most part, my colleagues and I were all “bricks and mortar” students, tied to required attendance during scheduled classes. We collectively agreed that this was frequently a bother, but we recognized the advantage of being able to sit together before or after class to discuss assignments, bring clarity to confusion, or simply commiserate on the difficulties of balancing family, school, and work obligations. In my own doctoral studies, week-to-week support and encouragement kept us a close-knit group, seeing us through to completed dissertations.
As our conversation continued, we began to lament our own lack of connectedness, not to our students (we communicate with them at least, if not more than, once a week) but to our faculty colleagues. Our consensus was that the focus on student-to-faculty contact left faculty-to-faculty contact seemingly an afterthought—or not a thought at all. I consider myself lucky that most of “my faculty” were friends or professional colleagues prior to our academic postings. Thus, we had established relationships outside our faculty roles.
But this whole idea of the socialization of faculty in distance education got me wondering: Are there criteria or guidelines for communication among faculty? I don’t mean the required staff meetings; I mean something similar to the requirements for type, and frequency, of interactions with the students, which are set forth by credentialing entities. I wondered what I could find in the literature or educational texts about faculty “connectedness.” And so my search began.
Continue for where my search began >>
I started with Keating’s text,1 the table of contents of which listed a chapter on Distance Education. Hmm, I thought, there must be something there. Several sections were enlightening and could very easily provide guidance for faculty-student interactions, but not so much for faculty to faculty. Granted, the basis for the text is curriculum development, so I am not denigrating the work; I just hoped a chapter on program development would include something on developing faculty networks.
As my search continued, I found the Online Journal of Distance Learning Administration. Notable was research presented by Bower,2 who described findings of an American Faculty Poll conducted in 2000 noting that “direct engagement with the students is one of the most important factors” in an educator’s decision to pursue an academic career.3 In this poll, a flexible work schedule was viewed as very important by 60% of those surveyed; those of us who are engaged in distance education have the most control (I would submit) over our schedules. But there was no evidence that faculty who taught online were represented in that survey—and no discussion of faculty-to-faculty connections.
Despite repeated searches, I found a paucity of research regarding socialization (or lack thereof) among faculty teaching in the online environment. In her dissertation, Heilman4 addressed perceptions of satisfaction with online teaching. One element she researched was faculty/peer relationships. Her participants noted that “networking and sharing with other online faculty members who work in another location” enhanced their satisfaction, but several noted that “lack of interactions or feeling isolated from their peers” diminished their satisfaction with online teaching. In reading their comments, I formed the impression that the interactions were initiated by the individual faculty, rather than facilitated by the institution.
Recently, I have seen blog posts addressing the issue of transforming clinicians to academics. There is a universal understanding that being an expert clinician does not necessarily mean you are a proficient educator. Moreover, transitioning from a face-to-face system to an online environment can be intimidating. Faculty, especially those new to the role, may need additional support.
Having an internal social network for online faculty is a means to achieving a supportive community and building a mentoring culture within an institution. A faculty member who has a sense of connectedness to other faculty (onsite and online) is as important to the successful online environment as is the development of a sense of community for students. The community must serve to enhance learning and teaching for both groups.
There are several published guidelines for successful online teaching—that is, what faculty can do for students. I have taken those principles, modified them, and applied them as suggestions for improving the socialization of faculty. With recognition of those who devised them5,6 and acknowledgement of the poetic license applied, here they are:
• Encourage faculty-to-faculty contact outside mandatory meetings
• Encourage faculty collaboration beyond course/institutional requirements
• Provide for live, interactive events that are fun.
With the ever-increasing number of educational institutions providing online programs (now at about 89%7), it is imperative that we as faculty and program administrators include socialization as a component of faculty orientation and training. What better than a connected faculty to enhance student achievement?
When we’re on site, my faculty colleagues and I plan dinner together. During commencement week, laughter and camaraderie from “unofficial” social activities allow us to relax, celebrate another successful class, and form memories that we carry with us throughout the year. What about your institutions? Please share your ideas about “staying connected” to colleagues in a digital environment by writing to NPEditor@frontlinemedcom.com.
References
1. Keating SB. Curriculum Development and Evaluation in Nursing. Philadelphia, PA: Lippincott Williams and Wilkins; 2006.
2. Bower BL. Distance education: facing the faculty challenge. Online J Distance Learning Admin. 2001;4(2).
3. Sanderson A, Phua VC, Herda D. The American Faculty Poll. Chicago: National Opinion Research Center; 2000.
4. Heilman JG. Higher education faculty satisfaction with online teaching [dissertation]. 2007. http://hdl.handle.net/2152/3796. Accessed February 15, 2016.
5. Koeckeritz J, Malkiewicz J, Henderson A. The seven principles of good practice: applications for online education in nursing. Nurse Educ. 2002;27(6):283-287.
6. Chickering AW, Gamson ZF. Seven principles for good practice in undergraduate education. AAHE Bulletin. 1987;39(7):3-7.
7. Parker K, Lenhart A, Moore K. The Digital Revolution and Higher Education: College Presidents, Public Differ on Value of Online Learning. Washington, DC: Pew Research Center; 2011.
Recently, six faculty colleagues and I were discussing socialization of students in distance-learning programs. Each of us shared concerns that had been voiced by students regarding the periods of isolation they frequently feel while studying or completing course assignments. The common theme was expressed as “not feeling connected” and “no real camaraderie” with fellow students. One of us also raised the issue of internal conflict; a student had described herself as enjoying the freedom to listen to lectures on her own schedule and not be obligated to attend class on a specific day at a specific time but simultaneously missing seeing her classmates on a weekly basis.
For the most part, my colleagues and I were all “bricks and mortar” students, tied to required attendance during scheduled classes. We collectively agreed that this was frequently a bother, but we recognized the advantage of being able to sit together before or after class to discuss assignments, bring clarity to confusion, or simply commiserate on the difficulties of balancing family, school, and work obligations. In my own doctoral studies, week-to-week support and encouragement kept us a close-knit group, seeing us through to completed dissertations.
As our conversation continued, we began to lament our own lack of connectedness, not to our students (we communicate with them at least, if not more than, once a week) but to our faculty colleagues. Our consensus was that the focus on student-to-faculty contact left faculty-to-faculty contact seemingly an afterthought—or not a thought at all. I consider myself lucky that most of “my faculty” were friends or professional colleagues prior to our academic postings. Thus, we had established relationships outside our faculty roles.
But this whole idea of the socialization of faculty in distance education got me wondering: Are there criteria or guidelines for communication among faculty? I don’t mean the required staff meetings; I mean something similar to the requirements for type, and frequency, of interactions with the students, which are set forth by credentialing entities. I wondered what I could find in the literature or educational texts about faculty “connectedness.” And so my search began.
Continue for where my search began >>
I started with Keating’s text,1 the table of contents of which listed a chapter on Distance Education. Hmm, I thought, there must be something there. Several sections were enlightening and could very easily provide guidance for faculty-student interactions, but not so much for faculty to faculty. Granted, the basis for the text is curriculum development, so I am not denigrating the work; I just hoped a chapter on program development would include something on developing faculty networks.
As my search continued, I found the Online Journal of Distance Learning Administration. Notable was research presented by Bower,2 who described findings of an American Faculty Poll conducted in 2000 noting that “direct engagement with the students is one of the most important factors” in an educator’s decision to pursue an academic career.3 In this poll, a flexible work schedule was viewed as very important by 60% of those surveyed; those of us who are engaged in distance education have the most control (I would submit) over our schedules. But there was no evidence that faculty who taught online were represented in that survey—and no discussion of faculty-to-faculty connections.
Despite repeated searches, I found a paucity of research regarding socialization (or lack thereof) among faculty teaching in the online environment. In her dissertation, Heilman4 addressed perceptions of satisfaction with online teaching. One element she researched was faculty/peer relationships. Her participants noted that “networking and sharing with other online faculty members who work in another location” enhanced their satisfaction, but several noted that “lack of interactions or feeling isolated from their peers” diminished their satisfaction with online teaching. In reading their comments, I formed the impression that the interactions were initiated by the individual faculty, rather than facilitated by the institution.
Recently, I have seen blog posts addressing the issue of transforming clinicians to academics. There is a universal understanding that being an expert clinician does not necessarily mean you are a proficient educator. Moreover, transitioning from a face-to-face system to an online environment can be intimidating. Faculty, especially those new to the role, may need additional support.
Having an internal social network for online faculty is a means to achieving a supportive community and building a mentoring culture within an institution. A faculty member who has a sense of connectedness to other faculty (onsite and online) is as important to the successful online environment as is the development of a sense of community for students. The community must serve to enhance learning and teaching for both groups.
There are several published guidelines for successful online teaching—that is, what faculty can do for students. I have taken those principles, modified them, and applied them as suggestions for improving the socialization of faculty. With recognition of those who devised them5,6 and acknowledgement of the poetic license applied, here they are:
• Encourage faculty-to-faculty contact outside mandatory meetings
• Encourage faculty collaboration beyond course/institutional requirements
• Provide for live, interactive events that are fun.
With the ever-increasing number of educational institutions providing online programs (now at about 89%7), it is imperative that we as faculty and program administrators include socialization as a component of faculty orientation and training. What better than a connected faculty to enhance student achievement?
When we’re on site, my faculty colleagues and I plan dinner together. During commencement week, laughter and camaraderie from “unofficial” social activities allow us to relax, celebrate another successful class, and form memories that we carry with us throughout the year. What about your institutions? Please share your ideas about “staying connected” to colleagues in a digital environment by writing to NPEditor@frontlinemedcom.com.
References
1. Keating SB. Curriculum Development and Evaluation in Nursing. Philadelphia, PA: Lippincott Williams and Wilkins; 2006.
2. Bower BL. Distance education: facing the faculty challenge. Online J Distance Learning Admin. 2001;4(2).
3. Sanderson A, Phua VC, Herda D. The American Faculty Poll. Chicago: National Opinion Research Center; 2000.
4. Heilman JG. Higher education faculty satisfaction with online teaching [dissertation]. 2007. http://hdl.handle.net/2152/3796. Accessed February 15, 2016.
5. Koeckeritz J, Malkiewicz J, Henderson A. The seven principles of good practice: applications for online education in nursing. Nurse Educ. 2002;27(6):283-287.
6. Chickering AW, Gamson ZF. Seven principles for good practice in undergraduate education. AAHE Bulletin. 1987;39(7):3-7.
7. Parker K, Lenhart A, Moore K. The Digital Revolution and Higher Education: College Presidents, Public Differ on Value of Online Learning. Washington, DC: Pew Research Center; 2011.
Try to Remember …
How often do you misplace your keys or forget why you walked into a room? When I was younger, I dismissed things such as losing my train of thought (my nephew calls that a brain fart), a neglected errand (probably not important enough), or getting lost trying to go somewhere (never was good at directions anyway).
Know that I was never a “list maker.” I gave that up—because I often could not remember where I’d put it. Usually, once I wrote something down, I would eventually (in the same day) recall whatever was on it, so I wouldn’t fret about where I left that list.
Names? I could always tell you where we met, what you were wearing, and where you were sitting. But your name? Forget about it. (Those who have met me know the truth in that statement!)
During particularly stressful or busy times, if I found myself a bit more “absentminded” than usual, I would joke, “Of all the things I’ve lost, I miss my mind the most.”
Now I wonder: Just how serious are those instances of memory lapse? Yes, occasional memory lapses are part of normal aging. Just like our joints, our brains are not as young as they used to be. Even a 90-year-old with a healthy brain has experienced a loss of 10% brain cell volume.1 And let’s be honest, in celebrating major accomplishments (or failures), some of us have killed a few additional brain cells along the way (wink, wink).
We know that as we age, just as our stride has slowed, so too has the sharpness of our recall dulled. However, at what point are those misfires of our brain no longer a minor nuisance?
Data from the Administration on Aging document that in 2013, an estimated 44.7 million US residents were 65 or older.2 An estimated 5 million of them had Alzheimer disease. That translates to one in nine people—scary! This number, researchers predict, will increase to 13.8 million by 2050.3
Moreover, these statistics become more startling as we recognize that the cost of providing long-term and hospice care to people with Alzheimer disease (and other forms of dementia) is estimated to increase from $203 billion in 2013 to $1.2 trillion in 2050 (in 2013 dollars).4 Therefore, it is imperative for us, both as individuals and as health care professionals, to know the warning signs of dementia and be attentive to even seemingly subtle changes in behavior.
Early recognition that these changes are more than minor lapses in memory is important. Delays in diagnosis can result in a reduction of access to available treatments and resources. Yet, at what point do we start to consider those minor instances of forgetfulness not as normal but as indications of developing cognitive problems? My colleagues in gerontology tell us it is when those changes negatively affect activities of daily living and ability to function.
Continue for the difference between my lifelong “geographic handicap” and a form of dementia >>
What is the difference between my lifelong “geographic handicap” and a form of dementia? Would I (or any of my family or friends) recognize it? The diagnosis of dementia is not based on a sole symptom; rather, it requires the existence of at least two types of impairment that are significant and interfere with daily life.
Thankfully, I have adjusted to being “temporarily misplaced” (I don’t call it lost) and smiling at you whilst I try to remember your name. It may seem I jest or am insensitive to a grave health issue—but I am very serious about our need to pay attention to ourselves, to those we care for, and to those we care about (including neighbors). I now live in an area where a “silver alert” (missing elder) is an almost daily occurrence.
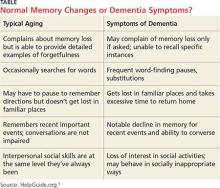
The table provides a comparison of normal-aging memory changes versus dementia symptoms; this is a tool we can use in practice and provide to our patients and their families.5 However, when changes in memory become so pervasive and severe that they are disrupting work, hobbies, social activities, and family relationships, we must recognize that they are the warning signs of Alzheimer disease.6 After reading multiple reports and guides, and witnessing the disease progression in neighbors, I share the three most significant hallmarks of the disease: impaired judgment, difficulty in recalling new information, and unusual behavior.7
It is important to remember—and to communicate to our patients—that memory loss itself does not meet the criteria for dementia. While some may be quick to fear that diagnosis, other factors that can contribute to cognitive problems are stress, depression, vitamin deficiency, thyroid disease, and even dehydration. All of these can be managed, with a resultant reversal of symptoms of memory loss.8 As always, a good health history, review of symptoms, and physical examination will guide us to an accurate diagnosis and plan of care.
There are multiple resources available for patients and families who receive a diagnosis of dementia or Alzheimer disease. Fear of the diagnosis need not blind us to the early warning signs. As NPs and PAs, despite our busy schedules, we must stop and listen to both the patient and the family, and ask the difficult questions about judgment and behavior in our aging patients.
REFERENCES
1. Doty L. Caregiving topics: early signs of dementia. http://alzonline.phhp.ufl.edu/en/reading/EarlySignsFeb08.pdf. Accessed December 11, 2015.
2. CDC. Older persons’ health. www.cdc.gov/nchs/fastats/older-american-health.htm. Accessed December 11, 2015.
3. Hebert LE, Weuve J, Scherr PA, Evans DL. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80:1778-1783.
4. Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimers Dement. 2013;9(2):20-245.
5. Wayne M, White M, Smith M. Understanding dementia. www.helpguide.org/articles/alzheimers-dementia/understanding-dementia.htm. Accessed December 11, 2015.
6. Smith M, Robinson L, Segal R. Age-related memory loss. www.helpguide.org/articles/memory/age-related-memory-loss.htm. Accessed December 11, 2015.
7. A guide to coping with Alzheimer’s disease: a Harvard Medical School Special Health Report. www.health.harvard.edu/special-health-reports/a-guide-to-coping-with-alzheimers-disease. Accessed December 11, 2015.
8. HelpGuide.org. What’s causing your memory loss? www.helpguide.org/harvard/whats-causing-your-memory-loss.htm. Accessed December 11, 2015.
How often do you misplace your keys or forget why you walked into a room? When I was younger, I dismissed things such as losing my train of thought (my nephew calls that a brain fart), a neglected errand (probably not important enough), or getting lost trying to go somewhere (never was good at directions anyway).
Know that I was never a “list maker.” I gave that up—because I often could not remember where I’d put it. Usually, once I wrote something down, I would eventually (in the same day) recall whatever was on it, so I wouldn’t fret about where I left that list.
Names? I could always tell you where we met, what you were wearing, and where you were sitting. But your name? Forget about it. (Those who have met me know the truth in that statement!)
During particularly stressful or busy times, if I found myself a bit more “absentminded” than usual, I would joke, “Of all the things I’ve lost, I miss my mind the most.”
Now I wonder: Just how serious are those instances of memory lapse? Yes, occasional memory lapses are part of normal aging. Just like our joints, our brains are not as young as they used to be. Even a 90-year-old with a healthy brain has experienced a loss of 10% brain cell volume.1 And let’s be honest, in celebrating major accomplishments (or failures), some of us have killed a few additional brain cells along the way (wink, wink).
We know that as we age, just as our stride has slowed, so too has the sharpness of our recall dulled. However, at what point are those misfires of our brain no longer a minor nuisance?
Data from the Administration on Aging document that in 2013, an estimated 44.7 million US residents were 65 or older.2 An estimated 5 million of them had Alzheimer disease. That translates to one in nine people—scary! This number, researchers predict, will increase to 13.8 million by 2050.3
Moreover, these statistics become more startling as we recognize that the cost of providing long-term and hospice care to people with Alzheimer disease (and other forms of dementia) is estimated to increase from $203 billion in 2013 to $1.2 trillion in 2050 (in 2013 dollars).4 Therefore, it is imperative for us, both as individuals and as health care professionals, to know the warning signs of dementia and be attentive to even seemingly subtle changes in behavior.
Early recognition that these changes are more than minor lapses in memory is important. Delays in diagnosis can result in a reduction of access to available treatments and resources. Yet, at what point do we start to consider those minor instances of forgetfulness not as normal but as indications of developing cognitive problems? My colleagues in gerontology tell us it is when those changes negatively affect activities of daily living and ability to function.
Continue for the difference between my lifelong “geographic handicap” and a form of dementia >>
What is the difference between my lifelong “geographic handicap” and a form of dementia? Would I (or any of my family or friends) recognize it? The diagnosis of dementia is not based on a sole symptom; rather, it requires the existence of at least two types of impairment that are significant and interfere with daily life.
Thankfully, I have adjusted to being “temporarily misplaced” (I don’t call it lost) and smiling at you whilst I try to remember your name. It may seem I jest or am insensitive to a grave health issue—but I am very serious about our need to pay attention to ourselves, to those we care for, and to those we care about (including neighbors). I now live in an area where a “silver alert” (missing elder) is an almost daily occurrence.
The table provides a comparison of normal-aging memory changes versus dementia symptoms; this is a tool we can use in practice and provide to our patients and their families.5 However, when changes in memory become so pervasive and severe that they are disrupting work, hobbies, social activities, and family relationships, we must recognize that they are the warning signs of Alzheimer disease.6 After reading multiple reports and guides, and witnessing the disease progression in neighbors, I share the three most significant hallmarks of the disease: impaired judgment, difficulty in recalling new information, and unusual behavior.7
It is important to remember—and to communicate to our patients—that memory loss itself does not meet the criteria for dementia. While some may be quick to fear that diagnosis, other factors that can contribute to cognitive problems are stress, depression, vitamin deficiency, thyroid disease, and even dehydration. All of these can be managed, with a resultant reversal of symptoms of memory loss.8 As always, a good health history, review of symptoms, and physical examination will guide us to an accurate diagnosis and plan of care.
There are multiple resources available for patients and families who receive a diagnosis of dementia or Alzheimer disease. Fear of the diagnosis need not blind us to the early warning signs. As NPs and PAs, despite our busy schedules, we must stop and listen to both the patient and the family, and ask the difficult questions about judgment and behavior in our aging patients.
REFERENCES
1. Doty L. Caregiving topics: early signs of dementia. http://alzonline.phhp.ufl.edu/en/reading/EarlySignsFeb08.pdf. Accessed December 11, 2015.
2. CDC. Older persons’ health. www.cdc.gov/nchs/fastats/older-american-health.htm. Accessed December 11, 2015.
3. Hebert LE, Weuve J, Scherr PA, Evans DL. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80:1778-1783.
4. Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimers Dement. 2013;9(2):20-245.
5. Wayne M, White M, Smith M. Understanding dementia. www.helpguide.org/articles/alzheimers-dementia/understanding-dementia.htm. Accessed December 11, 2015.
6. Smith M, Robinson L, Segal R. Age-related memory loss. www.helpguide.org/articles/memory/age-related-memory-loss.htm. Accessed December 11, 2015.
7. A guide to coping with Alzheimer’s disease: a Harvard Medical School Special Health Report. www.health.harvard.edu/special-health-reports/a-guide-to-coping-with-alzheimers-disease. Accessed December 11, 2015.
8. HelpGuide.org. What’s causing your memory loss? www.helpguide.org/harvard/whats-causing-your-memory-loss.htm. Accessed December 11, 2015.
How often do you misplace your keys or forget why you walked into a room? When I was younger, I dismissed things such as losing my train of thought (my nephew calls that a brain fart), a neglected errand (probably not important enough), or getting lost trying to go somewhere (never was good at directions anyway).
Know that I was never a “list maker.” I gave that up—because I often could not remember where I’d put it. Usually, once I wrote something down, I would eventually (in the same day) recall whatever was on it, so I wouldn’t fret about where I left that list.
Names? I could always tell you where we met, what you were wearing, and where you were sitting. But your name? Forget about it. (Those who have met me know the truth in that statement!)
During particularly stressful or busy times, if I found myself a bit more “absentminded” than usual, I would joke, “Of all the things I’ve lost, I miss my mind the most.”
Now I wonder: Just how serious are those instances of memory lapse? Yes, occasional memory lapses are part of normal aging. Just like our joints, our brains are not as young as they used to be. Even a 90-year-old with a healthy brain has experienced a loss of 10% brain cell volume.1 And let’s be honest, in celebrating major accomplishments (or failures), some of us have killed a few additional brain cells along the way (wink, wink).
We know that as we age, just as our stride has slowed, so too has the sharpness of our recall dulled. However, at what point are those misfires of our brain no longer a minor nuisance?
Data from the Administration on Aging document that in 2013, an estimated 44.7 million US residents were 65 or older.2 An estimated 5 million of them had Alzheimer disease. That translates to one in nine people—scary! This number, researchers predict, will increase to 13.8 million by 2050.3
Moreover, these statistics become more startling as we recognize that the cost of providing long-term and hospice care to people with Alzheimer disease (and other forms of dementia) is estimated to increase from $203 billion in 2013 to $1.2 trillion in 2050 (in 2013 dollars).4 Therefore, it is imperative for us, both as individuals and as health care professionals, to know the warning signs of dementia and be attentive to even seemingly subtle changes in behavior.
Early recognition that these changes are more than minor lapses in memory is important. Delays in diagnosis can result in a reduction of access to available treatments and resources. Yet, at what point do we start to consider those minor instances of forgetfulness not as normal but as indications of developing cognitive problems? My colleagues in gerontology tell us it is when those changes negatively affect activities of daily living and ability to function.
Continue for the difference between my lifelong “geographic handicap” and a form of dementia >>
What is the difference between my lifelong “geographic handicap” and a form of dementia? Would I (or any of my family or friends) recognize it? The diagnosis of dementia is not based on a sole symptom; rather, it requires the existence of at least two types of impairment that are significant and interfere with daily life.
Thankfully, I have adjusted to being “temporarily misplaced” (I don’t call it lost) and smiling at you whilst I try to remember your name. It may seem I jest or am insensitive to a grave health issue—but I am very serious about our need to pay attention to ourselves, to those we care for, and to those we care about (including neighbors). I now live in an area where a “silver alert” (missing elder) is an almost daily occurrence.
The table provides a comparison of normal-aging memory changes versus dementia symptoms; this is a tool we can use in practice and provide to our patients and their families.5 However, when changes in memory become so pervasive and severe that they are disrupting work, hobbies, social activities, and family relationships, we must recognize that they are the warning signs of Alzheimer disease.6 After reading multiple reports and guides, and witnessing the disease progression in neighbors, I share the three most significant hallmarks of the disease: impaired judgment, difficulty in recalling new information, and unusual behavior.7
It is important to remember—and to communicate to our patients—that memory loss itself does not meet the criteria for dementia. While some may be quick to fear that diagnosis, other factors that can contribute to cognitive problems are stress, depression, vitamin deficiency, thyroid disease, and even dehydration. All of these can be managed, with a resultant reversal of symptoms of memory loss.8 As always, a good health history, review of symptoms, and physical examination will guide us to an accurate diagnosis and plan of care.
There are multiple resources available for patients and families who receive a diagnosis of dementia or Alzheimer disease. Fear of the diagnosis need not blind us to the early warning signs. As NPs and PAs, despite our busy schedules, we must stop and listen to both the patient and the family, and ask the difficult questions about judgment and behavior in our aging patients.
REFERENCES
1. Doty L. Caregiving topics: early signs of dementia. http://alzonline.phhp.ufl.edu/en/reading/EarlySignsFeb08.pdf. Accessed December 11, 2015.
2. CDC. Older persons’ health. www.cdc.gov/nchs/fastats/older-american-health.htm. Accessed December 11, 2015.
3. Hebert LE, Weuve J, Scherr PA, Evans DL. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80:1778-1783.
4. Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimers Dement. 2013;9(2):20-245.
5. Wayne M, White M, Smith M. Understanding dementia. www.helpguide.org/articles/alzheimers-dementia/understanding-dementia.htm. Accessed December 11, 2015.
6. Smith M, Robinson L, Segal R. Age-related memory loss. www.helpguide.org/articles/memory/age-related-memory-loss.htm. Accessed December 11, 2015.
7. A guide to coping with Alzheimer’s disease: a Harvard Medical School Special Health Report. www.health.harvard.edu/special-health-reports/a-guide-to-coping-with-alzheimers-disease. Accessed December 11, 2015.
8. HelpGuide.org. What’s causing your memory loss? www.helpguide.org/harvard/whats-causing-your-memory-loss.htm. Accessed December 11, 2015.
Primum Non Nocere
In 1995, because of an inadvertent overdose of chemotherapy, a mother of two and beloved Boston Globe health reporter died.1 In 2001, an 18-month-old daughter and sister died of dehydration and an erroneously administered narcotic.2 In 2003, a father of two and award-winning producer for CBS died from a potentially deadly mix of drugs given with dangerous frequency.3
These are a mere representation of the number of medication errors that occur daily. In fact, on average, a hospitalized patient is subject to at least one medication error per day, which is a sobering statistic.1 These events and well-documented evidence of inadequate treatments have fueled research on prevention of medication errors—but those are but one component of the ongoing issue of patient safety in health care.
Patient safety has been on the agenda of the Institute of Medicine (IOM) for decades. Since the initial publication in 2000, the focus of To Err Is Human: Building a Safer Health System and the subsequent Quality Chasm series has been on how health care organizations emphasize patient safety, prevent medical errors, mitigate health care–associated infections and postoperative complications, and tackle breaches in safety when they occur. All these efforts concentrated primarily on medication-use processes, prescribing, packaging and education, and improving the “processes of care to ensure that patients are safe from accidental injury.”4 However, we have consistently overlooked another major problem in patient safety: diagnostic errors.
One aim of the Harvard Medical Practice Study I (1991) was developing contemporary and more reliable estimates of adverse events and negligence in hospitalized patients. The researchers defined negligence as “care that fell below the standard expected of physicians in their community.”5 In that study, the rate of adverse events due to negligence was 27.6%. In the subsequent Harvard Medical Practice Study II, researchers identified 1,276 adverse events and noted that 13.8% of them were the result of diagnostic errors.6 Further, in a systematic review of autopsy studies conducted over 40 years, data revealed that roughly 9% of subjects had a major health problem that went undetected while they were alive.6
The results of these studies are evidence that thousands of hospitalized patients die every year due to diagnostic errors. Despite data from autopsy and malpractice claims that identify diagnostic errors as preventable causes of morbidity and mortality, and the frequency with which misdiagnosis occurs, this matter has not received much consideration.7
In 2009, Newman-Toker and colleagues called attention to this oversight, recommending that diagnostic errors become the next focus of patient safety initiatives.7 Sadly, in a recent report from the IOM, we read that “most Americans will encounter at least one diagnostic error in their lifetime, sometimes with severe consequences for their physical and mental health.”8
And so we again turn our attention to improving how we deliver health care. The latest IOM report in the Quality Chasm series, Improving Diagnosis in Health Care, emphasizes the grave category of medical errors: errors of diagnosis, which include inaccurate or delayed diagnoses.8 We all know that correct and timely diagnosis is crucial to the ability to clarify a health problem, and it provides the basis for all decisions on how to solve that problem. While cure may not be possible in every situation, at the very least, our plan of care should not result in harm. What we also know is that we are members of a team, and it is within that team that we can take up the gauntlet of improving diagnosis and reducing the incidence of diagnostic errors.
The IOM Committee members who developed this report provided the following eight goals to achieve the outcome of improved diagnosis and reduced errors:
• Facilitate more effective teamwork in the diagnostic process among health care professionals, patients, and their families
• Enhance health care professional education and training in the diagnostic process
• Ensure that health information technologies support patients and health care professionals in the diagnostic process
• Develop and deploy approaches to identify, learn from, and reduce diagnostic errors and near misses in clinical practice
• Establish a work system and culture that supports the diagnostic process and improvements in diagnostic performance
• Develop a reporting environment and medical liability system that facilitates improved diagnosis through learning from diagnostic errors and near misses
• Design a payment and care delivery environment that supports the diagnostic process
• Provide dedicated funding for research on the diagnostic process and diagnostic errors.8
NPs and PAs are integral to the success of this initiative. Our responsibility, as key stakeholders in our health care system, is to identify situations that might result in these types of errors and be proactive in mitigating them. Moreover, it is our professional and moral obligation to take an active, even a leadership, role in this critical endeavor.
Read the report (available at www.nap.edu/21794) and lead the charge in your setting. I am interested in how you think this initiative will evolve, and what role you will take in advancing it as a priority in your setting; let me know by writing to NPEditor@frontlinemedcom.com.
REFERENCES
1. Aspden P, Wolcott J, Bootman JL, Cronenwett LR, eds; Committee on Identifying and Preventing Medication Errors, Institute of Medicine. Preventing Medication Errors: Quality Chasm Series. Washington, DC: National Academies Press; 2007:27.
2. Institute for Healthcare Improvement. What happened to Josie? www.ihi.org/education/IHIOpenSchool/resources/Pages/Activities/WhatHappenedtoJosieKing.aspx. Accessed October 5, 2015.
3. Andrzejczak OV. “60 Minutes” ace’s death echoes his own investigations. Houston Chronicle. July 30, 2009. www.chron.com/news/article/60-Minutes-ace-s-death-echoes-his-own-1747718.php. Accessed October 5, 2015.
4. Kohn LT, Corrigan JM, Donaldson MS, eds; Committee on Quality of Health Care in America, Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000.
5. Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients—results of the Harvard Medical Practice Study I. N Engl J Med. 1991; 324:370-376.
6. Leape LL, Brennan TA, Laird N, et al. The nature of adverse events in hospitalized patients—results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324: 377-384.
7. Newman-Toker DE, Pronovost PJ. Diagnostic errors—the next frontier for patient safety. JAMA. 2009;301(10):1060-1062.
8. Balogh EP, Miller BT, Ball JR, eds; Committee on Diagnostic Error in Health Care, Institute of Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press; 2015.
In 1995, because of an inadvertent overdose of chemotherapy, a mother of two and beloved Boston Globe health reporter died.1 In 2001, an 18-month-old daughter and sister died of dehydration and an erroneously administered narcotic.2 In 2003, a father of two and award-winning producer for CBS died from a potentially deadly mix of drugs given with dangerous frequency.3
These are a mere representation of the number of medication errors that occur daily. In fact, on average, a hospitalized patient is subject to at least one medication error per day, which is a sobering statistic.1 These events and well-documented evidence of inadequate treatments have fueled research on prevention of medication errors—but those are but one component of the ongoing issue of patient safety in health care.
Patient safety has been on the agenda of the Institute of Medicine (IOM) for decades. Since the initial publication in 2000, the focus of To Err Is Human: Building a Safer Health System and the subsequent Quality Chasm series has been on how health care organizations emphasize patient safety, prevent medical errors, mitigate health care–associated infections and postoperative complications, and tackle breaches in safety when they occur. All these efforts concentrated primarily on medication-use processes, prescribing, packaging and education, and improving the “processes of care to ensure that patients are safe from accidental injury.”4 However, we have consistently overlooked another major problem in patient safety: diagnostic errors.
One aim of the Harvard Medical Practice Study I (1991) was developing contemporary and more reliable estimates of adverse events and negligence in hospitalized patients. The researchers defined negligence as “care that fell below the standard expected of physicians in their community.”5 In that study, the rate of adverse events due to negligence was 27.6%. In the subsequent Harvard Medical Practice Study II, researchers identified 1,276 adverse events and noted that 13.8% of them were the result of diagnostic errors.6 Further, in a systematic review of autopsy studies conducted over 40 years, data revealed that roughly 9% of subjects had a major health problem that went undetected while they were alive.6
The results of these studies are evidence that thousands of hospitalized patients die every year due to diagnostic errors. Despite data from autopsy and malpractice claims that identify diagnostic errors as preventable causes of morbidity and mortality, and the frequency with which misdiagnosis occurs, this matter has not received much consideration.7
In 2009, Newman-Toker and colleagues called attention to this oversight, recommending that diagnostic errors become the next focus of patient safety initiatives.7 Sadly, in a recent report from the IOM, we read that “most Americans will encounter at least one diagnostic error in their lifetime, sometimes with severe consequences for their physical and mental health.”8
And so we again turn our attention to improving how we deliver health care. The latest IOM report in the Quality Chasm series, Improving Diagnosis in Health Care, emphasizes the grave category of medical errors: errors of diagnosis, which include inaccurate or delayed diagnoses.8 We all know that correct and timely diagnosis is crucial to the ability to clarify a health problem, and it provides the basis for all decisions on how to solve that problem. While cure may not be possible in every situation, at the very least, our plan of care should not result in harm. What we also know is that we are members of a team, and it is within that team that we can take up the gauntlet of improving diagnosis and reducing the incidence of diagnostic errors.
The IOM Committee members who developed this report provided the following eight goals to achieve the outcome of improved diagnosis and reduced errors:
• Facilitate more effective teamwork in the diagnostic process among health care professionals, patients, and their families
• Enhance health care professional education and training in the diagnostic process
• Ensure that health information technologies support patients and health care professionals in the diagnostic process
• Develop and deploy approaches to identify, learn from, and reduce diagnostic errors and near misses in clinical practice
• Establish a work system and culture that supports the diagnostic process and improvements in diagnostic performance
• Develop a reporting environment and medical liability system that facilitates improved diagnosis through learning from diagnostic errors and near misses
• Design a payment and care delivery environment that supports the diagnostic process
• Provide dedicated funding for research on the diagnostic process and diagnostic errors.8
NPs and PAs are integral to the success of this initiative. Our responsibility, as key stakeholders in our health care system, is to identify situations that might result in these types of errors and be proactive in mitigating them. Moreover, it is our professional and moral obligation to take an active, even a leadership, role in this critical endeavor.
Read the report (available at www.nap.edu/21794) and lead the charge in your setting. I am interested in how you think this initiative will evolve, and what role you will take in advancing it as a priority in your setting; let me know by writing to NPEditor@frontlinemedcom.com.
REFERENCES
1. Aspden P, Wolcott J, Bootman JL, Cronenwett LR, eds; Committee on Identifying and Preventing Medication Errors, Institute of Medicine. Preventing Medication Errors: Quality Chasm Series. Washington, DC: National Academies Press; 2007:27.
2. Institute for Healthcare Improvement. What happened to Josie? www.ihi.org/education/IHIOpenSchool/resources/Pages/Activities/WhatHappenedtoJosieKing.aspx. Accessed October 5, 2015.
3. Andrzejczak OV. “60 Minutes” ace’s death echoes his own investigations. Houston Chronicle. July 30, 2009. www.chron.com/news/article/60-Minutes-ace-s-death-echoes-his-own-1747718.php. Accessed October 5, 2015.
4. Kohn LT, Corrigan JM, Donaldson MS, eds; Committee on Quality of Health Care in America, Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000.
5. Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients—results of the Harvard Medical Practice Study I. N Engl J Med. 1991; 324:370-376.
6. Leape LL, Brennan TA, Laird N, et al. The nature of adverse events in hospitalized patients—results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324: 377-384.
7. Newman-Toker DE, Pronovost PJ. Diagnostic errors—the next frontier for patient safety. JAMA. 2009;301(10):1060-1062.
8. Balogh EP, Miller BT, Ball JR, eds; Committee on Diagnostic Error in Health Care, Institute of Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press; 2015.
In 1995, because of an inadvertent overdose of chemotherapy, a mother of two and beloved Boston Globe health reporter died.1 In 2001, an 18-month-old daughter and sister died of dehydration and an erroneously administered narcotic.2 In 2003, a father of two and award-winning producer for CBS died from a potentially deadly mix of drugs given with dangerous frequency.3
These are a mere representation of the number of medication errors that occur daily. In fact, on average, a hospitalized patient is subject to at least one medication error per day, which is a sobering statistic.1 These events and well-documented evidence of inadequate treatments have fueled research on prevention of medication errors—but those are but one component of the ongoing issue of patient safety in health care.
Patient safety has been on the agenda of the Institute of Medicine (IOM) for decades. Since the initial publication in 2000, the focus of To Err Is Human: Building a Safer Health System and the subsequent Quality Chasm series has been on how health care organizations emphasize patient safety, prevent medical errors, mitigate health care–associated infections and postoperative complications, and tackle breaches in safety when they occur. All these efforts concentrated primarily on medication-use processes, prescribing, packaging and education, and improving the “processes of care to ensure that patients are safe from accidental injury.”4 However, we have consistently overlooked another major problem in patient safety: diagnostic errors.
One aim of the Harvard Medical Practice Study I (1991) was developing contemporary and more reliable estimates of adverse events and negligence in hospitalized patients. The researchers defined negligence as “care that fell below the standard expected of physicians in their community.”5 In that study, the rate of adverse events due to negligence was 27.6%. In the subsequent Harvard Medical Practice Study II, researchers identified 1,276 adverse events and noted that 13.8% of them were the result of diagnostic errors.6 Further, in a systematic review of autopsy studies conducted over 40 years, data revealed that roughly 9% of subjects had a major health problem that went undetected while they were alive.6
The results of these studies are evidence that thousands of hospitalized patients die every year due to diagnostic errors. Despite data from autopsy and malpractice claims that identify diagnostic errors as preventable causes of morbidity and mortality, and the frequency with which misdiagnosis occurs, this matter has not received much consideration.7
In 2009, Newman-Toker and colleagues called attention to this oversight, recommending that diagnostic errors become the next focus of patient safety initiatives.7 Sadly, in a recent report from the IOM, we read that “most Americans will encounter at least one diagnostic error in their lifetime, sometimes with severe consequences for their physical and mental health.”8
And so we again turn our attention to improving how we deliver health care. The latest IOM report in the Quality Chasm series, Improving Diagnosis in Health Care, emphasizes the grave category of medical errors: errors of diagnosis, which include inaccurate or delayed diagnoses.8 We all know that correct and timely diagnosis is crucial to the ability to clarify a health problem, and it provides the basis for all decisions on how to solve that problem. While cure may not be possible in every situation, at the very least, our plan of care should not result in harm. What we also know is that we are members of a team, and it is within that team that we can take up the gauntlet of improving diagnosis and reducing the incidence of diagnostic errors.
The IOM Committee members who developed this report provided the following eight goals to achieve the outcome of improved diagnosis and reduced errors:
• Facilitate more effective teamwork in the diagnostic process among health care professionals, patients, and their families
• Enhance health care professional education and training in the diagnostic process
• Ensure that health information technologies support patients and health care professionals in the diagnostic process
• Develop and deploy approaches to identify, learn from, and reduce diagnostic errors and near misses in clinical practice
• Establish a work system and culture that supports the diagnostic process and improvements in diagnostic performance
• Develop a reporting environment and medical liability system that facilitates improved diagnosis through learning from diagnostic errors and near misses
• Design a payment and care delivery environment that supports the diagnostic process
• Provide dedicated funding for research on the diagnostic process and diagnostic errors.8
NPs and PAs are integral to the success of this initiative. Our responsibility, as key stakeholders in our health care system, is to identify situations that might result in these types of errors and be proactive in mitigating them. Moreover, it is our professional and moral obligation to take an active, even a leadership, role in this critical endeavor.
Read the report (available at www.nap.edu/21794) and lead the charge in your setting. I am interested in how you think this initiative will evolve, and what role you will take in advancing it as a priority in your setting; let me know by writing to NPEditor@frontlinemedcom.com.
REFERENCES
1. Aspden P, Wolcott J, Bootman JL, Cronenwett LR, eds; Committee on Identifying and Preventing Medication Errors, Institute of Medicine. Preventing Medication Errors: Quality Chasm Series. Washington, DC: National Academies Press; 2007:27.
2. Institute for Healthcare Improvement. What happened to Josie? www.ihi.org/education/IHIOpenSchool/resources/Pages/Activities/WhatHappenedtoJosieKing.aspx. Accessed October 5, 2015.
3. Andrzejczak OV. “60 Minutes” ace’s death echoes his own investigations. Houston Chronicle. July 30, 2009. www.chron.com/news/article/60-Minutes-ace-s-death-echoes-his-own-1747718.php. Accessed October 5, 2015.
4. Kohn LT, Corrigan JM, Donaldson MS, eds; Committee on Quality of Health Care in America, Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000.
5. Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients—results of the Harvard Medical Practice Study I. N Engl J Med. 1991; 324:370-376.
6. Leape LL, Brennan TA, Laird N, et al. The nature of adverse events in hospitalized patients—results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324: 377-384.
7. Newman-Toker DE, Pronovost PJ. Diagnostic errors—the next frontier for patient safety. JAMA. 2009;301(10):1060-1062.
8. Balogh EP, Miller BT, Ball JR, eds; Committee on Diagnostic Error in Health Care, Institute of Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press; 2015.
Be the Change You Wish to See
In a recent letter to the editors, we were queried as to the ratio of NP authors to PA authors represented in this journal and whether Clinician Reviews was changing its focus to PAs. Let me assure you, my NP colleagues, the journal always has been and always will be written for both professions. However, the query did give me pause—and the opportunity to encourage (as I have in the past) all NPs to pick up their pen (or keyboard) and start writing.
I often hear my NP colleagues diminish the work they do, the care they provide, the advocacy they undertake on behalf of patients and their families. Yet the stories of clinical problems they solve, access barriers they mitigate, or professional advances they have fostered are fascinating—and we want to read about them!
When I marvel at the accomplishments, and ask if the NP in question would write about his/her experience, the response is frequently “Oh, I can’t write” or “I could never author an article,” or (as most of us could say) “I’m too busy.”
I fully understand the hesitance of many with regard to penning an article (or being a lead for one of our clinical departments); many of us have been out of school for a bit and are so used to dictating clinical notes that we cringe at the thought of “trying” to write. I once had an NP tell me that she was not sure whether she could compose a full sentence anymore. Trust me, I could relate to her angst. I am reasonably confident that some of you are saying to yourself, “Yeah, sure.” Well, dear readers, it’s true.
When I was approached to undertake the position as NP Editor-in-Chief, I had much trepidation. I, too, lacked confidence in my writing ability and faith that anyone cared to read about what I thought or what I considered important. However, with the support of my colleagues and mentors, I was quickly disabused of those self-doubts.
We write every day—in one fashion or another. Think about it. Those of you with children: I am sure you have coached, restructured sentences, researched subject matter, and edited at least one book report. And what about e-mail? Surely, you compose at least one professional e-mail per day to a colleague or a patient. Is it ready for peer review, or does it meet the standard required for publication? Who knows? But it is writing. Moreover, the passion with which you communicate the information is why people read what you have to “say.”
It is said that a journey of a thousand miles begins with a single step (Lao Tsu, Chinese philosopher, 571-531 BC). So, too, does an article begin with one word or a single thought. If you are a regular reader of my editorials, you know that many of them (including this one!) start with a comment from a colleague, or something I read or heard in the news, or an occurrence that raised my ire. And so the seed of a column (limited to 1,000 words, by the way) is planted. Each of you has the seed of an article in you; I know you do.
This year, we celebrate the 50th anniversary of the NP profession, which was established because Loretta Ford and Henry Silva saw the need for better access to care for children. From the seed that they planted, the profession has grown and brought with it a monumental change in health care. (They likely weren’t thinking that far ahead at the time, but rather striving to address what they saw as an immediate and vital need.)
In 1985, a group of NPs saw the need for an organization dedicated to mitigating barriers to practice. A handful of people initiated a change—better representation for NPs—and a little entity named AANP began. As we know, the organization has flourished—all because a small group of people saw an opportunity to improve the status quo and stepped in to make a change. (To read more about the origins of AANP, “From the CR-chive”.)
My point is perhaps best summed up by a quote I read in an interview in the NY Times Book Review in the late 1960s. It stuck with me, to the extent that it became my mantra: “You can’t sit on the outside and complain if you don’t like something—go in and change it.”
Those of you willing to rise to this challenge will find that every publication posts its “guidelines for authors” on its website (and sometimes in the print edition). Take a few extra minutes when you are reading the journal or visiting the site to review those guidelines. Check out the types of articles or other submissions the editors accept and consider what you might contribute, based on your particular experiences, knowledge, and interest.
Do you have a particular specialty area or a “pet” disease state or condition that you want to share your expertise on? Have you learned something you wish you’d known sooner? Have you maneuvered through or around a particular barrier to practice or access? Others might benefit from knowing the keys to your accomplishment. We are quick to bemoan our plights; instead, share your success!
Start by jotting down a few words—the rest will follow. The great thing about writing is that you can do it anywhere, anytime. (For example, this editorial was written in an airport!) And please note: If you have the idea and the passion—and the wherewithal to start the writing process—there are dedicated editorial staff who will work with you to polish your submission for publication. Writing begins as a solitary pursuit, but you are not alone through the process.
So here is my challenge to you: Be an agent of change to increase the number of NP-authored columns in this publication. Have faith in your ability to write. Take it one word at a time; a few words form a sentence, a few sentences a paragraph—and before you know it, you’ve written an entire column or article.
Write from your head, your heart, or your outrage—but write! You can start by sending your thoughts on this editorial to NPEditor@frontlinemedcom.com.
In a recent letter to the editors, we were queried as to the ratio of NP authors to PA authors represented in this journal and whether Clinician Reviews was changing its focus to PAs. Let me assure you, my NP colleagues, the journal always has been and always will be written for both professions. However, the query did give me pause—and the opportunity to encourage (as I have in the past) all NPs to pick up their pen (or keyboard) and start writing.
I often hear my NP colleagues diminish the work they do, the care they provide, the advocacy they undertake on behalf of patients and their families. Yet the stories of clinical problems they solve, access barriers they mitigate, or professional advances they have fostered are fascinating—and we want to read about them!
When I marvel at the accomplishments, and ask if the NP in question would write about his/her experience, the response is frequently “Oh, I can’t write” or “I could never author an article,” or (as most of us could say) “I’m too busy.”
I fully understand the hesitance of many with regard to penning an article (or being a lead for one of our clinical departments); many of us have been out of school for a bit and are so used to dictating clinical notes that we cringe at the thought of “trying” to write. I once had an NP tell me that she was not sure whether she could compose a full sentence anymore. Trust me, I could relate to her angst. I am reasonably confident that some of you are saying to yourself, “Yeah, sure.” Well, dear readers, it’s true.
When I was approached to undertake the position as NP Editor-in-Chief, I had much trepidation. I, too, lacked confidence in my writing ability and faith that anyone cared to read about what I thought or what I considered important. However, with the support of my colleagues and mentors, I was quickly disabused of those self-doubts.
We write every day—in one fashion or another. Think about it. Those of you with children: I am sure you have coached, restructured sentences, researched subject matter, and edited at least one book report. And what about e-mail? Surely, you compose at least one professional e-mail per day to a colleague or a patient. Is it ready for peer review, or does it meet the standard required for publication? Who knows? But it is writing. Moreover, the passion with which you communicate the information is why people read what you have to “say.”
It is said that a journey of a thousand miles begins with a single step (Lao Tsu, Chinese philosopher, 571-531 BC). So, too, does an article begin with one word or a single thought. If you are a regular reader of my editorials, you know that many of them (including this one!) start with a comment from a colleague, or something I read or heard in the news, or an occurrence that raised my ire. And so the seed of a column (limited to 1,000 words, by the way) is planted. Each of you has the seed of an article in you; I know you do.
This year, we celebrate the 50th anniversary of the NP profession, which was established because Loretta Ford and Henry Silva saw the need for better access to care for children. From the seed that they planted, the profession has grown and brought with it a monumental change in health care. (They likely weren’t thinking that far ahead at the time, but rather striving to address what they saw as an immediate and vital need.)
In 1985, a group of NPs saw the need for an organization dedicated to mitigating barriers to practice. A handful of people initiated a change—better representation for NPs—and a little entity named AANP began. As we know, the organization has flourished—all because a small group of people saw an opportunity to improve the status quo and stepped in to make a change. (To read more about the origins of AANP, “From the CR-chive”.)
My point is perhaps best summed up by a quote I read in an interview in the NY Times Book Review in the late 1960s. It stuck with me, to the extent that it became my mantra: “You can’t sit on the outside and complain if you don’t like something—go in and change it.”
Those of you willing to rise to this challenge will find that every publication posts its “guidelines for authors” on its website (and sometimes in the print edition). Take a few extra minutes when you are reading the journal or visiting the site to review those guidelines. Check out the types of articles or other submissions the editors accept and consider what you might contribute, based on your particular experiences, knowledge, and interest.
Do you have a particular specialty area or a “pet” disease state or condition that you want to share your expertise on? Have you learned something you wish you’d known sooner? Have you maneuvered through or around a particular barrier to practice or access? Others might benefit from knowing the keys to your accomplishment. We are quick to bemoan our plights; instead, share your success!
Start by jotting down a few words—the rest will follow. The great thing about writing is that you can do it anywhere, anytime. (For example, this editorial was written in an airport!) And please note: If you have the idea and the passion—and the wherewithal to start the writing process—there are dedicated editorial staff who will work with you to polish your submission for publication. Writing begins as a solitary pursuit, but you are not alone through the process.
So here is my challenge to you: Be an agent of change to increase the number of NP-authored columns in this publication. Have faith in your ability to write. Take it one word at a time; a few words form a sentence, a few sentences a paragraph—and before you know it, you’ve written an entire column or article.
Write from your head, your heart, or your outrage—but write! You can start by sending your thoughts on this editorial to NPEditor@frontlinemedcom.com.
In a recent letter to the editors, we were queried as to the ratio of NP authors to PA authors represented in this journal and whether Clinician Reviews was changing its focus to PAs. Let me assure you, my NP colleagues, the journal always has been and always will be written for both professions. However, the query did give me pause—and the opportunity to encourage (as I have in the past) all NPs to pick up their pen (or keyboard) and start writing.
I often hear my NP colleagues diminish the work they do, the care they provide, the advocacy they undertake on behalf of patients and their families. Yet the stories of clinical problems they solve, access barriers they mitigate, or professional advances they have fostered are fascinating—and we want to read about them!
When I marvel at the accomplishments, and ask if the NP in question would write about his/her experience, the response is frequently “Oh, I can’t write” or “I could never author an article,” or (as most of us could say) “I’m too busy.”
I fully understand the hesitance of many with regard to penning an article (or being a lead for one of our clinical departments); many of us have been out of school for a bit and are so used to dictating clinical notes that we cringe at the thought of “trying” to write. I once had an NP tell me that she was not sure whether she could compose a full sentence anymore. Trust me, I could relate to her angst. I am reasonably confident that some of you are saying to yourself, “Yeah, sure.” Well, dear readers, it’s true.
When I was approached to undertake the position as NP Editor-in-Chief, I had much trepidation. I, too, lacked confidence in my writing ability and faith that anyone cared to read about what I thought or what I considered important. However, with the support of my colleagues and mentors, I was quickly disabused of those self-doubts.
We write every day—in one fashion or another. Think about it. Those of you with children: I am sure you have coached, restructured sentences, researched subject matter, and edited at least one book report. And what about e-mail? Surely, you compose at least one professional e-mail per day to a colleague or a patient. Is it ready for peer review, or does it meet the standard required for publication? Who knows? But it is writing. Moreover, the passion with which you communicate the information is why people read what you have to “say.”
It is said that a journey of a thousand miles begins with a single step (Lao Tsu, Chinese philosopher, 571-531 BC). So, too, does an article begin with one word or a single thought. If you are a regular reader of my editorials, you know that many of them (including this one!) start with a comment from a colleague, or something I read or heard in the news, or an occurrence that raised my ire. And so the seed of a column (limited to 1,000 words, by the way) is planted. Each of you has the seed of an article in you; I know you do.
This year, we celebrate the 50th anniversary of the NP profession, which was established because Loretta Ford and Henry Silva saw the need for better access to care for children. From the seed that they planted, the profession has grown and brought with it a monumental change in health care. (They likely weren’t thinking that far ahead at the time, but rather striving to address what they saw as an immediate and vital need.)
In 1985, a group of NPs saw the need for an organization dedicated to mitigating barriers to practice. A handful of people initiated a change—better representation for NPs—and a little entity named AANP began. As we know, the organization has flourished—all because a small group of people saw an opportunity to improve the status quo and stepped in to make a change. (To read more about the origins of AANP, “From the CR-chive”.)
My point is perhaps best summed up by a quote I read in an interview in the NY Times Book Review in the late 1960s. It stuck with me, to the extent that it became my mantra: “You can’t sit on the outside and complain if you don’t like something—go in and change it.”
Those of you willing to rise to this challenge will find that every publication posts its “guidelines for authors” on its website (and sometimes in the print edition). Take a few extra minutes when you are reading the journal or visiting the site to review those guidelines. Check out the types of articles or other submissions the editors accept and consider what you might contribute, based on your particular experiences, knowledge, and interest.
Do you have a particular specialty area or a “pet” disease state or condition that you want to share your expertise on? Have you learned something you wish you’d known sooner? Have you maneuvered through or around a particular barrier to practice or access? Others might benefit from knowing the keys to your accomplishment. We are quick to bemoan our plights; instead, share your success!
Start by jotting down a few words—the rest will follow. The great thing about writing is that you can do it anywhere, anytime. (For example, this editorial was written in an airport!) And please note: If you have the idea and the passion—and the wherewithal to start the writing process—there are dedicated editorial staff who will work with you to polish your submission for publication. Writing begins as a solitary pursuit, but you are not alone through the process.
So here is my challenge to you: Be an agent of change to increase the number of NP-authored columns in this publication. Have faith in your ability to write. Take it one word at a time; a few words form a sentence, a few sentences a paragraph—and before you know it, you’ve written an entire column or article.
Write from your head, your heart, or your outrage—but write! You can start by sending your thoughts on this editorial to NPEditor@frontlinemedcom.com.
C’mon, Give Us a Smile!
Dear readers, I assure you it is pure coincidence that your editors-in-chief would choose to write on similar topics in consecutive months. Although Randy Danielsen and I are simpatico in many ways, we do not actually sit down and coordinate our subject matter. It is simply a matter of similar tastes (ha) that leads me to present you with some musings on the same part of the anatomy that my counterpart focused on last month. Isn’t it about time the mouth got some attention?
So let me ask you: What is the first thing you notice about a person? I recently conducted a survey (albeit limited in scope and scientific rigor) to determine the answer to this question. What I found was that five out of six people notice someone’s face. Going one step further, I queried which specific component of the face they noticed; the majority said a person’s mouth and/or smile.
Smiling is a simple motion that requires only a fraction of the 36 facial muscles to produce. The pertinent percentage is source dependent—and controversial—so I will not include a specific percent or number here. What I will say is that having a smile to be proud of is not controversial at all. Moreover, what people evaluate (or, let’s be honest, pass judgment on) is the teeth as a component of that smile. Yet many children—who grow into adults, naturally—do not have healthy-looking teeth. And that, my friends, is a preventable indignity.
While conducting my research, I was intrigued to learn that Pierre Fauchard (1678-1761) was one of the first practitioners to promote scaling of the teeth and debridement of the root surfaces to prevent periodontal disease.1 Another interesting finding was that the first oral hygiene school opened in Bridgeport, Connecticut, in 1913; the Bridgeport School Board employed the first graduating class to clean the schoolchildren’s teeth, which resulted in a decreased incidence of dental caries.2 In 1945, Newburgh, New York, and Grand Rapids, Michigan, added fluoride to the public water supply, another step toward decreasing the incidence of dental caries.
Many of us recall the toothpaste commercial in which the young child comes home proudly announcing, “Look, Mom—no cavities.”3 That was more than 50 years ago, when having a cavity-free mouth was quite an accomplishment, given the limited access to dental care. And yet, sadly, access to oral health services—and the dental caries that result from lack of care—remain a serious public health problem.
But while we pride ourselves on (and admire) a beautiful smile, those pearly whites aren’t necessarily healthy. In fact, they can mask underlying oral health problems.4 It cannot be emphasized enough: Good dental health is essential to overall health.
In his editorial last month, Dr Danielsen reminded us that the mouth “is the gateway and window into health in our body.”5 We know that properly functioning teeth allow for good nutrition, which can contribute to overall health, while poor dentition can impede eating. (It can also cause speech impediments.) Unhealthy teeth and gums can contribute to pain syndromes and systemic conditions and can lead to bacterial infections in the gums, pharynx, and major organs.6 Moreover, chronic dental infections can compromise the treatment of patients with comprehensive medical conditions, including diabetes, hypertension, renal disease, or cancer.
Dental caries (or cavities) persist as the most common chronic condition among American children: 26% of preschoolers, 44% of kindergarteners, and more than half of adolescents experience preventable tooth decay.7,8 Cavities occur when certain bacteria in oral plaque utilize dietary sugars to produce acid; this gradually erodes the tooth enamel, resulting in a cavity.9 When these same bacteria spread, they cause serious facial infections that result in swelling, toxicity, and sometimes death.
The impact of oral disease is a major public health problem that must not be ignored. The disparities in oral health care cannot be mitigated simply by performing more dental procedures.9 We, as primary care providers, must emphasize the importance of prevention. We already do this with other aspects of health care; to neglect the mouth as part of the body is a regretful oversight.
As health care providers, we need to understand, and communicate to our patients, the basics of common problems such as periodontal disease—including risk factors that compromise overall health and wellness.9 We can also share with them prevention practices that will help them to manage their disease. These elements merge well with routine health maintenance.
Nurse practitioners, nurse-midwives, and physician assistants, as frontline health care providers, are in a prime position to intercede and improve the dental health of all our patients. But while we are the most likely health professionals to take the lead in advancing patient-centered care that includes a dental evaluation, our formal curricula do not include the necessary skills.
The Affordable Care Act (ACA) provided an opportunity to expand dental coverage to millions of children nationwide. The provision to designate oral health services as “essential health benefits” establishes oral health as a critical piece of overall health.10,11 Educational programs for NPs and PAs must follow suit and capitalize on the evidence-based knowledge and tools of our dental colleagues, so we can add oral health as an element of the health and wellness examination. The time has come to integrate the concepts of interprofessional oral health into the curriculum for NPs, PAs, and all health care providers.12
Remember, a “conscientiously applied program of oral hygiene and regular professional care” is an effective means of achieving a healthy smile!13 Let’s become providers of at least some of that professional care. Please share your thoughts with me at NPEditor@frontlinemedcom.com.
REFERENCES
1. Feinberg EM. A short history of modern dentistry. www.edwardfeinbergdmd.com/history-of-dentistry. Accessed April 8, 2015.
2. American Dental Association. History of dentistry timeline. www.ada.org/en/about-the-ada/ada-history-and-presidents-of-the-ada/ada-history-of-dentistry-timeline. Accessed April 8, 2015.
3. 1958 Crest toothpaste commercial. www.youtube.com/watch?v=v72NHYp8KD4. Accessed April 8, 2015.
4. Proctor & Gamble. Crest heritage. www.crest.com/about-crest/crestheritage.aspx. Accessed April 8, 2015.
5. Danielsen RDD. It’s all about the spit! Clin Rev. 2015;25(4):4,6.
6. Feinberg EM. The importance of dentistry. www.edwardfeinbergdmd.com/adult-den tistry/importance-of-dentistry. Accessed April 8, 2015.
7. American Dental Association and the CDC. Water fluoridation: nature’s way to prevent tooth decay. www.cdc.gov/Fluoridation/pdf/natures_way.pdf. Accessed April 8, 2015.
8. Dye BA, Tan S, Smith V, et al; National Center for Health Statistics. (2007), Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat. 2007;11(248).
9. American Dental Association. Four dental conditions—prevention summit primer (2013). www.ada.org/~/media/ADA/Public%20Programs/File/2013_Prevention_Summit_Primer_on_Four_Dental_Conditions.ashx. Accessed April 8, 2015.
10. Stahl EM, Reusch C. Ensuring access to pediatric dental benefits in the Affordable Care Act (ACA). http://neach.communitycatalyst.org/publications/asset/Pedi_dental_final_5-29-13.pdf. Accessed April 8, 2015.
11. Patient Protection and Affordable Care Act. Section 1302(b)(4)(F).
12. Haber J, Altman S, Moursi A, et al. Oral health challenges in pregnancy and childhood [webinar]. National Organization of Nurse Practitioner Faculties. 2015. www.nonpf.org/events/event_details.asp?id=508645. Accessed April 8, 2015.
13. American Dental Association, Council on Dental Therapeutics. Evaluation of Crest toothpaste. J Am Dent Assoc. 1960;61:272-274.
Dear readers, I assure you it is pure coincidence that your editors-in-chief would choose to write on similar topics in consecutive months. Although Randy Danielsen and I are simpatico in many ways, we do not actually sit down and coordinate our subject matter. It is simply a matter of similar tastes (ha) that leads me to present you with some musings on the same part of the anatomy that my counterpart focused on last month. Isn’t it about time the mouth got some attention?
So let me ask you: What is the first thing you notice about a person? I recently conducted a survey (albeit limited in scope and scientific rigor) to determine the answer to this question. What I found was that five out of six people notice someone’s face. Going one step further, I queried which specific component of the face they noticed; the majority said a person’s mouth and/or smile.
Smiling is a simple motion that requires only a fraction of the 36 facial muscles to produce. The pertinent percentage is source dependent—and controversial—so I will not include a specific percent or number here. What I will say is that having a smile to be proud of is not controversial at all. Moreover, what people evaluate (or, let’s be honest, pass judgment on) is the teeth as a component of that smile. Yet many children—who grow into adults, naturally—do not have healthy-looking teeth. And that, my friends, is a preventable indignity.
While conducting my research, I was intrigued to learn that Pierre Fauchard (1678-1761) was one of the first practitioners to promote scaling of the teeth and debridement of the root surfaces to prevent periodontal disease.1 Another interesting finding was that the first oral hygiene school opened in Bridgeport, Connecticut, in 1913; the Bridgeport School Board employed the first graduating class to clean the schoolchildren’s teeth, which resulted in a decreased incidence of dental caries.2 In 1945, Newburgh, New York, and Grand Rapids, Michigan, added fluoride to the public water supply, another step toward decreasing the incidence of dental caries.
Many of us recall the toothpaste commercial in which the young child comes home proudly announcing, “Look, Mom—no cavities.”3 That was more than 50 years ago, when having a cavity-free mouth was quite an accomplishment, given the limited access to dental care. And yet, sadly, access to oral health services—and the dental caries that result from lack of care—remain a serious public health problem.
But while we pride ourselves on (and admire) a beautiful smile, those pearly whites aren’t necessarily healthy. In fact, they can mask underlying oral health problems.4 It cannot be emphasized enough: Good dental health is essential to overall health.
In his editorial last month, Dr Danielsen reminded us that the mouth “is the gateway and window into health in our body.”5 We know that properly functioning teeth allow for good nutrition, which can contribute to overall health, while poor dentition can impede eating. (It can also cause speech impediments.) Unhealthy teeth and gums can contribute to pain syndromes and systemic conditions and can lead to bacterial infections in the gums, pharynx, and major organs.6 Moreover, chronic dental infections can compromise the treatment of patients with comprehensive medical conditions, including diabetes, hypertension, renal disease, or cancer.
Dental caries (or cavities) persist as the most common chronic condition among American children: 26% of preschoolers, 44% of kindergarteners, and more than half of adolescents experience preventable tooth decay.7,8 Cavities occur when certain bacteria in oral plaque utilize dietary sugars to produce acid; this gradually erodes the tooth enamel, resulting in a cavity.9 When these same bacteria spread, they cause serious facial infections that result in swelling, toxicity, and sometimes death.
The impact of oral disease is a major public health problem that must not be ignored. The disparities in oral health care cannot be mitigated simply by performing more dental procedures.9 We, as primary care providers, must emphasize the importance of prevention. We already do this with other aspects of health care; to neglect the mouth as part of the body is a regretful oversight.
As health care providers, we need to understand, and communicate to our patients, the basics of common problems such as periodontal disease—including risk factors that compromise overall health and wellness.9 We can also share with them prevention practices that will help them to manage their disease. These elements merge well with routine health maintenance.
Nurse practitioners, nurse-midwives, and physician assistants, as frontline health care providers, are in a prime position to intercede and improve the dental health of all our patients. But while we are the most likely health professionals to take the lead in advancing patient-centered care that includes a dental evaluation, our formal curricula do not include the necessary skills.
The Affordable Care Act (ACA) provided an opportunity to expand dental coverage to millions of children nationwide. The provision to designate oral health services as “essential health benefits” establishes oral health as a critical piece of overall health.10,11 Educational programs for NPs and PAs must follow suit and capitalize on the evidence-based knowledge and tools of our dental colleagues, so we can add oral health as an element of the health and wellness examination. The time has come to integrate the concepts of interprofessional oral health into the curriculum for NPs, PAs, and all health care providers.12
Remember, a “conscientiously applied program of oral hygiene and regular professional care” is an effective means of achieving a healthy smile!13 Let’s become providers of at least some of that professional care. Please share your thoughts with me at NPEditor@frontlinemedcom.com.
REFERENCES
1. Feinberg EM. A short history of modern dentistry. www.edwardfeinbergdmd.com/history-of-dentistry. Accessed April 8, 2015.
2. American Dental Association. History of dentistry timeline. www.ada.org/en/about-the-ada/ada-history-and-presidents-of-the-ada/ada-history-of-dentistry-timeline. Accessed April 8, 2015.
3. 1958 Crest toothpaste commercial. www.youtube.com/watch?v=v72NHYp8KD4. Accessed April 8, 2015.
4. Proctor & Gamble. Crest heritage. www.crest.com/about-crest/crestheritage.aspx. Accessed April 8, 2015.
5. Danielsen RDD. It’s all about the spit! Clin Rev. 2015;25(4):4,6.
6. Feinberg EM. The importance of dentistry. www.edwardfeinbergdmd.com/adult-den tistry/importance-of-dentistry. Accessed April 8, 2015.
7. American Dental Association and the CDC. Water fluoridation: nature’s way to prevent tooth decay. www.cdc.gov/Fluoridation/pdf/natures_way.pdf. Accessed April 8, 2015.
8. Dye BA, Tan S, Smith V, et al; National Center for Health Statistics. (2007), Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat. 2007;11(248).
9. American Dental Association. Four dental conditions—prevention summit primer (2013). www.ada.org/~/media/ADA/Public%20Programs/File/2013_Prevention_Summit_Primer_on_Four_Dental_Conditions.ashx. Accessed April 8, 2015.
10. Stahl EM, Reusch C. Ensuring access to pediatric dental benefits in the Affordable Care Act (ACA). http://neach.communitycatalyst.org/publications/asset/Pedi_dental_final_5-29-13.pdf. Accessed April 8, 2015.
11. Patient Protection and Affordable Care Act. Section 1302(b)(4)(F).
12. Haber J, Altman S, Moursi A, et al. Oral health challenges in pregnancy and childhood [webinar]. National Organization of Nurse Practitioner Faculties. 2015. www.nonpf.org/events/event_details.asp?id=508645. Accessed April 8, 2015.
13. American Dental Association, Council on Dental Therapeutics. Evaluation of Crest toothpaste. J Am Dent Assoc. 1960;61:272-274.
Dear readers, I assure you it is pure coincidence that your editors-in-chief would choose to write on similar topics in consecutive months. Although Randy Danielsen and I are simpatico in many ways, we do not actually sit down and coordinate our subject matter. It is simply a matter of similar tastes (ha) that leads me to present you with some musings on the same part of the anatomy that my counterpart focused on last month. Isn’t it about time the mouth got some attention?
So let me ask you: What is the first thing you notice about a person? I recently conducted a survey (albeit limited in scope and scientific rigor) to determine the answer to this question. What I found was that five out of six people notice someone’s face. Going one step further, I queried which specific component of the face they noticed; the majority said a person’s mouth and/or smile.
Smiling is a simple motion that requires only a fraction of the 36 facial muscles to produce. The pertinent percentage is source dependent—and controversial—so I will not include a specific percent or number here. What I will say is that having a smile to be proud of is not controversial at all. Moreover, what people evaluate (or, let’s be honest, pass judgment on) is the teeth as a component of that smile. Yet many children—who grow into adults, naturally—do not have healthy-looking teeth. And that, my friends, is a preventable indignity.
While conducting my research, I was intrigued to learn that Pierre Fauchard (1678-1761) was one of the first practitioners to promote scaling of the teeth and debridement of the root surfaces to prevent periodontal disease.1 Another interesting finding was that the first oral hygiene school opened in Bridgeport, Connecticut, in 1913; the Bridgeport School Board employed the first graduating class to clean the schoolchildren’s teeth, which resulted in a decreased incidence of dental caries.2 In 1945, Newburgh, New York, and Grand Rapids, Michigan, added fluoride to the public water supply, another step toward decreasing the incidence of dental caries.
Many of us recall the toothpaste commercial in which the young child comes home proudly announcing, “Look, Mom—no cavities.”3 That was more than 50 years ago, when having a cavity-free mouth was quite an accomplishment, given the limited access to dental care. And yet, sadly, access to oral health services—and the dental caries that result from lack of care—remain a serious public health problem.
But while we pride ourselves on (and admire) a beautiful smile, those pearly whites aren’t necessarily healthy. In fact, they can mask underlying oral health problems.4 It cannot be emphasized enough: Good dental health is essential to overall health.
In his editorial last month, Dr Danielsen reminded us that the mouth “is the gateway and window into health in our body.”5 We know that properly functioning teeth allow for good nutrition, which can contribute to overall health, while poor dentition can impede eating. (It can also cause speech impediments.) Unhealthy teeth and gums can contribute to pain syndromes and systemic conditions and can lead to bacterial infections in the gums, pharynx, and major organs.6 Moreover, chronic dental infections can compromise the treatment of patients with comprehensive medical conditions, including diabetes, hypertension, renal disease, or cancer.
Dental caries (or cavities) persist as the most common chronic condition among American children: 26% of preschoolers, 44% of kindergarteners, and more than half of adolescents experience preventable tooth decay.7,8 Cavities occur when certain bacteria in oral plaque utilize dietary sugars to produce acid; this gradually erodes the tooth enamel, resulting in a cavity.9 When these same bacteria spread, they cause serious facial infections that result in swelling, toxicity, and sometimes death.
The impact of oral disease is a major public health problem that must not be ignored. The disparities in oral health care cannot be mitigated simply by performing more dental procedures.9 We, as primary care providers, must emphasize the importance of prevention. We already do this with other aspects of health care; to neglect the mouth as part of the body is a regretful oversight.
As health care providers, we need to understand, and communicate to our patients, the basics of common problems such as periodontal disease—including risk factors that compromise overall health and wellness.9 We can also share with them prevention practices that will help them to manage their disease. These elements merge well with routine health maintenance.
Nurse practitioners, nurse-midwives, and physician assistants, as frontline health care providers, are in a prime position to intercede and improve the dental health of all our patients. But while we are the most likely health professionals to take the lead in advancing patient-centered care that includes a dental evaluation, our formal curricula do not include the necessary skills.
The Affordable Care Act (ACA) provided an opportunity to expand dental coverage to millions of children nationwide. The provision to designate oral health services as “essential health benefits” establishes oral health as a critical piece of overall health.10,11 Educational programs for NPs and PAs must follow suit and capitalize on the evidence-based knowledge and tools of our dental colleagues, so we can add oral health as an element of the health and wellness examination. The time has come to integrate the concepts of interprofessional oral health into the curriculum for NPs, PAs, and all health care providers.12
Remember, a “conscientiously applied program of oral hygiene and regular professional care” is an effective means of achieving a healthy smile!13 Let’s become providers of at least some of that professional care. Please share your thoughts with me at NPEditor@frontlinemedcom.com.
REFERENCES
1. Feinberg EM. A short history of modern dentistry. www.edwardfeinbergdmd.com/history-of-dentistry. Accessed April 8, 2015.
2. American Dental Association. History of dentistry timeline. www.ada.org/en/about-the-ada/ada-history-and-presidents-of-the-ada/ada-history-of-dentistry-timeline. Accessed April 8, 2015.
3. 1958 Crest toothpaste commercial. www.youtube.com/watch?v=v72NHYp8KD4. Accessed April 8, 2015.
4. Proctor & Gamble. Crest heritage. www.crest.com/about-crest/crestheritage.aspx. Accessed April 8, 2015.
5. Danielsen RDD. It’s all about the spit! Clin Rev. 2015;25(4):4,6.
6. Feinberg EM. The importance of dentistry. www.edwardfeinbergdmd.com/adult-den tistry/importance-of-dentistry. Accessed April 8, 2015.
7. American Dental Association and the CDC. Water fluoridation: nature’s way to prevent tooth decay. www.cdc.gov/Fluoridation/pdf/natures_way.pdf. Accessed April 8, 2015.
8. Dye BA, Tan S, Smith V, et al; National Center for Health Statistics. (2007), Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat. 2007;11(248).
9. American Dental Association. Four dental conditions—prevention summit primer (2013). www.ada.org/~/media/ADA/Public%20Programs/File/2013_Prevention_Summit_Primer_on_Four_Dental_Conditions.ashx. Accessed April 8, 2015.
10. Stahl EM, Reusch C. Ensuring access to pediatric dental benefits in the Affordable Care Act (ACA). http://neach.communitycatalyst.org/publications/asset/Pedi_dental_final_5-29-13.pdf. Accessed April 8, 2015.
11. Patient Protection and Affordable Care Act. Section 1302(b)(4)(F).
12. Haber J, Altman S, Moursi A, et al. Oral health challenges in pregnancy and childhood [webinar]. National Organization of Nurse Practitioner Faculties. 2015. www.nonpf.org/events/event_details.asp?id=508645. Accessed April 8, 2015.
13. American Dental Association, Council on Dental Therapeutics. Evaluation of Crest toothpaste. J Am Dent Assoc. 1960;61:272-274.
Don’t Put Me in, Coach
| On a recent Friday afternoon, I was watching a college basketball game on television. Seconds after the players returned to the court from a time-out, one player collided with another, knocking him backward. The opponent landed on his back, hitting his head so hard it bounced up and hit the floor again. Lying somewhat still, he held his head as though trying to make it stop moving. Moments later, he was assisted to his feet, insisting he was fine, but the referee sent him to the bench for evaluation—despite resistance from the player and his coach. The coach continued to pressure the referee, who firmly stood his ground. Zoom in: Player sitting on the bench, undergoing a neurologic evaluation. Even through the TV, it was evident the player was unable to hold his gaze through the visual field process. Score two points for the referee! In another game, on a different day with different teams, a similar event occurred: A player fell, banged his head, and was obviously stunned. Yet he was allowed to return to play. His mother came out of the stands protesting, insisting her son was hurt. The referee and coach dismissed her objections, and she was ushered back to her seat by security. Technical fouls for the coach and referee! While not every bump, blow, or jolt to the head will result in a traumatic brain injury (TBI), nonetheless, TBI has become a serious public health issue, contributing to one-third (30.5%) of all injury-related deaths.1 An estimated 1.7 million TBIs occur annually; between 2001 and 2005, nearly 208,000 emergency department visits for concussions and other TBIs related to sports and recreational activities were reported per year.1,2 Recently, we have begun to recognize that even the seemingly “benign” head injuries athletes sustain during play are not without some complications—short term as well as long term. In the past two or three years, researchers have started to focus on and explore the effects of “subconcussive” blows to the head, with unanticipated results. In a 2010 study of high school football players, researchers from Purdue University identified a previously unknown category of athletes who, despite having no clinically observable signs of concussion, showed measurable impairment of neurocognitive function (primarily visual working memory) on neurocognitive tests, as well as altered activation in neurophysiologic function on MRI.3 As a result of this and additional studies, repeated minor “bumps” are now viewed through a different lens—even the mild ones can take their toll, impeding language processing or motor skills. The May 2012 suicide of Junior Seau, a former professional football player who sustained repeated blows to the head during his career, was a further wake-up call. It has become increasingly clear that the blows to the head sustained by players in a variety of sports and recreational activities require more serious attention—and we need to address it earlier in an athlete’s career (amateur or professional), not once the irreparable damage is done. The first law to address concussion management in youth athletics was passed in Washington State in May 2009. By 2012, 42 additional states and the District of Columbia had passed similar laws.4 The intent of these “Return to Play” laws is to reduce the impact of youth sports and recreation–related concussions, and their tenets can extend to our college and professional athletes. The long-term effects of repeated blows to the head have only begun to surface. We need to be diligent in recognizing and preventing TBI in all athletes, because doing so can prevent further brain injury or even death. Arm yourself with information; the CDC Web site is an excellent resource (www.cdc.gov/concussion/sports/index.html). Finally, a message to all coaches and parents, athletes, and health care professionals: Getting your “bell rung” in a sports event should not be taken lightly. It must be recognized as the serious and potentially dangerous occurrence it is. So, don’t put him in, coach—he may not be ready to play! Share your thoughts and experiences with me at NPEditor@frontlinemedcom.com. References 2. Gilchrist J, Thomas KE, Xu L, et al. Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged ≤ 19 years—United States, 2001–2009. MMWR Morbid Mortal Wkly Rep. 2011;60: 1337-1342. 3. Talavage T, Nauman E, Breedlove E, et al. Functionally detected cognitive impairment in high school football players without clinically diagnosed concussion. J Neurotrauma. 2010; Oct 1 [Epub ahead of print]. 4. CDC National Center for Injury Prevention and Control. Implementing Return to Play: Learning from the Experiences of Early Implementers. www.cdc.gov/concussion/pdf/RTP_ Implementation-a.pdf. |
| On a recent Friday afternoon, I was watching a college basketball game on television. Seconds after the players returned to the court from a time-out, one player collided with another, knocking him backward. The opponent landed on his back, hitting his head so hard it bounced up and hit the floor again. Lying somewhat still, he held his head as though trying to make it stop moving. Moments later, he was assisted to his feet, insisting he was fine, but the referee sent him to the bench for evaluation—despite resistance from the player and his coach. The coach continued to pressure the referee, who firmly stood his ground. Zoom in: Player sitting on the bench, undergoing a neurologic evaluation. Even through the TV, it was evident the player was unable to hold his gaze through the visual field process. Score two points for the referee! In another game, on a different day with different teams, a similar event occurred: A player fell, banged his head, and was obviously stunned. Yet he was allowed to return to play. His mother came out of the stands protesting, insisting her son was hurt. The referee and coach dismissed her objections, and she was ushered back to her seat by security. Technical fouls for the coach and referee! While not every bump, blow, or jolt to the head will result in a traumatic brain injury (TBI), nonetheless, TBI has become a serious public health issue, contributing to one-third (30.5%) of all injury-related deaths.1 An estimated 1.7 million TBIs occur annually; between 2001 and 2005, nearly 208,000 emergency department visits for concussions and other TBIs related to sports and recreational activities were reported per year.1,2 Recently, we have begun to recognize that even the seemingly “benign” head injuries athletes sustain during play are not without some complications—short term as well as long term. In the past two or three years, researchers have started to focus on and explore the effects of “subconcussive” blows to the head, with unanticipated results. In a 2010 study of high school football players, researchers from Purdue University identified a previously unknown category of athletes who, despite having no clinically observable signs of concussion, showed measurable impairment of neurocognitive function (primarily visual working memory) on neurocognitive tests, as well as altered activation in neurophysiologic function on MRI.3 As a result of this and additional studies, repeated minor “bumps” are now viewed through a different lens—even the mild ones can take their toll, impeding language processing or motor skills. The May 2012 suicide of Junior Seau, a former professional football player who sustained repeated blows to the head during his career, was a further wake-up call. It has become increasingly clear that the blows to the head sustained by players in a variety of sports and recreational activities require more serious attention—and we need to address it earlier in an athlete’s career (amateur or professional), not once the irreparable damage is done. The first law to address concussion management in youth athletics was passed in Washington State in May 2009. By 2012, 42 additional states and the District of Columbia had passed similar laws.4 The intent of these “Return to Play” laws is to reduce the impact of youth sports and recreation–related concussions, and their tenets can extend to our college and professional athletes. The long-term effects of repeated blows to the head have only begun to surface. We need to be diligent in recognizing and preventing TBI in all athletes, because doing so can prevent further brain injury or even death. Arm yourself with information; the CDC Web site is an excellent resource (www.cdc.gov/concussion/sports/index.html). Finally, a message to all coaches and parents, athletes, and health care professionals: Getting your “bell rung” in a sports event should not be taken lightly. It must be recognized as the serious and potentially dangerous occurrence it is. So, don’t put him in, coach—he may not be ready to play! Share your thoughts and experiences with me at NPEditor@frontlinemedcom.com. References 2. Gilchrist J, Thomas KE, Xu L, et al. Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged ≤ 19 years—United States, 2001–2009. MMWR Morbid Mortal Wkly Rep. 2011;60: 1337-1342. 3. Talavage T, Nauman E, Breedlove E, et al. Functionally detected cognitive impairment in high school football players without clinically diagnosed concussion. J Neurotrauma. 2010; Oct 1 [Epub ahead of print]. 4. CDC National Center for Injury Prevention and Control. Implementing Return to Play: Learning from the Experiences of Early Implementers. www.cdc.gov/concussion/pdf/RTP_ Implementation-a.pdf. |
| On a recent Friday afternoon, I was watching a college basketball game on television. Seconds after the players returned to the court from a time-out, one player collided with another, knocking him backward. The opponent landed on his back, hitting his head so hard it bounced up and hit the floor again. Lying somewhat still, he held his head as though trying to make it stop moving. Moments later, he was assisted to his feet, insisting he was fine, but the referee sent him to the bench for evaluation—despite resistance from the player and his coach. The coach continued to pressure the referee, who firmly stood his ground. Zoom in: Player sitting on the bench, undergoing a neurologic evaluation. Even through the TV, it was evident the player was unable to hold his gaze through the visual field process. Score two points for the referee! In another game, on a different day with different teams, a similar event occurred: A player fell, banged his head, and was obviously stunned. Yet he was allowed to return to play. His mother came out of the stands protesting, insisting her son was hurt. The referee and coach dismissed her objections, and she was ushered back to her seat by security. Technical fouls for the coach and referee! While not every bump, blow, or jolt to the head will result in a traumatic brain injury (TBI), nonetheless, TBI has become a serious public health issue, contributing to one-third (30.5%) of all injury-related deaths.1 An estimated 1.7 million TBIs occur annually; between 2001 and 2005, nearly 208,000 emergency department visits for concussions and other TBIs related to sports and recreational activities were reported per year.1,2 Recently, we have begun to recognize that even the seemingly “benign” head injuries athletes sustain during play are not without some complications—short term as well as long term. In the past two or three years, researchers have started to focus on and explore the effects of “subconcussive” blows to the head, with unanticipated results. In a 2010 study of high school football players, researchers from Purdue University identified a previously unknown category of athletes who, despite having no clinically observable signs of concussion, showed measurable impairment of neurocognitive function (primarily visual working memory) on neurocognitive tests, as well as altered activation in neurophysiologic function on MRI.3 As a result of this and additional studies, repeated minor “bumps” are now viewed through a different lens—even the mild ones can take their toll, impeding language processing or motor skills. The May 2012 suicide of Junior Seau, a former professional football player who sustained repeated blows to the head during his career, was a further wake-up call. It has become increasingly clear that the blows to the head sustained by players in a variety of sports and recreational activities require more serious attention—and we need to address it earlier in an athlete’s career (amateur or professional), not once the irreparable damage is done. The first law to address concussion management in youth athletics was passed in Washington State in May 2009. By 2012, 42 additional states and the District of Columbia had passed similar laws.4 The intent of these “Return to Play” laws is to reduce the impact of youth sports and recreation–related concussions, and their tenets can extend to our college and professional athletes. The long-term effects of repeated blows to the head have only begun to surface. We need to be diligent in recognizing and preventing TBI in all athletes, because doing so can prevent further brain injury or even death. Arm yourself with information; the CDC Web site is an excellent resource (www.cdc.gov/concussion/sports/index.html). Finally, a message to all coaches and parents, athletes, and health care professionals: Getting your “bell rung” in a sports event should not be taken lightly. It must be recognized as the serious and potentially dangerous occurrence it is. So, don’t put him in, coach—he may not be ready to play! Share your thoughts and experiences with me at NPEditor@frontlinemedcom.com. References 2. Gilchrist J, Thomas KE, Xu L, et al. Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged ≤ 19 years—United States, 2001–2009. MMWR Morbid Mortal Wkly Rep. 2011;60: 1337-1342. 3. Talavage T, Nauman E, Breedlove E, et al. Functionally detected cognitive impairment in high school football players without clinically diagnosed concussion. J Neurotrauma. 2010; Oct 1 [Epub ahead of print]. 4. CDC National Center for Injury Prevention and Control. Implementing Return to Play: Learning from the Experiences of Early Implementers. www.cdc.gov/concussion/pdf/RTP_ Implementation-a.pdf. |
Don't Put Me in, Coach
On a recent Friday afternoon, I was watching a college basketball game on television. Seconds after the players returned to the court from a time-out, one player collided with another, knocking him backward. The opponent landed on his back, hitting his head so hard it bounced up and hit the floor again.
Lying somewhat still, he held his head as though trying to make it stop moving. Moments later, he was assisted to his feet, insisting he was fine, but the referee sent him to the bench for evaluation—despite resistance from the player and his coach. The coach continued to pressure the referee, who firmly stood his ground. Zoom in: Player sitting on the bench, undergoing a neurologic evaluation. Even through the TV, it was evident the player was unable to hold his gaze through the visual field process. Score two points for the referee! |
In another game, on a different day with different teams, a similar event occurred: A player fell, banged his head, and was obviously stunned. Yet he was allowed to return to play. His mother came out of the stands protesting, insisting her son was hurt. The referee and coach dismissed her objections, and she was ushered back to her seat by security. Technical fouls for the coach and referee! |
While not every bump, blow, or jolt to the head will result in a traumatic brain injury (TBI), nonetheless, TBI has become a serious public health issue, contributing to one-third (30.5%) of all injury-related deaths.1 An estimated 1.7 million TBIs occur annually; between 2001 and 2005, nearly 208,000 emergency department visits for concussions and other TBIs related to sports and recreational activities were reported per year.1,2 |
Recently, we have begun to recognize that even the seemingly "benign" head injuries athletes sustain during play are not without some complications—short term as well as long term. In the past two or three years, researchers have started to focus on and explore the effects of "subconcussive" blows to the head, with unanticipated results. |
In a 2010 study of high school football players, researchers from Purdue University identified a previously unknown category of athletes who, despite having no clinically observable signs of concussion, showed measurable impairment of neurocognitive function (primarily visual working memory) on neurocognitive tests, as well as altered activation in neurophysiologic function on MRI.3 As a result of this and additional studies, repeated minor "bumps" are now viewed through a different lens—even the mild ones can take their toll, impeding language processing or motor skills. |
The May 2012 suicide of Junior Seau, a former professional football player who sustained repeated blows to the head during his career, was a further wake-up call. It has become increasingly clear that the blows to the head sustained by players in a variety of sports and recreational activities require more serious attention—and we need to address it earlier in an athlete's career (amateur or professional), not once the irreparable damage is done. |
The first law to address concussion management in youth athletics was passed in Washington State in May 2009. By 2012, 42 additional states and the District of Columbia had passed similar laws.4 The intent of these "Return to Play" laws is to reduce the impact of youth sports and recreation–related concussions, and their tenets can extend to our college and professional athletes. |
The long-term effects of repeated blows to the head have only begun to surface. We need to be diligent in recognizing and preventing TBI in all athletes, because doing so can prevent further brain injury or even death. Arm yourself with information; the CDC Web site is an excellent resource (www.cdc.gov/concussion/sports/index.html). |
Finally, a message to all coaches and parents, athletes, and health care professionals: Getting your "bell rung" in a sports event should not be taken lightly. It must be recognized as the serious and potentially dangerous occurrence it is. So, don't put him in, coach—he may not be ready to play! |
Share your thoughts and experiences with me at NPEditor@frontlinemedcom.com.
|
On a recent Friday afternoon, I was watching a college basketball game on television. Seconds after the players returned to the court from a time-out, one player collided with another, knocking him backward. The opponent landed on his back, hitting his head so hard it bounced up and hit the floor again.
Lying somewhat still, he held his head as though trying to make it stop moving. Moments later, he was assisted to his feet, insisting he was fine, but the referee sent him to the bench for evaluation—despite resistance from the player and his coach. The coach continued to pressure the referee, who firmly stood his ground. Zoom in: Player sitting on the bench, undergoing a neurologic evaluation. Even through the TV, it was evident the player was unable to hold his gaze through the visual field process. Score two points for the referee! |
In another game, on a different day with different teams, a similar event occurred: A player fell, banged his head, and was obviously stunned. Yet he was allowed to return to play. His mother came out of the stands protesting, insisting her son was hurt. The referee and coach dismissed her objections, and she was ushered back to her seat by security. Technical fouls for the coach and referee! |
While not every bump, blow, or jolt to the head will result in a traumatic brain injury (TBI), nonetheless, TBI has become a serious public health issue, contributing to one-third (30.5%) of all injury-related deaths.1 An estimated 1.7 million TBIs occur annually; between 2001 and 2005, nearly 208,000 emergency department visits for concussions and other TBIs related to sports and recreational activities were reported per year.1,2 |
Recently, we have begun to recognize that even the seemingly "benign" head injuries athletes sustain during play are not without some complications—short term as well as long term. In the past two or three years, researchers have started to focus on and explore the effects of "subconcussive" blows to the head, with unanticipated results. |
In a 2010 study of high school football players, researchers from Purdue University identified a previously unknown category of athletes who, despite having no clinically observable signs of concussion, showed measurable impairment of neurocognitive function (primarily visual working memory) on neurocognitive tests, as well as altered activation in neurophysiologic function on MRI.3 As a result of this and additional studies, repeated minor "bumps" are now viewed through a different lens—even the mild ones can take their toll, impeding language processing or motor skills. |
The May 2012 suicide of Junior Seau, a former professional football player who sustained repeated blows to the head during his career, was a further wake-up call. It has become increasingly clear that the blows to the head sustained by players in a variety of sports and recreational activities require more serious attention—and we need to address it earlier in an athlete's career (amateur or professional), not once the irreparable damage is done. |
The first law to address concussion management in youth athletics was passed in Washington State in May 2009. By 2012, 42 additional states and the District of Columbia had passed similar laws.4 The intent of these "Return to Play" laws is to reduce the impact of youth sports and recreation–related concussions, and their tenets can extend to our college and professional athletes. |
The long-term effects of repeated blows to the head have only begun to surface. We need to be diligent in recognizing and preventing TBI in all athletes, because doing so can prevent further brain injury or even death. Arm yourself with information; the CDC Web site is an excellent resource (www.cdc.gov/concussion/sports/index.html). |
Finally, a message to all coaches and parents, athletes, and health care professionals: Getting your "bell rung" in a sports event should not be taken lightly. It must be recognized as the serious and potentially dangerous occurrence it is. So, don't put him in, coach—he may not be ready to play! |
Share your thoughts and experiences with me at NPEditor@frontlinemedcom.com.
|
On a recent Friday afternoon, I was watching a college basketball game on television. Seconds after the players returned to the court from a time-out, one player collided with another, knocking him backward. The opponent landed on his back, hitting his head so hard it bounced up and hit the floor again.
Lying somewhat still, he held his head as though trying to make it stop moving. Moments later, he was assisted to his feet, insisting he was fine, but the referee sent him to the bench for evaluation—despite resistance from the player and his coach. The coach continued to pressure the referee, who firmly stood his ground. Zoom in: Player sitting on the bench, undergoing a neurologic evaluation. Even through the TV, it was evident the player was unable to hold his gaze through the visual field process. Score two points for the referee! |
In another game, on a different day with different teams, a similar event occurred: A player fell, banged his head, and was obviously stunned. Yet he was allowed to return to play. His mother came out of the stands protesting, insisting her son was hurt. The referee and coach dismissed her objections, and she was ushered back to her seat by security. Technical fouls for the coach and referee! |
While not every bump, blow, or jolt to the head will result in a traumatic brain injury (TBI), nonetheless, TBI has become a serious public health issue, contributing to one-third (30.5%) of all injury-related deaths.1 An estimated 1.7 million TBIs occur annually; between 2001 and 2005, nearly 208,000 emergency department visits for concussions and other TBIs related to sports and recreational activities were reported per year.1,2 |
Recently, we have begun to recognize that even the seemingly "benign" head injuries athletes sustain during play are not without some complications—short term as well as long term. In the past two or three years, researchers have started to focus on and explore the effects of "subconcussive" blows to the head, with unanticipated results. |
In a 2010 study of high school football players, researchers from Purdue University identified a previously unknown category of athletes who, despite having no clinically observable signs of concussion, showed measurable impairment of neurocognitive function (primarily visual working memory) on neurocognitive tests, as well as altered activation in neurophysiologic function on MRI.3 As a result of this and additional studies, repeated minor "bumps" are now viewed through a different lens—even the mild ones can take their toll, impeding language processing or motor skills. |
The May 2012 suicide of Junior Seau, a former professional football player who sustained repeated blows to the head during his career, was a further wake-up call. It has become increasingly clear that the blows to the head sustained by players in a variety of sports and recreational activities require more serious attention—and we need to address it earlier in an athlete's career (amateur or professional), not once the irreparable damage is done. |
The first law to address concussion management in youth athletics was passed in Washington State in May 2009. By 2012, 42 additional states and the District of Columbia had passed similar laws.4 The intent of these "Return to Play" laws is to reduce the impact of youth sports and recreation–related concussions, and their tenets can extend to our college and professional athletes. |
The long-term effects of repeated blows to the head have only begun to surface. We need to be diligent in recognizing and preventing TBI in all athletes, because doing so can prevent further brain injury or even death. Arm yourself with information; the CDC Web site is an excellent resource (www.cdc.gov/concussion/sports/index.html). |
Finally, a message to all coaches and parents, athletes, and health care professionals: Getting your "bell rung" in a sports event should not be taken lightly. It must be recognized as the serious and potentially dangerous occurrence it is. So, don't put him in, coach—he may not be ready to play! |
Share your thoughts and experiences with me at NPEditor@frontlinemedcom.com.
|
How Safe?
During the weeks before writing this column, I had conversations with people from different professions, all seeming to ask the same question: Are hospital administrations and health care providers creating a “safety culture”? Safety culture—sure, we have implemented approaches to make our system safer. We emphasized “no-blame” reporting, among other things. But to my astonishment, my response was incorrect. No, I was told—that was not what they meant. What they wanted to know was whether the people were embracing the culture. That question was the impetus for the topic this month.
Since the publication of the seminal 1999 work To Err is Human by the Institute of Medicine,1 health care professionals, the industry, and consumers have striven to reduce and prevent medical errors. Systems have been developed and introduced to mitigate the potential for accidental injury or death in hospitals and other health care facilities. In some instances, insurers—both private and public—have begun to impose fines or have denied payment for services provided that were necessitated by a medical error. Yet despite these improvements, preventable errors persist, and the resulting costs—in quality of life, lives lost, and monetary measures—continue to mount.
Too frequently, we cause harm or fail to deliver the optimal benefits of our health care system. Initially, frustration with our error-vulnerable system was sufficient impetus to get us moving toward changing the status quo and committing ourselves to make our health care system a better, safer industry. More importantly, we strove to organize what was a “non-system,” in our determination to substantially improve the quality of health care in our country. Alas, we continue to struggle with the same (or at least similar) issues with quality that have created the chasm2 between the health care system we have now and one we know we could have.
After more than a decade of learning, listening, and teaching about health care quality, system-wide improvements, and the implementation of various tools to close that chasm, I wonder whether we are missing what might be the real bridge across the abyss. Have we made that quantum leap from fixing the blame to fixing the system? Have we become educated about an actual culture of safety in addition to educating ourselves on the mechanics of safety initiatives? We have changed the system to some degree, but have we truly changed the culture?
“Safety culture”—what did my colleagues mean? Off to the Internet I went, exploring the difference between what I thought I was promoting and what I was missing. Seems I had some gaps in my knowledge. And of course, in my own backyard were some of the innovators of what is known as the “Just Culture”3 or the “Fair and Just Culture.”4 Simply put, this means “giving constructive feedback and critical analysis in skillful ways, doing assessments that are based on facts, and having respect for the complexity of the situation.”4 It also means creating effective organizations that allow and encourage people to divulge their errors, and helps each organization’s team to learn from those errors.
In many instances, we continue to condemn and take disciplinary action against those who make an honest mistake, admit to it, and ask for help or provide insight in order to prevent similar occurrences in the future. By responding in this way to our colleagues who err, we run the risk of remaining unaware of the extent of errors and injuries and their consequences. There, I think, is where we miss an important opportunity to progress in moving our health care system forward.
We need to take steps toward securing free and uninhibited reporting.3 In this scenario, everyone functioning in our institution has the responsibility to identify, and the opportunity to remedy, any situation that might result in error or injury, or that has already had such a result. We know that error analysis—even of errors that do not cause injury—gives us the opportunity to identify system improvements that can prevent adverse events. But until and unless we become open and support the practice of admitting to an error—or reporting a situation in which an error occurred or could have occurred—the opportunity to mitigate the flaws that contributed to the event is lost. And that is the true tragedy: that we fail to learn from untoward events or errors. We are thus doomed to repeat them, both in our own facilities and across the entire health care system.
It is imperative for all disciplines to know that disclosing an unsafe situation or error is an opportunity to educate others about the risk and use pertinent information to improve the working and care environment. We need to change the focus in our system-wide culture from one that blames the individual provider to one that seeks to learn from the error. And we need to be honest with ourselves: In many situations, we have only given lip service to the concept that divulging errors should not result in punitive actions. This does not mean that we are relieved of accountability for the care we provide; rather, we remain obligated to act responsibly and function within our qualifications. In addition to the actions we take, we are also accountable to discuss errors of commission or omission, and to identify process improvements and/or systems corrections.4
Just as we have seen in the airline industry, it is time to change our culture of fear and defensiveness to a true “safety culture,” with a structure in which people can openly divulge their errors or report potential hazards, allowing the organization to learn from them. Until we fully embrace that approach, I fear it will take another decade before we can have a safe health care system.
REFERENCES
1. Kohn LT, Corrigan JM, Donaldson MS, eds; Committee on Quality of Health Care in America, Institute of Medicine, National Academy of Sciences. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000.
2. Committee on Quality Health Care in America, Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century (2001). www.iom.edu/~/media/Files/Report%20Files/2001/Crossing-the-Quality-Chasm/Quality%20Chasm%202001%20%20report%20brief.pdf. Accessed November 21, 2012.
3. Marx D. Patient Safety and the “Just Culture”: A Primer for Health Care Executives. New York, NY: Columbia University; 2001.
4. Dana-Farber Cancer Institute Principles of a Fair and Just Culture. www.macoalition.org/Initiatives/docs/Dana-Farber_PrinciplesJustCulture.pdf. Accessed November 21, 2012.
During the weeks before writing this column, I had conversations with people from different professions, all seeming to ask the same question: Are hospital administrations and health care providers creating a “safety culture”? Safety culture—sure, we have implemented approaches to make our system safer. We emphasized “no-blame” reporting, among other things. But to my astonishment, my response was incorrect. No, I was told—that was not what they meant. What they wanted to know was whether the people were embracing the culture. That question was the impetus for the topic this month.
Since the publication of the seminal 1999 work To Err is Human by the Institute of Medicine,1 health care professionals, the industry, and consumers have striven to reduce and prevent medical errors. Systems have been developed and introduced to mitigate the potential for accidental injury or death in hospitals and other health care facilities. In some instances, insurers—both private and public—have begun to impose fines or have denied payment for services provided that were necessitated by a medical error. Yet despite these improvements, preventable errors persist, and the resulting costs—in quality of life, lives lost, and monetary measures—continue to mount.
Too frequently, we cause harm or fail to deliver the optimal benefits of our health care system. Initially, frustration with our error-vulnerable system was sufficient impetus to get us moving toward changing the status quo and committing ourselves to make our health care system a better, safer industry. More importantly, we strove to organize what was a “non-system,” in our determination to substantially improve the quality of health care in our country. Alas, we continue to struggle with the same (or at least similar) issues with quality that have created the chasm2 between the health care system we have now and one we know we could have.
After more than a decade of learning, listening, and teaching about health care quality, system-wide improvements, and the implementation of various tools to close that chasm, I wonder whether we are missing what might be the real bridge across the abyss. Have we made that quantum leap from fixing the blame to fixing the system? Have we become educated about an actual culture of safety in addition to educating ourselves on the mechanics of safety initiatives? We have changed the system to some degree, but have we truly changed the culture?
“Safety culture”—what did my colleagues mean? Off to the Internet I went, exploring the difference between what I thought I was promoting and what I was missing. Seems I had some gaps in my knowledge. And of course, in my own backyard were some of the innovators of what is known as the “Just Culture”3 or the “Fair and Just Culture.”4 Simply put, this means “giving constructive feedback and critical analysis in skillful ways, doing assessments that are based on facts, and having respect for the complexity of the situation.”4 It also means creating effective organizations that allow and encourage people to divulge their errors, and helps each organization’s team to learn from those errors.
In many instances, we continue to condemn and take disciplinary action against those who make an honest mistake, admit to it, and ask for help or provide insight in order to prevent similar occurrences in the future. By responding in this way to our colleagues who err, we run the risk of remaining unaware of the extent of errors and injuries and their consequences. There, I think, is where we miss an important opportunity to progress in moving our health care system forward.
We need to take steps toward securing free and uninhibited reporting.3 In this scenario, everyone functioning in our institution has the responsibility to identify, and the opportunity to remedy, any situation that might result in error or injury, or that has already had such a result. We know that error analysis—even of errors that do not cause injury—gives us the opportunity to identify system improvements that can prevent adverse events. But until and unless we become open and support the practice of admitting to an error—or reporting a situation in which an error occurred or could have occurred—the opportunity to mitigate the flaws that contributed to the event is lost. And that is the true tragedy: that we fail to learn from untoward events or errors. We are thus doomed to repeat them, both in our own facilities and across the entire health care system.
It is imperative for all disciplines to know that disclosing an unsafe situation or error is an opportunity to educate others about the risk and use pertinent information to improve the working and care environment. We need to change the focus in our system-wide culture from one that blames the individual provider to one that seeks to learn from the error. And we need to be honest with ourselves: In many situations, we have only given lip service to the concept that divulging errors should not result in punitive actions. This does not mean that we are relieved of accountability for the care we provide; rather, we remain obligated to act responsibly and function within our qualifications. In addition to the actions we take, we are also accountable to discuss errors of commission or omission, and to identify process improvements and/or systems corrections.4
Just as we have seen in the airline industry, it is time to change our culture of fear and defensiveness to a true “safety culture,” with a structure in which people can openly divulge their errors or report potential hazards, allowing the organization to learn from them. Until we fully embrace that approach, I fear it will take another decade before we can have a safe health care system.
REFERENCES
1. Kohn LT, Corrigan JM, Donaldson MS, eds; Committee on Quality of Health Care in America, Institute of Medicine, National Academy of Sciences. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000.
2. Committee on Quality Health Care in America, Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century (2001). www.iom.edu/~/media/Files/Report%20Files/2001/Crossing-the-Quality-Chasm/Quality%20Chasm%202001%20%20report%20brief.pdf. Accessed November 21, 2012.
3. Marx D. Patient Safety and the “Just Culture”: A Primer for Health Care Executives. New York, NY: Columbia University; 2001.
4. Dana-Farber Cancer Institute Principles of a Fair and Just Culture. www.macoalition.org/Initiatives/docs/Dana-Farber_PrinciplesJustCulture.pdf. Accessed November 21, 2012.
During the weeks before writing this column, I had conversations with people from different professions, all seeming to ask the same question: Are hospital administrations and health care providers creating a “safety culture”? Safety culture—sure, we have implemented approaches to make our system safer. We emphasized “no-blame” reporting, among other things. But to my astonishment, my response was incorrect. No, I was told—that was not what they meant. What they wanted to know was whether the people were embracing the culture. That question was the impetus for the topic this month.
Since the publication of the seminal 1999 work To Err is Human by the Institute of Medicine,1 health care professionals, the industry, and consumers have striven to reduce and prevent medical errors. Systems have been developed and introduced to mitigate the potential for accidental injury or death in hospitals and other health care facilities. In some instances, insurers—both private and public—have begun to impose fines or have denied payment for services provided that were necessitated by a medical error. Yet despite these improvements, preventable errors persist, and the resulting costs—in quality of life, lives lost, and monetary measures—continue to mount.
Too frequently, we cause harm or fail to deliver the optimal benefits of our health care system. Initially, frustration with our error-vulnerable system was sufficient impetus to get us moving toward changing the status quo and committing ourselves to make our health care system a better, safer industry. More importantly, we strove to organize what was a “non-system,” in our determination to substantially improve the quality of health care in our country. Alas, we continue to struggle with the same (or at least similar) issues with quality that have created the chasm2 between the health care system we have now and one we know we could have.
After more than a decade of learning, listening, and teaching about health care quality, system-wide improvements, and the implementation of various tools to close that chasm, I wonder whether we are missing what might be the real bridge across the abyss. Have we made that quantum leap from fixing the blame to fixing the system? Have we become educated about an actual culture of safety in addition to educating ourselves on the mechanics of safety initiatives? We have changed the system to some degree, but have we truly changed the culture?
“Safety culture”—what did my colleagues mean? Off to the Internet I went, exploring the difference between what I thought I was promoting and what I was missing. Seems I had some gaps in my knowledge. And of course, in my own backyard were some of the innovators of what is known as the “Just Culture”3 or the “Fair and Just Culture.”4 Simply put, this means “giving constructive feedback and critical analysis in skillful ways, doing assessments that are based on facts, and having respect for the complexity of the situation.”4 It also means creating effective organizations that allow and encourage people to divulge their errors, and helps each organization’s team to learn from those errors.
In many instances, we continue to condemn and take disciplinary action against those who make an honest mistake, admit to it, and ask for help or provide insight in order to prevent similar occurrences in the future. By responding in this way to our colleagues who err, we run the risk of remaining unaware of the extent of errors and injuries and their consequences. There, I think, is where we miss an important opportunity to progress in moving our health care system forward.
We need to take steps toward securing free and uninhibited reporting.3 In this scenario, everyone functioning in our institution has the responsibility to identify, and the opportunity to remedy, any situation that might result in error or injury, or that has already had such a result. We know that error analysis—even of errors that do not cause injury—gives us the opportunity to identify system improvements that can prevent adverse events. But until and unless we become open and support the practice of admitting to an error—or reporting a situation in which an error occurred or could have occurred—the opportunity to mitigate the flaws that contributed to the event is lost. And that is the true tragedy: that we fail to learn from untoward events or errors. We are thus doomed to repeat them, both in our own facilities and across the entire health care system.
It is imperative for all disciplines to know that disclosing an unsafe situation or error is an opportunity to educate others about the risk and use pertinent information to improve the working and care environment. We need to change the focus in our system-wide culture from one that blames the individual provider to one that seeks to learn from the error. And we need to be honest with ourselves: In many situations, we have only given lip service to the concept that divulging errors should not result in punitive actions. This does not mean that we are relieved of accountability for the care we provide; rather, we remain obligated to act responsibly and function within our qualifications. In addition to the actions we take, we are also accountable to discuss errors of commission or omission, and to identify process improvements and/or systems corrections.4
Just as we have seen in the airline industry, it is time to change our culture of fear and defensiveness to a true “safety culture,” with a structure in which people can openly divulge their errors or report potential hazards, allowing the organization to learn from them. Until we fully embrace that approach, I fear it will take another decade before we can have a safe health care system.
REFERENCES
1. Kohn LT, Corrigan JM, Donaldson MS, eds; Committee on Quality of Health Care in America, Institute of Medicine, National Academy of Sciences. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000.
2. Committee on Quality Health Care in America, Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century (2001). www.iom.edu/~/media/Files/Report%20Files/2001/Crossing-the-Quality-Chasm/Quality%20Chasm%202001%20%20report%20brief.pdf. Accessed November 21, 2012.
3. Marx D. Patient Safety and the “Just Culture”: A Primer for Health Care Executives. New York, NY: Columbia University; 2001.
4. Dana-Farber Cancer Institute Principles of a Fair and Just Culture. www.macoalition.org/Initiatives/docs/Dana-Farber_PrinciplesJustCulture.pdf. Accessed November 21, 2012.