User login
Passing the ‘baton’ with pride
I was honored to be the third Editor-in-Chief of GIHN, from 2016 through 2021. GIHN is the official newspaper of the American Gastroenterological Association and has the widest readership of any AGA publication and is one that readers told us they read cover to cover. As such, each EIC and their Board of Editors must ensure balanced content that holds the interest of a diverse readership. I was privileged to work with a talented editorial board who reviewed articles, attended leadership meetings, and offered terrific suggestions throughout our tenure. I treasured their support and friendship.
Within each of the 60 monthly issues, we sought to highlight science, practice operations, national trends, and opinions and reviews that would be most important to basic scientists, clinical researchers, and academic and community clinicians, primarily from the United States but also from a worldwide readership. I was given a 300-word section to create editorial comments on pertinent topics that were important to gastroenterologists. Having a background in both community and academic practice, I tried to bring a balanced perspective to areas that often seem worlds apart.
The period between 2016 and 2021 also was a time of political upheaval in this country – something we could not ignore. I attempted to write about current events in a balanced way that kept a focus on patients and AGA’s core constituency. Not always an easy task. Sustainability of the Affordable Care Act was very much in question because of judicial and legislative challenges; had the ACA been overturned, our practices would be very different now.
In 2016, the first private equity–backed practice platform was created in south Florida. Little did we know how much that model would change community practice. Then, on Jan. 21, 2020, the first case of COVID 19 was diagnosed in Seattle (although earlier cases likely occurred). By March, many clinics and practices were closing, and we were altering our care delivery infrastructure in ways that would forever change practice. Trying to keep current with ever-changing science and policies was a challenge.
I will always treasure my time as EIC. I was happy (and proud) to pass this baton to Megan A. Adams MD, JD, MSc, my colleague and mentee at the University of Michigan. The partnership between AGA and Frontline Medical Communications has been successful for 15 years and will continue to be so.
Dr. Allen, now retired, was professor of medicine at the University of Michigan, Ann Arbor. He is secretary/treasurer for the American Gastroenterological Association, and declares no relevant conflicts of interest.
I was honored to be the third Editor-in-Chief of GIHN, from 2016 through 2021. GIHN is the official newspaper of the American Gastroenterological Association and has the widest readership of any AGA publication and is one that readers told us they read cover to cover. As such, each EIC and their Board of Editors must ensure balanced content that holds the interest of a diverse readership. I was privileged to work with a talented editorial board who reviewed articles, attended leadership meetings, and offered terrific suggestions throughout our tenure. I treasured their support and friendship.
Within each of the 60 monthly issues, we sought to highlight science, practice operations, national trends, and opinions and reviews that would be most important to basic scientists, clinical researchers, and academic and community clinicians, primarily from the United States but also from a worldwide readership. I was given a 300-word section to create editorial comments on pertinent topics that were important to gastroenterologists. Having a background in both community and academic practice, I tried to bring a balanced perspective to areas that often seem worlds apart.
The period between 2016 and 2021 also was a time of political upheaval in this country – something we could not ignore. I attempted to write about current events in a balanced way that kept a focus on patients and AGA’s core constituency. Not always an easy task. Sustainability of the Affordable Care Act was very much in question because of judicial and legislative challenges; had the ACA been overturned, our practices would be very different now.
In 2016, the first private equity–backed practice platform was created in south Florida. Little did we know how much that model would change community practice. Then, on Jan. 21, 2020, the first case of COVID 19 was diagnosed in Seattle (although earlier cases likely occurred). By March, many clinics and practices were closing, and we were altering our care delivery infrastructure in ways that would forever change practice. Trying to keep current with ever-changing science and policies was a challenge.
I will always treasure my time as EIC. I was happy (and proud) to pass this baton to Megan A. Adams MD, JD, MSc, my colleague and mentee at the University of Michigan. The partnership between AGA and Frontline Medical Communications has been successful for 15 years and will continue to be so.
Dr. Allen, now retired, was professor of medicine at the University of Michigan, Ann Arbor. He is secretary/treasurer for the American Gastroenterological Association, and declares no relevant conflicts of interest.
I was honored to be the third Editor-in-Chief of GIHN, from 2016 through 2021. GIHN is the official newspaper of the American Gastroenterological Association and has the widest readership of any AGA publication and is one that readers told us they read cover to cover. As such, each EIC and their Board of Editors must ensure balanced content that holds the interest of a diverse readership. I was privileged to work with a talented editorial board who reviewed articles, attended leadership meetings, and offered terrific suggestions throughout our tenure. I treasured their support and friendship.
Within each of the 60 monthly issues, we sought to highlight science, practice operations, national trends, and opinions and reviews that would be most important to basic scientists, clinical researchers, and academic and community clinicians, primarily from the United States but also from a worldwide readership. I was given a 300-word section to create editorial comments on pertinent topics that were important to gastroenterologists. Having a background in both community and academic practice, I tried to bring a balanced perspective to areas that often seem worlds apart.
The period between 2016 and 2021 also was a time of political upheaval in this country – something we could not ignore. I attempted to write about current events in a balanced way that kept a focus on patients and AGA’s core constituency. Not always an easy task. Sustainability of the Affordable Care Act was very much in question because of judicial and legislative challenges; had the ACA been overturned, our practices would be very different now.
In 2016, the first private equity–backed practice platform was created in south Florida. Little did we know how much that model would change community practice. Then, on Jan. 21, 2020, the first case of COVID 19 was diagnosed in Seattle (although earlier cases likely occurred). By March, many clinics and practices were closing, and we were altering our care delivery infrastructure in ways that would forever change practice. Trying to keep current with ever-changing science and policies was a challenge.
I will always treasure my time as EIC. I was happy (and proud) to pass this baton to Megan A. Adams MD, JD, MSc, my colleague and mentee at the University of Michigan. The partnership between AGA and Frontline Medical Communications has been successful for 15 years and will continue to be so.
Dr. Allen, now retired, was professor of medicine at the University of Michigan, Ann Arbor. He is secretary/treasurer for the American Gastroenterological Association, and declares no relevant conflicts of interest.
What to keep in mind as 2021 begins
As 2020 comes to a close, most of us are looking forward to a (hopefully) brighter 2021. This year has been full of challenges and new experiences, but we have learned a lot. Pandemic or not, there are some things that you and your practice can do to ensure that you are prepared to make 2021 a success.
Tips for your practice
Assess staff morale: It seems simple but checking in with your staff can go a long way. Everyone is dealing with challenges both in and out of the workplace. Check in, show them you care, and think of ways that you can make their work a positive experience in the new year. During our May 2020 GI division chief townhall, John Inadomi, MD, gave a great presentation on the importance of staff morale during the pandemic.
Listen to colleagues: Find out about their experiences, challenges, and solutions. In October, the American Gastroenterological Association held a town hall with some great information and resources called “Adapting to Changing Practice Paradigms.” The agenda covered topics from telehealth to private equity and planning for the next potential wave of COVID-19.
Celebrate the wins: It can often feel like not much went right in 2020, but we did accomplish significant wins for GIs, including achieving payment parity for telephone evaluation and management (E/M) visits with video visits, increases in digestive disease and GI cancer research funding, and inclusion/expansion of GI cancers research opportunities. We couldn’t have done it without you, though, and we will continue to need your help to move important issues forward in 2021. Get involved today! Visit “Get Involved” under Advocacy and Policy on www.gastro.org.
Prepare for E/M changes: The Current Procedural Terminology (CPT) E/M for new and established patient office/outpatient codes (99201-99205, 99211-99215), guidelines, and Medicare payments will undergo major changes beginning Jan. 1, 2021. See the AGA’s coding and reimbursement experts’ article from the March 2020 issue of GI & Hepatology News, “Prepare for major changes to E/M coding starting in 2021,” to learn about the changes and get resources to help practices prepare.
Keep up with new Medicare payment rules: The release of the 2021 physician payments and rules for the Medicare program was delayed this year because of the COVID-19 public health emergency. We were dismayed to learn that Medicare did not make any changes that substantively mitigated the expected cuts to most specialties. Instead of a 5% cut for GI, the Centers for Medicare & Medicaid Services now projects GI will experience a 4% payment cut for 2021. AGA is calling on Congress to pass legislation to stop the cuts. This situation is evolving quickly. Watch for AGA member alerts for breaking news and resources, including the AGA’s “Medicare plans significant payment cuts for 2021.”
Stay current on telehealth and telephone E/M coverage: The commercial payer community came together to cover telehealth (video visits) and telephone E/M at the beginning of the COVID-19 pandemic but have since regularly teased the end of coverage only to extend it just before it expires. It’s impossible to predict what each payer will do, but you can use the following resources to keep current on most payers’ policies and correct coding/reporting for telehealth and telephone E/M:
- “Current State Laws & Reimbursement Policies ” from the Center for Connected Health.
- “Coding for Telehealth & Virtual Visits During COVID-19” from the AGA University.
Check to see if you can report on additional quality measures: AGA has expanded the Merit-Based Incentive Payment System (MIPS) measure portfolio by assuming ownership and stewardship of two hepatitis C virus (HCV) measures from PCPI, including annually checking for HCV in active injection drug users (measure 387) and performing a one-time screening for HCV among patients at risk (measure 400). As a result, gastroenterologists can now report on even more GI-specific measures. There have been the following two changes to GI-specific measures in 2021:
- Measure 275: “Inflammatory Bowel Disease (IBD): Assessment of Hepatitis B Virus (HBV) Status Before Initiating Anti-TNF (Tumor Necrosis Factor) Therapy” now includes coding to allow reporting for all age groups, including pediatric populations.
- Measure 439: “Age Appropriate Screening Colonoscopy” now includes all colonoscopies for patients 50 years and older; however, there’s an exclusion for those patients between the ages of 50 and 85 years.
These changes will help more gastroenterologists qualify for these measures.
Dates and deadlines to remember
January 2021
- Jan. 1 – MIPS Performance Year 2021 begins.
- Jan. 4 – Submission window opens for MIPS Performance Year 2020.
- Changes to Improvement Activity category go into effect (if approved in final rule).
March 2021
- March 31 – First snapshot for Qualifying Participant (QP) determinations and MIPS APM participation.
April 2021
- April 1 – Registration begins for CMS web interface and Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS survey.
June 2021
- June 30 – Second snapshot for QP determinations and MIPS APM participation.
- June 30 – Registration ends for CMS web interface and CAHPS for MIPS survey.
July 2021
- CMS publishes proposed reimbursement values for 2022 in the Medicare Physician Fee Schedule proposed rule.
- CMS “Targeted Review” opens once CMS makes your MIPS payment adjustment available.
- July 1 - MIPS Performance Feedback Available. CMS will provide you with performance feedback based on the data you submitted for Performance Year 2020. You can use this feedback to improve your care and optimize the payments you receive from CMS in the future.
August 2021
- Aug. 31 - Targeted Review period closes (appeals process).
September 2021
- AMA releases CPT 2022 book, including a new CPT code for Peroral Endoscopic Myotomy (POEM).
October 2021
- Oct. 3 - Last day to start a 90-day performance period for promoting Interoperability and Improvement Activities.
November 2021
- CMS finalizes reimbursement values for 2022 in the MPFS final rule. New payment rates take effect Jan. 1, 2022.
December 2021
- Dec. 31 – Quality Payment Program Exception Applications window closes.
- Dec. 31 – MIPS Performance year 2020 ends.
- Dec. 31 – Fourth snapshot for full TIN APMs (Medicare Shared Savings Program).
G. Anton Decker, MD, is chair of the AGA Practice Management and Economics Committee, Mayo Clinic International; Dawn Francis, MD, is chair-elect of the AGA Practice Management and Economics Committee, Mayo Clinic, Jacksonville, Fla.
They have no conflicts of interest.
As 2020 comes to a close, most of us are looking forward to a (hopefully) brighter 2021. This year has been full of challenges and new experiences, but we have learned a lot. Pandemic or not, there are some things that you and your practice can do to ensure that you are prepared to make 2021 a success.
Tips for your practice
Assess staff morale: It seems simple but checking in with your staff can go a long way. Everyone is dealing with challenges both in and out of the workplace. Check in, show them you care, and think of ways that you can make their work a positive experience in the new year. During our May 2020 GI division chief townhall, John Inadomi, MD, gave a great presentation on the importance of staff morale during the pandemic.
Listen to colleagues: Find out about their experiences, challenges, and solutions. In October, the American Gastroenterological Association held a town hall with some great information and resources called “Adapting to Changing Practice Paradigms.” The agenda covered topics from telehealth to private equity and planning for the next potential wave of COVID-19.
Celebrate the wins: It can often feel like not much went right in 2020, but we did accomplish significant wins for GIs, including achieving payment parity for telephone evaluation and management (E/M) visits with video visits, increases in digestive disease and GI cancer research funding, and inclusion/expansion of GI cancers research opportunities. We couldn’t have done it without you, though, and we will continue to need your help to move important issues forward in 2021. Get involved today! Visit “Get Involved” under Advocacy and Policy on www.gastro.org.
Prepare for E/M changes: The Current Procedural Terminology (CPT) E/M for new and established patient office/outpatient codes (99201-99205, 99211-99215), guidelines, and Medicare payments will undergo major changes beginning Jan. 1, 2021. See the AGA’s coding and reimbursement experts’ article from the March 2020 issue of GI & Hepatology News, “Prepare for major changes to E/M coding starting in 2021,” to learn about the changes and get resources to help practices prepare.
Keep up with new Medicare payment rules: The release of the 2021 physician payments and rules for the Medicare program was delayed this year because of the COVID-19 public health emergency. We were dismayed to learn that Medicare did not make any changes that substantively mitigated the expected cuts to most specialties. Instead of a 5% cut for GI, the Centers for Medicare & Medicaid Services now projects GI will experience a 4% payment cut for 2021. AGA is calling on Congress to pass legislation to stop the cuts. This situation is evolving quickly. Watch for AGA member alerts for breaking news and resources, including the AGA’s “Medicare plans significant payment cuts for 2021.”
Stay current on telehealth and telephone E/M coverage: The commercial payer community came together to cover telehealth (video visits) and telephone E/M at the beginning of the COVID-19 pandemic but have since regularly teased the end of coverage only to extend it just before it expires. It’s impossible to predict what each payer will do, but you can use the following resources to keep current on most payers’ policies and correct coding/reporting for telehealth and telephone E/M:
- “Current State Laws & Reimbursement Policies ” from the Center for Connected Health.
- “Coding for Telehealth & Virtual Visits During COVID-19” from the AGA University.
Check to see if you can report on additional quality measures: AGA has expanded the Merit-Based Incentive Payment System (MIPS) measure portfolio by assuming ownership and stewardship of two hepatitis C virus (HCV) measures from PCPI, including annually checking for HCV in active injection drug users (measure 387) and performing a one-time screening for HCV among patients at risk (measure 400). As a result, gastroenterologists can now report on even more GI-specific measures. There have been the following two changes to GI-specific measures in 2021:
- Measure 275: “Inflammatory Bowel Disease (IBD): Assessment of Hepatitis B Virus (HBV) Status Before Initiating Anti-TNF (Tumor Necrosis Factor) Therapy” now includes coding to allow reporting for all age groups, including pediatric populations.
- Measure 439: “Age Appropriate Screening Colonoscopy” now includes all colonoscopies for patients 50 years and older; however, there’s an exclusion for those patients between the ages of 50 and 85 years.
These changes will help more gastroenterologists qualify for these measures.
Dates and deadlines to remember
January 2021
- Jan. 1 – MIPS Performance Year 2021 begins.
- Jan. 4 – Submission window opens for MIPS Performance Year 2020.
- Changes to Improvement Activity category go into effect (if approved in final rule).
March 2021
- March 31 – First snapshot for Qualifying Participant (QP) determinations and MIPS APM participation.
April 2021
- April 1 – Registration begins for CMS web interface and Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS survey.
June 2021
- June 30 – Second snapshot for QP determinations and MIPS APM participation.
- June 30 – Registration ends for CMS web interface and CAHPS for MIPS survey.
July 2021
- CMS publishes proposed reimbursement values for 2022 in the Medicare Physician Fee Schedule proposed rule.
- CMS “Targeted Review” opens once CMS makes your MIPS payment adjustment available.
- July 1 - MIPS Performance Feedback Available. CMS will provide you with performance feedback based on the data you submitted for Performance Year 2020. You can use this feedback to improve your care and optimize the payments you receive from CMS in the future.
August 2021
- Aug. 31 - Targeted Review period closes (appeals process).
September 2021
- AMA releases CPT 2022 book, including a new CPT code for Peroral Endoscopic Myotomy (POEM).
October 2021
- Oct. 3 - Last day to start a 90-day performance period for promoting Interoperability and Improvement Activities.
November 2021
- CMS finalizes reimbursement values for 2022 in the MPFS final rule. New payment rates take effect Jan. 1, 2022.
December 2021
- Dec. 31 – Quality Payment Program Exception Applications window closes.
- Dec. 31 – MIPS Performance year 2020 ends.
- Dec. 31 – Fourth snapshot for full TIN APMs (Medicare Shared Savings Program).
G. Anton Decker, MD, is chair of the AGA Practice Management and Economics Committee, Mayo Clinic International; Dawn Francis, MD, is chair-elect of the AGA Practice Management and Economics Committee, Mayo Clinic, Jacksonville, Fla.
They have no conflicts of interest.
As 2020 comes to a close, most of us are looking forward to a (hopefully) brighter 2021. This year has been full of challenges and new experiences, but we have learned a lot. Pandemic or not, there are some things that you and your practice can do to ensure that you are prepared to make 2021 a success.
Tips for your practice
Assess staff morale: It seems simple but checking in with your staff can go a long way. Everyone is dealing with challenges both in and out of the workplace. Check in, show them you care, and think of ways that you can make their work a positive experience in the new year. During our May 2020 GI division chief townhall, John Inadomi, MD, gave a great presentation on the importance of staff morale during the pandemic.
Listen to colleagues: Find out about their experiences, challenges, and solutions. In October, the American Gastroenterological Association held a town hall with some great information and resources called “Adapting to Changing Practice Paradigms.” The agenda covered topics from telehealth to private equity and planning for the next potential wave of COVID-19.
Celebrate the wins: It can often feel like not much went right in 2020, but we did accomplish significant wins for GIs, including achieving payment parity for telephone evaluation and management (E/M) visits with video visits, increases in digestive disease and GI cancer research funding, and inclusion/expansion of GI cancers research opportunities. We couldn’t have done it without you, though, and we will continue to need your help to move important issues forward in 2021. Get involved today! Visit “Get Involved” under Advocacy and Policy on www.gastro.org.
Prepare for E/M changes: The Current Procedural Terminology (CPT) E/M for new and established patient office/outpatient codes (99201-99205, 99211-99215), guidelines, and Medicare payments will undergo major changes beginning Jan. 1, 2021. See the AGA’s coding and reimbursement experts’ article from the March 2020 issue of GI & Hepatology News, “Prepare for major changes to E/M coding starting in 2021,” to learn about the changes and get resources to help practices prepare.
Keep up with new Medicare payment rules: The release of the 2021 physician payments and rules for the Medicare program was delayed this year because of the COVID-19 public health emergency. We were dismayed to learn that Medicare did not make any changes that substantively mitigated the expected cuts to most specialties. Instead of a 5% cut for GI, the Centers for Medicare & Medicaid Services now projects GI will experience a 4% payment cut for 2021. AGA is calling on Congress to pass legislation to stop the cuts. This situation is evolving quickly. Watch for AGA member alerts for breaking news and resources, including the AGA’s “Medicare plans significant payment cuts for 2021.”
Stay current on telehealth and telephone E/M coverage: The commercial payer community came together to cover telehealth (video visits) and telephone E/M at the beginning of the COVID-19 pandemic but have since regularly teased the end of coverage only to extend it just before it expires. It’s impossible to predict what each payer will do, but you can use the following resources to keep current on most payers’ policies and correct coding/reporting for telehealth and telephone E/M:
- “Current State Laws & Reimbursement Policies ” from the Center for Connected Health.
- “Coding for Telehealth & Virtual Visits During COVID-19” from the AGA University.
Check to see if you can report on additional quality measures: AGA has expanded the Merit-Based Incentive Payment System (MIPS) measure portfolio by assuming ownership and stewardship of two hepatitis C virus (HCV) measures from PCPI, including annually checking for HCV in active injection drug users (measure 387) and performing a one-time screening for HCV among patients at risk (measure 400). As a result, gastroenterologists can now report on even more GI-specific measures. There have been the following two changes to GI-specific measures in 2021:
- Measure 275: “Inflammatory Bowel Disease (IBD): Assessment of Hepatitis B Virus (HBV) Status Before Initiating Anti-TNF (Tumor Necrosis Factor) Therapy” now includes coding to allow reporting for all age groups, including pediatric populations.
- Measure 439: “Age Appropriate Screening Colonoscopy” now includes all colonoscopies for patients 50 years and older; however, there’s an exclusion for those patients between the ages of 50 and 85 years.
These changes will help more gastroenterologists qualify for these measures.
Dates and deadlines to remember
January 2021
- Jan. 1 – MIPS Performance Year 2021 begins.
- Jan. 4 – Submission window opens for MIPS Performance Year 2020.
- Changes to Improvement Activity category go into effect (if approved in final rule).
March 2021
- March 31 – First snapshot for Qualifying Participant (QP) determinations and MIPS APM participation.
April 2021
- April 1 – Registration begins for CMS web interface and Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS survey.
June 2021
- June 30 – Second snapshot for QP determinations and MIPS APM participation.
- June 30 – Registration ends for CMS web interface and CAHPS for MIPS survey.
July 2021
- CMS publishes proposed reimbursement values for 2022 in the Medicare Physician Fee Schedule proposed rule.
- CMS “Targeted Review” opens once CMS makes your MIPS payment adjustment available.
- July 1 - MIPS Performance Feedback Available. CMS will provide you with performance feedback based on the data you submitted for Performance Year 2020. You can use this feedback to improve your care and optimize the payments you receive from CMS in the future.
August 2021
- Aug. 31 - Targeted Review period closes (appeals process).
September 2021
- AMA releases CPT 2022 book, including a new CPT code for Peroral Endoscopic Myotomy (POEM).
October 2021
- Oct. 3 - Last day to start a 90-day performance period for promoting Interoperability and Improvement Activities.
November 2021
- CMS finalizes reimbursement values for 2022 in the MPFS final rule. New payment rates take effect Jan. 1, 2022.
December 2021
- Dec. 31 – Quality Payment Program Exception Applications window closes.
- Dec. 31 – MIPS Performance year 2020 ends.
- Dec. 31 – Fourth snapshot for full TIN APMs (Medicare Shared Savings Program).
G. Anton Decker, MD, is chair of the AGA Practice Management and Economics Committee, Mayo Clinic International; Dawn Francis, MD, is chair-elect of the AGA Practice Management and Economics Committee, Mayo Clinic, Jacksonville, Fla.
They have no conflicts of interest.
New models of gastroenterology practice
The variety of employment models available to gastroenterologists reflects the dynamic changes we are experiencing in medicine today. Delivery of gastrointestinal (GI) care in the United States continues to evolve in light of health care reform and the Affordable Care Act.1 Within the past decade, as health systems and payers continue to consolidate, regulatory pressures have increased steadily and new policies such as electronic documentation and mandatory quality metrics reporting have added new challenges to the emerging generation of gastroenterologists.2 Although the lay press tends to focus on health care costs, coverage, physician reimbursement, provider burnout, health system consolidation, and value-based payment models, relatively less has been published about emerging employment and practice models.
Here,
Background
When the senior author graduated from fellowship in 1983 (J.I.A.), gastroenterology practice model choices were limited to essentially 4: independent community-based, single-specialty, physician-owned practice (solo or small group); independent multispecialty physician-owned practice; hospital or health system–owned multispecialty practice; and academic practice (including the Veterans Administration Medical Centers).
In the private sector, young community gastroenterologists typically would join a physician-owned practice and spend time (2–5 y) as an employed physician in a partnership track. During this time, his/her salary was subsidized while he/she built a practice base. Then, they would buy into the Professional Association with cash or equity equivalents and become a partner. As a partner, he/she then had the opportunity to share in ancillary revenue streams such as facility fees derived from a practice-owned ambulatory endoscopy center (AEC). By contrast, young academic faculty would be hired as an instructor and, if successful, climb the traditional ladder track to assistant, associate, and professor of medicine in an academic medical center (AMC).
In the 1980s, a typical community GI practice comprised 1 to 8 physicians, with most having been formed by 1 or 2 male gastroenterologists in the early 1970s when flexible endoscopy moved into clinical practice. The three practices that eventually would become Minnesota Gastroenterology (where J.I.A. practiced) opened in 1972. In 1996, the three practices merged into a single group of 38 physicians with ownership in three AECs. Advanced practice nurses and physician assistants were not yet part of the equation. Colonoscopy represented 48% of procedure volume, accounts receivable (time between submitting an insurance claim and being paid) averaged 88 days, and physicians averaged 9000 work relative value units (wRVUs) per partner annually. By comparison, median wRVUs for a full-time community GI in 1996 was 10,422 according to the Medical Group Management Association.3 Annual gross revenue (before expenses) per physician was approximately $400,000, and overhead reached 38% and 47% of revenue (there were 2 divisions). Partner incomes were at the 12% level of the Medical Group Management Association for gastroenterologists (personal management notes of J.I.A.). Minnesota Gastroenterology was the largest single-specialty GI practice in 1996 and its consolidation foreshadowed a trend that has accelerated over the ensuing generation.
When one of the authors (N.K.) graduated from the University of California Los Angeles in 2017, the GI employment landscape had evolved considerably. At least five new models of GI practice had emerged: individual incorporation with a Professional Services Agreement (PSA), a clinician track within an AMC, large single-specialty group practice (partnership or employee), private equity-backed multistate practice, and locum tenens (Figure 1).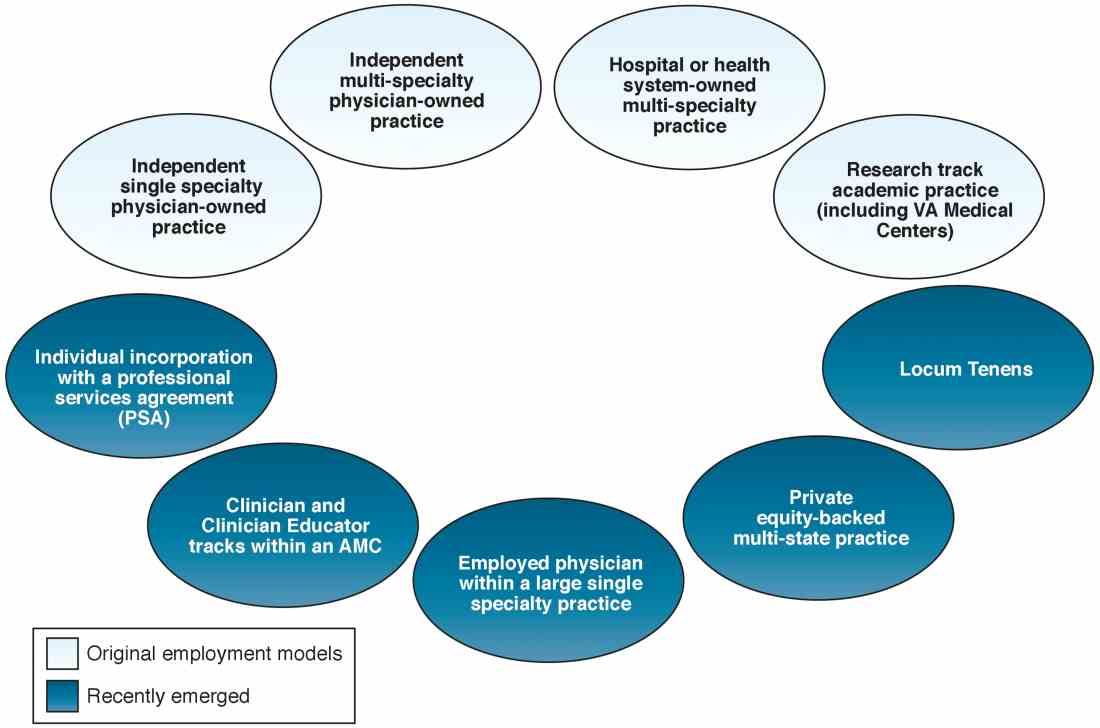
Employment models (light blue) available in the 1980s and those that have emerged as common models in the last decade (dark blue).
An individual corporation with a professional services agreement
For gastroenterologists at any career stage, the prospect of employment within a corporate entity, be it an academic university, hospital system, or private practice group, can be daunting. To that end, one central question facing nearly all gastroenterologists is: how much independence and flexibility, both clinically and financially, do I really want, and what can I do to realize my ideal job description?
An interesting alternative to direct health system employment occurs when a physician forms a solo corporation and then contracts with a hospital or health system under a PSA. Here, the physician provides professional services on a contractual basis, but retains control of finances and has more autonomy compared with employment. Essentially, the physician is a corporation of one, with hospital alignment rather than employment. For full disclosure, this is the employment model of one of the authors (N.K.).
A PSA arrangement is common for larger independent GI practices. Many practices have PSA arrangements with hospitals ranging from call coverage to full professional services. For an individual working within a PSA, income is not the traditional W-2 Internal Revenue Service arrangement in which taxes are removed automatically. Income derived from a PSA usually falls under an Internal Revenue Service Form 1099. The physician actually is employed through their practice corporation and relates to the hospital as an independent contractor.
There are four common variants of the PSA model.4 A Global Payment PSA is when a hospital contracts with the physician practice for specific services and pays a global rate linked to wRVUs. The rate is negotiated to encompass physician compensation, benefits, and practice overhead. The practice retains control of its own office functions and staff.
In a traditional PSA, the hospital contracts with physicians and pays them based on RVU production, but the hospital owns the administrative part of the practice (staff, billing, collections, equipment, and supplies).
A practice management arrangement occurs when the hospital employs the physician who provides professional services and a separate third party manages the practice via a separate management contract. Finally, a Carve-Out PSA can use any of the earlier-described PSA arrangements and certain services are carved out under line-item provisions. For example, a hospital could contract with a private GI group for endoscopic services or night call and write a PSA expressly for these purposes.
Some notable benefits of the PSA are that physicians can maintain financial and employment independence from the hospital and have more control over benefits packages, retirement savings options, and health insurance. Physicians also can provide services outside of the hospital (e.g., telemedicine or locums tenens — see later) without institutional restrictions or conflicts. Finally, physicians benefit from tax advantages of self-employment (with associated business-related tax deductions) through their corporation. The potential downsides of a PSA contract are the subtle expansion of services demanded (known as scope creep) or the possibility of contract termination (or nonrenewal) by the hospital. In addition, medical training does not equip physicians with the knowledge to navigate personal and corporate finances, benefits packages, and tax structures, so the learning curve can be quite steep. Nevertheless, PSAs can be an innovative employment model for gastroenterologists who wish to preserve autonomy and financial flexibility. In this model, legal advice by an attorney skilled in employment law is mandatory.
Academic clinicians track
Until recently, clinically oriented academic faculty were channeled into the traditional ladder faculty model in which advancement was contingent on publications, national recognition, grant support, and teaching. As competition for market share has intensified among regional health systems, many AMCs have developed purely clinical tracks in which research, publication, and teaching are not expected; salaries are linked to clinical productivity; and income may approximate the professional (but not ancillary) income of a community gastroenterologist.
Various models of this arrangement exist as well. For example, clinicians can be employed within a group that has a board and management structure distinct from the faculty group practice, as in the case of the Northeast Medical Group at Yale New Haven Health System5 and the University of Maryland Community Medical Group. In addition, clinicians can form an operating group separate from the faculty practice but as a controlled subsidiary (such as the University of Pittsburgh Community Medicine), separate operating group for primary care but specialists are employed within their respective departments (Emory Specialty Associates) or as a distinct clinical department within a faculty practice (University of California Los Angeles Medical Group Staff Physicians).
Irrespective of the employment model, these clinicians essentially work similar to community gastroenterologists but within the umbrella of an AMC. For young faculty whose interest is not in research or teaching, this can be an attractive option that maintains a tie to a university health system. For a seasoned clinician in community practice, this is an option to return to an academic environment. Usually, productivity expectations within the clinician track approximate those of a community practice gastroenterologist, but again total compensation may not be as great because ancillary income streams usually are not available. We expect this AMC employment track to become more prevalent as universities expand their footprints and acquire practices, hospitals, and ambulatory facilities distant from the main campus.
Large single-specialty practice
Consolidation of independent practices has been evident for 20 years and has accelerated as physicians in smaller practices have aged and burdens of practice have increased. Now, most urban centers have large mega-sized practices or super groups that have grown through practice mergers, acquisitions, and successful recruitment. Large practices can be modeled as a single integrated corporation (with ancillary components such as an AEC or infusion center) or as individual business units that are grouped under a single corporate entity.6
Within these large and mega-sized practices, differing employment options have emerged in addition to the traditional partnership track. These include payment on a per-diem basis, annual salary, or a mix of both. As opposed to partnership, the employment track avoids responsibility for governance and corporate liability, although not individual liability, and usually does not involve after-hours call. An employed physician usually does not benefit from ancillary income that derives from AEC facility fees, infusion centers, and pathology and anesthesia services.
Private equity ownership of gastroenterology practices
In June 2016, private equity entered the GI space with the investment of the Audax Group in a community GI practice based in Miami, Florida. The term private equity refers to capital that is not reported in public forums and comprises funds that investors directly invest into private companies or use to buy out public companies and turn them private.
According to their website, when the Audax Group invests in a medical practice, they provide capital for substantial infrastructure support, business experience, and acumen, but retain medical practice leaders as their clinical decision makers. They also bring proven expertise and economies of scale to resource-intensive aspects of a medical practice including information technology, regulation compliance, human resources, revenue cycle management, payroll, benefits, rents, and lease as examples. These components can be difficult to manage efficiently within independent medical practices, so many maturing practices are selling their practices to regional health systems. This multistate equity-backed medical practice is an alternative to health system acquisition, and may help physicians feel more in control of their practices and potentially share in the equity investment.
It is important to understand the employment structure and associations of any practice you are contemplating joining. The model devised by this group is meant to retain physician authority and responsibility while providing capital to support innovation and the development of needed infrastructure. Growth of market share and revenues can accrue back to physician owners. This is distinct from practices that are part of a health system in which there may be more of a corporate feeling and centralized governance.
Locum tenens
Locum tenens is a Latin phrase that means “to hold the place of.” According to the website of a large locum tenens company, this practice model originated in the 1970s when the federal government provided a grant to the University of Utah to provide physician services for underserved areas in the Western United States. The program proved so successful that hospital administrators who had difficulty recruiting staff physicians began asking for staffing assistance.
Today, a substantial number of physicians at all stages of their careers are working as locum tenens. They work as independent contractors so that income taxes are not withheld and benefits are the responsibility of the individual. As with the PSA arrangement, a physician would meet with both an accountant and labor lawyer to establish him or herself as a corporate entity for tax advantages and limited liability from litigation.
Early stage physicians who might be following a significant other or spouse to specific locations sometimes consider a locum tenens as a bridge to permanent positions. Late-stage physicians who no longer want to be tied to a small group or solo practice have become locum tenens physicians who enjoy multiple temporary employment positions nationwide. This pathway no longer is unusual and can be a satisfying means to expand employment horizons. As with all employment situations, due diligence is mandatory before signing with any locum tenens company.
Conclusions
The employment spectrum for gastroenterologists and other medical professionals has expanded greatly between the time the senior author and the junior author entered the workforce. Change is now the one constant in medicine, and medicine today largely is fast-paced, corporatized, and highly regulated. Finding an employment model that is comfortable for current physicians, whose life situations are quite diverse, can be challenging. but a variety of opportunities now exist.
Think carefully about what you truly desire as a medical professional and how you might shape your employment to realize your goals. Options are available for those with an open mind and persistence.
References
1. Sheen E, Dorn SD, Brill JV, et al. Health care reform and the road ahead for gastroenterology. Clin Gastroenterol Hepatol. 2012;10:1062-5.
2. Kosinski LR. Meaningful use and electronic medical records for the gastroenterology practice. Clin Gastroenterol Hepatol. 2010;8:494-7.
3. Medical Group Management Association (MGMA). Accessed January 20, 2017.
4. The Coker Group. PSAs as an Alternative to Employment: A Contemporary Option for Alignment and Integration. In: The Coker Group Thought Leadership – White Papers. March 2016.
5. Houston R, McGinnis T. Accountable care organizations: looking back and moving forward. Centers for Health Care Strategies Inc. Brief. January 2016. Accessed January 20, 2017.
6. Pallardy C. 7 gastroenterologists leading GI mega-practices. Becker’s GI and endoscopy 2015. Accessed January 20, 2017.
Dr. Allen is in the division of gastroenterology and hepatology, department of medicine, University of Michigan School of Medicine, Ann Arbor; he is also the Editor in Chief of GI & Hepatology News. Dr. Kaushal is in the division of gastroenterology, Adventist Health Systems, Sonora, Calif. The authors disclose no conflicts.
The variety of employment models available to gastroenterologists reflects the dynamic changes we are experiencing in medicine today. Delivery of gastrointestinal (GI) care in the United States continues to evolve in light of health care reform and the Affordable Care Act.1 Within the past decade, as health systems and payers continue to consolidate, regulatory pressures have increased steadily and new policies such as electronic documentation and mandatory quality metrics reporting have added new challenges to the emerging generation of gastroenterologists.2 Although the lay press tends to focus on health care costs, coverage, physician reimbursement, provider burnout, health system consolidation, and value-based payment models, relatively less has been published about emerging employment and practice models.
Here,
Background
When the senior author graduated from fellowship in 1983 (J.I.A.), gastroenterology practice model choices were limited to essentially 4: independent community-based, single-specialty, physician-owned practice (solo or small group); independent multispecialty physician-owned practice; hospital or health system–owned multispecialty practice; and academic practice (including the Veterans Administration Medical Centers).
In the private sector, young community gastroenterologists typically would join a physician-owned practice and spend time (2–5 y) as an employed physician in a partnership track. During this time, his/her salary was subsidized while he/she built a practice base. Then, they would buy into the Professional Association with cash or equity equivalents and become a partner. As a partner, he/she then had the opportunity to share in ancillary revenue streams such as facility fees derived from a practice-owned ambulatory endoscopy center (AEC). By contrast, young academic faculty would be hired as an instructor and, if successful, climb the traditional ladder track to assistant, associate, and professor of medicine in an academic medical center (AMC).
In the 1980s, a typical community GI practice comprised 1 to 8 physicians, with most having been formed by 1 or 2 male gastroenterologists in the early 1970s when flexible endoscopy moved into clinical practice. The three practices that eventually would become Minnesota Gastroenterology (where J.I.A. practiced) opened in 1972. In 1996, the three practices merged into a single group of 38 physicians with ownership in three AECs. Advanced practice nurses and physician assistants were not yet part of the equation. Colonoscopy represented 48% of procedure volume, accounts receivable (time between submitting an insurance claim and being paid) averaged 88 days, and physicians averaged 9000 work relative value units (wRVUs) per partner annually. By comparison, median wRVUs for a full-time community GI in 1996 was 10,422 according to the Medical Group Management Association.3 Annual gross revenue (before expenses) per physician was approximately $400,000, and overhead reached 38% and 47% of revenue (there were 2 divisions). Partner incomes were at the 12% level of the Medical Group Management Association for gastroenterologists (personal management notes of J.I.A.). Minnesota Gastroenterology was the largest single-specialty GI practice in 1996 and its consolidation foreshadowed a trend that has accelerated over the ensuing generation.
When one of the authors (N.K.) graduated from the University of California Los Angeles in 2017, the GI employment landscape had evolved considerably. At least five new models of GI practice had emerged: individual incorporation with a Professional Services Agreement (PSA), a clinician track within an AMC, large single-specialty group practice (partnership or employee), private equity-backed multistate practice, and locum tenens (Figure 1).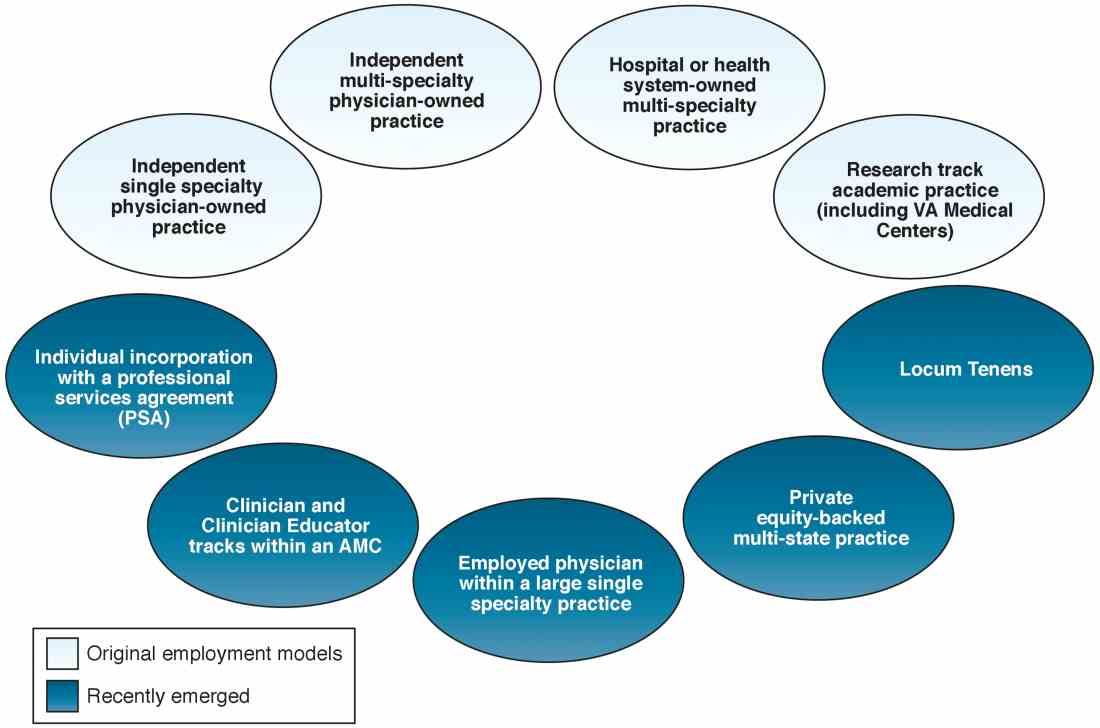
Employment models (light blue) available in the 1980s and those that have emerged as common models in the last decade (dark blue).
An individual corporation with a professional services agreement
For gastroenterologists at any career stage, the prospect of employment within a corporate entity, be it an academic university, hospital system, or private practice group, can be daunting. To that end, one central question facing nearly all gastroenterologists is: how much independence and flexibility, both clinically and financially, do I really want, and what can I do to realize my ideal job description?
An interesting alternative to direct health system employment occurs when a physician forms a solo corporation and then contracts with a hospital or health system under a PSA. Here, the physician provides professional services on a contractual basis, but retains control of finances and has more autonomy compared with employment. Essentially, the physician is a corporation of one, with hospital alignment rather than employment. For full disclosure, this is the employment model of one of the authors (N.K.).
A PSA arrangement is common for larger independent GI practices. Many practices have PSA arrangements with hospitals ranging from call coverage to full professional services. For an individual working within a PSA, income is not the traditional W-2 Internal Revenue Service arrangement in which taxes are removed automatically. Income derived from a PSA usually falls under an Internal Revenue Service Form 1099. The physician actually is employed through their practice corporation and relates to the hospital as an independent contractor.
There are four common variants of the PSA model.4 A Global Payment PSA is when a hospital contracts with the physician practice for specific services and pays a global rate linked to wRVUs. The rate is negotiated to encompass physician compensation, benefits, and practice overhead. The practice retains control of its own office functions and staff.
In a traditional PSA, the hospital contracts with physicians and pays them based on RVU production, but the hospital owns the administrative part of the practice (staff, billing, collections, equipment, and supplies).
A practice management arrangement occurs when the hospital employs the physician who provides professional services and a separate third party manages the practice via a separate management contract. Finally, a Carve-Out PSA can use any of the earlier-described PSA arrangements and certain services are carved out under line-item provisions. For example, a hospital could contract with a private GI group for endoscopic services or night call and write a PSA expressly for these purposes.
Some notable benefits of the PSA are that physicians can maintain financial and employment independence from the hospital and have more control over benefits packages, retirement savings options, and health insurance. Physicians also can provide services outside of the hospital (e.g., telemedicine or locums tenens — see later) without institutional restrictions or conflicts. Finally, physicians benefit from tax advantages of self-employment (with associated business-related tax deductions) through their corporation. The potential downsides of a PSA contract are the subtle expansion of services demanded (known as scope creep) or the possibility of contract termination (or nonrenewal) by the hospital. In addition, medical training does not equip physicians with the knowledge to navigate personal and corporate finances, benefits packages, and tax structures, so the learning curve can be quite steep. Nevertheless, PSAs can be an innovative employment model for gastroenterologists who wish to preserve autonomy and financial flexibility. In this model, legal advice by an attorney skilled in employment law is mandatory.
Academic clinicians track
Until recently, clinically oriented academic faculty were channeled into the traditional ladder faculty model in which advancement was contingent on publications, national recognition, grant support, and teaching. As competition for market share has intensified among regional health systems, many AMCs have developed purely clinical tracks in which research, publication, and teaching are not expected; salaries are linked to clinical productivity; and income may approximate the professional (but not ancillary) income of a community gastroenterologist.
Various models of this arrangement exist as well. For example, clinicians can be employed within a group that has a board and management structure distinct from the faculty group practice, as in the case of the Northeast Medical Group at Yale New Haven Health System5 and the University of Maryland Community Medical Group. In addition, clinicians can form an operating group separate from the faculty practice but as a controlled subsidiary (such as the University of Pittsburgh Community Medicine), separate operating group for primary care but specialists are employed within their respective departments (Emory Specialty Associates) or as a distinct clinical department within a faculty practice (University of California Los Angeles Medical Group Staff Physicians).
Irrespective of the employment model, these clinicians essentially work similar to community gastroenterologists but within the umbrella of an AMC. For young faculty whose interest is not in research or teaching, this can be an attractive option that maintains a tie to a university health system. For a seasoned clinician in community practice, this is an option to return to an academic environment. Usually, productivity expectations within the clinician track approximate those of a community practice gastroenterologist, but again total compensation may not be as great because ancillary income streams usually are not available. We expect this AMC employment track to become more prevalent as universities expand their footprints and acquire practices, hospitals, and ambulatory facilities distant from the main campus.
Large single-specialty practice
Consolidation of independent practices has been evident for 20 years and has accelerated as physicians in smaller practices have aged and burdens of practice have increased. Now, most urban centers have large mega-sized practices or super groups that have grown through practice mergers, acquisitions, and successful recruitment. Large practices can be modeled as a single integrated corporation (with ancillary components such as an AEC or infusion center) or as individual business units that are grouped under a single corporate entity.6
Within these large and mega-sized practices, differing employment options have emerged in addition to the traditional partnership track. These include payment on a per-diem basis, annual salary, or a mix of both. As opposed to partnership, the employment track avoids responsibility for governance and corporate liability, although not individual liability, and usually does not involve after-hours call. An employed physician usually does not benefit from ancillary income that derives from AEC facility fees, infusion centers, and pathology and anesthesia services.
Private equity ownership of gastroenterology practices
In June 2016, private equity entered the GI space with the investment of the Audax Group in a community GI practice based in Miami, Florida. The term private equity refers to capital that is not reported in public forums and comprises funds that investors directly invest into private companies or use to buy out public companies and turn them private.
According to their website, when the Audax Group invests in a medical practice, they provide capital for substantial infrastructure support, business experience, and acumen, but retain medical practice leaders as their clinical decision makers. They also bring proven expertise and economies of scale to resource-intensive aspects of a medical practice including information technology, regulation compliance, human resources, revenue cycle management, payroll, benefits, rents, and lease as examples. These components can be difficult to manage efficiently within independent medical practices, so many maturing practices are selling their practices to regional health systems. This multistate equity-backed medical practice is an alternative to health system acquisition, and may help physicians feel more in control of their practices and potentially share in the equity investment.
It is important to understand the employment structure and associations of any practice you are contemplating joining. The model devised by this group is meant to retain physician authority and responsibility while providing capital to support innovation and the development of needed infrastructure. Growth of market share and revenues can accrue back to physician owners. This is distinct from practices that are part of a health system in which there may be more of a corporate feeling and centralized governance.
Locum tenens
Locum tenens is a Latin phrase that means “to hold the place of.” According to the website of a large locum tenens company, this practice model originated in the 1970s when the federal government provided a grant to the University of Utah to provide physician services for underserved areas in the Western United States. The program proved so successful that hospital administrators who had difficulty recruiting staff physicians began asking for staffing assistance.
Today, a substantial number of physicians at all stages of their careers are working as locum tenens. They work as independent contractors so that income taxes are not withheld and benefits are the responsibility of the individual. As with the PSA arrangement, a physician would meet with both an accountant and labor lawyer to establish him or herself as a corporate entity for tax advantages and limited liability from litigation.
Early stage physicians who might be following a significant other or spouse to specific locations sometimes consider a locum tenens as a bridge to permanent positions. Late-stage physicians who no longer want to be tied to a small group or solo practice have become locum tenens physicians who enjoy multiple temporary employment positions nationwide. This pathway no longer is unusual and can be a satisfying means to expand employment horizons. As with all employment situations, due diligence is mandatory before signing with any locum tenens company.
Conclusions
The employment spectrum for gastroenterologists and other medical professionals has expanded greatly between the time the senior author and the junior author entered the workforce. Change is now the one constant in medicine, and medicine today largely is fast-paced, corporatized, and highly regulated. Finding an employment model that is comfortable for current physicians, whose life situations are quite diverse, can be challenging. but a variety of opportunities now exist.
Think carefully about what you truly desire as a medical professional and how you might shape your employment to realize your goals. Options are available for those with an open mind and persistence.
References
1. Sheen E, Dorn SD, Brill JV, et al. Health care reform and the road ahead for gastroenterology. Clin Gastroenterol Hepatol. 2012;10:1062-5.
2. Kosinski LR. Meaningful use and electronic medical records for the gastroenterology practice. Clin Gastroenterol Hepatol. 2010;8:494-7.
3. Medical Group Management Association (MGMA). Accessed January 20, 2017.
4. The Coker Group. PSAs as an Alternative to Employment: A Contemporary Option for Alignment and Integration. In: The Coker Group Thought Leadership – White Papers. March 2016.
5. Houston R, McGinnis T. Accountable care organizations: looking back and moving forward. Centers for Health Care Strategies Inc. Brief. January 2016. Accessed January 20, 2017.
6. Pallardy C. 7 gastroenterologists leading GI mega-practices. Becker’s GI and endoscopy 2015. Accessed January 20, 2017.
Dr. Allen is in the division of gastroenterology and hepatology, department of medicine, University of Michigan School of Medicine, Ann Arbor; he is also the Editor in Chief of GI & Hepatology News. Dr. Kaushal is in the division of gastroenterology, Adventist Health Systems, Sonora, Calif. The authors disclose no conflicts.
The variety of employment models available to gastroenterologists reflects the dynamic changes we are experiencing in medicine today. Delivery of gastrointestinal (GI) care in the United States continues to evolve in light of health care reform and the Affordable Care Act.1 Within the past decade, as health systems and payers continue to consolidate, regulatory pressures have increased steadily and new policies such as electronic documentation and mandatory quality metrics reporting have added new challenges to the emerging generation of gastroenterologists.2 Although the lay press tends to focus on health care costs, coverage, physician reimbursement, provider burnout, health system consolidation, and value-based payment models, relatively less has been published about emerging employment and practice models.
Here,
Background
When the senior author graduated from fellowship in 1983 (J.I.A.), gastroenterology practice model choices were limited to essentially 4: independent community-based, single-specialty, physician-owned practice (solo or small group); independent multispecialty physician-owned practice; hospital or health system–owned multispecialty practice; and academic practice (including the Veterans Administration Medical Centers).
In the private sector, young community gastroenterologists typically would join a physician-owned practice and spend time (2–5 y) as an employed physician in a partnership track. During this time, his/her salary was subsidized while he/she built a practice base. Then, they would buy into the Professional Association with cash or equity equivalents and become a partner. As a partner, he/she then had the opportunity to share in ancillary revenue streams such as facility fees derived from a practice-owned ambulatory endoscopy center (AEC). By contrast, young academic faculty would be hired as an instructor and, if successful, climb the traditional ladder track to assistant, associate, and professor of medicine in an academic medical center (AMC).
In the 1980s, a typical community GI practice comprised 1 to 8 physicians, with most having been formed by 1 or 2 male gastroenterologists in the early 1970s when flexible endoscopy moved into clinical practice. The three practices that eventually would become Minnesota Gastroenterology (where J.I.A. practiced) opened in 1972. In 1996, the three practices merged into a single group of 38 physicians with ownership in three AECs. Advanced practice nurses and physician assistants were not yet part of the equation. Colonoscopy represented 48% of procedure volume, accounts receivable (time between submitting an insurance claim and being paid) averaged 88 days, and physicians averaged 9000 work relative value units (wRVUs) per partner annually. By comparison, median wRVUs for a full-time community GI in 1996 was 10,422 according to the Medical Group Management Association.3 Annual gross revenue (before expenses) per physician was approximately $400,000, and overhead reached 38% and 47% of revenue (there were 2 divisions). Partner incomes were at the 12% level of the Medical Group Management Association for gastroenterologists (personal management notes of J.I.A.). Minnesota Gastroenterology was the largest single-specialty GI practice in 1996 and its consolidation foreshadowed a trend that has accelerated over the ensuing generation.
When one of the authors (N.K.) graduated from the University of California Los Angeles in 2017, the GI employment landscape had evolved considerably. At least five new models of GI practice had emerged: individual incorporation with a Professional Services Agreement (PSA), a clinician track within an AMC, large single-specialty group practice (partnership or employee), private equity-backed multistate practice, and locum tenens (Figure 1).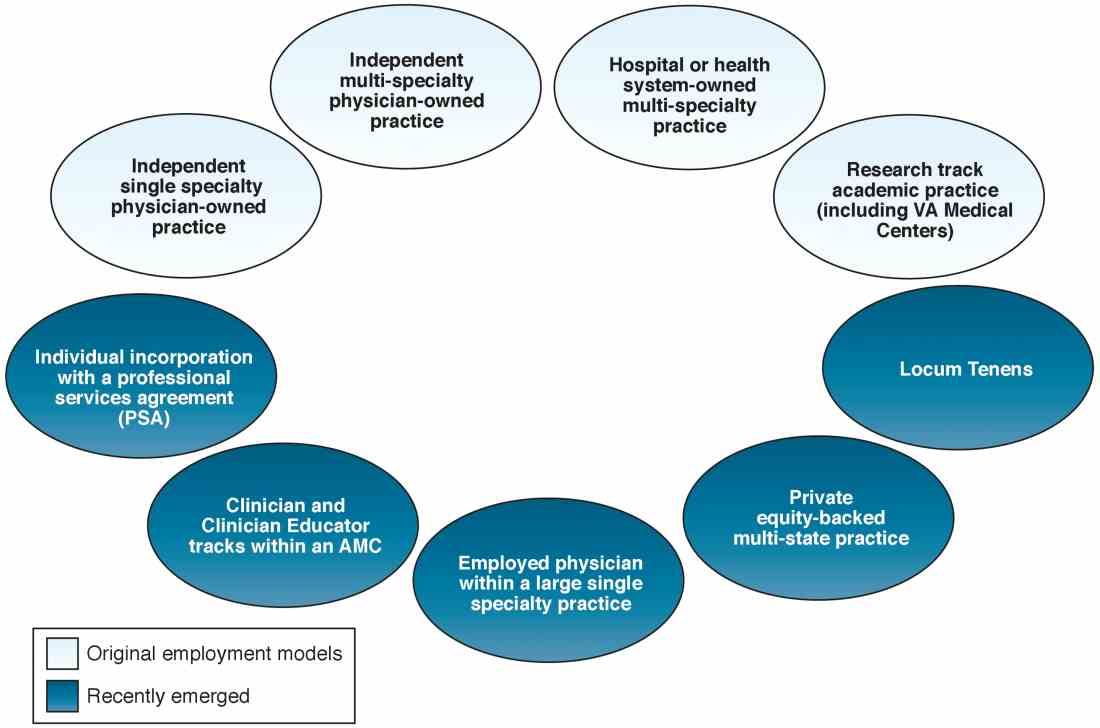
Employment models (light blue) available in the 1980s and those that have emerged as common models in the last decade (dark blue).
An individual corporation with a professional services agreement
For gastroenterologists at any career stage, the prospect of employment within a corporate entity, be it an academic university, hospital system, or private practice group, can be daunting. To that end, one central question facing nearly all gastroenterologists is: how much independence and flexibility, both clinically and financially, do I really want, and what can I do to realize my ideal job description?
An interesting alternative to direct health system employment occurs when a physician forms a solo corporation and then contracts with a hospital or health system under a PSA. Here, the physician provides professional services on a contractual basis, but retains control of finances and has more autonomy compared with employment. Essentially, the physician is a corporation of one, with hospital alignment rather than employment. For full disclosure, this is the employment model of one of the authors (N.K.).
A PSA arrangement is common for larger independent GI practices. Many practices have PSA arrangements with hospitals ranging from call coverage to full professional services. For an individual working within a PSA, income is not the traditional W-2 Internal Revenue Service arrangement in which taxes are removed automatically. Income derived from a PSA usually falls under an Internal Revenue Service Form 1099. The physician actually is employed through their practice corporation and relates to the hospital as an independent contractor.
There are four common variants of the PSA model.4 A Global Payment PSA is when a hospital contracts with the physician practice for specific services and pays a global rate linked to wRVUs. The rate is negotiated to encompass physician compensation, benefits, and practice overhead. The practice retains control of its own office functions and staff.
In a traditional PSA, the hospital contracts with physicians and pays them based on RVU production, but the hospital owns the administrative part of the practice (staff, billing, collections, equipment, and supplies).
A practice management arrangement occurs when the hospital employs the physician who provides professional services and a separate third party manages the practice via a separate management contract. Finally, a Carve-Out PSA can use any of the earlier-described PSA arrangements and certain services are carved out under line-item provisions. For example, a hospital could contract with a private GI group for endoscopic services or night call and write a PSA expressly for these purposes.
Some notable benefits of the PSA are that physicians can maintain financial and employment independence from the hospital and have more control over benefits packages, retirement savings options, and health insurance. Physicians also can provide services outside of the hospital (e.g., telemedicine or locums tenens — see later) without institutional restrictions or conflicts. Finally, physicians benefit from tax advantages of self-employment (with associated business-related tax deductions) through their corporation. The potential downsides of a PSA contract are the subtle expansion of services demanded (known as scope creep) or the possibility of contract termination (or nonrenewal) by the hospital. In addition, medical training does not equip physicians with the knowledge to navigate personal and corporate finances, benefits packages, and tax structures, so the learning curve can be quite steep. Nevertheless, PSAs can be an innovative employment model for gastroenterologists who wish to preserve autonomy and financial flexibility. In this model, legal advice by an attorney skilled in employment law is mandatory.
Academic clinicians track
Until recently, clinically oriented academic faculty were channeled into the traditional ladder faculty model in which advancement was contingent on publications, national recognition, grant support, and teaching. As competition for market share has intensified among regional health systems, many AMCs have developed purely clinical tracks in which research, publication, and teaching are not expected; salaries are linked to clinical productivity; and income may approximate the professional (but not ancillary) income of a community gastroenterologist.
Various models of this arrangement exist as well. For example, clinicians can be employed within a group that has a board and management structure distinct from the faculty group practice, as in the case of the Northeast Medical Group at Yale New Haven Health System5 and the University of Maryland Community Medical Group. In addition, clinicians can form an operating group separate from the faculty practice but as a controlled subsidiary (such as the University of Pittsburgh Community Medicine), separate operating group for primary care but specialists are employed within their respective departments (Emory Specialty Associates) or as a distinct clinical department within a faculty practice (University of California Los Angeles Medical Group Staff Physicians).
Irrespective of the employment model, these clinicians essentially work similar to community gastroenterologists but within the umbrella of an AMC. For young faculty whose interest is not in research or teaching, this can be an attractive option that maintains a tie to a university health system. For a seasoned clinician in community practice, this is an option to return to an academic environment. Usually, productivity expectations within the clinician track approximate those of a community practice gastroenterologist, but again total compensation may not be as great because ancillary income streams usually are not available. We expect this AMC employment track to become more prevalent as universities expand their footprints and acquire practices, hospitals, and ambulatory facilities distant from the main campus.
Large single-specialty practice
Consolidation of independent practices has been evident for 20 years and has accelerated as physicians in smaller practices have aged and burdens of practice have increased. Now, most urban centers have large mega-sized practices or super groups that have grown through practice mergers, acquisitions, and successful recruitment. Large practices can be modeled as a single integrated corporation (with ancillary components such as an AEC or infusion center) or as individual business units that are grouped under a single corporate entity.6
Within these large and mega-sized practices, differing employment options have emerged in addition to the traditional partnership track. These include payment on a per-diem basis, annual salary, or a mix of both. As opposed to partnership, the employment track avoids responsibility for governance and corporate liability, although not individual liability, and usually does not involve after-hours call. An employed physician usually does not benefit from ancillary income that derives from AEC facility fees, infusion centers, and pathology and anesthesia services.
Private equity ownership of gastroenterology practices
In June 2016, private equity entered the GI space with the investment of the Audax Group in a community GI practice based in Miami, Florida. The term private equity refers to capital that is not reported in public forums and comprises funds that investors directly invest into private companies or use to buy out public companies and turn them private.
According to their website, when the Audax Group invests in a medical practice, they provide capital for substantial infrastructure support, business experience, and acumen, but retain medical practice leaders as their clinical decision makers. They also bring proven expertise and economies of scale to resource-intensive aspects of a medical practice including information technology, regulation compliance, human resources, revenue cycle management, payroll, benefits, rents, and lease as examples. These components can be difficult to manage efficiently within independent medical practices, so many maturing practices are selling their practices to regional health systems. This multistate equity-backed medical practice is an alternative to health system acquisition, and may help physicians feel more in control of their practices and potentially share in the equity investment.
It is important to understand the employment structure and associations of any practice you are contemplating joining. The model devised by this group is meant to retain physician authority and responsibility while providing capital to support innovation and the development of needed infrastructure. Growth of market share and revenues can accrue back to physician owners. This is distinct from practices that are part of a health system in which there may be more of a corporate feeling and centralized governance.
Locum tenens
Locum tenens is a Latin phrase that means “to hold the place of.” According to the website of a large locum tenens company, this practice model originated in the 1970s when the federal government provided a grant to the University of Utah to provide physician services for underserved areas in the Western United States. The program proved so successful that hospital administrators who had difficulty recruiting staff physicians began asking for staffing assistance.
Today, a substantial number of physicians at all stages of their careers are working as locum tenens. They work as independent contractors so that income taxes are not withheld and benefits are the responsibility of the individual. As with the PSA arrangement, a physician would meet with both an accountant and labor lawyer to establish him or herself as a corporate entity for tax advantages and limited liability from litigation.
Early stage physicians who might be following a significant other or spouse to specific locations sometimes consider a locum tenens as a bridge to permanent positions. Late-stage physicians who no longer want to be tied to a small group or solo practice have become locum tenens physicians who enjoy multiple temporary employment positions nationwide. This pathway no longer is unusual and can be a satisfying means to expand employment horizons. As with all employment situations, due diligence is mandatory before signing with any locum tenens company.
Conclusions
The employment spectrum for gastroenterologists and other medical professionals has expanded greatly between the time the senior author and the junior author entered the workforce. Change is now the one constant in medicine, and medicine today largely is fast-paced, corporatized, and highly regulated. Finding an employment model that is comfortable for current physicians, whose life situations are quite diverse, can be challenging. but a variety of opportunities now exist.
Think carefully about what you truly desire as a medical professional and how you might shape your employment to realize your goals. Options are available for those with an open mind and persistence.
References
1. Sheen E, Dorn SD, Brill JV, et al. Health care reform and the road ahead for gastroenterology. Clin Gastroenterol Hepatol. 2012;10:1062-5.
2. Kosinski LR. Meaningful use and electronic medical records for the gastroenterology practice. Clin Gastroenterol Hepatol. 2010;8:494-7.
3. Medical Group Management Association (MGMA). Accessed January 20, 2017.
4. The Coker Group. PSAs as an Alternative to Employment: A Contemporary Option for Alignment and Integration. In: The Coker Group Thought Leadership – White Papers. March 2016.
5. Houston R, McGinnis T. Accountable care organizations: looking back and moving forward. Centers for Health Care Strategies Inc. Brief. January 2016. Accessed January 20, 2017.
6. Pallardy C. 7 gastroenterologists leading GI mega-practices. Becker’s GI and endoscopy 2015. Accessed January 20, 2017.
Dr. Allen is in the division of gastroenterology and hepatology, department of medicine, University of Michigan School of Medicine, Ann Arbor; he is also the Editor in Chief of GI & Hepatology News. Dr. Kaushal is in the division of gastroenterology, Adventist Health Systems, Sonora, Calif. The authors disclose no conflicts.
From Obamacare to Trumpcare – implications for gastroenterologists
The June issue of CGH was the final column under my management. I have enjoyed the opportunity to provide you with information about practice management and health care reform. I also have enjoyed working with the Clinical Gastroenterology and Hepatology board of editors, and Erin Landis and Brook Simpson from AGA headquarters. Beginning in July 2017, this section will become the responsibility of Ziad Gellad, MD, MPH, AGAF, from Duke University. I have worked with Ziad for many years, and he serves on my board of editors for GI & Hepatology News. I have great confidence in his knowledge and ability.
During the last 5 years, we have published 58 columns beginning with an article where I made several broad predictions. I have tried to present important concepts and management tools related to private and academic clinical practice, health care reform, and health economics. This article was written in early January 2017 just before the inauguration of Donald Trump. As I wrote, we did not know the full extent or the pace of “Repeal and Replace,” as Obamacare becomes Trumpcare (www.healthaffairs.org/obamacare-to-trumpcare).
The extent of current Republican control of federal and state governments is unprecedented in modern political history. Per Newt Gingrich (The Economist, Jan. 7, 2017, p. 25), this will be the third attempt, after Ronald Reagan’s election in 1980 and Gingrich’s “Contract with America” in 1994, to break free from a “Big Government” mindset initiated by Franklin Roosevelt’s New Deal. In this article, I will speculate how a right-leaning shift in American health care policy might impact the business model of gastroenterology. No matter how government regulations or funds flow change, we (physicians) will ultimately be responsible for digestive care provided to our patients. In the words of Martin Luther King Jr. (as he paraphrased Theodore Parker), “The arc of the moral universe is long, but it bends toward justice.” What is remembered by fewer people, however, are words he then added during his speeches: “but only if we march.”
John I. Allen, MD, MBA, AGAF
Editor in Chief
The first column was published in July 2012.1 I wrote about five dominant themes that would alter our gastroenterology practices in the ensuing years. They were 1) an increasing requirement for us to demonstrate value, 2) the need to think about population management in addition to individual patient care, 3) consolidation that would occur at all levels of health care delivery, 4) increasing cost pressure, and 5) how medical decisions would be linked to reimbursement (now called value-based payment). I fully expected the Patient Protection and Affordable Care Act (ACA) would shape the health care landscape for the rest of our careers. After the article’s publication, I was invited to speak about health care reform at many academic centers and private practices. My last talk before the election was in Pasadena, Calif. (Oct. 28, 2016) where I confidently spoke about the implications of President Clinton’s cementing ACA into the fabric of U.S. medicine.
Donald Trump is now the 45th President of the United States. Republicans hold a 52-48 majority in the Senate and a 241-194 majority in the House. As of January 2017, one Supreme Court seat was available, and three more may open because of retirements (Justice Ginsburg is 83 years old, Justice Kennedy is 80, and Justice Breyer is 78). Republicans control all three branches of government in 25 states and dominate in 8 others. Conservative politicians control a large majority of county and city boards.
Until this year, Republicans have controlled all three branches of government only twice since 1945 (modern political history), and only once (George Bush in 2005) did the president have a Senate majority.2 With his win, Mr. Trump can lead a conservative revolution to reverse key initiatives begun when the Democratic Party held majority power. Repeal of the ACA, signed into legislation on March 23, 2010, is the Republican Party’s top priority.
Equally important, Congress can alter previously implemented federal regulations. Each year about 3,000 regulations are written by federal agencies that act with authority delegated by Congress (albeit Congress retains power to overturn them). Regulations are published in the Federal Register as preliminary rules during each year, and Final Rules are published after a public comment period and implemented shortly thereafter. Regulations carry the force of law and are codified in the Code of Federal Regulations. The Code of Federal Regulations is divided into 50 sections (Titles), with Title 42 (Public Health) and Title 45 (Public Welfare) most pertinent to us.
Other policies are created through executive orders, issued by the president (federal) or governors (states), without involvement of legislative or judicial branches (they were not mentioned in the Constitution, by the way). Executive orders issued by President Obama could, theoretically, be overturned by new executive orders.
Repeal and replace
Destruction of the ACA is a top priority of President Trump and Republican leaders of both houses of Congress. The ACA was a Democratic bill (passed with no Republican support), although it had many similarities to previous Republican legislative ideas dating from 1993.3
Although outright repeal could be blocked by a Democratic filibuster, the law could be drastically modified through budget reconciliation whose passage takes only a simple Senate majority. Thus, a simple budget-related bill could serve as a vehicle to defund many parts of ACA, including money for Medicaid expansion, insurance risk corridors, money to offset out-of-pocket expenses and individual premium subsidies, for example.4,5
There would be substantial problems if ACA were repealed even with a 2- or 3-year delay, a scenario proposed to provide time for a replacement bill. On Jan. 4, 2017, the House Republican Study Committee introduced the American Health Care Reform Act (AHCRA) as a replacement proposal, with the stipulation that ACA would be repealed as of Jan. 1, 2018. This initial bill hinted at Republican intent and was detailed in a Health Affairs blog.6 Importantly, there were distinct similarities between this and prior Republican proposals put forward by Representative Tom Price (nominated to head the Department of Health & Human Services under President Trump) and Speaker of the House Paul Ryan.7,8
Consistently, Republicans have advocated for expansion of health savings accounts, altering the tax code to allow individuals to deduct health insurance premiums, establishment of association risk pools, imposition of malpractice limits, protections for people with preexisting conditions, and further restrictions on abortion coverage. The AHCRA changes financial subsidies for purchasing insurance from a tax credit (which can be paid to people even if they do not pay taxes) to a tax deduction (only applicable to people who pay taxes). Analysis of a similar proposal made by President Trump during the campaign found that this plan would increase the number of uninsured people by more than 15 million.
If ACA is repealed, effects would be broader than just factors related to insurance coverage.9 ACA provides for preventive care (including colonoscopy) without copays, education of additional medical personnel, closing the donut hole for Medicare Part D (medications), approval of generic biologics, and Medicaid expansions, among other initiatives. If ACA were defunded without restoring pre-ACA support for Disproportion Share Hospital charity care, research, and graduate medical education, then safety-net hospitals and many academic medical centers (AMCs) could face enormous funding cuts.10 Defunding Medicaid expansion would adversely affect states in many ways, as pointed out by Ayanian et al.11 Medicaid expansion had broad economic impact in states that accepted federal money to expand. In Michigan for example, 30,900 jobs were added to the state in 2016 because of Medicaid expansion, with two-thirds outside of the health care industry. President Obama defined his view about the effects of ACA repeal in the New England Journal of Medicine.12
Lessons learned
Economic principles and unique characteristics of United States health care help explain why solutions to its high cost and uneven coverage are so difficult to achieve. These include higher prices for goods in the United States compared with other countries, variation in price (unrelated to quality), restraints on government price negotiations, inefficiencies due to variation in size of delivery systems, and “moral hazard” related to rich insurance coverage, which are some of the factors that doom any simple solutions. These are reviewed by Victor Fuchs13 in an excellent article in Annals of Internal Medicine. Payment methods for health care services also distort resource use and efficiencies. Understanding the eight basic payment methodologies in health care and current predictions about future health care spending will be important in shaping reimbursement policies.14,15
Disruptions in health care are unpopular and, as Uve Reinardt stated: “Our health care financing system will always remain a horrendous mess and a fountain for such dismay among the providers of health care as well as among patients.”4 Lessons to inform the next iteration of health care policy, learned from the 2009-2010 experience, might be as follows:
1. If a bill is to be passed, the president must personally lead in explaining the bill to the public in simple terms.
2. Even the threat of repeal may disrupt the current market and force insurance companies to exit quickly.
3. Coverage must be affordable to individuals, state budgets, and health care providers. Because expansion states saw positive impacts to state budgets8 and mental health and substance abuse services became part of Medicaid benefits, how will a replacement bill maintain coverage and compensate for new state moneys used now for other imperatives such as education and infrastructure?
4. Health care is like a massive cargo ship, not a sports car, so a bill to replace the ACA may take a long time (and might never be passed).
5. Health care is intensely personal, so it will always be politically charged.
Ultimately, physicians will need to make strategic guesses and rapid adjustments to sustain financial viability and provide high-value care. Strategies differ depending on your practice situation. Keep in mind the five principles listed in the opening paragraph of this article. It is likely that the most important principle to factor into your practice strategy is continuing reduction in reimbursements. No matter what model is adopted to reform the ACA, the financial pot (Medicare, Medicaid, commercial insurance, bundled payments, fee-for-service payments) will be reduced, and the number of uninsured patients will increase. How would you change your practice if Medicare was your best payer (“manage to Medicare”)?
Independent practices
Physicians in small- to medium-size independent practices continue to struggle with reducing reimbursements, reporting burdens, increasing overhead expenses, crushing regulatory requirements, and provider burnout. Trumpcare will favor small practices more than Obamacare from a policy (not necessarily a financial) perspective. Regulations on small business and reporting burdens may ease, but the move toward value-based reimbursement as outlined in the MACRA (passed with overwhelming bipartisan support) will not end.16 Practices in small communities continue to thrive because they give excellent care with limited competition and low overhead. Some practices in suburban and urban centers struggle because payers tend to favor (with enhanced managed care rates) larger practices and health systems. Large, horizontally integrated, efficient gastroenterology practices will continue to thrive because they can develop a “must-have” position with payers. Building remote patient monitoring, teleconsulting, and capabilities around value demonstration will be strategically advantageous.
Options for independent physicians include 1) maintaining status quo, 2) retiring, or 3) exiting the independent business model through a practice sale. Traditionally, physicians who wanted to sell their practices turned to hospitals or health systems. Recently, a physician-run model funded by venture capital has emerged where reduced overhead (through centralization of services) is combined with enhanced power during payer negotiations (because of scale). This model has allowed practices to merge into a physician organization and remain free from health system employment.17
Large health systems
Physicians employed by large health systems, whether they are nonprofit, for-profit, or AMCs, will see their future tied directly to health system success. If bundled payment, alternative payment, and capitation models of health care financing continue to grow in popularity, then success will be determined by a health system’s market share and its ability to form true clinical integration. In a capitated environment, expansion of market share (especially of relatively healthy patients) will help support margins. However, financial success will come from a system’s ability to manage high-cost patients, those 5% of patients who consume 50% of health care resources.18
Hospitals with a financially challenged patient base (safety-net hospitals) will have enormous financial pressures going forward. Repeal of ACA without restoration of pre-ACA funding will affect directly the financial health of systems including AMCs. AMCs and other health systems will be forced to reduce fixed overhead, enhance productivity of faculty, and restrict nonfunded activities (teaching for example). Although most AMCs are now in an active acquisition mode, this strategy is naturally limited by the number of remaining acquisition targets. Traditional high managed care rates enjoyed by AMCs will shrink, as will federal research funding (which typically comes with high indirect financial support). Health systems and GI societies will need to dedicate much more attention to state policy makers as Trumpcare progresses.
Finally, all providers will need to manage the business implications of retail health. As people assume higher deductibles and copays and health savings accounts grow, patients will change their patterns of purchasing services. Reputation counts for less when people are facing large price differences, so attention to patient-centric amenities, price, patient engagement, and patient satisfaction will become even more important.
Conclusion
The United States has undergone a massive and rapid political transformation. The mandate felt by conservative politicians, perhaps not supported by numbers, will carry a conservative platform forward. In areas where progressive Democrats emphasized federal power and socialized regulation (religion, education, civil rights, income security, and health policy), conservatives will transfer decision power as much as possible to states, local communities, and individuals. Maintaining the concept of “health as a right” will test the conscience of all of us.
References
1. Allen, J.I. The road ahead. Clin Gastroenterol Hepatol. 2012;10:692-6.
2. Gill KE. Visual guide: the balance of power between Congress and the Presidency (1901-2016). Wired Pen. November 2016. Available from http://wiredpen.com/resources/political-commentary-and-analysis/a-visual-guide-balance-of-power-congress-presidency/. Accessed Dec. 30, 2016.
3. Mertens M. Chart: comparing health reform bills – Democrats and Republicans 2009, Republics 1993. Kaiser Health News. Feb. 24, 2010. Available from http://khn.org/022310-bill-comparison/. Accessed Jan. 8, 2017.
4. Hotchkiss M. Q&A: what a Trump presidency means for the Affordable Care Act. Nov. 16, 2016 News at Princeton. Princeton University. Available from https://www.princeton.edu/main/news/archive/S47/93/09C11/index.xml?section=topstories. Accessed Dec. 30, 2016.
5. Jost T. Taking stock of health reform: where we’ve been, where we’re going. Health Affairs Blog. Available from http://healthaffairs.org/blog/2016/12/06/taking-stock-of-health-reform-where-weve-been-where-were-going/. Accessed Dec. 30, 2016.
6. Jost T. The Republican Study Committee’s ACA replacement proposal (updated). Health Affairs Blog. Available from http://healthaffairs.org/blog/2017/01/05/the-republican-study-committees-aca-replacement-proposal/. Accessed Jan. 10, 2017.
7. Price T. Empowering patients first. Available from http://tomprice.house.gov/sites/tomprice.house.gov/files/HR%202300%20Empowering%20Patients%20First%20Act%202015.pdf. Accessed Dec. 30, 2016.
8. Ryan P. A better way. Available from https://abetterway.speaker.gov/_assets/pdf/ABetterWay-HealthCare-PolicyPaper.pdf. Accessed Dec. 30, 2016.
9. Oberlander, J. The end of Obamacare. N Engl J Med. 2017;376:1-3.
10. Goodnough A. Hospitals in safety net brace for health care law’s repeal. New York Times. Dec. 28, 2016. Available from http://www.nytimes.com/2016/12/28/health/hospitals-medicaid-obamacare-trump.html?smprod=nytcore-iphone&smid=nytcore-iphone-share&_r=0. Accessed Jan. 10, 2017.
11. Ayanian, J.Z., Ehrlich, G.M., Grimes, D.R., et al. Economic effects of Medicaid expansion in Michigan. N Engl J Med. 2017;376:407-10.
12. Obama, B.H. Repealing the ACA without a replacement: the risks to American health care. N Engl J Med. 2017;376:297-9.
13. Fuchs, V.R. Major concepts of health economics. Ann Intern Med. 2015;162:380-3.
14. Quinn, K. The 8 basic payment methods in health care. Ann Intern Med. 2015;163:300-6.
15. Schoenman JA. A detailed look at US health care spending: a presentation from the National Institute for Health Care Management (NIHCM). Oct. 25, 2012. Available from http://www.nihcm.org/images/stories/Health_care_spending_slides_-_MILI_-_Schoenman.pdf. Accessed Dec. 30, 2016.
16. Allen, J.I., Allen, C.C., Brill, J.V. Gastroenterology 2020: no time for WIMPs. Gastroenterology. 2016;150:295-9.
17. Sciacca R. Weekly Byte: GI roundtable and navigating uncharted waters in health care. The PMD Blog. Available from https://www.pmd.com/blog/post/weekly-byte-gi-roundtable-and-navigating-uncharted-waters-in-health-care. Accessed Jan. 10, 2017.
18. Powers, B.W., Chaguturu, S.K. ACOs and high-cost patients. N Engl J Med. 2016;374:203-5.
Dr. Allen is professor of medicine, University of Michigan School of Medicine, Institute for Health Care Policy and Innovations, and associate medical director of Network Strategy and Business Development – Michigan Medicine, Ann Arbor. He discloses no conflicts.
The June issue of CGH was the final column under my management. I have enjoyed the opportunity to provide you with information about practice management and health care reform. I also have enjoyed working with the Clinical Gastroenterology and Hepatology board of editors, and Erin Landis and Brook Simpson from AGA headquarters. Beginning in July 2017, this section will become the responsibility of Ziad Gellad, MD, MPH, AGAF, from Duke University. I have worked with Ziad for many years, and he serves on my board of editors for GI & Hepatology News. I have great confidence in his knowledge and ability.
During the last 5 years, we have published 58 columns beginning with an article where I made several broad predictions. I have tried to present important concepts and management tools related to private and academic clinical practice, health care reform, and health economics. This article was written in early January 2017 just before the inauguration of Donald Trump. As I wrote, we did not know the full extent or the pace of “Repeal and Replace,” as Obamacare becomes Trumpcare (www.healthaffairs.org/obamacare-to-trumpcare).
The extent of current Republican control of federal and state governments is unprecedented in modern political history. Per Newt Gingrich (The Economist, Jan. 7, 2017, p. 25), this will be the third attempt, after Ronald Reagan’s election in 1980 and Gingrich’s “Contract with America” in 1994, to break free from a “Big Government” mindset initiated by Franklin Roosevelt’s New Deal. In this article, I will speculate how a right-leaning shift in American health care policy might impact the business model of gastroenterology. No matter how government regulations or funds flow change, we (physicians) will ultimately be responsible for digestive care provided to our patients. In the words of Martin Luther King Jr. (as he paraphrased Theodore Parker), “The arc of the moral universe is long, but it bends toward justice.” What is remembered by fewer people, however, are words he then added during his speeches: “but only if we march.”
John I. Allen, MD, MBA, AGAF
Editor in Chief
The first column was published in July 2012.1 I wrote about five dominant themes that would alter our gastroenterology practices in the ensuing years. They were 1) an increasing requirement for us to demonstrate value, 2) the need to think about population management in addition to individual patient care, 3) consolidation that would occur at all levels of health care delivery, 4) increasing cost pressure, and 5) how medical decisions would be linked to reimbursement (now called value-based payment). I fully expected the Patient Protection and Affordable Care Act (ACA) would shape the health care landscape for the rest of our careers. After the article’s publication, I was invited to speak about health care reform at many academic centers and private practices. My last talk before the election was in Pasadena, Calif. (Oct. 28, 2016) where I confidently spoke about the implications of President Clinton’s cementing ACA into the fabric of U.S. medicine.
Donald Trump is now the 45th President of the United States. Republicans hold a 52-48 majority in the Senate and a 241-194 majority in the House. As of January 2017, one Supreme Court seat was available, and three more may open because of retirements (Justice Ginsburg is 83 years old, Justice Kennedy is 80, and Justice Breyer is 78). Republicans control all three branches of government in 25 states and dominate in 8 others. Conservative politicians control a large majority of county and city boards.
Until this year, Republicans have controlled all three branches of government only twice since 1945 (modern political history), and only once (George Bush in 2005) did the president have a Senate majority.2 With his win, Mr. Trump can lead a conservative revolution to reverse key initiatives begun when the Democratic Party held majority power. Repeal of the ACA, signed into legislation on March 23, 2010, is the Republican Party’s top priority.
Equally important, Congress can alter previously implemented federal regulations. Each year about 3,000 regulations are written by federal agencies that act with authority delegated by Congress (albeit Congress retains power to overturn them). Regulations are published in the Federal Register as preliminary rules during each year, and Final Rules are published after a public comment period and implemented shortly thereafter. Regulations carry the force of law and are codified in the Code of Federal Regulations. The Code of Federal Regulations is divided into 50 sections (Titles), with Title 42 (Public Health) and Title 45 (Public Welfare) most pertinent to us.
Other policies are created through executive orders, issued by the president (federal) or governors (states), without involvement of legislative or judicial branches (they were not mentioned in the Constitution, by the way). Executive orders issued by President Obama could, theoretically, be overturned by new executive orders.
Repeal and replace
Destruction of the ACA is a top priority of President Trump and Republican leaders of both houses of Congress. The ACA was a Democratic bill (passed with no Republican support), although it had many similarities to previous Republican legislative ideas dating from 1993.3
Although outright repeal could be blocked by a Democratic filibuster, the law could be drastically modified through budget reconciliation whose passage takes only a simple Senate majority. Thus, a simple budget-related bill could serve as a vehicle to defund many parts of ACA, including money for Medicaid expansion, insurance risk corridors, money to offset out-of-pocket expenses and individual premium subsidies, for example.4,5
There would be substantial problems if ACA were repealed even with a 2- or 3-year delay, a scenario proposed to provide time for a replacement bill. On Jan. 4, 2017, the House Republican Study Committee introduced the American Health Care Reform Act (AHCRA) as a replacement proposal, with the stipulation that ACA would be repealed as of Jan. 1, 2018. This initial bill hinted at Republican intent and was detailed in a Health Affairs blog.6 Importantly, there were distinct similarities between this and prior Republican proposals put forward by Representative Tom Price (nominated to head the Department of Health & Human Services under President Trump) and Speaker of the House Paul Ryan.7,8
Consistently, Republicans have advocated for expansion of health savings accounts, altering the tax code to allow individuals to deduct health insurance premiums, establishment of association risk pools, imposition of malpractice limits, protections for people with preexisting conditions, and further restrictions on abortion coverage. The AHCRA changes financial subsidies for purchasing insurance from a tax credit (which can be paid to people even if they do not pay taxes) to a tax deduction (only applicable to people who pay taxes). Analysis of a similar proposal made by President Trump during the campaign found that this plan would increase the number of uninsured people by more than 15 million.
If ACA is repealed, effects would be broader than just factors related to insurance coverage.9 ACA provides for preventive care (including colonoscopy) without copays, education of additional medical personnel, closing the donut hole for Medicare Part D (medications), approval of generic biologics, and Medicaid expansions, among other initiatives. If ACA were defunded without restoring pre-ACA support for Disproportion Share Hospital charity care, research, and graduate medical education, then safety-net hospitals and many academic medical centers (AMCs) could face enormous funding cuts.10 Defunding Medicaid expansion would adversely affect states in many ways, as pointed out by Ayanian et al.11 Medicaid expansion had broad economic impact in states that accepted federal money to expand. In Michigan for example, 30,900 jobs were added to the state in 2016 because of Medicaid expansion, with two-thirds outside of the health care industry. President Obama defined his view about the effects of ACA repeal in the New England Journal of Medicine.12
Lessons learned
Economic principles and unique characteristics of United States health care help explain why solutions to its high cost and uneven coverage are so difficult to achieve. These include higher prices for goods in the United States compared with other countries, variation in price (unrelated to quality), restraints on government price negotiations, inefficiencies due to variation in size of delivery systems, and “moral hazard” related to rich insurance coverage, which are some of the factors that doom any simple solutions. These are reviewed by Victor Fuchs13 in an excellent article in Annals of Internal Medicine. Payment methods for health care services also distort resource use and efficiencies. Understanding the eight basic payment methodologies in health care and current predictions about future health care spending will be important in shaping reimbursement policies.14,15
Disruptions in health care are unpopular and, as Uve Reinardt stated: “Our health care financing system will always remain a horrendous mess and a fountain for such dismay among the providers of health care as well as among patients.”4 Lessons to inform the next iteration of health care policy, learned from the 2009-2010 experience, might be as follows:
1. If a bill is to be passed, the president must personally lead in explaining the bill to the public in simple terms.
2. Even the threat of repeal may disrupt the current market and force insurance companies to exit quickly.
3. Coverage must be affordable to individuals, state budgets, and health care providers. Because expansion states saw positive impacts to state budgets8 and mental health and substance abuse services became part of Medicaid benefits, how will a replacement bill maintain coverage and compensate for new state moneys used now for other imperatives such as education and infrastructure?
4. Health care is like a massive cargo ship, not a sports car, so a bill to replace the ACA may take a long time (and might never be passed).
5. Health care is intensely personal, so it will always be politically charged.
Ultimately, physicians will need to make strategic guesses and rapid adjustments to sustain financial viability and provide high-value care. Strategies differ depending on your practice situation. Keep in mind the five principles listed in the opening paragraph of this article. It is likely that the most important principle to factor into your practice strategy is continuing reduction in reimbursements. No matter what model is adopted to reform the ACA, the financial pot (Medicare, Medicaid, commercial insurance, bundled payments, fee-for-service payments) will be reduced, and the number of uninsured patients will increase. How would you change your practice if Medicare was your best payer (“manage to Medicare”)?
Independent practices
Physicians in small- to medium-size independent practices continue to struggle with reducing reimbursements, reporting burdens, increasing overhead expenses, crushing regulatory requirements, and provider burnout. Trumpcare will favor small practices more than Obamacare from a policy (not necessarily a financial) perspective. Regulations on small business and reporting burdens may ease, but the move toward value-based reimbursement as outlined in the MACRA (passed with overwhelming bipartisan support) will not end.16 Practices in small communities continue to thrive because they give excellent care with limited competition and low overhead. Some practices in suburban and urban centers struggle because payers tend to favor (with enhanced managed care rates) larger practices and health systems. Large, horizontally integrated, efficient gastroenterology practices will continue to thrive because they can develop a “must-have” position with payers. Building remote patient monitoring, teleconsulting, and capabilities around value demonstration will be strategically advantageous.
Options for independent physicians include 1) maintaining status quo, 2) retiring, or 3) exiting the independent business model through a practice sale. Traditionally, physicians who wanted to sell their practices turned to hospitals or health systems. Recently, a physician-run model funded by venture capital has emerged where reduced overhead (through centralization of services) is combined with enhanced power during payer negotiations (because of scale). This model has allowed practices to merge into a physician organization and remain free from health system employment.17
Large health systems
Physicians employed by large health systems, whether they are nonprofit, for-profit, or AMCs, will see their future tied directly to health system success. If bundled payment, alternative payment, and capitation models of health care financing continue to grow in popularity, then success will be determined by a health system’s market share and its ability to form true clinical integration. In a capitated environment, expansion of market share (especially of relatively healthy patients) will help support margins. However, financial success will come from a system’s ability to manage high-cost patients, those 5% of patients who consume 50% of health care resources.18
Hospitals with a financially challenged patient base (safety-net hospitals) will have enormous financial pressures going forward. Repeal of ACA without restoration of pre-ACA funding will affect directly the financial health of systems including AMCs. AMCs and other health systems will be forced to reduce fixed overhead, enhance productivity of faculty, and restrict nonfunded activities (teaching for example). Although most AMCs are now in an active acquisition mode, this strategy is naturally limited by the number of remaining acquisition targets. Traditional high managed care rates enjoyed by AMCs will shrink, as will federal research funding (which typically comes with high indirect financial support). Health systems and GI societies will need to dedicate much more attention to state policy makers as Trumpcare progresses.
Finally, all providers will need to manage the business implications of retail health. As people assume higher deductibles and copays and health savings accounts grow, patients will change their patterns of purchasing services. Reputation counts for less when people are facing large price differences, so attention to patient-centric amenities, price, patient engagement, and patient satisfaction will become even more important.
Conclusion
The United States has undergone a massive and rapid political transformation. The mandate felt by conservative politicians, perhaps not supported by numbers, will carry a conservative platform forward. In areas where progressive Democrats emphasized federal power and socialized regulation (religion, education, civil rights, income security, and health policy), conservatives will transfer decision power as much as possible to states, local communities, and individuals. Maintaining the concept of “health as a right” will test the conscience of all of us.
References
1. Allen, J.I. The road ahead. Clin Gastroenterol Hepatol. 2012;10:692-6.
2. Gill KE. Visual guide: the balance of power between Congress and the Presidency (1901-2016). Wired Pen. November 2016. Available from http://wiredpen.com/resources/political-commentary-and-analysis/a-visual-guide-balance-of-power-congress-presidency/. Accessed Dec. 30, 2016.
3. Mertens M. Chart: comparing health reform bills – Democrats and Republicans 2009, Republics 1993. Kaiser Health News. Feb. 24, 2010. Available from http://khn.org/022310-bill-comparison/. Accessed Jan. 8, 2017.
4. Hotchkiss M. Q&A: what a Trump presidency means for the Affordable Care Act. Nov. 16, 2016 News at Princeton. Princeton University. Available from https://www.princeton.edu/main/news/archive/S47/93/09C11/index.xml?section=topstories. Accessed Dec. 30, 2016.
5. Jost T. Taking stock of health reform: where we’ve been, where we’re going. Health Affairs Blog. Available from http://healthaffairs.org/blog/2016/12/06/taking-stock-of-health-reform-where-weve-been-where-were-going/. Accessed Dec. 30, 2016.
6. Jost T. The Republican Study Committee’s ACA replacement proposal (updated). Health Affairs Blog. Available from http://healthaffairs.org/blog/2017/01/05/the-republican-study-committees-aca-replacement-proposal/. Accessed Jan. 10, 2017.
7. Price T. Empowering patients first. Available from http://tomprice.house.gov/sites/tomprice.house.gov/files/HR%202300%20Empowering%20Patients%20First%20Act%202015.pdf. Accessed Dec. 30, 2016.
8. Ryan P. A better way. Available from https://abetterway.speaker.gov/_assets/pdf/ABetterWay-HealthCare-PolicyPaper.pdf. Accessed Dec. 30, 2016.
9. Oberlander, J. The end of Obamacare. N Engl J Med. 2017;376:1-3.
10. Goodnough A. Hospitals in safety net brace for health care law’s repeal. New York Times. Dec. 28, 2016. Available from http://www.nytimes.com/2016/12/28/health/hospitals-medicaid-obamacare-trump.html?smprod=nytcore-iphone&smid=nytcore-iphone-share&_r=0. Accessed Jan. 10, 2017.
11. Ayanian, J.Z., Ehrlich, G.M., Grimes, D.R., et al. Economic effects of Medicaid expansion in Michigan. N Engl J Med. 2017;376:407-10.
12. Obama, B.H. Repealing the ACA without a replacement: the risks to American health care. N Engl J Med. 2017;376:297-9.
13. Fuchs, V.R. Major concepts of health economics. Ann Intern Med. 2015;162:380-3.
14. Quinn, K. The 8 basic payment methods in health care. Ann Intern Med. 2015;163:300-6.
15. Schoenman JA. A detailed look at US health care spending: a presentation from the National Institute for Health Care Management (NIHCM). Oct. 25, 2012. Available from http://www.nihcm.org/images/stories/Health_care_spending_slides_-_MILI_-_Schoenman.pdf. Accessed Dec. 30, 2016.
16. Allen, J.I., Allen, C.C., Brill, J.V. Gastroenterology 2020: no time for WIMPs. Gastroenterology. 2016;150:295-9.
17. Sciacca R. Weekly Byte: GI roundtable and navigating uncharted waters in health care. The PMD Blog. Available from https://www.pmd.com/blog/post/weekly-byte-gi-roundtable-and-navigating-uncharted-waters-in-health-care. Accessed Jan. 10, 2017.
18. Powers, B.W., Chaguturu, S.K. ACOs and high-cost patients. N Engl J Med. 2016;374:203-5.
Dr. Allen is professor of medicine, University of Michigan School of Medicine, Institute for Health Care Policy and Innovations, and associate medical director of Network Strategy and Business Development – Michigan Medicine, Ann Arbor. He discloses no conflicts.
The June issue of CGH was the final column under my management. I have enjoyed the opportunity to provide you with information about practice management and health care reform. I also have enjoyed working with the Clinical Gastroenterology and Hepatology board of editors, and Erin Landis and Brook Simpson from AGA headquarters. Beginning in July 2017, this section will become the responsibility of Ziad Gellad, MD, MPH, AGAF, from Duke University. I have worked with Ziad for many years, and he serves on my board of editors for GI & Hepatology News. I have great confidence in his knowledge and ability.
During the last 5 years, we have published 58 columns beginning with an article where I made several broad predictions. I have tried to present important concepts and management tools related to private and academic clinical practice, health care reform, and health economics. This article was written in early January 2017 just before the inauguration of Donald Trump. As I wrote, we did not know the full extent or the pace of “Repeal and Replace,” as Obamacare becomes Trumpcare (www.healthaffairs.org/obamacare-to-trumpcare).
The extent of current Republican control of federal and state governments is unprecedented in modern political history. Per Newt Gingrich (The Economist, Jan. 7, 2017, p. 25), this will be the third attempt, after Ronald Reagan’s election in 1980 and Gingrich’s “Contract with America” in 1994, to break free from a “Big Government” mindset initiated by Franklin Roosevelt’s New Deal. In this article, I will speculate how a right-leaning shift in American health care policy might impact the business model of gastroenterology. No matter how government regulations or funds flow change, we (physicians) will ultimately be responsible for digestive care provided to our patients. In the words of Martin Luther King Jr. (as he paraphrased Theodore Parker), “The arc of the moral universe is long, but it bends toward justice.” What is remembered by fewer people, however, are words he then added during his speeches: “but only if we march.”
John I. Allen, MD, MBA, AGAF
Editor in Chief
The first column was published in July 2012.1 I wrote about five dominant themes that would alter our gastroenterology practices in the ensuing years. They were 1) an increasing requirement for us to demonstrate value, 2) the need to think about population management in addition to individual patient care, 3) consolidation that would occur at all levels of health care delivery, 4) increasing cost pressure, and 5) how medical decisions would be linked to reimbursement (now called value-based payment). I fully expected the Patient Protection and Affordable Care Act (ACA) would shape the health care landscape for the rest of our careers. After the article’s publication, I was invited to speak about health care reform at many academic centers and private practices. My last talk before the election was in Pasadena, Calif. (Oct. 28, 2016) where I confidently spoke about the implications of President Clinton’s cementing ACA into the fabric of U.S. medicine.
Donald Trump is now the 45th President of the United States. Republicans hold a 52-48 majority in the Senate and a 241-194 majority in the House. As of January 2017, one Supreme Court seat was available, and three more may open because of retirements (Justice Ginsburg is 83 years old, Justice Kennedy is 80, and Justice Breyer is 78). Republicans control all three branches of government in 25 states and dominate in 8 others. Conservative politicians control a large majority of county and city boards.
Until this year, Republicans have controlled all three branches of government only twice since 1945 (modern political history), and only once (George Bush in 2005) did the president have a Senate majority.2 With his win, Mr. Trump can lead a conservative revolution to reverse key initiatives begun when the Democratic Party held majority power. Repeal of the ACA, signed into legislation on March 23, 2010, is the Republican Party’s top priority.
Equally important, Congress can alter previously implemented federal regulations. Each year about 3,000 regulations are written by federal agencies that act with authority delegated by Congress (albeit Congress retains power to overturn them). Regulations are published in the Federal Register as preliminary rules during each year, and Final Rules are published after a public comment period and implemented shortly thereafter. Regulations carry the force of law and are codified in the Code of Federal Regulations. The Code of Federal Regulations is divided into 50 sections (Titles), with Title 42 (Public Health) and Title 45 (Public Welfare) most pertinent to us.
Other policies are created through executive orders, issued by the president (federal) or governors (states), without involvement of legislative or judicial branches (they were not mentioned in the Constitution, by the way). Executive orders issued by President Obama could, theoretically, be overturned by new executive orders.
Repeal and replace
Destruction of the ACA is a top priority of President Trump and Republican leaders of both houses of Congress. The ACA was a Democratic bill (passed with no Republican support), although it had many similarities to previous Republican legislative ideas dating from 1993.3
Although outright repeal could be blocked by a Democratic filibuster, the law could be drastically modified through budget reconciliation whose passage takes only a simple Senate majority. Thus, a simple budget-related bill could serve as a vehicle to defund many parts of ACA, including money for Medicaid expansion, insurance risk corridors, money to offset out-of-pocket expenses and individual premium subsidies, for example.4,5
There would be substantial problems if ACA were repealed even with a 2- or 3-year delay, a scenario proposed to provide time for a replacement bill. On Jan. 4, 2017, the House Republican Study Committee introduced the American Health Care Reform Act (AHCRA) as a replacement proposal, with the stipulation that ACA would be repealed as of Jan. 1, 2018. This initial bill hinted at Republican intent and was detailed in a Health Affairs blog.6 Importantly, there were distinct similarities between this and prior Republican proposals put forward by Representative Tom Price (nominated to head the Department of Health & Human Services under President Trump) and Speaker of the House Paul Ryan.7,8
Consistently, Republicans have advocated for expansion of health savings accounts, altering the tax code to allow individuals to deduct health insurance premiums, establishment of association risk pools, imposition of malpractice limits, protections for people with preexisting conditions, and further restrictions on abortion coverage. The AHCRA changes financial subsidies for purchasing insurance from a tax credit (which can be paid to people even if they do not pay taxes) to a tax deduction (only applicable to people who pay taxes). Analysis of a similar proposal made by President Trump during the campaign found that this plan would increase the number of uninsured people by more than 15 million.
If ACA is repealed, effects would be broader than just factors related to insurance coverage.9 ACA provides for preventive care (including colonoscopy) without copays, education of additional medical personnel, closing the donut hole for Medicare Part D (medications), approval of generic biologics, and Medicaid expansions, among other initiatives. If ACA were defunded without restoring pre-ACA support for Disproportion Share Hospital charity care, research, and graduate medical education, then safety-net hospitals and many academic medical centers (AMCs) could face enormous funding cuts.10 Defunding Medicaid expansion would adversely affect states in many ways, as pointed out by Ayanian et al.11 Medicaid expansion had broad economic impact in states that accepted federal money to expand. In Michigan for example, 30,900 jobs were added to the state in 2016 because of Medicaid expansion, with two-thirds outside of the health care industry. President Obama defined his view about the effects of ACA repeal in the New England Journal of Medicine.12
Lessons learned
Economic principles and unique characteristics of United States health care help explain why solutions to its high cost and uneven coverage are so difficult to achieve. These include higher prices for goods in the United States compared with other countries, variation in price (unrelated to quality), restraints on government price negotiations, inefficiencies due to variation in size of delivery systems, and “moral hazard” related to rich insurance coverage, which are some of the factors that doom any simple solutions. These are reviewed by Victor Fuchs13 in an excellent article in Annals of Internal Medicine. Payment methods for health care services also distort resource use and efficiencies. Understanding the eight basic payment methodologies in health care and current predictions about future health care spending will be important in shaping reimbursement policies.14,15
Disruptions in health care are unpopular and, as Uve Reinardt stated: “Our health care financing system will always remain a horrendous mess and a fountain for such dismay among the providers of health care as well as among patients.”4 Lessons to inform the next iteration of health care policy, learned from the 2009-2010 experience, might be as follows:
1. If a bill is to be passed, the president must personally lead in explaining the bill to the public in simple terms.
2. Even the threat of repeal may disrupt the current market and force insurance companies to exit quickly.
3. Coverage must be affordable to individuals, state budgets, and health care providers. Because expansion states saw positive impacts to state budgets8 and mental health and substance abuse services became part of Medicaid benefits, how will a replacement bill maintain coverage and compensate for new state moneys used now for other imperatives such as education and infrastructure?
4. Health care is like a massive cargo ship, not a sports car, so a bill to replace the ACA may take a long time (and might never be passed).
5. Health care is intensely personal, so it will always be politically charged.
Ultimately, physicians will need to make strategic guesses and rapid adjustments to sustain financial viability and provide high-value care. Strategies differ depending on your practice situation. Keep in mind the five principles listed in the opening paragraph of this article. It is likely that the most important principle to factor into your practice strategy is continuing reduction in reimbursements. No matter what model is adopted to reform the ACA, the financial pot (Medicare, Medicaid, commercial insurance, bundled payments, fee-for-service payments) will be reduced, and the number of uninsured patients will increase. How would you change your practice if Medicare was your best payer (“manage to Medicare”)?
Independent practices
Physicians in small- to medium-size independent practices continue to struggle with reducing reimbursements, reporting burdens, increasing overhead expenses, crushing regulatory requirements, and provider burnout. Trumpcare will favor small practices more than Obamacare from a policy (not necessarily a financial) perspective. Regulations on small business and reporting burdens may ease, but the move toward value-based reimbursement as outlined in the MACRA (passed with overwhelming bipartisan support) will not end.16 Practices in small communities continue to thrive because they give excellent care with limited competition and low overhead. Some practices in suburban and urban centers struggle because payers tend to favor (with enhanced managed care rates) larger practices and health systems. Large, horizontally integrated, efficient gastroenterology practices will continue to thrive because they can develop a “must-have” position with payers. Building remote patient monitoring, teleconsulting, and capabilities around value demonstration will be strategically advantageous.
Options for independent physicians include 1) maintaining status quo, 2) retiring, or 3) exiting the independent business model through a practice sale. Traditionally, physicians who wanted to sell their practices turned to hospitals or health systems. Recently, a physician-run model funded by venture capital has emerged where reduced overhead (through centralization of services) is combined with enhanced power during payer negotiations (because of scale). This model has allowed practices to merge into a physician organization and remain free from health system employment.17
Large health systems
Physicians employed by large health systems, whether they are nonprofit, for-profit, or AMCs, will see their future tied directly to health system success. If bundled payment, alternative payment, and capitation models of health care financing continue to grow in popularity, then success will be determined by a health system’s market share and its ability to form true clinical integration. In a capitated environment, expansion of market share (especially of relatively healthy patients) will help support margins. However, financial success will come from a system’s ability to manage high-cost patients, those 5% of patients who consume 50% of health care resources.18
Hospitals with a financially challenged patient base (safety-net hospitals) will have enormous financial pressures going forward. Repeal of ACA without restoration of pre-ACA funding will affect directly the financial health of systems including AMCs. AMCs and other health systems will be forced to reduce fixed overhead, enhance productivity of faculty, and restrict nonfunded activities (teaching for example). Although most AMCs are now in an active acquisition mode, this strategy is naturally limited by the number of remaining acquisition targets. Traditional high managed care rates enjoyed by AMCs will shrink, as will federal research funding (which typically comes with high indirect financial support). Health systems and GI societies will need to dedicate much more attention to state policy makers as Trumpcare progresses.
Finally, all providers will need to manage the business implications of retail health. As people assume higher deductibles and copays and health savings accounts grow, patients will change their patterns of purchasing services. Reputation counts for less when people are facing large price differences, so attention to patient-centric amenities, price, patient engagement, and patient satisfaction will become even more important.
Conclusion
The United States has undergone a massive and rapid political transformation. The mandate felt by conservative politicians, perhaps not supported by numbers, will carry a conservative platform forward. In areas where progressive Democrats emphasized federal power and socialized regulation (religion, education, civil rights, income security, and health policy), conservatives will transfer decision power as much as possible to states, local communities, and individuals. Maintaining the concept of “health as a right” will test the conscience of all of us.
References
1. Allen, J.I. The road ahead. Clin Gastroenterol Hepatol. 2012;10:692-6.
2. Gill KE. Visual guide: the balance of power between Congress and the Presidency (1901-2016). Wired Pen. November 2016. Available from http://wiredpen.com/resources/political-commentary-and-analysis/a-visual-guide-balance-of-power-congress-presidency/. Accessed Dec. 30, 2016.
3. Mertens M. Chart: comparing health reform bills – Democrats and Republicans 2009, Republics 1993. Kaiser Health News. Feb. 24, 2010. Available from http://khn.org/022310-bill-comparison/. Accessed Jan. 8, 2017.
4. Hotchkiss M. Q&A: what a Trump presidency means for the Affordable Care Act. Nov. 16, 2016 News at Princeton. Princeton University. Available from https://www.princeton.edu/main/news/archive/S47/93/09C11/index.xml?section=topstories. Accessed Dec. 30, 2016.
5. Jost T. Taking stock of health reform: where we’ve been, where we’re going. Health Affairs Blog. Available from http://healthaffairs.org/blog/2016/12/06/taking-stock-of-health-reform-where-weve-been-where-were-going/. Accessed Dec. 30, 2016.
6. Jost T. The Republican Study Committee’s ACA replacement proposal (updated). Health Affairs Blog. Available from http://healthaffairs.org/blog/2017/01/05/the-republican-study-committees-aca-replacement-proposal/. Accessed Jan. 10, 2017.
7. Price T. Empowering patients first. Available from http://tomprice.house.gov/sites/tomprice.house.gov/files/HR%202300%20Empowering%20Patients%20First%20Act%202015.pdf. Accessed Dec. 30, 2016.
8. Ryan P. A better way. Available from https://abetterway.speaker.gov/_assets/pdf/ABetterWay-HealthCare-PolicyPaper.pdf. Accessed Dec. 30, 2016.
9. Oberlander, J. The end of Obamacare. N Engl J Med. 2017;376:1-3.
10. Goodnough A. Hospitals in safety net brace for health care law’s repeal. New York Times. Dec. 28, 2016. Available from http://www.nytimes.com/2016/12/28/health/hospitals-medicaid-obamacare-trump.html?smprod=nytcore-iphone&smid=nytcore-iphone-share&_r=0. Accessed Jan. 10, 2017.
11. Ayanian, J.Z., Ehrlich, G.M., Grimes, D.R., et al. Economic effects of Medicaid expansion in Michigan. N Engl J Med. 2017;376:407-10.
12. Obama, B.H. Repealing the ACA without a replacement: the risks to American health care. N Engl J Med. 2017;376:297-9.
13. Fuchs, V.R. Major concepts of health economics. Ann Intern Med. 2015;162:380-3.
14. Quinn, K. The 8 basic payment methods in health care. Ann Intern Med. 2015;163:300-6.
15. Schoenman JA. A detailed look at US health care spending: a presentation from the National Institute for Health Care Management (NIHCM). Oct. 25, 2012. Available from http://www.nihcm.org/images/stories/Health_care_spending_slides_-_MILI_-_Schoenman.pdf. Accessed Dec. 30, 2016.
16. Allen, J.I., Allen, C.C., Brill, J.V. Gastroenterology 2020: no time for WIMPs. Gastroenterology. 2016;150:295-9.
17. Sciacca R. Weekly Byte: GI roundtable and navigating uncharted waters in health care. The PMD Blog. Available from https://www.pmd.com/blog/post/weekly-byte-gi-roundtable-and-navigating-uncharted-waters-in-health-care. Accessed Jan. 10, 2017.
18. Powers, B.W., Chaguturu, S.K. ACOs and high-cost patients. N Engl J Med. 2016;374:203-5.
Dr. Allen is professor of medicine, University of Michigan School of Medicine, Institute for Health Care Policy and Innovations, and associate medical director of Network Strategy and Business Development – Michigan Medicine, Ann Arbor. He discloses no conflicts.
AGA Strategic Plan 2015–2020: Something that matters
I’m proud to share with you the new strategic plan of the American Gastroenterological Association (AGA). Thanks to the hundreds of members who worked to ensure that the plan is responsive to the needs of thousands in the gastroenterology community and their patients.
Throughout the process of developing the strategic plan, the phrase “start something that matters1” echoed through my head. In 1897, a group of physicians started the AGA to make a difference in the lives of their colleagues and their patients. Since that time, AGA has been the driving force behind advances that matter in gastroenterology and hepatology research and practice. We have made staggering scientific discoveries and applied them to improve patient care. However, we still have so much more to learn, and that’s why the AGA Strategic Plan matters.
AGA, at our heart, is a learning organization. This new strategic plan will lead us to new discoveries in GI science, new tools to improve patient care, new ways to educate ourselves and the gastroenterologists of the future. Together we will shape a bright future for gastroenterology and our patients.
Ultimately, the AGA Strategic Plan will mobilize the resources of our organization to fulfill our mission of advancing the science and practice of gastroenterology.
Overview of the plan
Two words describe each of the 3 fundamental AGA areas as illustrated in the triangular portion of the plan (Figure 1). For example practice and quality were paired intentionally to emphasize their close connection and the AGA’s increasing commitment to increasing the “value” (defined as quality per unit cost) of our GI and liver care.
Research is critical to our advancing science, but needs to be coupled with AGA’s commitment to promote innovation in medical device and therapeutic advances, through the AGA Center for GI Innovation and Technology and the AGA Center for Diagnostics and Therapeutics.
Finally, education must be paired with training our physician and provider workforce in new and emerging technologies. The plan includes specific reference to patients. Throughout the four goals and supporting strategies, patient engagement, patient voice and patient experience all are emphasized.
AGA Strategic Plan at a glance
Practice & quality
Define optimal clinical practice and help gastroenterologists provide high-quality, high-value care.
• Within the framework of the Triple Aim, define high value care for GI disorders.
• Increase the number of gastroenterologists reporting on quality of care.
• Build and engage an active grassroots network to communicate and advise AGA of emerging practice issues and trends.
• Address evolving practice and reimbursement models in all practice settings.
Research & innovation
Foster scientific discovery and the application of new knowledge to improve care of patients with digestive disease.
• Target junior faculty engaged in research for special support.
• Increase strategic innovation and research collaborations to promote high-value clinical care.
• Support promising advances in research and innovation.
Education & training
Engage members and other GI health providers through personalized education across the continuum of their careers.
• Help members satisfy requirements for certification, recertification, continuing medical education and licensure.
• Educate members about emerging technologies, procedures and scientific discoveries to improve patient care.
• Help members and other learners develop their careers and navigate transitions.
• Use state-of-the-art and innovative technology platforms for learning.
Advocacy
Influence public policies to support quality patient care, improve the practice of gastroenterology, and advance digestive disease research and education.
• Pursue policies that ensure patients have access to appropriate, affordable, high-value GI care.
• Increase opportunities for funding digestive disease research.
• Develop a grassroots network to advocate for improvements in patient care, increased research funding and the viability of GI practice.
• Strongly advocate for sufficient federal funding of academic training programs.
Publications
Lead the GI/hepatology category of scientific journals in rank, reach and accessibility while meeting the readership needs of basic and clinical investigators, practitioners, young GIs and trainees.
• Achieve and maintain high impact factors for all journals.
• Rank highest in the field for meeting the readership needs of basic and clinical investigators, practitioners, young GIs and trainees.
• Expand journals’ reach via new content dissemination technologies.
• Increase usage of the journals’ digital platforms.
Organizational vitality
Maintain a robust and diverse membership, develop society leaders, foster strategic collaborations, and maintain an infrastructure that supports AGA mission and goals.
• Increase AGA’s membership.
• Develop a sustainable global strategy.
• Conduct leadership development and prepare members to serve in volunteer leadership positions within AGA.
• Strive for diversity at all levels within the association, including governance, committee structure, staffing and program development. Diversity is an inclusive concept that encompasses race, ethnicity, national origin, religion, gender, age, sexual orientation and disability.
The planning process
In revising the plan, AGA leadership decided to focus in some interesting and innovative ways. Before Digestive Disease Week (DDW) 2014, Anil Rustgi (immediate past president) and I appointed 4 task forces each composed of scientists, academic clinicians, community practitioners, and AGA staff. The task forces were assigned to consider 1 of 3 topics, reflected in the triangular figure of our plan (Figure 1): research and innovation, practice and quality, and education and training. We also assigned AGA leadership and staff to focus on additional AGA areas including advocacy, publications, communications and organizational vitality.
The task forces identified key goals and strategies at meetings during DDW and subsequent teleconferences. Input from more than 75 members and staff helped shape the initial plan. In July 2014, the AGA Governing Board met for a 3-day retreat during which ideas were distilled into the plan we have today.
Reference
1. Mycoskie B. Start something that matters. New York, NY: Spiegel and Grau, 2011.
Acknowledgements
Thanks to everyone who contributed to this plan and those who will use it and improve upon it in the future. We all look forward to a bright future for gastroenterology. This article appeared previously in Gastroenterology (2015;148:1053–4). The author discloses no conflicts.
I’m proud to share with you the new strategic plan of the American Gastroenterological Association (AGA). Thanks to the hundreds of members who worked to ensure that the plan is responsive to the needs of thousands in the gastroenterology community and their patients.
Throughout the process of developing the strategic plan, the phrase “start something that matters1” echoed through my head. In 1897, a group of physicians started the AGA to make a difference in the lives of their colleagues and their patients. Since that time, AGA has been the driving force behind advances that matter in gastroenterology and hepatology research and practice. We have made staggering scientific discoveries and applied them to improve patient care. However, we still have so much more to learn, and that’s why the AGA Strategic Plan matters.
AGA, at our heart, is a learning organization. This new strategic plan will lead us to new discoveries in GI science, new tools to improve patient care, new ways to educate ourselves and the gastroenterologists of the future. Together we will shape a bright future for gastroenterology and our patients.
Ultimately, the AGA Strategic Plan will mobilize the resources of our organization to fulfill our mission of advancing the science and practice of gastroenterology.
Overview of the plan
Two words describe each of the 3 fundamental AGA areas as illustrated in the triangular portion of the plan (Figure 1). For example practice and quality were paired intentionally to emphasize their close connection and the AGA’s increasing commitment to increasing the “value” (defined as quality per unit cost) of our GI and liver care.
Research is critical to our advancing science, but needs to be coupled with AGA’s commitment to promote innovation in medical device and therapeutic advances, through the AGA Center for GI Innovation and Technology and the AGA Center for Diagnostics and Therapeutics.
Finally, education must be paired with training our physician and provider workforce in new and emerging technologies. The plan includes specific reference to patients. Throughout the four goals and supporting strategies, patient engagement, patient voice and patient experience all are emphasized.
AGA Strategic Plan at a glance
Practice & quality
Define optimal clinical practice and help gastroenterologists provide high-quality, high-value care.
• Within the framework of the Triple Aim, define high value care for GI disorders.
• Increase the number of gastroenterologists reporting on quality of care.
• Build and engage an active grassroots network to communicate and advise AGA of emerging practice issues and trends.
• Address evolving practice and reimbursement models in all practice settings.
Research & innovation
Foster scientific discovery and the application of new knowledge to improve care of patients with digestive disease.
• Target junior faculty engaged in research for special support.
• Increase strategic innovation and research collaborations to promote high-value clinical care.
• Support promising advances in research and innovation.
Education & training
Engage members and other GI health providers through personalized education across the continuum of their careers.
• Help members satisfy requirements for certification, recertification, continuing medical education and licensure.
• Educate members about emerging technologies, procedures and scientific discoveries to improve patient care.
• Help members and other learners develop their careers and navigate transitions.
• Use state-of-the-art and innovative technology platforms for learning.
Advocacy
Influence public policies to support quality patient care, improve the practice of gastroenterology, and advance digestive disease research and education.
• Pursue policies that ensure patients have access to appropriate, affordable, high-value GI care.
• Increase opportunities for funding digestive disease research.
• Develop a grassroots network to advocate for improvements in patient care, increased research funding and the viability of GI practice.
• Strongly advocate for sufficient federal funding of academic training programs.
Publications
Lead the GI/hepatology category of scientific journals in rank, reach and accessibility while meeting the readership needs of basic and clinical investigators, practitioners, young GIs and trainees.
• Achieve and maintain high impact factors for all journals.
• Rank highest in the field for meeting the readership needs of basic and clinical investigators, practitioners, young GIs and trainees.
• Expand journals’ reach via new content dissemination technologies.
• Increase usage of the journals’ digital platforms.
Organizational vitality
Maintain a robust and diverse membership, develop society leaders, foster strategic collaborations, and maintain an infrastructure that supports AGA mission and goals.
• Increase AGA’s membership.
• Develop a sustainable global strategy.
• Conduct leadership development and prepare members to serve in volunteer leadership positions within AGA.
• Strive for diversity at all levels within the association, including governance, committee structure, staffing and program development. Diversity is an inclusive concept that encompasses race, ethnicity, national origin, religion, gender, age, sexual orientation and disability.
The planning process
In revising the plan, AGA leadership decided to focus in some interesting and innovative ways. Before Digestive Disease Week (DDW) 2014, Anil Rustgi (immediate past president) and I appointed 4 task forces each composed of scientists, academic clinicians, community practitioners, and AGA staff. The task forces were assigned to consider 1 of 3 topics, reflected in the triangular figure of our plan (Figure 1): research and innovation, practice and quality, and education and training. We also assigned AGA leadership and staff to focus on additional AGA areas including advocacy, publications, communications and organizational vitality.
The task forces identified key goals and strategies at meetings during DDW and subsequent teleconferences. Input from more than 75 members and staff helped shape the initial plan. In July 2014, the AGA Governing Board met for a 3-day retreat during which ideas were distilled into the plan we have today.
Reference
1. Mycoskie B. Start something that matters. New York, NY: Spiegel and Grau, 2011.
Acknowledgements
Thanks to everyone who contributed to this plan and those who will use it and improve upon it in the future. We all look forward to a bright future for gastroenterology. This article appeared previously in Gastroenterology (2015;148:1053–4). The author discloses no conflicts.
I’m proud to share with you the new strategic plan of the American Gastroenterological Association (AGA). Thanks to the hundreds of members who worked to ensure that the plan is responsive to the needs of thousands in the gastroenterology community and their patients.
Throughout the process of developing the strategic plan, the phrase “start something that matters1” echoed through my head. In 1897, a group of physicians started the AGA to make a difference in the lives of their colleagues and their patients. Since that time, AGA has been the driving force behind advances that matter in gastroenterology and hepatology research and practice. We have made staggering scientific discoveries and applied them to improve patient care. However, we still have so much more to learn, and that’s why the AGA Strategic Plan matters.
AGA, at our heart, is a learning organization. This new strategic plan will lead us to new discoveries in GI science, new tools to improve patient care, new ways to educate ourselves and the gastroenterologists of the future. Together we will shape a bright future for gastroenterology and our patients.
Ultimately, the AGA Strategic Plan will mobilize the resources of our organization to fulfill our mission of advancing the science and practice of gastroenterology.
Overview of the plan
Two words describe each of the 3 fundamental AGA areas as illustrated in the triangular portion of the plan (Figure 1). For example practice and quality were paired intentionally to emphasize their close connection and the AGA’s increasing commitment to increasing the “value” (defined as quality per unit cost) of our GI and liver care.
Research is critical to our advancing science, but needs to be coupled with AGA’s commitment to promote innovation in medical device and therapeutic advances, through the AGA Center for GI Innovation and Technology and the AGA Center for Diagnostics and Therapeutics.
Finally, education must be paired with training our physician and provider workforce in new and emerging technologies. The plan includes specific reference to patients. Throughout the four goals and supporting strategies, patient engagement, patient voice and patient experience all are emphasized.
AGA Strategic Plan at a glance
Practice & quality
Define optimal clinical practice and help gastroenterologists provide high-quality, high-value care.
• Within the framework of the Triple Aim, define high value care for GI disorders.
• Increase the number of gastroenterologists reporting on quality of care.
• Build and engage an active grassroots network to communicate and advise AGA of emerging practice issues and trends.
• Address evolving practice and reimbursement models in all practice settings.
Research & innovation
Foster scientific discovery and the application of new knowledge to improve care of patients with digestive disease.
• Target junior faculty engaged in research for special support.
• Increase strategic innovation and research collaborations to promote high-value clinical care.
• Support promising advances in research and innovation.
Education & training
Engage members and other GI health providers through personalized education across the continuum of their careers.
• Help members satisfy requirements for certification, recertification, continuing medical education and licensure.
• Educate members about emerging technologies, procedures and scientific discoveries to improve patient care.
• Help members and other learners develop their careers and navigate transitions.
• Use state-of-the-art and innovative technology platforms for learning.
Advocacy
Influence public policies to support quality patient care, improve the practice of gastroenterology, and advance digestive disease research and education.
• Pursue policies that ensure patients have access to appropriate, affordable, high-value GI care.
• Increase opportunities for funding digestive disease research.
• Develop a grassroots network to advocate for improvements in patient care, increased research funding and the viability of GI practice.
• Strongly advocate for sufficient federal funding of academic training programs.
Publications
Lead the GI/hepatology category of scientific journals in rank, reach and accessibility while meeting the readership needs of basic and clinical investigators, practitioners, young GIs and trainees.
• Achieve and maintain high impact factors for all journals.
• Rank highest in the field for meeting the readership needs of basic and clinical investigators, practitioners, young GIs and trainees.
• Expand journals’ reach via new content dissemination technologies.
• Increase usage of the journals’ digital platforms.
Organizational vitality
Maintain a robust and diverse membership, develop society leaders, foster strategic collaborations, and maintain an infrastructure that supports AGA mission and goals.
• Increase AGA’s membership.
• Develop a sustainable global strategy.
• Conduct leadership development and prepare members to serve in volunteer leadership positions within AGA.
• Strive for diversity at all levels within the association, including governance, committee structure, staffing and program development. Diversity is an inclusive concept that encompasses race, ethnicity, national origin, religion, gender, age, sexual orientation and disability.
The planning process
In revising the plan, AGA leadership decided to focus in some interesting and innovative ways. Before Digestive Disease Week (DDW) 2014, Anil Rustgi (immediate past president) and I appointed 4 task forces each composed of scientists, academic clinicians, community practitioners, and AGA staff. The task forces were assigned to consider 1 of 3 topics, reflected in the triangular figure of our plan (Figure 1): research and innovation, practice and quality, and education and training. We also assigned AGA leadership and staff to focus on additional AGA areas including advocacy, publications, communications and organizational vitality.
The task forces identified key goals and strategies at meetings during DDW and subsequent teleconferences. Input from more than 75 members and staff helped shape the initial plan. In July 2014, the AGA Governing Board met for a 3-day retreat during which ideas were distilled into the plan we have today.
Reference
1. Mycoskie B. Start something that matters. New York, NY: Spiegel and Grau, 2011.
Acknowledgements
Thanks to everyone who contributed to this plan and those who will use it and improve upon it in the future. We all look forward to a bright future for gastroenterology. This article appeared previously in Gastroenterology (2015;148:1053–4). The author discloses no conflicts.
President, AGA Institute
AGA President provides perspective on the Medicare Final Rule
CMS recently announced that they are delaying alteration of colonoscopy relative value units (RVUs) as part of the Medicare Physician Fee Schedule Final Rule for 2015, which is welcome news. More information on this decision is available in the December issue of GI & Hepatology News.
AGA believes that CMS acted in response to an intensive educational effort coordinated among multiple medical and surgical societies. Six societies involved in colonoscopy all worked together to educate CMS about the importance of maintaining fair reimbursement for a cancer prevention procedure that has helped lower the annual incidence of colon cancer by 30% over the last decade. This effort was launched last year after the announcement of the reduction in value for upper endoscopy codes in the 2014 final rule. We all understood that the entire family of endoscopy codes was to be reviewed by the AMA’s Relative Value Update Committee (RUC), with recommendations submitted to CMS for a final decision.
Through intensive work with CMS and the RUC, GI RUC/CPT representatives convinced the RUC to first focus on upper endoscopy, and then lower endoscopy codes. When the upper endoscopy codes were submitted by the RUC, we were disappointed in the interim final values, but then were further astounded by the fact that CMS rejected 78% of the RUC recommendations and further reduced upper GI endoscopy RVU levels. This was historically unprecedented. To put it in perspective, CMS accepted the RUC recommendations for nearly 90% of all other codes reviewed by the RUC for the 2014 MPFS fee schedule. It was a clear wake-up call for us to mobilize an educational campaign. We also were dismayed that the upper endoscopy codes were not published until the final rule, which was delayed in 2014 due to the government shutdown. This only allowed a month for GIs to prepare their practices for the reduced codes.
We approached several congressmen, urging them to reach out and encourage CMS to adopt a more transparent process when re-valuing significant codes such as this. This effort, which was led by Rep. Bill Cassidy (R-La.), and Sen. Kelly Ayotte (R-N.H.), garnered the support of 46 representatives in the House and 11 senators. AGA, ACG, and ASGE also arranged several meetings with CMS, including a joint meeting between our presidents (and senior staff) and Marilynn Tavenner, CMS administrator, on May 22. Ms. Tavenner was very polite and open to our urging to delay implementation of the colonoscopy code changes. The three societies also worked together to launch an intense campaign (http://www.valueofcolonoscopy.org) to educate legislators, patients, and other key stakeholders about the importance of following a fair and transparent valuation process and maintaining fair reimbursement for this life-saving procedure.
I personally am proud to have partnered with Dr. Harry Sarles, ACG president, and Dr. Colleen Schmitt, ASGE president, in jointly working on these communications. This effort was a clear demonstration of the importance of our society leadership and advocacy efforts and the power of partnership.
CMS recently announced that they are delaying alteration of colonoscopy relative value units (RVUs) as part of the Medicare Physician Fee Schedule Final Rule for 2015, which is welcome news. More information on this decision is available in the December issue of GI & Hepatology News.
AGA believes that CMS acted in response to an intensive educational effort coordinated among multiple medical and surgical societies. Six societies involved in colonoscopy all worked together to educate CMS about the importance of maintaining fair reimbursement for a cancer prevention procedure that has helped lower the annual incidence of colon cancer by 30% over the last decade. This effort was launched last year after the announcement of the reduction in value for upper endoscopy codes in the 2014 final rule. We all understood that the entire family of endoscopy codes was to be reviewed by the AMA’s Relative Value Update Committee (RUC), with recommendations submitted to CMS for a final decision.
Through intensive work with CMS and the RUC, GI RUC/CPT representatives convinced the RUC to first focus on upper endoscopy, and then lower endoscopy codes. When the upper endoscopy codes were submitted by the RUC, we were disappointed in the interim final values, but then were further astounded by the fact that CMS rejected 78% of the RUC recommendations and further reduced upper GI endoscopy RVU levels. This was historically unprecedented. To put it in perspective, CMS accepted the RUC recommendations for nearly 90% of all other codes reviewed by the RUC for the 2014 MPFS fee schedule. It was a clear wake-up call for us to mobilize an educational campaign. We also were dismayed that the upper endoscopy codes were not published until the final rule, which was delayed in 2014 due to the government shutdown. This only allowed a month for GIs to prepare their practices for the reduced codes.
We approached several congressmen, urging them to reach out and encourage CMS to adopt a more transparent process when re-valuing significant codes such as this. This effort, which was led by Rep. Bill Cassidy (R-La.), and Sen. Kelly Ayotte (R-N.H.), garnered the support of 46 representatives in the House and 11 senators. AGA, ACG, and ASGE also arranged several meetings with CMS, including a joint meeting between our presidents (and senior staff) and Marilynn Tavenner, CMS administrator, on May 22. Ms. Tavenner was very polite and open to our urging to delay implementation of the colonoscopy code changes. The three societies also worked together to launch an intense campaign (http://www.valueofcolonoscopy.org) to educate legislators, patients, and other key stakeholders about the importance of following a fair and transparent valuation process and maintaining fair reimbursement for this life-saving procedure.
I personally am proud to have partnered with Dr. Harry Sarles, ACG president, and Dr. Colleen Schmitt, ASGE president, in jointly working on these communications. This effort was a clear demonstration of the importance of our society leadership and advocacy efforts and the power of partnership.
CMS recently announced that they are delaying alteration of colonoscopy relative value units (RVUs) as part of the Medicare Physician Fee Schedule Final Rule for 2015, which is welcome news. More information on this decision is available in the December issue of GI & Hepatology News.
AGA believes that CMS acted in response to an intensive educational effort coordinated among multiple medical and surgical societies. Six societies involved in colonoscopy all worked together to educate CMS about the importance of maintaining fair reimbursement for a cancer prevention procedure that has helped lower the annual incidence of colon cancer by 30% over the last decade. This effort was launched last year after the announcement of the reduction in value for upper endoscopy codes in the 2014 final rule. We all understood that the entire family of endoscopy codes was to be reviewed by the AMA’s Relative Value Update Committee (RUC), with recommendations submitted to CMS for a final decision.
Through intensive work with CMS and the RUC, GI RUC/CPT representatives convinced the RUC to first focus on upper endoscopy, and then lower endoscopy codes. When the upper endoscopy codes were submitted by the RUC, we were disappointed in the interim final values, but then were further astounded by the fact that CMS rejected 78% of the RUC recommendations and further reduced upper GI endoscopy RVU levels. This was historically unprecedented. To put it in perspective, CMS accepted the RUC recommendations for nearly 90% of all other codes reviewed by the RUC for the 2014 MPFS fee schedule. It was a clear wake-up call for us to mobilize an educational campaign. We also were dismayed that the upper endoscopy codes were not published until the final rule, which was delayed in 2014 due to the government shutdown. This only allowed a month for GIs to prepare their practices for the reduced codes.
We approached several congressmen, urging them to reach out and encourage CMS to adopt a more transparent process when re-valuing significant codes such as this. This effort, which was led by Rep. Bill Cassidy (R-La.), and Sen. Kelly Ayotte (R-N.H.), garnered the support of 46 representatives in the House and 11 senators. AGA, ACG, and ASGE also arranged several meetings with CMS, including a joint meeting between our presidents (and senior staff) and Marilynn Tavenner, CMS administrator, on May 22. Ms. Tavenner was very polite and open to our urging to delay implementation of the colonoscopy code changes. The three societies also worked together to launch an intense campaign (http://www.valueofcolonoscopy.org) to educate legislators, patients, and other key stakeholders about the importance of following a fair and transparent valuation process and maintaining fair reimbursement for this life-saving procedure.
I personally am proud to have partnered with Dr. Harry Sarles, ACG president, and Dr. Colleen Schmitt, ASGE president, in jointly working on these communications. This effort was a clear demonstration of the importance of our society leadership and advocacy efforts and the power of partnership.
Practice-owned pathology services: Controversies and pitfalls – The use of special stains
The US Government Accountability Office (GAO) released a study on June 24, 2013, calling for "action" to address higher use of anatomic pathology services by providers who "self-refer" (i.e., those that have ownership positions in pathology labs). The report suggested that profit and not science drove utilization, including that of special stains. The relationship between luminal gastroenterology and pathology has been close since the beginning of flexible endoscopy and is inherent to excellent patient care and management.
As we began to diagnose predictive conditions (e.g., dysplasia) in addition to endpoint disease (e.g., cancer), the need for communication and closer cooperation became even more important. Endoscopists can help the pathologist with disease context and demographic information, allowing a more exact choice of histologic tools to aid diagnoses. In this article, I teamed up with a pathologist from a large independent GI group to explore these areas of potential controversy.
John I. Allen, M.D., M.B.A., AGAF, Special Section Editor
Gastroenterologists have long enjoyed a close working relationship with gastrointestinal (GI) pathologists as much of our endoscopic work is accompanied by biopsies. Excellent communication between the endoscopist and pathologist is critical for maximizing the diagnostic value of the biopsy and leads to an environment where the integrated team adds substantial value to patient health outcomes.1
During the last decade, a number of community gastroenterologists have added pathology services to their practices as the enhanced communication resulting from such integration improves patient care in both qualitative and quantitative ways. For example, reduced time from biopsy to patient reporting minimizes the patient’s anxiety as they await results. The development of special GI pathology expertise within the practice aids the gastroenterologist in his/her understanding of the pathology report.2
Business arrangements for in-house pathology vary and are beyond the scope of this article. These will be covered in subsequent publications in the Practice Management Toolbox.
The Centers for Medicaid and Medicare Services (CMS) prohibit physicians from referring patients for designated health services delivered by entities in which they or a family member have a financial relationship. These proscriptions are commonly referred to as Stark Laws. Anatomic pathology services, with Healthcare Common Procedure Coding System (HCPCS) codes in the 883xx family, are an exempted service. The primary code is 88305 and encompasses any biopsy taken by endoscopy, colonoscopy, or sigmoidoscopy. Add-on codes for additional studies are 88312, 88313, and 88342.
In June 2013, the United States Government General Accountability Office (GAO) issued a report in response to requests from several Congressmen concerning the increased use of anatomic pathology services by providers who self-refer to pathology labs owned and operated by their practices.3 The report analyzed expenditures for Medicare Part B services by using the above stated HCPCS codes from 2007 to 2011. They found an increase of 5.9% annually, and the rate of anatomic pathology billing to Medicare from dermatology, urology, and GI practices that owned pathology labs was significantly higher compared with those practices that did not self-refer. Both the rate of biopsies (related to procedures) and the numbers of special stains were higher, leading the GAO to recommend that CMS both analyze these trends directly and potentially limit such self-referral. To date, the Secretary of Health and Human Services has rejected these recommendations.
Fellowship training in GI medicine encourages GI pathology training so that the gastroenterologist can understand the language of pathology. Even with this training, pathology reports can be confusing. The pathologist also needs to understand the language of the gastroenterologist. Incorporating pathologists within the practice helps translate the esoteric language of pathology into the clinical language of the gastroenterologist.
Treating a disease at its earliest manifestation is the most effective point of intervention. Therefore, an important objective of medicine is to find disease in its nascent form or, if it is neoplastic, in its precursor form before it is capable of spreading. Pathology evolved to identify and detect these early manifestations of disease. The transformation of pathology from a specialty that confirms a diagnosis after a disease is fully manifest to a specialty that identifies a population at risk conferred an additional mandate on the pathologist so that the pathologist is called on to make a diagnosis earlier and earlier in the diagnostic cascade. The integration of both specialties into a single team maximizes communication and minimizes confusion.
The diagnostic algorithm begins with the standard stain
The diagnostic algorithm for rendering a complete surgical pathology interpretation begins with the pathologist examining the initial slide stained with H&E. This stain differentiates cytoplasmic and nuclear detail and allows a morphologic interpretation (i.e., "what does the lesion look like?"). At this level, the pathologist uses heuristic rules of thumb to make an approximate diagnosis. The experienced and well-trained pathologist knows that morphology only gives an 80%-85% confidence level in diagnosis. To achieve diagnostic accuracy and reproducibility approaching 100%, the trained pathologist is expected to triage the specimen and determine the need for any additional studies. In this modern setting, heuristic rules of thumb that are based on morphology are anachronistic, whereas establishing the correct diagnosis is paramount. This need is recognized in CMS regulation 80.6.5 that allows the pathologist to use whatever special studies are necessary as long as certain criteria are met.4
The definition of special stains
"Special stain" is an expansive term used for both chargeable and nonchargeable studies. Chargeable special studies are defined as add-on studies. In fact, the most common special study is nonchargeable and is known as leveling the block. Leveling the block obtains additional slides stained with H&E to ensure that the tissue examined on the microscope slide is fully representative of the disease process. This service is considered to be part of the H&E diagnosis and is not compensated.
In the Capital Digestive Care LLC laboratory, additional levels on the block have increased the adenoma detection rate by approximately 2% (personal observation). In cases of malignancy, Capital Digestive Care often obtains 30 additional slides to ensure complete sampling of the lesion and preservation of precious tissue in case additional studies are necessary. These studies are used to evaluate site of origin, prognostic factors such as vascular invasion, and expression of mismatched repair proteins as surrogate markers to microsatellite instability lesions and Lynch syndrome.
A common situation where a special stain is useful is in the diagnosis of Helicobacter pylori infection. The use of special stains is not unique to Helicobacter. There is a legion of other diagnoses that require special stains to reveal them, differentiate them from mimics, confirm their existence, or eliminate them as a possibility. An exhaustive listing of special stains and their uses is beyond the scope of this article. However, anexample is the use of additional studies to differentiate various forms of peripheral nerve sheath tumors, or to differentiate hyperplastic polyps from serrated polyps, or in the classification of mature B-cell lymphomas, or the use of the homeobox antigen CDX2 to identify an adenocarcinoma as being of intestinal phenotype.
In seeking to detect Barrett’s esophagus, Harrison et al.4 recommend eight separate biopsies as the best chance to come to an accurate diagnosis of intestinal metaplasia. In many cases, it is difficult for an endoscopist to retrieve eight biopsies from patients in whom Barrett’s esophagus is suspected. The conscientious pathologist will perform extensive leveling of the block and use ancillary studies such as Alcian blue to highlight rare goblet cells or differentiate pseudogoblet cells from true goblet.5
The add-on study is chargeable if reported as "negative for" or "positive for" a particular diagnosis. As an example, the ancillary study for Helicobacter is correctly interpreted as positive for Helicobacter or negative for Helicobacter. The add-on confers the ability for precise classification of disease. The positive interpretation indicates Helicobacter as an etiology, and a negative interpretation excludes Helicobacter as an etiology. Many pathologists substitute the term noncontributory for "negative for." This is incorrect. Negative information contributes to the final diagnosis because it excludes diagnostic possibilities and therefore is contributory. If the ancillary study truly does not contribute to the final diagnosis, then the noncontributory service should not have been done and is nonchargeable.
Ancillary studies increase sensitivity and specificity
Traditionally, pathologists performed a gross examination and examined large segments of tissue and sampled areas that were abnormal to sight and touch. When biopsies are obtained by endoscopy, it is the gastroenterologist who performs the gross examination during endoscopy. In this setting, the pathologist is blind to the gross appearance of the lesion. Nevertheless, the pathologist is called on to render a complete interpretation and is dependent on the eyes and hands of the gastroenterologist to procure a diagnostic sample. It is evident that in the modern setting, such a sampling is inherently limited and requires the pathologist and gastroenterologist to work as an integrated team to render a complete interpretation.
In the best of circumstances, the biopsy is small and in some cases it is an incomplete representation of a disease process. The pathologist is under considerable pressure to arrive at a correct and timely diagnosis because his or her interpretation potentially has substantial consequences to patient care. Ancillary studies or special stains enhance the ability to finesse information out of a small biopsy. The small size and incompleteness of the biopsy often result in disagreements of interpretation by pathologists. It is not uncommon for the gastroenterologist to encounter disagreements among pathologists in biopsy interpretation. Special stains often minimize disagreements because there are objective standards by which opinions become fact.
Lack of gold standard
Pathology literature often documents large interobserver variability in which two or more pathologists cannot agree on the diagnosis. There is also intraobserver variability in which the same pathologist on different days may arrive at a different conclusion. As the diagnosis moves from overt manifestation of disease to subtle alterations indicating the likelihood of disease development, this interobserver variability increases, and it is evident that the likelihood of diagnostic error increases. As the pathologist moves further up the diagnostic stream and closer to the point of disease origin, the morphologic markers are often obscure and little differentiated and require increasingly powerful tools to extract information. These tools are known as add-on or special studies.
Barrett’s esophagus is surveyed to prevent the development of esophageal adenocarcinoma. The end point of Barrett’s esophagus surveillance is the establishment of low- or high-grade dysplasia, carcinoma in situ, or invasive carcinoma because these diagnoses lead to additional therapeutic interventions. It would seem evident that a process such as dysplasia, which has been established in pathology almost since its inception, would be well defined and the criteria well delineated. However, a seminal article on Barrett’s dysplasia showed that 12 leading GI pathologists from centers of excellence in Barrett’s esophagus showed a large interobserver variability for all non–high-grade dysplasia diagnoses even after there was a consensus conference as to what morphologic changes should be categorized as dysplasia. The results showed a 90% agreement if two diagnostic categories were used (negative or high-grade dysplasia vs. high-grade dysplasia or more significant lesion) and a 75% agreement if three diagnostic categories were used (BE, negative for dysplasia, BE indefinite for dysplasia or low-grade dysplasia, and BE with high-grade dysplasia or more significant lesion).
The authors also showed a "barbell distribution" of agreement in that there was fairly good agreement at the low and high end of the spectrum (negative for dysplasia and high-grade dysplasia) and very poor agreement in the middle ground between indefinite for dysplasia and low-grade dysplasia. Even so, they never reached a level of greater than 90% agreement.5
This inherent subjectivity to morphologic analysis means there is no gold standard. If no gold standard exists, then it is evident that comparison of diagnostic acumen between pathologists and institutions is meritless. These limitations have led pathologists to test various biomarkers or ancillary studies to help and increase accuracy and precision and to render reproducible diagnoses between pathologists. It is universally accepted that high-grade dysplasia is the best predictor of progression in Barrett’s esophagus to adenocarcinoma. However, the practical application of this standard is limited by the subjective nature of the criteria for establishing high-grade dysplasia and that some reactive conditions cannot be readily distinguished from high-grade dysplasia by histological assessment alone. Therefore, pathologists use biomarkers to distinguish dysplasia from its histological mimics and to help and grade the level of dysplasia.6
The problem of interobserver variability is not limited to Barrett’s esophagus but extends to colon cancer screening. For colon cancer screening, risk stratification is based on the size and morphology of the lesion. The gastroenterologist determines the size of the lesion at colonoscopy, and the pathologist then defines the morphology. There is no consensus among pathologists as to what constitutes high-grade dysplasia and villous morphology, and the endoscopic estimate of polyp size is unreliable.7,8
The reason for errors and disagreement is the inherently subjective nature of pathology. The best way to resolve this dilemma is to bring more objective standards to bear and to establish a gold standard. One way of objectifying a subjective interpretation is to submit it to a binary "yes"/"no" test. This is the role of add-on studies.
Liability
The pathologist is a physician subject to litigation as are all health care providers. The pathologist’s clinical counterpart shares the burden of the missed pathologic diagnosis. The use of ancillary studies increases the likelihood of a correct diagnosis and minimizes the likelihood of the missed or wrong diagnosis.
Conclusion
In the end, the eye sees what the mind knows, but what the mind knows and the eye sees are highly variable among many pathologists; and in some cases the result is a nonreproducible diagnosis. Clearly, this is not an acceptable state. If a diagnosis cannot be reproducibly rendered between pathologists in the same institution or between collaborative institutions, any study that relies on such diagnosis is inherently flawed. The pathologist, the clinician, and the patient should expect and demand the "right" or at least the "best" answer. However, this lack of reproducibility means that the patient who has their slides sent to a large number of institutions seeking the "right diagnosis" is on a fool’s errand. The objective information bought by ancillary studies achieves this goal in some cases. The failure to use ancillary studies fully may do the patient and the clinical community a gross disservice.
The GAO report showing possible overuse related to conflict of interest has initiated considerable interest, scrutiny, and conversation in Congress and CMS.1
Recent reductions in the reimbursement for 88305 have tempered the need for further cost reductions (at the expense of pathologists and owners of laboratory services), but we can expect Congress to revisit this issue in the future. Our best defense for preservation of this Stark exemption is to practice evidence-based medicine where we can defend our decisions on the basis of patient needs and improved health outcomes.
References
1. Snover, D.C. Maximizing the value of the endoscopist-pathologist partnership in the management of colorectal polyps and carcinoma. Gastrointest. Endosc. Clin. N. Am. 2010;20:641-57.
2. Sarles, H. Gastrointestinal pathology: incorporating a GI pathology laboratory into your practice. Gastroenterol. Endoscopy News. 2011;June:1-4.
3. GAO 13-445 Medicare and Self-Referral of Anatomic Pathology Services. 2013. Available at: www.gao.gov/products/gao-13-445. Accessed September 22, 2013.
4. Harrison, R., Perry, I., Haddadin, W. et al. Detection of intestinal metaplasia in Barrett’s esophagus: an observational comparator study suggests the need for a minimum of eight biopsies. Am. J. Gastroenterol. 2007;102:1154-61.
5. Montgomery, E. Reproducibility of the diagnosis of dysplasia in Barrett esophagus: a reaffirmation. Hum. Pathol. 2001;32:368-78.
6. Fels, Elliott D.R. and Fitzgerald, R.C. Molecular markers for Barrett’s esophagus and its progression to cancer. Curr. Opin. Gastroenterol. 2013;29:437-45.
7. Mahajan, D., Downs-Kelly, E., Liu, X. et al. Reproducibility of the villous component and high grade dysplasia in colorectal adenomas < 1 cm. Am. J. Surg. Pathol. 2013;37:427-33.
8. Eichenseer, P.J. Endoscopic miss-sizing of polyps changes colorectal cancer surveillance recommendations. Dis. Colon Rectum 2013;56:315-21.
Dr. Baybick is medical director of Capital Digestive Care, LLC, Laboratory Division, Bowie, Md.; Dr. Allen is professor of medicine, and clinical chief of gastroenterology and hepatology at the Yale School of Medicine, New Haven, Conn. The authors disclose no conflicts of interest.
Content from this column was originally published in the "Practice Management: The Road Ahead" section of Clinical Gastroenterology and Hepatology (2014;12:3-6).
"Practice Management Toolbox" provides key information and resources necessary for facing the unique challenges of today’s clinical practices.
Resources for Practical Application: To view additional online resources about this topic and to access our Coding Corner, visit, www.cghjournal.org/content/practice_management.
The US Government Accountability Office (GAO) released a study on June 24, 2013, calling for "action" to address higher use of anatomic pathology services by providers who "self-refer" (i.e., those that have ownership positions in pathology labs). The report suggested that profit and not science drove utilization, including that of special stains. The relationship between luminal gastroenterology and pathology has been close since the beginning of flexible endoscopy and is inherent to excellent patient care and management.
As we began to diagnose predictive conditions (e.g., dysplasia) in addition to endpoint disease (e.g., cancer), the need for communication and closer cooperation became even more important. Endoscopists can help the pathologist with disease context and demographic information, allowing a more exact choice of histologic tools to aid diagnoses. In this article, I teamed up with a pathologist from a large independent GI group to explore these areas of potential controversy.
John I. Allen, M.D., M.B.A., AGAF, Special Section Editor
Gastroenterologists have long enjoyed a close working relationship with gastrointestinal (GI) pathologists as much of our endoscopic work is accompanied by biopsies. Excellent communication between the endoscopist and pathologist is critical for maximizing the diagnostic value of the biopsy and leads to an environment where the integrated team adds substantial value to patient health outcomes.1
During the last decade, a number of community gastroenterologists have added pathology services to their practices as the enhanced communication resulting from such integration improves patient care in both qualitative and quantitative ways. For example, reduced time from biopsy to patient reporting minimizes the patient’s anxiety as they await results. The development of special GI pathology expertise within the practice aids the gastroenterologist in his/her understanding of the pathology report.2
Business arrangements for in-house pathology vary and are beyond the scope of this article. These will be covered in subsequent publications in the Practice Management Toolbox.
The Centers for Medicaid and Medicare Services (CMS) prohibit physicians from referring patients for designated health services delivered by entities in which they or a family member have a financial relationship. These proscriptions are commonly referred to as Stark Laws. Anatomic pathology services, with Healthcare Common Procedure Coding System (HCPCS) codes in the 883xx family, are an exempted service. The primary code is 88305 and encompasses any biopsy taken by endoscopy, colonoscopy, or sigmoidoscopy. Add-on codes for additional studies are 88312, 88313, and 88342.
In June 2013, the United States Government General Accountability Office (GAO) issued a report in response to requests from several Congressmen concerning the increased use of anatomic pathology services by providers who self-refer to pathology labs owned and operated by their practices.3 The report analyzed expenditures for Medicare Part B services by using the above stated HCPCS codes from 2007 to 2011. They found an increase of 5.9% annually, and the rate of anatomic pathology billing to Medicare from dermatology, urology, and GI practices that owned pathology labs was significantly higher compared with those practices that did not self-refer. Both the rate of biopsies (related to procedures) and the numbers of special stains were higher, leading the GAO to recommend that CMS both analyze these trends directly and potentially limit such self-referral. To date, the Secretary of Health and Human Services has rejected these recommendations.
Fellowship training in GI medicine encourages GI pathology training so that the gastroenterologist can understand the language of pathology. Even with this training, pathology reports can be confusing. The pathologist also needs to understand the language of the gastroenterologist. Incorporating pathologists within the practice helps translate the esoteric language of pathology into the clinical language of the gastroenterologist.
Treating a disease at its earliest manifestation is the most effective point of intervention. Therefore, an important objective of medicine is to find disease in its nascent form or, if it is neoplastic, in its precursor form before it is capable of spreading. Pathology evolved to identify and detect these early manifestations of disease. The transformation of pathology from a specialty that confirms a diagnosis after a disease is fully manifest to a specialty that identifies a population at risk conferred an additional mandate on the pathologist so that the pathologist is called on to make a diagnosis earlier and earlier in the diagnostic cascade. The integration of both specialties into a single team maximizes communication and minimizes confusion.
The diagnostic algorithm begins with the standard stain
The diagnostic algorithm for rendering a complete surgical pathology interpretation begins with the pathologist examining the initial slide stained with H&E. This stain differentiates cytoplasmic and nuclear detail and allows a morphologic interpretation (i.e., "what does the lesion look like?"). At this level, the pathologist uses heuristic rules of thumb to make an approximate diagnosis. The experienced and well-trained pathologist knows that morphology only gives an 80%-85% confidence level in diagnosis. To achieve diagnostic accuracy and reproducibility approaching 100%, the trained pathologist is expected to triage the specimen and determine the need for any additional studies. In this modern setting, heuristic rules of thumb that are based on morphology are anachronistic, whereas establishing the correct diagnosis is paramount. This need is recognized in CMS regulation 80.6.5 that allows the pathologist to use whatever special studies are necessary as long as certain criteria are met.4
The definition of special stains
"Special stain" is an expansive term used for both chargeable and nonchargeable studies. Chargeable special studies are defined as add-on studies. In fact, the most common special study is nonchargeable and is known as leveling the block. Leveling the block obtains additional slides stained with H&E to ensure that the tissue examined on the microscope slide is fully representative of the disease process. This service is considered to be part of the H&E diagnosis and is not compensated.
In the Capital Digestive Care LLC laboratory, additional levels on the block have increased the adenoma detection rate by approximately 2% (personal observation). In cases of malignancy, Capital Digestive Care often obtains 30 additional slides to ensure complete sampling of the lesion and preservation of precious tissue in case additional studies are necessary. These studies are used to evaluate site of origin, prognostic factors such as vascular invasion, and expression of mismatched repair proteins as surrogate markers to microsatellite instability lesions and Lynch syndrome.
A common situation where a special stain is useful is in the diagnosis of Helicobacter pylori infection. The use of special stains is not unique to Helicobacter. There is a legion of other diagnoses that require special stains to reveal them, differentiate them from mimics, confirm their existence, or eliminate them as a possibility. An exhaustive listing of special stains and their uses is beyond the scope of this article. However, anexample is the use of additional studies to differentiate various forms of peripheral nerve sheath tumors, or to differentiate hyperplastic polyps from serrated polyps, or in the classification of mature B-cell lymphomas, or the use of the homeobox antigen CDX2 to identify an adenocarcinoma as being of intestinal phenotype.
In seeking to detect Barrett’s esophagus, Harrison et al.4 recommend eight separate biopsies as the best chance to come to an accurate diagnosis of intestinal metaplasia. In many cases, it is difficult for an endoscopist to retrieve eight biopsies from patients in whom Barrett’s esophagus is suspected. The conscientious pathologist will perform extensive leveling of the block and use ancillary studies such as Alcian blue to highlight rare goblet cells or differentiate pseudogoblet cells from true goblet.5
The add-on study is chargeable if reported as "negative for" or "positive for" a particular diagnosis. As an example, the ancillary study for Helicobacter is correctly interpreted as positive for Helicobacter or negative for Helicobacter. The add-on confers the ability for precise classification of disease. The positive interpretation indicates Helicobacter as an etiology, and a negative interpretation excludes Helicobacter as an etiology. Many pathologists substitute the term noncontributory for "negative for." This is incorrect. Negative information contributes to the final diagnosis because it excludes diagnostic possibilities and therefore is contributory. If the ancillary study truly does not contribute to the final diagnosis, then the noncontributory service should not have been done and is nonchargeable.
Ancillary studies increase sensitivity and specificity
Traditionally, pathologists performed a gross examination and examined large segments of tissue and sampled areas that were abnormal to sight and touch. When biopsies are obtained by endoscopy, it is the gastroenterologist who performs the gross examination during endoscopy. In this setting, the pathologist is blind to the gross appearance of the lesion. Nevertheless, the pathologist is called on to render a complete interpretation and is dependent on the eyes and hands of the gastroenterologist to procure a diagnostic sample. It is evident that in the modern setting, such a sampling is inherently limited and requires the pathologist and gastroenterologist to work as an integrated team to render a complete interpretation.
In the best of circumstances, the biopsy is small and in some cases it is an incomplete representation of a disease process. The pathologist is under considerable pressure to arrive at a correct and timely diagnosis because his or her interpretation potentially has substantial consequences to patient care. Ancillary studies or special stains enhance the ability to finesse information out of a small biopsy. The small size and incompleteness of the biopsy often result in disagreements of interpretation by pathologists. It is not uncommon for the gastroenterologist to encounter disagreements among pathologists in biopsy interpretation. Special stains often minimize disagreements because there are objective standards by which opinions become fact.
Lack of gold standard
Pathology literature often documents large interobserver variability in which two or more pathologists cannot agree on the diagnosis. There is also intraobserver variability in which the same pathologist on different days may arrive at a different conclusion. As the diagnosis moves from overt manifestation of disease to subtle alterations indicating the likelihood of disease development, this interobserver variability increases, and it is evident that the likelihood of diagnostic error increases. As the pathologist moves further up the diagnostic stream and closer to the point of disease origin, the morphologic markers are often obscure and little differentiated and require increasingly powerful tools to extract information. These tools are known as add-on or special studies.
Barrett’s esophagus is surveyed to prevent the development of esophageal adenocarcinoma. The end point of Barrett’s esophagus surveillance is the establishment of low- or high-grade dysplasia, carcinoma in situ, or invasive carcinoma because these diagnoses lead to additional therapeutic interventions. It would seem evident that a process such as dysplasia, which has been established in pathology almost since its inception, would be well defined and the criteria well delineated. However, a seminal article on Barrett’s dysplasia showed that 12 leading GI pathologists from centers of excellence in Barrett’s esophagus showed a large interobserver variability for all non–high-grade dysplasia diagnoses even after there was a consensus conference as to what morphologic changes should be categorized as dysplasia. The results showed a 90% agreement if two diagnostic categories were used (negative or high-grade dysplasia vs. high-grade dysplasia or more significant lesion) and a 75% agreement if three diagnostic categories were used (BE, negative for dysplasia, BE indefinite for dysplasia or low-grade dysplasia, and BE with high-grade dysplasia or more significant lesion).
The authors also showed a "barbell distribution" of agreement in that there was fairly good agreement at the low and high end of the spectrum (negative for dysplasia and high-grade dysplasia) and very poor agreement in the middle ground between indefinite for dysplasia and low-grade dysplasia. Even so, they never reached a level of greater than 90% agreement.5
This inherent subjectivity to morphologic analysis means there is no gold standard. If no gold standard exists, then it is evident that comparison of diagnostic acumen between pathologists and institutions is meritless. These limitations have led pathologists to test various biomarkers or ancillary studies to help and increase accuracy and precision and to render reproducible diagnoses between pathologists. It is universally accepted that high-grade dysplasia is the best predictor of progression in Barrett’s esophagus to adenocarcinoma. However, the practical application of this standard is limited by the subjective nature of the criteria for establishing high-grade dysplasia and that some reactive conditions cannot be readily distinguished from high-grade dysplasia by histological assessment alone. Therefore, pathologists use biomarkers to distinguish dysplasia from its histological mimics and to help and grade the level of dysplasia.6
The problem of interobserver variability is not limited to Barrett’s esophagus but extends to colon cancer screening. For colon cancer screening, risk stratification is based on the size and morphology of the lesion. The gastroenterologist determines the size of the lesion at colonoscopy, and the pathologist then defines the morphology. There is no consensus among pathologists as to what constitutes high-grade dysplasia and villous morphology, and the endoscopic estimate of polyp size is unreliable.7,8
The reason for errors and disagreement is the inherently subjective nature of pathology. The best way to resolve this dilemma is to bring more objective standards to bear and to establish a gold standard. One way of objectifying a subjective interpretation is to submit it to a binary "yes"/"no" test. This is the role of add-on studies.
Liability
The pathologist is a physician subject to litigation as are all health care providers. The pathologist’s clinical counterpart shares the burden of the missed pathologic diagnosis. The use of ancillary studies increases the likelihood of a correct diagnosis and minimizes the likelihood of the missed or wrong diagnosis.
Conclusion
In the end, the eye sees what the mind knows, but what the mind knows and the eye sees are highly variable among many pathologists; and in some cases the result is a nonreproducible diagnosis. Clearly, this is not an acceptable state. If a diagnosis cannot be reproducibly rendered between pathologists in the same institution or between collaborative institutions, any study that relies on such diagnosis is inherently flawed. The pathologist, the clinician, and the patient should expect and demand the "right" or at least the "best" answer. However, this lack of reproducibility means that the patient who has their slides sent to a large number of institutions seeking the "right diagnosis" is on a fool’s errand. The objective information bought by ancillary studies achieves this goal in some cases. The failure to use ancillary studies fully may do the patient and the clinical community a gross disservice.
The GAO report showing possible overuse related to conflict of interest has initiated considerable interest, scrutiny, and conversation in Congress and CMS.1
Recent reductions in the reimbursement for 88305 have tempered the need for further cost reductions (at the expense of pathologists and owners of laboratory services), but we can expect Congress to revisit this issue in the future. Our best defense for preservation of this Stark exemption is to practice evidence-based medicine where we can defend our decisions on the basis of patient needs and improved health outcomes.
References
1. Snover, D.C. Maximizing the value of the endoscopist-pathologist partnership in the management of colorectal polyps and carcinoma. Gastrointest. Endosc. Clin. N. Am. 2010;20:641-57.
2. Sarles, H. Gastrointestinal pathology: incorporating a GI pathology laboratory into your practice. Gastroenterol. Endoscopy News. 2011;June:1-4.
3. GAO 13-445 Medicare and Self-Referral of Anatomic Pathology Services. 2013. Available at: www.gao.gov/products/gao-13-445. Accessed September 22, 2013.
4. Harrison, R., Perry, I., Haddadin, W. et al. Detection of intestinal metaplasia in Barrett’s esophagus: an observational comparator study suggests the need for a minimum of eight biopsies. Am. J. Gastroenterol. 2007;102:1154-61.
5. Montgomery, E. Reproducibility of the diagnosis of dysplasia in Barrett esophagus: a reaffirmation. Hum. Pathol. 2001;32:368-78.
6. Fels, Elliott D.R. and Fitzgerald, R.C. Molecular markers for Barrett’s esophagus and its progression to cancer. Curr. Opin. Gastroenterol. 2013;29:437-45.
7. Mahajan, D., Downs-Kelly, E., Liu, X. et al. Reproducibility of the villous component and high grade dysplasia in colorectal adenomas < 1 cm. Am. J. Surg. Pathol. 2013;37:427-33.
8. Eichenseer, P.J. Endoscopic miss-sizing of polyps changes colorectal cancer surveillance recommendations. Dis. Colon Rectum 2013;56:315-21.
Dr. Baybick is medical director of Capital Digestive Care, LLC, Laboratory Division, Bowie, Md.; Dr. Allen is professor of medicine, and clinical chief of gastroenterology and hepatology at the Yale School of Medicine, New Haven, Conn. The authors disclose no conflicts of interest.
Content from this column was originally published in the "Practice Management: The Road Ahead" section of Clinical Gastroenterology and Hepatology (2014;12:3-6).
"Practice Management Toolbox" provides key information and resources necessary for facing the unique challenges of today’s clinical practices.
Resources for Practical Application: To view additional online resources about this topic and to access our Coding Corner, visit, www.cghjournal.org/content/practice_management.
The US Government Accountability Office (GAO) released a study on June 24, 2013, calling for "action" to address higher use of anatomic pathology services by providers who "self-refer" (i.e., those that have ownership positions in pathology labs). The report suggested that profit and not science drove utilization, including that of special stains. The relationship between luminal gastroenterology and pathology has been close since the beginning of flexible endoscopy and is inherent to excellent patient care and management.
As we began to diagnose predictive conditions (e.g., dysplasia) in addition to endpoint disease (e.g., cancer), the need for communication and closer cooperation became even more important. Endoscopists can help the pathologist with disease context and demographic information, allowing a more exact choice of histologic tools to aid diagnoses. In this article, I teamed up with a pathologist from a large independent GI group to explore these areas of potential controversy.
John I. Allen, M.D., M.B.A., AGAF, Special Section Editor
Gastroenterologists have long enjoyed a close working relationship with gastrointestinal (GI) pathologists as much of our endoscopic work is accompanied by biopsies. Excellent communication between the endoscopist and pathologist is critical for maximizing the diagnostic value of the biopsy and leads to an environment where the integrated team adds substantial value to patient health outcomes.1
During the last decade, a number of community gastroenterologists have added pathology services to their practices as the enhanced communication resulting from such integration improves patient care in both qualitative and quantitative ways. For example, reduced time from biopsy to patient reporting minimizes the patient’s anxiety as they await results. The development of special GI pathology expertise within the practice aids the gastroenterologist in his/her understanding of the pathology report.2
Business arrangements for in-house pathology vary and are beyond the scope of this article. These will be covered in subsequent publications in the Practice Management Toolbox.
The Centers for Medicaid and Medicare Services (CMS) prohibit physicians from referring patients for designated health services delivered by entities in which they or a family member have a financial relationship. These proscriptions are commonly referred to as Stark Laws. Anatomic pathology services, with Healthcare Common Procedure Coding System (HCPCS) codes in the 883xx family, are an exempted service. The primary code is 88305 and encompasses any biopsy taken by endoscopy, colonoscopy, or sigmoidoscopy. Add-on codes for additional studies are 88312, 88313, and 88342.
In June 2013, the United States Government General Accountability Office (GAO) issued a report in response to requests from several Congressmen concerning the increased use of anatomic pathology services by providers who self-refer to pathology labs owned and operated by their practices.3 The report analyzed expenditures for Medicare Part B services by using the above stated HCPCS codes from 2007 to 2011. They found an increase of 5.9% annually, and the rate of anatomic pathology billing to Medicare from dermatology, urology, and GI practices that owned pathology labs was significantly higher compared with those practices that did not self-refer. Both the rate of biopsies (related to procedures) and the numbers of special stains were higher, leading the GAO to recommend that CMS both analyze these trends directly and potentially limit such self-referral. To date, the Secretary of Health and Human Services has rejected these recommendations.
Fellowship training in GI medicine encourages GI pathology training so that the gastroenterologist can understand the language of pathology. Even with this training, pathology reports can be confusing. The pathologist also needs to understand the language of the gastroenterologist. Incorporating pathologists within the practice helps translate the esoteric language of pathology into the clinical language of the gastroenterologist.
Treating a disease at its earliest manifestation is the most effective point of intervention. Therefore, an important objective of medicine is to find disease in its nascent form or, if it is neoplastic, in its precursor form before it is capable of spreading. Pathology evolved to identify and detect these early manifestations of disease. The transformation of pathology from a specialty that confirms a diagnosis after a disease is fully manifest to a specialty that identifies a population at risk conferred an additional mandate on the pathologist so that the pathologist is called on to make a diagnosis earlier and earlier in the diagnostic cascade. The integration of both specialties into a single team maximizes communication and minimizes confusion.
The diagnostic algorithm begins with the standard stain
The diagnostic algorithm for rendering a complete surgical pathology interpretation begins with the pathologist examining the initial slide stained with H&E. This stain differentiates cytoplasmic and nuclear detail and allows a morphologic interpretation (i.e., "what does the lesion look like?"). At this level, the pathologist uses heuristic rules of thumb to make an approximate diagnosis. The experienced and well-trained pathologist knows that morphology only gives an 80%-85% confidence level in diagnosis. To achieve diagnostic accuracy and reproducibility approaching 100%, the trained pathologist is expected to triage the specimen and determine the need for any additional studies. In this modern setting, heuristic rules of thumb that are based on morphology are anachronistic, whereas establishing the correct diagnosis is paramount. This need is recognized in CMS regulation 80.6.5 that allows the pathologist to use whatever special studies are necessary as long as certain criteria are met.4
The definition of special stains
"Special stain" is an expansive term used for both chargeable and nonchargeable studies. Chargeable special studies are defined as add-on studies. In fact, the most common special study is nonchargeable and is known as leveling the block. Leveling the block obtains additional slides stained with H&E to ensure that the tissue examined on the microscope slide is fully representative of the disease process. This service is considered to be part of the H&E diagnosis and is not compensated.
In the Capital Digestive Care LLC laboratory, additional levels on the block have increased the adenoma detection rate by approximately 2% (personal observation). In cases of malignancy, Capital Digestive Care often obtains 30 additional slides to ensure complete sampling of the lesion and preservation of precious tissue in case additional studies are necessary. These studies are used to evaluate site of origin, prognostic factors such as vascular invasion, and expression of mismatched repair proteins as surrogate markers to microsatellite instability lesions and Lynch syndrome.
A common situation where a special stain is useful is in the diagnosis of Helicobacter pylori infection. The use of special stains is not unique to Helicobacter. There is a legion of other diagnoses that require special stains to reveal them, differentiate them from mimics, confirm their existence, or eliminate them as a possibility. An exhaustive listing of special stains and their uses is beyond the scope of this article. However, anexample is the use of additional studies to differentiate various forms of peripheral nerve sheath tumors, or to differentiate hyperplastic polyps from serrated polyps, or in the classification of mature B-cell lymphomas, or the use of the homeobox antigen CDX2 to identify an adenocarcinoma as being of intestinal phenotype.
In seeking to detect Barrett’s esophagus, Harrison et al.4 recommend eight separate biopsies as the best chance to come to an accurate diagnosis of intestinal metaplasia. In many cases, it is difficult for an endoscopist to retrieve eight biopsies from patients in whom Barrett’s esophagus is suspected. The conscientious pathologist will perform extensive leveling of the block and use ancillary studies such as Alcian blue to highlight rare goblet cells or differentiate pseudogoblet cells from true goblet.5
The add-on study is chargeable if reported as "negative for" or "positive for" a particular diagnosis. As an example, the ancillary study for Helicobacter is correctly interpreted as positive for Helicobacter or negative for Helicobacter. The add-on confers the ability for precise classification of disease. The positive interpretation indicates Helicobacter as an etiology, and a negative interpretation excludes Helicobacter as an etiology. Many pathologists substitute the term noncontributory for "negative for." This is incorrect. Negative information contributes to the final diagnosis because it excludes diagnostic possibilities and therefore is contributory. If the ancillary study truly does not contribute to the final diagnosis, then the noncontributory service should not have been done and is nonchargeable.
Ancillary studies increase sensitivity and specificity
Traditionally, pathologists performed a gross examination and examined large segments of tissue and sampled areas that were abnormal to sight and touch. When biopsies are obtained by endoscopy, it is the gastroenterologist who performs the gross examination during endoscopy. In this setting, the pathologist is blind to the gross appearance of the lesion. Nevertheless, the pathologist is called on to render a complete interpretation and is dependent on the eyes and hands of the gastroenterologist to procure a diagnostic sample. It is evident that in the modern setting, such a sampling is inherently limited and requires the pathologist and gastroenterologist to work as an integrated team to render a complete interpretation.
In the best of circumstances, the biopsy is small and in some cases it is an incomplete representation of a disease process. The pathologist is under considerable pressure to arrive at a correct and timely diagnosis because his or her interpretation potentially has substantial consequences to patient care. Ancillary studies or special stains enhance the ability to finesse information out of a small biopsy. The small size and incompleteness of the biopsy often result in disagreements of interpretation by pathologists. It is not uncommon for the gastroenterologist to encounter disagreements among pathologists in biopsy interpretation. Special stains often minimize disagreements because there are objective standards by which opinions become fact.
Lack of gold standard
Pathology literature often documents large interobserver variability in which two or more pathologists cannot agree on the diagnosis. There is also intraobserver variability in which the same pathologist on different days may arrive at a different conclusion. As the diagnosis moves from overt manifestation of disease to subtle alterations indicating the likelihood of disease development, this interobserver variability increases, and it is evident that the likelihood of diagnostic error increases. As the pathologist moves further up the diagnostic stream and closer to the point of disease origin, the morphologic markers are often obscure and little differentiated and require increasingly powerful tools to extract information. These tools are known as add-on or special studies.
Barrett’s esophagus is surveyed to prevent the development of esophageal adenocarcinoma. The end point of Barrett’s esophagus surveillance is the establishment of low- or high-grade dysplasia, carcinoma in situ, or invasive carcinoma because these diagnoses lead to additional therapeutic interventions. It would seem evident that a process such as dysplasia, which has been established in pathology almost since its inception, would be well defined and the criteria well delineated. However, a seminal article on Barrett’s dysplasia showed that 12 leading GI pathologists from centers of excellence in Barrett’s esophagus showed a large interobserver variability for all non–high-grade dysplasia diagnoses even after there was a consensus conference as to what morphologic changes should be categorized as dysplasia. The results showed a 90% agreement if two diagnostic categories were used (negative or high-grade dysplasia vs. high-grade dysplasia or more significant lesion) and a 75% agreement if three diagnostic categories were used (BE, negative for dysplasia, BE indefinite for dysplasia or low-grade dysplasia, and BE with high-grade dysplasia or more significant lesion).
The authors also showed a "barbell distribution" of agreement in that there was fairly good agreement at the low and high end of the spectrum (negative for dysplasia and high-grade dysplasia) and very poor agreement in the middle ground between indefinite for dysplasia and low-grade dysplasia. Even so, they never reached a level of greater than 90% agreement.5
This inherent subjectivity to morphologic analysis means there is no gold standard. If no gold standard exists, then it is evident that comparison of diagnostic acumen between pathologists and institutions is meritless. These limitations have led pathologists to test various biomarkers or ancillary studies to help and increase accuracy and precision and to render reproducible diagnoses between pathologists. It is universally accepted that high-grade dysplasia is the best predictor of progression in Barrett’s esophagus to adenocarcinoma. However, the practical application of this standard is limited by the subjective nature of the criteria for establishing high-grade dysplasia and that some reactive conditions cannot be readily distinguished from high-grade dysplasia by histological assessment alone. Therefore, pathologists use biomarkers to distinguish dysplasia from its histological mimics and to help and grade the level of dysplasia.6
The problem of interobserver variability is not limited to Barrett’s esophagus but extends to colon cancer screening. For colon cancer screening, risk stratification is based on the size and morphology of the lesion. The gastroenterologist determines the size of the lesion at colonoscopy, and the pathologist then defines the morphology. There is no consensus among pathologists as to what constitutes high-grade dysplasia and villous morphology, and the endoscopic estimate of polyp size is unreliable.7,8
The reason for errors and disagreement is the inherently subjective nature of pathology. The best way to resolve this dilemma is to bring more objective standards to bear and to establish a gold standard. One way of objectifying a subjective interpretation is to submit it to a binary "yes"/"no" test. This is the role of add-on studies.
Liability
The pathologist is a physician subject to litigation as are all health care providers. The pathologist’s clinical counterpart shares the burden of the missed pathologic diagnosis. The use of ancillary studies increases the likelihood of a correct diagnosis and minimizes the likelihood of the missed or wrong diagnosis.
Conclusion
In the end, the eye sees what the mind knows, but what the mind knows and the eye sees are highly variable among many pathologists; and in some cases the result is a nonreproducible diagnosis. Clearly, this is not an acceptable state. If a diagnosis cannot be reproducibly rendered between pathologists in the same institution or between collaborative institutions, any study that relies on such diagnosis is inherently flawed. The pathologist, the clinician, and the patient should expect and demand the "right" or at least the "best" answer. However, this lack of reproducibility means that the patient who has their slides sent to a large number of institutions seeking the "right diagnosis" is on a fool’s errand. The objective information bought by ancillary studies achieves this goal in some cases. The failure to use ancillary studies fully may do the patient and the clinical community a gross disservice.
The GAO report showing possible overuse related to conflict of interest has initiated considerable interest, scrutiny, and conversation in Congress and CMS.1
Recent reductions in the reimbursement for 88305 have tempered the need for further cost reductions (at the expense of pathologists and owners of laboratory services), but we can expect Congress to revisit this issue in the future. Our best defense for preservation of this Stark exemption is to practice evidence-based medicine where we can defend our decisions on the basis of patient needs and improved health outcomes.
References
1. Snover, D.C. Maximizing the value of the endoscopist-pathologist partnership in the management of colorectal polyps and carcinoma. Gastrointest. Endosc. Clin. N. Am. 2010;20:641-57.
2. Sarles, H. Gastrointestinal pathology: incorporating a GI pathology laboratory into your practice. Gastroenterol. Endoscopy News. 2011;June:1-4.
3. GAO 13-445 Medicare and Self-Referral of Anatomic Pathology Services. 2013. Available at: www.gao.gov/products/gao-13-445. Accessed September 22, 2013.
4. Harrison, R., Perry, I., Haddadin, W. et al. Detection of intestinal metaplasia in Barrett’s esophagus: an observational comparator study suggests the need for a minimum of eight biopsies. Am. J. Gastroenterol. 2007;102:1154-61.
5. Montgomery, E. Reproducibility of the diagnosis of dysplasia in Barrett esophagus: a reaffirmation. Hum. Pathol. 2001;32:368-78.
6. Fels, Elliott D.R. and Fitzgerald, R.C. Molecular markers for Barrett’s esophagus and its progression to cancer. Curr. Opin. Gastroenterol. 2013;29:437-45.
7. Mahajan, D., Downs-Kelly, E., Liu, X. et al. Reproducibility of the villous component and high grade dysplasia in colorectal adenomas < 1 cm. Am. J. Surg. Pathol. 2013;37:427-33.
8. Eichenseer, P.J. Endoscopic miss-sizing of polyps changes colorectal cancer surveillance recommendations. Dis. Colon Rectum 2013;56:315-21.
Dr. Baybick is medical director of Capital Digestive Care, LLC, Laboratory Division, Bowie, Md.; Dr. Allen is professor of medicine, and clinical chief of gastroenterology and hepatology at the Yale School of Medicine, New Haven, Conn. The authors disclose no conflicts of interest.
Content from this column was originally published in the "Practice Management: The Road Ahead" section of Clinical Gastroenterology and Hepatology (2014;12:3-6).
"Practice Management Toolbox" provides key information and resources necessary for facing the unique challenges of today’s clinical practices.
Resources for Practical Application: To view additional online resources about this topic and to access our Coding Corner, visit, www.cghjournal.org/content/practice_management.










