User login
The current state of antiplatelet therapy in acute coronary syndromes: The data and the real world
The final event leading to acute coronary syndromes (ACS) is spontaneous atherosclerotic plaque rupture. This event is analogous to the plaque rupture caused by percutaneous coronary intervention (PCI). Both events initiate a platelet response that starts with the adhesion of platelets to the vessel wall, followed by the activation and then aggregation of platelets.
The clinical consequences of intravascular platelet activation and aggregation are well known: death, myocardial infarction (MI), myocardial ischemia, and arrhythmias. In terms of health care burden, ACS is the primary or secondary diagnosis in 1.57 million hospitalizations annually in the United States—specifically, unstable angina or MI without ST-segment elevation in 1.24 million hospitalizations, and MI with ST-segment elevation in 330,000 hospitalizations.1
This real-world impact of ACS is tempered by the real-world use and effectiveness of our antiplatelet drug therapies, which is the focus of this article. I begin with a brief review of the evidence surrounding three major antiplatelet therapies used in ACS management—aspirin, clopidogrel, and the glycoprotein IIb/IIIa inhibitors. I then review the updated evidence-based guidelines for the use of antiplatelet therapies in ACS. I conclude with an overview of how US hospitals are actually using these therapies, with a focus on two particularly important challenges—bleeding risk and appropriate dosing—and on initiatives under way to bridge the gap between recommended antiplatelet therapy for ACS and actual clinical practice.
ANTIPLATELET THERAPY IN ACUTE CORONARY SYNDROMES
Aspirin
Although aspirin has long been the bedrock of antiplatelet therapy in patients with ACS, its effects on the heart are still being elucidated. Several placebo-controlled trials of aspirin, each with relatively few subjects, have been conducted in the setting of ACS without ST-segment elevation.2–5 Although confidence intervals were wide, these studies showed a favorable effect of aspirin relative to placebo on the risk of death and nonfatal MI.
Clopidogrel and dual antiplatelet therapy
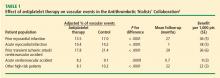
CURE trial: prevention of recurrent events in patients with ACS. Dual antiplatelet therapy with the thienopyridine agent clopidogrel plus aspirin was investigated in patients presenting with ACS without ST-segment elevation in the landmark CURE trial (Clopidogrel in Unstable Angina to Prevent Recurrent Events).7 This study randomized 12,562 patients presenting within 24 hours of ACS symptom onset to either clopidogrel or placebo, in addition to aspirin, for 3 to 12 months. Clopidogrel was administered as a loading dose of 300 mg followed by a maintenance dosage of 75 mg/day. Randomization to clopidogrel was associated with a highly significant 20% relative reduction in the primary end point, a composite of cardiovascular death, MI, or stroke at 12 months (9.3% incidence with clopidogrel vs 11.4% with placebo; P = .00009). Despite this impressive reduction in ischemic events with clopidogrel, the cumulative event rate continued to increase over the course of the 12-month trial in both study arms. This persistent recurrence of ischemic and thrombotic events has been observed in all antiplatelet trials to date, in spite of the addition of more potent antiplatelet regimens.
Two subanalyses of the CURE results yielded further insights. One analysis examined the timing of benefit from clopidogrel, finding that benefit emerged within 24 hours of treatment and continued consistently throughout the study’s follow-up period (mean of 9 months), supporting the notion of both early and late benefit from more potent antiplatelet therapy in ACS.8 A separate subgroup analysis found that the efficacy advantage of clopidogrel plus aspirin over aspirin alone was similar regardless of whether patients were managed medically or underwent revascularization (PCI or coronary artery bypass graft surgery [CABG]).9
CHARISMA trial: prevention of events in a broad at-risk population. Several years before the CURE trial, clopidogrel was initially evaluated as monotherapy in patients with prior ischemic events in the large randomized trial known as CAPRIE (Clopidogrel Versus Aspirin in Patients at Risk of Ischemic Events), in which aspirin was the comparator.10 Rates of the primary end point—a composite of vascular death, MI, or stroke—over a mean follow-up of 1.9 years were 5.3% in patients assigned to clopidogrel versus 5.8% in those assigned to aspirin, a relative reduction of 8.7% in favor of clopidogrel (P = .043).
The CAPRIE study set the stage for CHARISMA (Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance), which set out to determine whether dual antiplatelet therapy with clopidogrel plus aspirin conferred benefit over aspirin alone in a broad population of patients at high risk for atherothrombotic events.11 No significant additive benefit was observed with dual antiplatelet therapy in the overall CHARISMA population in terms of the composite end point of MI, stroke, or cardiovascular death over the median follow-up of 27.6 months.11
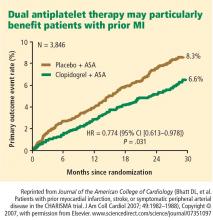
The investigators then analyzed outcomes in a large subgroup of the CHARISMA population—the 9,478 patients who had established vascular disease, ie, prior MI, stroke, or symptomatic peripheral arterial disease.12 Rates of the composite end point (MI, stroke, or cardiovascular death) in this subgroup were 7.3% with clopidogrel plus aspirin versus 8.8% with aspirin alone, representing a 1.5% absolute reduction and a 17% relative reduction with dual antiplatelet therapy (P = .01). The CHARISMA investigators concluded that there appears to be a gradient of benefit from dual antiplatelet therapy depending on the patient’s risk of thrombotic events.
Importance of longer-term therapy. Similarly, additional recent data indicate that interrupting clopidogrel therapy leads to an abrupt increase in risk among patients who experienced ACS months beforehand. Analysis of a large registry of medically treated patients and revascularized patients with ACS showed a clustering of adverse cardiovascular events in the first 90 days after clopidogrel discontinuation, an increase that was particularly pronounced in the medically treated patients.13 Like the findings from the CHARISMA subanalysis above, these data suggest that continuing clopidogrel therapy beyond 1 year may be beneficial, although the ideal duration of therapy and the patient groups most likely to benefit requires further study.
Glycoprotein IIb/IIIa inhibitors
The glycoprotein IIb/IIIa inhibitors—abciximab, eptifibatide, and tirofiban—are parenteral drugs that block the final common pathway of platelet aggregation. With increased focus on the upstream inhibition of platelet activation and the wider availability of more potent oral antiplatelet drugs, the use of glycoprotein IIb/IIIa inhibitors has been declining in recent years.
Efficacy in ACS. A number of placebo-controlled trials of glycoprotein IIb/IIIa inhibitors have been conducted in the setting of ACS without ST-segment elevation. In each trial, the glycoprotein IIb/IIIa inhibitor was associated with a significant reduction in 30-day rates of a composite of death and nonfatal MI. A 2002 pooled analysis of these trials demonstrated an overall 8% relative risk reduction in this end point with active glycoprotein IIb/IIIa inhibitor therapy (P = .037).14 Interpreting the benefit of glycoprotein IIb/IIIa blockade in the setting of clopidogrel therapy, however, is more challenging since upstream use of clopidogrel was rare at the time these studies were performed.
An outlier in the aforementioned pooled analysis was the GUSTO IV-ACS study (Global Utilization of Strategies to open Occluded coronary arteries trial IV in Acute Coronary Syndromes), in which abciximab showed no significant benefit over placebo on the primary end point of death or MI at 30 days.15 This study included 7,800 patients with ACS without ST-segment elevation who were being treated with aspirin and unfractionated or low-molecular-weight heparin and were then randomized to placebo or abciximab. Abciximab was given as a front-loaded bolus followed by an infusion lasting either 24 or 48 hours.
A trend toward higher all-cause mortality was observed with longer infusions of abciximab in the GUSTO IV-ACS trial.15 A hypothesis emerged that a front-loaded regimen of abciximab is suitable for patients undergoing PCI, in whom platelet activation and the risk of adverse outcomes is greatest in the catheterization laboratory, but is less well suited for medically managed patients, in whom levels of platelet aggregation and risk are ongoing.
Timing of treatment. The optimal timing of glycoprotein IIb/IIIa inhibitor initiation remains controversial. Boersma et al pooled data from three randomized placebo-controlled trials and stratified the results into outcomes before PCI and outcomes immediately following PCI.16 Glycoprotein IIb/IIIa inhibition was associated with a 34% relative reduction in the risk of death or MI during 72 hours of medical management prior to PCI (P = .001) and an enhanced 41% relative reduction in this end point in the 48 hours following PCI when PCI was performed during administration of the study drug (P = .001). The investigators concluded that glycoprotein IIb/IIIa blockade should be initiated early after hospital admission and continued until after PCI in patients who undergo the procedure.
The effect of upstream glycoprotein IIb/IIIa inhibitor use was more ambiguous in the recent Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) trial of patients with ACS being managed invasively. At 1 year, upstream use—as compared with in-lab use—of glycoprotein IIb/IIIa inhibitors was associated with a reduction in the rate of ischemic events among patients treated with the direct thrombin inhibitor bivalirudin (17.4% vs 21.5%, respectively; P < .01) but not among patients treated with unfractionated heparin or low-molecular-weight heparin (17.2% vs 18.4%; P = .44).17
Ongoing clinical trial results may shed further light on the considerable clinical uncertainty that remains regarding the benefits of upstream glycoprotein IIb/IIIa inhibitor use in patients with ACS.
Enrollment has just been completed in a large randomized trial designed to prospectively assess the optimal timing of glycoprotein IIb/IIIa inhibitor initiation in patients with high-risk ACS without ST-segment elevation in whom an invasive strategy is planned no sooner than the next calendar day.18 The study, known as EARLY-ACS, is randomizing patients to eptifibatide or placebo begun within 8 hours of hospital arrival, with provisional eptifibatide available in the catheterization laboratory. The primary end point is a 96-hour composite of all-cause mortality, nonfatal MI, recurrent ischemia requiring urgent revascularization, or need for thrombotic bailout with a glycoprotein IIb/IIIa inhibitor during PCI. Data should be available in 2009.
ANTIPLATELET THERAPY GUIDELINES IN NON-ST-ELEVATION ACUTE CORONARY SYNDROMES
In 2007, the American College of Cardiology (ACC) and American Heart Association (AHA) updated their joint guidelines for the use of antiplatelet therapy in the management of patients with unstable angina or MI without ST-segment elevation.19 These guidelines incorporate a large degree of flexibility in the choice of antiplatelet therapy, which can make implementation of their recommendations challenging.
The guidelines contain classes of recommendations based on the magnitude of benefit (I, IIa, IIb, III) and levels of evidence (A, B, C). Following here are key recommendations from the updated guidelines (bulleted and in italics, with the class and level of the recommendation noted in parentheses),19 supplemented with additional commentary where appropriate.
Antiplatelet therapy: General recommendations
- Aspirin should be given to all patients as soon as possible after presentation and continued indefinitely in patients not known to be intolerant of aspirin (class I, level A).
- Clopidogrel should be given to patients unable to take aspirin because of hypersensitivity or major gastrointestinal (GI) intolerance (class I, level A).
This recommendation is based on data from the CURE trial7 and the earlier CAPRIE study.10 The clopidogrel regimen recommended is a 300-mg loading dose followed by a maintenance dosage of 75 mg/day. The incidence of aspirin intolerance is approximately 5%, depending on how intolerance is defined. A significant proportion of patients will stop aspirin because of GI upset or trivial bleeding, failing to understand the true benefits of aspirin. A much smaller subset—perhaps 1 in 1,000—has a true allergy to aspirin.
- Patients with a history of GI bleeding with the use of either aspirin or clopidogrel should be prescribed a proton pump inhibitor or another drug that has been shown to minimize the risk of bleeding (class I, level B).
Initial invasive strategy
- For patients in whom an early invasive strategy is planned, therapy with either clopidogrel or a glycoprotein IIb/IIIa inhibitor should be started upstream (before diagnostic angiography) in addition to aspirin (class I, level A).
This recommendation does not give preference to either agent because head-to-head comparisons of antiplatelet and antithrombotic therapies in this setting are not available.
- Unless PCI is planned very shortly after presentation, either eptifibatide or tirofiban should be the glycoprotein IIb/IIIa inhibitor of choice; if there is no appreciable delay to angiography and PCI is planned, abciximab is indicated (class I, level B).
This recommendation is based on findings of the GUSTO IV-ACS study.15
- When an initial invasive strategy is selected, initiating therapy with both clopidogrel and a glycoprotein IIb/IIIa inhibitor is reasonable (class IIa, level B).
Clearly, the guidelines offer some leeway to allow for different practice patterns in the use of an initial invasive strategy. In my practice, if a patient is high risk and has a low likelihood of early CABG, I use both clopidogrel and a glycoprotein IIb/IIIa inhibitor upstream (prior to going to the catheterization laboratory). If a patient has a reasonable likelihood of requiring CABG, I eliminate the thienopyridine and treat with a glycoprotein IIb/IIIa inhibitor. If a patient is at increased risk of bleeding, I forgo the glycoprotein IIb/IIIa inhibitor in favor of clopidogrel.
- In patients who are going to the catheterization laboratory, omitting a glycoprotein IIb/IIIa inhibitor upstream is reasonable if a loading dose of clopidogrel was given and the use of bivalirudin is planned (class IIa, level B).
This recommendation takes into account the duration of clopidogrel’s antiplatelet effect and recognizes the likely limited benefit of glycoprotein IIb/IIIa inhibitors in patients who proceed rapidly to the catheterization laboratory.
Initial conservative strategy
- In patients being managed conservatively (ie, noninvasively), clopidogrel should be given as a loading dose of at least 300 mg followed by a maintenance dosage of at least 75 mg/day, in addition to aspirin and anticoagulant therapy as soon as possible, and continued for at least 1 month (class I, level A) and, ideally, up to 1 year (class I, level B).
- If patients who undergo an initial conservative management strategy have recurrent symptoms/ischemia, or if heart failure or serious arrhythmias develop, diagnostic angiography is recommended (class I, level A). Either a glycoprotein IIb/IIIa inhibitor (class I, level A) or clopidogrel (class I, level A) should be added to aspirin and anticoagulant therapy upstream (before angiography) in these patients (class I, level C).
- Patients classified as low risk based on stress testing should continue aspirin indefinitely (class I, level A). Clopidogrel should be continued for at least 1 month (class I, level A) and, ideally, up to 1 year (class I, level B). If a glycoprotein IIb/IIIa inhibitor had been started previously, it should be discontinued (class I, level A).
- Patients with coronary artery disease confirmed by angiography in whom a medical management strategy (rather than PCI) is selected should be continued on aspirin indefinitely (class I, level A). If clopidogrel has not already been started, a loading dose should be given (class I, level A). If started previously, glycoprotein IIb/IIIa inhibitor therapy should be discontinued (class I, level B).
- For patients managed medically without stenting, 75 to 162 mg/day of aspirin should be prescribed indefinitely (class I, level A), along with 75 mg/day of clopidogrel for at least 1 month (class I, level A) and, ideally, for up to 1 year (class I, level B).
Antiplatelet guidelines for stenting
Antiplatelet therapy is more complicated in the setting of stenting.
- For patients in whom bare metal stents are implanted, aspirin should be prescribed at a dosage of 162 to 325 mg/day for at least 1 month (class I, level B) and then continued indefinitely at 75 to 162 mg/day (class I, level A). In addition, 75 mg/day of clopidogrel should be continued for at least 1 month and, ideally, up to 1 year unless the patient is at increased risk of bleeding (in which case it should be given for at least 2 weeks) (class I, level B).
- For patients receiving drug-eluting stents, aspirin is recommended at a dosage of 162 to 325 mg/day for at least 3 months in those with a sirolimus-eluting stent and at least 6 months in those with a paclitaxel-eluting stent, after which it should be continued indefinitely at 75 to 162 mg/day (class I, level B). In addition, clopidogrel 75 mg/day is recommended for at least 12 months regardless of the type of drug-eluting stent (class I, level B).
No mention is made of dual antiplatelet therapy beyond 1 year.
At my institution, Duke University Medical Center, patients are assessed carefully for their ability and willingness to adhere to extended antiplatelet therapy before drug-eluting stents are implanted. This assessment includes an evaluation of their insurance status, their history of adherence to other prescribed drug regimens, their education level, and the dispenser of their medications.
No guidance on concomitant anticoagulation
One omission in the current ACC/AHA guidelines is the lack of guidance for patients who require concomitant antiplatelet therapy and anticoagulation. Such guidance is needed, as many patients with ACS also have indications for long-term anticoagulation, such as atrial fibrillation or valvular heart disease requiring prosthetic valves. The ACC/AHA guidelines recommend simply that anticoagulation be added to patients’ antiplatelet regimens.
HOW ARE WE DOING? APPLICATION OF GUIDELINES IN PRACTICE
No discussion of guidelines is complete without consideration of their implementation. Those interested in the use of antiplatelet therapy in ACS are fortunate to have the Acute Coronary Treatment and Intervention Outcomes Network (ACTION) Registry, a collaborative voluntary surveillance system launched in January 2007 to assess patient characteristics, treatment, and short-term outcomes in patients with ACS (MI with and without ST-segment elevation). In addition to the registry, ACTION offers guidance on measuring ACS outcomes and establishing programs for implementing evidence-based guideline recommendations in clinical practice, improving the quality and safety of ACS care, and potentially investigating novel quality-improvement methods.20
Findings from ACTION’s first 12 months
In its first 12 months (January–December 2007), the ACTION Registry captured data from 31,036 ACS cases from several hundred US hospitals, according to the ACTION National Cardiovascular Data Registry Annual Report (personal communication from Matthew T. Roe, MD, September 2008). Data were collected at two time points: acutely (during the first 24 hours after presentation) and at hospital discharge. One caveat to interpreting data from the ACTION Registry is the voluntary and retrospective reporting system on which it relies.
Intervention rates. Among patients with non-ST-segment MI in whom catheterization was not contraindicated, 85% underwent catheterization and 70% did so within 48 hours of presentation; 53% underwent PCI and 45% did so within 48 hours of presentation; and 13% underwent CABG. The median time to catheterization was 21 hours, and the median time to PCI was 19 hours.
Although many patients who go to the catheterization laboratory are managed invasively, many do not undergo PCI and are managed medically or with CABG following coronary angiography. The message, therefore, is that local practice patterns should be taken into consideration when results from clinical trials are applied to clinical practice.
Acute antiplatelet therapy. The 2007 ACTION Registry data showed that aspirin was used acutely (< 24 hours) in almost all patients in whom it was not contraindicated (97%), clopidogrel was used in 59%, and glycoprotein IIb/IIIa inhibitors were used in 44%. Given the ACC/AHA guidelines’ strong endorsement (class I, level A) of clopidogrel in this setting, one would expect wider use of clopidogrel in this context. Moreover, this relatively low rate of clopidogrel use (59%) cannot be explained by use of glycoprotein IIb/IIIa inhibitors instead, since this rate comprises patients who received clopidogrel either with or without a concomitant glycoprotein IIb/IIIa inhibitor; only 12% of patients received a glycoprotein IIb/IIIa inhibitor without clopidogrel. In contrast, a full 28% of patients received neither clopidogrel nor a glycoprotein IIb/IIIa inhibitor, contrary to current ACC/AHA guideline recommendations.
Antiplatelet therapy at discharge. At discharge, 97% of ACTION Registry patients were being treated with aspirin and 73% with clopidogrel. Notably, the use of clopidogrel at discharge was highly correlated with overall management strategy: whereas it was used in 97% of patients undergoing PCI, it was used in only 53% of patients being managed medically and in 31% of those undergoing CABG. These findings are somewhat reassuring since they generally mirror the strength of evidence supporting clopidogrel use in these different settings.
IMPORTANT REAL-WORLD CONSIDERATIONS: BLEEDING AND DOSING
Do not neglect bleeding risk
As antiplatelet therapy becomes more potent in an effort to reduce ischemic events, bleeding risk has become a concern. Major bleeding events occur in more than 10% of patients with ACS receiving antiplatelet therapy,21 although lower rates have been reported in clinical trials in which carefully selected populations are enrolled.7,14,22–24
Major bleeding affects overall outcomes. Major bleeding has clinical significance. The Global Registry of Acute Coronary Events (GRACE), which analyzed data from 24,000 patients with ACS, revealed that major bleeding was associated with significantly worse outcomes: rates of in-hospital death were three times as high—15.3% versus 5.3%—in patients who had major bleeding episodes compared with those who did not (odds ratio = 1.64 [95% CI, 1.18–2.28]).25 The relationship between bleeding and adverse overall outcomes is not fully understood but is nevertheless real and has been observed in multiple databases.
Risk factors for bleeding mirror those for ischemic events. Models are currently being developed to predict bleeding. Unfortunately, the factors that predict bleeding tend to also predict recurrent ischemic events. As a result, patients who stand to benefit most from antithrombotic therapies also are at the greatest risk of bleeding from those therapies.
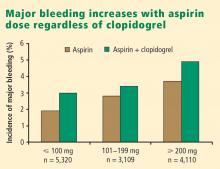
Additive risk from dual antiplatelet therapy. The additional bleeding risk from adding clopidogrel to aspirin is often not fully appreciated. In the CURE trial, the absolute excess risk of major bleeding by adding clopidogrel to aspirin was 1% (3.7% vs 2.7%), which translates to a 35% relative increase compared with aspirin alone.7 In that trial, major bleeding was most prevalent in patients undergoing CABG, and the rate of major bleeding was increased by more than 50% in patients receiving dual antiplatelet therapy when clopidogrel was discontinued 5 days or less before CABG (compared with CABG patients randomized to aspirin alone). This prompted the recommendation that clopidogrel be discontinued more than 5 days prior to CABG.
Similarly, the CHARISMA trial, which used the GUSTO scale for bleeding classification, revealed a significant excess of moderate bleeding with the combination of clopidogrel and aspirin relative to aspirin alone (2.1% vs 1.3%; P < .001) and a nonsignificant trend toward an excess of GUSTO-defined severe bleeding.11
Dosing: Time to end ‘one size fits all’ approach
Dosing of antiplatelet therapies has traditionally been a “one size fits all” strategy, but the importance of tailored therapy and dosing is starting to be realized.
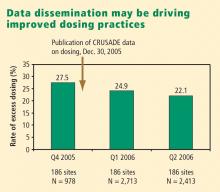
Excess dosing of glycoprotein IIb/IIIa inhibitors is common, dangerous. As an example, the CRUSADE initiative, an ongoing national database of patients with high-risk ACS without ST-segment elevation, showed that 27% of patients treated with glycoprotein IIb/IIIa inhibitors at 400 participating US hospitals in 2004 were overdosed, based on dose-adjustment recommendations in the medications’ package inserts.27 Patients who received excessive doses were significantly more likely to suffer major bleeding than were those who were dosed correctly (odds ratio = 1.46 [95% CI, 1.22–1.73]), an increased risk that was particularly pronounced in women.
Quality-improvement initiatives. The above-mentioned CRUSADE initiative, which was launched in 2001 and involves hundreds of participating US hospitals, has served as a road map for improving dosing practices in antithrombotic therapy. Like the newer ACTION Registry,20 CRUSADE issued performance report cards to its participating hospitals in which antithrombotic medication use over the prior 12 months was compared with each institution’s past performance and with data from similar hospitals across the nation.
SUMMARY AND CONCLUSIONS
Managing antiplatelet therapy for patients with ACS is complex, given the array of medications available and the various combinations in which they can be used. Therapy is likely to become even more complicated, as several new medications are under review by the US Food and Drug Administration or in phase 3 clinical trials.
Current antiplatelet therapy for patients with ACS is suboptimal. Ischemic event recurrence rates continue to rise despite the use of current antiplatelet therapies, bleeding remains an underappreciated risk, and dosing often varies from evidence-based recommendations. Developing prospective strategies for antiplatelet therapy will improve utilization in keeping with a more evidence-based approach. Current ACC/AHA guidelines are the beginning of a roadmap to optimal use of antiplatelet drugs, and quality-improvement initiatives linked to national registries like ACTION promise even more guidance toward optimal therapy through institution-specific benchmarking and performance reports.
Thus far, more effective antiplatelet therapy has led to a greater risk of bleeding. Emerging novel antiplatelet agents and smarter use of existing therapies have the potential to improve both ischemic and bleeding outcomes.
- Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics—2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2007; 115:e69–e171.
- Cairns JA, Gent M, Singer J, et al. Aspirin, sulfinpyrazone, or both in unstable angina: results of a Canadian multicenter trial. N Engl J Med 1985; 313:1369–1375.
- Lewis HD Jr, Davis JW, Archibald DG, et al. Protective effects of aspirin against acute myocardial infarction and death in men with unstable angina: results of a Veterans Administration Cooperative Study. N Engl J Med 1983; 309:396–403.
- Théroux P, Ouimet H, McCans J, et al. Aspirin, heparin, or both to treat acute unstable angina. N Engl J Med 1988; 319:1105–1111.
- Wallentin LC. Aspirin (75 mg/day) after an episode of unstable coronary artery disease: long-term effects on the risk for myocardial infarction, occurrence of severe angina and the need for revascularization: Research Group on Instability in Coronary Artery Disease in Southeast Sweden. J Am Coll Cardiol 1991; 18:1587–1593.
- Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomized trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002; 324:71–86.
- Yusuf S, Zhao F, Mehta SR, et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 2001; 345:494–502.
- Yusuf S, Mehta SR, Zhao F, et al. Early and late effects of clopidogrel in patients with acute coronary syndromes. Circulation 2003; 107:966–972.
- Fox KA, Mehta SR, Peters R, et al. Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non-ST-elevation acute coronary syndrome: the Clopidogrel in Unstable angina to prevent Recurrent ischemic Events (CURE) Trial. Circulation 2004; 110:1202–1208.
- CAPRIE Steering Committee. A randomized, blinded trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet 1996; 348:1329–1339.
- Bhatt DL, Fox KA, Hacke W, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med 2006; 354:1706–1717.
- Bhatt DL, Flather MD, Hacke W, et al. Patients with prior myocardial infarction, stroke, or symptomatic peripheral arterial disease in the CHARISMA trial. J Am Coll Cardiol 2007; 49:1982–1988.
- Ho PM, Peterson ED, Wang L, et al. Incidence of death and acute myocardial infarction associated with stopping clopidogrel after acute coronary syndrome. JAMA 2008; 299:532–539.
- Boersma E, Harrington RA, Moliterno DJ, et al. Platelet glycoprotein IIb/IIIa inhibitors in acute coronary syndromes: a meta-analysis of all major randomised clinical trials. Lancet 2002; 359:189–198.
- Simoons ML, GUSTO IV-ACS Investigators. Effect of glycoprotein IIb/IIIa receptor blocker abciximab on outcome in patients with acute coronary syndromes without early coronary revascularisation: the GUSTO IV-ACS randomised trial. Lancet 2001; 357:1915–1924.
- Boersma E, Akkerhuis KM, Théroux P, Calif RM, Topol EJ, Simoons ML. Platelet glycoprotein IIb/IIIa receptor inhibition in non-ST-elevation acute coronary syndromes: early benefit during medical treatment only, with additional protection during percutaneous coronary intervention. Circulation 1999; 100:2045–2048.
- White HD, Ohman EM, Lincoff AM, et al. Safety and efficacy of bivalirudin with and without glycoprotein IIb/IIIa inhibitors in patients with acute coronary syndromes undergoing percutaneous coronary intervention. J Am Coll Cardiol 2008; 52:807–814.
- EARLY-ACS: glycoprotein IIb/IIIa inhibition in patients with non-ST-segment elevation acute coronary syndrome. Clinical Trials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00089895. Updated December 17, 2008. Accessed December 18, 2008.
- Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2007; 50:e1–e157.
- ACTION Registry–GWTG. National Cardiovascular Data Registry Web site. http://www.ncdr.com/WebNCDR/Action/default.aspx. Accessed December 22, 2008.
- Alexander KP, Chen AY, Roe MT, et al. Excess dosing of antiplatelet and antithrombin agents in the treatment of non-ST-segment elevation acute coronary syndromes. JAMA 2005; 294:3108–3116.
- Cohen M, Demers C, Gurfinkel EP, et al. A comparison of low-molecular-weight heparin with unfractionated heparin for unstable coronary artery disease: Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q-Wave Coronary Events Study Group. N Engl J Med 1997; 337:447–452.
- Petersen JL, Mahaffey KW, Hasselblad V, et al. Efficacy and bleeding complications among patients randomized to enoxaparin or unfractionated heparin for antithrombin therapy in non-ST-segment elevation acute coronary syndromes: a systematic overview. JAMA 2004; 292:89–96.
- The PURSUIT Trial Investigators. Inhibition of platelet glycoprotein IIb/IIIa with eptifibatide in patients with acute coronary syndromes. N Engl J Med 1998; 339:436–443.
- Moscucci M, Fox KA, Cannon CP, et al. Predictors of major bleeding in acute coronary syndromes: the Global Registry of Acute Coronary Events (GRACE). Eur Heart J 2003; 24:1815–1823.
- Peters RJ, Mehta SR, Fox KA, et al. Effects of aspirin dose when used alone or in combination with clopidogrel in patients with acute coronary syndromes: observations from the Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) study. Circulation 2003; 108:1682–1687.
- Alexander KP, Chen AY, Newby LK, et al. Sex differences in major bleeding with glycoprotein IIb/IIIa inhibitors: results from the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines) initiative. Circulation 2006; 114:1380–1387.
- Alexander KP, Chen AY, Roe MT, et al. Excess dosing of antiplatelet and antithrombin agents in the treatment of non-ST-segment elevation acute coronary syndromes. JAMA 2005; 294:3108–3116.
- Alexander KP, Chen AY, Roe MT, et al. Decline in GP 2b3a inhibitor overdosing with site-specific feedback in CRUSADE [AHA abstract 3527]. Circulation 2007; 116:II_798–II_799.
The final event leading to acute coronary syndromes (ACS) is spontaneous atherosclerotic plaque rupture. This event is analogous to the plaque rupture caused by percutaneous coronary intervention (PCI). Both events initiate a platelet response that starts with the adhesion of platelets to the vessel wall, followed by the activation and then aggregation of platelets.
The clinical consequences of intravascular platelet activation and aggregation are well known: death, myocardial infarction (MI), myocardial ischemia, and arrhythmias. In terms of health care burden, ACS is the primary or secondary diagnosis in 1.57 million hospitalizations annually in the United States—specifically, unstable angina or MI without ST-segment elevation in 1.24 million hospitalizations, and MI with ST-segment elevation in 330,000 hospitalizations.1
This real-world impact of ACS is tempered by the real-world use and effectiveness of our antiplatelet drug therapies, which is the focus of this article. I begin with a brief review of the evidence surrounding three major antiplatelet therapies used in ACS management—aspirin, clopidogrel, and the glycoprotein IIb/IIIa inhibitors. I then review the updated evidence-based guidelines for the use of antiplatelet therapies in ACS. I conclude with an overview of how US hospitals are actually using these therapies, with a focus on two particularly important challenges—bleeding risk and appropriate dosing—and on initiatives under way to bridge the gap between recommended antiplatelet therapy for ACS and actual clinical practice.
ANTIPLATELET THERAPY IN ACUTE CORONARY SYNDROMES
Aspirin
Although aspirin has long been the bedrock of antiplatelet therapy in patients with ACS, its effects on the heart are still being elucidated. Several placebo-controlled trials of aspirin, each with relatively few subjects, have been conducted in the setting of ACS without ST-segment elevation.2–5 Although confidence intervals were wide, these studies showed a favorable effect of aspirin relative to placebo on the risk of death and nonfatal MI.
Clopidogrel and dual antiplatelet therapy
CURE trial: prevention of recurrent events in patients with ACS. Dual antiplatelet therapy with the thienopyridine agent clopidogrel plus aspirin was investigated in patients presenting with ACS without ST-segment elevation in the landmark CURE trial (Clopidogrel in Unstable Angina to Prevent Recurrent Events).7 This study randomized 12,562 patients presenting within 24 hours of ACS symptom onset to either clopidogrel or placebo, in addition to aspirin, for 3 to 12 months. Clopidogrel was administered as a loading dose of 300 mg followed by a maintenance dosage of 75 mg/day. Randomization to clopidogrel was associated with a highly significant 20% relative reduction in the primary end point, a composite of cardiovascular death, MI, or stroke at 12 months (9.3% incidence with clopidogrel vs 11.4% with placebo; P = .00009). Despite this impressive reduction in ischemic events with clopidogrel, the cumulative event rate continued to increase over the course of the 12-month trial in both study arms. This persistent recurrence of ischemic and thrombotic events has been observed in all antiplatelet trials to date, in spite of the addition of more potent antiplatelet regimens.
Two subanalyses of the CURE results yielded further insights. One analysis examined the timing of benefit from clopidogrel, finding that benefit emerged within 24 hours of treatment and continued consistently throughout the study’s follow-up period (mean of 9 months), supporting the notion of both early and late benefit from more potent antiplatelet therapy in ACS.8 A separate subgroup analysis found that the efficacy advantage of clopidogrel plus aspirin over aspirin alone was similar regardless of whether patients were managed medically or underwent revascularization (PCI or coronary artery bypass graft surgery [CABG]).9
CHARISMA trial: prevention of events in a broad at-risk population. Several years before the CURE trial, clopidogrel was initially evaluated as monotherapy in patients with prior ischemic events in the large randomized trial known as CAPRIE (Clopidogrel Versus Aspirin in Patients at Risk of Ischemic Events), in which aspirin was the comparator.10 Rates of the primary end point—a composite of vascular death, MI, or stroke—over a mean follow-up of 1.9 years were 5.3% in patients assigned to clopidogrel versus 5.8% in those assigned to aspirin, a relative reduction of 8.7% in favor of clopidogrel (P = .043).
The CAPRIE study set the stage for CHARISMA (Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance), which set out to determine whether dual antiplatelet therapy with clopidogrel plus aspirin conferred benefit over aspirin alone in a broad population of patients at high risk for atherothrombotic events.11 No significant additive benefit was observed with dual antiplatelet therapy in the overall CHARISMA population in terms of the composite end point of MI, stroke, or cardiovascular death over the median follow-up of 27.6 months.11
The investigators then analyzed outcomes in a large subgroup of the CHARISMA population—the 9,478 patients who had established vascular disease, ie, prior MI, stroke, or symptomatic peripheral arterial disease.12 Rates of the composite end point (MI, stroke, or cardiovascular death) in this subgroup were 7.3% with clopidogrel plus aspirin versus 8.8% with aspirin alone, representing a 1.5% absolute reduction and a 17% relative reduction with dual antiplatelet therapy (P = .01). The CHARISMA investigators concluded that there appears to be a gradient of benefit from dual antiplatelet therapy depending on the patient’s risk of thrombotic events.
Importance of longer-term therapy. Similarly, additional recent data indicate that interrupting clopidogrel therapy leads to an abrupt increase in risk among patients who experienced ACS months beforehand. Analysis of a large registry of medically treated patients and revascularized patients with ACS showed a clustering of adverse cardiovascular events in the first 90 days after clopidogrel discontinuation, an increase that was particularly pronounced in the medically treated patients.13 Like the findings from the CHARISMA subanalysis above, these data suggest that continuing clopidogrel therapy beyond 1 year may be beneficial, although the ideal duration of therapy and the patient groups most likely to benefit requires further study.
Glycoprotein IIb/IIIa inhibitors
The glycoprotein IIb/IIIa inhibitors—abciximab, eptifibatide, and tirofiban—are parenteral drugs that block the final common pathway of platelet aggregation. With increased focus on the upstream inhibition of platelet activation and the wider availability of more potent oral antiplatelet drugs, the use of glycoprotein IIb/IIIa inhibitors has been declining in recent years.
Efficacy in ACS. A number of placebo-controlled trials of glycoprotein IIb/IIIa inhibitors have been conducted in the setting of ACS without ST-segment elevation. In each trial, the glycoprotein IIb/IIIa inhibitor was associated with a significant reduction in 30-day rates of a composite of death and nonfatal MI. A 2002 pooled analysis of these trials demonstrated an overall 8% relative risk reduction in this end point with active glycoprotein IIb/IIIa inhibitor therapy (P = .037).14 Interpreting the benefit of glycoprotein IIb/IIIa blockade in the setting of clopidogrel therapy, however, is more challenging since upstream use of clopidogrel was rare at the time these studies were performed.
An outlier in the aforementioned pooled analysis was the GUSTO IV-ACS study (Global Utilization of Strategies to open Occluded coronary arteries trial IV in Acute Coronary Syndromes), in which abciximab showed no significant benefit over placebo on the primary end point of death or MI at 30 days.15 This study included 7,800 patients with ACS without ST-segment elevation who were being treated with aspirin and unfractionated or low-molecular-weight heparin and were then randomized to placebo or abciximab. Abciximab was given as a front-loaded bolus followed by an infusion lasting either 24 or 48 hours.
A trend toward higher all-cause mortality was observed with longer infusions of abciximab in the GUSTO IV-ACS trial.15 A hypothesis emerged that a front-loaded regimen of abciximab is suitable for patients undergoing PCI, in whom platelet activation and the risk of adverse outcomes is greatest in the catheterization laboratory, but is less well suited for medically managed patients, in whom levels of platelet aggregation and risk are ongoing.
Timing of treatment. The optimal timing of glycoprotein IIb/IIIa inhibitor initiation remains controversial. Boersma et al pooled data from three randomized placebo-controlled trials and stratified the results into outcomes before PCI and outcomes immediately following PCI.16 Glycoprotein IIb/IIIa inhibition was associated with a 34% relative reduction in the risk of death or MI during 72 hours of medical management prior to PCI (P = .001) and an enhanced 41% relative reduction in this end point in the 48 hours following PCI when PCI was performed during administration of the study drug (P = .001). The investigators concluded that glycoprotein IIb/IIIa blockade should be initiated early after hospital admission and continued until after PCI in patients who undergo the procedure.
The effect of upstream glycoprotein IIb/IIIa inhibitor use was more ambiguous in the recent Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) trial of patients with ACS being managed invasively. At 1 year, upstream use—as compared with in-lab use—of glycoprotein IIb/IIIa inhibitors was associated with a reduction in the rate of ischemic events among patients treated with the direct thrombin inhibitor bivalirudin (17.4% vs 21.5%, respectively; P < .01) but not among patients treated with unfractionated heparin or low-molecular-weight heparin (17.2% vs 18.4%; P = .44).17
Ongoing clinical trial results may shed further light on the considerable clinical uncertainty that remains regarding the benefits of upstream glycoprotein IIb/IIIa inhibitor use in patients with ACS.
Enrollment has just been completed in a large randomized trial designed to prospectively assess the optimal timing of glycoprotein IIb/IIIa inhibitor initiation in patients with high-risk ACS without ST-segment elevation in whom an invasive strategy is planned no sooner than the next calendar day.18 The study, known as EARLY-ACS, is randomizing patients to eptifibatide or placebo begun within 8 hours of hospital arrival, with provisional eptifibatide available in the catheterization laboratory. The primary end point is a 96-hour composite of all-cause mortality, nonfatal MI, recurrent ischemia requiring urgent revascularization, or need for thrombotic bailout with a glycoprotein IIb/IIIa inhibitor during PCI. Data should be available in 2009.
ANTIPLATELET THERAPY GUIDELINES IN NON-ST-ELEVATION ACUTE CORONARY SYNDROMES
In 2007, the American College of Cardiology (ACC) and American Heart Association (AHA) updated their joint guidelines for the use of antiplatelet therapy in the management of patients with unstable angina or MI without ST-segment elevation.19 These guidelines incorporate a large degree of flexibility in the choice of antiplatelet therapy, which can make implementation of their recommendations challenging.
The guidelines contain classes of recommendations based on the magnitude of benefit (I, IIa, IIb, III) and levels of evidence (A, B, C). Following here are key recommendations from the updated guidelines (bulleted and in italics, with the class and level of the recommendation noted in parentheses),19 supplemented with additional commentary where appropriate.
Antiplatelet therapy: General recommendations
- Aspirin should be given to all patients as soon as possible after presentation and continued indefinitely in patients not known to be intolerant of aspirin (class I, level A).
- Clopidogrel should be given to patients unable to take aspirin because of hypersensitivity or major gastrointestinal (GI) intolerance (class I, level A).
This recommendation is based on data from the CURE trial7 and the earlier CAPRIE study.10 The clopidogrel regimen recommended is a 300-mg loading dose followed by a maintenance dosage of 75 mg/day. The incidence of aspirin intolerance is approximately 5%, depending on how intolerance is defined. A significant proportion of patients will stop aspirin because of GI upset or trivial bleeding, failing to understand the true benefits of aspirin. A much smaller subset—perhaps 1 in 1,000—has a true allergy to aspirin.
- Patients with a history of GI bleeding with the use of either aspirin or clopidogrel should be prescribed a proton pump inhibitor or another drug that has been shown to minimize the risk of bleeding (class I, level B).
Initial invasive strategy
- For patients in whom an early invasive strategy is planned, therapy with either clopidogrel or a glycoprotein IIb/IIIa inhibitor should be started upstream (before diagnostic angiography) in addition to aspirin (class I, level A).
This recommendation does not give preference to either agent because head-to-head comparisons of antiplatelet and antithrombotic therapies in this setting are not available.
- Unless PCI is planned very shortly after presentation, either eptifibatide or tirofiban should be the glycoprotein IIb/IIIa inhibitor of choice; if there is no appreciable delay to angiography and PCI is planned, abciximab is indicated (class I, level B).
This recommendation is based on findings of the GUSTO IV-ACS study.15
- When an initial invasive strategy is selected, initiating therapy with both clopidogrel and a glycoprotein IIb/IIIa inhibitor is reasonable (class IIa, level B).
Clearly, the guidelines offer some leeway to allow for different practice patterns in the use of an initial invasive strategy. In my practice, if a patient is high risk and has a low likelihood of early CABG, I use both clopidogrel and a glycoprotein IIb/IIIa inhibitor upstream (prior to going to the catheterization laboratory). If a patient has a reasonable likelihood of requiring CABG, I eliminate the thienopyridine and treat with a glycoprotein IIb/IIIa inhibitor. If a patient is at increased risk of bleeding, I forgo the glycoprotein IIb/IIIa inhibitor in favor of clopidogrel.
- In patients who are going to the catheterization laboratory, omitting a glycoprotein IIb/IIIa inhibitor upstream is reasonable if a loading dose of clopidogrel was given and the use of bivalirudin is planned (class IIa, level B).
This recommendation takes into account the duration of clopidogrel’s antiplatelet effect and recognizes the likely limited benefit of glycoprotein IIb/IIIa inhibitors in patients who proceed rapidly to the catheterization laboratory.
Initial conservative strategy
- In patients being managed conservatively (ie, noninvasively), clopidogrel should be given as a loading dose of at least 300 mg followed by a maintenance dosage of at least 75 mg/day, in addition to aspirin and anticoagulant therapy as soon as possible, and continued for at least 1 month (class I, level A) and, ideally, up to 1 year (class I, level B).
- If patients who undergo an initial conservative management strategy have recurrent symptoms/ischemia, or if heart failure or serious arrhythmias develop, diagnostic angiography is recommended (class I, level A). Either a glycoprotein IIb/IIIa inhibitor (class I, level A) or clopidogrel (class I, level A) should be added to aspirin and anticoagulant therapy upstream (before angiography) in these patients (class I, level C).
- Patients classified as low risk based on stress testing should continue aspirin indefinitely (class I, level A). Clopidogrel should be continued for at least 1 month (class I, level A) and, ideally, up to 1 year (class I, level B). If a glycoprotein IIb/IIIa inhibitor had been started previously, it should be discontinued (class I, level A).
- Patients with coronary artery disease confirmed by angiography in whom a medical management strategy (rather than PCI) is selected should be continued on aspirin indefinitely (class I, level A). If clopidogrel has not already been started, a loading dose should be given (class I, level A). If started previously, glycoprotein IIb/IIIa inhibitor therapy should be discontinued (class I, level B).
- For patients managed medically without stenting, 75 to 162 mg/day of aspirin should be prescribed indefinitely (class I, level A), along with 75 mg/day of clopidogrel for at least 1 month (class I, level A) and, ideally, for up to 1 year (class I, level B).
Antiplatelet guidelines for stenting
Antiplatelet therapy is more complicated in the setting of stenting.
- For patients in whom bare metal stents are implanted, aspirin should be prescribed at a dosage of 162 to 325 mg/day for at least 1 month (class I, level B) and then continued indefinitely at 75 to 162 mg/day (class I, level A). In addition, 75 mg/day of clopidogrel should be continued for at least 1 month and, ideally, up to 1 year unless the patient is at increased risk of bleeding (in which case it should be given for at least 2 weeks) (class I, level B).
- For patients receiving drug-eluting stents, aspirin is recommended at a dosage of 162 to 325 mg/day for at least 3 months in those with a sirolimus-eluting stent and at least 6 months in those with a paclitaxel-eluting stent, after which it should be continued indefinitely at 75 to 162 mg/day (class I, level B). In addition, clopidogrel 75 mg/day is recommended for at least 12 months regardless of the type of drug-eluting stent (class I, level B).
No mention is made of dual antiplatelet therapy beyond 1 year.
At my institution, Duke University Medical Center, patients are assessed carefully for their ability and willingness to adhere to extended antiplatelet therapy before drug-eluting stents are implanted. This assessment includes an evaluation of their insurance status, their history of adherence to other prescribed drug regimens, their education level, and the dispenser of their medications.
No guidance on concomitant anticoagulation
One omission in the current ACC/AHA guidelines is the lack of guidance for patients who require concomitant antiplatelet therapy and anticoagulation. Such guidance is needed, as many patients with ACS also have indications for long-term anticoagulation, such as atrial fibrillation or valvular heart disease requiring prosthetic valves. The ACC/AHA guidelines recommend simply that anticoagulation be added to patients’ antiplatelet regimens.
HOW ARE WE DOING? APPLICATION OF GUIDELINES IN PRACTICE
No discussion of guidelines is complete without consideration of their implementation. Those interested in the use of antiplatelet therapy in ACS are fortunate to have the Acute Coronary Treatment and Intervention Outcomes Network (ACTION) Registry, a collaborative voluntary surveillance system launched in January 2007 to assess patient characteristics, treatment, and short-term outcomes in patients with ACS (MI with and without ST-segment elevation). In addition to the registry, ACTION offers guidance on measuring ACS outcomes and establishing programs for implementing evidence-based guideline recommendations in clinical practice, improving the quality and safety of ACS care, and potentially investigating novel quality-improvement methods.20
Findings from ACTION’s first 12 months
In its first 12 months (January–December 2007), the ACTION Registry captured data from 31,036 ACS cases from several hundred US hospitals, according to the ACTION National Cardiovascular Data Registry Annual Report (personal communication from Matthew T. Roe, MD, September 2008). Data were collected at two time points: acutely (during the first 24 hours after presentation) and at hospital discharge. One caveat to interpreting data from the ACTION Registry is the voluntary and retrospective reporting system on which it relies.
Intervention rates. Among patients with non-ST-segment MI in whom catheterization was not contraindicated, 85% underwent catheterization and 70% did so within 48 hours of presentation; 53% underwent PCI and 45% did so within 48 hours of presentation; and 13% underwent CABG. The median time to catheterization was 21 hours, and the median time to PCI was 19 hours.
Although many patients who go to the catheterization laboratory are managed invasively, many do not undergo PCI and are managed medically or with CABG following coronary angiography. The message, therefore, is that local practice patterns should be taken into consideration when results from clinical trials are applied to clinical practice.
Acute antiplatelet therapy. The 2007 ACTION Registry data showed that aspirin was used acutely (< 24 hours) in almost all patients in whom it was not contraindicated (97%), clopidogrel was used in 59%, and glycoprotein IIb/IIIa inhibitors were used in 44%. Given the ACC/AHA guidelines’ strong endorsement (class I, level A) of clopidogrel in this setting, one would expect wider use of clopidogrel in this context. Moreover, this relatively low rate of clopidogrel use (59%) cannot be explained by use of glycoprotein IIb/IIIa inhibitors instead, since this rate comprises patients who received clopidogrel either with or without a concomitant glycoprotein IIb/IIIa inhibitor; only 12% of patients received a glycoprotein IIb/IIIa inhibitor without clopidogrel. In contrast, a full 28% of patients received neither clopidogrel nor a glycoprotein IIb/IIIa inhibitor, contrary to current ACC/AHA guideline recommendations.
Antiplatelet therapy at discharge. At discharge, 97% of ACTION Registry patients were being treated with aspirin and 73% with clopidogrel. Notably, the use of clopidogrel at discharge was highly correlated with overall management strategy: whereas it was used in 97% of patients undergoing PCI, it was used in only 53% of patients being managed medically and in 31% of those undergoing CABG. These findings are somewhat reassuring since they generally mirror the strength of evidence supporting clopidogrel use in these different settings.
IMPORTANT REAL-WORLD CONSIDERATIONS: BLEEDING AND DOSING
Do not neglect bleeding risk
As antiplatelet therapy becomes more potent in an effort to reduce ischemic events, bleeding risk has become a concern. Major bleeding events occur in more than 10% of patients with ACS receiving antiplatelet therapy,21 although lower rates have been reported in clinical trials in which carefully selected populations are enrolled.7,14,22–24
Major bleeding affects overall outcomes. Major bleeding has clinical significance. The Global Registry of Acute Coronary Events (GRACE), which analyzed data from 24,000 patients with ACS, revealed that major bleeding was associated with significantly worse outcomes: rates of in-hospital death were three times as high—15.3% versus 5.3%—in patients who had major bleeding episodes compared with those who did not (odds ratio = 1.64 [95% CI, 1.18–2.28]).25 The relationship between bleeding and adverse overall outcomes is not fully understood but is nevertheless real and has been observed in multiple databases.
Risk factors for bleeding mirror those for ischemic events. Models are currently being developed to predict bleeding. Unfortunately, the factors that predict bleeding tend to also predict recurrent ischemic events. As a result, patients who stand to benefit most from antithrombotic therapies also are at the greatest risk of bleeding from those therapies.
Additive risk from dual antiplatelet therapy. The additional bleeding risk from adding clopidogrel to aspirin is often not fully appreciated. In the CURE trial, the absolute excess risk of major bleeding by adding clopidogrel to aspirin was 1% (3.7% vs 2.7%), which translates to a 35% relative increase compared with aspirin alone.7 In that trial, major bleeding was most prevalent in patients undergoing CABG, and the rate of major bleeding was increased by more than 50% in patients receiving dual antiplatelet therapy when clopidogrel was discontinued 5 days or less before CABG (compared with CABG patients randomized to aspirin alone). This prompted the recommendation that clopidogrel be discontinued more than 5 days prior to CABG.
Similarly, the CHARISMA trial, which used the GUSTO scale for bleeding classification, revealed a significant excess of moderate bleeding with the combination of clopidogrel and aspirin relative to aspirin alone (2.1% vs 1.3%; P < .001) and a nonsignificant trend toward an excess of GUSTO-defined severe bleeding.11
Dosing: Time to end ‘one size fits all’ approach
Dosing of antiplatelet therapies has traditionally been a “one size fits all” strategy, but the importance of tailored therapy and dosing is starting to be realized.
Excess dosing of glycoprotein IIb/IIIa inhibitors is common, dangerous. As an example, the CRUSADE initiative, an ongoing national database of patients with high-risk ACS without ST-segment elevation, showed that 27% of patients treated with glycoprotein IIb/IIIa inhibitors at 400 participating US hospitals in 2004 were overdosed, based on dose-adjustment recommendations in the medications’ package inserts.27 Patients who received excessive doses were significantly more likely to suffer major bleeding than were those who were dosed correctly (odds ratio = 1.46 [95% CI, 1.22–1.73]), an increased risk that was particularly pronounced in women.
Quality-improvement initiatives. The above-mentioned CRUSADE initiative, which was launched in 2001 and involves hundreds of participating US hospitals, has served as a road map for improving dosing practices in antithrombotic therapy. Like the newer ACTION Registry,20 CRUSADE issued performance report cards to its participating hospitals in which antithrombotic medication use over the prior 12 months was compared with each institution’s past performance and with data from similar hospitals across the nation.
SUMMARY AND CONCLUSIONS
Managing antiplatelet therapy for patients with ACS is complex, given the array of medications available and the various combinations in which they can be used. Therapy is likely to become even more complicated, as several new medications are under review by the US Food and Drug Administration or in phase 3 clinical trials.
Current antiplatelet therapy for patients with ACS is suboptimal. Ischemic event recurrence rates continue to rise despite the use of current antiplatelet therapies, bleeding remains an underappreciated risk, and dosing often varies from evidence-based recommendations. Developing prospective strategies for antiplatelet therapy will improve utilization in keeping with a more evidence-based approach. Current ACC/AHA guidelines are the beginning of a roadmap to optimal use of antiplatelet drugs, and quality-improvement initiatives linked to national registries like ACTION promise even more guidance toward optimal therapy through institution-specific benchmarking and performance reports.
Thus far, more effective antiplatelet therapy has led to a greater risk of bleeding. Emerging novel antiplatelet agents and smarter use of existing therapies have the potential to improve both ischemic and bleeding outcomes.
The final event leading to acute coronary syndromes (ACS) is spontaneous atherosclerotic plaque rupture. This event is analogous to the plaque rupture caused by percutaneous coronary intervention (PCI). Both events initiate a platelet response that starts with the adhesion of platelets to the vessel wall, followed by the activation and then aggregation of platelets.
The clinical consequences of intravascular platelet activation and aggregation are well known: death, myocardial infarction (MI), myocardial ischemia, and arrhythmias. In terms of health care burden, ACS is the primary or secondary diagnosis in 1.57 million hospitalizations annually in the United States—specifically, unstable angina or MI without ST-segment elevation in 1.24 million hospitalizations, and MI with ST-segment elevation in 330,000 hospitalizations.1
This real-world impact of ACS is tempered by the real-world use and effectiveness of our antiplatelet drug therapies, which is the focus of this article. I begin with a brief review of the evidence surrounding three major antiplatelet therapies used in ACS management—aspirin, clopidogrel, and the glycoprotein IIb/IIIa inhibitors. I then review the updated evidence-based guidelines for the use of antiplatelet therapies in ACS. I conclude with an overview of how US hospitals are actually using these therapies, with a focus on two particularly important challenges—bleeding risk and appropriate dosing—and on initiatives under way to bridge the gap between recommended antiplatelet therapy for ACS and actual clinical practice.
ANTIPLATELET THERAPY IN ACUTE CORONARY SYNDROMES
Aspirin
Although aspirin has long been the bedrock of antiplatelet therapy in patients with ACS, its effects on the heart are still being elucidated. Several placebo-controlled trials of aspirin, each with relatively few subjects, have been conducted in the setting of ACS without ST-segment elevation.2–5 Although confidence intervals were wide, these studies showed a favorable effect of aspirin relative to placebo on the risk of death and nonfatal MI.
Clopidogrel and dual antiplatelet therapy
CURE trial: prevention of recurrent events in patients with ACS. Dual antiplatelet therapy with the thienopyridine agent clopidogrel plus aspirin was investigated in patients presenting with ACS without ST-segment elevation in the landmark CURE trial (Clopidogrel in Unstable Angina to Prevent Recurrent Events).7 This study randomized 12,562 patients presenting within 24 hours of ACS symptom onset to either clopidogrel or placebo, in addition to aspirin, for 3 to 12 months. Clopidogrel was administered as a loading dose of 300 mg followed by a maintenance dosage of 75 mg/day. Randomization to clopidogrel was associated with a highly significant 20% relative reduction in the primary end point, a composite of cardiovascular death, MI, or stroke at 12 months (9.3% incidence with clopidogrel vs 11.4% with placebo; P = .00009). Despite this impressive reduction in ischemic events with clopidogrel, the cumulative event rate continued to increase over the course of the 12-month trial in both study arms. This persistent recurrence of ischemic and thrombotic events has been observed in all antiplatelet trials to date, in spite of the addition of more potent antiplatelet regimens.
Two subanalyses of the CURE results yielded further insights. One analysis examined the timing of benefit from clopidogrel, finding that benefit emerged within 24 hours of treatment and continued consistently throughout the study’s follow-up period (mean of 9 months), supporting the notion of both early and late benefit from more potent antiplatelet therapy in ACS.8 A separate subgroup analysis found that the efficacy advantage of clopidogrel plus aspirin over aspirin alone was similar regardless of whether patients were managed medically or underwent revascularization (PCI or coronary artery bypass graft surgery [CABG]).9
CHARISMA trial: prevention of events in a broad at-risk population. Several years before the CURE trial, clopidogrel was initially evaluated as monotherapy in patients with prior ischemic events in the large randomized trial known as CAPRIE (Clopidogrel Versus Aspirin in Patients at Risk of Ischemic Events), in which aspirin was the comparator.10 Rates of the primary end point—a composite of vascular death, MI, or stroke—over a mean follow-up of 1.9 years were 5.3% in patients assigned to clopidogrel versus 5.8% in those assigned to aspirin, a relative reduction of 8.7% in favor of clopidogrel (P = .043).
The CAPRIE study set the stage for CHARISMA (Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance), which set out to determine whether dual antiplatelet therapy with clopidogrel plus aspirin conferred benefit over aspirin alone in a broad population of patients at high risk for atherothrombotic events.11 No significant additive benefit was observed with dual antiplatelet therapy in the overall CHARISMA population in terms of the composite end point of MI, stroke, or cardiovascular death over the median follow-up of 27.6 months.11
The investigators then analyzed outcomes in a large subgroup of the CHARISMA population—the 9,478 patients who had established vascular disease, ie, prior MI, stroke, or symptomatic peripheral arterial disease.12 Rates of the composite end point (MI, stroke, or cardiovascular death) in this subgroup were 7.3% with clopidogrel plus aspirin versus 8.8% with aspirin alone, representing a 1.5% absolute reduction and a 17% relative reduction with dual antiplatelet therapy (P = .01). The CHARISMA investigators concluded that there appears to be a gradient of benefit from dual antiplatelet therapy depending on the patient’s risk of thrombotic events.
Importance of longer-term therapy. Similarly, additional recent data indicate that interrupting clopidogrel therapy leads to an abrupt increase in risk among patients who experienced ACS months beforehand. Analysis of a large registry of medically treated patients and revascularized patients with ACS showed a clustering of adverse cardiovascular events in the first 90 days after clopidogrel discontinuation, an increase that was particularly pronounced in the medically treated patients.13 Like the findings from the CHARISMA subanalysis above, these data suggest that continuing clopidogrel therapy beyond 1 year may be beneficial, although the ideal duration of therapy and the patient groups most likely to benefit requires further study.
Glycoprotein IIb/IIIa inhibitors
The glycoprotein IIb/IIIa inhibitors—abciximab, eptifibatide, and tirofiban—are parenteral drugs that block the final common pathway of platelet aggregation. With increased focus on the upstream inhibition of platelet activation and the wider availability of more potent oral antiplatelet drugs, the use of glycoprotein IIb/IIIa inhibitors has been declining in recent years.
Efficacy in ACS. A number of placebo-controlled trials of glycoprotein IIb/IIIa inhibitors have been conducted in the setting of ACS without ST-segment elevation. In each trial, the glycoprotein IIb/IIIa inhibitor was associated with a significant reduction in 30-day rates of a composite of death and nonfatal MI. A 2002 pooled analysis of these trials demonstrated an overall 8% relative risk reduction in this end point with active glycoprotein IIb/IIIa inhibitor therapy (P = .037).14 Interpreting the benefit of glycoprotein IIb/IIIa blockade in the setting of clopidogrel therapy, however, is more challenging since upstream use of clopidogrel was rare at the time these studies were performed.
An outlier in the aforementioned pooled analysis was the GUSTO IV-ACS study (Global Utilization of Strategies to open Occluded coronary arteries trial IV in Acute Coronary Syndromes), in which abciximab showed no significant benefit over placebo on the primary end point of death or MI at 30 days.15 This study included 7,800 patients with ACS without ST-segment elevation who were being treated with aspirin and unfractionated or low-molecular-weight heparin and were then randomized to placebo or abciximab. Abciximab was given as a front-loaded bolus followed by an infusion lasting either 24 or 48 hours.
A trend toward higher all-cause mortality was observed with longer infusions of abciximab in the GUSTO IV-ACS trial.15 A hypothesis emerged that a front-loaded regimen of abciximab is suitable for patients undergoing PCI, in whom platelet activation and the risk of adverse outcomes is greatest in the catheterization laboratory, but is less well suited for medically managed patients, in whom levels of platelet aggregation and risk are ongoing.
Timing of treatment. The optimal timing of glycoprotein IIb/IIIa inhibitor initiation remains controversial. Boersma et al pooled data from three randomized placebo-controlled trials and stratified the results into outcomes before PCI and outcomes immediately following PCI.16 Glycoprotein IIb/IIIa inhibition was associated with a 34% relative reduction in the risk of death or MI during 72 hours of medical management prior to PCI (P = .001) and an enhanced 41% relative reduction in this end point in the 48 hours following PCI when PCI was performed during administration of the study drug (P = .001). The investigators concluded that glycoprotein IIb/IIIa blockade should be initiated early after hospital admission and continued until after PCI in patients who undergo the procedure.
The effect of upstream glycoprotein IIb/IIIa inhibitor use was more ambiguous in the recent Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) trial of patients with ACS being managed invasively. At 1 year, upstream use—as compared with in-lab use—of glycoprotein IIb/IIIa inhibitors was associated with a reduction in the rate of ischemic events among patients treated with the direct thrombin inhibitor bivalirudin (17.4% vs 21.5%, respectively; P < .01) but not among patients treated with unfractionated heparin or low-molecular-weight heparin (17.2% vs 18.4%; P = .44).17
Ongoing clinical trial results may shed further light on the considerable clinical uncertainty that remains regarding the benefits of upstream glycoprotein IIb/IIIa inhibitor use in patients with ACS.
Enrollment has just been completed in a large randomized trial designed to prospectively assess the optimal timing of glycoprotein IIb/IIIa inhibitor initiation in patients with high-risk ACS without ST-segment elevation in whom an invasive strategy is planned no sooner than the next calendar day.18 The study, known as EARLY-ACS, is randomizing patients to eptifibatide or placebo begun within 8 hours of hospital arrival, with provisional eptifibatide available in the catheterization laboratory. The primary end point is a 96-hour composite of all-cause mortality, nonfatal MI, recurrent ischemia requiring urgent revascularization, or need for thrombotic bailout with a glycoprotein IIb/IIIa inhibitor during PCI. Data should be available in 2009.
ANTIPLATELET THERAPY GUIDELINES IN NON-ST-ELEVATION ACUTE CORONARY SYNDROMES
In 2007, the American College of Cardiology (ACC) and American Heart Association (AHA) updated their joint guidelines for the use of antiplatelet therapy in the management of patients with unstable angina or MI without ST-segment elevation.19 These guidelines incorporate a large degree of flexibility in the choice of antiplatelet therapy, which can make implementation of their recommendations challenging.
The guidelines contain classes of recommendations based on the magnitude of benefit (I, IIa, IIb, III) and levels of evidence (A, B, C). Following here are key recommendations from the updated guidelines (bulleted and in italics, with the class and level of the recommendation noted in parentheses),19 supplemented with additional commentary where appropriate.
Antiplatelet therapy: General recommendations
- Aspirin should be given to all patients as soon as possible after presentation and continued indefinitely in patients not known to be intolerant of aspirin (class I, level A).
- Clopidogrel should be given to patients unable to take aspirin because of hypersensitivity or major gastrointestinal (GI) intolerance (class I, level A).
This recommendation is based on data from the CURE trial7 and the earlier CAPRIE study.10 The clopidogrel regimen recommended is a 300-mg loading dose followed by a maintenance dosage of 75 mg/day. The incidence of aspirin intolerance is approximately 5%, depending on how intolerance is defined. A significant proportion of patients will stop aspirin because of GI upset or trivial bleeding, failing to understand the true benefits of aspirin. A much smaller subset—perhaps 1 in 1,000—has a true allergy to aspirin.
- Patients with a history of GI bleeding with the use of either aspirin or clopidogrel should be prescribed a proton pump inhibitor or another drug that has been shown to minimize the risk of bleeding (class I, level B).
Initial invasive strategy
- For patients in whom an early invasive strategy is planned, therapy with either clopidogrel or a glycoprotein IIb/IIIa inhibitor should be started upstream (before diagnostic angiography) in addition to aspirin (class I, level A).
This recommendation does not give preference to either agent because head-to-head comparisons of antiplatelet and antithrombotic therapies in this setting are not available.
- Unless PCI is planned very shortly after presentation, either eptifibatide or tirofiban should be the glycoprotein IIb/IIIa inhibitor of choice; if there is no appreciable delay to angiography and PCI is planned, abciximab is indicated (class I, level B).
This recommendation is based on findings of the GUSTO IV-ACS study.15
- When an initial invasive strategy is selected, initiating therapy with both clopidogrel and a glycoprotein IIb/IIIa inhibitor is reasonable (class IIa, level B).
Clearly, the guidelines offer some leeway to allow for different practice patterns in the use of an initial invasive strategy. In my practice, if a patient is high risk and has a low likelihood of early CABG, I use both clopidogrel and a glycoprotein IIb/IIIa inhibitor upstream (prior to going to the catheterization laboratory). If a patient has a reasonable likelihood of requiring CABG, I eliminate the thienopyridine and treat with a glycoprotein IIb/IIIa inhibitor. If a patient is at increased risk of bleeding, I forgo the glycoprotein IIb/IIIa inhibitor in favor of clopidogrel.
- In patients who are going to the catheterization laboratory, omitting a glycoprotein IIb/IIIa inhibitor upstream is reasonable if a loading dose of clopidogrel was given and the use of bivalirudin is planned (class IIa, level B).
This recommendation takes into account the duration of clopidogrel’s antiplatelet effect and recognizes the likely limited benefit of glycoprotein IIb/IIIa inhibitors in patients who proceed rapidly to the catheterization laboratory.
Initial conservative strategy
- In patients being managed conservatively (ie, noninvasively), clopidogrel should be given as a loading dose of at least 300 mg followed by a maintenance dosage of at least 75 mg/day, in addition to aspirin and anticoagulant therapy as soon as possible, and continued for at least 1 month (class I, level A) and, ideally, up to 1 year (class I, level B).
- If patients who undergo an initial conservative management strategy have recurrent symptoms/ischemia, or if heart failure or serious arrhythmias develop, diagnostic angiography is recommended (class I, level A). Either a glycoprotein IIb/IIIa inhibitor (class I, level A) or clopidogrel (class I, level A) should be added to aspirin and anticoagulant therapy upstream (before angiography) in these patients (class I, level C).
- Patients classified as low risk based on stress testing should continue aspirin indefinitely (class I, level A). Clopidogrel should be continued for at least 1 month (class I, level A) and, ideally, up to 1 year (class I, level B). If a glycoprotein IIb/IIIa inhibitor had been started previously, it should be discontinued (class I, level A).
- Patients with coronary artery disease confirmed by angiography in whom a medical management strategy (rather than PCI) is selected should be continued on aspirin indefinitely (class I, level A). If clopidogrel has not already been started, a loading dose should be given (class I, level A). If started previously, glycoprotein IIb/IIIa inhibitor therapy should be discontinued (class I, level B).
- For patients managed medically without stenting, 75 to 162 mg/day of aspirin should be prescribed indefinitely (class I, level A), along with 75 mg/day of clopidogrel for at least 1 month (class I, level A) and, ideally, for up to 1 year (class I, level B).
Antiplatelet guidelines for stenting
Antiplatelet therapy is more complicated in the setting of stenting.
- For patients in whom bare metal stents are implanted, aspirin should be prescribed at a dosage of 162 to 325 mg/day for at least 1 month (class I, level B) and then continued indefinitely at 75 to 162 mg/day (class I, level A). In addition, 75 mg/day of clopidogrel should be continued for at least 1 month and, ideally, up to 1 year unless the patient is at increased risk of bleeding (in which case it should be given for at least 2 weeks) (class I, level B).
- For patients receiving drug-eluting stents, aspirin is recommended at a dosage of 162 to 325 mg/day for at least 3 months in those with a sirolimus-eluting stent and at least 6 months in those with a paclitaxel-eluting stent, after which it should be continued indefinitely at 75 to 162 mg/day (class I, level B). In addition, clopidogrel 75 mg/day is recommended for at least 12 months regardless of the type of drug-eluting stent (class I, level B).
No mention is made of dual antiplatelet therapy beyond 1 year.
At my institution, Duke University Medical Center, patients are assessed carefully for their ability and willingness to adhere to extended antiplatelet therapy before drug-eluting stents are implanted. This assessment includes an evaluation of their insurance status, their history of adherence to other prescribed drug regimens, their education level, and the dispenser of their medications.
No guidance on concomitant anticoagulation
One omission in the current ACC/AHA guidelines is the lack of guidance for patients who require concomitant antiplatelet therapy and anticoagulation. Such guidance is needed, as many patients with ACS also have indications for long-term anticoagulation, such as atrial fibrillation or valvular heart disease requiring prosthetic valves. The ACC/AHA guidelines recommend simply that anticoagulation be added to patients’ antiplatelet regimens.
HOW ARE WE DOING? APPLICATION OF GUIDELINES IN PRACTICE
No discussion of guidelines is complete without consideration of their implementation. Those interested in the use of antiplatelet therapy in ACS are fortunate to have the Acute Coronary Treatment and Intervention Outcomes Network (ACTION) Registry, a collaborative voluntary surveillance system launched in January 2007 to assess patient characteristics, treatment, and short-term outcomes in patients with ACS (MI with and without ST-segment elevation). In addition to the registry, ACTION offers guidance on measuring ACS outcomes and establishing programs for implementing evidence-based guideline recommendations in clinical practice, improving the quality and safety of ACS care, and potentially investigating novel quality-improvement methods.20
Findings from ACTION’s first 12 months
In its first 12 months (January–December 2007), the ACTION Registry captured data from 31,036 ACS cases from several hundred US hospitals, according to the ACTION National Cardiovascular Data Registry Annual Report (personal communication from Matthew T. Roe, MD, September 2008). Data were collected at two time points: acutely (during the first 24 hours after presentation) and at hospital discharge. One caveat to interpreting data from the ACTION Registry is the voluntary and retrospective reporting system on which it relies.
Intervention rates. Among patients with non-ST-segment MI in whom catheterization was not contraindicated, 85% underwent catheterization and 70% did so within 48 hours of presentation; 53% underwent PCI and 45% did so within 48 hours of presentation; and 13% underwent CABG. The median time to catheterization was 21 hours, and the median time to PCI was 19 hours.
Although many patients who go to the catheterization laboratory are managed invasively, many do not undergo PCI and are managed medically or with CABG following coronary angiography. The message, therefore, is that local practice patterns should be taken into consideration when results from clinical trials are applied to clinical practice.
Acute antiplatelet therapy. The 2007 ACTION Registry data showed that aspirin was used acutely (< 24 hours) in almost all patients in whom it was not contraindicated (97%), clopidogrel was used in 59%, and glycoprotein IIb/IIIa inhibitors were used in 44%. Given the ACC/AHA guidelines’ strong endorsement (class I, level A) of clopidogrel in this setting, one would expect wider use of clopidogrel in this context. Moreover, this relatively low rate of clopidogrel use (59%) cannot be explained by use of glycoprotein IIb/IIIa inhibitors instead, since this rate comprises patients who received clopidogrel either with or without a concomitant glycoprotein IIb/IIIa inhibitor; only 12% of patients received a glycoprotein IIb/IIIa inhibitor without clopidogrel. In contrast, a full 28% of patients received neither clopidogrel nor a glycoprotein IIb/IIIa inhibitor, contrary to current ACC/AHA guideline recommendations.
Antiplatelet therapy at discharge. At discharge, 97% of ACTION Registry patients were being treated with aspirin and 73% with clopidogrel. Notably, the use of clopidogrel at discharge was highly correlated with overall management strategy: whereas it was used in 97% of patients undergoing PCI, it was used in only 53% of patients being managed medically and in 31% of those undergoing CABG. These findings are somewhat reassuring since they generally mirror the strength of evidence supporting clopidogrel use in these different settings.
IMPORTANT REAL-WORLD CONSIDERATIONS: BLEEDING AND DOSING
Do not neglect bleeding risk
As antiplatelet therapy becomes more potent in an effort to reduce ischemic events, bleeding risk has become a concern. Major bleeding events occur in more than 10% of patients with ACS receiving antiplatelet therapy,21 although lower rates have been reported in clinical trials in which carefully selected populations are enrolled.7,14,22–24
Major bleeding affects overall outcomes. Major bleeding has clinical significance. The Global Registry of Acute Coronary Events (GRACE), which analyzed data from 24,000 patients with ACS, revealed that major bleeding was associated with significantly worse outcomes: rates of in-hospital death were three times as high—15.3% versus 5.3%—in patients who had major bleeding episodes compared with those who did not (odds ratio = 1.64 [95% CI, 1.18–2.28]).25 The relationship between bleeding and adverse overall outcomes is not fully understood but is nevertheless real and has been observed in multiple databases.
Risk factors for bleeding mirror those for ischemic events. Models are currently being developed to predict bleeding. Unfortunately, the factors that predict bleeding tend to also predict recurrent ischemic events. As a result, patients who stand to benefit most from antithrombotic therapies also are at the greatest risk of bleeding from those therapies.
Additive risk from dual antiplatelet therapy. The additional bleeding risk from adding clopidogrel to aspirin is often not fully appreciated. In the CURE trial, the absolute excess risk of major bleeding by adding clopidogrel to aspirin was 1% (3.7% vs 2.7%), which translates to a 35% relative increase compared with aspirin alone.7 In that trial, major bleeding was most prevalent in patients undergoing CABG, and the rate of major bleeding was increased by more than 50% in patients receiving dual antiplatelet therapy when clopidogrel was discontinued 5 days or less before CABG (compared with CABG patients randomized to aspirin alone). This prompted the recommendation that clopidogrel be discontinued more than 5 days prior to CABG.
Similarly, the CHARISMA trial, which used the GUSTO scale for bleeding classification, revealed a significant excess of moderate bleeding with the combination of clopidogrel and aspirin relative to aspirin alone (2.1% vs 1.3%; P < .001) and a nonsignificant trend toward an excess of GUSTO-defined severe bleeding.11
Dosing: Time to end ‘one size fits all’ approach
Dosing of antiplatelet therapies has traditionally been a “one size fits all” strategy, but the importance of tailored therapy and dosing is starting to be realized.
Excess dosing of glycoprotein IIb/IIIa inhibitors is common, dangerous. As an example, the CRUSADE initiative, an ongoing national database of patients with high-risk ACS without ST-segment elevation, showed that 27% of patients treated with glycoprotein IIb/IIIa inhibitors at 400 participating US hospitals in 2004 were overdosed, based on dose-adjustment recommendations in the medications’ package inserts.27 Patients who received excessive doses were significantly more likely to suffer major bleeding than were those who were dosed correctly (odds ratio = 1.46 [95% CI, 1.22–1.73]), an increased risk that was particularly pronounced in women.
Quality-improvement initiatives. The above-mentioned CRUSADE initiative, which was launched in 2001 and involves hundreds of participating US hospitals, has served as a road map for improving dosing practices in antithrombotic therapy. Like the newer ACTION Registry,20 CRUSADE issued performance report cards to its participating hospitals in which antithrombotic medication use over the prior 12 months was compared with each institution’s past performance and with data from similar hospitals across the nation.
SUMMARY AND CONCLUSIONS
Managing antiplatelet therapy for patients with ACS is complex, given the array of medications available and the various combinations in which they can be used. Therapy is likely to become even more complicated, as several new medications are under review by the US Food and Drug Administration or in phase 3 clinical trials.
Current antiplatelet therapy for patients with ACS is suboptimal. Ischemic event recurrence rates continue to rise despite the use of current antiplatelet therapies, bleeding remains an underappreciated risk, and dosing often varies from evidence-based recommendations. Developing prospective strategies for antiplatelet therapy will improve utilization in keeping with a more evidence-based approach. Current ACC/AHA guidelines are the beginning of a roadmap to optimal use of antiplatelet drugs, and quality-improvement initiatives linked to national registries like ACTION promise even more guidance toward optimal therapy through institution-specific benchmarking and performance reports.
Thus far, more effective antiplatelet therapy has led to a greater risk of bleeding. Emerging novel antiplatelet agents and smarter use of existing therapies have the potential to improve both ischemic and bleeding outcomes.
- Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics—2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2007; 115:e69–e171.
- Cairns JA, Gent M, Singer J, et al. Aspirin, sulfinpyrazone, or both in unstable angina: results of a Canadian multicenter trial. N Engl J Med 1985; 313:1369–1375.
- Lewis HD Jr, Davis JW, Archibald DG, et al. Protective effects of aspirin against acute myocardial infarction and death in men with unstable angina: results of a Veterans Administration Cooperative Study. N Engl J Med 1983; 309:396–403.
- Théroux P, Ouimet H, McCans J, et al. Aspirin, heparin, or both to treat acute unstable angina. N Engl J Med 1988; 319:1105–1111.
- Wallentin LC. Aspirin (75 mg/day) after an episode of unstable coronary artery disease: long-term effects on the risk for myocardial infarction, occurrence of severe angina and the need for revascularization: Research Group on Instability in Coronary Artery Disease in Southeast Sweden. J Am Coll Cardiol 1991; 18:1587–1593.
- Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomized trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002; 324:71–86.
- Yusuf S, Zhao F, Mehta SR, et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 2001; 345:494–502.
- Yusuf S, Mehta SR, Zhao F, et al. Early and late effects of clopidogrel in patients with acute coronary syndromes. Circulation 2003; 107:966–972.
- Fox KA, Mehta SR, Peters R, et al. Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non-ST-elevation acute coronary syndrome: the Clopidogrel in Unstable angina to prevent Recurrent ischemic Events (CURE) Trial. Circulation 2004; 110:1202–1208.
- CAPRIE Steering Committee. A randomized, blinded trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet 1996; 348:1329–1339.
- Bhatt DL, Fox KA, Hacke W, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med 2006; 354:1706–1717.
- Bhatt DL, Flather MD, Hacke W, et al. Patients with prior myocardial infarction, stroke, or symptomatic peripheral arterial disease in the CHARISMA trial. J Am Coll Cardiol 2007; 49:1982–1988.
- Ho PM, Peterson ED, Wang L, et al. Incidence of death and acute myocardial infarction associated with stopping clopidogrel after acute coronary syndrome. JAMA 2008; 299:532–539.
- Boersma E, Harrington RA, Moliterno DJ, et al. Platelet glycoprotein IIb/IIIa inhibitors in acute coronary syndromes: a meta-analysis of all major randomised clinical trials. Lancet 2002; 359:189–198.
- Simoons ML, GUSTO IV-ACS Investigators. Effect of glycoprotein IIb/IIIa receptor blocker abciximab on outcome in patients with acute coronary syndromes without early coronary revascularisation: the GUSTO IV-ACS randomised trial. Lancet 2001; 357:1915–1924.
- Boersma E, Akkerhuis KM, Théroux P, Calif RM, Topol EJ, Simoons ML. Platelet glycoprotein IIb/IIIa receptor inhibition in non-ST-elevation acute coronary syndromes: early benefit during medical treatment only, with additional protection during percutaneous coronary intervention. Circulation 1999; 100:2045–2048.
- White HD, Ohman EM, Lincoff AM, et al. Safety and efficacy of bivalirudin with and without glycoprotein IIb/IIIa inhibitors in patients with acute coronary syndromes undergoing percutaneous coronary intervention. J Am Coll Cardiol 2008; 52:807–814.
- EARLY-ACS: glycoprotein IIb/IIIa inhibition in patients with non-ST-segment elevation acute coronary syndrome. Clinical Trials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00089895. Updated December 17, 2008. Accessed December 18, 2008.
- Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2007; 50:e1–e157.
- ACTION Registry–GWTG. National Cardiovascular Data Registry Web site. http://www.ncdr.com/WebNCDR/Action/default.aspx. Accessed December 22, 2008.
- Alexander KP, Chen AY, Roe MT, et al. Excess dosing of antiplatelet and antithrombin agents in the treatment of non-ST-segment elevation acute coronary syndromes. JAMA 2005; 294:3108–3116.
- Cohen M, Demers C, Gurfinkel EP, et al. A comparison of low-molecular-weight heparin with unfractionated heparin for unstable coronary artery disease: Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q-Wave Coronary Events Study Group. N Engl J Med 1997; 337:447–452.
- Petersen JL, Mahaffey KW, Hasselblad V, et al. Efficacy and bleeding complications among patients randomized to enoxaparin or unfractionated heparin for antithrombin therapy in non-ST-segment elevation acute coronary syndromes: a systematic overview. JAMA 2004; 292:89–96.
- The PURSUIT Trial Investigators. Inhibition of platelet glycoprotein IIb/IIIa with eptifibatide in patients with acute coronary syndromes. N Engl J Med 1998; 339:436–443.
- Moscucci M, Fox KA, Cannon CP, et al. Predictors of major bleeding in acute coronary syndromes: the Global Registry of Acute Coronary Events (GRACE). Eur Heart J 2003; 24:1815–1823.
- Peters RJ, Mehta SR, Fox KA, et al. Effects of aspirin dose when used alone or in combination with clopidogrel in patients with acute coronary syndromes: observations from the Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) study. Circulation 2003; 108:1682–1687.
- Alexander KP, Chen AY, Newby LK, et al. Sex differences in major bleeding with glycoprotein IIb/IIIa inhibitors: results from the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines) initiative. Circulation 2006; 114:1380–1387.
- Alexander KP, Chen AY, Roe MT, et al. Excess dosing of antiplatelet and antithrombin agents in the treatment of non-ST-segment elevation acute coronary syndromes. JAMA 2005; 294:3108–3116.
- Alexander KP, Chen AY, Roe MT, et al. Decline in GP 2b3a inhibitor overdosing with site-specific feedback in CRUSADE [AHA abstract 3527]. Circulation 2007; 116:II_798–II_799.
- Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics—2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2007; 115:e69–e171.
- Cairns JA, Gent M, Singer J, et al. Aspirin, sulfinpyrazone, or both in unstable angina: results of a Canadian multicenter trial. N Engl J Med 1985; 313:1369–1375.
- Lewis HD Jr, Davis JW, Archibald DG, et al. Protective effects of aspirin against acute myocardial infarction and death in men with unstable angina: results of a Veterans Administration Cooperative Study. N Engl J Med 1983; 309:396–403.
- Théroux P, Ouimet H, McCans J, et al. Aspirin, heparin, or both to treat acute unstable angina. N Engl J Med 1988; 319:1105–1111.
- Wallentin LC. Aspirin (75 mg/day) after an episode of unstable coronary artery disease: long-term effects on the risk for myocardial infarction, occurrence of severe angina and the need for revascularization: Research Group on Instability in Coronary Artery Disease in Southeast Sweden. J Am Coll Cardiol 1991; 18:1587–1593.
- Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomized trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002; 324:71–86.
- Yusuf S, Zhao F, Mehta SR, et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 2001; 345:494–502.
- Yusuf S, Mehta SR, Zhao F, et al. Early and late effects of clopidogrel in patients with acute coronary syndromes. Circulation 2003; 107:966–972.
- Fox KA, Mehta SR, Peters R, et al. Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non-ST-elevation acute coronary syndrome: the Clopidogrel in Unstable angina to prevent Recurrent ischemic Events (CURE) Trial. Circulation 2004; 110:1202–1208.
- CAPRIE Steering Committee. A randomized, blinded trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet 1996; 348:1329–1339.
- Bhatt DL, Fox KA, Hacke W, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med 2006; 354:1706–1717.
- Bhatt DL, Flather MD, Hacke W, et al. Patients with prior myocardial infarction, stroke, or symptomatic peripheral arterial disease in the CHARISMA trial. J Am Coll Cardiol 2007; 49:1982–1988.
- Ho PM, Peterson ED, Wang L, et al. Incidence of death and acute myocardial infarction associated with stopping clopidogrel after acute coronary syndrome. JAMA 2008; 299:532–539.
- Boersma E, Harrington RA, Moliterno DJ, et al. Platelet glycoprotein IIb/IIIa inhibitors in acute coronary syndromes: a meta-analysis of all major randomised clinical trials. Lancet 2002; 359:189–198.
- Simoons ML, GUSTO IV-ACS Investigators. Effect of glycoprotein IIb/IIIa receptor blocker abciximab on outcome in patients with acute coronary syndromes without early coronary revascularisation: the GUSTO IV-ACS randomised trial. Lancet 2001; 357:1915–1924.
- Boersma E, Akkerhuis KM, Théroux P, Calif RM, Topol EJ, Simoons ML. Platelet glycoprotein IIb/IIIa receptor inhibition in non-ST-elevation acute coronary syndromes: early benefit during medical treatment only, with additional protection during percutaneous coronary intervention. Circulation 1999; 100:2045–2048.
- White HD, Ohman EM, Lincoff AM, et al. Safety and efficacy of bivalirudin with and without glycoprotein IIb/IIIa inhibitors in patients with acute coronary syndromes undergoing percutaneous coronary intervention. J Am Coll Cardiol 2008; 52:807–814.
- EARLY-ACS: glycoprotein IIb/IIIa inhibition in patients with non-ST-segment elevation acute coronary syndrome. Clinical Trials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00089895. Updated December 17, 2008. Accessed December 18, 2008.
- Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2007; 50:e1–e157.
- ACTION Registry–GWTG. National Cardiovascular Data Registry Web site. http://www.ncdr.com/WebNCDR/Action/default.aspx. Accessed December 22, 2008.
- Alexander KP, Chen AY, Roe MT, et al. Excess dosing of antiplatelet and antithrombin agents in the treatment of non-ST-segment elevation acute coronary syndromes. JAMA 2005; 294:3108–3116.
- Cohen M, Demers C, Gurfinkel EP, et al. A comparison of low-molecular-weight heparin with unfractionated heparin for unstable coronary artery disease: Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q-Wave Coronary Events Study Group. N Engl J Med 1997; 337:447–452.
- Petersen JL, Mahaffey KW, Hasselblad V, et al. Efficacy and bleeding complications among patients randomized to enoxaparin or unfractionated heparin for antithrombin therapy in non-ST-segment elevation acute coronary syndromes: a systematic overview. JAMA 2004; 292:89–96.
- The PURSUIT Trial Investigators. Inhibition of platelet glycoprotein IIb/IIIa with eptifibatide in patients with acute coronary syndromes. N Engl J Med 1998; 339:436–443.
- Moscucci M, Fox KA, Cannon CP, et al. Predictors of major bleeding in acute coronary syndromes: the Global Registry of Acute Coronary Events (GRACE). Eur Heart J 2003; 24:1815–1823.
- Peters RJ, Mehta SR, Fox KA, et al. Effects of aspirin dose when used alone or in combination with clopidogrel in patients with acute coronary syndromes: observations from the Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) study. Circulation 2003; 108:1682–1687.
- Alexander KP, Chen AY, Newby LK, et al. Sex differences in major bleeding with glycoprotein IIb/IIIa inhibitors: results from the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines) initiative. Circulation 2006; 114:1380–1387.
- Alexander KP, Chen AY, Roe MT, et al. Excess dosing of antiplatelet and antithrombin agents in the treatment of non-ST-segment elevation acute coronary syndromes. JAMA 2005; 294:3108–3116.
- Alexander KP, Chen AY, Roe MT, et al. Decline in GP 2b3a inhibitor overdosing with site-specific feedback in CRUSADE [AHA abstract 3527]. Circulation 2007; 116:II_798–II_799.
KEY POINTS
- Recurrent ischemic events have been observed in all antiplatelet trials to date, in spite of the addition of more potent antiplatelet regimens.
- There appears to be a gradient of benefit from dual antiplatelet therapy depending on patients’ risk of thrombotic events (the greater the risk, the greater the benefit).
- Local practice patterns in interventional therapy for ACS should be taken into consideration when applying results from clinical trials to clinical practice.
- ACS patients who stand to benefit most from antiplatelet therapies also are at the greatest risk of bleeding from those therapies.
- The importance of a tailored approach to antiplatelet therapy and dosing is becoming more widely recognized.
Platelet response in practice: Applying new insights and tools for testing and treatment
CASE STUDY: THROMBOSIS AFTER STENTING DESPITE ANTIPLATELET THERAPY
Dr. Deepak Bhatt: We have taken in a wealth of terrific information from the three preceding talks in this symposium. Let’s now share some questions from the audience and explore some of the points raised in the preceding talks in a bit more practical detail for clinicians. Our three prior speakers are joined in this panel discussion by Cleveland Clinic’s Dr. Frank Peacock, who brings an emergency medicine perspective.
Let’s begin with a case-based question supplied from the audience. The patient is a 42-year-old morbidly obese man without diabetes who had a non-ST-elevation myocardial infarction (MI) less than 1 year ago. A drug-eluting stent was placed at the time of his MI, and now restenosis has occurred. He is on aspirin and clopidogrel 75 mg/day. Do you recommend running a vasodilator-stimulated phosphoprotein (VASP) test and possibly increasing the clopidogrel dose to 150 mg/ day, or should the patient just be switched to prasugrel (assuming it is commercially available) without running the VASP test?
I’ll take a quick initial stab at this question. Studies of antiplatelet therapies to prevent instent restenosis have been a mixed bag. Some of the trials with glycoprotein IIb/IIIa inhibitors have shown an effect on restenosis, but most have not. Similarly, some of the analyses of the thienopyridines ticlopodine and clopidogrel have shown an effect on restenosis, but most have not.
For the most part, restenosis does not appear to be heavily mediated by platelets, at least not in a way that we can influence by therapy. On the other hand, stent thrombosis is highly platelet mediated, so I would alter the case to one in which stent thrombosis is the clinical problem. Assuming that the patient has been adherent to his antiplatelet regimen, which tests would you perform, and how would you act on the information from those tests?
Dr. Kandice Kottke-Marchant: The 2007 guidelines on acute coronary syndrome (ACS) management from the American College of Cardiology and American Heart Association (ACC/AHA)1 do not address platelet function testing, and almost none of the clinical trials of antiplatelet agents had an arm that included testing and dose adjustment based on platelet function studies. Platelet testing is available at some centers; at Cleveland Clinic, we use platelet aggregation testing. One can do platelet aggregation testing on a patient-by-patient basis; if inhibition appears to be suboptimal, a treatment decision should be made, but there is little guidance from the literature to steer that decision. I have seen clinicians increase the dose of clopidogrel or aspirin in response to platelet function tests, which occasionally triggers a confirmatory call from the pharmacy department.
Dr. Bhatt: When I was still at Cleveland Clinic, our chief medical resident did an analysis of platelet function testing, and it was remarkable how much testing was performed and how often it changed management, largely in the absence of any outcomes data, as Dr. Kottke-Marchant pointed out. Dr. Alexander, what are your recommendations with respect to platelet function testing today?
Dr. John Alexander: The case you describe is one in which applying evidence is not easy. There are no trials to supply any evidence to change therapy in this patient, a morbidly obese man receiving 75 mg/day of clopidogrel. There is certainly a rationale, however, to believe that a standard “one size fits all” 75-mg daily dose of clopidogrel may not be enough for him. The trade-off with a higher dosage is a higher risk of bleeding, however, so I would first be sure that he has been adherent to his current regimen of clopidogrel and aspirin.
Dr. Bhatt: Is there a role for point-of-care testing to determine whether he is adherent to the medicines?
Dr. Kottke-Marchant: Several of the point-of-care tests, such as the VerifyNow rapid platelet function analyzer, have specific cartridges for aspirin and for clopidogrel. If platelets were not being inhibited, it would suggest that the doses were too low, given the patient’s weight, but you probably would not be able to determine whether he was resistant to clopidogrel.
Dr. W. Frank Peacock: One way to verify that patients are taking their aspirin is to take a small urine sample and squirt in 2 mL of ferric chloride. If the sample turns purple, it means they are taking their aspirin. Once that is established, you can try to determine whether the drug is working on their platelets.
Dr. Alexander: Another potential explanation for stent thrombosis is faulty stent placement. In this case I would consider asking an interventional colleague to perform intravascular ultrasonography to make sure the stent was implanted properly before I changed the patient’s antithrombotic therapy.
Dr. Bhatt: That’s a great technical point. We always want to make sure that a case of stent thrombosis is not due to a mechanical problem. We should be asking: Is the stent properly sized and well opposed? Is there a distal dissection or any other issue that could predispose to stent thrombosis?
Dr. Alexander: This case illustrates a host of other challenges that underscore how much more work we need to do to define optimal antiplatelet therapy. Suppose we perform platelet function testing and find a low level of platelet inhibition in this patient with stent thrombosis, and we change his antiplatelet regimen. When should we test him again? If we retest in 3 months and find that he has a higher than expected level of platelet inhibition on the new antiplatelet regimen, do we dial down the intensity? Once again, there is no evidence to guide these decisions, and levels of platelet inhibition are driven not just by the medications but also by what is going on in the patient’s platelets—it is quite multifactorial.
POINT-OF-CARE PLATELET FUNCTION TESTING: CURRENT LIMITS, FUTURE ROLES
Dr. Bhatt: While we’re discussing platelet function testing, I found it interesting, Dr. Kottke-Marchant, that you said the use of bleeding time as a platelet test is finally going away. Testing of bleeding time has been around forever, but I agree that it doesn’t have much value in clinical practice. Do you think bleeding time will continue to have any role in drug development? Most phase 2 trials, and certainly phase 1 trials, still capture bleeding time to assess whether or not a drug is working. Should that, too, be jettisoned, or does bleeding time still have some merit in this context?
Dr. Kottke-Marchant: I would jettison it in drug development as well because of the considerable variability in bleeding time. It is not a test that can be standardized, and no quality control can be done. The results depend on skin turgor, age, and many other variables.
We need a global assay that will pick up multiple aspects of platelet function, such as flow-based adhesion, aggregation, and granule release. The bleeding time is a shear-dependent test, whereas the platelet aggregation test that is used in most drug trials is an artificial assay that measures only aggregation, but not under shear. The VerifyNow rapid platelet function analyzer does not measure platelets under shear and is not a global assay.
Dr. Marc Sabatine: I would underscore the need for a reliable point-of-care test of platelet function. When we prescribe a statin or an antihypertensive drug, we don’t just send the patient out the door and hope that everything will be okay. We measure the response, knowing that genotype, environmental factors, or medication factors can affect the response. When we prescribe an antiplatelet drug, we need a reliable point-of-care device to make certain that the patient is getting appropriate platelet inhibition.
I am reminded of a recent study of point-of-care measurement of platelet inhibition in patients receiving clopidogrel prior to nonemergent percutaneous coronary intervention (PCI).2 Rather than just treating patients with PCI and sending them out the door, the investigators kept giving patients clopidogrel and measuring their platelet inhibition until they achieved an appropriate degree of inhibition, after which PCI was performed. Event rates were significantly reduced in the patient group treated this way, which suggests a need to individualize therapy and move away from the “one size fits all” mindset.
Dr. Bhatt: Dr. Peacock, you’ve led a study of point-of-care assays in the emergency department. What might ultimately be the role of point-of-care testing in emergency medicine, and might it influence drug selection?
Dr. Peacock: My short answer is that I think there will be a role for point-of-care testing, with all the caveats that have been discussed. There may even be a day when we do genetic testing and look for DNA. Honestly, though, I’m somewhat of a skeptic because I’m not looking at the genetics. I see many patients who do crack cocaine who come to the emergency room with chest pain and have risk factors, but I send these patients home because they are not having an event. The real question is, “Is it an event?” If a patient is having an event and he or she has platelet resistance or hyperreactivity—whatever we term it—then you have to decide the next step.
As you mentioned, we just completed a study that evaluated a couple hundred patients for platelet inhibition resistance to aspirin, and one finding was that the incidence of platelet resistance to aspirin was much lower than we had anticipated. Studies from the literature suggest that the prevalence of resistance is around 30%, but in our study it was 6.5%.3
Dr. Kottke-Marchant: It depends on how and in whom you measure resistance. Different tests will give you different numbers. Even among studies using the same measurement techniques, the results depend on the patient population. If it’s a fairly stable cardiac population, you may see aspirin resistance rates of 4% or 5%. If it’s a population of patients who have had multiple MIs, the rate may be higher.
Dr. Peacock: That’s exactly my point. In the emergency department we see a mixed bag. We see many people who have had no prior events and have no acute event occurring. So in that setting you are going to get results that suggest that no intervention is required, whereas in that small percentage of patients in whom something is happening, your drug choice may be different.
Dr. Alexander: We are still talking about resistance to antiplatelet drugs as though it were a patient-level variable, but it’s my impression that it changes over time and within a patient.
Dr. Kottke-Marchant: It can change over time. There aren’t many good longitudinal studies. Most of the studies of “aspirin resistance” are really snapshot studies with measurements taken at one point in time. A term I prefer is “platelet reactivity.” To really assess treatment efficacy, we are going to have to look at the basal level of platelet reactivity.
WHAT ROLE FOR GENOTYPING IN GUIDING ANTIPLATELET THERAPY?
Dr. Bhatt: Dr. Peacock alluded to a potential role for genetic testing. Dr. Sabatine, you have done a lot of interesting work with genotyping in the TRITON-TIMI 38 study of prasugrel and clopidogrel. What is the future role of genotyping in determining which antiplatelet therapy is best for which patient?
Dr. Sabatine: As I mentioned, cytochrome P450 enzymes play a critical role in the metabolism of clopidogrel. These enzymes are fairly polymorphic—mutations in their encoding genes are responsible for subtle changes in effect, unlike the traditional mutations that we think about for sickle cell disease, for example. A wealth of data has been published showing that genetic variants are associated with decreased functional activity of cytochrome P450 enzymes, demonstrating the pharmacologic importance of these variants.
Individuals who carry variant alleles appear to respond differently to clopidogrel. A variety of small studies show that those who carry specific variants—particularly in the CYP2C19 enzyme, but in other enzymes as well—appear to have a diminished response to clopidogrel. There are also data showing that individuals with a diminished response to clopidogrel have worse outcomes.4 Our group is studying the impact of genetic variants that decrease the functional activity of cytochrome P450 enzymes on clinical outcomes. (Editor’s note: This study has since been published by Mega et al.5)
The practical implication may lie in point-of-care genotyping, which appears possible and will be clinically useful if a strong link can be demonstrated between genotype and outcomes. If point-of-care genotyping becomes practical, it will raise the question of whether both genotyping and platelet aggregation testing are needed. I think they might indeed be complementary in risk prediction, as is the case with genetic variants that affect low-density lipoprotein cholesterol (LDL-C) levels. In the lipid arena, we have seen that genetic effects and lipid levels provide independent incremental information about risk. That’s because of the high degree of variation in LDL-C levels: an LDL-C measurement is a snapshot in time, yet a variety of factors can influence LDL-C levels. In contrast, genotype is an invariant factor. Similarly, in the platelet arena, platelet aggregation studies and genotyping may be synergistic in predicting an individual’s predisposition to events and response to medications.
Dr. Bhatt: While we’re discussing pathways of metabolism, the literature, though scant, suggests a potential interaction between proton pump inhibitors and clopidogrel. I was co-chair of a recent American College of Cardiology/ American Heart Association/American College of Gastro-enterology consensus document that endorsed liberal use of proton pump inhibitors in patients who are at gastrointestinal risk, including those on antiplatelet therapy.6 The gastroenterologists believed strongly that proton pump inhibitors were safe and in fact underused in these patients. What do you think about the clopidogrel–proton pump inhibitor interaction? Should we be concerned?
Dr. Sabatine: Proton pump inhibitors are not only substrates for, but also inhibitors of, CYP2C19, a key enzyme that helps transform clopidogrel into an active metabolite. For this reason, there has been interest in whether concomitant use of proton pump inhibitors would blunt the efficacy of clopidogrel. The same concern was raised about giving clopidogrel with certain statin drugs that are also metabolized by the cytochrome P450 system, and several studies have shown an effect of these statins on clopidogrel’s platelet inhibition. However, there is no evidence that coadministration of these statins has affected clinical outcomes with clopidogrel in clinical trials. So it may be that while competition for the cytochrome P450 system is one factor, it’s not enough of a factor to tip the scale and result in a clinical event. The same may be true of coadministration of proton pump inhibitors; meanwhile, we await definitive data that concomitant use with clopidogrel leads to higher rates of ischemic events.
DIAGNOSTIC UNCERTAINTY IN THE EMERGENCY SETTING
Dr. Bhatt: We heard about quite a few new antiplatelet drugs in Dr. Sabatine’s presentation, some of which will likely be taken up in clinical practice. Dr. Peacock, from an emergency department perspective, how will you integrate all these new agents with the numerous therapies already available? What should emergency departments do to come to grips with and ultimately take advantage of these different forms of therapy as well as emerging platelet function tests?
Dr. Peacock: The piece that’s unique or especially pertinent to the emergency department is diagnostic uncertainty. Diagnosis and management are easy when a patient has an ST-elevation MI because we all know what that looks like and we know what to do in response. To some extent non-ST-elevation MI is fairly simple too. ACS is a lot more difficult because we don’t have a good definition for unstable angina, and that’s where diagnosis and management become problematic. And with high-sensitivity troponins coming out now, the question of non-ST-elevation MI is going to get more and more confusing because we will have a lot more patients who meet criteria without having an acute coronary artery event.
So it is going to be important that studies be designed correctly. A lot of the studies reviewed today were efficacy studies, showing that a particular drug works well in a carefully defined population, but they were not efficiency studies: they did not take into account the real-world diagnostic uncertainty—and inevitable misdiagnoses—that emergency departments encounter before starting therapy.
Take the CURE trial, for example. It was a great study, showing that clopidogrel reduced the hazard ratio for major coronary events by 20% in patients with unstable angina,7 and the message was that everybody should be using clopidogrel. A close look at the study, however, reveals that about half the patients did not receive clopidogrel in the emergency department. When patients did receive it early, it was driven by the cardiologist, who was absolutely certain of the diagnosis. But if the study was not designed to test early use, then it is a big leap to extrapolate its findings to this circumstance.
Many of the patients in the CURE trial were enrolled the day after presentation, when their diagnosis was certain—ie, they had a rise in troponin after their symptoms. But when a patient first arrives in the emergency department, we are not certain of the diagnosis. And if we use a drug such as clopidogrel, with a duration of action as long as 5 days, we have committed the entire medical system to a certain course of management for that period of time. If we get the diagnosis wrong, this commitment could restrict management options for up to 5 days.
The question for emergency physicians becomes, “How long is long enough to know whether I can pull the trigger on a therapy and be correct?” With all the new drugs coming along, the way to answer this is to do efficiency studies in a real-world environment in addition to efficacy studies.
Dr. Alexander: Yes, one of the biggest limitations of antiplatelet drug studies to date is that they usually haven’t really addressed the timing of drug initiation. We often assume that if a drug is shown to be beneficial, then it should be started as soon as possible. As we just heard, that may have been an unfounded extrapolation from the CURE trial. The same sort of thing happened with the ISIS trial of aspirin in patients with ST-elevation MI.8 In response to the ISIS results, clinicians rushed to give patients aspirin right away even though many of the patients in the trial may have received their aspirin the day after presentation. For these reasons, the EARLY-ACS study,9 which is addressing a very simple question—whether early upstream use of glycoprotein IIb/IIIa inhibitors is beneficial—has been a challenging trial to complete.
WHAT ROLE FOR THIENOPYRIDINE PRETREATMENT?
Dr. Bhatt: Dr. Sabatine, you presented data from the large TRITON-TIMI 38 trial comparing prasugrel with clopidogrel. I’m interested in how you would use prasugrel in practice, assuming it receives marketing approval, especially in light of its bleeding risk, particularly in patients in whom coronary artery bypass graft surgery (CABG) is planned. Many hospitals pretreat patients with clopidogrel in the emergency department. How would you manage a patient who shows up in the emergency room with ACS? Would you give clopidogrel, would you wait and give prasugrel, or would you do something else? If you gave clopidogrel, what loading dose would you use—300 mg, 600 mg, or, as some have suggested, 900 or 1,200 mg?
Dr. Sabatine: I am a strong proponent of pretreatment. Data from multiple studies show a benefit to this strategy, and even the original CURE trial showed a roughly 30% reduction in ischemic events within the first 24 hours of clopidogrel initiation.7
I think the dosing strategy depends on how the patient is going to be managed. If management is going to be conservative, then I would start the patient on 300 mg of clopidogrel when he or she came in. If the patient is going to the cardiac catheterization laboratory in a few hours, I would pretreat with 600 mg of clopidogrel. For prasugrel, the need for pretreatment is less clear, given the drug’s faster onset of action and greater degree of platelet inhibition. In the TRITON-TIMI 38 study,10 prasugrel was given, by and large, after diagnostic angiography, and thus one could use that approach in practice.
In terms of clopidogrel versus prasugrel, I would embrace prasugrel for the large majority of my patients, being mindful of the risk of bleeding. I would not hesitate to give the medication to diabetics or to younger, more robust patients. The 50% reduction in stent thrombosis with prasugrel versus clopidogrel in TRITON-TIMI 38 is huge,11 given that the risk of death with stent thrombosis is probably 25% or greater. So I would want to have prasugrel on board to reduce the risk of stent thrombosis, especially if a drug-eluting stent were being implanted.
Dr. Bhatt: Dr. Alexander, let’s get your take on a similar scenario. Assuming that prasugrel gains marketing approval, how would you manage patients with non-ST-elevation MI who present to the emergency department? Would you pretreat with clopidogrel? Would you wait until angiography and then, depending on the anatomy, treat with prasugrel? Or would you potentially pretreat with prasugrel, which has not been studied and would not be a labeled indication? How would you reconcile the data?
Dr. Alexander: At Duke, I expect that prasugrel will not be used prior to the catheterization laboratory in patients with non-ST-elevation ACS due to concerns about whether the patients will undergo PCI or be managed medically or with CABG.
Dr. Bhatt: That makes sense, since there was a fair amount of bleeding with prasugrel in those patients in TRITON-TIMI 38.
Dr. Alexander: Correct. Moreover, at Duke we don’t use as much upstream clopidogrel as we would, based on the evidence, if I were managing all the patients. There is still a lot of pushback about upstream clopidogrel from our surgeons because patients are going to surgery quickly these days, sometimes just a day after catheterization, and that’s when a loading dose of clopidogrel can be problematic. We are also still fairly heavy users of glycoprotein IIb/IIIa inhibitors.
Where I can see prasugrel being used prior to the cath lab at Duke is in ST-elevation MI, where the rate of PCI is very high. In primary angioplasty for ST-elevation MI, it would likely be given upstream. The bigger issue for us will be that we serve as a referral base for a lot of regional hospitals, and thus have some influence on their practices.
Dr. Bhatt: In that case, what would you advise those regional hospitals to do for non-ST-elevation MI?
Dr. Alexander: For the time being, we would advise continuing with our current practice, which is to load clopidogrel in patients in whom there is a reasonable certainty that CABG will not be performed, and to use glycoprotein IIb/IIIa inhibitors in high-risk patients. As we get more experience with prasugrel or with additional trial results, however, that practice could easily change.
Dr. Bhatt: So you would still use glycoprotein IIb/IIIa inhibitors?
Dr. Alexander: Yes, I advocate upstream clopidogrel use, but not all my colleagues do. Based on the guidelines, I’d use one or the other—either clopidogrel or a glycoprotein IIb/IIIa inhibitor. As I mentioned in my talk, if a patient is at high risk for bleeding, I am more inclined to use clopidogrel, although patients at higher risk of bleeding are often at higher risk for ischemic events as well.
WHAT’S DRIVEN THE DROPOFF IN GLYCOPROTEIN IIb/IIIa INHIBITOR USE?
Dr. Bhatt: While we’re on the topic of glycoprotein IIb/IIIa inhibitors, a question card from the audience asks why there has been a decrease in glycoprotein IIb/ IIIa inhibitor use and whether this decline is appropriate or inappropriate. Have clopidogrel pretreatment, higher loading doses of clopidogrel, and use of the direct thrombin inhibitor bivalirudin contributed to the decrease in glycoprotein IIb/IIIa inhibitor use?
Dr. Alexander: I do think that the decline has been driven by the changing environment, with greater use of other antithrombotic strategies that include clopidogrel and bivalirudin, as you suggest, as well as an increased attention to bleeding. From an evidence-based standpoint, we don’t know whether the decrease in glycoprotein IIb/IIIa use is appropriate or not because the studies of these agents were conducted before the widespread upstream use of clopidogrel and bivalirudin. Clopidogrel is attractive because it’s a pill given as one dose in the emergency department, the wards, or the catheterization laboratory, rather than a much more complicated infusion with weight-based dosing and dosage adjustments based on creatinine clearance. It is possible that we should perhaps be dosing clopidogrel the same way, but we don’t know that yet.
PRASUGREL IN PRACTICE: HOW LOW CAN THE DOSE GO, AND IS THERE A GENDER EFFECT?
Dr. Bhatt: Let’s stick with this focus on dosing but turn back to discussion of prasugrel. In your presentation of the TRITON-TIMI 38 data, Dr. Sabatine, you proposed a potential prasugrel dosage modification, down to a 5-mg loading dose, in subgroups that were identified as being at high bleeding risk—namely, elderly patients and patients with low body weight. However, no outcomes data with 5 mg of prasugrel came out of TRITON-TIMI 38.10 Is this proposed modification based on pharmacokinetic extrapolation? Could clinicians be comfortable using 5 mg of prasugrel, assuming the drug receives regulatory approval and a 5-mg tablet would be available?
Dr. Sabatine: Of course, evidence at the grade A level would consist of a trial showing that patients who received a lower dose enjoyed the same benefit as those who got standard dosing in TRITON-TIMI 38—a 60-mg loading dose followed by 10 mg/day—with an acceptable risk profile. However, such a trial would be difficult and costly to conduct, and would take roughly half a decade to pull off. It is only through large trials like TRITON-TIMI 38 that you identify subgroups that respond differently, and then to go back and do a separate trial for those subgroups takes a great deal of time. It may not be practical.
I think the Food and Drug Administration is moving toward embracing careful pharmacokinetic/pharmacodynamic substudies within trials, with these substudies having adequate numbers of subjects to provide a sense for the ideal target dose and what an acceptable dose range would be, without limiting approval to a single dose. The analogy would be warfarin dosing, with the aim being to figure out an acceptable dose range, discover which patients fall outside that range, and then model the effect of a lower dose in those patients. Thus, approving a 5-mg dose of prasugrel based on TRITON-TIMI 38 would be a reasonable approach if this dose passed muster under pharmacokinetic/pharmacodynamic modeling. If this approach were taken, there would clearly be a need for postmarketing surveillance to confirm whether the modeling on the effects of the lower dose was borne out by actual outcomes.
Dr. Bhatt: The audience has posed another interesting question raised by TRITON-TIMI 38: Can you comment on the lesser effect of prasugrel in women?
Dr. Sabatine: It is true that there was not a statistically significant effect of prasugrel among women in TRITON-TIMI 38, but statistical tests among subgroups found no significant heterogeneity for the effect between men and women, and that is the relevant measure to determine any gender effect. Keep in mind that not all subgroups represent a univariate slice of the population. For example, women generally have lower body weight than men, and since prasugrel’s net clinical benefit was reduced in patients with lower body weight, that may explain some of the differing extent of effect between men and women.
Dr. Bhatt: That’s a good point about the lack of heterogeneity between men and women. In fact, a meta-analysis of clopidogrel data conducted by one of the fellows I work with revealed that men and women appear to benefit similarly from clopidogrel.12 There was a slight signal of excess bleeding in women, but there were more elderly women in the pooled population, which may have been a confounding factor. As best as anyone can tell, antiplate-let therapy works well in both men and women.
NAVIGATING MANAGEMENT ACROSS THE SPECTRUM OF CARE
Dr. Bhatt: I would like to explore a bit further how all of these issues translate across the spectrum of care, beginning in the emergency department, which we know is a key component of the entire ACS management strategy for a health care system. What should emergency medicine doctors do, given all of the potential options—clopidogrel, different loading doses of clopidogrel, prasugrel, glycoprotein IIb/IIIa inhibitors, even bivalirudin?
Dr. Peacock: It depends on the practice setting. Some emergency physicians work at community hospitals with no backup. They must have relationships with the larger centers to which they’ll be transferring patients, because ACS patients should not be staying at community hospitals. These emergency physicians must have close relationships with the physicians who will be receiving their patients, and they know the potential head-butting with surgeons surrounding early clopidogrel use better than anybody does. If they treat with clopidogrel in the emergency room, and it turns out that the patient needs to go to the catheterization laboratory, can the receiving hospital use platelet testing to shorten the standard 5-day interval from treatment to catheterization?
Dr. Bhatt: Yes, that’s a rather useful, although not completely validated, way of using point-of-care platelet testing—to potentially reduce the time to surgery.
Dr. Peacock: Right. So if the policies for handling these types of transfer-related issues are worked out in advance, all players have a pathway to follow, which can allow quick action when necessary. If you don’t have these issues worked out in advance, you either lose many opportunities to act quickly in the emergency room or you risk taking actions that will cause problems later in the course of management.
Dr. Alexander: I totally agree. The key is to sit down with all the players involved—the surgeons, the interventional cardiologists, the intensivists, the emergency room personnel—and come up with strategies for different populations of patients. Write down the collective strategy and hang it on the wall so that everybody can be comfortable with it. The strategy can be reevaluated when prasugrel or other new antithrombotic drugs come on the market.
Dr. Peacock: The other environment is the academic center, which is even more challenging, but for different reasons. At a large academic center like the Cleveland Clinic, any of 25 different cardiologists may be taking call and receiving patients from the emergency department on a particular night. A lot of phone interaction is required to elicit the planned management strategy, including if and when the patient will be going to the cath lab. Individualizing care to a particular cardiologist then becomes a time-consuming challenge, especially in clinical situations where outcomes are time-dependent.
Dr. Alexander: Agreed. Management needs to be integrated across the entire spectrum of care. The anticoagulants that we plan to use in the cath lab will affect the antithrombotic regimen used upstream.
Dr. Kottke-Marchant: One circumstance where platelet function testing has been helpful is in determining the washout of the clopidogrel effect before surgery. At Cleveland Clinic, we have implemented platelet function testing in this circumstance instead of waiting a blanket 5 days after clopidogrel administration to go to surgery. A return to normal platelet function on platelet aggregation testing, depending on the cutoff value used, is an indicator that the patient can proceed to surgery.
Dr. Bhatt: That’s a logical approach. How should we be using antiplatelet therapy in the medically managed patient, Dr. Alexander?
Dr. Alexander: When I think of medical management, I include patients who don’t go to the cath lab, but also those who do, with regards to their management prior to and following their time in the cath lab.
In patients who don’t go to the cath lab for angiography, the ACC/AHA guidelines recommend aspirin and either clopidogrel, a glycoprotein IIb/IIIa inhibitor, or both.1 In making this choice, I consider the patient’s risk of bleeding and the dosing complexity of the regimen, especially with the use of glycoprotein IIb/IIIa inhibitors in a patient with renal insufficiency. In a patient at relatively low risk for bleeding, I often use both clopidogrel and a glycoprotein IIb/IIIa inhibitor, although this strategy does not have a lot of data to support it.
The more challenging population consists of patients who go to the cath lab but do not undergo PCI; this population is managed medically too. We often drop the ball with clopidogrel in this population. Many patients in whom PCI is not performed do not receive clopidogrel upstream, for all of the reasons we’ve discussed, and there is pretty good evidence that if clopidogrel is not instituted before hospital discharge, the patient is not likely to be receiving it at 30 days either. We have an obligation to treat these patients.
Treatment following bypass surgery is much murkier, and I don’t really know what we should be doing. The ACC/AHA guidelines suggest that clopidogrel be started in a patient with non-ST-elevation ACS after bypass surgery,1 but I believe the evidence to support that recommendation is pretty weak.
Dr. Bhatt: Well, the CURE trial did contain a sizeable group that underwent bypass surgery,7 and although this group was underpowered in some respects, it was still a very large group, so I personally favor treatment in those patients. We should mention that an ongoing trial called TRILOGY ACS is comparing clopidogrel and prasugrel specifically in patients who are being managed medically,13 so more data on this strategy will be emerging.
ARE GUIDELINES DESTINED TO BECOME EVER MORE COMPLEX?
Dr. Bhatt: Here’s a comment and question from the audience that pulls together a lot of what we’ve discussed while also looking forward: The antiplatelet therapy guidelines are already complicated. If the ongoing studies of emerging antiplatelet drugs all have results that are qualitatively similar to those of the TRITON-TIMI 38 study of prasugrel—ie, better efficacy with more potent therapy but more bleeding—how do you foresee these antiplatelet drugs being used in clinical practice?
Dr. Sabatine: The contrast between the US guidelines and the European guidelines for ACS management is stark. The US guidelines—from the ACC and AHA1—are essentially an encyclopedia that includes nearly every trial of anti-platelet therapy in ACS along with complicated algorithms; they do a wonderful job of being complete. The European guidelines14 are probably one tenth the size of their US counterpart document, and they suggest treatments for various patient types; they are very simple.
In a sense, the US guidelines lay out the data and force practitioners to evaluate the trials and consider how our patients fit into the study populations. In this way they are analogous to current guidelines for anticoagulant therapy. Several anticoagulants have been compared with heparin in clinical trials. These newer anticoagulants appear to reduce the risk of ischemic events compared with heparin; some have lower rates of bleeding, while others have higher rates of bleeding. There have been few head-to-head studies of these agents, however, so we wind up with guidelines that are not definitive but rather suggest agents to “consider” in various settings.
It’s unlikely that a head-to-head trial will be conducted comparing prasugrel with the reversible P2Y12 antagonist AZD6140, assuming that both are approved for marketing. If the drugs appear equally efficacious in placebo-controlled trials, it will take consensus to determine the appropriate choice at your hospital, factoring in your patient profile, the cost of the drugs, and other variables. It’s more complicated when one agent is slightly more efficacious but causes more bleeding or, conversely, a little less efficacious but less apt to cause bleeding. In such cases, you may need to tailor therapy to the patient, trying to gauge bleeding risk. All of the emerging data appear to point to the importance of bleeding on outcomes: patients who bleed fare poorly, in part due to the bleeding itself and in part perhaps because they have a proclivity for bleeding.
THE FUTURE: MONITORING-BASED DOSING AND NICHE ANTIPLATELETS?
Dr. Bhatt: That’s a good observation. Let’s wrap up by having the other panelists share any final thoughts you may have.
Dr. Alexander: I’d like to return to the issue of measuring antiplatelet response and using it to guide therapy. Earlier we cited the examples of antihypertensive therapy and lipid-lowering therapy to support this model of monitoring-based treatment. Guidelines for dyslipidemia treatment recommend using LDL-C levels to guide therapy, but this practice is difficult to study in a randomized trial. In fact, none of the randomized trials of statins used LDL-C levels to guide therapy. They all studied fixed doses of statins versus placebo or fixed doses of another statin. Higher doses of statins were always beneficial compared with lower doses, and this finding was extrapolated into the guidelines as a justification to treat to target LDL-C levels.
Dr. Bhatt: It’s not even necessarily clear that LDL-C level is the best target, if you consider the JUPITER trial, in which patients received statin therapy based on their baseline level of high-sensitivity C-reactive protein, not their LDL-C level.15 It goes to show how incomplete our knowledge of a class of drugs may be, even decades after the drugs are introduced.
Dr. Kottke-Marchant: To speak to Dr. Alexander’s point, dose adjustment guided by platelet monitoring is a bit more problematic for antiplatelet drugs that are irreversible inhibitors, such as clopidogrel and aspirin, than for those that are reversible inhibitors, which are being developed and may eventually make more sense to use. From a drug development standpoint, a drug that requires monitoring and dose adjustment will not gain wide acceptance because it will increase medical costs and morbidity.
Dr. Bhatt: Yes, we know from experience with warfarin that doctors and patients don’t like the ongoing need for monitoring and testing.
Dr. Peacock: The drugs that are going to be adopted by the emergency department are those with the shortest half-lives, for several reasons: (1) using a drug with a short half-life won’t commit us to a particular course of action; (2) the potential for drug interactions is lower; and (3) in the event of an erroneous diagnosis, the consequence of misapplication may be mitigated by early recognition and termination of the drug. If we later decide that we’ve gone down the wrong therapeutic road or reached a wrong diagnosis, or if a complication occurs, we can turn off the therapy quickly. That level of flexibility is needed.
Dr. Kottke-Marchant: I think we are moving into an era of niche antiplatelet drugs. One might be used in a patient going to surgery, for example, and another for long-term therapy.
Dr. Peacock: One thing that I don’t have a feel for is how to transition from one drug to another. When you change drugs for a patient, it so often seems like it goes badly. If we’re eventually going to use drugs with ultra-short half-lives in the in the emergency department for the first day or two, and then switch patients to a pill for a week, a lot more platelet function testing may be needed.
- Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/ non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2007; 50:e1–e157.
- Bonello L, Camoin-Jau L, Arques S, et al. Adjusted clopidogrel loading doses according to vasodilator-stimulated phosphoprotein phosphorylation index decrease rate of major adverse cardiovascular events in patients with clopidogrel resistance: a multicenter randomized prospective study. J Am Coll Cardiol 2008; 51:1404–1411.
- Glauser J, Emerman CL, Bhatt DL, Peacock WF. Platelet aspirin resistance in emergency department patients with suspected acute coronary syndrome. Am J Emerg Med. In press
- Patti G, Nusca A, Mangiacapra F, Gatto L, D’Ambrosio A, Di Sciascio G. Point-of-care measurement of clopidogrel responsiveness predicts clinical outcome in patients undergoing percutaneous coronary intervention. J Am Coll Cardiol 2008; 52:1128–1133.
- Mega JL, Close SL, Wiviott SD, et al. Cytochrome P-450 polymorphisms and response to clopidogrel. N Engl J Med 2009; 360:354–362.
- Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use. J Am Coll Cardiol 2008; 52:1502–1517.
- Fox KA, Mehta SR, Peters R, et al. Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non-ST-elevation acute coronary syndrome: the Clopidogrel in Unstable angina to prevent Recurrent ischemic Events (CURE) Trial. Circulation 2004; 110:1202–1208.
- ISIS-2 Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Lancet 1988; 2:349–360.
- EARLY-ACS: Glycoprotein IIb/IIIa inhibition in patients with non-ST-segment elevation acute coronary syndrome. Clinical Trials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00089895. Updated December 17, 2008. Accessed December 18, 2008.
- Wiviott SD, Braunwald E, McCabe CH, et al; TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007; 357:2001–2015.
- Wiviott SD, Braunwald E, McCabe CH, et al. Intensive oral anti-platelet therapy for reduction of ischaemic events including stent thrombosis in patients with acute coronary dyndromes treated with percutaneous coronary intervention and stenting in the TRITON-TIMI 38 trial: a subanalysis of a randomised trial. Lancet 2008; 371:1353–1363.
- Berger JS, Bhatt DL, Chen Z, et al. The relationship between sex, mortality and cardiovascular events among patients with established cardiovascular disease: a meta-analysis [ACC abstract 1012-149]. J Am Coll Cardiol 2008; 51 10 suppl A:A247.
- TRILOGY ACS: A comparison of prasugrel and clopidogrel in acute coronary syndrome subjects. ClinicalTrials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00699998. Updated December 15, 2008. Accessed January 2, 2009.
- Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J 2007; 28:1598–1660.
- Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008; 359:2195–2207.
CASE STUDY: THROMBOSIS AFTER STENTING DESPITE ANTIPLATELET THERAPY
Dr. Deepak Bhatt: We have taken in a wealth of terrific information from the three preceding talks in this symposium. Let’s now share some questions from the audience and explore some of the points raised in the preceding talks in a bit more practical detail for clinicians. Our three prior speakers are joined in this panel discussion by Cleveland Clinic’s Dr. Frank Peacock, who brings an emergency medicine perspective.
Let’s begin with a case-based question supplied from the audience. The patient is a 42-year-old morbidly obese man without diabetes who had a non-ST-elevation myocardial infarction (MI) less than 1 year ago. A drug-eluting stent was placed at the time of his MI, and now restenosis has occurred. He is on aspirin and clopidogrel 75 mg/day. Do you recommend running a vasodilator-stimulated phosphoprotein (VASP) test and possibly increasing the clopidogrel dose to 150 mg/ day, or should the patient just be switched to prasugrel (assuming it is commercially available) without running the VASP test?
I’ll take a quick initial stab at this question. Studies of antiplatelet therapies to prevent instent restenosis have been a mixed bag. Some of the trials with glycoprotein IIb/IIIa inhibitors have shown an effect on restenosis, but most have not. Similarly, some of the analyses of the thienopyridines ticlopodine and clopidogrel have shown an effect on restenosis, but most have not.
For the most part, restenosis does not appear to be heavily mediated by platelets, at least not in a way that we can influence by therapy. On the other hand, stent thrombosis is highly platelet mediated, so I would alter the case to one in which stent thrombosis is the clinical problem. Assuming that the patient has been adherent to his antiplatelet regimen, which tests would you perform, and how would you act on the information from those tests?
Dr. Kandice Kottke-Marchant: The 2007 guidelines on acute coronary syndrome (ACS) management from the American College of Cardiology and American Heart Association (ACC/AHA)1 do not address platelet function testing, and almost none of the clinical trials of antiplatelet agents had an arm that included testing and dose adjustment based on platelet function studies. Platelet testing is available at some centers; at Cleveland Clinic, we use platelet aggregation testing. One can do platelet aggregation testing on a patient-by-patient basis; if inhibition appears to be suboptimal, a treatment decision should be made, but there is little guidance from the literature to steer that decision. I have seen clinicians increase the dose of clopidogrel or aspirin in response to platelet function tests, which occasionally triggers a confirmatory call from the pharmacy department.
Dr. Bhatt: When I was still at Cleveland Clinic, our chief medical resident did an analysis of platelet function testing, and it was remarkable how much testing was performed and how often it changed management, largely in the absence of any outcomes data, as Dr. Kottke-Marchant pointed out. Dr. Alexander, what are your recommendations with respect to platelet function testing today?
Dr. John Alexander: The case you describe is one in which applying evidence is not easy. There are no trials to supply any evidence to change therapy in this patient, a morbidly obese man receiving 75 mg/day of clopidogrel. There is certainly a rationale, however, to believe that a standard “one size fits all” 75-mg daily dose of clopidogrel may not be enough for him. The trade-off with a higher dosage is a higher risk of bleeding, however, so I would first be sure that he has been adherent to his current regimen of clopidogrel and aspirin.
Dr. Bhatt: Is there a role for point-of-care testing to determine whether he is adherent to the medicines?
Dr. Kottke-Marchant: Several of the point-of-care tests, such as the VerifyNow rapid platelet function analyzer, have specific cartridges for aspirin and for clopidogrel. If platelets were not being inhibited, it would suggest that the doses were too low, given the patient’s weight, but you probably would not be able to determine whether he was resistant to clopidogrel.
Dr. W. Frank Peacock: One way to verify that patients are taking their aspirin is to take a small urine sample and squirt in 2 mL of ferric chloride. If the sample turns purple, it means they are taking their aspirin. Once that is established, you can try to determine whether the drug is working on their platelets.
Dr. Alexander: Another potential explanation for stent thrombosis is faulty stent placement. In this case I would consider asking an interventional colleague to perform intravascular ultrasonography to make sure the stent was implanted properly before I changed the patient’s antithrombotic therapy.
Dr. Bhatt: That’s a great technical point. We always want to make sure that a case of stent thrombosis is not due to a mechanical problem. We should be asking: Is the stent properly sized and well opposed? Is there a distal dissection or any other issue that could predispose to stent thrombosis?
Dr. Alexander: This case illustrates a host of other challenges that underscore how much more work we need to do to define optimal antiplatelet therapy. Suppose we perform platelet function testing and find a low level of platelet inhibition in this patient with stent thrombosis, and we change his antiplatelet regimen. When should we test him again? If we retest in 3 months and find that he has a higher than expected level of platelet inhibition on the new antiplatelet regimen, do we dial down the intensity? Once again, there is no evidence to guide these decisions, and levels of platelet inhibition are driven not just by the medications but also by what is going on in the patient’s platelets—it is quite multifactorial.
POINT-OF-CARE PLATELET FUNCTION TESTING: CURRENT LIMITS, FUTURE ROLES
Dr. Bhatt: While we’re discussing platelet function testing, I found it interesting, Dr. Kottke-Marchant, that you said the use of bleeding time as a platelet test is finally going away. Testing of bleeding time has been around forever, but I agree that it doesn’t have much value in clinical practice. Do you think bleeding time will continue to have any role in drug development? Most phase 2 trials, and certainly phase 1 trials, still capture bleeding time to assess whether or not a drug is working. Should that, too, be jettisoned, or does bleeding time still have some merit in this context?
Dr. Kottke-Marchant: I would jettison it in drug development as well because of the considerable variability in bleeding time. It is not a test that can be standardized, and no quality control can be done. The results depend on skin turgor, age, and many other variables.
We need a global assay that will pick up multiple aspects of platelet function, such as flow-based adhesion, aggregation, and granule release. The bleeding time is a shear-dependent test, whereas the platelet aggregation test that is used in most drug trials is an artificial assay that measures only aggregation, but not under shear. The VerifyNow rapid platelet function analyzer does not measure platelets under shear and is not a global assay.
Dr. Marc Sabatine: I would underscore the need for a reliable point-of-care test of platelet function. When we prescribe a statin or an antihypertensive drug, we don’t just send the patient out the door and hope that everything will be okay. We measure the response, knowing that genotype, environmental factors, or medication factors can affect the response. When we prescribe an antiplatelet drug, we need a reliable point-of-care device to make certain that the patient is getting appropriate platelet inhibition.
I am reminded of a recent study of point-of-care measurement of platelet inhibition in patients receiving clopidogrel prior to nonemergent percutaneous coronary intervention (PCI).2 Rather than just treating patients with PCI and sending them out the door, the investigators kept giving patients clopidogrel and measuring their platelet inhibition until they achieved an appropriate degree of inhibition, after which PCI was performed. Event rates were significantly reduced in the patient group treated this way, which suggests a need to individualize therapy and move away from the “one size fits all” mindset.
Dr. Bhatt: Dr. Peacock, you’ve led a study of point-of-care assays in the emergency department. What might ultimately be the role of point-of-care testing in emergency medicine, and might it influence drug selection?
Dr. Peacock: My short answer is that I think there will be a role for point-of-care testing, with all the caveats that have been discussed. There may even be a day when we do genetic testing and look for DNA. Honestly, though, I’m somewhat of a skeptic because I’m not looking at the genetics. I see many patients who do crack cocaine who come to the emergency room with chest pain and have risk factors, but I send these patients home because they are not having an event. The real question is, “Is it an event?” If a patient is having an event and he or she has platelet resistance or hyperreactivity—whatever we term it—then you have to decide the next step.
As you mentioned, we just completed a study that evaluated a couple hundred patients for platelet inhibition resistance to aspirin, and one finding was that the incidence of platelet resistance to aspirin was much lower than we had anticipated. Studies from the literature suggest that the prevalence of resistance is around 30%, but in our study it was 6.5%.3
Dr. Kottke-Marchant: It depends on how and in whom you measure resistance. Different tests will give you different numbers. Even among studies using the same measurement techniques, the results depend on the patient population. If it’s a fairly stable cardiac population, you may see aspirin resistance rates of 4% or 5%. If it’s a population of patients who have had multiple MIs, the rate may be higher.
Dr. Peacock: That’s exactly my point. In the emergency department we see a mixed bag. We see many people who have had no prior events and have no acute event occurring. So in that setting you are going to get results that suggest that no intervention is required, whereas in that small percentage of patients in whom something is happening, your drug choice may be different.
Dr. Alexander: We are still talking about resistance to antiplatelet drugs as though it were a patient-level variable, but it’s my impression that it changes over time and within a patient.
Dr. Kottke-Marchant: It can change over time. There aren’t many good longitudinal studies. Most of the studies of “aspirin resistance” are really snapshot studies with measurements taken at one point in time. A term I prefer is “platelet reactivity.” To really assess treatment efficacy, we are going to have to look at the basal level of platelet reactivity.
WHAT ROLE FOR GENOTYPING IN GUIDING ANTIPLATELET THERAPY?
Dr. Bhatt: Dr. Peacock alluded to a potential role for genetic testing. Dr. Sabatine, you have done a lot of interesting work with genotyping in the TRITON-TIMI 38 study of prasugrel and clopidogrel. What is the future role of genotyping in determining which antiplatelet therapy is best for which patient?
Dr. Sabatine: As I mentioned, cytochrome P450 enzymes play a critical role in the metabolism of clopidogrel. These enzymes are fairly polymorphic—mutations in their encoding genes are responsible for subtle changes in effect, unlike the traditional mutations that we think about for sickle cell disease, for example. A wealth of data has been published showing that genetic variants are associated with decreased functional activity of cytochrome P450 enzymes, demonstrating the pharmacologic importance of these variants.
Individuals who carry variant alleles appear to respond differently to clopidogrel. A variety of small studies show that those who carry specific variants—particularly in the CYP2C19 enzyme, but in other enzymes as well—appear to have a diminished response to clopidogrel. There are also data showing that individuals with a diminished response to clopidogrel have worse outcomes.4 Our group is studying the impact of genetic variants that decrease the functional activity of cytochrome P450 enzymes on clinical outcomes. (Editor’s note: This study has since been published by Mega et al.5)
The practical implication may lie in point-of-care genotyping, which appears possible and will be clinically useful if a strong link can be demonstrated between genotype and outcomes. If point-of-care genotyping becomes practical, it will raise the question of whether both genotyping and platelet aggregation testing are needed. I think they might indeed be complementary in risk prediction, as is the case with genetic variants that affect low-density lipoprotein cholesterol (LDL-C) levels. In the lipid arena, we have seen that genetic effects and lipid levels provide independent incremental information about risk. That’s because of the high degree of variation in LDL-C levels: an LDL-C measurement is a snapshot in time, yet a variety of factors can influence LDL-C levels. In contrast, genotype is an invariant factor. Similarly, in the platelet arena, platelet aggregation studies and genotyping may be synergistic in predicting an individual’s predisposition to events and response to medications.
Dr. Bhatt: While we’re discussing pathways of metabolism, the literature, though scant, suggests a potential interaction between proton pump inhibitors and clopidogrel. I was co-chair of a recent American College of Cardiology/ American Heart Association/American College of Gastro-enterology consensus document that endorsed liberal use of proton pump inhibitors in patients who are at gastrointestinal risk, including those on antiplatelet therapy.6 The gastroenterologists believed strongly that proton pump inhibitors were safe and in fact underused in these patients. What do you think about the clopidogrel–proton pump inhibitor interaction? Should we be concerned?
Dr. Sabatine: Proton pump inhibitors are not only substrates for, but also inhibitors of, CYP2C19, a key enzyme that helps transform clopidogrel into an active metabolite. For this reason, there has been interest in whether concomitant use of proton pump inhibitors would blunt the efficacy of clopidogrel. The same concern was raised about giving clopidogrel with certain statin drugs that are also metabolized by the cytochrome P450 system, and several studies have shown an effect of these statins on clopidogrel’s platelet inhibition. However, there is no evidence that coadministration of these statins has affected clinical outcomes with clopidogrel in clinical trials. So it may be that while competition for the cytochrome P450 system is one factor, it’s not enough of a factor to tip the scale and result in a clinical event. The same may be true of coadministration of proton pump inhibitors; meanwhile, we await definitive data that concomitant use with clopidogrel leads to higher rates of ischemic events.
DIAGNOSTIC UNCERTAINTY IN THE EMERGENCY SETTING
Dr. Bhatt: We heard about quite a few new antiplatelet drugs in Dr. Sabatine’s presentation, some of which will likely be taken up in clinical practice. Dr. Peacock, from an emergency department perspective, how will you integrate all these new agents with the numerous therapies already available? What should emergency departments do to come to grips with and ultimately take advantage of these different forms of therapy as well as emerging platelet function tests?
Dr. Peacock: The piece that’s unique or especially pertinent to the emergency department is diagnostic uncertainty. Diagnosis and management are easy when a patient has an ST-elevation MI because we all know what that looks like and we know what to do in response. To some extent non-ST-elevation MI is fairly simple too. ACS is a lot more difficult because we don’t have a good definition for unstable angina, and that’s where diagnosis and management become problematic. And with high-sensitivity troponins coming out now, the question of non-ST-elevation MI is going to get more and more confusing because we will have a lot more patients who meet criteria without having an acute coronary artery event.
So it is going to be important that studies be designed correctly. A lot of the studies reviewed today were efficacy studies, showing that a particular drug works well in a carefully defined population, but they were not efficiency studies: they did not take into account the real-world diagnostic uncertainty—and inevitable misdiagnoses—that emergency departments encounter before starting therapy.
Take the CURE trial, for example. It was a great study, showing that clopidogrel reduced the hazard ratio for major coronary events by 20% in patients with unstable angina,7 and the message was that everybody should be using clopidogrel. A close look at the study, however, reveals that about half the patients did not receive clopidogrel in the emergency department. When patients did receive it early, it was driven by the cardiologist, who was absolutely certain of the diagnosis. But if the study was not designed to test early use, then it is a big leap to extrapolate its findings to this circumstance.
Many of the patients in the CURE trial were enrolled the day after presentation, when their diagnosis was certain—ie, they had a rise in troponin after their symptoms. But when a patient first arrives in the emergency department, we are not certain of the diagnosis. And if we use a drug such as clopidogrel, with a duration of action as long as 5 days, we have committed the entire medical system to a certain course of management for that period of time. If we get the diagnosis wrong, this commitment could restrict management options for up to 5 days.
The question for emergency physicians becomes, “How long is long enough to know whether I can pull the trigger on a therapy and be correct?” With all the new drugs coming along, the way to answer this is to do efficiency studies in a real-world environment in addition to efficacy studies.
Dr. Alexander: Yes, one of the biggest limitations of antiplatelet drug studies to date is that they usually haven’t really addressed the timing of drug initiation. We often assume that if a drug is shown to be beneficial, then it should be started as soon as possible. As we just heard, that may have been an unfounded extrapolation from the CURE trial. The same sort of thing happened with the ISIS trial of aspirin in patients with ST-elevation MI.8 In response to the ISIS results, clinicians rushed to give patients aspirin right away even though many of the patients in the trial may have received their aspirin the day after presentation. For these reasons, the EARLY-ACS study,9 which is addressing a very simple question—whether early upstream use of glycoprotein IIb/IIIa inhibitors is beneficial—has been a challenging trial to complete.
WHAT ROLE FOR THIENOPYRIDINE PRETREATMENT?
Dr. Bhatt: Dr. Sabatine, you presented data from the large TRITON-TIMI 38 trial comparing prasugrel with clopidogrel. I’m interested in how you would use prasugrel in practice, assuming it receives marketing approval, especially in light of its bleeding risk, particularly in patients in whom coronary artery bypass graft surgery (CABG) is planned. Many hospitals pretreat patients with clopidogrel in the emergency department. How would you manage a patient who shows up in the emergency room with ACS? Would you give clopidogrel, would you wait and give prasugrel, or would you do something else? If you gave clopidogrel, what loading dose would you use—300 mg, 600 mg, or, as some have suggested, 900 or 1,200 mg?
Dr. Sabatine: I am a strong proponent of pretreatment. Data from multiple studies show a benefit to this strategy, and even the original CURE trial showed a roughly 30% reduction in ischemic events within the first 24 hours of clopidogrel initiation.7
I think the dosing strategy depends on how the patient is going to be managed. If management is going to be conservative, then I would start the patient on 300 mg of clopidogrel when he or she came in. If the patient is going to the cardiac catheterization laboratory in a few hours, I would pretreat with 600 mg of clopidogrel. For prasugrel, the need for pretreatment is less clear, given the drug’s faster onset of action and greater degree of platelet inhibition. In the TRITON-TIMI 38 study,10 prasugrel was given, by and large, after diagnostic angiography, and thus one could use that approach in practice.
In terms of clopidogrel versus prasugrel, I would embrace prasugrel for the large majority of my patients, being mindful of the risk of bleeding. I would not hesitate to give the medication to diabetics or to younger, more robust patients. The 50% reduction in stent thrombosis with prasugrel versus clopidogrel in TRITON-TIMI 38 is huge,11 given that the risk of death with stent thrombosis is probably 25% or greater. So I would want to have prasugrel on board to reduce the risk of stent thrombosis, especially if a drug-eluting stent were being implanted.
Dr. Bhatt: Dr. Alexander, let’s get your take on a similar scenario. Assuming that prasugrel gains marketing approval, how would you manage patients with non-ST-elevation MI who present to the emergency department? Would you pretreat with clopidogrel? Would you wait until angiography and then, depending on the anatomy, treat with prasugrel? Or would you potentially pretreat with prasugrel, which has not been studied and would not be a labeled indication? How would you reconcile the data?
Dr. Alexander: At Duke, I expect that prasugrel will not be used prior to the catheterization laboratory in patients with non-ST-elevation ACS due to concerns about whether the patients will undergo PCI or be managed medically or with CABG.
Dr. Bhatt: That makes sense, since there was a fair amount of bleeding with prasugrel in those patients in TRITON-TIMI 38.
Dr. Alexander: Correct. Moreover, at Duke we don’t use as much upstream clopidogrel as we would, based on the evidence, if I were managing all the patients. There is still a lot of pushback about upstream clopidogrel from our surgeons because patients are going to surgery quickly these days, sometimes just a day after catheterization, and that’s when a loading dose of clopidogrel can be problematic. We are also still fairly heavy users of glycoprotein IIb/IIIa inhibitors.
Where I can see prasugrel being used prior to the cath lab at Duke is in ST-elevation MI, where the rate of PCI is very high. In primary angioplasty for ST-elevation MI, it would likely be given upstream. The bigger issue for us will be that we serve as a referral base for a lot of regional hospitals, and thus have some influence on their practices.
Dr. Bhatt: In that case, what would you advise those regional hospitals to do for non-ST-elevation MI?
Dr. Alexander: For the time being, we would advise continuing with our current practice, which is to load clopidogrel in patients in whom there is a reasonable certainty that CABG will not be performed, and to use glycoprotein IIb/IIIa inhibitors in high-risk patients. As we get more experience with prasugrel or with additional trial results, however, that practice could easily change.
Dr. Bhatt: So you would still use glycoprotein IIb/IIIa inhibitors?
Dr. Alexander: Yes, I advocate upstream clopidogrel use, but not all my colleagues do. Based on the guidelines, I’d use one or the other—either clopidogrel or a glycoprotein IIb/IIIa inhibitor. As I mentioned in my talk, if a patient is at high risk for bleeding, I am more inclined to use clopidogrel, although patients at higher risk of bleeding are often at higher risk for ischemic events as well.
WHAT’S DRIVEN THE DROPOFF IN GLYCOPROTEIN IIb/IIIa INHIBITOR USE?
Dr. Bhatt: While we’re on the topic of glycoprotein IIb/IIIa inhibitors, a question card from the audience asks why there has been a decrease in glycoprotein IIb/ IIIa inhibitor use and whether this decline is appropriate or inappropriate. Have clopidogrel pretreatment, higher loading doses of clopidogrel, and use of the direct thrombin inhibitor bivalirudin contributed to the decrease in glycoprotein IIb/IIIa inhibitor use?
Dr. Alexander: I do think that the decline has been driven by the changing environment, with greater use of other antithrombotic strategies that include clopidogrel and bivalirudin, as you suggest, as well as an increased attention to bleeding. From an evidence-based standpoint, we don’t know whether the decrease in glycoprotein IIb/IIIa use is appropriate or not because the studies of these agents were conducted before the widespread upstream use of clopidogrel and bivalirudin. Clopidogrel is attractive because it’s a pill given as one dose in the emergency department, the wards, or the catheterization laboratory, rather than a much more complicated infusion with weight-based dosing and dosage adjustments based on creatinine clearance. It is possible that we should perhaps be dosing clopidogrel the same way, but we don’t know that yet.
PRASUGREL IN PRACTICE: HOW LOW CAN THE DOSE GO, AND IS THERE A GENDER EFFECT?
Dr. Bhatt: Let’s stick with this focus on dosing but turn back to discussion of prasugrel. In your presentation of the TRITON-TIMI 38 data, Dr. Sabatine, you proposed a potential prasugrel dosage modification, down to a 5-mg loading dose, in subgroups that were identified as being at high bleeding risk—namely, elderly patients and patients with low body weight. However, no outcomes data with 5 mg of prasugrel came out of TRITON-TIMI 38.10 Is this proposed modification based on pharmacokinetic extrapolation? Could clinicians be comfortable using 5 mg of prasugrel, assuming the drug receives regulatory approval and a 5-mg tablet would be available?
Dr. Sabatine: Of course, evidence at the grade A level would consist of a trial showing that patients who received a lower dose enjoyed the same benefit as those who got standard dosing in TRITON-TIMI 38—a 60-mg loading dose followed by 10 mg/day—with an acceptable risk profile. However, such a trial would be difficult and costly to conduct, and would take roughly half a decade to pull off. It is only through large trials like TRITON-TIMI 38 that you identify subgroups that respond differently, and then to go back and do a separate trial for those subgroups takes a great deal of time. It may not be practical.
I think the Food and Drug Administration is moving toward embracing careful pharmacokinetic/pharmacodynamic substudies within trials, with these substudies having adequate numbers of subjects to provide a sense for the ideal target dose and what an acceptable dose range would be, without limiting approval to a single dose. The analogy would be warfarin dosing, with the aim being to figure out an acceptable dose range, discover which patients fall outside that range, and then model the effect of a lower dose in those patients. Thus, approving a 5-mg dose of prasugrel based on TRITON-TIMI 38 would be a reasonable approach if this dose passed muster under pharmacokinetic/pharmacodynamic modeling. If this approach were taken, there would clearly be a need for postmarketing surveillance to confirm whether the modeling on the effects of the lower dose was borne out by actual outcomes.
Dr. Bhatt: The audience has posed another interesting question raised by TRITON-TIMI 38: Can you comment on the lesser effect of prasugrel in women?
Dr. Sabatine: It is true that there was not a statistically significant effect of prasugrel among women in TRITON-TIMI 38, but statistical tests among subgroups found no significant heterogeneity for the effect between men and women, and that is the relevant measure to determine any gender effect. Keep in mind that not all subgroups represent a univariate slice of the population. For example, women generally have lower body weight than men, and since prasugrel’s net clinical benefit was reduced in patients with lower body weight, that may explain some of the differing extent of effect between men and women.
Dr. Bhatt: That’s a good point about the lack of heterogeneity between men and women. In fact, a meta-analysis of clopidogrel data conducted by one of the fellows I work with revealed that men and women appear to benefit similarly from clopidogrel.12 There was a slight signal of excess bleeding in women, but there were more elderly women in the pooled population, which may have been a confounding factor. As best as anyone can tell, antiplate-let therapy works well in both men and women.
NAVIGATING MANAGEMENT ACROSS THE SPECTRUM OF CARE
Dr. Bhatt: I would like to explore a bit further how all of these issues translate across the spectrum of care, beginning in the emergency department, which we know is a key component of the entire ACS management strategy for a health care system. What should emergency medicine doctors do, given all of the potential options—clopidogrel, different loading doses of clopidogrel, prasugrel, glycoprotein IIb/IIIa inhibitors, even bivalirudin?
Dr. Peacock: It depends on the practice setting. Some emergency physicians work at community hospitals with no backup. They must have relationships with the larger centers to which they’ll be transferring patients, because ACS patients should not be staying at community hospitals. These emergency physicians must have close relationships with the physicians who will be receiving their patients, and they know the potential head-butting with surgeons surrounding early clopidogrel use better than anybody does. If they treat with clopidogrel in the emergency room, and it turns out that the patient needs to go to the catheterization laboratory, can the receiving hospital use platelet testing to shorten the standard 5-day interval from treatment to catheterization?
Dr. Bhatt: Yes, that’s a rather useful, although not completely validated, way of using point-of-care platelet testing—to potentially reduce the time to surgery.
Dr. Peacock: Right. So if the policies for handling these types of transfer-related issues are worked out in advance, all players have a pathway to follow, which can allow quick action when necessary. If you don’t have these issues worked out in advance, you either lose many opportunities to act quickly in the emergency room or you risk taking actions that will cause problems later in the course of management.
Dr. Alexander: I totally agree. The key is to sit down with all the players involved—the surgeons, the interventional cardiologists, the intensivists, the emergency room personnel—and come up with strategies for different populations of patients. Write down the collective strategy and hang it on the wall so that everybody can be comfortable with it. The strategy can be reevaluated when prasugrel or other new antithrombotic drugs come on the market.
Dr. Peacock: The other environment is the academic center, which is even more challenging, but for different reasons. At a large academic center like the Cleveland Clinic, any of 25 different cardiologists may be taking call and receiving patients from the emergency department on a particular night. A lot of phone interaction is required to elicit the planned management strategy, including if and when the patient will be going to the cath lab. Individualizing care to a particular cardiologist then becomes a time-consuming challenge, especially in clinical situations where outcomes are time-dependent.
Dr. Alexander: Agreed. Management needs to be integrated across the entire spectrum of care. The anticoagulants that we plan to use in the cath lab will affect the antithrombotic regimen used upstream.
Dr. Kottke-Marchant: One circumstance where platelet function testing has been helpful is in determining the washout of the clopidogrel effect before surgery. At Cleveland Clinic, we have implemented platelet function testing in this circumstance instead of waiting a blanket 5 days after clopidogrel administration to go to surgery. A return to normal platelet function on platelet aggregation testing, depending on the cutoff value used, is an indicator that the patient can proceed to surgery.
Dr. Bhatt: That’s a logical approach. How should we be using antiplatelet therapy in the medically managed patient, Dr. Alexander?
Dr. Alexander: When I think of medical management, I include patients who don’t go to the cath lab, but also those who do, with regards to their management prior to and following their time in the cath lab.
In patients who don’t go to the cath lab for angiography, the ACC/AHA guidelines recommend aspirin and either clopidogrel, a glycoprotein IIb/IIIa inhibitor, or both.1 In making this choice, I consider the patient’s risk of bleeding and the dosing complexity of the regimen, especially with the use of glycoprotein IIb/IIIa inhibitors in a patient with renal insufficiency. In a patient at relatively low risk for bleeding, I often use both clopidogrel and a glycoprotein IIb/IIIa inhibitor, although this strategy does not have a lot of data to support it.
The more challenging population consists of patients who go to the cath lab but do not undergo PCI; this population is managed medically too. We often drop the ball with clopidogrel in this population. Many patients in whom PCI is not performed do not receive clopidogrel upstream, for all of the reasons we’ve discussed, and there is pretty good evidence that if clopidogrel is not instituted before hospital discharge, the patient is not likely to be receiving it at 30 days either. We have an obligation to treat these patients.
Treatment following bypass surgery is much murkier, and I don’t really know what we should be doing. The ACC/AHA guidelines suggest that clopidogrel be started in a patient with non-ST-elevation ACS after bypass surgery,1 but I believe the evidence to support that recommendation is pretty weak.
Dr. Bhatt: Well, the CURE trial did contain a sizeable group that underwent bypass surgery,7 and although this group was underpowered in some respects, it was still a very large group, so I personally favor treatment in those patients. We should mention that an ongoing trial called TRILOGY ACS is comparing clopidogrel and prasugrel specifically in patients who are being managed medically,13 so more data on this strategy will be emerging.
ARE GUIDELINES DESTINED TO BECOME EVER MORE COMPLEX?
Dr. Bhatt: Here’s a comment and question from the audience that pulls together a lot of what we’ve discussed while also looking forward: The antiplatelet therapy guidelines are already complicated. If the ongoing studies of emerging antiplatelet drugs all have results that are qualitatively similar to those of the TRITON-TIMI 38 study of prasugrel—ie, better efficacy with more potent therapy but more bleeding—how do you foresee these antiplatelet drugs being used in clinical practice?
Dr. Sabatine: The contrast between the US guidelines and the European guidelines for ACS management is stark. The US guidelines—from the ACC and AHA1—are essentially an encyclopedia that includes nearly every trial of anti-platelet therapy in ACS along with complicated algorithms; they do a wonderful job of being complete. The European guidelines14 are probably one tenth the size of their US counterpart document, and they suggest treatments for various patient types; they are very simple.
In a sense, the US guidelines lay out the data and force practitioners to evaluate the trials and consider how our patients fit into the study populations. In this way they are analogous to current guidelines for anticoagulant therapy. Several anticoagulants have been compared with heparin in clinical trials. These newer anticoagulants appear to reduce the risk of ischemic events compared with heparin; some have lower rates of bleeding, while others have higher rates of bleeding. There have been few head-to-head studies of these agents, however, so we wind up with guidelines that are not definitive but rather suggest agents to “consider” in various settings.
It’s unlikely that a head-to-head trial will be conducted comparing prasugrel with the reversible P2Y12 antagonist AZD6140, assuming that both are approved for marketing. If the drugs appear equally efficacious in placebo-controlled trials, it will take consensus to determine the appropriate choice at your hospital, factoring in your patient profile, the cost of the drugs, and other variables. It’s more complicated when one agent is slightly more efficacious but causes more bleeding or, conversely, a little less efficacious but less apt to cause bleeding. In such cases, you may need to tailor therapy to the patient, trying to gauge bleeding risk. All of the emerging data appear to point to the importance of bleeding on outcomes: patients who bleed fare poorly, in part due to the bleeding itself and in part perhaps because they have a proclivity for bleeding.
THE FUTURE: MONITORING-BASED DOSING AND NICHE ANTIPLATELETS?
Dr. Bhatt: That’s a good observation. Let’s wrap up by having the other panelists share any final thoughts you may have.
Dr. Alexander: I’d like to return to the issue of measuring antiplatelet response and using it to guide therapy. Earlier we cited the examples of antihypertensive therapy and lipid-lowering therapy to support this model of monitoring-based treatment. Guidelines for dyslipidemia treatment recommend using LDL-C levels to guide therapy, but this practice is difficult to study in a randomized trial. In fact, none of the randomized trials of statins used LDL-C levels to guide therapy. They all studied fixed doses of statins versus placebo or fixed doses of another statin. Higher doses of statins were always beneficial compared with lower doses, and this finding was extrapolated into the guidelines as a justification to treat to target LDL-C levels.
Dr. Bhatt: It’s not even necessarily clear that LDL-C level is the best target, if you consider the JUPITER trial, in which patients received statin therapy based on their baseline level of high-sensitivity C-reactive protein, not their LDL-C level.15 It goes to show how incomplete our knowledge of a class of drugs may be, even decades after the drugs are introduced.
Dr. Kottke-Marchant: To speak to Dr. Alexander’s point, dose adjustment guided by platelet monitoring is a bit more problematic for antiplatelet drugs that are irreversible inhibitors, such as clopidogrel and aspirin, than for those that are reversible inhibitors, which are being developed and may eventually make more sense to use. From a drug development standpoint, a drug that requires monitoring and dose adjustment will not gain wide acceptance because it will increase medical costs and morbidity.
Dr. Bhatt: Yes, we know from experience with warfarin that doctors and patients don’t like the ongoing need for monitoring and testing.
Dr. Peacock: The drugs that are going to be adopted by the emergency department are those with the shortest half-lives, for several reasons: (1) using a drug with a short half-life won’t commit us to a particular course of action; (2) the potential for drug interactions is lower; and (3) in the event of an erroneous diagnosis, the consequence of misapplication may be mitigated by early recognition and termination of the drug. If we later decide that we’ve gone down the wrong therapeutic road or reached a wrong diagnosis, or if a complication occurs, we can turn off the therapy quickly. That level of flexibility is needed.
Dr. Kottke-Marchant: I think we are moving into an era of niche antiplatelet drugs. One might be used in a patient going to surgery, for example, and another for long-term therapy.
Dr. Peacock: One thing that I don’t have a feel for is how to transition from one drug to another. When you change drugs for a patient, it so often seems like it goes badly. If we’re eventually going to use drugs with ultra-short half-lives in the in the emergency department for the first day or two, and then switch patients to a pill for a week, a lot more platelet function testing may be needed.
CASE STUDY: THROMBOSIS AFTER STENTING DESPITE ANTIPLATELET THERAPY
Dr. Deepak Bhatt: We have taken in a wealth of terrific information from the three preceding talks in this symposium. Let’s now share some questions from the audience and explore some of the points raised in the preceding talks in a bit more practical detail for clinicians. Our three prior speakers are joined in this panel discussion by Cleveland Clinic’s Dr. Frank Peacock, who brings an emergency medicine perspective.
Let’s begin with a case-based question supplied from the audience. The patient is a 42-year-old morbidly obese man without diabetes who had a non-ST-elevation myocardial infarction (MI) less than 1 year ago. A drug-eluting stent was placed at the time of his MI, and now restenosis has occurred. He is on aspirin and clopidogrel 75 mg/day. Do you recommend running a vasodilator-stimulated phosphoprotein (VASP) test and possibly increasing the clopidogrel dose to 150 mg/ day, or should the patient just be switched to prasugrel (assuming it is commercially available) without running the VASP test?
I’ll take a quick initial stab at this question. Studies of antiplatelet therapies to prevent instent restenosis have been a mixed bag. Some of the trials with glycoprotein IIb/IIIa inhibitors have shown an effect on restenosis, but most have not. Similarly, some of the analyses of the thienopyridines ticlopodine and clopidogrel have shown an effect on restenosis, but most have not.
For the most part, restenosis does not appear to be heavily mediated by platelets, at least not in a way that we can influence by therapy. On the other hand, stent thrombosis is highly platelet mediated, so I would alter the case to one in which stent thrombosis is the clinical problem. Assuming that the patient has been adherent to his antiplatelet regimen, which tests would you perform, and how would you act on the information from those tests?
Dr. Kandice Kottke-Marchant: The 2007 guidelines on acute coronary syndrome (ACS) management from the American College of Cardiology and American Heart Association (ACC/AHA)1 do not address platelet function testing, and almost none of the clinical trials of antiplatelet agents had an arm that included testing and dose adjustment based on platelet function studies. Platelet testing is available at some centers; at Cleveland Clinic, we use platelet aggregation testing. One can do platelet aggregation testing on a patient-by-patient basis; if inhibition appears to be suboptimal, a treatment decision should be made, but there is little guidance from the literature to steer that decision. I have seen clinicians increase the dose of clopidogrel or aspirin in response to platelet function tests, which occasionally triggers a confirmatory call from the pharmacy department.
Dr. Bhatt: When I was still at Cleveland Clinic, our chief medical resident did an analysis of platelet function testing, and it was remarkable how much testing was performed and how often it changed management, largely in the absence of any outcomes data, as Dr. Kottke-Marchant pointed out. Dr. Alexander, what are your recommendations with respect to platelet function testing today?
Dr. John Alexander: The case you describe is one in which applying evidence is not easy. There are no trials to supply any evidence to change therapy in this patient, a morbidly obese man receiving 75 mg/day of clopidogrel. There is certainly a rationale, however, to believe that a standard “one size fits all” 75-mg daily dose of clopidogrel may not be enough for him. The trade-off with a higher dosage is a higher risk of bleeding, however, so I would first be sure that he has been adherent to his current regimen of clopidogrel and aspirin.
Dr. Bhatt: Is there a role for point-of-care testing to determine whether he is adherent to the medicines?
Dr. Kottke-Marchant: Several of the point-of-care tests, such as the VerifyNow rapid platelet function analyzer, have specific cartridges for aspirin and for clopidogrel. If platelets were not being inhibited, it would suggest that the doses were too low, given the patient’s weight, but you probably would not be able to determine whether he was resistant to clopidogrel.
Dr. W. Frank Peacock: One way to verify that patients are taking their aspirin is to take a small urine sample and squirt in 2 mL of ferric chloride. If the sample turns purple, it means they are taking their aspirin. Once that is established, you can try to determine whether the drug is working on their platelets.
Dr. Alexander: Another potential explanation for stent thrombosis is faulty stent placement. In this case I would consider asking an interventional colleague to perform intravascular ultrasonography to make sure the stent was implanted properly before I changed the patient’s antithrombotic therapy.
Dr. Bhatt: That’s a great technical point. We always want to make sure that a case of stent thrombosis is not due to a mechanical problem. We should be asking: Is the stent properly sized and well opposed? Is there a distal dissection or any other issue that could predispose to stent thrombosis?
Dr. Alexander: This case illustrates a host of other challenges that underscore how much more work we need to do to define optimal antiplatelet therapy. Suppose we perform platelet function testing and find a low level of platelet inhibition in this patient with stent thrombosis, and we change his antiplatelet regimen. When should we test him again? If we retest in 3 months and find that he has a higher than expected level of platelet inhibition on the new antiplatelet regimen, do we dial down the intensity? Once again, there is no evidence to guide these decisions, and levels of platelet inhibition are driven not just by the medications but also by what is going on in the patient’s platelets—it is quite multifactorial.
POINT-OF-CARE PLATELET FUNCTION TESTING: CURRENT LIMITS, FUTURE ROLES
Dr. Bhatt: While we’re discussing platelet function testing, I found it interesting, Dr. Kottke-Marchant, that you said the use of bleeding time as a platelet test is finally going away. Testing of bleeding time has been around forever, but I agree that it doesn’t have much value in clinical practice. Do you think bleeding time will continue to have any role in drug development? Most phase 2 trials, and certainly phase 1 trials, still capture bleeding time to assess whether or not a drug is working. Should that, too, be jettisoned, or does bleeding time still have some merit in this context?
Dr. Kottke-Marchant: I would jettison it in drug development as well because of the considerable variability in bleeding time. It is not a test that can be standardized, and no quality control can be done. The results depend on skin turgor, age, and many other variables.
We need a global assay that will pick up multiple aspects of platelet function, such as flow-based adhesion, aggregation, and granule release. The bleeding time is a shear-dependent test, whereas the platelet aggregation test that is used in most drug trials is an artificial assay that measures only aggregation, but not under shear. The VerifyNow rapid platelet function analyzer does not measure platelets under shear and is not a global assay.
Dr. Marc Sabatine: I would underscore the need for a reliable point-of-care test of platelet function. When we prescribe a statin or an antihypertensive drug, we don’t just send the patient out the door and hope that everything will be okay. We measure the response, knowing that genotype, environmental factors, or medication factors can affect the response. When we prescribe an antiplatelet drug, we need a reliable point-of-care device to make certain that the patient is getting appropriate platelet inhibition.
I am reminded of a recent study of point-of-care measurement of platelet inhibition in patients receiving clopidogrel prior to nonemergent percutaneous coronary intervention (PCI).2 Rather than just treating patients with PCI and sending them out the door, the investigators kept giving patients clopidogrel and measuring their platelet inhibition until they achieved an appropriate degree of inhibition, after which PCI was performed. Event rates were significantly reduced in the patient group treated this way, which suggests a need to individualize therapy and move away from the “one size fits all” mindset.
Dr. Bhatt: Dr. Peacock, you’ve led a study of point-of-care assays in the emergency department. What might ultimately be the role of point-of-care testing in emergency medicine, and might it influence drug selection?
Dr. Peacock: My short answer is that I think there will be a role for point-of-care testing, with all the caveats that have been discussed. There may even be a day when we do genetic testing and look for DNA. Honestly, though, I’m somewhat of a skeptic because I’m not looking at the genetics. I see many patients who do crack cocaine who come to the emergency room with chest pain and have risk factors, but I send these patients home because they are not having an event. The real question is, “Is it an event?” If a patient is having an event and he or she has platelet resistance or hyperreactivity—whatever we term it—then you have to decide the next step.
As you mentioned, we just completed a study that evaluated a couple hundred patients for platelet inhibition resistance to aspirin, and one finding was that the incidence of platelet resistance to aspirin was much lower than we had anticipated. Studies from the literature suggest that the prevalence of resistance is around 30%, but in our study it was 6.5%.3
Dr. Kottke-Marchant: It depends on how and in whom you measure resistance. Different tests will give you different numbers. Even among studies using the same measurement techniques, the results depend on the patient population. If it’s a fairly stable cardiac population, you may see aspirin resistance rates of 4% or 5%. If it’s a population of patients who have had multiple MIs, the rate may be higher.
Dr. Peacock: That’s exactly my point. In the emergency department we see a mixed bag. We see many people who have had no prior events and have no acute event occurring. So in that setting you are going to get results that suggest that no intervention is required, whereas in that small percentage of patients in whom something is happening, your drug choice may be different.
Dr. Alexander: We are still talking about resistance to antiplatelet drugs as though it were a patient-level variable, but it’s my impression that it changes over time and within a patient.
Dr. Kottke-Marchant: It can change over time. There aren’t many good longitudinal studies. Most of the studies of “aspirin resistance” are really snapshot studies with measurements taken at one point in time. A term I prefer is “platelet reactivity.” To really assess treatment efficacy, we are going to have to look at the basal level of platelet reactivity.
WHAT ROLE FOR GENOTYPING IN GUIDING ANTIPLATELET THERAPY?
Dr. Bhatt: Dr. Peacock alluded to a potential role for genetic testing. Dr. Sabatine, you have done a lot of interesting work with genotyping in the TRITON-TIMI 38 study of prasugrel and clopidogrel. What is the future role of genotyping in determining which antiplatelet therapy is best for which patient?
Dr. Sabatine: As I mentioned, cytochrome P450 enzymes play a critical role in the metabolism of clopidogrel. These enzymes are fairly polymorphic—mutations in their encoding genes are responsible for subtle changes in effect, unlike the traditional mutations that we think about for sickle cell disease, for example. A wealth of data has been published showing that genetic variants are associated with decreased functional activity of cytochrome P450 enzymes, demonstrating the pharmacologic importance of these variants.
Individuals who carry variant alleles appear to respond differently to clopidogrel. A variety of small studies show that those who carry specific variants—particularly in the CYP2C19 enzyme, but in other enzymes as well—appear to have a diminished response to clopidogrel. There are also data showing that individuals with a diminished response to clopidogrel have worse outcomes.4 Our group is studying the impact of genetic variants that decrease the functional activity of cytochrome P450 enzymes on clinical outcomes. (Editor’s note: This study has since been published by Mega et al.5)
The practical implication may lie in point-of-care genotyping, which appears possible and will be clinically useful if a strong link can be demonstrated between genotype and outcomes. If point-of-care genotyping becomes practical, it will raise the question of whether both genotyping and platelet aggregation testing are needed. I think they might indeed be complementary in risk prediction, as is the case with genetic variants that affect low-density lipoprotein cholesterol (LDL-C) levels. In the lipid arena, we have seen that genetic effects and lipid levels provide independent incremental information about risk. That’s because of the high degree of variation in LDL-C levels: an LDL-C measurement is a snapshot in time, yet a variety of factors can influence LDL-C levels. In contrast, genotype is an invariant factor. Similarly, in the platelet arena, platelet aggregation studies and genotyping may be synergistic in predicting an individual’s predisposition to events and response to medications.
Dr. Bhatt: While we’re discussing pathways of metabolism, the literature, though scant, suggests a potential interaction between proton pump inhibitors and clopidogrel. I was co-chair of a recent American College of Cardiology/ American Heart Association/American College of Gastro-enterology consensus document that endorsed liberal use of proton pump inhibitors in patients who are at gastrointestinal risk, including those on antiplatelet therapy.6 The gastroenterologists believed strongly that proton pump inhibitors were safe and in fact underused in these patients. What do you think about the clopidogrel–proton pump inhibitor interaction? Should we be concerned?
Dr. Sabatine: Proton pump inhibitors are not only substrates for, but also inhibitors of, CYP2C19, a key enzyme that helps transform clopidogrel into an active metabolite. For this reason, there has been interest in whether concomitant use of proton pump inhibitors would blunt the efficacy of clopidogrel. The same concern was raised about giving clopidogrel with certain statin drugs that are also metabolized by the cytochrome P450 system, and several studies have shown an effect of these statins on clopidogrel’s platelet inhibition. However, there is no evidence that coadministration of these statins has affected clinical outcomes with clopidogrel in clinical trials. So it may be that while competition for the cytochrome P450 system is one factor, it’s not enough of a factor to tip the scale and result in a clinical event. The same may be true of coadministration of proton pump inhibitors; meanwhile, we await definitive data that concomitant use with clopidogrel leads to higher rates of ischemic events.
DIAGNOSTIC UNCERTAINTY IN THE EMERGENCY SETTING
Dr. Bhatt: We heard about quite a few new antiplatelet drugs in Dr. Sabatine’s presentation, some of which will likely be taken up in clinical practice. Dr. Peacock, from an emergency department perspective, how will you integrate all these new agents with the numerous therapies already available? What should emergency departments do to come to grips with and ultimately take advantage of these different forms of therapy as well as emerging platelet function tests?
Dr. Peacock: The piece that’s unique or especially pertinent to the emergency department is diagnostic uncertainty. Diagnosis and management are easy when a patient has an ST-elevation MI because we all know what that looks like and we know what to do in response. To some extent non-ST-elevation MI is fairly simple too. ACS is a lot more difficult because we don’t have a good definition for unstable angina, and that’s where diagnosis and management become problematic. And with high-sensitivity troponins coming out now, the question of non-ST-elevation MI is going to get more and more confusing because we will have a lot more patients who meet criteria without having an acute coronary artery event.
So it is going to be important that studies be designed correctly. A lot of the studies reviewed today were efficacy studies, showing that a particular drug works well in a carefully defined population, but they were not efficiency studies: they did not take into account the real-world diagnostic uncertainty—and inevitable misdiagnoses—that emergency departments encounter before starting therapy.
Take the CURE trial, for example. It was a great study, showing that clopidogrel reduced the hazard ratio for major coronary events by 20% in patients with unstable angina,7 and the message was that everybody should be using clopidogrel. A close look at the study, however, reveals that about half the patients did not receive clopidogrel in the emergency department. When patients did receive it early, it was driven by the cardiologist, who was absolutely certain of the diagnosis. But if the study was not designed to test early use, then it is a big leap to extrapolate its findings to this circumstance.
Many of the patients in the CURE trial were enrolled the day after presentation, when their diagnosis was certain—ie, they had a rise in troponin after their symptoms. But when a patient first arrives in the emergency department, we are not certain of the diagnosis. And if we use a drug such as clopidogrel, with a duration of action as long as 5 days, we have committed the entire medical system to a certain course of management for that period of time. If we get the diagnosis wrong, this commitment could restrict management options for up to 5 days.
The question for emergency physicians becomes, “How long is long enough to know whether I can pull the trigger on a therapy and be correct?” With all the new drugs coming along, the way to answer this is to do efficiency studies in a real-world environment in addition to efficacy studies.
Dr. Alexander: Yes, one of the biggest limitations of antiplatelet drug studies to date is that they usually haven’t really addressed the timing of drug initiation. We often assume that if a drug is shown to be beneficial, then it should be started as soon as possible. As we just heard, that may have been an unfounded extrapolation from the CURE trial. The same sort of thing happened with the ISIS trial of aspirin in patients with ST-elevation MI.8 In response to the ISIS results, clinicians rushed to give patients aspirin right away even though many of the patients in the trial may have received their aspirin the day after presentation. For these reasons, the EARLY-ACS study,9 which is addressing a very simple question—whether early upstream use of glycoprotein IIb/IIIa inhibitors is beneficial—has been a challenging trial to complete.
WHAT ROLE FOR THIENOPYRIDINE PRETREATMENT?
Dr. Bhatt: Dr. Sabatine, you presented data from the large TRITON-TIMI 38 trial comparing prasugrel with clopidogrel. I’m interested in how you would use prasugrel in practice, assuming it receives marketing approval, especially in light of its bleeding risk, particularly in patients in whom coronary artery bypass graft surgery (CABG) is planned. Many hospitals pretreat patients with clopidogrel in the emergency department. How would you manage a patient who shows up in the emergency room with ACS? Would you give clopidogrel, would you wait and give prasugrel, or would you do something else? If you gave clopidogrel, what loading dose would you use—300 mg, 600 mg, or, as some have suggested, 900 or 1,200 mg?
Dr. Sabatine: I am a strong proponent of pretreatment. Data from multiple studies show a benefit to this strategy, and even the original CURE trial showed a roughly 30% reduction in ischemic events within the first 24 hours of clopidogrel initiation.7
I think the dosing strategy depends on how the patient is going to be managed. If management is going to be conservative, then I would start the patient on 300 mg of clopidogrel when he or she came in. If the patient is going to the cardiac catheterization laboratory in a few hours, I would pretreat with 600 mg of clopidogrel. For prasugrel, the need for pretreatment is less clear, given the drug’s faster onset of action and greater degree of platelet inhibition. In the TRITON-TIMI 38 study,10 prasugrel was given, by and large, after diagnostic angiography, and thus one could use that approach in practice.
In terms of clopidogrel versus prasugrel, I would embrace prasugrel for the large majority of my patients, being mindful of the risk of bleeding. I would not hesitate to give the medication to diabetics or to younger, more robust patients. The 50% reduction in stent thrombosis with prasugrel versus clopidogrel in TRITON-TIMI 38 is huge,11 given that the risk of death with stent thrombosis is probably 25% or greater. So I would want to have prasugrel on board to reduce the risk of stent thrombosis, especially if a drug-eluting stent were being implanted.
Dr. Bhatt: Dr. Alexander, let’s get your take on a similar scenario. Assuming that prasugrel gains marketing approval, how would you manage patients with non-ST-elevation MI who present to the emergency department? Would you pretreat with clopidogrel? Would you wait until angiography and then, depending on the anatomy, treat with prasugrel? Or would you potentially pretreat with prasugrel, which has not been studied and would not be a labeled indication? How would you reconcile the data?
Dr. Alexander: At Duke, I expect that prasugrel will not be used prior to the catheterization laboratory in patients with non-ST-elevation ACS due to concerns about whether the patients will undergo PCI or be managed medically or with CABG.
Dr. Bhatt: That makes sense, since there was a fair amount of bleeding with prasugrel in those patients in TRITON-TIMI 38.
Dr. Alexander: Correct. Moreover, at Duke we don’t use as much upstream clopidogrel as we would, based on the evidence, if I were managing all the patients. There is still a lot of pushback about upstream clopidogrel from our surgeons because patients are going to surgery quickly these days, sometimes just a day after catheterization, and that’s when a loading dose of clopidogrel can be problematic. We are also still fairly heavy users of glycoprotein IIb/IIIa inhibitors.
Where I can see prasugrel being used prior to the cath lab at Duke is in ST-elevation MI, where the rate of PCI is very high. In primary angioplasty for ST-elevation MI, it would likely be given upstream. The bigger issue for us will be that we serve as a referral base for a lot of regional hospitals, and thus have some influence on their practices.
Dr. Bhatt: In that case, what would you advise those regional hospitals to do for non-ST-elevation MI?
Dr. Alexander: For the time being, we would advise continuing with our current practice, which is to load clopidogrel in patients in whom there is a reasonable certainty that CABG will not be performed, and to use glycoprotein IIb/IIIa inhibitors in high-risk patients. As we get more experience with prasugrel or with additional trial results, however, that practice could easily change.
Dr. Bhatt: So you would still use glycoprotein IIb/IIIa inhibitors?
Dr. Alexander: Yes, I advocate upstream clopidogrel use, but not all my colleagues do. Based on the guidelines, I’d use one or the other—either clopidogrel or a glycoprotein IIb/IIIa inhibitor. As I mentioned in my talk, if a patient is at high risk for bleeding, I am more inclined to use clopidogrel, although patients at higher risk of bleeding are often at higher risk for ischemic events as well.
WHAT’S DRIVEN THE DROPOFF IN GLYCOPROTEIN IIb/IIIa INHIBITOR USE?
Dr. Bhatt: While we’re on the topic of glycoprotein IIb/IIIa inhibitors, a question card from the audience asks why there has been a decrease in glycoprotein IIb/ IIIa inhibitor use and whether this decline is appropriate or inappropriate. Have clopidogrel pretreatment, higher loading doses of clopidogrel, and use of the direct thrombin inhibitor bivalirudin contributed to the decrease in glycoprotein IIb/IIIa inhibitor use?
Dr. Alexander: I do think that the decline has been driven by the changing environment, with greater use of other antithrombotic strategies that include clopidogrel and bivalirudin, as you suggest, as well as an increased attention to bleeding. From an evidence-based standpoint, we don’t know whether the decrease in glycoprotein IIb/IIIa use is appropriate or not because the studies of these agents were conducted before the widespread upstream use of clopidogrel and bivalirudin. Clopidogrel is attractive because it’s a pill given as one dose in the emergency department, the wards, or the catheterization laboratory, rather than a much more complicated infusion with weight-based dosing and dosage adjustments based on creatinine clearance. It is possible that we should perhaps be dosing clopidogrel the same way, but we don’t know that yet.
PRASUGREL IN PRACTICE: HOW LOW CAN THE DOSE GO, AND IS THERE A GENDER EFFECT?
Dr. Bhatt: Let’s stick with this focus on dosing but turn back to discussion of prasugrel. In your presentation of the TRITON-TIMI 38 data, Dr. Sabatine, you proposed a potential prasugrel dosage modification, down to a 5-mg loading dose, in subgroups that were identified as being at high bleeding risk—namely, elderly patients and patients with low body weight. However, no outcomes data with 5 mg of prasugrel came out of TRITON-TIMI 38.10 Is this proposed modification based on pharmacokinetic extrapolation? Could clinicians be comfortable using 5 mg of prasugrel, assuming the drug receives regulatory approval and a 5-mg tablet would be available?
Dr. Sabatine: Of course, evidence at the grade A level would consist of a trial showing that patients who received a lower dose enjoyed the same benefit as those who got standard dosing in TRITON-TIMI 38—a 60-mg loading dose followed by 10 mg/day—with an acceptable risk profile. However, such a trial would be difficult and costly to conduct, and would take roughly half a decade to pull off. It is only through large trials like TRITON-TIMI 38 that you identify subgroups that respond differently, and then to go back and do a separate trial for those subgroups takes a great deal of time. It may not be practical.
I think the Food and Drug Administration is moving toward embracing careful pharmacokinetic/pharmacodynamic substudies within trials, with these substudies having adequate numbers of subjects to provide a sense for the ideal target dose and what an acceptable dose range would be, without limiting approval to a single dose. The analogy would be warfarin dosing, with the aim being to figure out an acceptable dose range, discover which patients fall outside that range, and then model the effect of a lower dose in those patients. Thus, approving a 5-mg dose of prasugrel based on TRITON-TIMI 38 would be a reasonable approach if this dose passed muster under pharmacokinetic/pharmacodynamic modeling. If this approach were taken, there would clearly be a need for postmarketing surveillance to confirm whether the modeling on the effects of the lower dose was borne out by actual outcomes.
Dr. Bhatt: The audience has posed another interesting question raised by TRITON-TIMI 38: Can you comment on the lesser effect of prasugrel in women?
Dr. Sabatine: It is true that there was not a statistically significant effect of prasugrel among women in TRITON-TIMI 38, but statistical tests among subgroups found no significant heterogeneity for the effect between men and women, and that is the relevant measure to determine any gender effect. Keep in mind that not all subgroups represent a univariate slice of the population. For example, women generally have lower body weight than men, and since prasugrel’s net clinical benefit was reduced in patients with lower body weight, that may explain some of the differing extent of effect between men and women.
Dr. Bhatt: That’s a good point about the lack of heterogeneity between men and women. In fact, a meta-analysis of clopidogrel data conducted by one of the fellows I work with revealed that men and women appear to benefit similarly from clopidogrel.12 There was a slight signal of excess bleeding in women, but there were more elderly women in the pooled population, which may have been a confounding factor. As best as anyone can tell, antiplate-let therapy works well in both men and women.
NAVIGATING MANAGEMENT ACROSS THE SPECTRUM OF CARE
Dr. Bhatt: I would like to explore a bit further how all of these issues translate across the spectrum of care, beginning in the emergency department, which we know is a key component of the entire ACS management strategy for a health care system. What should emergency medicine doctors do, given all of the potential options—clopidogrel, different loading doses of clopidogrel, prasugrel, glycoprotein IIb/IIIa inhibitors, even bivalirudin?
Dr. Peacock: It depends on the practice setting. Some emergency physicians work at community hospitals with no backup. They must have relationships with the larger centers to which they’ll be transferring patients, because ACS patients should not be staying at community hospitals. These emergency physicians must have close relationships with the physicians who will be receiving their patients, and they know the potential head-butting with surgeons surrounding early clopidogrel use better than anybody does. If they treat with clopidogrel in the emergency room, and it turns out that the patient needs to go to the catheterization laboratory, can the receiving hospital use platelet testing to shorten the standard 5-day interval from treatment to catheterization?
Dr. Bhatt: Yes, that’s a rather useful, although not completely validated, way of using point-of-care platelet testing—to potentially reduce the time to surgery.
Dr. Peacock: Right. So if the policies for handling these types of transfer-related issues are worked out in advance, all players have a pathway to follow, which can allow quick action when necessary. If you don’t have these issues worked out in advance, you either lose many opportunities to act quickly in the emergency room or you risk taking actions that will cause problems later in the course of management.
Dr. Alexander: I totally agree. The key is to sit down with all the players involved—the surgeons, the interventional cardiologists, the intensivists, the emergency room personnel—and come up with strategies for different populations of patients. Write down the collective strategy and hang it on the wall so that everybody can be comfortable with it. The strategy can be reevaluated when prasugrel or other new antithrombotic drugs come on the market.
Dr. Peacock: The other environment is the academic center, which is even more challenging, but for different reasons. At a large academic center like the Cleveland Clinic, any of 25 different cardiologists may be taking call and receiving patients from the emergency department on a particular night. A lot of phone interaction is required to elicit the planned management strategy, including if and when the patient will be going to the cath lab. Individualizing care to a particular cardiologist then becomes a time-consuming challenge, especially in clinical situations where outcomes are time-dependent.
Dr. Alexander: Agreed. Management needs to be integrated across the entire spectrum of care. The anticoagulants that we plan to use in the cath lab will affect the antithrombotic regimen used upstream.
Dr. Kottke-Marchant: One circumstance where platelet function testing has been helpful is in determining the washout of the clopidogrel effect before surgery. At Cleveland Clinic, we have implemented platelet function testing in this circumstance instead of waiting a blanket 5 days after clopidogrel administration to go to surgery. A return to normal platelet function on platelet aggregation testing, depending on the cutoff value used, is an indicator that the patient can proceed to surgery.
Dr. Bhatt: That’s a logical approach. How should we be using antiplatelet therapy in the medically managed patient, Dr. Alexander?
Dr. Alexander: When I think of medical management, I include patients who don’t go to the cath lab, but also those who do, with regards to their management prior to and following their time in the cath lab.
In patients who don’t go to the cath lab for angiography, the ACC/AHA guidelines recommend aspirin and either clopidogrel, a glycoprotein IIb/IIIa inhibitor, or both.1 In making this choice, I consider the patient’s risk of bleeding and the dosing complexity of the regimen, especially with the use of glycoprotein IIb/IIIa inhibitors in a patient with renal insufficiency. In a patient at relatively low risk for bleeding, I often use both clopidogrel and a glycoprotein IIb/IIIa inhibitor, although this strategy does not have a lot of data to support it.
The more challenging population consists of patients who go to the cath lab but do not undergo PCI; this population is managed medically too. We often drop the ball with clopidogrel in this population. Many patients in whom PCI is not performed do not receive clopidogrel upstream, for all of the reasons we’ve discussed, and there is pretty good evidence that if clopidogrel is not instituted before hospital discharge, the patient is not likely to be receiving it at 30 days either. We have an obligation to treat these patients.
Treatment following bypass surgery is much murkier, and I don’t really know what we should be doing. The ACC/AHA guidelines suggest that clopidogrel be started in a patient with non-ST-elevation ACS after bypass surgery,1 but I believe the evidence to support that recommendation is pretty weak.
Dr. Bhatt: Well, the CURE trial did contain a sizeable group that underwent bypass surgery,7 and although this group was underpowered in some respects, it was still a very large group, so I personally favor treatment in those patients. We should mention that an ongoing trial called TRILOGY ACS is comparing clopidogrel and prasugrel specifically in patients who are being managed medically,13 so more data on this strategy will be emerging.
ARE GUIDELINES DESTINED TO BECOME EVER MORE COMPLEX?
Dr. Bhatt: Here’s a comment and question from the audience that pulls together a lot of what we’ve discussed while also looking forward: The antiplatelet therapy guidelines are already complicated. If the ongoing studies of emerging antiplatelet drugs all have results that are qualitatively similar to those of the TRITON-TIMI 38 study of prasugrel—ie, better efficacy with more potent therapy but more bleeding—how do you foresee these antiplatelet drugs being used in clinical practice?
Dr. Sabatine: The contrast between the US guidelines and the European guidelines for ACS management is stark. The US guidelines—from the ACC and AHA1—are essentially an encyclopedia that includes nearly every trial of anti-platelet therapy in ACS along with complicated algorithms; they do a wonderful job of being complete. The European guidelines14 are probably one tenth the size of their US counterpart document, and they suggest treatments for various patient types; they are very simple.
In a sense, the US guidelines lay out the data and force practitioners to evaluate the trials and consider how our patients fit into the study populations. In this way they are analogous to current guidelines for anticoagulant therapy. Several anticoagulants have been compared with heparin in clinical trials. These newer anticoagulants appear to reduce the risk of ischemic events compared with heparin; some have lower rates of bleeding, while others have higher rates of bleeding. There have been few head-to-head studies of these agents, however, so we wind up with guidelines that are not definitive but rather suggest agents to “consider” in various settings.
It’s unlikely that a head-to-head trial will be conducted comparing prasugrel with the reversible P2Y12 antagonist AZD6140, assuming that both are approved for marketing. If the drugs appear equally efficacious in placebo-controlled trials, it will take consensus to determine the appropriate choice at your hospital, factoring in your patient profile, the cost of the drugs, and other variables. It’s more complicated when one agent is slightly more efficacious but causes more bleeding or, conversely, a little less efficacious but less apt to cause bleeding. In such cases, you may need to tailor therapy to the patient, trying to gauge bleeding risk. All of the emerging data appear to point to the importance of bleeding on outcomes: patients who bleed fare poorly, in part due to the bleeding itself and in part perhaps because they have a proclivity for bleeding.
THE FUTURE: MONITORING-BASED DOSING AND NICHE ANTIPLATELETS?
Dr. Bhatt: That’s a good observation. Let’s wrap up by having the other panelists share any final thoughts you may have.
Dr. Alexander: I’d like to return to the issue of measuring antiplatelet response and using it to guide therapy. Earlier we cited the examples of antihypertensive therapy and lipid-lowering therapy to support this model of monitoring-based treatment. Guidelines for dyslipidemia treatment recommend using LDL-C levels to guide therapy, but this practice is difficult to study in a randomized trial. In fact, none of the randomized trials of statins used LDL-C levels to guide therapy. They all studied fixed doses of statins versus placebo or fixed doses of another statin. Higher doses of statins were always beneficial compared with lower doses, and this finding was extrapolated into the guidelines as a justification to treat to target LDL-C levels.
Dr. Bhatt: It’s not even necessarily clear that LDL-C level is the best target, if you consider the JUPITER trial, in which patients received statin therapy based on their baseline level of high-sensitivity C-reactive protein, not their LDL-C level.15 It goes to show how incomplete our knowledge of a class of drugs may be, even decades after the drugs are introduced.
Dr. Kottke-Marchant: To speak to Dr. Alexander’s point, dose adjustment guided by platelet monitoring is a bit more problematic for antiplatelet drugs that are irreversible inhibitors, such as clopidogrel and aspirin, than for those that are reversible inhibitors, which are being developed and may eventually make more sense to use. From a drug development standpoint, a drug that requires monitoring and dose adjustment will not gain wide acceptance because it will increase medical costs and morbidity.
Dr. Bhatt: Yes, we know from experience with warfarin that doctors and patients don’t like the ongoing need for monitoring and testing.
Dr. Peacock: The drugs that are going to be adopted by the emergency department are those with the shortest half-lives, for several reasons: (1) using a drug with a short half-life won’t commit us to a particular course of action; (2) the potential for drug interactions is lower; and (3) in the event of an erroneous diagnosis, the consequence of misapplication may be mitigated by early recognition and termination of the drug. If we later decide that we’ve gone down the wrong therapeutic road or reached a wrong diagnosis, or if a complication occurs, we can turn off the therapy quickly. That level of flexibility is needed.
Dr. Kottke-Marchant: I think we are moving into an era of niche antiplatelet drugs. One might be used in a patient going to surgery, for example, and another for long-term therapy.
Dr. Peacock: One thing that I don’t have a feel for is how to transition from one drug to another. When you change drugs for a patient, it so often seems like it goes badly. If we’re eventually going to use drugs with ultra-short half-lives in the in the emergency department for the first day or two, and then switch patients to a pill for a week, a lot more platelet function testing may be needed.
- Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/ non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2007; 50:e1–e157.
- Bonello L, Camoin-Jau L, Arques S, et al. Adjusted clopidogrel loading doses according to vasodilator-stimulated phosphoprotein phosphorylation index decrease rate of major adverse cardiovascular events in patients with clopidogrel resistance: a multicenter randomized prospective study. J Am Coll Cardiol 2008; 51:1404–1411.
- Glauser J, Emerman CL, Bhatt DL, Peacock WF. Platelet aspirin resistance in emergency department patients with suspected acute coronary syndrome. Am J Emerg Med. In press
- Patti G, Nusca A, Mangiacapra F, Gatto L, D’Ambrosio A, Di Sciascio G. Point-of-care measurement of clopidogrel responsiveness predicts clinical outcome in patients undergoing percutaneous coronary intervention. J Am Coll Cardiol 2008; 52:1128–1133.
- Mega JL, Close SL, Wiviott SD, et al. Cytochrome P-450 polymorphisms and response to clopidogrel. N Engl J Med 2009; 360:354–362.
- Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use. J Am Coll Cardiol 2008; 52:1502–1517.
- Fox KA, Mehta SR, Peters R, et al. Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non-ST-elevation acute coronary syndrome: the Clopidogrel in Unstable angina to prevent Recurrent ischemic Events (CURE) Trial. Circulation 2004; 110:1202–1208.
- ISIS-2 Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Lancet 1988; 2:349–360.
- EARLY-ACS: Glycoprotein IIb/IIIa inhibition in patients with non-ST-segment elevation acute coronary syndrome. Clinical Trials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00089895. Updated December 17, 2008. Accessed December 18, 2008.
- Wiviott SD, Braunwald E, McCabe CH, et al; TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007; 357:2001–2015.
- Wiviott SD, Braunwald E, McCabe CH, et al. Intensive oral anti-platelet therapy for reduction of ischaemic events including stent thrombosis in patients with acute coronary dyndromes treated with percutaneous coronary intervention and stenting in the TRITON-TIMI 38 trial: a subanalysis of a randomised trial. Lancet 2008; 371:1353–1363.
- Berger JS, Bhatt DL, Chen Z, et al. The relationship between sex, mortality and cardiovascular events among patients with established cardiovascular disease: a meta-analysis [ACC abstract 1012-149]. J Am Coll Cardiol 2008; 51 10 suppl A:A247.
- TRILOGY ACS: A comparison of prasugrel and clopidogrel in acute coronary syndrome subjects. ClinicalTrials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00699998. Updated December 15, 2008. Accessed January 2, 2009.
- Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J 2007; 28:1598–1660.
- Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008; 359:2195–2207.
- Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/ non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2007; 50:e1–e157.
- Bonello L, Camoin-Jau L, Arques S, et al. Adjusted clopidogrel loading doses according to vasodilator-stimulated phosphoprotein phosphorylation index decrease rate of major adverse cardiovascular events in patients with clopidogrel resistance: a multicenter randomized prospective study. J Am Coll Cardiol 2008; 51:1404–1411.
- Glauser J, Emerman CL, Bhatt DL, Peacock WF. Platelet aspirin resistance in emergency department patients with suspected acute coronary syndrome. Am J Emerg Med. In press
- Patti G, Nusca A, Mangiacapra F, Gatto L, D’Ambrosio A, Di Sciascio G. Point-of-care measurement of clopidogrel responsiveness predicts clinical outcome in patients undergoing percutaneous coronary intervention. J Am Coll Cardiol 2008; 52:1128–1133.
- Mega JL, Close SL, Wiviott SD, et al. Cytochrome P-450 polymorphisms and response to clopidogrel. N Engl J Med 2009; 360:354–362.
- Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use. J Am Coll Cardiol 2008; 52:1502–1517.
- Fox KA, Mehta SR, Peters R, et al. Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non-ST-elevation acute coronary syndrome: the Clopidogrel in Unstable angina to prevent Recurrent ischemic Events (CURE) Trial. Circulation 2004; 110:1202–1208.
- ISIS-2 Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Lancet 1988; 2:349–360.
- EARLY-ACS: Glycoprotein IIb/IIIa inhibition in patients with non-ST-segment elevation acute coronary syndrome. Clinical Trials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00089895. Updated December 17, 2008. Accessed December 18, 2008.
- Wiviott SD, Braunwald E, McCabe CH, et al; TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007; 357:2001–2015.
- Wiviott SD, Braunwald E, McCabe CH, et al. Intensive oral anti-platelet therapy for reduction of ischaemic events including stent thrombosis in patients with acute coronary dyndromes treated with percutaneous coronary intervention and stenting in the TRITON-TIMI 38 trial: a subanalysis of a randomised trial. Lancet 2008; 371:1353–1363.
- Berger JS, Bhatt DL, Chen Z, et al. The relationship between sex, mortality and cardiovascular events among patients with established cardiovascular disease: a meta-analysis [ACC abstract 1012-149]. J Am Coll Cardiol 2008; 51 10 suppl A:A247.
- TRILOGY ACS: A comparison of prasugrel and clopidogrel in acute coronary syndrome subjects. ClinicalTrials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00699998. Updated December 15, 2008. Accessed January 2, 2009.
- Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J 2007; 28:1598–1660.
- Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008; 359:2195–2207.