User login
You have identified a pelvic mass in your teenage patient. What now?
Pelvic masses frequently are the reason for the medical evaluation of young women and girls. Regardless of what prompted the work-up that led to the mass’ discovery, the patient inevitably will be sent to a gynecologist for further evaluation, and such a practitioner should be involved whenever there is suspicion for a mass involving the reproductive tract.
While it does not happen often, it is possible that a mass diagnosed as ovarian, based on imaging, is then determined to be of another organ system at the time of surgery. Most frequently, this occurs with ruptured appendicitis, as the presence of an appendiceal abscess can mimic a complex ovarian mass or tubo-ovarian abscess (TOA).1
The full differential diagnosis of non-gynecologic pelvic masses is extensive and includes mesenteric duplication cysts, presacral masses, pelvic kidney, peritoneal inclusion cysts, and urachal cysts (TABLE). It can be difficult to distinguish pathology as gynecologic or nongynecologic even if a thorough work-up is performed.
Differential diagnosis for a pelvic mass
|
In this review, we offer several cases involving varying presentations of pelvic masses related to the reproductive tract.
Case 1: Severe pelvic pain in an 18-year-old
An 18-year-old adolescent presents to your office reporting worsening pelvic pain over the past 3 days. The pain is severe in the left lower quadrant. She reports a foul discharge and thinks she has a fever but hasn’t checked her temperature. She says she has been sexually active in the past few months with 2 different male partners. She has not been using condoms consistently and hasn’t been tested for sexually transmitted infections. Physical examination reveals a mucopurulent discharge at the cervix and copious white blood cells noted on wet mount. Bimanual examination reveals cervical motion tenderness and tenderness over the left adnexa. Ultrasound reveals a mass in the left adnexa with debris and internal echoes.
Diagnosis: Tubo-ovarian abscess.
Treatment: Admission to the hospital for intravenous antibiotic therapy.
It is important to note that TOAs can be seen in patients who have not been sexually active, as well as in cases related not to an ascending infection but rather to a history of pelvic surgery or complex structural anomaly.2 The majority of the time a TOA is a result of pelvic inflammatory disease (PID). Often, patients with uncomplicated PID can be treated on an outpatient basis if they meet strict criteria, but patients with a TOA need to be treated as an inpatient due to the severity of this infection.
Clinical pearl. If a patient has an IUD in place, close clinical follow up is critical to determine response to therapy. The Centers for Disease Control and Prevention’s sexually transmitted infection treatment guidelines state that removal of the IUD is not mandatory, but if the patient is not responding to treatment removal ultimately may be necessary. The IUD should be removed if there is no improvement in the patient’s symptoms with antibiotic therapy, there is no decrease in size of the TOA with antibiotic therapy, or if there is no positive test of cure after treatment for the TOA is completed.
If a patient has progressive abdominal pain and other findings consistent with infectious etiology, consider that a ruptured appendix could have a very similar appearance to a TOA. Computed tomography can be a useful tool to aid in firm diagnosis in cases in which gastroenterologic entities must be ruled out, but ultimately the gold standard of diagnosis for both of these procedures is diagnostic laparoscopy. Diagnostic surgery can be performed if the patient does not respond to medical therapy. In an effort to avoid surgical intervention, interventional radiology may be an option to drain the TOA. If this is performed, it is useful to repeat the ultrasound to confirm resolution prior to removal of the drain.
Case 2: Acute-onset severe pelvic pain in a young adolescent
A 12-year-old girl presents to the emergency department with acute-onset right lower quadrant pain. She states that about 2 hours ago she was playing in the yard and suddenly doubled over with pain. She also has had nausea and vomiting since that time.
She is in obvious distress and is resting in the fetal position. Examination reveals normal vital signs and tenderness to palpation over the right lower pelvic quadrant. There is no palpable abdominal mass. Genital examination reveals Tanner stage 4 external genitalia with normal introitus and patent, intact, annular hymen.
An abdominal ultrasound reveals a normal appendix, and pelvic ultrasonography reveals that the right ovary is enlarged (volume = 25 mL). The left ovary shows no obvious mass and a volume of 8 mL.
She is taken to the operating room, where you perform diagnostic laparoscopy.
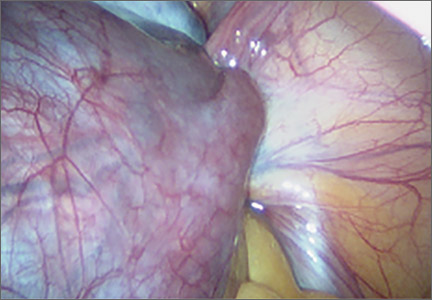
Diagnosis: Adnexal torsion (FIGURE 1).
Treatment: Surgical detorsion with or without cystectomy.
Ultrasonography certainly can be useful in determining the size of an adnexal mass. An adnexal volume of less than 20 mL is strong evidence against adnexal torsion in an adolescent. This information, in addition to the remainder of the clinical picture, can be used to determine if surgery is immediately necessary or can be delayed.3
Several studies have attempted to draw a link between size of an ovarian mass and risk of malignancy. Unfortunately, such attempts have been unsuccessful, especially for large and small masses.4 In addition, many studies have explored the use of Doppler technology to confirm a diagnosis of torsion found on sonography. Studies have shown, however, that diminished or absent Doppler flow is not a reliable finding and that ovarian blood flow can be preserved in cases of surgically confirmed adnexal torsion.5
Torsion ultimately is a clinical diagnosis, and medical history and physical examination are critical in the decision-making process. The decision to go to the operating room for further evaluation never should be made based on ultrasound findings alone, as not all ovarian torsions result in a mass greater than 20 mL.
Clinical pearl. In the setting of a known adnexal cyst, it is important to impress upon patients and their parents the warning signs of torsion and the need to proceed directly to the emergency center if acute pelvic pain occurs.
Historically, adnexal torsion is correlated with oophorectomy, but recent studies indicate that ovarian function can be preserved in the majority of cases with detorsion and cystectomy alone.6,7 In cases in which no cyst is present, detorsion is therapeutic.
In addition, studies have shown that the appearance of the ovary is not indicative of damage to the ovary. Regardless of “necrotic” appearance, the adnexa should be preserved.8,9 Ovarian function after detorsion also has been assessed in a case series that showed normal follicular development on ultrasonography in more than 90% of patients after detorsion. In this group, 6 of 102 patients with torsion eventually underwent in vitro fertilization and, in all 6 patients, oocytes retrieved from the ischemic ovary were fertilized.10
Case 3: 15-year-old girl with nontender, palpable abdominal mass
A 15-year-old adolescent comes to your office for a well woman exam and to establish gynecologic care. Abdominal examination reveals a mass below the umbilicus that is nontender to palpation. The remainder of the examination is normal, and the patient is sent for ultrasonography. Results reveal a complex-appearing mass in the left ovary that measures 8 cm x 7 cm x 8 cm. The report states that the mass shows areas of fat and calcifications. There are no other abnormalities noted in the abdomen or pelvis.
Diagnosis: Dermoid cyst.
Treatment: Surgical intervention versus expectant management.
Germ cell ovarian tumors are a diverse category of tumors that include both benign and malignant disease. The ovarian teratoma (“dermoid”) is the most common and perhaps best-known example of a benign ovarian germ cell tumor (FIGURE 2). While the incidence in the general population is unknown, dermoids account for approximately 65% of adnexal masses in pediatric patients presenting for treatment.11 Most of the time, patients with ovarian dermoids will be asymptomatic; however, pain is the most common presenting symptom.
The spectrum of sonographic features includes:
- mixed echogenicity with posterior sound attenuation owing to sebaceous material and hair within the cyst
- echogenic interface at the edge of the mass that obscures deep structures (the tip-of-the-iceberg sign)
- mural hyperechoic Rokitansky nodule (dermoid plug)
- shadowing due to calcific or dental (tooth) components
- presence of layered-fluid levels
- multiple thin, echogenic bands caused by hair in the cyst cavity (the dot-dash pattern)
- absence of internal vascularity noted with color Doppler evaluation.
The notation of internal vascularity is concerning for malignancy.12
Fortunately, malignant ovarian germ cell tumors are much less common than benign lesions. Of these, the most common pediatric ovarian germ cell tumor is dysgerminoma (FIGURE 3).13
Clinical pearl. A unique consideration in patients with dysgerminoma or choriocarcinoma is the possible diagnosis of XY gonadal dysgenesis, or Swyer syndrome.14,15 This may be seen in young girls with female external genitalia and primary amenorrhea. Depending on the level of concern, obtaining a karyotype also may be beneficial.13
Sex cord−stromal tumors also are relatively common in the pediatric population.16 Of these, granulosa cell tumors are the most common and account for 2% to 5% of ovarian malignancies regardless of age at diagnosis. Juvenile-type granulosa ovarian cancers occur mainly in premenarchal girls and comprise roughly 5% of all granulosa cell tumors.17 The presenting problem usually is precocious puberty. Therefore, in any situation in which a prepubertal girl is developing too early and peripheral precocious puberty is suspected, sonography should be obtained to rule out a hormone-producing ovarian mass. Tumor markers most helpful in this situation include estradiol, testosterone, and inhibin B.17
When an adolescent is diagnosed with ovarian cancer, it is ideal to perform a fertility-sparing procedure whenever it is reasonable.18 While dermoid cysts can look concerning on sonography because of their heterogeneous appearance, the vast majority can be safely and effectively resected without oophorectomy in order to preserve fertility, as in most cases they are benign. Nonetheless, cystectomy does have a small, theoretic risk of cyst rupture, with the potential for pelvic peritonitis from dermoid content spillage.19 In the vast majority of cases in which a benign adnexal mass is identified, ovarian cystectomy is appropriate and oophorectomy is not indicated.20
Another very rare presentation of mature cystic teratoma can include acute neurologic decline in cases of paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis. Frequently, these teratomas will be small in size and discovered only incidentally during the work-up of a patient with altered mental status. Resection is indicated as soon as possible to stop the neurologic decline.21
Case 4: Cyclic pelvic pain and a pelvic mass in a 16-year-old
A 16-year-old adolescent presents to your office for evaluation of cyclic pelvic pain. She states that menarche occurred at age 12 years and menses have been irregular ever since, occurring every few months and associated with significant pain with the onset of bleeding.
Physical examination reveals Tanner stage 4 breasts and Tanner stage 4 external genitalia. The introitus is normal with a visible intact, annular hymen. A mildly tender palpable mass at the level of the umbilicus is noted. The patient consents to having a Q-tip placed in the vagina, which reveals a bulge in the left vaginal wall that is nontender and fluctuant. Pelvic ultrasonography reveals uterine didelphys and an obstructed left hemivagina. A renal ultrasound reveals an absent left kidney.
Diagnosis: OHVIRA (obstructed hemivagina and ipsilateral renal anomaly) syndrome.
Treatment: Surgical resection of the vaginal septum.
Masses that appear complex on imaging can be deceiving, as they also can be related to obstructive reproductive tract anomalies. “Pelvic mass” is often the working diagnosis in cases of imperforate hymen, vaginal atresia, cervical agenesis, and uterine didelphys with obstructed hemivagina. This underscores the importance of taking an accurate menstrual history as well as performing a thorough physical examination. Usually this does not require an internal vaginal examination if the patient is unable to tolerate one, but a rectal examination can provide similar information in a patient presenting with a “pelvic mass” who will consent to this portion of the exam.
Clinical pearl. If a patient is not comfortable consenting to a rectal exam, a lubricated Q-tip can be used to palpate the vagina to minimize patient discomfort.
Before performing surgery…
Vaginal surgery can be corrective in the majority of these cases; however, magnetic resonance imaging is the gold standard for diagnosis and should be performed prior to surgical planning to further characterize the anomaly.22 Because Müllerian anomalies are associated with renal malformation such as absent kidney, pelvic kidney, collecting system duplication, or ectopic ureteral insertion around 40% of the time, imaging studies to assess for these structures is important prior to surgical intervention.23 If the patient is symptomatic and surgery cannot be performed immediately in a safe manner, she may require admission for pain control and placement of a Foley catheter (if the mass is obstructing urinary flow) until surgery can be performed safely.
A comprehensive review of Müllerian anomalies is beyond the scope of this article; it is important to note that these clinical scenarios are always unique and treatment should be individualized.
Conclusion
There are many sources of pelvic masses in children, adolescents, and young women; not all sources will be gynecologic. To avoid unnecessary surgical intervention, it is important to obtain as much information as possible from the patient’s history, physical examination, and laboratory and imaging studies.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Petroianu A, Alberti LR. Accuracy of the new radiographic sign of fecal loading in the cecum for differential diagnosis of acute appendicitis in comparison with other inflammatory diseases of right abdomen: a prospective study. J Med Life. 2012;5(1):85–91.
2. Emans SJ, Laufer MR, eds. Goldstein’s Pediatric and Adolescent Gynecology. Philadelphia: Lippincott Williams & Wilkins; 2011.
3. Linam LE, Darolia R, Naffaa LN, et al. US findings of adnexal torsion in children and adolescents: size really does matter. Pediatr Radiol. 2007;37(10):1013–1019.
4. DiLegge A, Testa AC, Ameye L, et al. Lesion size affects diagnostic performance of IOTA logistic regression models, IOTA simple rules and risk of malignancy index in discriminating between benign and malignant adnexal masses. Ultrasound Obstet Gynecol. 2012;40(3):345–354.
5. Rosado WM, Trambert MA, Gosink BB, Pretorius DH. Adnexal torsion: diagnosis by using Doppler sonography. Am J Roentgenol. 1992;159(6):1251–1253.
6. Cocmen A, Karaca M, Sari A. Conservative laparoscopic approach to adnexal torsion. Arch Gynecol Obstet. 2008;227(6):535–538.
7. Oelsner G, Shashar D. Adnexal torsion. Clin Obstet Gynecol. 2006;49(3):459–463.
8. Cass DL. Ovarian torsion. Semin Pediatr Surg. 2005;14(2):86–92.
9. Mazouni C, Bretelle F, Menard JP, et al. Diagnosis of adnexal torsion and predictive factors of adnexal necrosis. Gynecol Obstet Fertil. 2005;33(3):102–106.
10. Oelsner G, Cohen SB, Soriano D, et al. Minimal surgery for the twisted ischaemic adnexa can preserve ovarian function. Hum Reprod. 2003;18(12):2599–2602.
11. Ehren, IM, Mahour GH, Isaacs H Jr. Benign and malignant ovarian tumors in children and adolescents. A review of 63 cases. Am J Surg. 1984;147(3):339–344.
12. Sanfilippo JS, Lara-Torre E, Edmonds DK, Templeman C, eds. Clinical Pediatric and Adolescent Gynecology. 450 pp., illustrated, with CD-ROM. New York: Informa Healthcare; 2009.
13. Chieffi P, Chieffi S, Franco R, Sinisi AA. Recent advances in the biology of germ cell tumors: implications for the diagnosis and treatment. J Endocrinol Invest. 2012;35(11):1015–1020.
14. Lee AC, Fong C. Ovarian choriocarcinoma as the first manifestation of 46,XY pure gonadal dysgenesis. J Pediatr Hematol Oncol. 2011;33(1):e29–e31.
15. Stachowicz-Stencel T, Synakiewicz A, Izycka-Swieszewska E, Kobierska-Gulida G, Belcerska A. Malignant germ cell tumors associated with Swyer Syndrome. Pediatr Blood Cancer. 2011;56(3):482–483.
16. Barakat RR, Markman M, Randall M. Principles and Practice of Gynecologic Oncology. Philadelphia: Lippincott Williams & Wilkins; 2009.
17. Gell JS, Stannard MW, Ramnani DM, Bradshaw KD. Juvenile granulosa cell tumor in a 13-year-old girl with enchondromatosis (Ollier’s disease): a case report. J Pediatr Adolesc Gynecol. 1998;11(3):147–150.
18. Maltaris T, Boehm D, Dittrich R, Seufert R, Koelbl H. Reproduction beyond cancer: a message of hope for young women. Gynecol Oncol. 2006;103(3):1109–1121.
19. Ozcan R, Kuruoglu S, Dervisoglu S, Elicevik M, Emir H, Buyukunal C. Ovarian-sparing surgery for teratomas in children. Pediatr Surg Int. 2013;29(3):233–237.
20. Eskander RN, Bristow RE, Saenz NC, Saenz CC. A retrospective review of the effect of surgeon specialty on the management of 190 benign and malignant pediatric and adolescent adnexal masses. J Pediatr Adolesc Gynecol. 2011;24(5):282–285.
21. Dalmau J, Tuzun E, Wu HY, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61(1):25–36.
22. Behr SC, Courtier JL, Qayyum A. Imaging of Müllerian duct anomalies. Radiographics. 2012;32(6):E233–E250.
23. Hall-Craggs MA, Kirkham A, Creighton SM. Renal and urological abnormalities occurring with Müllerian anomalies. J Pediatr Urol. 2013;9(1):27–32.
Pelvic masses frequently are the reason for the medical evaluation of young women and girls. Regardless of what prompted the work-up that led to the mass’ discovery, the patient inevitably will be sent to a gynecologist for further evaluation, and such a practitioner should be involved whenever there is suspicion for a mass involving the reproductive tract.
While it does not happen often, it is possible that a mass diagnosed as ovarian, based on imaging, is then determined to be of another organ system at the time of surgery. Most frequently, this occurs with ruptured appendicitis, as the presence of an appendiceal abscess can mimic a complex ovarian mass or tubo-ovarian abscess (TOA).1
The full differential diagnosis of non-gynecologic pelvic masses is extensive and includes mesenteric duplication cysts, presacral masses, pelvic kidney, peritoneal inclusion cysts, and urachal cysts (TABLE). It can be difficult to distinguish pathology as gynecologic or nongynecologic even if a thorough work-up is performed.
Differential diagnosis for a pelvic mass
|
In this review, we offer several cases involving varying presentations of pelvic masses related to the reproductive tract.
Case 1: Severe pelvic pain in an 18-year-old
An 18-year-old adolescent presents to your office reporting worsening pelvic pain over the past 3 days. The pain is severe in the left lower quadrant. She reports a foul discharge and thinks she has a fever but hasn’t checked her temperature. She says she has been sexually active in the past few months with 2 different male partners. She has not been using condoms consistently and hasn’t been tested for sexually transmitted infections. Physical examination reveals a mucopurulent discharge at the cervix and copious white blood cells noted on wet mount. Bimanual examination reveals cervical motion tenderness and tenderness over the left adnexa. Ultrasound reveals a mass in the left adnexa with debris and internal echoes.
Diagnosis: Tubo-ovarian abscess.
Treatment: Admission to the hospital for intravenous antibiotic therapy.
It is important to note that TOAs can be seen in patients who have not been sexually active, as well as in cases related not to an ascending infection but rather to a history of pelvic surgery or complex structural anomaly.2 The majority of the time a TOA is a result of pelvic inflammatory disease (PID). Often, patients with uncomplicated PID can be treated on an outpatient basis if they meet strict criteria, but patients with a TOA need to be treated as an inpatient due to the severity of this infection.
Clinical pearl. If a patient has an IUD in place, close clinical follow up is critical to determine response to therapy. The Centers for Disease Control and Prevention’s sexually transmitted infection treatment guidelines state that removal of the IUD is not mandatory, but if the patient is not responding to treatment removal ultimately may be necessary. The IUD should be removed if there is no improvement in the patient’s symptoms with antibiotic therapy, there is no decrease in size of the TOA with antibiotic therapy, or if there is no positive test of cure after treatment for the TOA is completed.
If a patient has progressive abdominal pain and other findings consistent with infectious etiology, consider that a ruptured appendix could have a very similar appearance to a TOA. Computed tomography can be a useful tool to aid in firm diagnosis in cases in which gastroenterologic entities must be ruled out, but ultimately the gold standard of diagnosis for both of these procedures is diagnostic laparoscopy. Diagnostic surgery can be performed if the patient does not respond to medical therapy. In an effort to avoid surgical intervention, interventional radiology may be an option to drain the TOA. If this is performed, it is useful to repeat the ultrasound to confirm resolution prior to removal of the drain.
Case 2: Acute-onset severe pelvic pain in a young adolescent
A 12-year-old girl presents to the emergency department with acute-onset right lower quadrant pain. She states that about 2 hours ago she was playing in the yard and suddenly doubled over with pain. She also has had nausea and vomiting since that time.
She is in obvious distress and is resting in the fetal position. Examination reveals normal vital signs and tenderness to palpation over the right lower pelvic quadrant. There is no palpable abdominal mass. Genital examination reveals Tanner stage 4 external genitalia with normal introitus and patent, intact, annular hymen.
An abdominal ultrasound reveals a normal appendix, and pelvic ultrasonography reveals that the right ovary is enlarged (volume = 25 mL). The left ovary shows no obvious mass and a volume of 8 mL.
She is taken to the operating room, where you perform diagnostic laparoscopy.
Diagnosis: Adnexal torsion (FIGURE 1).
Treatment: Surgical detorsion with or without cystectomy.
Ultrasonography certainly can be useful in determining the size of an adnexal mass. An adnexal volume of less than 20 mL is strong evidence against adnexal torsion in an adolescent. This information, in addition to the remainder of the clinical picture, can be used to determine if surgery is immediately necessary or can be delayed.3
Several studies have attempted to draw a link between size of an ovarian mass and risk of malignancy. Unfortunately, such attempts have been unsuccessful, especially for large and small masses.4 In addition, many studies have explored the use of Doppler technology to confirm a diagnosis of torsion found on sonography. Studies have shown, however, that diminished or absent Doppler flow is not a reliable finding and that ovarian blood flow can be preserved in cases of surgically confirmed adnexal torsion.5
Torsion ultimately is a clinical diagnosis, and medical history and physical examination are critical in the decision-making process. The decision to go to the operating room for further evaluation never should be made based on ultrasound findings alone, as not all ovarian torsions result in a mass greater than 20 mL.
Clinical pearl. In the setting of a known adnexal cyst, it is important to impress upon patients and their parents the warning signs of torsion and the need to proceed directly to the emergency center if acute pelvic pain occurs.
Historically, adnexal torsion is correlated with oophorectomy, but recent studies indicate that ovarian function can be preserved in the majority of cases with detorsion and cystectomy alone.6,7 In cases in which no cyst is present, detorsion is therapeutic.
In addition, studies have shown that the appearance of the ovary is not indicative of damage to the ovary. Regardless of “necrotic” appearance, the adnexa should be preserved.8,9 Ovarian function after detorsion also has been assessed in a case series that showed normal follicular development on ultrasonography in more than 90% of patients after detorsion. In this group, 6 of 102 patients with torsion eventually underwent in vitro fertilization and, in all 6 patients, oocytes retrieved from the ischemic ovary were fertilized.10
Case 3: 15-year-old girl with nontender, palpable abdominal mass
A 15-year-old adolescent comes to your office for a well woman exam and to establish gynecologic care. Abdominal examination reveals a mass below the umbilicus that is nontender to palpation. The remainder of the examination is normal, and the patient is sent for ultrasonography. Results reveal a complex-appearing mass in the left ovary that measures 8 cm x 7 cm x 8 cm. The report states that the mass shows areas of fat and calcifications. There are no other abnormalities noted in the abdomen or pelvis.
Diagnosis: Dermoid cyst.
Treatment: Surgical intervention versus expectant management.
Germ cell ovarian tumors are a diverse category of tumors that include both benign and malignant disease. The ovarian teratoma (“dermoid”) is the most common and perhaps best-known example of a benign ovarian germ cell tumor (FIGURE 2). While the incidence in the general population is unknown, dermoids account for approximately 65% of adnexal masses in pediatric patients presenting for treatment.11 Most of the time, patients with ovarian dermoids will be asymptomatic; however, pain is the most common presenting symptom.
The spectrum of sonographic features includes:
- mixed echogenicity with posterior sound attenuation owing to sebaceous material and hair within the cyst
- echogenic interface at the edge of the mass that obscures deep structures (the tip-of-the-iceberg sign)
- mural hyperechoic Rokitansky nodule (dermoid plug)
- shadowing due to calcific or dental (tooth) components
- presence of layered-fluid levels
- multiple thin, echogenic bands caused by hair in the cyst cavity (the dot-dash pattern)
- absence of internal vascularity noted with color Doppler evaluation.
The notation of internal vascularity is concerning for malignancy.12
Fortunately, malignant ovarian germ cell tumors are much less common than benign lesions. Of these, the most common pediatric ovarian germ cell tumor is dysgerminoma (FIGURE 3).13
Clinical pearl. A unique consideration in patients with dysgerminoma or choriocarcinoma is the possible diagnosis of XY gonadal dysgenesis, or Swyer syndrome.14,15 This may be seen in young girls with female external genitalia and primary amenorrhea. Depending on the level of concern, obtaining a karyotype also may be beneficial.13
Sex cord−stromal tumors also are relatively common in the pediatric population.16 Of these, granulosa cell tumors are the most common and account for 2% to 5% of ovarian malignancies regardless of age at diagnosis. Juvenile-type granulosa ovarian cancers occur mainly in premenarchal girls and comprise roughly 5% of all granulosa cell tumors.17 The presenting problem usually is precocious puberty. Therefore, in any situation in which a prepubertal girl is developing too early and peripheral precocious puberty is suspected, sonography should be obtained to rule out a hormone-producing ovarian mass. Tumor markers most helpful in this situation include estradiol, testosterone, and inhibin B.17
When an adolescent is diagnosed with ovarian cancer, it is ideal to perform a fertility-sparing procedure whenever it is reasonable.18 While dermoid cysts can look concerning on sonography because of their heterogeneous appearance, the vast majority can be safely and effectively resected without oophorectomy in order to preserve fertility, as in most cases they are benign. Nonetheless, cystectomy does have a small, theoretic risk of cyst rupture, with the potential for pelvic peritonitis from dermoid content spillage.19 In the vast majority of cases in which a benign adnexal mass is identified, ovarian cystectomy is appropriate and oophorectomy is not indicated.20
Another very rare presentation of mature cystic teratoma can include acute neurologic decline in cases of paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis. Frequently, these teratomas will be small in size and discovered only incidentally during the work-up of a patient with altered mental status. Resection is indicated as soon as possible to stop the neurologic decline.21
Case 4: Cyclic pelvic pain and a pelvic mass in a 16-year-old
A 16-year-old adolescent presents to your office for evaluation of cyclic pelvic pain. She states that menarche occurred at age 12 years and menses have been irregular ever since, occurring every few months and associated with significant pain with the onset of bleeding.
Physical examination reveals Tanner stage 4 breasts and Tanner stage 4 external genitalia. The introitus is normal with a visible intact, annular hymen. A mildly tender palpable mass at the level of the umbilicus is noted. The patient consents to having a Q-tip placed in the vagina, which reveals a bulge in the left vaginal wall that is nontender and fluctuant. Pelvic ultrasonography reveals uterine didelphys and an obstructed left hemivagina. A renal ultrasound reveals an absent left kidney.
Diagnosis: OHVIRA (obstructed hemivagina and ipsilateral renal anomaly) syndrome.
Treatment: Surgical resection of the vaginal septum.
Masses that appear complex on imaging can be deceiving, as they also can be related to obstructive reproductive tract anomalies. “Pelvic mass” is often the working diagnosis in cases of imperforate hymen, vaginal atresia, cervical agenesis, and uterine didelphys with obstructed hemivagina. This underscores the importance of taking an accurate menstrual history as well as performing a thorough physical examination. Usually this does not require an internal vaginal examination if the patient is unable to tolerate one, but a rectal examination can provide similar information in a patient presenting with a “pelvic mass” who will consent to this portion of the exam.
Clinical pearl. If a patient is not comfortable consenting to a rectal exam, a lubricated Q-tip can be used to palpate the vagina to minimize patient discomfort.
Before performing surgery…
Vaginal surgery can be corrective in the majority of these cases; however, magnetic resonance imaging is the gold standard for diagnosis and should be performed prior to surgical planning to further characterize the anomaly.22 Because Müllerian anomalies are associated with renal malformation such as absent kidney, pelvic kidney, collecting system duplication, or ectopic ureteral insertion around 40% of the time, imaging studies to assess for these structures is important prior to surgical intervention.23 If the patient is symptomatic and surgery cannot be performed immediately in a safe manner, she may require admission for pain control and placement of a Foley catheter (if the mass is obstructing urinary flow) until surgery can be performed safely.
A comprehensive review of Müllerian anomalies is beyond the scope of this article; it is important to note that these clinical scenarios are always unique and treatment should be individualized.
Conclusion
There are many sources of pelvic masses in children, adolescents, and young women; not all sources will be gynecologic. To avoid unnecessary surgical intervention, it is important to obtain as much information as possible from the patient’s history, physical examination, and laboratory and imaging studies.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Pelvic masses frequently are the reason for the medical evaluation of young women and girls. Regardless of what prompted the work-up that led to the mass’ discovery, the patient inevitably will be sent to a gynecologist for further evaluation, and such a practitioner should be involved whenever there is suspicion for a mass involving the reproductive tract.
While it does not happen often, it is possible that a mass diagnosed as ovarian, based on imaging, is then determined to be of another organ system at the time of surgery. Most frequently, this occurs with ruptured appendicitis, as the presence of an appendiceal abscess can mimic a complex ovarian mass or tubo-ovarian abscess (TOA).1
The full differential diagnosis of non-gynecologic pelvic masses is extensive and includes mesenteric duplication cysts, presacral masses, pelvic kidney, peritoneal inclusion cysts, and urachal cysts (TABLE). It can be difficult to distinguish pathology as gynecologic or nongynecologic even if a thorough work-up is performed.
Differential diagnosis for a pelvic mass
|
In this review, we offer several cases involving varying presentations of pelvic masses related to the reproductive tract.
Case 1: Severe pelvic pain in an 18-year-old
An 18-year-old adolescent presents to your office reporting worsening pelvic pain over the past 3 days. The pain is severe in the left lower quadrant. She reports a foul discharge and thinks she has a fever but hasn’t checked her temperature. She says she has been sexually active in the past few months with 2 different male partners. She has not been using condoms consistently and hasn’t been tested for sexually transmitted infections. Physical examination reveals a mucopurulent discharge at the cervix and copious white blood cells noted on wet mount. Bimanual examination reveals cervical motion tenderness and tenderness over the left adnexa. Ultrasound reveals a mass in the left adnexa with debris and internal echoes.
Diagnosis: Tubo-ovarian abscess.
Treatment: Admission to the hospital for intravenous antibiotic therapy.
It is important to note that TOAs can be seen in patients who have not been sexually active, as well as in cases related not to an ascending infection but rather to a history of pelvic surgery or complex structural anomaly.2 The majority of the time a TOA is a result of pelvic inflammatory disease (PID). Often, patients with uncomplicated PID can be treated on an outpatient basis if they meet strict criteria, but patients with a TOA need to be treated as an inpatient due to the severity of this infection.
Clinical pearl. If a patient has an IUD in place, close clinical follow up is critical to determine response to therapy. The Centers for Disease Control and Prevention’s sexually transmitted infection treatment guidelines state that removal of the IUD is not mandatory, but if the patient is not responding to treatment removal ultimately may be necessary. The IUD should be removed if there is no improvement in the patient’s symptoms with antibiotic therapy, there is no decrease in size of the TOA with antibiotic therapy, or if there is no positive test of cure after treatment for the TOA is completed.
If a patient has progressive abdominal pain and other findings consistent with infectious etiology, consider that a ruptured appendix could have a very similar appearance to a TOA. Computed tomography can be a useful tool to aid in firm diagnosis in cases in which gastroenterologic entities must be ruled out, but ultimately the gold standard of diagnosis for both of these procedures is diagnostic laparoscopy. Diagnostic surgery can be performed if the patient does not respond to medical therapy. In an effort to avoid surgical intervention, interventional radiology may be an option to drain the TOA. If this is performed, it is useful to repeat the ultrasound to confirm resolution prior to removal of the drain.
Case 2: Acute-onset severe pelvic pain in a young adolescent
A 12-year-old girl presents to the emergency department with acute-onset right lower quadrant pain. She states that about 2 hours ago she was playing in the yard and suddenly doubled over with pain. She also has had nausea and vomiting since that time.
She is in obvious distress and is resting in the fetal position. Examination reveals normal vital signs and tenderness to palpation over the right lower pelvic quadrant. There is no palpable abdominal mass. Genital examination reveals Tanner stage 4 external genitalia with normal introitus and patent, intact, annular hymen.
An abdominal ultrasound reveals a normal appendix, and pelvic ultrasonography reveals that the right ovary is enlarged (volume = 25 mL). The left ovary shows no obvious mass and a volume of 8 mL.
She is taken to the operating room, where you perform diagnostic laparoscopy.
Diagnosis: Adnexal torsion (FIGURE 1).
Treatment: Surgical detorsion with or without cystectomy.
Ultrasonography certainly can be useful in determining the size of an adnexal mass. An adnexal volume of less than 20 mL is strong evidence against adnexal torsion in an adolescent. This information, in addition to the remainder of the clinical picture, can be used to determine if surgery is immediately necessary or can be delayed.3
Several studies have attempted to draw a link between size of an ovarian mass and risk of malignancy. Unfortunately, such attempts have been unsuccessful, especially for large and small masses.4 In addition, many studies have explored the use of Doppler technology to confirm a diagnosis of torsion found on sonography. Studies have shown, however, that diminished or absent Doppler flow is not a reliable finding and that ovarian blood flow can be preserved in cases of surgically confirmed adnexal torsion.5
Torsion ultimately is a clinical diagnosis, and medical history and physical examination are critical in the decision-making process. The decision to go to the operating room for further evaluation never should be made based on ultrasound findings alone, as not all ovarian torsions result in a mass greater than 20 mL.
Clinical pearl. In the setting of a known adnexal cyst, it is important to impress upon patients and their parents the warning signs of torsion and the need to proceed directly to the emergency center if acute pelvic pain occurs.
Historically, adnexal torsion is correlated with oophorectomy, but recent studies indicate that ovarian function can be preserved in the majority of cases with detorsion and cystectomy alone.6,7 In cases in which no cyst is present, detorsion is therapeutic.
In addition, studies have shown that the appearance of the ovary is not indicative of damage to the ovary. Regardless of “necrotic” appearance, the adnexa should be preserved.8,9 Ovarian function after detorsion also has been assessed in a case series that showed normal follicular development on ultrasonography in more than 90% of patients after detorsion. In this group, 6 of 102 patients with torsion eventually underwent in vitro fertilization and, in all 6 patients, oocytes retrieved from the ischemic ovary were fertilized.10
Case 3: 15-year-old girl with nontender, palpable abdominal mass
A 15-year-old adolescent comes to your office for a well woman exam and to establish gynecologic care. Abdominal examination reveals a mass below the umbilicus that is nontender to palpation. The remainder of the examination is normal, and the patient is sent for ultrasonography. Results reveal a complex-appearing mass in the left ovary that measures 8 cm x 7 cm x 8 cm. The report states that the mass shows areas of fat and calcifications. There are no other abnormalities noted in the abdomen or pelvis.
Diagnosis: Dermoid cyst.
Treatment: Surgical intervention versus expectant management.
Germ cell ovarian tumors are a diverse category of tumors that include both benign and malignant disease. The ovarian teratoma (“dermoid”) is the most common and perhaps best-known example of a benign ovarian germ cell tumor (FIGURE 2). While the incidence in the general population is unknown, dermoids account for approximately 65% of adnexal masses in pediatric patients presenting for treatment.11 Most of the time, patients with ovarian dermoids will be asymptomatic; however, pain is the most common presenting symptom.
The spectrum of sonographic features includes:
- mixed echogenicity with posterior sound attenuation owing to sebaceous material and hair within the cyst
- echogenic interface at the edge of the mass that obscures deep structures (the tip-of-the-iceberg sign)
- mural hyperechoic Rokitansky nodule (dermoid plug)
- shadowing due to calcific or dental (tooth) components
- presence of layered-fluid levels
- multiple thin, echogenic bands caused by hair in the cyst cavity (the dot-dash pattern)
- absence of internal vascularity noted with color Doppler evaluation.
The notation of internal vascularity is concerning for malignancy.12
Fortunately, malignant ovarian germ cell tumors are much less common than benign lesions. Of these, the most common pediatric ovarian germ cell tumor is dysgerminoma (FIGURE 3).13
Clinical pearl. A unique consideration in patients with dysgerminoma or choriocarcinoma is the possible diagnosis of XY gonadal dysgenesis, or Swyer syndrome.14,15 This may be seen in young girls with female external genitalia and primary amenorrhea. Depending on the level of concern, obtaining a karyotype also may be beneficial.13
Sex cord−stromal tumors also are relatively common in the pediatric population.16 Of these, granulosa cell tumors are the most common and account for 2% to 5% of ovarian malignancies regardless of age at diagnosis. Juvenile-type granulosa ovarian cancers occur mainly in premenarchal girls and comprise roughly 5% of all granulosa cell tumors.17 The presenting problem usually is precocious puberty. Therefore, in any situation in which a prepubertal girl is developing too early and peripheral precocious puberty is suspected, sonography should be obtained to rule out a hormone-producing ovarian mass. Tumor markers most helpful in this situation include estradiol, testosterone, and inhibin B.17
When an adolescent is diagnosed with ovarian cancer, it is ideal to perform a fertility-sparing procedure whenever it is reasonable.18 While dermoid cysts can look concerning on sonography because of their heterogeneous appearance, the vast majority can be safely and effectively resected without oophorectomy in order to preserve fertility, as in most cases they are benign. Nonetheless, cystectomy does have a small, theoretic risk of cyst rupture, with the potential for pelvic peritonitis from dermoid content spillage.19 In the vast majority of cases in which a benign adnexal mass is identified, ovarian cystectomy is appropriate and oophorectomy is not indicated.20
Another very rare presentation of mature cystic teratoma can include acute neurologic decline in cases of paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis. Frequently, these teratomas will be small in size and discovered only incidentally during the work-up of a patient with altered mental status. Resection is indicated as soon as possible to stop the neurologic decline.21
Case 4: Cyclic pelvic pain and a pelvic mass in a 16-year-old
A 16-year-old adolescent presents to your office for evaluation of cyclic pelvic pain. She states that menarche occurred at age 12 years and menses have been irregular ever since, occurring every few months and associated with significant pain with the onset of bleeding.
Physical examination reveals Tanner stage 4 breasts and Tanner stage 4 external genitalia. The introitus is normal with a visible intact, annular hymen. A mildly tender palpable mass at the level of the umbilicus is noted. The patient consents to having a Q-tip placed in the vagina, which reveals a bulge in the left vaginal wall that is nontender and fluctuant. Pelvic ultrasonography reveals uterine didelphys and an obstructed left hemivagina. A renal ultrasound reveals an absent left kidney.
Diagnosis: OHVIRA (obstructed hemivagina and ipsilateral renal anomaly) syndrome.
Treatment: Surgical resection of the vaginal septum.
Masses that appear complex on imaging can be deceiving, as they also can be related to obstructive reproductive tract anomalies. “Pelvic mass” is often the working diagnosis in cases of imperforate hymen, vaginal atresia, cervical agenesis, and uterine didelphys with obstructed hemivagina. This underscores the importance of taking an accurate menstrual history as well as performing a thorough physical examination. Usually this does not require an internal vaginal examination if the patient is unable to tolerate one, but a rectal examination can provide similar information in a patient presenting with a “pelvic mass” who will consent to this portion of the exam.
Clinical pearl. If a patient is not comfortable consenting to a rectal exam, a lubricated Q-tip can be used to palpate the vagina to minimize patient discomfort.
Before performing surgery…
Vaginal surgery can be corrective in the majority of these cases; however, magnetic resonance imaging is the gold standard for diagnosis and should be performed prior to surgical planning to further characterize the anomaly.22 Because Müllerian anomalies are associated with renal malformation such as absent kidney, pelvic kidney, collecting system duplication, or ectopic ureteral insertion around 40% of the time, imaging studies to assess for these structures is important prior to surgical intervention.23 If the patient is symptomatic and surgery cannot be performed immediately in a safe manner, she may require admission for pain control and placement of a Foley catheter (if the mass is obstructing urinary flow) until surgery can be performed safely.
A comprehensive review of Müllerian anomalies is beyond the scope of this article; it is important to note that these clinical scenarios are always unique and treatment should be individualized.
Conclusion
There are many sources of pelvic masses in children, adolescents, and young women; not all sources will be gynecologic. To avoid unnecessary surgical intervention, it is important to obtain as much information as possible from the patient’s history, physical examination, and laboratory and imaging studies.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Petroianu A, Alberti LR. Accuracy of the new radiographic sign of fecal loading in the cecum for differential diagnosis of acute appendicitis in comparison with other inflammatory diseases of right abdomen: a prospective study. J Med Life. 2012;5(1):85–91.
2. Emans SJ, Laufer MR, eds. Goldstein’s Pediatric and Adolescent Gynecology. Philadelphia: Lippincott Williams & Wilkins; 2011.
3. Linam LE, Darolia R, Naffaa LN, et al. US findings of adnexal torsion in children and adolescents: size really does matter. Pediatr Radiol. 2007;37(10):1013–1019.
4. DiLegge A, Testa AC, Ameye L, et al. Lesion size affects diagnostic performance of IOTA logistic regression models, IOTA simple rules and risk of malignancy index in discriminating between benign and malignant adnexal masses. Ultrasound Obstet Gynecol. 2012;40(3):345–354.
5. Rosado WM, Trambert MA, Gosink BB, Pretorius DH. Adnexal torsion: diagnosis by using Doppler sonography. Am J Roentgenol. 1992;159(6):1251–1253.
6. Cocmen A, Karaca M, Sari A. Conservative laparoscopic approach to adnexal torsion. Arch Gynecol Obstet. 2008;227(6):535–538.
7. Oelsner G, Shashar D. Adnexal torsion. Clin Obstet Gynecol. 2006;49(3):459–463.
8. Cass DL. Ovarian torsion. Semin Pediatr Surg. 2005;14(2):86–92.
9. Mazouni C, Bretelle F, Menard JP, et al. Diagnosis of adnexal torsion and predictive factors of adnexal necrosis. Gynecol Obstet Fertil. 2005;33(3):102–106.
10. Oelsner G, Cohen SB, Soriano D, et al. Minimal surgery for the twisted ischaemic adnexa can preserve ovarian function. Hum Reprod. 2003;18(12):2599–2602.
11. Ehren, IM, Mahour GH, Isaacs H Jr. Benign and malignant ovarian tumors in children and adolescents. A review of 63 cases. Am J Surg. 1984;147(3):339–344.
12. Sanfilippo JS, Lara-Torre E, Edmonds DK, Templeman C, eds. Clinical Pediatric and Adolescent Gynecology. 450 pp., illustrated, with CD-ROM. New York: Informa Healthcare; 2009.
13. Chieffi P, Chieffi S, Franco R, Sinisi AA. Recent advances in the biology of germ cell tumors: implications for the diagnosis and treatment. J Endocrinol Invest. 2012;35(11):1015–1020.
14. Lee AC, Fong C. Ovarian choriocarcinoma as the first manifestation of 46,XY pure gonadal dysgenesis. J Pediatr Hematol Oncol. 2011;33(1):e29–e31.
15. Stachowicz-Stencel T, Synakiewicz A, Izycka-Swieszewska E, Kobierska-Gulida G, Belcerska A. Malignant germ cell tumors associated with Swyer Syndrome. Pediatr Blood Cancer. 2011;56(3):482–483.
16. Barakat RR, Markman M, Randall M. Principles and Practice of Gynecologic Oncology. Philadelphia: Lippincott Williams & Wilkins; 2009.
17. Gell JS, Stannard MW, Ramnani DM, Bradshaw KD. Juvenile granulosa cell tumor in a 13-year-old girl with enchondromatosis (Ollier’s disease): a case report. J Pediatr Adolesc Gynecol. 1998;11(3):147–150.
18. Maltaris T, Boehm D, Dittrich R, Seufert R, Koelbl H. Reproduction beyond cancer: a message of hope for young women. Gynecol Oncol. 2006;103(3):1109–1121.
19. Ozcan R, Kuruoglu S, Dervisoglu S, Elicevik M, Emir H, Buyukunal C. Ovarian-sparing surgery for teratomas in children. Pediatr Surg Int. 2013;29(3):233–237.
20. Eskander RN, Bristow RE, Saenz NC, Saenz CC. A retrospective review of the effect of surgeon specialty on the management of 190 benign and malignant pediatric and adolescent adnexal masses. J Pediatr Adolesc Gynecol. 2011;24(5):282–285.
21. Dalmau J, Tuzun E, Wu HY, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61(1):25–36.
22. Behr SC, Courtier JL, Qayyum A. Imaging of Müllerian duct anomalies. Radiographics. 2012;32(6):E233–E250.
23. Hall-Craggs MA, Kirkham A, Creighton SM. Renal and urological abnormalities occurring with Müllerian anomalies. J Pediatr Urol. 2013;9(1):27–32.
1. Petroianu A, Alberti LR. Accuracy of the new radiographic sign of fecal loading in the cecum for differential diagnosis of acute appendicitis in comparison with other inflammatory diseases of right abdomen: a prospective study. J Med Life. 2012;5(1):85–91.
2. Emans SJ, Laufer MR, eds. Goldstein’s Pediatric and Adolescent Gynecology. Philadelphia: Lippincott Williams & Wilkins; 2011.
3. Linam LE, Darolia R, Naffaa LN, et al. US findings of adnexal torsion in children and adolescents: size really does matter. Pediatr Radiol. 2007;37(10):1013–1019.
4. DiLegge A, Testa AC, Ameye L, et al. Lesion size affects diagnostic performance of IOTA logistic regression models, IOTA simple rules and risk of malignancy index in discriminating between benign and malignant adnexal masses. Ultrasound Obstet Gynecol. 2012;40(3):345–354.
5. Rosado WM, Trambert MA, Gosink BB, Pretorius DH. Adnexal torsion: diagnosis by using Doppler sonography. Am J Roentgenol. 1992;159(6):1251–1253.
6. Cocmen A, Karaca M, Sari A. Conservative laparoscopic approach to adnexal torsion. Arch Gynecol Obstet. 2008;227(6):535–538.
7. Oelsner G, Shashar D. Adnexal torsion. Clin Obstet Gynecol. 2006;49(3):459–463.
8. Cass DL. Ovarian torsion. Semin Pediatr Surg. 2005;14(2):86–92.
9. Mazouni C, Bretelle F, Menard JP, et al. Diagnosis of adnexal torsion and predictive factors of adnexal necrosis. Gynecol Obstet Fertil. 2005;33(3):102–106.
10. Oelsner G, Cohen SB, Soriano D, et al. Minimal surgery for the twisted ischaemic adnexa can preserve ovarian function. Hum Reprod. 2003;18(12):2599–2602.
11. Ehren, IM, Mahour GH, Isaacs H Jr. Benign and malignant ovarian tumors in children and adolescents. A review of 63 cases. Am J Surg. 1984;147(3):339–344.
12. Sanfilippo JS, Lara-Torre E, Edmonds DK, Templeman C, eds. Clinical Pediatric and Adolescent Gynecology. 450 pp., illustrated, with CD-ROM. New York: Informa Healthcare; 2009.
13. Chieffi P, Chieffi S, Franco R, Sinisi AA. Recent advances in the biology of germ cell tumors: implications for the diagnosis and treatment. J Endocrinol Invest. 2012;35(11):1015–1020.
14. Lee AC, Fong C. Ovarian choriocarcinoma as the first manifestation of 46,XY pure gonadal dysgenesis. J Pediatr Hematol Oncol. 2011;33(1):e29–e31.
15. Stachowicz-Stencel T, Synakiewicz A, Izycka-Swieszewska E, Kobierska-Gulida G, Belcerska A. Malignant germ cell tumors associated with Swyer Syndrome. Pediatr Blood Cancer. 2011;56(3):482–483.
16. Barakat RR, Markman M, Randall M. Principles and Practice of Gynecologic Oncology. Philadelphia: Lippincott Williams & Wilkins; 2009.
17. Gell JS, Stannard MW, Ramnani DM, Bradshaw KD. Juvenile granulosa cell tumor in a 13-year-old girl with enchondromatosis (Ollier’s disease): a case report. J Pediatr Adolesc Gynecol. 1998;11(3):147–150.
18. Maltaris T, Boehm D, Dittrich R, Seufert R, Koelbl H. Reproduction beyond cancer: a message of hope for young women. Gynecol Oncol. 2006;103(3):1109–1121.
19. Ozcan R, Kuruoglu S, Dervisoglu S, Elicevik M, Emir H, Buyukunal C. Ovarian-sparing surgery for teratomas in children. Pediatr Surg Int. 2013;29(3):233–237.
20. Eskander RN, Bristow RE, Saenz NC, Saenz CC. A retrospective review of the effect of surgeon specialty on the management of 190 benign and malignant pediatric and adolescent adnexal masses. J Pediatr Adolesc Gynecol. 2011;24(5):282–285.
21. Dalmau J, Tuzun E, Wu HY, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61(1):25–36.
22. Behr SC, Courtier JL, Qayyum A. Imaging of Müllerian duct anomalies. Radiographics. 2012;32(6):E233–E250.
23. Hall-Craggs MA, Kirkham A, Creighton SM. Renal and urological abnormalities occurring with Müllerian anomalies. J Pediatr Urol. 2013;9(1):27–32.
In this Article
- A case of adnexal torsion
- Pediatric ovarian germ cell tumors
- A teenager with significant cyclic pelvic pain