User login
Sudden unexpected death in epilepsy: Impact, mechanisms, and prevention
The intimate interplay between heart and brain is well illustrated in epilepsy and may underlie the mechanism of one of its most devastating consequences: sudden unexpected death in epilepsy (SUDEP). This article will briefly describe the potential mechanisms of SUDEP, elaborate on the evidence for a likely cardiac pathophysiology, and review considerations in SUDEP prevention. We begin with a couple of brief case presentations and an epidemiologic overview to illustrate the concept and significance of SUDEP.
CASE PRESENTATIONS
A patient with near-SUDEP
The following is an actual message received by one of the authors:
Dr. Najm: A quick note regarding a 27-year-old male patient of yours with cerebral palsy and seizure disorder. Yesterday, while being transported from floor to floor, he had a cardiac arrest and was successfully resuscitated. Immediately after the code he developed seizures, which were treated with phenytoin and lorazepam. He is now in the neurointensive care unit. Thank you.
This case represents a scenario of near-SUDEP in which death was prevented by the fortuitous presence of immediate medical assistance at the time of cardiac arrest. Had this patient been home at the time of this incident, he almost certainly would have simply been found dead in his bed, like many SUDEP victims.
A typical case with multiple risk factors
A 32-year-old man underwent left temporal lobectomy at the Cleveland Clinic for treatment of medically refractory focal epilepsy. His seizure frequency improved after surgery, but he continued to have rare convulsions. Nevertheless, he discontinued all his anticonvulsant medications on his own. One year later, he was found dead on his bathroom floor. No obvious cause of death was identified.
This case illustrates several characteristics of the patient typically at risk for SUDEP: young, male, with intractable poorly controlled epilepsy, and not taking antiepileptic medications.
EPIDEMIOLOGY AND RISK FACTORS
Epilepsy affects 1% of the US population. Among those affected by epilepsy, SUDEP is a common cause of mortality. Estimates of SUDEP incidence range from 0.7 to 1.3 cases per 1,000 patient-years in large cohorts of patients with epilepsy1,2 and from 3.5 to 9.3 cases per 1,000 patient-years in anticonvulsant drug registries, medical device registries, and epilepsy surgery programs.3–5 SUDEP accounts for up to 17% of all deaths in patients with epilepsy6,7 and exceeds the expected rate of sudden death in the general population by nearly 24 times.6,8
Several potential risk factors for SUDEP have been investigated, but results from different studies are conflicting. Consistently identified risk factors include young age, early onset of seizures, refractoriness of epilepsy, the presence of generalized tonic-clonic seizures, male sex, and being in bed at the time of death. Weaker risk factors include being in the prone position at the time of death, having one or more subtherapeutic blood levels of anticonvulsant medication, having a structural brain lesion, and being asleep.9 The current consensus is that SUDEP is primarily a “seizure-related” occurrence, but the exact mechanisms underlying SUDEP are unknown.
PROPOSED MECHANISMS
Pulmonary pathophysiology
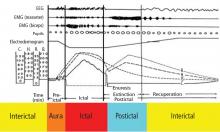
Central apnea and acute neurogenic pulmonary edema are the two major proposed pathways linking seizures to SUDEP. Evidence exists for each pathway.
Central apnea. In a prospective study of patients in an epilepsy monitoring unit, central apnea lasting at least 10 seconds was observed postictally in 40% of the recorded seizures.10 Otherwise healthy young epilepsy patients have been reported to develop central apnea immediately following complex partial seizures.11 Neurotransmitters mediating the brain’s own seizure-terminating mechanism could also be inhibiting the brainstem and causing postictal apnea.
Acute neurogenic pulmonary edema has been well described in relation to severe head injury and subarachnoid hemorrhage. Pulmonary edema is frequently found in SUDEP patients at autopsy.12 Intense generalized vasoconstriction induced by massive seizure-related sympathetic outburst can lead to increased pulmonary vascular resistance, and thereby may mediate acute pulmonary edema.
These two mechanisms—central apnea and acute neurogenic pulmonary edema—are not mutually exclusive. In the only animal model of SUDEP, one third of animals died from hypoventilation and had associated pulmonary edema at autopsy.13 Limited opportunities for realistic and practical interventions to reverse SUDEP risks related to pulmonary causes have hindered further development of these concepts.
Cardiac pathophysiology
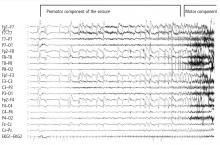
The most significant and widely discussed cardiac mechanism of SUDEP is cardiac arrhythmia precipitated by seizure discharges acting via the autonomic nervous system.14–19
Experimental evidence. Heart rate changes, including bradycardia, tachycardia, and even asystole, have been repeatedly provoked by electrical brain stimulation of the limbic system and insular cortex.19 Some studies have suggested a lateralized influence of the insulae on cardiovascular autonomic control. In one study, intraoperative stimulation of the left posterior insula elicited a cardioinhibitory response and hypotension, whereas stimulation of the right anterior insula elicited tachycardia and hypertension.20 Such results have not always been reproducible.21–23 Other studies have suggested a localization-related influence of the limbic system on cardiovascular responses. Stimulation of the amygdala has not led to the ictal tachycardia that is commonly seen in epileptic seizures, suggesting that cortical involvement is needed for the development of tachycardia.24
SUDEP PREVENTION
Epilepsy control is first line of defense
A careful consideration of the incidence of SUDEP in various patient populations suggests that controlling patients’ epilepsy might just be the best method of preventing SUDEP. While estimated SUDEP incidence ranges from 0.7 to 1.3 cases per 1,000 patient-years in population-based studies of patients with epilepsy,1,2 this rate escalates by nearly tenfold (3.5 to 9.3 cases per 1,000 patient-years) in cohorts with severe epilepsy, such as those derived from anticonvulsant drug registries, medical device registries, and referral centers.3–5 Therefore, medical control of seizures might reduce the incidence of SUDEP.
Epilepsy surgery cuts SUDEP risk for many patients
Studies involving epilepsy surgery programs also suggest that successful epilepsy surgery reduces the impending risks of SUDEP. In cohorts in which the estimated risk of SUDEP is almost 1% per year without surgery, SUDEP incidence was significantly lower following epilepsy surgery. In a study of 305 patients who underwent temporal lobe epilepsy surgery in the United Kingdom, the incidence of SUDEP following surgery was 2.2 cases per 1,000 person-years, and only one-third of SUDEP cases were among seizure-free patients.31 A similar incidence of 2.4 cases per 1,000 person-years was seen following epilepsy surgery in 596 Swedish patients; none of the 6 SUDEP patients in that study was seizure free.32 In a US study, no SUDEP cases occurred among 256 seizure-free patients with a follow-up of about 5 years after epilepsy surgery.33
In our own experience at the Cleveland Clinic, we have reported on outcomes among 70 patients who underwent frontal lobectomy34 and among 371 patients who underwent temporal lobectomy.35 In the frontal lobectomy study,34 2 of the 39 patients who had persistent seizures following surgery died of SUDEP during follow-up, whereas none of the 31 patients who remained seizure free were dead up to 10 years after surgery. In the temporal lobectomy report,35 2 of the 141 patients with ongoing postoperative seizures died of SUDEP, as compared with none of the 230 patients who were seizure free after a mean follow-up of 5.5 years.
Additional means of prophylaxis needed
Unfortunately, as many as 30% to 40% of patients with epilepsy continue to suffer intractable epilepsy despite all the available treatment modalities, including epilepsy surgery. For these patients, controlling seizures to reduce the risk of SUDEP is neither a possible nor a realistic means of avoiding this devastating condition, and alternative methods of prophylaxis must be sought.
CONCLUSIONS AND FUTURE RESEARCH
Patients with refractory epilepsy currently face a lifelong risk of sudden death as high as 1% per year.3 Elucidating the mechanisms of SUDEP might lead to preventive measures, which could have significant implications in reducing mortality in this patient population. Abundant evidence exists that autonomic dysfunction and cardiac arrhythmias are associated with seizures. The missing links in establishing a cardiac mechanism for SUDEP now include the following: (1) evidence of cardiac arrhythmias generally observed in seizures as a risk factor for SUDEP, (2) determination of clear electrophysiologic characteristics—from EEG and ECG standpoints—of patients at risk for SUDEP, and (3) clarification of the role of cardiac mechanisms in SUDEP and the role that cerebral influences on autonomic function might play. Early identification of patients at risk of SUDEP would offer a unique opportunity for early intervention to prevent this devastating condition.
- Nilsson L, Farahmand BY, Persson PG, Thiblin I, Tomson T. Risk factors for sudden unexpected death in epilepsy: a case-control study. Lancet 1999; 353:888–893.
- Tennis P, Cole TB, Annegers JF, Leestma JE, McNutt M, Rajput A. Cohort study of incidence of sudden unexplained death in persons with seizure disorder treated with antiepileptic drugs in Saskatchewan, Canada. Epilepsia 1995; 36:29–36.
- Dasheiff RM. Sudden unexpected death in epilepsy: a series from an epilepsy surgery program and speculation on the relationship to sudden cardiac death. J Clin Neurophysiol 1991; 8:216–222.
- Leestma JE, Annegers JF, Brodie MJ, et al. Sudden unexplained death in epilepsy: observations from a large clinical development program. Epilepsia 1997; 38:47–55.
- Sperling MR, Feldman H, Kinman J, Liporace JD, O’Connor MJ. Seizure control and mortality in epilepsy. Ann Neurol 1999; 46:45–50.
- Ficker DM. Sudden unexplained death and injury in epilepsy. Epilepsia 2000; 41(Suppl 2):S7–S12.
- Pedley TA, Hauser WA. Sudden death in epilepsy: a wake-up call for management. Lancet 2002; 359:1790–1791.
- Ficker DM, So EL, Shen WK, et al. Population-based study of the incidence of sudden unexplained death in epilepsy. Neurology 1998; 51:1270–1274.
- Monté CP, Arends JB, Tan IY, Aldenkamp AP, Limburg M, de Krom MC. Sudden unexpected death in epilepsy patients: risk factors. A systematic review. Seizure 2007; 16:1–7.
- Nashef L, Walker F, Allen P, Sander JW, Shorvon SD, Fish DR. Apnoea and bradycardia during epileptic seizures: relation to sudden death in epilepsy. J Neurol Neurosurg Psychiatry 1996; 60:297–300.
- So EL, Sam MC, Lagerlund TL. Postictal central apnea as a cause of SUDEP: evidence from near-SUDEP incident. Epilepsia 2000; 41:1494–1497.
- Terrence CF, Rao GR, Perper JA. Neurogenic pulmonary edema in unexpected, unexplained death of epileptic patients. Ann Neurol 1981; 9:458–464.
- Johnston SC, Horn JK, Valente J, Simon RP. The role of hypoventilation in a sheep model of epileptic sudden death. Ann Neurol 1995; 37:531–537.
- Blumhardt LD, Smith PE, Owen L. Electrocardiographic accompaniments of temporal lobe epileptic seizures. Lancet 1986; 1:1051–1056.
- Nei M, Ho RT, Abou-Khalil BW, et al. EEG and ECG in sudden unexplained death in epilepsy. Epilepsia 2004; 45:338–345.
- Nei M, Ho RT, Sperling MR. EKG abnormalities during partial seizures in refractory epilepsy. Epilepsia 2000; 41:542–548.
- Opherk C, Coromilas J, Hirsch LJ. Heart rate and EKG changes in 102 seizures: analysis of influencing factors. Epilepsy Res 2002; 52:117–127.
- Tigaran S, Mølgaard H, McClelland R, Dam M, Jaffe AS. Evidence of cardiac ischemia during seizures in drug refractory epilepsy patients. Neurology 2003; 60:492–495.
- Leung H, Kwan P, Elger CE. Finding the missing link between ictal bradyarrhythmia, ictal asystole, and sudden unexpected death in epilepsy. Epilepsy Behav 2006; 9:19–30.
- Yasui Y, Breder CD, Saper CB, Cechetto DF. Autonomic responses and efferent pathways from the insular cortex in the rat. J Comp Neurol 1991; 303:355–374.
- Jokeit H, Noerpel I, Herbord E, Ebner A. Heart rate does not decrease after right hemispheric amobarbital injection. Neurology 2000; 54:2347–2348.
- Zamrini EY, Meador KJ, Loring DW, et al. Unilateral cerebral inactivation produces differential left/right heart rate responses. Neurology 1990; 40:1408–1411.
- Yoon BW, Morillo CA, Cechetto DF, Hachinski V. Cerebral hemispheric lateralization in cardiac autonomic control. Arch Neurol 1997; 54:741–744.
- Keilson MJ, Hauser WA, Magrill JP. Electrocardiographic changes during electrographic seizures. Arch Neurol 1989; 46:1169–1170.
- Keilson MJ, Hauser WA, Magrill JP, Goldman M. ECG abnormalities in patients with epilepsy. Neurology 1987; 37:1624–1626.
- Galimberti CA, Marchioni E, Barzizza F, Manni R, Sartori I, Tartara A. Partial epileptic seizures of different origin variably affect cardiac rhythm. Epilepsia 1996; 37:742–747.
- Liedholm LJ, Gudjonsson O. Cardiac arrest due to partial epileptic seizures. Neurology 1992; 42:824–829.
- Leung H, Schindler K, Kwan P, Elger C. Asystole induced by electrical stimulation of the left cingulate gyrus. Epileptic Disord 2007; 9:77–81.
- Blum AS, Ives JR, Goldberger AL, et al. Oxygen desaturations triggered by partial seizures: implications for cardiopulmonary instability in epilepsy. Epilepsia 2000; 41:536–541.
- Langan Y, Nashef L, Sander JW. Case-control study of SUDEP. Neurology 2005; 64:1131–1133.
- Hennessy MJ, Langan Y, Elwes RD, Binnie CD, Polkey CE, Nashef L. A study of mortality after temporal lobe epilepsy surgery. Neurology 1999; 53:1276–1283.
- Nilsson L, Ahlbom A, Farahmand BY, Tomson T. Mortality in a population-based cohort of epilepsy surgery patients. Epilepsia 2003; 44:575–581.
- Sperling MR, Harris A, Nei M, Liporace JD, O’Connor MJ. Mortality after epilepsy surgery. Epilepsia 2005; 46(Suppl 11):49–53.
- Jeha LE, Najm I, Bingaman W, Dinner D, Widdess-Walsh P, Lüders H. Surgical outcome and prognostic factors of frontal lobe epilepsy surgery. Brain 2007; 130:574–584.
- Jeha LE, Najm IM, Bingaman WE, et al. Predictors of outcome after temporal lobectomy for the treatment of intractable epilepsy. Neurology 2006; 66:1938–1940.
The intimate interplay between heart and brain is well illustrated in epilepsy and may underlie the mechanism of one of its most devastating consequences: sudden unexpected death in epilepsy (SUDEP). This article will briefly describe the potential mechanisms of SUDEP, elaborate on the evidence for a likely cardiac pathophysiology, and review considerations in SUDEP prevention. We begin with a couple of brief case presentations and an epidemiologic overview to illustrate the concept and significance of SUDEP.
CASE PRESENTATIONS
A patient with near-SUDEP
The following is an actual message received by one of the authors:
Dr. Najm: A quick note regarding a 27-year-old male patient of yours with cerebral palsy and seizure disorder. Yesterday, while being transported from floor to floor, he had a cardiac arrest and was successfully resuscitated. Immediately after the code he developed seizures, which were treated with phenytoin and lorazepam. He is now in the neurointensive care unit. Thank you.
This case represents a scenario of near-SUDEP in which death was prevented by the fortuitous presence of immediate medical assistance at the time of cardiac arrest. Had this patient been home at the time of this incident, he almost certainly would have simply been found dead in his bed, like many SUDEP victims.
A typical case with multiple risk factors
A 32-year-old man underwent left temporal lobectomy at the Cleveland Clinic for treatment of medically refractory focal epilepsy. His seizure frequency improved after surgery, but he continued to have rare convulsions. Nevertheless, he discontinued all his anticonvulsant medications on his own. One year later, he was found dead on his bathroom floor. No obvious cause of death was identified.
This case illustrates several characteristics of the patient typically at risk for SUDEP: young, male, with intractable poorly controlled epilepsy, and not taking antiepileptic medications.
EPIDEMIOLOGY AND RISK FACTORS
Epilepsy affects 1% of the US population. Among those affected by epilepsy, SUDEP is a common cause of mortality. Estimates of SUDEP incidence range from 0.7 to 1.3 cases per 1,000 patient-years in large cohorts of patients with epilepsy1,2 and from 3.5 to 9.3 cases per 1,000 patient-years in anticonvulsant drug registries, medical device registries, and epilepsy surgery programs.3–5 SUDEP accounts for up to 17% of all deaths in patients with epilepsy6,7 and exceeds the expected rate of sudden death in the general population by nearly 24 times.6,8
Several potential risk factors for SUDEP have been investigated, but results from different studies are conflicting. Consistently identified risk factors include young age, early onset of seizures, refractoriness of epilepsy, the presence of generalized tonic-clonic seizures, male sex, and being in bed at the time of death. Weaker risk factors include being in the prone position at the time of death, having one or more subtherapeutic blood levels of anticonvulsant medication, having a structural brain lesion, and being asleep.9 The current consensus is that SUDEP is primarily a “seizure-related” occurrence, but the exact mechanisms underlying SUDEP are unknown.
PROPOSED MECHANISMS
Pulmonary pathophysiology
Central apnea and acute neurogenic pulmonary edema are the two major proposed pathways linking seizures to SUDEP. Evidence exists for each pathway.
Central apnea. In a prospective study of patients in an epilepsy monitoring unit, central apnea lasting at least 10 seconds was observed postictally in 40% of the recorded seizures.10 Otherwise healthy young epilepsy patients have been reported to develop central apnea immediately following complex partial seizures.11 Neurotransmitters mediating the brain’s own seizure-terminating mechanism could also be inhibiting the brainstem and causing postictal apnea.
Acute neurogenic pulmonary edema has been well described in relation to severe head injury and subarachnoid hemorrhage. Pulmonary edema is frequently found in SUDEP patients at autopsy.12 Intense generalized vasoconstriction induced by massive seizure-related sympathetic outburst can lead to increased pulmonary vascular resistance, and thereby may mediate acute pulmonary edema.
These two mechanisms—central apnea and acute neurogenic pulmonary edema—are not mutually exclusive. In the only animal model of SUDEP, one third of animals died from hypoventilation and had associated pulmonary edema at autopsy.13 Limited opportunities for realistic and practical interventions to reverse SUDEP risks related to pulmonary causes have hindered further development of these concepts.
Cardiac pathophysiology
The most significant and widely discussed cardiac mechanism of SUDEP is cardiac arrhythmia precipitated by seizure discharges acting via the autonomic nervous system.14–19
Experimental evidence. Heart rate changes, including bradycardia, tachycardia, and even asystole, have been repeatedly provoked by electrical brain stimulation of the limbic system and insular cortex.19 Some studies have suggested a lateralized influence of the insulae on cardiovascular autonomic control. In one study, intraoperative stimulation of the left posterior insula elicited a cardioinhibitory response and hypotension, whereas stimulation of the right anterior insula elicited tachycardia and hypertension.20 Such results have not always been reproducible.21–23 Other studies have suggested a localization-related influence of the limbic system on cardiovascular responses. Stimulation of the amygdala has not led to the ictal tachycardia that is commonly seen in epileptic seizures, suggesting that cortical involvement is needed for the development of tachycardia.24
SUDEP PREVENTION
Epilepsy control is first line of defense
A careful consideration of the incidence of SUDEP in various patient populations suggests that controlling patients’ epilepsy might just be the best method of preventing SUDEP. While estimated SUDEP incidence ranges from 0.7 to 1.3 cases per 1,000 patient-years in population-based studies of patients with epilepsy,1,2 this rate escalates by nearly tenfold (3.5 to 9.3 cases per 1,000 patient-years) in cohorts with severe epilepsy, such as those derived from anticonvulsant drug registries, medical device registries, and referral centers.3–5 Therefore, medical control of seizures might reduce the incidence of SUDEP.
Epilepsy surgery cuts SUDEP risk for many patients
Studies involving epilepsy surgery programs also suggest that successful epilepsy surgery reduces the impending risks of SUDEP. In cohorts in which the estimated risk of SUDEP is almost 1% per year without surgery, SUDEP incidence was significantly lower following epilepsy surgery. In a study of 305 patients who underwent temporal lobe epilepsy surgery in the United Kingdom, the incidence of SUDEP following surgery was 2.2 cases per 1,000 person-years, and only one-third of SUDEP cases were among seizure-free patients.31 A similar incidence of 2.4 cases per 1,000 person-years was seen following epilepsy surgery in 596 Swedish patients; none of the 6 SUDEP patients in that study was seizure free.32 In a US study, no SUDEP cases occurred among 256 seizure-free patients with a follow-up of about 5 years after epilepsy surgery.33
In our own experience at the Cleveland Clinic, we have reported on outcomes among 70 patients who underwent frontal lobectomy34 and among 371 patients who underwent temporal lobectomy.35 In the frontal lobectomy study,34 2 of the 39 patients who had persistent seizures following surgery died of SUDEP during follow-up, whereas none of the 31 patients who remained seizure free were dead up to 10 years after surgery. In the temporal lobectomy report,35 2 of the 141 patients with ongoing postoperative seizures died of SUDEP, as compared with none of the 230 patients who were seizure free after a mean follow-up of 5.5 years.
Additional means of prophylaxis needed
Unfortunately, as many as 30% to 40% of patients with epilepsy continue to suffer intractable epilepsy despite all the available treatment modalities, including epilepsy surgery. For these patients, controlling seizures to reduce the risk of SUDEP is neither a possible nor a realistic means of avoiding this devastating condition, and alternative methods of prophylaxis must be sought.
CONCLUSIONS AND FUTURE RESEARCH
Patients with refractory epilepsy currently face a lifelong risk of sudden death as high as 1% per year.3 Elucidating the mechanisms of SUDEP might lead to preventive measures, which could have significant implications in reducing mortality in this patient population. Abundant evidence exists that autonomic dysfunction and cardiac arrhythmias are associated with seizures. The missing links in establishing a cardiac mechanism for SUDEP now include the following: (1) evidence of cardiac arrhythmias generally observed in seizures as a risk factor for SUDEP, (2) determination of clear electrophysiologic characteristics—from EEG and ECG standpoints—of patients at risk for SUDEP, and (3) clarification of the role of cardiac mechanisms in SUDEP and the role that cerebral influences on autonomic function might play. Early identification of patients at risk of SUDEP would offer a unique opportunity for early intervention to prevent this devastating condition.
The intimate interplay between heart and brain is well illustrated in epilepsy and may underlie the mechanism of one of its most devastating consequences: sudden unexpected death in epilepsy (SUDEP). This article will briefly describe the potential mechanisms of SUDEP, elaborate on the evidence for a likely cardiac pathophysiology, and review considerations in SUDEP prevention. We begin with a couple of brief case presentations and an epidemiologic overview to illustrate the concept and significance of SUDEP.
CASE PRESENTATIONS
A patient with near-SUDEP
The following is an actual message received by one of the authors:
Dr. Najm: A quick note regarding a 27-year-old male patient of yours with cerebral palsy and seizure disorder. Yesterday, while being transported from floor to floor, he had a cardiac arrest and was successfully resuscitated. Immediately after the code he developed seizures, which were treated with phenytoin and lorazepam. He is now in the neurointensive care unit. Thank you.
This case represents a scenario of near-SUDEP in which death was prevented by the fortuitous presence of immediate medical assistance at the time of cardiac arrest. Had this patient been home at the time of this incident, he almost certainly would have simply been found dead in his bed, like many SUDEP victims.
A typical case with multiple risk factors
A 32-year-old man underwent left temporal lobectomy at the Cleveland Clinic for treatment of medically refractory focal epilepsy. His seizure frequency improved after surgery, but he continued to have rare convulsions. Nevertheless, he discontinued all his anticonvulsant medications on his own. One year later, he was found dead on his bathroom floor. No obvious cause of death was identified.
This case illustrates several characteristics of the patient typically at risk for SUDEP: young, male, with intractable poorly controlled epilepsy, and not taking antiepileptic medications.
EPIDEMIOLOGY AND RISK FACTORS
Epilepsy affects 1% of the US population. Among those affected by epilepsy, SUDEP is a common cause of mortality. Estimates of SUDEP incidence range from 0.7 to 1.3 cases per 1,000 patient-years in large cohorts of patients with epilepsy1,2 and from 3.5 to 9.3 cases per 1,000 patient-years in anticonvulsant drug registries, medical device registries, and epilepsy surgery programs.3–5 SUDEP accounts for up to 17% of all deaths in patients with epilepsy6,7 and exceeds the expected rate of sudden death in the general population by nearly 24 times.6,8
Several potential risk factors for SUDEP have been investigated, but results from different studies are conflicting. Consistently identified risk factors include young age, early onset of seizures, refractoriness of epilepsy, the presence of generalized tonic-clonic seizures, male sex, and being in bed at the time of death. Weaker risk factors include being in the prone position at the time of death, having one or more subtherapeutic blood levels of anticonvulsant medication, having a structural brain lesion, and being asleep.9 The current consensus is that SUDEP is primarily a “seizure-related” occurrence, but the exact mechanisms underlying SUDEP are unknown.
PROPOSED MECHANISMS
Pulmonary pathophysiology
Central apnea and acute neurogenic pulmonary edema are the two major proposed pathways linking seizures to SUDEP. Evidence exists for each pathway.
Central apnea. In a prospective study of patients in an epilepsy monitoring unit, central apnea lasting at least 10 seconds was observed postictally in 40% of the recorded seizures.10 Otherwise healthy young epilepsy patients have been reported to develop central apnea immediately following complex partial seizures.11 Neurotransmitters mediating the brain’s own seizure-terminating mechanism could also be inhibiting the brainstem and causing postictal apnea.
Acute neurogenic pulmonary edema has been well described in relation to severe head injury and subarachnoid hemorrhage. Pulmonary edema is frequently found in SUDEP patients at autopsy.12 Intense generalized vasoconstriction induced by massive seizure-related sympathetic outburst can lead to increased pulmonary vascular resistance, and thereby may mediate acute pulmonary edema.
These two mechanisms—central apnea and acute neurogenic pulmonary edema—are not mutually exclusive. In the only animal model of SUDEP, one third of animals died from hypoventilation and had associated pulmonary edema at autopsy.13 Limited opportunities for realistic and practical interventions to reverse SUDEP risks related to pulmonary causes have hindered further development of these concepts.
Cardiac pathophysiology
The most significant and widely discussed cardiac mechanism of SUDEP is cardiac arrhythmia precipitated by seizure discharges acting via the autonomic nervous system.14–19
Experimental evidence. Heart rate changes, including bradycardia, tachycardia, and even asystole, have been repeatedly provoked by electrical brain stimulation of the limbic system and insular cortex.19 Some studies have suggested a lateralized influence of the insulae on cardiovascular autonomic control. In one study, intraoperative stimulation of the left posterior insula elicited a cardioinhibitory response and hypotension, whereas stimulation of the right anterior insula elicited tachycardia and hypertension.20 Such results have not always been reproducible.21–23 Other studies have suggested a localization-related influence of the limbic system on cardiovascular responses. Stimulation of the amygdala has not led to the ictal tachycardia that is commonly seen in epileptic seizures, suggesting that cortical involvement is needed for the development of tachycardia.24
SUDEP PREVENTION
Epilepsy control is first line of defense
A careful consideration of the incidence of SUDEP in various patient populations suggests that controlling patients’ epilepsy might just be the best method of preventing SUDEP. While estimated SUDEP incidence ranges from 0.7 to 1.3 cases per 1,000 patient-years in population-based studies of patients with epilepsy,1,2 this rate escalates by nearly tenfold (3.5 to 9.3 cases per 1,000 patient-years) in cohorts with severe epilepsy, such as those derived from anticonvulsant drug registries, medical device registries, and referral centers.3–5 Therefore, medical control of seizures might reduce the incidence of SUDEP.
Epilepsy surgery cuts SUDEP risk for many patients
Studies involving epilepsy surgery programs also suggest that successful epilepsy surgery reduces the impending risks of SUDEP. In cohorts in which the estimated risk of SUDEP is almost 1% per year without surgery, SUDEP incidence was significantly lower following epilepsy surgery. In a study of 305 patients who underwent temporal lobe epilepsy surgery in the United Kingdom, the incidence of SUDEP following surgery was 2.2 cases per 1,000 person-years, and only one-third of SUDEP cases were among seizure-free patients.31 A similar incidence of 2.4 cases per 1,000 person-years was seen following epilepsy surgery in 596 Swedish patients; none of the 6 SUDEP patients in that study was seizure free.32 In a US study, no SUDEP cases occurred among 256 seizure-free patients with a follow-up of about 5 years after epilepsy surgery.33
In our own experience at the Cleveland Clinic, we have reported on outcomes among 70 patients who underwent frontal lobectomy34 and among 371 patients who underwent temporal lobectomy.35 In the frontal lobectomy study,34 2 of the 39 patients who had persistent seizures following surgery died of SUDEP during follow-up, whereas none of the 31 patients who remained seizure free were dead up to 10 years after surgery. In the temporal lobectomy report,35 2 of the 141 patients with ongoing postoperative seizures died of SUDEP, as compared with none of the 230 patients who were seizure free after a mean follow-up of 5.5 years.
Additional means of prophylaxis needed
Unfortunately, as many as 30% to 40% of patients with epilepsy continue to suffer intractable epilepsy despite all the available treatment modalities, including epilepsy surgery. For these patients, controlling seizures to reduce the risk of SUDEP is neither a possible nor a realistic means of avoiding this devastating condition, and alternative methods of prophylaxis must be sought.
CONCLUSIONS AND FUTURE RESEARCH
Patients with refractory epilepsy currently face a lifelong risk of sudden death as high as 1% per year.3 Elucidating the mechanisms of SUDEP might lead to preventive measures, which could have significant implications in reducing mortality in this patient population. Abundant evidence exists that autonomic dysfunction and cardiac arrhythmias are associated with seizures. The missing links in establishing a cardiac mechanism for SUDEP now include the following: (1) evidence of cardiac arrhythmias generally observed in seizures as a risk factor for SUDEP, (2) determination of clear electrophysiologic characteristics—from EEG and ECG standpoints—of patients at risk for SUDEP, and (3) clarification of the role of cardiac mechanisms in SUDEP and the role that cerebral influences on autonomic function might play. Early identification of patients at risk of SUDEP would offer a unique opportunity for early intervention to prevent this devastating condition.
- Nilsson L, Farahmand BY, Persson PG, Thiblin I, Tomson T. Risk factors for sudden unexpected death in epilepsy: a case-control study. Lancet 1999; 353:888–893.
- Tennis P, Cole TB, Annegers JF, Leestma JE, McNutt M, Rajput A. Cohort study of incidence of sudden unexplained death in persons with seizure disorder treated with antiepileptic drugs in Saskatchewan, Canada. Epilepsia 1995; 36:29–36.
- Dasheiff RM. Sudden unexpected death in epilepsy: a series from an epilepsy surgery program and speculation on the relationship to sudden cardiac death. J Clin Neurophysiol 1991; 8:216–222.
- Leestma JE, Annegers JF, Brodie MJ, et al. Sudden unexplained death in epilepsy: observations from a large clinical development program. Epilepsia 1997; 38:47–55.
- Sperling MR, Feldman H, Kinman J, Liporace JD, O’Connor MJ. Seizure control and mortality in epilepsy. Ann Neurol 1999; 46:45–50.
- Ficker DM. Sudden unexplained death and injury in epilepsy. Epilepsia 2000; 41(Suppl 2):S7–S12.
- Pedley TA, Hauser WA. Sudden death in epilepsy: a wake-up call for management. Lancet 2002; 359:1790–1791.
- Ficker DM, So EL, Shen WK, et al. Population-based study of the incidence of sudden unexplained death in epilepsy. Neurology 1998; 51:1270–1274.
- Monté CP, Arends JB, Tan IY, Aldenkamp AP, Limburg M, de Krom MC. Sudden unexpected death in epilepsy patients: risk factors. A systematic review. Seizure 2007; 16:1–7.
- Nashef L, Walker F, Allen P, Sander JW, Shorvon SD, Fish DR. Apnoea and bradycardia during epileptic seizures: relation to sudden death in epilepsy. J Neurol Neurosurg Psychiatry 1996; 60:297–300.
- So EL, Sam MC, Lagerlund TL. Postictal central apnea as a cause of SUDEP: evidence from near-SUDEP incident. Epilepsia 2000; 41:1494–1497.
- Terrence CF, Rao GR, Perper JA. Neurogenic pulmonary edema in unexpected, unexplained death of epileptic patients. Ann Neurol 1981; 9:458–464.
- Johnston SC, Horn JK, Valente J, Simon RP. The role of hypoventilation in a sheep model of epileptic sudden death. Ann Neurol 1995; 37:531–537.
- Blumhardt LD, Smith PE, Owen L. Electrocardiographic accompaniments of temporal lobe epileptic seizures. Lancet 1986; 1:1051–1056.
- Nei M, Ho RT, Abou-Khalil BW, et al. EEG and ECG in sudden unexplained death in epilepsy. Epilepsia 2004; 45:338–345.
- Nei M, Ho RT, Sperling MR. EKG abnormalities during partial seizures in refractory epilepsy. Epilepsia 2000; 41:542–548.
- Opherk C, Coromilas J, Hirsch LJ. Heart rate and EKG changes in 102 seizures: analysis of influencing factors. Epilepsy Res 2002; 52:117–127.
- Tigaran S, Mølgaard H, McClelland R, Dam M, Jaffe AS. Evidence of cardiac ischemia during seizures in drug refractory epilepsy patients. Neurology 2003; 60:492–495.
- Leung H, Kwan P, Elger CE. Finding the missing link between ictal bradyarrhythmia, ictal asystole, and sudden unexpected death in epilepsy. Epilepsy Behav 2006; 9:19–30.
- Yasui Y, Breder CD, Saper CB, Cechetto DF. Autonomic responses and efferent pathways from the insular cortex in the rat. J Comp Neurol 1991; 303:355–374.
- Jokeit H, Noerpel I, Herbord E, Ebner A. Heart rate does not decrease after right hemispheric amobarbital injection. Neurology 2000; 54:2347–2348.
- Zamrini EY, Meador KJ, Loring DW, et al. Unilateral cerebral inactivation produces differential left/right heart rate responses. Neurology 1990; 40:1408–1411.
- Yoon BW, Morillo CA, Cechetto DF, Hachinski V. Cerebral hemispheric lateralization in cardiac autonomic control. Arch Neurol 1997; 54:741–744.
- Keilson MJ, Hauser WA, Magrill JP. Electrocardiographic changes during electrographic seizures. Arch Neurol 1989; 46:1169–1170.
- Keilson MJ, Hauser WA, Magrill JP, Goldman M. ECG abnormalities in patients with epilepsy. Neurology 1987; 37:1624–1626.
- Galimberti CA, Marchioni E, Barzizza F, Manni R, Sartori I, Tartara A. Partial epileptic seizures of different origin variably affect cardiac rhythm. Epilepsia 1996; 37:742–747.
- Liedholm LJ, Gudjonsson O. Cardiac arrest due to partial epileptic seizures. Neurology 1992; 42:824–829.
- Leung H, Schindler K, Kwan P, Elger C. Asystole induced by electrical stimulation of the left cingulate gyrus. Epileptic Disord 2007; 9:77–81.
- Blum AS, Ives JR, Goldberger AL, et al. Oxygen desaturations triggered by partial seizures: implications for cardiopulmonary instability in epilepsy. Epilepsia 2000; 41:536–541.
- Langan Y, Nashef L, Sander JW. Case-control study of SUDEP. Neurology 2005; 64:1131–1133.
- Hennessy MJ, Langan Y, Elwes RD, Binnie CD, Polkey CE, Nashef L. A study of mortality after temporal lobe epilepsy surgery. Neurology 1999; 53:1276–1283.
- Nilsson L, Ahlbom A, Farahmand BY, Tomson T. Mortality in a population-based cohort of epilepsy surgery patients. Epilepsia 2003; 44:575–581.
- Sperling MR, Harris A, Nei M, Liporace JD, O’Connor MJ. Mortality after epilepsy surgery. Epilepsia 2005; 46(Suppl 11):49–53.
- Jeha LE, Najm I, Bingaman W, Dinner D, Widdess-Walsh P, Lüders H. Surgical outcome and prognostic factors of frontal lobe epilepsy surgery. Brain 2007; 130:574–584.
- Jeha LE, Najm IM, Bingaman WE, et al. Predictors of outcome after temporal lobectomy for the treatment of intractable epilepsy. Neurology 2006; 66:1938–1940.
- Nilsson L, Farahmand BY, Persson PG, Thiblin I, Tomson T. Risk factors for sudden unexpected death in epilepsy: a case-control study. Lancet 1999; 353:888–893.
- Tennis P, Cole TB, Annegers JF, Leestma JE, McNutt M, Rajput A. Cohort study of incidence of sudden unexplained death in persons with seizure disorder treated with antiepileptic drugs in Saskatchewan, Canada. Epilepsia 1995; 36:29–36.
- Dasheiff RM. Sudden unexpected death in epilepsy: a series from an epilepsy surgery program and speculation on the relationship to sudden cardiac death. J Clin Neurophysiol 1991; 8:216–222.
- Leestma JE, Annegers JF, Brodie MJ, et al. Sudden unexplained death in epilepsy: observations from a large clinical development program. Epilepsia 1997; 38:47–55.
- Sperling MR, Feldman H, Kinman J, Liporace JD, O’Connor MJ. Seizure control and mortality in epilepsy. Ann Neurol 1999; 46:45–50.
- Ficker DM. Sudden unexplained death and injury in epilepsy. Epilepsia 2000; 41(Suppl 2):S7–S12.
- Pedley TA, Hauser WA. Sudden death in epilepsy: a wake-up call for management. Lancet 2002; 359:1790–1791.
- Ficker DM, So EL, Shen WK, et al. Population-based study of the incidence of sudden unexplained death in epilepsy. Neurology 1998; 51:1270–1274.
- Monté CP, Arends JB, Tan IY, Aldenkamp AP, Limburg M, de Krom MC. Sudden unexpected death in epilepsy patients: risk factors. A systematic review. Seizure 2007; 16:1–7.
- Nashef L, Walker F, Allen P, Sander JW, Shorvon SD, Fish DR. Apnoea and bradycardia during epileptic seizures: relation to sudden death in epilepsy. J Neurol Neurosurg Psychiatry 1996; 60:297–300.
- So EL, Sam MC, Lagerlund TL. Postictal central apnea as a cause of SUDEP: evidence from near-SUDEP incident. Epilepsia 2000; 41:1494–1497.
- Terrence CF, Rao GR, Perper JA. Neurogenic pulmonary edema in unexpected, unexplained death of epileptic patients. Ann Neurol 1981; 9:458–464.
- Johnston SC, Horn JK, Valente J, Simon RP. The role of hypoventilation in a sheep model of epileptic sudden death. Ann Neurol 1995; 37:531–537.
- Blumhardt LD, Smith PE, Owen L. Electrocardiographic accompaniments of temporal lobe epileptic seizures. Lancet 1986; 1:1051–1056.
- Nei M, Ho RT, Abou-Khalil BW, et al. EEG and ECG in sudden unexplained death in epilepsy. Epilepsia 2004; 45:338–345.
- Nei M, Ho RT, Sperling MR. EKG abnormalities during partial seizures in refractory epilepsy. Epilepsia 2000; 41:542–548.
- Opherk C, Coromilas J, Hirsch LJ. Heart rate and EKG changes in 102 seizures: analysis of influencing factors. Epilepsy Res 2002; 52:117–127.
- Tigaran S, Mølgaard H, McClelland R, Dam M, Jaffe AS. Evidence of cardiac ischemia during seizures in drug refractory epilepsy patients. Neurology 2003; 60:492–495.
- Leung H, Kwan P, Elger CE. Finding the missing link between ictal bradyarrhythmia, ictal asystole, and sudden unexpected death in epilepsy. Epilepsy Behav 2006; 9:19–30.
- Yasui Y, Breder CD, Saper CB, Cechetto DF. Autonomic responses and efferent pathways from the insular cortex in the rat. J Comp Neurol 1991; 303:355–374.
- Jokeit H, Noerpel I, Herbord E, Ebner A. Heart rate does not decrease after right hemispheric amobarbital injection. Neurology 2000; 54:2347–2348.
- Zamrini EY, Meador KJ, Loring DW, et al. Unilateral cerebral inactivation produces differential left/right heart rate responses. Neurology 1990; 40:1408–1411.
- Yoon BW, Morillo CA, Cechetto DF, Hachinski V. Cerebral hemispheric lateralization in cardiac autonomic control. Arch Neurol 1997; 54:741–744.
- Keilson MJ, Hauser WA, Magrill JP. Electrocardiographic changes during electrographic seizures. Arch Neurol 1989; 46:1169–1170.
- Keilson MJ, Hauser WA, Magrill JP, Goldman M. ECG abnormalities in patients with epilepsy. Neurology 1987; 37:1624–1626.
- Galimberti CA, Marchioni E, Barzizza F, Manni R, Sartori I, Tartara A. Partial epileptic seizures of different origin variably affect cardiac rhythm. Epilepsia 1996; 37:742–747.
- Liedholm LJ, Gudjonsson O. Cardiac arrest due to partial epileptic seizures. Neurology 1992; 42:824–829.
- Leung H, Schindler K, Kwan P, Elger C. Asystole induced by electrical stimulation of the left cingulate gyrus. Epileptic Disord 2007; 9:77–81.
- Blum AS, Ives JR, Goldberger AL, et al. Oxygen desaturations triggered by partial seizures: implications for cardiopulmonary instability in epilepsy. Epilepsia 2000; 41:536–541.
- Langan Y, Nashef L, Sander JW. Case-control study of SUDEP. Neurology 2005; 64:1131–1133.
- Hennessy MJ, Langan Y, Elwes RD, Binnie CD, Polkey CE, Nashef L. A study of mortality after temporal lobe epilepsy surgery. Neurology 1999; 53:1276–1283.
- Nilsson L, Ahlbom A, Farahmand BY, Tomson T. Mortality in a population-based cohort of epilepsy surgery patients. Epilepsia 2003; 44:575–581.
- Sperling MR, Harris A, Nei M, Liporace JD, O’Connor MJ. Mortality after epilepsy surgery. Epilepsia 2005; 46(Suppl 11):49–53.
- Jeha LE, Najm I, Bingaman W, Dinner D, Widdess-Walsh P, Lüders H. Surgical outcome and prognostic factors of frontal lobe epilepsy surgery. Brain 2007; 130:574–584.
- Jeha LE, Najm IM, Bingaman WE, et al. Predictors of outcome after temporal lobectomy for the treatment of intractable epilepsy. Neurology 2006; 66:1938–1940.