User login
Plagues that will haunt us long after the COVID-19 pandemic is gone
As we struggle to gradually emerge from the horrid coronavirus disease 2019 (COVID-19) pandemic that has disrupted our lives and killed hundreds of thousands of people in the United States, we harbor the hope that life will return to “normal.” But while it will certainly be a great relief to put this deadly virus behind us, many other epidemics will continue to plague our society and taint our culture.
Scientific ingenuity has led to the development of several vaccines in record time (aka “warp speed”) that will help defeat the deadly scourge of COVID-19. The pandemic is likely to peter out 2 years after its onset. We will all be grateful for such a rapid resolution of the worst health crisis the world has faced in a century, which will enable medical, economic, and social recovery. But as we eventually resume our lives and rejoice in resuming the pursuit of happiness, we will quickly realize that all is not well in our society just because the viral pandemic is gone.
Perhaps the ordeal of the COVID-19 pandemic, and the agony that was universally shared, will open our collective eyes to a jarring reality: many other epidemics will continue to permeate society and cause endless grief and suffering to many of our fellow humans. And thanks to our training as psychiatric physicians, we have developed extra “receptors” to the darker side of the human condition. As we help many of our psychiatric patients rendered sicker under the unbearable stress of the pandemic, we must not overlook the plight of so many others who do not show up in our clinics for health care, yet suffer enormously but imperceptibly. And no vaccine can come to the rescue of those who continue to live in quiet desperation.
Long-standing epidemics
It is truly unfortunate that many of the epidemics I am referring to have persisted for so long that they have become “fixtures” of contemporary societies. They have become “endemic epidemics” with no urgency to squelch them, as with the COVID-19 pandemic. The benign neglect that perpetuates these serious epidemics has had a malignant effect of “grudging resignation” that nothing can be done to reverse them. Unlike the viral epidemic that engulfed everyone around the world and triggered a massive and unified push to defeat the virus, these long-standing epidemics continue to afflict subgroups who are left to fend for themselves. These individuals deserve our empathy and warrant our determination to lift them from their miserable existence.
Consider some of the widespread epidemics that preceded the pandemic and will, in all likelihood, persist after the pandemic’s burden is lifted:
- millions of people living in poverty and hunger
- widespread racism
- smoldering social injustice
- appalling human trafficking, especially targeting children and women
- child abuse and neglect that leads to psychosis, depression, and suicide in adulthood
- gun violence, which kills many innocent people
- domestic violence that inflicts both physical and mental harm on families
- suicide, both attempts and completions, which continues to increase annually
- the festering stigma of mental illness that adds insult to injury for psychiatric patients
- alcohol and drug addictions, which destroy lives and corrode the fabric of society
- lack of access to mental health care for millions of people who need it
- lack of parity for psychiatric disorders, which is so unjust for our patients
- venomous political hatred and hyperpartisanship, which permeates our culture and can lead to violence, as we recently witnessed
- physician burnout, due to many causes, even before the stresses of COVID-19
- the ongoing agony of wars and terrorism, including dangerous cyberattacks
- the deleterious effect of social media on everyone, especially children.
Most of these epidemics claim thousands of lives each year, and yet no concerted public health effort is being mounted to counteract them, as we are seeing with the COVID-19 pandemic. Much is being written about each of them, but there has been little tangible action, so they persist. They have become a perpetual underbelly of our society that is essentially ignored or simply given the usual lip service.
It will take a herculean effort by policymakers, the judicial system, the medical establishment, and faith organizations to put an end to these life-threatening epidemics. It may appear too daunting to mount a war on so many fronts, but that should not deter us all from launching a strategic plan to create meaningful tactics and solutions. And just as was done with the COVID-19 pandemic, both mitigation measures as well as effective interventions must be employed in this campaign against the epidemic “hydra.”
Continue to: It is tragic...
It is tragic that so many fellow humans are allowed to suffer or die while the rest of us watch, or worse, turn a blind eye and never get involved. A civilized society must never neglect so many of its suffering citizens. As psychiatrists, we are aware of those human travesties around us, but we are often so overwhelmed with our work and personal responsibilities that few of us are passionately advocating or setting aside some time for those victimized by one or more of these endemic pandemics. And unless we all decide to be actively, meaningfully involved, many lives will continue to be lost every day, but without the daily “casualty count” displayed on television screens, as is the case with COVID-19 causalities.
Regrettably, maybe that old saw is true: out of sight, out of mind.
As we struggle to gradually emerge from the horrid coronavirus disease 2019 (COVID-19) pandemic that has disrupted our lives and killed hundreds of thousands of people in the United States, we harbor the hope that life will return to “normal.” But while it will certainly be a great relief to put this deadly virus behind us, many other epidemics will continue to plague our society and taint our culture.
Scientific ingenuity has led to the development of several vaccines in record time (aka “warp speed”) that will help defeat the deadly scourge of COVID-19. The pandemic is likely to peter out 2 years after its onset. We will all be grateful for such a rapid resolution of the worst health crisis the world has faced in a century, which will enable medical, economic, and social recovery. But as we eventually resume our lives and rejoice in resuming the pursuit of happiness, we will quickly realize that all is not well in our society just because the viral pandemic is gone.
Perhaps the ordeal of the COVID-19 pandemic, and the agony that was universally shared, will open our collective eyes to a jarring reality: many other epidemics will continue to permeate society and cause endless grief and suffering to many of our fellow humans. And thanks to our training as psychiatric physicians, we have developed extra “receptors” to the darker side of the human condition. As we help many of our psychiatric patients rendered sicker under the unbearable stress of the pandemic, we must not overlook the plight of so many others who do not show up in our clinics for health care, yet suffer enormously but imperceptibly. And no vaccine can come to the rescue of those who continue to live in quiet desperation.
Long-standing epidemics
It is truly unfortunate that many of the epidemics I am referring to have persisted for so long that they have become “fixtures” of contemporary societies. They have become “endemic epidemics” with no urgency to squelch them, as with the COVID-19 pandemic. The benign neglect that perpetuates these serious epidemics has had a malignant effect of “grudging resignation” that nothing can be done to reverse them. Unlike the viral epidemic that engulfed everyone around the world and triggered a massive and unified push to defeat the virus, these long-standing epidemics continue to afflict subgroups who are left to fend for themselves. These individuals deserve our empathy and warrant our determination to lift them from their miserable existence.
Consider some of the widespread epidemics that preceded the pandemic and will, in all likelihood, persist after the pandemic’s burden is lifted:
- millions of people living in poverty and hunger
- widespread racism
- smoldering social injustice
- appalling human trafficking, especially targeting children and women
- child abuse and neglect that leads to psychosis, depression, and suicide in adulthood
- gun violence, which kills many innocent people
- domestic violence that inflicts both physical and mental harm on families
- suicide, both attempts and completions, which continues to increase annually
- the festering stigma of mental illness that adds insult to injury for psychiatric patients
- alcohol and drug addictions, which destroy lives and corrode the fabric of society
- lack of access to mental health care for millions of people who need it
- lack of parity for psychiatric disorders, which is so unjust for our patients
- venomous political hatred and hyperpartisanship, which permeates our culture and can lead to violence, as we recently witnessed
- physician burnout, due to many causes, even before the stresses of COVID-19
- the ongoing agony of wars and terrorism, including dangerous cyberattacks
- the deleterious effect of social media on everyone, especially children.
Most of these epidemics claim thousands of lives each year, and yet no concerted public health effort is being mounted to counteract them, as we are seeing with the COVID-19 pandemic. Much is being written about each of them, but there has been little tangible action, so they persist. They have become a perpetual underbelly of our society that is essentially ignored or simply given the usual lip service.
It will take a herculean effort by policymakers, the judicial system, the medical establishment, and faith organizations to put an end to these life-threatening epidemics. It may appear too daunting to mount a war on so many fronts, but that should not deter us all from launching a strategic plan to create meaningful tactics and solutions. And just as was done with the COVID-19 pandemic, both mitigation measures as well as effective interventions must be employed in this campaign against the epidemic “hydra.”
Continue to: It is tragic...
It is tragic that so many fellow humans are allowed to suffer or die while the rest of us watch, or worse, turn a blind eye and never get involved. A civilized society must never neglect so many of its suffering citizens. As psychiatrists, we are aware of those human travesties around us, but we are often so overwhelmed with our work and personal responsibilities that few of us are passionately advocating or setting aside some time for those victimized by one or more of these endemic pandemics. And unless we all decide to be actively, meaningfully involved, many lives will continue to be lost every day, but without the daily “casualty count” displayed on television screens, as is the case with COVID-19 causalities.
Regrettably, maybe that old saw is true: out of sight, out of mind.
As we struggle to gradually emerge from the horrid coronavirus disease 2019 (COVID-19) pandemic that has disrupted our lives and killed hundreds of thousands of people in the United States, we harbor the hope that life will return to “normal.” But while it will certainly be a great relief to put this deadly virus behind us, many other epidemics will continue to plague our society and taint our culture.
Scientific ingenuity has led to the development of several vaccines in record time (aka “warp speed”) that will help defeat the deadly scourge of COVID-19. The pandemic is likely to peter out 2 years after its onset. We will all be grateful for such a rapid resolution of the worst health crisis the world has faced in a century, which will enable medical, economic, and social recovery. But as we eventually resume our lives and rejoice in resuming the pursuit of happiness, we will quickly realize that all is not well in our society just because the viral pandemic is gone.
Perhaps the ordeal of the COVID-19 pandemic, and the agony that was universally shared, will open our collective eyes to a jarring reality: many other epidemics will continue to permeate society and cause endless grief and suffering to many of our fellow humans. And thanks to our training as psychiatric physicians, we have developed extra “receptors” to the darker side of the human condition. As we help many of our psychiatric patients rendered sicker under the unbearable stress of the pandemic, we must not overlook the plight of so many others who do not show up in our clinics for health care, yet suffer enormously but imperceptibly. And no vaccine can come to the rescue of those who continue to live in quiet desperation.
Long-standing epidemics
It is truly unfortunate that many of the epidemics I am referring to have persisted for so long that they have become “fixtures” of contemporary societies. They have become “endemic epidemics” with no urgency to squelch them, as with the COVID-19 pandemic. The benign neglect that perpetuates these serious epidemics has had a malignant effect of “grudging resignation” that nothing can be done to reverse them. Unlike the viral epidemic that engulfed everyone around the world and triggered a massive and unified push to defeat the virus, these long-standing epidemics continue to afflict subgroups who are left to fend for themselves. These individuals deserve our empathy and warrant our determination to lift them from their miserable existence.
Consider some of the widespread epidemics that preceded the pandemic and will, in all likelihood, persist after the pandemic’s burden is lifted:
- millions of people living in poverty and hunger
- widespread racism
- smoldering social injustice
- appalling human trafficking, especially targeting children and women
- child abuse and neglect that leads to psychosis, depression, and suicide in adulthood
- gun violence, which kills many innocent people
- domestic violence that inflicts both physical and mental harm on families
- suicide, both attempts and completions, which continues to increase annually
- the festering stigma of mental illness that adds insult to injury for psychiatric patients
- alcohol and drug addictions, which destroy lives and corrode the fabric of society
- lack of access to mental health care for millions of people who need it
- lack of parity for psychiatric disorders, which is so unjust for our patients
- venomous political hatred and hyperpartisanship, which permeates our culture and can lead to violence, as we recently witnessed
- physician burnout, due to many causes, even before the stresses of COVID-19
- the ongoing agony of wars and terrorism, including dangerous cyberattacks
- the deleterious effect of social media on everyone, especially children.
Most of these epidemics claim thousands of lives each year, and yet no concerted public health effort is being mounted to counteract them, as we are seeing with the COVID-19 pandemic. Much is being written about each of them, but there has been little tangible action, so they persist. They have become a perpetual underbelly of our society that is essentially ignored or simply given the usual lip service.
It will take a herculean effort by policymakers, the judicial system, the medical establishment, and faith organizations to put an end to these life-threatening epidemics. It may appear too daunting to mount a war on so many fronts, but that should not deter us all from launching a strategic plan to create meaningful tactics and solutions. And just as was done with the COVID-19 pandemic, both mitigation measures as well as effective interventions must be employed in this campaign against the epidemic “hydra.”
Continue to: It is tragic...
It is tragic that so many fellow humans are allowed to suffer or die while the rest of us watch, or worse, turn a blind eye and never get involved. A civilized society must never neglect so many of its suffering citizens. As psychiatrists, we are aware of those human travesties around us, but we are often so overwhelmed with our work and personal responsibilities that few of us are passionately advocating or setting aside some time for those victimized by one or more of these endemic pandemics. And unless we all decide to be actively, meaningfully involved, many lives will continue to be lost every day, but without the daily “casualty count” displayed on television screens, as is the case with COVID-19 causalities.
Regrettably, maybe that old saw is true: out of sight, out of mind.
Let’s ‘cancel’ these obsolete terms in DSM
Psychiatry has made significant scientific advances over the past century. However, it is still saddled with archaic terms, with pejorative connotations, disguised as official medical diagnoses. It is time to “cancel” those terms and replace them with ones that are neutral and have not accumulated baggage.
This process of “creative destruction” of psychiatric terminology is long overdue. It is frankly disturbing that the psychiatric jargon used around the time that the American Psychiatric Association was established 175 years ago (1844) is now considered insults and epithets. We no longer work in “lunatic asylums for the insane,” and our patients with intellectual disabilities are no longer classified as “morons,” “idiots,” or “imbeciles.” Such “diagnoses” have certainly contributed to the stigma of psychiatric brain disorders. Even the noble word “asylum” has acquired a negative valence because in the past it referred to hospitals that housed persons with serious mental illness.
Thankfully, some of the outrageous terms fabricated during the condemnable and dark era of slavery 2 centuries ago were never adopted by organized psychiatry. The absurd diagnosis of “negritude,” whose tenet was that black skin is a disease curable by whitening the skin, was “invented” by none other than Benjamin Rush, the Father of Psychiatry, whose conflicted soul was depicted by concomitantly owning a slave and positioning himself as an ardent abolitionist!
Terms that need to be replaced
Fast-forward to the modern era and consider the following:
Borderline personality disorder. It is truly tragic how this confusing and non-scientific term is used as an official diagnosis for a set of seriously ill persons. It is loaded with obloquy, indignity, and derision that completely ignore the tumult, self-harm, and disability with which patients who carry this label are burdened throughout their lives, despite being intelligent. This is a serious brain disorder that has been shown to be highly genetic and is characterized by many well-established structural brain abnormalities that have been documented in neuroimaging studies.1,2 Borderline personality should not be classified as a personality disorder but as an illness with multiple signs and symptoms, including mood lability, anger, impulsivity, self-cutting, suicidal urges, feelings of abandonment, and micro-psychotic episodes. A more clinically accurate term should be coined very soon to replace borderline personality, which should be discarded to the trash heap of obsolete psychiatric terms, and no longer inflicted on patients.
Neurosis. What is the justification for continuing to use the term “neurotic” for a person who has an anxiety disorder? Is it used because Jung and Freud propagated the term “neurosis” (after it was coined by William Cullen in 1769)? Neurosis has degenerated from a psychiatric diagnosis to a scornful snub that must never be used for any patient.
Schizophrenia. This diagnosis, coined by Eugen Bleuler to replace the narrow and pessimistic “dementia praecox” proposed by Emil Kraepelin in the 1920s, initially seemed to be a neutral description of a thought disorder (split associations, not split personality). Bleuler was perceptive enough to call his book Dementia Praecox or the Group of Schizophrenias, which is consistent with the modern scientific research that confirms schizophrenia is a very heterogeneous syndrome with hundreds of genetic and environmental biotypes with a similar phenotype but a wide range of severity, treatment response, and functional outcomes. However, in subsequent decades, schizophrenia became one of the most demeaning labels in psychiatry, casting a shadow of hopelessness and disability on the people who have this serious neurologic condition with many psychiatric symptoms. The term that should replace schizophrenia should be no more degrading than stroke, multiple sclerosis, or myocardial infarction.
Continue to: Over the past 15 years...
Over the past 15 years, an expanding group of schizophrenia experts have agreed that this term must be changed to one that reflects the core features of this syndrome, and have proposed terms such as “salience syndrome,” “psychosis-spectrum,” and “reality distortion and cognitive impairment disorder.”3 In fact, several countries have already adopted a new official diagnosis for schizophrenia.4 Japan now uses the term “integration disorder,” which has significantly reduced the stigma of this brain disorder.5 South Korea changed the name to “attunement disorder.” Hong Kong and Taiwan now use “dysfunction of thought and perception.” Some researchers recommend calling schizophrenia “Bleuler’s syndrome,” a neutral eponymous designation.
One of the most irritating things about the term schizophrenia is the widespread misconception that it means “split personality.” This prompts some sports announcers to call a football team “schizophrenic” if they play well in the first half and badly in the second. The stock market is labeled “schizophrenic” if it goes up one day and way down on the next. No other medical term is misused by the media as often as the term schizophrenia.
Narcissistic personality disorder. The origin of this diagnostic category is the concept of “malignant narcissism” coined by Erich Fromm in 1964, which he designated as “the quintessence of evil.” I strongly object to implying that evil is part of any psychiatric diagnosis. Numerous studies have found structural brain abnormalities (in both gray and white matter) in patients diagnosed with psychopathic traits.6 Later, malignant narcissism was reframed as narcissistic personality disorder in 1971 by Herbert Rosenfeld. Although malignant narcissism was never accepted by either the DSM or the International Classification of Diseases, narcissistic personality disorder has been included in the DSM for the past few decades. This diagnosis reeks of disparagement and negativity. Persons with narcissistic personality disorder have been shown to have pathological brain changes in resting-state functional connectivity,7 weakened frontostriatal white matter connectivity,8,9 and a reduced frontal thickness and cortical volume.10 A distorted sense of self and others is a socially disabling disorder that should generate empathy, not disdain. Narcissistic personality disorder should be replaced by a term that accurately describes its behavioral pathology, and should not incorporate Greek mythology.
Mania. This is another unfortunate diagnosis that immediately evokes a negative image of patients who suffer from a potentially lethal brain disorder. It was fortunate that Robert Kendall coined the term “bipolar disorder” to replace “manic-depressive illness,” but mania is still being used within bipolar disorder as a prominent clinical phase. While depression accurately describes the mood in the other phase of this disorder, the term mania evokes wild, irrational behavior. Because the actual mood symptom cluster in mania is either elation/grandiosity or irritability/anger, why not replace mania with “elation/irritability phase of bipolar disorder”? It is more descriptive of the patient’s mood and is less pejorative.
Nomenclature is vital, and words do matter, especially when used as a diagnostic medical term. Psychiatry must “cancel” its archaic names, which are infused with negative connotations. Reinventing the psychiatric lexicon is a necessary act of renewal in a specialty where a poorly worded diagnostic label can morph into the equivalent of a “scarlet letter.” Think of other contemptuous terms, such as refrigerator mother, male hysteria, moral insanity, toxic parents, inadequate personality disorder, neurasthenia, or catastrophic schizophrenia.
General medicine regularly discards many of its obsolete terms.11 These include terms such as ablepsy, ague, camp fever, bloody flux, chlorosis, catarrh, consumption, dropsy, French pox, phthisis, milk sickness, and scrumpox.
Think also of how society abandoned the antediluvian names of boys and girls. Few parents these days would name their son Ackley, Allard, Arundel, Awarnach, Beldon, Durward, Grower, Kenlm, or Legolan, or name their daughter Afton, Agrona, Arantxa, Corliss, Demelza, Eartha, Maida, Obsession, Radella, or Sacrifice.In summary, a necessary part of psychiatry’s progress is shedding obsolete terminology, even if it means slaughtering some widely used “traditional” vocabulary. It is a necessary act of renewal, and the image of psychiatry will be burnished by it.
1. Nasrallah HA. Borderline personality disorder is a heritable brain disease. Current Psychiatry. 2014;13(4):19-20,32.
2. Sagarwala R, Nasrallah HA. White matter pathology in patients with borderline personality disorder: a review of controlled DTI studies. Ann Clin Psychiatry. 2020;32(4):281-286.
3. Keshavan MS, Tandon R, Nasrallah HA. Renaming schizophrenia: keeping up with the facts. Schizophr Res. 2013;148(1-3):1-2.
4. Lasalvia A, Penta E, Sartorius N, et al. Should the label “schizophrenia” be abandoned? Schizophr Res. 2015;162(1-3):276-284.
5. Takahashi H, Ideno T, Okubo S, et al. Impact of changing the Japanese term for “schizophrenia” for reasons of stereotypical beliefs of schizophrenia in Japanese youth. Schizophr Res. 2009;112(1-3):149-152.
6. Johanson M, Vaurio D, Tiihunen J, et al. A systematic literature review of neuroimaging of psychopathic traits. Front Psychiatry. 2020;10:1027.
7. Yang, W, Cun L, Du X, et al. Gender differences in brain structure and resting-state functional connectivity related to narcissistic personality. Sci Rep. 2015;5:10924.
8. Chester DS, Cynam DR, Powell DK, et al. Narcissismis associated with weakened frontostriatal connectivity: a DTI study. Soc Cogn Affect Neurosci. 2016;11(7):1036-1040.
9. Nenadic I, Gullmar D, Dietzek M, et al. Brain structure in narcissistic personality disorder: a VBM and DTI pilot study. Psychiatry Res. 2015;231(2):184-186.
10. Mao Y, Sang N, Wang Y, et al. Reduced frontal cortex thickness and cortical volume associated with pathological narcissism. Neuroscience. 2016;378:51-57.
11. Nasrallah HA. The transient truths of medical ‘progress.’ Current Psychiatry. 2014;13(6):23-24.
Psychiatry has made significant scientific advances over the past century. However, it is still saddled with archaic terms, with pejorative connotations, disguised as official medical diagnoses. It is time to “cancel” those terms and replace them with ones that are neutral and have not accumulated baggage.
This process of “creative destruction” of psychiatric terminology is long overdue. It is frankly disturbing that the psychiatric jargon used around the time that the American Psychiatric Association was established 175 years ago (1844) is now considered insults and epithets. We no longer work in “lunatic asylums for the insane,” and our patients with intellectual disabilities are no longer classified as “morons,” “idiots,” or “imbeciles.” Such “diagnoses” have certainly contributed to the stigma of psychiatric brain disorders. Even the noble word “asylum” has acquired a negative valence because in the past it referred to hospitals that housed persons with serious mental illness.
Thankfully, some of the outrageous terms fabricated during the condemnable and dark era of slavery 2 centuries ago were never adopted by organized psychiatry. The absurd diagnosis of “negritude,” whose tenet was that black skin is a disease curable by whitening the skin, was “invented” by none other than Benjamin Rush, the Father of Psychiatry, whose conflicted soul was depicted by concomitantly owning a slave and positioning himself as an ardent abolitionist!
Terms that need to be replaced
Fast-forward to the modern era and consider the following:
Borderline personality disorder. It is truly tragic how this confusing and non-scientific term is used as an official diagnosis for a set of seriously ill persons. It is loaded with obloquy, indignity, and derision that completely ignore the tumult, self-harm, and disability with which patients who carry this label are burdened throughout their lives, despite being intelligent. This is a serious brain disorder that has been shown to be highly genetic and is characterized by many well-established structural brain abnormalities that have been documented in neuroimaging studies.1,2 Borderline personality should not be classified as a personality disorder but as an illness with multiple signs and symptoms, including mood lability, anger, impulsivity, self-cutting, suicidal urges, feelings of abandonment, and micro-psychotic episodes. A more clinically accurate term should be coined very soon to replace borderline personality, which should be discarded to the trash heap of obsolete psychiatric terms, and no longer inflicted on patients.
Neurosis. What is the justification for continuing to use the term “neurotic” for a person who has an anxiety disorder? Is it used because Jung and Freud propagated the term “neurosis” (after it was coined by William Cullen in 1769)? Neurosis has degenerated from a psychiatric diagnosis to a scornful snub that must never be used for any patient.
Schizophrenia. This diagnosis, coined by Eugen Bleuler to replace the narrow and pessimistic “dementia praecox” proposed by Emil Kraepelin in the 1920s, initially seemed to be a neutral description of a thought disorder (split associations, not split personality). Bleuler was perceptive enough to call his book Dementia Praecox or the Group of Schizophrenias, which is consistent with the modern scientific research that confirms schizophrenia is a very heterogeneous syndrome with hundreds of genetic and environmental biotypes with a similar phenotype but a wide range of severity, treatment response, and functional outcomes. However, in subsequent decades, schizophrenia became one of the most demeaning labels in psychiatry, casting a shadow of hopelessness and disability on the people who have this serious neurologic condition with many psychiatric symptoms. The term that should replace schizophrenia should be no more degrading than stroke, multiple sclerosis, or myocardial infarction.
Continue to: Over the past 15 years...
Over the past 15 years, an expanding group of schizophrenia experts have agreed that this term must be changed to one that reflects the core features of this syndrome, and have proposed terms such as “salience syndrome,” “psychosis-spectrum,” and “reality distortion and cognitive impairment disorder.”3 In fact, several countries have already adopted a new official diagnosis for schizophrenia.4 Japan now uses the term “integration disorder,” which has significantly reduced the stigma of this brain disorder.5 South Korea changed the name to “attunement disorder.” Hong Kong and Taiwan now use “dysfunction of thought and perception.” Some researchers recommend calling schizophrenia “Bleuler’s syndrome,” a neutral eponymous designation.
One of the most irritating things about the term schizophrenia is the widespread misconception that it means “split personality.” This prompts some sports announcers to call a football team “schizophrenic” if they play well in the first half and badly in the second. The stock market is labeled “schizophrenic” if it goes up one day and way down on the next. No other medical term is misused by the media as often as the term schizophrenia.
Narcissistic personality disorder. The origin of this diagnostic category is the concept of “malignant narcissism” coined by Erich Fromm in 1964, which he designated as “the quintessence of evil.” I strongly object to implying that evil is part of any psychiatric diagnosis. Numerous studies have found structural brain abnormalities (in both gray and white matter) in patients diagnosed with psychopathic traits.6 Later, malignant narcissism was reframed as narcissistic personality disorder in 1971 by Herbert Rosenfeld. Although malignant narcissism was never accepted by either the DSM or the International Classification of Diseases, narcissistic personality disorder has been included in the DSM for the past few decades. This diagnosis reeks of disparagement and negativity. Persons with narcissistic personality disorder have been shown to have pathological brain changes in resting-state functional connectivity,7 weakened frontostriatal white matter connectivity,8,9 and a reduced frontal thickness and cortical volume.10 A distorted sense of self and others is a socially disabling disorder that should generate empathy, not disdain. Narcissistic personality disorder should be replaced by a term that accurately describes its behavioral pathology, and should not incorporate Greek mythology.
Mania. This is another unfortunate diagnosis that immediately evokes a negative image of patients who suffer from a potentially lethal brain disorder. It was fortunate that Robert Kendall coined the term “bipolar disorder” to replace “manic-depressive illness,” but mania is still being used within bipolar disorder as a prominent clinical phase. While depression accurately describes the mood in the other phase of this disorder, the term mania evokes wild, irrational behavior. Because the actual mood symptom cluster in mania is either elation/grandiosity or irritability/anger, why not replace mania with “elation/irritability phase of bipolar disorder”? It is more descriptive of the patient’s mood and is less pejorative.
Nomenclature is vital, and words do matter, especially when used as a diagnostic medical term. Psychiatry must “cancel” its archaic names, which are infused with negative connotations. Reinventing the psychiatric lexicon is a necessary act of renewal in a specialty where a poorly worded diagnostic label can morph into the equivalent of a “scarlet letter.” Think of other contemptuous terms, such as refrigerator mother, male hysteria, moral insanity, toxic parents, inadequate personality disorder, neurasthenia, or catastrophic schizophrenia.
General medicine regularly discards many of its obsolete terms.11 These include terms such as ablepsy, ague, camp fever, bloody flux, chlorosis, catarrh, consumption, dropsy, French pox, phthisis, milk sickness, and scrumpox.
Think also of how society abandoned the antediluvian names of boys and girls. Few parents these days would name their son Ackley, Allard, Arundel, Awarnach, Beldon, Durward, Grower, Kenlm, or Legolan, or name their daughter Afton, Agrona, Arantxa, Corliss, Demelza, Eartha, Maida, Obsession, Radella, or Sacrifice.In summary, a necessary part of psychiatry’s progress is shedding obsolete terminology, even if it means slaughtering some widely used “traditional” vocabulary. It is a necessary act of renewal, and the image of psychiatry will be burnished by it.
Psychiatry has made significant scientific advances over the past century. However, it is still saddled with archaic terms, with pejorative connotations, disguised as official medical diagnoses. It is time to “cancel” those terms and replace them with ones that are neutral and have not accumulated baggage.
This process of “creative destruction” of psychiatric terminology is long overdue. It is frankly disturbing that the psychiatric jargon used around the time that the American Psychiatric Association was established 175 years ago (1844) is now considered insults and epithets. We no longer work in “lunatic asylums for the insane,” and our patients with intellectual disabilities are no longer classified as “morons,” “idiots,” or “imbeciles.” Such “diagnoses” have certainly contributed to the stigma of psychiatric brain disorders. Even the noble word “asylum” has acquired a negative valence because in the past it referred to hospitals that housed persons with serious mental illness.
Thankfully, some of the outrageous terms fabricated during the condemnable and dark era of slavery 2 centuries ago were never adopted by organized psychiatry. The absurd diagnosis of “negritude,” whose tenet was that black skin is a disease curable by whitening the skin, was “invented” by none other than Benjamin Rush, the Father of Psychiatry, whose conflicted soul was depicted by concomitantly owning a slave and positioning himself as an ardent abolitionist!
Terms that need to be replaced
Fast-forward to the modern era and consider the following:
Borderline personality disorder. It is truly tragic how this confusing and non-scientific term is used as an official diagnosis for a set of seriously ill persons. It is loaded with obloquy, indignity, and derision that completely ignore the tumult, self-harm, and disability with which patients who carry this label are burdened throughout their lives, despite being intelligent. This is a serious brain disorder that has been shown to be highly genetic and is characterized by many well-established structural brain abnormalities that have been documented in neuroimaging studies.1,2 Borderline personality should not be classified as a personality disorder but as an illness with multiple signs and symptoms, including mood lability, anger, impulsivity, self-cutting, suicidal urges, feelings of abandonment, and micro-psychotic episodes. A more clinically accurate term should be coined very soon to replace borderline personality, which should be discarded to the trash heap of obsolete psychiatric terms, and no longer inflicted on patients.
Neurosis. What is the justification for continuing to use the term “neurotic” for a person who has an anxiety disorder? Is it used because Jung and Freud propagated the term “neurosis” (after it was coined by William Cullen in 1769)? Neurosis has degenerated from a psychiatric diagnosis to a scornful snub that must never be used for any patient.
Schizophrenia. This diagnosis, coined by Eugen Bleuler to replace the narrow and pessimistic “dementia praecox” proposed by Emil Kraepelin in the 1920s, initially seemed to be a neutral description of a thought disorder (split associations, not split personality). Bleuler was perceptive enough to call his book Dementia Praecox or the Group of Schizophrenias, which is consistent with the modern scientific research that confirms schizophrenia is a very heterogeneous syndrome with hundreds of genetic and environmental biotypes with a similar phenotype but a wide range of severity, treatment response, and functional outcomes. However, in subsequent decades, schizophrenia became one of the most demeaning labels in psychiatry, casting a shadow of hopelessness and disability on the people who have this serious neurologic condition with many psychiatric symptoms. The term that should replace schizophrenia should be no more degrading than stroke, multiple sclerosis, or myocardial infarction.
Continue to: Over the past 15 years...
Over the past 15 years, an expanding group of schizophrenia experts have agreed that this term must be changed to one that reflects the core features of this syndrome, and have proposed terms such as “salience syndrome,” “psychosis-spectrum,” and “reality distortion and cognitive impairment disorder.”3 In fact, several countries have already adopted a new official diagnosis for schizophrenia.4 Japan now uses the term “integration disorder,” which has significantly reduced the stigma of this brain disorder.5 South Korea changed the name to “attunement disorder.” Hong Kong and Taiwan now use “dysfunction of thought and perception.” Some researchers recommend calling schizophrenia “Bleuler’s syndrome,” a neutral eponymous designation.
One of the most irritating things about the term schizophrenia is the widespread misconception that it means “split personality.” This prompts some sports announcers to call a football team “schizophrenic” if they play well in the first half and badly in the second. The stock market is labeled “schizophrenic” if it goes up one day and way down on the next. No other medical term is misused by the media as often as the term schizophrenia.
Narcissistic personality disorder. The origin of this diagnostic category is the concept of “malignant narcissism” coined by Erich Fromm in 1964, which he designated as “the quintessence of evil.” I strongly object to implying that evil is part of any psychiatric diagnosis. Numerous studies have found structural brain abnormalities (in both gray and white matter) in patients diagnosed with psychopathic traits.6 Later, malignant narcissism was reframed as narcissistic personality disorder in 1971 by Herbert Rosenfeld. Although malignant narcissism was never accepted by either the DSM or the International Classification of Diseases, narcissistic personality disorder has been included in the DSM for the past few decades. This diagnosis reeks of disparagement and negativity. Persons with narcissistic personality disorder have been shown to have pathological brain changes in resting-state functional connectivity,7 weakened frontostriatal white matter connectivity,8,9 and a reduced frontal thickness and cortical volume.10 A distorted sense of self and others is a socially disabling disorder that should generate empathy, not disdain. Narcissistic personality disorder should be replaced by a term that accurately describes its behavioral pathology, and should not incorporate Greek mythology.
Mania. This is another unfortunate diagnosis that immediately evokes a negative image of patients who suffer from a potentially lethal brain disorder. It was fortunate that Robert Kendall coined the term “bipolar disorder” to replace “manic-depressive illness,” but mania is still being used within bipolar disorder as a prominent clinical phase. While depression accurately describes the mood in the other phase of this disorder, the term mania evokes wild, irrational behavior. Because the actual mood symptom cluster in mania is either elation/grandiosity or irritability/anger, why not replace mania with “elation/irritability phase of bipolar disorder”? It is more descriptive of the patient’s mood and is less pejorative.
Nomenclature is vital, and words do matter, especially when used as a diagnostic medical term. Psychiatry must “cancel” its archaic names, which are infused with negative connotations. Reinventing the psychiatric lexicon is a necessary act of renewal in a specialty where a poorly worded diagnostic label can morph into the equivalent of a “scarlet letter.” Think of other contemptuous terms, such as refrigerator mother, male hysteria, moral insanity, toxic parents, inadequate personality disorder, neurasthenia, or catastrophic schizophrenia.
General medicine regularly discards many of its obsolete terms.11 These include terms such as ablepsy, ague, camp fever, bloody flux, chlorosis, catarrh, consumption, dropsy, French pox, phthisis, milk sickness, and scrumpox.
Think also of how society abandoned the antediluvian names of boys and girls. Few parents these days would name their son Ackley, Allard, Arundel, Awarnach, Beldon, Durward, Grower, Kenlm, or Legolan, or name their daughter Afton, Agrona, Arantxa, Corliss, Demelza, Eartha, Maida, Obsession, Radella, or Sacrifice.In summary, a necessary part of psychiatry’s progress is shedding obsolete terminology, even if it means slaughtering some widely used “traditional” vocabulary. It is a necessary act of renewal, and the image of psychiatry will be burnished by it.
1. Nasrallah HA. Borderline personality disorder is a heritable brain disease. Current Psychiatry. 2014;13(4):19-20,32.
2. Sagarwala R, Nasrallah HA. White matter pathology in patients with borderline personality disorder: a review of controlled DTI studies. Ann Clin Psychiatry. 2020;32(4):281-286.
3. Keshavan MS, Tandon R, Nasrallah HA. Renaming schizophrenia: keeping up with the facts. Schizophr Res. 2013;148(1-3):1-2.
4. Lasalvia A, Penta E, Sartorius N, et al. Should the label “schizophrenia” be abandoned? Schizophr Res. 2015;162(1-3):276-284.
5. Takahashi H, Ideno T, Okubo S, et al. Impact of changing the Japanese term for “schizophrenia” for reasons of stereotypical beliefs of schizophrenia in Japanese youth. Schizophr Res. 2009;112(1-3):149-152.
6. Johanson M, Vaurio D, Tiihunen J, et al. A systematic literature review of neuroimaging of psychopathic traits. Front Psychiatry. 2020;10:1027.
7. Yang, W, Cun L, Du X, et al. Gender differences in brain structure and resting-state functional connectivity related to narcissistic personality. Sci Rep. 2015;5:10924.
8. Chester DS, Cynam DR, Powell DK, et al. Narcissismis associated with weakened frontostriatal connectivity: a DTI study. Soc Cogn Affect Neurosci. 2016;11(7):1036-1040.
9. Nenadic I, Gullmar D, Dietzek M, et al. Brain structure in narcissistic personality disorder: a VBM and DTI pilot study. Psychiatry Res. 2015;231(2):184-186.
10. Mao Y, Sang N, Wang Y, et al. Reduced frontal cortex thickness and cortical volume associated with pathological narcissism. Neuroscience. 2016;378:51-57.
11. Nasrallah HA. The transient truths of medical ‘progress.’ Current Psychiatry. 2014;13(6):23-24.
1. Nasrallah HA. Borderline personality disorder is a heritable brain disease. Current Psychiatry. 2014;13(4):19-20,32.
2. Sagarwala R, Nasrallah HA. White matter pathology in patients with borderline personality disorder: a review of controlled DTI studies. Ann Clin Psychiatry. 2020;32(4):281-286.
3. Keshavan MS, Tandon R, Nasrallah HA. Renaming schizophrenia: keeping up with the facts. Schizophr Res. 2013;148(1-3):1-2.
4. Lasalvia A, Penta E, Sartorius N, et al. Should the label “schizophrenia” be abandoned? Schizophr Res. 2015;162(1-3):276-284.
5. Takahashi H, Ideno T, Okubo S, et al. Impact of changing the Japanese term for “schizophrenia” for reasons of stereotypical beliefs of schizophrenia in Japanese youth. Schizophr Res. 2009;112(1-3):149-152.
6. Johanson M, Vaurio D, Tiihunen J, et al. A systematic literature review of neuroimaging of psychopathic traits. Front Psychiatry. 2020;10:1027.
7. Yang, W, Cun L, Du X, et al. Gender differences in brain structure and resting-state functional connectivity related to narcissistic personality. Sci Rep. 2015;5:10924.
8. Chester DS, Cynam DR, Powell DK, et al. Narcissismis associated with weakened frontostriatal connectivity: a DTI study. Soc Cogn Affect Neurosci. 2016;11(7):1036-1040.
9. Nenadic I, Gullmar D, Dietzek M, et al. Brain structure in narcissistic personality disorder: a VBM and DTI pilot study. Psychiatry Res. 2015;231(2):184-186.
10. Mao Y, Sang N, Wang Y, et al. Reduced frontal cortex thickness and cortical volume associated with pathological narcissism. Neuroscience. 2016;378:51-57.
11. Nasrallah HA. The transient truths of medical ‘progress.’ Current Psychiatry. 2014;13(6):23-24.
2020: The year a viral asteroid collided with planet earth
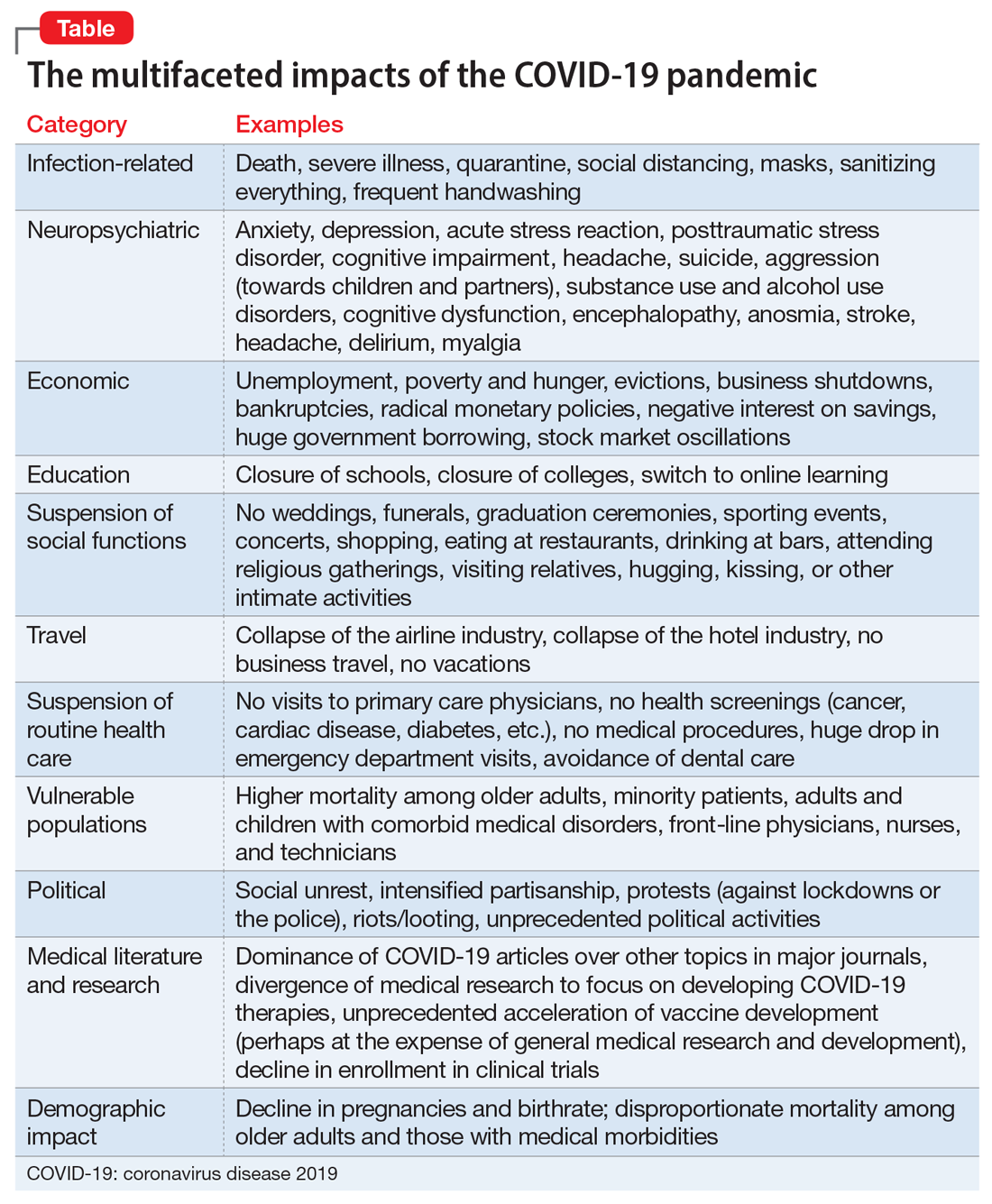
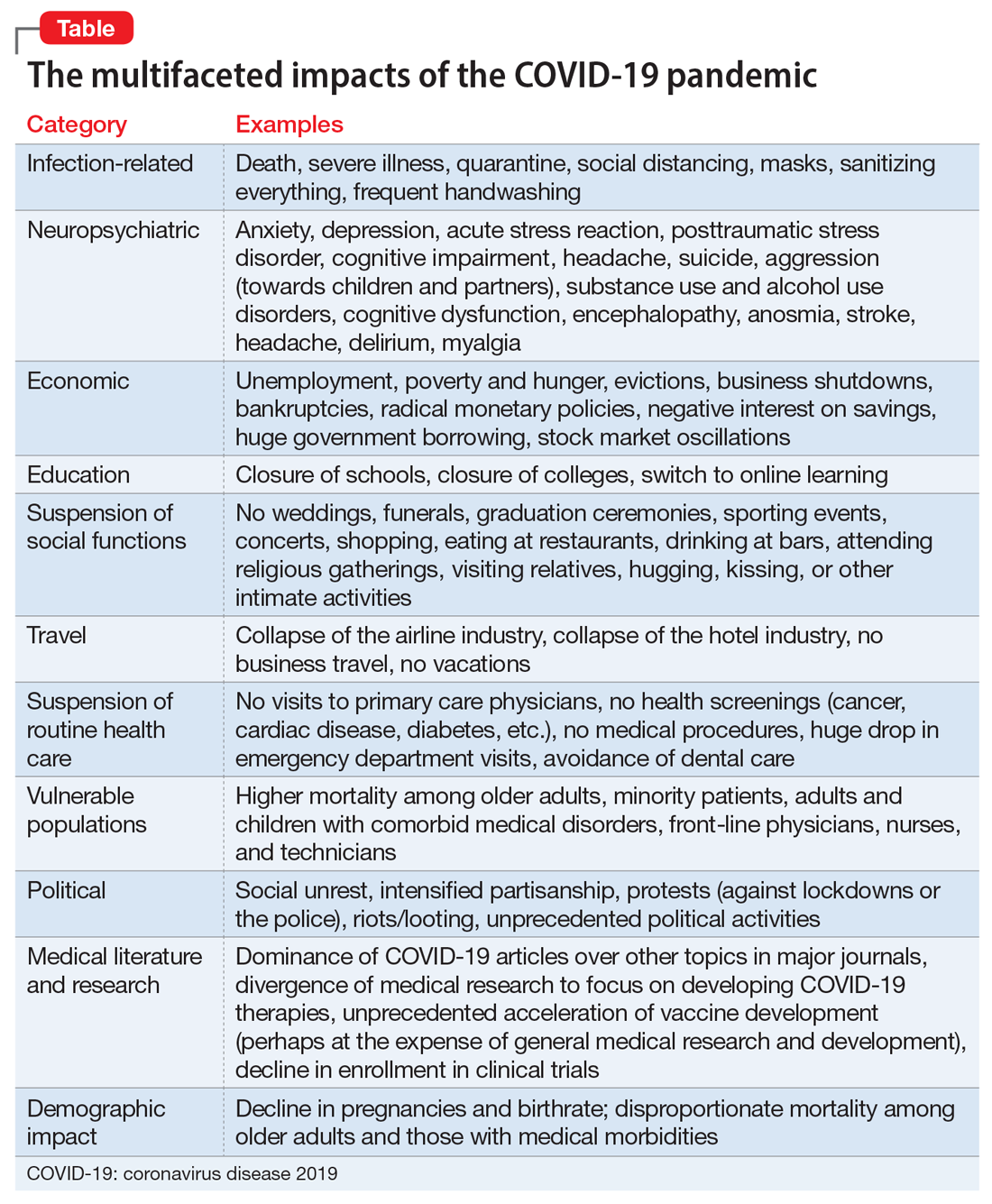
Finally, 2020 is coming to an end, but the agony its viral pandemic inflicted on the entire world population will continue for a long time. And much as we would like to forget its damaging effects, it will surely be etched into our brains for the rest of our lives. The children who suffered the pain of the coronavirus disease 2019 (COVID-19) pandemic will endure its emotional scars for the rest of the 21st century.
Reading about the plagues of the past doesn’t come close to experiencing it and suffering through it. COVID-19 will continue to have ripple effects on every aspect of life on this planet, on individuals and on societies all over the world, especially on the biopsychosocial well-being of billions of humans around the globe.
Unprecedented disruptions
Think of the unprecedented disruptions inflicted by the trauma of the COVID-19 pandemic on our neural circuits. One of the wonders of the human brain is its continuous remodeling due to experiential neuroplasticity, and the formation of dendritic spines that immediately encode the memories of every experience. The turmoil of 2020 and its virulent pandemic will be forever etched into our collective brains, especially in our hippocampi and amygdalae. The impact on the developing brains of our children and grandchildren could be profound and may induce epigenetic changes that trigger psychopathology in the future.1,2
As with the dinosaurs, the 2020 pandemic is like a “viral asteroid” that left devastation on our social fabric and psychological well-being in its wake. We now have deep empathy with our 1918 ancestors and their tribulations, although so far, in the United States the proportion of people infected with COVID-19 (3% as of mid-November 20203) is dwarfed by the proportion infected with the influenza virus a century ago (30%). As of mid-November 2020, the number of global COVID-19 deaths (1.3 million3) was a tiny fraction of the 1918 influenza pandemic deaths (50 million worldwide and 675,000 in the United States4). Amazingly, researchers did not even know whether the killer germ was a virus or a bacterium until 1930, and it then took another 75 years to decode the genome of the influenza virus in 2005. In contrast, it took only a few short weeks to decode the genome of the virus that causes COVID-19 (severe acute respiratory syndrome-related coronavirus 2), and to begin developing multiple vaccines “at warp speed.” No vaccine or therapies were ever developed for victims of the 1918 pandemic.
An abundance of articles has been published about the pandemic since it ambushed us early in 2020, including many in
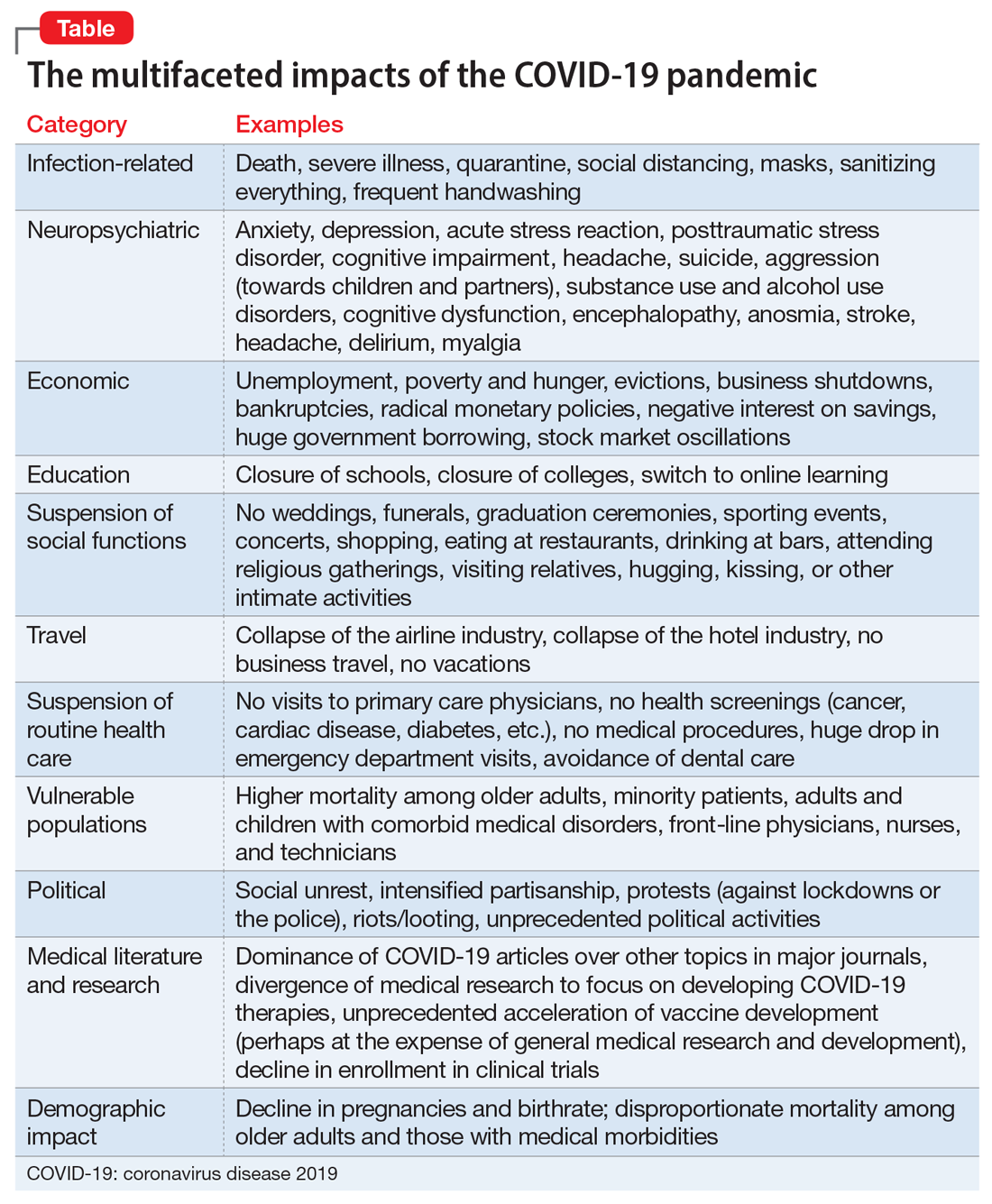
Most psychiatrists are familiar with the Holmes and Rahe Stress Scale,22 which contains 43 life events that cumulatively can progressively increase the odds of physical illness. It is likely that most of the world’s population will score very high on the Holmes and Rahe Stress Scale, which would predict an increased risk of medical illness, even after the pandemic subsides.
Exacerbating the situation is that hospitals and clinics had to shut down most of their operations to focus their resources on treating patients with COVID-19 in ICUs. This halted all routine screenings for cancer and heart, kidney, liver, lung, or brain diseases. In addition, diagnostic or therapeutic procedures such as endoscopies, colonoscopies, angiograms, or biopsies abruptly stopped, resulting in a surge of non–COVID-19 medical disorders and mortality as reported in several articles across many specialties.23 Going forward, in addition to COVID-19 morbidity and mortality, there is a significant likelihood of an increase in myriad medical disorders. The COVID-19 pandemic is obviously inflicting both direct and indirect casualties as it stretches into the next year and perhaps longer. The only hope for the community of nations is the rapid arrival of evidence-based treatments and vaccine(s).
Continue to: A progression of relentless stress
A progression of relentless stress
At the core of this pandemic is relentless stress. When it began in early 2020, the pandemic ignited an acute stress reaction due to the fear of death and the oddness of being isolated at home. Aggravating the acute stress was the realization that life as we knew it suddenly disappeared and all business or social activities had come to a screeching halt. It was almost surreal when streets usually bustling with human activity (such as Times Square in New York or Michigan Avenue in Chicago) became completely deserted and eerily silent. In addition, more stress was generated from watching television or scrolling through social media and being inundated with morbid and frightening news and updates about the number of individuals who became infected or died, and the official projections of tens of thousands or even hundreds of thousands of fatalities. Further intensifying the stress was hearing that there was a shortage of personal protective equipment (even masks), a lack of ventilators, and the absence of any medications to fight the overwhelming viral infection. Especially stressed were the front-line physicians and nurses, who heroically transcended their fears to save their patients’ lives. The sight of refrigerated trucks serving as temporary morgues outside hospital doors was chilling. The world became a macabre place where people died in hospitals without any relative to hold their hands or comfort them, and then were buried quickly without any formal funerals due to mandatory social distancing. The inability of families to grieve for their loved ones added another poignant layer of sadness and distress to the survivors who were unable to bid their loved ones goodbye. This was a jarring example of adding insult to injury.
With the protraction of the exceptional changes imposed by the pandemic, the acute stress reaction transmuted into posttraumatic stress disorder (PTSD) on a wide scale. Millions of previously healthy individuals began to succumb to the symptoms of PTSD (irritability, hypervigilance, intrusive thoughts, avoidance, insomnia, and bad dreams). The heaviest burden was inflicted on our patients, across all ages, with preexisting psychiatric conditions, who comprise approximately 25% of the population per the classic Epidemiological Catchment Area (ECA) study.24 These vulnerable patients, whom we see in our clinics and hospitals every day, had a significant exacerbation of their psychopathology, including anxiety, depression, psychosis, binge eating disorder, obsessive-compulsive disorder, alcohol and substance use disorders, child abuse, and intimate partner violence.25,26 The saving grace was the rapid adoption of telepsychiatry, which our psychiatric patients rapidly accepted. Many of them found it more convenient than dressing and driving and parking at the clinic. It also enabled psychiatrists to obtain useful collateral information from family members or partners.
If something good comes from this catastrophic social stress that emotionally hobbled the entire population, it would be the dilution of the stigma of mental illness because everyone has become more empathic due to their personal experience. Optimistically, this may also help expedite true health care parity for psychiatric brain disorders. And perhaps the government may see the need to train more psychiatrists and fund a higher number of residency stipends to all training programs.
Quo vadis COVID-19?
So, looking through the dense fog of the pandemic fatigue, what will 2021 bring us? Will waves of COVID-19 lead to pandemic exhaustion? Will the frayed public mental health care system be able to handle the surge of frayed nerves? Will social distancing intensify the widespread emotional disquietude? Will the children be able to manifest resilience and avoid disabling psychiatric disorders? Will the survivors of COVID-19 infections suffer from post–COVD-19 neuropsychiatric and other medical sequelae? Will efficacious therapies and vaccines emerge to blunt the spread of the virus? Will we all be able to gather in stadiums and arenas to enjoy sporting events, shows, and concerts? Will eating at our favorite restaurants become routine again? Will engaged couples be able to organize well-attended weddings and receptions? Will airplanes and hotels be fully booked again? Importantly, will all children and college students be able to resume their education in person and socialize ad lib? Will we be able to shed our masks and hug each other hello and goodbye? Will scientific journals and social media cover a wide array of topics again as before? Will the number of deaths dwindle to zero, and will we return to worrying mainly about the usual seasonal flu? Will everyone be able to leave home and go to work again?
I hope that the thick dust of this 2020 viral asteroid will settle in 2021, and that “normalcy” is eventually restored to our lives, allowing us to deal with other ongoing stresses such as social unrest and political hyperpartisanship.
1. Baumeister D, Akhtar R, Ciufolini S, et al. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Mol Psychiatry. 2016;21(5):642-649.
2. Zatti C, Rosa V, Barros A, et al. Childhood trauma and suicide attempt: a meta-analysis of longitudinal studies from the last decade. Psychiatry Res. 2017;256:353-358.
3. Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/. Accessed November 11, 2020.
4. Centers for Disease Control and Prevention. 1918 Pandemic. https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html. Accessed November 4, 2020.
5. Chepke C. Drive-up pharmacotherapy during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):29-30.
6. Sharma RA, Maheshwari S, Bronsther R. COVID-19 in the era of loneliness. Current Psychiatry. 2020;19(5):31-33.
7. Joshi KG. Taking care of ourselves during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):46-47.
8. Frank B, Peterson T, Gupta S, et al. Telepsychiatry: what you need to know. Current Psychiatry. 2020;19(6):16-23.
9. Chahal K. Neuropsychiatric manifestations of COVID-19. Current Psychiatry. 2020;19(6):31-33.
10. Arbuck D. Changes in patient behavior during COVID-19: what I’ve observed. Current Psychiatry. 2020;19(6):46-47.
11. Joshi KG. Telepsychiatry during COVID-19: understanding the rules. Current Psychiatry. 2020;19(6):e12-e14.
12. Komrad MS. Medical ethics in the time of COVID-19. Current Psychiatry. 2020;19(7):29-32,46.
13. Brooks V. COVID-19’s effects on emergency psychiatry. Current Psychiatry. 2020;19(7):33-36,38-39.
14. Desarbo JR, DeSarbo L. Anorexia nervosa and COVID-19. Current Psychiatry. 2020;19(8):23-28.
15. Freudenreich O, Kontos N, Querques J. COVID-19 and patients with serious mental illness. Current Psychiatry. 2020;19(9):24-27,33-39.
16. Ryznar E. Evaluating patients’ decision-making capacity during COVID-19. Current Psychiatry. 2020;19(10):34-40.
17. Saeed SA, Hebishi K. The psychiatric consequences of COVID-19: 8 studies. Current Psychiatry. 2020;19(11):22-24,28-30,32-35.
18. Lodhi S, Marett C. Using seclusion to prevent COVID-19 transmission on inpatient psychiatry units. Current Psychiatry. 2020;19(11):37-41,53.
19. Nasrallah HA. COVID-19 and the precipitous dismantlement of societal norms. Current Psychiatry. 2020;19(7):12-14,16-17.
20. Nasrallah HA. The cataclysmic COVID-19 pandemic: THIS CHANGES EVERYTHING! Current Psychiatry. 2020;19(5):7-8,16.
21. Nasrallah HA. During a viral pandemic, anxiety is endemic: the psychiatric aspects of COVID-19. Current Psychiatry. 2020;19(4):e3-e5.
22. Holmes TH, Rahe RH. The social readjustment rating scale. Journal of Psychosomatic Research. 1967;11(2):213-218.
23. Berkwits M, Flanagin A, Bauchner H, et al. The COVID-19 pandemic and the JAMA Network. JAMA. 2020;324(12):1159-1160.
24. Robins LN, Regier DA, eds. Psychiatric disorders in America. The Epidemiologic Catchment Area study. New York, NY: The Free Press; 1991.
25. Meninger KA. Psychosis associated with influenza. I. General data: statistical analysis. JAMA. 1919;72(4):235-241.
26. Simon NM, Saxe GN, Marmar CR. Mental health disorders related to COVID-19-related deaths. JAMA. 2020;324(15):1493-1494.
Finally, 2020 is coming to an end, but the agony its viral pandemic inflicted on the entire world population will continue for a long time. And much as we would like to forget its damaging effects, it will surely be etched into our brains for the rest of our lives. The children who suffered the pain of the coronavirus disease 2019 (COVID-19) pandemic will endure its emotional scars for the rest of the 21st century.
Reading about the plagues of the past doesn’t come close to experiencing it and suffering through it. COVID-19 will continue to have ripple effects on every aspect of life on this planet, on individuals and on societies all over the world, especially on the biopsychosocial well-being of billions of humans around the globe.
Unprecedented disruptions
Think of the unprecedented disruptions inflicted by the trauma of the COVID-19 pandemic on our neural circuits. One of the wonders of the human brain is its continuous remodeling due to experiential neuroplasticity, and the formation of dendritic spines that immediately encode the memories of every experience. The turmoil of 2020 and its virulent pandemic will be forever etched into our collective brains, especially in our hippocampi and amygdalae. The impact on the developing brains of our children and grandchildren could be profound and may induce epigenetic changes that trigger psychopathology in the future.1,2
As with the dinosaurs, the 2020 pandemic is like a “viral asteroid” that left devastation on our social fabric and psychological well-being in its wake. We now have deep empathy with our 1918 ancestors and their tribulations, although so far, in the United States the proportion of people infected with COVID-19 (3% as of mid-November 20203) is dwarfed by the proportion infected with the influenza virus a century ago (30%). As of mid-November 2020, the number of global COVID-19 deaths (1.3 million3) was a tiny fraction of the 1918 influenza pandemic deaths (50 million worldwide and 675,000 in the United States4). Amazingly, researchers did not even know whether the killer germ was a virus or a bacterium until 1930, and it then took another 75 years to decode the genome of the influenza virus in 2005. In contrast, it took only a few short weeks to decode the genome of the virus that causes COVID-19 (severe acute respiratory syndrome-related coronavirus 2), and to begin developing multiple vaccines “at warp speed.” No vaccine or therapies were ever developed for victims of the 1918 pandemic.
An abundance of articles has been published about the pandemic since it ambushed us early in 2020, including many in
Most psychiatrists are familiar with the Holmes and Rahe Stress Scale,22 which contains 43 life events that cumulatively can progressively increase the odds of physical illness. It is likely that most of the world’s population will score very high on the Holmes and Rahe Stress Scale, which would predict an increased risk of medical illness, even after the pandemic subsides.
Exacerbating the situation is that hospitals and clinics had to shut down most of their operations to focus their resources on treating patients with COVID-19 in ICUs. This halted all routine screenings for cancer and heart, kidney, liver, lung, or brain diseases. In addition, diagnostic or therapeutic procedures such as endoscopies, colonoscopies, angiograms, or biopsies abruptly stopped, resulting in a surge of non–COVID-19 medical disorders and mortality as reported in several articles across many specialties.23 Going forward, in addition to COVID-19 morbidity and mortality, there is a significant likelihood of an increase in myriad medical disorders. The COVID-19 pandemic is obviously inflicting both direct and indirect casualties as it stretches into the next year and perhaps longer. The only hope for the community of nations is the rapid arrival of evidence-based treatments and vaccine(s).
Continue to: A progression of relentless stress
A progression of relentless stress
At the core of this pandemic is relentless stress. When it began in early 2020, the pandemic ignited an acute stress reaction due to the fear of death and the oddness of being isolated at home. Aggravating the acute stress was the realization that life as we knew it suddenly disappeared and all business or social activities had come to a screeching halt. It was almost surreal when streets usually bustling with human activity (such as Times Square in New York or Michigan Avenue in Chicago) became completely deserted and eerily silent. In addition, more stress was generated from watching television or scrolling through social media and being inundated with morbid and frightening news and updates about the number of individuals who became infected or died, and the official projections of tens of thousands or even hundreds of thousands of fatalities. Further intensifying the stress was hearing that there was a shortage of personal protective equipment (even masks), a lack of ventilators, and the absence of any medications to fight the overwhelming viral infection. Especially stressed were the front-line physicians and nurses, who heroically transcended their fears to save their patients’ lives. The sight of refrigerated trucks serving as temporary morgues outside hospital doors was chilling. The world became a macabre place where people died in hospitals without any relative to hold their hands or comfort them, and then were buried quickly without any formal funerals due to mandatory social distancing. The inability of families to grieve for their loved ones added another poignant layer of sadness and distress to the survivors who were unable to bid their loved ones goodbye. This was a jarring example of adding insult to injury.
With the protraction of the exceptional changes imposed by the pandemic, the acute stress reaction transmuted into posttraumatic stress disorder (PTSD) on a wide scale. Millions of previously healthy individuals began to succumb to the symptoms of PTSD (irritability, hypervigilance, intrusive thoughts, avoidance, insomnia, and bad dreams). The heaviest burden was inflicted on our patients, across all ages, with preexisting psychiatric conditions, who comprise approximately 25% of the population per the classic Epidemiological Catchment Area (ECA) study.24 These vulnerable patients, whom we see in our clinics and hospitals every day, had a significant exacerbation of their psychopathology, including anxiety, depression, psychosis, binge eating disorder, obsessive-compulsive disorder, alcohol and substance use disorders, child abuse, and intimate partner violence.25,26 The saving grace was the rapid adoption of telepsychiatry, which our psychiatric patients rapidly accepted. Many of them found it more convenient than dressing and driving and parking at the clinic. It also enabled psychiatrists to obtain useful collateral information from family members or partners.
If something good comes from this catastrophic social stress that emotionally hobbled the entire population, it would be the dilution of the stigma of mental illness because everyone has become more empathic due to their personal experience. Optimistically, this may also help expedite true health care parity for psychiatric brain disorders. And perhaps the government may see the need to train more psychiatrists and fund a higher number of residency stipends to all training programs.
Quo vadis COVID-19?
So, looking through the dense fog of the pandemic fatigue, what will 2021 bring us? Will waves of COVID-19 lead to pandemic exhaustion? Will the frayed public mental health care system be able to handle the surge of frayed nerves? Will social distancing intensify the widespread emotional disquietude? Will the children be able to manifest resilience and avoid disabling psychiatric disorders? Will the survivors of COVID-19 infections suffer from post–COVD-19 neuropsychiatric and other medical sequelae? Will efficacious therapies and vaccines emerge to blunt the spread of the virus? Will we all be able to gather in stadiums and arenas to enjoy sporting events, shows, and concerts? Will eating at our favorite restaurants become routine again? Will engaged couples be able to organize well-attended weddings and receptions? Will airplanes and hotels be fully booked again? Importantly, will all children and college students be able to resume their education in person and socialize ad lib? Will we be able to shed our masks and hug each other hello and goodbye? Will scientific journals and social media cover a wide array of topics again as before? Will the number of deaths dwindle to zero, and will we return to worrying mainly about the usual seasonal flu? Will everyone be able to leave home and go to work again?
I hope that the thick dust of this 2020 viral asteroid will settle in 2021, and that “normalcy” is eventually restored to our lives, allowing us to deal with other ongoing stresses such as social unrest and political hyperpartisanship.
Finally, 2020 is coming to an end, but the agony its viral pandemic inflicted on the entire world population will continue for a long time. And much as we would like to forget its damaging effects, it will surely be etched into our brains for the rest of our lives. The children who suffered the pain of the coronavirus disease 2019 (COVID-19) pandemic will endure its emotional scars for the rest of the 21st century.
Reading about the plagues of the past doesn’t come close to experiencing it and suffering through it. COVID-19 will continue to have ripple effects on every aspect of life on this planet, on individuals and on societies all over the world, especially on the biopsychosocial well-being of billions of humans around the globe.
Unprecedented disruptions
Think of the unprecedented disruptions inflicted by the trauma of the COVID-19 pandemic on our neural circuits. One of the wonders of the human brain is its continuous remodeling due to experiential neuroplasticity, and the formation of dendritic spines that immediately encode the memories of every experience. The turmoil of 2020 and its virulent pandemic will be forever etched into our collective brains, especially in our hippocampi and amygdalae. The impact on the developing brains of our children and grandchildren could be profound and may induce epigenetic changes that trigger psychopathology in the future.1,2
As with the dinosaurs, the 2020 pandemic is like a “viral asteroid” that left devastation on our social fabric and psychological well-being in its wake. We now have deep empathy with our 1918 ancestors and their tribulations, although so far, in the United States the proportion of people infected with COVID-19 (3% as of mid-November 20203) is dwarfed by the proportion infected with the influenza virus a century ago (30%). As of mid-November 2020, the number of global COVID-19 deaths (1.3 million3) was a tiny fraction of the 1918 influenza pandemic deaths (50 million worldwide and 675,000 in the United States4). Amazingly, researchers did not even know whether the killer germ was a virus or a bacterium until 1930, and it then took another 75 years to decode the genome of the influenza virus in 2005. In contrast, it took only a few short weeks to decode the genome of the virus that causes COVID-19 (severe acute respiratory syndrome-related coronavirus 2), and to begin developing multiple vaccines “at warp speed.” No vaccine or therapies were ever developed for victims of the 1918 pandemic.
An abundance of articles has been published about the pandemic since it ambushed us early in 2020, including many in
Most psychiatrists are familiar with the Holmes and Rahe Stress Scale,22 which contains 43 life events that cumulatively can progressively increase the odds of physical illness. It is likely that most of the world’s population will score very high on the Holmes and Rahe Stress Scale, which would predict an increased risk of medical illness, even after the pandemic subsides.
Exacerbating the situation is that hospitals and clinics had to shut down most of their operations to focus their resources on treating patients with COVID-19 in ICUs. This halted all routine screenings for cancer and heart, kidney, liver, lung, or brain diseases. In addition, diagnostic or therapeutic procedures such as endoscopies, colonoscopies, angiograms, or biopsies abruptly stopped, resulting in a surge of non–COVID-19 medical disorders and mortality as reported in several articles across many specialties.23 Going forward, in addition to COVID-19 morbidity and mortality, there is a significant likelihood of an increase in myriad medical disorders. The COVID-19 pandemic is obviously inflicting both direct and indirect casualties as it stretches into the next year and perhaps longer. The only hope for the community of nations is the rapid arrival of evidence-based treatments and vaccine(s).
Continue to: A progression of relentless stress
A progression of relentless stress
At the core of this pandemic is relentless stress. When it began in early 2020, the pandemic ignited an acute stress reaction due to the fear of death and the oddness of being isolated at home. Aggravating the acute stress was the realization that life as we knew it suddenly disappeared and all business or social activities had come to a screeching halt. It was almost surreal when streets usually bustling with human activity (such as Times Square in New York or Michigan Avenue in Chicago) became completely deserted and eerily silent. In addition, more stress was generated from watching television or scrolling through social media and being inundated with morbid and frightening news and updates about the number of individuals who became infected or died, and the official projections of tens of thousands or even hundreds of thousands of fatalities. Further intensifying the stress was hearing that there was a shortage of personal protective equipment (even masks), a lack of ventilators, and the absence of any medications to fight the overwhelming viral infection. Especially stressed were the front-line physicians and nurses, who heroically transcended their fears to save their patients’ lives. The sight of refrigerated trucks serving as temporary morgues outside hospital doors was chilling. The world became a macabre place where people died in hospitals without any relative to hold their hands or comfort them, and then were buried quickly without any formal funerals due to mandatory social distancing. The inability of families to grieve for their loved ones added another poignant layer of sadness and distress to the survivors who were unable to bid their loved ones goodbye. This was a jarring example of adding insult to injury.
With the protraction of the exceptional changes imposed by the pandemic, the acute stress reaction transmuted into posttraumatic stress disorder (PTSD) on a wide scale. Millions of previously healthy individuals began to succumb to the symptoms of PTSD (irritability, hypervigilance, intrusive thoughts, avoidance, insomnia, and bad dreams). The heaviest burden was inflicted on our patients, across all ages, with preexisting psychiatric conditions, who comprise approximately 25% of the population per the classic Epidemiological Catchment Area (ECA) study.24 These vulnerable patients, whom we see in our clinics and hospitals every day, had a significant exacerbation of their psychopathology, including anxiety, depression, psychosis, binge eating disorder, obsessive-compulsive disorder, alcohol and substance use disorders, child abuse, and intimate partner violence.25,26 The saving grace was the rapid adoption of telepsychiatry, which our psychiatric patients rapidly accepted. Many of them found it more convenient than dressing and driving and parking at the clinic. It also enabled psychiatrists to obtain useful collateral information from family members or partners.
If something good comes from this catastrophic social stress that emotionally hobbled the entire population, it would be the dilution of the stigma of mental illness because everyone has become more empathic due to their personal experience. Optimistically, this may also help expedite true health care parity for psychiatric brain disorders. And perhaps the government may see the need to train more psychiatrists and fund a higher number of residency stipends to all training programs.
Quo vadis COVID-19?
So, looking through the dense fog of the pandemic fatigue, what will 2021 bring us? Will waves of COVID-19 lead to pandemic exhaustion? Will the frayed public mental health care system be able to handle the surge of frayed nerves? Will social distancing intensify the widespread emotional disquietude? Will the children be able to manifest resilience and avoid disabling psychiatric disorders? Will the survivors of COVID-19 infections suffer from post–COVD-19 neuropsychiatric and other medical sequelae? Will efficacious therapies and vaccines emerge to blunt the spread of the virus? Will we all be able to gather in stadiums and arenas to enjoy sporting events, shows, and concerts? Will eating at our favorite restaurants become routine again? Will engaged couples be able to organize well-attended weddings and receptions? Will airplanes and hotels be fully booked again? Importantly, will all children and college students be able to resume their education in person and socialize ad lib? Will we be able to shed our masks and hug each other hello and goodbye? Will scientific journals and social media cover a wide array of topics again as before? Will the number of deaths dwindle to zero, and will we return to worrying mainly about the usual seasonal flu? Will everyone be able to leave home and go to work again?
I hope that the thick dust of this 2020 viral asteroid will settle in 2021, and that “normalcy” is eventually restored to our lives, allowing us to deal with other ongoing stresses such as social unrest and political hyperpartisanship.
1. Baumeister D, Akhtar R, Ciufolini S, et al. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Mol Psychiatry. 2016;21(5):642-649.
2. Zatti C, Rosa V, Barros A, et al. Childhood trauma and suicide attempt: a meta-analysis of longitudinal studies from the last decade. Psychiatry Res. 2017;256:353-358.
3. Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/. Accessed November 11, 2020.
4. Centers for Disease Control and Prevention. 1918 Pandemic. https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html. Accessed November 4, 2020.
5. Chepke C. Drive-up pharmacotherapy during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):29-30.
6. Sharma RA, Maheshwari S, Bronsther R. COVID-19 in the era of loneliness. Current Psychiatry. 2020;19(5):31-33.
7. Joshi KG. Taking care of ourselves during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):46-47.
8. Frank B, Peterson T, Gupta S, et al. Telepsychiatry: what you need to know. Current Psychiatry. 2020;19(6):16-23.
9. Chahal K. Neuropsychiatric manifestations of COVID-19. Current Psychiatry. 2020;19(6):31-33.
10. Arbuck D. Changes in patient behavior during COVID-19: what I’ve observed. Current Psychiatry. 2020;19(6):46-47.
11. Joshi KG. Telepsychiatry during COVID-19: understanding the rules. Current Psychiatry. 2020;19(6):e12-e14.
12. Komrad MS. Medical ethics in the time of COVID-19. Current Psychiatry. 2020;19(7):29-32,46.
13. Brooks V. COVID-19’s effects on emergency psychiatry. Current Psychiatry. 2020;19(7):33-36,38-39.
14. Desarbo JR, DeSarbo L. Anorexia nervosa and COVID-19. Current Psychiatry. 2020;19(8):23-28.
15. Freudenreich O, Kontos N, Querques J. COVID-19 and patients with serious mental illness. Current Psychiatry. 2020;19(9):24-27,33-39.
16. Ryznar E. Evaluating patients’ decision-making capacity during COVID-19. Current Psychiatry. 2020;19(10):34-40.
17. Saeed SA, Hebishi K. The psychiatric consequences of COVID-19: 8 studies. Current Psychiatry. 2020;19(11):22-24,28-30,32-35.
18. Lodhi S, Marett C. Using seclusion to prevent COVID-19 transmission on inpatient psychiatry units. Current Psychiatry. 2020;19(11):37-41,53.
19. Nasrallah HA. COVID-19 and the precipitous dismantlement of societal norms. Current Psychiatry. 2020;19(7):12-14,16-17.
20. Nasrallah HA. The cataclysmic COVID-19 pandemic: THIS CHANGES EVERYTHING! Current Psychiatry. 2020;19(5):7-8,16.
21. Nasrallah HA. During a viral pandemic, anxiety is endemic: the psychiatric aspects of COVID-19. Current Psychiatry. 2020;19(4):e3-e5.
22. Holmes TH, Rahe RH. The social readjustment rating scale. Journal of Psychosomatic Research. 1967;11(2):213-218.
23. Berkwits M, Flanagin A, Bauchner H, et al. The COVID-19 pandemic and the JAMA Network. JAMA. 2020;324(12):1159-1160.
24. Robins LN, Regier DA, eds. Psychiatric disorders in America. The Epidemiologic Catchment Area study. New York, NY: The Free Press; 1991.
25. Meninger KA. Psychosis associated with influenza. I. General data: statistical analysis. JAMA. 1919;72(4):235-241.
26. Simon NM, Saxe GN, Marmar CR. Mental health disorders related to COVID-19-related deaths. JAMA. 2020;324(15):1493-1494.
1. Baumeister D, Akhtar R, Ciufolini S, et al. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Mol Psychiatry. 2016;21(5):642-649.
2. Zatti C, Rosa V, Barros A, et al. Childhood trauma and suicide attempt: a meta-analysis of longitudinal studies from the last decade. Psychiatry Res. 2017;256:353-358.
3. Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/. Accessed November 11, 2020.
4. Centers for Disease Control and Prevention. 1918 Pandemic. https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html. Accessed November 4, 2020.
5. Chepke C. Drive-up pharmacotherapy during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):29-30.
6. Sharma RA, Maheshwari S, Bronsther R. COVID-19 in the era of loneliness. Current Psychiatry. 2020;19(5):31-33.
7. Joshi KG. Taking care of ourselves during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):46-47.
8. Frank B, Peterson T, Gupta S, et al. Telepsychiatry: what you need to know. Current Psychiatry. 2020;19(6):16-23.
9. Chahal K. Neuropsychiatric manifestations of COVID-19. Current Psychiatry. 2020;19(6):31-33.
10. Arbuck D. Changes in patient behavior during COVID-19: what I’ve observed. Current Psychiatry. 2020;19(6):46-47.
11. Joshi KG. Telepsychiatry during COVID-19: understanding the rules. Current Psychiatry. 2020;19(6):e12-e14.
12. Komrad MS. Medical ethics in the time of COVID-19. Current Psychiatry. 2020;19(7):29-32,46.
13. Brooks V. COVID-19’s effects on emergency psychiatry. Current Psychiatry. 2020;19(7):33-36,38-39.
14. Desarbo JR, DeSarbo L. Anorexia nervosa and COVID-19. Current Psychiatry. 2020;19(8):23-28.
15. Freudenreich O, Kontos N, Querques J. COVID-19 and patients with serious mental illness. Current Psychiatry. 2020;19(9):24-27,33-39.
16. Ryznar E. Evaluating patients’ decision-making capacity during COVID-19. Current Psychiatry. 2020;19(10):34-40.
17. Saeed SA, Hebishi K. The psychiatric consequences of COVID-19: 8 studies. Current Psychiatry. 2020;19(11):22-24,28-30,32-35.
18. Lodhi S, Marett C. Using seclusion to prevent COVID-19 transmission on inpatient psychiatry units. Current Psychiatry. 2020;19(11):37-41,53.
19. Nasrallah HA. COVID-19 and the precipitous dismantlement of societal norms. Current Psychiatry. 2020;19(7):12-14,16-17.
20. Nasrallah HA. The cataclysmic COVID-19 pandemic: THIS CHANGES EVERYTHING! Current Psychiatry. 2020;19(5):7-8,16.
21. Nasrallah HA. During a viral pandemic, anxiety is endemic: the psychiatric aspects of COVID-19. Current Psychiatry. 2020;19(4):e3-e5.
22. Holmes TH, Rahe RH. The social readjustment rating scale. Journal of Psychosomatic Research. 1967;11(2):213-218.
23. Berkwits M, Flanagin A, Bauchner H, et al. The COVID-19 pandemic and the JAMA Network. JAMA. 2020;324(12):1159-1160.
24. Robins LN, Regier DA, eds. Psychiatric disorders in America. The Epidemiologic Catchment Area study. New York, NY: The Free Press; 1991.
25. Meninger KA. Psychosis associated with influenza. I. General data: statistical analysis. JAMA. 1919;72(4):235-241.
26. Simon NM, Saxe GN, Marmar CR. Mental health disorders related to COVID-19-related deaths. JAMA. 2020;324(15):1493-1494.
Unmet needs in the pharmacotherapy of psychiatric brain syndromes
Let’s face it: The greatest unmet need in psychiatry is discovering a treatment for the infamous syndrome of toxic political extremism. Its ugly symptoms include blind hatred, visceral malice, bigotry, vandalism, hypocrisy, racism, hubris, intransigence, narcissism, demagoguery, mutual contempt, and intense schadenfreude.
This corrosive affliction has engulfed and polluted our society, and compromised our well-being and quality of life. Treating this malignant syndrome is beyond the reach of psychopharmacology!
Thus, we psychiatrists should focus on the mood, psychotic, anxiety, and addiction syndromes that we encounter daily in our hospitals, clinics, and private offices. They affect tens of millions of patients. We currently have many psychotropic medications for these conditions. When combined with psychotherapy, the resulting synergy can be magical and immensely gratifying. However, some of those agents have limited efficacy due to the extensive heterogeneity of syndromes such as schizophrenia or depression, which are often confounded with comorbidities. A perfect balance between efficacy, tolerability, and safety are often hard to come by in pharmacotherapy.
The most glaring psychopharmacologic unmet need is that 80% of DSM disorders still do not have a single FDA-approved (evidence-based) medication.1 It will take decades, hundreds of billions of dollars, and the motivation of the often-maligned pharmaceutical industry (indispensable, because they are the only entity with the large R&D infrastructure to develop medications for psychiatry). Both academic and clinical psychiatrists must advise pharmaceutical companies about the unmet needs in our field and urge them to develop novel pharmacotherapies to address the gaps in the clinical care of psychiatric patients.
An inventory of unmet needs
With that in mind, here is a list of unmet needs I have been thinking about lately, and hoping that they will be resolved to help our patients achieve better clinical and functional outcomes.
Rapid-onset antipsychotics. The discovery that ketamine can rapidly convert refractory patients who are chronically depressed or suicidal to normal mood within a few hours shattered the dogma that weeks and months are needed for severe depression to improve, let alone achieve full remission. There is a similar dogma about psychosis requiring a protracted duration of antipsychotic treatment to attain significant impact. A rapid-acting antipsychotic agent would represent a major advance in psychiatry and its pharmaco-economic benefits would be substantial, given the high cost of inpatient hospitalization. Just as neurobiologic research guided the discovery of ketamine as a dramatic paradigm shift in treating depression, targeted research, especially focusing on glutamate pathways, may help identify a rapid-onset agent, whether oral, intranasal, IV, or even (why not) intrathecal. Research is known to enhance serendipity, which has been kind to psychiatry and has led to the discovery of several pharmacologic therapies in psychiatry, such as chlorpromazine, monoamine oxidase inhibitor antidepressants, and lithium.
Long-acting antidepressants and anxiolytics. This can be regarded as low-hanging fruit. Several technologies have been developed for long-acting formulations, yet they have been exploited mainly for antipsychotic medications. Some of these technologies can be employed to convert commonly used antidepressants (such as selective serotonin reuptake inhibitors) into long-acting antidepressants that can also reduce anxiety. Nonadherence among patients with depression is quite common, and relapses may lead to suicide attempts. The use of injectable, long-acting antidepressants can also reduce the incidence of overdoses because the patient will not have possession of potentially fatal pills.
Continue to: Long-acting mood stabilizers
Long-acting mood stabilizers. The rationale for long-acting mood stabilizers is the same as for long-acting antidepressants. Patients with bipolar disorder are known to stop taking their medications because they miss their “highs.” Some long-acting antipsychotics are approved for bipolar disorder, but these are often associated with adverse effects, such as metabolic dysregulation, extrapyramidal symptoms, and tardive dyskinesia. Mood stabilizers are essential for the bipolar spectrum.
A “real” treatment for alcohol use disorders that eliminates craving for alcohol. Alcoholism is associated with more than 100 medical complications and is one of the leading causes of disability in the world. It is frustrating that very few drug companies have focused on this widely prevalent brain disorder, which is also a common comorbid condition in many psychiatric syndromes.
Treatment-resistance pharmacotherapy solutions. All psychiatric syndromes are heterogeneous and contain ≥1 subgroups (biotypes) that fail to respond to what is considered the “standard” psychopharmacologic treatment (such as antipsychotics, antidepressants, mood stabilizers, or anti-obsessive medications). Technically, those so-called treatment-resistant subtypes need medications with a different mechanism of action. For example, clozapine for treatment-resistant schizophrenia and ketamine for treatment-resistant depression provide proof that treatment resistance is treatable but by a mechanism of action that is completely different from that of standard therapies, such as N-methyl-
Negative symptoms of schizophrenia cause significant functional disability and are well known to be a major unmet need. Some promising data are emerging on agents such as pimavanserin, cariprazine, and roluperidone, which is encouraging, but nothing is approved yet.
Cognitive deficits of schizophrenia, both neurocognition and social cognition, are another major unmet need that impair function in many patients. Many attempts to develop a pharmacologic treatment for these serious cognitive impairments have been made, but several candidates that initially appeared promising have bitten the dust. A focus on modulating the glutamate NMDA receptor may eventually lead to a breakthrough, and that may also help patients with bipolar disorder and major depressive disorder, both of whom also have cognitive deficits in several domains, albeit less severe than those experienced by patients with schizophrenia.
Continue to: Personality disorders
Personality disorders, especially borderline personality disorder, are very challenging to treat pharmacologically despite their prevalence and serious disruption to people’s lives. Hardly any FDA clinical trials have been conducted on any personality disorder. It is an unmet need that all psychiatrists would love to see addressed. But the mythical notion that personality disorders are untreatable may be an impediment in the pursuit of novel pharmacotherapy for borderline, narcissistic, antisocial, or schizotypal personality disorders, and other disorders. Heart attacks and religious conversion often change the baseline personality dramatically.
Childhood disorders. Apart from attention-deficit/hyperactivity disorder (ADHD), very few childhood psychiatric disorders have an FDA-approved medication. Why do drug companies avoid conducting controlled clinical trials in children age <10 who have autism, spectrum disorders, conduct disorder, oppositional defiant disorder, and other disorders? Effective pharmacotherapy for these children can be regarded as a desirable early intervention that may short-circuit their progression to serious adult psychopathology.
Parsimonious psychopharmacology for the treatment of trans-diagnostic psychiatric disorders. Recent research strongly suggests there is a strong overlap among psychiatric conditions, genetically, clinically, and biologically.2,3 For example, bipolar disorder is frequently accompanied by anxiety or substance use, patients with schizophrenia often experience anxiety, depression, or substance use, and ADHD has been found to share genes with autism.4,5
Eating disorders. There are no truly efficacious pharmacologic treatments for anorexia or bulimia nervosa. Research in this area is thin, and needs to be beefed up.
Sexual disorders. A huge unmet need exists for the pharmacotherapy of many sexual disorders that can have serious legal consequences (paraphilias) or quality-of-life repercussions (low sexual desire and orgasm disorders).
Continue to: A coordinated effort
A coordinated effort
It will take a massive collaboration among multiple stakeholders to launch the herculean process of addressing the unmet needs of all the above psychiatric disorders. This includes:
- the pharmaceutical industry (to provide the massive financial investment and R&D expertise)
- the federal government (to provide incentives)
- the FDA (to allow novel clinical trial designs)
- academic psychiatrists (to conduct research to discover the pathophysiology of psychiatric diseases)
- clinical psychiatrists (to provide consultations and advise about the clinical gaps in current psychopharmacological treatments)
- psychiatric patients (who are needed to volunteer for large-scale clinical trials).
This will be a veritable “psychiatric Manhattan Project” to advance the treatment of numerous psychiatric illnesses. The greatest benefit of discovering cures for disabling mental disorders is the evaporation of the virulent stigma that continues to plague our patients.
As for the political extremism that has corroded our society, it may be beyond pharmacologic redemption. An antidote to the “kool aid” has not yet been invented…
1. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian J Psychiatr. 2009;2(1):29-36.
2. Nasrallah HA. Is there only 1 neurobiologic disorder, with different clinical expressions? Current Psychiatry. 2015;14(7):10-12.
3. Nasrallah HA. Pleiotropy of psychiatric disorders will reinvent DSM. Current Psychiatry. 2013;12(4):6-7.
4. Caspi A, Moffitt TE. All for one and one for all: mental disorders in one dimension. Am J Psychiatry. 2018;175(9):831-844.
5. Marshall M. Roots of mental illness. Nature. 2020;581:19-21.
Let’s face it: The greatest unmet need in psychiatry is discovering a treatment for the infamous syndrome of toxic political extremism. Its ugly symptoms include blind hatred, visceral malice, bigotry, vandalism, hypocrisy, racism, hubris, intransigence, narcissism, demagoguery, mutual contempt, and intense schadenfreude.
This corrosive affliction has engulfed and polluted our society, and compromised our well-being and quality of life. Treating this malignant syndrome is beyond the reach of psychopharmacology!
Thus, we psychiatrists should focus on the mood, psychotic, anxiety, and addiction syndromes that we encounter daily in our hospitals, clinics, and private offices. They affect tens of millions of patients. We currently have many psychotropic medications for these conditions. When combined with psychotherapy, the resulting synergy can be magical and immensely gratifying. However, some of those agents have limited efficacy due to the extensive heterogeneity of syndromes such as schizophrenia or depression, which are often confounded with comorbidities. A perfect balance between efficacy, tolerability, and safety are often hard to come by in pharmacotherapy.
The most glaring psychopharmacologic unmet need is that 80% of DSM disorders still do not have a single FDA-approved (evidence-based) medication.1 It will take decades, hundreds of billions of dollars, and the motivation of the often-maligned pharmaceutical industry (indispensable, because they are the only entity with the large R&D infrastructure to develop medications for psychiatry). Both academic and clinical psychiatrists must advise pharmaceutical companies about the unmet needs in our field and urge them to develop novel pharmacotherapies to address the gaps in the clinical care of psychiatric patients.
An inventory of unmet needs
With that in mind, here is a list of unmet needs I have been thinking about lately, and hoping that they will be resolved to help our patients achieve better clinical and functional outcomes.
Rapid-onset antipsychotics. The discovery that ketamine can rapidly convert refractory patients who are chronically depressed or suicidal to normal mood within a few hours shattered the dogma that weeks and months are needed for severe depression to improve, let alone achieve full remission. There is a similar dogma about psychosis requiring a protracted duration of antipsychotic treatment to attain significant impact. A rapid-acting antipsychotic agent would represent a major advance in psychiatry and its pharmaco-economic benefits would be substantial, given the high cost of inpatient hospitalization. Just as neurobiologic research guided the discovery of ketamine as a dramatic paradigm shift in treating depression, targeted research, especially focusing on glutamate pathways, may help identify a rapid-onset agent, whether oral, intranasal, IV, or even (why not) intrathecal. Research is known to enhance serendipity, which has been kind to psychiatry and has led to the discovery of several pharmacologic therapies in psychiatry, such as chlorpromazine, monoamine oxidase inhibitor antidepressants, and lithium.
Long-acting antidepressants and anxiolytics. This can be regarded as low-hanging fruit. Several technologies have been developed for long-acting formulations, yet they have been exploited mainly for antipsychotic medications. Some of these technologies can be employed to convert commonly used antidepressants (such as selective serotonin reuptake inhibitors) into long-acting antidepressants that can also reduce anxiety. Nonadherence among patients with depression is quite common, and relapses may lead to suicide attempts. The use of injectable, long-acting antidepressants can also reduce the incidence of overdoses because the patient will not have possession of potentially fatal pills.
Continue to: Long-acting mood stabilizers
Long-acting mood stabilizers. The rationale for long-acting mood stabilizers is the same as for long-acting antidepressants. Patients with bipolar disorder are known to stop taking their medications because they miss their “highs.” Some long-acting antipsychotics are approved for bipolar disorder, but these are often associated with adverse effects, such as metabolic dysregulation, extrapyramidal symptoms, and tardive dyskinesia. Mood stabilizers are essential for the bipolar spectrum.
A “real” treatment for alcohol use disorders that eliminates craving for alcohol. Alcoholism is associated with more than 100 medical complications and is one of the leading causes of disability in the world. It is frustrating that very few drug companies have focused on this widely prevalent brain disorder, which is also a common comorbid condition in many psychiatric syndromes.
Treatment-resistance pharmacotherapy solutions. All psychiatric syndromes are heterogeneous and contain ≥1 subgroups (biotypes) that fail to respond to what is considered the “standard” psychopharmacologic treatment (such as antipsychotics, antidepressants, mood stabilizers, or anti-obsessive medications). Technically, those so-called treatment-resistant subtypes need medications with a different mechanism of action. For example, clozapine for treatment-resistant schizophrenia and ketamine for treatment-resistant depression provide proof that treatment resistance is treatable but by a mechanism of action that is completely different from that of standard therapies, such as N-methyl-
Negative symptoms of schizophrenia cause significant functional disability and are well known to be a major unmet need. Some promising data are emerging on agents such as pimavanserin, cariprazine, and roluperidone, which is encouraging, but nothing is approved yet.
Cognitive deficits of schizophrenia, both neurocognition and social cognition, are another major unmet need that impair function in many patients. Many attempts to develop a pharmacologic treatment for these serious cognitive impairments have been made, but several candidates that initially appeared promising have bitten the dust. A focus on modulating the glutamate NMDA receptor may eventually lead to a breakthrough, and that may also help patients with bipolar disorder and major depressive disorder, both of whom also have cognitive deficits in several domains, albeit less severe than those experienced by patients with schizophrenia.
Continue to: Personality disorders
Personality disorders, especially borderline personality disorder, are very challenging to treat pharmacologically despite their prevalence and serious disruption to people’s lives. Hardly any FDA clinical trials have been conducted on any personality disorder. It is an unmet need that all psychiatrists would love to see addressed. But the mythical notion that personality disorders are untreatable may be an impediment in the pursuit of novel pharmacotherapy for borderline, narcissistic, antisocial, or schizotypal personality disorders, and other disorders. Heart attacks and religious conversion often change the baseline personality dramatically.
Childhood disorders. Apart from attention-deficit/hyperactivity disorder (ADHD), very few childhood psychiatric disorders have an FDA-approved medication. Why do drug companies avoid conducting controlled clinical trials in children age <10 who have autism, spectrum disorders, conduct disorder, oppositional defiant disorder, and other disorders? Effective pharmacotherapy for these children can be regarded as a desirable early intervention that may short-circuit their progression to serious adult psychopathology.
Parsimonious psychopharmacology for the treatment of trans-diagnostic psychiatric disorders. Recent research strongly suggests there is a strong overlap among psychiatric conditions, genetically, clinically, and biologically.2,3 For example, bipolar disorder is frequently accompanied by anxiety or substance use, patients with schizophrenia often experience anxiety, depression, or substance use, and ADHD has been found to share genes with autism.4,5
Eating disorders. There are no truly efficacious pharmacologic treatments for anorexia or bulimia nervosa. Research in this area is thin, and needs to be beefed up.
Sexual disorders. A huge unmet need exists for the pharmacotherapy of many sexual disorders that can have serious legal consequences (paraphilias) or quality-of-life repercussions (low sexual desire and orgasm disorders).
Continue to: A coordinated effort
A coordinated effort
It will take a massive collaboration among multiple stakeholders to launch the herculean process of addressing the unmet needs of all the above psychiatric disorders. This includes:
- the pharmaceutical industry (to provide the massive financial investment and R&D expertise)
- the federal government (to provide incentives)
- the FDA (to allow novel clinical trial designs)
- academic psychiatrists (to conduct research to discover the pathophysiology of psychiatric diseases)
- clinical psychiatrists (to provide consultations and advise about the clinical gaps in current psychopharmacological treatments)
- psychiatric patients (who are needed to volunteer for large-scale clinical trials).
This will be a veritable “psychiatric Manhattan Project” to advance the treatment of numerous psychiatric illnesses. The greatest benefit of discovering cures for disabling mental disorders is the evaporation of the virulent stigma that continues to plague our patients.
As for the political extremism that has corroded our society, it may be beyond pharmacologic redemption. An antidote to the “kool aid” has not yet been invented…
Let’s face it: The greatest unmet need in psychiatry is discovering a treatment for the infamous syndrome of toxic political extremism. Its ugly symptoms include blind hatred, visceral malice, bigotry, vandalism, hypocrisy, racism, hubris, intransigence, narcissism, demagoguery, mutual contempt, and intense schadenfreude.
This corrosive affliction has engulfed and polluted our society, and compromised our well-being and quality of life. Treating this malignant syndrome is beyond the reach of psychopharmacology!
Thus, we psychiatrists should focus on the mood, psychotic, anxiety, and addiction syndromes that we encounter daily in our hospitals, clinics, and private offices. They affect tens of millions of patients. We currently have many psychotropic medications for these conditions. When combined with psychotherapy, the resulting synergy can be magical and immensely gratifying. However, some of those agents have limited efficacy due to the extensive heterogeneity of syndromes such as schizophrenia or depression, which are often confounded with comorbidities. A perfect balance between efficacy, tolerability, and safety are often hard to come by in pharmacotherapy.
The most glaring psychopharmacologic unmet need is that 80% of DSM disorders still do not have a single FDA-approved (evidence-based) medication.1 It will take decades, hundreds of billions of dollars, and the motivation of the often-maligned pharmaceutical industry (indispensable, because they are the only entity with the large R&D infrastructure to develop medications for psychiatry). Both academic and clinical psychiatrists must advise pharmaceutical companies about the unmet needs in our field and urge them to develop novel pharmacotherapies to address the gaps in the clinical care of psychiatric patients.
An inventory of unmet needs
With that in mind, here is a list of unmet needs I have been thinking about lately, and hoping that they will be resolved to help our patients achieve better clinical and functional outcomes.
Rapid-onset antipsychotics. The discovery that ketamine can rapidly convert refractory patients who are chronically depressed or suicidal to normal mood within a few hours shattered the dogma that weeks and months are needed for severe depression to improve, let alone achieve full remission. There is a similar dogma about psychosis requiring a protracted duration of antipsychotic treatment to attain significant impact. A rapid-acting antipsychotic agent would represent a major advance in psychiatry and its pharmaco-economic benefits would be substantial, given the high cost of inpatient hospitalization. Just as neurobiologic research guided the discovery of ketamine as a dramatic paradigm shift in treating depression, targeted research, especially focusing on glutamate pathways, may help identify a rapid-onset agent, whether oral, intranasal, IV, or even (why not) intrathecal. Research is known to enhance serendipity, which has been kind to psychiatry and has led to the discovery of several pharmacologic therapies in psychiatry, such as chlorpromazine, monoamine oxidase inhibitor antidepressants, and lithium.
Long-acting antidepressants and anxiolytics. This can be regarded as low-hanging fruit. Several technologies have been developed for long-acting formulations, yet they have been exploited mainly for antipsychotic medications. Some of these technologies can be employed to convert commonly used antidepressants (such as selective serotonin reuptake inhibitors) into long-acting antidepressants that can also reduce anxiety. Nonadherence among patients with depression is quite common, and relapses may lead to suicide attempts. The use of injectable, long-acting antidepressants can also reduce the incidence of overdoses because the patient will not have possession of potentially fatal pills.
Continue to: Long-acting mood stabilizers
Long-acting mood stabilizers. The rationale for long-acting mood stabilizers is the same as for long-acting antidepressants. Patients with bipolar disorder are known to stop taking their medications because they miss their “highs.” Some long-acting antipsychotics are approved for bipolar disorder, but these are often associated with adverse effects, such as metabolic dysregulation, extrapyramidal symptoms, and tardive dyskinesia. Mood stabilizers are essential for the bipolar spectrum.
A “real” treatment for alcohol use disorders that eliminates craving for alcohol. Alcoholism is associated with more than 100 medical complications and is one of the leading causes of disability in the world. It is frustrating that very few drug companies have focused on this widely prevalent brain disorder, which is also a common comorbid condition in many psychiatric syndromes.
Treatment-resistance pharmacotherapy solutions. All psychiatric syndromes are heterogeneous and contain ≥1 subgroups (biotypes) that fail to respond to what is considered the “standard” psychopharmacologic treatment (such as antipsychotics, antidepressants, mood stabilizers, or anti-obsessive medications). Technically, those so-called treatment-resistant subtypes need medications with a different mechanism of action. For example, clozapine for treatment-resistant schizophrenia and ketamine for treatment-resistant depression provide proof that treatment resistance is treatable but by a mechanism of action that is completely different from that of standard therapies, such as N-methyl-
Negative symptoms of schizophrenia cause significant functional disability and are well known to be a major unmet need. Some promising data are emerging on agents such as pimavanserin, cariprazine, and roluperidone, which is encouraging, but nothing is approved yet.
Cognitive deficits of schizophrenia, both neurocognition and social cognition, are another major unmet need that impair function in many patients. Many attempts to develop a pharmacologic treatment for these serious cognitive impairments have been made, but several candidates that initially appeared promising have bitten the dust. A focus on modulating the glutamate NMDA receptor may eventually lead to a breakthrough, and that may also help patients with bipolar disorder and major depressive disorder, both of whom also have cognitive deficits in several domains, albeit less severe than those experienced by patients with schizophrenia.
Continue to: Personality disorders
Personality disorders, especially borderline personality disorder, are very challenging to treat pharmacologically despite their prevalence and serious disruption to people’s lives. Hardly any FDA clinical trials have been conducted on any personality disorder. It is an unmet need that all psychiatrists would love to see addressed. But the mythical notion that personality disorders are untreatable may be an impediment in the pursuit of novel pharmacotherapy for borderline, narcissistic, antisocial, or schizotypal personality disorders, and other disorders. Heart attacks and religious conversion often change the baseline personality dramatically.
Childhood disorders. Apart from attention-deficit/hyperactivity disorder (ADHD), very few childhood psychiatric disorders have an FDA-approved medication. Why do drug companies avoid conducting controlled clinical trials in children age <10 who have autism, spectrum disorders, conduct disorder, oppositional defiant disorder, and other disorders? Effective pharmacotherapy for these children can be regarded as a desirable early intervention that may short-circuit their progression to serious adult psychopathology.
Parsimonious psychopharmacology for the treatment of trans-diagnostic psychiatric disorders. Recent research strongly suggests there is a strong overlap among psychiatric conditions, genetically, clinically, and biologically.2,3 For example, bipolar disorder is frequently accompanied by anxiety or substance use, patients with schizophrenia often experience anxiety, depression, or substance use, and ADHD has been found to share genes with autism.4,5
Eating disorders. There are no truly efficacious pharmacologic treatments for anorexia or bulimia nervosa. Research in this area is thin, and needs to be beefed up.
Sexual disorders. A huge unmet need exists for the pharmacotherapy of many sexual disorders that can have serious legal consequences (paraphilias) or quality-of-life repercussions (low sexual desire and orgasm disorders).
Continue to: A coordinated effort
A coordinated effort
It will take a massive collaboration among multiple stakeholders to launch the herculean process of addressing the unmet needs of all the above psychiatric disorders. This includes:
- the pharmaceutical industry (to provide the massive financial investment and R&D expertise)
- the federal government (to provide incentives)
- the FDA (to allow novel clinical trial designs)
- academic psychiatrists (to conduct research to discover the pathophysiology of psychiatric diseases)
- clinical psychiatrists (to provide consultations and advise about the clinical gaps in current psychopharmacological treatments)
- psychiatric patients (who are needed to volunteer for large-scale clinical trials).
This will be a veritable “psychiatric Manhattan Project” to advance the treatment of numerous psychiatric illnesses. The greatest benefit of discovering cures for disabling mental disorders is the evaporation of the virulent stigma that continues to plague our patients.
As for the political extremism that has corroded our society, it may be beyond pharmacologic redemption. An antidote to the “kool aid” has not yet been invented…
1. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian J Psychiatr. 2009;2(1):29-36.
2. Nasrallah HA. Is there only 1 neurobiologic disorder, with different clinical expressions? Current Psychiatry. 2015;14(7):10-12.
3. Nasrallah HA. Pleiotropy of psychiatric disorders will reinvent DSM. Current Psychiatry. 2013;12(4):6-7.
4. Caspi A, Moffitt TE. All for one and one for all: mental disorders in one dimension. Am J Psychiatry. 2018;175(9):831-844.
5. Marshall M. Roots of mental illness. Nature. 2020;581:19-21.
1. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian J Psychiatr. 2009;2(1):29-36.
2. Nasrallah HA. Is there only 1 neurobiologic disorder, with different clinical expressions? Current Psychiatry. 2015;14(7):10-12.
3. Nasrallah HA. Pleiotropy of psychiatric disorders will reinvent DSM. Current Psychiatry. 2013;12(4):6-7.
4. Caspi A, Moffitt TE. All for one and one for all: mental disorders in one dimension. Am J Psychiatry. 2018;175(9):831-844.
5. Marshall M. Roots of mental illness. Nature. 2020;581:19-21.
Neuro-politics: Will you vote with your cortex or limbic system?
It’s election season again. Every 4 years, October becomes the purgatory month of politics. But this year, it’s even more complicated, being juxtaposed against a chaotic mosaic of a viral pandemic, economic travails, social upheaval, and exceptionally toxic political hyperpartisanship.
The widespread expectation is that citizens will vote for their party’s candidates, but there is now a body of evidence suggesting that our brains may be pre-wired to be liberal or conservative.
Enter neuro-politics. This discipline is younger than neuro-economics, neuro-law, neuro-ethics, neuro-marketing, neuro-art, neuro-culture, or neuro-esthetics. Neuro-politics focuses on the intersection of politics with neuroscience.1 However, there are many antecedents to neuro-politics reflected in the writings of Plato, Aristotle, Niccolò Machiavelli, John Locke, Baruch Spinoza, Henri Bergson, William James, and others.
Neuro-politics attempts to generate data to answer a variety of questions about political behavior, such as:
- Is political orientation associated with differences in certain brain regions?
- Are there reliable neural biomarkers of political orientation?
- Is political orientation modifiable, and if so, why are some individuals ferociously entrenched to one political dogma while others are able to untether themselves and adopt another political doctrine?
- What are the brain characteristics of “swing voters” who may align themselves with different parties in different election cycles?
- Is there a “religification” of politics among the ardent fanatics who regard the tenets of their political beliefs as “articles of faith?”
- Is the brain modified by certain attributes (such as educational level, age, sex, marital status, race, ethnicity, and religious affiliation) that translate to political decision-making?
- Can neuro-politics explain the sprouting of psychiatric symptoms such as obsessions, anxiety, irritability, anger, hatred, and conspiracy theories?
- Is political extremism driven by cortical structures, limbic structures, or both?
Politics and the brain
Here is a brief review of some studies that examined the relationship of political orientation or voting behavior with brain structure and function:
1. Roger Sperry, the 1981 Nobel Laureate (for his studies on split-brain patients) reported that in patients who underwent callosotomy, both cerebral hemispheres gave the same ratings of politicians when their photos were shown to each hemisphere separately.2
2. A functional magnetic resonance imaging (fMRI) study found that the faces of candidates activated participants’ ventromedial and anterior prefrontal cortices. Amygdala activation was associated with the intensity of the emotion.3
Continue to: A skin conductance...
3. A skin conductance study reported that politically liberal individuals had low reactivity to sudden noises and threatening stimuli, while conservative counterparts demonstrated high physiological reactions to noises and stimuli.4
4. Images of a losing candidate elicited greater activation on fMRI in the insula and ventral anterior cingulate compared to no activation by exposure to an image of the winning candidate.5
5. Another fMRI study found that “individualism” was associated with activation of the medial prefrontal cortex and temporo-parietal junction when participants listened to a set of political statements. On the other hand, “conservatism” activated the dorsolateral prefrontal cortex, while “radicalism” activated the ventral striatum and posterior cingulate.6
6. An EEG activity study of healthy individuals revealed desynchronization in the alpha band related to the politicians who lost simulated elections and were judged as “less trustworthy” when the participant watched their faces.7
7. A structural MRI study of young adults reported that liberalism was associated with increased gray matter volume in the anterior cingulate, while conservatism was associated with increased volume of the right amygdala. The authors replicated their findings and concluded there is a possible link between brain structure and psychological mechanisms that mediate political attitudes.8
Continue to: To examine the effect of...
8. To examine the effect of a “first impression” based on the physical appearance of candidates, researchers compared individuals with damage to the lateral orbitofrontal cortex (OFC) with a group that had frontal damage that spared the lateral OFC and another group of matched healthy volunteers. They used a simulated elections paradigm in which participants voted based solely on photographs of the candidates’ faces. Only the group with OFC damage was influenced by attractiveness, while those with an intact frontal lobe or non-OFC frontal damage relied on other data, such as competence.9 These researchers concluded that an intact OFC is necessary for political decision-making.
9. A study using cognitive tasks reported that liberals are more adept at dealing with novel information than conservatives.10
What part of your brain will you use?
Regardless of the data generated by the neuro-politics studies, the bottom line is: What part of your brain do you use when you cast your vote for an issue, a representative, a senator, or a president? Is it a purely intellectual decision (ie, cortical), or is it driven by visceral emotions (ie, limbic)? Do you believe that every single item in your party’s platform is right and virtuous, while every item in the other party’s platform is wrong and evil? Can you think of any redeeming feature of the candidate you hate or the party you despise?
One attribute that we psychiatrists possess by virtue of our training and clinical work is that we are able to transcend dichotomies and to perceive nuances and shades of gray about controversial issues. So I hope we employ the circuits of our brain where wisdom putatively resides11 and which may develop further (via neuroplasticity) with the conduct of psychotherapy.12 Those brain circuits include:
- prefrontal cortex (for emotional regulation, decision-making, and value relativism)
- lateral prefrontal cortex (to facilitate calculated, reason-based decision-making)
- medial prefrontal cortex (for emotional valence and pro-social attitudes and behaviors).
However, being human, it is quite likely that our amygdala may “seep through” and color our judgment and decisions. But let us try to cast a vote that is not only good for the country but also good for our patients, many of whom may not even be able to vote. Election season is a time to make a positive difference in our patients’ lives, not just ours. Let’s hope our brains exploit this unique opportunity.
1. Schreiber D. Neuropolitics: twenty years later. Politics Life Sci. 2017;36(2):114-131.
2. Sperry RW, Zaidel E, Zaidel D. Self recognition and social awareness in the deconnected minor hemisphere. Neuropsychologia. 1979;17(2):153-166.
3. Knutson KM, Wood JN, Spampinato MV, et al. Politics on the brain: an FMRI investigation. Soc Neurosci. 2006;1(1):25-40.
4. Oxley DR, Smith KB, Alford JR, et al. Political attitudes vary with physiological traits. Science. 2008;321(5896):1667-1670.
5. Spezio ML, Rangel A, Alvarez RM, et al. A neural basis for the effect of candidate appearance on election outcomes. Soc Cogn Affect Neurosci. 2008;3(4):344-352.
6. Zamboni G, Gozzi M, Krueger F, et al. Individualism, conservatism, and radicalism as criteria for processing political beliefs: a parametric fMRI study. Soc Neurosci. 2009;4(5):367-383.
7. Vecchiato G, Toppi J, Cincotti F, et al. Neuropolitics: EEG spectral maps related to a political vote based on the first impression of the candidate’s face. Conf Proc IEEE Eng Med Biol Soc. 2010;2010:2902-2905.
8. Kanai R, Feilden T, Firth C, et al. Political orientations are correlated with brain structure in young adults. Curr Biol. 2011;21(8):677-680.
9. Xia C, Stolle D, Gidengil E, et al. Lateral orbitofrontal cortex links social impressions to political choices. J Neurosci. 2015;35(22):8507-8514.
10. Bernabel RT, Oliveira A. Conservatism and liberalism predict performance in two nonideological cognitive tasks. Politics Life Sci. 2017;36(2):49-59.
11. Meeks TW, Jeste DV. Neurobiology of wisdom: a literature overview. Arch Gen Psychiatry. 2009;66(4):355-365.
12. Nasrallah HA. Does psychiatric practice make us wiser? Current Psychiatry. 2009;8(10):12,14.
It’s election season again. Every 4 years, October becomes the purgatory month of politics. But this year, it’s even more complicated, being juxtaposed against a chaotic mosaic of a viral pandemic, economic travails, social upheaval, and exceptionally toxic political hyperpartisanship.
The widespread expectation is that citizens will vote for their party’s candidates, but there is now a body of evidence suggesting that our brains may be pre-wired to be liberal or conservative.
Enter neuro-politics. This discipline is younger than neuro-economics, neuro-law, neuro-ethics, neuro-marketing, neuro-art, neuro-culture, or neuro-esthetics. Neuro-politics focuses on the intersection of politics with neuroscience.1 However, there are many antecedents to neuro-politics reflected in the writings of Plato, Aristotle, Niccolò Machiavelli, John Locke, Baruch Spinoza, Henri Bergson, William James, and others.
Neuro-politics attempts to generate data to answer a variety of questions about political behavior, such as:
- Is political orientation associated with differences in certain brain regions?
- Are there reliable neural biomarkers of political orientation?
- Is political orientation modifiable, and if so, why are some individuals ferociously entrenched to one political dogma while others are able to untether themselves and adopt another political doctrine?
- What are the brain characteristics of “swing voters” who may align themselves with different parties in different election cycles?
- Is there a “religification” of politics among the ardent fanatics who regard the tenets of their political beliefs as “articles of faith?”
- Is the brain modified by certain attributes (such as educational level, age, sex, marital status, race, ethnicity, and religious affiliation) that translate to political decision-making?
- Can neuro-politics explain the sprouting of psychiatric symptoms such as obsessions, anxiety, irritability, anger, hatred, and conspiracy theories?
- Is political extremism driven by cortical structures, limbic structures, or both?
Politics and the brain
Here is a brief review of some studies that examined the relationship of political orientation or voting behavior with brain structure and function:
1. Roger Sperry, the 1981 Nobel Laureate (for his studies on split-brain patients) reported that in patients who underwent callosotomy, both cerebral hemispheres gave the same ratings of politicians when their photos were shown to each hemisphere separately.2
2. A functional magnetic resonance imaging (fMRI) study found that the faces of candidates activated participants’ ventromedial and anterior prefrontal cortices. Amygdala activation was associated with the intensity of the emotion.3
Continue to: A skin conductance...
3. A skin conductance study reported that politically liberal individuals had low reactivity to sudden noises and threatening stimuli, while conservative counterparts demonstrated high physiological reactions to noises and stimuli.4
4. Images of a losing candidate elicited greater activation on fMRI in the insula and ventral anterior cingulate compared to no activation by exposure to an image of the winning candidate.5
5. Another fMRI study found that “individualism” was associated with activation of the medial prefrontal cortex and temporo-parietal junction when participants listened to a set of political statements. On the other hand, “conservatism” activated the dorsolateral prefrontal cortex, while “radicalism” activated the ventral striatum and posterior cingulate.6
6. An EEG activity study of healthy individuals revealed desynchronization in the alpha band related to the politicians who lost simulated elections and were judged as “less trustworthy” when the participant watched their faces.7
7. A structural MRI study of young adults reported that liberalism was associated with increased gray matter volume in the anterior cingulate, while conservatism was associated with increased volume of the right amygdala. The authors replicated their findings and concluded there is a possible link between brain structure and psychological mechanisms that mediate political attitudes.8
Continue to: To examine the effect of...
8. To examine the effect of a “first impression” based on the physical appearance of candidates, researchers compared individuals with damage to the lateral orbitofrontal cortex (OFC) with a group that had frontal damage that spared the lateral OFC and another group of matched healthy volunteers. They used a simulated elections paradigm in which participants voted based solely on photographs of the candidates’ faces. Only the group with OFC damage was influenced by attractiveness, while those with an intact frontal lobe or non-OFC frontal damage relied on other data, such as competence.9 These researchers concluded that an intact OFC is necessary for political decision-making.
9. A study using cognitive tasks reported that liberals are more adept at dealing with novel information than conservatives.10
What part of your brain will you use?
Regardless of the data generated by the neuro-politics studies, the bottom line is: What part of your brain do you use when you cast your vote for an issue, a representative, a senator, or a president? Is it a purely intellectual decision (ie, cortical), or is it driven by visceral emotions (ie, limbic)? Do you believe that every single item in your party’s platform is right and virtuous, while every item in the other party’s platform is wrong and evil? Can you think of any redeeming feature of the candidate you hate or the party you despise?
One attribute that we psychiatrists possess by virtue of our training and clinical work is that we are able to transcend dichotomies and to perceive nuances and shades of gray about controversial issues. So I hope we employ the circuits of our brain where wisdom putatively resides11 and which may develop further (via neuroplasticity) with the conduct of psychotherapy.12 Those brain circuits include:
- prefrontal cortex (for emotional regulation, decision-making, and value relativism)
- lateral prefrontal cortex (to facilitate calculated, reason-based decision-making)
- medial prefrontal cortex (for emotional valence and pro-social attitudes and behaviors).
However, being human, it is quite likely that our amygdala may “seep through” and color our judgment and decisions. But let us try to cast a vote that is not only good for the country but also good for our patients, many of whom may not even be able to vote. Election season is a time to make a positive difference in our patients’ lives, not just ours. Let’s hope our brains exploit this unique opportunity.
It’s election season again. Every 4 years, October becomes the purgatory month of politics. But this year, it’s even more complicated, being juxtaposed against a chaotic mosaic of a viral pandemic, economic travails, social upheaval, and exceptionally toxic political hyperpartisanship.
The widespread expectation is that citizens will vote for their party’s candidates, but there is now a body of evidence suggesting that our brains may be pre-wired to be liberal or conservative.
Enter neuro-politics. This discipline is younger than neuro-economics, neuro-law, neuro-ethics, neuro-marketing, neuro-art, neuro-culture, or neuro-esthetics. Neuro-politics focuses on the intersection of politics with neuroscience.1 However, there are many antecedents to neuro-politics reflected in the writings of Plato, Aristotle, Niccolò Machiavelli, John Locke, Baruch Spinoza, Henri Bergson, William James, and others.
Neuro-politics attempts to generate data to answer a variety of questions about political behavior, such as:
- Is political orientation associated with differences in certain brain regions?
- Are there reliable neural biomarkers of political orientation?
- Is political orientation modifiable, and if so, why are some individuals ferociously entrenched to one political dogma while others are able to untether themselves and adopt another political doctrine?
- What are the brain characteristics of “swing voters” who may align themselves with different parties in different election cycles?
- Is there a “religification” of politics among the ardent fanatics who regard the tenets of their political beliefs as “articles of faith?”
- Is the brain modified by certain attributes (such as educational level, age, sex, marital status, race, ethnicity, and religious affiliation) that translate to political decision-making?
- Can neuro-politics explain the sprouting of psychiatric symptoms such as obsessions, anxiety, irritability, anger, hatred, and conspiracy theories?
- Is political extremism driven by cortical structures, limbic structures, or both?
Politics and the brain
Here is a brief review of some studies that examined the relationship of political orientation or voting behavior with brain structure and function:
1. Roger Sperry, the 1981 Nobel Laureate (for his studies on split-brain patients) reported that in patients who underwent callosotomy, both cerebral hemispheres gave the same ratings of politicians when their photos were shown to each hemisphere separately.2
2. A functional magnetic resonance imaging (fMRI) study found that the faces of candidates activated participants’ ventromedial and anterior prefrontal cortices. Amygdala activation was associated with the intensity of the emotion.3
Continue to: A skin conductance...
3. A skin conductance study reported that politically liberal individuals had low reactivity to sudden noises and threatening stimuli, while conservative counterparts demonstrated high physiological reactions to noises and stimuli.4
4. Images of a losing candidate elicited greater activation on fMRI in the insula and ventral anterior cingulate compared to no activation by exposure to an image of the winning candidate.5
5. Another fMRI study found that “individualism” was associated with activation of the medial prefrontal cortex and temporo-parietal junction when participants listened to a set of political statements. On the other hand, “conservatism” activated the dorsolateral prefrontal cortex, while “radicalism” activated the ventral striatum and posterior cingulate.6
6. An EEG activity study of healthy individuals revealed desynchronization in the alpha band related to the politicians who lost simulated elections and were judged as “less trustworthy” when the participant watched their faces.7
7. A structural MRI study of young adults reported that liberalism was associated with increased gray matter volume in the anterior cingulate, while conservatism was associated with increased volume of the right amygdala. The authors replicated their findings and concluded there is a possible link between brain structure and psychological mechanisms that mediate political attitudes.8
Continue to: To examine the effect of...
8. To examine the effect of a “first impression” based on the physical appearance of candidates, researchers compared individuals with damage to the lateral orbitofrontal cortex (OFC) with a group that had frontal damage that spared the lateral OFC and another group of matched healthy volunteers. They used a simulated elections paradigm in which participants voted based solely on photographs of the candidates’ faces. Only the group with OFC damage was influenced by attractiveness, while those with an intact frontal lobe or non-OFC frontal damage relied on other data, such as competence.9 These researchers concluded that an intact OFC is necessary for political decision-making.
9. A study using cognitive tasks reported that liberals are more adept at dealing with novel information than conservatives.10
What part of your brain will you use?
Regardless of the data generated by the neuro-politics studies, the bottom line is: What part of your brain do you use when you cast your vote for an issue, a representative, a senator, or a president? Is it a purely intellectual decision (ie, cortical), or is it driven by visceral emotions (ie, limbic)? Do you believe that every single item in your party’s platform is right and virtuous, while every item in the other party’s platform is wrong and evil? Can you think of any redeeming feature of the candidate you hate or the party you despise?
One attribute that we psychiatrists possess by virtue of our training and clinical work is that we are able to transcend dichotomies and to perceive nuances and shades of gray about controversial issues. So I hope we employ the circuits of our brain where wisdom putatively resides11 and which may develop further (via neuroplasticity) with the conduct of psychotherapy.12 Those brain circuits include:
- prefrontal cortex (for emotional regulation, decision-making, and value relativism)
- lateral prefrontal cortex (to facilitate calculated, reason-based decision-making)
- medial prefrontal cortex (for emotional valence and pro-social attitudes and behaviors).
However, being human, it is quite likely that our amygdala may “seep through” and color our judgment and decisions. But let us try to cast a vote that is not only good for the country but also good for our patients, many of whom may not even be able to vote. Election season is a time to make a positive difference in our patients’ lives, not just ours. Let’s hope our brains exploit this unique opportunity.
1. Schreiber D. Neuropolitics: twenty years later. Politics Life Sci. 2017;36(2):114-131.
2. Sperry RW, Zaidel E, Zaidel D. Self recognition and social awareness in the deconnected minor hemisphere. Neuropsychologia. 1979;17(2):153-166.
3. Knutson KM, Wood JN, Spampinato MV, et al. Politics on the brain: an FMRI investigation. Soc Neurosci. 2006;1(1):25-40.
4. Oxley DR, Smith KB, Alford JR, et al. Political attitudes vary with physiological traits. Science. 2008;321(5896):1667-1670.
5. Spezio ML, Rangel A, Alvarez RM, et al. A neural basis for the effect of candidate appearance on election outcomes. Soc Cogn Affect Neurosci. 2008;3(4):344-352.
6. Zamboni G, Gozzi M, Krueger F, et al. Individualism, conservatism, and radicalism as criteria for processing political beliefs: a parametric fMRI study. Soc Neurosci. 2009;4(5):367-383.
7. Vecchiato G, Toppi J, Cincotti F, et al. Neuropolitics: EEG spectral maps related to a political vote based on the first impression of the candidate’s face. Conf Proc IEEE Eng Med Biol Soc. 2010;2010:2902-2905.
8. Kanai R, Feilden T, Firth C, et al. Political orientations are correlated with brain structure in young adults. Curr Biol. 2011;21(8):677-680.
9. Xia C, Stolle D, Gidengil E, et al. Lateral orbitofrontal cortex links social impressions to political choices. J Neurosci. 2015;35(22):8507-8514.
10. Bernabel RT, Oliveira A. Conservatism and liberalism predict performance in two nonideological cognitive tasks. Politics Life Sci. 2017;36(2):49-59.
11. Meeks TW, Jeste DV. Neurobiology of wisdom: a literature overview. Arch Gen Psychiatry. 2009;66(4):355-365.
12. Nasrallah HA. Does psychiatric practice make us wiser? Current Psychiatry. 2009;8(10):12,14.
1. Schreiber D. Neuropolitics: twenty years later. Politics Life Sci. 2017;36(2):114-131.
2. Sperry RW, Zaidel E, Zaidel D. Self recognition and social awareness in the deconnected minor hemisphere. Neuropsychologia. 1979;17(2):153-166.
3. Knutson KM, Wood JN, Spampinato MV, et al. Politics on the brain: an FMRI investigation. Soc Neurosci. 2006;1(1):25-40.
4. Oxley DR, Smith KB, Alford JR, et al. Political attitudes vary with physiological traits. Science. 2008;321(5896):1667-1670.
5. Spezio ML, Rangel A, Alvarez RM, et al. A neural basis for the effect of candidate appearance on election outcomes. Soc Cogn Affect Neurosci. 2008;3(4):344-352.
6. Zamboni G, Gozzi M, Krueger F, et al. Individualism, conservatism, and radicalism as criteria for processing political beliefs: a parametric fMRI study. Soc Neurosci. 2009;4(5):367-383.
7. Vecchiato G, Toppi J, Cincotti F, et al. Neuropolitics: EEG spectral maps related to a political vote based on the first impression of the candidate’s face. Conf Proc IEEE Eng Med Biol Soc. 2010;2010:2902-2905.
8. Kanai R, Feilden T, Firth C, et al. Political orientations are correlated with brain structure in young adults. Curr Biol. 2011;21(8):677-680.
9. Xia C, Stolle D, Gidengil E, et al. Lateral orbitofrontal cortex links social impressions to political choices. J Neurosci. 2015;35(22):8507-8514.
10. Bernabel RT, Oliveira A. Conservatism and liberalism predict performance in two nonideological cognitive tasks. Politics Life Sci. 2017;36(2):49-59.
11. Meeks TW, Jeste DV. Neurobiology of wisdom: a literature overview. Arch Gen Psychiatry. 2009;66(4):355-365.
12. Nasrallah HA. Does psychiatric practice make us wiser? Current Psychiatry. 2009;8(10):12,14.
Revamp the MOC
There are few things that psychiatrists have come to despise more than the American Board of Psychiatry and Neurology (ABPN) Maintenance of Certification (MOC) program. It has become a professional boondoggle for psychiatric practitioners.
The program needs an overhaul and simplification. There are better, more efficient, cost-effective ways to ensure psychiatric physicians’ ongoing clinical competence after they complete their residency training. Technological advances can also facilitate a more valid assessment of competence without having to jump through more and more hoops between recertifications every 10 years.
I passed the boards long before the MOC was created. For 20 years, I also served as a senior examiner for the oral boards, where clinical competency was rigorously assessed by direct observations of psychiatrists examining and establishing rapport with patients and formulating the data into a differential diagnosis, treatment plan, and prognosis. It is noteworthy that psychiatrists who sat for the oral boards had already passed a written exam that tested their cognitive knowledge. Yet approximately one-third of the candidates failed the live oral exam, which clearly implies that passing a written exam is necessary but not sufficient to establish clinical competence, which is the primary purpose of board certification. It was an unfortunate decision to discontinue the face-to-face oral board exam, which is so vital for psychiatry, and to replace it with a written exam and a barrage of time-consuming activities to document lifelong learning and self-assessment, but not genuine clinical competence. The MOC has been MOCkingly referred to as a major pain in the neck for practically all psychiatrists who were not grandfathered with lifetime certification, as was the case in the first 60 years of the ABPN.
Benefits of the patient-based oral exam
Let’s face it: Passing a patient-based oral exam was the ideal mechanism to establish that a psychiatric physician deserved to be a diplomate of the ABPN. During the oral exam, the candidate’s skills were observed from the minute he/she met the patient. The candidate was then observed as he/she systematically explored a wide range of past and current psychiatric symptoms; reviewed the patient’s developmental, medical, family, and social histories; and conducted a competent mental status exam while demonstrating an empathic stance, responding to the patient’s often subtle verbal and nonverbal cues, establishing rapport, and providing psychoeducation before concluding the interview. All these essential components of a psychiatric exam were observed in a compact 30-minute tour de force of clinical skills, communication, and cognitive acumen. This was followed by another 30 minutes of organizing and presenting the clinical data to 2 or 3 colleagues/examiners, in a coherent fashion, connecting all the dots, formulating the case, presenting a meaningful differential diagnosis, and suggesting a rational array of potential treatment options across the biopsychosocial continuum. To top it off, the candidate had to respond effectively, in an evidence-based manner, to a series of questions related to the disease state, its treatment, adverse effects, and prognosis.
It was a joy to watch many colleagues navigate this clinical examination with skill and competence, without crumbling under the pressure of the examiners’ scrutiny. There were some who passed with flying colors, and others who passed despite having a forgivable minor gap here and there because of their overall strong performance. Finally, there were those who stumbled in several components across data collection, doctor–patient interactions, synthesis of the clinical findings, or treatment recommendations. These candidates inevitably received a failing grade by a consensus of 3 examiners. That they failed to demonstrate clinical competence despite having passed the required written exams a year earlier proved that the true competency of a psychiatrist cannot be judged solely by passing a written test but requires a clinical examination of a live patient.
The oral exams represented an unimpeachable evaluation of clinical competence. The examiners often spoke of how they would feel confident and comfortable with referring a family member to those who successfully passed this rigorous, authentic exam on real patients. It was justifiable to give lifetime certification to those who passed the oral exam. Those permanently certified psychiatrists maintained their lifelong learning by having an unrestricted state medical license, which is contingent on acquiring 50 category 1 continuing medical education (CME) credits annually. Why not restore lifelong certification for those who pass both a written and oral exam, as long as they maintain a valid medical license?
According to the ABPN 2019 Annual Report,1 31,514 psychiatrists have received lifetime certification, of whom an estimated 9,547 were still clinically active in 2019. This is the “grandfathered” cohort of psychiatrists to which I belong. I was tested on neurologic patients, not just psychiatric patients, a tribute to the strong bridge that existed between these sister brain specialties. As of 2019, of the 33,277 psychiatrists who received a time-limited certification, 29,343 were still clinically active, an attrition rate of 12% over the past 25 years. This includes psychiatrists who found the MOC too onerous to complete, or are in private practice where MOC is not a vital requirement. However, these days most psychiatrists are obligated to be recertified because so many entities require it. This includes hiring institutions, government agencies (Medicare/Medicaid), health insurance companies, hospital medical staff for privileging and credentialing, and various regulatory boards, such as The Joint Commission, the Accreditation Council for Graduate Medical Education, and academic medical centers. Because most psychiatrists are involved with at least one of these entities, 29,343 have no choice but to perform all the requirements of the MOC, with its countless hours, numerous documentations, and many fees, to remain certified by the ABPN. Notably absent is an alternative mechanism for a certification process that is widely accepted by all agencies and institutions. Psychiatrists are actively seeking alternatives.
Continue to: The ABPN...
The ABPN, long regarded as an esteemed nonprofit organization, has been accused of being a monopoly. Some angry psychiatrists have filed a class action lawsuit to demand other board certification methods. Some have gone to the media to complain about the American Board of Medical Specialties (of which the ABPN is a member board), accusing both of unfair regulations or of raking in substantial profits to support excessively compensated executives. Perception often trumps reality, so no matter how vigorously the ABPN defends itself, its procedures, or its MOC requirements, its customers—psychiatric physicians—feel oppressed or exploited.
How the MOC can be improved
So what can be done to improve the MOC? The need for recertification is arguably necessary to document clinical competency over an approximately 40-year psychiatric career following residency. I conducted a brief survey of
Significant advances in remote communication technology should be harnessed by the ABPN (or the APA, if it decides to conduct its own board certification) to restore the old model at a fraction of the cost. The oral exams have been replaced by a written exam that is not an accurate reflection or documentation of clinical competence. The traditional oral exam (after passing a written exam) was a magnificent but costly feat of massive logistical complexity, with >1,000 candidates and examiners traveling to a city where the ABPN arranged for several hospitals to shut down their clinics for 2 full days to use their clinical offices for the oral exams. Multiple teams examined the candidates twice on the same day: once with a live patient, and again with a video of a real patient. The examiners filled out scoring cards after observing the candidates conduct the live interview or discussing the video. A consensus grade of pass or fail was documented. At the end of the 2 days, examiners and candidates boarded buses to the airport. It was a highly expensive process (exam fees + airfare + hotel + food). Twice a year, the examiners generously donated their time to the ABPN without compensation, as a token of love for and service to the profession.
That initial certification of a written exam, followed by an oral exam, validated the competence of a psychiatrist both cognitively and clinically. The lifetime certification was truly earned. The same model can now be replicated virtually via videoconferencing at a far lower cost to the ABPN, the candidates, and the examiners. The MOC 10-year recertification can be reduced to a written exam with clinical vignettes and an unrestricted license to practice medicine in any state, which implies that the psychiatrist has received the 50 CME annual credits to renew the license. The rest of the bells and whistles can be strongly recommended but not required. The cost in time and money to both the ABPN and the candidates can be significantly reduced, but more importantly, the clinical competence will be validated at baseline with virtual oral boards after passing the written exam (formerly labeled as part I, preceding the part II oral boards).
The traditional board certification model of the past should be resurrected via videoconferencing and offered as an option to the candidates who prefer it to the current MOC. The MOC can then be simplified to lifetime certification or to only a written exam with clinical vignettes every 10 years to ensure that psychiatrists continue to incorporate relevant clinical and treatment advances in their practice. The KISS principle (keep it simple, stupid) worked very well for many generations of psychiatrists in the past, and will work again going forward if offered as an option. Psychiatrists can then focus on treating patients instead of being burdened by the many time-consuming requirements and hoops of the current MOC.
1. American Board of Psychiatry and Neurology. 2019 Annual Report. https://www.abpn.com/wp-content/uploads/2020/05/ABPN_2019_Annual_Report.pdf. Accessed August 14, 2020.
There are few things that psychiatrists have come to despise more than the American Board of Psychiatry and Neurology (ABPN) Maintenance of Certification (MOC) program. It has become a professional boondoggle for psychiatric practitioners.
The program needs an overhaul and simplification. There are better, more efficient, cost-effective ways to ensure psychiatric physicians’ ongoing clinical competence after they complete their residency training. Technological advances can also facilitate a more valid assessment of competence without having to jump through more and more hoops between recertifications every 10 years.
I passed the boards long before the MOC was created. For 20 years, I also served as a senior examiner for the oral boards, where clinical competency was rigorously assessed by direct observations of psychiatrists examining and establishing rapport with patients and formulating the data into a differential diagnosis, treatment plan, and prognosis. It is noteworthy that psychiatrists who sat for the oral boards had already passed a written exam that tested their cognitive knowledge. Yet approximately one-third of the candidates failed the live oral exam, which clearly implies that passing a written exam is necessary but not sufficient to establish clinical competence, which is the primary purpose of board certification. It was an unfortunate decision to discontinue the face-to-face oral board exam, which is so vital for psychiatry, and to replace it with a written exam and a barrage of time-consuming activities to document lifelong learning and self-assessment, but not genuine clinical competence. The MOC has been MOCkingly referred to as a major pain in the neck for practically all psychiatrists who were not grandfathered with lifetime certification, as was the case in the first 60 years of the ABPN.
Benefits of the patient-based oral exam
Let’s face it: Passing a patient-based oral exam was the ideal mechanism to establish that a psychiatric physician deserved to be a diplomate of the ABPN. During the oral exam, the candidate’s skills were observed from the minute he/she met the patient. The candidate was then observed as he/she systematically explored a wide range of past and current psychiatric symptoms; reviewed the patient’s developmental, medical, family, and social histories; and conducted a competent mental status exam while demonstrating an empathic stance, responding to the patient’s often subtle verbal and nonverbal cues, establishing rapport, and providing psychoeducation before concluding the interview. All these essential components of a psychiatric exam were observed in a compact 30-minute tour de force of clinical skills, communication, and cognitive acumen. This was followed by another 30 minutes of organizing and presenting the clinical data to 2 or 3 colleagues/examiners, in a coherent fashion, connecting all the dots, formulating the case, presenting a meaningful differential diagnosis, and suggesting a rational array of potential treatment options across the biopsychosocial continuum. To top it off, the candidate had to respond effectively, in an evidence-based manner, to a series of questions related to the disease state, its treatment, adverse effects, and prognosis.
It was a joy to watch many colleagues navigate this clinical examination with skill and competence, without crumbling under the pressure of the examiners’ scrutiny. There were some who passed with flying colors, and others who passed despite having a forgivable minor gap here and there because of their overall strong performance. Finally, there were those who stumbled in several components across data collection, doctor–patient interactions, synthesis of the clinical findings, or treatment recommendations. These candidates inevitably received a failing grade by a consensus of 3 examiners. That they failed to demonstrate clinical competence despite having passed the required written exams a year earlier proved that the true competency of a psychiatrist cannot be judged solely by passing a written test but requires a clinical examination of a live patient.
The oral exams represented an unimpeachable evaluation of clinical competence. The examiners often spoke of how they would feel confident and comfortable with referring a family member to those who successfully passed this rigorous, authentic exam on real patients. It was justifiable to give lifetime certification to those who passed the oral exam. Those permanently certified psychiatrists maintained their lifelong learning by having an unrestricted state medical license, which is contingent on acquiring 50 category 1 continuing medical education (CME) credits annually. Why not restore lifelong certification for those who pass both a written and oral exam, as long as they maintain a valid medical license?
According to the ABPN 2019 Annual Report,1 31,514 psychiatrists have received lifetime certification, of whom an estimated 9,547 were still clinically active in 2019. This is the “grandfathered” cohort of psychiatrists to which I belong. I was tested on neurologic patients, not just psychiatric patients, a tribute to the strong bridge that existed between these sister brain specialties. As of 2019, of the 33,277 psychiatrists who received a time-limited certification, 29,343 were still clinically active, an attrition rate of 12% over the past 25 years. This includes psychiatrists who found the MOC too onerous to complete, or are in private practice where MOC is not a vital requirement. However, these days most psychiatrists are obligated to be recertified because so many entities require it. This includes hiring institutions, government agencies (Medicare/Medicaid), health insurance companies, hospital medical staff for privileging and credentialing, and various regulatory boards, such as The Joint Commission, the Accreditation Council for Graduate Medical Education, and academic medical centers. Because most psychiatrists are involved with at least one of these entities, 29,343 have no choice but to perform all the requirements of the MOC, with its countless hours, numerous documentations, and many fees, to remain certified by the ABPN. Notably absent is an alternative mechanism for a certification process that is widely accepted by all agencies and institutions. Psychiatrists are actively seeking alternatives.
Continue to: The ABPN...
The ABPN, long regarded as an esteemed nonprofit organization, has been accused of being a monopoly. Some angry psychiatrists have filed a class action lawsuit to demand other board certification methods. Some have gone to the media to complain about the American Board of Medical Specialties (of which the ABPN is a member board), accusing both of unfair regulations or of raking in substantial profits to support excessively compensated executives. Perception often trumps reality, so no matter how vigorously the ABPN defends itself, its procedures, or its MOC requirements, its customers—psychiatric physicians—feel oppressed or exploited.
How the MOC can be improved
So what can be done to improve the MOC? The need for recertification is arguably necessary to document clinical competency over an approximately 40-year psychiatric career following residency. I conducted a brief survey of
Significant advances in remote communication technology should be harnessed by the ABPN (or the APA, if it decides to conduct its own board certification) to restore the old model at a fraction of the cost. The oral exams have been replaced by a written exam that is not an accurate reflection or documentation of clinical competence. The traditional oral exam (after passing a written exam) was a magnificent but costly feat of massive logistical complexity, with >1,000 candidates and examiners traveling to a city where the ABPN arranged for several hospitals to shut down their clinics for 2 full days to use their clinical offices for the oral exams. Multiple teams examined the candidates twice on the same day: once with a live patient, and again with a video of a real patient. The examiners filled out scoring cards after observing the candidates conduct the live interview or discussing the video. A consensus grade of pass or fail was documented. At the end of the 2 days, examiners and candidates boarded buses to the airport. It was a highly expensive process (exam fees + airfare + hotel + food). Twice a year, the examiners generously donated their time to the ABPN without compensation, as a token of love for and service to the profession.
That initial certification of a written exam, followed by an oral exam, validated the competence of a psychiatrist both cognitively and clinically. The lifetime certification was truly earned. The same model can now be replicated virtually via videoconferencing at a far lower cost to the ABPN, the candidates, and the examiners. The MOC 10-year recertification can be reduced to a written exam with clinical vignettes and an unrestricted license to practice medicine in any state, which implies that the psychiatrist has received the 50 CME annual credits to renew the license. The rest of the bells and whistles can be strongly recommended but not required. The cost in time and money to both the ABPN and the candidates can be significantly reduced, but more importantly, the clinical competence will be validated at baseline with virtual oral boards after passing the written exam (formerly labeled as part I, preceding the part II oral boards).
The traditional board certification model of the past should be resurrected via videoconferencing and offered as an option to the candidates who prefer it to the current MOC. The MOC can then be simplified to lifetime certification or to only a written exam with clinical vignettes every 10 years to ensure that psychiatrists continue to incorporate relevant clinical and treatment advances in their practice. The KISS principle (keep it simple, stupid) worked very well for many generations of psychiatrists in the past, and will work again going forward if offered as an option. Psychiatrists can then focus on treating patients instead of being burdened by the many time-consuming requirements and hoops of the current MOC.
There are few things that psychiatrists have come to despise more than the American Board of Psychiatry and Neurology (ABPN) Maintenance of Certification (MOC) program. It has become a professional boondoggle for psychiatric practitioners.
The program needs an overhaul and simplification. There are better, more efficient, cost-effective ways to ensure psychiatric physicians’ ongoing clinical competence after they complete their residency training. Technological advances can also facilitate a more valid assessment of competence without having to jump through more and more hoops between recertifications every 10 years.
I passed the boards long before the MOC was created. For 20 years, I also served as a senior examiner for the oral boards, where clinical competency was rigorously assessed by direct observations of psychiatrists examining and establishing rapport with patients and formulating the data into a differential diagnosis, treatment plan, and prognosis. It is noteworthy that psychiatrists who sat for the oral boards had already passed a written exam that tested their cognitive knowledge. Yet approximately one-third of the candidates failed the live oral exam, which clearly implies that passing a written exam is necessary but not sufficient to establish clinical competence, which is the primary purpose of board certification. It was an unfortunate decision to discontinue the face-to-face oral board exam, which is so vital for psychiatry, and to replace it with a written exam and a barrage of time-consuming activities to document lifelong learning and self-assessment, but not genuine clinical competence. The MOC has been MOCkingly referred to as a major pain in the neck for practically all psychiatrists who were not grandfathered with lifetime certification, as was the case in the first 60 years of the ABPN.
Benefits of the patient-based oral exam
Let’s face it: Passing a patient-based oral exam was the ideal mechanism to establish that a psychiatric physician deserved to be a diplomate of the ABPN. During the oral exam, the candidate’s skills were observed from the minute he/she met the patient. The candidate was then observed as he/she systematically explored a wide range of past and current psychiatric symptoms; reviewed the patient’s developmental, medical, family, and social histories; and conducted a competent mental status exam while demonstrating an empathic stance, responding to the patient’s often subtle verbal and nonverbal cues, establishing rapport, and providing psychoeducation before concluding the interview. All these essential components of a psychiatric exam were observed in a compact 30-minute tour de force of clinical skills, communication, and cognitive acumen. This was followed by another 30 minutes of organizing and presenting the clinical data to 2 or 3 colleagues/examiners, in a coherent fashion, connecting all the dots, formulating the case, presenting a meaningful differential diagnosis, and suggesting a rational array of potential treatment options across the biopsychosocial continuum. To top it off, the candidate had to respond effectively, in an evidence-based manner, to a series of questions related to the disease state, its treatment, adverse effects, and prognosis.
It was a joy to watch many colleagues navigate this clinical examination with skill and competence, without crumbling under the pressure of the examiners’ scrutiny. There were some who passed with flying colors, and others who passed despite having a forgivable minor gap here and there because of their overall strong performance. Finally, there were those who stumbled in several components across data collection, doctor–patient interactions, synthesis of the clinical findings, or treatment recommendations. These candidates inevitably received a failing grade by a consensus of 3 examiners. That they failed to demonstrate clinical competence despite having passed the required written exams a year earlier proved that the true competency of a psychiatrist cannot be judged solely by passing a written test but requires a clinical examination of a live patient.
The oral exams represented an unimpeachable evaluation of clinical competence. The examiners often spoke of how they would feel confident and comfortable with referring a family member to those who successfully passed this rigorous, authentic exam on real patients. It was justifiable to give lifetime certification to those who passed the oral exam. Those permanently certified psychiatrists maintained their lifelong learning by having an unrestricted state medical license, which is contingent on acquiring 50 category 1 continuing medical education (CME) credits annually. Why not restore lifelong certification for those who pass both a written and oral exam, as long as they maintain a valid medical license?
According to the ABPN 2019 Annual Report,1 31,514 psychiatrists have received lifetime certification, of whom an estimated 9,547 were still clinically active in 2019. This is the “grandfathered” cohort of psychiatrists to which I belong. I was tested on neurologic patients, not just psychiatric patients, a tribute to the strong bridge that existed between these sister brain specialties. As of 2019, of the 33,277 psychiatrists who received a time-limited certification, 29,343 were still clinically active, an attrition rate of 12% over the past 25 years. This includes psychiatrists who found the MOC too onerous to complete, or are in private practice where MOC is not a vital requirement. However, these days most psychiatrists are obligated to be recertified because so many entities require it. This includes hiring institutions, government agencies (Medicare/Medicaid), health insurance companies, hospital medical staff for privileging and credentialing, and various regulatory boards, such as The Joint Commission, the Accreditation Council for Graduate Medical Education, and academic medical centers. Because most psychiatrists are involved with at least one of these entities, 29,343 have no choice but to perform all the requirements of the MOC, with its countless hours, numerous documentations, and many fees, to remain certified by the ABPN. Notably absent is an alternative mechanism for a certification process that is widely accepted by all agencies and institutions. Psychiatrists are actively seeking alternatives.
Continue to: The ABPN...
The ABPN, long regarded as an esteemed nonprofit organization, has been accused of being a monopoly. Some angry psychiatrists have filed a class action lawsuit to demand other board certification methods. Some have gone to the media to complain about the American Board of Medical Specialties (of which the ABPN is a member board), accusing both of unfair regulations or of raking in substantial profits to support excessively compensated executives. Perception often trumps reality, so no matter how vigorously the ABPN defends itself, its procedures, or its MOC requirements, its customers—psychiatric physicians—feel oppressed or exploited.
How the MOC can be improved
So what can be done to improve the MOC? The need for recertification is arguably necessary to document clinical competency over an approximately 40-year psychiatric career following residency. I conducted a brief survey of
Significant advances in remote communication technology should be harnessed by the ABPN (or the APA, if it decides to conduct its own board certification) to restore the old model at a fraction of the cost. The oral exams have been replaced by a written exam that is not an accurate reflection or documentation of clinical competence. The traditional oral exam (after passing a written exam) was a magnificent but costly feat of massive logistical complexity, with >1,000 candidates and examiners traveling to a city where the ABPN arranged for several hospitals to shut down their clinics for 2 full days to use their clinical offices for the oral exams. Multiple teams examined the candidates twice on the same day: once with a live patient, and again with a video of a real patient. The examiners filled out scoring cards after observing the candidates conduct the live interview or discussing the video. A consensus grade of pass or fail was documented. At the end of the 2 days, examiners and candidates boarded buses to the airport. It was a highly expensive process (exam fees + airfare + hotel + food). Twice a year, the examiners generously donated their time to the ABPN without compensation, as a token of love for and service to the profession.
That initial certification of a written exam, followed by an oral exam, validated the competence of a psychiatrist both cognitively and clinically. The lifetime certification was truly earned. The same model can now be replicated virtually via videoconferencing at a far lower cost to the ABPN, the candidates, and the examiners. The MOC 10-year recertification can be reduced to a written exam with clinical vignettes and an unrestricted license to practice medicine in any state, which implies that the psychiatrist has received the 50 CME annual credits to renew the license. The rest of the bells and whistles can be strongly recommended but not required. The cost in time and money to both the ABPN and the candidates can be significantly reduced, but more importantly, the clinical competence will be validated at baseline with virtual oral boards after passing the written exam (formerly labeled as part I, preceding the part II oral boards).
The traditional board certification model of the past should be resurrected via videoconferencing and offered as an option to the candidates who prefer it to the current MOC. The MOC can then be simplified to lifetime certification or to only a written exam with clinical vignettes every 10 years to ensure that psychiatrists continue to incorporate relevant clinical and treatment advances in their practice. The KISS principle (keep it simple, stupid) worked very well for many generations of psychiatrists in the past, and will work again going forward if offered as an option. Psychiatrists can then focus on treating patients instead of being burdened by the many time-consuming requirements and hoops of the current MOC.
1. American Board of Psychiatry and Neurology. 2019 Annual Report. https://www.abpn.com/wp-content/uploads/2020/05/ABPN_2019_Annual_Report.pdf. Accessed August 14, 2020.
1. American Board of Psychiatry and Neurology. 2019 Annual Report. https://www.abpn.com/wp-content/uploads/2020/05/ABPN_2019_Annual_Report.pdf. Accessed August 14, 2020.
Enduring the ordeal of a quadruple threat is especially arduous for psychiatric patients
These are unusually stressful days for everyone, especially our patients. We are all experiencing a turbulent mix of emotions as we try to cope with a confluence of threats to both our lives and to life as we know it. Peace of mind has become so elusive due to the relentless overlapping waves of fear, sadness, anger, and uncertainty. We are all grieving in a different way, but our psychiatric patients are suffering the most.
Fear. It only takes 1 traumatic event to trigger posttraumatic stress disorder (PTSD). Yet over the past few months, we have been afflicted by 4 jarring traumatic events, individually and as a society. Just a few months ago, it would have been impossible to imagine the conflux of 4 concurrent seismic threats to our well-being. A toxic political zeitgeist was the backdrop, which we bemoaned and tried to compartmentalize, despite the corrosive political environment shrouding the country. Then the deadly coronavirus disease 2019 (COVID-19) pandemic suddenly arrived, imposing draconian health-preserving measures that impacted every individual’s daily life in countless detrimental ways. Fear prevailed as we all sheltered at home, stopped commuting to work, canceled all trips, distanced ourselves from our friends and relatives, and watched depressing and anxiety-provoking television and read online news throughout our waking hours. Hoarding food and household supplies became endemic due to fear about survival.
Sadness. The agonizing prospect of a national financial necrosis followed the threat of serious illness or death. The economy came to a screeching halt, hemorrhaging millions of jobs. Unemployed parents stayed home with their morose children whose schools were shuttered, leaving them deprived of socializing with their friends. The government hurried with financial chemotherapy, printing trillions of dollars to prevent economic collapse, to avert potential poverty and hunger for many. The fear of the pandemic became coupled with sadness over the loss of livelihoods and grief for the loss of liberty and the ability to pursue happiness, or even small pleasures.
Anger. Then a tsunami of anger was generated by the brutal and sadistic death of a black man in police custody. This was a spark that ignited a massive amount of previously dormant racial tension dating back to the dark days of slavery. Peaceful protests were marred by destructive riots. The explosive fury was perhaps intensified by the protestors having been being locked up for weeks and having to wear masks, both of which were symbolic of being held down and “unable to breathe,” like the murdered Mr. George Floyd.
An epidemic of destroying statues followed. Heavy statues that appeared invincible for decades were dismantled from their plinth in a matter of minutes, signifying extreme frustration with the social injustice that remains despite the transformational laws of the Civil Rights Acts of 1960 and 1964. Suddenly—like falling dominoes—statues, flags, names of military bases, and previously venerated monuments were removed, changed, vandalized, or threatened with destruction. The founders of the republic were also maligned because they were slave owners 2 centuries ago. The paradigm shift spawned by the rage over racial inequality was disconcerting and dramatic. The anger and rampage spawned a sense that a tipping point in our society has been reached.
Uncertainty. The confluence of political instability, a deadly pandemic, economic collapse, and racial tensions were like the 4 horsemen of mass PTSD. The result was an agonizing uncertainty about the impact of these changes, and whether a sense of normalcy will ever return. It became apparent to all of us that our social structure has changed forever across multiple fundamental domains: public health, social, political, and financial. The wait for a vaccine for COVID-19 seems interminable, and racial healing and harmony seems elusive. Economic recovery may be possible, but political detoxification appears unlikely. The fate of police departments, condemned because of the deplorable and illegal acts of a few, and the safety of citizens, usually guaranteed by law and order, seem uncertain. Like COVID-19, angst has rapidly spread across the population.
The price our patients pay
The ingredients of a large-scale societal PTSD, similar to what probably happens during a world war, are now in place. Even resilient individuals may buckle during quadruple ordeals such as this one. So imagine what is happening to our patients, rendered fragile and vulnerable to threats by their pre-existing psychiatric illness. They all pay a heavy price. Patients with anxiety disorders will decompensate, with more panic attacks. Patients burdened by depression will worsen, with more hopelessness, despair, and suicidal ideation due to anxiety and loneliness. Patients with bipolar disorder will become more labile and irritable, and their comorbid anxiety will intensify. Patients with schizophrenia will become more paranoid, depressed, and anxious. Patients with autism will become more agitated and aggressive because their cherished daily routines are disrupted. Patients with obsessive-compulsive disorder will react to their germaphobia by washing their hands and cleaning everything around them even more frequently, and they (along with everyone else) will become hoarders.
Hope and healing
As psychiatrists, we are determined to transcend our own stress, rise above it all, and attend to the pervasive sadness, grief, anger, and uncertainty all around us, but especially among our patients, for whom the anguish of a psychiatric disorder is further compounded by 4 additional ordeals. This is our moment of truth as healers of our patients’ souls, because they look to us to provide them with hope to help navigate these trying times into full health. And we psychiatrists, along with fellow mental health professionals, are up to this unprecedented challenge.
These are unusually stressful days for everyone, especially our patients. We are all experiencing a turbulent mix of emotions as we try to cope with a confluence of threats to both our lives and to life as we know it. Peace of mind has become so elusive due to the relentless overlapping waves of fear, sadness, anger, and uncertainty. We are all grieving in a different way, but our psychiatric patients are suffering the most.
Fear. It only takes 1 traumatic event to trigger posttraumatic stress disorder (PTSD). Yet over the past few months, we have been afflicted by 4 jarring traumatic events, individually and as a society. Just a few months ago, it would have been impossible to imagine the conflux of 4 concurrent seismic threats to our well-being. A toxic political zeitgeist was the backdrop, which we bemoaned and tried to compartmentalize, despite the corrosive political environment shrouding the country. Then the deadly coronavirus disease 2019 (COVID-19) pandemic suddenly arrived, imposing draconian health-preserving measures that impacted every individual’s daily life in countless detrimental ways. Fear prevailed as we all sheltered at home, stopped commuting to work, canceled all trips, distanced ourselves from our friends and relatives, and watched depressing and anxiety-provoking television and read online news throughout our waking hours. Hoarding food and household supplies became endemic due to fear about survival.
Sadness. The agonizing prospect of a national financial necrosis followed the threat of serious illness or death. The economy came to a screeching halt, hemorrhaging millions of jobs. Unemployed parents stayed home with their morose children whose schools were shuttered, leaving them deprived of socializing with their friends. The government hurried with financial chemotherapy, printing trillions of dollars to prevent economic collapse, to avert potential poverty and hunger for many. The fear of the pandemic became coupled with sadness over the loss of livelihoods and grief for the loss of liberty and the ability to pursue happiness, or even small pleasures.
Anger. Then a tsunami of anger was generated by the brutal and sadistic death of a black man in police custody. This was a spark that ignited a massive amount of previously dormant racial tension dating back to the dark days of slavery. Peaceful protests were marred by destructive riots. The explosive fury was perhaps intensified by the protestors having been being locked up for weeks and having to wear masks, both of which were symbolic of being held down and “unable to breathe,” like the murdered Mr. George Floyd.
An epidemic of destroying statues followed. Heavy statues that appeared invincible for decades were dismantled from their plinth in a matter of minutes, signifying extreme frustration with the social injustice that remains despite the transformational laws of the Civil Rights Acts of 1960 and 1964. Suddenly—like falling dominoes—statues, flags, names of military bases, and previously venerated monuments were removed, changed, vandalized, or threatened with destruction. The founders of the republic were also maligned because they were slave owners 2 centuries ago. The paradigm shift spawned by the rage over racial inequality was disconcerting and dramatic. The anger and rampage spawned a sense that a tipping point in our society has been reached.
Uncertainty. The confluence of political instability, a deadly pandemic, economic collapse, and racial tensions were like the 4 horsemen of mass PTSD. The result was an agonizing uncertainty about the impact of these changes, and whether a sense of normalcy will ever return. It became apparent to all of us that our social structure has changed forever across multiple fundamental domains: public health, social, political, and financial. The wait for a vaccine for COVID-19 seems interminable, and racial healing and harmony seems elusive. Economic recovery may be possible, but political detoxification appears unlikely. The fate of police departments, condemned because of the deplorable and illegal acts of a few, and the safety of citizens, usually guaranteed by law and order, seem uncertain. Like COVID-19, angst has rapidly spread across the population.
The price our patients pay
The ingredients of a large-scale societal PTSD, similar to what probably happens during a world war, are now in place. Even resilient individuals may buckle during quadruple ordeals such as this one. So imagine what is happening to our patients, rendered fragile and vulnerable to threats by their pre-existing psychiatric illness. They all pay a heavy price. Patients with anxiety disorders will decompensate, with more panic attacks. Patients burdened by depression will worsen, with more hopelessness, despair, and suicidal ideation due to anxiety and loneliness. Patients with bipolar disorder will become more labile and irritable, and their comorbid anxiety will intensify. Patients with schizophrenia will become more paranoid, depressed, and anxious. Patients with autism will become more agitated and aggressive because their cherished daily routines are disrupted. Patients with obsessive-compulsive disorder will react to their germaphobia by washing their hands and cleaning everything around them even more frequently, and they (along with everyone else) will become hoarders.
Hope and healing
As psychiatrists, we are determined to transcend our own stress, rise above it all, and attend to the pervasive sadness, grief, anger, and uncertainty all around us, but especially among our patients, for whom the anguish of a psychiatric disorder is further compounded by 4 additional ordeals. This is our moment of truth as healers of our patients’ souls, because they look to us to provide them with hope to help navigate these trying times into full health. And we psychiatrists, along with fellow mental health professionals, are up to this unprecedented challenge.
These are unusually stressful days for everyone, especially our patients. We are all experiencing a turbulent mix of emotions as we try to cope with a confluence of threats to both our lives and to life as we know it. Peace of mind has become so elusive due to the relentless overlapping waves of fear, sadness, anger, and uncertainty. We are all grieving in a different way, but our psychiatric patients are suffering the most.
Fear. It only takes 1 traumatic event to trigger posttraumatic stress disorder (PTSD). Yet over the past few months, we have been afflicted by 4 jarring traumatic events, individually and as a society. Just a few months ago, it would have been impossible to imagine the conflux of 4 concurrent seismic threats to our well-being. A toxic political zeitgeist was the backdrop, which we bemoaned and tried to compartmentalize, despite the corrosive political environment shrouding the country. Then the deadly coronavirus disease 2019 (COVID-19) pandemic suddenly arrived, imposing draconian health-preserving measures that impacted every individual’s daily life in countless detrimental ways. Fear prevailed as we all sheltered at home, stopped commuting to work, canceled all trips, distanced ourselves from our friends and relatives, and watched depressing and anxiety-provoking television and read online news throughout our waking hours. Hoarding food and household supplies became endemic due to fear about survival.
Sadness. The agonizing prospect of a national financial necrosis followed the threat of serious illness or death. The economy came to a screeching halt, hemorrhaging millions of jobs. Unemployed parents stayed home with their morose children whose schools were shuttered, leaving them deprived of socializing with their friends. The government hurried with financial chemotherapy, printing trillions of dollars to prevent economic collapse, to avert potential poverty and hunger for many. The fear of the pandemic became coupled with sadness over the loss of livelihoods and grief for the loss of liberty and the ability to pursue happiness, or even small pleasures.
Anger. Then a tsunami of anger was generated by the brutal and sadistic death of a black man in police custody. This was a spark that ignited a massive amount of previously dormant racial tension dating back to the dark days of slavery. Peaceful protests were marred by destructive riots. The explosive fury was perhaps intensified by the protestors having been being locked up for weeks and having to wear masks, both of which were symbolic of being held down and “unable to breathe,” like the murdered Mr. George Floyd.
An epidemic of destroying statues followed. Heavy statues that appeared invincible for decades were dismantled from their plinth in a matter of minutes, signifying extreme frustration with the social injustice that remains despite the transformational laws of the Civil Rights Acts of 1960 and 1964. Suddenly—like falling dominoes—statues, flags, names of military bases, and previously venerated monuments were removed, changed, vandalized, or threatened with destruction. The founders of the republic were also maligned because they were slave owners 2 centuries ago. The paradigm shift spawned by the rage over racial inequality was disconcerting and dramatic. The anger and rampage spawned a sense that a tipping point in our society has been reached.
Uncertainty. The confluence of political instability, a deadly pandemic, economic collapse, and racial tensions were like the 4 horsemen of mass PTSD. The result was an agonizing uncertainty about the impact of these changes, and whether a sense of normalcy will ever return. It became apparent to all of us that our social structure has changed forever across multiple fundamental domains: public health, social, political, and financial. The wait for a vaccine for COVID-19 seems interminable, and racial healing and harmony seems elusive. Economic recovery may be possible, but political detoxification appears unlikely. The fate of police departments, condemned because of the deplorable and illegal acts of a few, and the safety of citizens, usually guaranteed by law and order, seem uncertain. Like COVID-19, angst has rapidly spread across the population.
The price our patients pay
The ingredients of a large-scale societal PTSD, similar to what probably happens during a world war, are now in place. Even resilient individuals may buckle during quadruple ordeals such as this one. So imagine what is happening to our patients, rendered fragile and vulnerable to threats by their pre-existing psychiatric illness. They all pay a heavy price. Patients with anxiety disorders will decompensate, with more panic attacks. Patients burdened by depression will worsen, with more hopelessness, despair, and suicidal ideation due to anxiety and loneliness. Patients with bipolar disorder will become more labile and irritable, and their comorbid anxiety will intensify. Patients with schizophrenia will become more paranoid, depressed, and anxious. Patients with autism will become more agitated and aggressive because their cherished daily routines are disrupted. Patients with obsessive-compulsive disorder will react to their germaphobia by washing their hands and cleaning everything around them even more frequently, and they (along with everyone else) will become hoarders.
Hope and healing
As psychiatrists, we are determined to transcend our own stress, rise above it all, and attend to the pervasive sadness, grief, anger, and uncertainty all around us, but especially among our patients, for whom the anguish of a psychiatric disorder is further compounded by 4 additional ordeals. This is our moment of truth as healers of our patients’ souls, because they look to us to provide them with hope to help navigate these trying times into full health. And we psychiatrists, along with fellow mental health professionals, are up to this unprecedented challenge.
COVID-19 and the precipitous dismantlement of societal norms
As the life-altering coronavirus disease 2019 (COVID-19) pandemic gradually ebbs, we are all its survivors. Now, we are experiencing COVID-19 fatigue, trying to emerge from its dense fog that pervaded every facet of our lives. We are fully cognizant that there will not be a return to the previous “normal.” The pernicious virus had a transformative effect that did not spare any component of our society. Full recovery will not be easy.
As the uncertainty lingers about another devastating return of the pandemic later this year, we can see the reverberation of this invisible assault on human existence. Although a relatively small fraction of the population lost their lives, the rest of us are valiantly trying to readjust to the multiple ways our world has changed. Consider the following abrupt and sweeping burdens inflicted by the pandemic within a few short weeks:
Mental health. The acute stress of thanatophobia generated a triad of anxiety, depression, and nosophobia on a large scale. The demand for psychiatric care rapidly escalated. Suicide rate increased not only because of the stress of being locked down at home (alien to most people’s lifestyle) but because of the coincidental timing of the pandemic during April and May, the peak time of year for suicide. Animal researchers use immobilization as a paradigm to stress a rat or mouse. Many humans immobilized during the pandemic have developed exquisite empathy towards those rodents! The impact on children may also have long-term effects because playing and socializing with friends is a vital part of their lives. Parents have noticed dysphoria and acting out among their children, and an intense compensatory preoccupation with video games and electronic communications with friends.
Physical health. Medical care focused heavily on COVID-19 victims, to the detriment of all other medical conditions. Non-COVID-19 hospital admissions plummeted, and all elective surgeries and procedures were put on hold, depriving many people of medical care they badly needed. Emergency department (ED) visits also declined dramatically, including the usual flow of heart attacks, stroke, pulmonary embolus, asthma attacks, etc. The minimization of driving greatly reduced the admission of accident victims to EDs. Colonoscopies, cardiac stents, hip replacements, MRIs, mammography, and other procedures that are vital to maintain health and quality of life were halted. Dentists shuttered their practices due to the high risk of infection from exposure to oral secretions and breathing. One can only imagine the suffering of having a toothache with no dental help available, and how that might lead to narcotic abuse.
Social health. The imperative of social distancing disrupted most ordinary human activities, such as dining out, sitting in an auditorium for Grand Rounds or a lecture, visiting friends at their homes, the cherished interactions between grandparents and grandchildren (the lack of which I painfully experienced), and even seeing each other’s smiles behind the ubiquitous masks. And forget about hugging or kissing. The aversion to being near anyone who is coughing or sneezing led to an adaptive social paranoia and the social shunning of anyone who appeared to have an upper respiratory infection, even if it was unrelated to COVID-19.
Redemption for the pharmaceutical industry. The deadly pandemic intensified the public’s awareness of the importance of developing treatments and vaccines for COVID-19. The often-demonized pharmaceutical companies, with their extensive R&D infrastructure, emerged as a major source of hope for discovering an effective treatment for the coronavirus infection, or—better still—one or more vaccines that will enable society to return to its normal functions. It was quite impressive how many pharmaceutical companies “came to the rescue” with clinical trials to repurpose existing medications or to develop new ones. It was very encouraging to see multiple vaccine candidates being developed and expedited for testing around the world. A process that usually takes years was reduced to a few months, thanks to the existing technical infrastructure and thousands of scientists who enable rapid drug development. It is possible that the public may gradually modify its perception of the pharmaceutical industry from a “corporate villain” to an “indispensable health industry” for urgent medical crises such as a pandemic, and also for hundreds of medical diseases that are still in need of safe, effective therapies.
Economic burden. The unimaginable nightmare scenario of a total shutdown of all businesses led to the unprecedented loss of millions of jobs and livelihoods, reflected in miles-long lines of families at food banks. Overnight, the government switched from worrying about its $20-trillion deficit to printing several more trillion dollars to rescue the economy from collapse. The huge magnitude of a trillion can be appreciated if one is aware that it takes roughly 32 years to count to 1 billion, and 32,000 years to count to 1 trillion. Stimulating the economy while the gross domestic product threatens to sink by terrifying percentages (20% to 30%) was urgently needed, even though it meant mortgaging the future, especially when interest rates, and servicing the debt, will inevitably rise from the current zero to much higher levels in the future. The collapse of the once-thriving airline industry (bookings were down an estimated 98%) is an example of why desperate measures were needed to salvage an economy paralyzed by a viral pandemic.
Continue to: Political repercussions
Political repercussions. In our already hyperpartisan country, the COVID-19 crisis created more fissures across party lines. The blame game escalated as each side tried to exploit the crisis for political gain during a presidential election year. None of the leaders, from mayors to governors to the president, had any notion of how to wisely manage an unforeseen catastrophic pandemic. Thus, a political cacophony has developed, further exacerbating the public’s anxiety and uncertainty, especially about how and when the pandemic will end.
Education disruption. Never before have all schools and colleges around the country abruptly closed and sent students of all ages to shelter at home. Massive havoc ensued, with a wholesale switch to solitary online learning, the loss of the unique school and college social experience in the classroom and on campus, and the loss of experiencing commencement to receive a diploma (an important milestone for every graduate). Even medical students were not allowed to complete their clinical rotations and were sent home to attend online classes. A complete paradigm shift emerged about entrance exams: the SAT and ACT were eliminated for college applicants, and the MCAT for medical school applicants. This was unthinkable before the pandemic descended upon us, but benchmarks suddenly evaporated to adjust to the new reality. Then there followed disastrous financial losses by institutions of higher learning as well as academic medical centers and teaching hospitals, all slashing their budgets, furloughing employees, cutting salaries, and eliminating programs. Even the “sacred” tenure of senior faculty became a casualty of the financial “exigency.” Children’s nutrition suffered, especially among those in lower socioeconomic groups for whom the main meal of the day was the school lunch, and was made worse by their parents’ loss of income. For millions of people, the emotional toll was inevitable following the draconian measure of closing all educational institutions to contain the spread of the pandemic.
Family burden. Sheltering at home might have been fun for a few days, but after many weeks, it festered into a major stress, especially for those living in a small house, condominium, or apartment. The resilience of many families was tested as the exercise of freedoms collided with the fear of getting infected. Families were deprived of celebrating birthdays, weddings, funerals, graduation parties, retirement parties, Mother’s Day, Father’s Day, and various religious holidays, including Easter, Passover, and Eid al-Fitr.
Sexual burden. Intimacy and sexual contact between consenting adults living apart were sacrificed on the altar of the pernicious viral pandemic. Mandatory social distancing of 6 feet or more to avoid each other’s droplets emanating from simple speech, not just sneezing or coughing, makes intimacy practically impossible. Thus, physical closeness became taboo, and avoiding another person’s saliva or body secretions became a must to avoid contracting the virus. Being single was quite a lonely experience during this pandemic!
Entertainment deprivation. Americans are known to thrive on an extensive diet of spectator sports. Going to football, basketball, baseball, or hockey games to root for one’s team is intrinsically American. The pursuit of happiness extends to attending concerts, movies, Broadway shows, theme parks, and cruises with thousands of others. The pandemic ripped all those pleasurable leisure activities from our daily lives, leaving a big hole in people’s lives at the precise time fun activities were needed as a useful diversion from the dismal stress of a pandemic. To make things worse, it is uncertain when (if ever) such group activities will be restored, especially if the pandemic returns with another wave. But optimists would hurry to remind us that the “Roaring 20s” blossomed in the decade following the 1918 Spanish Flu pandemic.
Continue to: Legal system
Legal system. Astounding changes were instigated by the pandemic, such as the release of thousands of inmates, including felons, to avoid the spread of the virus in crowded prisons. For us psychiatrists, the silver lining in that unexpected action is that many of those released were patients with mental illness who were incarcerated because of the lack of hospitals that would take them. The police started issuing citations instead of arresting and jailing violators. Enforcement of the law was welcome when it targeted those who gouged the public for personal profit during the scarcity of masks, sanitizers, or even toilet paper and soap.
Medical practice. In addition to delaying medical care for patients, the freeze on so-called elective surgeries or procedures (many of which were actually necessary) was financially ruinous for physicians. Another regrettable consequence of the pandemic is a drop in pediatric vaccinations because parents were reluctant to take their children to the pediatrician. On a more positive note, the massive switch to telehealth was advantageous for both patients and psychiatrists because this technology is well-suited for psychiatric care. Fortunately, regulations that hampered telepsychiatry practice were substantially loosened or eliminated, and even the usually sacrosanct HIPAA regulations were temporarily sidelined.
Medical research. Both human and animal research came to a screeching halt, and many research assistants were furloughed. Data collection was disrupted, and a generation of scientific and medical discoveries became a casualty of the pandemic.
Medical literature. It was stunning to see how quickly COVID-19 occupied most of the pages of prominent journals. The scholarly articles were frankly quite useful, covering topics ranging from risk factors to early symptoms to treatment and pathophysiology across multiple organs. As with other paradigm shifts, there was an accelerated publication push, sometimes with expedited peer reviews to inform health care workers and the public while the pandemic was still raging. However, a couple of very prominent journals had to retract flawed articles that were hastily published without the usual due diligence and rigorous peer review. The pandemic clearly disrupted the science publishing process.
Travel effects. The steep reduction of flights (by 98%) was financially catastrophic, not only for airline companies but to business travel across the country. However, fewer cars on the road resulted in fewer accidents and deaths, and also reduced pollution. Paradoxically, to prevent crowding in subways, trains, and buses, officials reversed their traditional instructions and advised the public to drive their own cars instead of using public transportation!
Continue to: Heroism of front-line medical personnel
Heroism of front-line medical personnel. Everyone saluted and prayed for the health care professionals working at the bedside of highly infectious patients who needed 24/7 intensive care. Many have died while carrying out the noble but hazardous medical duties. Those heroes deserve our lasting respect and admiration.
The COVID-19 pandemic insidiously permeated and altered every aspect of our complex society and revealed how fragile our “normal lifestyle” really is. It is possible that nothing will ever be the same again, and an uneasy sense of vulnerability will engulf us as we cautiously return to a “new normal.” Even our language has expanded with the lexicon of pandemic terminology (Table). We all pray and hope that this plague never returns. And let’s hope one or more vaccines are developed soon so we can manage future recurrences like the annual flu season. In the meantime, keep your masks and sanitizers close by…
Postscript: Shortly after I completed this editorial, the ongoing COVID-19 plague was overshadowed by the scourge of racism, with massive protests, at times laced by violence, triggered by the death of a black man in custody of the police, under condemnable circumstances. The COVID-19 pandemic and the necessary social distancing it requires were temporarily ignored during the ensuing protests. The combined effect of those overlapping scourges are jarring to the country’s psyche, complicating and perhaps sabotaging the social recovery from the pandemic.
As the life-altering coronavirus disease 2019 (COVID-19) pandemic gradually ebbs, we are all its survivors. Now, we are experiencing COVID-19 fatigue, trying to emerge from its dense fog that pervaded every facet of our lives. We are fully cognizant that there will not be a return to the previous “normal.” The pernicious virus had a transformative effect that did not spare any component of our society. Full recovery will not be easy.
As the uncertainty lingers about another devastating return of the pandemic later this year, we can see the reverberation of this invisible assault on human existence. Although a relatively small fraction of the population lost their lives, the rest of us are valiantly trying to readjust to the multiple ways our world has changed. Consider the following abrupt and sweeping burdens inflicted by the pandemic within a few short weeks:
Mental health. The acute stress of thanatophobia generated a triad of anxiety, depression, and nosophobia on a large scale. The demand for psychiatric care rapidly escalated. Suicide rate increased not only because of the stress of being locked down at home (alien to most people’s lifestyle) but because of the coincidental timing of the pandemic during April and May, the peak time of year for suicide. Animal researchers use immobilization as a paradigm to stress a rat or mouse. Many humans immobilized during the pandemic have developed exquisite empathy towards those rodents! The impact on children may also have long-term effects because playing and socializing with friends is a vital part of their lives. Parents have noticed dysphoria and acting out among their children, and an intense compensatory preoccupation with video games and electronic communications with friends.
Physical health. Medical care focused heavily on COVID-19 victims, to the detriment of all other medical conditions. Non-COVID-19 hospital admissions plummeted, and all elective surgeries and procedures were put on hold, depriving many people of medical care they badly needed. Emergency department (ED) visits also declined dramatically, including the usual flow of heart attacks, stroke, pulmonary embolus, asthma attacks, etc. The minimization of driving greatly reduced the admission of accident victims to EDs. Colonoscopies, cardiac stents, hip replacements, MRIs, mammography, and other procedures that are vital to maintain health and quality of life were halted. Dentists shuttered their practices due to the high risk of infection from exposure to oral secretions and breathing. One can only imagine the suffering of having a toothache with no dental help available, and how that might lead to narcotic abuse.
Social health. The imperative of social distancing disrupted most ordinary human activities, such as dining out, sitting in an auditorium for Grand Rounds or a lecture, visiting friends at their homes, the cherished interactions between grandparents and grandchildren (the lack of which I painfully experienced), and even seeing each other’s smiles behind the ubiquitous masks. And forget about hugging or kissing. The aversion to being near anyone who is coughing or sneezing led to an adaptive social paranoia and the social shunning of anyone who appeared to have an upper respiratory infection, even if it was unrelated to COVID-19.
Redemption for the pharmaceutical industry. The deadly pandemic intensified the public’s awareness of the importance of developing treatments and vaccines for COVID-19. The often-demonized pharmaceutical companies, with their extensive R&D infrastructure, emerged as a major source of hope for discovering an effective treatment for the coronavirus infection, or—better still—one or more vaccines that will enable society to return to its normal functions. It was quite impressive how many pharmaceutical companies “came to the rescue” with clinical trials to repurpose existing medications or to develop new ones. It was very encouraging to see multiple vaccine candidates being developed and expedited for testing around the world. A process that usually takes years was reduced to a few months, thanks to the existing technical infrastructure and thousands of scientists who enable rapid drug development. It is possible that the public may gradually modify its perception of the pharmaceutical industry from a “corporate villain” to an “indispensable health industry” for urgent medical crises such as a pandemic, and also for hundreds of medical diseases that are still in need of safe, effective therapies.
Economic burden. The unimaginable nightmare scenario of a total shutdown of all businesses led to the unprecedented loss of millions of jobs and livelihoods, reflected in miles-long lines of families at food banks. Overnight, the government switched from worrying about its $20-trillion deficit to printing several more trillion dollars to rescue the economy from collapse. The huge magnitude of a trillion can be appreciated if one is aware that it takes roughly 32 years to count to 1 billion, and 32,000 years to count to 1 trillion. Stimulating the economy while the gross domestic product threatens to sink by terrifying percentages (20% to 30%) was urgently needed, even though it meant mortgaging the future, especially when interest rates, and servicing the debt, will inevitably rise from the current zero to much higher levels in the future. The collapse of the once-thriving airline industry (bookings were down an estimated 98%) is an example of why desperate measures were needed to salvage an economy paralyzed by a viral pandemic.
Continue to: Political repercussions
Political repercussions. In our already hyperpartisan country, the COVID-19 crisis created more fissures across party lines. The blame game escalated as each side tried to exploit the crisis for political gain during a presidential election year. None of the leaders, from mayors to governors to the president, had any notion of how to wisely manage an unforeseen catastrophic pandemic. Thus, a political cacophony has developed, further exacerbating the public’s anxiety and uncertainty, especially about how and when the pandemic will end.
Education disruption. Never before have all schools and colleges around the country abruptly closed and sent students of all ages to shelter at home. Massive havoc ensued, with a wholesale switch to solitary online learning, the loss of the unique school and college social experience in the classroom and on campus, and the loss of experiencing commencement to receive a diploma (an important milestone for every graduate). Even medical students were not allowed to complete their clinical rotations and were sent home to attend online classes. A complete paradigm shift emerged about entrance exams: the SAT and ACT were eliminated for college applicants, and the MCAT for medical school applicants. This was unthinkable before the pandemic descended upon us, but benchmarks suddenly evaporated to adjust to the new reality. Then there followed disastrous financial losses by institutions of higher learning as well as academic medical centers and teaching hospitals, all slashing their budgets, furloughing employees, cutting salaries, and eliminating programs. Even the “sacred” tenure of senior faculty became a casualty of the financial “exigency.” Children’s nutrition suffered, especially among those in lower socioeconomic groups for whom the main meal of the day was the school lunch, and was made worse by their parents’ loss of income. For millions of people, the emotional toll was inevitable following the draconian measure of closing all educational institutions to contain the spread of the pandemic.
Family burden. Sheltering at home might have been fun for a few days, but after many weeks, it festered into a major stress, especially for those living in a small house, condominium, or apartment. The resilience of many families was tested as the exercise of freedoms collided with the fear of getting infected. Families were deprived of celebrating birthdays, weddings, funerals, graduation parties, retirement parties, Mother’s Day, Father’s Day, and various religious holidays, including Easter, Passover, and Eid al-Fitr.
Sexual burden. Intimacy and sexual contact between consenting adults living apart were sacrificed on the altar of the pernicious viral pandemic. Mandatory social distancing of 6 feet or more to avoid each other’s droplets emanating from simple speech, not just sneezing or coughing, makes intimacy practically impossible. Thus, physical closeness became taboo, and avoiding another person’s saliva or body secretions became a must to avoid contracting the virus. Being single was quite a lonely experience during this pandemic!
Entertainment deprivation. Americans are known to thrive on an extensive diet of spectator sports. Going to football, basketball, baseball, or hockey games to root for one’s team is intrinsically American. The pursuit of happiness extends to attending concerts, movies, Broadway shows, theme parks, and cruises with thousands of others. The pandemic ripped all those pleasurable leisure activities from our daily lives, leaving a big hole in people’s lives at the precise time fun activities were needed as a useful diversion from the dismal stress of a pandemic. To make things worse, it is uncertain when (if ever) such group activities will be restored, especially if the pandemic returns with another wave. But optimists would hurry to remind us that the “Roaring 20s” blossomed in the decade following the 1918 Spanish Flu pandemic.
Continue to: Legal system
Legal system. Astounding changes were instigated by the pandemic, such as the release of thousands of inmates, including felons, to avoid the spread of the virus in crowded prisons. For us psychiatrists, the silver lining in that unexpected action is that many of those released were patients with mental illness who were incarcerated because of the lack of hospitals that would take them. The police started issuing citations instead of arresting and jailing violators. Enforcement of the law was welcome when it targeted those who gouged the public for personal profit during the scarcity of masks, sanitizers, or even toilet paper and soap.
Medical practice. In addition to delaying medical care for patients, the freeze on so-called elective surgeries or procedures (many of which were actually necessary) was financially ruinous for physicians. Another regrettable consequence of the pandemic is a drop in pediatric vaccinations because parents were reluctant to take their children to the pediatrician. On a more positive note, the massive switch to telehealth was advantageous for both patients and psychiatrists because this technology is well-suited for psychiatric care. Fortunately, regulations that hampered telepsychiatry practice were substantially loosened or eliminated, and even the usually sacrosanct HIPAA regulations were temporarily sidelined.
Medical research. Both human and animal research came to a screeching halt, and many research assistants were furloughed. Data collection was disrupted, and a generation of scientific and medical discoveries became a casualty of the pandemic.
Medical literature. It was stunning to see how quickly COVID-19 occupied most of the pages of prominent journals. The scholarly articles were frankly quite useful, covering topics ranging from risk factors to early symptoms to treatment and pathophysiology across multiple organs. As with other paradigm shifts, there was an accelerated publication push, sometimes with expedited peer reviews to inform health care workers and the public while the pandemic was still raging. However, a couple of very prominent journals had to retract flawed articles that were hastily published without the usual due diligence and rigorous peer review. The pandemic clearly disrupted the science publishing process.
Travel effects. The steep reduction of flights (by 98%) was financially catastrophic, not only for airline companies but to business travel across the country. However, fewer cars on the road resulted in fewer accidents and deaths, and also reduced pollution. Paradoxically, to prevent crowding in subways, trains, and buses, officials reversed their traditional instructions and advised the public to drive their own cars instead of using public transportation!
Continue to: Heroism of front-line medical personnel
Heroism of front-line medical personnel. Everyone saluted and prayed for the health care professionals working at the bedside of highly infectious patients who needed 24/7 intensive care. Many have died while carrying out the noble but hazardous medical duties. Those heroes deserve our lasting respect and admiration.
The COVID-19 pandemic insidiously permeated and altered every aspect of our complex society and revealed how fragile our “normal lifestyle” really is. It is possible that nothing will ever be the same again, and an uneasy sense of vulnerability will engulf us as we cautiously return to a “new normal.” Even our language has expanded with the lexicon of pandemic terminology (Table). We all pray and hope that this plague never returns. And let’s hope one or more vaccines are developed soon so we can manage future recurrences like the annual flu season. In the meantime, keep your masks and sanitizers close by…
Postscript: Shortly after I completed this editorial, the ongoing COVID-19 plague was overshadowed by the scourge of racism, with massive protests, at times laced by violence, triggered by the death of a black man in custody of the police, under condemnable circumstances. The COVID-19 pandemic and the necessary social distancing it requires were temporarily ignored during the ensuing protests. The combined effect of those overlapping scourges are jarring to the country’s psyche, complicating and perhaps sabotaging the social recovery from the pandemic.
As the life-altering coronavirus disease 2019 (COVID-19) pandemic gradually ebbs, we are all its survivors. Now, we are experiencing COVID-19 fatigue, trying to emerge from its dense fog that pervaded every facet of our lives. We are fully cognizant that there will not be a return to the previous “normal.” The pernicious virus had a transformative effect that did not spare any component of our society. Full recovery will not be easy.
As the uncertainty lingers about another devastating return of the pandemic later this year, we can see the reverberation of this invisible assault on human existence. Although a relatively small fraction of the population lost their lives, the rest of us are valiantly trying to readjust to the multiple ways our world has changed. Consider the following abrupt and sweeping burdens inflicted by the pandemic within a few short weeks:
Mental health. The acute stress of thanatophobia generated a triad of anxiety, depression, and nosophobia on a large scale. The demand for psychiatric care rapidly escalated. Suicide rate increased not only because of the stress of being locked down at home (alien to most people’s lifestyle) but because of the coincidental timing of the pandemic during April and May, the peak time of year for suicide. Animal researchers use immobilization as a paradigm to stress a rat or mouse. Many humans immobilized during the pandemic have developed exquisite empathy towards those rodents! The impact on children may also have long-term effects because playing and socializing with friends is a vital part of their lives. Parents have noticed dysphoria and acting out among their children, and an intense compensatory preoccupation with video games and electronic communications with friends.
Physical health. Medical care focused heavily on COVID-19 victims, to the detriment of all other medical conditions. Non-COVID-19 hospital admissions plummeted, and all elective surgeries and procedures were put on hold, depriving many people of medical care they badly needed. Emergency department (ED) visits also declined dramatically, including the usual flow of heart attacks, stroke, pulmonary embolus, asthma attacks, etc. The minimization of driving greatly reduced the admission of accident victims to EDs. Colonoscopies, cardiac stents, hip replacements, MRIs, mammography, and other procedures that are vital to maintain health and quality of life were halted. Dentists shuttered their practices due to the high risk of infection from exposure to oral secretions and breathing. One can only imagine the suffering of having a toothache with no dental help available, and how that might lead to narcotic abuse.
Social health. The imperative of social distancing disrupted most ordinary human activities, such as dining out, sitting in an auditorium for Grand Rounds or a lecture, visiting friends at their homes, the cherished interactions between grandparents and grandchildren (the lack of which I painfully experienced), and even seeing each other’s smiles behind the ubiquitous masks. And forget about hugging or kissing. The aversion to being near anyone who is coughing or sneezing led to an adaptive social paranoia and the social shunning of anyone who appeared to have an upper respiratory infection, even if it was unrelated to COVID-19.
Redemption for the pharmaceutical industry. The deadly pandemic intensified the public’s awareness of the importance of developing treatments and vaccines for COVID-19. The often-demonized pharmaceutical companies, with their extensive R&D infrastructure, emerged as a major source of hope for discovering an effective treatment for the coronavirus infection, or—better still—one or more vaccines that will enable society to return to its normal functions. It was quite impressive how many pharmaceutical companies “came to the rescue” with clinical trials to repurpose existing medications or to develop new ones. It was very encouraging to see multiple vaccine candidates being developed and expedited for testing around the world. A process that usually takes years was reduced to a few months, thanks to the existing technical infrastructure and thousands of scientists who enable rapid drug development. It is possible that the public may gradually modify its perception of the pharmaceutical industry from a “corporate villain” to an “indispensable health industry” for urgent medical crises such as a pandemic, and also for hundreds of medical diseases that are still in need of safe, effective therapies.
Economic burden. The unimaginable nightmare scenario of a total shutdown of all businesses led to the unprecedented loss of millions of jobs and livelihoods, reflected in miles-long lines of families at food banks. Overnight, the government switched from worrying about its $20-trillion deficit to printing several more trillion dollars to rescue the economy from collapse. The huge magnitude of a trillion can be appreciated if one is aware that it takes roughly 32 years to count to 1 billion, and 32,000 years to count to 1 trillion. Stimulating the economy while the gross domestic product threatens to sink by terrifying percentages (20% to 30%) was urgently needed, even though it meant mortgaging the future, especially when interest rates, and servicing the debt, will inevitably rise from the current zero to much higher levels in the future. The collapse of the once-thriving airline industry (bookings were down an estimated 98%) is an example of why desperate measures were needed to salvage an economy paralyzed by a viral pandemic.
Continue to: Political repercussions
Political repercussions. In our already hyperpartisan country, the COVID-19 crisis created more fissures across party lines. The blame game escalated as each side tried to exploit the crisis for political gain during a presidential election year. None of the leaders, from mayors to governors to the president, had any notion of how to wisely manage an unforeseen catastrophic pandemic. Thus, a political cacophony has developed, further exacerbating the public’s anxiety and uncertainty, especially about how and when the pandemic will end.
Education disruption. Never before have all schools and colleges around the country abruptly closed and sent students of all ages to shelter at home. Massive havoc ensued, with a wholesale switch to solitary online learning, the loss of the unique school and college social experience in the classroom and on campus, and the loss of experiencing commencement to receive a diploma (an important milestone for every graduate). Even medical students were not allowed to complete their clinical rotations and were sent home to attend online classes. A complete paradigm shift emerged about entrance exams: the SAT and ACT were eliminated for college applicants, and the MCAT for medical school applicants. This was unthinkable before the pandemic descended upon us, but benchmarks suddenly evaporated to adjust to the new reality. Then there followed disastrous financial losses by institutions of higher learning as well as academic medical centers and teaching hospitals, all slashing their budgets, furloughing employees, cutting salaries, and eliminating programs. Even the “sacred” tenure of senior faculty became a casualty of the financial “exigency.” Children’s nutrition suffered, especially among those in lower socioeconomic groups for whom the main meal of the day was the school lunch, and was made worse by their parents’ loss of income. For millions of people, the emotional toll was inevitable following the draconian measure of closing all educational institutions to contain the spread of the pandemic.
Family burden. Sheltering at home might have been fun for a few days, but after many weeks, it festered into a major stress, especially for those living in a small house, condominium, or apartment. The resilience of many families was tested as the exercise of freedoms collided with the fear of getting infected. Families were deprived of celebrating birthdays, weddings, funerals, graduation parties, retirement parties, Mother’s Day, Father’s Day, and various religious holidays, including Easter, Passover, and Eid al-Fitr.
Sexual burden. Intimacy and sexual contact between consenting adults living apart were sacrificed on the altar of the pernicious viral pandemic. Mandatory social distancing of 6 feet or more to avoid each other’s droplets emanating from simple speech, not just sneezing or coughing, makes intimacy practically impossible. Thus, physical closeness became taboo, and avoiding another person’s saliva or body secretions became a must to avoid contracting the virus. Being single was quite a lonely experience during this pandemic!
Entertainment deprivation. Americans are known to thrive on an extensive diet of spectator sports. Going to football, basketball, baseball, or hockey games to root for one’s team is intrinsically American. The pursuit of happiness extends to attending concerts, movies, Broadway shows, theme parks, and cruises with thousands of others. The pandemic ripped all those pleasurable leisure activities from our daily lives, leaving a big hole in people’s lives at the precise time fun activities were needed as a useful diversion from the dismal stress of a pandemic. To make things worse, it is uncertain when (if ever) such group activities will be restored, especially if the pandemic returns with another wave. But optimists would hurry to remind us that the “Roaring 20s” blossomed in the decade following the 1918 Spanish Flu pandemic.
Continue to: Legal system
Legal system. Astounding changes were instigated by the pandemic, such as the release of thousands of inmates, including felons, to avoid the spread of the virus in crowded prisons. For us psychiatrists, the silver lining in that unexpected action is that many of those released were patients with mental illness who were incarcerated because of the lack of hospitals that would take them. The police started issuing citations instead of arresting and jailing violators. Enforcement of the law was welcome when it targeted those who gouged the public for personal profit during the scarcity of masks, sanitizers, or even toilet paper and soap.
Medical practice. In addition to delaying medical care for patients, the freeze on so-called elective surgeries or procedures (many of which were actually necessary) was financially ruinous for physicians. Another regrettable consequence of the pandemic is a drop in pediatric vaccinations because parents were reluctant to take their children to the pediatrician. On a more positive note, the massive switch to telehealth was advantageous for both patients and psychiatrists because this technology is well-suited for psychiatric care. Fortunately, regulations that hampered telepsychiatry practice were substantially loosened or eliminated, and even the usually sacrosanct HIPAA regulations were temporarily sidelined.
Medical research. Both human and animal research came to a screeching halt, and many research assistants were furloughed. Data collection was disrupted, and a generation of scientific and medical discoveries became a casualty of the pandemic.
Medical literature. It was stunning to see how quickly COVID-19 occupied most of the pages of prominent journals. The scholarly articles were frankly quite useful, covering topics ranging from risk factors to early symptoms to treatment and pathophysiology across multiple organs. As with other paradigm shifts, there was an accelerated publication push, sometimes with expedited peer reviews to inform health care workers and the public while the pandemic was still raging. However, a couple of very prominent journals had to retract flawed articles that were hastily published without the usual due diligence and rigorous peer review. The pandemic clearly disrupted the science publishing process.
Travel effects. The steep reduction of flights (by 98%) was financially catastrophic, not only for airline companies but to business travel across the country. However, fewer cars on the road resulted in fewer accidents and deaths, and also reduced pollution. Paradoxically, to prevent crowding in subways, trains, and buses, officials reversed their traditional instructions and advised the public to drive their own cars instead of using public transportation!
Continue to: Heroism of front-line medical personnel
Heroism of front-line medical personnel. Everyone saluted and prayed for the health care professionals working at the bedside of highly infectious patients who needed 24/7 intensive care. Many have died while carrying out the noble but hazardous medical duties. Those heroes deserve our lasting respect and admiration.
The COVID-19 pandemic insidiously permeated and altered every aspect of our complex society and revealed how fragile our “normal lifestyle” really is. It is possible that nothing will ever be the same again, and an uneasy sense of vulnerability will engulf us as we cautiously return to a “new normal.” Even our language has expanded with the lexicon of pandemic terminology (Table). We all pray and hope that this plague never returns. And let’s hope one or more vaccines are developed soon so we can manage future recurrences like the annual flu season. In the meantime, keep your masks and sanitizers close by…
Postscript: Shortly after I completed this editorial, the ongoing COVID-19 plague was overshadowed by the scourge of racism, with massive protests, at times laced by violence, triggered by the death of a black man in custody of the police, under condemnable circumstances. The COVID-19 pandemic and the necessary social distancing it requires were temporarily ignored during the ensuing protests. The combined effect of those overlapping scourges are jarring to the country’s psyche, complicating and perhaps sabotaging the social recovery from the pandemic.
Stop calling it ‘behavioral health’: Psychiatry is much more
Psychiatry has been historically plagued by absurd misnomers. It started with the laughable “mental hygiene,” coined by William Sweetser, MD, in 1843, 1 year before the original 13 members of the Association of Medical Superintendents of American Institutions for the Insane established what in 1921 was renamed the American Psychiatric Association. Mental hygiene evokes an image of psychiatrists scrubbing the brains of mentally ill patients with soap and water! That term was neither medically nor scientifically appropriate, but it stuck for decades.
Enter “mental health.” In 1949, the National Institute of Mental Health was established. It is the 5th oldest of the 27 Institutes and Centers of the National Institutes of Health. Then, in 1963, Congress passed the Community Mental Health Act, which established Community Mental Health Centers around the country. It is perplexing that the term “health” was used instead of “illness,” when psychiatry is a medical specialty that treats mental disorders. Health is certainly the goal of all medical specialties, but cardiology was never called “heart health,” neurology was never called “brain health,” and pediatrics was never called “children’s health.” Like all its sister medical specialties, psychiatry treats disease and syndromes, but somehow, it has been transmogrified into “mental health.” Perhaps it was meant to be a euphemism to disguise and avert the unfortunate stigma associated with mental illness back during the institutionalization era.
The advent of ‘behavioral health’
Then suddenly, the term “behavioral health” was coined and began to be used as a substitute for psychiatry, further distorting psychiatry’s medical identity. Behavioral health is completely different from psychiatry. It refers to healthy behaviors that people should uphold throughout their lives to maintain their overall health and well-being, including eating a balanced diet, exercising regularly, avoiding tobacco and drugs of abuse, practicing safe sex, and establishing meaningful social relationships. So behavioral health promotes a healthy lifestyle, and that could very aptly apply to cardiology, pulmonology, nephrology, or hepatology, where good nutrition and avoiding weight gain, smoking, and sedentary living can reduce the risk for various medical diseases and early mortality. For dermatologists, behavioral health is avoiding sunburn, and for dentists, it is regular brushing and flossing.
Thus, behavioral health is a term that broadly promotes physical health and well-being, and should not be conflated with mental disorders. It is by no means synonymous with psychiatry, a medical discipline that addresses serious disorders of thought, emotions, affect, delusions, hallucinations, suicide, homicide, impulsivity, obsessions and compulsions, motivation, memory, attention, and judgment. Psychiatry is far more than behaviors that promote healthy living. Psychiatry contends with acute and chronic mental disorders, similar to other chronic medical conditions such as chronic heart, lung, gastrointestinal, or kidney diseases. Psychiatric disorders can emerge in individuals despite—and irrespective of—a healthy lifestyle promoted by behavioral health. Most psychiatric disorders have been shown to be highly genetic, and can be triggered by gene-environment interactions, even in the context of a healthful life that behavioral health advocates and fecundates.
I dislike conspiracy theories, but it is legitimate to inquire: Was there a “malicious intent” by insurance companies and managed-care entities when they abruptly replaced the medically accurate term “psychiatry” with the counterfactual “behavioral health”? Did they intend to portray psychiatry as somehow “different” from other medical specialties? Did this phraseological acrobatics facilitate and justify the carving out of psychiatric and addiction care, cursed with an anemic budget and absence of parity for persons with psychiatric brain disorders? Somehow, using behavioral health instead of psychiatry has the unfortunate connotation that patients with mental illness are “misbehaving” by not practicing healthy living, rather than being genuinely medically ill through no fault of their own. That’s a surreptitious de-medicalization of psychiatric brain disorders. It is very likely that the same companies that propagated behavioral health are the ones who came up with the demeaning term “providers,” which lumps physicians with nonphysicians, diluting the medical identify of psychiatrists, and implying a non-equivalence of psychiatric disorders with other medical conditions, which perpetuates stigma.
An erroneous epithet
We are psychiatric physicians, not “behavioral health advisors.” We are graduates of medical schools where we had clinical psychiatric experiences rotating with internal medicine, surgery, obstetrics and gynecology, and pediatrics. We did not have behavioral health rotations. And after graduating with an MD, we spent 4 additional years in psychiatric residency training, not behavioral health training, and we treated very sick patients in emergency departments and on inpatient units, not on behavioral health wards. We receive our board certification from the American Board of Psychiatry and Neurology, not from a behavioral health board. As psychiatrists, we are regularly consulted on the cases of medical and surgical patients who develop psychiatric disorders, which has absolutely nothing to do with behavioral health. Our psychiatric outpatient clinics require extensive medical knowledge and psychopharmacological skills, not behavioral health.
As part of our work as physicians and psychiatrists, we do counsel patients on adopting a healthy lifestyle because many of them have comorbid medical conditions such as diabetes, hypertension, dyslipidemia, chronic obstructive pulmonary disease, asthma, and kidney and gastrointestinal disorders. We practice collaborative care with primary care physicians so we can jointly manage patients’ physical and mental disorders, and help them optimize their lifestyles. Thus, behavioral health is a tiny component of what psychiatrists do, and it does not come close to defining our comprehensive medical care. Similarly, neurologists and cardiologists should not be labeled as behavior health specialties simply because they counsel their patients on how to lower the risk of strokes or heart attacks due to unhealthy lifestyles.
So, let’s call a spade a spade. Psychiatry is psychiatric medical care, not behavioral health. Let’s abandon this erroneous epithet and change the signs outside hospitals and clinics to “psychiatric medicine” facilities. I guarantee that orthopedists would not like it all if you call their specialty “bone health,” and may break your leg if you label their discipline “bone hygiene”… after washing it with soap and water, of course!
Psychiatry has been historically plagued by absurd misnomers. It started with the laughable “mental hygiene,” coined by William Sweetser, MD, in 1843, 1 year before the original 13 members of the Association of Medical Superintendents of American Institutions for the Insane established what in 1921 was renamed the American Psychiatric Association. Mental hygiene evokes an image of psychiatrists scrubbing the brains of mentally ill patients with soap and water! That term was neither medically nor scientifically appropriate, but it stuck for decades.
Enter “mental health.” In 1949, the National Institute of Mental Health was established. It is the 5th oldest of the 27 Institutes and Centers of the National Institutes of Health. Then, in 1963, Congress passed the Community Mental Health Act, which established Community Mental Health Centers around the country. It is perplexing that the term “health” was used instead of “illness,” when psychiatry is a medical specialty that treats mental disorders. Health is certainly the goal of all medical specialties, but cardiology was never called “heart health,” neurology was never called “brain health,” and pediatrics was never called “children’s health.” Like all its sister medical specialties, psychiatry treats disease and syndromes, but somehow, it has been transmogrified into “mental health.” Perhaps it was meant to be a euphemism to disguise and avert the unfortunate stigma associated with mental illness back during the institutionalization era.
The advent of ‘behavioral health’
Then suddenly, the term “behavioral health” was coined and began to be used as a substitute for psychiatry, further distorting psychiatry’s medical identity. Behavioral health is completely different from psychiatry. It refers to healthy behaviors that people should uphold throughout their lives to maintain their overall health and well-being, including eating a balanced diet, exercising regularly, avoiding tobacco and drugs of abuse, practicing safe sex, and establishing meaningful social relationships. So behavioral health promotes a healthy lifestyle, and that could very aptly apply to cardiology, pulmonology, nephrology, or hepatology, where good nutrition and avoiding weight gain, smoking, and sedentary living can reduce the risk for various medical diseases and early mortality. For dermatologists, behavioral health is avoiding sunburn, and for dentists, it is regular brushing and flossing.
Thus, behavioral health is a term that broadly promotes physical health and well-being, and should not be conflated with mental disorders. It is by no means synonymous with psychiatry, a medical discipline that addresses serious disorders of thought, emotions, affect, delusions, hallucinations, suicide, homicide, impulsivity, obsessions and compulsions, motivation, memory, attention, and judgment. Psychiatry is far more than behaviors that promote healthy living. Psychiatry contends with acute and chronic mental disorders, similar to other chronic medical conditions such as chronic heart, lung, gastrointestinal, or kidney diseases. Psychiatric disorders can emerge in individuals despite—and irrespective of—a healthy lifestyle promoted by behavioral health. Most psychiatric disorders have been shown to be highly genetic, and can be triggered by gene-environment interactions, even in the context of a healthful life that behavioral health advocates and fecundates.
I dislike conspiracy theories, but it is legitimate to inquire: Was there a “malicious intent” by insurance companies and managed-care entities when they abruptly replaced the medically accurate term “psychiatry” with the counterfactual “behavioral health”? Did they intend to portray psychiatry as somehow “different” from other medical specialties? Did this phraseological acrobatics facilitate and justify the carving out of psychiatric and addiction care, cursed with an anemic budget and absence of parity for persons with psychiatric brain disorders? Somehow, using behavioral health instead of psychiatry has the unfortunate connotation that patients with mental illness are “misbehaving” by not practicing healthy living, rather than being genuinely medically ill through no fault of their own. That’s a surreptitious de-medicalization of psychiatric brain disorders. It is very likely that the same companies that propagated behavioral health are the ones who came up with the demeaning term “providers,” which lumps physicians with nonphysicians, diluting the medical identify of psychiatrists, and implying a non-equivalence of psychiatric disorders with other medical conditions, which perpetuates stigma.
An erroneous epithet
We are psychiatric physicians, not “behavioral health advisors.” We are graduates of medical schools where we had clinical psychiatric experiences rotating with internal medicine, surgery, obstetrics and gynecology, and pediatrics. We did not have behavioral health rotations. And after graduating with an MD, we spent 4 additional years in psychiatric residency training, not behavioral health training, and we treated very sick patients in emergency departments and on inpatient units, not on behavioral health wards. We receive our board certification from the American Board of Psychiatry and Neurology, not from a behavioral health board. As psychiatrists, we are regularly consulted on the cases of medical and surgical patients who develop psychiatric disorders, which has absolutely nothing to do with behavioral health. Our psychiatric outpatient clinics require extensive medical knowledge and psychopharmacological skills, not behavioral health.
As part of our work as physicians and psychiatrists, we do counsel patients on adopting a healthy lifestyle because many of them have comorbid medical conditions such as diabetes, hypertension, dyslipidemia, chronic obstructive pulmonary disease, asthma, and kidney and gastrointestinal disorders. We practice collaborative care with primary care physicians so we can jointly manage patients’ physical and mental disorders, and help them optimize their lifestyles. Thus, behavioral health is a tiny component of what psychiatrists do, and it does not come close to defining our comprehensive medical care. Similarly, neurologists and cardiologists should not be labeled as behavior health specialties simply because they counsel their patients on how to lower the risk of strokes or heart attacks due to unhealthy lifestyles.
So, let’s call a spade a spade. Psychiatry is psychiatric medical care, not behavioral health. Let’s abandon this erroneous epithet and change the signs outside hospitals and clinics to “psychiatric medicine” facilities. I guarantee that orthopedists would not like it all if you call their specialty “bone health,” and may break your leg if you label their discipline “bone hygiene”… after washing it with soap and water, of course!
Psychiatry has been historically plagued by absurd misnomers. It started with the laughable “mental hygiene,” coined by William Sweetser, MD, in 1843, 1 year before the original 13 members of the Association of Medical Superintendents of American Institutions for the Insane established what in 1921 was renamed the American Psychiatric Association. Mental hygiene evokes an image of psychiatrists scrubbing the brains of mentally ill patients with soap and water! That term was neither medically nor scientifically appropriate, but it stuck for decades.
Enter “mental health.” In 1949, the National Institute of Mental Health was established. It is the 5th oldest of the 27 Institutes and Centers of the National Institutes of Health. Then, in 1963, Congress passed the Community Mental Health Act, which established Community Mental Health Centers around the country. It is perplexing that the term “health” was used instead of “illness,” when psychiatry is a medical specialty that treats mental disorders. Health is certainly the goal of all medical specialties, but cardiology was never called “heart health,” neurology was never called “brain health,” and pediatrics was never called “children’s health.” Like all its sister medical specialties, psychiatry treats disease and syndromes, but somehow, it has been transmogrified into “mental health.” Perhaps it was meant to be a euphemism to disguise and avert the unfortunate stigma associated with mental illness back during the institutionalization era.
The advent of ‘behavioral health’
Then suddenly, the term “behavioral health” was coined and began to be used as a substitute for psychiatry, further distorting psychiatry’s medical identity. Behavioral health is completely different from psychiatry. It refers to healthy behaviors that people should uphold throughout their lives to maintain their overall health and well-being, including eating a balanced diet, exercising regularly, avoiding tobacco and drugs of abuse, practicing safe sex, and establishing meaningful social relationships. So behavioral health promotes a healthy lifestyle, and that could very aptly apply to cardiology, pulmonology, nephrology, or hepatology, where good nutrition and avoiding weight gain, smoking, and sedentary living can reduce the risk for various medical diseases and early mortality. For dermatologists, behavioral health is avoiding sunburn, and for dentists, it is regular brushing and flossing.
Thus, behavioral health is a term that broadly promotes physical health and well-being, and should not be conflated with mental disorders. It is by no means synonymous with psychiatry, a medical discipline that addresses serious disorders of thought, emotions, affect, delusions, hallucinations, suicide, homicide, impulsivity, obsessions and compulsions, motivation, memory, attention, and judgment. Psychiatry is far more than behaviors that promote healthy living. Psychiatry contends with acute and chronic mental disorders, similar to other chronic medical conditions such as chronic heart, lung, gastrointestinal, or kidney diseases. Psychiatric disorders can emerge in individuals despite—and irrespective of—a healthy lifestyle promoted by behavioral health. Most psychiatric disorders have been shown to be highly genetic, and can be triggered by gene-environment interactions, even in the context of a healthful life that behavioral health advocates and fecundates.
I dislike conspiracy theories, but it is legitimate to inquire: Was there a “malicious intent” by insurance companies and managed-care entities when they abruptly replaced the medically accurate term “psychiatry” with the counterfactual “behavioral health”? Did they intend to portray psychiatry as somehow “different” from other medical specialties? Did this phraseological acrobatics facilitate and justify the carving out of psychiatric and addiction care, cursed with an anemic budget and absence of parity for persons with psychiatric brain disorders? Somehow, using behavioral health instead of psychiatry has the unfortunate connotation that patients with mental illness are “misbehaving” by not practicing healthy living, rather than being genuinely medically ill through no fault of their own. That’s a surreptitious de-medicalization of psychiatric brain disorders. It is very likely that the same companies that propagated behavioral health are the ones who came up with the demeaning term “providers,” which lumps physicians with nonphysicians, diluting the medical identify of psychiatrists, and implying a non-equivalence of psychiatric disorders with other medical conditions, which perpetuates stigma.
An erroneous epithet
We are psychiatric physicians, not “behavioral health advisors.” We are graduates of medical schools where we had clinical psychiatric experiences rotating with internal medicine, surgery, obstetrics and gynecology, and pediatrics. We did not have behavioral health rotations. And after graduating with an MD, we spent 4 additional years in psychiatric residency training, not behavioral health training, and we treated very sick patients in emergency departments and on inpatient units, not on behavioral health wards. We receive our board certification from the American Board of Psychiatry and Neurology, not from a behavioral health board. As psychiatrists, we are regularly consulted on the cases of medical and surgical patients who develop psychiatric disorders, which has absolutely nothing to do with behavioral health. Our psychiatric outpatient clinics require extensive medical knowledge and psychopharmacological skills, not behavioral health.
As part of our work as physicians and psychiatrists, we do counsel patients on adopting a healthy lifestyle because many of them have comorbid medical conditions such as diabetes, hypertension, dyslipidemia, chronic obstructive pulmonary disease, asthma, and kidney and gastrointestinal disorders. We practice collaborative care with primary care physicians so we can jointly manage patients’ physical and mental disorders, and help them optimize their lifestyles. Thus, behavioral health is a tiny component of what psychiatrists do, and it does not come close to defining our comprehensive medical care. Similarly, neurologists and cardiologists should not be labeled as behavior health specialties simply because they counsel their patients on how to lower the risk of strokes or heart attacks due to unhealthy lifestyles.
So, let’s call a spade a spade. Psychiatry is psychiatric medical care, not behavioral health. Let’s abandon this erroneous epithet and change the signs outside hospitals and clinics to “psychiatric medicine” facilities. I guarantee that orthopedists would not like it all if you call their specialty “bone health,” and may break your leg if you label their discipline “bone hygiene”… after washing it with soap and water, of course!
The cataclysmic COVID-19 pandemic: THIS CHANGES EVERYTHING!
It was unthinkable, but it has happened. A virulent and invisible virus, 10 microns in size, with no vaccine or cure yet, shut down our nation, the third largest country in the world with 330 million people. Overnight, our thriving cities became ghost towns. Schools were closed. Millions of businesses, restaurants, and stores were abruptly shuttered. Sporting events were instantly canceled. Air travel came to a halt.
The largest economy in the world started to tank. Millions of people lost their jobs and were forced to stay home. The vital structures of society were dismantled. Our vibrant culture came to a screeching halt. It’s a nightmare scenario that even the most imaginative science fiction writers could not have envisioned. By any measure, the coronavirus disease 2019 (COVID-19) pandemic unraveled everything, and became a human catastrophe and a social calamity reminiscent of the deadly 1918 influenza pandemic, or the devastating plagues that decimated Europe during the Middle Ages.
The human toll in death and suffering was the real disaster. Emergency departments and hospitals filled up with victims of the scourge, sickly and unable to breathe as the virus hijacked their red blood cells and lungs, and destroyed their alveoli. Compounding the disaster was a lack of medical supplies. The country was clearly caught off-guard, completely unprepared for the scale of the pandemic and the massive onslaught of desperately ill people requiring intensive care and special equipment. In addition, health care staff became stretched beyond the limit, and entire hospitals were transformed overnight into highly specialized ICUs. Medical care for millions with non-COVID-19 conditions was put on hold so that vital resources could be diverted to the desperately ill victims of these infections. Many physicians, nurses, and respiratory therapists—laudable heroes—succumbed to the perverse virus exhaled by their patients.
Insidious social effects
COVID-19 is not only a murderer, but also a thief. It stole our Spring; our religious holidays (Easter and Passover); classroom education in schools and colleges; the Prom; weddings; graduation ceremonies; proper funerals; concerts; football, basketball, hockey, and baseball games; Broadway shows; and even data from animal research. More important, it robbed us of our peace of mind, our liberty, and our pursuit of small pleasures such as family gatherings or schmoozing with friends at a nice restaurant. COVID-19 is a cruel, dastardly scoundrel.
I write this editorial as I sit at home, which I have not left for several weeks, like hundreds of millions in our country and around the world. We were all glued to TV news or the internet to learn about the latest updates, including the grim news of those who got infected, hospitalized, or passed away. Fear of dying permeated all age groups, especially those who were older and infirmed.
Making it worse was the relentless uncertainty. When will it end? Gradually or suddenly? When is it going to be safe to go to work again, or to visit our loved ones and our friends? When can we see our patients face-to-face instead of remotely by phone or video conferencing? When can we have live meetings instead of virtual video conferences? When will stores open so we can shop? When can we take our children or grandchildren to a baseball game or a show? Will the virus return next winter for another cycle of mayhem and social paralysis? When will the economy start to rebound, and how long will that take? Will our retirement accounts recoup their losses? So many questions with no clear answers. A malignant uncertainty, indeed.
And there are our patients who live with anxiety and depression, whose anguish is intensifying as they sit alone in their apartments or homes, struggling to cope with this sudden, overwhelming stress. How will they react to this pandemic? Obviously, a life-threatening event such as a deadly pandemic with no cure is likely to produce an acute stress reaction and, ultimately, posttraumatic stress disorder (PTSD). And if COVID-19 returns next year for another unwelcome visit, PTSD symptoms will get a booster shot and lead to severe anxiety, depression, or suicide. Psychiatrists and other mental health professionals, who were already stretched thin, must contend with another crisis that has destabilized millions of patients receiving psychiatric care, or new patients who seek help for themselves or their family members.
Continue to: One intervention that is emerging...
One intervention that is emerging on a large scale is online therapy. This includes reassurance and supportive therapy, cognitive-behavioral therapy, relaxation techniques, stress management, resilience training, mindfulness, and online group therapy. Those therapies can be effective for stress-induced anxiety and dysphoria when pharmacotherapy is not available, and can provide patients with tools and techniques that can be implemented by the patients themselves in the absence of a physician or nurse practitioner to prescribe a medication.
Lessons learned
This pandemic has taught us many lessons: that life as we know it should not be taken for granted, and can change drastically overnight; that human life is fragile and can be destroyed rapidly and ruthlessly on an unimaginable scale by an invisible enemy; that scientific drug development research by the often maligned pharmaceutical industry is indispensable to our well-being; that policymakers must always prepare for the worst and must have a well-designed disaster plan; that modifying human behavior and full compliance with public health measures are vital and can be the most effective way to prevent the spread of catastrophic pandemics, viral or otherwise; that we must all learn how to be resilient to cope with solitude and restricted mobility or socialization; that the human ingenuity and innovation that created technologies to enable virtual connectivity among us, even when we are isolated, has been a lifesaver during health crises such as the COVID-19 pandemic; that the clinicians and health care workers treating highly infectious and desperately ill patients are genuine heroes who deserve our respect and gratitude; and that magnificent altruism outstrips and outshines the selfish hoarding and profiteering that may emerge during life-threatening pandemics.
And that we shall overcome this horrid pandemic, a ghastly tribulation that changed everything.
It was unthinkable, but it has happened. A virulent and invisible virus, 10 microns in size, with no vaccine or cure yet, shut down our nation, the third largest country in the world with 330 million people. Overnight, our thriving cities became ghost towns. Schools were closed. Millions of businesses, restaurants, and stores were abruptly shuttered. Sporting events were instantly canceled. Air travel came to a halt.
The largest economy in the world started to tank. Millions of people lost their jobs and were forced to stay home. The vital structures of society were dismantled. Our vibrant culture came to a screeching halt. It’s a nightmare scenario that even the most imaginative science fiction writers could not have envisioned. By any measure, the coronavirus disease 2019 (COVID-19) pandemic unraveled everything, and became a human catastrophe and a social calamity reminiscent of the deadly 1918 influenza pandemic, or the devastating plagues that decimated Europe during the Middle Ages.
The human toll in death and suffering was the real disaster. Emergency departments and hospitals filled up with victims of the scourge, sickly and unable to breathe as the virus hijacked their red blood cells and lungs, and destroyed their alveoli. Compounding the disaster was a lack of medical supplies. The country was clearly caught off-guard, completely unprepared for the scale of the pandemic and the massive onslaught of desperately ill people requiring intensive care and special equipment. In addition, health care staff became stretched beyond the limit, and entire hospitals were transformed overnight into highly specialized ICUs. Medical care for millions with non-COVID-19 conditions was put on hold so that vital resources could be diverted to the desperately ill victims of these infections. Many physicians, nurses, and respiratory therapists—laudable heroes—succumbed to the perverse virus exhaled by their patients.
Insidious social effects
COVID-19 is not only a murderer, but also a thief. It stole our Spring; our religious holidays (Easter and Passover); classroom education in schools and colleges; the Prom; weddings; graduation ceremonies; proper funerals; concerts; football, basketball, hockey, and baseball games; Broadway shows; and even data from animal research. More important, it robbed us of our peace of mind, our liberty, and our pursuit of small pleasures such as family gatherings or schmoozing with friends at a nice restaurant. COVID-19 is a cruel, dastardly scoundrel.
I write this editorial as I sit at home, which I have not left for several weeks, like hundreds of millions in our country and around the world. We were all glued to TV news or the internet to learn about the latest updates, including the grim news of those who got infected, hospitalized, or passed away. Fear of dying permeated all age groups, especially those who were older and infirmed.
Making it worse was the relentless uncertainty. When will it end? Gradually or suddenly? When is it going to be safe to go to work again, or to visit our loved ones and our friends? When can we see our patients face-to-face instead of remotely by phone or video conferencing? When can we have live meetings instead of virtual video conferences? When will stores open so we can shop? When can we take our children or grandchildren to a baseball game or a show? Will the virus return next winter for another cycle of mayhem and social paralysis? When will the economy start to rebound, and how long will that take? Will our retirement accounts recoup their losses? So many questions with no clear answers. A malignant uncertainty, indeed.
And there are our patients who live with anxiety and depression, whose anguish is intensifying as they sit alone in their apartments or homes, struggling to cope with this sudden, overwhelming stress. How will they react to this pandemic? Obviously, a life-threatening event such as a deadly pandemic with no cure is likely to produce an acute stress reaction and, ultimately, posttraumatic stress disorder (PTSD). And if COVID-19 returns next year for another unwelcome visit, PTSD symptoms will get a booster shot and lead to severe anxiety, depression, or suicide. Psychiatrists and other mental health professionals, who were already stretched thin, must contend with another crisis that has destabilized millions of patients receiving psychiatric care, or new patients who seek help for themselves or their family members.
Continue to: One intervention that is emerging...
One intervention that is emerging on a large scale is online therapy. This includes reassurance and supportive therapy, cognitive-behavioral therapy, relaxation techniques, stress management, resilience training, mindfulness, and online group therapy. Those therapies can be effective for stress-induced anxiety and dysphoria when pharmacotherapy is not available, and can provide patients with tools and techniques that can be implemented by the patients themselves in the absence of a physician or nurse practitioner to prescribe a medication.
Lessons learned
This pandemic has taught us many lessons: that life as we know it should not be taken for granted, and can change drastically overnight; that human life is fragile and can be destroyed rapidly and ruthlessly on an unimaginable scale by an invisible enemy; that scientific drug development research by the often maligned pharmaceutical industry is indispensable to our well-being; that policymakers must always prepare for the worst and must have a well-designed disaster plan; that modifying human behavior and full compliance with public health measures are vital and can be the most effective way to prevent the spread of catastrophic pandemics, viral or otherwise; that we must all learn how to be resilient to cope with solitude and restricted mobility or socialization; that the human ingenuity and innovation that created technologies to enable virtual connectivity among us, even when we are isolated, has been a lifesaver during health crises such as the COVID-19 pandemic; that the clinicians and health care workers treating highly infectious and desperately ill patients are genuine heroes who deserve our respect and gratitude; and that magnificent altruism outstrips and outshines the selfish hoarding and profiteering that may emerge during life-threatening pandemics.
And that we shall overcome this horrid pandemic, a ghastly tribulation that changed everything.
It was unthinkable, but it has happened. A virulent and invisible virus, 10 microns in size, with no vaccine or cure yet, shut down our nation, the third largest country in the world with 330 million people. Overnight, our thriving cities became ghost towns. Schools were closed. Millions of businesses, restaurants, and stores were abruptly shuttered. Sporting events were instantly canceled. Air travel came to a halt.
The largest economy in the world started to tank. Millions of people lost their jobs and were forced to stay home. The vital structures of society were dismantled. Our vibrant culture came to a screeching halt. It’s a nightmare scenario that even the most imaginative science fiction writers could not have envisioned. By any measure, the coronavirus disease 2019 (COVID-19) pandemic unraveled everything, and became a human catastrophe and a social calamity reminiscent of the deadly 1918 influenza pandemic, or the devastating plagues that decimated Europe during the Middle Ages.
The human toll in death and suffering was the real disaster. Emergency departments and hospitals filled up with victims of the scourge, sickly and unable to breathe as the virus hijacked their red blood cells and lungs, and destroyed their alveoli. Compounding the disaster was a lack of medical supplies. The country was clearly caught off-guard, completely unprepared for the scale of the pandemic and the massive onslaught of desperately ill people requiring intensive care and special equipment. In addition, health care staff became stretched beyond the limit, and entire hospitals were transformed overnight into highly specialized ICUs. Medical care for millions with non-COVID-19 conditions was put on hold so that vital resources could be diverted to the desperately ill victims of these infections. Many physicians, nurses, and respiratory therapists—laudable heroes—succumbed to the perverse virus exhaled by their patients.
Insidious social effects
COVID-19 is not only a murderer, but also a thief. It stole our Spring; our religious holidays (Easter and Passover); classroom education in schools and colleges; the Prom; weddings; graduation ceremonies; proper funerals; concerts; football, basketball, hockey, and baseball games; Broadway shows; and even data from animal research. More important, it robbed us of our peace of mind, our liberty, and our pursuit of small pleasures such as family gatherings or schmoozing with friends at a nice restaurant. COVID-19 is a cruel, dastardly scoundrel.
I write this editorial as I sit at home, which I have not left for several weeks, like hundreds of millions in our country and around the world. We were all glued to TV news or the internet to learn about the latest updates, including the grim news of those who got infected, hospitalized, or passed away. Fear of dying permeated all age groups, especially those who were older and infirmed.
Making it worse was the relentless uncertainty. When will it end? Gradually or suddenly? When is it going to be safe to go to work again, or to visit our loved ones and our friends? When can we see our patients face-to-face instead of remotely by phone or video conferencing? When can we have live meetings instead of virtual video conferences? When will stores open so we can shop? When can we take our children or grandchildren to a baseball game or a show? Will the virus return next winter for another cycle of mayhem and social paralysis? When will the economy start to rebound, and how long will that take? Will our retirement accounts recoup their losses? So many questions with no clear answers. A malignant uncertainty, indeed.
And there are our patients who live with anxiety and depression, whose anguish is intensifying as they sit alone in their apartments or homes, struggling to cope with this sudden, overwhelming stress. How will they react to this pandemic? Obviously, a life-threatening event such as a deadly pandemic with no cure is likely to produce an acute stress reaction and, ultimately, posttraumatic stress disorder (PTSD). And if COVID-19 returns next year for another unwelcome visit, PTSD symptoms will get a booster shot and lead to severe anxiety, depression, or suicide. Psychiatrists and other mental health professionals, who were already stretched thin, must contend with another crisis that has destabilized millions of patients receiving psychiatric care, or new patients who seek help for themselves or their family members.
Continue to: One intervention that is emerging...
One intervention that is emerging on a large scale is online therapy. This includes reassurance and supportive therapy, cognitive-behavioral therapy, relaxation techniques, stress management, resilience training, mindfulness, and online group therapy. Those therapies can be effective for stress-induced anxiety and dysphoria when pharmacotherapy is not available, and can provide patients with tools and techniques that can be implemented by the patients themselves in the absence of a physician or nurse practitioner to prescribe a medication.
Lessons learned
This pandemic has taught us many lessons: that life as we know it should not be taken for granted, and can change drastically overnight; that human life is fragile and can be destroyed rapidly and ruthlessly on an unimaginable scale by an invisible enemy; that scientific drug development research by the often maligned pharmaceutical industry is indispensable to our well-being; that policymakers must always prepare for the worst and must have a well-designed disaster plan; that modifying human behavior and full compliance with public health measures are vital and can be the most effective way to prevent the spread of catastrophic pandemics, viral or otherwise; that we must all learn how to be resilient to cope with solitude and restricted mobility or socialization; that the human ingenuity and innovation that created technologies to enable virtual connectivity among us, even when we are isolated, has been a lifesaver during health crises such as the COVID-19 pandemic; that the clinicians and health care workers treating highly infectious and desperately ill patients are genuine heroes who deserve our respect and gratitude; and that magnificent altruism outstrips and outshines the selfish hoarding and profiteering that may emerge during life-threatening pandemics.
And that we shall overcome this horrid pandemic, a ghastly tribulation that changed everything.