User login
Retrospective Review on the Safety and Efficacy of Direct Oral Anticoagulants Compared With Warfarin in Patients With Cirrhosis
Coagulation in patients with cirrhosis is a complicated area of evolving research. Patients with cirrhosis were originally thought to be naturally anticoagulated due to the decreased production of clotting factors and platelets, combined with an increased international normalized ratio (INR).1 New data have shown that patients with cirrhosis are at a concomitant risk of bleeding and thrombosis due to increased platelet aggregation, decreased fibrinolysis, and decreased production of natural anticoagulants such as protein C and antithrombin.1 Traditionally, patients with cirrhosis needing anticoagulation therapy for comorbid conditions, such as nonvalvular atrial fibrillation (NVAF) or venous thromboembolism (VTE) were placed on warfarin therapy. Managing warfarin in patients with cirrhosis poses a challenge to clinicians due to the many food and drug interactions, narrow therapeutic index, and complications with maintaining a therapeutic INR.1
Direct oral anticoagulants (DOACs) have several benefits over warfarin therapy, including convenience, decreased monitoring, decreased drug and dietary restrictions, and faster onset of action.2 Conversely, DOACs undergo extensive hepatic metabolism giving rise to concerns about supratherapeutic drug levels and increased bleeding rates in patients with liver dysfunction.1 Consequently, patients with cirrhosis were excluded from the pivotal trials establishing DOACs for NVAF and VTE treatment. Exclusion of these patients in major clinical trials alongside the challenges of managing warfarin warrant an evaluation of the efficacy and safety of DOACs in patients with cirrhosis.
Recent retrospective studies have examined the use of DOACs in patients with cirrhosis and found favorable results. A retrospective chart review by Intagliata and colleagues consisting of 39 patients with cirrhosis using either a DOAC or warfarin found similar rates of all-cause bleeding and major bleeding between the 2 groups.3 A retrospective cohort study by Hum and colleagues consisting of 45 patients with cirrhosis compared the use of DOACs with warfarin or low-molecular weight heparin (LMWH).4 Hum and colleagues found patients prescribed a DOAC had significantly fewer major bleeding events than did patients using warfarin or LMWH.4 The largest retrospective cohort study consisted of 233 patients with chronic liver disease and found no differences among all-cause bleeding and major bleeding rates between patients using DOACs compared with those of patients using warfarin.5
The purpose of this research is to evaluate the safety and efficacy of DOACs in veteran patients with cirrhosis compared with patients using warfarin.
Methods
A retrospective single-center chart review was conducted at the Michael E. DeBakey Veterans Affairs Medical Center (MEDVAMC) in Houston, Texas, between October 31, 2014 and October 31, 2018. Patients included in the study were adults aged ≥ 18 years with a diagnosis of cirrhosis and prescribed any of the following oral anticoagulants: apixaban, dabigatran, edoxaban, rivaroxaban, or warfarin. Patients prescribed apixaban, dabigatran, edoxaban, or rivaroxaban were collectively grouped into the DOAC group, while patients prescribed warfarin were classified as the standard of care comparator group.
A diagnosis of cirrhosis was confirmed using a combination of the codes from the ninth and tenth editions of the International Classification of Diseases (ICD) for cirrhosis, documentation of diagnostic confirmation by clinicians from the gastroenterology or hepatology services, and positive liver biopsy result. Liver function tests, liver ultrasound results, and FibroSure biomarker assays were used to aid in confirming the diagnosis of cirrhosis but were not considered definitive. Patients were excluded from the trial if they had indications for anticoagulation other than NVAF and VTE and/or were prescribed triple antithrombotic therapy (dual antiplatelet therapy plus an anticoagulant). Patients who switched anticoagulant therapy during the trial period (ie, switched from warfarin to a DOAC) were also excluded from the analysis.
Patient demographic characteristics that were collected included weight; body mass index (BMI); etiology of cirrhosis; Child-Turcotte-Pugh, Model for End-Stage Liver Disease (MELD), and CHA2DS2-VASc score; concomitant antiplatelet, nonsteroidal anti-inflammatory drug (NSAID), proton pump inhibitor (PPI), and histamine-2 receptor antagonist
Two patient lists were used to identify patients for inclusion in the warfarin arm. The first patient list was generated using the US Department of Veterans Affairs (VA) Cirrhosis Tracker, which identified patients with an ICD-9/10 code for cirrhosis and an INR laboratory value. Patients generated from the VA Cirrhosis Tracker with an INR > 1.5 were screened for a warfarin prescription and then evaluated for full study inclusion. The second patient list was generated using the VA Advanced Liver Disease Dashboard which identified patients with ICD-9/10 codes for advanced liver disease and an active warfarin prescription. Patients with an active warfarin prescription were then evaluated for full study inclusion. A single patient list was generated to identify patients for inclusion in the DOAC arm. This patient list was generated using the VA DOAC dashboard, which identified patients with an active DOAC prescription and an ICD-9/10 code for cirrhosis. Patients with an ICD-9/10 code for cirrhosis and prescribed a DOAC were screened for full study inclusion. Patient data were collected from the MEDVAMC Computerized Patient Record System (CPRS) electronic health record (EHR). The research study was approved by the Baylor College of Medicine Institutional Review Board and the VA Office of Research and Development.
Outcomes
The primary endpoint for the study was all-cause bleeding. The secondary endpoints for the study were major bleeding and failed efficacy. Major bleeding was defined using the International Society on Thrombosis and Haemostasis (ISTH) 2005 definition: fatal bleeding, symptomatic bleeding in a critical organ area (ie, intracranial, intraspinal, intraocular, retroperitoneal, intraarticular, pericardial, or intramuscular with compartment syndrome), or bleeding causing a fall in hemoglobin level of > 2 g/dL or leading to the transfusion of ≥ 2 units of red cells.6 Failed efficacy was a combination endpoint that included development of VTE, stroke, myocardial infarction (MI), and/or death. A prespecified subgroup analysis was conducted at the end of the study period to analyze trends in the DOAC and warfarin groups with respect to all-cause bleeding. All-cause bleeding risk was stratified by weight, BMI, Child-Turcotte-Pugh score, MELD score, presence of gastric and/or esophageal varices, active malignancies, percentage of time within therapeutic INR range in the warfarin group, indications for anticoagulation, and antiplatelet, NSAID, PPI, and H2RA therapy.
Statistical Analysis
Data were analyzed using descriptive and inferential statistics. Continuous data were analyzed using the Student t test, and categorical data were analyzed using the Fisher exact test. Previous studies determined an all-cause bleeding rate of 10 to 17% for warfarin compared with 5% for DOACs.7,8 To detect a 12% difference in the all-cause bleeding rate between DOACs and warfarin, 212 patients would be needed to achieve 80% power at an α level of 0.05.
Results
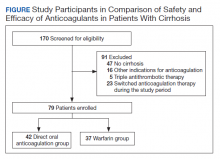
A total of 170 patients were screened, and after applying inclusion and exclusion criteria, 79 patients were enrolled in the study (Figure). The DOAC group included 42 patients, and the warfarin group included 37 patients. In the DOAC group, 69.1% (n = 29) of patients were taking apixaban, 21.4% (n = 9) rivaroxaban, and 9.5% (n = 4) dabigatran. There were no patients prescribed edoxaban during the study period.
Baseline characteristics were similar between the 2 groups except for Child-Turcotte-Pugh score, MELD score, mean INR, and number of days on anticoagulation therapy (Table 1). Most of the patients were male (98.7%), and the mean age was 71 years. The most common causes of cirrhosis were viral (29.1%), nonalcoholic fatty liver disease (NAFLD) (24.1%), multiple causes (22.8%), and alcohol (21.5%). Sixty-two patients (78.5%) had a NVAF indication for anticoagulation. The average CHA2DS2-VASc score was 3.7. Aspirin was prescribed in 51.9% (n = 41) of patients, and PPIs were prescribed in 48.1% (n = 38) of patients. At inclusion, esophageal varices were present in 13 patients and active malignancies were present in 6 patients.
Statistically significant differences in baseline characteristics were found between mean INR, Child-Turcotte-Pugh scores, MELD scores, and number of days on anticoagulant therapy. The mean INR was 1.3 in the DOAC group compared with 2.1 in the warfarin group (P = .0001). Eighty-one percent (n = 34) of patients in the DOAC group had a Child-Turcotte-Pugh score of A compared with 43.2% (n = 16) of patients in the warfarin group (P = .0009). Eight patients in the DOAC group had a Child-Turcotte-Pugh score of B compared with 19 patients in the warfarin group (P = .004). The mean MELD score was 9.4 in the DOAC group compared with 16.3 in the warfarin group (P = .0001). The mean days on anticoagulant therapy was 500.4 days for the DOAC group compared with 1,652.4 days for the warfarin group (P = .0001).
Safety Outcome
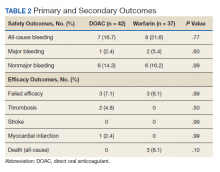
The primary outcome comparing all-cause bleeding rates between patients on DOACs compared with warfarin are listed in Table 2. With respect to the primary outcome, 7 (16.7%) patients on DOACs experienced a bleeding event compared with 8 (21.6%) patients on warfarin (P = .77). No statistically significant differences were detected between the DOAC and warfarin groups with respect to all-cause bleeding. Seven bleeding events occurred in the DOAC group; 1 met the qualification for major bleeding with a suspected gastrointestinal (GI) bleed.6 The other 6 bleeding episodes in the DOAC group consisted of hematoma, epistaxis, hematuria, and hematochezia. Eight bleeding events occurred in the warfarin group; 2 met the qualification for major bleeding with an intracranial hemorrhage and upper GI bleed.6 The other 6 bleeding episodes in the warfarin group consisted of epistaxis, bleeding gums, hematuria, and hematochezia. There were no statistically significant differences between the rates of major bleeding and nonmajor bleeding between the DOAC and warfarin groups.
Efficacy Outcomes
There were 3 events in the DOAC group and 3 events in the warfarin group (P = .99). In the DOAC group, 2 patients experienced a pulmonary embolism, and 1 patient experienced a MI. In the warfarin group, 3 patients died (end-stage heart failure, unknown cause due to death at an outside hospital, and sepsis/organ failure). There were no statistically significant differences between the composite endpoint of failed efficacy or the individual endpoints of VTE, stroke, MI, and death.
Subgroup Analysis
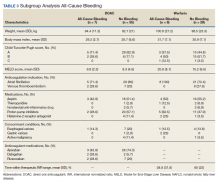
A prespecified subgroup analysis was conducted to determine risk factors for all-cause bleeding within each treatment group (Table 3). No significant trends were observed in the following risk factors: Child-Turcotte-Pugh score, indication for anticoagulation, use of NSAIDs, PPIs or H2RAs, presence of gastric or esophageal varices, active malignancies, and time within therapeutic INR range in the warfarin group. Patients with bleeding events had slightly increased weight and BMI vs patients without bleeding events. Within the warfarin group, patients with bleeding events had slightly elevated MELD scores compared to patients without bleeding events. There was an equal balance of patients prescribed aspirin therapy between the groups with and without bleeding events. Overall, no significant risk factors were identified for all-cause bleeding.
Discussion
Initially, patients with cirrhosis were excluded from DOAC trials due to concerns for increased bleeding risk with hepatically eliminated medications. New retrospective research has concluded that in patients with cirrhosis, DOACs have similar or lower bleeding rates when compared directly to warfarin.9,10
In this study, no statistically significant differences were detected between the primary and secondary outcomes of all-cause bleeding, major bleeding, or failed efficacy. Subgroup analysis did not identify any significant risk factors with respect to all-cause bleeding among patients in the DOAC and warfarin groups. To meet 80% power, 212 patients needed to be enrolled in the study; however, only 79 patients were enrolled, and power was not met. The results of this study should be interpreted cautiously as hypothesis-generating due to the small sample size. Strengths of this study include similar baseline characteristics between the DOAC and warfarin groups, 4-year length of retrospective data review, and availability of both inpatient and outpatient EHR limiting the amount of missing data points.
Baseline characteristics were similar between the groups except for mean INR, Child-Turcotte-Pugh score, MELD score, and number of days on anticoagulation therapy. The difference in mean INR between groups is expected as patients in the warfarin group have a goal INR of 2 to 3 to maintain therapeutic efficacy and safety. INR is not used as a marker of efficacy or safety with DOACs; therefore, a consistent elevation in INR is not expected. Child- Turcotte-Pugh scores are calculated using INR levels.11 When calculating the score, patients with an INR < 1.7 receive 1 point; patients with an INR between 1.7 and 2.3 receive 2 points.11 Therefore, patients in the warfarin group will have artificially inflated Child-Turcotte-Pugh scores as this group has goal INR levels of 2 to 3. This makes Child-Turcotte-Pugh scores unreliable markers of disease severity in patients using warfarin therapy. When the INR scores for patients prescribed warfarin were replaced with values < 1.7, the statistical difference disappeared between the warfarin and DOAC groups. The same effect is seen on MELD scores for patients prescribed warfarin therapy. The MELD score is calculated using INR levels.12 MELD scores also will be artificially elevated in patients prescribed warfarin therapy due to the INR elevation to between 2 and 3. When MELD scores for patients prescribed warfarin were replaced with values similar to those in the DOAC group, the statistical difference disappeared between the warfarin and DOAC groups.
The last statistically significant difference was found in number of days on anticoagulant therapy. This difference was expected as warfarin is the standard of care for anticoagulation treatment in patients with cirrhosis. The first DOAC, dabigatran, was not approved by the US Food and Drug Administration until 2010.13 DOACs have only recently been used in patients with cirrhosis accounting for the statistically significant difference in days on anticoagulation therapy between the warfarin and DOAC groups.
Limitations
The inability to meet power or evaluate adherence and appropriate renal dose adjustments for DOACs limited this study. This study was conducted at a single center in a predominantly male veteran population and therefore may not be generalizable to other populations. A majority of patients in the DOAC group were prescribed apixaban (69.1%), which may have affected the overall rate of major bleeding in the DOAC group. Pivotal trials of apixaban have shown a consistent decreased risk of major bleeding in patients with NVAF or VTE when compared with warfarin.14,15 Therefore, the results of this study may not be generalizable to all DOACs.
An inherent limitation of this study was the inability to collect data verifying adherence in the DOAC group. However, in the warfarin group, percentage of time within the therapeutic INR range of 2 to 3 was collected. While not a direct marker of adherence, this does allow for limited evaluation of therapeutic efficacy and safety within the warfarin group. Last, proper dosing of DOACs in patients with and without adequate renal function was not evaluated in this study.
Conclusions
The results of this study are consistent with other retrospective research and literature reviews. There were no statistically significant differences identified between the rates of all-cause bleeding, major bleeding, and failed efficacy between the DOAC and warfarin groups. DOACs may be a safe alternative to warfarin in patients with cirrhosis requiring anticoagulation for NVAF or VTE, but large randomized trials are required to confirm these results.
1. Qamar A, Vaduganathan M, Greenberger NJ, Giugliano RP. Oral anticoagulation in patients with liver disease. J Am Coll Cardiol. 2018;71(19):2162-2175. doi:10.1016/j.jacc.2018.03.023
2. Priyanka P, Kupec JT, Krafft M, Shah NA, Reynolds GJ. Newer oral anticoagulants in the treatment of acute portal vein thrombosis in patients with and without cirrhosis. Int J Hepatol. 2018;2018:8432781. Published 2018 Jun 5. doi:10.1155/2018/8432781
3. Intagliata NM, Henry ZH, Maitland H, et al. Direct oral anticoagulants in cirrhosis patients pose similar risks of bleeding when compared to traditional anticoagulation. Dig Dis Sci. 2016;61(6):1721-1727. doi:10.1007/s10620-015-4012-2
4. Hum J, Shatzel JJ, Jou JH, Deloughery TG. The efficacy and safety of direct oral anticoagulants vs traditional anticoagulants in cirrhosis. Eur J Haematol. 2017;98(4):393-397. doi:10.1111/ejh.12844
5. Goriacko P, Veltri KT. Safety of direct oral anticoagulants vs warfarin in patients with chronic liver disease and atrial fibrillation. Eur J Haematol. 2018;100(5):488-493. doi:10.1111/ejh.13045
6. Schulman S, Kearon C; Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692-694. doi:10.1111/j.1538-7836.2005.01204.x
7. Rubboli A, Becattini C, Verheugt FW. Incidence, clinical impact and risk of bleeding during oral anticoagulation therapy. World J Cardiol. 2011;3(11):351-358. doi:10.4330/wjc.v3.i11.351
8. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955-962. doi:10.1016/S0140-6736(13)62343-0
9. Hoolwerf EW, Kraaijpoel N, Büller HR, van Es N. Direct oral anticoagulants in patients with liver cirrhosis: A systematic review. Thromb Res. 2018;170:102-108. doi:10.1016/j.thromres.2018.08.011
10. Steuber TD, Howard ML, Nisly SA. Direct oral anticoagulants in chronic liver disease. Ann Pharmacother. 2019;53(10):1042-1049. doi:10.1177/1060028019841582
11. Janevska D, Chaloska-Ivanova V, Janevski V. Hepatocellular carcinoma: risk factors, diagnosis and treatment. Open Access Maced J Med Sci. 2015;3(4):732-736. doi:10.3889/oamjms.2015.111
12. Singal AK, Kamath PS. Model for End-Stage Liver Disease. J Clin Exp Hepatol. 2013;3(1):50-60. doi:10.1016/j.jceh.2012.11.002
13. Joppa SA, Salciccioli J, Adamski J, et al. A practical review of the emerging direct anticoagulants, laboratory monitoring, and reversal agents. J Clin Med. 2018;7(2):29. Published 2018 Feb 11. doi:10.3390/jcm7020029
14. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981-992. doi:10.1056/NEJMoa1107039
15. Agnelli G, Buller HR, Cohen A, et al. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369(9):799-808. doi:10.1056/NEJMoa1302507
Coagulation in patients with cirrhosis is a complicated area of evolving research. Patients with cirrhosis were originally thought to be naturally anticoagulated due to the decreased production of clotting factors and platelets, combined with an increased international normalized ratio (INR).1 New data have shown that patients with cirrhosis are at a concomitant risk of bleeding and thrombosis due to increased platelet aggregation, decreased fibrinolysis, and decreased production of natural anticoagulants such as protein C and antithrombin.1 Traditionally, patients with cirrhosis needing anticoagulation therapy for comorbid conditions, such as nonvalvular atrial fibrillation (NVAF) or venous thromboembolism (VTE) were placed on warfarin therapy. Managing warfarin in patients with cirrhosis poses a challenge to clinicians due to the many food and drug interactions, narrow therapeutic index, and complications with maintaining a therapeutic INR.1
Direct oral anticoagulants (DOACs) have several benefits over warfarin therapy, including convenience, decreased monitoring, decreased drug and dietary restrictions, and faster onset of action.2 Conversely, DOACs undergo extensive hepatic metabolism giving rise to concerns about supratherapeutic drug levels and increased bleeding rates in patients with liver dysfunction.1 Consequently, patients with cirrhosis were excluded from the pivotal trials establishing DOACs for NVAF and VTE treatment. Exclusion of these patients in major clinical trials alongside the challenges of managing warfarin warrant an evaluation of the efficacy and safety of DOACs in patients with cirrhosis.
Recent retrospective studies have examined the use of DOACs in patients with cirrhosis and found favorable results. A retrospective chart review by Intagliata and colleagues consisting of 39 patients with cirrhosis using either a DOAC or warfarin found similar rates of all-cause bleeding and major bleeding between the 2 groups.3 A retrospective cohort study by Hum and colleagues consisting of 45 patients with cirrhosis compared the use of DOACs with warfarin or low-molecular weight heparin (LMWH).4 Hum and colleagues found patients prescribed a DOAC had significantly fewer major bleeding events than did patients using warfarin or LMWH.4 The largest retrospective cohort study consisted of 233 patients with chronic liver disease and found no differences among all-cause bleeding and major bleeding rates between patients using DOACs compared with those of patients using warfarin.5
The purpose of this research is to evaluate the safety and efficacy of DOACs in veteran patients with cirrhosis compared with patients using warfarin.
Methods
A retrospective single-center chart review was conducted at the Michael E. DeBakey Veterans Affairs Medical Center (MEDVAMC) in Houston, Texas, between October 31, 2014 and October 31, 2018. Patients included in the study were adults aged ≥ 18 years with a diagnosis of cirrhosis and prescribed any of the following oral anticoagulants: apixaban, dabigatran, edoxaban, rivaroxaban, or warfarin. Patients prescribed apixaban, dabigatran, edoxaban, or rivaroxaban were collectively grouped into the DOAC group, while patients prescribed warfarin were classified as the standard of care comparator group.
A diagnosis of cirrhosis was confirmed using a combination of the codes from the ninth and tenth editions of the International Classification of Diseases (ICD) for cirrhosis, documentation of diagnostic confirmation by clinicians from the gastroenterology or hepatology services, and positive liver biopsy result. Liver function tests, liver ultrasound results, and FibroSure biomarker assays were used to aid in confirming the diagnosis of cirrhosis but were not considered definitive. Patients were excluded from the trial if they had indications for anticoagulation other than NVAF and VTE and/or were prescribed triple antithrombotic therapy (dual antiplatelet therapy plus an anticoagulant). Patients who switched anticoagulant therapy during the trial period (ie, switched from warfarin to a DOAC) were also excluded from the analysis.
Patient demographic characteristics that were collected included weight; body mass index (BMI); etiology of cirrhosis; Child-Turcotte-Pugh, Model for End-Stage Liver Disease (MELD), and CHA2DS2-VASc score; concomitant antiplatelet, nonsteroidal anti-inflammatory drug (NSAID), proton pump inhibitor (PPI), and histamine-2 receptor antagonist
Two patient lists were used to identify patients for inclusion in the warfarin arm. The first patient list was generated using the US Department of Veterans Affairs (VA) Cirrhosis Tracker, which identified patients with an ICD-9/10 code for cirrhosis and an INR laboratory value. Patients generated from the VA Cirrhosis Tracker with an INR > 1.5 were screened for a warfarin prescription and then evaluated for full study inclusion. The second patient list was generated using the VA Advanced Liver Disease Dashboard which identified patients with ICD-9/10 codes for advanced liver disease and an active warfarin prescription. Patients with an active warfarin prescription were then evaluated for full study inclusion. A single patient list was generated to identify patients for inclusion in the DOAC arm. This patient list was generated using the VA DOAC dashboard, which identified patients with an active DOAC prescription and an ICD-9/10 code for cirrhosis. Patients with an ICD-9/10 code for cirrhosis and prescribed a DOAC were screened for full study inclusion. Patient data were collected from the MEDVAMC Computerized Patient Record System (CPRS) electronic health record (EHR). The research study was approved by the Baylor College of Medicine Institutional Review Board and the VA Office of Research and Development.
Outcomes
The primary endpoint for the study was all-cause bleeding. The secondary endpoints for the study were major bleeding and failed efficacy. Major bleeding was defined using the International Society on Thrombosis and Haemostasis (ISTH) 2005 definition: fatal bleeding, symptomatic bleeding in a critical organ area (ie, intracranial, intraspinal, intraocular, retroperitoneal, intraarticular, pericardial, or intramuscular with compartment syndrome), or bleeding causing a fall in hemoglobin level of > 2 g/dL or leading to the transfusion of ≥ 2 units of red cells.6 Failed efficacy was a combination endpoint that included development of VTE, stroke, myocardial infarction (MI), and/or death. A prespecified subgroup analysis was conducted at the end of the study period to analyze trends in the DOAC and warfarin groups with respect to all-cause bleeding. All-cause bleeding risk was stratified by weight, BMI, Child-Turcotte-Pugh score, MELD score, presence of gastric and/or esophageal varices, active malignancies, percentage of time within therapeutic INR range in the warfarin group, indications for anticoagulation, and antiplatelet, NSAID, PPI, and H2RA therapy.
Statistical Analysis
Data were analyzed using descriptive and inferential statistics. Continuous data were analyzed using the Student t test, and categorical data were analyzed using the Fisher exact test. Previous studies determined an all-cause bleeding rate of 10 to 17% for warfarin compared with 5% for DOACs.7,8 To detect a 12% difference in the all-cause bleeding rate between DOACs and warfarin, 212 patients would be needed to achieve 80% power at an α level of 0.05.
Results
A total of 170 patients were screened, and after applying inclusion and exclusion criteria, 79 patients were enrolled in the study (Figure). The DOAC group included 42 patients, and the warfarin group included 37 patients. In the DOAC group, 69.1% (n = 29) of patients were taking apixaban, 21.4% (n = 9) rivaroxaban, and 9.5% (n = 4) dabigatran. There were no patients prescribed edoxaban during the study period.
Baseline characteristics were similar between the 2 groups except for Child-Turcotte-Pugh score, MELD score, mean INR, and number of days on anticoagulation therapy (Table 1). Most of the patients were male (98.7%), and the mean age was 71 years. The most common causes of cirrhosis were viral (29.1%), nonalcoholic fatty liver disease (NAFLD) (24.1%), multiple causes (22.8%), and alcohol (21.5%). Sixty-two patients (78.5%) had a NVAF indication for anticoagulation. The average CHA2DS2-VASc score was 3.7. Aspirin was prescribed in 51.9% (n = 41) of patients, and PPIs were prescribed in 48.1% (n = 38) of patients. At inclusion, esophageal varices were present in 13 patients and active malignancies were present in 6 patients.
Statistically significant differences in baseline characteristics were found between mean INR, Child-Turcotte-Pugh scores, MELD scores, and number of days on anticoagulant therapy. The mean INR was 1.3 in the DOAC group compared with 2.1 in the warfarin group (P = .0001). Eighty-one percent (n = 34) of patients in the DOAC group had a Child-Turcotte-Pugh score of A compared with 43.2% (n = 16) of patients in the warfarin group (P = .0009). Eight patients in the DOAC group had a Child-Turcotte-Pugh score of B compared with 19 patients in the warfarin group (P = .004). The mean MELD score was 9.4 in the DOAC group compared with 16.3 in the warfarin group (P = .0001). The mean days on anticoagulant therapy was 500.4 days for the DOAC group compared with 1,652.4 days for the warfarin group (P = .0001).
Safety Outcome
The primary outcome comparing all-cause bleeding rates between patients on DOACs compared with warfarin are listed in Table 2. With respect to the primary outcome, 7 (16.7%) patients on DOACs experienced a bleeding event compared with 8 (21.6%) patients on warfarin (P = .77). No statistically significant differences were detected between the DOAC and warfarin groups with respect to all-cause bleeding. Seven bleeding events occurred in the DOAC group; 1 met the qualification for major bleeding with a suspected gastrointestinal (GI) bleed.6 The other 6 bleeding episodes in the DOAC group consisted of hematoma, epistaxis, hematuria, and hematochezia. Eight bleeding events occurred in the warfarin group; 2 met the qualification for major bleeding with an intracranial hemorrhage and upper GI bleed.6 The other 6 bleeding episodes in the warfarin group consisted of epistaxis, bleeding gums, hematuria, and hematochezia. There were no statistically significant differences between the rates of major bleeding and nonmajor bleeding between the DOAC and warfarin groups.
Efficacy Outcomes
There were 3 events in the DOAC group and 3 events in the warfarin group (P = .99). In the DOAC group, 2 patients experienced a pulmonary embolism, and 1 patient experienced a MI. In the warfarin group, 3 patients died (end-stage heart failure, unknown cause due to death at an outside hospital, and sepsis/organ failure). There were no statistically significant differences between the composite endpoint of failed efficacy or the individual endpoints of VTE, stroke, MI, and death.
Subgroup Analysis
A prespecified subgroup analysis was conducted to determine risk factors for all-cause bleeding within each treatment group (Table 3). No significant trends were observed in the following risk factors: Child-Turcotte-Pugh score, indication for anticoagulation, use of NSAIDs, PPIs or H2RAs, presence of gastric or esophageal varices, active malignancies, and time within therapeutic INR range in the warfarin group. Patients with bleeding events had slightly increased weight and BMI vs patients without bleeding events. Within the warfarin group, patients with bleeding events had slightly elevated MELD scores compared to patients without bleeding events. There was an equal balance of patients prescribed aspirin therapy between the groups with and without bleeding events. Overall, no significant risk factors were identified for all-cause bleeding.
Discussion
Initially, patients with cirrhosis were excluded from DOAC trials due to concerns for increased bleeding risk with hepatically eliminated medications. New retrospective research has concluded that in patients with cirrhosis, DOACs have similar or lower bleeding rates when compared directly to warfarin.9,10
In this study, no statistically significant differences were detected between the primary and secondary outcomes of all-cause bleeding, major bleeding, or failed efficacy. Subgroup analysis did not identify any significant risk factors with respect to all-cause bleeding among patients in the DOAC and warfarin groups. To meet 80% power, 212 patients needed to be enrolled in the study; however, only 79 patients were enrolled, and power was not met. The results of this study should be interpreted cautiously as hypothesis-generating due to the small sample size. Strengths of this study include similar baseline characteristics between the DOAC and warfarin groups, 4-year length of retrospective data review, and availability of both inpatient and outpatient EHR limiting the amount of missing data points.
Baseline characteristics were similar between the groups except for mean INR, Child-Turcotte-Pugh score, MELD score, and number of days on anticoagulation therapy. The difference in mean INR between groups is expected as patients in the warfarin group have a goal INR of 2 to 3 to maintain therapeutic efficacy and safety. INR is not used as a marker of efficacy or safety with DOACs; therefore, a consistent elevation in INR is not expected. Child- Turcotte-Pugh scores are calculated using INR levels.11 When calculating the score, patients with an INR < 1.7 receive 1 point; patients with an INR between 1.7 and 2.3 receive 2 points.11 Therefore, patients in the warfarin group will have artificially inflated Child-Turcotte-Pugh scores as this group has goal INR levels of 2 to 3. This makes Child-Turcotte-Pugh scores unreliable markers of disease severity in patients using warfarin therapy. When the INR scores for patients prescribed warfarin were replaced with values < 1.7, the statistical difference disappeared between the warfarin and DOAC groups. The same effect is seen on MELD scores for patients prescribed warfarin therapy. The MELD score is calculated using INR levels.12 MELD scores also will be artificially elevated in patients prescribed warfarin therapy due to the INR elevation to between 2 and 3. When MELD scores for patients prescribed warfarin were replaced with values similar to those in the DOAC group, the statistical difference disappeared between the warfarin and DOAC groups.
The last statistically significant difference was found in number of days on anticoagulant therapy. This difference was expected as warfarin is the standard of care for anticoagulation treatment in patients with cirrhosis. The first DOAC, dabigatran, was not approved by the US Food and Drug Administration until 2010.13 DOACs have only recently been used in patients with cirrhosis accounting for the statistically significant difference in days on anticoagulation therapy between the warfarin and DOAC groups.
Limitations
The inability to meet power or evaluate adherence and appropriate renal dose adjustments for DOACs limited this study. This study was conducted at a single center in a predominantly male veteran population and therefore may not be generalizable to other populations. A majority of patients in the DOAC group were prescribed apixaban (69.1%), which may have affected the overall rate of major bleeding in the DOAC group. Pivotal trials of apixaban have shown a consistent decreased risk of major bleeding in patients with NVAF or VTE when compared with warfarin.14,15 Therefore, the results of this study may not be generalizable to all DOACs.
An inherent limitation of this study was the inability to collect data verifying adherence in the DOAC group. However, in the warfarin group, percentage of time within the therapeutic INR range of 2 to 3 was collected. While not a direct marker of adherence, this does allow for limited evaluation of therapeutic efficacy and safety within the warfarin group. Last, proper dosing of DOACs in patients with and without adequate renal function was not evaluated in this study.
Conclusions
The results of this study are consistent with other retrospective research and literature reviews. There were no statistically significant differences identified between the rates of all-cause bleeding, major bleeding, and failed efficacy between the DOAC and warfarin groups. DOACs may be a safe alternative to warfarin in patients with cirrhosis requiring anticoagulation for NVAF or VTE, but large randomized trials are required to confirm these results.
Coagulation in patients with cirrhosis is a complicated area of evolving research. Patients with cirrhosis were originally thought to be naturally anticoagulated due to the decreased production of clotting factors and platelets, combined with an increased international normalized ratio (INR).1 New data have shown that patients with cirrhosis are at a concomitant risk of bleeding and thrombosis due to increased platelet aggregation, decreased fibrinolysis, and decreased production of natural anticoagulants such as protein C and antithrombin.1 Traditionally, patients with cirrhosis needing anticoagulation therapy for comorbid conditions, such as nonvalvular atrial fibrillation (NVAF) or venous thromboembolism (VTE) were placed on warfarin therapy. Managing warfarin in patients with cirrhosis poses a challenge to clinicians due to the many food and drug interactions, narrow therapeutic index, and complications with maintaining a therapeutic INR.1
Direct oral anticoagulants (DOACs) have several benefits over warfarin therapy, including convenience, decreased monitoring, decreased drug and dietary restrictions, and faster onset of action.2 Conversely, DOACs undergo extensive hepatic metabolism giving rise to concerns about supratherapeutic drug levels and increased bleeding rates in patients with liver dysfunction.1 Consequently, patients with cirrhosis were excluded from the pivotal trials establishing DOACs for NVAF and VTE treatment. Exclusion of these patients in major clinical trials alongside the challenges of managing warfarin warrant an evaluation of the efficacy and safety of DOACs in patients with cirrhosis.
Recent retrospective studies have examined the use of DOACs in patients with cirrhosis and found favorable results. A retrospective chart review by Intagliata and colleagues consisting of 39 patients with cirrhosis using either a DOAC or warfarin found similar rates of all-cause bleeding and major bleeding between the 2 groups.3 A retrospective cohort study by Hum and colleagues consisting of 45 patients with cirrhosis compared the use of DOACs with warfarin or low-molecular weight heparin (LMWH).4 Hum and colleagues found patients prescribed a DOAC had significantly fewer major bleeding events than did patients using warfarin or LMWH.4 The largest retrospective cohort study consisted of 233 patients with chronic liver disease and found no differences among all-cause bleeding and major bleeding rates between patients using DOACs compared with those of patients using warfarin.5
The purpose of this research is to evaluate the safety and efficacy of DOACs in veteran patients with cirrhosis compared with patients using warfarin.
Methods
A retrospective single-center chart review was conducted at the Michael E. DeBakey Veterans Affairs Medical Center (MEDVAMC) in Houston, Texas, between October 31, 2014 and October 31, 2018. Patients included in the study were adults aged ≥ 18 years with a diagnosis of cirrhosis and prescribed any of the following oral anticoagulants: apixaban, dabigatran, edoxaban, rivaroxaban, or warfarin. Patients prescribed apixaban, dabigatran, edoxaban, or rivaroxaban were collectively grouped into the DOAC group, while patients prescribed warfarin were classified as the standard of care comparator group.
A diagnosis of cirrhosis was confirmed using a combination of the codes from the ninth and tenth editions of the International Classification of Diseases (ICD) for cirrhosis, documentation of diagnostic confirmation by clinicians from the gastroenterology or hepatology services, and positive liver biopsy result. Liver function tests, liver ultrasound results, and FibroSure biomarker assays were used to aid in confirming the diagnosis of cirrhosis but were not considered definitive. Patients were excluded from the trial if they had indications for anticoagulation other than NVAF and VTE and/or were prescribed triple antithrombotic therapy (dual antiplatelet therapy plus an anticoagulant). Patients who switched anticoagulant therapy during the trial period (ie, switched from warfarin to a DOAC) were also excluded from the analysis.
Patient demographic characteristics that were collected included weight; body mass index (BMI); etiology of cirrhosis; Child-Turcotte-Pugh, Model for End-Stage Liver Disease (MELD), and CHA2DS2-VASc score; concomitant antiplatelet, nonsteroidal anti-inflammatory drug (NSAID), proton pump inhibitor (PPI), and histamine-2 receptor antagonist
Two patient lists were used to identify patients for inclusion in the warfarin arm. The first patient list was generated using the US Department of Veterans Affairs (VA) Cirrhosis Tracker, which identified patients with an ICD-9/10 code for cirrhosis and an INR laboratory value. Patients generated from the VA Cirrhosis Tracker with an INR > 1.5 were screened for a warfarin prescription and then evaluated for full study inclusion. The second patient list was generated using the VA Advanced Liver Disease Dashboard which identified patients with ICD-9/10 codes for advanced liver disease and an active warfarin prescription. Patients with an active warfarin prescription were then evaluated for full study inclusion. A single patient list was generated to identify patients for inclusion in the DOAC arm. This patient list was generated using the VA DOAC dashboard, which identified patients with an active DOAC prescription and an ICD-9/10 code for cirrhosis. Patients with an ICD-9/10 code for cirrhosis and prescribed a DOAC were screened for full study inclusion. Patient data were collected from the MEDVAMC Computerized Patient Record System (CPRS) electronic health record (EHR). The research study was approved by the Baylor College of Medicine Institutional Review Board and the VA Office of Research and Development.
Outcomes
The primary endpoint for the study was all-cause bleeding. The secondary endpoints for the study were major bleeding and failed efficacy. Major bleeding was defined using the International Society on Thrombosis and Haemostasis (ISTH) 2005 definition: fatal bleeding, symptomatic bleeding in a critical organ area (ie, intracranial, intraspinal, intraocular, retroperitoneal, intraarticular, pericardial, or intramuscular with compartment syndrome), or bleeding causing a fall in hemoglobin level of > 2 g/dL or leading to the transfusion of ≥ 2 units of red cells.6 Failed efficacy was a combination endpoint that included development of VTE, stroke, myocardial infarction (MI), and/or death. A prespecified subgroup analysis was conducted at the end of the study period to analyze trends in the DOAC and warfarin groups with respect to all-cause bleeding. All-cause bleeding risk was stratified by weight, BMI, Child-Turcotte-Pugh score, MELD score, presence of gastric and/or esophageal varices, active malignancies, percentage of time within therapeutic INR range in the warfarin group, indications for anticoagulation, and antiplatelet, NSAID, PPI, and H2RA therapy.
Statistical Analysis
Data were analyzed using descriptive and inferential statistics. Continuous data were analyzed using the Student t test, and categorical data were analyzed using the Fisher exact test. Previous studies determined an all-cause bleeding rate of 10 to 17% for warfarin compared with 5% for DOACs.7,8 To detect a 12% difference in the all-cause bleeding rate between DOACs and warfarin, 212 patients would be needed to achieve 80% power at an α level of 0.05.
Results
A total of 170 patients were screened, and after applying inclusion and exclusion criteria, 79 patients were enrolled in the study (Figure). The DOAC group included 42 patients, and the warfarin group included 37 patients. In the DOAC group, 69.1% (n = 29) of patients were taking apixaban, 21.4% (n = 9) rivaroxaban, and 9.5% (n = 4) dabigatran. There were no patients prescribed edoxaban during the study period.
Baseline characteristics were similar between the 2 groups except for Child-Turcotte-Pugh score, MELD score, mean INR, and number of days on anticoagulation therapy (Table 1). Most of the patients were male (98.7%), and the mean age was 71 years. The most common causes of cirrhosis were viral (29.1%), nonalcoholic fatty liver disease (NAFLD) (24.1%), multiple causes (22.8%), and alcohol (21.5%). Sixty-two patients (78.5%) had a NVAF indication for anticoagulation. The average CHA2DS2-VASc score was 3.7. Aspirin was prescribed in 51.9% (n = 41) of patients, and PPIs were prescribed in 48.1% (n = 38) of patients. At inclusion, esophageal varices were present in 13 patients and active malignancies were present in 6 patients.
Statistically significant differences in baseline characteristics were found between mean INR, Child-Turcotte-Pugh scores, MELD scores, and number of days on anticoagulant therapy. The mean INR was 1.3 in the DOAC group compared with 2.1 in the warfarin group (P = .0001). Eighty-one percent (n = 34) of patients in the DOAC group had a Child-Turcotte-Pugh score of A compared with 43.2% (n = 16) of patients in the warfarin group (P = .0009). Eight patients in the DOAC group had a Child-Turcotte-Pugh score of B compared with 19 patients in the warfarin group (P = .004). The mean MELD score was 9.4 in the DOAC group compared with 16.3 in the warfarin group (P = .0001). The mean days on anticoagulant therapy was 500.4 days for the DOAC group compared with 1,652.4 days for the warfarin group (P = .0001).
Safety Outcome
The primary outcome comparing all-cause bleeding rates between patients on DOACs compared with warfarin are listed in Table 2. With respect to the primary outcome, 7 (16.7%) patients on DOACs experienced a bleeding event compared with 8 (21.6%) patients on warfarin (P = .77). No statistically significant differences were detected between the DOAC and warfarin groups with respect to all-cause bleeding. Seven bleeding events occurred in the DOAC group; 1 met the qualification for major bleeding with a suspected gastrointestinal (GI) bleed.6 The other 6 bleeding episodes in the DOAC group consisted of hematoma, epistaxis, hematuria, and hematochezia. Eight bleeding events occurred in the warfarin group; 2 met the qualification for major bleeding with an intracranial hemorrhage and upper GI bleed.6 The other 6 bleeding episodes in the warfarin group consisted of epistaxis, bleeding gums, hematuria, and hematochezia. There were no statistically significant differences between the rates of major bleeding and nonmajor bleeding between the DOAC and warfarin groups.
Efficacy Outcomes
There were 3 events in the DOAC group and 3 events in the warfarin group (P = .99). In the DOAC group, 2 patients experienced a pulmonary embolism, and 1 patient experienced a MI. In the warfarin group, 3 patients died (end-stage heart failure, unknown cause due to death at an outside hospital, and sepsis/organ failure). There were no statistically significant differences between the composite endpoint of failed efficacy or the individual endpoints of VTE, stroke, MI, and death.
Subgroup Analysis
A prespecified subgroup analysis was conducted to determine risk factors for all-cause bleeding within each treatment group (Table 3). No significant trends were observed in the following risk factors: Child-Turcotte-Pugh score, indication for anticoagulation, use of NSAIDs, PPIs or H2RAs, presence of gastric or esophageal varices, active malignancies, and time within therapeutic INR range in the warfarin group. Patients with bleeding events had slightly increased weight and BMI vs patients without bleeding events. Within the warfarin group, patients with bleeding events had slightly elevated MELD scores compared to patients without bleeding events. There was an equal balance of patients prescribed aspirin therapy between the groups with and without bleeding events. Overall, no significant risk factors were identified for all-cause bleeding.
Discussion
Initially, patients with cirrhosis were excluded from DOAC trials due to concerns for increased bleeding risk with hepatically eliminated medications. New retrospective research has concluded that in patients with cirrhosis, DOACs have similar or lower bleeding rates when compared directly to warfarin.9,10
In this study, no statistically significant differences were detected between the primary and secondary outcomes of all-cause bleeding, major bleeding, or failed efficacy. Subgroup analysis did not identify any significant risk factors with respect to all-cause bleeding among patients in the DOAC and warfarin groups. To meet 80% power, 212 patients needed to be enrolled in the study; however, only 79 patients were enrolled, and power was not met. The results of this study should be interpreted cautiously as hypothesis-generating due to the small sample size. Strengths of this study include similar baseline characteristics between the DOAC and warfarin groups, 4-year length of retrospective data review, and availability of both inpatient and outpatient EHR limiting the amount of missing data points.
Baseline characteristics were similar between the groups except for mean INR, Child-Turcotte-Pugh score, MELD score, and number of days on anticoagulation therapy. The difference in mean INR between groups is expected as patients in the warfarin group have a goal INR of 2 to 3 to maintain therapeutic efficacy and safety. INR is not used as a marker of efficacy or safety with DOACs; therefore, a consistent elevation in INR is not expected. Child- Turcotte-Pugh scores are calculated using INR levels.11 When calculating the score, patients with an INR < 1.7 receive 1 point; patients with an INR between 1.7 and 2.3 receive 2 points.11 Therefore, patients in the warfarin group will have artificially inflated Child-Turcotte-Pugh scores as this group has goal INR levels of 2 to 3. This makes Child-Turcotte-Pugh scores unreliable markers of disease severity in patients using warfarin therapy. When the INR scores for patients prescribed warfarin were replaced with values < 1.7, the statistical difference disappeared between the warfarin and DOAC groups. The same effect is seen on MELD scores for patients prescribed warfarin therapy. The MELD score is calculated using INR levels.12 MELD scores also will be artificially elevated in patients prescribed warfarin therapy due to the INR elevation to between 2 and 3. When MELD scores for patients prescribed warfarin were replaced with values similar to those in the DOAC group, the statistical difference disappeared between the warfarin and DOAC groups.
The last statistically significant difference was found in number of days on anticoagulant therapy. This difference was expected as warfarin is the standard of care for anticoagulation treatment in patients with cirrhosis. The first DOAC, dabigatran, was not approved by the US Food and Drug Administration until 2010.13 DOACs have only recently been used in patients with cirrhosis accounting for the statistically significant difference in days on anticoagulation therapy between the warfarin and DOAC groups.
Limitations
The inability to meet power or evaluate adherence and appropriate renal dose adjustments for DOACs limited this study. This study was conducted at a single center in a predominantly male veteran population and therefore may not be generalizable to other populations. A majority of patients in the DOAC group were prescribed apixaban (69.1%), which may have affected the overall rate of major bleeding in the DOAC group. Pivotal trials of apixaban have shown a consistent decreased risk of major bleeding in patients with NVAF or VTE when compared with warfarin.14,15 Therefore, the results of this study may not be generalizable to all DOACs.
An inherent limitation of this study was the inability to collect data verifying adherence in the DOAC group. However, in the warfarin group, percentage of time within the therapeutic INR range of 2 to 3 was collected. While not a direct marker of adherence, this does allow for limited evaluation of therapeutic efficacy and safety within the warfarin group. Last, proper dosing of DOACs in patients with and without adequate renal function was not evaluated in this study.
Conclusions
The results of this study are consistent with other retrospective research and literature reviews. There were no statistically significant differences identified between the rates of all-cause bleeding, major bleeding, and failed efficacy between the DOAC and warfarin groups. DOACs may be a safe alternative to warfarin in patients with cirrhosis requiring anticoagulation for NVAF or VTE, but large randomized trials are required to confirm these results.
1. Qamar A, Vaduganathan M, Greenberger NJ, Giugliano RP. Oral anticoagulation in patients with liver disease. J Am Coll Cardiol. 2018;71(19):2162-2175. doi:10.1016/j.jacc.2018.03.023
2. Priyanka P, Kupec JT, Krafft M, Shah NA, Reynolds GJ. Newer oral anticoagulants in the treatment of acute portal vein thrombosis in patients with and without cirrhosis. Int J Hepatol. 2018;2018:8432781. Published 2018 Jun 5. doi:10.1155/2018/8432781
3. Intagliata NM, Henry ZH, Maitland H, et al. Direct oral anticoagulants in cirrhosis patients pose similar risks of bleeding when compared to traditional anticoagulation. Dig Dis Sci. 2016;61(6):1721-1727. doi:10.1007/s10620-015-4012-2
4. Hum J, Shatzel JJ, Jou JH, Deloughery TG. The efficacy and safety of direct oral anticoagulants vs traditional anticoagulants in cirrhosis. Eur J Haematol. 2017;98(4):393-397. doi:10.1111/ejh.12844
5. Goriacko P, Veltri KT. Safety of direct oral anticoagulants vs warfarin in patients with chronic liver disease and atrial fibrillation. Eur J Haematol. 2018;100(5):488-493. doi:10.1111/ejh.13045
6. Schulman S, Kearon C; Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692-694. doi:10.1111/j.1538-7836.2005.01204.x
7. Rubboli A, Becattini C, Verheugt FW. Incidence, clinical impact and risk of bleeding during oral anticoagulation therapy. World J Cardiol. 2011;3(11):351-358. doi:10.4330/wjc.v3.i11.351
8. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955-962. doi:10.1016/S0140-6736(13)62343-0
9. Hoolwerf EW, Kraaijpoel N, Büller HR, van Es N. Direct oral anticoagulants in patients with liver cirrhosis: A systematic review. Thromb Res. 2018;170:102-108. doi:10.1016/j.thromres.2018.08.011
10. Steuber TD, Howard ML, Nisly SA. Direct oral anticoagulants in chronic liver disease. Ann Pharmacother. 2019;53(10):1042-1049. doi:10.1177/1060028019841582
11. Janevska D, Chaloska-Ivanova V, Janevski V. Hepatocellular carcinoma: risk factors, diagnosis and treatment. Open Access Maced J Med Sci. 2015;3(4):732-736. doi:10.3889/oamjms.2015.111
12. Singal AK, Kamath PS. Model for End-Stage Liver Disease. J Clin Exp Hepatol. 2013;3(1):50-60. doi:10.1016/j.jceh.2012.11.002
13. Joppa SA, Salciccioli J, Adamski J, et al. A practical review of the emerging direct anticoagulants, laboratory monitoring, and reversal agents. J Clin Med. 2018;7(2):29. Published 2018 Feb 11. doi:10.3390/jcm7020029
14. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981-992. doi:10.1056/NEJMoa1107039
15. Agnelli G, Buller HR, Cohen A, et al. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369(9):799-808. doi:10.1056/NEJMoa1302507
1. Qamar A, Vaduganathan M, Greenberger NJ, Giugliano RP. Oral anticoagulation in patients with liver disease. J Am Coll Cardiol. 2018;71(19):2162-2175. doi:10.1016/j.jacc.2018.03.023
2. Priyanka P, Kupec JT, Krafft M, Shah NA, Reynolds GJ. Newer oral anticoagulants in the treatment of acute portal vein thrombosis in patients with and without cirrhosis. Int J Hepatol. 2018;2018:8432781. Published 2018 Jun 5. doi:10.1155/2018/8432781
3. Intagliata NM, Henry ZH, Maitland H, et al. Direct oral anticoagulants in cirrhosis patients pose similar risks of bleeding when compared to traditional anticoagulation. Dig Dis Sci. 2016;61(6):1721-1727. doi:10.1007/s10620-015-4012-2
4. Hum J, Shatzel JJ, Jou JH, Deloughery TG. The efficacy and safety of direct oral anticoagulants vs traditional anticoagulants in cirrhosis. Eur J Haematol. 2017;98(4):393-397. doi:10.1111/ejh.12844
5. Goriacko P, Veltri KT. Safety of direct oral anticoagulants vs warfarin in patients with chronic liver disease and atrial fibrillation. Eur J Haematol. 2018;100(5):488-493. doi:10.1111/ejh.13045
6. Schulman S, Kearon C; Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692-694. doi:10.1111/j.1538-7836.2005.01204.x
7. Rubboli A, Becattini C, Verheugt FW. Incidence, clinical impact and risk of bleeding during oral anticoagulation therapy. World J Cardiol. 2011;3(11):351-358. doi:10.4330/wjc.v3.i11.351
8. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955-962. doi:10.1016/S0140-6736(13)62343-0
9. Hoolwerf EW, Kraaijpoel N, Büller HR, van Es N. Direct oral anticoagulants in patients with liver cirrhosis: A systematic review. Thromb Res. 2018;170:102-108. doi:10.1016/j.thromres.2018.08.011
10. Steuber TD, Howard ML, Nisly SA. Direct oral anticoagulants in chronic liver disease. Ann Pharmacother. 2019;53(10):1042-1049. doi:10.1177/1060028019841582
11. Janevska D, Chaloska-Ivanova V, Janevski V. Hepatocellular carcinoma: risk factors, diagnosis and treatment. Open Access Maced J Med Sci. 2015;3(4):732-736. doi:10.3889/oamjms.2015.111
12. Singal AK, Kamath PS. Model for End-Stage Liver Disease. J Clin Exp Hepatol. 2013;3(1):50-60. doi:10.1016/j.jceh.2012.11.002
13. Joppa SA, Salciccioli J, Adamski J, et al. A practical review of the emerging direct anticoagulants, laboratory monitoring, and reversal agents. J Clin Med. 2018;7(2):29. Published 2018 Feb 11. doi:10.3390/jcm7020029
14. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981-992. doi:10.1056/NEJMoa1107039
15. Agnelli G, Buller HR, Cohen A, et al. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369(9):799-808. doi:10.1056/NEJMoa1302507
Enoxaparin vs Continuous Heparin for Periprocedural Bridging in Patients With Atrial Fibrillation and Advanced Chronic Kidney Disease
There has been a long-standing controversy in the use of parenteral anticoagulation for perioperative bridging in patients with atrial fibrillation (AF) pursuing elective surgery.1 The decision to bridge is dependent on the patient’s risk of thromboembolic complications and susceptibility to bleed.1 The BRIDGE trial showed noninferiority in rate of stroke and embolism events between low molecular weight heparins (LMWHs) and no perioperative bridging.2 However, according to the American College of Chest Physicians (CHEST) 2012 guidelines, patients in the BRIDGE trial would be deemed low risk for thromboembolic events displayed by a mean CHADS2 (congestive heart failure [CHF], hypertension, age, diabetes mellitus, and stroke/transient ischemic attack) score of 2.3. Also, the BRIDGE study and many others excluded patients with advanced forms of chronic kidney disease (CKD).2,3
Similar to patients with AF, patients with advanced CKD (ACKD, stage 4 and 5 CKD) have an increased risk of stroke and venous thromboembolism (VTE).4,5 Patients with AF and ACKD have not been adequately studied for perioperative anticoagulation bridging outcomes. Although unfractionated heparin (UFH) is preferred over LMWH in ACKD patients,enoxaparin can be used in this population.1,6 Enoxaparin 1 mg/kg once daily is approved by the US Food and Drug Administration (FDA) for use in patients with severe renal insufficiency defined as creatinine clearance (CrCl) < 30 mL/min. This dosage adjustment is subsequent to studies with enoxaparin 1 mg/kg twice daily that showed a significant increase in major and minor bleeding in severe renal-insufficient patients with CrCl < 30 mL/min vs patients with CrCl > 30 mL/min.7 When comparing the myocardial infarction (MI) outcomes of severe renal-insufficient patients in the ExTRACT-TIMI 25 trial, enoxaparin 1 mg/kg once daily had no significant difference in nonfatal major bleeding vs UFH.8 In patients without renal impairment (no documentation of kidney disease), bridging therapy with LMWH was completed more than UFH in < 24 hours of hospital stay and with similar rates of VTEs and major bleeding.9 In addition to its ability to be administered outpatient, enoxaparin has a more predictable pharmacokinetic profile, allowing for less monitoring and a lower incidence of heparin-induced thrombocytopenia (HIT) vs that of UFH.6
The Michael E. DeBakey Veteran Affairs Medical Center (MEDVAMC) in Houston, Texas, is one of the largest US Department of Veterans Affairs (VA) hospitals in the US, managing > 150,000 veterans in Southeast Texas and other southern states. As a referral center for traveling patients, it is crucial that MEDVAMC decrease hospital length of stay (LOS) to increase space for incoming patients. Reducing LOS also reduces costs and may have a correlation with decreasing the incidence of nosocomial infections. Because of its significance to this facility, hospital LOS is an appropriate primary outcome for this study.
To our knowledge, bridging outcomes between LMWH and UFH in patients with AF and ACKD have never been studied. We hypothesized that using enoxaparin instead of heparin for periprocedural management would result in decreased hospital LOS, leading to a lower economic burden and lower incidence of nosocomial infections with no significant differences in major and minor bleeding and thromboembolic complications.10
Methods
This study was a single-center, retrospective chart review of adult patients from January 2008 to September 2017. The review was conducted at MEDVAMC and was approved by the research and development committee and by the Baylor College of Medicine Institutional Review Board. Formal consent was not required.
Included patients were aged ≥ 18 years with diagnoses of AF or atrial flutter and ACKD as recognized by a glomerular filtration rate (eGFR) of < 30 mL/min/1.73 m2 as calculated by use of the Modification of Diet in Renal Disease Study (MDRD) equation.11 Patients must have previously been on warfarin and required temporary interruption of warfarin for an elective procedure. During the interruption of warfarin therapy, a requirement was set for patients to be on periprocedural anticoagulation with subcutaneous (SC) enoxaparin 1 mg/kg daily or continuous IV heparin per MEDVAMC heparin protocol. Patients were excluded if they had experienced major bleeding in the 6 weeks prior to the elective procedure, had current thrombocytopenia (platelet count < 100 × 109/L), or had a history of heparin-induced thrombocytopenia (HIT) or a heparin allergy.
This patient population was identified using TheraDoc Clinical Surveillance Software System (Charlotte, NC), which has prebuilt alert reviews for anticoagulation medications, including enoxaparin and heparin. An alert for patients on enoxaparin with serum creatinine (SCr) > 1.5 mg/dL was used to screen patients who met the inclusion criteria. A second alert identified patients on heparin. The VA Computerized Patient Record System (CPRS) was used to collect patient data.
Economic Analysis
An economic analysis was conducted using data from the VA Managerial Cost Accounting Reports. Data on the national average cost per bed day was used for the purpose of extrapolating this information to multiple VA institutions.12 National average cost per day was determined by dividing the total cost by the number of bed days for the identified treating specialty during the fiscal period of 2018. Average cost per day data included costs for bed day, surgery, radiology services, laboratory tests, pharmacy services, treatment location (ie, intensive care units [ICUs]) and all other costs associated with an inpatient stay. A cost analysis was performed using this average cost per bed day and the mean LOS between enoxaparin and UFH for each treating specialty. The major outcome of the cost analysis was the total cost per average inpatient stay. The national average cost per bed day for each treating specialty was multiplied by the average LOS found for each treating specialty in this study; the sum of all the average costs per inpatient stay for the treating specialties resulted in the total cost per average inpatient stay. Permission to use these data was granted by the Pharmacy and Critical Care Services at MEDVAMC.
Patient Demographics and Characteristics
Data were collected on patient demographics (Table 1). Nosocomial infections, stroke/transient ischemic attack, MI, VTE, major and minor bleeding, and death are defined in Table 2.
The primary outcome of the study was hospital LOS. The study was powered at 90% for α = .05, which gives a required study population of 114 (1:1 enrollment ratio) patients to determine a statistically significant difference in hospital stay. This sample size was calculated using the mean hospital LOS (the primary objective) in the REGIMEN registry for LMWH (4.6 days) and UFH (10.3 days).9 To our knowledge, the incidence of nosocomial infections (a secondary outcome) has not been studied in this patient population; therefore, there was no basis to assess an appropriate sample size to find a difference in this outcome. Furthermore, the goal was to collect as many patients as possible to best assess this variable. Because of an expected high exclusion rate, 504 patients were reviewed to target a sample size of 120 patients. Due to the single-center nature of this review, the secondary outcomes of thromboembolic complications and major and minor bleeding were expected to be underpowered.
The final analysis compared the enoxaparin arm with the UFH arm. Univariate differences between the treatment groups were compared using the Fisher exact test for categorical variables. Demographic data and other continuous variables were analyzed by an unpaired t test to compare means between the 2 arms. Outcomes and characteristics were deemed statistically significant when α (P value) was < .05. All P values reported were 2-tailed with a 95% CI. No statistical analysis was performed for the cost differences (based on LOS per treating specialty) in the 2 treatment arms. Statistical analyses were completed by utilizing GraphPad Software (San Diego, CA).
Results
In total, 50 patients were analyzed in the study. There were 36 patients bridged with IV UFH at a concentration of 25,000 U/250 mL with an initial infusion rate of 12 U/kg/h. For the other arm, 14 patients were anticoagulated with renally dosed enoxaparin 1 mg/kg/d with an average daily dose of 89.3 mg; the mean actual body weight in this group was 90.9 mg (correlates with enoxaparin daily dose). Physicians of the primary team decided which parenteral anticoagulant to use. The difference in mean duration of inpatient parental anticoagulation between both groups was not statistically significant: enoxaparin at 7.1 days and UFH at 9.6 days (P = .19). Patients in the enoxaparin arm were off warfarin therapy for an average of 6.0 days vs 7.5 days for the UFH group (P = .29). The duration of outpatient anticoagulation with enoxaparin was not analyzed in this study.
Patient and Procedure Characteristics
All patients had AF or atrial flutter with 86% of patients (n = 43) having a CHADS2 > 2 and 48% (n = 29) having a CHA2DS2VASc > 4. Overall, the mean age was 71.3 years with similarities in ethnicity distribution. Patients had multiple comorbidities as shown by a mean Charlson Comorbidity Index (CCI) of 7.7 and an increased risk of bleeding as evidenced by 98% (n = 48) of patients having a HAS-BLED score of ≥ 3. A greater percentage of patients bridged with enoxaparin had DM, history of stroke and MI, and a heart valve, whereas UFH patients were more likely to be in stage 5 CKD (eGFR < 15 mL/min/1.73m2) with a significantly lower mean eGFR (16.76 vs 22.64, P = .03). Furthermore, there were more patients on hemodialysis in the UFH (50%) arm vs enoxaparin (21%) arm and a lower mean CrCl with UFH (20.1 mL/min) compared with enoxaparin (24.9 mL/min); however, the differences in hemodialysis and mean CrCl were not statistically significant. There were no patients on peritoneal dialysis in this review.
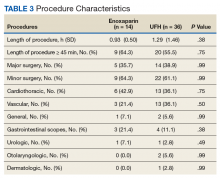
Procedure Characteristics
The average Revised Cardiac Risk Index (RCRI) score was about 3, indicating that these patients were at a Class IV risk (11%) of having a perioperative cardiac event (Table 3). Nineteen patients (38%) elected for a major surgery with all but 1 of the surgeries (major or minor) being invasive. The average length of surgery was 1.2 hours, and patients were more likely to undergo cardiothoracic procedures (38%). There were 2 out of 14 (14%) patients on enoxaparin who were able to have surgery as an outpatient; whereas this did not occur in patients on UFH. The procedures completed for these patients were a colostomy (minor surgery) and arteriovenous graft repair (major surgery). There were no statistically significant differences regarding types of procedures between the 2 arms.
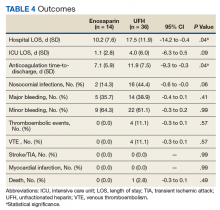
Outcomes
The primary outcome of this study, hospital LOS, differed significantly in the enoxaparin arm vs UFH: 10.2 days vs 17.5 days, P = .04 (Table 4). The time-to-discharge from initiation of parenteral anticoagulation was significantly reduced with enoxaparin (7.1 days) compared with UFH (11.9 days); P = .04. Although also reduced in the enoxaparin arm, ICU LOS did not show statistical significance (1.1 days vs 4.0 days, P = .09).
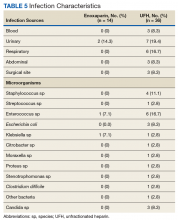
About 36% (n = 18) of patients in this study acquired an infection during hospitalization for elective surgery. The most common microorganism and site of infection were Enterococcus species and urinary tract, respectively (Table 5). Nearly half (44%, n = 16) of the patients in the UFH group had a nosocomial infection vs 14% (n = 2) of enoxaparin-bridged patients with a difference approaching significance; P = .056. Both patients in the enoxaparin group had the urinary tract as the primary source of infection; 1 of these patients had a urologic procedure.
Major bleeding occurred in 7% (n = 1) of enoxaparin patients vs 22% (n = 8) in the UFH arm, but this was not found to be statistically significant (P = .41). Minor bleeding was similar between enoxaparin and UFH arms (14% vs 19%, P = .99). Regarding thromboembolic complications, the enoxaparin group (0%) had a numerical reduction compared to UFH (11%) with VTE (n = 4) being the only occurrence of the composite outcome (P = .57). There were 4 deaths within 30 days posthospitalization—all were from the UFH group (P = .57). Due to the small sample size of this study, these outcomes (bleeding and thrombotic events) were not powered to detect a statistically significant difference.
Economic Analysis
The average cost differences (Table 6) of hospitalization between enoxaparin and UFH were calculated using the average LOS per treating specialty multiplied by the national average cost of the MCO for an inpatient bed day in 2018.12 The treating specialty with the longest average LOS in the enoxaparin arm was thoracic (4.7 days). The UFH arm also had a large LOS (average days) for the thoracic specialty (6.4 days); however, the vascular specialty (6.7 days) had the longest average LOS in this group. Due to a mean LOS of 10.2 days in the enoxaparin arm, which was further stratified by treating specialty, the total cost per average inpatient stay was calculated as $51,710. On the other hand, patients in the UFH arm had a total cost per average inpatient stay of $92,848.
Monitoring
Anti-factor Xa levels for LMWH monitoring were not analyzed in this study due to a lack of values collected; only 1 patient had an anti-factor Xa level checked during this time frame. Infusion rates of UFH were adjusted based on aPTT levels collected per MEDVAMC inpatient anticoagulation protocol. The average percentage of aPTT in therapeutic range was 46.3% and the mean time-to-therapeutic range (SD) was about 2.4 (1.3) days. Due to this study’s retrospective nature, there were inconsistencies with availability of documentation of UFH infusion rates. For this reason, these values were not analyzed further.
Discussion
In 2017, the American College of Cardiology published the Periprocedural Anticoagulation Expert Consensus Pathway, which recommends for patients with AF at low risk (CHA2DS2VASc 1-4) of thromboembolism to not be bridged (unless patient had a prior VTE or stroke/TIA).13 Nearly half the patients in this study, were classified as moderate-to-high thrombotic risk as evidenced by a CHA2DS2VASc > 4 with a mean score of 4.8. Due to this study’s retrospective design from 2008 to 2017, many of the clinicians may have referenced the 2008 CHEST antithrombotic guidelines when making the decision to bridge patients; these guidelines and the previous MEDVAMC anticoagulation protocol recommend bridging patients with AF with CHADS2 > 2 (moderate-to-high thrombotic risk) in which all but 1 of the patients in this study met criteria.1,14 In contrast to the landmark BRIDGE trial, the mean CHADS2 score in this study was 3.6; this is an indication that our patient population was of individuals at an increased risk of stroke and embolism.
In addition to thromboembolic complications, patients in the current study also were at increased risk of clinically relevant bleeding with a mean HAS-BLED score of 4.1 and nearly all patients having a score > 3. The complexity of the veteran population also was displayed by this study’s mean CCI (7.7) and RCRI (3.0) indicating a 0% estimated 10-year survival and a 11% increase in having a perioperative cardiac event, respectively. A mean CCI of 7.7 is associated with a 13.3 relative risk of death within 6 years postoperation.15 All patients had a diagnosis of hypertension, and > 75% had this diagnosis complicated by DM. In addition, this patient population was of those with extensive cardiovascular disease or increased risk, which makes for a clinically relevant application of patients who would require periprocedural bridging.
Another positive aspect of this study is that all the baseline characteristics, apart from renal function, were similar between arms, helping to strengthen the ability to adequately compare the 2 bridging modalities. Our assumption for the reasoning that more stage 5 CKD and dialysis patients were anticoagulated with UFH vs enoxaparin is a result of concern for an increased risk of bleeding with a medication that is renally cleared 30% less in CrCl < 30 mL/min.16 Although, enoxaparin 1 mg/kg/d is FDA approved as a therapeutic anticoagulant option, clinicians at MEDVAMC likely had reservations about its use in end-stage CKD patients. Unlike many studies, including the BRIDGE trial, patients with ACKD were not excluded from this trial, and the outcomes with enoxaparin are available for interpretation.
To no surprise, for patients included in this study, enoxaparin use led to shorter hospital LOS, reduced ICU LOS, and a quicker time-to-discharge from initiation. This is credited to the 100% bioavailability of SC enoxaparin in conjunction with its means to be a therapeutic option as an outpatient.16 Unlike IV UFH, patients requiring bridging can be discharged on SC injections of enoxaparin until a therapeutic INR is maintained with warfarin.The duration of hospital LOS in both arms were longer in this study compared with that of other studies.9 This may be due to clinicians being more cautious with renal insufficient patients, and the patients included in this study had multiple comorbidities. According to an economic analysis performed by Amorosi and colleagues in 2004, bridging with enoxaparin instead of UFH can save up to $3,733 per patient and reduce bridging costs by 63% to 85% driven primarily by decreased hospital LOS.10
Economic Outcome
In our study, we conducted a cost analysis using national VA data that indicated a $41,138 or 44% reduction in total cost per average inpatient stay when bridging 1 patient with enoxaparin vs UFH. The benefit of this cost analysis is that it reflects direct costs at VA institutions nationally; this will allow these data to be useful for practitioners at MEDVAMC and other VA hospitals. Stratifying the costs by treating specialty instead of treatment location minimized skewing of the data as there were some patients with long LOS in the ICU. No patients in the enoxaparin arm were treated in otolaryngology, which may have skewed the data. The data included direct costs for beds as well as costs for multiple services, such as procedures, pharmacy, nursing, laboratory tests, and imaging. Unlike the Amorosi study, our review did not include acquisition costs for enoxaparin syringes and bags of UFH or laboratory costs for aPTT and anti-factor Xa levels in part because of the data source and the difficulty calculating costs over a 10-year span.
Patients in the enoxaparin arm had a trend toward fewer occurrences of hospital-acquired infections than did those in the UFH arm, which we believe is due to a decreased LOS (in both total hospital and ICU days) and fewer blood draws needed for monitoring. This also may be attributed to a longer mean duration of surgery in the UFH arm (1.3 hours) vs enoxaparin (0.9 hours). The percentage of patients with procedures ≥ 45 minutes and the types of procedures between both arms were similar. However, these outcomes were not statistically significant. In addition, elderly males who are hospitalized may require a catheter (due to urinary retention), and catheter-associated urinary tract infection (CAUTI) is one of the highest reported infections in acute care hospitals in the US. This is in line with our patient population and may be a supplementary reason for the increase in infection incidence with UFH. Though, whether urinary catheters were used in these patients was not evaluated in this study.
Despite being at an increased risk of experiencing a major adverse cardiovascular event (MACE), no patients in either arm had a stroke/TIA or MI within 30 days postprocedure. The only occurrences documented were VTEs, which happened only in 4 patients on UFH. Four people died in this study, solely in the UFH arm. The incidence of thromboembolic complications and death along with major and minor bleeding cannot be deduced as meaningful as this study was underpowered for these outcomes. Despite anti-factor Xa monitoring being recommended in ACKD patients on enoxaparin, this monitoring was not routinely performed in this study. Another limitation was the inability to adequately assess the appropriateness of nurse-adjusted UFH infusion rates largely due to the retrospective nature of this study. The variability of aPTT percentage in therapeutic range and time-to-therapeutic range reported was indicative of the difficulties of monitoring for the safety and efficacy of UFH.
In 1991, Cruickshank and colleagues conducted a study in which a standard nomogram (similar to the MEDVAMC nomogram) for the adjustment of IV heparin was implemented at a single hospital.17 The success rate (aPTT percentage in therapeutic range) was 59.4% and average time-to-therapeutic range was about 1 day. The success rate (46.3%) and time-to-therapeutic range (2.4 days) in our study were lower and longer, respectively, than was expected. One potential reason for this discrepancy could be the differences in indication as the patients in Cruickshank and colleagues were being treated for VTE, whereas patients in our study had AF or atrial flutter. Also, there were inconsistencies in the availability of documentation of monitoring parameters for heparin due to the study time frame and retrospective design. Patients on UFH who are not within the therapeutic range in a timely manner are at greater risk of MACE and major/minor bleeding. Our study was not powered to detect these findings.
Strengths and Limitations
A significant limitation of this study was its small sample size; the study was not able to meet power for the primary outcome; it is unknown whether our study met power for nosocomial infections. The study also was not a powered review of other adverse events, such as thromboembolic complications, bleeding, and death. The study had an uneven number of patients, which made it more difficult to appropriately compare 2 patient populations; the study also did not include medians for patient characteristics and outcomes.
Due to this study’s time frame, the clinical pharmacy services at MEDVAMC were not as robust as they are now, which is the reason the decisions on which anticoagulant to use were primarily physician based. The use of TheraDoc to identify patients posed the risk of missing patients who may not have had the appropriate laboratory tests performed (ie, SCr). Patients on UFH had a reduced eGFR compared with that of enoxaparin, which may limit our extrapolation of enoxaparin’s use in end-stage renal disease. The reduced eGFR and higher number of dialysis patients in the UFH arm may have increased the occurrence of more labile INRs and bleeding outcomes. Patients on hemodialysis typically have more comorbidities and an increased risk of infection due to the frequent use of catheters and needles to access the bloodstream. In addition, the potential differences in catheter use and duration between groups were not identified. If these parameters were studied, the data collected may have helped better explain the reasoning for increased incidence of infection in the UFH arm.
Strengths of this study include a complex patient population with similar characteristics, distribution of ethnicities representative of the US population, patients at moderate-to-high thrombotic risk, the analysis of nosocomial infections, and the exclusion of patients with normal renal function or moderate CKD.
Conclusion
To our knowledge, this is the first study to compare periprocedural bridging outcomes and incidence of nosocomial infections in patients with AF and ACKD. This review provides new evidence that in this patient population, enoxaparin is a potential anticoagulant to reduce hospital LOS and hospital-acquired infections. Compared with UFH, bridging with enoxaparin reduced hospital LOS and anticoagulation time-to-discharge by 7 and 5 days, respectively, and decreased the incidence of nosocomial infections by 30%. Using the mean LOS per treating specialty for both arms, bridging 1 patient with AF with enoxaparin vs UFH can potentially lead to an estimated $40,000 (44%) reduction in total cost of hospitalization. Enoxaparin also had no numeric differences in mortality and adverse events (stroke/TIA, MI, VTE) vs that of UFH, but it is important to note that this study was not powered to find a significant difference in these outcomes. Due to the mean eGFR of patients on enoxaparin being 22.6 mL/min/1.73 m2 and only 1 in 5 having stage 5 CKD, at this time, we do not recommend enoxaparin for periprocedural use in stage 5 CKD or in patients on hemodialysis. Larger studies are needed, including randomized trials, in this patient population to further evaluate these outcomes and assess the use of enoxaparin in patients with ACKD.
1. Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2)(suppl):e326S-350S.
2. Douketis JD, Spyropoulos AC, Kaatz S, et al; BRIDGE Investigators. Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med. 2015;373(9):823-833.
3. Hammerstingl C, Schmitz A, Fimmers R, Omran H. Bridging of chronic oral anticoagulation with enoxaparin in patients with atrial fibrillation: results from the prospective BRAVE registry. Cardiovasc Ther. 2009;27(4):230-238.
4. Dad T, Weiner DE. Stroke and chronic kidney disease: epidemiology, pathogenesis, and management across kidney disease stages. Semin Nephrol. 2015;35(4):311-322.
5. Wattanakit K, Cushman M. Chronic kidney disease and venous thromboembolism: epidemiology and mechanisms. Curr Opin Pulm Med. 2009;15(5):408-412.
6. Saltiel M. Dosing low molecular weight heparins in kidney disease. J Pharm Pract. 2010;23(3):205-209.
7. Spinler SA, Inverso SM, Cohen M, Goodman SG, Stringer KA, Antman EM; ESSENCE and TIMI 11B Investigators. Safety and efficacy of unfractionated heparin versus enoxaparin in patients who are obese and patients with severe renal impairment: analysis from the ESSENCE and TIMI 11B studies. Am Heart J. 2003;146(1):33-41.
8. Fox KA, Antman EM, Montalescot G, et al. The impact of renal dysfunction on outcomes in the ExTRACT-TIMI 25 trial. J Am Coll Cardiol. 2007;49(23):2249-2255.
9. Spyropoulos AC, Turpie AG, Dunn AS, et al; REGIMEN Investigators. Clinical outcomes with unfractionated heparin or low-molecular-weight heparin as bridging therapy in patients on long-term oral anticoagulants: the REGIMEN registry. J Thromb Haemost. 2006;4(6):1246-1252.
10. Amorosi SL, Tsilimingras K, Thompson D, Fanikos J, Weinstein MC, Goldhaber SZ. Cost analysis of “bridging therapy” with low-molecular-weight heparin versus unfractionated heparin during temporary interruption of chronic anticoagulation. Am J Cardiol. 2004;93(4):509-511.
11. Inker LA, Astor BC, Fox CH, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63(5):713-735.
12. US Department of Veteran Affairs. Managerial Cost Accounting Financial User Support Reports: fiscal year 2018. https://www.herc.research.va.gov/include/page.asp?id=managerial-cost-accounting. [Source not verified.]
13. Doherty JU, Gluckman TJ, Hucker WJ, et al. 2017 ACC Expert Consensus Decision Pathway for Periprocedural Management of Anticoagulation in Patients With Nonvalvular Atrial Fibrillation: a report of the American College of Cardiology Clinical Expert Consensus Document Task Force. J Am Coll Cardiol. 2017;69(7):871-898.
14. Kearon C, Kahn SR, Agnelli G, et al. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 suppl):454S-545S.
15. Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245-1251.
16. Lovenox [package insert]. Bridgewater, NJ: Sanofi-Aventis; December 2017.
17. Cruickshank MK, Levine MN, Hirsh J, Roberts R, Siguenza M. A standard heparin nomogram for the management of heparin therapy. Arch Intern Med. 1991;151(2):333-337.
18. Steinberg BA, Peterson ED, Kim S, et al; Outcomes Registry for Better Informed Treatment of Atrial Fibrillation Investigators and Patients. Use and outcomes associated with bridging during anticoagulation interruptions in patients with atrial fibrillation: findings from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Circulation. 2015;131(5):488-494.
19. Verheugt FW, Steinhubl SR, Hamon M, et al. Incidence, prognostic impact, and influence of antithrombotic therapy on access and nonaccess site bleeding in percutaneous coronary intervention. JACC Cardiovasc Interv. 2011;4(2):191-197.
20. Bijsterveld NR, Peters RJ, Murphy SA, Bernink PJ, Tijssen JG, Cohen M. Recurrent cardiac ischemic events early after discontinuation of short-term heparin treatment in acute coronary syndromes: results from the Thrombolysis in Myocardial Infarction (TIMI) 11B and Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q-Wave Coronary Events (ESSENCE) studies. J Am Coll Cardiol. 2003;42(12):2083-2089.
There has been a long-standing controversy in the use of parenteral anticoagulation for perioperative bridging in patients with atrial fibrillation (AF) pursuing elective surgery.1 The decision to bridge is dependent on the patient’s risk of thromboembolic complications and susceptibility to bleed.1 The BRIDGE trial showed noninferiority in rate of stroke and embolism events between low molecular weight heparins (LMWHs) and no perioperative bridging.2 However, according to the American College of Chest Physicians (CHEST) 2012 guidelines, patients in the BRIDGE trial would be deemed low risk for thromboembolic events displayed by a mean CHADS2 (congestive heart failure [CHF], hypertension, age, diabetes mellitus, and stroke/transient ischemic attack) score of 2.3. Also, the BRIDGE study and many others excluded patients with advanced forms of chronic kidney disease (CKD).2,3
Similar to patients with AF, patients with advanced CKD (ACKD, stage 4 and 5 CKD) have an increased risk of stroke and venous thromboembolism (VTE).4,5 Patients with AF and ACKD have not been adequately studied for perioperative anticoagulation bridging outcomes. Although unfractionated heparin (UFH) is preferred over LMWH in ACKD patients,enoxaparin can be used in this population.1,6 Enoxaparin 1 mg/kg once daily is approved by the US Food and Drug Administration (FDA) for use in patients with severe renal insufficiency defined as creatinine clearance (CrCl) < 30 mL/min. This dosage adjustment is subsequent to studies with enoxaparin 1 mg/kg twice daily that showed a significant increase in major and minor bleeding in severe renal-insufficient patients with CrCl < 30 mL/min vs patients with CrCl > 30 mL/min.7 When comparing the myocardial infarction (MI) outcomes of severe renal-insufficient patients in the ExTRACT-TIMI 25 trial, enoxaparin 1 mg/kg once daily had no significant difference in nonfatal major bleeding vs UFH.8 In patients without renal impairment (no documentation of kidney disease), bridging therapy with LMWH was completed more than UFH in < 24 hours of hospital stay and with similar rates of VTEs and major bleeding.9 In addition to its ability to be administered outpatient, enoxaparin has a more predictable pharmacokinetic profile, allowing for less monitoring and a lower incidence of heparin-induced thrombocytopenia (HIT) vs that of UFH.6
The Michael E. DeBakey Veteran Affairs Medical Center (MEDVAMC) in Houston, Texas, is one of the largest US Department of Veterans Affairs (VA) hospitals in the US, managing > 150,000 veterans in Southeast Texas and other southern states. As a referral center for traveling patients, it is crucial that MEDVAMC decrease hospital length of stay (LOS) to increase space for incoming patients. Reducing LOS also reduces costs and may have a correlation with decreasing the incidence of nosocomial infections. Because of its significance to this facility, hospital LOS is an appropriate primary outcome for this study.
To our knowledge, bridging outcomes between LMWH and UFH in patients with AF and ACKD have never been studied. We hypothesized that using enoxaparin instead of heparin for periprocedural management would result in decreased hospital LOS, leading to a lower economic burden and lower incidence of nosocomial infections with no significant differences in major and minor bleeding and thromboembolic complications.10
Methods
This study was a single-center, retrospective chart review of adult patients from January 2008 to September 2017. The review was conducted at MEDVAMC and was approved by the research and development committee and by the Baylor College of Medicine Institutional Review Board. Formal consent was not required.
Included patients were aged ≥ 18 years with diagnoses of AF or atrial flutter and ACKD as recognized by a glomerular filtration rate (eGFR) of < 30 mL/min/1.73 m2 as calculated by use of the Modification of Diet in Renal Disease Study (MDRD) equation.11 Patients must have previously been on warfarin and required temporary interruption of warfarin for an elective procedure. During the interruption of warfarin therapy, a requirement was set for patients to be on periprocedural anticoagulation with subcutaneous (SC) enoxaparin 1 mg/kg daily or continuous IV heparin per MEDVAMC heparin protocol. Patients were excluded if they had experienced major bleeding in the 6 weeks prior to the elective procedure, had current thrombocytopenia (platelet count < 100 × 109/L), or had a history of heparin-induced thrombocytopenia (HIT) or a heparin allergy.
This patient population was identified using TheraDoc Clinical Surveillance Software System (Charlotte, NC), which has prebuilt alert reviews for anticoagulation medications, including enoxaparin and heparin. An alert for patients on enoxaparin with serum creatinine (SCr) > 1.5 mg/dL was used to screen patients who met the inclusion criteria. A second alert identified patients on heparin. The VA Computerized Patient Record System (CPRS) was used to collect patient data.
Economic Analysis
An economic analysis was conducted using data from the VA Managerial Cost Accounting Reports. Data on the national average cost per bed day was used for the purpose of extrapolating this information to multiple VA institutions.12 National average cost per day was determined by dividing the total cost by the number of bed days for the identified treating specialty during the fiscal period of 2018. Average cost per day data included costs for bed day, surgery, radiology services, laboratory tests, pharmacy services, treatment location (ie, intensive care units [ICUs]) and all other costs associated with an inpatient stay. A cost analysis was performed using this average cost per bed day and the mean LOS between enoxaparin and UFH for each treating specialty. The major outcome of the cost analysis was the total cost per average inpatient stay. The national average cost per bed day for each treating specialty was multiplied by the average LOS found for each treating specialty in this study; the sum of all the average costs per inpatient stay for the treating specialties resulted in the total cost per average inpatient stay. Permission to use these data was granted by the Pharmacy and Critical Care Services at MEDVAMC.
Patient Demographics and Characteristics
Data were collected on patient demographics (Table 1). Nosocomial infections, stroke/transient ischemic attack, MI, VTE, major and minor bleeding, and death are defined in Table 2.
The primary outcome of the study was hospital LOS. The study was powered at 90% for α = .05, which gives a required study population of 114 (1:1 enrollment ratio) patients to determine a statistically significant difference in hospital stay. This sample size was calculated using the mean hospital LOS (the primary objective) in the REGIMEN registry for LMWH (4.6 days) and UFH (10.3 days).9 To our knowledge, the incidence of nosocomial infections (a secondary outcome) has not been studied in this patient population; therefore, there was no basis to assess an appropriate sample size to find a difference in this outcome. Furthermore, the goal was to collect as many patients as possible to best assess this variable. Because of an expected high exclusion rate, 504 patients were reviewed to target a sample size of 120 patients. Due to the single-center nature of this review, the secondary outcomes of thromboembolic complications and major and minor bleeding were expected to be underpowered.
The final analysis compared the enoxaparin arm with the UFH arm. Univariate differences between the treatment groups were compared using the Fisher exact test for categorical variables. Demographic data and other continuous variables were analyzed by an unpaired t test to compare means between the 2 arms. Outcomes and characteristics were deemed statistically significant when α (P value) was < .05. All P values reported were 2-tailed with a 95% CI. No statistical analysis was performed for the cost differences (based on LOS per treating specialty) in the 2 treatment arms. Statistical analyses were completed by utilizing GraphPad Software (San Diego, CA).
Results
In total, 50 patients were analyzed in the study. There were 36 patients bridged with IV UFH at a concentration of 25,000 U/250 mL with an initial infusion rate of 12 U/kg/h. For the other arm, 14 patients were anticoagulated with renally dosed enoxaparin 1 mg/kg/d with an average daily dose of 89.3 mg; the mean actual body weight in this group was 90.9 mg (correlates with enoxaparin daily dose). Physicians of the primary team decided which parenteral anticoagulant to use. The difference in mean duration of inpatient parental anticoagulation between both groups was not statistically significant: enoxaparin at 7.1 days and UFH at 9.6 days (P = .19). Patients in the enoxaparin arm were off warfarin therapy for an average of 6.0 days vs 7.5 days for the UFH group (P = .29). The duration of outpatient anticoagulation with enoxaparin was not analyzed in this study.
Patient and Procedure Characteristics
All patients had AF or atrial flutter with 86% of patients (n = 43) having a CHADS2 > 2 and 48% (n = 29) having a CHA2DS2VASc > 4. Overall, the mean age was 71.3 years with similarities in ethnicity distribution. Patients had multiple comorbidities as shown by a mean Charlson Comorbidity Index (CCI) of 7.7 and an increased risk of bleeding as evidenced by 98% (n = 48) of patients having a HAS-BLED score of ≥ 3. A greater percentage of patients bridged with enoxaparin had DM, history of stroke and MI, and a heart valve, whereas UFH patients were more likely to be in stage 5 CKD (eGFR < 15 mL/min/1.73m2) with a significantly lower mean eGFR (16.76 vs 22.64, P = .03). Furthermore, there were more patients on hemodialysis in the UFH (50%) arm vs enoxaparin (21%) arm and a lower mean CrCl with UFH (20.1 mL/min) compared with enoxaparin (24.9 mL/min); however, the differences in hemodialysis and mean CrCl were not statistically significant. There were no patients on peritoneal dialysis in this review.
Procedure Characteristics
The average Revised Cardiac Risk Index (RCRI) score was about 3, indicating that these patients were at a Class IV risk (11%) of having a perioperative cardiac event (Table 3). Nineteen patients (38%) elected for a major surgery with all but 1 of the surgeries (major or minor) being invasive. The average length of surgery was 1.2 hours, and patients were more likely to undergo cardiothoracic procedures (38%). There were 2 out of 14 (14%) patients on enoxaparin who were able to have surgery as an outpatient; whereas this did not occur in patients on UFH. The procedures completed for these patients were a colostomy (minor surgery) and arteriovenous graft repair (major surgery). There were no statistically significant differences regarding types of procedures between the 2 arms.
Outcomes
The primary outcome of this study, hospital LOS, differed significantly in the enoxaparin arm vs UFH: 10.2 days vs 17.5 days, P = .04 (Table 4). The time-to-discharge from initiation of parenteral anticoagulation was significantly reduced with enoxaparin (7.1 days) compared with UFH (11.9 days); P = .04. Although also reduced in the enoxaparin arm, ICU LOS did not show statistical significance (1.1 days vs 4.0 days, P = .09).
About 36% (n = 18) of patients in this study acquired an infection during hospitalization for elective surgery. The most common microorganism and site of infection were Enterococcus species and urinary tract, respectively (Table 5). Nearly half (44%, n = 16) of the patients in the UFH group had a nosocomial infection vs 14% (n = 2) of enoxaparin-bridged patients with a difference approaching significance; P = .056. Both patients in the enoxaparin group had the urinary tract as the primary source of infection; 1 of these patients had a urologic procedure.
Major bleeding occurred in 7% (n = 1) of enoxaparin patients vs 22% (n = 8) in the UFH arm, but this was not found to be statistically significant (P = .41). Minor bleeding was similar between enoxaparin and UFH arms (14% vs 19%, P = .99). Regarding thromboembolic complications, the enoxaparin group (0%) had a numerical reduction compared to UFH (11%) with VTE (n = 4) being the only occurrence of the composite outcome (P = .57). There were 4 deaths within 30 days posthospitalization—all were from the UFH group (P = .57). Due to the small sample size of this study, these outcomes (bleeding and thrombotic events) were not powered to detect a statistically significant difference.
Economic Analysis
The average cost differences (Table 6) of hospitalization between enoxaparin and UFH were calculated using the average LOS per treating specialty multiplied by the national average cost of the MCO for an inpatient bed day in 2018.12 The treating specialty with the longest average LOS in the enoxaparin arm was thoracic (4.7 days). The UFH arm also had a large LOS (average days) for the thoracic specialty (6.4 days); however, the vascular specialty (6.7 days) had the longest average LOS in this group. Due to a mean LOS of 10.2 days in the enoxaparin arm, which was further stratified by treating specialty, the total cost per average inpatient stay was calculated as $51,710. On the other hand, patients in the UFH arm had a total cost per average inpatient stay of $92,848.
Monitoring
Anti-factor Xa levels for LMWH monitoring were not analyzed in this study due to a lack of values collected; only 1 patient had an anti-factor Xa level checked during this time frame. Infusion rates of UFH were adjusted based on aPTT levels collected per MEDVAMC inpatient anticoagulation protocol. The average percentage of aPTT in therapeutic range was 46.3% and the mean time-to-therapeutic range (SD) was about 2.4 (1.3) days. Due to this study’s retrospective nature, there were inconsistencies with availability of documentation of UFH infusion rates. For this reason, these values were not analyzed further.
Discussion
In 2017, the American College of Cardiology published the Periprocedural Anticoagulation Expert Consensus Pathway, which recommends for patients with AF at low risk (CHA2DS2VASc 1-4) of thromboembolism to not be bridged (unless patient had a prior VTE or stroke/TIA).13 Nearly half the patients in this study, were classified as moderate-to-high thrombotic risk as evidenced by a CHA2DS2VASc > 4 with a mean score of 4.8. Due to this study’s retrospective design from 2008 to 2017, many of the clinicians may have referenced the 2008 CHEST antithrombotic guidelines when making the decision to bridge patients; these guidelines and the previous MEDVAMC anticoagulation protocol recommend bridging patients with AF with CHADS2 > 2 (moderate-to-high thrombotic risk) in which all but 1 of the patients in this study met criteria.1,14 In contrast to the landmark BRIDGE trial, the mean CHADS2 score in this study was 3.6; this is an indication that our patient population was of individuals at an increased risk of stroke and embolism.
In addition to thromboembolic complications, patients in the current study also were at increased risk of clinically relevant bleeding with a mean HAS-BLED score of 4.1 and nearly all patients having a score > 3. The complexity of the veteran population also was displayed by this study’s mean CCI (7.7) and RCRI (3.0) indicating a 0% estimated 10-year survival and a 11% increase in having a perioperative cardiac event, respectively. A mean CCI of 7.7 is associated with a 13.3 relative risk of death within 6 years postoperation.15 All patients had a diagnosis of hypertension, and > 75% had this diagnosis complicated by DM. In addition, this patient population was of those with extensive cardiovascular disease or increased risk, which makes for a clinically relevant application of patients who would require periprocedural bridging.
Another positive aspect of this study is that all the baseline characteristics, apart from renal function, were similar between arms, helping to strengthen the ability to adequately compare the 2 bridging modalities. Our assumption for the reasoning that more stage 5 CKD and dialysis patients were anticoagulated with UFH vs enoxaparin is a result of concern for an increased risk of bleeding with a medication that is renally cleared 30% less in CrCl < 30 mL/min.16 Although, enoxaparin 1 mg/kg/d is FDA approved as a therapeutic anticoagulant option, clinicians at MEDVAMC likely had reservations about its use in end-stage CKD patients. Unlike many studies, including the BRIDGE trial, patients with ACKD were not excluded from this trial, and the outcomes with enoxaparin are available for interpretation.
To no surprise, for patients included in this study, enoxaparin use led to shorter hospital LOS, reduced ICU LOS, and a quicker time-to-discharge from initiation. This is credited to the 100% bioavailability of SC enoxaparin in conjunction with its means to be a therapeutic option as an outpatient.16 Unlike IV UFH, patients requiring bridging can be discharged on SC injections of enoxaparin until a therapeutic INR is maintained with warfarin.The duration of hospital LOS in both arms were longer in this study compared with that of other studies.9 This may be due to clinicians being more cautious with renal insufficient patients, and the patients included in this study had multiple comorbidities. According to an economic analysis performed by Amorosi and colleagues in 2004, bridging with enoxaparin instead of UFH can save up to $3,733 per patient and reduce bridging costs by 63% to 85% driven primarily by decreased hospital LOS.10
Economic Outcome
In our study, we conducted a cost analysis using national VA data that indicated a $41,138 or 44% reduction in total cost per average inpatient stay when bridging 1 patient with enoxaparin vs UFH. The benefit of this cost analysis is that it reflects direct costs at VA institutions nationally; this will allow these data to be useful for practitioners at MEDVAMC and other VA hospitals. Stratifying the costs by treating specialty instead of treatment location minimized skewing of the data as there were some patients with long LOS in the ICU. No patients in the enoxaparin arm were treated in otolaryngology, which may have skewed the data. The data included direct costs for beds as well as costs for multiple services, such as procedures, pharmacy, nursing, laboratory tests, and imaging. Unlike the Amorosi study, our review did not include acquisition costs for enoxaparin syringes and bags of UFH or laboratory costs for aPTT and anti-factor Xa levels in part because of the data source and the difficulty calculating costs over a 10-year span.
Patients in the enoxaparin arm had a trend toward fewer occurrences of hospital-acquired infections than did those in the UFH arm, which we believe is due to a decreased LOS (in both total hospital and ICU days) and fewer blood draws needed for monitoring. This also may be attributed to a longer mean duration of surgery in the UFH arm (1.3 hours) vs enoxaparin (0.9 hours). The percentage of patients with procedures ≥ 45 minutes and the types of procedures between both arms were similar. However, these outcomes were not statistically significant. In addition, elderly males who are hospitalized may require a catheter (due to urinary retention), and catheter-associated urinary tract infection (CAUTI) is one of the highest reported infections in acute care hospitals in the US. This is in line with our patient population and may be a supplementary reason for the increase in infection incidence with UFH. Though, whether urinary catheters were used in these patients was not evaluated in this study.
Despite being at an increased risk of experiencing a major adverse cardiovascular event (MACE), no patients in either arm had a stroke/TIA or MI within 30 days postprocedure. The only occurrences documented were VTEs, which happened only in 4 patients on UFH. Four people died in this study, solely in the UFH arm. The incidence of thromboembolic complications and death along with major and minor bleeding cannot be deduced as meaningful as this study was underpowered for these outcomes. Despite anti-factor Xa monitoring being recommended in ACKD patients on enoxaparin, this monitoring was not routinely performed in this study. Another limitation was the inability to adequately assess the appropriateness of nurse-adjusted UFH infusion rates largely due to the retrospective nature of this study. The variability of aPTT percentage in therapeutic range and time-to-therapeutic range reported was indicative of the difficulties of monitoring for the safety and efficacy of UFH.
In 1991, Cruickshank and colleagues conducted a study in which a standard nomogram (similar to the MEDVAMC nomogram) for the adjustment of IV heparin was implemented at a single hospital.17 The success rate (aPTT percentage in therapeutic range) was 59.4% and average time-to-therapeutic range was about 1 day. The success rate (46.3%) and time-to-therapeutic range (2.4 days) in our study were lower and longer, respectively, than was expected. One potential reason for this discrepancy could be the differences in indication as the patients in Cruickshank and colleagues were being treated for VTE, whereas patients in our study had AF or atrial flutter. Also, there were inconsistencies in the availability of documentation of monitoring parameters for heparin due to the study time frame and retrospective design. Patients on UFH who are not within the therapeutic range in a timely manner are at greater risk of MACE and major/minor bleeding. Our study was not powered to detect these findings.
Strengths and Limitations
A significant limitation of this study was its small sample size; the study was not able to meet power for the primary outcome; it is unknown whether our study met power for nosocomial infections. The study also was not a powered review of other adverse events, such as thromboembolic complications, bleeding, and death. The study had an uneven number of patients, which made it more difficult to appropriately compare 2 patient populations; the study also did not include medians for patient characteristics and outcomes.
Due to this study’s time frame, the clinical pharmacy services at MEDVAMC were not as robust as they are now, which is the reason the decisions on which anticoagulant to use were primarily physician based. The use of TheraDoc to identify patients posed the risk of missing patients who may not have had the appropriate laboratory tests performed (ie, SCr). Patients on UFH had a reduced eGFR compared with that of enoxaparin, which may limit our extrapolation of enoxaparin’s use in end-stage renal disease. The reduced eGFR and higher number of dialysis patients in the UFH arm may have increased the occurrence of more labile INRs and bleeding outcomes. Patients on hemodialysis typically have more comorbidities and an increased risk of infection due to the frequent use of catheters and needles to access the bloodstream. In addition, the potential differences in catheter use and duration between groups were not identified. If these parameters were studied, the data collected may have helped better explain the reasoning for increased incidence of infection in the UFH arm.
Strengths of this study include a complex patient population with similar characteristics, distribution of ethnicities representative of the US population, patients at moderate-to-high thrombotic risk, the analysis of nosocomial infections, and the exclusion of patients with normal renal function or moderate CKD.
Conclusion
To our knowledge, this is the first study to compare periprocedural bridging outcomes and incidence of nosocomial infections in patients with AF and ACKD. This review provides new evidence that in this patient population, enoxaparin is a potential anticoagulant to reduce hospital LOS and hospital-acquired infections. Compared with UFH, bridging with enoxaparin reduced hospital LOS and anticoagulation time-to-discharge by 7 and 5 days, respectively, and decreased the incidence of nosocomial infections by 30%. Using the mean LOS per treating specialty for both arms, bridging 1 patient with AF with enoxaparin vs UFH can potentially lead to an estimated $40,000 (44%) reduction in total cost of hospitalization. Enoxaparin also had no numeric differences in mortality and adverse events (stroke/TIA, MI, VTE) vs that of UFH, but it is important to note that this study was not powered to find a significant difference in these outcomes. Due to the mean eGFR of patients on enoxaparin being 22.6 mL/min/1.73 m2 and only 1 in 5 having stage 5 CKD, at this time, we do not recommend enoxaparin for periprocedural use in stage 5 CKD or in patients on hemodialysis. Larger studies are needed, including randomized trials, in this patient population to further evaluate these outcomes and assess the use of enoxaparin in patients with ACKD.
There has been a long-standing controversy in the use of parenteral anticoagulation for perioperative bridging in patients with atrial fibrillation (AF) pursuing elective surgery.1 The decision to bridge is dependent on the patient’s risk of thromboembolic complications and susceptibility to bleed.1 The BRIDGE trial showed noninferiority in rate of stroke and embolism events between low molecular weight heparins (LMWHs) and no perioperative bridging.2 However, according to the American College of Chest Physicians (CHEST) 2012 guidelines, patients in the BRIDGE trial would be deemed low risk for thromboembolic events displayed by a mean CHADS2 (congestive heart failure [CHF], hypertension, age, diabetes mellitus, and stroke/transient ischemic attack) score of 2.3. Also, the BRIDGE study and many others excluded patients with advanced forms of chronic kidney disease (CKD).2,3
Similar to patients with AF, patients with advanced CKD (ACKD, stage 4 and 5 CKD) have an increased risk of stroke and venous thromboembolism (VTE).4,5 Patients with AF and ACKD have not been adequately studied for perioperative anticoagulation bridging outcomes. Although unfractionated heparin (UFH) is preferred over LMWH in ACKD patients,enoxaparin can be used in this population.1,6 Enoxaparin 1 mg/kg once daily is approved by the US Food and Drug Administration (FDA) for use in patients with severe renal insufficiency defined as creatinine clearance (CrCl) < 30 mL/min. This dosage adjustment is subsequent to studies with enoxaparin 1 mg/kg twice daily that showed a significant increase in major and minor bleeding in severe renal-insufficient patients with CrCl < 30 mL/min vs patients with CrCl > 30 mL/min.7 When comparing the myocardial infarction (MI) outcomes of severe renal-insufficient patients in the ExTRACT-TIMI 25 trial, enoxaparin 1 mg/kg once daily had no significant difference in nonfatal major bleeding vs UFH.8 In patients without renal impairment (no documentation of kidney disease), bridging therapy with LMWH was completed more than UFH in < 24 hours of hospital stay and with similar rates of VTEs and major bleeding.9 In addition to its ability to be administered outpatient, enoxaparin has a more predictable pharmacokinetic profile, allowing for less monitoring and a lower incidence of heparin-induced thrombocytopenia (HIT) vs that of UFH.6
The Michael E. DeBakey Veteran Affairs Medical Center (MEDVAMC) in Houston, Texas, is one of the largest US Department of Veterans Affairs (VA) hospitals in the US, managing > 150,000 veterans in Southeast Texas and other southern states. As a referral center for traveling patients, it is crucial that MEDVAMC decrease hospital length of stay (LOS) to increase space for incoming patients. Reducing LOS also reduces costs and may have a correlation with decreasing the incidence of nosocomial infections. Because of its significance to this facility, hospital LOS is an appropriate primary outcome for this study.
To our knowledge, bridging outcomes between LMWH and UFH in patients with AF and ACKD have never been studied. We hypothesized that using enoxaparin instead of heparin for periprocedural management would result in decreased hospital LOS, leading to a lower economic burden and lower incidence of nosocomial infections with no significant differences in major and minor bleeding and thromboembolic complications.10
Methods
This study was a single-center, retrospective chart review of adult patients from January 2008 to September 2017. The review was conducted at MEDVAMC and was approved by the research and development committee and by the Baylor College of Medicine Institutional Review Board. Formal consent was not required.
Included patients were aged ≥ 18 years with diagnoses of AF or atrial flutter and ACKD as recognized by a glomerular filtration rate (eGFR) of < 30 mL/min/1.73 m2 as calculated by use of the Modification of Diet in Renal Disease Study (MDRD) equation.11 Patients must have previously been on warfarin and required temporary interruption of warfarin for an elective procedure. During the interruption of warfarin therapy, a requirement was set for patients to be on periprocedural anticoagulation with subcutaneous (SC) enoxaparin 1 mg/kg daily or continuous IV heparin per MEDVAMC heparin protocol. Patients were excluded if they had experienced major bleeding in the 6 weeks prior to the elective procedure, had current thrombocytopenia (platelet count < 100 × 109/L), or had a history of heparin-induced thrombocytopenia (HIT) or a heparin allergy.
This patient population was identified using TheraDoc Clinical Surveillance Software System (Charlotte, NC), which has prebuilt alert reviews for anticoagulation medications, including enoxaparin and heparin. An alert for patients on enoxaparin with serum creatinine (SCr) > 1.5 mg/dL was used to screen patients who met the inclusion criteria. A second alert identified patients on heparin. The VA Computerized Patient Record System (CPRS) was used to collect patient data.
Economic Analysis
An economic analysis was conducted using data from the VA Managerial Cost Accounting Reports. Data on the national average cost per bed day was used for the purpose of extrapolating this information to multiple VA institutions.12 National average cost per day was determined by dividing the total cost by the number of bed days for the identified treating specialty during the fiscal period of 2018. Average cost per day data included costs for bed day, surgery, radiology services, laboratory tests, pharmacy services, treatment location (ie, intensive care units [ICUs]) and all other costs associated with an inpatient stay. A cost analysis was performed using this average cost per bed day and the mean LOS between enoxaparin and UFH for each treating specialty. The major outcome of the cost analysis was the total cost per average inpatient stay. The national average cost per bed day for each treating specialty was multiplied by the average LOS found for each treating specialty in this study; the sum of all the average costs per inpatient stay for the treating specialties resulted in the total cost per average inpatient stay. Permission to use these data was granted by the Pharmacy and Critical Care Services at MEDVAMC.
Patient Demographics and Characteristics
Data were collected on patient demographics (Table 1). Nosocomial infections, stroke/transient ischemic attack, MI, VTE, major and minor bleeding, and death are defined in Table 2.
The primary outcome of the study was hospital LOS. The study was powered at 90% for α = .05, which gives a required study population of 114 (1:1 enrollment ratio) patients to determine a statistically significant difference in hospital stay. This sample size was calculated using the mean hospital LOS (the primary objective) in the REGIMEN registry for LMWH (4.6 days) and UFH (10.3 days).9 To our knowledge, the incidence of nosocomial infections (a secondary outcome) has not been studied in this patient population; therefore, there was no basis to assess an appropriate sample size to find a difference in this outcome. Furthermore, the goal was to collect as many patients as possible to best assess this variable. Because of an expected high exclusion rate, 504 patients were reviewed to target a sample size of 120 patients. Due to the single-center nature of this review, the secondary outcomes of thromboembolic complications and major and minor bleeding were expected to be underpowered.
The final analysis compared the enoxaparin arm with the UFH arm. Univariate differences between the treatment groups were compared using the Fisher exact test for categorical variables. Demographic data and other continuous variables were analyzed by an unpaired t test to compare means between the 2 arms. Outcomes and characteristics were deemed statistically significant when α (P value) was < .05. All P values reported were 2-tailed with a 95% CI. No statistical analysis was performed for the cost differences (based on LOS per treating specialty) in the 2 treatment arms. Statistical analyses were completed by utilizing GraphPad Software (San Diego, CA).
Results
In total, 50 patients were analyzed in the study. There were 36 patients bridged with IV UFH at a concentration of 25,000 U/250 mL with an initial infusion rate of 12 U/kg/h. For the other arm, 14 patients were anticoagulated with renally dosed enoxaparin 1 mg/kg/d with an average daily dose of 89.3 mg; the mean actual body weight in this group was 90.9 mg (correlates with enoxaparin daily dose). Physicians of the primary team decided which parenteral anticoagulant to use. The difference in mean duration of inpatient parental anticoagulation between both groups was not statistically significant: enoxaparin at 7.1 days and UFH at 9.6 days (P = .19). Patients in the enoxaparin arm were off warfarin therapy for an average of 6.0 days vs 7.5 days for the UFH group (P = .29). The duration of outpatient anticoagulation with enoxaparin was not analyzed in this study.
Patient and Procedure Characteristics
All patients had AF or atrial flutter with 86% of patients (n = 43) having a CHADS2 > 2 and 48% (n = 29) having a CHA2DS2VASc > 4. Overall, the mean age was 71.3 years with similarities in ethnicity distribution. Patients had multiple comorbidities as shown by a mean Charlson Comorbidity Index (CCI) of 7.7 and an increased risk of bleeding as evidenced by 98% (n = 48) of patients having a HAS-BLED score of ≥ 3. A greater percentage of patients bridged with enoxaparin had DM, history of stroke and MI, and a heart valve, whereas UFH patients were more likely to be in stage 5 CKD (eGFR < 15 mL/min/1.73m2) with a significantly lower mean eGFR (16.76 vs 22.64, P = .03). Furthermore, there were more patients on hemodialysis in the UFH (50%) arm vs enoxaparin (21%) arm and a lower mean CrCl with UFH (20.1 mL/min) compared with enoxaparin (24.9 mL/min); however, the differences in hemodialysis and mean CrCl were not statistically significant. There were no patients on peritoneal dialysis in this review.
Procedure Characteristics
The average Revised Cardiac Risk Index (RCRI) score was about 3, indicating that these patients were at a Class IV risk (11%) of having a perioperative cardiac event (Table 3). Nineteen patients (38%) elected for a major surgery with all but 1 of the surgeries (major or minor) being invasive. The average length of surgery was 1.2 hours, and patients were more likely to undergo cardiothoracic procedures (38%). There were 2 out of 14 (14%) patients on enoxaparin who were able to have surgery as an outpatient; whereas this did not occur in patients on UFH. The procedures completed for these patients were a colostomy (minor surgery) and arteriovenous graft repair (major surgery). There were no statistically significant differences regarding types of procedures between the 2 arms.
Outcomes
The primary outcome of this study, hospital LOS, differed significantly in the enoxaparin arm vs UFH: 10.2 days vs 17.5 days, P = .04 (Table 4). The time-to-discharge from initiation of parenteral anticoagulation was significantly reduced with enoxaparin (7.1 days) compared with UFH (11.9 days); P = .04. Although also reduced in the enoxaparin arm, ICU LOS did not show statistical significance (1.1 days vs 4.0 days, P = .09).
About 36% (n = 18) of patients in this study acquired an infection during hospitalization for elective surgery. The most common microorganism and site of infection were Enterococcus species and urinary tract, respectively (Table 5). Nearly half (44%, n = 16) of the patients in the UFH group had a nosocomial infection vs 14% (n = 2) of enoxaparin-bridged patients with a difference approaching significance; P = .056. Both patients in the enoxaparin group had the urinary tract as the primary source of infection; 1 of these patients had a urologic procedure.
Major bleeding occurred in 7% (n = 1) of enoxaparin patients vs 22% (n = 8) in the UFH arm, but this was not found to be statistically significant (P = .41). Minor bleeding was similar between enoxaparin and UFH arms (14% vs 19%, P = .99). Regarding thromboembolic complications, the enoxaparin group (0%) had a numerical reduction compared to UFH (11%) with VTE (n = 4) being the only occurrence of the composite outcome (P = .57). There were 4 deaths within 30 days posthospitalization—all were from the UFH group (P = .57). Due to the small sample size of this study, these outcomes (bleeding and thrombotic events) were not powered to detect a statistically significant difference.
Economic Analysis
The average cost differences (Table 6) of hospitalization between enoxaparin and UFH were calculated using the average LOS per treating specialty multiplied by the national average cost of the MCO for an inpatient bed day in 2018.12 The treating specialty with the longest average LOS in the enoxaparin arm was thoracic (4.7 days). The UFH arm also had a large LOS (average days) for the thoracic specialty (6.4 days); however, the vascular specialty (6.7 days) had the longest average LOS in this group. Due to a mean LOS of 10.2 days in the enoxaparin arm, which was further stratified by treating specialty, the total cost per average inpatient stay was calculated as $51,710. On the other hand, patients in the UFH arm had a total cost per average inpatient stay of $92,848.
Monitoring
Anti-factor Xa levels for LMWH monitoring were not analyzed in this study due to a lack of values collected; only 1 patient had an anti-factor Xa level checked during this time frame. Infusion rates of UFH were adjusted based on aPTT levels collected per MEDVAMC inpatient anticoagulation protocol. The average percentage of aPTT in therapeutic range was 46.3% and the mean time-to-therapeutic range (SD) was about 2.4 (1.3) days. Due to this study’s retrospective nature, there were inconsistencies with availability of documentation of UFH infusion rates. For this reason, these values were not analyzed further.
Discussion
In 2017, the American College of Cardiology published the Periprocedural Anticoagulation Expert Consensus Pathway, which recommends for patients with AF at low risk (CHA2DS2VASc 1-4) of thromboembolism to not be bridged (unless patient had a prior VTE or stroke/TIA).13 Nearly half the patients in this study, were classified as moderate-to-high thrombotic risk as evidenced by a CHA2DS2VASc > 4 with a mean score of 4.8. Due to this study’s retrospective design from 2008 to 2017, many of the clinicians may have referenced the 2008 CHEST antithrombotic guidelines when making the decision to bridge patients; these guidelines and the previous MEDVAMC anticoagulation protocol recommend bridging patients with AF with CHADS2 > 2 (moderate-to-high thrombotic risk) in which all but 1 of the patients in this study met criteria.1,14 In contrast to the landmark BRIDGE trial, the mean CHADS2 score in this study was 3.6; this is an indication that our patient population was of individuals at an increased risk of stroke and embolism.
In addition to thromboembolic complications, patients in the current study also were at increased risk of clinically relevant bleeding with a mean HAS-BLED score of 4.1 and nearly all patients having a score > 3. The complexity of the veteran population also was displayed by this study’s mean CCI (7.7) and RCRI (3.0) indicating a 0% estimated 10-year survival and a 11% increase in having a perioperative cardiac event, respectively. A mean CCI of 7.7 is associated with a 13.3 relative risk of death within 6 years postoperation.15 All patients had a diagnosis of hypertension, and > 75% had this diagnosis complicated by DM. In addition, this patient population was of those with extensive cardiovascular disease or increased risk, which makes for a clinically relevant application of patients who would require periprocedural bridging.
Another positive aspect of this study is that all the baseline characteristics, apart from renal function, were similar between arms, helping to strengthen the ability to adequately compare the 2 bridging modalities. Our assumption for the reasoning that more stage 5 CKD and dialysis patients were anticoagulated with UFH vs enoxaparin is a result of concern for an increased risk of bleeding with a medication that is renally cleared 30% less in CrCl < 30 mL/min.16 Although, enoxaparin 1 mg/kg/d is FDA approved as a therapeutic anticoagulant option, clinicians at MEDVAMC likely had reservations about its use in end-stage CKD patients. Unlike many studies, including the BRIDGE trial, patients with ACKD were not excluded from this trial, and the outcomes with enoxaparin are available for interpretation.
To no surprise, for patients included in this study, enoxaparin use led to shorter hospital LOS, reduced ICU LOS, and a quicker time-to-discharge from initiation. This is credited to the 100% bioavailability of SC enoxaparin in conjunction with its means to be a therapeutic option as an outpatient.16 Unlike IV UFH, patients requiring bridging can be discharged on SC injections of enoxaparin until a therapeutic INR is maintained with warfarin.The duration of hospital LOS in both arms were longer in this study compared with that of other studies.9 This may be due to clinicians being more cautious with renal insufficient patients, and the patients included in this study had multiple comorbidities. According to an economic analysis performed by Amorosi and colleagues in 2004, bridging with enoxaparin instead of UFH can save up to $3,733 per patient and reduce bridging costs by 63% to 85% driven primarily by decreased hospital LOS.10
Economic Outcome
In our study, we conducted a cost analysis using national VA data that indicated a $41,138 or 44% reduction in total cost per average inpatient stay when bridging 1 patient with enoxaparin vs UFH. The benefit of this cost analysis is that it reflects direct costs at VA institutions nationally; this will allow these data to be useful for practitioners at MEDVAMC and other VA hospitals. Stratifying the costs by treating specialty instead of treatment location minimized skewing of the data as there were some patients with long LOS in the ICU. No patients in the enoxaparin arm were treated in otolaryngology, which may have skewed the data. The data included direct costs for beds as well as costs for multiple services, such as procedures, pharmacy, nursing, laboratory tests, and imaging. Unlike the Amorosi study, our review did not include acquisition costs for enoxaparin syringes and bags of UFH or laboratory costs for aPTT and anti-factor Xa levels in part because of the data source and the difficulty calculating costs over a 10-year span.
Patients in the enoxaparin arm had a trend toward fewer occurrences of hospital-acquired infections than did those in the UFH arm, which we believe is due to a decreased LOS (in both total hospital and ICU days) and fewer blood draws needed for monitoring. This also may be attributed to a longer mean duration of surgery in the UFH arm (1.3 hours) vs enoxaparin (0.9 hours). The percentage of patients with procedures ≥ 45 minutes and the types of procedures between both arms were similar. However, these outcomes were not statistically significant. In addition, elderly males who are hospitalized may require a catheter (due to urinary retention), and catheter-associated urinary tract infection (CAUTI) is one of the highest reported infections in acute care hospitals in the US. This is in line with our patient population and may be a supplementary reason for the increase in infection incidence with UFH. Though, whether urinary catheters were used in these patients was not evaluated in this study.
Despite being at an increased risk of experiencing a major adverse cardiovascular event (MACE), no patients in either arm had a stroke/TIA or MI within 30 days postprocedure. The only occurrences documented were VTEs, which happened only in 4 patients on UFH. Four people died in this study, solely in the UFH arm. The incidence of thromboembolic complications and death along with major and minor bleeding cannot be deduced as meaningful as this study was underpowered for these outcomes. Despite anti-factor Xa monitoring being recommended in ACKD patients on enoxaparin, this monitoring was not routinely performed in this study. Another limitation was the inability to adequately assess the appropriateness of nurse-adjusted UFH infusion rates largely due to the retrospective nature of this study. The variability of aPTT percentage in therapeutic range and time-to-therapeutic range reported was indicative of the difficulties of monitoring for the safety and efficacy of UFH.
In 1991, Cruickshank and colleagues conducted a study in which a standard nomogram (similar to the MEDVAMC nomogram) for the adjustment of IV heparin was implemented at a single hospital.17 The success rate (aPTT percentage in therapeutic range) was 59.4% and average time-to-therapeutic range was about 1 day. The success rate (46.3%) and time-to-therapeutic range (2.4 days) in our study were lower and longer, respectively, than was expected. One potential reason for this discrepancy could be the differences in indication as the patients in Cruickshank and colleagues were being treated for VTE, whereas patients in our study had AF or atrial flutter. Also, there were inconsistencies in the availability of documentation of monitoring parameters for heparin due to the study time frame and retrospective design. Patients on UFH who are not within the therapeutic range in a timely manner are at greater risk of MACE and major/minor bleeding. Our study was not powered to detect these findings.
Strengths and Limitations
A significant limitation of this study was its small sample size; the study was not able to meet power for the primary outcome; it is unknown whether our study met power for nosocomial infections. The study also was not a powered review of other adverse events, such as thromboembolic complications, bleeding, and death. The study had an uneven number of patients, which made it more difficult to appropriately compare 2 patient populations; the study also did not include medians for patient characteristics and outcomes.
Due to this study’s time frame, the clinical pharmacy services at MEDVAMC were not as robust as they are now, which is the reason the decisions on which anticoagulant to use were primarily physician based. The use of TheraDoc to identify patients posed the risk of missing patients who may not have had the appropriate laboratory tests performed (ie, SCr). Patients on UFH had a reduced eGFR compared with that of enoxaparin, which may limit our extrapolation of enoxaparin’s use in end-stage renal disease. The reduced eGFR and higher number of dialysis patients in the UFH arm may have increased the occurrence of more labile INRs and bleeding outcomes. Patients on hemodialysis typically have more comorbidities and an increased risk of infection due to the frequent use of catheters and needles to access the bloodstream. In addition, the potential differences in catheter use and duration between groups were not identified. If these parameters were studied, the data collected may have helped better explain the reasoning for increased incidence of infection in the UFH arm.
Strengths of this study include a complex patient population with similar characteristics, distribution of ethnicities representative of the US population, patients at moderate-to-high thrombotic risk, the analysis of nosocomial infections, and the exclusion of patients with normal renal function or moderate CKD.
Conclusion
To our knowledge, this is the first study to compare periprocedural bridging outcomes and incidence of nosocomial infections in patients with AF and ACKD. This review provides new evidence that in this patient population, enoxaparin is a potential anticoagulant to reduce hospital LOS and hospital-acquired infections. Compared with UFH, bridging with enoxaparin reduced hospital LOS and anticoagulation time-to-discharge by 7 and 5 days, respectively, and decreased the incidence of nosocomial infections by 30%. Using the mean LOS per treating specialty for both arms, bridging 1 patient with AF with enoxaparin vs UFH can potentially lead to an estimated $40,000 (44%) reduction in total cost of hospitalization. Enoxaparin also had no numeric differences in mortality and adverse events (stroke/TIA, MI, VTE) vs that of UFH, but it is important to note that this study was not powered to find a significant difference in these outcomes. Due to the mean eGFR of patients on enoxaparin being 22.6 mL/min/1.73 m2 and only 1 in 5 having stage 5 CKD, at this time, we do not recommend enoxaparin for periprocedural use in stage 5 CKD or in patients on hemodialysis. Larger studies are needed, including randomized trials, in this patient population to further evaluate these outcomes and assess the use of enoxaparin in patients with ACKD.
1. Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2)(suppl):e326S-350S.
2. Douketis JD, Spyropoulos AC, Kaatz S, et al; BRIDGE Investigators. Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med. 2015;373(9):823-833.
3. Hammerstingl C, Schmitz A, Fimmers R, Omran H. Bridging of chronic oral anticoagulation with enoxaparin in patients with atrial fibrillation: results from the prospective BRAVE registry. Cardiovasc Ther. 2009;27(4):230-238.
4. Dad T, Weiner DE. Stroke and chronic kidney disease: epidemiology, pathogenesis, and management across kidney disease stages. Semin Nephrol. 2015;35(4):311-322.
5. Wattanakit K, Cushman M. Chronic kidney disease and venous thromboembolism: epidemiology and mechanisms. Curr Opin Pulm Med. 2009;15(5):408-412.
6. Saltiel M. Dosing low molecular weight heparins in kidney disease. J Pharm Pract. 2010;23(3):205-209.
7. Spinler SA, Inverso SM, Cohen M, Goodman SG, Stringer KA, Antman EM; ESSENCE and TIMI 11B Investigators. Safety and efficacy of unfractionated heparin versus enoxaparin in patients who are obese and patients with severe renal impairment: analysis from the ESSENCE and TIMI 11B studies. Am Heart J. 2003;146(1):33-41.
8. Fox KA, Antman EM, Montalescot G, et al. The impact of renal dysfunction on outcomes in the ExTRACT-TIMI 25 trial. J Am Coll Cardiol. 2007;49(23):2249-2255.
9. Spyropoulos AC, Turpie AG, Dunn AS, et al; REGIMEN Investigators. Clinical outcomes with unfractionated heparin or low-molecular-weight heparin as bridging therapy in patients on long-term oral anticoagulants: the REGIMEN registry. J Thromb Haemost. 2006;4(6):1246-1252.
10. Amorosi SL, Tsilimingras K, Thompson D, Fanikos J, Weinstein MC, Goldhaber SZ. Cost analysis of “bridging therapy” with low-molecular-weight heparin versus unfractionated heparin during temporary interruption of chronic anticoagulation. Am J Cardiol. 2004;93(4):509-511.
11. Inker LA, Astor BC, Fox CH, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63(5):713-735.
12. US Department of Veteran Affairs. Managerial Cost Accounting Financial User Support Reports: fiscal year 2018. https://www.herc.research.va.gov/include/page.asp?id=managerial-cost-accounting. [Source not verified.]
13. Doherty JU, Gluckman TJ, Hucker WJ, et al. 2017 ACC Expert Consensus Decision Pathway for Periprocedural Management of Anticoagulation in Patients With Nonvalvular Atrial Fibrillation: a report of the American College of Cardiology Clinical Expert Consensus Document Task Force. J Am Coll Cardiol. 2017;69(7):871-898.
14. Kearon C, Kahn SR, Agnelli G, et al. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 suppl):454S-545S.
15. Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245-1251.
16. Lovenox [package insert]. Bridgewater, NJ: Sanofi-Aventis; December 2017.
17. Cruickshank MK, Levine MN, Hirsh J, Roberts R, Siguenza M. A standard heparin nomogram for the management of heparin therapy. Arch Intern Med. 1991;151(2):333-337.
18. Steinberg BA, Peterson ED, Kim S, et al; Outcomes Registry for Better Informed Treatment of Atrial Fibrillation Investigators and Patients. Use and outcomes associated with bridging during anticoagulation interruptions in patients with atrial fibrillation: findings from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Circulation. 2015;131(5):488-494.
19. Verheugt FW, Steinhubl SR, Hamon M, et al. Incidence, prognostic impact, and influence of antithrombotic therapy on access and nonaccess site bleeding in percutaneous coronary intervention. JACC Cardiovasc Interv. 2011;4(2):191-197.
20. Bijsterveld NR, Peters RJ, Murphy SA, Bernink PJ, Tijssen JG, Cohen M. Recurrent cardiac ischemic events early after discontinuation of short-term heparin treatment in acute coronary syndromes: results from the Thrombolysis in Myocardial Infarction (TIMI) 11B and Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q-Wave Coronary Events (ESSENCE) studies. J Am Coll Cardiol. 2003;42(12):2083-2089.
1. Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2)(suppl):e326S-350S.
2. Douketis JD, Spyropoulos AC, Kaatz S, et al; BRIDGE Investigators. Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med. 2015;373(9):823-833.
3. Hammerstingl C, Schmitz A, Fimmers R, Omran H. Bridging of chronic oral anticoagulation with enoxaparin in patients with atrial fibrillation: results from the prospective BRAVE registry. Cardiovasc Ther. 2009;27(4):230-238.
4. Dad T, Weiner DE. Stroke and chronic kidney disease: epidemiology, pathogenesis, and management across kidney disease stages. Semin Nephrol. 2015;35(4):311-322.
5. Wattanakit K, Cushman M. Chronic kidney disease and venous thromboembolism: epidemiology and mechanisms. Curr Opin Pulm Med. 2009;15(5):408-412.
6. Saltiel M. Dosing low molecular weight heparins in kidney disease. J Pharm Pract. 2010;23(3):205-209.
7. Spinler SA, Inverso SM, Cohen M, Goodman SG, Stringer KA, Antman EM; ESSENCE and TIMI 11B Investigators. Safety and efficacy of unfractionated heparin versus enoxaparin in patients who are obese and patients with severe renal impairment: analysis from the ESSENCE and TIMI 11B studies. Am Heart J. 2003;146(1):33-41.
8. Fox KA, Antman EM, Montalescot G, et al. The impact of renal dysfunction on outcomes in the ExTRACT-TIMI 25 trial. J Am Coll Cardiol. 2007;49(23):2249-2255.
9. Spyropoulos AC, Turpie AG, Dunn AS, et al; REGIMEN Investigators. Clinical outcomes with unfractionated heparin or low-molecular-weight heparin as bridging therapy in patients on long-term oral anticoagulants: the REGIMEN registry. J Thromb Haemost. 2006;4(6):1246-1252.
10. Amorosi SL, Tsilimingras K, Thompson D, Fanikos J, Weinstein MC, Goldhaber SZ. Cost analysis of “bridging therapy” with low-molecular-weight heparin versus unfractionated heparin during temporary interruption of chronic anticoagulation. Am J Cardiol. 2004;93(4):509-511.
11. Inker LA, Astor BC, Fox CH, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63(5):713-735.
12. US Department of Veteran Affairs. Managerial Cost Accounting Financial User Support Reports: fiscal year 2018. https://www.herc.research.va.gov/include/page.asp?id=managerial-cost-accounting. [Source not verified.]
13. Doherty JU, Gluckman TJ, Hucker WJ, et al. 2017 ACC Expert Consensus Decision Pathway for Periprocedural Management of Anticoagulation in Patients With Nonvalvular Atrial Fibrillation: a report of the American College of Cardiology Clinical Expert Consensus Document Task Force. J Am Coll Cardiol. 2017;69(7):871-898.
14. Kearon C, Kahn SR, Agnelli G, et al. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 suppl):454S-545S.
15. Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245-1251.
16. Lovenox [package insert]. Bridgewater, NJ: Sanofi-Aventis; December 2017.
17. Cruickshank MK, Levine MN, Hirsh J, Roberts R, Siguenza M. A standard heparin nomogram for the management of heparin therapy. Arch Intern Med. 1991;151(2):333-337.
18. Steinberg BA, Peterson ED, Kim S, et al; Outcomes Registry for Better Informed Treatment of Atrial Fibrillation Investigators and Patients. Use and outcomes associated with bridging during anticoagulation interruptions in patients with atrial fibrillation: findings from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Circulation. 2015;131(5):488-494.
19. Verheugt FW, Steinhubl SR, Hamon M, et al. Incidence, prognostic impact, and influence of antithrombotic therapy on access and nonaccess site bleeding in percutaneous coronary intervention. JACC Cardiovasc Interv. 2011;4(2):191-197.
20. Bijsterveld NR, Peters RJ, Murphy SA, Bernink PJ, Tijssen JG, Cohen M. Recurrent cardiac ischemic events early after discontinuation of short-term heparin treatment in acute coronary syndromes: results from the Thrombolysis in Myocardial Infarction (TIMI) 11B and Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q-Wave Coronary Events (ESSENCE) studies. J Am Coll Cardiol. 2003;42(12):2083-2089.