User login
Higher dietary vitamin A linked to lower SCC risk
in a large prospective study published in JAMA Dermatology.
There was also an inverse association between intake of carotenoids and risk of cutaneous SCC over the follow-up period of 26-28 years. The results of the study support “the protective role of vitamin A against SCC development,” wrote Jongwoo Kim, MD, of Brown University, Providence, R.I., and Inje University, Seoul, South Korea, and coauthors. “Our data further support the contention that supplemental and dietary vitamin A may be beneficial in preventing SCC,” they added.
The study evaluated intake of vitamin A and carotenoids and SCC risk with data from the Health Professionals Follow-Up Study (1986-2012) of 48,400 men, and the Nurses’ Health Study (1984-2012) of 75,170 women. Participants in those studies completed questionnaires based on lifestyle and medical history. Only white participants were included, because of the low number of SCC cases and low SCC risk in nonwhite participants, and participants who did not report diet and those who had a history of melanoma, SCC, or other cancer diagnoses at baseline were excluded.
Over the follow-up of 26-28 years, a total of 3,978 SCC cases were confirmed using pathological records. The investigators used different quintiles based on the median total amount of vitamin A intake. Using quintile 1 (lowest intake) as a reference, the pooled multivariate hazard ratios of vitamin A intake were 0.97, 0.97, 0.93, and 0.83 for quintiles 2, 3, 4, and 5, respectively (P less than .001 for the trend, in order of increasing quintiles).
In addition, they reported that greater intakes of retinol and several carotenoids were also significantly associated with a lower SCC risk.
The results were “generally consistent between men and women,” and “the inverse associations appeared to be more prominent among those with moles and those with burn or blistering sunburn reaction as children or adolescents,” they wrote.
The large sample size, prospective design, and confirmation of SCC cases by histology are among the strengths of the study, while a key limitation of the study was the homogeneous nature of the study population, which “may limit the generalizability of our findings,” the authors wrote.
The study was funded by the National Institutes of Health and Inje University (South Korea). One author reported serving as a consultant for AbbVie, Amgen, the Centers for Disease Control and Prevention, Janssen, Merck, Novartis, and Pfizer; and as a compensated investigator for Amgen, Regeneron, and Sanofi. Dr. Kim and the remaining three authors reported no disclosures.
SOURCE: Kim J et al. JAMA Dermatol. 2019 Jul 31. doi: 10.1001/jamadermatol.2019.1937.
in a large prospective study published in JAMA Dermatology.
There was also an inverse association between intake of carotenoids and risk of cutaneous SCC over the follow-up period of 26-28 years. The results of the study support “the protective role of vitamin A against SCC development,” wrote Jongwoo Kim, MD, of Brown University, Providence, R.I., and Inje University, Seoul, South Korea, and coauthors. “Our data further support the contention that supplemental and dietary vitamin A may be beneficial in preventing SCC,” they added.
The study evaluated intake of vitamin A and carotenoids and SCC risk with data from the Health Professionals Follow-Up Study (1986-2012) of 48,400 men, and the Nurses’ Health Study (1984-2012) of 75,170 women. Participants in those studies completed questionnaires based on lifestyle and medical history. Only white participants were included, because of the low number of SCC cases and low SCC risk in nonwhite participants, and participants who did not report diet and those who had a history of melanoma, SCC, or other cancer diagnoses at baseline were excluded.
Over the follow-up of 26-28 years, a total of 3,978 SCC cases were confirmed using pathological records. The investigators used different quintiles based on the median total amount of vitamin A intake. Using quintile 1 (lowest intake) as a reference, the pooled multivariate hazard ratios of vitamin A intake were 0.97, 0.97, 0.93, and 0.83 for quintiles 2, 3, 4, and 5, respectively (P less than .001 for the trend, in order of increasing quintiles).
In addition, they reported that greater intakes of retinol and several carotenoids were also significantly associated with a lower SCC risk.
The results were “generally consistent between men and women,” and “the inverse associations appeared to be more prominent among those with moles and those with burn or blistering sunburn reaction as children or adolescents,” they wrote.
The large sample size, prospective design, and confirmation of SCC cases by histology are among the strengths of the study, while a key limitation of the study was the homogeneous nature of the study population, which “may limit the generalizability of our findings,” the authors wrote.
The study was funded by the National Institutes of Health and Inje University (South Korea). One author reported serving as a consultant for AbbVie, Amgen, the Centers for Disease Control and Prevention, Janssen, Merck, Novartis, and Pfizer; and as a compensated investigator for Amgen, Regeneron, and Sanofi. Dr. Kim and the remaining three authors reported no disclosures.
SOURCE: Kim J et al. JAMA Dermatol. 2019 Jul 31. doi: 10.1001/jamadermatol.2019.1937.
in a large prospective study published in JAMA Dermatology.
There was also an inverse association between intake of carotenoids and risk of cutaneous SCC over the follow-up period of 26-28 years. The results of the study support “the protective role of vitamin A against SCC development,” wrote Jongwoo Kim, MD, of Brown University, Providence, R.I., and Inje University, Seoul, South Korea, and coauthors. “Our data further support the contention that supplemental and dietary vitamin A may be beneficial in preventing SCC,” they added.
The study evaluated intake of vitamin A and carotenoids and SCC risk with data from the Health Professionals Follow-Up Study (1986-2012) of 48,400 men, and the Nurses’ Health Study (1984-2012) of 75,170 women. Participants in those studies completed questionnaires based on lifestyle and medical history. Only white participants were included, because of the low number of SCC cases and low SCC risk in nonwhite participants, and participants who did not report diet and those who had a history of melanoma, SCC, or other cancer diagnoses at baseline were excluded.
Over the follow-up of 26-28 years, a total of 3,978 SCC cases were confirmed using pathological records. The investigators used different quintiles based on the median total amount of vitamin A intake. Using quintile 1 (lowest intake) as a reference, the pooled multivariate hazard ratios of vitamin A intake were 0.97, 0.97, 0.93, and 0.83 for quintiles 2, 3, 4, and 5, respectively (P less than .001 for the trend, in order of increasing quintiles).
In addition, they reported that greater intakes of retinol and several carotenoids were also significantly associated with a lower SCC risk.
The results were “generally consistent between men and women,” and “the inverse associations appeared to be more prominent among those with moles and those with burn or blistering sunburn reaction as children or adolescents,” they wrote.
The large sample size, prospective design, and confirmation of SCC cases by histology are among the strengths of the study, while a key limitation of the study was the homogeneous nature of the study population, which “may limit the generalizability of our findings,” the authors wrote.
The study was funded by the National Institutes of Health and Inje University (South Korea). One author reported serving as a consultant for AbbVie, Amgen, the Centers for Disease Control and Prevention, Janssen, Merck, Novartis, and Pfizer; and as a compensated investigator for Amgen, Regeneron, and Sanofi. Dr. Kim and the remaining three authors reported no disclosures.
SOURCE: Kim J et al. JAMA Dermatol. 2019 Jul 31. doi: 10.1001/jamadermatol.2019.1937.
FROM JAMA DERMATOLOGY
Standard chemotherapy remains superior in early breast cancer
Standard adjuvant chemotherapy remained superior to capecitabine in older patients with early breast cancer, according to long-term follow-up results from a randomized study.
“We previously reported the primary analysis after a median follow-up of 2.4 years,” wrote Hyman B. Muss, MD, of the University of North Carolina, Chapel Hill, and his colleagues in Journal of Clinical Oncology.
“We now assess the risks and benefits of treatment after a median follow-up time of 11.4 years,” they said.
The Cancer and Leukemia Group B 49907 trial included 633 women aged 65 years and over with early breast cancer. Study patients were randomly assigned to receive either standard adjuvant chemotherapy (either cyclophosphamide and doxorubicin, methotrexate and fluorouracil, or cyclophosphamide) or capecitabine.
The study was designed to evaluate noninferiority of capecitabine versus standard chemotherapy. The primary outcome measured was recurrence-free survival (RFS); overall survival (OS) was included as a secondary endpoint.
After analysis, the researchers reported that the 10-year RFS rates were 56% with standard chemotherapy versus 50% with capecitabine (hazard ratio, 0.80; P = .03).
In addition, the breast cancer–specific survival rates were 88% and 82% in patients treated with standard chemotherapy, compared with capecitabine, respectively (hazard ratio, 0.62; P = .03). OS rates were 62% and 56% in the same groups (HR, 0.84; P = .16).
“With longer follow-up, RFS remains superior for standard adjuvant chemotherapy versus capecitabine, especially in patients with hormone receptor–negative disease,” Dr. Muss and his colleagues wrote.
The researchers acknowledged that the presence of comorbidities in this older population may diminish overall survival benefits.
“Optimally, we must increase the number of older patients in cancer clinical trials to have accurate data on outcomes, especially toxicity, for newer agents,” they concluded.
The study was funded by the National Cancer Institute of the National Institutes of Health. The authors reported financial affiliations with Boehringer Ingelheim, Celgene, Genentech, Novartis, Puma Biotechnology, Pfizer, Sanofi, Seattle Genetics, and several others.
SOURCE: Muss HB et al. J Clin Oncol. 2019 Jul 24. doi: 10.1200/JCO.19.00647.
Standard adjuvant chemotherapy remained superior to capecitabine in older patients with early breast cancer, according to long-term follow-up results from a randomized study.
“We previously reported the primary analysis after a median follow-up of 2.4 years,” wrote Hyman B. Muss, MD, of the University of North Carolina, Chapel Hill, and his colleagues in Journal of Clinical Oncology.
“We now assess the risks and benefits of treatment after a median follow-up time of 11.4 years,” they said.
The Cancer and Leukemia Group B 49907 trial included 633 women aged 65 years and over with early breast cancer. Study patients were randomly assigned to receive either standard adjuvant chemotherapy (either cyclophosphamide and doxorubicin, methotrexate and fluorouracil, or cyclophosphamide) or capecitabine.
The study was designed to evaluate noninferiority of capecitabine versus standard chemotherapy. The primary outcome measured was recurrence-free survival (RFS); overall survival (OS) was included as a secondary endpoint.
After analysis, the researchers reported that the 10-year RFS rates were 56% with standard chemotherapy versus 50% with capecitabine (hazard ratio, 0.80; P = .03).
In addition, the breast cancer–specific survival rates were 88% and 82% in patients treated with standard chemotherapy, compared with capecitabine, respectively (hazard ratio, 0.62; P = .03). OS rates were 62% and 56% in the same groups (HR, 0.84; P = .16).
“With longer follow-up, RFS remains superior for standard adjuvant chemotherapy versus capecitabine, especially in patients with hormone receptor–negative disease,” Dr. Muss and his colleagues wrote.
The researchers acknowledged that the presence of comorbidities in this older population may diminish overall survival benefits.
“Optimally, we must increase the number of older patients in cancer clinical trials to have accurate data on outcomes, especially toxicity, for newer agents,” they concluded.
The study was funded by the National Cancer Institute of the National Institutes of Health. The authors reported financial affiliations with Boehringer Ingelheim, Celgene, Genentech, Novartis, Puma Biotechnology, Pfizer, Sanofi, Seattle Genetics, and several others.
SOURCE: Muss HB et al. J Clin Oncol. 2019 Jul 24. doi: 10.1200/JCO.19.00647.
Standard adjuvant chemotherapy remained superior to capecitabine in older patients with early breast cancer, according to long-term follow-up results from a randomized study.
“We previously reported the primary analysis after a median follow-up of 2.4 years,” wrote Hyman B. Muss, MD, of the University of North Carolina, Chapel Hill, and his colleagues in Journal of Clinical Oncology.
“We now assess the risks and benefits of treatment after a median follow-up time of 11.4 years,” they said.
The Cancer and Leukemia Group B 49907 trial included 633 women aged 65 years and over with early breast cancer. Study patients were randomly assigned to receive either standard adjuvant chemotherapy (either cyclophosphamide and doxorubicin, methotrexate and fluorouracil, or cyclophosphamide) or capecitabine.
The study was designed to evaluate noninferiority of capecitabine versus standard chemotherapy. The primary outcome measured was recurrence-free survival (RFS); overall survival (OS) was included as a secondary endpoint.
After analysis, the researchers reported that the 10-year RFS rates were 56% with standard chemotherapy versus 50% with capecitabine (hazard ratio, 0.80; P = .03).
In addition, the breast cancer–specific survival rates were 88% and 82% in patients treated with standard chemotherapy, compared with capecitabine, respectively (hazard ratio, 0.62; P = .03). OS rates were 62% and 56% in the same groups (HR, 0.84; P = .16).
“With longer follow-up, RFS remains superior for standard adjuvant chemotherapy versus capecitabine, especially in patients with hormone receptor–negative disease,” Dr. Muss and his colleagues wrote.
The researchers acknowledged that the presence of comorbidities in this older population may diminish overall survival benefits.
“Optimally, we must increase the number of older patients in cancer clinical trials to have accurate data on outcomes, especially toxicity, for newer agents,” they concluded.
The study was funded by the National Cancer Institute of the National Institutes of Health. The authors reported financial affiliations with Boehringer Ingelheim, Celgene, Genentech, Novartis, Puma Biotechnology, Pfizer, Sanofi, Seattle Genetics, and several others.
SOURCE: Muss HB et al. J Clin Oncol. 2019 Jul 24. doi: 10.1200/JCO.19.00647.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Administrative data may reduce costs of economic analysis
The use of administrative data may improve the accuracy and reduce costs of oncology clinical trial economic analyses, according to a retrospective study.
“We investigated whether administrative data could improve the performance of cancer trial economic analysis,” Timothy P. Hanna, MD, MSc, PhD, of Queen’s University in Kingston, Ont., and colleagues wrote in the Journal of Oncology Practice.
The researchers linked clinical trial and health administrative data to evaluate the utility of administrative data in a group of 572 patients with previously treated metastatic colorectal cancer.
The phase 3 trial assessed cetuximab plus best supportive care versus best supportive care alone in these patients. The trial data set was used to obtain information related to resource utilization, such as hospitalization or treatment costs, in addition to clinical reports, such as vital status.
Several measures were estimated by the team, including the incremental cost-effectiveness ratio (ICER) and total costs.
After analysis, the researchers found that ICER measures were comparable with the use of administrative data versus trial data alone ($164,378 vs. $211,128 per QALY added up to last contact).
“Up to trial date of last contact, vital status was in agreement for more than 96% of patients,” Dr. Hanna and colleagues reported.
These findings highlight the potential utility of administrative data in reducing the costs of collecting applicable data from clinical trials alone.
“A harmonized approach has the potential to provide more complete information on clinical trial participants at reduced cost,” they concluded.
The study was funded by the Institute for Clinical Evaluative Sciences and Queen’s University. The authors reported financial affiliations with Amgen, Janssen, Novartis, and UpToDate.
SOURCE: Hanna TP et al. J Oncol Pract. 2019 Jul 15. doi: 10.1200/JOP.18.00691.
The use of administrative data may improve the accuracy and reduce costs of oncology clinical trial economic analyses, according to a retrospective study.
“We investigated whether administrative data could improve the performance of cancer trial economic analysis,” Timothy P. Hanna, MD, MSc, PhD, of Queen’s University in Kingston, Ont., and colleagues wrote in the Journal of Oncology Practice.
The researchers linked clinical trial and health administrative data to evaluate the utility of administrative data in a group of 572 patients with previously treated metastatic colorectal cancer.
The phase 3 trial assessed cetuximab plus best supportive care versus best supportive care alone in these patients. The trial data set was used to obtain information related to resource utilization, such as hospitalization or treatment costs, in addition to clinical reports, such as vital status.
Several measures were estimated by the team, including the incremental cost-effectiveness ratio (ICER) and total costs.
After analysis, the researchers found that ICER measures were comparable with the use of administrative data versus trial data alone ($164,378 vs. $211,128 per QALY added up to last contact).
“Up to trial date of last contact, vital status was in agreement for more than 96% of patients,” Dr. Hanna and colleagues reported.
These findings highlight the potential utility of administrative data in reducing the costs of collecting applicable data from clinical trials alone.
“A harmonized approach has the potential to provide more complete information on clinical trial participants at reduced cost,” they concluded.
The study was funded by the Institute for Clinical Evaluative Sciences and Queen’s University. The authors reported financial affiliations with Amgen, Janssen, Novartis, and UpToDate.
SOURCE: Hanna TP et al. J Oncol Pract. 2019 Jul 15. doi: 10.1200/JOP.18.00691.
The use of administrative data may improve the accuracy and reduce costs of oncology clinical trial economic analyses, according to a retrospective study.
“We investigated whether administrative data could improve the performance of cancer trial economic analysis,” Timothy P. Hanna, MD, MSc, PhD, of Queen’s University in Kingston, Ont., and colleagues wrote in the Journal of Oncology Practice.
The researchers linked clinical trial and health administrative data to evaluate the utility of administrative data in a group of 572 patients with previously treated metastatic colorectal cancer.
The phase 3 trial assessed cetuximab plus best supportive care versus best supportive care alone in these patients. The trial data set was used to obtain information related to resource utilization, such as hospitalization or treatment costs, in addition to clinical reports, such as vital status.
Several measures were estimated by the team, including the incremental cost-effectiveness ratio (ICER) and total costs.
After analysis, the researchers found that ICER measures were comparable with the use of administrative data versus trial data alone ($164,378 vs. $211,128 per QALY added up to last contact).
“Up to trial date of last contact, vital status was in agreement for more than 96% of patients,” Dr. Hanna and colleagues reported.
These findings highlight the potential utility of administrative data in reducing the costs of collecting applicable data from clinical trials alone.
“A harmonized approach has the potential to provide more complete information on clinical trial participants at reduced cost,” they concluded.
The study was funded by the Institute for Clinical Evaluative Sciences and Queen’s University. The authors reported financial affiliations with Amgen, Janssen, Novartis, and UpToDate.
SOURCE: Hanna TP et al. J Oncol Pract. 2019 Jul 15. doi: 10.1200/JOP.18.00691.
FROM JOURNAL OF ONCOLOGY PRACTICE
Flavopiridol elicits poor response in mantle cell lymphoma, DLBCL
Flavopiridol – also known as alvocidib – showed minimal clinical response in patients with relapsed or refractory mantle cell lymphoma (MCL), diffuse large B-cell lymphoma (DLBCL), and other B-cell lymphomas, according to results from a single-center, phase 1/2 trial.
“Promising preclinical data in cell lines derived from MCL and activated DLBCL led to a series of clinical trials of flavopiridol in various hematological malignancies,” wrote Milos D. Miljković, MD, and colleagues in the lymphoid malignancies branch of the National Cancer Institute in Bethesda, Md. The findings were published in a letter to the editor in Leukemia & Lymphoma.
The study included 28 patients with relapsed/refractory MCL, DLBCL, transformed follicular lymphoma, and primary mediastinal B-cell lymphoma who received a hybrid dosing regimen of the novel CDK inhibitor. Flavopiridol was administered as a 30-minute bolus, followed by a 4-hour infusion.
The researchers used an intrapatient dose escalation between the first and successive cycles, in addition to a three-plus-three interpatient escalation, to lessen the risk of tumor lysis syndrome (TLS).
The primary outcomes were the clinical response rate, maximum tolerated dose, dose-limiting toxicities, and toxicity profile of the hybrid dosing regimen.
Of 26 evaluable patients, one patient with DLBCL maintained a partial response for 84 days (overall response rate, 3.8%). One patient with MCL had a 50% decrease in the size of target lesions at 2 months, but this was not sustained at 4 months. In total, nine patients had stable disease for a disease control rate of 38.4%.
“[Flavopiridol] had minimal efficacy in patients with relapsed/refractory non-Hodgkin B-cell lymphoma, casting doubt on the utility of CDK inhibition in this disease,” the researchers wrote.
With respect to safety, there were eight dose-limiting toxicities reported in three patients. These included grade 3 TLS, elevated transaminase levels, hypoalbuminemia, hyperkalemia, non-neutropenic infection, and grade 4 metabolic acidosis and gastrointestinal perforation.
The most common treatment-related toxicities were hematologic, including neutropenia, anemia, thrombocytopenia, leukocytosis, and lymphopenia.
Dr. Miljković and colleagues noted that CDK inhibitor therapy may elicit better responses when used in combination with other agents.
“Ongoing trials of more specific CDK inhibitors in combination with other agents will help elucidate their role in lymphoma treatment,” they wrote.
The trial is sponsored by the National Cancer Institute and the study authors are employees of the National Cancer Institute.
SOURCE: Miljkovic MD et al. Leuk Lymphoma. 2019 Jun 17. doi: 10.1080/10428194.2019.1627540.
Flavopiridol – also known as alvocidib – showed minimal clinical response in patients with relapsed or refractory mantle cell lymphoma (MCL), diffuse large B-cell lymphoma (DLBCL), and other B-cell lymphomas, according to results from a single-center, phase 1/2 trial.
“Promising preclinical data in cell lines derived from MCL and activated DLBCL led to a series of clinical trials of flavopiridol in various hematological malignancies,” wrote Milos D. Miljković, MD, and colleagues in the lymphoid malignancies branch of the National Cancer Institute in Bethesda, Md. The findings were published in a letter to the editor in Leukemia & Lymphoma.
The study included 28 patients with relapsed/refractory MCL, DLBCL, transformed follicular lymphoma, and primary mediastinal B-cell lymphoma who received a hybrid dosing regimen of the novel CDK inhibitor. Flavopiridol was administered as a 30-minute bolus, followed by a 4-hour infusion.
The researchers used an intrapatient dose escalation between the first and successive cycles, in addition to a three-plus-three interpatient escalation, to lessen the risk of tumor lysis syndrome (TLS).
The primary outcomes were the clinical response rate, maximum tolerated dose, dose-limiting toxicities, and toxicity profile of the hybrid dosing regimen.
Of 26 evaluable patients, one patient with DLBCL maintained a partial response for 84 days (overall response rate, 3.8%). One patient with MCL had a 50% decrease in the size of target lesions at 2 months, but this was not sustained at 4 months. In total, nine patients had stable disease for a disease control rate of 38.4%.
“[Flavopiridol] had minimal efficacy in patients with relapsed/refractory non-Hodgkin B-cell lymphoma, casting doubt on the utility of CDK inhibition in this disease,” the researchers wrote.
With respect to safety, there were eight dose-limiting toxicities reported in three patients. These included grade 3 TLS, elevated transaminase levels, hypoalbuminemia, hyperkalemia, non-neutropenic infection, and grade 4 metabolic acidosis and gastrointestinal perforation.
The most common treatment-related toxicities were hematologic, including neutropenia, anemia, thrombocytopenia, leukocytosis, and lymphopenia.
Dr. Miljković and colleagues noted that CDK inhibitor therapy may elicit better responses when used in combination with other agents.
“Ongoing trials of more specific CDK inhibitors in combination with other agents will help elucidate their role in lymphoma treatment,” they wrote.
The trial is sponsored by the National Cancer Institute and the study authors are employees of the National Cancer Institute.
SOURCE: Miljkovic MD et al. Leuk Lymphoma. 2019 Jun 17. doi: 10.1080/10428194.2019.1627540.
Flavopiridol – also known as alvocidib – showed minimal clinical response in patients with relapsed or refractory mantle cell lymphoma (MCL), diffuse large B-cell lymphoma (DLBCL), and other B-cell lymphomas, according to results from a single-center, phase 1/2 trial.
“Promising preclinical data in cell lines derived from MCL and activated DLBCL led to a series of clinical trials of flavopiridol in various hematological malignancies,” wrote Milos D. Miljković, MD, and colleagues in the lymphoid malignancies branch of the National Cancer Institute in Bethesda, Md. The findings were published in a letter to the editor in Leukemia & Lymphoma.
The study included 28 patients with relapsed/refractory MCL, DLBCL, transformed follicular lymphoma, and primary mediastinal B-cell lymphoma who received a hybrid dosing regimen of the novel CDK inhibitor. Flavopiridol was administered as a 30-minute bolus, followed by a 4-hour infusion.
The researchers used an intrapatient dose escalation between the first and successive cycles, in addition to a three-plus-three interpatient escalation, to lessen the risk of tumor lysis syndrome (TLS).
The primary outcomes were the clinical response rate, maximum tolerated dose, dose-limiting toxicities, and toxicity profile of the hybrid dosing regimen.
Of 26 evaluable patients, one patient with DLBCL maintained a partial response for 84 days (overall response rate, 3.8%). One patient with MCL had a 50% decrease in the size of target lesions at 2 months, but this was not sustained at 4 months. In total, nine patients had stable disease for a disease control rate of 38.4%.
“[Flavopiridol] had minimal efficacy in patients with relapsed/refractory non-Hodgkin B-cell lymphoma, casting doubt on the utility of CDK inhibition in this disease,” the researchers wrote.
With respect to safety, there were eight dose-limiting toxicities reported in three patients. These included grade 3 TLS, elevated transaminase levels, hypoalbuminemia, hyperkalemia, non-neutropenic infection, and grade 4 metabolic acidosis and gastrointestinal perforation.
The most common treatment-related toxicities were hematologic, including neutropenia, anemia, thrombocytopenia, leukocytosis, and lymphopenia.
Dr. Miljković and colleagues noted that CDK inhibitor therapy may elicit better responses when used in combination with other agents.
“Ongoing trials of more specific CDK inhibitors in combination with other agents will help elucidate their role in lymphoma treatment,” they wrote.
The trial is sponsored by the National Cancer Institute and the study authors are employees of the National Cancer Institute.
SOURCE: Miljkovic MD et al. Leuk Lymphoma. 2019 Jun 17. doi: 10.1080/10428194.2019.1627540.
FROM LEUKEMIA & LYMPHOMA
How to recognize pediatric leukemia cutis
Researchers have characterized the clinical presentation, progression, and prognosis of leukemia cutis in a pediatric population, according to findings from a retrospective case series.
“To our knowledge, this is the largest reported case series of pediatric leukemia cutis,” wrote Elena Corina Andriescu of the University of Texas, Houston, and colleagues. The results were published in Pediatric Dermatology.
The study included 31 children with histologically confirmed leukemia cutis at one of two pediatric institutions. The researchers reviewed medical records to distinguish common features among patients.
Various clinical data, including disease subtype, related symptoms, management, and prognosis, were collected from January 1993 to March 2014. The children in the case series ranged in age up to 19 years with a median age at diagnosis of 26.8 months.
After analysis, the researchers reported that the magnitude and morphology of disease lesions differed among pediatric patients, with the most common sites being the lower extremities and head. The most common morphologies were nodules and papules. Additionally, the researchers found that lesions were often erythematous, violaceous, or both colors.
The majority of patients (65%) presented with concomitant systemic leukemia and leukemia cutis. The most common types of leukemia associated with the skin condition were acute myeloid leukemia (in 74% of cases) and acute lymphoblastic leukemia (in 16% of cases). The researchers saw no significant differences in leukemia cutis morphology or distribution based on the leukemia diagnosis.
“Most cases of leukemia cutis arose during initial leukemia episodes, rather than with relapsed leukemia,” they added.
Because of an insufficiency of specific genetic data, investigators were unable to make prognostic inferences in the majority of participants.
Two key limitations of the study were the small sample size and retrospective design. As a result, the investigators were unable to prospectively classify skin findings in a systematic manner. Despite these limitations, the authors noted that these findings add to the present knowledge of leukemia cutis in pediatric patients.
“Importantly, the presence of [leukemia cutis] changed the management of systemic leukemia in one‐third of patients,” the researchers wrote. “The potential for major changes in treatment plans such as adding radiation therapy and deferring hematopoietic stem cell transplantation underscores the importance of diagnosing [leukemia cutis].”
No funding sources were reported. The authors did not report conflicts of interest.
SOURCE: Andriescu EC et al. Pediatr Dermatol. 2019 Jul 5. doi: 10.1111/pde.13864.
Researchers have characterized the clinical presentation, progression, and prognosis of leukemia cutis in a pediatric population, according to findings from a retrospective case series.
“To our knowledge, this is the largest reported case series of pediatric leukemia cutis,” wrote Elena Corina Andriescu of the University of Texas, Houston, and colleagues. The results were published in Pediatric Dermatology.
The study included 31 children with histologically confirmed leukemia cutis at one of two pediatric institutions. The researchers reviewed medical records to distinguish common features among patients.
Various clinical data, including disease subtype, related symptoms, management, and prognosis, were collected from January 1993 to March 2014. The children in the case series ranged in age up to 19 years with a median age at diagnosis of 26.8 months.
After analysis, the researchers reported that the magnitude and morphology of disease lesions differed among pediatric patients, with the most common sites being the lower extremities and head. The most common morphologies were nodules and papules. Additionally, the researchers found that lesions were often erythematous, violaceous, or both colors.
The majority of patients (65%) presented with concomitant systemic leukemia and leukemia cutis. The most common types of leukemia associated with the skin condition were acute myeloid leukemia (in 74% of cases) and acute lymphoblastic leukemia (in 16% of cases). The researchers saw no significant differences in leukemia cutis morphology or distribution based on the leukemia diagnosis.
“Most cases of leukemia cutis arose during initial leukemia episodes, rather than with relapsed leukemia,” they added.
Because of an insufficiency of specific genetic data, investigators were unable to make prognostic inferences in the majority of participants.
Two key limitations of the study were the small sample size and retrospective design. As a result, the investigators were unable to prospectively classify skin findings in a systematic manner. Despite these limitations, the authors noted that these findings add to the present knowledge of leukemia cutis in pediatric patients.
“Importantly, the presence of [leukemia cutis] changed the management of systemic leukemia in one‐third of patients,” the researchers wrote. “The potential for major changes in treatment plans such as adding radiation therapy and deferring hematopoietic stem cell transplantation underscores the importance of diagnosing [leukemia cutis].”
No funding sources were reported. The authors did not report conflicts of interest.
SOURCE: Andriescu EC et al. Pediatr Dermatol. 2019 Jul 5. doi: 10.1111/pde.13864.
Researchers have characterized the clinical presentation, progression, and prognosis of leukemia cutis in a pediatric population, according to findings from a retrospective case series.
“To our knowledge, this is the largest reported case series of pediatric leukemia cutis,” wrote Elena Corina Andriescu of the University of Texas, Houston, and colleagues. The results were published in Pediatric Dermatology.
The study included 31 children with histologically confirmed leukemia cutis at one of two pediatric institutions. The researchers reviewed medical records to distinguish common features among patients.
Various clinical data, including disease subtype, related symptoms, management, and prognosis, were collected from January 1993 to March 2014. The children in the case series ranged in age up to 19 years with a median age at diagnosis of 26.8 months.
After analysis, the researchers reported that the magnitude and morphology of disease lesions differed among pediatric patients, with the most common sites being the lower extremities and head. The most common morphologies were nodules and papules. Additionally, the researchers found that lesions were often erythematous, violaceous, or both colors.
The majority of patients (65%) presented with concomitant systemic leukemia and leukemia cutis. The most common types of leukemia associated with the skin condition were acute myeloid leukemia (in 74% of cases) and acute lymphoblastic leukemia (in 16% of cases). The researchers saw no significant differences in leukemia cutis morphology or distribution based on the leukemia diagnosis.
“Most cases of leukemia cutis arose during initial leukemia episodes, rather than with relapsed leukemia,” they added.
Because of an insufficiency of specific genetic data, investigators were unable to make prognostic inferences in the majority of participants.
Two key limitations of the study were the small sample size and retrospective design. As a result, the investigators were unable to prospectively classify skin findings in a systematic manner. Despite these limitations, the authors noted that these findings add to the present knowledge of leukemia cutis in pediatric patients.
“Importantly, the presence of [leukemia cutis] changed the management of systemic leukemia in one‐third of patients,” the researchers wrote. “The potential for major changes in treatment plans such as adding radiation therapy and deferring hematopoietic stem cell transplantation underscores the importance of diagnosing [leukemia cutis].”
No funding sources were reported. The authors did not report conflicts of interest.
SOURCE: Andriescu EC et al. Pediatr Dermatol. 2019 Jul 5. doi: 10.1111/pde.13864.
FROM PEDIATRIC DERMATOLOGY
Combo RT/pembro may show synergy in NSCLC
Combination radiotherapy and pembrolizumab may improve clinical outcomes by means of synergy in the treatment of patients with non–small cell lung cancer (NSCLC), according to results from two recent studies.
“The best way to combine immunotherapy with ablative therapies in the curative setting is an area of active investigation,” wrote Joshua M. Bauml, MD, of the University of Pennsylvania, Philadelphia, and colleagues.
Dr. Bauml and colleagues recently reported the results of a phase 2 study exploring the addition of pembrolizumab following the completion of locally ablative therapy in patients with oligometastatic NSCLC in JAMA Oncology.
The single-arm trial included 51 patients who received intravenous pembrolizumab (200 mg every 21 days) for a total of 8 cycles within 4-12 weeks of local ablative therapy completion. Study participants were administered locally ablative therapy to all recognized sites of malignancy.
The researchers measured two primary efficacy outcomes: progression-free survival (PFS) from the initiation of ablative therapy and the PFS from initiation of pembrolizumab. Secondary endpoints were safety, quality of life, and overall survival (OS).
Among patients who received pembrolizumab after ablative therapy, the median PFS was 19.1 months (95% CI, 9.4-28.7 months), which was significantly longer than the historical outcome (median PFS, 6.6 months; P = .005). In addition, the 24-month OS was 77.5%. With respect to safety, no decrease in quality of life or new safety signals were reported in the study.
One key limitation of the study was the single-arm design. As a result, distinguishing the effects of pembrolizumab over ablative therapy alone is not possible with the present data.
“This study is the first to show improved outcomes for immunotherapy after locally ablative therapy in patients with oligometastatic NSCLC,” Dr. Bauml and his colleagues wrote.
In another phase 2 trial (PEMBRO-RT study) reported in the same issue, Willemijn S.M.E. Theelen, MD, of the Netherlands Cancer Institute in Amsterdam and colleagues examined the use of pembrolizumab after stereotactic body radiotherapy or pembrolizumab alone in patients with recurrent metastatic NSCLC.
“This study evaluates whether stereotactic body radiotherapy enhances the effect of immune checkpoint blockade,” wrote Dr. Theelen and colleagues.
The PEMBRO-RT study included 76 patients with recurrent metastatic NSCLC who were randomized to pembrolizumab following radiotherapy or pembrolizumab alone. Intravenous pembrolizumab was administered at 200 mg/kg every 3 weeks, with the first dose given within 7 days after completion of radiotherapy.
The primary outcome was the overall response rate (ORR) at 12 weeks. Secondary outcomes included OS, PFS, and safety.
Among patients who received pembrolizumab after radiotherapy versus pembrolizumab alone, the ORR at 12 weeks was 36% and 18%, respectively (P = .07). In addition, the median PFS and OS were not statistically significant (P = .19 and P = .16, respectively).
“Positive results were largely influenced by the PD-L1–negative subgroup, which had significantly improved progression-free survival and overall survival,” the researchers wrote.
With respect to safety, no differences in grade 3-5 adverse effects were observed between the treatment groups. In addition, no significant differences were seen in pulmonary toxicities.
One key limitation of the study was the lack of information regarding optimal radiotherapy dosing and schedule.
“The results of this study are encouraging, and further evaluation in a larger phase 2/3 trial is recommended,” Dr. Theelen and colleagues wrote.
Further studies are needed to fully understand the links between combination radiotherapy and pembrolizumab in patients with NSCLC.
The study by Dr. Bauml and colleagues was funded by the Abramson Cancer Center and Merck & Co. The authors reported financial affiliations with Amgen, AstraZeneca, Bristol-Myers Squibb, Celgene, Janssen, Takeda, and several others.
The study by Dr. Theelen and colleagues was funded by Merck Sharp & Dohme. The authors reported financial affiliations with AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Merck Sharp & Dohme, Roche, Takeda, and several others.
SOURCE: Bauml JM et al. JAMA Oncol. 2019 Jul 11. doi: 10.1001/jamaoncol.2019.1449. Theelen WSME et al. JAMA Oncol. 2019 Jul 11. doi: 10.1001/jamaoncol.2019.1478.
Over the last 20 years, significant advances have been made in the development of ablative radiotherapy and immunotherapy, particularly in the oncology setting. More recently, combination radiation therapy (RT) and immuno-oncology (IO) approaches have emerged, and the body of evidence for this novel treatment strategy continues to grow.
Recent studies have suggested that combined RT/IO therapy may confer survival benefit for patients with non–small cell lung cancer (NSCLC). Limitations of these studies include design, which have been largely case reports and single-center studies. The recent findings reported by Bauml et al. and Theelen et al. provide insight into the combined use of immune checkpoint blockade and radiotherapy in patients with NSCLC.
While the study by Dr. Theelen and colleagues did not reach its prespecified endpoint, the findings showed promise in some patient subpopulations. Dr. Bauml and colleagues reported favorable survival outcomes in their study, notably progression-free survival, following radical local therapy, when compared with historical outcomes. Intriguingly, the combination approach in both studies was well tolerated, with little to no grade 3-5 toxicities reported.
Taken together, these data constitute early evidence indicative of possible synergy between both therapies. In response, well-designed phase 3 studies are warranted to further explore these effects.
Joshua Walker, MD, PhD, is affiliated with Oregon Health & Science University in Portland. Billy W. Loo Jr., MD, PhD, is with Stanford (Calif.) University. Dr. Walker reported no conflicts of interest. Dr. Loo reported receiving research support from Varian Medical Systems and is a board member of TibaRay. These comments are adapted from their editorial (JAMA Oncol. 2019 Jul 11. doi: 10.1001/jamaoncol.2019.1448 ).
Over the last 20 years, significant advances have been made in the development of ablative radiotherapy and immunotherapy, particularly in the oncology setting. More recently, combination radiation therapy (RT) and immuno-oncology (IO) approaches have emerged, and the body of evidence for this novel treatment strategy continues to grow.
Recent studies have suggested that combined RT/IO therapy may confer survival benefit for patients with non–small cell lung cancer (NSCLC). Limitations of these studies include design, which have been largely case reports and single-center studies. The recent findings reported by Bauml et al. and Theelen et al. provide insight into the combined use of immune checkpoint blockade and radiotherapy in patients with NSCLC.
While the study by Dr. Theelen and colleagues did not reach its prespecified endpoint, the findings showed promise in some patient subpopulations. Dr. Bauml and colleagues reported favorable survival outcomes in their study, notably progression-free survival, following radical local therapy, when compared with historical outcomes. Intriguingly, the combination approach in both studies was well tolerated, with little to no grade 3-5 toxicities reported.
Taken together, these data constitute early evidence indicative of possible synergy between both therapies. In response, well-designed phase 3 studies are warranted to further explore these effects.
Joshua Walker, MD, PhD, is affiliated with Oregon Health & Science University in Portland. Billy W. Loo Jr., MD, PhD, is with Stanford (Calif.) University. Dr. Walker reported no conflicts of interest. Dr. Loo reported receiving research support from Varian Medical Systems and is a board member of TibaRay. These comments are adapted from their editorial (JAMA Oncol. 2019 Jul 11. doi: 10.1001/jamaoncol.2019.1448 ).
Over the last 20 years, significant advances have been made in the development of ablative radiotherapy and immunotherapy, particularly in the oncology setting. More recently, combination radiation therapy (RT) and immuno-oncology (IO) approaches have emerged, and the body of evidence for this novel treatment strategy continues to grow.
Recent studies have suggested that combined RT/IO therapy may confer survival benefit for patients with non–small cell lung cancer (NSCLC). Limitations of these studies include design, which have been largely case reports and single-center studies. The recent findings reported by Bauml et al. and Theelen et al. provide insight into the combined use of immune checkpoint blockade and radiotherapy in patients with NSCLC.
While the study by Dr. Theelen and colleagues did not reach its prespecified endpoint, the findings showed promise in some patient subpopulations. Dr. Bauml and colleagues reported favorable survival outcomes in their study, notably progression-free survival, following radical local therapy, when compared with historical outcomes. Intriguingly, the combination approach in both studies was well tolerated, with little to no grade 3-5 toxicities reported.
Taken together, these data constitute early evidence indicative of possible synergy between both therapies. In response, well-designed phase 3 studies are warranted to further explore these effects.
Joshua Walker, MD, PhD, is affiliated with Oregon Health & Science University in Portland. Billy W. Loo Jr., MD, PhD, is with Stanford (Calif.) University. Dr. Walker reported no conflicts of interest. Dr. Loo reported receiving research support from Varian Medical Systems and is a board member of TibaRay. These comments are adapted from their editorial (JAMA Oncol. 2019 Jul 11. doi: 10.1001/jamaoncol.2019.1448 ).
Combination radiotherapy and pembrolizumab may improve clinical outcomes by means of synergy in the treatment of patients with non–small cell lung cancer (NSCLC), according to results from two recent studies.
“The best way to combine immunotherapy with ablative therapies in the curative setting is an area of active investigation,” wrote Joshua M. Bauml, MD, of the University of Pennsylvania, Philadelphia, and colleagues.
Dr. Bauml and colleagues recently reported the results of a phase 2 study exploring the addition of pembrolizumab following the completion of locally ablative therapy in patients with oligometastatic NSCLC in JAMA Oncology.
The single-arm trial included 51 patients who received intravenous pembrolizumab (200 mg every 21 days) for a total of 8 cycles within 4-12 weeks of local ablative therapy completion. Study participants were administered locally ablative therapy to all recognized sites of malignancy.
The researchers measured two primary efficacy outcomes: progression-free survival (PFS) from the initiation of ablative therapy and the PFS from initiation of pembrolizumab. Secondary endpoints were safety, quality of life, and overall survival (OS).
Among patients who received pembrolizumab after ablative therapy, the median PFS was 19.1 months (95% CI, 9.4-28.7 months), which was significantly longer than the historical outcome (median PFS, 6.6 months; P = .005). In addition, the 24-month OS was 77.5%. With respect to safety, no decrease in quality of life or new safety signals were reported in the study.
One key limitation of the study was the single-arm design. As a result, distinguishing the effects of pembrolizumab over ablative therapy alone is not possible with the present data.
“This study is the first to show improved outcomes for immunotherapy after locally ablative therapy in patients with oligometastatic NSCLC,” Dr. Bauml and his colleagues wrote.
In another phase 2 trial (PEMBRO-RT study) reported in the same issue, Willemijn S.M.E. Theelen, MD, of the Netherlands Cancer Institute in Amsterdam and colleagues examined the use of pembrolizumab after stereotactic body radiotherapy or pembrolizumab alone in patients with recurrent metastatic NSCLC.
“This study evaluates whether stereotactic body radiotherapy enhances the effect of immune checkpoint blockade,” wrote Dr. Theelen and colleagues.
The PEMBRO-RT study included 76 patients with recurrent metastatic NSCLC who were randomized to pembrolizumab following radiotherapy or pembrolizumab alone. Intravenous pembrolizumab was administered at 200 mg/kg every 3 weeks, with the first dose given within 7 days after completion of radiotherapy.
The primary outcome was the overall response rate (ORR) at 12 weeks. Secondary outcomes included OS, PFS, and safety.
Among patients who received pembrolizumab after radiotherapy versus pembrolizumab alone, the ORR at 12 weeks was 36% and 18%, respectively (P = .07). In addition, the median PFS and OS were not statistically significant (P = .19 and P = .16, respectively).
“Positive results were largely influenced by the PD-L1–negative subgroup, which had significantly improved progression-free survival and overall survival,” the researchers wrote.
With respect to safety, no differences in grade 3-5 adverse effects were observed between the treatment groups. In addition, no significant differences were seen in pulmonary toxicities.
One key limitation of the study was the lack of information regarding optimal radiotherapy dosing and schedule.
“The results of this study are encouraging, and further evaluation in a larger phase 2/3 trial is recommended,” Dr. Theelen and colleagues wrote.
Further studies are needed to fully understand the links between combination radiotherapy and pembrolizumab in patients with NSCLC.
The study by Dr. Bauml and colleagues was funded by the Abramson Cancer Center and Merck & Co. The authors reported financial affiliations with Amgen, AstraZeneca, Bristol-Myers Squibb, Celgene, Janssen, Takeda, and several others.
The study by Dr. Theelen and colleagues was funded by Merck Sharp & Dohme. The authors reported financial affiliations with AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Merck Sharp & Dohme, Roche, Takeda, and several others.
SOURCE: Bauml JM et al. JAMA Oncol. 2019 Jul 11. doi: 10.1001/jamaoncol.2019.1449. Theelen WSME et al. JAMA Oncol. 2019 Jul 11. doi: 10.1001/jamaoncol.2019.1478.
Combination radiotherapy and pembrolizumab may improve clinical outcomes by means of synergy in the treatment of patients with non–small cell lung cancer (NSCLC), according to results from two recent studies.
“The best way to combine immunotherapy with ablative therapies in the curative setting is an area of active investigation,” wrote Joshua M. Bauml, MD, of the University of Pennsylvania, Philadelphia, and colleagues.
Dr. Bauml and colleagues recently reported the results of a phase 2 study exploring the addition of pembrolizumab following the completion of locally ablative therapy in patients with oligometastatic NSCLC in JAMA Oncology.
The single-arm trial included 51 patients who received intravenous pembrolizumab (200 mg every 21 days) for a total of 8 cycles within 4-12 weeks of local ablative therapy completion. Study participants were administered locally ablative therapy to all recognized sites of malignancy.
The researchers measured two primary efficacy outcomes: progression-free survival (PFS) from the initiation of ablative therapy and the PFS from initiation of pembrolizumab. Secondary endpoints were safety, quality of life, and overall survival (OS).
Among patients who received pembrolizumab after ablative therapy, the median PFS was 19.1 months (95% CI, 9.4-28.7 months), which was significantly longer than the historical outcome (median PFS, 6.6 months; P = .005). In addition, the 24-month OS was 77.5%. With respect to safety, no decrease in quality of life or new safety signals were reported in the study.
One key limitation of the study was the single-arm design. As a result, distinguishing the effects of pembrolizumab over ablative therapy alone is not possible with the present data.
“This study is the first to show improved outcomes for immunotherapy after locally ablative therapy in patients with oligometastatic NSCLC,” Dr. Bauml and his colleagues wrote.
In another phase 2 trial (PEMBRO-RT study) reported in the same issue, Willemijn S.M.E. Theelen, MD, of the Netherlands Cancer Institute in Amsterdam and colleagues examined the use of pembrolizumab after stereotactic body radiotherapy or pembrolizumab alone in patients with recurrent metastatic NSCLC.
“This study evaluates whether stereotactic body radiotherapy enhances the effect of immune checkpoint blockade,” wrote Dr. Theelen and colleagues.
The PEMBRO-RT study included 76 patients with recurrent metastatic NSCLC who were randomized to pembrolizumab following radiotherapy or pembrolizumab alone. Intravenous pembrolizumab was administered at 200 mg/kg every 3 weeks, with the first dose given within 7 days after completion of radiotherapy.
The primary outcome was the overall response rate (ORR) at 12 weeks. Secondary outcomes included OS, PFS, and safety.
Among patients who received pembrolizumab after radiotherapy versus pembrolizumab alone, the ORR at 12 weeks was 36% and 18%, respectively (P = .07). In addition, the median PFS and OS were not statistically significant (P = .19 and P = .16, respectively).
“Positive results were largely influenced by the PD-L1–negative subgroup, which had significantly improved progression-free survival and overall survival,” the researchers wrote.
With respect to safety, no differences in grade 3-5 adverse effects were observed between the treatment groups. In addition, no significant differences were seen in pulmonary toxicities.
One key limitation of the study was the lack of information regarding optimal radiotherapy dosing and schedule.
“The results of this study are encouraging, and further evaluation in a larger phase 2/3 trial is recommended,” Dr. Theelen and colleagues wrote.
Further studies are needed to fully understand the links between combination radiotherapy and pembrolizumab in patients with NSCLC.
The study by Dr. Bauml and colleagues was funded by the Abramson Cancer Center and Merck & Co. The authors reported financial affiliations with Amgen, AstraZeneca, Bristol-Myers Squibb, Celgene, Janssen, Takeda, and several others.
The study by Dr. Theelen and colleagues was funded by Merck Sharp & Dohme. The authors reported financial affiliations with AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Merck Sharp & Dohme, Roche, Takeda, and several others.
SOURCE: Bauml JM et al. JAMA Oncol. 2019 Jul 11. doi: 10.1001/jamaoncol.2019.1449. Theelen WSME et al. JAMA Oncol. 2019 Jul 11. doi: 10.1001/jamaoncol.2019.1478.
FROM JAMA ONCOLOGY
Vaginal microbiota composition linked to ovarian cancer risk
Women with epithelial ovarian cancer or BRCA1 mutational status were more likely to present with a community type O cervicovaginal microbiota relative to age-matched controls, according to a case-control analysis.
The results suggest that the composition of the cervicovaginal microbiome may have a key role in ovarian carcinogenesis. In addition, dysbiosis could be an important risk factor in women at high risk for the disease.
“Our aim was to establish whether women with, or at risk of developing, ovarian cancer have an imbalanced cervicovaginal microbiome,” wrote Nuno R Nené, PhD, of University College London, and colleagues. Their report is in The Lancet Oncology.
The researchers conducted a case-control study of adult females located in five European countries. Study participants were divided into two sets that consisted of 176 females with ovarian cancer and 109 females with a BRCA1 mutation, but without a diagnosis of ovarian cancer.
The two sets were matched with a combination of healthy controls and others with benign gynecologic disorders. Each cohort was split into females younger than 50 years and those over age 50.
In the analysis, females younger than 50 years with ovarian cancer were more likely to have a community type O microbiota relative to age-matched controls (adjusted odds ratio, 2.80; P = .020).
In the BRCA set, women with a BRCA1 mutation who were younger than 50 years were also more likely to present with a community type O microbiota than were wild type age-matched controls (adjusted odds ratio, 2.79; P = .012).
“In both sets, we noted that the younger the participants, the stronger the association between community type O microbiota and ovarian cancer or BRCA1 mutation status,” the researchers wrote.
They acknowledged that a key limitation of the study was the homogenous patient population. Since the vaginal microbiome can vary based on ethnicity, the generalizability of the results may be limited.
“Our findings warrant further detailed analyses of the vaginal microbiome, especially in high-risk women,” they concluded.
The study was funded by the EU’s Horizon 2020 Research and Innovation Programme, the EU’s Horizon 2020 European Research Council Programme, and The Eve Appeal. The authors reported financial affiliations with Eurofins, AstraZeneca, Biocad, Clovis, Pharmamar, Roche, Takeda, and Tesaro.
SOURCE: Nené NR et al. Lancet Oncol. 2019 Jul 9. doi: 10.1016/S1470-2045(19)30340-7.
One question that remains from the current study is whether the human microbiota is an important factor in the pathogenesis and development of ovarian cancer.
Currently, there has been no evidence directly linking the composition of the human microbiota to ovarian cancer. As a result, causation has yet to be established by means of randomized studies, since the majority of completed studies have been cross-sectional in nature. As a highly heterogeneous condition, several factors may be involved, including a variety of host reproductive, genetic, microbiota, and lifestyle considerations.
While various mechanisms have been proposed, other less familiar causes could also be implicated. For example, Dr. Nené and colleagues found an association between BRCA1 mutation carriers younger than 50 years of age and the presence of community type O microbiota, while only 10%-15% of females with incident ovarian cancers exhibit this mutation. These findings accentuate the complexities of ovarian cancer pathophysiology.
Despite the suggested benefits of probiotic therapy, there remains a call for systems biology strategies in ovarian cancer research. In a similar manner, the human microbiota needs to be considered in future research.
Hans Verstraelen, MD, MPH, PhD, is affiliated with Ghent University and the Ghent University Hospital in Belgium. Dr. Verstraelen reported no competing interests. These comments are adapted from his editorial (Lancet Oncol. 2019 Jul 9. doi: 10.1016/ S1470-2045[19]30340-7 ).
One question that remains from the current study is whether the human microbiota is an important factor in the pathogenesis and development of ovarian cancer.
Currently, there has been no evidence directly linking the composition of the human microbiota to ovarian cancer. As a result, causation has yet to be established by means of randomized studies, since the majority of completed studies have been cross-sectional in nature. As a highly heterogeneous condition, several factors may be involved, including a variety of host reproductive, genetic, microbiota, and lifestyle considerations.
While various mechanisms have been proposed, other less familiar causes could also be implicated. For example, Dr. Nené and colleagues found an association between BRCA1 mutation carriers younger than 50 years of age and the presence of community type O microbiota, while only 10%-15% of females with incident ovarian cancers exhibit this mutation. These findings accentuate the complexities of ovarian cancer pathophysiology.
Despite the suggested benefits of probiotic therapy, there remains a call for systems biology strategies in ovarian cancer research. In a similar manner, the human microbiota needs to be considered in future research.
Hans Verstraelen, MD, MPH, PhD, is affiliated with Ghent University and the Ghent University Hospital in Belgium. Dr. Verstraelen reported no competing interests. These comments are adapted from his editorial (Lancet Oncol. 2019 Jul 9. doi: 10.1016/ S1470-2045[19]30340-7 ).
One question that remains from the current study is whether the human microbiota is an important factor in the pathogenesis and development of ovarian cancer.
Currently, there has been no evidence directly linking the composition of the human microbiota to ovarian cancer. As a result, causation has yet to be established by means of randomized studies, since the majority of completed studies have been cross-sectional in nature. As a highly heterogeneous condition, several factors may be involved, including a variety of host reproductive, genetic, microbiota, and lifestyle considerations.
While various mechanisms have been proposed, other less familiar causes could also be implicated. For example, Dr. Nené and colleagues found an association between BRCA1 mutation carriers younger than 50 years of age and the presence of community type O microbiota, while only 10%-15% of females with incident ovarian cancers exhibit this mutation. These findings accentuate the complexities of ovarian cancer pathophysiology.
Despite the suggested benefits of probiotic therapy, there remains a call for systems biology strategies in ovarian cancer research. In a similar manner, the human microbiota needs to be considered in future research.
Hans Verstraelen, MD, MPH, PhD, is affiliated with Ghent University and the Ghent University Hospital in Belgium. Dr. Verstraelen reported no competing interests. These comments are adapted from his editorial (Lancet Oncol. 2019 Jul 9. doi: 10.1016/ S1470-2045[19]30340-7 ).
Women with epithelial ovarian cancer or BRCA1 mutational status were more likely to present with a community type O cervicovaginal microbiota relative to age-matched controls, according to a case-control analysis.
The results suggest that the composition of the cervicovaginal microbiome may have a key role in ovarian carcinogenesis. In addition, dysbiosis could be an important risk factor in women at high risk for the disease.
“Our aim was to establish whether women with, or at risk of developing, ovarian cancer have an imbalanced cervicovaginal microbiome,” wrote Nuno R Nené, PhD, of University College London, and colleagues. Their report is in The Lancet Oncology.
The researchers conducted a case-control study of adult females located in five European countries. Study participants were divided into two sets that consisted of 176 females with ovarian cancer and 109 females with a BRCA1 mutation, but without a diagnosis of ovarian cancer.
The two sets were matched with a combination of healthy controls and others with benign gynecologic disorders. Each cohort was split into females younger than 50 years and those over age 50.
In the analysis, females younger than 50 years with ovarian cancer were more likely to have a community type O microbiota relative to age-matched controls (adjusted odds ratio, 2.80; P = .020).
In the BRCA set, women with a BRCA1 mutation who were younger than 50 years were also more likely to present with a community type O microbiota than were wild type age-matched controls (adjusted odds ratio, 2.79; P = .012).
“In both sets, we noted that the younger the participants, the stronger the association between community type O microbiota and ovarian cancer or BRCA1 mutation status,” the researchers wrote.
They acknowledged that a key limitation of the study was the homogenous patient population. Since the vaginal microbiome can vary based on ethnicity, the generalizability of the results may be limited.
“Our findings warrant further detailed analyses of the vaginal microbiome, especially in high-risk women,” they concluded.
The study was funded by the EU’s Horizon 2020 Research and Innovation Programme, the EU’s Horizon 2020 European Research Council Programme, and The Eve Appeal. The authors reported financial affiliations with Eurofins, AstraZeneca, Biocad, Clovis, Pharmamar, Roche, Takeda, and Tesaro.
SOURCE: Nené NR et al. Lancet Oncol. 2019 Jul 9. doi: 10.1016/S1470-2045(19)30340-7.
Women with epithelial ovarian cancer or BRCA1 mutational status were more likely to present with a community type O cervicovaginal microbiota relative to age-matched controls, according to a case-control analysis.
The results suggest that the composition of the cervicovaginal microbiome may have a key role in ovarian carcinogenesis. In addition, dysbiosis could be an important risk factor in women at high risk for the disease.
“Our aim was to establish whether women with, or at risk of developing, ovarian cancer have an imbalanced cervicovaginal microbiome,” wrote Nuno R Nené, PhD, of University College London, and colleagues. Their report is in The Lancet Oncology.
The researchers conducted a case-control study of adult females located in five European countries. Study participants were divided into two sets that consisted of 176 females with ovarian cancer and 109 females with a BRCA1 mutation, but without a diagnosis of ovarian cancer.
The two sets were matched with a combination of healthy controls and others with benign gynecologic disorders. Each cohort was split into females younger than 50 years and those over age 50.
In the analysis, females younger than 50 years with ovarian cancer were more likely to have a community type O microbiota relative to age-matched controls (adjusted odds ratio, 2.80; P = .020).
In the BRCA set, women with a BRCA1 mutation who were younger than 50 years were also more likely to present with a community type O microbiota than were wild type age-matched controls (adjusted odds ratio, 2.79; P = .012).
“In both sets, we noted that the younger the participants, the stronger the association between community type O microbiota and ovarian cancer or BRCA1 mutation status,” the researchers wrote.
They acknowledged that a key limitation of the study was the homogenous patient population. Since the vaginal microbiome can vary based on ethnicity, the generalizability of the results may be limited.
“Our findings warrant further detailed analyses of the vaginal microbiome, especially in high-risk women,” they concluded.
The study was funded by the EU’s Horizon 2020 Research and Innovation Programme, the EU’s Horizon 2020 European Research Council Programme, and The Eve Appeal. The authors reported financial affiliations with Eurofins, AstraZeneca, Biocad, Clovis, Pharmamar, Roche, Takeda, and Tesaro.
SOURCE: Nené NR et al. Lancet Oncol. 2019 Jul 9. doi: 10.1016/S1470-2045(19)30340-7.
Labor outcomes unchanged by alternate anesthesia in bleeding disorder patients
Among pregnant women with inherited bleeding disorders, having a contraindication to regional anesthesia appears not to impact labor outcomes, according to a retrospective analysis.
“The purpose of this study was to determine the anesthetic use in labour in a cohort of women with inherited bleeding disorders,” wrote Sean C. Boyd, of Coombe Women & Infants University Hospital in Dublin, Ireland, and colleagues. The findings were reported in the European Journal of Obstetrics & Gynecology and Reproductive Biology.
The study comprised 97 pregnant women with an inherited bleeding disorder and outcomes related to 130 delivered newborns.
The researchers reviewed medical records of patients with a variety of inherited bleeding disorders: type 1 von Willebrand disease (VWD), deficiencies of factors VII, VIII, IX, X, and XI, combined deficiencies, and others.
Various clinical data, including both obstetric and anesthetic outcomes, were collected from January 2011 to December 2016.
When researchers compared pregnancies where regional anesthesia was contraindicated to those in which it was considered safe, women with a contraindication were more likely to receive general anesthesia for cesarean section (20% vs. 1%), more likely to use a remifentanil infusion (31% vs. 0), and more likely to require prophylactic hemostatic support for delivery (61% vs. 1%).
Vaginal (71% vs. 65%; P = .4) and caesarean section (29% vs. 32%; P = .28) delivery rates were similar between the two groups.
Rates of postpartum hemorrhage were greater in pregnancies where regional anesthesia was contraindicated (24% vs. 12%), but not significantly different (P = .07). No cases of vertebral canal hematoma or neonatal hemorrhage were reported among participants.
“Women are anxious about analgesia and anesthesia in labour and understandably, more so, when they are aware that they are unable to have an epidural or spinal,” the researchers wrote. “This study shows what alternative analgesia is used in labour and, reassuringly, that labour outcome is the same.”
Two key limitations of the study were the small sample size and the wide range of included bleeding disorders.
No funding sources were reported. The authors did not report conflicts of interest.
SOURCE: Boyd SC et al. Eur J Obstet Gynecol Reprod Biol. 2019 Jun 3. doi: 10.1016/j.ejogrb.2019.05.043.
Among pregnant women with inherited bleeding disorders, having a contraindication to regional anesthesia appears not to impact labor outcomes, according to a retrospective analysis.
“The purpose of this study was to determine the anesthetic use in labour in a cohort of women with inherited bleeding disorders,” wrote Sean C. Boyd, of Coombe Women & Infants University Hospital in Dublin, Ireland, and colleagues. The findings were reported in the European Journal of Obstetrics & Gynecology and Reproductive Biology.
The study comprised 97 pregnant women with an inherited bleeding disorder and outcomes related to 130 delivered newborns.
The researchers reviewed medical records of patients with a variety of inherited bleeding disorders: type 1 von Willebrand disease (VWD), deficiencies of factors VII, VIII, IX, X, and XI, combined deficiencies, and others.
Various clinical data, including both obstetric and anesthetic outcomes, were collected from January 2011 to December 2016.
When researchers compared pregnancies where regional anesthesia was contraindicated to those in which it was considered safe, women with a contraindication were more likely to receive general anesthesia for cesarean section (20% vs. 1%), more likely to use a remifentanil infusion (31% vs. 0), and more likely to require prophylactic hemostatic support for delivery (61% vs. 1%).
Vaginal (71% vs. 65%; P = .4) and caesarean section (29% vs. 32%; P = .28) delivery rates were similar between the two groups.
Rates of postpartum hemorrhage were greater in pregnancies where regional anesthesia was contraindicated (24% vs. 12%), but not significantly different (P = .07). No cases of vertebral canal hematoma or neonatal hemorrhage were reported among participants.
“Women are anxious about analgesia and anesthesia in labour and understandably, more so, when they are aware that they are unable to have an epidural or spinal,” the researchers wrote. “This study shows what alternative analgesia is used in labour and, reassuringly, that labour outcome is the same.”
Two key limitations of the study were the small sample size and the wide range of included bleeding disorders.
No funding sources were reported. The authors did not report conflicts of interest.
SOURCE: Boyd SC et al. Eur J Obstet Gynecol Reprod Biol. 2019 Jun 3. doi: 10.1016/j.ejogrb.2019.05.043.
Among pregnant women with inherited bleeding disorders, having a contraindication to regional anesthesia appears not to impact labor outcomes, according to a retrospective analysis.
“The purpose of this study was to determine the anesthetic use in labour in a cohort of women with inherited bleeding disorders,” wrote Sean C. Boyd, of Coombe Women & Infants University Hospital in Dublin, Ireland, and colleagues. The findings were reported in the European Journal of Obstetrics & Gynecology and Reproductive Biology.
The study comprised 97 pregnant women with an inherited bleeding disorder and outcomes related to 130 delivered newborns.
The researchers reviewed medical records of patients with a variety of inherited bleeding disorders: type 1 von Willebrand disease (VWD), deficiencies of factors VII, VIII, IX, X, and XI, combined deficiencies, and others.
Various clinical data, including both obstetric and anesthetic outcomes, were collected from January 2011 to December 2016.
When researchers compared pregnancies where regional anesthesia was contraindicated to those in which it was considered safe, women with a contraindication were more likely to receive general anesthesia for cesarean section (20% vs. 1%), more likely to use a remifentanil infusion (31% vs. 0), and more likely to require prophylactic hemostatic support for delivery (61% vs. 1%).
Vaginal (71% vs. 65%; P = .4) and caesarean section (29% vs. 32%; P = .28) delivery rates were similar between the two groups.
Rates of postpartum hemorrhage were greater in pregnancies where regional anesthesia was contraindicated (24% vs. 12%), but not significantly different (P = .07). No cases of vertebral canal hematoma or neonatal hemorrhage were reported among participants.
“Women are anxious about analgesia and anesthesia in labour and understandably, more so, when they are aware that they are unable to have an epidural or spinal,” the researchers wrote. “This study shows what alternative analgesia is used in labour and, reassuringly, that labour outcome is the same.”
Two key limitations of the study were the small sample size and the wide range of included bleeding disorders.
No funding sources were reported. The authors did not report conflicts of interest.
SOURCE: Boyd SC et al. Eur J Obstet Gynecol Reprod Biol. 2019 Jun 3. doi: 10.1016/j.ejogrb.2019.05.043.
FROM THE EUROPEAN JOURNAL OF OBSTETRICS & GYNECOLOGY AND REPRODUCTIVE BIOLOGY
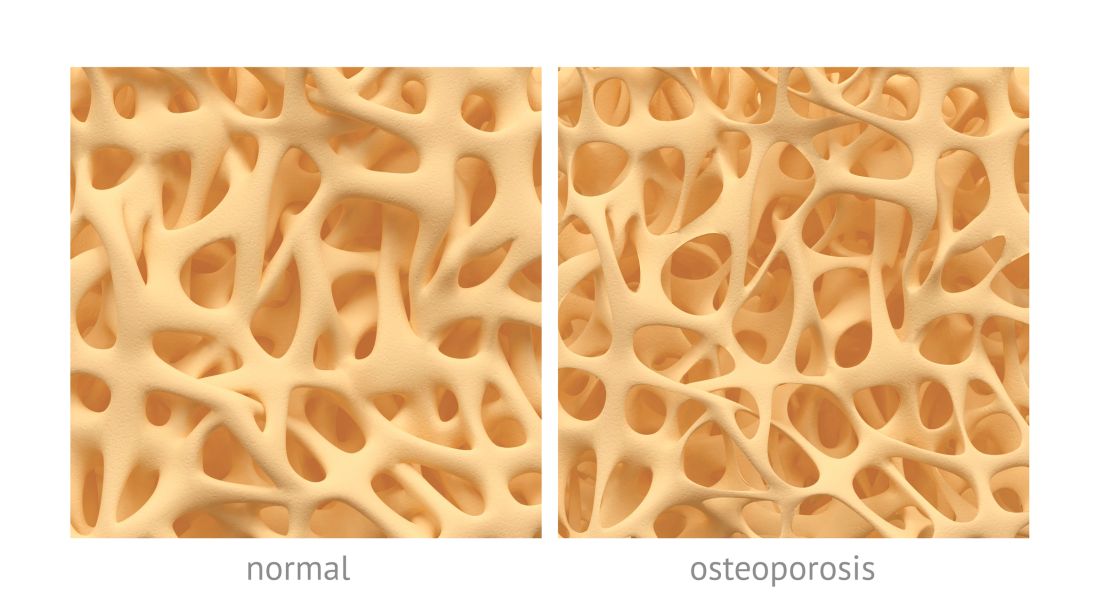
Osteoporotic fracture risk appears higher in adults with hemophilia
Adults with newly diagnosed hemophilia may be at a higher risk of developing osteoporotic fractures, according to results from a retrospective study.
Sheng-Hui Tuan, MD, of Cishan Hospital in Kaohsiung, Taiwan, and colleagues conducted a population-based nationwide cohort study that included 75 patients with hemophilia and 300 control subjects without hemophilia matched for age and sex. Data was obtained from a national insurance database in Taiwan from January 2000 to December 2013. The findings were published in Haemophilia.
The primary outcome measured was newly diagnosed osteoporotic fractures, defined as wrist, vertebral, and hip fractures among individuals from both groups. Patients with osteoporotic fractures before hemophilia diagnosis were excluded.
In the analysis, the team calculated hazard ratios and incidence rates of new-onset osteoporotic fractures in both cohorts.
After analysis, the researchers found that the risk of developing new-onset osteoporotic fractures was greater in the hemophilia group versus the comparison group (HR, 5.41; 95% confidence interval, 2.42-12.1; P less than .001).
After adjusting for covariates, such as socioeconomic status, age, sex, and other comorbidities, patients with hemophilia had a 337% higher risk of developing osteoporotic fractures post diagnosis versus matched controls (95% CI, 1.88-10.17; P = .001).
“The risk of osteoporotic fractures following haemophilia increased with time and was significantly higher at 5 years after the diagnosis,” the researchers wrote.
The underlying mechanisms driving these associations remain unknown, according to the authors. Possible risk factors include reduced physical activity, HIV and hepatitis C virus infections, and arthropathy.
The researchers acknowledged that a key limitation of the study was the absence of some relevant clinical information within the database. As a result, information bias could have lowered the accuracy of the analysis.
No funding sources were reported. The authors reported having no conflicts of interest.
SOURCE: Tuan S-H et al. Haemophilia. 2019 Jul 7. doi: 10.1111/hae.13814.
Adults with newly diagnosed hemophilia may be at a higher risk of developing osteoporotic fractures, according to results from a retrospective study.
Sheng-Hui Tuan, MD, of Cishan Hospital in Kaohsiung, Taiwan, and colleagues conducted a population-based nationwide cohort study that included 75 patients with hemophilia and 300 control subjects without hemophilia matched for age and sex. Data was obtained from a national insurance database in Taiwan from January 2000 to December 2013. The findings were published in Haemophilia.
The primary outcome measured was newly diagnosed osteoporotic fractures, defined as wrist, vertebral, and hip fractures among individuals from both groups. Patients with osteoporotic fractures before hemophilia diagnosis were excluded.
In the analysis, the team calculated hazard ratios and incidence rates of new-onset osteoporotic fractures in both cohorts.
After analysis, the researchers found that the risk of developing new-onset osteoporotic fractures was greater in the hemophilia group versus the comparison group (HR, 5.41; 95% confidence interval, 2.42-12.1; P less than .001).
After adjusting for covariates, such as socioeconomic status, age, sex, and other comorbidities, patients with hemophilia had a 337% higher risk of developing osteoporotic fractures post diagnosis versus matched controls (95% CI, 1.88-10.17; P = .001).
“The risk of osteoporotic fractures following haemophilia increased with time and was significantly higher at 5 years after the diagnosis,” the researchers wrote.
The underlying mechanisms driving these associations remain unknown, according to the authors. Possible risk factors include reduced physical activity, HIV and hepatitis C virus infections, and arthropathy.
The researchers acknowledged that a key limitation of the study was the absence of some relevant clinical information within the database. As a result, information bias could have lowered the accuracy of the analysis.
No funding sources were reported. The authors reported having no conflicts of interest.
SOURCE: Tuan S-H et al. Haemophilia. 2019 Jul 7. doi: 10.1111/hae.13814.
Adults with newly diagnosed hemophilia may be at a higher risk of developing osteoporotic fractures, according to results from a retrospective study.
Sheng-Hui Tuan, MD, of Cishan Hospital in Kaohsiung, Taiwan, and colleagues conducted a population-based nationwide cohort study that included 75 patients with hemophilia and 300 control subjects without hemophilia matched for age and sex. Data was obtained from a national insurance database in Taiwan from January 2000 to December 2013. The findings were published in Haemophilia.
The primary outcome measured was newly diagnosed osteoporotic fractures, defined as wrist, vertebral, and hip fractures among individuals from both groups. Patients with osteoporotic fractures before hemophilia diagnosis were excluded.
In the analysis, the team calculated hazard ratios and incidence rates of new-onset osteoporotic fractures in both cohorts.
After analysis, the researchers found that the risk of developing new-onset osteoporotic fractures was greater in the hemophilia group versus the comparison group (HR, 5.41; 95% confidence interval, 2.42-12.1; P less than .001).
After adjusting for covariates, such as socioeconomic status, age, sex, and other comorbidities, patients with hemophilia had a 337% higher risk of developing osteoporotic fractures post diagnosis versus matched controls (95% CI, 1.88-10.17; P = .001).
“The risk of osteoporotic fractures following haemophilia increased with time and was significantly higher at 5 years after the diagnosis,” the researchers wrote.
The underlying mechanisms driving these associations remain unknown, according to the authors. Possible risk factors include reduced physical activity, HIV and hepatitis C virus infections, and arthropathy.
The researchers acknowledged that a key limitation of the study was the absence of some relevant clinical information within the database. As a result, information bias could have lowered the accuracy of the analysis.
No funding sources were reported. The authors reported having no conflicts of interest.
SOURCE: Tuan S-H et al. Haemophilia. 2019 Jul 7. doi: 10.1111/hae.13814.
FROM HAEMOPHILIA
Novel point-of-care assay appears accurate in monitoring hemophilia A
A novel point-of-care assay demonstrated sensitivity to monitor coagulation factor replacement therapy in patients with severe hemophilia A, with and without inhibitors, according to recent study findings.
The ClotChip assay is a novel factor-replacement therapy monitoring tool that uses a dielectric microsensor to assess whole-blood coagulation in patients with severe hemophilia A.
Debnath Maji of Case Western Reserve University, Cleveland, and colleagues evaluated the novel assay in attempt to address the unmet need of reliable monitoring of coagulation factor–replacement therapy. While global haemostasis assays are available to measure the missing function, these tools require expert interpretation, are technically challenging to operate, and may be unavailable at the bedside, they wrote in Haemophilia.
They evaluated the analytical capabilities of the assay in 6 patients with inhibitors and 12 patients without inhibitors. A total of 50 healthy controls were included in the study.
The team collected whole blood samples pre- and postcoagulation factor–replacement therapy. Measurements were also conducted on the thrombin generation assay (TGA), thromboelastography (TEG), and rotational thromboelastometry (ROTEM) global assays for comparison.
After analysis, the researchers found that ClotChip T-peak parameters showed a significant reduction for samples obtained post–factor replacement therapy versus pretherapy among patients with and without inhibitors (P = .028 and P = .0001, respectively).
Additionally, ClotChip T-peak values exhibited strong correlations with factor VIII clotting activity, clotting time parameters of ROTEM, and peak thrombin and endogenous thrombin potential of TGA.
“Taken together, these data suggest that the ClotChip T-peak parameter is sensitive to detection and correction of coagulopathy in children with haemophilia with and without inhibitors, as indicated by T-peak reaching reference‐range values after coagulation factor replacement therapy,” the researchers wrote.
One key limitation of the study was the small sample size, which may limit the generalizability of the findings.
The novel assay may be an appropriate tool for “real-world” decision making around the use of coagulation factor replacement therapy in patients with severe hemophilia A, they added.
The study was funded by the National Institutes of Health, the American Heart Association, and a Veterans Affairs Research Center of Excellence at Case Western Reserve University. The authors reported financial affiliations with Bayer, Bioverativ, Shire, and XaTek.
SOURCE: Maji D et al. Haemophilia. 2019 Jul 7. doi: 10.1111/hae.13799.
A novel point-of-care assay demonstrated sensitivity to monitor coagulation factor replacement therapy in patients with severe hemophilia A, with and without inhibitors, according to recent study findings.
The ClotChip assay is a novel factor-replacement therapy monitoring tool that uses a dielectric microsensor to assess whole-blood coagulation in patients with severe hemophilia A.
Debnath Maji of Case Western Reserve University, Cleveland, and colleagues evaluated the novel assay in attempt to address the unmet need of reliable monitoring of coagulation factor–replacement therapy. While global haemostasis assays are available to measure the missing function, these tools require expert interpretation, are technically challenging to operate, and may be unavailable at the bedside, they wrote in Haemophilia.
They evaluated the analytical capabilities of the assay in 6 patients with inhibitors and 12 patients without inhibitors. A total of 50 healthy controls were included in the study.
The team collected whole blood samples pre- and postcoagulation factor–replacement therapy. Measurements were also conducted on the thrombin generation assay (TGA), thromboelastography (TEG), and rotational thromboelastometry (ROTEM) global assays for comparison.
After analysis, the researchers found that ClotChip T-peak parameters showed a significant reduction for samples obtained post–factor replacement therapy versus pretherapy among patients with and without inhibitors (P = .028 and P = .0001, respectively).
Additionally, ClotChip T-peak values exhibited strong correlations with factor VIII clotting activity, clotting time parameters of ROTEM, and peak thrombin and endogenous thrombin potential of TGA.
“Taken together, these data suggest that the ClotChip T-peak parameter is sensitive to detection and correction of coagulopathy in children with haemophilia with and without inhibitors, as indicated by T-peak reaching reference‐range values after coagulation factor replacement therapy,” the researchers wrote.
One key limitation of the study was the small sample size, which may limit the generalizability of the findings.
The novel assay may be an appropriate tool for “real-world” decision making around the use of coagulation factor replacement therapy in patients with severe hemophilia A, they added.
The study was funded by the National Institutes of Health, the American Heart Association, and a Veterans Affairs Research Center of Excellence at Case Western Reserve University. The authors reported financial affiliations with Bayer, Bioverativ, Shire, and XaTek.
SOURCE: Maji D et al. Haemophilia. 2019 Jul 7. doi: 10.1111/hae.13799.
A novel point-of-care assay demonstrated sensitivity to monitor coagulation factor replacement therapy in patients with severe hemophilia A, with and without inhibitors, according to recent study findings.
The ClotChip assay is a novel factor-replacement therapy monitoring tool that uses a dielectric microsensor to assess whole-blood coagulation in patients with severe hemophilia A.
Debnath Maji of Case Western Reserve University, Cleveland, and colleagues evaluated the novel assay in attempt to address the unmet need of reliable monitoring of coagulation factor–replacement therapy. While global haemostasis assays are available to measure the missing function, these tools require expert interpretation, are technically challenging to operate, and may be unavailable at the bedside, they wrote in Haemophilia.
They evaluated the analytical capabilities of the assay in 6 patients with inhibitors and 12 patients without inhibitors. A total of 50 healthy controls were included in the study.
The team collected whole blood samples pre- and postcoagulation factor–replacement therapy. Measurements were also conducted on the thrombin generation assay (TGA), thromboelastography (TEG), and rotational thromboelastometry (ROTEM) global assays for comparison.
After analysis, the researchers found that ClotChip T-peak parameters showed a significant reduction for samples obtained post–factor replacement therapy versus pretherapy among patients with and without inhibitors (P = .028 and P = .0001, respectively).
Additionally, ClotChip T-peak values exhibited strong correlations with factor VIII clotting activity, clotting time parameters of ROTEM, and peak thrombin and endogenous thrombin potential of TGA.
“Taken together, these data suggest that the ClotChip T-peak parameter is sensitive to detection and correction of coagulopathy in children with haemophilia with and without inhibitors, as indicated by T-peak reaching reference‐range values after coagulation factor replacement therapy,” the researchers wrote.
One key limitation of the study was the small sample size, which may limit the generalizability of the findings.
The novel assay may be an appropriate tool for “real-world” decision making around the use of coagulation factor replacement therapy in patients with severe hemophilia A, they added.
The study was funded by the National Institutes of Health, the American Heart Association, and a Veterans Affairs Research Center of Excellence at Case Western Reserve University. The authors reported financial affiliations with Bayer, Bioverativ, Shire, and XaTek.
SOURCE: Maji D et al. Haemophilia. 2019 Jul 7. doi: 10.1111/hae.13799.
FROM HAEMOPHILIA