User login
Heart failure in African Americans: Disparities can be overcome
African Americans are disproportionately affected by heart failure and have not experienced the same benefit from treatment as white patients have. Much of the disparity can be blamed on modifiable risk factors such as uncontrolled hypertension and on suboptimal health care. When African Americans are treated according to guidelines, discrepant outcomes can be minimized.
In this article, we review the processes contributing to heart failure in African Americans, its management, and challenges with regard to disparities.
HEART FAILURE IS INCREASING
Despite 20 years of progress in understanding the pathophysiology of heart failure and developing medical and surgical therapies for it, its prevalence and associated morbidity are increasing in the United States. In 2010, 6.6 million (2.8%) of the adults in the United States had heart failure,1 and the prevalence is expected to increase by about 25% by 2030.
DISPARITIES IN INCIDENCE, OUTCOMES
Heart failure is more prevalent in African Americans than in whites, imposes higher rates of death and morbidity, and has a more malignant course.1–6
According to American Heart Association statistics, the annual incidence of heart failure in whites is approximately 6 per 1,000 person-years, while in African Americans it is 9.1 per 1,000 person-years.1 In the Atherosclerosis Risk in Communities study, the incidence of new heart failure was 1.0 per 1,000 person-years in Chinese Americans, 2.4 in whites, 3.5 in Hispanics, and 4.6 in African Americans.2
Moreover, when hospitalized for heart failure, African Americans have a 45% greater risk of death or decline in functional status than whites.7
Heart failure also occurs earlier in African Americans. Bibbins-Domingo et al8 reported that heart failure before age 50 was 20 times more frequent in African Americans than in whites. Functional and structural cardiac changes appeared an average of 10 years before the onset of symptoms and were strongly associated with the development of subsequent heart failure.8
In the Women’s Health Initiative, African American women had higher rates of heart failure than white women, perhaps in part because of higher rates of diabetes.9
Heart failure with preserved ejection fraction
About half of patients who have signs and symptoms of heart failure have a normal (“preserved”) ejection fraction. The incidence of this condition, previously called diastolic heart failure, appears to be similar between African Americans and whites. However, African Americans appear to have a greater incidence of factors that predispose to it and tend to present later in the course.10 For example, African Americans have higher left ventricular mass and wall thickness and a higher incidence of left ventricular hypertrophy than white patients.11–13 In addition, those with heart failure with preserved ejection fraction tend to be younger, female, more likely to have hypertension and diabetes, and less likely to have coronary artery disease, and tend to have worse renal function than their white counterparts.14,15 The predisposition to diastolic impairment persists even after adjusting for risk factors.11–15 The mortality rate in African Americans with heart failure with preserved ejection fraction and without coronary artery disease may also be higher than that of comparable white patients.16
WHY DO AFRICAN AMERICANS HAVE MORE HEART FAILURE?
Modifiable risk factors
In African Americans, the higher percentage of cases of heart failure is attributable to modifiable risk factors such as hypertension, hyperglycemia, left ventricular hypertrophy, and smoking, and fewer cases are due to ischemic heart disease.2,3 Nonischemic cardiomyopathy predominates in African Americans, whereas ischemic cardiomyopathy predominates in whites.
Hypertension, diabetes, obesity, and chronic kidney disease all portend subsequent heart failure and are common in African Americans, but hypertension is the main culprit.3,5,8,17–21 The prevalence of hypertension in African Americans is among the highest in the world, and because African Americans are more likely to have poorer control of their hypertension, they consequently have more target-organ damage.22 Indeed, in many hypertensive African Americans who develop heart failure, the hypertension is poorly controlled. However, even after adjusting for risk factors, and particularly blood pressure control, African Americans remain at higher risk of heart failure.23
The specific mechanistic links between hypertension and heart failure remain to be identified. Despite having a higher prevalence of left ventricular hypertrophy and left ventricular remodeling, African Americans with heart failure tend toward systolic heart failure, as opposed to heart failure with preserved ejection fraction.
Neurohormonal imbalances and endothelial dysfunction
Derangements in the renin-angiotensin-aldosterone and adrenergic axes are likely the main pathophysiologic mechanisms in the genesis of heart failure in all populations. However, other factors may underlie the enhanced disease burden in African Americans.
Impaired endothelial function, as evidenced by impaired digital and brachial artery vasomotion, is very common in African Americans.24–26 The small arteries of African Americans are less elastic than those of whites and Chinese.27 The underlying mechanism may be related to increased oxidative stress, decreased nitric oxide availability, exaggerated vasoconstrictor response, and attenuated responsiveness to vasodilators and nitric oxide.28–31
Genetic polymorphisms
An important caveat in discussing racial differences in heart failure is that “race” is completely arbitrary and is based on sociopolitical rather than scientific or physiologic definitions. Perceived genetic influences are likely to represent complex gene-gene, gene-environment, and gene-drug interactions.
This is especially true for African Americans, who are a markedly heterogeneous group. The US Office of Management and Budget defines “black” or “African American” as having origins in any of the black racial groups of Africa (www.census.gov/2010census/data). Thus, “African American” includes sixth-generation descendants of African slaves, recently immigrated Jamaicans, and black descendants of French and Spanish people.
Most African Americans have some European ancestry. In one study, the estimated proportion of European ancestry ranged from 7% in Jamaicans of African descent to approximately 23% in African Americans in New Orleans.32
Nevertheless, several polymorphisms associated with the risk of heart failure may provide insight into some of the “race-based” differences in pathophysiology and response to medications and, it is hoped, may eventually serve as the basis for tailored therapy. Genes of interest include those for:
- Beta 1 adrenergic receptor
- Alpha 2c receptor33
- Aldosterone synthase34
- G protein
- Transforming growth factor beta
- Nitric oxide synthase35
- Transthyrectin.36,37
Socioeconomic factors and quality of care
Heart failure patients—and especially African Americans—have high rates of hospital readmission, and socioeconomic factors have been implicated. In more than 40,000 patients with heart failure, lower income was a significant predictor of hospital readmission.38 Socioeconomic factors in turn could account for delay in seeking treatment for worsening symptoms, failure to recognize symptoms, limited disease awareness, inadequate access to health care, noncompliance with follow-up appointments, and poor adherence to recommended treatment, all of which are common in African American patients.38,39
African Americans also report more discrimination from health care providers, have more concerns about blood pressure medications, and are more likely to have misperceptions about high blood pressure (eg, that it is not serious), all of which may interfere with optimal blood pressure control.40 Managing heart failure in African Americans should include trying to identify and eliminate barriers to attaining treatment goals.
PREVENTING HEART FAILURE BY REDUCING RISK FACTORS
The American College of Cardiology Foundation and American Heart Association, in their 2013 guidelines, underscored the progressive nature of heart failure by defining four stages of the disease, from stage A (at risk) through stage D (refractory heart failure) (Figure 1).41 They also emphasized the importance of preventing it.
A thorough clinical assessment, with appropriate assessment for risk factors and intervention at stage A, is critical in preventing left ventricular remodeling and heart failure. These risk factors include hypertension, hyperlipidemia, atherosclerosis, diabetes mellitus, valvular disease, obesity, physical inactivity, excessive alcohol intake, poor diet, and smoking.
Hypertension is especially important in African Americans and requires vigorous screening and aggressive treatment. Antihypertensive drugs should be prescribed early, with a lower threshold for escalating therapy with combinations of drugs, as most patients require more than one.
There is considerable debate about the appropriate blood pressure thresholds for diagnosing hypertension and the optimal target blood pressures in African Americans. The 2014 report of the Joint National Committee recommends a similar hypertension treatment target of 140/90 mm Hg for all patients except older adults (for whom 150/90 mm Hg is acceptable), and no separate target for African Americans.42 Previous guidelines from this committee recommended thiazide-type diuretics as first-line therapy for hypertension in African Americans43; the new ones recommend thiazide-type diuretics or calcium channel blockers. However, in those with left ventricular systolic dysfunction, hypertension treatment should include drugs shown to reduce the risk of death in heart failure—ie, angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, hydralazine, nitrates, and aldosterone receptor antagonists.
Salt intake should be reduced to less than 3 g per day (1,200 mg of sodium per day), which has been shown to substantially reduce rates of cardiovascular morbidity and mortality and health care costs.44 Since most Americans consume 7 to 10 g of salt per day, strict salt restriction should be encouraged as a preventive measure.
Diabetes should be screened for and treated in African Americans per current American Diabetes Association guidelines.
Dyslipidemia should also be screened for and treated per guidelines.45
Smoking cessation, moderation of alcohol intake, and avoidance of illicit drugs should be encouraged. Given that African Americans develop heart failure at a relatively early age, the level of vigilance should be high and the threshold for screening should be low.
Healthy neighborhoods, healthy people
Neighborhoods can be designed and built with wellness in mind, incorporating features such as access to healthy food and walkability. Living in such neighborhoods leads to more physical activity and less obesity, although this relationship may be less robust in African Americans.46–49
Environmental factors are multifactorial in African Americans and extend beyond those afforded by the built environment. For instance, lack of safety may hinder the potential benefit of an otherwise walkable neighborhood. These interactions are highly complex, and more investigation is needed to determine the effect of built environments on risk factors in African Americans.
DRUG THERAPY FOR HEART FAILURE IN AFRICAN AMERICANS
Use standard therapies
ACE inhibitors, beta-blockers, and aldosterone antagonists are the standard of care in heart failure, with digoxin (Lanoxin) and diuretics used as adjuncts to control symptoms.
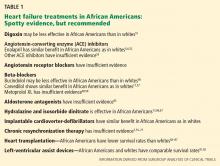
African Americans may respond differently than whites to some of these drugs (Table 1). However, these findings should be interpreted with caution, since most of them came from subgroup analyses of trials in which African Americans accounted for as many as 28% to as few as 1%.50 To date, no data unequivocally show that we should use standard heart failure therapies any differently in African Americans than in whites.
Digoxin: Limited role to control symptoms
Post hoc analysis of the Digitalis Investigation Group trial, in which 14% of the patients were nonwhite, revealed that compared with placebo, digitalis (and achieving a serum digitalis concentration of 0.5 to 0.9 ng/mL) was associated with lower rates of all-cause mortality in most subgroups—except nonwhites.51
In general, digoxin has a limited role in heart failure, since other drugs are available that substantially modify outcomes. However, it can be considered in patients who have persistent heart failure symptoms.
ACE inhibitors, ARBs are recommended
ACE inhibitors are recommended for patients with New York Heart Association (NYHA) class I, II, III, or IV heart failure (class I recommendation, ie, “recommended”; level of evidence A on a scale of A, B, and C) and as part of standard therapy for African American patients with heart failure with symptomatic or asymptomatic left ventricular systolic dysfunction (class I recommendation; level of evidence C).41
Although African American patients did not appear to derive any benefit from enalapril (Vasotec) in the Studies of Left Ventricular Dysfunction (SOLVD) trial,52 a subsequent analysis that involved the SOLVD Prevention Trial did not find any differences between African Americans and whites in response to this agent.6 Similarly, a meta-analysis did not suggest differences in ACE-inhibitor efficacy in reducing adverse cardiovascular outcomes in heart failure between African Americans and non–African Americans.53
Of note: African Americans have a 3% to 4% higher incidence of angioedema from ACE inhibitors than whites.54,55
Angiotensin receptor blockers (ARBs) can be used as substitute therapy in African Americans who cannot tolerate ACE inhibitors (class IIa recommendation, ie, “reasonable”; level of evidence B).41
Beta-blockers also recommended
Beta-blockers are recommended in NYHA class I, II, III, and IV heart failure (class I recommendation; level of evidence A) and as part of standard therapy for African Americans with heart failure due to symptomatic left ventricular systolic dysfunction (class I recommendation; level of evidence B) and asymptomatic left ventricular systolic dysfunction (level of evidence C).41
Carvedilol (Coreg) and metoprolol (Lopressor) are the standard beta-blockers used to treat heart failure, and these drugs should be used in African Americans as well as in whites.15,53,56–59 Of interest, however, race-specific differences may exist in the beta-adrenergic pathway.60,61
Aldosterone antagonists: More study needed
Aldosterone antagonists, also called mineralocorticoid antagonists, ie, spironolactone (Aldactone) and eplerenone (Inspra), are recommended in addition to beta-blockers and ACE inhibitors for NYHA class II–IV heart failure, unless contraindicated (class I recommendation; level of evidence A).
However, trials of aldosterone antagonists to date have enrolled few African Americans.62–64 The limited data suggest that African Americans with heart failure may be less responsive to the renal effects of spironolactone, demonstrating less of an increase in serum potassium levels, and there are essentially no data to guide the use of these drugs in African Americans with heart failure.65 Further study is needed. But in the absence of data to the contrary, these agents, should also be used in African American patients with class III or IV heart failure.
Hydralazine plus nitrates: Recommended for African Americans
Hydralazine plus isosorbide dinitrate (available as BiDil) is recommended as part of standard therapy, in addition to beta-blockers and ACE inhibitors specifically for African Americans with left ventricular systolic dysfunction and NYHA class III or IV heart failure (class I recommendation; level of evidence A), as well as NYHA class II heart failure (class I recommendation; level of evidence B).41
Preliminary evidence for this combination came from the Department of Veterans Affairs Cooperative Vasodilator-Heart Failure Trials.66
Subsequently, the African-American Heart Failure Trial67 was conducted in self-identified African American patients with NYHA class III or IV heart failure on standard heart failure therapy, including an ACE inhibitor if tolerated. Patients were randomly assigned to receive a fixed combination of isosorbide 20 mg and hydralazine 37.5 mg, one or two tablets three times a day, or placebo. The target dose of isosorbide dinitrate was 120 mg, and the target dose of hydralazine was 225 mg daily. Follow-up was up to 18 months. The study was terminated early because of a significant 43% improvement in overall survival for the patients in the isosorbide-hydralazine group. In addition, the rate of first hospitalization was 39% lower and the mean improvement in quality-of-life scores was 52% greater with isosorbide-hydralazine than with placebo.67
There has been much debate about whether the benefit seen in this trial was the result of a hemodynamic effect, blood pressure response, or neurohormonal modulation. The benefit is less likely from a reduction in blood pressure, as the patients who had low blood pressure derived a mortality benefit similar to those with higher blood pressure, despite no further reduction in their blood pressure.68
Treatment for heart failure with preserved ejection fraction
Although there are no data on how to manage heart failure with preserved ejection fraction that are specific to African Americans, the ACCF/AHA guideline41 recommends treating systolic and diastolic hypertension (class I, level of evidence B) according to published clinical practice guidelines and using diuretics to alleviate volume overload (class I; level of evidence C). Revascularization and management of atrial fibrillation are also “reasonable,” as are the use of ARBs, ACE inhibitors, and beta-blockers in the management of hypertension (class IIa; level of evidence C). ARBs may also be considered to reduce hospitalization in symptomatic patients with heart failure with preserved ejection fraction (class IIb, ie, “may be considered”; level of evidence B).
For acute decompensated heart failure
One of the greatest challenges in heart failure is treating patients who present with acute decompensated heart failure.
As in the general population, the major precipitating factor for hospitalization with decompensated heart failure in African Americans is nonadherence to prescribed dietary and medication regimens.35 African Americans with acute decompensated heart failure tend to be younger and to have nonischemic cardiomyopathy, hypertension, diabetes, and obesity, but a lower risk of death.35,69,70 Up to 44% have uncontrolled hypertension.35
Inotropes and vasodilators have undergone multiple trials in the acutely decompensated state in the general population, but no trial has demonstrated a reduction in the mortality rate, and some showed a higher mortality rate. Thus, the treatment of acute decompensated heart failure remains primarily consensus-guided and symptom-focused.
Loop diuretics have been the mainstay in managing fluid retention and congestion in heart failure. The Diuretic Optimization Strategies Evaluation trial tested low-dose vs high-dose intravenous furosemide (Lasix) given either as a continuous infusion or as intermittent intravenous boluses. All strategies were safe and effective.71
Although ultrafiltration is an effective method of decongestion in heart failure and has been associated with a reduction in hospitalization, it is also associated with worsening renal function.72 The Cardiorenal Rescue Study in Acute Decompensated Heart Failure73 compared ultrafiltration vs stepped diuretic therapy. In this trial, which enrolled approximately 26% nonwhites, stepped diuretic therapy was superior to ultrafiltration in preserving renal function in acute decompensated heart failure, although the efficacy of fluid removal was similar.
Both studies were small, and subgroup analyses are not likely to yield useful information. Nevertheless, these data support the use of intravenous diuretics, by continuous infusion or bolus, in acute decompensated heart failure.
Despite no benefit in terms of the mortality rate, inotropes continue to be used in some cases of acute decompensated heart failure, and African Americans appear to have a response to milrinone (Primacor IV) similar to that in whites.69
In a nonrandomized study in which most patients were black, high-dose intravenous nitroglycerin appeared to be safe and associated with less need for ventilator support and intensive care unit admission, compared retrospectively with a population that did not receive high-dose nitroglycerin.74
Given the different profile of the African American patient with acute decompensated heart failure, prospective studies would be useful in determining the best management strategy.
TREATMENTS FOR ADVANCED HEART FAILURE
Cardiac resynchronization and implantable cardioverter-defibrillators
Cardiac resynchronization therapy is indicated for patients with NYHA class II, III, and ambulatory class IV heart failure and left ventricular ejection fraction less than or equal to 35%, sinus rhythm, left bundle branch block, and a QRS duration greater than or equal to 150 ms (class I recommendation; level of evidence A for class NYHA III and IV; level of evidence B for NYHA class II).41
An implantable cardioverter-defibrillator is recommended in patients with NYHA class II or III heart failure for primary prevention of sudden cardiac death in selected patients with nonischemic dilated cardiomyopathy or ischemic heart disease (class I recommendation; level of evidence A).
However, few members of racial and ethnic minorities were included in trials of implantable cardioverter-defibrillators75,76 or cardiac resynchronization,7,77,78 so that subgroup analysis is limited. Use of an implantable cardioverter-defibrillator showed similar reduction in mortality between African Americans and whites, and compliance with device implantation and medical therapy was comparable.79
Among patients discharged from hospitals in the American Heart Association’s Get With the Guidelines–Heart Failure Quality Improvement Program, fewer than 40% of potentially eligible patients received an implantable cardioverter-defibrillator, and rates were significantly lower for African Americans.80 When they can get cardiac resynchronization therapy, African Americans appear to experience similar benefit from it.81
Heart transplantation: Poorer outcomes in African Americans?
Heart transplantation remains the most effective and durable therapy for advanced heart failure. Median survival approaches 14 years.82
However, a retrospective study found that African American recipients had an 11.5% lower 10-year survival rate than whites, which persisted after adjusting for risk, donor-recipient matching by race, and censoring of deaths in the first year.83 Although socioeconomic factors and poor human leukocyte antigen matching have been implicated, a retrospective cohort study showed that African American recipients had a higher risk of death than white recipients even after adjustment for recipient, transplant, and socioeconomic factors.84–87 African Americans were more likely to die of graft failure or of a cardiovascular cause than white patients, but were less likely to die of infection or malignancy. Although mortality rates decreased over time for all transplant recipients, the disparity in mortality rates between African Americans and whites remained essentially unchanged.84
Among all donor-recipient combinations, African American recipients of hearts from African American donors had the highest risk of death.88
Limited access to transplantation persists, particularly for African Americans of lower socioeconomic status. African Americans are more likely than whites to be uninsured, and the funding requirement to be placed on the transplantation list disproportionately affects African Americans.89,90
Left-ventricular assist devices
Left-ventricular assist devices (LVADs) improve survival in heart transplantation candidates and heart failure patients who do not qualify for transplantation. After LVAD implantation, African American patients have similar 1- and 2-year survival rates and no difference in readmission rates compared with whites.91,92
Access to LVAD implantation, however, is significantly influenced by race, and African Americans are significantly less likely to receive one (OR = 0.29).93 Further investigation is required to identify disparities in outcome, access, and contributing factors.
DISPARITIES CAN BE MINIMIZED
In general, heart failure in African Americans is characterized by a high prevalence of hypertension as a major risk factor and potentially different pathogenesis than in the general population. Furthermore, heart failure in African Americans is more prevalent, occurs at an early age, and has a more severe course than in whites, perhaps because of a higher prevalence of risk factors such as diabetes mellitus, obesity, and again, hypertension. These disparities are multifactorial and involve a complex interplay between genes, environment, and socioeconomic factors.
For now, heart failure in African Americans should be treated according to standard evidenced-based strategies, which include a combination of isosorbide dinitrate and hydralazine in addition to other neurohormonal modifying agents (ACE inhibitors, beta-blockers, aldosterone antagonists), a strategy demonstrated to reduce mortality rates in African Americans. When treated according to guidelines, disparities in outcomes can be minimized.
However, many questions about managing heart failure remain unanswered, since African Americans have been markedly underrepresented in clinical trials. Clinical trials need to enroll enough African Americans to answer the questions of interest. Disparities in outcomes must be investigated in a scientific and hypothesis-driven manner. The effect of the built environment on African Americans needs more study as well, as success with these strategies may be impeded by unrecognized factors.
Preventing heart failure should be a priority. Efforts should be directed toward detecting and modifying risk factors early, managing hypertension aggressively, and identifying left ventricular dysfunction early.
- Go AS, Mozaffarian D, Roger VL, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation 2013; 127:e6–e245.
- Bahrami H, Kronmal R, Bluemke DA, et al. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med 2008; 168:2138–2145.
- Loehr LR, Rosamond WD, Chang PP, Folsom AR, Chambless LE. Heart failure incidence and survival (from the Atherosclerosis Risk in Communities study). Am J Cardiol 2008; 101:1016–1022.
- Kalogeropoulos A, Georgiopoulou V, Kritchevsky SB, et al. Epidemiology of incident heart failure in a contemporary elderly cohort: the health, aging, and body composition study. Arch Intern Med 2009; 169:708–715.
- Dries DL, Exner DV, Gersh BJ, Cooper HA, Carson PE, Domanski MJ. Racial differences in the outcome of left ventricular dysfunction. N Engl J Med 1999; 340:609–616.
- Exner DV, Dries DL, Domanski MJ, Cohn JN. Lesser response to angiotensin-converting-enzyme inhibitor therapy in black as compared with white patients with left ventricular dysfunction. N Engl J Med 2001; 344:1351–1357.
- Bardy GH, Lee KL, Mark DB, et al; Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005; 352:225–237.
- Bibbins-Domingo K, Pletcher MJ, Lin F, et al. Racial differences in incident heart failure among young adults. N Engl J Med 2009; 360:1179–1190.
- Eaton CB, Abdulbaki AM, Margolis KL, et al. Racial and ethnic differences in incident hospitalized heart failure in postmenopausal women: the Women’s Health Initiative. Circulation 2012; 126:688–696.
- Ilksoy N, Hoffman M, Moore RH, Easley K, Jacobson TA. Comparison of African-American patients with systolic heart failure versus preserved ejection fraction. Am J Cardiol 2006; 98:806–808.
- Sharp A, Tapp R, Francis DP, et al. Ethnicity and left ventricular diastolic function in hypertension an ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial) substudy. J Am Coll Cardiol 2008; 52:1015–1021.
- Kizer JR, Arnett DK, Bella JN, et al. Differences in left ventricular structure between black and white hypertensive adults: the Hypertension Genetic Epidemiology Network study. Hypertension 2004; 43:1182–1188.
- Drazner MH, Dries DL, Peshock RM, et al. Left ventricular hypertrophy is more prevalent in blacks than whites in the general population: the Dallas Heart Study. Hypertension 2005; 46:124–129.
- East MA, Peterson ED, Shaw LK, Gattis WA, O’Connor CM. Racial differences in the outcomes of patients with diastolic heart failure. Am Heart J 2004; 148:151–156.
- Klapholz M, Maurer M, Lowe AM, et al; New York Heart Failure Consortium. Hospitalization for heart failure in the presence of a normal left ventricular ejection fraction: results of the New York Heart Failure Registry. J Am Coll Cardiol 2004; 43:1432–1438.
- Agoston I, Cameron CS, Yao D, Dela Rosa A, Mann DL, Deswal A. Comparison of outcomes of white versus black patients hospitalized with heart failure and preserved ejection fraction. Am J Cardiol 2004; 94:1003–1007.
- Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. US Carvedilol Heart Failure Study Group. N Engl J Med 1996; 334:1349–1355.
- Yancy CW, Strong M. The natural history, epidemiology, and prognosis of heart failure in African Americans. Congest Heart Fail 2004; 10:15–18.
- Velagaleti RS, Gona P, Larson MG, et al. Multimarker approach for the prediction of heart failure incidence in the community. Circulation 2010; 122:1700–1706.
- Deswal A, Petersen NJ, Urbauer DL, Wright SM, Beyth R. Racial variations in quality of care and outcomes in an ambulatory heart failure cohort. Am Heart J 2006; 152:348–354.
- Howard G, Prineas R, Moy C, et al. Racial and geographic differences in awareness, treatment, and control of hypertension: the REasons for Geographic And Racial Differences in Stroke study. Stroke 2006; 37:1171–1178.
- Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med 2005; 165:2098–2104.
- Okin PM, Kjeldsen SE, Dahlöf B, Devereux RB. Racial differences in incident heart failure during antihypertensive therapy. Circ Cardiovasc Qual Outcomes 2011; 4:157–164.
- Mulukutla SR, Venkitachalam L, Bambs C, et al. Black race is associated with digital artery endothelial dysfunction: results from the Heart SCORE study. Eur Heart J 2010; 31:2808–2815.
- Campia U, Choucair WK, Bryant MB, Waclawiw MA, Cardillo C, Panza JA. Reduced endothelium-dependent and -independent dilation of conductance arteries in African Americans. J Am Coll Cardiol 2002; 40:754–760.
- Perregaux D, Chaudhuri A, Rao S, et al. Brachial vascular reactivity in blacks. Hypertension 2000; 36:866–871.
- Duprez DA, Jacobs DR, Lutsey PL, et al. Race/ethnic and sex differences in large and small artery elasticity—results of the multiethnic study of atherosclerosis (MESA). Ethn Dis 2009; 19:243–250.
- Kalinowski L, Dobrucki IT, Malinski T. Race-specific differences in endothelial function: predisposition of African Americans to vascular diseases. Circulation 2004; 109:2511–2517.
- Kojda G, Harrison D. Interactions between NO and reactive oxygen species: pathophysiological importance in atherosclerosis, hypertension, diabetes and heart failure. Cardiovasc Res 1999; 43:562–571.
- Gattás GJ, Kato M, Soares-Vieira JA, et al. Ethnicity and glutathione S-transferase (GSTM1/GSTT1) polymorphisms in a Brazilian population. Braz J Med Biol Res 2004; 37:451–458.
- Li R, Lyn D, Lapu-Bula R, et al. Relation of endothelial nitric oxide synthase gene to plasma nitric oxide level, endothelial function, and blood pressure in African Americans. Am J Hypertens 2004; 17:560–567.
- Parra EJ, Marcini A, Akey J, et al. Estimating African American admixture proportions by use of population-specific alleles. Am J Hum Genet 1998; 63:1839–1851.
- Small KM, Wagoner LE, Levin AM, Kardia SL, Liggett SB. Synergistic polymorphisms of beta1- and alpha2C-adrenergic receptors and the risk of congestive heart failure. N Engl J Med 2002; 347:1135–1142.
- McNamara DM, Tam SW, Sabolinski ML, et al. Aldosterone synthase promoter polymorphism predicts outcome in African Americans with heart failure: results from the A-HeFT Trial. J Am Coll Cardiol 2006; 48:1277–1282.
- McNamara DM, Tam SW, Sabolinski ML, et al. Endothelial nitric oxide synthase (NOS3) polymorphisms in African Americans with heart failure: results from the A-HeFT trial. J Card Fail 2009; 15:191–198.
- Jacobson DR, Pastore RD, Yaghoubian R, et al. Variant-sequence transthyretin (isoleucine 122) in late-onset cardiac amyloidosis in black Americans. N Engl J Med 1997; 336:466–473.
- Buxbaum J, Alexander A, Koziol J, Tagoe C, Fox E, Kitzman D. Significance of the amyloidogenic transthyretin Val 122 Ile allele in African Americans in the Arteriosclerosis Risk in Communities (ARIC) and Cardiovascular Health (CHS) Studies. Am Heart J 2010; 159:864–870.
- Philbin EF, Dec GW, Jenkins PL, DiSalvo TG. Socioeconomic status as an independent risk factor for hospital readmission for heart failure. Am J Cardiol 2001; 87:1367–1371.
- Evangelista LS, Dracup K, Doering LV. Racial differences in treatment-seeking delays among heart failure patients. J Card Fail 2002; 8:381–386.
- Kressin NR, Orner MB, Manze M, Glickman ME, Berlowitz D. Understanding contributors to racial disparities in blood pressure control. Circ Cardiovasc Qual Outcomes 2010; 3:173–180.
- Yancy CW, Jessup M, Bozkurt B, et al; ACCF/AHA Task Force Members. 2013 ACCF/AHA guideline for the management of heart failure. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; 62:e147–e329.
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults. Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2013; doi: 10.1001/jama.2013.284427. E-pub ahead of print.
- Chobanian AV, Bakris GL, Black HR, et al; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42:1206–1252.
- Bibbins-Domingo K, Chertow GM, Coxson PG, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med 2010; 362:590–599.
- Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; published online Nov 13. DOI: 10.1016/j.jacc.2013.11.002.
- Casagrande SS, Whitt-Glover MC, Lancaster KJ, Odoms-Young AM, Gary TL. Built environment and health behaviors among African Americans: a systematic review. Am J Prev Med 2009; 36:174–181.
- Gustat J, Rice J, Parker KM, Becker AB, Farley TA. Effect of changes to the neighborhood built environment on physical activity in a low-income African American neighborhood. Prev Chronic Dis 2012; 9:E57.
- Casagrande SS, Franco M, Gittelsohn J, et al. Healthy food availability and the association with BMI in Baltimore, Maryland. Public Health Nutr 2011; 14:1001–1007.
- Stewart JE, Battersby SE, Lopez-De Fede A, Remington KC, Hardin JW, Mayfield-Smith K. Diabetes and the socioeconomic and built environment: geovisualization of disease prevalence and potential contextual associations using ring maps. Int J Health Geogr 2011; 10:18.
- Franciosa JA, Ferdinand KC, Yancy CW; Consensus Statement on Heart Failure in African Americans Writing Group. Treatment of heart failure in African Americans: a consensus statement. Congest Heart Fail 2010; 16:27–38.
- Ahmed A, Rich MW, Love TE, et al. Digoxin and reduction in mortality and hospitalization in heart failure: a comprehensive post hoc analysis of the DIG trial. Eur Heart J 2006; 27:178–186.
- Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure.The SOLVD Investigators. N Engl J Med 1991; 325:293–302.
- Shekelle PG, Rich MW, Morton SC, et al. Efficacy of angiotensin-converting enzyme inhibitors and beta-blockers in the management of left ventricular systolic dysfunction according to race, gender, and diabetic status: a meta-analysis of major clinical trials. J Am Coll Cardiol 2003; 41:1529–1538.
- Gibbs CR, Lip GY, Beevers DG. Angioedema due to ACE inhibitors: increased risk in patients of African origin. Br J Clin Pharmacol 1999; 48:861–865.
- Brown NJ, Ray WA, Snowden M, Griffin MR. Black Americans have an increased rate of angiotensin converting enzyme inhibitor-associated angioedema. Clin Pharmacol Ther 1996; 60:8–13.
- Beta-Blocker Evaluation of Survival Trial Investigators. A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure. N Engl J Med 2001; 344:1659–1667.
- Packer M, Coats AJ, Fowler MB, et al; Carvedilol Prospective Randomized Cumulative Survival Study Group. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001; 344:1651–1658.
- Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 1999; 353:2001–2007.
- Goldstein S, Deedwania P, Gottlieb S, Wikstrand J; MERIT-HF Study Group. Metoprolol CR/XL in black patients with heart failure (from the Metoprolol CR/XL randomized intervention trial in chronic heart failure). Am J Cardiol 2003; 92:478–480.
- Bristow MR, Murphy GA, Krause-Steinrauf H, et al. An alpha2C-adrenergic receptor polymorphism alters the norepinephrine-lowering effects and therapeutic response of the beta-blocker bucindolol in chronic heart failure. Circ Heart Fail 2010; 3:21–28.
- Bristow MR, Krause-Steinrauf H, Nuzzo R, et al. Effect of baseline or changes in adrenergic activity on clinical outcomes in the beta-blocker evaluation of survival trial. Circulation 2004; 110:1437–1442.
- Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med 1999; 341:709–717.
- Pitt B, Remme W, Zannad F, et al; Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study Investigators. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 2003; 348:1309–1321.
- Zannad F, McMurray JJ, Krum H, et al; EMPHASIS-HF Study Group. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med 2011; 364:11–21.
- Cavallari LH, Groo VL, Momary KM, Fontana D, Viana MA, Vaitkus P. Racial differences in potassium response to spironolactone in heart failure. Congest Heart Fail 2006; 12:200–205.
- Cohn JN, Johnson G, Ziesche S, et al. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med 1991; 325:303–310.
- Taylor AL, Ziesche S, Yancy C, et al; African-American Heart Failure Trial Investigators. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med 2004; 351:2049–2057.
- Anand IS, Tam SW, Rector TS, et al. Influence of blood pressure on the effectiveness of a fixed-dose combination of isosorbide dinitrate and hydralazine in the African-American Heart Failure Trial. J Am Coll Cardiol 2007; 49:32–39.
- Echols MR, Felker GM, Thomas KL, et al. Racial differences in the characteristics of patients admitted for acute decompensated heart failure and their relation to outcomes: results from the OPTIME-CHF trial. J Card Fail 2006; 12:684–688.
- Kamath SA, Drazner MH, Wynne J, Fonarow GC, Yancy CW. Characteristics and outcomes in African American patients with decompensated heart failure. Arch Intern Med 2008; 168:1152–1158.
- Felker GM, Lee KL, Bull DA, et al; NHLBI Heart Failure Clinical Research Network. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med 2011; 364:797–805.
- Costanzo MR, Guglin ME, Saltzberg MT, et al; UNLOAD Trial Investigators. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol 2007; 49:675–683.
- Bart BA, Goldsmith SR, Lee KL, et al; Heart Failure Clinical Research Network. Ultrafiltration in decompensated heart failure with cardiorenal syndrome. N Engl J Med 2012; 367:2296–2304.
- Levy P, Compton S, Welch R, et al. Treatment of severe decompensated heart failure with high-dose intravenous nitroglycerin: a feasibility and outcome analysis. Ann Emerg Med 2007; 50:144–152.
- Cleland JG, Daubert JC, Erdmann E, et al; Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 2005; 352:1539–1549.
- Young JB, Abraham WT, Smith AL, et al; Multicenter InSync ICD Randomized Clinical Evaluation (MIRACLE ICD) Trial Investigators. Combined cardiac resynchronization and implantable cardioversion defibrillation in advanced chronic heart failure: the MIRACLE ICD Trial. JAMA 2003; 289:2685–2694.
- Moss AJ, Zareba W, Hall WJ, et al; Multicenter Automatic Defibrillator Implantation Trial II Investigators. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002; 346:877–883.
- Bristow MR, Saxon LA, Boehmer J, et al; Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) Investigators. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med 2004; 350:2140–2150.
- Mitchell JE, Hellkamp AS, Mark DB, et al; SCD-HeFT Investigators. Outcome in African Americans and other minorities in the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT). Am Heart J 2008; 155:501–506.
- Hernandez AF, Fonarow GC, Liang L, et al. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. JAMA 2007; 298:1525–1532.
- Farmer SA, Kirkpatrick JN, Heidenreich PA, Curtis JP, Wang Y, Groeneveld PW. Ethnic and racial disparities in cardiac resynchronization therapy. Heart Rhythm 2009; 6:325–331.
- Colvin-Adams M, Smith JM, Heubner BM, et al. OPTN/SRTR 2011 Annual Data Report: heart. Am J Transplant 2013; 13(suppl 1):119–148.
- Allen JG, Weiss ES, Arnaoutakis GJ, et al. The impact of race on survival after heart transplantation: an analysis of more than 20,000 patients. Ann Thorac Surg 2010; 89:1956–1964.
- Liu V, Bhattacharya J, Weill D, Hlatky MA. Persistent racial disparities in survival after heart transplantation. Circulation 2011; 123:1642–1649.
- Mahle WT, Kanter KR, Vincent RN. Disparities in outcome for black patients after pediatric heart transplantation. J Pediatr 2005; 147:739–743.
- Park MH, Tolman DE, Kimball PM. Disproportionate HLA matching may contribute to racial disparity in patient survival following cardiac transplantation. Clin Transplant 1996; 10(6 Pt 2):625–628.
- Park MH, Tolman DE, Kimball PM. The impact of race and HLA matching on long-term survival following cardiac transplantation. Transplant Proc 1997; 29:1460–1463.
- Callender CO, Cherikh WS, Miles PV, et al. Blacks as donors for transplantation: suboptimal outcomes overcome by transplantation into other minorities. Transplant Proc 2008; 40:995–1000.
- King LP, Siminoff LA, Meyer DM, et al. Health insurance and cardiac transplantation: a call for reform. J Am Coll Cardiol 2005; 45:1388–1391.
- Ozminkowski RJ, White AJ, Hassol A, Murphy M. Minimizing racial disparity regarding receipt of a cadaver kidney transplant. Am J Kidney Dis 1997; 30:749–759.
- Aggarwal A, Gupta A, Pappas PS, Tatooles A, Bhat G. Racial differences in patients with left ventricular assist devices. ASAIO J 2012; 58:499–502.
- Tsiouris A, Brewer RJ, Borgi J, Nemeh H, Paone G, Morgan JA. Continuous-flow left ventricular assist device implantation as a bridge to transplantation or destination therapy: racial disparities in outcomes. J Heart Lung Transplant 2013; 32:299–304.
- Joyce DL, Conte JV, Russell SD, Joyce LD, Chang DC. Disparities in access to left ventricular assist device therapy. J Surg Res 2009; 152:111–117.
African Americans are disproportionately affected by heart failure and have not experienced the same benefit from treatment as white patients have. Much of the disparity can be blamed on modifiable risk factors such as uncontrolled hypertension and on suboptimal health care. When African Americans are treated according to guidelines, discrepant outcomes can be minimized.
In this article, we review the processes contributing to heart failure in African Americans, its management, and challenges with regard to disparities.
HEART FAILURE IS INCREASING
Despite 20 years of progress in understanding the pathophysiology of heart failure and developing medical and surgical therapies for it, its prevalence and associated morbidity are increasing in the United States. In 2010, 6.6 million (2.8%) of the adults in the United States had heart failure,1 and the prevalence is expected to increase by about 25% by 2030.
DISPARITIES IN INCIDENCE, OUTCOMES
Heart failure is more prevalent in African Americans than in whites, imposes higher rates of death and morbidity, and has a more malignant course.1–6
According to American Heart Association statistics, the annual incidence of heart failure in whites is approximately 6 per 1,000 person-years, while in African Americans it is 9.1 per 1,000 person-years.1 In the Atherosclerosis Risk in Communities study, the incidence of new heart failure was 1.0 per 1,000 person-years in Chinese Americans, 2.4 in whites, 3.5 in Hispanics, and 4.6 in African Americans.2
Moreover, when hospitalized for heart failure, African Americans have a 45% greater risk of death or decline in functional status than whites.7
Heart failure also occurs earlier in African Americans. Bibbins-Domingo et al8 reported that heart failure before age 50 was 20 times more frequent in African Americans than in whites. Functional and structural cardiac changes appeared an average of 10 years before the onset of symptoms and were strongly associated with the development of subsequent heart failure.8
In the Women’s Health Initiative, African American women had higher rates of heart failure than white women, perhaps in part because of higher rates of diabetes.9
Heart failure with preserved ejection fraction
About half of patients who have signs and symptoms of heart failure have a normal (“preserved”) ejection fraction. The incidence of this condition, previously called diastolic heart failure, appears to be similar between African Americans and whites. However, African Americans appear to have a greater incidence of factors that predispose to it and tend to present later in the course.10 For example, African Americans have higher left ventricular mass and wall thickness and a higher incidence of left ventricular hypertrophy than white patients.11–13 In addition, those with heart failure with preserved ejection fraction tend to be younger, female, more likely to have hypertension and diabetes, and less likely to have coronary artery disease, and tend to have worse renal function than their white counterparts.14,15 The predisposition to diastolic impairment persists even after adjusting for risk factors.11–15 The mortality rate in African Americans with heart failure with preserved ejection fraction and without coronary artery disease may also be higher than that of comparable white patients.16
WHY DO AFRICAN AMERICANS HAVE MORE HEART FAILURE?
Modifiable risk factors
In African Americans, the higher percentage of cases of heart failure is attributable to modifiable risk factors such as hypertension, hyperglycemia, left ventricular hypertrophy, and smoking, and fewer cases are due to ischemic heart disease.2,3 Nonischemic cardiomyopathy predominates in African Americans, whereas ischemic cardiomyopathy predominates in whites.
Hypertension, diabetes, obesity, and chronic kidney disease all portend subsequent heart failure and are common in African Americans, but hypertension is the main culprit.3,5,8,17–21 The prevalence of hypertension in African Americans is among the highest in the world, and because African Americans are more likely to have poorer control of their hypertension, they consequently have more target-organ damage.22 Indeed, in many hypertensive African Americans who develop heart failure, the hypertension is poorly controlled. However, even after adjusting for risk factors, and particularly blood pressure control, African Americans remain at higher risk of heart failure.23
The specific mechanistic links between hypertension and heart failure remain to be identified. Despite having a higher prevalence of left ventricular hypertrophy and left ventricular remodeling, African Americans with heart failure tend toward systolic heart failure, as opposed to heart failure with preserved ejection fraction.
Neurohormonal imbalances and endothelial dysfunction
Derangements in the renin-angiotensin-aldosterone and adrenergic axes are likely the main pathophysiologic mechanisms in the genesis of heart failure in all populations. However, other factors may underlie the enhanced disease burden in African Americans.
Impaired endothelial function, as evidenced by impaired digital and brachial artery vasomotion, is very common in African Americans.24–26 The small arteries of African Americans are less elastic than those of whites and Chinese.27 The underlying mechanism may be related to increased oxidative stress, decreased nitric oxide availability, exaggerated vasoconstrictor response, and attenuated responsiveness to vasodilators and nitric oxide.28–31
Genetic polymorphisms
An important caveat in discussing racial differences in heart failure is that “race” is completely arbitrary and is based on sociopolitical rather than scientific or physiologic definitions. Perceived genetic influences are likely to represent complex gene-gene, gene-environment, and gene-drug interactions.
This is especially true for African Americans, who are a markedly heterogeneous group. The US Office of Management and Budget defines “black” or “African American” as having origins in any of the black racial groups of Africa (www.census.gov/2010census/data). Thus, “African American” includes sixth-generation descendants of African slaves, recently immigrated Jamaicans, and black descendants of French and Spanish people.
Most African Americans have some European ancestry. In one study, the estimated proportion of European ancestry ranged from 7% in Jamaicans of African descent to approximately 23% in African Americans in New Orleans.32
Nevertheless, several polymorphisms associated with the risk of heart failure may provide insight into some of the “race-based” differences in pathophysiology and response to medications and, it is hoped, may eventually serve as the basis for tailored therapy. Genes of interest include those for:
- Beta 1 adrenergic receptor
- Alpha 2c receptor33
- Aldosterone synthase34
- G protein
- Transforming growth factor beta
- Nitric oxide synthase35
- Transthyrectin.36,37
Socioeconomic factors and quality of care
Heart failure patients—and especially African Americans—have high rates of hospital readmission, and socioeconomic factors have been implicated. In more than 40,000 patients with heart failure, lower income was a significant predictor of hospital readmission.38 Socioeconomic factors in turn could account for delay in seeking treatment for worsening symptoms, failure to recognize symptoms, limited disease awareness, inadequate access to health care, noncompliance with follow-up appointments, and poor adherence to recommended treatment, all of which are common in African American patients.38,39
African Americans also report more discrimination from health care providers, have more concerns about blood pressure medications, and are more likely to have misperceptions about high blood pressure (eg, that it is not serious), all of which may interfere with optimal blood pressure control.40 Managing heart failure in African Americans should include trying to identify and eliminate barriers to attaining treatment goals.
PREVENTING HEART FAILURE BY REDUCING RISK FACTORS
The American College of Cardiology Foundation and American Heart Association, in their 2013 guidelines, underscored the progressive nature of heart failure by defining four stages of the disease, from stage A (at risk) through stage D (refractory heart failure) (Figure 1).41 They also emphasized the importance of preventing it.
A thorough clinical assessment, with appropriate assessment for risk factors and intervention at stage A, is critical in preventing left ventricular remodeling and heart failure. These risk factors include hypertension, hyperlipidemia, atherosclerosis, diabetes mellitus, valvular disease, obesity, physical inactivity, excessive alcohol intake, poor diet, and smoking.
Hypertension is especially important in African Americans and requires vigorous screening and aggressive treatment. Antihypertensive drugs should be prescribed early, with a lower threshold for escalating therapy with combinations of drugs, as most patients require more than one.
There is considerable debate about the appropriate blood pressure thresholds for diagnosing hypertension and the optimal target blood pressures in African Americans. The 2014 report of the Joint National Committee recommends a similar hypertension treatment target of 140/90 mm Hg for all patients except older adults (for whom 150/90 mm Hg is acceptable), and no separate target for African Americans.42 Previous guidelines from this committee recommended thiazide-type diuretics as first-line therapy for hypertension in African Americans43; the new ones recommend thiazide-type diuretics or calcium channel blockers. However, in those with left ventricular systolic dysfunction, hypertension treatment should include drugs shown to reduce the risk of death in heart failure—ie, angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, hydralazine, nitrates, and aldosterone receptor antagonists.
Salt intake should be reduced to less than 3 g per day (1,200 mg of sodium per day), which has been shown to substantially reduce rates of cardiovascular morbidity and mortality and health care costs.44 Since most Americans consume 7 to 10 g of salt per day, strict salt restriction should be encouraged as a preventive measure.
Diabetes should be screened for and treated in African Americans per current American Diabetes Association guidelines.
Dyslipidemia should also be screened for and treated per guidelines.45
Smoking cessation, moderation of alcohol intake, and avoidance of illicit drugs should be encouraged. Given that African Americans develop heart failure at a relatively early age, the level of vigilance should be high and the threshold for screening should be low.
Healthy neighborhoods, healthy people
Neighborhoods can be designed and built with wellness in mind, incorporating features such as access to healthy food and walkability. Living in such neighborhoods leads to more physical activity and less obesity, although this relationship may be less robust in African Americans.46–49
Environmental factors are multifactorial in African Americans and extend beyond those afforded by the built environment. For instance, lack of safety may hinder the potential benefit of an otherwise walkable neighborhood. These interactions are highly complex, and more investigation is needed to determine the effect of built environments on risk factors in African Americans.
DRUG THERAPY FOR HEART FAILURE IN AFRICAN AMERICANS
Use standard therapies
ACE inhibitors, beta-blockers, and aldosterone antagonists are the standard of care in heart failure, with digoxin (Lanoxin) and diuretics used as adjuncts to control symptoms.
African Americans may respond differently than whites to some of these drugs (Table 1). However, these findings should be interpreted with caution, since most of them came from subgroup analyses of trials in which African Americans accounted for as many as 28% to as few as 1%.50 To date, no data unequivocally show that we should use standard heart failure therapies any differently in African Americans than in whites.
Digoxin: Limited role to control symptoms
Post hoc analysis of the Digitalis Investigation Group trial, in which 14% of the patients were nonwhite, revealed that compared with placebo, digitalis (and achieving a serum digitalis concentration of 0.5 to 0.9 ng/mL) was associated with lower rates of all-cause mortality in most subgroups—except nonwhites.51
In general, digoxin has a limited role in heart failure, since other drugs are available that substantially modify outcomes. However, it can be considered in patients who have persistent heart failure symptoms.
ACE inhibitors, ARBs are recommended
ACE inhibitors are recommended for patients with New York Heart Association (NYHA) class I, II, III, or IV heart failure (class I recommendation, ie, “recommended”; level of evidence A on a scale of A, B, and C) and as part of standard therapy for African American patients with heart failure with symptomatic or asymptomatic left ventricular systolic dysfunction (class I recommendation; level of evidence C).41
Although African American patients did not appear to derive any benefit from enalapril (Vasotec) in the Studies of Left Ventricular Dysfunction (SOLVD) trial,52 a subsequent analysis that involved the SOLVD Prevention Trial did not find any differences between African Americans and whites in response to this agent.6 Similarly, a meta-analysis did not suggest differences in ACE-inhibitor efficacy in reducing adverse cardiovascular outcomes in heart failure between African Americans and non–African Americans.53
Of note: African Americans have a 3% to 4% higher incidence of angioedema from ACE inhibitors than whites.54,55
Angiotensin receptor blockers (ARBs) can be used as substitute therapy in African Americans who cannot tolerate ACE inhibitors (class IIa recommendation, ie, “reasonable”; level of evidence B).41
Beta-blockers also recommended
Beta-blockers are recommended in NYHA class I, II, III, and IV heart failure (class I recommendation; level of evidence A) and as part of standard therapy for African Americans with heart failure due to symptomatic left ventricular systolic dysfunction (class I recommendation; level of evidence B) and asymptomatic left ventricular systolic dysfunction (level of evidence C).41
Carvedilol (Coreg) and metoprolol (Lopressor) are the standard beta-blockers used to treat heart failure, and these drugs should be used in African Americans as well as in whites.15,53,56–59 Of interest, however, race-specific differences may exist in the beta-adrenergic pathway.60,61
Aldosterone antagonists: More study needed
Aldosterone antagonists, also called mineralocorticoid antagonists, ie, spironolactone (Aldactone) and eplerenone (Inspra), are recommended in addition to beta-blockers and ACE inhibitors for NYHA class II–IV heart failure, unless contraindicated (class I recommendation; level of evidence A).
However, trials of aldosterone antagonists to date have enrolled few African Americans.62–64 The limited data suggest that African Americans with heart failure may be less responsive to the renal effects of spironolactone, demonstrating less of an increase in serum potassium levels, and there are essentially no data to guide the use of these drugs in African Americans with heart failure.65 Further study is needed. But in the absence of data to the contrary, these agents, should also be used in African American patients with class III or IV heart failure.
Hydralazine plus nitrates: Recommended for African Americans
Hydralazine plus isosorbide dinitrate (available as BiDil) is recommended as part of standard therapy, in addition to beta-blockers and ACE inhibitors specifically for African Americans with left ventricular systolic dysfunction and NYHA class III or IV heart failure (class I recommendation; level of evidence A), as well as NYHA class II heart failure (class I recommendation; level of evidence B).41
Preliminary evidence for this combination came from the Department of Veterans Affairs Cooperative Vasodilator-Heart Failure Trials.66
Subsequently, the African-American Heart Failure Trial67 was conducted in self-identified African American patients with NYHA class III or IV heart failure on standard heart failure therapy, including an ACE inhibitor if tolerated. Patients were randomly assigned to receive a fixed combination of isosorbide 20 mg and hydralazine 37.5 mg, one or two tablets three times a day, or placebo. The target dose of isosorbide dinitrate was 120 mg, and the target dose of hydralazine was 225 mg daily. Follow-up was up to 18 months. The study was terminated early because of a significant 43% improvement in overall survival for the patients in the isosorbide-hydralazine group. In addition, the rate of first hospitalization was 39% lower and the mean improvement in quality-of-life scores was 52% greater with isosorbide-hydralazine than with placebo.67
There has been much debate about whether the benefit seen in this trial was the result of a hemodynamic effect, blood pressure response, or neurohormonal modulation. The benefit is less likely from a reduction in blood pressure, as the patients who had low blood pressure derived a mortality benefit similar to those with higher blood pressure, despite no further reduction in their blood pressure.68
Treatment for heart failure with preserved ejection fraction
Although there are no data on how to manage heart failure with preserved ejection fraction that are specific to African Americans, the ACCF/AHA guideline41 recommends treating systolic and diastolic hypertension (class I, level of evidence B) according to published clinical practice guidelines and using diuretics to alleviate volume overload (class I; level of evidence C). Revascularization and management of atrial fibrillation are also “reasonable,” as are the use of ARBs, ACE inhibitors, and beta-blockers in the management of hypertension (class IIa; level of evidence C). ARBs may also be considered to reduce hospitalization in symptomatic patients with heart failure with preserved ejection fraction (class IIb, ie, “may be considered”; level of evidence B).
For acute decompensated heart failure
One of the greatest challenges in heart failure is treating patients who present with acute decompensated heart failure.
As in the general population, the major precipitating factor for hospitalization with decompensated heart failure in African Americans is nonadherence to prescribed dietary and medication regimens.35 African Americans with acute decompensated heart failure tend to be younger and to have nonischemic cardiomyopathy, hypertension, diabetes, and obesity, but a lower risk of death.35,69,70 Up to 44% have uncontrolled hypertension.35
Inotropes and vasodilators have undergone multiple trials in the acutely decompensated state in the general population, but no trial has demonstrated a reduction in the mortality rate, and some showed a higher mortality rate. Thus, the treatment of acute decompensated heart failure remains primarily consensus-guided and symptom-focused.
Loop diuretics have been the mainstay in managing fluid retention and congestion in heart failure. The Diuretic Optimization Strategies Evaluation trial tested low-dose vs high-dose intravenous furosemide (Lasix) given either as a continuous infusion or as intermittent intravenous boluses. All strategies were safe and effective.71
Although ultrafiltration is an effective method of decongestion in heart failure and has been associated with a reduction in hospitalization, it is also associated with worsening renal function.72 The Cardiorenal Rescue Study in Acute Decompensated Heart Failure73 compared ultrafiltration vs stepped diuretic therapy. In this trial, which enrolled approximately 26% nonwhites, stepped diuretic therapy was superior to ultrafiltration in preserving renal function in acute decompensated heart failure, although the efficacy of fluid removal was similar.
Both studies were small, and subgroup analyses are not likely to yield useful information. Nevertheless, these data support the use of intravenous diuretics, by continuous infusion or bolus, in acute decompensated heart failure.
Despite no benefit in terms of the mortality rate, inotropes continue to be used in some cases of acute decompensated heart failure, and African Americans appear to have a response to milrinone (Primacor IV) similar to that in whites.69
In a nonrandomized study in which most patients were black, high-dose intravenous nitroglycerin appeared to be safe and associated with less need for ventilator support and intensive care unit admission, compared retrospectively with a population that did not receive high-dose nitroglycerin.74
Given the different profile of the African American patient with acute decompensated heart failure, prospective studies would be useful in determining the best management strategy.
TREATMENTS FOR ADVANCED HEART FAILURE
Cardiac resynchronization and implantable cardioverter-defibrillators
Cardiac resynchronization therapy is indicated for patients with NYHA class II, III, and ambulatory class IV heart failure and left ventricular ejection fraction less than or equal to 35%, sinus rhythm, left bundle branch block, and a QRS duration greater than or equal to 150 ms (class I recommendation; level of evidence A for class NYHA III and IV; level of evidence B for NYHA class II).41
An implantable cardioverter-defibrillator is recommended in patients with NYHA class II or III heart failure for primary prevention of sudden cardiac death in selected patients with nonischemic dilated cardiomyopathy or ischemic heart disease (class I recommendation; level of evidence A).
However, few members of racial and ethnic minorities were included in trials of implantable cardioverter-defibrillators75,76 or cardiac resynchronization,7,77,78 so that subgroup analysis is limited. Use of an implantable cardioverter-defibrillator showed similar reduction in mortality between African Americans and whites, and compliance with device implantation and medical therapy was comparable.79
Among patients discharged from hospitals in the American Heart Association’s Get With the Guidelines–Heart Failure Quality Improvement Program, fewer than 40% of potentially eligible patients received an implantable cardioverter-defibrillator, and rates were significantly lower for African Americans.80 When they can get cardiac resynchronization therapy, African Americans appear to experience similar benefit from it.81
Heart transplantation: Poorer outcomes in African Americans?
Heart transplantation remains the most effective and durable therapy for advanced heart failure. Median survival approaches 14 years.82
However, a retrospective study found that African American recipients had an 11.5% lower 10-year survival rate than whites, which persisted after adjusting for risk, donor-recipient matching by race, and censoring of deaths in the first year.83 Although socioeconomic factors and poor human leukocyte antigen matching have been implicated, a retrospective cohort study showed that African American recipients had a higher risk of death than white recipients even after adjustment for recipient, transplant, and socioeconomic factors.84–87 African Americans were more likely to die of graft failure or of a cardiovascular cause than white patients, but were less likely to die of infection or malignancy. Although mortality rates decreased over time for all transplant recipients, the disparity in mortality rates between African Americans and whites remained essentially unchanged.84
Among all donor-recipient combinations, African American recipients of hearts from African American donors had the highest risk of death.88
Limited access to transplantation persists, particularly for African Americans of lower socioeconomic status. African Americans are more likely than whites to be uninsured, and the funding requirement to be placed on the transplantation list disproportionately affects African Americans.89,90
Left-ventricular assist devices
Left-ventricular assist devices (LVADs) improve survival in heart transplantation candidates and heart failure patients who do not qualify for transplantation. After LVAD implantation, African American patients have similar 1- and 2-year survival rates and no difference in readmission rates compared with whites.91,92
Access to LVAD implantation, however, is significantly influenced by race, and African Americans are significantly less likely to receive one (OR = 0.29).93 Further investigation is required to identify disparities in outcome, access, and contributing factors.
DISPARITIES CAN BE MINIMIZED
In general, heart failure in African Americans is characterized by a high prevalence of hypertension as a major risk factor and potentially different pathogenesis than in the general population. Furthermore, heart failure in African Americans is more prevalent, occurs at an early age, and has a more severe course than in whites, perhaps because of a higher prevalence of risk factors such as diabetes mellitus, obesity, and again, hypertension. These disparities are multifactorial and involve a complex interplay between genes, environment, and socioeconomic factors.
For now, heart failure in African Americans should be treated according to standard evidenced-based strategies, which include a combination of isosorbide dinitrate and hydralazine in addition to other neurohormonal modifying agents (ACE inhibitors, beta-blockers, aldosterone antagonists), a strategy demonstrated to reduce mortality rates in African Americans. When treated according to guidelines, disparities in outcomes can be minimized.
However, many questions about managing heart failure remain unanswered, since African Americans have been markedly underrepresented in clinical trials. Clinical trials need to enroll enough African Americans to answer the questions of interest. Disparities in outcomes must be investigated in a scientific and hypothesis-driven manner. The effect of the built environment on African Americans needs more study as well, as success with these strategies may be impeded by unrecognized factors.
Preventing heart failure should be a priority. Efforts should be directed toward detecting and modifying risk factors early, managing hypertension aggressively, and identifying left ventricular dysfunction early.
African Americans are disproportionately affected by heart failure and have not experienced the same benefit from treatment as white patients have. Much of the disparity can be blamed on modifiable risk factors such as uncontrolled hypertension and on suboptimal health care. When African Americans are treated according to guidelines, discrepant outcomes can be minimized.
In this article, we review the processes contributing to heart failure in African Americans, its management, and challenges with regard to disparities.
HEART FAILURE IS INCREASING
Despite 20 years of progress in understanding the pathophysiology of heart failure and developing medical and surgical therapies for it, its prevalence and associated morbidity are increasing in the United States. In 2010, 6.6 million (2.8%) of the adults in the United States had heart failure,1 and the prevalence is expected to increase by about 25% by 2030.
DISPARITIES IN INCIDENCE, OUTCOMES
Heart failure is more prevalent in African Americans than in whites, imposes higher rates of death and morbidity, and has a more malignant course.1–6
According to American Heart Association statistics, the annual incidence of heart failure in whites is approximately 6 per 1,000 person-years, while in African Americans it is 9.1 per 1,000 person-years.1 In the Atherosclerosis Risk in Communities study, the incidence of new heart failure was 1.0 per 1,000 person-years in Chinese Americans, 2.4 in whites, 3.5 in Hispanics, and 4.6 in African Americans.2
Moreover, when hospitalized for heart failure, African Americans have a 45% greater risk of death or decline in functional status than whites.7
Heart failure also occurs earlier in African Americans. Bibbins-Domingo et al8 reported that heart failure before age 50 was 20 times more frequent in African Americans than in whites. Functional and structural cardiac changes appeared an average of 10 years before the onset of symptoms and were strongly associated with the development of subsequent heart failure.8
In the Women’s Health Initiative, African American women had higher rates of heart failure than white women, perhaps in part because of higher rates of diabetes.9
Heart failure with preserved ejection fraction
About half of patients who have signs and symptoms of heart failure have a normal (“preserved”) ejection fraction. The incidence of this condition, previously called diastolic heart failure, appears to be similar between African Americans and whites. However, African Americans appear to have a greater incidence of factors that predispose to it and tend to present later in the course.10 For example, African Americans have higher left ventricular mass and wall thickness and a higher incidence of left ventricular hypertrophy than white patients.11–13 In addition, those with heart failure with preserved ejection fraction tend to be younger, female, more likely to have hypertension and diabetes, and less likely to have coronary artery disease, and tend to have worse renal function than their white counterparts.14,15 The predisposition to diastolic impairment persists even after adjusting for risk factors.11–15 The mortality rate in African Americans with heart failure with preserved ejection fraction and without coronary artery disease may also be higher than that of comparable white patients.16
WHY DO AFRICAN AMERICANS HAVE MORE HEART FAILURE?
Modifiable risk factors
In African Americans, the higher percentage of cases of heart failure is attributable to modifiable risk factors such as hypertension, hyperglycemia, left ventricular hypertrophy, and smoking, and fewer cases are due to ischemic heart disease.2,3 Nonischemic cardiomyopathy predominates in African Americans, whereas ischemic cardiomyopathy predominates in whites.
Hypertension, diabetes, obesity, and chronic kidney disease all portend subsequent heart failure and are common in African Americans, but hypertension is the main culprit.3,5,8,17–21 The prevalence of hypertension in African Americans is among the highest in the world, and because African Americans are more likely to have poorer control of their hypertension, they consequently have more target-organ damage.22 Indeed, in many hypertensive African Americans who develop heart failure, the hypertension is poorly controlled. However, even after adjusting for risk factors, and particularly blood pressure control, African Americans remain at higher risk of heart failure.23
The specific mechanistic links between hypertension and heart failure remain to be identified. Despite having a higher prevalence of left ventricular hypertrophy and left ventricular remodeling, African Americans with heart failure tend toward systolic heart failure, as opposed to heart failure with preserved ejection fraction.
Neurohormonal imbalances and endothelial dysfunction
Derangements in the renin-angiotensin-aldosterone and adrenergic axes are likely the main pathophysiologic mechanisms in the genesis of heart failure in all populations. However, other factors may underlie the enhanced disease burden in African Americans.
Impaired endothelial function, as evidenced by impaired digital and brachial artery vasomotion, is very common in African Americans.24–26 The small arteries of African Americans are less elastic than those of whites and Chinese.27 The underlying mechanism may be related to increased oxidative stress, decreased nitric oxide availability, exaggerated vasoconstrictor response, and attenuated responsiveness to vasodilators and nitric oxide.28–31
Genetic polymorphisms
An important caveat in discussing racial differences in heart failure is that “race” is completely arbitrary and is based on sociopolitical rather than scientific or physiologic definitions. Perceived genetic influences are likely to represent complex gene-gene, gene-environment, and gene-drug interactions.
This is especially true for African Americans, who are a markedly heterogeneous group. The US Office of Management and Budget defines “black” or “African American” as having origins in any of the black racial groups of Africa (www.census.gov/2010census/data). Thus, “African American” includes sixth-generation descendants of African slaves, recently immigrated Jamaicans, and black descendants of French and Spanish people.
Most African Americans have some European ancestry. In one study, the estimated proportion of European ancestry ranged from 7% in Jamaicans of African descent to approximately 23% in African Americans in New Orleans.32
Nevertheless, several polymorphisms associated with the risk of heart failure may provide insight into some of the “race-based” differences in pathophysiology and response to medications and, it is hoped, may eventually serve as the basis for tailored therapy. Genes of interest include those for:
- Beta 1 adrenergic receptor
- Alpha 2c receptor33
- Aldosterone synthase34
- G protein
- Transforming growth factor beta
- Nitric oxide synthase35
- Transthyrectin.36,37
Socioeconomic factors and quality of care
Heart failure patients—and especially African Americans—have high rates of hospital readmission, and socioeconomic factors have been implicated. In more than 40,000 patients with heart failure, lower income was a significant predictor of hospital readmission.38 Socioeconomic factors in turn could account for delay in seeking treatment for worsening symptoms, failure to recognize symptoms, limited disease awareness, inadequate access to health care, noncompliance with follow-up appointments, and poor adherence to recommended treatment, all of which are common in African American patients.38,39
African Americans also report more discrimination from health care providers, have more concerns about blood pressure medications, and are more likely to have misperceptions about high blood pressure (eg, that it is not serious), all of which may interfere with optimal blood pressure control.40 Managing heart failure in African Americans should include trying to identify and eliminate barriers to attaining treatment goals.
PREVENTING HEART FAILURE BY REDUCING RISK FACTORS
The American College of Cardiology Foundation and American Heart Association, in their 2013 guidelines, underscored the progressive nature of heart failure by defining four stages of the disease, from stage A (at risk) through stage D (refractory heart failure) (Figure 1).41 They also emphasized the importance of preventing it.
A thorough clinical assessment, with appropriate assessment for risk factors and intervention at stage A, is critical in preventing left ventricular remodeling and heart failure. These risk factors include hypertension, hyperlipidemia, atherosclerosis, diabetes mellitus, valvular disease, obesity, physical inactivity, excessive alcohol intake, poor diet, and smoking.
Hypertension is especially important in African Americans and requires vigorous screening and aggressive treatment. Antihypertensive drugs should be prescribed early, with a lower threshold for escalating therapy with combinations of drugs, as most patients require more than one.
There is considerable debate about the appropriate blood pressure thresholds for diagnosing hypertension and the optimal target blood pressures in African Americans. The 2014 report of the Joint National Committee recommends a similar hypertension treatment target of 140/90 mm Hg for all patients except older adults (for whom 150/90 mm Hg is acceptable), and no separate target for African Americans.42 Previous guidelines from this committee recommended thiazide-type diuretics as first-line therapy for hypertension in African Americans43; the new ones recommend thiazide-type diuretics or calcium channel blockers. However, in those with left ventricular systolic dysfunction, hypertension treatment should include drugs shown to reduce the risk of death in heart failure—ie, angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, hydralazine, nitrates, and aldosterone receptor antagonists.
Salt intake should be reduced to less than 3 g per day (1,200 mg of sodium per day), which has been shown to substantially reduce rates of cardiovascular morbidity and mortality and health care costs.44 Since most Americans consume 7 to 10 g of salt per day, strict salt restriction should be encouraged as a preventive measure.
Diabetes should be screened for and treated in African Americans per current American Diabetes Association guidelines.
Dyslipidemia should also be screened for and treated per guidelines.45
Smoking cessation, moderation of alcohol intake, and avoidance of illicit drugs should be encouraged. Given that African Americans develop heart failure at a relatively early age, the level of vigilance should be high and the threshold for screening should be low.
Healthy neighborhoods, healthy people
Neighborhoods can be designed and built with wellness in mind, incorporating features such as access to healthy food and walkability. Living in such neighborhoods leads to more physical activity and less obesity, although this relationship may be less robust in African Americans.46–49
Environmental factors are multifactorial in African Americans and extend beyond those afforded by the built environment. For instance, lack of safety may hinder the potential benefit of an otherwise walkable neighborhood. These interactions are highly complex, and more investigation is needed to determine the effect of built environments on risk factors in African Americans.
DRUG THERAPY FOR HEART FAILURE IN AFRICAN AMERICANS
Use standard therapies
ACE inhibitors, beta-blockers, and aldosterone antagonists are the standard of care in heart failure, with digoxin (Lanoxin) and diuretics used as adjuncts to control symptoms.
African Americans may respond differently than whites to some of these drugs (Table 1). However, these findings should be interpreted with caution, since most of them came from subgroup analyses of trials in which African Americans accounted for as many as 28% to as few as 1%.50 To date, no data unequivocally show that we should use standard heart failure therapies any differently in African Americans than in whites.
Digoxin: Limited role to control symptoms
Post hoc analysis of the Digitalis Investigation Group trial, in which 14% of the patients were nonwhite, revealed that compared with placebo, digitalis (and achieving a serum digitalis concentration of 0.5 to 0.9 ng/mL) was associated with lower rates of all-cause mortality in most subgroups—except nonwhites.51
In general, digoxin has a limited role in heart failure, since other drugs are available that substantially modify outcomes. However, it can be considered in patients who have persistent heart failure symptoms.
ACE inhibitors, ARBs are recommended
ACE inhibitors are recommended for patients with New York Heart Association (NYHA) class I, II, III, or IV heart failure (class I recommendation, ie, “recommended”; level of evidence A on a scale of A, B, and C) and as part of standard therapy for African American patients with heart failure with symptomatic or asymptomatic left ventricular systolic dysfunction (class I recommendation; level of evidence C).41
Although African American patients did not appear to derive any benefit from enalapril (Vasotec) in the Studies of Left Ventricular Dysfunction (SOLVD) trial,52 a subsequent analysis that involved the SOLVD Prevention Trial did not find any differences between African Americans and whites in response to this agent.6 Similarly, a meta-analysis did not suggest differences in ACE-inhibitor efficacy in reducing adverse cardiovascular outcomes in heart failure between African Americans and non–African Americans.53
Of note: African Americans have a 3% to 4% higher incidence of angioedema from ACE inhibitors than whites.54,55
Angiotensin receptor blockers (ARBs) can be used as substitute therapy in African Americans who cannot tolerate ACE inhibitors (class IIa recommendation, ie, “reasonable”; level of evidence B).41
Beta-blockers also recommended
Beta-blockers are recommended in NYHA class I, II, III, and IV heart failure (class I recommendation; level of evidence A) and as part of standard therapy for African Americans with heart failure due to symptomatic left ventricular systolic dysfunction (class I recommendation; level of evidence B) and asymptomatic left ventricular systolic dysfunction (level of evidence C).41
Carvedilol (Coreg) and metoprolol (Lopressor) are the standard beta-blockers used to treat heart failure, and these drugs should be used in African Americans as well as in whites.15,53,56–59 Of interest, however, race-specific differences may exist in the beta-adrenergic pathway.60,61
Aldosterone antagonists: More study needed
Aldosterone antagonists, also called mineralocorticoid antagonists, ie, spironolactone (Aldactone) and eplerenone (Inspra), are recommended in addition to beta-blockers and ACE inhibitors for NYHA class II–IV heart failure, unless contraindicated (class I recommendation; level of evidence A).
However, trials of aldosterone antagonists to date have enrolled few African Americans.62–64 The limited data suggest that African Americans with heart failure may be less responsive to the renal effects of spironolactone, demonstrating less of an increase in serum potassium levels, and there are essentially no data to guide the use of these drugs in African Americans with heart failure.65 Further study is needed. But in the absence of data to the contrary, these agents, should also be used in African American patients with class III or IV heart failure.
Hydralazine plus nitrates: Recommended for African Americans
Hydralazine plus isosorbide dinitrate (available as BiDil) is recommended as part of standard therapy, in addition to beta-blockers and ACE inhibitors specifically for African Americans with left ventricular systolic dysfunction and NYHA class III or IV heart failure (class I recommendation; level of evidence A), as well as NYHA class II heart failure (class I recommendation; level of evidence B).41
Preliminary evidence for this combination came from the Department of Veterans Affairs Cooperative Vasodilator-Heart Failure Trials.66
Subsequently, the African-American Heart Failure Trial67 was conducted in self-identified African American patients with NYHA class III or IV heart failure on standard heart failure therapy, including an ACE inhibitor if tolerated. Patients were randomly assigned to receive a fixed combination of isosorbide 20 mg and hydralazine 37.5 mg, one or two tablets three times a day, or placebo. The target dose of isosorbide dinitrate was 120 mg, and the target dose of hydralazine was 225 mg daily. Follow-up was up to 18 months. The study was terminated early because of a significant 43% improvement in overall survival for the patients in the isosorbide-hydralazine group. In addition, the rate of first hospitalization was 39% lower and the mean improvement in quality-of-life scores was 52% greater with isosorbide-hydralazine than with placebo.67
There has been much debate about whether the benefit seen in this trial was the result of a hemodynamic effect, blood pressure response, or neurohormonal modulation. The benefit is less likely from a reduction in blood pressure, as the patients who had low blood pressure derived a mortality benefit similar to those with higher blood pressure, despite no further reduction in their blood pressure.68
Treatment for heart failure with preserved ejection fraction
Although there are no data on how to manage heart failure with preserved ejection fraction that are specific to African Americans, the ACCF/AHA guideline41 recommends treating systolic and diastolic hypertension (class I, level of evidence B) according to published clinical practice guidelines and using diuretics to alleviate volume overload (class I; level of evidence C). Revascularization and management of atrial fibrillation are also “reasonable,” as are the use of ARBs, ACE inhibitors, and beta-blockers in the management of hypertension (class IIa; level of evidence C). ARBs may also be considered to reduce hospitalization in symptomatic patients with heart failure with preserved ejection fraction (class IIb, ie, “may be considered”; level of evidence B).
For acute decompensated heart failure
One of the greatest challenges in heart failure is treating patients who present with acute decompensated heart failure.
As in the general population, the major precipitating factor for hospitalization with decompensated heart failure in African Americans is nonadherence to prescribed dietary and medication regimens.35 African Americans with acute decompensated heart failure tend to be younger and to have nonischemic cardiomyopathy, hypertension, diabetes, and obesity, but a lower risk of death.35,69,70 Up to 44% have uncontrolled hypertension.35
Inotropes and vasodilators have undergone multiple trials in the acutely decompensated state in the general population, but no trial has demonstrated a reduction in the mortality rate, and some showed a higher mortality rate. Thus, the treatment of acute decompensated heart failure remains primarily consensus-guided and symptom-focused.
Loop diuretics have been the mainstay in managing fluid retention and congestion in heart failure. The Diuretic Optimization Strategies Evaluation trial tested low-dose vs high-dose intravenous furosemide (Lasix) given either as a continuous infusion or as intermittent intravenous boluses. All strategies were safe and effective.71
Although ultrafiltration is an effective method of decongestion in heart failure and has been associated with a reduction in hospitalization, it is also associated with worsening renal function.72 The Cardiorenal Rescue Study in Acute Decompensated Heart Failure73 compared ultrafiltration vs stepped diuretic therapy. In this trial, which enrolled approximately 26% nonwhites, stepped diuretic therapy was superior to ultrafiltration in preserving renal function in acute decompensated heart failure, although the efficacy of fluid removal was similar.
Both studies were small, and subgroup analyses are not likely to yield useful information. Nevertheless, these data support the use of intravenous diuretics, by continuous infusion or bolus, in acute decompensated heart failure.
Despite no benefit in terms of the mortality rate, inotropes continue to be used in some cases of acute decompensated heart failure, and African Americans appear to have a response to milrinone (Primacor IV) similar to that in whites.69
In a nonrandomized study in which most patients were black, high-dose intravenous nitroglycerin appeared to be safe and associated with less need for ventilator support and intensive care unit admission, compared retrospectively with a population that did not receive high-dose nitroglycerin.74
Given the different profile of the African American patient with acute decompensated heart failure, prospective studies would be useful in determining the best management strategy.
TREATMENTS FOR ADVANCED HEART FAILURE
Cardiac resynchronization and implantable cardioverter-defibrillators
Cardiac resynchronization therapy is indicated for patients with NYHA class II, III, and ambulatory class IV heart failure and left ventricular ejection fraction less than or equal to 35%, sinus rhythm, left bundle branch block, and a QRS duration greater than or equal to 150 ms (class I recommendation; level of evidence A for class NYHA III and IV; level of evidence B for NYHA class II).41
An implantable cardioverter-defibrillator is recommended in patients with NYHA class II or III heart failure for primary prevention of sudden cardiac death in selected patients with nonischemic dilated cardiomyopathy or ischemic heart disease (class I recommendation; level of evidence A).
However, few members of racial and ethnic minorities were included in trials of implantable cardioverter-defibrillators75,76 or cardiac resynchronization,7,77,78 so that subgroup analysis is limited. Use of an implantable cardioverter-defibrillator showed similar reduction in mortality between African Americans and whites, and compliance with device implantation and medical therapy was comparable.79
Among patients discharged from hospitals in the American Heart Association’s Get With the Guidelines–Heart Failure Quality Improvement Program, fewer than 40% of potentially eligible patients received an implantable cardioverter-defibrillator, and rates were significantly lower for African Americans.80 When they can get cardiac resynchronization therapy, African Americans appear to experience similar benefit from it.81
Heart transplantation: Poorer outcomes in African Americans?
Heart transplantation remains the most effective and durable therapy for advanced heart failure. Median survival approaches 14 years.82
However, a retrospective study found that African American recipients had an 11.5% lower 10-year survival rate than whites, which persisted after adjusting for risk, donor-recipient matching by race, and censoring of deaths in the first year.83 Although socioeconomic factors and poor human leukocyte antigen matching have been implicated, a retrospective cohort study showed that African American recipients had a higher risk of death than white recipients even after adjustment for recipient, transplant, and socioeconomic factors.84–87 African Americans were more likely to die of graft failure or of a cardiovascular cause than white patients, but were less likely to die of infection or malignancy. Although mortality rates decreased over time for all transplant recipients, the disparity in mortality rates between African Americans and whites remained essentially unchanged.84
Among all donor-recipient combinations, African American recipients of hearts from African American donors had the highest risk of death.88
Limited access to transplantation persists, particularly for African Americans of lower socioeconomic status. African Americans are more likely than whites to be uninsured, and the funding requirement to be placed on the transplantation list disproportionately affects African Americans.89,90
Left-ventricular assist devices
Left-ventricular assist devices (LVADs) improve survival in heart transplantation candidates and heart failure patients who do not qualify for transplantation. After LVAD implantation, African American patients have similar 1- and 2-year survival rates and no difference in readmission rates compared with whites.91,92
Access to LVAD implantation, however, is significantly influenced by race, and African Americans are significantly less likely to receive one (OR = 0.29).93 Further investigation is required to identify disparities in outcome, access, and contributing factors.
DISPARITIES CAN BE MINIMIZED
In general, heart failure in African Americans is characterized by a high prevalence of hypertension as a major risk factor and potentially different pathogenesis than in the general population. Furthermore, heart failure in African Americans is more prevalent, occurs at an early age, and has a more severe course than in whites, perhaps because of a higher prevalence of risk factors such as diabetes mellitus, obesity, and again, hypertension. These disparities are multifactorial and involve a complex interplay between genes, environment, and socioeconomic factors.
For now, heart failure in African Americans should be treated according to standard evidenced-based strategies, which include a combination of isosorbide dinitrate and hydralazine in addition to other neurohormonal modifying agents (ACE inhibitors, beta-blockers, aldosterone antagonists), a strategy demonstrated to reduce mortality rates in African Americans. When treated according to guidelines, disparities in outcomes can be minimized.
However, many questions about managing heart failure remain unanswered, since African Americans have been markedly underrepresented in clinical trials. Clinical trials need to enroll enough African Americans to answer the questions of interest. Disparities in outcomes must be investigated in a scientific and hypothesis-driven manner. The effect of the built environment on African Americans needs more study as well, as success with these strategies may be impeded by unrecognized factors.
Preventing heart failure should be a priority. Efforts should be directed toward detecting and modifying risk factors early, managing hypertension aggressively, and identifying left ventricular dysfunction early.
- Go AS, Mozaffarian D, Roger VL, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation 2013; 127:e6–e245.
- Bahrami H, Kronmal R, Bluemke DA, et al. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med 2008; 168:2138–2145.
- Loehr LR, Rosamond WD, Chang PP, Folsom AR, Chambless LE. Heart failure incidence and survival (from the Atherosclerosis Risk in Communities study). Am J Cardiol 2008; 101:1016–1022.
- Kalogeropoulos A, Georgiopoulou V, Kritchevsky SB, et al. Epidemiology of incident heart failure in a contemporary elderly cohort: the health, aging, and body composition study. Arch Intern Med 2009; 169:708–715.
- Dries DL, Exner DV, Gersh BJ, Cooper HA, Carson PE, Domanski MJ. Racial differences in the outcome of left ventricular dysfunction. N Engl J Med 1999; 340:609–616.
- Exner DV, Dries DL, Domanski MJ, Cohn JN. Lesser response to angiotensin-converting-enzyme inhibitor therapy in black as compared with white patients with left ventricular dysfunction. N Engl J Med 2001; 344:1351–1357.
- Bardy GH, Lee KL, Mark DB, et al; Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005; 352:225–237.
- Bibbins-Domingo K, Pletcher MJ, Lin F, et al. Racial differences in incident heart failure among young adults. N Engl J Med 2009; 360:1179–1190.
- Eaton CB, Abdulbaki AM, Margolis KL, et al. Racial and ethnic differences in incident hospitalized heart failure in postmenopausal women: the Women’s Health Initiative. Circulation 2012; 126:688–696.
- Ilksoy N, Hoffman M, Moore RH, Easley K, Jacobson TA. Comparison of African-American patients with systolic heart failure versus preserved ejection fraction. Am J Cardiol 2006; 98:806–808.
- Sharp A, Tapp R, Francis DP, et al. Ethnicity and left ventricular diastolic function in hypertension an ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial) substudy. J Am Coll Cardiol 2008; 52:1015–1021.
- Kizer JR, Arnett DK, Bella JN, et al. Differences in left ventricular structure between black and white hypertensive adults: the Hypertension Genetic Epidemiology Network study. Hypertension 2004; 43:1182–1188.
- Drazner MH, Dries DL, Peshock RM, et al. Left ventricular hypertrophy is more prevalent in blacks than whites in the general population: the Dallas Heart Study. Hypertension 2005; 46:124–129.
- East MA, Peterson ED, Shaw LK, Gattis WA, O’Connor CM. Racial differences in the outcomes of patients with diastolic heart failure. Am Heart J 2004; 148:151–156.
- Klapholz M, Maurer M, Lowe AM, et al; New York Heart Failure Consortium. Hospitalization for heart failure in the presence of a normal left ventricular ejection fraction: results of the New York Heart Failure Registry. J Am Coll Cardiol 2004; 43:1432–1438.
- Agoston I, Cameron CS, Yao D, Dela Rosa A, Mann DL, Deswal A. Comparison of outcomes of white versus black patients hospitalized with heart failure and preserved ejection fraction. Am J Cardiol 2004; 94:1003–1007.
- Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. US Carvedilol Heart Failure Study Group. N Engl J Med 1996; 334:1349–1355.
- Yancy CW, Strong M. The natural history, epidemiology, and prognosis of heart failure in African Americans. Congest Heart Fail 2004; 10:15–18.
- Velagaleti RS, Gona P, Larson MG, et al. Multimarker approach for the prediction of heart failure incidence in the community. Circulation 2010; 122:1700–1706.
- Deswal A, Petersen NJ, Urbauer DL, Wright SM, Beyth R. Racial variations in quality of care and outcomes in an ambulatory heart failure cohort. Am Heart J 2006; 152:348–354.
- Howard G, Prineas R, Moy C, et al. Racial and geographic differences in awareness, treatment, and control of hypertension: the REasons for Geographic And Racial Differences in Stroke study. Stroke 2006; 37:1171–1178.
- Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med 2005; 165:2098–2104.
- Okin PM, Kjeldsen SE, Dahlöf B, Devereux RB. Racial differences in incident heart failure during antihypertensive therapy. Circ Cardiovasc Qual Outcomes 2011; 4:157–164.
- Mulukutla SR, Venkitachalam L, Bambs C, et al. Black race is associated with digital artery endothelial dysfunction: results from the Heart SCORE study. Eur Heart J 2010; 31:2808–2815.
- Campia U, Choucair WK, Bryant MB, Waclawiw MA, Cardillo C, Panza JA. Reduced endothelium-dependent and -independent dilation of conductance arteries in African Americans. J Am Coll Cardiol 2002; 40:754–760.
- Perregaux D, Chaudhuri A, Rao S, et al. Brachial vascular reactivity in blacks. Hypertension 2000; 36:866–871.
- Duprez DA, Jacobs DR, Lutsey PL, et al. Race/ethnic and sex differences in large and small artery elasticity—results of the multiethnic study of atherosclerosis (MESA). Ethn Dis 2009; 19:243–250.
- Kalinowski L, Dobrucki IT, Malinski T. Race-specific differences in endothelial function: predisposition of African Americans to vascular diseases. Circulation 2004; 109:2511–2517.
- Kojda G, Harrison D. Interactions between NO and reactive oxygen species: pathophysiological importance in atherosclerosis, hypertension, diabetes and heart failure. Cardiovasc Res 1999; 43:562–571.
- Gattás GJ, Kato M, Soares-Vieira JA, et al. Ethnicity and glutathione S-transferase (GSTM1/GSTT1) polymorphisms in a Brazilian population. Braz J Med Biol Res 2004; 37:451–458.
- Li R, Lyn D, Lapu-Bula R, et al. Relation of endothelial nitric oxide synthase gene to plasma nitric oxide level, endothelial function, and blood pressure in African Americans. Am J Hypertens 2004; 17:560–567.
- Parra EJ, Marcini A, Akey J, et al. Estimating African American admixture proportions by use of population-specific alleles. Am J Hum Genet 1998; 63:1839–1851.
- Small KM, Wagoner LE, Levin AM, Kardia SL, Liggett SB. Synergistic polymorphisms of beta1- and alpha2C-adrenergic receptors and the risk of congestive heart failure. N Engl J Med 2002; 347:1135–1142.
- McNamara DM, Tam SW, Sabolinski ML, et al. Aldosterone synthase promoter polymorphism predicts outcome in African Americans with heart failure: results from the A-HeFT Trial. J Am Coll Cardiol 2006; 48:1277–1282.
- McNamara DM, Tam SW, Sabolinski ML, et al. Endothelial nitric oxide synthase (NOS3) polymorphisms in African Americans with heart failure: results from the A-HeFT trial. J Card Fail 2009; 15:191–198.
- Jacobson DR, Pastore RD, Yaghoubian R, et al. Variant-sequence transthyretin (isoleucine 122) in late-onset cardiac amyloidosis in black Americans. N Engl J Med 1997; 336:466–473.
- Buxbaum J, Alexander A, Koziol J, Tagoe C, Fox E, Kitzman D. Significance of the amyloidogenic transthyretin Val 122 Ile allele in African Americans in the Arteriosclerosis Risk in Communities (ARIC) and Cardiovascular Health (CHS) Studies. Am Heart J 2010; 159:864–870.
- Philbin EF, Dec GW, Jenkins PL, DiSalvo TG. Socioeconomic status as an independent risk factor for hospital readmission for heart failure. Am J Cardiol 2001; 87:1367–1371.
- Evangelista LS, Dracup K, Doering LV. Racial differences in treatment-seeking delays among heart failure patients. J Card Fail 2002; 8:381–386.
- Kressin NR, Orner MB, Manze M, Glickman ME, Berlowitz D. Understanding contributors to racial disparities in blood pressure control. Circ Cardiovasc Qual Outcomes 2010; 3:173–180.
- Yancy CW, Jessup M, Bozkurt B, et al; ACCF/AHA Task Force Members. 2013 ACCF/AHA guideline for the management of heart failure. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; 62:e147–e329.
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults. Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2013; doi: 10.1001/jama.2013.284427. E-pub ahead of print.
- Chobanian AV, Bakris GL, Black HR, et al; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42:1206–1252.
- Bibbins-Domingo K, Chertow GM, Coxson PG, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med 2010; 362:590–599.
- Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; published online Nov 13. DOI: 10.1016/j.jacc.2013.11.002.
- Casagrande SS, Whitt-Glover MC, Lancaster KJ, Odoms-Young AM, Gary TL. Built environment and health behaviors among African Americans: a systematic review. Am J Prev Med 2009; 36:174–181.
- Gustat J, Rice J, Parker KM, Becker AB, Farley TA. Effect of changes to the neighborhood built environment on physical activity in a low-income African American neighborhood. Prev Chronic Dis 2012; 9:E57.
- Casagrande SS, Franco M, Gittelsohn J, et al. Healthy food availability and the association with BMI in Baltimore, Maryland. Public Health Nutr 2011; 14:1001–1007.
- Stewart JE, Battersby SE, Lopez-De Fede A, Remington KC, Hardin JW, Mayfield-Smith K. Diabetes and the socioeconomic and built environment: geovisualization of disease prevalence and potential contextual associations using ring maps. Int J Health Geogr 2011; 10:18.
- Franciosa JA, Ferdinand KC, Yancy CW; Consensus Statement on Heart Failure in African Americans Writing Group. Treatment of heart failure in African Americans: a consensus statement. Congest Heart Fail 2010; 16:27–38.
- Ahmed A, Rich MW, Love TE, et al. Digoxin and reduction in mortality and hospitalization in heart failure: a comprehensive post hoc analysis of the DIG trial. Eur Heart J 2006; 27:178–186.
- Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure.The SOLVD Investigators. N Engl J Med 1991; 325:293–302.
- Shekelle PG, Rich MW, Morton SC, et al. Efficacy of angiotensin-converting enzyme inhibitors and beta-blockers in the management of left ventricular systolic dysfunction according to race, gender, and diabetic status: a meta-analysis of major clinical trials. J Am Coll Cardiol 2003; 41:1529–1538.
- Gibbs CR, Lip GY, Beevers DG. Angioedema due to ACE inhibitors: increased risk in patients of African origin. Br J Clin Pharmacol 1999; 48:861–865.
- Brown NJ, Ray WA, Snowden M, Griffin MR. Black Americans have an increased rate of angiotensin converting enzyme inhibitor-associated angioedema. Clin Pharmacol Ther 1996; 60:8–13.
- Beta-Blocker Evaluation of Survival Trial Investigators. A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure. N Engl J Med 2001; 344:1659–1667.
- Packer M, Coats AJ, Fowler MB, et al; Carvedilol Prospective Randomized Cumulative Survival Study Group. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001; 344:1651–1658.
- Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 1999; 353:2001–2007.
- Goldstein S, Deedwania P, Gottlieb S, Wikstrand J; MERIT-HF Study Group. Metoprolol CR/XL in black patients with heart failure (from the Metoprolol CR/XL randomized intervention trial in chronic heart failure). Am J Cardiol 2003; 92:478–480.
- Bristow MR, Murphy GA, Krause-Steinrauf H, et al. An alpha2C-adrenergic receptor polymorphism alters the norepinephrine-lowering effects and therapeutic response of the beta-blocker bucindolol in chronic heart failure. Circ Heart Fail 2010; 3:21–28.
- Bristow MR, Krause-Steinrauf H, Nuzzo R, et al. Effect of baseline or changes in adrenergic activity on clinical outcomes in the beta-blocker evaluation of survival trial. Circulation 2004; 110:1437–1442.
- Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med 1999; 341:709–717.
- Pitt B, Remme W, Zannad F, et al; Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study Investigators. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 2003; 348:1309–1321.
- Zannad F, McMurray JJ, Krum H, et al; EMPHASIS-HF Study Group. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med 2011; 364:11–21.
- Cavallari LH, Groo VL, Momary KM, Fontana D, Viana MA, Vaitkus P. Racial differences in potassium response to spironolactone in heart failure. Congest Heart Fail 2006; 12:200–205.
- Cohn JN, Johnson G, Ziesche S, et al. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med 1991; 325:303–310.
- Taylor AL, Ziesche S, Yancy C, et al; African-American Heart Failure Trial Investigators. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med 2004; 351:2049–2057.
- Anand IS, Tam SW, Rector TS, et al. Influence of blood pressure on the effectiveness of a fixed-dose combination of isosorbide dinitrate and hydralazine in the African-American Heart Failure Trial. J Am Coll Cardiol 2007; 49:32–39.
- Echols MR, Felker GM, Thomas KL, et al. Racial differences in the characteristics of patients admitted for acute decompensated heart failure and their relation to outcomes: results from the OPTIME-CHF trial. J Card Fail 2006; 12:684–688.
- Kamath SA, Drazner MH, Wynne J, Fonarow GC, Yancy CW. Characteristics and outcomes in African American patients with decompensated heart failure. Arch Intern Med 2008; 168:1152–1158.
- Felker GM, Lee KL, Bull DA, et al; NHLBI Heart Failure Clinical Research Network. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med 2011; 364:797–805.
- Costanzo MR, Guglin ME, Saltzberg MT, et al; UNLOAD Trial Investigators. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol 2007; 49:675–683.
- Bart BA, Goldsmith SR, Lee KL, et al; Heart Failure Clinical Research Network. Ultrafiltration in decompensated heart failure with cardiorenal syndrome. N Engl J Med 2012; 367:2296–2304.
- Levy P, Compton S, Welch R, et al. Treatment of severe decompensated heart failure with high-dose intravenous nitroglycerin: a feasibility and outcome analysis. Ann Emerg Med 2007; 50:144–152.
- Cleland JG, Daubert JC, Erdmann E, et al; Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 2005; 352:1539–1549.
- Young JB, Abraham WT, Smith AL, et al; Multicenter InSync ICD Randomized Clinical Evaluation (MIRACLE ICD) Trial Investigators. Combined cardiac resynchronization and implantable cardioversion defibrillation in advanced chronic heart failure: the MIRACLE ICD Trial. JAMA 2003; 289:2685–2694.
- Moss AJ, Zareba W, Hall WJ, et al; Multicenter Automatic Defibrillator Implantation Trial II Investigators. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002; 346:877–883.
- Bristow MR, Saxon LA, Boehmer J, et al; Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) Investigators. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med 2004; 350:2140–2150.
- Mitchell JE, Hellkamp AS, Mark DB, et al; SCD-HeFT Investigators. Outcome in African Americans and other minorities in the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT). Am Heart J 2008; 155:501–506.
- Hernandez AF, Fonarow GC, Liang L, et al. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. JAMA 2007; 298:1525–1532.
- Farmer SA, Kirkpatrick JN, Heidenreich PA, Curtis JP, Wang Y, Groeneveld PW. Ethnic and racial disparities in cardiac resynchronization therapy. Heart Rhythm 2009; 6:325–331.
- Colvin-Adams M, Smith JM, Heubner BM, et al. OPTN/SRTR 2011 Annual Data Report: heart. Am J Transplant 2013; 13(suppl 1):119–148.
- Allen JG, Weiss ES, Arnaoutakis GJ, et al. The impact of race on survival after heart transplantation: an analysis of more than 20,000 patients. Ann Thorac Surg 2010; 89:1956–1964.
- Liu V, Bhattacharya J, Weill D, Hlatky MA. Persistent racial disparities in survival after heart transplantation. Circulation 2011; 123:1642–1649.
- Mahle WT, Kanter KR, Vincent RN. Disparities in outcome for black patients after pediatric heart transplantation. J Pediatr 2005; 147:739–743.
- Park MH, Tolman DE, Kimball PM. Disproportionate HLA matching may contribute to racial disparity in patient survival following cardiac transplantation. Clin Transplant 1996; 10(6 Pt 2):625–628.
- Park MH, Tolman DE, Kimball PM. The impact of race and HLA matching on long-term survival following cardiac transplantation. Transplant Proc 1997; 29:1460–1463.
- Callender CO, Cherikh WS, Miles PV, et al. Blacks as donors for transplantation: suboptimal outcomes overcome by transplantation into other minorities. Transplant Proc 2008; 40:995–1000.
- King LP, Siminoff LA, Meyer DM, et al. Health insurance and cardiac transplantation: a call for reform. J Am Coll Cardiol 2005; 45:1388–1391.
- Ozminkowski RJ, White AJ, Hassol A, Murphy M. Minimizing racial disparity regarding receipt of a cadaver kidney transplant. Am J Kidney Dis 1997; 30:749–759.
- Aggarwal A, Gupta A, Pappas PS, Tatooles A, Bhat G. Racial differences in patients with left ventricular assist devices. ASAIO J 2012; 58:499–502.
- Tsiouris A, Brewer RJ, Borgi J, Nemeh H, Paone G, Morgan JA. Continuous-flow left ventricular assist device implantation as a bridge to transplantation or destination therapy: racial disparities in outcomes. J Heart Lung Transplant 2013; 32:299–304.
- Joyce DL, Conte JV, Russell SD, Joyce LD, Chang DC. Disparities in access to left ventricular assist device therapy. J Surg Res 2009; 152:111–117.
- Go AS, Mozaffarian D, Roger VL, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation 2013; 127:e6–e245.
- Bahrami H, Kronmal R, Bluemke DA, et al. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med 2008; 168:2138–2145.
- Loehr LR, Rosamond WD, Chang PP, Folsom AR, Chambless LE. Heart failure incidence and survival (from the Atherosclerosis Risk in Communities study). Am J Cardiol 2008; 101:1016–1022.
- Kalogeropoulos A, Georgiopoulou V, Kritchevsky SB, et al. Epidemiology of incident heart failure in a contemporary elderly cohort: the health, aging, and body composition study. Arch Intern Med 2009; 169:708–715.
- Dries DL, Exner DV, Gersh BJ, Cooper HA, Carson PE, Domanski MJ. Racial differences in the outcome of left ventricular dysfunction. N Engl J Med 1999; 340:609–616.
- Exner DV, Dries DL, Domanski MJ, Cohn JN. Lesser response to angiotensin-converting-enzyme inhibitor therapy in black as compared with white patients with left ventricular dysfunction. N Engl J Med 2001; 344:1351–1357.
- Bardy GH, Lee KL, Mark DB, et al; Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005; 352:225–237.
- Bibbins-Domingo K, Pletcher MJ, Lin F, et al. Racial differences in incident heart failure among young adults. N Engl J Med 2009; 360:1179–1190.
- Eaton CB, Abdulbaki AM, Margolis KL, et al. Racial and ethnic differences in incident hospitalized heart failure in postmenopausal women: the Women’s Health Initiative. Circulation 2012; 126:688–696.
- Ilksoy N, Hoffman M, Moore RH, Easley K, Jacobson TA. Comparison of African-American patients with systolic heart failure versus preserved ejection fraction. Am J Cardiol 2006; 98:806–808.
- Sharp A, Tapp R, Francis DP, et al. Ethnicity and left ventricular diastolic function in hypertension an ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial) substudy. J Am Coll Cardiol 2008; 52:1015–1021.
- Kizer JR, Arnett DK, Bella JN, et al. Differences in left ventricular structure between black and white hypertensive adults: the Hypertension Genetic Epidemiology Network study. Hypertension 2004; 43:1182–1188.
- Drazner MH, Dries DL, Peshock RM, et al. Left ventricular hypertrophy is more prevalent in blacks than whites in the general population: the Dallas Heart Study. Hypertension 2005; 46:124–129.
- East MA, Peterson ED, Shaw LK, Gattis WA, O’Connor CM. Racial differences in the outcomes of patients with diastolic heart failure. Am Heart J 2004; 148:151–156.
- Klapholz M, Maurer M, Lowe AM, et al; New York Heart Failure Consortium. Hospitalization for heart failure in the presence of a normal left ventricular ejection fraction: results of the New York Heart Failure Registry. J Am Coll Cardiol 2004; 43:1432–1438.
- Agoston I, Cameron CS, Yao D, Dela Rosa A, Mann DL, Deswal A. Comparison of outcomes of white versus black patients hospitalized with heart failure and preserved ejection fraction. Am J Cardiol 2004; 94:1003–1007.
- Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. US Carvedilol Heart Failure Study Group. N Engl J Med 1996; 334:1349–1355.
- Yancy CW, Strong M. The natural history, epidemiology, and prognosis of heart failure in African Americans. Congest Heart Fail 2004; 10:15–18.
- Velagaleti RS, Gona P, Larson MG, et al. Multimarker approach for the prediction of heart failure incidence in the community. Circulation 2010; 122:1700–1706.
- Deswal A, Petersen NJ, Urbauer DL, Wright SM, Beyth R. Racial variations in quality of care and outcomes in an ambulatory heart failure cohort. Am Heart J 2006; 152:348–354.
- Howard G, Prineas R, Moy C, et al. Racial and geographic differences in awareness, treatment, and control of hypertension: the REasons for Geographic And Racial Differences in Stroke study. Stroke 2006; 37:1171–1178.
- Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med 2005; 165:2098–2104.
- Okin PM, Kjeldsen SE, Dahlöf B, Devereux RB. Racial differences in incident heart failure during antihypertensive therapy. Circ Cardiovasc Qual Outcomes 2011; 4:157–164.
- Mulukutla SR, Venkitachalam L, Bambs C, et al. Black race is associated with digital artery endothelial dysfunction: results from the Heart SCORE study. Eur Heart J 2010; 31:2808–2815.
- Campia U, Choucair WK, Bryant MB, Waclawiw MA, Cardillo C, Panza JA. Reduced endothelium-dependent and -independent dilation of conductance arteries in African Americans. J Am Coll Cardiol 2002; 40:754–760.
- Perregaux D, Chaudhuri A, Rao S, et al. Brachial vascular reactivity in blacks. Hypertension 2000; 36:866–871.
- Duprez DA, Jacobs DR, Lutsey PL, et al. Race/ethnic and sex differences in large and small artery elasticity—results of the multiethnic study of atherosclerosis (MESA). Ethn Dis 2009; 19:243–250.
- Kalinowski L, Dobrucki IT, Malinski T. Race-specific differences in endothelial function: predisposition of African Americans to vascular diseases. Circulation 2004; 109:2511–2517.
- Kojda G, Harrison D. Interactions between NO and reactive oxygen species: pathophysiological importance in atherosclerosis, hypertension, diabetes and heart failure. Cardiovasc Res 1999; 43:562–571.
- Gattás GJ, Kato M, Soares-Vieira JA, et al. Ethnicity and glutathione S-transferase (GSTM1/GSTT1) polymorphisms in a Brazilian population. Braz J Med Biol Res 2004; 37:451–458.
- Li R, Lyn D, Lapu-Bula R, et al. Relation of endothelial nitric oxide synthase gene to plasma nitric oxide level, endothelial function, and blood pressure in African Americans. Am J Hypertens 2004; 17:560–567.
- Parra EJ, Marcini A, Akey J, et al. Estimating African American admixture proportions by use of population-specific alleles. Am J Hum Genet 1998; 63:1839–1851.
- Small KM, Wagoner LE, Levin AM, Kardia SL, Liggett SB. Synergistic polymorphisms of beta1- and alpha2C-adrenergic receptors and the risk of congestive heart failure. N Engl J Med 2002; 347:1135–1142.
- McNamara DM, Tam SW, Sabolinski ML, et al. Aldosterone synthase promoter polymorphism predicts outcome in African Americans with heart failure: results from the A-HeFT Trial. J Am Coll Cardiol 2006; 48:1277–1282.
- McNamara DM, Tam SW, Sabolinski ML, et al. Endothelial nitric oxide synthase (NOS3) polymorphisms in African Americans with heart failure: results from the A-HeFT trial. J Card Fail 2009; 15:191–198.
- Jacobson DR, Pastore RD, Yaghoubian R, et al. Variant-sequence transthyretin (isoleucine 122) in late-onset cardiac amyloidosis in black Americans. N Engl J Med 1997; 336:466–473.
- Buxbaum J, Alexander A, Koziol J, Tagoe C, Fox E, Kitzman D. Significance of the amyloidogenic transthyretin Val 122 Ile allele in African Americans in the Arteriosclerosis Risk in Communities (ARIC) and Cardiovascular Health (CHS) Studies. Am Heart J 2010; 159:864–870.
- Philbin EF, Dec GW, Jenkins PL, DiSalvo TG. Socioeconomic status as an independent risk factor for hospital readmission for heart failure. Am J Cardiol 2001; 87:1367–1371.
- Evangelista LS, Dracup K, Doering LV. Racial differences in treatment-seeking delays among heart failure patients. J Card Fail 2002; 8:381–386.
- Kressin NR, Orner MB, Manze M, Glickman ME, Berlowitz D. Understanding contributors to racial disparities in blood pressure control. Circ Cardiovasc Qual Outcomes 2010; 3:173–180.
- Yancy CW, Jessup M, Bozkurt B, et al; ACCF/AHA Task Force Members. 2013 ACCF/AHA guideline for the management of heart failure. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; 62:e147–e329.
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults. Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2013; doi: 10.1001/jama.2013.284427. E-pub ahead of print.
- Chobanian AV, Bakris GL, Black HR, et al; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42:1206–1252.
- Bibbins-Domingo K, Chertow GM, Coxson PG, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med 2010; 362:590–599.
- Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; published online Nov 13. DOI: 10.1016/j.jacc.2013.11.002.
- Casagrande SS, Whitt-Glover MC, Lancaster KJ, Odoms-Young AM, Gary TL. Built environment and health behaviors among African Americans: a systematic review. Am J Prev Med 2009; 36:174–181.
- Gustat J, Rice J, Parker KM, Becker AB, Farley TA. Effect of changes to the neighborhood built environment on physical activity in a low-income African American neighborhood. Prev Chronic Dis 2012; 9:E57.
- Casagrande SS, Franco M, Gittelsohn J, et al. Healthy food availability and the association with BMI in Baltimore, Maryland. Public Health Nutr 2011; 14:1001–1007.
- Stewart JE, Battersby SE, Lopez-De Fede A, Remington KC, Hardin JW, Mayfield-Smith K. Diabetes and the socioeconomic and built environment: geovisualization of disease prevalence and potential contextual associations using ring maps. Int J Health Geogr 2011; 10:18.
- Franciosa JA, Ferdinand KC, Yancy CW; Consensus Statement on Heart Failure in African Americans Writing Group. Treatment of heart failure in African Americans: a consensus statement. Congest Heart Fail 2010; 16:27–38.
- Ahmed A, Rich MW, Love TE, et al. Digoxin and reduction in mortality and hospitalization in heart failure: a comprehensive post hoc analysis of the DIG trial. Eur Heart J 2006; 27:178–186.
- Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure.The SOLVD Investigators. N Engl J Med 1991; 325:293–302.
- Shekelle PG, Rich MW, Morton SC, et al. Efficacy of angiotensin-converting enzyme inhibitors and beta-blockers in the management of left ventricular systolic dysfunction according to race, gender, and diabetic status: a meta-analysis of major clinical trials. J Am Coll Cardiol 2003; 41:1529–1538.
- Gibbs CR, Lip GY, Beevers DG. Angioedema due to ACE inhibitors: increased risk in patients of African origin. Br J Clin Pharmacol 1999; 48:861–865.
- Brown NJ, Ray WA, Snowden M, Griffin MR. Black Americans have an increased rate of angiotensin converting enzyme inhibitor-associated angioedema. Clin Pharmacol Ther 1996; 60:8–13.
- Beta-Blocker Evaluation of Survival Trial Investigators. A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure. N Engl J Med 2001; 344:1659–1667.
- Packer M, Coats AJ, Fowler MB, et al; Carvedilol Prospective Randomized Cumulative Survival Study Group. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001; 344:1651–1658.
- Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 1999; 353:2001–2007.
- Goldstein S, Deedwania P, Gottlieb S, Wikstrand J; MERIT-HF Study Group. Metoprolol CR/XL in black patients with heart failure (from the Metoprolol CR/XL randomized intervention trial in chronic heart failure). Am J Cardiol 2003; 92:478–480.
- Bristow MR, Murphy GA, Krause-Steinrauf H, et al. An alpha2C-adrenergic receptor polymorphism alters the norepinephrine-lowering effects and therapeutic response of the beta-blocker bucindolol in chronic heart failure. Circ Heart Fail 2010; 3:21–28.
- Bristow MR, Krause-Steinrauf H, Nuzzo R, et al. Effect of baseline or changes in adrenergic activity on clinical outcomes in the beta-blocker evaluation of survival trial. Circulation 2004; 110:1437–1442.
- Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med 1999; 341:709–717.
- Pitt B, Remme W, Zannad F, et al; Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study Investigators. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 2003; 348:1309–1321.
- Zannad F, McMurray JJ, Krum H, et al; EMPHASIS-HF Study Group. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med 2011; 364:11–21.
- Cavallari LH, Groo VL, Momary KM, Fontana D, Viana MA, Vaitkus P. Racial differences in potassium response to spironolactone in heart failure. Congest Heart Fail 2006; 12:200–205.
- Cohn JN, Johnson G, Ziesche S, et al. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med 1991; 325:303–310.
- Taylor AL, Ziesche S, Yancy C, et al; African-American Heart Failure Trial Investigators. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med 2004; 351:2049–2057.
- Anand IS, Tam SW, Rector TS, et al. Influence of blood pressure on the effectiveness of a fixed-dose combination of isosorbide dinitrate and hydralazine in the African-American Heart Failure Trial. J Am Coll Cardiol 2007; 49:32–39.
- Echols MR, Felker GM, Thomas KL, et al. Racial differences in the characteristics of patients admitted for acute decompensated heart failure and their relation to outcomes: results from the OPTIME-CHF trial. J Card Fail 2006; 12:684–688.
- Kamath SA, Drazner MH, Wynne J, Fonarow GC, Yancy CW. Characteristics and outcomes in African American patients with decompensated heart failure. Arch Intern Med 2008; 168:1152–1158.
- Felker GM, Lee KL, Bull DA, et al; NHLBI Heart Failure Clinical Research Network. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med 2011; 364:797–805.
- Costanzo MR, Guglin ME, Saltzberg MT, et al; UNLOAD Trial Investigators. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol 2007; 49:675–683.
- Bart BA, Goldsmith SR, Lee KL, et al; Heart Failure Clinical Research Network. Ultrafiltration in decompensated heart failure with cardiorenal syndrome. N Engl J Med 2012; 367:2296–2304.
- Levy P, Compton S, Welch R, et al. Treatment of severe decompensated heart failure with high-dose intravenous nitroglycerin: a feasibility and outcome analysis. Ann Emerg Med 2007; 50:144–152.
- Cleland JG, Daubert JC, Erdmann E, et al; Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 2005; 352:1539–1549.
- Young JB, Abraham WT, Smith AL, et al; Multicenter InSync ICD Randomized Clinical Evaluation (MIRACLE ICD) Trial Investigators. Combined cardiac resynchronization and implantable cardioversion defibrillation in advanced chronic heart failure: the MIRACLE ICD Trial. JAMA 2003; 289:2685–2694.
- Moss AJ, Zareba W, Hall WJ, et al; Multicenter Automatic Defibrillator Implantation Trial II Investigators. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002; 346:877–883.
- Bristow MR, Saxon LA, Boehmer J, et al; Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) Investigators. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med 2004; 350:2140–2150.
- Mitchell JE, Hellkamp AS, Mark DB, et al; SCD-HeFT Investigators. Outcome in African Americans and other minorities in the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT). Am Heart J 2008; 155:501–506.
- Hernandez AF, Fonarow GC, Liang L, et al. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. JAMA 2007; 298:1525–1532.
- Farmer SA, Kirkpatrick JN, Heidenreich PA, Curtis JP, Wang Y, Groeneveld PW. Ethnic and racial disparities in cardiac resynchronization therapy. Heart Rhythm 2009; 6:325–331.
- Colvin-Adams M, Smith JM, Heubner BM, et al. OPTN/SRTR 2011 Annual Data Report: heart. Am J Transplant 2013; 13(suppl 1):119–148.
- Allen JG, Weiss ES, Arnaoutakis GJ, et al. The impact of race on survival after heart transplantation: an analysis of more than 20,000 patients. Ann Thorac Surg 2010; 89:1956–1964.
- Liu V, Bhattacharya J, Weill D, Hlatky MA. Persistent racial disparities in survival after heart transplantation. Circulation 2011; 123:1642–1649.
- Mahle WT, Kanter KR, Vincent RN. Disparities in outcome for black patients after pediatric heart transplantation. J Pediatr 2005; 147:739–743.
- Park MH, Tolman DE, Kimball PM. Disproportionate HLA matching may contribute to racial disparity in patient survival following cardiac transplantation. Clin Transplant 1996; 10(6 Pt 2):625–628.
- Park MH, Tolman DE, Kimball PM. The impact of race and HLA matching on long-term survival following cardiac transplantation. Transplant Proc 1997; 29:1460–1463.
- Callender CO, Cherikh WS, Miles PV, et al. Blacks as donors for transplantation: suboptimal outcomes overcome by transplantation into other minorities. Transplant Proc 2008; 40:995–1000.
- King LP, Siminoff LA, Meyer DM, et al. Health insurance and cardiac transplantation: a call for reform. J Am Coll Cardiol 2005; 45:1388–1391.
- Ozminkowski RJ, White AJ, Hassol A, Murphy M. Minimizing racial disparity regarding receipt of a cadaver kidney transplant. Am J Kidney Dis 1997; 30:749–759.
- Aggarwal A, Gupta A, Pappas PS, Tatooles A, Bhat G. Racial differences in patients with left ventricular assist devices. ASAIO J 2012; 58:499–502.
- Tsiouris A, Brewer RJ, Borgi J, Nemeh H, Paone G, Morgan JA. Continuous-flow left ventricular assist device implantation as a bridge to transplantation or destination therapy: racial disparities in outcomes. J Heart Lung Transplant 2013; 32:299–304.
- Joyce DL, Conte JV, Russell SD, Joyce LD, Chang DC. Disparities in access to left ventricular assist device therapy. J Surg Res 2009; 152:111–117.
KEY POINTS
- The natural history, epidemiology, and outcomes of heart failure in African Americans differ from those in whites.
- Hypertension is the predominant risk factor for heart failure in African Americans, and aggressive management of hypertension may substantially reduce the incidence and consequences of heart failure in this population.
- Heart failure in African Americans should be treated according to the same evidenced-based strategies as in the general population. In addition, a combination of isosorbide dinitrate and hydralazine is recommended in African Americans.
- Many questions remain unanswered, since African Americans have been markedly underrepresented in clinical trials.