User login
Clinical Progress Note: Direct Oral Anticoagulants for Treatment of Venous Thromboembolism in Children
Venous thromboembolism (VTE) is a life-threatening event occurring with increasing frequency in hospitalized children and an incidence of more than 58 events per 10,000 hospitalizations.1 In pediatric patients, VTEs occur less often than in adults, have bimodal peaks in neonates and adolescents, and are typically provoked, with central venous access as the most common risk factor.1,
Treatment of pediatric VTE includes unfractionated heparin (UFH), low-molecular-weight heparin (LMWH), and vitamin K antagonists (ie, warfarin). These agents have limitations, including parenteral administration, frequent lab monitoring, and drug/dietary interactions complicating use. Only recently have there been pediatric studies to assess these agents’ pharmacokinetics, pharmacodynamics, safety, and efficacy.2
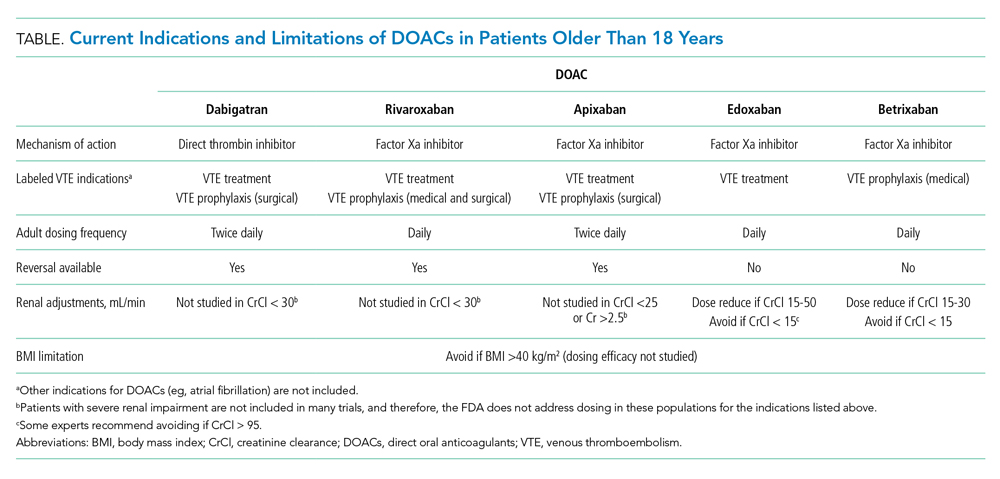
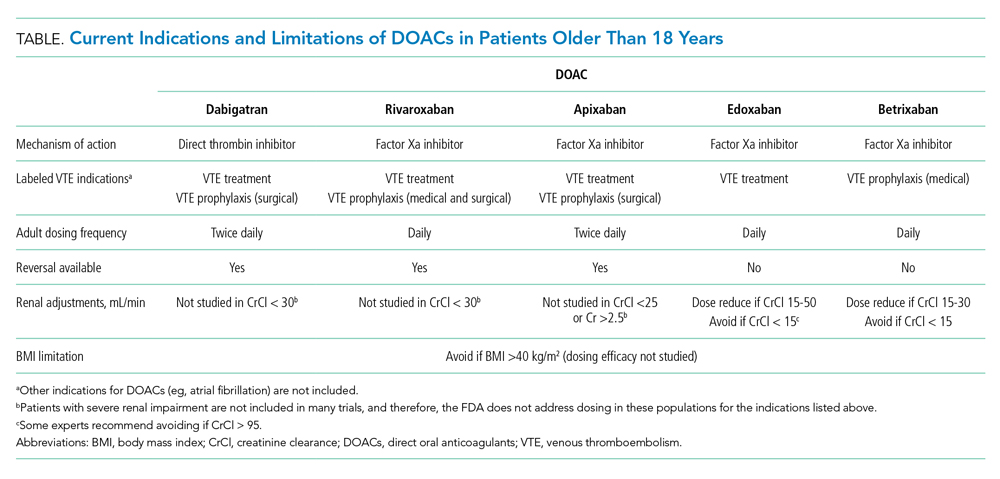
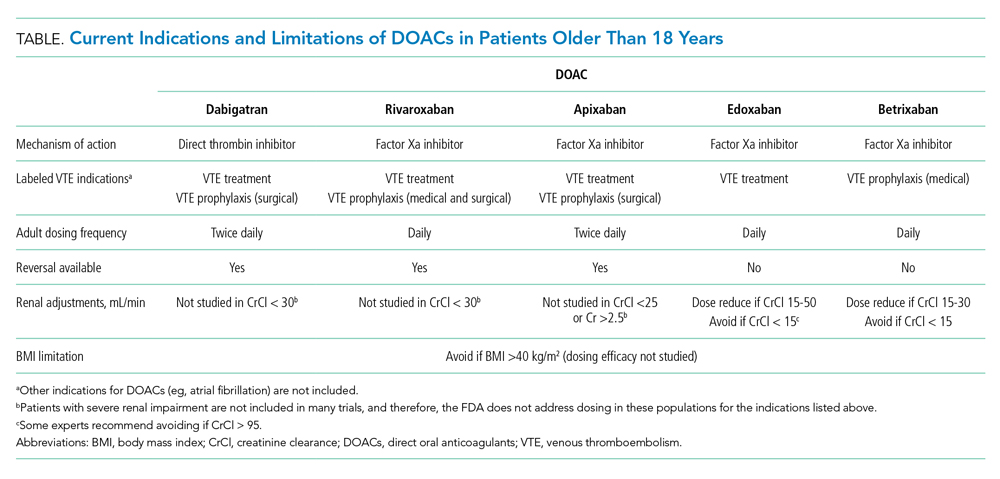
Direct oral anticoagulants (DOACs) commonly used to treat VTE in adults have two mechanisms of action: direct thrombin (activated factor II) inhibition (ie, dabigatran) and activated factor X (Xa) inhibition (ie, rivaroxaban, apixaban, edoxaban, betrixaban). DOACs offer practical advantages over and efficacy similar to that of warfarin and heparin products, including oral administration, predictable pharmacology, no required lab monitoring, and fewer drug/dietary interactions. DOACs are already approved for VTE treatment in patients 18 years and older.3
This clinical practice update synthesizes 6 years (2014-2020) of literature regarding DOACs for treatment of VTE, focusing on their current role in patients 18 years and older and their emerging role in pediatric patients.
USE IN ADULTS
DOACs are approved by the US Food and Drug Administration (FDA) for multiple anticoagulation indications in adults, including treatment and prevention of acute VTE and prevention of stroke in nonvalvular atrial fibrillation (Table). DOACs are well tolerated by most adults; however, use in certain populations, including patients with liver disease with coagulopathy, advanced renal disease (creatinine clearance <30 mL/min), and class III obesity (body mass index [BMI] >40 kg/m2), requires caution.4,5 For adult patients with VTE without contraindications, DOACs are considered equivalent to warfarin; current CHEST guidelines even suggest preference of DOACs over warfarin.5 While it is prudent to exercise caution when extrapolating adult data to children, these data have informed ongoing pediatric DOAC clinical trials.
The efficacy and safety of each of the DOACs (aside from betrixaban, which is indicated only for prophylaxis) have compared with warfarin for treatment of VTE in adults.6 A meta-analysis of six clinical trials determined DOACs are noninferior to warfarin for VTE treatment.3 Only two of six trials included patients with provoked VTEs. The meta-analysis found no difference in rates of recurrent symptomatic VTE (primary outcome; relative risk [RR], 0.91; 95% CI, 0.79-1.06) or all-cause mortality (secondary outcome; RR, 0.98; 95% CI, 0.84-1.14). Additionally, DOACs were shown as possibly safer than warfarin due to fewer major bleeding events, particularly fatal bleeding (RR, 0.36; 95% CI, 0.15-0.84) and intracranial bleeding (RR, 0.34; 95% CI, 0.17-0.69). For clinically relevant nonmajor bleeding (eg, gastrointestinal bleeding requiring <2 U packed red blood cells), results were similar (RR, 0.73; 95% CI, 0.58-0.93).
DOACs appear to have effectiveness comparable with that of warfarin. A retrospective matched cohort study of 59,525 patients with acute VTE compared outcomes of patients on DOACs (95% on rivaroxaban) with those of patients on warfarin.6 There were no differences in all-cause mortality or major bleeding. Another retrospective cohort study of 62,431 patients with acute VTE compared rivaroxaban and apixaban with warfarin, as well as rivaroxaban and apixaban with each other.7 There were no differences in 3- and 6-month mortality between warfarin and DOAC users or between rivaroxaban and apixaban users.
Initial approval of DOACs brought concerns about reversibility in the setting of bleeding or urgent procedural need. Clinical practice guidelines, primarily based on observational studies and laboratory parameters in vitro or in healthy volunteers, recommend activated prothrombin complex concentrates as a first-line intervention.8 However, specific agents have now been FDA-approved for DOAC reversal.
Idarucizumab is an FDA-approved (2015) monoclonal antibody with high affinity for dabigatran. Approval was based on a multicenter prospective cohort study of 503 patients taking dabigatran who presented with major bleeding (301 patients) or requiring an urgent surgery (202 patients).9 Idarucizumab resulted in a median time to bleeding cessation of 2.5 hours for those 134 patients in whom time to bleeding cessation could be assessed. Patients with intracranial bleeding were excluded from the timed portion because follow up imaging was not mandated. For those requiring surgery, 93% had normal periprocedural hemostasis.
Andexanet alfa is an FDA-approved (2018) drug for reversal of apixaban and rivaroxaban that acts as a catalytically inactive decoy Xa molecule, binding Xa inhibitors with high affinity. A multicenter prospective cohort study of 352 patients on Xa inhibitors with major bleeding found administration of andexanet alfa resulted in excellent or good hemostasis in 82% of patients (204/249 patients) at 12 hours.10 There was no difference between rivaroxaban and apixaban patients. Both idarucizumab and andexanet alfa remain expensive and not universally available, but availability and use will likely increase with time.
EVIDENCE FOR USE IN CHILDREN
In pediatric patients, most VTEs are provoked, with the most common risk factor being presence of a central line. Frequency of this risk factor varies based on age (>60% of cases in older children and nearly 90% in neonates).1 The most recent American Society of Hematology guidelines recommend treating pediatric symptomatic VTE with anticoagulation and treating asymptomatic VTE instead of observation.2 These recommendations rely on evidence in adult patients due to the current paucity of evidence in pediatrics.
“Pediatric investigation plans” are the cornerstone for ongoing clinical trials of DOACs in pediatrics. While studies evaluating safety and efficacy of standard anticoagulants (UFH, LMWH, and warfarin) in pediatrics exist, clinical trials at the time of drug development did not include pediatric patients. This means none of the currently used anticoagulants were initially developed or approved for children.1 Under the Pediatric Research Equity Act of 2007, the FDA requires pharmaceutical companies to submit a New Drug Application to perform pediatric studies of drugs deemed likely for use in pediatric patients. Pediatric investigation plans allow for establishing safety, efficacy, dosing, and administration routes in pediatric populations. All four DOACs currently approved for treatment of VTE in adults have ongoing efficacy and safety clinical trials for children.
The first and only published clinical trial of DOAC efficacy and safety in pediatrics compared rivaroxaban to standard treatment of acute VTE (Appendix Table).11 The industry-sponsored, open-label EINSTEIN-Jr trial randomized patients aged 0 to 17 years 2:1 to weight-based rivaroxaban or standard treatment after receiving initial parenteral therapy for 5 to 9 days. While most patients were treated for at least 3 months, patients younger than 2 years with line-related thrombosis were treated for only 1 month. The study population mostly consisted of patients with initial, symptomatic, provoked VTE, with types ranging from cerebral venous sinus thrombosis to catheter-associated thrombosis. VTE risk factors, which varied by age, included presence of a central line, major infection, surgery, or trauma. While most VTEs in pediatric patients are expected to be central-line related, in the EINSTEIN-Jr trial only 25.2% of VTEs were central line–associated. The study evaluated symptomatic recurrent VTE (primary efficacy outcome) and clinically relevant bleeding (safety outcome). No significant difference was found between treatment groups in efficacy or safety outcomes, and there were no treatment-related deaths. While the trial was not powered to assess noninferiority due to low incidence of VTE in pediatrics, the absolute number of symptomatic recurrent VTEs was lower in the rivaroxaban group compared with the standard-care group (1% vs 3%). The investigators concluded that rivaroxaban is similarly efficacious and safe in children as compared with adults. FDA approval of rivaroxaban in pediatrics is expected given the trial’s favorable results. Clinicians may wish to consider whether the studied population is comparable with their own patients because the trial had a lower percentage of line-associated VTE than previously reported in the pediatric population.
Multiple clinical trials evaluating the efficacy and safety of other DOACs in pediatric patients are currently underway (Appendix Table).12-14 Apixaban and edoxaban have active multicenter, randomized, open-label clinical trials recruiting patients up to age 17 who have imaging-confirmed acute VTE. A similar trial for dabigatran has recently completed recruitment. Outcome measures include recurrent VTE, VTE-related mortality, and major or clinically relevant non-major bleeding. Like EINSTEIN-Jr, patients in the dabigatran and edoxaban trials were treated with parenteral therapy for at least 5 days prior to randomization.12,14 In the apixaban trial, participants can be randomized without initial parenteral treatment.13 Betrixaban, the newest DOAC approved in adults, does not currently have any open pediatric trials.
AREAS IN NEED OF FUTURE STUDY
Lack of approved reversal agents may initially limit DOAC use in children. An open-label study examining idarucizumab safety has completed enrollment, but it has not yet published results.15 To date, there are no pediatric clinical trials examining andexanet alpha. Future work will need to establish efficacy and safety of reversal agents in pediatrics.
DOACs have not been adequately studied in populations of patients with comorbidities, such as liver disease, renal disease, altered enteral absorption, and BMI higher than 40. Physiologic differences in children with cancer and in neonates merit further evaluation of DOAC safety and efficacy. While ongoing trials established weight-based dosing regimens for children, longitudinal studies will need to ensure adequate anticoagulation, especially in the populations listed here.
The safety outcomes in most DOAC studies include clinically relevant bleeding and VTE-related mortality. These outcomes are much less common in pediatric patients than they are in adults, and future studies may need to expand safety outcomes to those more frequently seen in children. Primary and secondary endpoint variability in pediatric DOAC clinical trials presents challenges interpreting and comparing study results.
SUMMARY
VTE is an increasingly common complication in hospitalized children contributing to significant morbidity.1 For decades, the only treatment options have been UFH, LMWH, or warfarin. DOACs offer many advantages compared with standard anticoagulation options. The only clinical trial evaluating efficacy and safety of DOACs published to date demonstrates that pediatric patients taking rivaroxaban have outcomes similar to those of patients receiving standard care. It is expected that DOACs will gain FDA approval for treatment of VTE in pediatric patients in the near future; therefore, hospitalists should understand indications for use of these medications.
1. Monagle P, Newall F. Management of thrombosis in children and neonates: practical use of anticoagulants in children. Hematology Am Soc Hematol Educ Program. 2018;2018(1):399-404. https://doi.org/10.1182/asheducation-2018.1.399
2. Monagle P, Cuello CA, Augustine C, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: treatment of pediatric venous thromboembolism. Blood Adv. 2018;2(22):3292-3316. https://doi.org/10.1182/bloodadvances.2018024786
3. Gómez-Outes A, Terleira-Fernández AI, Lecumberri R, Suárez-Gea ML, Vargas-Castrillón E. Direct oral anticoagulants in the treatment of acute venous thromboembolism: a systematic review and meta-analysis. Thromb Res. 2014;134(4):774-782. https://doi.org/10.1016/j.thromres.2014.06.020
4. Martin K, Beyer-Westendorf J, Davidson BL, Huisman MV, Sandset PM, Moll S. Use of the direct oral anticoagulants in obese patients: guidance from the SSC of the ISTH. J Thromb Haemost. 2016;14(6):1308-1313. https://doi.org/10.1111/jth.13323
5. Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315-352. https://doi.org/10.1016/j.chest.2015.11.026
6. Jun M, Lix LM, Durand M, et al. Comparative safety of direct oral anticoagulants and warfarin in venous thromboembolism: multicentre, population based, observational study. BMJ. 2017;359:j4323. https://doi.org/10.1136/bmj.j4323
7. Roetker NS, Lutsey PL, Zakai NA, Alonso A, Adam TJ, MacLehose RF. All-cause mortality risk with direct oral anticoagulants and warfarin in the primary treatment of venous thromboembolism. Thromb Haemost. 2018;118(9):1637-1645. https://doi.org/10.1055/s-0038-1668521
8. Hoffman M, Goldstein JN, Levy JH. The impact of prothrombin complex concentrates when treating DOAC-associated bleeding: a review. Int J Emerg Med. 2018;11(1):55. https://doi.org/10.1186/s12245-018-0215-6
9. Pollack CV Jr, Reilly PA, van Ryn J, et al. Idarucizumab for dabigatran reversal - full cohort analysis. N Engl J Med. 2017;377(5):431-441. https://doi.org/10.1056/nejmoa1707278
10. Connolly SJ, Crowther M, Eikelboom JW, et al. Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Engl J Med. 2019;380(14):1326-1335. https://doi.org/10.1056/nejmoa1814051
11. Male C, Lensing AWA, Palumbo JS, et al. Rivaroxaban compared with standard anticoagulants for the treatment of acute venous thromboembolism in children: a randomised, controlled, phase 3 trial. Lancet Haematol. 2020;7(1):e18-e27. https://doi.org/10.1016/s2352-3026(19)30219-4
12. Open label study comparing efficacy and safety of dabigatran etexilate to standard of care in paediatric patients with venous thromboembolism (VTE). ClinicalTrials.gov identifier: NCT01895777. Posted July 11, 2013. Updated July 7, 2020. Accessed September 23, 2020. https://clinicaltrials.gov/ct2/show/NCT01895777
13. Apixaban for the acute treatment of venous thromboembolism in children. ClinicalTrials.gov identifier: NCT02464969. Posted June 8, 2015. Updated September 10, 2020. Accessed September 23, 2020. https://clinicaltrials.gov/ct2/show/NCT02464969
14. Hokusai study in pediatric patients with confirmed venous thromboembolism (VTE). ClinicalTrials.gov identifier: NCT02798471. Posted June 14, 2016. Update March 6, 2020. Accessed September 23, 2020. https://clinicaltrials.gov/ct2/show/NCT02798471
15. Reversal dabigatran anticoagulant effect with idarucizumab. ClinicalTrials.gov Identifier: NCT02815670. Posted June 28, 2016. Updated April 14, 2020. Accessed September 23, 2020. https://clinicaltrials.gov/ct2/show/NCT02815670
Venous thromboembolism (VTE) is a life-threatening event occurring with increasing frequency in hospitalized children and an incidence of more than 58 events per 10,000 hospitalizations.1 In pediatric patients, VTEs occur less often than in adults, have bimodal peaks in neonates and adolescents, and are typically provoked, with central venous access as the most common risk factor.1,
Treatment of pediatric VTE includes unfractionated heparin (UFH), low-molecular-weight heparin (LMWH), and vitamin K antagonists (ie, warfarin). These agents have limitations, including parenteral administration, frequent lab monitoring, and drug/dietary interactions complicating use. Only recently have there been pediatric studies to assess these agents’ pharmacokinetics, pharmacodynamics, safety, and efficacy.2
Direct oral anticoagulants (DOACs) commonly used to treat VTE in adults have two mechanisms of action: direct thrombin (activated factor II) inhibition (ie, dabigatran) and activated factor X (Xa) inhibition (ie, rivaroxaban, apixaban, edoxaban, betrixaban). DOACs offer practical advantages over and efficacy similar to that of warfarin and heparin products, including oral administration, predictable pharmacology, no required lab monitoring, and fewer drug/dietary interactions. DOACs are already approved for VTE treatment in patients 18 years and older.3
This clinical practice update synthesizes 6 years (2014-2020) of literature regarding DOACs for treatment of VTE, focusing on their current role in patients 18 years and older and their emerging role in pediatric patients.
USE IN ADULTS
DOACs are approved by the US Food and Drug Administration (FDA) for multiple anticoagulation indications in adults, including treatment and prevention of acute VTE and prevention of stroke in nonvalvular atrial fibrillation (Table). DOACs are well tolerated by most adults; however, use in certain populations, including patients with liver disease with coagulopathy, advanced renal disease (creatinine clearance <30 mL/min), and class III obesity (body mass index [BMI] >40 kg/m2), requires caution.4,5 For adult patients with VTE without contraindications, DOACs are considered equivalent to warfarin; current CHEST guidelines even suggest preference of DOACs over warfarin.5 While it is prudent to exercise caution when extrapolating adult data to children, these data have informed ongoing pediatric DOAC clinical trials.
The efficacy and safety of each of the DOACs (aside from betrixaban, which is indicated only for prophylaxis) have compared with warfarin for treatment of VTE in adults.6 A meta-analysis of six clinical trials determined DOACs are noninferior to warfarin for VTE treatment.3 Only two of six trials included patients with provoked VTEs. The meta-analysis found no difference in rates of recurrent symptomatic VTE (primary outcome; relative risk [RR], 0.91; 95% CI, 0.79-1.06) or all-cause mortality (secondary outcome; RR, 0.98; 95% CI, 0.84-1.14). Additionally, DOACs were shown as possibly safer than warfarin due to fewer major bleeding events, particularly fatal bleeding (RR, 0.36; 95% CI, 0.15-0.84) and intracranial bleeding (RR, 0.34; 95% CI, 0.17-0.69). For clinically relevant nonmajor bleeding (eg, gastrointestinal bleeding requiring <2 U packed red blood cells), results were similar (RR, 0.73; 95% CI, 0.58-0.93).
DOACs appear to have effectiveness comparable with that of warfarin. A retrospective matched cohort study of 59,525 patients with acute VTE compared outcomes of patients on DOACs (95% on rivaroxaban) with those of patients on warfarin.6 There were no differences in all-cause mortality or major bleeding. Another retrospective cohort study of 62,431 patients with acute VTE compared rivaroxaban and apixaban with warfarin, as well as rivaroxaban and apixaban with each other.7 There were no differences in 3- and 6-month mortality between warfarin and DOAC users or between rivaroxaban and apixaban users.
Initial approval of DOACs brought concerns about reversibility in the setting of bleeding or urgent procedural need. Clinical practice guidelines, primarily based on observational studies and laboratory parameters in vitro or in healthy volunteers, recommend activated prothrombin complex concentrates as a first-line intervention.8 However, specific agents have now been FDA-approved for DOAC reversal.
Idarucizumab is an FDA-approved (2015) monoclonal antibody with high affinity for dabigatran. Approval was based on a multicenter prospective cohort study of 503 patients taking dabigatran who presented with major bleeding (301 patients) or requiring an urgent surgery (202 patients).9 Idarucizumab resulted in a median time to bleeding cessation of 2.5 hours for those 134 patients in whom time to bleeding cessation could be assessed. Patients with intracranial bleeding were excluded from the timed portion because follow up imaging was not mandated. For those requiring surgery, 93% had normal periprocedural hemostasis.
Andexanet alfa is an FDA-approved (2018) drug for reversal of apixaban and rivaroxaban that acts as a catalytically inactive decoy Xa molecule, binding Xa inhibitors with high affinity. A multicenter prospective cohort study of 352 patients on Xa inhibitors with major bleeding found administration of andexanet alfa resulted in excellent or good hemostasis in 82% of patients (204/249 patients) at 12 hours.10 There was no difference between rivaroxaban and apixaban patients. Both idarucizumab and andexanet alfa remain expensive and not universally available, but availability and use will likely increase with time.
EVIDENCE FOR USE IN CHILDREN
In pediatric patients, most VTEs are provoked, with the most common risk factor being presence of a central line. Frequency of this risk factor varies based on age (>60% of cases in older children and nearly 90% in neonates).1 The most recent American Society of Hematology guidelines recommend treating pediatric symptomatic VTE with anticoagulation and treating asymptomatic VTE instead of observation.2 These recommendations rely on evidence in adult patients due to the current paucity of evidence in pediatrics.
“Pediatric investigation plans” are the cornerstone for ongoing clinical trials of DOACs in pediatrics. While studies evaluating safety and efficacy of standard anticoagulants (UFH, LMWH, and warfarin) in pediatrics exist, clinical trials at the time of drug development did not include pediatric patients. This means none of the currently used anticoagulants were initially developed or approved for children.1 Under the Pediatric Research Equity Act of 2007, the FDA requires pharmaceutical companies to submit a New Drug Application to perform pediatric studies of drugs deemed likely for use in pediatric patients. Pediatric investigation plans allow for establishing safety, efficacy, dosing, and administration routes in pediatric populations. All four DOACs currently approved for treatment of VTE in adults have ongoing efficacy and safety clinical trials for children.
The first and only published clinical trial of DOAC efficacy and safety in pediatrics compared rivaroxaban to standard treatment of acute VTE (Appendix Table).11 The industry-sponsored, open-label EINSTEIN-Jr trial randomized patients aged 0 to 17 years 2:1 to weight-based rivaroxaban or standard treatment after receiving initial parenteral therapy for 5 to 9 days. While most patients were treated for at least 3 months, patients younger than 2 years with line-related thrombosis were treated for only 1 month. The study population mostly consisted of patients with initial, symptomatic, provoked VTE, with types ranging from cerebral venous sinus thrombosis to catheter-associated thrombosis. VTE risk factors, which varied by age, included presence of a central line, major infection, surgery, or trauma. While most VTEs in pediatric patients are expected to be central-line related, in the EINSTEIN-Jr trial only 25.2% of VTEs were central line–associated. The study evaluated symptomatic recurrent VTE (primary efficacy outcome) and clinically relevant bleeding (safety outcome). No significant difference was found between treatment groups in efficacy or safety outcomes, and there were no treatment-related deaths. While the trial was not powered to assess noninferiority due to low incidence of VTE in pediatrics, the absolute number of symptomatic recurrent VTEs was lower in the rivaroxaban group compared with the standard-care group (1% vs 3%). The investigators concluded that rivaroxaban is similarly efficacious and safe in children as compared with adults. FDA approval of rivaroxaban in pediatrics is expected given the trial’s favorable results. Clinicians may wish to consider whether the studied population is comparable with their own patients because the trial had a lower percentage of line-associated VTE than previously reported in the pediatric population.
Multiple clinical trials evaluating the efficacy and safety of other DOACs in pediatric patients are currently underway (Appendix Table).12-14 Apixaban and edoxaban have active multicenter, randomized, open-label clinical trials recruiting patients up to age 17 who have imaging-confirmed acute VTE. A similar trial for dabigatran has recently completed recruitment. Outcome measures include recurrent VTE, VTE-related mortality, and major or clinically relevant non-major bleeding. Like EINSTEIN-Jr, patients in the dabigatran and edoxaban trials were treated with parenteral therapy for at least 5 days prior to randomization.12,14 In the apixaban trial, participants can be randomized without initial parenteral treatment.13 Betrixaban, the newest DOAC approved in adults, does not currently have any open pediatric trials.
AREAS IN NEED OF FUTURE STUDY
Lack of approved reversal agents may initially limit DOAC use in children. An open-label study examining idarucizumab safety has completed enrollment, but it has not yet published results.15 To date, there are no pediatric clinical trials examining andexanet alpha. Future work will need to establish efficacy and safety of reversal agents in pediatrics.
DOACs have not been adequately studied in populations of patients with comorbidities, such as liver disease, renal disease, altered enteral absorption, and BMI higher than 40. Physiologic differences in children with cancer and in neonates merit further evaluation of DOAC safety and efficacy. While ongoing trials established weight-based dosing regimens for children, longitudinal studies will need to ensure adequate anticoagulation, especially in the populations listed here.
The safety outcomes in most DOAC studies include clinically relevant bleeding and VTE-related mortality. These outcomes are much less common in pediatric patients than they are in adults, and future studies may need to expand safety outcomes to those more frequently seen in children. Primary and secondary endpoint variability in pediatric DOAC clinical trials presents challenges interpreting and comparing study results.
SUMMARY
VTE is an increasingly common complication in hospitalized children contributing to significant morbidity.1 For decades, the only treatment options have been UFH, LMWH, or warfarin. DOACs offer many advantages compared with standard anticoagulation options. The only clinical trial evaluating efficacy and safety of DOACs published to date demonstrates that pediatric patients taking rivaroxaban have outcomes similar to those of patients receiving standard care. It is expected that DOACs will gain FDA approval for treatment of VTE in pediatric patients in the near future; therefore, hospitalists should understand indications for use of these medications.
Venous thromboembolism (VTE) is a life-threatening event occurring with increasing frequency in hospitalized children and an incidence of more than 58 events per 10,000 hospitalizations.1 In pediatric patients, VTEs occur less often than in adults, have bimodal peaks in neonates and adolescents, and are typically provoked, with central venous access as the most common risk factor.1,
Treatment of pediatric VTE includes unfractionated heparin (UFH), low-molecular-weight heparin (LMWH), and vitamin K antagonists (ie, warfarin). These agents have limitations, including parenteral administration, frequent lab monitoring, and drug/dietary interactions complicating use. Only recently have there been pediatric studies to assess these agents’ pharmacokinetics, pharmacodynamics, safety, and efficacy.2
Direct oral anticoagulants (DOACs) commonly used to treat VTE in adults have two mechanisms of action: direct thrombin (activated factor II) inhibition (ie, dabigatran) and activated factor X (Xa) inhibition (ie, rivaroxaban, apixaban, edoxaban, betrixaban). DOACs offer practical advantages over and efficacy similar to that of warfarin and heparin products, including oral administration, predictable pharmacology, no required lab monitoring, and fewer drug/dietary interactions. DOACs are already approved for VTE treatment in patients 18 years and older.3
This clinical practice update synthesizes 6 years (2014-2020) of literature regarding DOACs for treatment of VTE, focusing on their current role in patients 18 years and older and their emerging role in pediatric patients.
USE IN ADULTS
DOACs are approved by the US Food and Drug Administration (FDA) for multiple anticoagulation indications in adults, including treatment and prevention of acute VTE and prevention of stroke in nonvalvular atrial fibrillation (Table). DOACs are well tolerated by most adults; however, use in certain populations, including patients with liver disease with coagulopathy, advanced renal disease (creatinine clearance <30 mL/min), and class III obesity (body mass index [BMI] >40 kg/m2), requires caution.4,5 For adult patients with VTE without contraindications, DOACs are considered equivalent to warfarin; current CHEST guidelines even suggest preference of DOACs over warfarin.5 While it is prudent to exercise caution when extrapolating adult data to children, these data have informed ongoing pediatric DOAC clinical trials.
The efficacy and safety of each of the DOACs (aside from betrixaban, which is indicated only for prophylaxis) have compared with warfarin for treatment of VTE in adults.6 A meta-analysis of six clinical trials determined DOACs are noninferior to warfarin for VTE treatment.3 Only two of six trials included patients with provoked VTEs. The meta-analysis found no difference in rates of recurrent symptomatic VTE (primary outcome; relative risk [RR], 0.91; 95% CI, 0.79-1.06) or all-cause mortality (secondary outcome; RR, 0.98; 95% CI, 0.84-1.14). Additionally, DOACs were shown as possibly safer than warfarin due to fewer major bleeding events, particularly fatal bleeding (RR, 0.36; 95% CI, 0.15-0.84) and intracranial bleeding (RR, 0.34; 95% CI, 0.17-0.69). For clinically relevant nonmajor bleeding (eg, gastrointestinal bleeding requiring <2 U packed red blood cells), results were similar (RR, 0.73; 95% CI, 0.58-0.93).
DOACs appear to have effectiveness comparable with that of warfarin. A retrospective matched cohort study of 59,525 patients with acute VTE compared outcomes of patients on DOACs (95% on rivaroxaban) with those of patients on warfarin.6 There were no differences in all-cause mortality or major bleeding. Another retrospective cohort study of 62,431 patients with acute VTE compared rivaroxaban and apixaban with warfarin, as well as rivaroxaban and apixaban with each other.7 There were no differences in 3- and 6-month mortality between warfarin and DOAC users or between rivaroxaban and apixaban users.
Initial approval of DOACs brought concerns about reversibility in the setting of bleeding or urgent procedural need. Clinical practice guidelines, primarily based on observational studies and laboratory parameters in vitro or in healthy volunteers, recommend activated prothrombin complex concentrates as a first-line intervention.8 However, specific agents have now been FDA-approved for DOAC reversal.
Idarucizumab is an FDA-approved (2015) monoclonal antibody with high affinity for dabigatran. Approval was based on a multicenter prospective cohort study of 503 patients taking dabigatran who presented with major bleeding (301 patients) or requiring an urgent surgery (202 patients).9 Idarucizumab resulted in a median time to bleeding cessation of 2.5 hours for those 134 patients in whom time to bleeding cessation could be assessed. Patients with intracranial bleeding were excluded from the timed portion because follow up imaging was not mandated. For those requiring surgery, 93% had normal periprocedural hemostasis.
Andexanet alfa is an FDA-approved (2018) drug for reversal of apixaban and rivaroxaban that acts as a catalytically inactive decoy Xa molecule, binding Xa inhibitors with high affinity. A multicenter prospective cohort study of 352 patients on Xa inhibitors with major bleeding found administration of andexanet alfa resulted in excellent or good hemostasis in 82% of patients (204/249 patients) at 12 hours.10 There was no difference between rivaroxaban and apixaban patients. Both idarucizumab and andexanet alfa remain expensive and not universally available, but availability and use will likely increase with time.
EVIDENCE FOR USE IN CHILDREN
In pediatric patients, most VTEs are provoked, with the most common risk factor being presence of a central line. Frequency of this risk factor varies based on age (>60% of cases in older children and nearly 90% in neonates).1 The most recent American Society of Hematology guidelines recommend treating pediatric symptomatic VTE with anticoagulation and treating asymptomatic VTE instead of observation.2 These recommendations rely on evidence in adult patients due to the current paucity of evidence in pediatrics.
“Pediatric investigation plans” are the cornerstone for ongoing clinical trials of DOACs in pediatrics. While studies evaluating safety and efficacy of standard anticoagulants (UFH, LMWH, and warfarin) in pediatrics exist, clinical trials at the time of drug development did not include pediatric patients. This means none of the currently used anticoagulants were initially developed or approved for children.1 Under the Pediatric Research Equity Act of 2007, the FDA requires pharmaceutical companies to submit a New Drug Application to perform pediatric studies of drugs deemed likely for use in pediatric patients. Pediatric investigation plans allow for establishing safety, efficacy, dosing, and administration routes in pediatric populations. All four DOACs currently approved for treatment of VTE in adults have ongoing efficacy and safety clinical trials for children.
The first and only published clinical trial of DOAC efficacy and safety in pediatrics compared rivaroxaban to standard treatment of acute VTE (Appendix Table).11 The industry-sponsored, open-label EINSTEIN-Jr trial randomized patients aged 0 to 17 years 2:1 to weight-based rivaroxaban or standard treatment after receiving initial parenteral therapy for 5 to 9 days. While most patients were treated for at least 3 months, patients younger than 2 years with line-related thrombosis were treated for only 1 month. The study population mostly consisted of patients with initial, symptomatic, provoked VTE, with types ranging from cerebral venous sinus thrombosis to catheter-associated thrombosis. VTE risk factors, which varied by age, included presence of a central line, major infection, surgery, or trauma. While most VTEs in pediatric patients are expected to be central-line related, in the EINSTEIN-Jr trial only 25.2% of VTEs were central line–associated. The study evaluated symptomatic recurrent VTE (primary efficacy outcome) and clinically relevant bleeding (safety outcome). No significant difference was found between treatment groups in efficacy or safety outcomes, and there were no treatment-related deaths. While the trial was not powered to assess noninferiority due to low incidence of VTE in pediatrics, the absolute number of symptomatic recurrent VTEs was lower in the rivaroxaban group compared with the standard-care group (1% vs 3%). The investigators concluded that rivaroxaban is similarly efficacious and safe in children as compared with adults. FDA approval of rivaroxaban in pediatrics is expected given the trial’s favorable results. Clinicians may wish to consider whether the studied population is comparable with their own patients because the trial had a lower percentage of line-associated VTE than previously reported in the pediatric population.
Multiple clinical trials evaluating the efficacy and safety of other DOACs in pediatric patients are currently underway (Appendix Table).12-14 Apixaban and edoxaban have active multicenter, randomized, open-label clinical trials recruiting patients up to age 17 who have imaging-confirmed acute VTE. A similar trial for dabigatran has recently completed recruitment. Outcome measures include recurrent VTE, VTE-related mortality, and major or clinically relevant non-major bleeding. Like EINSTEIN-Jr, patients in the dabigatran and edoxaban trials were treated with parenteral therapy for at least 5 days prior to randomization.12,14 In the apixaban trial, participants can be randomized without initial parenteral treatment.13 Betrixaban, the newest DOAC approved in adults, does not currently have any open pediatric trials.
AREAS IN NEED OF FUTURE STUDY
Lack of approved reversal agents may initially limit DOAC use in children. An open-label study examining idarucizumab safety has completed enrollment, but it has not yet published results.15 To date, there are no pediatric clinical trials examining andexanet alpha. Future work will need to establish efficacy and safety of reversal agents in pediatrics.
DOACs have not been adequately studied in populations of patients with comorbidities, such as liver disease, renal disease, altered enteral absorption, and BMI higher than 40. Physiologic differences in children with cancer and in neonates merit further evaluation of DOAC safety and efficacy. While ongoing trials established weight-based dosing regimens for children, longitudinal studies will need to ensure adequate anticoagulation, especially in the populations listed here.
The safety outcomes in most DOAC studies include clinically relevant bleeding and VTE-related mortality. These outcomes are much less common in pediatric patients than they are in adults, and future studies may need to expand safety outcomes to those more frequently seen in children. Primary and secondary endpoint variability in pediatric DOAC clinical trials presents challenges interpreting and comparing study results.
SUMMARY
VTE is an increasingly common complication in hospitalized children contributing to significant morbidity.1 For decades, the only treatment options have been UFH, LMWH, or warfarin. DOACs offer many advantages compared with standard anticoagulation options. The only clinical trial evaluating efficacy and safety of DOACs published to date demonstrates that pediatric patients taking rivaroxaban have outcomes similar to those of patients receiving standard care. It is expected that DOACs will gain FDA approval for treatment of VTE in pediatric patients in the near future; therefore, hospitalists should understand indications for use of these medications.
1. Monagle P, Newall F. Management of thrombosis in children and neonates: practical use of anticoagulants in children. Hematology Am Soc Hematol Educ Program. 2018;2018(1):399-404. https://doi.org/10.1182/asheducation-2018.1.399
2. Monagle P, Cuello CA, Augustine C, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: treatment of pediatric venous thromboembolism. Blood Adv. 2018;2(22):3292-3316. https://doi.org/10.1182/bloodadvances.2018024786
3. Gómez-Outes A, Terleira-Fernández AI, Lecumberri R, Suárez-Gea ML, Vargas-Castrillón E. Direct oral anticoagulants in the treatment of acute venous thromboembolism: a systematic review and meta-analysis. Thromb Res. 2014;134(4):774-782. https://doi.org/10.1016/j.thromres.2014.06.020
4. Martin K, Beyer-Westendorf J, Davidson BL, Huisman MV, Sandset PM, Moll S. Use of the direct oral anticoagulants in obese patients: guidance from the SSC of the ISTH. J Thromb Haemost. 2016;14(6):1308-1313. https://doi.org/10.1111/jth.13323
5. Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315-352. https://doi.org/10.1016/j.chest.2015.11.026
6. Jun M, Lix LM, Durand M, et al. Comparative safety of direct oral anticoagulants and warfarin in venous thromboembolism: multicentre, population based, observational study. BMJ. 2017;359:j4323. https://doi.org/10.1136/bmj.j4323
7. Roetker NS, Lutsey PL, Zakai NA, Alonso A, Adam TJ, MacLehose RF. All-cause mortality risk with direct oral anticoagulants and warfarin in the primary treatment of venous thromboembolism. Thromb Haemost. 2018;118(9):1637-1645. https://doi.org/10.1055/s-0038-1668521
8. Hoffman M, Goldstein JN, Levy JH. The impact of prothrombin complex concentrates when treating DOAC-associated bleeding: a review. Int J Emerg Med. 2018;11(1):55. https://doi.org/10.1186/s12245-018-0215-6
9. Pollack CV Jr, Reilly PA, van Ryn J, et al. Idarucizumab for dabigatran reversal - full cohort analysis. N Engl J Med. 2017;377(5):431-441. https://doi.org/10.1056/nejmoa1707278
10. Connolly SJ, Crowther M, Eikelboom JW, et al. Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Engl J Med. 2019;380(14):1326-1335. https://doi.org/10.1056/nejmoa1814051
11. Male C, Lensing AWA, Palumbo JS, et al. Rivaroxaban compared with standard anticoagulants for the treatment of acute venous thromboembolism in children: a randomised, controlled, phase 3 trial. Lancet Haematol. 2020;7(1):e18-e27. https://doi.org/10.1016/s2352-3026(19)30219-4
12. Open label study comparing efficacy and safety of dabigatran etexilate to standard of care in paediatric patients with venous thromboembolism (VTE). ClinicalTrials.gov identifier: NCT01895777. Posted July 11, 2013. Updated July 7, 2020. Accessed September 23, 2020. https://clinicaltrials.gov/ct2/show/NCT01895777
13. Apixaban for the acute treatment of venous thromboembolism in children. ClinicalTrials.gov identifier: NCT02464969. Posted June 8, 2015. Updated September 10, 2020. Accessed September 23, 2020. https://clinicaltrials.gov/ct2/show/NCT02464969
14. Hokusai study in pediatric patients with confirmed venous thromboembolism (VTE). ClinicalTrials.gov identifier: NCT02798471. Posted June 14, 2016. Update March 6, 2020. Accessed September 23, 2020. https://clinicaltrials.gov/ct2/show/NCT02798471
15. Reversal dabigatran anticoagulant effect with idarucizumab. ClinicalTrials.gov Identifier: NCT02815670. Posted June 28, 2016. Updated April 14, 2020. Accessed September 23, 2020. https://clinicaltrials.gov/ct2/show/NCT02815670
1. Monagle P, Newall F. Management of thrombosis in children and neonates: practical use of anticoagulants in children. Hematology Am Soc Hematol Educ Program. 2018;2018(1):399-404. https://doi.org/10.1182/asheducation-2018.1.399
2. Monagle P, Cuello CA, Augustine C, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: treatment of pediatric venous thromboembolism. Blood Adv. 2018;2(22):3292-3316. https://doi.org/10.1182/bloodadvances.2018024786
3. Gómez-Outes A, Terleira-Fernández AI, Lecumberri R, Suárez-Gea ML, Vargas-Castrillón E. Direct oral anticoagulants in the treatment of acute venous thromboembolism: a systematic review and meta-analysis. Thromb Res. 2014;134(4):774-782. https://doi.org/10.1016/j.thromres.2014.06.020
4. Martin K, Beyer-Westendorf J, Davidson BL, Huisman MV, Sandset PM, Moll S. Use of the direct oral anticoagulants in obese patients: guidance from the SSC of the ISTH. J Thromb Haemost. 2016;14(6):1308-1313. https://doi.org/10.1111/jth.13323
5. Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315-352. https://doi.org/10.1016/j.chest.2015.11.026
6. Jun M, Lix LM, Durand M, et al. Comparative safety of direct oral anticoagulants and warfarin in venous thromboembolism: multicentre, population based, observational study. BMJ. 2017;359:j4323. https://doi.org/10.1136/bmj.j4323
7. Roetker NS, Lutsey PL, Zakai NA, Alonso A, Adam TJ, MacLehose RF. All-cause mortality risk with direct oral anticoagulants and warfarin in the primary treatment of venous thromboembolism. Thromb Haemost. 2018;118(9):1637-1645. https://doi.org/10.1055/s-0038-1668521
8. Hoffman M, Goldstein JN, Levy JH. The impact of prothrombin complex concentrates when treating DOAC-associated bleeding: a review. Int J Emerg Med. 2018;11(1):55. https://doi.org/10.1186/s12245-018-0215-6
9. Pollack CV Jr, Reilly PA, van Ryn J, et al. Idarucizumab for dabigatran reversal - full cohort analysis. N Engl J Med. 2017;377(5):431-441. https://doi.org/10.1056/nejmoa1707278
10. Connolly SJ, Crowther M, Eikelboom JW, et al. Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Engl J Med. 2019;380(14):1326-1335. https://doi.org/10.1056/nejmoa1814051
11. Male C, Lensing AWA, Palumbo JS, et al. Rivaroxaban compared with standard anticoagulants for the treatment of acute venous thromboembolism in children: a randomised, controlled, phase 3 trial. Lancet Haematol. 2020;7(1):e18-e27. https://doi.org/10.1016/s2352-3026(19)30219-4
12. Open label study comparing efficacy and safety of dabigatran etexilate to standard of care in paediatric patients with venous thromboembolism (VTE). ClinicalTrials.gov identifier: NCT01895777. Posted July 11, 2013. Updated July 7, 2020. Accessed September 23, 2020. https://clinicaltrials.gov/ct2/show/NCT01895777
13. Apixaban for the acute treatment of venous thromboembolism in children. ClinicalTrials.gov identifier: NCT02464969. Posted June 8, 2015. Updated September 10, 2020. Accessed September 23, 2020. https://clinicaltrials.gov/ct2/show/NCT02464969
14. Hokusai study in pediatric patients with confirmed venous thromboembolism (VTE). ClinicalTrials.gov identifier: NCT02798471. Posted June 14, 2016. Update March 6, 2020. Accessed September 23, 2020. https://clinicaltrials.gov/ct2/show/NCT02798471
15. Reversal dabigatran anticoagulant effect with idarucizumab. ClinicalTrials.gov Identifier: NCT02815670. Posted June 28, 2016. Updated April 14, 2020. Accessed September 23, 2020. https://clinicaltrials.gov/ct2/show/NCT02815670
© 2021 Society of Hospital Medicine
Children’s Hospitals Caring for Adults During a Pandemic: Pragmatic Considerations and Approaches
Health systems around the world have been called upon to expand acute care capacity to manage the current and projected surge of adults with COVID-19, the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1 There has been mixed guidance on how pediatric facilities should consolidate and coordinate pediatric care in a way that optimizes the capacity of hospital beds, staff, and supplies, such as ventilators and medications, for both adults and children in a community.2 Furthermore, if and how these pediatric facilities should expand capacity to care for adult patients safely is uncertain.
For the last 5 years, both Boston Children’s Hospital and Cincinnati Children’s Hospital Medical Center have been caring for specific adult populations in free-standing pediatric hospitals because of the increasing prevalence of young adults with rare, complex, and historically fatal conditions (eg, chromosomal abnormalities). In the past, low life expectancies for children with such conditions contributed to the evolution of specialized care in pediatric health systems that often does not exist in adult health systems. Our teams in Boston and Cincinnati have gained insight into the multifaceted infrastructure and teams necessary to provide safe care for adults hospitalized in a pediatric setting.
In this perspective piece, we will highlight important principles that pediatric facilities and providers should prioritize if they anticipate caring for hospitalized adults during this pandemic. Designing and implementing an adult care model requires iteratively addressing the following key areas: development of a multistakeholder team, system readiness for intensive care unit (ICU) care of adults, institutional situation awareness, scope of practice, staffing considerations, patient safety, and patient populations and special considerations (eg, adults with chronic conditions of childhood onset). With these areas in mind, pediatric facilities should then consider whether they have the capacity to manage hospitalized adults.
DEVELOPMENT OF A MULTISTAKEHOLDER TEAM
Providing care for any hospitalized patient requires engagement with many health system stakeholders. By involving key stakeholders early in the planning process for our adult care model, we were able to anticipate potential obstacles when caring for a unique subset of patients and gain support of multidisciplinary partners. For instance, inclusion of bedside and support staff highlighted specific needs, such as nurses with adult training and a revised formulary to include common adult medications (eg, clopidogrel for adults with a drug-eluting stent).
Responding to the surge of hospitalized adult patients will require increasing hospital capacity.3 In pediatric settings, this will require consideration of innovative care models. These care models may include pediatric systems flexing to care for adult patients. We recommend hospital leaders from both pediatric and adult facilities have formal discussions on the best ways for pediatric facilities to respond to serve their local population. Inclusion of other key stakeholders will ensure factors imperative to the safe care of adults will not be missed.
SYSTEM READINESS FOR ICU CARE OF ADULTS
There were three levels of consideration for the use of our local pediatric ICU for these patients. First, our institutional policies allow care for adults throughout the system, which we describe in more detail later, in the “Scope of Practice” section. Second, our free-standing pediatric hospital ICUs have accreditation for the care of adults. Third, we developed clear guidelines for subspecialists regarding when adults can safely be admitted or transferred to the pediatric ICU.
Responding to a crisis still necessitates establishing a clear care-escalation plan. An initial barrier may be that some systems do not have a pediatric ICU accredited for care of patients above a certain age. During a crisis, however, as hospital volumes and mortalities rise, states may pursue executive orders, as New York State did, that ease these age restrictions.4 Otherwise, we recommend a clear transfer plan to an adult ICU or emergency credentialing and privileging of adult intensivists. Both of these options may pose challenges during a pandemic because adult ICUs will likely be full.
INSTITUTIONAL SITUATION AWARENESS
Institutional situation awareness for the identification and mitigation of risks inherent in adult care in a pediatric setting is essential for patient safety. Tracking of admitted adult patients via our electronic health record (EHR) occurs daily by an adult care–team member. Our adult care teams partner with physician safety officers and attend daily institutional multidisciplinary safety huddles to create a shared mental model for the care of adult patients. Daily huddle reports include discussion regarding the number of admitted adults, review of illness acuity, consultative advice on management, and contingency planning for potential decompensation.5,6 This integration into institutional huddles has been instrumental in proactively identifying hospitalized adults who are at risk for clinical decompensation and mitigating those risks.
Should a pediatric system admit adults to new sites or units, we recommend leveraging preexisting patient safety infrastructure similarly to identify and mitigate risks. If possible, any institutional communication about adult patients should involve adult-trained staff. Mechanisms for tracking patients will depend on local EHRs but are important to guide regular check-ins with providers caring for those patients.
SCOPE OF PRACTICE
Multiple levels of regulation affect a provider’s scope of practice. The most general of these regulations are state guidelines, followed by local institutional policy. Our institutions require consults for older adults—age varies at our specific institutions—by our adult-care team for assessment of risk and comanagement of adult-specific comorbidities. Additionally, we have agreements with our affiliated adult health facilities that allow in-person adult subspecialty consultation.
While state and institutional policies lay the foundation for pediatric systems considering new adult-care models, provider-level considerations are also needed. Often the patient’s age is a primary consideration, but comorbid conditions also affect the provider’s comfort and ability to care for these patients. We urge practitioners to exercise the full range of their capacities, but also to think critically about the ethical scope of one’s practice. As healthcare providers, it is our duty to hold each other accountable, voice concerns, and advocate to increase health system capacity equitably.7 It’s paramount that channels of communication, in-person or virtual, be arranged for supportive adult subspecialist consultation.
STAFFING CONSIDERATIONS
Med-Peds physicians and advanced practice providers are the foundation of the clinical care provided to adults at our institutions. Our Med-Peds providers practice in both the free-standing pediatric hospital and an affiliated adult health system. They offer expertise in adult clinical care and navigate between pediatric and adult systems when the need arises (eg, adult requiring urgent intervention for an acute myocardial infarction). Adult competencies of other staff must be addressed. For example, our cardiac ICUs include nurses with adult clinical care experience because critically ill adults with congenital heart disease are admitted. Advanced Care Life Support (ACLS) training is also required for staff caring for adults throughout the hospital.
There are many ways, even during a crisis, to develop an adult care model in a pediatric setting. Depending on workforce availability, internal medicine, Med-Peds, family medicine, critical care, and emergency medicine physicians could serve on either a primary service or as a consultant to support pediatrics-trained providers in caring for adults should the patient volume and acuity require staffing restructuring. Adult subspecialty access must be addressed. Telehealth may play a significant role in extending clinicians in all of these clinical roles both during the current crisis but also in underresourced settings.8 A clear process and indication for emergency or temporary credentialing and privileging necessitates understanding and addressing such challenges early. Training in adult care, or lack thereof, for other staff, such as nurses and respiratory therapists, is also crucial to consider.
PATIENT SAFETY
Adults are more likely than children to have comorbidities and clinical deterioration while hospitalized. At our institutions, when a rapid response team is called for an adult patient, an adult care–team provider responds to aid in clinical management and determines the appropriate care setting. Additionally, given that the incidence of coronary artery disease increases starting at age 35 years,9 our systems have developed procedures for managing time-sensitive conditions seen more commonly in adults, such as acute myocardial infarction, stroke, and pulmonary embolism. Despite simulation training for pediatric providers and staff, it is clear that implementing these procedures is highly dependent on involvement of the adult care team.
With the urgency of implementation, pediatric systems should consider increasing the number of providers and staff with ACLS training, especially for rapid response and code teams. Many pediatric systems may need to evaluate how their code carts are stocked and ensure they are equipped with appropriate medication dosages and sizes of supplies. Emergent and accessible adult care will be needed, especially for issues with time-to-intervention criteria like acute myocardial infarction and stroke. Hospitalized adults with COVID-19 may also have a higher incidence of arrhythmia, cardiac ischemia, and stroke.10 Consider proactively simulating common COVID-19–related scenarios to build interdisciplinary teamwork in emergency scenarios. Interhospital agreements and pathways exist for sharing medications. Outreach to pharmacies may be indicated to ensure accessibility for medications not commonly found in pediatric systems.
PATIENT POPULATIONS AND SPECIAL CONSIDERATIONS
Our children’s hospitals care for certain adult populations with chronic conditions of childhood origin because of the availability of subspecialty clinical expertise. Our adult care team aids in contingency planning to help determine place of admission (adult vs pediatric hospital) depending on patient clinical needs and system expertise. For instance, an adult with congenital heart disease may have two cardiologists—one for congenital heart disease and one for coronary artery disease. Patients with an acute issue such as new-onset arrhythmia may be admitted to our pediatric hospital; however, for a stroke they would be admitted to the adult hospital.
While important and tempting to address this issue first, creating criteria to determine which patient population to admit should be a last consideration during a pandemic. Consider if the decision to admit should be determined based on COVID-19 infection status. From there, types of conditions thought to be within the purview of pediatric practice can be considered. These include basic infectious diseases pathology (eg, skin/soft-tissue infections and pyelonephritis) and chronic conditions of childhood origin (eg, cystic fibrosis, diabetes, and inflammatory bowel disease), which have specialty providers who could work across an extended age range. Conditions potentially more challenging to safely care for in pediatric facilities include acute cardiac conditions (eg, angina, acute coronary syndrome, and arrhythmias), alcohol withdrawal, end-stage liver or kidney disease, and gastrointestinal bleeds. Considerations need to be made for research protocols and novel therapies only available at adult institutions. Through this whole process, it is especially crucial to note care equity and ensure that all patients have access to the highest attainable care possible.
CONCLUSION
Policymakers at pediatric facilities should think critically about their institution’s capacity to manage adults. In some circumstances, the decision might be to not admit adult patients based on the factors discussed in this paper or other contextual factors of the local healthcare systems. Our role in providing care for adults in pediatric hospitals involves not only ensuring age-appropriate care, but also in supporting patients and other healthcare providers to navigate a fragmented health system. Our adult-care models required building relationships between pediatric and adult health systems. Building these relationships in the setting of crisis can strengthen health systems and healthcare communities beyond the era of COVID-19. Because it’s promoted enhanced collaboration between pediatric and adult facilities, COVID-19 can be a platform to build a better system to support our already vulnerable young adults with chronic conditions of childhood origin for years to come.
1. Cavallo JJ, Donoho DA, Forman HP. Hospital capacity and operations in the coronavirus disease 2019 (COVID-19) Pandemic—planning for the Nth patient. JAMA Health Forum. 2020;1(3):e200345. https://jamanetwork.com/channels/health-forum/fullarticle/2763353. Accessed March 30, 2020.
2. Children’s Hospital Association. Consolidating Pediatric Hospital Care to Increase Capacity for Adults with COVID-19. https://www.childrenshospitals.org/Quality-and-Performance/COVID19/Resources/Consolidating-Pediatric-Hospital-Care-Increase-Capacity-Adults-COVID19. Accessed March 28, 2020.
3. Campbell J. Andrew Cuomo’s order to hospitals: expand capacity or face state takeover. Democrat & Chronicle. April 1, 2020. https://www.democratandchronicle.com/story/news/politics/albany/2020/04/01/coronavirus-cuomo-order-state-hospital-takeover/5100134002/. Accessed April 2, 2020.
4. New York State Education Department, Office of the Professions. COVID-19 Executive Orders. http://www.op.nysed.gov/COVID-19_EO.html. Accessed April 2, 2020.
5. Brady PW, Muething S, Kotagal U, et al. Improving situation awareness to reduce unrecognized clinical deterioration and serious safety events. Pediatrics. 2013;131(1):e298-e308. https://doi.org/10.1542/peds.2012-1364.
6. Conway-Habes EE, Herbst BF, Herbst LA, et al. Using quality improvement to introduce and standardize the National Early Warning Score (NEWS) for adult inpatients at a children’s hospital. Hosp Pediatr. 2017;7(3):156-163. https://doi.org/10.1542/hpeds.2016-0117.
7. Berry JG, Bloom S, Foley S, Palfrey JS. Health inequity in children and youth with chronic health conditions. Pediatrics. 2010;126(Suppl 3):S111-S119. https://doi.org/10.1542/peds.2010-1466D.
8. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020:1357633X20916567. https://doi.org/10.1177/1357633X20916567.
9. Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139-e596. https://doi.org/10.1161/CIR.0000000000000757.
10. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020. https://doi.org/10.1001/jama.2020.2648.
Health systems around the world have been called upon to expand acute care capacity to manage the current and projected surge of adults with COVID-19, the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1 There has been mixed guidance on how pediatric facilities should consolidate and coordinate pediatric care in a way that optimizes the capacity of hospital beds, staff, and supplies, such as ventilators and medications, for both adults and children in a community.2 Furthermore, if and how these pediatric facilities should expand capacity to care for adult patients safely is uncertain.
For the last 5 years, both Boston Children’s Hospital and Cincinnati Children’s Hospital Medical Center have been caring for specific adult populations in free-standing pediatric hospitals because of the increasing prevalence of young adults with rare, complex, and historically fatal conditions (eg, chromosomal abnormalities). In the past, low life expectancies for children with such conditions contributed to the evolution of specialized care in pediatric health systems that often does not exist in adult health systems. Our teams in Boston and Cincinnati have gained insight into the multifaceted infrastructure and teams necessary to provide safe care for adults hospitalized in a pediatric setting.
In this perspective piece, we will highlight important principles that pediatric facilities and providers should prioritize if they anticipate caring for hospitalized adults during this pandemic. Designing and implementing an adult care model requires iteratively addressing the following key areas: development of a multistakeholder team, system readiness for intensive care unit (ICU) care of adults, institutional situation awareness, scope of practice, staffing considerations, patient safety, and patient populations and special considerations (eg, adults with chronic conditions of childhood onset). With these areas in mind, pediatric facilities should then consider whether they have the capacity to manage hospitalized adults.
DEVELOPMENT OF A MULTISTAKEHOLDER TEAM
Providing care for any hospitalized patient requires engagement with many health system stakeholders. By involving key stakeholders early in the planning process for our adult care model, we were able to anticipate potential obstacles when caring for a unique subset of patients and gain support of multidisciplinary partners. For instance, inclusion of bedside and support staff highlighted specific needs, such as nurses with adult training and a revised formulary to include common adult medications (eg, clopidogrel for adults with a drug-eluting stent).
Responding to the surge of hospitalized adult patients will require increasing hospital capacity.3 In pediatric settings, this will require consideration of innovative care models. These care models may include pediatric systems flexing to care for adult patients. We recommend hospital leaders from both pediatric and adult facilities have formal discussions on the best ways for pediatric facilities to respond to serve their local population. Inclusion of other key stakeholders will ensure factors imperative to the safe care of adults will not be missed.
SYSTEM READINESS FOR ICU CARE OF ADULTS
There were three levels of consideration for the use of our local pediatric ICU for these patients. First, our institutional policies allow care for adults throughout the system, which we describe in more detail later, in the “Scope of Practice” section. Second, our free-standing pediatric hospital ICUs have accreditation for the care of adults. Third, we developed clear guidelines for subspecialists regarding when adults can safely be admitted or transferred to the pediatric ICU.
Responding to a crisis still necessitates establishing a clear care-escalation plan. An initial barrier may be that some systems do not have a pediatric ICU accredited for care of patients above a certain age. During a crisis, however, as hospital volumes and mortalities rise, states may pursue executive orders, as New York State did, that ease these age restrictions.4 Otherwise, we recommend a clear transfer plan to an adult ICU or emergency credentialing and privileging of adult intensivists. Both of these options may pose challenges during a pandemic because adult ICUs will likely be full.
INSTITUTIONAL SITUATION AWARENESS
Institutional situation awareness for the identification and mitigation of risks inherent in adult care in a pediatric setting is essential for patient safety. Tracking of admitted adult patients via our electronic health record (EHR) occurs daily by an adult care–team member. Our adult care teams partner with physician safety officers and attend daily institutional multidisciplinary safety huddles to create a shared mental model for the care of adult patients. Daily huddle reports include discussion regarding the number of admitted adults, review of illness acuity, consultative advice on management, and contingency planning for potential decompensation.5,6 This integration into institutional huddles has been instrumental in proactively identifying hospitalized adults who are at risk for clinical decompensation and mitigating those risks.
Should a pediatric system admit adults to new sites or units, we recommend leveraging preexisting patient safety infrastructure similarly to identify and mitigate risks. If possible, any institutional communication about adult patients should involve adult-trained staff. Mechanisms for tracking patients will depend on local EHRs but are important to guide regular check-ins with providers caring for those patients.
SCOPE OF PRACTICE
Multiple levels of regulation affect a provider’s scope of practice. The most general of these regulations are state guidelines, followed by local institutional policy. Our institutions require consults for older adults—age varies at our specific institutions—by our adult-care team for assessment of risk and comanagement of adult-specific comorbidities. Additionally, we have agreements with our affiliated adult health facilities that allow in-person adult subspecialty consultation.
While state and institutional policies lay the foundation for pediatric systems considering new adult-care models, provider-level considerations are also needed. Often the patient’s age is a primary consideration, but comorbid conditions also affect the provider’s comfort and ability to care for these patients. We urge practitioners to exercise the full range of their capacities, but also to think critically about the ethical scope of one’s practice. As healthcare providers, it is our duty to hold each other accountable, voice concerns, and advocate to increase health system capacity equitably.7 It’s paramount that channels of communication, in-person or virtual, be arranged for supportive adult subspecialist consultation.
STAFFING CONSIDERATIONS
Med-Peds physicians and advanced practice providers are the foundation of the clinical care provided to adults at our institutions. Our Med-Peds providers practice in both the free-standing pediatric hospital and an affiliated adult health system. They offer expertise in adult clinical care and navigate between pediatric and adult systems when the need arises (eg, adult requiring urgent intervention for an acute myocardial infarction). Adult competencies of other staff must be addressed. For example, our cardiac ICUs include nurses with adult clinical care experience because critically ill adults with congenital heart disease are admitted. Advanced Care Life Support (ACLS) training is also required for staff caring for adults throughout the hospital.
There are many ways, even during a crisis, to develop an adult care model in a pediatric setting. Depending on workforce availability, internal medicine, Med-Peds, family medicine, critical care, and emergency medicine physicians could serve on either a primary service or as a consultant to support pediatrics-trained providers in caring for adults should the patient volume and acuity require staffing restructuring. Adult subspecialty access must be addressed. Telehealth may play a significant role in extending clinicians in all of these clinical roles both during the current crisis but also in underresourced settings.8 A clear process and indication for emergency or temporary credentialing and privileging necessitates understanding and addressing such challenges early. Training in adult care, or lack thereof, for other staff, such as nurses and respiratory therapists, is also crucial to consider.
PATIENT SAFETY
Adults are more likely than children to have comorbidities and clinical deterioration while hospitalized. At our institutions, when a rapid response team is called for an adult patient, an adult care–team provider responds to aid in clinical management and determines the appropriate care setting. Additionally, given that the incidence of coronary artery disease increases starting at age 35 years,9 our systems have developed procedures for managing time-sensitive conditions seen more commonly in adults, such as acute myocardial infarction, stroke, and pulmonary embolism. Despite simulation training for pediatric providers and staff, it is clear that implementing these procedures is highly dependent on involvement of the adult care team.
With the urgency of implementation, pediatric systems should consider increasing the number of providers and staff with ACLS training, especially for rapid response and code teams. Many pediatric systems may need to evaluate how their code carts are stocked and ensure they are equipped with appropriate medication dosages and sizes of supplies. Emergent and accessible adult care will be needed, especially for issues with time-to-intervention criteria like acute myocardial infarction and stroke. Hospitalized adults with COVID-19 may also have a higher incidence of arrhythmia, cardiac ischemia, and stroke.10 Consider proactively simulating common COVID-19–related scenarios to build interdisciplinary teamwork in emergency scenarios. Interhospital agreements and pathways exist for sharing medications. Outreach to pharmacies may be indicated to ensure accessibility for medications not commonly found in pediatric systems.
PATIENT POPULATIONS AND SPECIAL CONSIDERATIONS
Our children’s hospitals care for certain adult populations with chronic conditions of childhood origin because of the availability of subspecialty clinical expertise. Our adult care team aids in contingency planning to help determine place of admission (adult vs pediatric hospital) depending on patient clinical needs and system expertise. For instance, an adult with congenital heart disease may have two cardiologists—one for congenital heart disease and one for coronary artery disease. Patients with an acute issue such as new-onset arrhythmia may be admitted to our pediatric hospital; however, for a stroke they would be admitted to the adult hospital.
While important and tempting to address this issue first, creating criteria to determine which patient population to admit should be a last consideration during a pandemic. Consider if the decision to admit should be determined based on COVID-19 infection status. From there, types of conditions thought to be within the purview of pediatric practice can be considered. These include basic infectious diseases pathology (eg, skin/soft-tissue infections and pyelonephritis) and chronic conditions of childhood origin (eg, cystic fibrosis, diabetes, and inflammatory bowel disease), which have specialty providers who could work across an extended age range. Conditions potentially more challenging to safely care for in pediatric facilities include acute cardiac conditions (eg, angina, acute coronary syndrome, and arrhythmias), alcohol withdrawal, end-stage liver or kidney disease, and gastrointestinal bleeds. Considerations need to be made for research protocols and novel therapies only available at adult institutions. Through this whole process, it is especially crucial to note care equity and ensure that all patients have access to the highest attainable care possible.
CONCLUSION
Policymakers at pediatric facilities should think critically about their institution’s capacity to manage adults. In some circumstances, the decision might be to not admit adult patients based on the factors discussed in this paper or other contextual factors of the local healthcare systems. Our role in providing care for adults in pediatric hospitals involves not only ensuring age-appropriate care, but also in supporting patients and other healthcare providers to navigate a fragmented health system. Our adult-care models required building relationships between pediatric and adult health systems. Building these relationships in the setting of crisis can strengthen health systems and healthcare communities beyond the era of COVID-19. Because it’s promoted enhanced collaboration between pediatric and adult facilities, COVID-19 can be a platform to build a better system to support our already vulnerable young adults with chronic conditions of childhood origin for years to come.
Health systems around the world have been called upon to expand acute care capacity to manage the current and projected surge of adults with COVID-19, the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1 There has been mixed guidance on how pediatric facilities should consolidate and coordinate pediatric care in a way that optimizes the capacity of hospital beds, staff, and supplies, such as ventilators and medications, for both adults and children in a community.2 Furthermore, if and how these pediatric facilities should expand capacity to care for adult patients safely is uncertain.
For the last 5 years, both Boston Children’s Hospital and Cincinnati Children’s Hospital Medical Center have been caring for specific adult populations in free-standing pediatric hospitals because of the increasing prevalence of young adults with rare, complex, and historically fatal conditions (eg, chromosomal abnormalities). In the past, low life expectancies for children with such conditions contributed to the evolution of specialized care in pediatric health systems that often does not exist in adult health systems. Our teams in Boston and Cincinnati have gained insight into the multifaceted infrastructure and teams necessary to provide safe care for adults hospitalized in a pediatric setting.
In this perspective piece, we will highlight important principles that pediatric facilities and providers should prioritize if they anticipate caring for hospitalized adults during this pandemic. Designing and implementing an adult care model requires iteratively addressing the following key areas: development of a multistakeholder team, system readiness for intensive care unit (ICU) care of adults, institutional situation awareness, scope of practice, staffing considerations, patient safety, and patient populations and special considerations (eg, adults with chronic conditions of childhood onset). With these areas in mind, pediatric facilities should then consider whether they have the capacity to manage hospitalized adults.
DEVELOPMENT OF A MULTISTAKEHOLDER TEAM
Providing care for any hospitalized patient requires engagement with many health system stakeholders. By involving key stakeholders early in the planning process for our adult care model, we were able to anticipate potential obstacles when caring for a unique subset of patients and gain support of multidisciplinary partners. For instance, inclusion of bedside and support staff highlighted specific needs, such as nurses with adult training and a revised formulary to include common adult medications (eg, clopidogrel for adults with a drug-eluting stent).
Responding to the surge of hospitalized adult patients will require increasing hospital capacity.3 In pediatric settings, this will require consideration of innovative care models. These care models may include pediatric systems flexing to care for adult patients. We recommend hospital leaders from both pediatric and adult facilities have formal discussions on the best ways for pediatric facilities to respond to serve their local population. Inclusion of other key stakeholders will ensure factors imperative to the safe care of adults will not be missed.
SYSTEM READINESS FOR ICU CARE OF ADULTS
There were three levels of consideration for the use of our local pediatric ICU for these patients. First, our institutional policies allow care for adults throughout the system, which we describe in more detail later, in the “Scope of Practice” section. Second, our free-standing pediatric hospital ICUs have accreditation for the care of adults. Third, we developed clear guidelines for subspecialists regarding when adults can safely be admitted or transferred to the pediatric ICU.
Responding to a crisis still necessitates establishing a clear care-escalation plan. An initial barrier may be that some systems do not have a pediatric ICU accredited for care of patients above a certain age. During a crisis, however, as hospital volumes and mortalities rise, states may pursue executive orders, as New York State did, that ease these age restrictions.4 Otherwise, we recommend a clear transfer plan to an adult ICU or emergency credentialing and privileging of adult intensivists. Both of these options may pose challenges during a pandemic because adult ICUs will likely be full.
INSTITUTIONAL SITUATION AWARENESS
Institutional situation awareness for the identification and mitigation of risks inherent in adult care in a pediatric setting is essential for patient safety. Tracking of admitted adult patients via our electronic health record (EHR) occurs daily by an adult care–team member. Our adult care teams partner with physician safety officers and attend daily institutional multidisciplinary safety huddles to create a shared mental model for the care of adult patients. Daily huddle reports include discussion regarding the number of admitted adults, review of illness acuity, consultative advice on management, and contingency planning for potential decompensation.5,6 This integration into institutional huddles has been instrumental in proactively identifying hospitalized adults who are at risk for clinical decompensation and mitigating those risks.
Should a pediatric system admit adults to new sites or units, we recommend leveraging preexisting patient safety infrastructure similarly to identify and mitigate risks. If possible, any institutional communication about adult patients should involve adult-trained staff. Mechanisms for tracking patients will depend on local EHRs but are important to guide regular check-ins with providers caring for those patients.
SCOPE OF PRACTICE
Multiple levels of regulation affect a provider’s scope of practice. The most general of these regulations are state guidelines, followed by local institutional policy. Our institutions require consults for older adults—age varies at our specific institutions—by our adult-care team for assessment of risk and comanagement of adult-specific comorbidities. Additionally, we have agreements with our affiliated adult health facilities that allow in-person adult subspecialty consultation.
While state and institutional policies lay the foundation for pediatric systems considering new adult-care models, provider-level considerations are also needed. Often the patient’s age is a primary consideration, but comorbid conditions also affect the provider’s comfort and ability to care for these patients. We urge practitioners to exercise the full range of their capacities, but also to think critically about the ethical scope of one’s practice. As healthcare providers, it is our duty to hold each other accountable, voice concerns, and advocate to increase health system capacity equitably.7 It’s paramount that channels of communication, in-person or virtual, be arranged for supportive adult subspecialist consultation.
STAFFING CONSIDERATIONS
Med-Peds physicians and advanced practice providers are the foundation of the clinical care provided to adults at our institutions. Our Med-Peds providers practice in both the free-standing pediatric hospital and an affiliated adult health system. They offer expertise in adult clinical care and navigate between pediatric and adult systems when the need arises (eg, adult requiring urgent intervention for an acute myocardial infarction). Adult competencies of other staff must be addressed. For example, our cardiac ICUs include nurses with adult clinical care experience because critically ill adults with congenital heart disease are admitted. Advanced Care Life Support (ACLS) training is also required for staff caring for adults throughout the hospital.
There are many ways, even during a crisis, to develop an adult care model in a pediatric setting. Depending on workforce availability, internal medicine, Med-Peds, family medicine, critical care, and emergency medicine physicians could serve on either a primary service or as a consultant to support pediatrics-trained providers in caring for adults should the patient volume and acuity require staffing restructuring. Adult subspecialty access must be addressed. Telehealth may play a significant role in extending clinicians in all of these clinical roles both during the current crisis but also in underresourced settings.8 A clear process and indication for emergency or temporary credentialing and privileging necessitates understanding and addressing such challenges early. Training in adult care, or lack thereof, for other staff, such as nurses and respiratory therapists, is also crucial to consider.
PATIENT SAFETY
Adults are more likely than children to have comorbidities and clinical deterioration while hospitalized. At our institutions, when a rapid response team is called for an adult patient, an adult care–team provider responds to aid in clinical management and determines the appropriate care setting. Additionally, given that the incidence of coronary artery disease increases starting at age 35 years,9 our systems have developed procedures for managing time-sensitive conditions seen more commonly in adults, such as acute myocardial infarction, stroke, and pulmonary embolism. Despite simulation training for pediatric providers and staff, it is clear that implementing these procedures is highly dependent on involvement of the adult care team.
With the urgency of implementation, pediatric systems should consider increasing the number of providers and staff with ACLS training, especially for rapid response and code teams. Many pediatric systems may need to evaluate how their code carts are stocked and ensure they are equipped with appropriate medication dosages and sizes of supplies. Emergent and accessible adult care will be needed, especially for issues with time-to-intervention criteria like acute myocardial infarction and stroke. Hospitalized adults with COVID-19 may also have a higher incidence of arrhythmia, cardiac ischemia, and stroke.10 Consider proactively simulating common COVID-19–related scenarios to build interdisciplinary teamwork in emergency scenarios. Interhospital agreements and pathways exist for sharing medications. Outreach to pharmacies may be indicated to ensure accessibility for medications not commonly found in pediatric systems.
PATIENT POPULATIONS AND SPECIAL CONSIDERATIONS
Our children’s hospitals care for certain adult populations with chronic conditions of childhood origin because of the availability of subspecialty clinical expertise. Our adult care team aids in contingency planning to help determine place of admission (adult vs pediatric hospital) depending on patient clinical needs and system expertise. For instance, an adult with congenital heart disease may have two cardiologists—one for congenital heart disease and one for coronary artery disease. Patients with an acute issue such as new-onset arrhythmia may be admitted to our pediatric hospital; however, for a stroke they would be admitted to the adult hospital.
While important and tempting to address this issue first, creating criteria to determine which patient population to admit should be a last consideration during a pandemic. Consider if the decision to admit should be determined based on COVID-19 infection status. From there, types of conditions thought to be within the purview of pediatric practice can be considered. These include basic infectious diseases pathology (eg, skin/soft-tissue infections and pyelonephritis) and chronic conditions of childhood origin (eg, cystic fibrosis, diabetes, and inflammatory bowel disease), which have specialty providers who could work across an extended age range. Conditions potentially more challenging to safely care for in pediatric facilities include acute cardiac conditions (eg, angina, acute coronary syndrome, and arrhythmias), alcohol withdrawal, end-stage liver or kidney disease, and gastrointestinal bleeds. Considerations need to be made for research protocols and novel therapies only available at adult institutions. Through this whole process, it is especially crucial to note care equity and ensure that all patients have access to the highest attainable care possible.
CONCLUSION
Policymakers at pediatric facilities should think critically about their institution’s capacity to manage adults. In some circumstances, the decision might be to not admit adult patients based on the factors discussed in this paper or other contextual factors of the local healthcare systems. Our role in providing care for adults in pediatric hospitals involves not only ensuring age-appropriate care, but also in supporting patients and other healthcare providers to navigate a fragmented health system. Our adult-care models required building relationships between pediatric and adult health systems. Building these relationships in the setting of crisis can strengthen health systems and healthcare communities beyond the era of COVID-19. Because it’s promoted enhanced collaboration between pediatric and adult facilities, COVID-19 can be a platform to build a better system to support our already vulnerable young adults with chronic conditions of childhood origin for years to come.
1. Cavallo JJ, Donoho DA, Forman HP. Hospital capacity and operations in the coronavirus disease 2019 (COVID-19) Pandemic—planning for the Nth patient. JAMA Health Forum. 2020;1(3):e200345. https://jamanetwork.com/channels/health-forum/fullarticle/2763353. Accessed March 30, 2020.
2. Children’s Hospital Association. Consolidating Pediatric Hospital Care to Increase Capacity for Adults with COVID-19. https://www.childrenshospitals.org/Quality-and-Performance/COVID19/Resources/Consolidating-Pediatric-Hospital-Care-Increase-Capacity-Adults-COVID19. Accessed March 28, 2020.
3. Campbell J. Andrew Cuomo’s order to hospitals: expand capacity or face state takeover. Democrat & Chronicle. April 1, 2020. https://www.democratandchronicle.com/story/news/politics/albany/2020/04/01/coronavirus-cuomo-order-state-hospital-takeover/5100134002/. Accessed April 2, 2020.
4. New York State Education Department, Office of the Professions. COVID-19 Executive Orders. http://www.op.nysed.gov/COVID-19_EO.html. Accessed April 2, 2020.
5. Brady PW, Muething S, Kotagal U, et al. Improving situation awareness to reduce unrecognized clinical deterioration and serious safety events. Pediatrics. 2013;131(1):e298-e308. https://doi.org/10.1542/peds.2012-1364.
6. Conway-Habes EE, Herbst BF, Herbst LA, et al. Using quality improvement to introduce and standardize the National Early Warning Score (NEWS) for adult inpatients at a children’s hospital. Hosp Pediatr. 2017;7(3):156-163. https://doi.org/10.1542/hpeds.2016-0117.
7. Berry JG, Bloom S, Foley S, Palfrey JS. Health inequity in children and youth with chronic health conditions. Pediatrics. 2010;126(Suppl 3):S111-S119. https://doi.org/10.1542/peds.2010-1466D.
8. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020:1357633X20916567. https://doi.org/10.1177/1357633X20916567.
9. Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139-e596. https://doi.org/10.1161/CIR.0000000000000757.
10. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020. https://doi.org/10.1001/jama.2020.2648.
1. Cavallo JJ, Donoho DA, Forman HP. Hospital capacity and operations in the coronavirus disease 2019 (COVID-19) Pandemic—planning for the Nth patient. JAMA Health Forum. 2020;1(3):e200345. https://jamanetwork.com/channels/health-forum/fullarticle/2763353. Accessed March 30, 2020.
2. Children’s Hospital Association. Consolidating Pediatric Hospital Care to Increase Capacity for Adults with COVID-19. https://www.childrenshospitals.org/Quality-and-Performance/COVID19/Resources/Consolidating-Pediatric-Hospital-Care-Increase-Capacity-Adults-COVID19. Accessed March 28, 2020.
3. Campbell J. Andrew Cuomo’s order to hospitals: expand capacity or face state takeover. Democrat & Chronicle. April 1, 2020. https://www.democratandchronicle.com/story/news/politics/albany/2020/04/01/coronavirus-cuomo-order-state-hospital-takeover/5100134002/. Accessed April 2, 2020.
4. New York State Education Department, Office of the Professions. COVID-19 Executive Orders. http://www.op.nysed.gov/COVID-19_EO.html. Accessed April 2, 2020.
5. Brady PW, Muething S, Kotagal U, et al. Improving situation awareness to reduce unrecognized clinical deterioration and serious safety events. Pediatrics. 2013;131(1):e298-e308. https://doi.org/10.1542/peds.2012-1364.
6. Conway-Habes EE, Herbst BF, Herbst LA, et al. Using quality improvement to introduce and standardize the National Early Warning Score (NEWS) for adult inpatients at a children’s hospital. Hosp Pediatr. 2017;7(3):156-163. https://doi.org/10.1542/hpeds.2016-0117.
7. Berry JG, Bloom S, Foley S, Palfrey JS. Health inequity in children and youth with chronic health conditions. Pediatrics. 2010;126(Suppl 3):S111-S119. https://doi.org/10.1542/peds.2010-1466D.
8. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020:1357633X20916567. https://doi.org/10.1177/1357633X20916567.
9. Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139-e596. https://doi.org/10.1161/CIR.0000000000000757.
10. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020. https://doi.org/10.1001/jama.2020.2648.
© 2020 Society of Hospital Medicine