User login
Hemorrhage; bladder laceration during hysterectomy
Hemorrhage; bladder laceration during hysterectomy
A 46-year-old woman reported increasingly frequent and painful menstrual periods to her Gyn. Estrogen-progestin contraceptives were relatively contraindicated because of the patient’s hyp
The patient began to hemorrhage immediately after surgery; nurses informed the Gyn of this multiple times over the next several hours. After 7 hours, the Gyn examined the patient, found that she was in hemorrhagic shock, and advised a hysterectomy was necessary. During surgery, the Gyn lacerated the patient’s bladder twice, which required a urologist to repair. Postoperatively, the patient had a stroke, respiratory failure, and kidney failure.
PATIENT'S CLAIM: The Gyn’s morcellation technique was negligent. He did not respond to the nurses for 7 hours. If he had responded earlier, she might not have lost her uterus. He was also negligent for injuring the patient’s bladder during the second surgery.
PHYSICIAN'S DEFENSE: The case was settled during mediation.
VERDICT: A confidential North Carolina settlement was reached.
Bowel injured during BSO
In 2013, a 52-year-old woman underwent bilateral salpingo-oophorectomy (BSO) performed by a Gyn. Postoperatively, she was found to have a 1.5-cm bowel perforation. After surgical repair, she developed a wound infection and wound breakdown. She was treated with a vacuum-assisted wound closure device. She later developed a ventral hernia and an intra-abdominal abscess leading to a colostomy, which eventually was reversed. At trial, she had a low-output bowel-to-skin fistula and extensive abdominal scarring.
PATIENT'S CLAIM: The surgeon should have known to perform open BSO rather than laparoscopic surgery based on her 3 prior abdominal surgeries that would have left severe adhesions. He caused a perforation and/or thermal injury to the sigmoid colon during the BSO. He should have consulted a general surgeon when encountering the adhesions. The surgeon failed to readmit her on a timely basis for treatment of the suspected bowel injury.
PHYSICIAN'S DEFENSE: The severe adhesions encountered during BSO surgery could not have been predicted; no adhesions were noted during a 2004 surgery. The adhesions precluded procedure completion. He attempted to lyse the adhesions to create a visual field for removing the ovaries but they could not be visualized. After using a harmonic scalpel for lysis, he inspected the bowel portions that he could see and found no thermal injury or perforation.
VERDICT: An Illinois defense verdict was returned.
Multiple injuries after LVH
A woman was found to have a 4-cm uterine fibroid in April 2007. She received medical management.
In May 2008, she reported left lower quadrant pain to her Gyn. A pelvic ultrasound showed an increase in the fibroid’s diameter to 5.8 cm. On December 4 she underwent laparoscopic-assisted vaginal hysterectomy (LVH). The Gyn performed intraoperative cystoscopy. The patient was discharged the following day.
Over the next several weeks, the patient experienced urinary tract symptoms that progressed to rust-colored urine and incontinence. On December 31 she was found to have bilateral vesicovaginal fistulas. By early April 2009, urologists had placed ureteral stents on 2 separate occasions and performed 2 bilateral reimplantation procedures. On April 28, 2009, a urologist placed a stent in the right ureter but was unable to place a stent in the left ureter. The right stent was removed prior to another reconstructive surgery on August 18. Two stents were also placed on August 26 and were removed on October 6. She underwent annual ultrasounds that revealed minimal hydronephrosis. Except for urinary frequency, the patient’s symptoms had subsided by trial.
PATIENT'S CLAIM: The Gyn fell below the standard of care during the LVH when he negligently cauterized and/or burned the patient’s ureters.
PHYSICIAN'S DEFENSE: The Gyn denied negligence. She argued that, following the cystoscopy, both of the patient’s ureteral orifices discharged indigo carmine–stained urine, an indication that there was no injury to the ureters.
VERDICT: A Nevada defense verdict was returned.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Hemorrhage; bladder laceration during hysterectomy
A 46-year-old woman reported increasingly frequent and painful menstrual periods to her Gyn. Estrogen-progestin contraceptives were relatively contraindicated because of the patient’s hyp
The patient began to hemorrhage immediately after surgery; nurses informed the Gyn of this multiple times over the next several hours. After 7 hours, the Gyn examined the patient, found that she was in hemorrhagic shock, and advised a hysterectomy was necessary. During surgery, the Gyn lacerated the patient’s bladder twice, which required a urologist to repair. Postoperatively, the patient had a stroke, respiratory failure, and kidney failure.
PATIENT'S CLAIM: The Gyn’s morcellation technique was negligent. He did not respond to the nurses for 7 hours. If he had responded earlier, she might not have lost her uterus. He was also negligent for injuring the patient’s bladder during the second surgery.
PHYSICIAN'S DEFENSE: The case was settled during mediation.
VERDICT: A confidential North Carolina settlement was reached.
Bowel injured during BSO
In 2013, a 52-year-old woman underwent bilateral salpingo-oophorectomy (BSO) performed by a Gyn. Postoperatively, she was found to have a 1.5-cm bowel perforation. After surgical repair, she developed a wound infection and wound breakdown. She was treated with a vacuum-assisted wound closure device. She later developed a ventral hernia and an intra-abdominal abscess leading to a colostomy, which eventually was reversed. At trial, she had a low-output bowel-to-skin fistula and extensive abdominal scarring.
PATIENT'S CLAIM: The surgeon should have known to perform open BSO rather than laparoscopic surgery based on her 3 prior abdominal surgeries that would have left severe adhesions. He caused a perforation and/or thermal injury to the sigmoid colon during the BSO. He should have consulted a general surgeon when encountering the adhesions. The surgeon failed to readmit her on a timely basis for treatment of the suspected bowel injury.
PHYSICIAN'S DEFENSE: The severe adhesions encountered during BSO surgery could not have been predicted; no adhesions were noted during a 2004 surgery. The adhesions precluded procedure completion. He attempted to lyse the adhesions to create a visual field for removing the ovaries but they could not be visualized. After using a harmonic scalpel for lysis, he inspected the bowel portions that he could see and found no thermal injury or perforation.
VERDICT: An Illinois defense verdict was returned.
Multiple injuries after LVH
A woman was found to have a 4-cm uterine fibroid in April 2007. She received medical management.
In May 2008, she reported left lower quadrant pain to her Gyn. A pelvic ultrasound showed an increase in the fibroid’s diameter to 5.8 cm. On December 4 she underwent laparoscopic-assisted vaginal hysterectomy (LVH). The Gyn performed intraoperative cystoscopy. The patient was discharged the following day.
Over the next several weeks, the patient experienced urinary tract symptoms that progressed to rust-colored urine and incontinence. On December 31 she was found to have bilateral vesicovaginal fistulas. By early April 2009, urologists had placed ureteral stents on 2 separate occasions and performed 2 bilateral reimplantation procedures. On April 28, 2009, a urologist placed a stent in the right ureter but was unable to place a stent in the left ureter. The right stent was removed prior to another reconstructive surgery on August 18. Two stents were also placed on August 26 and were removed on October 6. She underwent annual ultrasounds that revealed minimal hydronephrosis. Except for urinary frequency, the patient’s symptoms had subsided by trial.
PATIENT'S CLAIM: The Gyn fell below the standard of care during the LVH when he negligently cauterized and/or burned the patient’s ureters.
PHYSICIAN'S DEFENSE: The Gyn denied negligence. She argued that, following the cystoscopy, both of the patient’s ureteral orifices discharged indigo carmine–stained urine, an indication that there was no injury to the ureters.
VERDICT: A Nevada defense verdict was returned.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Hemorrhage; bladder laceration during hysterectomy
A 46-year-old woman reported increasingly frequent and painful menstrual periods to her Gyn. Estrogen-progestin contraceptives were relatively contraindicated because of the patient’s hyp
The patient began to hemorrhage immediately after surgery; nurses informed the Gyn of this multiple times over the next several hours. After 7 hours, the Gyn examined the patient, found that she was in hemorrhagic shock, and advised a hysterectomy was necessary. During surgery, the Gyn lacerated the patient’s bladder twice, which required a urologist to repair. Postoperatively, the patient had a stroke, respiratory failure, and kidney failure.
PATIENT'S CLAIM: The Gyn’s morcellation technique was negligent. He did not respond to the nurses for 7 hours. If he had responded earlier, she might not have lost her uterus. He was also negligent for injuring the patient’s bladder during the second surgery.
PHYSICIAN'S DEFENSE: The case was settled during mediation.
VERDICT: A confidential North Carolina settlement was reached.
Bowel injured during BSO
In 2013, a 52-year-old woman underwent bilateral salpingo-oophorectomy (BSO) performed by a Gyn. Postoperatively, she was found to have a 1.5-cm bowel perforation. After surgical repair, she developed a wound infection and wound breakdown. She was treated with a vacuum-assisted wound closure device. She later developed a ventral hernia and an intra-abdominal abscess leading to a colostomy, which eventually was reversed. At trial, she had a low-output bowel-to-skin fistula and extensive abdominal scarring.
PATIENT'S CLAIM: The surgeon should have known to perform open BSO rather than laparoscopic surgery based on her 3 prior abdominal surgeries that would have left severe adhesions. He caused a perforation and/or thermal injury to the sigmoid colon during the BSO. He should have consulted a general surgeon when encountering the adhesions. The surgeon failed to readmit her on a timely basis for treatment of the suspected bowel injury.
PHYSICIAN'S DEFENSE: The severe adhesions encountered during BSO surgery could not have been predicted; no adhesions were noted during a 2004 surgery. The adhesions precluded procedure completion. He attempted to lyse the adhesions to create a visual field for removing the ovaries but they could not be visualized. After using a harmonic scalpel for lysis, he inspected the bowel portions that he could see and found no thermal injury or perforation.
VERDICT: An Illinois defense verdict was returned.
Multiple injuries after LVH
A woman was found to have a 4-cm uterine fibroid in April 2007. She received medical management.
In May 2008, she reported left lower quadrant pain to her Gyn. A pelvic ultrasound showed an increase in the fibroid’s diameter to 5.8 cm. On December 4 she underwent laparoscopic-assisted vaginal hysterectomy (LVH). The Gyn performed intraoperative cystoscopy. The patient was discharged the following day.
Over the next several weeks, the patient experienced urinary tract symptoms that progressed to rust-colored urine and incontinence. On December 31 she was found to have bilateral vesicovaginal fistulas. By early April 2009, urologists had placed ureteral stents on 2 separate occasions and performed 2 bilateral reimplantation procedures. On April 28, 2009, a urologist placed a stent in the right ureter but was unable to place a stent in the left ureter. The right stent was removed prior to another reconstructive surgery on August 18. Two stents were also placed on August 26 and were removed on October 6. She underwent annual ultrasounds that revealed minimal hydronephrosis. Except for urinary frequency, the patient’s symptoms had subsided by trial.
PATIENT'S CLAIM: The Gyn fell below the standard of care during the LVH when he negligently cauterized and/or burned the patient’s ureters.
PHYSICIAN'S DEFENSE: The Gyn denied negligence. She argued that, following the cystoscopy, both of the patient’s ureteral orifices discharged indigo carmine–stained urine, an indication that there was no injury to the ureters.
VERDICT: A Nevada defense verdict was returned.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
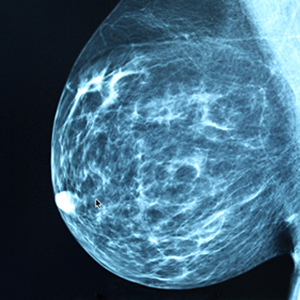
Delayed diagnosis of breast cancer: $15M award
Delayed diagnosis of breast cancer: $15M award
A woman in her mid-50s had been seen by a breast surgeon for 16 years for regular mammograms and sonograms. In May 2009, the breast surgeon misinterpreted a mammogram as negative, as did a radiologist who re-read the mammogram weeks later. In December 2010, the patient returned to the breast surgeon with nipple discharge. No further testing was conducted. In October 2011, the patient was found to have Stage IIIA breast cancer involving 4 lymph nodes. She underwent left radical mastectomy, chemotherapy, radiation therapy, and breast reconstruction. At time of trial, the cancer had invaded her vertebrae, was Stage IV, and most likely incurable.
PATIENT'S CLAIM: Although the surgeon admittedly did not possess the qualifications required under the Mammography Quality Standards Act, he interpreted about 5,000 mammograms per year in his office. In this case, he failed to detect a small breast tumor in May 2009. He also failed to perform testing when the patient reported nipple discharge. A more timely diagnosis of breast cancer at Stage I would have provided a 90% chance of long-term survival.
DEFENDANTS' DEFENSE: The defense held the radiologist fully liable because the surgeon was not a qualified interpreter of mammography, therefore relying on the radiologist’s interpretation. The radiologist was legally responsible for the missed diagnosis.
VERDICT: A $15M New York verdict was reached, finding the breast surgeon 75% at fault and the radiologist 25%. The radiologist settled before the trial (the jury was not informed of this). The breast surgeon was responsible for $11.25M. The defense indicated intent to appeal.
Alleged failure to evacuate uterus after cesarean delivery
A 37-year-old woman underwent cesarean delivery (CD) performed by 2 ObGyns. After delivery, she began to hemorrhage and the uterus became atonic. Hysterectomy was performed but the bleeding did not stop. The ObGyns called in 3 other ObGyns. During exploratory laparotomy, the bleeding was halted.
PATIENT'S CLAIM: She and her husband had hoped to have more children but the hysterectomy precluded that. She sued all 5 ObGyns, alleging that the delivering ObGyns failed to properly perform the CD and that each physician failed to properly perform the laparotomy, causing a large scar. The claim was discontinued against the 3 surgical ObGyns; trial addressed the 2 delivering ObGyns.
The patient’s expert ObGyn remarked that the hemorrhage was caused by a small placental remnant that remained in the uterus as a result of inadequate evacuation following delivery. The presence of the remnant was indicated by the uterine atony and should have prompted immediate investigation. The physicians’ notes did not document exploration of the uterus prior to closure.
PHYSICIAN'S DEFENSE: The defense’s expert contended that atony would not be a result of a small remnant of placenta. The patient’s uterus was properly evacuated, the hemorrhage was an unforeseeable complication, and the ObGyns properly addressed the hemorrhage.
VERDICT: A New York defense verdict was returned.
Alleged bowel injury during hysterectomy
Two days after a woman underwent a hysterectomy performed by her ObGyn, she went to the emergency department with increasing pain. Her ObGyn admitted her to the hospital. A general surgeon performed an exploratory laparotomy the next day that revealed an abscess; a 1-cm perforation of the patient’s bowel was surgically repaired. The patient had a difficult recovery. She developed pneumonia and respiratory failure. She underwent multiple repair surgeries for recurrent abscesses and fistulas because the wound was slow to heal.
PATIENT'S CLAIM: The ObGyn’s surgical technique was negligent. He injured the bowel when inserting a trocar and did not identify the injury in a timely manner. The expert witness commented that such an injury can sometimes be a surgical complication, but not in this case: the ObGyn rushed the procedure because he had another patient waiting for CD at another hospital.
PHYSICIAN'S DEFENSE: The ObGyn denied negligence and contended that the trocar used in surgery was too blunt to have caused a perforation. It would have been obvious to the ObGyn during surgery if a perforation had occurred. The perforation developed days after surgery within an abscess.
VERDICT: A Mississippi defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Delayed diagnosis of breast cancer: $15M award
A woman in her mid-50s had been seen by a breast surgeon for 16 years for regular mammograms and sonograms. In May 2009, the breast surgeon misinterpreted a mammogram as negative, as did a radiologist who re-read the mammogram weeks later. In December 2010, the patient returned to the breast surgeon with nipple discharge. No further testing was conducted. In October 2011, the patient was found to have Stage IIIA breast cancer involving 4 lymph nodes. She underwent left radical mastectomy, chemotherapy, radiation therapy, and breast reconstruction. At time of trial, the cancer had invaded her vertebrae, was Stage IV, and most likely incurable.
PATIENT'S CLAIM: Although the surgeon admittedly did not possess the qualifications required under the Mammography Quality Standards Act, he interpreted about 5,000 mammograms per year in his office. In this case, he failed to detect a small breast tumor in May 2009. He also failed to perform testing when the patient reported nipple discharge. A more timely diagnosis of breast cancer at Stage I would have provided a 90% chance of long-term survival.
DEFENDANTS' DEFENSE: The defense held the radiologist fully liable because the surgeon was not a qualified interpreter of mammography, therefore relying on the radiologist’s interpretation. The radiologist was legally responsible for the missed diagnosis.
VERDICT: A $15M New York verdict was reached, finding the breast surgeon 75% at fault and the radiologist 25%. The radiologist settled before the trial (the jury was not informed of this). The breast surgeon was responsible for $11.25M. The defense indicated intent to appeal.
Alleged failure to evacuate uterus after cesarean delivery
A 37-year-old woman underwent cesarean delivery (CD) performed by 2 ObGyns. After delivery, she began to hemorrhage and the uterus became atonic. Hysterectomy was performed but the bleeding did not stop. The ObGyns called in 3 other ObGyns. During exploratory laparotomy, the bleeding was halted.
PATIENT'S CLAIM: She and her husband had hoped to have more children but the hysterectomy precluded that. She sued all 5 ObGyns, alleging that the delivering ObGyns failed to properly perform the CD and that each physician failed to properly perform the laparotomy, causing a large scar. The claim was discontinued against the 3 surgical ObGyns; trial addressed the 2 delivering ObGyns.
The patient’s expert ObGyn remarked that the hemorrhage was caused by a small placental remnant that remained in the uterus as a result of inadequate evacuation following delivery. The presence of the remnant was indicated by the uterine atony and should have prompted immediate investigation. The physicians’ notes did not document exploration of the uterus prior to closure.
PHYSICIAN'S DEFENSE: The defense’s expert contended that atony would not be a result of a small remnant of placenta. The patient’s uterus was properly evacuated, the hemorrhage was an unforeseeable complication, and the ObGyns properly addressed the hemorrhage.
VERDICT: A New York defense verdict was returned.
Alleged bowel injury during hysterectomy
Two days after a woman underwent a hysterectomy performed by her ObGyn, she went to the emergency department with increasing pain. Her ObGyn admitted her to the hospital. A general surgeon performed an exploratory laparotomy the next day that revealed an abscess; a 1-cm perforation of the patient’s bowel was surgically repaired. The patient had a difficult recovery. She developed pneumonia and respiratory failure. She underwent multiple repair surgeries for recurrent abscesses and fistulas because the wound was slow to heal.
PATIENT'S CLAIM: The ObGyn’s surgical technique was negligent. He injured the bowel when inserting a trocar and did not identify the injury in a timely manner. The expert witness commented that such an injury can sometimes be a surgical complication, but not in this case: the ObGyn rushed the procedure because he had another patient waiting for CD at another hospital.
PHYSICIAN'S DEFENSE: The ObGyn denied negligence and contended that the trocar used in surgery was too blunt to have caused a perforation. It would have been obvious to the ObGyn during surgery if a perforation had occurred. The perforation developed days after surgery within an abscess.
VERDICT: A Mississippi defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Delayed diagnosis of breast cancer: $15M award
A woman in her mid-50s had been seen by a breast surgeon for 16 years for regular mammograms and sonograms. In May 2009, the breast surgeon misinterpreted a mammogram as negative, as did a radiologist who re-read the mammogram weeks later. In December 2010, the patient returned to the breast surgeon with nipple discharge. No further testing was conducted. In October 2011, the patient was found to have Stage IIIA breast cancer involving 4 lymph nodes. She underwent left radical mastectomy, chemotherapy, radiation therapy, and breast reconstruction. At time of trial, the cancer had invaded her vertebrae, was Stage IV, and most likely incurable.
PATIENT'S CLAIM: Although the surgeon admittedly did not possess the qualifications required under the Mammography Quality Standards Act, he interpreted about 5,000 mammograms per year in his office. In this case, he failed to detect a small breast tumor in May 2009. He also failed to perform testing when the patient reported nipple discharge. A more timely diagnosis of breast cancer at Stage I would have provided a 90% chance of long-term survival.
DEFENDANTS' DEFENSE: The defense held the radiologist fully liable because the surgeon was not a qualified interpreter of mammography, therefore relying on the radiologist’s interpretation. The radiologist was legally responsible for the missed diagnosis.
VERDICT: A $15M New York verdict was reached, finding the breast surgeon 75% at fault and the radiologist 25%. The radiologist settled before the trial (the jury was not informed of this). The breast surgeon was responsible for $11.25M. The defense indicated intent to appeal.
Alleged failure to evacuate uterus after cesarean delivery
A 37-year-old woman underwent cesarean delivery (CD) performed by 2 ObGyns. After delivery, she began to hemorrhage and the uterus became atonic. Hysterectomy was performed but the bleeding did not stop. The ObGyns called in 3 other ObGyns. During exploratory laparotomy, the bleeding was halted.
PATIENT'S CLAIM: She and her husband had hoped to have more children but the hysterectomy precluded that. She sued all 5 ObGyns, alleging that the delivering ObGyns failed to properly perform the CD and that each physician failed to properly perform the laparotomy, causing a large scar. The claim was discontinued against the 3 surgical ObGyns; trial addressed the 2 delivering ObGyns.
The patient’s expert ObGyn remarked that the hemorrhage was caused by a small placental remnant that remained in the uterus as a result of inadequate evacuation following delivery. The presence of the remnant was indicated by the uterine atony and should have prompted immediate investigation. The physicians’ notes did not document exploration of the uterus prior to closure.
PHYSICIAN'S DEFENSE: The defense’s expert contended that atony would not be a result of a small remnant of placenta. The patient’s uterus was properly evacuated, the hemorrhage was an unforeseeable complication, and the ObGyns properly addressed the hemorrhage.
VERDICT: A New York defense verdict was returned.
Alleged bowel injury during hysterectomy
Two days after a woman underwent a hysterectomy performed by her ObGyn, she went to the emergency department with increasing pain. Her ObGyn admitted her to the hospital. A general surgeon performed an exploratory laparotomy the next day that revealed an abscess; a 1-cm perforation of the patient’s bowel was surgically repaired. The patient had a difficult recovery. She developed pneumonia and respiratory failure. She underwent multiple repair surgeries for recurrent abscesses and fistulas because the wound was slow to heal.
PATIENT'S CLAIM: The ObGyn’s surgical technique was negligent. He injured the bowel when inserting a trocar and did not identify the injury in a timely manner. The expert witness commented that such an injury can sometimes be a surgical complication, but not in this case: the ObGyn rushed the procedure because he had another patient waiting for CD at another hospital.
PHYSICIAN'S DEFENSE: The ObGyn denied negligence and contended that the trocar used in surgery was too blunt to have caused a perforation. It would have been obvious to the ObGyn during surgery if a perforation had occurred. The perforation developed days after surgery within an abscess.
VERDICT: A Mississippi defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Why did testing stop at EKG—especially given family history? ... More
Why did testing stop at EKG—especially given family history?
AFTER COMPLAINING OF CHEST PAIN, a 37-year-old man underwent an electrocardiogram (EKG) examination. The doctor concluded that the pain was not cardiac in nature. Two years later, the patient died of a sudden cardiac event associated with coronary atherosclerotic disease.
PLAINTIFF’S CLAIM The decedent suffered from high cholesterol and had a family history of cardiac issues, yet no additional testing was performed when the patient’s complaints continued.
THE DEFENSE No information on the defense is available.
VERDICT $3 million settlement.
COMMENT This is déjà vu for me. A colleague of mine had a nearly identical case a few years ago, but the patient died several days later. In the case described here, the high cholesterol and family history were red flags. A normal EKG does not rule out angina. I do wonder what happened, however, in the 2 years between the office visit and the patient’s sudden death. The chest pain at the office visit may well have been non-cardiac, but it appears the jury was not convinced.
2 FPs overlook boy’s proteinuria; delay in Dx costs him a kidney
AN 11-YEAR-OLD BOY underwent a laparoscopic appendectomy that included a urinalysis. Following the surgery, the surgeon notified the family physician (FP) that the patient’s urinalysis showed >300 mg/dL of protein. The result was unusual and required follow-up. The surgeon felt that the urinalysis result might be related to the proximity of the appendicitis to the boy’s ureter. The boy was evaluated on several other occasions by the FP, but no work-up was performed.
Three years later, the boy saw a different FP, who noted that the child had elevated blood pressure and blurry vision—among other symptoms. The boy’s renal function tests were documented as abnormal; however, the patient and his mother were never notified of this. Also, the patient was never referred to a nephrologist or neurologist and there was no intervention for a potential kidney abnormality.
Two years later, an associate of the FP ordered further blood tests that showed a clear abnormality with regard to the integrity of the child’s kidney function. The boy was evaluated at a hospital and diagnosed with end-stage renal disease. He received a kidney transplant 3 months later and requires lifetime medical care as a result of the transplant. The boy will likely require further transplants in 10-year increments.
PLAINTIFF’S CLAIM Both FPs deviated from the accepted standard of care when they failed to order further testing as a result of the abnormal laboratory tests. Earlier intervention may have prolonged the life of the boy’s kidney, thereby postponing the need for kidney replacements.
THE DEFENSE No information on the defense is available.
VERDICT $1.25 million Massachusetts settlement.
COMMENT 300 mg/dL is a significant amount of proteinuria and requires further testing. Why didn’t the FP follow up? Was a summary of the hospitalization sent to him/her? Certainly the diagnosis should have been made by the second FP, and the patient should’ve been referred to a nephrologist. A lawsuit would most likely have been averted had this happened. Delayed diagnosis accounts for a high proportion of malpractice suits against FPs.
Duodenal ulcer mistakenly attributed to Crohn’s disease
A 47-YEAR-OLD MAN with a history of Crohn’s disease began experiencing persistent abdominal pain. He hadn’t had symptoms of his Crohn’s disease in over 12 years. Nevertheless, doctors diagnosed his pain as an aggravation of the disease and gave him treatment based on this diagnosis. In fact, though, the man had an acute duodenal ulcer that had progressed and perforated. The patient underwent 12 surgeries (with complications) and almost 2 years of near-constant hospitalization as a result of the misdiagnosis. He now requires 24-hour care in all aspects of his life.
PLAINTIFF’S CLAIM The doctors were negligent in their failure to consider and diagnose a peptic ulcer when the plaintiff’s symptoms indicated issues other than Crohn’s disease.
THE DEFENSE No information on the defense is available.
VERDICT $28 million Maryland verdict.
COMMENT I suspect this was a tough diagnosis, given the patient’s prior history of Crohn’s disease. We are not told the nature of the abdominal pain. If the patient had classic epigastric pain, peptic ulcer disease should have been investigated. This case serves as a reminder that patients can have more than one disease of an organ system, and it reminds us of the need for a careful history and close follow-up if a complaint does not resolve.
Why did testing stop at EKG—especially given family history?
AFTER COMPLAINING OF CHEST PAIN, a 37-year-old man underwent an electrocardiogram (EKG) examination. The doctor concluded that the pain was not cardiac in nature. Two years later, the patient died of a sudden cardiac event associated with coronary atherosclerotic disease.
PLAINTIFF’S CLAIM The decedent suffered from high cholesterol and had a family history of cardiac issues, yet no additional testing was performed when the patient’s complaints continued.
THE DEFENSE No information on the defense is available.
VERDICT $3 million settlement.
COMMENT This is déjà vu for me. A colleague of mine had a nearly identical case a few years ago, but the patient died several days later. In the case described here, the high cholesterol and family history were red flags. A normal EKG does not rule out angina. I do wonder what happened, however, in the 2 years between the office visit and the patient’s sudden death. The chest pain at the office visit may well have been non-cardiac, but it appears the jury was not convinced.
2 FPs overlook boy’s proteinuria; delay in Dx costs him a kidney
AN 11-YEAR-OLD BOY underwent a laparoscopic appendectomy that included a urinalysis. Following the surgery, the surgeon notified the family physician (FP) that the patient’s urinalysis showed >300 mg/dL of protein. The result was unusual and required follow-up. The surgeon felt that the urinalysis result might be related to the proximity of the appendicitis to the boy’s ureter. The boy was evaluated on several other occasions by the FP, but no work-up was performed.
Three years later, the boy saw a different FP, who noted that the child had elevated blood pressure and blurry vision—among other symptoms. The boy’s renal function tests were documented as abnormal; however, the patient and his mother were never notified of this. Also, the patient was never referred to a nephrologist or neurologist and there was no intervention for a potential kidney abnormality.
Two years later, an associate of the FP ordered further blood tests that showed a clear abnormality with regard to the integrity of the child’s kidney function. The boy was evaluated at a hospital and diagnosed with end-stage renal disease. He received a kidney transplant 3 months later and requires lifetime medical care as a result of the transplant. The boy will likely require further transplants in 10-year increments.
PLAINTIFF’S CLAIM Both FPs deviated from the accepted standard of care when they failed to order further testing as a result of the abnormal laboratory tests. Earlier intervention may have prolonged the life of the boy’s kidney, thereby postponing the need for kidney replacements.
THE DEFENSE No information on the defense is available.
VERDICT $1.25 million Massachusetts settlement.
COMMENT 300 mg/dL is a significant amount of proteinuria and requires further testing. Why didn’t the FP follow up? Was a summary of the hospitalization sent to him/her? Certainly the diagnosis should have been made by the second FP, and the patient should’ve been referred to a nephrologist. A lawsuit would most likely have been averted had this happened. Delayed diagnosis accounts for a high proportion of malpractice suits against FPs.
Duodenal ulcer mistakenly attributed to Crohn’s disease
A 47-YEAR-OLD MAN with a history of Crohn’s disease began experiencing persistent abdominal pain. He hadn’t had symptoms of his Crohn’s disease in over 12 years. Nevertheless, doctors diagnosed his pain as an aggravation of the disease and gave him treatment based on this diagnosis. In fact, though, the man had an acute duodenal ulcer that had progressed and perforated. The patient underwent 12 surgeries (with complications) and almost 2 years of near-constant hospitalization as a result of the misdiagnosis. He now requires 24-hour care in all aspects of his life.
PLAINTIFF’S CLAIM The doctors were negligent in their failure to consider and diagnose a peptic ulcer when the plaintiff’s symptoms indicated issues other than Crohn’s disease.
THE DEFENSE No information on the defense is available.
VERDICT $28 million Maryland verdict.
COMMENT I suspect this was a tough diagnosis, given the patient’s prior history of Crohn’s disease. We are not told the nature of the abdominal pain. If the patient had classic epigastric pain, peptic ulcer disease should have been investigated. This case serves as a reminder that patients can have more than one disease of an organ system, and it reminds us of the need for a careful history and close follow-up if a complaint does not resolve.
Why did testing stop at EKG—especially given family history?
AFTER COMPLAINING OF CHEST PAIN, a 37-year-old man underwent an electrocardiogram (EKG) examination. The doctor concluded that the pain was not cardiac in nature. Two years later, the patient died of a sudden cardiac event associated with coronary atherosclerotic disease.
PLAINTIFF’S CLAIM The decedent suffered from high cholesterol and had a family history of cardiac issues, yet no additional testing was performed when the patient’s complaints continued.
THE DEFENSE No information on the defense is available.
VERDICT $3 million settlement.
COMMENT This is déjà vu for me. A colleague of mine had a nearly identical case a few years ago, but the patient died several days later. In the case described here, the high cholesterol and family history were red flags. A normal EKG does not rule out angina. I do wonder what happened, however, in the 2 years between the office visit and the patient’s sudden death. The chest pain at the office visit may well have been non-cardiac, but it appears the jury was not convinced.
2 FPs overlook boy’s proteinuria; delay in Dx costs him a kidney
AN 11-YEAR-OLD BOY underwent a laparoscopic appendectomy that included a urinalysis. Following the surgery, the surgeon notified the family physician (FP) that the patient’s urinalysis showed >300 mg/dL of protein. The result was unusual and required follow-up. The surgeon felt that the urinalysis result might be related to the proximity of the appendicitis to the boy’s ureter. The boy was evaluated on several other occasions by the FP, but no work-up was performed.
Three years later, the boy saw a different FP, who noted that the child had elevated blood pressure and blurry vision—among other symptoms. The boy’s renal function tests were documented as abnormal; however, the patient and his mother were never notified of this. Also, the patient was never referred to a nephrologist or neurologist and there was no intervention for a potential kidney abnormality.
Two years later, an associate of the FP ordered further blood tests that showed a clear abnormality with regard to the integrity of the child’s kidney function. The boy was evaluated at a hospital and diagnosed with end-stage renal disease. He received a kidney transplant 3 months later and requires lifetime medical care as a result of the transplant. The boy will likely require further transplants in 10-year increments.
PLAINTIFF’S CLAIM Both FPs deviated from the accepted standard of care when they failed to order further testing as a result of the abnormal laboratory tests. Earlier intervention may have prolonged the life of the boy’s kidney, thereby postponing the need for kidney replacements.
THE DEFENSE No information on the defense is available.
VERDICT $1.25 million Massachusetts settlement.
COMMENT 300 mg/dL is a significant amount of proteinuria and requires further testing. Why didn’t the FP follow up? Was a summary of the hospitalization sent to him/her? Certainly the diagnosis should have been made by the second FP, and the patient should’ve been referred to a nephrologist. A lawsuit would most likely have been averted had this happened. Delayed diagnosis accounts for a high proportion of malpractice suits against FPs.
Duodenal ulcer mistakenly attributed to Crohn’s disease
A 47-YEAR-OLD MAN with a history of Crohn’s disease began experiencing persistent abdominal pain. He hadn’t had symptoms of his Crohn’s disease in over 12 years. Nevertheless, doctors diagnosed his pain as an aggravation of the disease and gave him treatment based on this diagnosis. In fact, though, the man had an acute duodenal ulcer that had progressed and perforated. The patient underwent 12 surgeries (with complications) and almost 2 years of near-constant hospitalization as a result of the misdiagnosis. He now requires 24-hour care in all aspects of his life.
PLAINTIFF’S CLAIM The doctors were negligent in their failure to consider and diagnose a peptic ulcer when the plaintiff’s symptoms indicated issues other than Crohn’s disease.
THE DEFENSE No information on the defense is available.
VERDICT $28 million Maryland verdict.
COMMENT I suspect this was a tough diagnosis, given the patient’s prior history of Crohn’s disease. We are not told the nature of the abdominal pain. If the patient had classic epigastric pain, peptic ulcer disease should have been investigated. This case serves as a reminder that patients can have more than one disease of an organ system, and it reminds us of the need for a careful history and close follow-up if a complaint does not resolve.
Large scar after multiple procedures
Large scar after multiple procedures
A woman with a history of 3 cesarean deliveries, a tubal ligation reversal, and an abdominoplasty discussed treatment for a large uterine fibroid with her ObGyn. She wanted to avoid a large scar. The ObGyn informed the patient that a laparoscopic hysterectomy could not be promised until her pelvic area was inspected to see if minimally invasive surgery safely could be performed.
During surgery, the ObGyn discovered that pelvic adhesions had distorted the patient’s anatomy; he converted to laparotomy, which left a larger scar.
Two days after surgery, the patient was found to have a bowel injury and underwent additional surgery that included placement of surgical mesh, leaving an enlarged scar.
PATIENT'S CLAIM:
The ObGyn was negligent in injuring the patient’s bowel during hysterectomy and not detecting the injury intraoperatively. Her scars were larger because of the additional repair operation.
PHYSICIAN'S DEFENSE:
Bowel injury is a known complication of the procedure. Many bowel injuries are not detected intraoperatively. The ObGyn made every effort to prevent and check for injury during the procedure.
VERDICT:
An Illinois defense verdict was returned.
Uterus and bowel injured during D&C: $1.5M verdict
A 56-year-old woman underwent hysteroscopy and dilation and curettage (D&C). During the procedure, the gynecologist recognized that he had perforated the uterus and injured the bowel and called in a general surgeon to resect 5 cm of the bowel and repair the uterus.
PATIENT'S CLAIM:
The patient has a large abdominal scar and a chronically distended abdomen. She experienced a year of daily pain and suffering. The D&C was unnecessary and improperly performed: the standard of care is for the gynecologist to operate in a gentle manner; that did not occur.
PHYSICIAN'S DEFENSE:
The D&C was medically necessary. The gynecologist exercised the proper standard of care.
VERDICT:
A $1.5 million New Jersey verdict was returned. The jury found the D&C necessary, but determined that the gynecologist deviated from the accepted standard of care in his performance of the procedure.
Injured ureter allegedly not treated
On December 6, a 42-year-old woman underwent hysterectomy. Postoperatively, she reported increasing dysuria with pain and fever.
On December 13, a computed tomography (CT) scan suggested a partial ureter obstruction. Despite test results, the gynecologist elected to continue to monitor the patient.
The patient’s symptoms continued to worsen and, on December 27, she underwent a second CT scan that identified an obstructed ureter. The gynecologist referred the patient to a urologist, who determined that the patient had sustained a significant ureter injury that required placement of a nephrostomy tube.
PATIENT'S CLAIM:
The gynecologist failed to identify the injury during surgery. The gynecologist was negligent in not consulting a urologist after results of the first CT scan.
PHYSICIAN'S DEFENSE:
Uterine injury is a known complication of the procedure. The gynecologist inspected adjacent organs during surgery but did not find an injury. Postoperative treatment was appropriate.
VERDICT:
The case was presented before a medical review board that concluded that there was no error after the first injury, there was no duty to trace the ureter, and a urology consult was not required after the first CT scan. A Louisiana defense verdict was returned.
Was FHR properly monitored?
After a failed nonstress test, a mother was admitted to triage for blood pressure monitoring. Fetal heart-rate (FHR) monitoring was discontinued at that time. Later that day, FHR monitoring was resumed, fetal distress was detected, and an emergency cesarean delivery was performed. Placental abruption resulted in hypoxia in the baby; she received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The pregnancy was at high risk because of the mother’s hypertension. The ObGyns misread the FHR at admission and discontinued FHR monitoring too early. If continuous FHR monitoring had occurred, fetal distress would have been detected earlier, resulting in a better outcome for the baby.
PHYSICIAN'S DEFENSE:
There were no signs of fetal distress when the FHR monitoring was discontinued. Placental abruption is an acute event that cannot be predicted.
VERDICT:
A Missouri defense verdict was returned.
Should the ObGyn have come to the hospital earlier?
At 39 weeks’ gestation, a mother arrived at the hospital for induction of labor. That evening, the ObGyn, who was not at the hospital, was notified that the mother had an elevated temperature and that the FHR indicated tachycardia. The ObGyn prescribed antibiotics, and the fever subsided. After an hour, the patient was fully dilated and started to push under a nurse’s supervision. Twenty minutes later, the ObGyn was notified that the fetus was experiencing variable decelerations. The ObGyn arrived in 30 minutes and ordered a cesarean delivery. The baby was born 24 minutes later.
The baby began to have seizures 10 hours after birth. He was transferred to another hospital and remained in the neonatal intensive care unit for 15 days. The child received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The ObGyn was negligent in not coming to the hospital when the mother was feverish and the fetus tachycardic. The baby experienced an acute hypoxic ischemic injury; an earlier cesarean delivery would have avoided brain injury.
PHYSICIAN'S DEFENSE:
There was no negligence. The infant did not meet all the criteria for an acute hypoxic ischemic injury. Based on a computed tomography scan taken after the seizures began, the infant’s brain injury most likely occurred hours before birth.
VERDICT:
A Virginia defense verdict was returned.
Large scar after multiple procedures
A woman with a history of 3 cesarean deliveries, a tubal ligation reversal, and an abdominoplasty discussed treatment for a large uterine fibroid with her ObGyn. She wanted to avoid a large scar. The ObGyn informed the patient that a laparoscopic hysterectomy could not be promised until her pelvic area was inspected to see if minimally invasive surgery safely could be performed.
During surgery, the ObGyn discovered that pelvic adhesions had distorted the patient’s anatomy; he converted to laparotomy, which left a larger scar.
Two days after surgery, the patient was found to have a bowel injury and underwent additional surgery that included placement of surgical mesh, leaving an enlarged scar.
PATIENT'S CLAIM:
The ObGyn was negligent in injuring the patient’s bowel during hysterectomy and not detecting the injury intraoperatively. Her scars were larger because of the additional repair operation.
PHYSICIAN'S DEFENSE:
Bowel injury is a known complication of the procedure. Many bowel injuries are not detected intraoperatively. The ObGyn made every effort to prevent and check for injury during the procedure.
VERDICT:
An Illinois defense verdict was returned.
Uterus and bowel injured during D&C: $1.5M verdict
A 56-year-old woman underwent hysteroscopy and dilation and curettage (D&C). During the procedure, the gynecologist recognized that he had perforated the uterus and injured the bowel and called in a general surgeon to resect 5 cm of the bowel and repair the uterus.
PATIENT'S CLAIM:
The patient has a large abdominal scar and a chronically distended abdomen. She experienced a year of daily pain and suffering. The D&C was unnecessary and improperly performed: the standard of care is for the gynecologist to operate in a gentle manner; that did not occur.
PHYSICIAN'S DEFENSE:
The D&C was medically necessary. The gynecologist exercised the proper standard of care.
VERDICT:
A $1.5 million New Jersey verdict was returned. The jury found the D&C necessary, but determined that the gynecologist deviated from the accepted standard of care in his performance of the procedure.
Injured ureter allegedly not treated
On December 6, a 42-year-old woman underwent hysterectomy. Postoperatively, she reported increasing dysuria with pain and fever.
On December 13, a computed tomography (CT) scan suggested a partial ureter obstruction. Despite test results, the gynecologist elected to continue to monitor the patient.
The patient’s symptoms continued to worsen and, on December 27, she underwent a second CT scan that identified an obstructed ureter. The gynecologist referred the patient to a urologist, who determined that the patient had sustained a significant ureter injury that required placement of a nephrostomy tube.
PATIENT'S CLAIM:
The gynecologist failed to identify the injury during surgery. The gynecologist was negligent in not consulting a urologist after results of the first CT scan.
PHYSICIAN'S DEFENSE:
Uterine injury is a known complication of the procedure. The gynecologist inspected adjacent organs during surgery but did not find an injury. Postoperative treatment was appropriate.
VERDICT:
The case was presented before a medical review board that concluded that there was no error after the first injury, there was no duty to trace the ureter, and a urology consult was not required after the first CT scan. A Louisiana defense verdict was returned.
Was FHR properly monitored?
After a failed nonstress test, a mother was admitted to triage for blood pressure monitoring. Fetal heart-rate (FHR) monitoring was discontinued at that time. Later that day, FHR monitoring was resumed, fetal distress was detected, and an emergency cesarean delivery was performed. Placental abruption resulted in hypoxia in the baby; she received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The pregnancy was at high risk because of the mother’s hypertension. The ObGyns misread the FHR at admission and discontinued FHR monitoring too early. If continuous FHR monitoring had occurred, fetal distress would have been detected earlier, resulting in a better outcome for the baby.
PHYSICIAN'S DEFENSE:
There were no signs of fetal distress when the FHR monitoring was discontinued. Placental abruption is an acute event that cannot be predicted.
VERDICT:
A Missouri defense verdict was returned.
Should the ObGyn have come to the hospital earlier?
At 39 weeks’ gestation, a mother arrived at the hospital for induction of labor. That evening, the ObGyn, who was not at the hospital, was notified that the mother had an elevated temperature and that the FHR indicated tachycardia. The ObGyn prescribed antibiotics, and the fever subsided. After an hour, the patient was fully dilated and started to push under a nurse’s supervision. Twenty minutes later, the ObGyn was notified that the fetus was experiencing variable decelerations. The ObGyn arrived in 30 minutes and ordered a cesarean delivery. The baby was born 24 minutes later.
The baby began to have seizures 10 hours after birth. He was transferred to another hospital and remained in the neonatal intensive care unit for 15 days. The child received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The ObGyn was negligent in not coming to the hospital when the mother was feverish and the fetus tachycardic. The baby experienced an acute hypoxic ischemic injury; an earlier cesarean delivery would have avoided brain injury.
PHYSICIAN'S DEFENSE:
There was no negligence. The infant did not meet all the criteria for an acute hypoxic ischemic injury. Based on a computed tomography scan taken after the seizures began, the infant’s brain injury most likely occurred hours before birth.
VERDICT:
A Virginia defense verdict was returned.
Large scar after multiple procedures
A woman with a history of 3 cesarean deliveries, a tubal ligation reversal, and an abdominoplasty discussed treatment for a large uterine fibroid with her ObGyn. She wanted to avoid a large scar. The ObGyn informed the patient that a laparoscopic hysterectomy could not be promised until her pelvic area was inspected to see if minimally invasive surgery safely could be performed.
During surgery, the ObGyn discovered that pelvic adhesions had distorted the patient’s anatomy; he converted to laparotomy, which left a larger scar.
Two days after surgery, the patient was found to have a bowel injury and underwent additional surgery that included placement of surgical mesh, leaving an enlarged scar.
PATIENT'S CLAIM:
The ObGyn was negligent in injuring the patient’s bowel during hysterectomy and not detecting the injury intraoperatively. Her scars were larger because of the additional repair operation.
PHYSICIAN'S DEFENSE:
Bowel injury is a known complication of the procedure. Many bowel injuries are not detected intraoperatively. The ObGyn made every effort to prevent and check for injury during the procedure.
VERDICT:
An Illinois defense verdict was returned.
Uterus and bowel injured during D&C: $1.5M verdict
A 56-year-old woman underwent hysteroscopy and dilation and curettage (D&C). During the procedure, the gynecologist recognized that he had perforated the uterus and injured the bowel and called in a general surgeon to resect 5 cm of the bowel and repair the uterus.
PATIENT'S CLAIM:
The patient has a large abdominal scar and a chronically distended abdomen. She experienced a year of daily pain and suffering. The D&C was unnecessary and improperly performed: the standard of care is for the gynecologist to operate in a gentle manner; that did not occur.
PHYSICIAN'S DEFENSE:
The D&C was medically necessary. The gynecologist exercised the proper standard of care.
VERDICT:
A $1.5 million New Jersey verdict was returned. The jury found the D&C necessary, but determined that the gynecologist deviated from the accepted standard of care in his performance of the procedure.
Injured ureter allegedly not treated
On December 6, a 42-year-old woman underwent hysterectomy. Postoperatively, she reported increasing dysuria with pain and fever.
On December 13, a computed tomography (CT) scan suggested a partial ureter obstruction. Despite test results, the gynecologist elected to continue to monitor the patient.
The patient’s symptoms continued to worsen and, on December 27, she underwent a second CT scan that identified an obstructed ureter. The gynecologist referred the patient to a urologist, who determined that the patient had sustained a significant ureter injury that required placement of a nephrostomy tube.
PATIENT'S CLAIM:
The gynecologist failed to identify the injury during surgery. The gynecologist was negligent in not consulting a urologist after results of the first CT scan.
PHYSICIAN'S DEFENSE:
Uterine injury is a known complication of the procedure. The gynecologist inspected adjacent organs during surgery but did not find an injury. Postoperative treatment was appropriate.
VERDICT:
The case was presented before a medical review board that concluded that there was no error after the first injury, there was no duty to trace the ureter, and a urology consult was not required after the first CT scan. A Louisiana defense verdict was returned.
Was FHR properly monitored?
After a failed nonstress test, a mother was admitted to triage for blood pressure monitoring. Fetal heart-rate (FHR) monitoring was discontinued at that time. Later that day, FHR monitoring was resumed, fetal distress was detected, and an emergency cesarean delivery was performed. Placental abruption resulted in hypoxia in the baby; she received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The pregnancy was at high risk because of the mother’s hypertension. The ObGyns misread the FHR at admission and discontinued FHR monitoring too early. If continuous FHR monitoring had occurred, fetal distress would have been detected earlier, resulting in a better outcome for the baby.
PHYSICIAN'S DEFENSE:
There were no signs of fetal distress when the FHR monitoring was discontinued. Placental abruption is an acute event that cannot be predicted.
VERDICT:
A Missouri defense verdict was returned.
Should the ObGyn have come to the hospital earlier?
At 39 weeks’ gestation, a mother arrived at the hospital for induction of labor. That evening, the ObGyn, who was not at the hospital, was notified that the mother had an elevated temperature and that the FHR indicated tachycardia. The ObGyn prescribed antibiotics, and the fever subsided. After an hour, the patient was fully dilated and started to push under a nurse’s supervision. Twenty minutes later, the ObGyn was notified that the fetus was experiencing variable decelerations. The ObGyn arrived in 30 minutes and ordered a cesarean delivery. The baby was born 24 minutes later.
The baby began to have seizures 10 hours after birth. He was transferred to another hospital and remained in the neonatal intensive care unit for 15 days. The child received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The ObGyn was negligent in not coming to the hospital when the mother was feverish and the fetus tachycardic. The baby experienced an acute hypoxic ischemic injury; an earlier cesarean delivery would have avoided brain injury.
PHYSICIAN'S DEFENSE:
There was no negligence. The infant did not meet all the criteria for an acute hypoxic ischemic injury. Based on a computed tomography scan taken after the seizures began, the infant’s brain injury most likely occurred hours before birth.
VERDICT:
A Virginia defense verdict was returned.