User login
The ongoing search for answers
Hidden in the Dec. 1, 2022, issue of the New England Journal of Medicine was a small article on using deferiprone for Parkinson’s disease.
The idea behind it makes sense. A key factor in Parkinson’s disease is a loss of cells in the substantia nigra. The cells that have been lost have a build-up of iron content, suggesting that iron contributes to their demise. Therefore, maybe using an iron chelating agent to remove it may help.
Like I said, it makes sense.
Unfortunately, it didn’t quite work that way. In spite of a clear reduction of nigrostriatal iron, compared with the placebo group, the treated patients had worse MDS-UPDRS scores over 36 weeks than those on the placebo.
Back to the drawing board.
I’m not criticizing the people who did the study – it seemed like a reasonable hypothesis, and testing it is the only way we find out if it’s correct. We learn just as much, if not more, from a negative study as from a positive one, incrementally working toward the answer with each.
We face the same thing with the amyloid theory in Alzheimer’s disease. Getting rid of amyloid should fix the problem.
But it doesn’t, at least not completely. Even lecanemab, the latest-and-greatest of treatments, only shows a 27% slowing in disease progression. This is certainly meaningful – I’m not knocking it – but we’re still far from a cure. To date we haven’t even stopped disease progression, let alone reversed it.
Although the new drugs have a remarkable mechanism of action, the clinical results aren’t nearly as good as one would expect if amyloid was the whole issue.
Which, at this point, it probably isn’t, anymore than nigrostriatal iron deposition is the sole cause of Parkinson’s disease.
Right now we’re better able to find planets 27,700 light years away (SWEEPS-11) than we are at knowing the cause of neuronal changes in the person sitting across the desk from us. That’s not saying we won’t have the answers someday, it just means we don’t have them now.
I was in my 3rd year of medical school in January of 1992, (surgery rotation at the Omaha VA, to be specific) when the first definitive planet outside our solar system was identified. Today, 31 years later, the number of exoplanets stands at 5,297.
But the laws of physics are generally a lot more predictable than those of biology.
That doesn’t mean we won’t find the answers, or more effective treatments, eventually. But it will take more time, work, and studies – with both positive and negative results – to get there.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Hidden in the Dec. 1, 2022, issue of the New England Journal of Medicine was a small article on using deferiprone for Parkinson’s disease.
The idea behind it makes sense. A key factor in Parkinson’s disease is a loss of cells in the substantia nigra. The cells that have been lost have a build-up of iron content, suggesting that iron contributes to their demise. Therefore, maybe using an iron chelating agent to remove it may help.
Like I said, it makes sense.
Unfortunately, it didn’t quite work that way. In spite of a clear reduction of nigrostriatal iron, compared with the placebo group, the treated patients had worse MDS-UPDRS scores over 36 weeks than those on the placebo.
Back to the drawing board.
I’m not criticizing the people who did the study – it seemed like a reasonable hypothesis, and testing it is the only way we find out if it’s correct. We learn just as much, if not more, from a negative study as from a positive one, incrementally working toward the answer with each.
We face the same thing with the amyloid theory in Alzheimer’s disease. Getting rid of amyloid should fix the problem.
But it doesn’t, at least not completely. Even lecanemab, the latest-and-greatest of treatments, only shows a 27% slowing in disease progression. This is certainly meaningful – I’m not knocking it – but we’re still far from a cure. To date we haven’t even stopped disease progression, let alone reversed it.
Although the new drugs have a remarkable mechanism of action, the clinical results aren’t nearly as good as one would expect if amyloid was the whole issue.
Which, at this point, it probably isn’t, anymore than nigrostriatal iron deposition is the sole cause of Parkinson’s disease.
Right now we’re better able to find planets 27,700 light years away (SWEEPS-11) than we are at knowing the cause of neuronal changes in the person sitting across the desk from us. That’s not saying we won’t have the answers someday, it just means we don’t have them now.
I was in my 3rd year of medical school in January of 1992, (surgery rotation at the Omaha VA, to be specific) when the first definitive planet outside our solar system was identified. Today, 31 years later, the number of exoplanets stands at 5,297.
But the laws of physics are generally a lot more predictable than those of biology.
That doesn’t mean we won’t find the answers, or more effective treatments, eventually. But it will take more time, work, and studies – with both positive and negative results – to get there.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Hidden in the Dec. 1, 2022, issue of the New England Journal of Medicine was a small article on using deferiprone for Parkinson’s disease.
The idea behind it makes sense. A key factor in Parkinson’s disease is a loss of cells in the substantia nigra. The cells that have been lost have a build-up of iron content, suggesting that iron contributes to their demise. Therefore, maybe using an iron chelating agent to remove it may help.
Like I said, it makes sense.
Unfortunately, it didn’t quite work that way. In spite of a clear reduction of nigrostriatal iron, compared with the placebo group, the treated patients had worse MDS-UPDRS scores over 36 weeks than those on the placebo.
Back to the drawing board.
I’m not criticizing the people who did the study – it seemed like a reasonable hypothesis, and testing it is the only way we find out if it’s correct. We learn just as much, if not more, from a negative study as from a positive one, incrementally working toward the answer with each.
We face the same thing with the amyloid theory in Alzheimer’s disease. Getting rid of amyloid should fix the problem.
But it doesn’t, at least not completely. Even lecanemab, the latest-and-greatest of treatments, only shows a 27% slowing in disease progression. This is certainly meaningful – I’m not knocking it – but we’re still far from a cure. To date we haven’t even stopped disease progression, let alone reversed it.
Although the new drugs have a remarkable mechanism of action, the clinical results aren’t nearly as good as one would expect if amyloid was the whole issue.
Which, at this point, it probably isn’t, anymore than nigrostriatal iron deposition is the sole cause of Parkinson’s disease.
Right now we’re better able to find planets 27,700 light years away (SWEEPS-11) than we are at knowing the cause of neuronal changes in the person sitting across the desk from us. That’s not saying we won’t have the answers someday, it just means we don’t have them now.
I was in my 3rd year of medical school in January of 1992, (surgery rotation at the Omaha VA, to be specific) when the first definitive planet outside our solar system was identified. Today, 31 years later, the number of exoplanets stands at 5,297.
But the laws of physics are generally a lot more predictable than those of biology.
That doesn’t mean we won’t find the answers, or more effective treatments, eventually. But it will take more time, work, and studies – with both positive and negative results – to get there.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Holding out hope for ambroxol
How many of you hadn’t heard of ambroxol until the last few weeks?
How many of you have gotten at least one call asking for a prescription for it in that time?
I’ll raise my hand on both accounts.
Ambroxol seems relatively innocuous – an over-the-counter cold medication commonly used on planet Earth (though not approved in the U.S. for whatever reason). But in the last few years some interesting data have cropped up that it may help with Parkinson’s disease.
“May” being the key word here.
Now, I’m not saying it will or won’t do something. The trials that are being started will show that. It would be totally awesome if it did.
But we’ve been here before: The hope that some old, inexpensive, and widely available medication would turn out to have an amazing benefit we didn’t anticipate. We saw this with hydroxychloroquine and ivermectin during the pandemic. Before that we saw all kinds of speculative ideas that statins would be effective for diseases from multiple sclerosis to Alzheimer’s disease.
And, as with many incurable diseases, patients and their families are hoping for a breakthrough. We have plenty of treatments for Parkinson’s disease, but no cures yet. So any potentially effective drug news makes the rounds quickly on news sites, patient advocacy sites, Facebook, and others.
Like the childrens’ telephone game, each time the story is repeated it changes a bit. We’ve gone from an article saying the drug is starting clinical trials to see if it works, to it being a cure now on the marketplace.
Which is when people start calling my office. Most are disappointed to learn that its benefit (if any) is unknown and that it’s not even available. A few get confrontational, accusing me of withholding treatment, when “everyone knows” the drug works.
Believe me, if I had a cure I’d be thrilled to be able to offer it.
I understand that patients and families want a cure.
I understand hope.
I want ambroxol to work for Parkinson’s disease and make a huge difference in the lives of those affected by it. Maybe it will. Or maybe it won’t.
But these things take time to figure out. None of the amazing medications and hi-tech toys we have came about overnight. They were all years in the making.
That’s how science works, and medicine is as much a science as an art.
The art is being able to explain this to patients, and still allow them to hope.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How many of you hadn’t heard of ambroxol until the last few weeks?
How many of you have gotten at least one call asking for a prescription for it in that time?
I’ll raise my hand on both accounts.
Ambroxol seems relatively innocuous – an over-the-counter cold medication commonly used on planet Earth (though not approved in the U.S. for whatever reason). But in the last few years some interesting data have cropped up that it may help with Parkinson’s disease.
“May” being the key word here.
Now, I’m not saying it will or won’t do something. The trials that are being started will show that. It would be totally awesome if it did.
But we’ve been here before: The hope that some old, inexpensive, and widely available medication would turn out to have an amazing benefit we didn’t anticipate. We saw this with hydroxychloroquine and ivermectin during the pandemic. Before that we saw all kinds of speculative ideas that statins would be effective for diseases from multiple sclerosis to Alzheimer’s disease.
And, as with many incurable diseases, patients and their families are hoping for a breakthrough. We have plenty of treatments for Parkinson’s disease, but no cures yet. So any potentially effective drug news makes the rounds quickly on news sites, patient advocacy sites, Facebook, and others.
Like the childrens’ telephone game, each time the story is repeated it changes a bit. We’ve gone from an article saying the drug is starting clinical trials to see if it works, to it being a cure now on the marketplace.
Which is when people start calling my office. Most are disappointed to learn that its benefit (if any) is unknown and that it’s not even available. A few get confrontational, accusing me of withholding treatment, when “everyone knows” the drug works.
Believe me, if I had a cure I’d be thrilled to be able to offer it.
I understand that patients and families want a cure.
I understand hope.
I want ambroxol to work for Parkinson’s disease and make a huge difference in the lives of those affected by it. Maybe it will. Or maybe it won’t.
But these things take time to figure out. None of the amazing medications and hi-tech toys we have came about overnight. They were all years in the making.
That’s how science works, and medicine is as much a science as an art.
The art is being able to explain this to patients, and still allow them to hope.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How many of you hadn’t heard of ambroxol until the last few weeks?
How many of you have gotten at least one call asking for a prescription for it in that time?
I’ll raise my hand on both accounts.
Ambroxol seems relatively innocuous – an over-the-counter cold medication commonly used on planet Earth (though not approved in the U.S. for whatever reason). But in the last few years some interesting data have cropped up that it may help with Parkinson’s disease.
“May” being the key word here.
Now, I’m not saying it will or won’t do something. The trials that are being started will show that. It would be totally awesome if it did.
But we’ve been here before: The hope that some old, inexpensive, and widely available medication would turn out to have an amazing benefit we didn’t anticipate. We saw this with hydroxychloroquine and ivermectin during the pandemic. Before that we saw all kinds of speculative ideas that statins would be effective for diseases from multiple sclerosis to Alzheimer’s disease.
And, as with many incurable diseases, patients and their families are hoping for a breakthrough. We have plenty of treatments for Parkinson’s disease, but no cures yet. So any potentially effective drug news makes the rounds quickly on news sites, patient advocacy sites, Facebook, and others.
Like the childrens’ telephone game, each time the story is repeated it changes a bit. We’ve gone from an article saying the drug is starting clinical trials to see if it works, to it being a cure now on the marketplace.
Which is when people start calling my office. Most are disappointed to learn that its benefit (if any) is unknown and that it’s not even available. A few get confrontational, accusing me of withholding treatment, when “everyone knows” the drug works.
Believe me, if I had a cure I’d be thrilled to be able to offer it.
I understand that patients and families want a cure.
I understand hope.
I want ambroxol to work for Parkinson’s disease and make a huge difference in the lives of those affected by it. Maybe it will. Or maybe it won’t.
But these things take time to figure out. None of the amazing medications and hi-tech toys we have came about overnight. They were all years in the making.
That’s how science works, and medicine is as much a science as an art.
The art is being able to explain this to patients, and still allow them to hope.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Diagnosing rare disorders
When I was a resident (back in the Cretaceous era), the idea of autoimmune encephalitis was just beginning to take hold. It was kind of like Bigfoot. A few reports, vague articles, the occasional sighting of what may or may not be a case. …
Unlike Bigfoot, however, the evidence quickly added up until there was no question that such a disorder existed. Then disorder became disorders, and now it seems a few more types are added to the list each year.
This doesn’t change the fact that they’re still, in the grand scheme of general neurology, relatively rare, though no one questions that they exist.
Today people still wishfully take pictures of Bigfoot, but they turn out to be images of bears or other animals, or tricks of light and shadow.
This is an issue with human thought. Many times we see what we want to see, especially if it’s more interesting than a mundane alternative.
An autoimmune encephalitis article in the January 2023 issue of JAMA Neurology looked into this. On reviewing 393 patients diagnosed with the disorder, the researchers found that 27% of them actually didn’t have it at all. Such things as functional disorders, neurodegenerative diseases, and primary psychiatric diagnoses were, instead, the culprits.
I’m not criticizing those who made an incorrect diagnosis. We all do. That’s the nature of medicine.
Which is worse? Missing the diagnosis entirely and not treating, or diagnosing a patient with something else and treating incorrectly? I guess it depends on the disease and nature of treatment.
Certainly, finding a case of autoimmune encephalitis is more interesting than, say toxic-metabolic encephalopathy from a bladder infection, just as getting a picture of Bigfoot is way more cool than one of a bear with mange.
But we need to be careful when faced with equivocal labs and data lest we read too much into them. There are too many gray zones in medicine to lead you astray. Not to say we won’t be.
But it’s not just rare diseases. In the early 1990s two different studies found that 24% of patients diagnosed with Parkinson’s disease were found to have something else on autopsy.
That was 30 years ago. Now we have DaT scans to help. Maybe our abilities as neurologists have also gotten better (though I don’t think the neurological exam has changed much since Charcot).
Our gadgets, labs, and treatments get better every year. We have tools available to us now that were unthinkable a generation ago. For that matter, they were unthinkable when I began my career.
But they don’t change the fact that human error never goes away. All of us are susceptible to it, and all of us make mistakes.
Such is the way of medicine now, and likely always. All we can do is our best and keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
When I was a resident (back in the Cretaceous era), the idea of autoimmune encephalitis was just beginning to take hold. It was kind of like Bigfoot. A few reports, vague articles, the occasional sighting of what may or may not be a case. …
Unlike Bigfoot, however, the evidence quickly added up until there was no question that such a disorder existed. Then disorder became disorders, and now it seems a few more types are added to the list each year.
This doesn’t change the fact that they’re still, in the grand scheme of general neurology, relatively rare, though no one questions that they exist.
Today people still wishfully take pictures of Bigfoot, but they turn out to be images of bears or other animals, or tricks of light and shadow.
This is an issue with human thought. Many times we see what we want to see, especially if it’s more interesting than a mundane alternative.
An autoimmune encephalitis article in the January 2023 issue of JAMA Neurology looked into this. On reviewing 393 patients diagnosed with the disorder, the researchers found that 27% of them actually didn’t have it at all. Such things as functional disorders, neurodegenerative diseases, and primary psychiatric diagnoses were, instead, the culprits.
I’m not criticizing those who made an incorrect diagnosis. We all do. That’s the nature of medicine.
Which is worse? Missing the diagnosis entirely and not treating, or diagnosing a patient with something else and treating incorrectly? I guess it depends on the disease and nature of treatment.
Certainly, finding a case of autoimmune encephalitis is more interesting than, say toxic-metabolic encephalopathy from a bladder infection, just as getting a picture of Bigfoot is way more cool than one of a bear with mange.
But we need to be careful when faced with equivocal labs and data lest we read too much into them. There are too many gray zones in medicine to lead you astray. Not to say we won’t be.
But it’s not just rare diseases. In the early 1990s two different studies found that 24% of patients diagnosed with Parkinson’s disease were found to have something else on autopsy.
That was 30 years ago. Now we have DaT scans to help. Maybe our abilities as neurologists have also gotten better (though I don’t think the neurological exam has changed much since Charcot).
Our gadgets, labs, and treatments get better every year. We have tools available to us now that were unthinkable a generation ago. For that matter, they were unthinkable when I began my career.
But they don’t change the fact that human error never goes away. All of us are susceptible to it, and all of us make mistakes.
Such is the way of medicine now, and likely always. All we can do is our best and keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
When I was a resident (back in the Cretaceous era), the idea of autoimmune encephalitis was just beginning to take hold. It was kind of like Bigfoot. A few reports, vague articles, the occasional sighting of what may or may not be a case. …
Unlike Bigfoot, however, the evidence quickly added up until there was no question that such a disorder existed. Then disorder became disorders, and now it seems a few more types are added to the list each year.
This doesn’t change the fact that they’re still, in the grand scheme of general neurology, relatively rare, though no one questions that they exist.
Today people still wishfully take pictures of Bigfoot, but they turn out to be images of bears or other animals, or tricks of light and shadow.
This is an issue with human thought. Many times we see what we want to see, especially if it’s more interesting than a mundane alternative.
An autoimmune encephalitis article in the January 2023 issue of JAMA Neurology looked into this. On reviewing 393 patients diagnosed with the disorder, the researchers found that 27% of them actually didn’t have it at all. Such things as functional disorders, neurodegenerative diseases, and primary psychiatric diagnoses were, instead, the culprits.
I’m not criticizing those who made an incorrect diagnosis. We all do. That’s the nature of medicine.
Which is worse? Missing the diagnosis entirely and not treating, or diagnosing a patient with something else and treating incorrectly? I guess it depends on the disease and nature of treatment.
Certainly, finding a case of autoimmune encephalitis is more interesting than, say toxic-metabolic encephalopathy from a bladder infection, just as getting a picture of Bigfoot is way more cool than one of a bear with mange.
But we need to be careful when faced with equivocal labs and data lest we read too much into them. There are too many gray zones in medicine to lead you astray. Not to say we won’t be.
But it’s not just rare diseases. In the early 1990s two different studies found that 24% of patients diagnosed with Parkinson’s disease were found to have something else on autopsy.
That was 30 years ago. Now we have DaT scans to help. Maybe our abilities as neurologists have also gotten better (though I don’t think the neurological exam has changed much since Charcot).
Our gadgets, labs, and treatments get better every year. We have tools available to us now that were unthinkable a generation ago. For that matter, they were unthinkable when I began my career.
But they don’t change the fact that human error never goes away. All of us are susceptible to it, and all of us make mistakes.
Such is the way of medicine now, and likely always. All we can do is our best and keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Why is a healthy diet so hard to maintain?
Does this surprise anyone?
Although first publicized in 1975, the diet really didn’t gain attention until the 1990s. But, since then, the evidence in its favor has steadily grown.
Granted, while it was codified into a diet then, the benefits of fruits and vegetables weren’t exactly a secret beforehand. I’m pretty sure all of us remember being told to eat our vegetables (often repeatedly) while growing up.
So it’s not like we, both medical and nonmedical people, should be surprised at the results.
Is it really going to change anyone’s dietary habits?
Of course it will! It’s the beginning of the new year, and this time people are actually going to stick with their resolutions! For the first time they understand that ... who am I kidding?
For some people (hopefully myself included) there will be success at eating better and taking care of themselves. For most it will be Groundhog Day, both literally and figuratively, when February comes around.
It makes me wonder why this is. We all know what’s good for us. The evidence to support the Mediterranean diet is solid. The foods on it are widely available, often at lower cost than the usual American protein-heavy and processed foods habits. They’re flexible, and, generally taste good.
Yet, for all the evidence behind it, most won’t stick with it. Too many years of habits. Too many stressful days at work that lower our willpower to stick with it. Too many convenient reasons to count.
The question really isn’t “what’s the best diet?” That’s been answered. Realistically I don’t see that changing anytime soon.
The real question is “how do I stick with it?”
And another 5, 10, or 20 years of annually trying to figure out what the best diet is won’t change that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Does this surprise anyone?
Although first publicized in 1975, the diet really didn’t gain attention until the 1990s. But, since then, the evidence in its favor has steadily grown.
Granted, while it was codified into a diet then, the benefits of fruits and vegetables weren’t exactly a secret beforehand. I’m pretty sure all of us remember being told to eat our vegetables (often repeatedly) while growing up.
So it’s not like we, both medical and nonmedical people, should be surprised at the results.
Is it really going to change anyone’s dietary habits?
Of course it will! It’s the beginning of the new year, and this time people are actually going to stick with their resolutions! For the first time they understand that ... who am I kidding?
For some people (hopefully myself included) there will be success at eating better and taking care of themselves. For most it will be Groundhog Day, both literally and figuratively, when February comes around.
It makes me wonder why this is. We all know what’s good for us. The evidence to support the Mediterranean diet is solid. The foods on it are widely available, often at lower cost than the usual American protein-heavy and processed foods habits. They’re flexible, and, generally taste good.
Yet, for all the evidence behind it, most won’t stick with it. Too many years of habits. Too many stressful days at work that lower our willpower to stick with it. Too many convenient reasons to count.
The question really isn’t “what’s the best diet?” That’s been answered. Realistically I don’t see that changing anytime soon.
The real question is “how do I stick with it?”
And another 5, 10, or 20 years of annually trying to figure out what the best diet is won’t change that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Does this surprise anyone?
Although first publicized in 1975, the diet really didn’t gain attention until the 1990s. But, since then, the evidence in its favor has steadily grown.
Granted, while it was codified into a diet then, the benefits of fruits and vegetables weren’t exactly a secret beforehand. I’m pretty sure all of us remember being told to eat our vegetables (often repeatedly) while growing up.
So it’s not like we, both medical and nonmedical people, should be surprised at the results.
Is it really going to change anyone’s dietary habits?
Of course it will! It’s the beginning of the new year, and this time people are actually going to stick with their resolutions! For the first time they understand that ... who am I kidding?
For some people (hopefully myself included) there will be success at eating better and taking care of themselves. For most it will be Groundhog Day, both literally and figuratively, when February comes around.
It makes me wonder why this is. We all know what’s good for us. The evidence to support the Mediterranean diet is solid. The foods on it are widely available, often at lower cost than the usual American protein-heavy and processed foods habits. They’re flexible, and, generally taste good.
Yet, for all the evidence behind it, most won’t stick with it. Too many years of habits. Too many stressful days at work that lower our willpower to stick with it. Too many convenient reasons to count.
The question really isn’t “what’s the best diet?” That’s been answered. Realistically I don’t see that changing anytime soon.
The real question is “how do I stick with it?”
And another 5, 10, or 20 years of annually trying to figure out what the best diet is won’t change that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Grateful and hopeful
My year is now over. My staff and I started the habit of closing down mid-December in 2013, when we realized that patients generally didn’t want to come in then, either.
To me a year really ends the day we close up for the holidays. I put away the season’s decorations, send the final batch to my billing company, and lock the door. Not much of a New Year’s, but at my age it’s not a holiday I mark, anyway. It’s more a relief that my office year, at least, is done.
So it’s always a time for reflection, between the more mundane work of returning calls, reviewing the tests that come in, and getting taxes ready. I try to relax as much as I can (given the weird state of our times, I haven’t left town since November 2019, so this is my vacation for now).
Plus, my kids all come home. I have no idea how much longer that’s going to happen, so I’ll enjoy it while I can.
It’s now almost 3 years since I last rounded at a hospital, and I can’t say I miss it. While I usually have plenty to do on my breaks and weekends, and the occasional patient call to return, it’s nice to know that I can stay in my robe, PJs, and slippers through it all.
2022 certainly wasn’t bad for my family and me, though not as good as any of us hoped. The world, already battered by the pandemic, was thrown into greater uncertainty by the war in Europe and its ramifications across the globe. In comparison, I’m very grateful that higher prices are the extent of my suffering as compared with what the people of Ukraine are going through.
But, at the end of it all, my little practice and two wonderful staff are still here, just as we’ve been since 2000. My kids will (hopefully) all be through college by the end of 2023 and moving on with their lives. I love them, and will miss them if they move away, but part of being a parent is accepting that your kids are only visitors and have their own paths to follow.
For my staff I’m glad they’ve stuck with me through good and bad times, and that we still have fun together – even when we haven’t worked under the same roof in a while.
For my patients and their families we’ve seen a few glimmers of optimism in treatments and hopefully they’ll continue to grow and be built upon. Heaven knows my field – and many others – can use them.
And so,
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
My year is now over. My staff and I started the habit of closing down mid-December in 2013, when we realized that patients generally didn’t want to come in then, either.
To me a year really ends the day we close up for the holidays. I put away the season’s decorations, send the final batch to my billing company, and lock the door. Not much of a New Year’s, but at my age it’s not a holiday I mark, anyway. It’s more a relief that my office year, at least, is done.
So it’s always a time for reflection, between the more mundane work of returning calls, reviewing the tests that come in, and getting taxes ready. I try to relax as much as I can (given the weird state of our times, I haven’t left town since November 2019, so this is my vacation for now).
Plus, my kids all come home. I have no idea how much longer that’s going to happen, so I’ll enjoy it while I can.
It’s now almost 3 years since I last rounded at a hospital, and I can’t say I miss it. While I usually have plenty to do on my breaks and weekends, and the occasional patient call to return, it’s nice to know that I can stay in my robe, PJs, and slippers through it all.
2022 certainly wasn’t bad for my family and me, though not as good as any of us hoped. The world, already battered by the pandemic, was thrown into greater uncertainty by the war in Europe and its ramifications across the globe. In comparison, I’m very grateful that higher prices are the extent of my suffering as compared with what the people of Ukraine are going through.
But, at the end of it all, my little practice and two wonderful staff are still here, just as we’ve been since 2000. My kids will (hopefully) all be through college by the end of 2023 and moving on with their lives. I love them, and will miss them if they move away, but part of being a parent is accepting that your kids are only visitors and have their own paths to follow.
For my staff I’m glad they’ve stuck with me through good and bad times, and that we still have fun together – even when we haven’t worked under the same roof in a while.
For my patients and their families we’ve seen a few glimmers of optimism in treatments and hopefully they’ll continue to grow and be built upon. Heaven knows my field – and many others – can use them.
And so,
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
My year is now over. My staff and I started the habit of closing down mid-December in 2013, when we realized that patients generally didn’t want to come in then, either.
To me a year really ends the day we close up for the holidays. I put away the season’s decorations, send the final batch to my billing company, and lock the door. Not much of a New Year’s, but at my age it’s not a holiday I mark, anyway. It’s more a relief that my office year, at least, is done.
So it’s always a time for reflection, between the more mundane work of returning calls, reviewing the tests that come in, and getting taxes ready. I try to relax as much as I can (given the weird state of our times, I haven’t left town since November 2019, so this is my vacation for now).
Plus, my kids all come home. I have no idea how much longer that’s going to happen, so I’ll enjoy it while I can.
It’s now almost 3 years since I last rounded at a hospital, and I can’t say I miss it. While I usually have plenty to do on my breaks and weekends, and the occasional patient call to return, it’s nice to know that I can stay in my robe, PJs, and slippers through it all.
2022 certainly wasn’t bad for my family and me, though not as good as any of us hoped. The world, already battered by the pandemic, was thrown into greater uncertainty by the war in Europe and its ramifications across the globe. In comparison, I’m very grateful that higher prices are the extent of my suffering as compared with what the people of Ukraine are going through.
But, at the end of it all, my little practice and two wonderful staff are still here, just as we’ve been since 2000. My kids will (hopefully) all be through college by the end of 2023 and moving on with their lives. I love them, and will miss them if they move away, but part of being a parent is accepting that your kids are only visitors and have their own paths to follow.
For my staff I’m glad they’ve stuck with me through good and bad times, and that we still have fun together – even when we haven’t worked under the same roof in a while.
For my patients and their families we’ve seen a few glimmers of optimism in treatments and hopefully they’ll continue to grow and be built upon. Heaven knows my field – and many others – can use them.
And so,
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Taking our own advice
Like many Americans, I’m overweight. Working 70-80 hours a week doesn’t leave much time for exercise. I try to do what I can, such as using stairs instead of the elevator, but in a two-story office building that doesn’t get you very far. And when I get home there are still tests to read, dictations to do, finances to catch up on ... which leaves little time for anything else other than eating and sleeping.
Eating better? Easier said than done. When I was single, back in residency, that was easy. I only had one person to shop for and feed, but in a family you need to find something that will keep everyone happy, and with three teenagers that ain’t easy. Everyone wants this, that, or the other, and none of it seems to be particularly good for you.
In the modern era convenience generally beats pretty much everything else. Our lives are hurried. At some point it’s just easier to pick something up or order out than to go to the effort of preparing your own meals. Of course, it’s possible to get something healthy for takeout, but the unhealthy menu items sound so much better, and by that time of day I’m tired, hungry, and stressed, and the will power I had in the morning is pretty much gone.
It’s kind of a medical paradox. Those of us taking care of others often don’t do the same for ourselves. Part of this, as noted in a recent Medscape article, is that we live on schedules that are unrelated to the typical 9-to-5 jobs that most other professionals have, not to mention a very different set of stressors.
At least I haven’t started smoking.
As the article points out, I’m not alone. In fact, it’s reassuring to know other physicians are dealing with the same situation. We often assume we’re alone in our struggles, when the actual truth is the opposite.
All of our medical training doesn’t mean we’re not human. It would be nice if the job made us better able to practice what we preach, but human nature is older than medicine, and we’re susceptible to the same faults and temptations as those of our patients.
And always will be.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Like many Americans, I’m overweight. Working 70-80 hours a week doesn’t leave much time for exercise. I try to do what I can, such as using stairs instead of the elevator, but in a two-story office building that doesn’t get you very far. And when I get home there are still tests to read, dictations to do, finances to catch up on ... which leaves little time for anything else other than eating and sleeping.
Eating better? Easier said than done. When I was single, back in residency, that was easy. I only had one person to shop for and feed, but in a family you need to find something that will keep everyone happy, and with three teenagers that ain’t easy. Everyone wants this, that, or the other, and none of it seems to be particularly good for you.
In the modern era convenience generally beats pretty much everything else. Our lives are hurried. At some point it’s just easier to pick something up or order out than to go to the effort of preparing your own meals. Of course, it’s possible to get something healthy for takeout, but the unhealthy menu items sound so much better, and by that time of day I’m tired, hungry, and stressed, and the will power I had in the morning is pretty much gone.
It’s kind of a medical paradox. Those of us taking care of others often don’t do the same for ourselves. Part of this, as noted in a recent Medscape article, is that we live on schedules that are unrelated to the typical 9-to-5 jobs that most other professionals have, not to mention a very different set of stressors.
At least I haven’t started smoking.
As the article points out, I’m not alone. In fact, it’s reassuring to know other physicians are dealing with the same situation. We often assume we’re alone in our struggles, when the actual truth is the opposite.
All of our medical training doesn’t mean we’re not human. It would be nice if the job made us better able to practice what we preach, but human nature is older than medicine, and we’re susceptible to the same faults and temptations as those of our patients.
And always will be.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Like many Americans, I’m overweight. Working 70-80 hours a week doesn’t leave much time for exercise. I try to do what I can, such as using stairs instead of the elevator, but in a two-story office building that doesn’t get you very far. And when I get home there are still tests to read, dictations to do, finances to catch up on ... which leaves little time for anything else other than eating and sleeping.
Eating better? Easier said than done. When I was single, back in residency, that was easy. I only had one person to shop for and feed, but in a family you need to find something that will keep everyone happy, and with three teenagers that ain’t easy. Everyone wants this, that, or the other, and none of it seems to be particularly good for you.
In the modern era convenience generally beats pretty much everything else. Our lives are hurried. At some point it’s just easier to pick something up or order out than to go to the effort of preparing your own meals. Of course, it’s possible to get something healthy for takeout, but the unhealthy menu items sound so much better, and by that time of day I’m tired, hungry, and stressed, and the will power I had in the morning is pretty much gone.
It’s kind of a medical paradox. Those of us taking care of others often don’t do the same for ourselves. Part of this, as noted in a recent Medscape article, is that we live on schedules that are unrelated to the typical 9-to-5 jobs that most other professionals have, not to mention a very different set of stressors.
At least I haven’t started smoking.
As the article points out, I’m not alone. In fact, it’s reassuring to know other physicians are dealing with the same situation. We often assume we’re alone in our struggles, when the actual truth is the opposite.
All of our medical training doesn’t mean we’re not human. It would be nice if the job made us better able to practice what we preach, but human nature is older than medicine, and we’re susceptible to the same faults and temptations as those of our patients.
And always will be.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Dialing down the negativity
I don’t do email. Or texting. You want to talk to me and my staff? Pick up a phone.
Some people say I’m old fashioned, or not patient-friendly, or whatever.
I don’t care.
To me there are too many issues with things that can get missed in emails, too many security concerns, too many ways to alter them so it looks like something different was said.
Now, a recent study of an EHR system found that 3% of emails from patients had negative, if not downright nasty, sentiments expressed to their physicians.
Here’s some examples:
“I hope and expect that you will spend eternity in hell. You are an abusive, nasty, cheap person.”
“Your office is full of liars, hypocrites and I will do everything in my power to prevent anyone from going to your bullsh** office again.”
The study also noted that the most common expletive used by patients is the F-bomb, and that words with violent connotations, such as “shoot,” “fight,” and “kill” were often used in such emails. The last are definitely concerning in an era of increased violence directed at doctors and other health care workers who are just trying to do their jobs.
Now, I know doctors are a microcosm of society. Like patients, most are decent people trying their best, but a few are ... not particularly nice.
But still, I don’t think we, or anyone for that matter, need to be getting emails of this nature. It certainly doesn’t put anyone in a good position, or allow for objective, unbiased, care. Even if they’re only 3% of emails, that can still be quite a few.
Who needs that?
One of the issues with email is that it’s easy to type something nasty and hit “send,” then later have it occur to you that maybe you should have calmed down first. Granted, that sort of thing can (and does) happen when talking to another person (by phone or in person), but it’s harder.
Direct personal contact, especially face-to-face, appears to lessen impulsive reactions for most. The other person isn’t an invisible email address, they’re someone you’re talking to. You can read tone-of-voice and facial expressions. Again, I’m aware people still can lose their cool in person, but it’s harder.
and running into the next exam room. Plus, it ensures that all noncritical patient interactions occur during business hours, when we’re in doctor mode, rather than at 2:45 a.m. when we look at the iPhone while waiting for the dog to come back in. That’s a terrible time to receive and send medical (or any) emails for both doctor and patient.
A lot rides on every one of my patient interactions, and that’s why I still want them done directly. If that makes me old-fashioned, so be it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I don’t do email. Or texting. You want to talk to me and my staff? Pick up a phone.
Some people say I’m old fashioned, or not patient-friendly, or whatever.
I don’t care.
To me there are too many issues with things that can get missed in emails, too many security concerns, too many ways to alter them so it looks like something different was said.
Now, a recent study of an EHR system found that 3% of emails from patients had negative, if not downright nasty, sentiments expressed to their physicians.
Here’s some examples:
“I hope and expect that you will spend eternity in hell. You are an abusive, nasty, cheap person.”
“Your office is full of liars, hypocrites and I will do everything in my power to prevent anyone from going to your bullsh** office again.”
The study also noted that the most common expletive used by patients is the F-bomb, and that words with violent connotations, such as “shoot,” “fight,” and “kill” were often used in such emails. The last are definitely concerning in an era of increased violence directed at doctors and other health care workers who are just trying to do their jobs.
Now, I know doctors are a microcosm of society. Like patients, most are decent people trying their best, but a few are ... not particularly nice.
But still, I don’t think we, or anyone for that matter, need to be getting emails of this nature. It certainly doesn’t put anyone in a good position, or allow for objective, unbiased, care. Even if they’re only 3% of emails, that can still be quite a few.
Who needs that?
One of the issues with email is that it’s easy to type something nasty and hit “send,” then later have it occur to you that maybe you should have calmed down first. Granted, that sort of thing can (and does) happen when talking to another person (by phone or in person), but it’s harder.
Direct personal contact, especially face-to-face, appears to lessen impulsive reactions for most. The other person isn’t an invisible email address, they’re someone you’re talking to. You can read tone-of-voice and facial expressions. Again, I’m aware people still can lose their cool in person, but it’s harder.
and running into the next exam room. Plus, it ensures that all noncritical patient interactions occur during business hours, when we’re in doctor mode, rather than at 2:45 a.m. when we look at the iPhone while waiting for the dog to come back in. That’s a terrible time to receive and send medical (or any) emails for both doctor and patient.
A lot rides on every one of my patient interactions, and that’s why I still want them done directly. If that makes me old-fashioned, so be it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I don’t do email. Or texting. You want to talk to me and my staff? Pick up a phone.
Some people say I’m old fashioned, or not patient-friendly, or whatever.
I don’t care.
To me there are too many issues with things that can get missed in emails, too many security concerns, too many ways to alter them so it looks like something different was said.
Now, a recent study of an EHR system found that 3% of emails from patients had negative, if not downright nasty, sentiments expressed to their physicians.
Here’s some examples:
“I hope and expect that you will spend eternity in hell. You are an abusive, nasty, cheap person.”
“Your office is full of liars, hypocrites and I will do everything in my power to prevent anyone from going to your bullsh** office again.”
The study also noted that the most common expletive used by patients is the F-bomb, and that words with violent connotations, such as “shoot,” “fight,” and “kill” were often used in such emails. The last are definitely concerning in an era of increased violence directed at doctors and other health care workers who are just trying to do their jobs.
Now, I know doctors are a microcosm of society. Like patients, most are decent people trying their best, but a few are ... not particularly nice.
But still, I don’t think we, or anyone for that matter, need to be getting emails of this nature. It certainly doesn’t put anyone in a good position, or allow for objective, unbiased, care. Even if they’re only 3% of emails, that can still be quite a few.
Who needs that?
One of the issues with email is that it’s easy to type something nasty and hit “send,” then later have it occur to you that maybe you should have calmed down first. Granted, that sort of thing can (and does) happen when talking to another person (by phone or in person), but it’s harder.
Direct personal contact, especially face-to-face, appears to lessen impulsive reactions for most. The other person isn’t an invisible email address, they’re someone you’re talking to. You can read tone-of-voice and facial expressions. Again, I’m aware people still can lose their cool in person, but it’s harder.
and running into the next exam room. Plus, it ensures that all noncritical patient interactions occur during business hours, when we’re in doctor mode, rather than at 2:45 a.m. when we look at the iPhone while waiting for the dog to come back in. That’s a terrible time to receive and send medical (or any) emails for both doctor and patient.
A lot rides on every one of my patient interactions, and that’s why I still want them done directly. If that makes me old-fashioned, so be it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Jump starting thankfulness
One night, at the beginning of Thanksgiving week, my son called from his place across town. His car was having trouble starting, so I went to see what was up.
I got to his place to find his car wouldn’t start, even though the battery was only a few months old. I used my car to jump his, left him mine, and headed back. My plan was to leave it at our usual repair place and walk home.
Easier said than done.
I’d just gotten on the 101, the main loop freeway for the Phoenix metro area, when his car completely died. The lights flickered, the gauges stopped working, and then the engine cut out. Mercifully I was able to pull over into the right emergency lane as it did so. I was nowhere near an exit.
Not even the emergency flashers worked. It was dark. I was on a major freeway. I couldn’t make myself visible. Cars and trucks were whizzing by 2-3 feet to my left, and I was hoping they’d see me.
I called AAA and explained the situation. They were sending a tow truck, but it could take up to another 3 hours. I sent some quick texts to family to let them know what was up. I called the AZ highway patrol to let them know my predicament, in case they wanted to come put a flare or two behind me (they didn’t).
And then I settled in. Seatbelt on, staring at the road in front of me ... and had nothing to do.
When was the last time you had absolutely nothing to do?
It’s pretty rare these days. I mean, we all have breaks in the action, so we watch a cute animal video, or play a round of Wordle, or whatever.
But I had none of that. No books, iPad, or computer. Sure, I had my phone, but it was less than 50% charged with no way to charge it, and so I wanted to conserve that in case I needed it.
I don’t think I’ve ever had a moment like this since I began carrying a phone in 1998. There was, literally, nothing to do but wait. I couldn’t even try to nod off with the seat unadjustable and cars whizzing by.
So my mind wandered, and I thought. I turned over office cases. I went through year-end finances. I thought about my current predicament. I stared endlessly at the road ahead and cars passing me.
At some point I began to realize that I’m actually pretty lucky, and that nothing was nearly as bad as it had seemed earlier in the day. As the initial adrenaline rush drained out of me I calmed down and the things I’d been worrying about that afternoon seemed workable.
The tow truck pulled in front of me, ending my reverie. Mercifully, it had only taken them an hour. I was home 45 minutes later.
I was thankful to be home and I was thankful that nothing more serious had happened in a potentially bad situation.
And, somewhere in there,
In today’s world of endless screens and texts and calls and notifications, it’s easy to lose track of that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
One night, at the beginning of Thanksgiving week, my son called from his place across town. His car was having trouble starting, so I went to see what was up.
I got to his place to find his car wouldn’t start, even though the battery was only a few months old. I used my car to jump his, left him mine, and headed back. My plan was to leave it at our usual repair place and walk home.
Easier said than done.
I’d just gotten on the 101, the main loop freeway for the Phoenix metro area, when his car completely died. The lights flickered, the gauges stopped working, and then the engine cut out. Mercifully I was able to pull over into the right emergency lane as it did so. I was nowhere near an exit.
Not even the emergency flashers worked. It was dark. I was on a major freeway. I couldn’t make myself visible. Cars and trucks were whizzing by 2-3 feet to my left, and I was hoping they’d see me.
I called AAA and explained the situation. They were sending a tow truck, but it could take up to another 3 hours. I sent some quick texts to family to let them know what was up. I called the AZ highway patrol to let them know my predicament, in case they wanted to come put a flare or two behind me (they didn’t).
And then I settled in. Seatbelt on, staring at the road in front of me ... and had nothing to do.
When was the last time you had absolutely nothing to do?
It’s pretty rare these days. I mean, we all have breaks in the action, so we watch a cute animal video, or play a round of Wordle, or whatever.
But I had none of that. No books, iPad, or computer. Sure, I had my phone, but it was less than 50% charged with no way to charge it, and so I wanted to conserve that in case I needed it.
I don’t think I’ve ever had a moment like this since I began carrying a phone in 1998. There was, literally, nothing to do but wait. I couldn’t even try to nod off with the seat unadjustable and cars whizzing by.
So my mind wandered, and I thought. I turned over office cases. I went through year-end finances. I thought about my current predicament. I stared endlessly at the road ahead and cars passing me.
At some point I began to realize that I’m actually pretty lucky, and that nothing was nearly as bad as it had seemed earlier in the day. As the initial adrenaline rush drained out of me I calmed down and the things I’d been worrying about that afternoon seemed workable.
The tow truck pulled in front of me, ending my reverie. Mercifully, it had only taken them an hour. I was home 45 minutes later.
I was thankful to be home and I was thankful that nothing more serious had happened in a potentially bad situation.
And, somewhere in there,
In today’s world of endless screens and texts and calls and notifications, it’s easy to lose track of that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
One night, at the beginning of Thanksgiving week, my son called from his place across town. His car was having trouble starting, so I went to see what was up.
I got to his place to find his car wouldn’t start, even though the battery was only a few months old. I used my car to jump his, left him mine, and headed back. My plan was to leave it at our usual repair place and walk home.
Easier said than done.
I’d just gotten on the 101, the main loop freeway for the Phoenix metro area, when his car completely died. The lights flickered, the gauges stopped working, and then the engine cut out. Mercifully I was able to pull over into the right emergency lane as it did so. I was nowhere near an exit.
Not even the emergency flashers worked. It was dark. I was on a major freeway. I couldn’t make myself visible. Cars and trucks were whizzing by 2-3 feet to my left, and I was hoping they’d see me.
I called AAA and explained the situation. They were sending a tow truck, but it could take up to another 3 hours. I sent some quick texts to family to let them know what was up. I called the AZ highway patrol to let them know my predicament, in case they wanted to come put a flare or two behind me (they didn’t).
And then I settled in. Seatbelt on, staring at the road in front of me ... and had nothing to do.
When was the last time you had absolutely nothing to do?
It’s pretty rare these days. I mean, we all have breaks in the action, so we watch a cute animal video, or play a round of Wordle, or whatever.
But I had none of that. No books, iPad, or computer. Sure, I had my phone, but it was less than 50% charged with no way to charge it, and so I wanted to conserve that in case I needed it.
I don’t think I’ve ever had a moment like this since I began carrying a phone in 1998. There was, literally, nothing to do but wait. I couldn’t even try to nod off with the seat unadjustable and cars whizzing by.
So my mind wandered, and I thought. I turned over office cases. I went through year-end finances. I thought about my current predicament. I stared endlessly at the road ahead and cars passing me.
At some point I began to realize that I’m actually pretty lucky, and that nothing was nearly as bad as it had seemed earlier in the day. As the initial adrenaline rush drained out of me I calmed down and the things I’d been worrying about that afternoon seemed workable.
The tow truck pulled in front of me, ending my reverie. Mercifully, it had only taken them an hour. I was home 45 minutes later.
I was thankful to be home and I was thankful that nothing more serious had happened in a potentially bad situation.
And, somewhere in there,
In today’s world of endless screens and texts and calls and notifications, it’s easy to lose track of that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Earlier diagnosis of Alzheimer’s: A good start, but then what?
In the October 2022 issue of JAMA Neurology was a research article and accompanying editorial on the ATN (amyloid/tau/neurodegeneration) framework for diagnosing and treating Alzheimer’s disease.
If the new generation of Alzheimer’s treatments can reverse pathology before the symptoms are apparent, it certainly makes sense to treat people as early as possible. In a terrible disease with only partially effective treatments now, this is encouraging news.
So this testing, as it stands now, would involve amyloid PET and tau PET scans, not to mention other screening tests such as MRI, labs, and the occasional lumbar puncture or EEG.
But it raises new questions.
Who should we be testing? If the new agents work on a presymptomatic basis, should we test everyone over 50, or 60, or 70? Or just those with memory concerns? Realistically, a lot of people come to general neurologists with memory worries, the majority of whom have nothing ominous. Those numbers are going to skyrocket as soon as the “have you been forgetting things? Ask your doctor” ads hit the airwaves. They’ll suggest, as much as the FDA will allow, that if you can’t find your car keys, you may have early dementia and need to be worked up promptly to keep from getting worse.
Who’s going to see these people? I’m sure it’s good for business, which I have no problem with, but most neurology practices are booked out a bit as it is. The influx of people panicked because they forgot their Netflix password will add to that.
How are we going to treat them? Even if we ignore aducanumab, which has more than enough baggage, lecanemab, donanemab, and gantenerumab are all waiting in the wings. Is one drug better for patients with certain scan findings? Or clearly safer? Keep in mind that, even at this early stage, we are already grappling with the potentially serious complication of ARIA [amyloid related imaging abnormalities]. The incidence is only going to go up as these new drugs enter the market. These questions rapidly move the drug outside the comfort zone of many general neurologists, and there aren’t nearly enough dementia subspecialists out there to handle the number of patients involved.
And lastly, from the more practical view, who’s going to pay for this? I’m not trying to prioritize money over people, but it’s a legitimate question that will have to be answered. PET scans aren’t cheap, and we’re talking about doing two of them. Neither are MRIs, or lumbar punctures. If we’re going to put guidelines out (like we do for mammograms and colonoscopies) for screening asymptomatic people over 70, or even mildly forgetful patients ... that’s a lot of dollars. Is there going to be some limitation on the testing based on who would benefit the most? What do we tell the patients and families outside of that range? And that’s even before we start factoring in the drug costs. In October, Forbes listed potential lecanemab prices as being anywhere from $9,000 to $35,000 per year.
I’m not trying to be Debbie Downer here. The fact that these drugs are here is, hopefully, the start of a new era in treatment of what will still be an incurable disease. Aricept (and its cousins) and Namenda were stepping stones in their day, and these are the next ones.
But these are questions that need to be answered. And soon.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In the October 2022 issue of JAMA Neurology was a research article and accompanying editorial on the ATN (amyloid/tau/neurodegeneration) framework for diagnosing and treating Alzheimer’s disease.
If the new generation of Alzheimer’s treatments can reverse pathology before the symptoms are apparent, it certainly makes sense to treat people as early as possible. In a terrible disease with only partially effective treatments now, this is encouraging news.
So this testing, as it stands now, would involve amyloid PET and tau PET scans, not to mention other screening tests such as MRI, labs, and the occasional lumbar puncture or EEG.
But it raises new questions.
Who should we be testing? If the new agents work on a presymptomatic basis, should we test everyone over 50, or 60, or 70? Or just those with memory concerns? Realistically, a lot of people come to general neurologists with memory worries, the majority of whom have nothing ominous. Those numbers are going to skyrocket as soon as the “have you been forgetting things? Ask your doctor” ads hit the airwaves. They’ll suggest, as much as the FDA will allow, that if you can’t find your car keys, you may have early dementia and need to be worked up promptly to keep from getting worse.
Who’s going to see these people? I’m sure it’s good for business, which I have no problem with, but most neurology practices are booked out a bit as it is. The influx of people panicked because they forgot their Netflix password will add to that.
How are we going to treat them? Even if we ignore aducanumab, which has more than enough baggage, lecanemab, donanemab, and gantenerumab are all waiting in the wings. Is one drug better for patients with certain scan findings? Or clearly safer? Keep in mind that, even at this early stage, we are already grappling with the potentially serious complication of ARIA [amyloid related imaging abnormalities]. The incidence is only going to go up as these new drugs enter the market. These questions rapidly move the drug outside the comfort zone of many general neurologists, and there aren’t nearly enough dementia subspecialists out there to handle the number of patients involved.
And lastly, from the more practical view, who’s going to pay for this? I’m not trying to prioritize money over people, but it’s a legitimate question that will have to be answered. PET scans aren’t cheap, and we’re talking about doing two of them. Neither are MRIs, or lumbar punctures. If we’re going to put guidelines out (like we do for mammograms and colonoscopies) for screening asymptomatic people over 70, or even mildly forgetful patients ... that’s a lot of dollars. Is there going to be some limitation on the testing based on who would benefit the most? What do we tell the patients and families outside of that range? And that’s even before we start factoring in the drug costs. In October, Forbes listed potential lecanemab prices as being anywhere from $9,000 to $35,000 per year.
I’m not trying to be Debbie Downer here. The fact that these drugs are here is, hopefully, the start of a new era in treatment of what will still be an incurable disease. Aricept (and its cousins) and Namenda were stepping stones in their day, and these are the next ones.
But these are questions that need to be answered. And soon.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In the October 2022 issue of JAMA Neurology was a research article and accompanying editorial on the ATN (amyloid/tau/neurodegeneration) framework for diagnosing and treating Alzheimer’s disease.
If the new generation of Alzheimer’s treatments can reverse pathology before the symptoms are apparent, it certainly makes sense to treat people as early as possible. In a terrible disease with only partially effective treatments now, this is encouraging news.
So this testing, as it stands now, would involve amyloid PET and tau PET scans, not to mention other screening tests such as MRI, labs, and the occasional lumbar puncture or EEG.
But it raises new questions.
Who should we be testing? If the new agents work on a presymptomatic basis, should we test everyone over 50, or 60, or 70? Or just those with memory concerns? Realistically, a lot of people come to general neurologists with memory worries, the majority of whom have nothing ominous. Those numbers are going to skyrocket as soon as the “have you been forgetting things? Ask your doctor” ads hit the airwaves. They’ll suggest, as much as the FDA will allow, that if you can’t find your car keys, you may have early dementia and need to be worked up promptly to keep from getting worse.
Who’s going to see these people? I’m sure it’s good for business, which I have no problem with, but most neurology practices are booked out a bit as it is. The influx of people panicked because they forgot their Netflix password will add to that.
How are we going to treat them? Even if we ignore aducanumab, which has more than enough baggage, lecanemab, donanemab, and gantenerumab are all waiting in the wings. Is one drug better for patients with certain scan findings? Or clearly safer? Keep in mind that, even at this early stage, we are already grappling with the potentially serious complication of ARIA [amyloid related imaging abnormalities]. The incidence is only going to go up as these new drugs enter the market. These questions rapidly move the drug outside the comfort zone of many general neurologists, and there aren’t nearly enough dementia subspecialists out there to handle the number of patients involved.
And lastly, from the more practical view, who’s going to pay for this? I’m not trying to prioritize money over people, but it’s a legitimate question that will have to be answered. PET scans aren’t cheap, and we’re talking about doing two of them. Neither are MRIs, or lumbar punctures. If we’re going to put guidelines out (like we do for mammograms and colonoscopies) for screening asymptomatic people over 70, or even mildly forgetful patients ... that’s a lot of dollars. Is there going to be some limitation on the testing based on who would benefit the most? What do we tell the patients and families outside of that range? And that’s even before we start factoring in the drug costs. In October, Forbes listed potential lecanemab prices as being anywhere from $9,000 to $35,000 per year.
I’m not trying to be Debbie Downer here. The fact that these drugs are here is, hopefully, the start of a new era in treatment of what will still be an incurable disease. Aricept (and its cousins) and Namenda were stepping stones in their day, and these are the next ones.
But these are questions that need to be answered. And soon.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
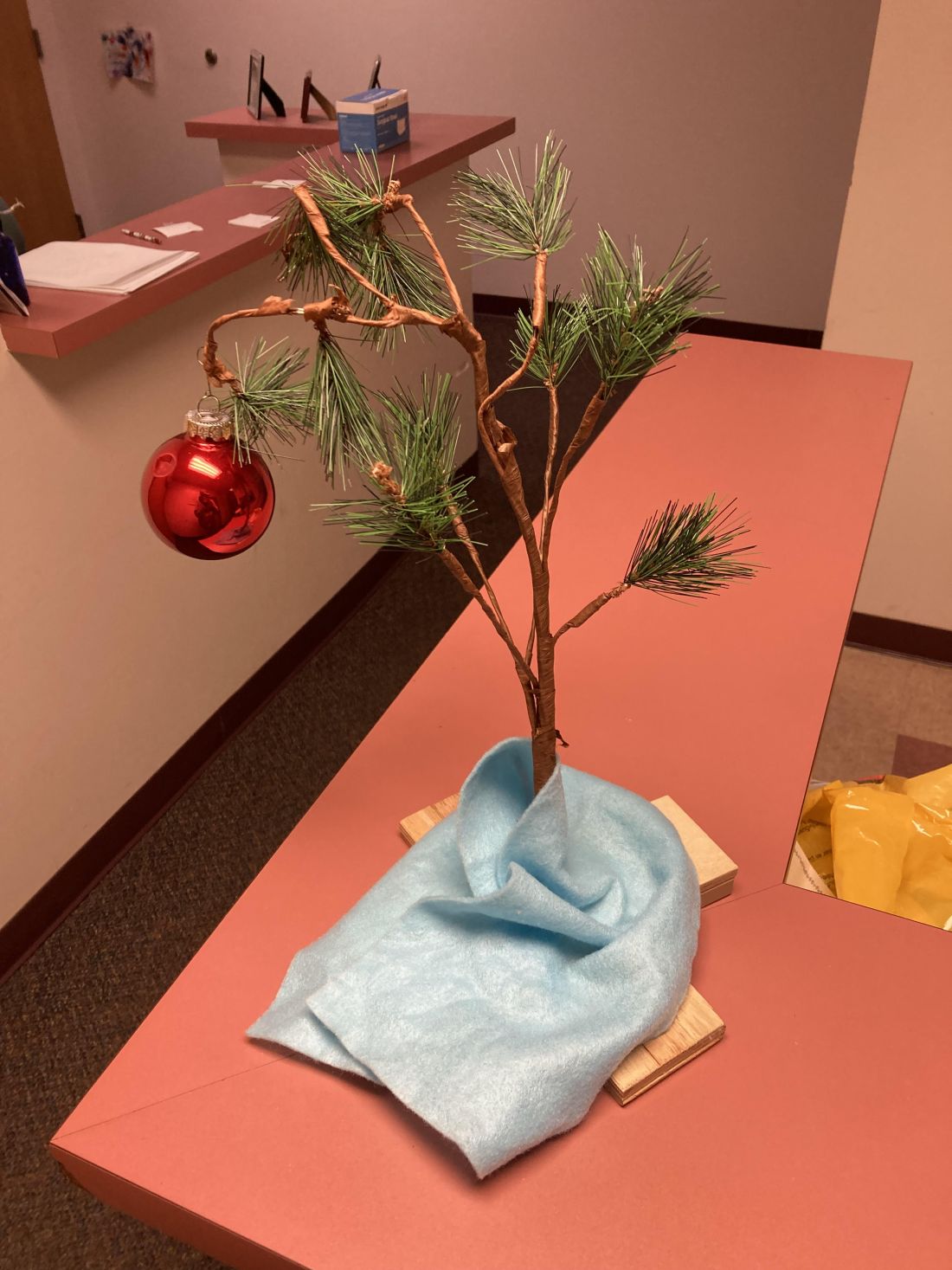
The Charlie Brown tree
I put a Christmas tree up early in November.
It’s not like it’s a real tree, or even a fancy one. For that matter, I’m Jewish.
Growing up in the 1970s one thing that could be relied on every year was the Charlie Brown Christmas special. It never changed. By age 5 you knew most of the lines, and loved the highlight when Charlie Brown brings home the saddest-looking tree ever, which collapses when he puts a single bauble on it.
Years ago, my kids gave me a Charlie Brown tree as a gift. It even plays the late Vince Guaraldi’s immortal Peanuts theme when you push a button. I forgot about it for a few years, then discovered it, and immediately brought it to my office.
I’m not a fan of holiday creep, where they move up earlier in the year, so I used to put it up after Thanksgiving. But we close the office 2-3 weeks later for the rest of the year. I like the tree, my staff likes the tree, and my patients like the tree, so I just started putting it up in early November so we can enjoy it for a month.
It’s whimsical and brings back memories of innocence, childhood, and (of course) Peanuts. It sets a cheerful tone when you see it there. Very few of my patients can resist pressing the button and playing the music as they go by.
The start of a new year is a relatively arbitrary date, chosen long ago. But its approach is always a reminder that life goes on. We continue our trips around the sun. Good times and bad times come and go, but time never stops.
In bad years the tree reminds me that it’s coming to an end, and to look toward the next. In good years it reminds me that it’s time to be ready for the surprises of the coming one.
In mid-December, after the patients are done for the last day of the year, I quietly put it away. It’s a vaguely somber moment, but at the same time I’m glad to know I now have 2-3 weeks of home time. It mostly involves working at my desk and returning phone calls, but there’s also time to relax with my kids, do jigsaw puzzles, and enjoy the Phoenix winter weather as a break before the next round starts.
To those who disagree with my choice of decoration or its timing, I simply respond: “Good grief!”
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I put a Christmas tree up early in November.
It’s not like it’s a real tree, or even a fancy one. For that matter, I’m Jewish.
Growing up in the 1970s one thing that could be relied on every year was the Charlie Brown Christmas special. It never changed. By age 5 you knew most of the lines, and loved the highlight when Charlie Brown brings home the saddest-looking tree ever, which collapses when he puts a single bauble on it.
Years ago, my kids gave me a Charlie Brown tree as a gift. It even plays the late Vince Guaraldi’s immortal Peanuts theme when you push a button. I forgot about it for a few years, then discovered it, and immediately brought it to my office.
I’m not a fan of holiday creep, where they move up earlier in the year, so I used to put it up after Thanksgiving. But we close the office 2-3 weeks later for the rest of the year. I like the tree, my staff likes the tree, and my patients like the tree, so I just started putting it up in early November so we can enjoy it for a month.
It’s whimsical and brings back memories of innocence, childhood, and (of course) Peanuts. It sets a cheerful tone when you see it there. Very few of my patients can resist pressing the button and playing the music as they go by.
The start of a new year is a relatively arbitrary date, chosen long ago. But its approach is always a reminder that life goes on. We continue our trips around the sun. Good times and bad times come and go, but time never stops.
In bad years the tree reminds me that it’s coming to an end, and to look toward the next. In good years it reminds me that it’s time to be ready for the surprises of the coming one.
In mid-December, after the patients are done for the last day of the year, I quietly put it away. It’s a vaguely somber moment, but at the same time I’m glad to know I now have 2-3 weeks of home time. It mostly involves working at my desk and returning phone calls, but there’s also time to relax with my kids, do jigsaw puzzles, and enjoy the Phoenix winter weather as a break before the next round starts.
To those who disagree with my choice of decoration or its timing, I simply respond: “Good grief!”
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I put a Christmas tree up early in November.
It’s not like it’s a real tree, or even a fancy one. For that matter, I’m Jewish.
Growing up in the 1970s one thing that could be relied on every year was the Charlie Brown Christmas special. It never changed. By age 5 you knew most of the lines, and loved the highlight when Charlie Brown brings home the saddest-looking tree ever, which collapses when he puts a single bauble on it.
Years ago, my kids gave me a Charlie Brown tree as a gift. It even plays the late Vince Guaraldi’s immortal Peanuts theme when you push a button. I forgot about it for a few years, then discovered it, and immediately brought it to my office.
I’m not a fan of holiday creep, where they move up earlier in the year, so I used to put it up after Thanksgiving. But we close the office 2-3 weeks later for the rest of the year. I like the tree, my staff likes the tree, and my patients like the tree, so I just started putting it up in early November so we can enjoy it for a month.
It’s whimsical and brings back memories of innocence, childhood, and (of course) Peanuts. It sets a cheerful tone when you see it there. Very few of my patients can resist pressing the button and playing the music as they go by.
The start of a new year is a relatively arbitrary date, chosen long ago. But its approach is always a reminder that life goes on. We continue our trips around the sun. Good times and bad times come and go, but time never stops.
In bad years the tree reminds me that it’s coming to an end, and to look toward the next. In good years it reminds me that it’s time to be ready for the surprises of the coming one.
In mid-December, after the patients are done for the last day of the year, I quietly put it away. It’s a vaguely somber moment, but at the same time I’m glad to know I now have 2-3 weeks of home time. It mostly involves working at my desk and returning phone calls, but there’s also time to relax with my kids, do jigsaw puzzles, and enjoy the Phoenix winter weather as a break before the next round starts.
To those who disagree with my choice of decoration or its timing, I simply respond: “Good grief!”
Dr. Block has a solo neurology practice in Scottsdale, Ariz.