User login
American Society of Hematology (ASH): ASH 2015
VIDEO: High-intensity conditioning stands ground in MDS, AML
ORLANDO – Reduced-intensity conditioning regimens failed to show a significant survival benefit over high-intensity regimens in myelodysplastic syndrome or acute myeloid leukemia in the phase III MAVERICK trial.
Pretransplant reduced intensity conditioning (RIC) also resulted in a significantly higher risk of relapse and inferior relapse-free survival vs. myeloablative conditioning (MAC).
The findings, reported in the late-breaking abstract (LBA-8) session at the annual meeting of the American Society of Hematology, generated a lively debate over the study construct and whether its conclusion that MAC remain “the treatment of choice” in appropriate candidates should be applied to both diseases.
Session comoderator Dr. David P. Steensma, a myelodysplasia physician at the Dana-Farber Cancer Institute in Boston, said in an interview that the data will not change his practice and that physicians should continue to “push the envelope” and provide as intense a conditioning regimen as their patients can tolerate.
“The take-home message is that using a reduced conditioning regimen whatever your choice might be, even though it is gentler on the patient and may be easier for them to go through the transplant, the biggest risk is still the disease, the underlying leukemia or myelodysplasia coming back. And the benefit from reduced intensity is not enough to outweigh that risk.”
To sort out this complex trial, we spoke with study author Dr. Bart L. Scott of the Fred Hutchinson Cancer Research Center at the University of Washington, Seattle.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Reduced-intensity conditioning regimens failed to show a significant survival benefit over high-intensity regimens in myelodysplastic syndrome or acute myeloid leukemia in the phase III MAVERICK trial.
Pretransplant reduced intensity conditioning (RIC) also resulted in a significantly higher risk of relapse and inferior relapse-free survival vs. myeloablative conditioning (MAC).
The findings, reported in the late-breaking abstract (LBA-8) session at the annual meeting of the American Society of Hematology, generated a lively debate over the study construct and whether its conclusion that MAC remain “the treatment of choice” in appropriate candidates should be applied to both diseases.
Session comoderator Dr. David P. Steensma, a myelodysplasia physician at the Dana-Farber Cancer Institute in Boston, said in an interview that the data will not change his practice and that physicians should continue to “push the envelope” and provide as intense a conditioning regimen as their patients can tolerate.
“The take-home message is that using a reduced conditioning regimen whatever your choice might be, even though it is gentler on the patient and may be easier for them to go through the transplant, the biggest risk is still the disease, the underlying leukemia or myelodysplasia coming back. And the benefit from reduced intensity is not enough to outweigh that risk.”
To sort out this complex trial, we spoke with study author Dr. Bart L. Scott of the Fred Hutchinson Cancer Research Center at the University of Washington, Seattle.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Reduced-intensity conditioning regimens failed to show a significant survival benefit over high-intensity regimens in myelodysplastic syndrome or acute myeloid leukemia in the phase III MAVERICK trial.
Pretransplant reduced intensity conditioning (RIC) also resulted in a significantly higher risk of relapse and inferior relapse-free survival vs. myeloablative conditioning (MAC).
The findings, reported in the late-breaking abstract (LBA-8) session at the annual meeting of the American Society of Hematology, generated a lively debate over the study construct and whether its conclusion that MAC remain “the treatment of choice” in appropriate candidates should be applied to both diseases.
Session comoderator Dr. David P. Steensma, a myelodysplasia physician at the Dana-Farber Cancer Institute in Boston, said in an interview that the data will not change his practice and that physicians should continue to “push the envelope” and provide as intense a conditioning regimen as their patients can tolerate.
“The take-home message is that using a reduced conditioning regimen whatever your choice might be, even though it is gentler on the patient and may be easier for them to go through the transplant, the biggest risk is still the disease, the underlying leukemia or myelodysplasia coming back. And the benefit from reduced intensity is not enough to outweigh that risk.”
To sort out this complex trial, we spoke with study author Dr. Bart L. Scott of the Fred Hutchinson Cancer Research Center at the University of Washington, Seattle.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASH 2015
Upfront idelalisib carries high risk for acute liver toxicity
ORLANDO – Idelalisib given as first-line therapy for patients with chronic lymphocytic leukemia carries a high risk of early fulminant hepatotoxicity requiring drug interruption and steroids, investigators reported.
Among 24 patients who received idelalisib (Zydelig) monotherapy in a phase II trial of a combination of idelalisib followed by idelalisib concurrent with ofatumumab (Arzerra) as first-line therapy for chronic lymphocytic leukemia (CLL), 12 patients developed acute hepatotoxicity, marked by rapidly soaring levels of transaminase within about 28 days of starting therapy. An additional four patients developed hepatotoxicity at around 130 days, noted Dr. Benjamin L. Lampson, a clinical fellow in medicine at the Dana-Farber Cancer Institute in Boston.
“Multiple lines of evidence suggest that this early hepatotoxicity is immune mediated. The proportion of regulatory T cells in the peripheral blood decrease on idelalisib therapy, providing a possible explanation for the development of early hepatotoxicity,” he said at the annual meeting of the American Society of Hematology.
The toxicities occur more frequently among younger and less heavily pretreated patients, and are likely due to on-target, immune-mediated effects, he noted.
Dr. Lampson presented data on the first 24 patients in an ongoing phase II trial. Patients with previously untreated CLL receive idelalisib 150 mg twice daily for 56 days, in an attempt to mobilize neoplastic B cells from the peripheral lymphoid tissues and into the bloodstream.
Following the monotherapy phase, patients are given ofatumumab in an attempt to clear the disease from peripheral blood.
“This dosing strategy is slightly different than what has been previously been used in trials combining these particular drugs. Specifically, previously reported trials have started these agents simultaneously without a lead-in period of monotherapy,” Dr. Lampson explained.
When the lead-in phase is completed, patients receive idelalisib plus ofatumumab infusions once weekly for 8 weeks, followed by once-monthly infusions for 4 months. Patients then continue on idelalisib indefinitely. The primary endpoint is the overall response rate assessed 2 months after the completion of the combination therapy.
For the first 24 patients treated as of Nov. 9, 2015, the median time on therapy was 7.7 months and median follow-up was 14.7 months.
The median patient age was 67.4 years (range 57.6-84.9). CLL genetics showed that 13 patients had unmutated immunoglobulin heavy chain variable region (IgHV) disease, 4 had the 17p deletion and TP53 mutation, 1 had deletion 11q, and 13 had deletion 13q; some patients had more than one mutation.
“What we began to notice after enrolling just a few subjects on the trial was that severe hepatotoxicity was occurring shortly after initiating idelalisib,” Dr. Lampson said.
He presented one case, a 58-year-old man who was in the idelalisib monotherapy phase of the study. He developed grade 3 hepatotoxicity 28 days after starting the drug, despite having a normal liver function test just 1 day earlier. The drug was stopped, but his liver function tests continued to rise, suggesting a self-perpetuating or self-sustaining process.
On day 32, the patient was admitted to the hospital, and on day 33 he was started on steroids, based on the hypothesis that the hepatotoxicity might have been immune mediated. Two days after initiation of steroids, his liver function tests continued to rise, whereupon he was started on mycophenolate mofetil.
“With these two forms of immunosuppression, the [liver function tests] did eventually normalize, although the steroids and mycophenolate had to be tapered over a period of many weeks. And this patient was not the only patient to experience toxicity; in fact, hepatotoxicity was frequent and often severe,” he said.
At the time of maximum incidence, week 4, the percentage of patients with any hepatotoxicity was 46%, with 13% at grade 4, and 21% at grade 3.
“The median time to initial development of hepatotoxicity is 28 days. This suggests that the mechanism of hepatotoxicity is not immediate, but takes time to develop, consistent with an adaptive immune response. Furthermore, hepatotoxicity is typically occurring before the first dose of ofatumumab is occurring at week 8, suggesting idelalisib alone is the cause of the hepatotoxicity,” Dr. Lampson said.
A comparison of data from the ongoing study and from three previous studies – two with idelalisib in relapsed refractory disease, and one as first-line therapy in patients 65 and older – showed that grade 3 or greater hepatotoxicity was lowest in a phase I trial of idelalisib in which patients had received a median of five prior lines of therapy, occurring in only 1.9% of patients. In contrast, in the current study, 52% of patients experienced grade 3 or 4 transaminitis at some point in the trial.
Evidence for the hepatotoxicity being an on-target immune-mediated effect comes from lymphocytic infiltrate on liver biopsy and lymphocytic colitis in idelalisib-treated patients. Additional evidence comes from the fact that the toxicity is both treatable and preventable with steroids, he said.
He cautioned that hepatotoxicity can recur rapidly when the drug is reintroduced.
“In general, our experience has been if idelalisib is resumed while the subject remains on steroids, the drug is more likely to be tolerated and the subject eventually can be tapered off steroids,” he said.
Asked by an audience member whether patients who are receiving idelalisib in the first-line setting should also receive steroids, Dr. Lampson said that they closely monitor patient liver enzymes around 28 days, and if grade 1 transaminitis is detected, patients are automatically started on low-dose steroids.
The study is sponsored by the Dana-Farber Cancer Institute in collaboration with Gilead Sciences and GlaxoSmithKline. Dr. Lampson and colleagues declared no relevant conflicts of interest.
ORLANDO – Idelalisib given as first-line therapy for patients with chronic lymphocytic leukemia carries a high risk of early fulminant hepatotoxicity requiring drug interruption and steroids, investigators reported.
Among 24 patients who received idelalisib (Zydelig) monotherapy in a phase II trial of a combination of idelalisib followed by idelalisib concurrent with ofatumumab (Arzerra) as first-line therapy for chronic lymphocytic leukemia (CLL), 12 patients developed acute hepatotoxicity, marked by rapidly soaring levels of transaminase within about 28 days of starting therapy. An additional four patients developed hepatotoxicity at around 130 days, noted Dr. Benjamin L. Lampson, a clinical fellow in medicine at the Dana-Farber Cancer Institute in Boston.
“Multiple lines of evidence suggest that this early hepatotoxicity is immune mediated. The proportion of regulatory T cells in the peripheral blood decrease on idelalisib therapy, providing a possible explanation for the development of early hepatotoxicity,” he said at the annual meeting of the American Society of Hematology.
The toxicities occur more frequently among younger and less heavily pretreated patients, and are likely due to on-target, immune-mediated effects, he noted.
Dr. Lampson presented data on the first 24 patients in an ongoing phase II trial. Patients with previously untreated CLL receive idelalisib 150 mg twice daily for 56 days, in an attempt to mobilize neoplastic B cells from the peripheral lymphoid tissues and into the bloodstream.
Following the monotherapy phase, patients are given ofatumumab in an attempt to clear the disease from peripheral blood.
“This dosing strategy is slightly different than what has been previously been used in trials combining these particular drugs. Specifically, previously reported trials have started these agents simultaneously without a lead-in period of monotherapy,” Dr. Lampson explained.
When the lead-in phase is completed, patients receive idelalisib plus ofatumumab infusions once weekly for 8 weeks, followed by once-monthly infusions for 4 months. Patients then continue on idelalisib indefinitely. The primary endpoint is the overall response rate assessed 2 months after the completion of the combination therapy.
For the first 24 patients treated as of Nov. 9, 2015, the median time on therapy was 7.7 months and median follow-up was 14.7 months.
The median patient age was 67.4 years (range 57.6-84.9). CLL genetics showed that 13 patients had unmutated immunoglobulin heavy chain variable region (IgHV) disease, 4 had the 17p deletion and TP53 mutation, 1 had deletion 11q, and 13 had deletion 13q; some patients had more than one mutation.
“What we began to notice after enrolling just a few subjects on the trial was that severe hepatotoxicity was occurring shortly after initiating idelalisib,” Dr. Lampson said.
He presented one case, a 58-year-old man who was in the idelalisib monotherapy phase of the study. He developed grade 3 hepatotoxicity 28 days after starting the drug, despite having a normal liver function test just 1 day earlier. The drug was stopped, but his liver function tests continued to rise, suggesting a self-perpetuating or self-sustaining process.
On day 32, the patient was admitted to the hospital, and on day 33 he was started on steroids, based on the hypothesis that the hepatotoxicity might have been immune mediated. Two days after initiation of steroids, his liver function tests continued to rise, whereupon he was started on mycophenolate mofetil.
“With these two forms of immunosuppression, the [liver function tests] did eventually normalize, although the steroids and mycophenolate had to be tapered over a period of many weeks. And this patient was not the only patient to experience toxicity; in fact, hepatotoxicity was frequent and often severe,” he said.
At the time of maximum incidence, week 4, the percentage of patients with any hepatotoxicity was 46%, with 13% at grade 4, and 21% at grade 3.
“The median time to initial development of hepatotoxicity is 28 days. This suggests that the mechanism of hepatotoxicity is not immediate, but takes time to develop, consistent with an adaptive immune response. Furthermore, hepatotoxicity is typically occurring before the first dose of ofatumumab is occurring at week 8, suggesting idelalisib alone is the cause of the hepatotoxicity,” Dr. Lampson said.
A comparison of data from the ongoing study and from three previous studies – two with idelalisib in relapsed refractory disease, and one as first-line therapy in patients 65 and older – showed that grade 3 or greater hepatotoxicity was lowest in a phase I trial of idelalisib in which patients had received a median of five prior lines of therapy, occurring in only 1.9% of patients. In contrast, in the current study, 52% of patients experienced grade 3 or 4 transaminitis at some point in the trial.
Evidence for the hepatotoxicity being an on-target immune-mediated effect comes from lymphocytic infiltrate on liver biopsy and lymphocytic colitis in idelalisib-treated patients. Additional evidence comes from the fact that the toxicity is both treatable and preventable with steroids, he said.
He cautioned that hepatotoxicity can recur rapidly when the drug is reintroduced.
“In general, our experience has been if idelalisib is resumed while the subject remains on steroids, the drug is more likely to be tolerated and the subject eventually can be tapered off steroids,” he said.
Asked by an audience member whether patients who are receiving idelalisib in the first-line setting should also receive steroids, Dr. Lampson said that they closely monitor patient liver enzymes around 28 days, and if grade 1 transaminitis is detected, patients are automatically started on low-dose steroids.
The study is sponsored by the Dana-Farber Cancer Institute in collaboration with Gilead Sciences and GlaxoSmithKline. Dr. Lampson and colleagues declared no relevant conflicts of interest.
ORLANDO – Idelalisib given as first-line therapy for patients with chronic lymphocytic leukemia carries a high risk of early fulminant hepatotoxicity requiring drug interruption and steroids, investigators reported.
Among 24 patients who received idelalisib (Zydelig) monotherapy in a phase II trial of a combination of idelalisib followed by idelalisib concurrent with ofatumumab (Arzerra) as first-line therapy for chronic lymphocytic leukemia (CLL), 12 patients developed acute hepatotoxicity, marked by rapidly soaring levels of transaminase within about 28 days of starting therapy. An additional four patients developed hepatotoxicity at around 130 days, noted Dr. Benjamin L. Lampson, a clinical fellow in medicine at the Dana-Farber Cancer Institute in Boston.
“Multiple lines of evidence suggest that this early hepatotoxicity is immune mediated. The proportion of regulatory T cells in the peripheral blood decrease on idelalisib therapy, providing a possible explanation for the development of early hepatotoxicity,” he said at the annual meeting of the American Society of Hematology.
The toxicities occur more frequently among younger and less heavily pretreated patients, and are likely due to on-target, immune-mediated effects, he noted.
Dr. Lampson presented data on the first 24 patients in an ongoing phase II trial. Patients with previously untreated CLL receive idelalisib 150 mg twice daily for 56 days, in an attempt to mobilize neoplastic B cells from the peripheral lymphoid tissues and into the bloodstream.
Following the monotherapy phase, patients are given ofatumumab in an attempt to clear the disease from peripheral blood.
“This dosing strategy is slightly different than what has been previously been used in trials combining these particular drugs. Specifically, previously reported trials have started these agents simultaneously without a lead-in period of monotherapy,” Dr. Lampson explained.
When the lead-in phase is completed, patients receive idelalisib plus ofatumumab infusions once weekly for 8 weeks, followed by once-monthly infusions for 4 months. Patients then continue on idelalisib indefinitely. The primary endpoint is the overall response rate assessed 2 months after the completion of the combination therapy.
For the first 24 patients treated as of Nov. 9, 2015, the median time on therapy was 7.7 months and median follow-up was 14.7 months.
The median patient age was 67.4 years (range 57.6-84.9). CLL genetics showed that 13 patients had unmutated immunoglobulin heavy chain variable region (IgHV) disease, 4 had the 17p deletion and TP53 mutation, 1 had deletion 11q, and 13 had deletion 13q; some patients had more than one mutation.
“What we began to notice after enrolling just a few subjects on the trial was that severe hepatotoxicity was occurring shortly after initiating idelalisib,” Dr. Lampson said.
He presented one case, a 58-year-old man who was in the idelalisib monotherapy phase of the study. He developed grade 3 hepatotoxicity 28 days after starting the drug, despite having a normal liver function test just 1 day earlier. The drug was stopped, but his liver function tests continued to rise, suggesting a self-perpetuating or self-sustaining process.
On day 32, the patient was admitted to the hospital, and on day 33 he was started on steroids, based on the hypothesis that the hepatotoxicity might have been immune mediated. Two days after initiation of steroids, his liver function tests continued to rise, whereupon he was started on mycophenolate mofetil.
“With these two forms of immunosuppression, the [liver function tests] did eventually normalize, although the steroids and mycophenolate had to be tapered over a period of many weeks. And this patient was not the only patient to experience toxicity; in fact, hepatotoxicity was frequent and often severe,” he said.
At the time of maximum incidence, week 4, the percentage of patients with any hepatotoxicity was 46%, with 13% at grade 4, and 21% at grade 3.
“The median time to initial development of hepatotoxicity is 28 days. This suggests that the mechanism of hepatotoxicity is not immediate, but takes time to develop, consistent with an adaptive immune response. Furthermore, hepatotoxicity is typically occurring before the first dose of ofatumumab is occurring at week 8, suggesting idelalisib alone is the cause of the hepatotoxicity,” Dr. Lampson said.
A comparison of data from the ongoing study and from three previous studies – two with idelalisib in relapsed refractory disease, and one as first-line therapy in patients 65 and older – showed that grade 3 or greater hepatotoxicity was lowest in a phase I trial of idelalisib in which patients had received a median of five prior lines of therapy, occurring in only 1.9% of patients. In contrast, in the current study, 52% of patients experienced grade 3 or 4 transaminitis at some point in the trial.
Evidence for the hepatotoxicity being an on-target immune-mediated effect comes from lymphocytic infiltrate on liver biopsy and lymphocytic colitis in idelalisib-treated patients. Additional evidence comes from the fact that the toxicity is both treatable and preventable with steroids, he said.
He cautioned that hepatotoxicity can recur rapidly when the drug is reintroduced.
“In general, our experience has been if idelalisib is resumed while the subject remains on steroids, the drug is more likely to be tolerated and the subject eventually can be tapered off steroids,” he said.
Asked by an audience member whether patients who are receiving idelalisib in the first-line setting should also receive steroids, Dr. Lampson said that they closely monitor patient liver enzymes around 28 days, and if grade 1 transaminitis is detected, patients are automatically started on low-dose steroids.
The study is sponsored by the Dana-Farber Cancer Institute in collaboration with Gilead Sciences and GlaxoSmithKline. Dr. Lampson and colleagues declared no relevant conflicts of interest.
AT ASH 2015
Key clinical point: Idelalisib in the first-line setting is associated with significant risk of hepatotoxicity, with a peak incidence at about 28 days of therapy.
Major finding: More than half (52%) of patients with newly diagnosed chronic lymphocytic leukemia had grade 3 or 4 hepatotoxicity with idelalisib monotherapy.
Data source: Ongoing phase II clinical trial with data on 24 patients.
Disclosures: The study is sponsored by the Dana-Farber Cancer Institute in collaboration with Gilead Sciences and GlaxoSmithKline. Dr. Lampson and colleagues declared no relevant conflicts of interest.
ASH: Prasugrel does not reduce vaso-occlusive crises in sickle cell anemia
Platelet inhibitor prasugrel has failed to show a significant reduction in the rate of vaso-occlusive crises events in children and adolescents with sickle cell anemia, according to data presented Dec. 8 at the annual meeting of the American Society of Hematology.
The phase III randomized placebo-controlled trial of 341 children and adolescents (aged 2-17 years), known as the Determining Effects of Platelet Inhibition on Vaso-Occlusive Events (DOVE) trial – simultaneously published in the New England Journal of Medicine – showed the rate of vaso-occlusive crises was 2.30 per person-year in the prasugrel group and 2.77 in the placebo group (rate ratio 0.83, 95% confidence interval 0.66-1.05, P = 0.12), with a slightly greater but still nonsignificant reduction among the older patients aged 12-17 years.
Treatment with prasugrel did not achieve any significant reductions in secondary outcomes of hospitalizations for vaso-occlusive crises, red-cell transfusions, pain rate or intensity, analgesic use, or school absences, compared with placebo. Platelet reactivity, however, was significantly lower in the prasugrel group (N Engl J Med. 2015, Dec 8. doi: 10.1056/NEJMoa1512021).
“Sickle cell anemia is a heterogeneous and complex disease in which platelet activation is only one of several mechanisms of vascular injury, which perhaps explains why prasugrel was ineffective,” wrote Dr. Matthew M. Heeney of Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, and his coauthors.
“However, the nonsignificant effect of prasugrel in the oldest age group may suggest that platelet activation is relatively more important in these older patients, a hypothesis that is consistent with the fact that endothelial dysfunction in sickle cell disease is progressive.”
Daiichi Sankyo and Eli Lilly funded the study. Several authors disclosed ties with Eli Lilly or other pharmaceutical companies. Three authors were employees of Eli Lilly, and one was an employee of Daiichi Sankyo.
Platelet inhibitor prasugrel has failed to show a significant reduction in the rate of vaso-occlusive crises events in children and adolescents with sickle cell anemia, according to data presented Dec. 8 at the annual meeting of the American Society of Hematology.
The phase III randomized placebo-controlled trial of 341 children and adolescents (aged 2-17 years), known as the Determining Effects of Platelet Inhibition on Vaso-Occlusive Events (DOVE) trial – simultaneously published in the New England Journal of Medicine – showed the rate of vaso-occlusive crises was 2.30 per person-year in the prasugrel group and 2.77 in the placebo group (rate ratio 0.83, 95% confidence interval 0.66-1.05, P = 0.12), with a slightly greater but still nonsignificant reduction among the older patients aged 12-17 years.
Treatment with prasugrel did not achieve any significant reductions in secondary outcomes of hospitalizations for vaso-occlusive crises, red-cell transfusions, pain rate or intensity, analgesic use, or school absences, compared with placebo. Platelet reactivity, however, was significantly lower in the prasugrel group (N Engl J Med. 2015, Dec 8. doi: 10.1056/NEJMoa1512021).
“Sickle cell anemia is a heterogeneous and complex disease in which platelet activation is only one of several mechanisms of vascular injury, which perhaps explains why prasugrel was ineffective,” wrote Dr. Matthew M. Heeney of Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, and his coauthors.
“However, the nonsignificant effect of prasugrel in the oldest age group may suggest that platelet activation is relatively more important in these older patients, a hypothesis that is consistent with the fact that endothelial dysfunction in sickle cell disease is progressive.”
Daiichi Sankyo and Eli Lilly funded the study. Several authors disclosed ties with Eli Lilly or other pharmaceutical companies. Three authors were employees of Eli Lilly, and one was an employee of Daiichi Sankyo.
Platelet inhibitor prasugrel has failed to show a significant reduction in the rate of vaso-occlusive crises events in children and adolescents with sickle cell anemia, according to data presented Dec. 8 at the annual meeting of the American Society of Hematology.
The phase III randomized placebo-controlled trial of 341 children and adolescents (aged 2-17 years), known as the Determining Effects of Platelet Inhibition on Vaso-Occlusive Events (DOVE) trial – simultaneously published in the New England Journal of Medicine – showed the rate of vaso-occlusive crises was 2.30 per person-year in the prasugrel group and 2.77 in the placebo group (rate ratio 0.83, 95% confidence interval 0.66-1.05, P = 0.12), with a slightly greater but still nonsignificant reduction among the older patients aged 12-17 years.
Treatment with prasugrel did not achieve any significant reductions in secondary outcomes of hospitalizations for vaso-occlusive crises, red-cell transfusions, pain rate or intensity, analgesic use, or school absences, compared with placebo. Platelet reactivity, however, was significantly lower in the prasugrel group (N Engl J Med. 2015, Dec 8. doi: 10.1056/NEJMoa1512021).
“Sickle cell anemia is a heterogeneous and complex disease in which platelet activation is only one of several mechanisms of vascular injury, which perhaps explains why prasugrel was ineffective,” wrote Dr. Matthew M. Heeney of Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, and his coauthors.
“However, the nonsignificant effect of prasugrel in the oldest age group may suggest that platelet activation is relatively more important in these older patients, a hypothesis that is consistent with the fact that endothelial dysfunction in sickle cell disease is progressive.”
Daiichi Sankyo and Eli Lilly funded the study. Several authors disclosed ties with Eli Lilly or other pharmaceutical companies. Three authors were employees of Eli Lilly, and one was an employee of Daiichi Sankyo.
FROM ASH 2015
Key clinical point: Platelet inhibitor prasugrel does not reduce the rate of vaso-occlusive crises events in young patients with sickle cell anemia.
Major finding: Prasugrel did not achieve a significant reduction in vaso-occlusive crises, compared with placebo.
Data source: A phase III randomized placebo-controlled trial of 341 children and adolescents with sickle cell anemia.
Disclosures: Daiichi Sankyo and Eli Lilly funded the study. Several authors disclosed ties with Eli Lilly or other pharmaceutical companies. Three authors were employees of Eli Lilly, and one was an employee of Daiichi Sankyo.
VIDEO: ASH highlights five Choosing Wisely initiatives
ORLANDO – Five “Choosing Wisely” initiatives selected from other specialties were featured at the annual meeting of the American Society of Hematology.
Dr. Lisa Hicks of St. Michael’s Hospital in Toronto led ASH’s Choosing Wisely list and moderated their presentation and the discussion of this year’s recommendations at the meeting. In a video interview, Dr. Hicks discussed the five recommendations and how hematologists can influence better patient care through cross-specialty collaborations. The complete Choosing Wisely list is available at www.hematology.org/choosingwisely
The 2015 Choosing Wisely recommendations, selected from recommendations made previously by other organizations, are:
• Don’t image for suspected pulmonary embolism (PE) without moderate or high pre-test probability of PE. (American College of Radiology)
• Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability. (Society of Hospital Medicine)
• Don’t routinely order thrombophilia testing on patients undergoing a routine infertility evaluation. (American Society of Reproductive Medicine)
• Don’t transfuse red blood cells for iron deficiency without hemodynamic instability. (American Association of Blood Banks)
• Avoid using PET or PET-CT scanning as part of routine follow-up care to monitor for a cancer recurrence in asymptomatic patients who have finished initial treatment to eliminate the cancer unless there is high-level evidence that such imaging will change the outcome. (American Society of Clinical Oncology)
Choosing Wisely is an initiative of the ABIM Foundation. Dr. Hicks had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Five “Choosing Wisely” initiatives selected from other specialties were featured at the annual meeting of the American Society of Hematology.
Dr. Lisa Hicks of St. Michael’s Hospital in Toronto led ASH’s Choosing Wisely list and moderated their presentation and the discussion of this year’s recommendations at the meeting. In a video interview, Dr. Hicks discussed the five recommendations and how hematologists can influence better patient care through cross-specialty collaborations. The complete Choosing Wisely list is available at www.hematology.org/choosingwisely
The 2015 Choosing Wisely recommendations, selected from recommendations made previously by other organizations, are:
• Don’t image for suspected pulmonary embolism (PE) without moderate or high pre-test probability of PE. (American College of Radiology)
• Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability. (Society of Hospital Medicine)
• Don’t routinely order thrombophilia testing on patients undergoing a routine infertility evaluation. (American Society of Reproductive Medicine)
• Don’t transfuse red blood cells for iron deficiency without hemodynamic instability. (American Association of Blood Banks)
• Avoid using PET or PET-CT scanning as part of routine follow-up care to monitor for a cancer recurrence in asymptomatic patients who have finished initial treatment to eliminate the cancer unless there is high-level evidence that such imaging will change the outcome. (American Society of Clinical Oncology)
Choosing Wisely is an initiative of the ABIM Foundation. Dr. Hicks had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Five “Choosing Wisely” initiatives selected from other specialties were featured at the annual meeting of the American Society of Hematology.
Dr. Lisa Hicks of St. Michael’s Hospital in Toronto led ASH’s Choosing Wisely list and moderated their presentation and the discussion of this year’s recommendations at the meeting. In a video interview, Dr. Hicks discussed the five recommendations and how hematologists can influence better patient care through cross-specialty collaborations. The complete Choosing Wisely list is available at www.hematology.org/choosingwisely
The 2015 Choosing Wisely recommendations, selected from recommendations made previously by other organizations, are:
• Don’t image for suspected pulmonary embolism (PE) without moderate or high pre-test probability of PE. (American College of Radiology)
• Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability. (Society of Hospital Medicine)
• Don’t routinely order thrombophilia testing on patients undergoing a routine infertility evaluation. (American Society of Reproductive Medicine)
• Don’t transfuse red blood cells for iron deficiency without hemodynamic instability. (American Association of Blood Banks)
• Avoid using PET or PET-CT scanning as part of routine follow-up care to monitor for a cancer recurrence in asymptomatic patients who have finished initial treatment to eliminate the cancer unless there is high-level evidence that such imaging will change the outcome. (American Society of Clinical Oncology)
Choosing Wisely is an initiative of the ABIM Foundation. Dr. Hicks had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASH 2015
RBC storage duration doesn’t affect outcomes in kids

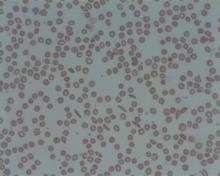
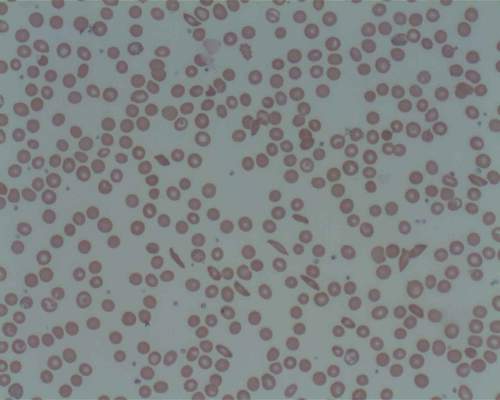
Photo by Elise Amendola
ORLANDO, FL—The storage duration of red blood cells (RBCs) doesn’t affect transfusion outcomes in children with lactic acidosis due to severe anemia, according to a new study.
Investigators found no significant differences in lactate levels, 30-day recovery, survival, or adverse events between children who received RBCs stored for 25 to 35 days and children who received RBCs stored for 1 to 10 days.
These results were published in JAMA and presented at the 2015 ASH Annual Meeting as abstract 769.
Christine Cserti-Gazdewich, MD, of University Health Network in Toronto, Canada, provided insights on the data during a press conference at ASH.
A concern of the investigators, according to Dr Cserti-Gazdewich, was that previous studies on blood storage were conducted in “high-income countries in high-technology care settings with blood inventory wealth, and findings may not be generalizable to the other half of the world.”
She pointed out that, in less developed countries, the shortfall in blood availability compared to the need is up to 3-fold.
So the investigators examined whether longer-stored red blood cells actually deliver oxygen in a manner not worse than shorter-stored or fresh blood and examined it at the extremes of storage duration in the context of a very high-dose need.
The team evaluated 290 children (aged 6 months to 60 months) with elevated blood lactate levels due to severe anemia who presented at a university-affiliated national referral hospital in Kampala, Uganda.
The children were randomized to receive RBC units stored for 25 to 35 days (longer-storage group, n=145) or RBCs stored for 1 to 10 days (shorter-storage group, n=145).
All units were leukoreduced prior to storage. All patients received 10 mL/kg of RBCs during hours 0 through 2 and, if indicated per protocol, an additional 10 mL/kg during hours 4 through 6.
In the entire population, the mean presenting hemoglobin level was 3.7 g/dL, and the mean lactate level was 9.3 mmol/L. The median RBC unit storage duration was 8 days (range, 7-9) for the shorter-storage group and 32 days (range, 30-34) for the longer-storage group.
Results
The investigators found that RBC units maintained under standard storage conditions for 25 to 35 days were not inferior to RBC units stored for up to 10 days.
The study’s primary endpoint was the proportion of patients with a lactate level of 3 mmol/L or lower at 8 hours, using a margin of noninferiority equal to an absolute difference of 25%.
The proportion of patients meeting this endpoint was 0.61 in the longer-storage group and 0.58 in the shorter-storage group (P<0.001 for noninferiority).
Average lactate levels were not statistically different between the 2 groups at 0, 2, 4, 6, 8, or 24 hours. And there was no statistical difference in the median time to achieve a blood lactate of 3 mmol/L or lower at 4 hours (hazard ratio=0.99, P=0.92).
Cerebral tissue oxygen saturation rose significantly during transfusion, but there was no significant difference between the 2 storage groups. The median area under the curve of cerebral tissue oxygen saturation during transfusion was 679 (range, 334-1156) for the longer-storage group and 521 (range, 303-835) for the shorter-storage group (P=0.25).
There was no significant difference between the longer-storage group and the shorter-storage group in the persistence of stupor or coma 8 hours after transfusion (12.6% and 19.6%, respectively, P=0.11) or the persistence of respiratory distress at 8 hours (28.7% and 30%, respectively, P=0.79).
The median length of hospital stay was 4 days (range, 2-6) in the longer-storage group and 4 days (range, 3-7) in the shorter-storage group.
There were 8 deaths, 3 in the longer-storage group and 5 in the shorter-storage group, during the 24 hours from the start of transfusion. Four additional patients, 2 in each group, died in the hospital after the initial 24-hour observation period.
The proportion of patients who had returned to good health by 30 days was 86% of the longer-storage group and 93% of the shorter-storage group (P=0.13).
“By every single measure we explored, and we explored many, we found that long-stored blood was not inferior . . . ,” Dr Csert-Gazdewich said. “We truly found no justification to shorten the current storage duration of red cells as judged by the fundamental role to deliver oxygen.” ![]()

Photo by Elise Amendola
ORLANDO, FL—The storage duration of red blood cells (RBCs) doesn’t affect transfusion outcomes in children with lactic acidosis due to severe anemia, according to a new study.
Investigators found no significant differences in lactate levels, 30-day recovery, survival, or adverse events between children who received RBCs stored for 25 to 35 days and children who received RBCs stored for 1 to 10 days.
These results were published in JAMA and presented at the 2015 ASH Annual Meeting as abstract 769.
Christine Cserti-Gazdewich, MD, of University Health Network in Toronto, Canada, provided insights on the data during a press conference at ASH.
A concern of the investigators, according to Dr Cserti-Gazdewich, was that previous studies on blood storage were conducted in “high-income countries in high-technology care settings with blood inventory wealth, and findings may not be generalizable to the other half of the world.”
She pointed out that, in less developed countries, the shortfall in blood availability compared to the need is up to 3-fold.
So the investigators examined whether longer-stored red blood cells actually deliver oxygen in a manner not worse than shorter-stored or fresh blood and examined it at the extremes of storage duration in the context of a very high-dose need.
The team evaluated 290 children (aged 6 months to 60 months) with elevated blood lactate levels due to severe anemia who presented at a university-affiliated national referral hospital in Kampala, Uganda.
The children were randomized to receive RBC units stored for 25 to 35 days (longer-storage group, n=145) or RBCs stored for 1 to 10 days (shorter-storage group, n=145).
All units were leukoreduced prior to storage. All patients received 10 mL/kg of RBCs during hours 0 through 2 and, if indicated per protocol, an additional 10 mL/kg during hours 4 through 6.
In the entire population, the mean presenting hemoglobin level was 3.7 g/dL, and the mean lactate level was 9.3 mmol/L. The median RBC unit storage duration was 8 days (range, 7-9) for the shorter-storage group and 32 days (range, 30-34) for the longer-storage group.
Results
The investigators found that RBC units maintained under standard storage conditions for 25 to 35 days were not inferior to RBC units stored for up to 10 days.
The study’s primary endpoint was the proportion of patients with a lactate level of 3 mmol/L or lower at 8 hours, using a margin of noninferiority equal to an absolute difference of 25%.
The proportion of patients meeting this endpoint was 0.61 in the longer-storage group and 0.58 in the shorter-storage group (P<0.001 for noninferiority).
Average lactate levels were not statistically different between the 2 groups at 0, 2, 4, 6, 8, or 24 hours. And there was no statistical difference in the median time to achieve a blood lactate of 3 mmol/L or lower at 4 hours (hazard ratio=0.99, P=0.92).
Cerebral tissue oxygen saturation rose significantly during transfusion, but there was no significant difference between the 2 storage groups. The median area under the curve of cerebral tissue oxygen saturation during transfusion was 679 (range, 334-1156) for the longer-storage group and 521 (range, 303-835) for the shorter-storage group (P=0.25).
There was no significant difference between the longer-storage group and the shorter-storage group in the persistence of stupor or coma 8 hours after transfusion (12.6% and 19.6%, respectively, P=0.11) or the persistence of respiratory distress at 8 hours (28.7% and 30%, respectively, P=0.79).
The median length of hospital stay was 4 days (range, 2-6) in the longer-storage group and 4 days (range, 3-7) in the shorter-storage group.
There were 8 deaths, 3 in the longer-storage group and 5 in the shorter-storage group, during the 24 hours from the start of transfusion. Four additional patients, 2 in each group, died in the hospital after the initial 24-hour observation period.
The proportion of patients who had returned to good health by 30 days was 86% of the longer-storage group and 93% of the shorter-storage group (P=0.13).
“By every single measure we explored, and we explored many, we found that long-stored blood was not inferior . . . ,” Dr Csert-Gazdewich said. “We truly found no justification to shorten the current storage duration of red cells as judged by the fundamental role to deliver oxygen.” ![]()

Photo by Elise Amendola
ORLANDO, FL—The storage duration of red blood cells (RBCs) doesn’t affect transfusion outcomes in children with lactic acidosis due to severe anemia, according to a new study.
Investigators found no significant differences in lactate levels, 30-day recovery, survival, or adverse events between children who received RBCs stored for 25 to 35 days and children who received RBCs stored for 1 to 10 days.
These results were published in JAMA and presented at the 2015 ASH Annual Meeting as abstract 769.
Christine Cserti-Gazdewich, MD, of University Health Network in Toronto, Canada, provided insights on the data during a press conference at ASH.
A concern of the investigators, according to Dr Cserti-Gazdewich, was that previous studies on blood storage were conducted in “high-income countries in high-technology care settings with blood inventory wealth, and findings may not be generalizable to the other half of the world.”
She pointed out that, in less developed countries, the shortfall in blood availability compared to the need is up to 3-fold.
So the investigators examined whether longer-stored red blood cells actually deliver oxygen in a manner not worse than shorter-stored or fresh blood and examined it at the extremes of storage duration in the context of a very high-dose need.
The team evaluated 290 children (aged 6 months to 60 months) with elevated blood lactate levels due to severe anemia who presented at a university-affiliated national referral hospital in Kampala, Uganda.
The children were randomized to receive RBC units stored for 25 to 35 days (longer-storage group, n=145) or RBCs stored for 1 to 10 days (shorter-storage group, n=145).
All units were leukoreduced prior to storage. All patients received 10 mL/kg of RBCs during hours 0 through 2 and, if indicated per protocol, an additional 10 mL/kg during hours 4 through 6.
In the entire population, the mean presenting hemoglobin level was 3.7 g/dL, and the mean lactate level was 9.3 mmol/L. The median RBC unit storage duration was 8 days (range, 7-9) for the shorter-storage group and 32 days (range, 30-34) for the longer-storage group.
Results
The investigators found that RBC units maintained under standard storage conditions for 25 to 35 days were not inferior to RBC units stored for up to 10 days.
The study’s primary endpoint was the proportion of patients with a lactate level of 3 mmol/L or lower at 8 hours, using a margin of noninferiority equal to an absolute difference of 25%.
The proportion of patients meeting this endpoint was 0.61 in the longer-storage group and 0.58 in the shorter-storage group (P<0.001 for noninferiority).
Average lactate levels were not statistically different between the 2 groups at 0, 2, 4, 6, 8, or 24 hours. And there was no statistical difference in the median time to achieve a blood lactate of 3 mmol/L or lower at 4 hours (hazard ratio=0.99, P=0.92).
Cerebral tissue oxygen saturation rose significantly during transfusion, but there was no significant difference between the 2 storage groups. The median area under the curve of cerebral tissue oxygen saturation during transfusion was 679 (range, 334-1156) for the longer-storage group and 521 (range, 303-835) for the shorter-storage group (P=0.25).
There was no significant difference between the longer-storage group and the shorter-storage group in the persistence of stupor or coma 8 hours after transfusion (12.6% and 19.6%, respectively, P=0.11) or the persistence of respiratory distress at 8 hours (28.7% and 30%, respectively, P=0.79).
The median length of hospital stay was 4 days (range, 2-6) in the longer-storage group and 4 days (range, 3-7) in the shorter-storage group.
There were 8 deaths, 3 in the longer-storage group and 5 in the shorter-storage group, during the 24 hours from the start of transfusion. Four additional patients, 2 in each group, died in the hospital after the initial 24-hour observation period.
The proportion of patients who had returned to good health by 30 days was 86% of the longer-storage group and 93% of the shorter-storage group (P=0.13).
“By every single measure we explored, and we explored many, we found that long-stored blood was not inferior . . . ,” Dr Csert-Gazdewich said. “We truly found no justification to shorten the current storage duration of red cells as judged by the fundamental role to deliver oxygen.” ![]()
Ibrutinib ‘treatment of choice’ in rel/ref MCL
Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—The BTK inhibitor ibrutinib should be considered the treatment of choice for patients with relapsed or refractory mantle cell lymphoma (MCL), according to a speaker at the 2015 ASH Annual Meeting.
Results of the phase 3 RAY trial showed that ibrutinib can prolong progression-free survival (PFS) when compared to the mTOR inhibitor temsirolimus.
There was no significant difference in overall survival (OS) between the treatment arms, but this outcome was influenced by the fact that patients were allowed to cross over from the temsirolimus arm to the ibrutinib arm after they progressed.
A majority of patients in both arms experienced adverse events (AEs), and the incidence of grade 3 or higher AEs was high—about 70% with ibrutinib and 90% with temsirolimus.
Simon Rule, MD, of Derriford Hospital in Plymouth, UK, presented these results at the meeting as abstract 469. The study has been published in The Lancet as well.
The research was sponsored by Janssen Biotech, Inc., which is jointly developing and commercializing ibrutinib with Pharmacyclics LLC, an AbbVie company.
Study design
The trial included 280 patients with relapsed or refractory MCL. They were enrolled from December 2012 to November 2013.
The patients were randomized to receive oral ibrutinib (n=139) at 560 mg or intravenous temsirolimus (n=141) at 175 mg on days 1, 8, and 15 of cycle 1 and 75 mg on days 1, 8, and 15 of all subsequent 21-day cycles until disease progression or unacceptable toxicity.
Starting July 2014, patients were allowed to cross over from the ibrutinib arm to the temsirolimus arm if they had progressive disease, as confirmed by an independent review committee. Thirty-two patients ultimately crossed over.
Patient characteristics
Baseline characteristics were similar between the treatment arms. The median age was 67 (range, 39-84) in the ibrutinib arm and 68 (range, 34-88) in the temsirolimus arm. Most patients had an ECOG performance status of 0 (48.2% and 47.5%, respectively) or 1 (51.1% in both arms).
The median number of prior therapies was 2 in both arms (range, 1-9). A majority of patients had 1 to 2 prior lines of therapy—68.3% in the ibrutinib arm and 66% in the temsirolimus arm.
The median time from the end of last therapy was 8.25 months for the ibrutinib arm and 7.03 months for the temsirolimus arm. And about 30% of patients in each arm were refractory to their last therapy—25.9% and 33.3%, respectively.
About half of patients in each arm had intermediate-risk disease (46.8% in the ibrutinib arm and 48.9% in the temsirolimus arm), followed by low-risk (31.7% and 29.8%, respectively) and high-risk disease (21.6% and 21.3%, respectively).
Most patients had stage IV disease—80.6% in the ibrutinib arm and 85.1% in the temsirolimus arm.
PFS
The study’s primary endpoint was PFS, as assessed by an independent review committee.
At a median follow-up of 20 months, the median PFS was 14.6 months for patients in the ibrutinib arm and 6.2 months for patients in the temsirolimus arm (hazard ratio=0.43, P<0.0001). At 2 years, the PFS was 41% in the ibrutinib arm and 7% in the temsirolimus arm.
Dr Rule noted that, looking at these data, people might question the validity of temsirolimus as a comparator to ibrutinib for this patient population.
“If you look at the median PFS for temsirolimus here, it’s 6.2 months,” he said. “In the registration study for Velcade—bortezomib—in the US, PFS was 6.5 months. If you look at the median PFS in the lenalidomide study that got registration, it was 4 months. So [the PFS for temsirolimus] is very representative of an oral novel agent in the context of mantle cell lymphoma.”
Dr Rule also pointed out that the improvement in PFS with ibrutinib was consistent across subgroups (ie, older age, risk score, tumor bulk, refractory disease). The only exception was patients with blastoid histology, but this was a very small group.
Secondary endpoints
The median OS was not reached in the ibrutinib arm but was 21.3 months in the temsirolimus arm.
This difference was not statistically significant, but Dr Rule noted that the trial was not powered for OS, and the analysis is confounded by the crossover. Twenty-three percent of patients in the temsirolimus arm ultimately received ibrutinib.
The overall response rate (ORR) was 71.9% in the ibrutinib arm and 40.4% in the temsirolimus arm (P<0.0001), according to the independent review committee. The complete response rates were 18.7% (n=26) and 1.4% (n=2), respectively.
The median duration of response was not reached with ibrutinib but was 7 months for temsirolimus. The median time to next treatment was not reached with ibrutinib, but it was 11.6 months in the temsirolimus arm (P<0.0001).
And the median duration of study treatment was 14.4 months in the ibrutinib arm and 3 months in the temsirolimus arm.
Timing counts
Dr Rule also presented response and PFS data according to the number of prior therapies patients received.
He noted that patients were more likely to respond to temsirolimus if they had received fewer prior therapies, but this was not the case with ibrutinib. Ibrutinib produced consistent ORRs regardless of when it was given.
In the ibrutinib arm, the ORR was 71.9% for patients who had received 1 prior line of therapy, 68.4% for those who received 2 prior therapies, and 75% for those who received 3 prior therapies. In the temsirolimus arm, the ORRs were 48%, 39.5%, and 33.3%, respectively.
Conversely, patients had a greater PFS benefit if they received ibrutinib earlier in their treatment course, but this was not true for temsirolimus.
At the median follow-up of 20 months, PFS was more than 60% for ibrutinib-treated patients who had received 1 prior line of therapy and less than 30% for ibrutinib-treated patients who received 2 or more prior lines of therapy. PFS was less than 15% for patients in the temsirolimus arm, regardless of their number of prior therapies.
“So that’s perhaps the first hint that, if we’re going to be using [ibrutinib], we should be using it earlier on,” Dr Rule said. “And I also suspect that, with further follow-up with this study, if this holds up, there will be, indeed, a survival benefit observed.”
Safety
“Despite patients on the ibrutinib arm being exposed to drug more than 4 times longer than those with temsirolimus, the frequency of most cumulative adverse events was lower in the ibrutinib arm,” Dr Rule said.
Still, he noted that most patients had some adverse events. And grade 3 or higher adverse events were reported in 67.6% of patients on ibrutinib and 87.1% of patients on temsirolimus.
Grade 3 or higher AEs included atrial fibrillation (AFib) and major bleeding. AFib occurred in 4.3% of patients in the ibrutinib arm and 1.4% in the temsirolimus arm. Major bleeding occurred in 10.1% and 6.5%, respectively.
Five of the 6 patients with AFib in the ibrutinib arm and all 3 patients who developed AFib in the temsirolimus arm had risk factors for AFib prior to treatment. None of these patients discontinued treatment due to AFib.
Dr Rule said there was no evidence to suggest that either drug increases the risk of second primary malignancies, although 3.6% of patients in the ibrutinib arm and 2.9% in the temsirolimus arm were diagnosed with second primary malignancies (mostly non-melanoma skin cancers).
The most common treatment-emergent AEs (≥20%) of any grade for the ibrutinib arm were diarrhea (28.8%), cough (22.3%), and fatigue (22.3%).
The most common treatment-emergent AEs (>20%) of any grade for the temsirolimus arm were thrombocytopenia (56.1%), anemia (43.2%), diarrhea (30.9%), fatigue (28.8%), neutropenia (25.9%), epistaxis (23.7%), cough (22.3%), peripheral edema (22.3%), nausea (21.6%), pyrexia (20.9%), and stomatitis (20.9%).
The most common hematologic AEs (≥10%) in the ibrutinib and temsirolimus arms, respectively, were thrombocytopenia (18% vs 56.1%), anemia (18% vs 43.2%), and neutropenia (15.8% vs 25.9%).
Six percent of patients in the ibrutinib arm and 26% in the temsirolimus arm discontinued treatment due to AEs.
At a median follow-up of 20 months, 42% of patients in the ibrutinib arm and 45% in the temsirolimus arm had died. The most common cause of death associated with ibrutinib was disease progression, and deaths in the temsirolimus arm were primarily attributed to AEs. ![]()
Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—The BTK inhibitor ibrutinib should be considered the treatment of choice for patients with relapsed or refractory mantle cell lymphoma (MCL), according to a speaker at the 2015 ASH Annual Meeting.
Results of the phase 3 RAY trial showed that ibrutinib can prolong progression-free survival (PFS) when compared to the mTOR inhibitor temsirolimus.
There was no significant difference in overall survival (OS) between the treatment arms, but this outcome was influenced by the fact that patients were allowed to cross over from the temsirolimus arm to the ibrutinib arm after they progressed.
A majority of patients in both arms experienced adverse events (AEs), and the incidence of grade 3 or higher AEs was high—about 70% with ibrutinib and 90% with temsirolimus.
Simon Rule, MD, of Derriford Hospital in Plymouth, UK, presented these results at the meeting as abstract 469. The study has been published in The Lancet as well.
The research was sponsored by Janssen Biotech, Inc., which is jointly developing and commercializing ibrutinib with Pharmacyclics LLC, an AbbVie company.
Study design
The trial included 280 patients with relapsed or refractory MCL. They were enrolled from December 2012 to November 2013.
The patients were randomized to receive oral ibrutinib (n=139) at 560 mg or intravenous temsirolimus (n=141) at 175 mg on days 1, 8, and 15 of cycle 1 and 75 mg on days 1, 8, and 15 of all subsequent 21-day cycles until disease progression or unacceptable toxicity.
Starting July 2014, patients were allowed to cross over from the ibrutinib arm to the temsirolimus arm if they had progressive disease, as confirmed by an independent review committee. Thirty-two patients ultimately crossed over.
Patient characteristics
Baseline characteristics were similar between the treatment arms. The median age was 67 (range, 39-84) in the ibrutinib arm and 68 (range, 34-88) in the temsirolimus arm. Most patients had an ECOG performance status of 0 (48.2% and 47.5%, respectively) or 1 (51.1% in both arms).
The median number of prior therapies was 2 in both arms (range, 1-9). A majority of patients had 1 to 2 prior lines of therapy—68.3% in the ibrutinib arm and 66% in the temsirolimus arm.
The median time from the end of last therapy was 8.25 months for the ibrutinib arm and 7.03 months for the temsirolimus arm. And about 30% of patients in each arm were refractory to their last therapy—25.9% and 33.3%, respectively.
About half of patients in each arm had intermediate-risk disease (46.8% in the ibrutinib arm and 48.9% in the temsirolimus arm), followed by low-risk (31.7% and 29.8%, respectively) and high-risk disease (21.6% and 21.3%, respectively).
Most patients had stage IV disease—80.6% in the ibrutinib arm and 85.1% in the temsirolimus arm.
PFS
The study’s primary endpoint was PFS, as assessed by an independent review committee.
At a median follow-up of 20 months, the median PFS was 14.6 months for patients in the ibrutinib arm and 6.2 months for patients in the temsirolimus arm (hazard ratio=0.43, P<0.0001). At 2 years, the PFS was 41% in the ibrutinib arm and 7% in the temsirolimus arm.
Dr Rule noted that, looking at these data, people might question the validity of temsirolimus as a comparator to ibrutinib for this patient population.
“If you look at the median PFS for temsirolimus here, it’s 6.2 months,” he said. “In the registration study for Velcade—bortezomib—in the US, PFS was 6.5 months. If you look at the median PFS in the lenalidomide study that got registration, it was 4 months. So [the PFS for temsirolimus] is very representative of an oral novel agent in the context of mantle cell lymphoma.”
Dr Rule also pointed out that the improvement in PFS with ibrutinib was consistent across subgroups (ie, older age, risk score, tumor bulk, refractory disease). The only exception was patients with blastoid histology, but this was a very small group.
Secondary endpoints
The median OS was not reached in the ibrutinib arm but was 21.3 months in the temsirolimus arm.
This difference was not statistically significant, but Dr Rule noted that the trial was not powered for OS, and the analysis is confounded by the crossover. Twenty-three percent of patients in the temsirolimus arm ultimately received ibrutinib.
The overall response rate (ORR) was 71.9% in the ibrutinib arm and 40.4% in the temsirolimus arm (P<0.0001), according to the independent review committee. The complete response rates were 18.7% (n=26) and 1.4% (n=2), respectively.
The median duration of response was not reached with ibrutinib but was 7 months for temsirolimus. The median time to next treatment was not reached with ibrutinib, but it was 11.6 months in the temsirolimus arm (P<0.0001).
And the median duration of study treatment was 14.4 months in the ibrutinib arm and 3 months in the temsirolimus arm.
Timing counts
Dr Rule also presented response and PFS data according to the number of prior therapies patients received.
He noted that patients were more likely to respond to temsirolimus if they had received fewer prior therapies, but this was not the case with ibrutinib. Ibrutinib produced consistent ORRs regardless of when it was given.
In the ibrutinib arm, the ORR was 71.9% for patients who had received 1 prior line of therapy, 68.4% for those who received 2 prior therapies, and 75% for those who received 3 prior therapies. In the temsirolimus arm, the ORRs were 48%, 39.5%, and 33.3%, respectively.
Conversely, patients had a greater PFS benefit if they received ibrutinib earlier in their treatment course, but this was not true for temsirolimus.
At the median follow-up of 20 months, PFS was more than 60% for ibrutinib-treated patients who had received 1 prior line of therapy and less than 30% for ibrutinib-treated patients who received 2 or more prior lines of therapy. PFS was less than 15% for patients in the temsirolimus arm, regardless of their number of prior therapies.
“So that’s perhaps the first hint that, if we’re going to be using [ibrutinib], we should be using it earlier on,” Dr Rule said. “And I also suspect that, with further follow-up with this study, if this holds up, there will be, indeed, a survival benefit observed.”
Safety
“Despite patients on the ibrutinib arm being exposed to drug more than 4 times longer than those with temsirolimus, the frequency of most cumulative adverse events was lower in the ibrutinib arm,” Dr Rule said.
Still, he noted that most patients had some adverse events. And grade 3 or higher adverse events were reported in 67.6% of patients on ibrutinib and 87.1% of patients on temsirolimus.
Grade 3 or higher AEs included atrial fibrillation (AFib) and major bleeding. AFib occurred in 4.3% of patients in the ibrutinib arm and 1.4% in the temsirolimus arm. Major bleeding occurred in 10.1% and 6.5%, respectively.
Five of the 6 patients with AFib in the ibrutinib arm and all 3 patients who developed AFib in the temsirolimus arm had risk factors for AFib prior to treatment. None of these patients discontinued treatment due to AFib.
Dr Rule said there was no evidence to suggest that either drug increases the risk of second primary malignancies, although 3.6% of patients in the ibrutinib arm and 2.9% in the temsirolimus arm were diagnosed with second primary malignancies (mostly non-melanoma skin cancers).
The most common treatment-emergent AEs (≥20%) of any grade for the ibrutinib arm were diarrhea (28.8%), cough (22.3%), and fatigue (22.3%).
The most common treatment-emergent AEs (>20%) of any grade for the temsirolimus arm were thrombocytopenia (56.1%), anemia (43.2%), diarrhea (30.9%), fatigue (28.8%), neutropenia (25.9%), epistaxis (23.7%), cough (22.3%), peripheral edema (22.3%), nausea (21.6%), pyrexia (20.9%), and stomatitis (20.9%).
The most common hematologic AEs (≥10%) in the ibrutinib and temsirolimus arms, respectively, were thrombocytopenia (18% vs 56.1%), anemia (18% vs 43.2%), and neutropenia (15.8% vs 25.9%).
Six percent of patients in the ibrutinib arm and 26% in the temsirolimus arm discontinued treatment due to AEs.
At a median follow-up of 20 months, 42% of patients in the ibrutinib arm and 45% in the temsirolimus arm had died. The most common cause of death associated with ibrutinib was disease progression, and deaths in the temsirolimus arm were primarily attributed to AEs. ![]()
Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—The BTK inhibitor ibrutinib should be considered the treatment of choice for patients with relapsed or refractory mantle cell lymphoma (MCL), according to a speaker at the 2015 ASH Annual Meeting.
Results of the phase 3 RAY trial showed that ibrutinib can prolong progression-free survival (PFS) when compared to the mTOR inhibitor temsirolimus.
There was no significant difference in overall survival (OS) between the treatment arms, but this outcome was influenced by the fact that patients were allowed to cross over from the temsirolimus arm to the ibrutinib arm after they progressed.
A majority of patients in both arms experienced adverse events (AEs), and the incidence of grade 3 or higher AEs was high—about 70% with ibrutinib and 90% with temsirolimus.
Simon Rule, MD, of Derriford Hospital in Plymouth, UK, presented these results at the meeting as abstract 469. The study has been published in The Lancet as well.
The research was sponsored by Janssen Biotech, Inc., which is jointly developing and commercializing ibrutinib with Pharmacyclics LLC, an AbbVie company.
Study design
The trial included 280 patients with relapsed or refractory MCL. They were enrolled from December 2012 to November 2013.
The patients were randomized to receive oral ibrutinib (n=139) at 560 mg or intravenous temsirolimus (n=141) at 175 mg on days 1, 8, and 15 of cycle 1 and 75 mg on days 1, 8, and 15 of all subsequent 21-day cycles until disease progression or unacceptable toxicity.
Starting July 2014, patients were allowed to cross over from the ibrutinib arm to the temsirolimus arm if they had progressive disease, as confirmed by an independent review committee. Thirty-two patients ultimately crossed over.
Patient characteristics
Baseline characteristics were similar between the treatment arms. The median age was 67 (range, 39-84) in the ibrutinib arm and 68 (range, 34-88) in the temsirolimus arm. Most patients had an ECOG performance status of 0 (48.2% and 47.5%, respectively) or 1 (51.1% in both arms).
The median number of prior therapies was 2 in both arms (range, 1-9). A majority of patients had 1 to 2 prior lines of therapy—68.3% in the ibrutinib arm and 66% in the temsirolimus arm.
The median time from the end of last therapy was 8.25 months for the ibrutinib arm and 7.03 months for the temsirolimus arm. And about 30% of patients in each arm were refractory to their last therapy—25.9% and 33.3%, respectively.
About half of patients in each arm had intermediate-risk disease (46.8% in the ibrutinib arm and 48.9% in the temsirolimus arm), followed by low-risk (31.7% and 29.8%, respectively) and high-risk disease (21.6% and 21.3%, respectively).
Most patients had stage IV disease—80.6% in the ibrutinib arm and 85.1% in the temsirolimus arm.
PFS
The study’s primary endpoint was PFS, as assessed by an independent review committee.
At a median follow-up of 20 months, the median PFS was 14.6 months for patients in the ibrutinib arm and 6.2 months for patients in the temsirolimus arm (hazard ratio=0.43, P<0.0001). At 2 years, the PFS was 41% in the ibrutinib arm and 7% in the temsirolimus arm.
Dr Rule noted that, looking at these data, people might question the validity of temsirolimus as a comparator to ibrutinib for this patient population.
“If you look at the median PFS for temsirolimus here, it’s 6.2 months,” he said. “In the registration study for Velcade—bortezomib—in the US, PFS was 6.5 months. If you look at the median PFS in the lenalidomide study that got registration, it was 4 months. So [the PFS for temsirolimus] is very representative of an oral novel agent in the context of mantle cell lymphoma.”
Dr Rule also pointed out that the improvement in PFS with ibrutinib was consistent across subgroups (ie, older age, risk score, tumor bulk, refractory disease). The only exception was patients with blastoid histology, but this was a very small group.
Secondary endpoints
The median OS was not reached in the ibrutinib arm but was 21.3 months in the temsirolimus arm.
This difference was not statistically significant, but Dr Rule noted that the trial was not powered for OS, and the analysis is confounded by the crossover. Twenty-three percent of patients in the temsirolimus arm ultimately received ibrutinib.
The overall response rate (ORR) was 71.9% in the ibrutinib arm and 40.4% in the temsirolimus arm (P<0.0001), according to the independent review committee. The complete response rates were 18.7% (n=26) and 1.4% (n=2), respectively.
The median duration of response was not reached with ibrutinib but was 7 months for temsirolimus. The median time to next treatment was not reached with ibrutinib, but it was 11.6 months in the temsirolimus arm (P<0.0001).
And the median duration of study treatment was 14.4 months in the ibrutinib arm and 3 months in the temsirolimus arm.
Timing counts
Dr Rule also presented response and PFS data according to the number of prior therapies patients received.
He noted that patients were more likely to respond to temsirolimus if they had received fewer prior therapies, but this was not the case with ibrutinib. Ibrutinib produced consistent ORRs regardless of when it was given.
In the ibrutinib arm, the ORR was 71.9% for patients who had received 1 prior line of therapy, 68.4% for those who received 2 prior therapies, and 75% for those who received 3 prior therapies. In the temsirolimus arm, the ORRs were 48%, 39.5%, and 33.3%, respectively.
Conversely, patients had a greater PFS benefit if they received ibrutinib earlier in their treatment course, but this was not true for temsirolimus.
At the median follow-up of 20 months, PFS was more than 60% for ibrutinib-treated patients who had received 1 prior line of therapy and less than 30% for ibrutinib-treated patients who received 2 or more prior lines of therapy. PFS was less than 15% for patients in the temsirolimus arm, regardless of their number of prior therapies.
“So that’s perhaps the first hint that, if we’re going to be using [ibrutinib], we should be using it earlier on,” Dr Rule said. “And I also suspect that, with further follow-up with this study, if this holds up, there will be, indeed, a survival benefit observed.”
Safety
“Despite patients on the ibrutinib arm being exposed to drug more than 4 times longer than those with temsirolimus, the frequency of most cumulative adverse events was lower in the ibrutinib arm,” Dr Rule said.
Still, he noted that most patients had some adverse events. And grade 3 or higher adverse events were reported in 67.6% of patients on ibrutinib and 87.1% of patients on temsirolimus.
Grade 3 or higher AEs included atrial fibrillation (AFib) and major bleeding. AFib occurred in 4.3% of patients in the ibrutinib arm and 1.4% in the temsirolimus arm. Major bleeding occurred in 10.1% and 6.5%, respectively.
Five of the 6 patients with AFib in the ibrutinib arm and all 3 patients who developed AFib in the temsirolimus arm had risk factors for AFib prior to treatment. None of these patients discontinued treatment due to AFib.
Dr Rule said there was no evidence to suggest that either drug increases the risk of second primary malignancies, although 3.6% of patients in the ibrutinib arm and 2.9% in the temsirolimus arm were diagnosed with second primary malignancies (mostly non-melanoma skin cancers).
The most common treatment-emergent AEs (≥20%) of any grade for the ibrutinib arm were diarrhea (28.8%), cough (22.3%), and fatigue (22.3%).
The most common treatment-emergent AEs (>20%) of any grade for the temsirolimus arm were thrombocytopenia (56.1%), anemia (43.2%), diarrhea (30.9%), fatigue (28.8%), neutropenia (25.9%), epistaxis (23.7%), cough (22.3%), peripheral edema (22.3%), nausea (21.6%), pyrexia (20.9%), and stomatitis (20.9%).
The most common hematologic AEs (≥10%) in the ibrutinib and temsirolimus arms, respectively, were thrombocytopenia (18% vs 56.1%), anemia (18% vs 43.2%), and neutropenia (15.8% vs 25.9%).
Six percent of patients in the ibrutinib arm and 26% in the temsirolimus arm discontinued treatment due to AEs.
At a median follow-up of 20 months, 42% of patients in the ibrutinib arm and 45% in the temsirolimus arm had died. The most common cause of death associated with ibrutinib was disease progression, and deaths in the temsirolimus arm were primarily attributed to AEs. ![]()
ALL patients over-report their 6MP compliance, researchers say

Photo courtesy of ASH
ORLANDO, FL—A study comparing subjective versus objective reporting of treatment compliance in patients with acute lymphoblastic leukemia (ALL) has shown that about a fourth of patients over-report how compliant they are with taking 6-mercaptopurine (6MP) as part of their maintenance therapy.
An earlier analysis of the Children’s Oncology Group (COG) AALL03N1 compliance study showed that adherence rates of less than 95% were associated with a 3.7-fold increased risk of relapse.
And about 40% of patients were non-adherent. Yet patients indicate they are taking their medication when questioned.
“We ask our patients if they are taking their meds,” said Wendy Landier, PhD, “and they tell us they are.”
“Even in this cohort who were being closely monitored and knew that they were being closely monitored electronically and were asked to self-report, we found over-reporting.”
Dr Landier, of the University of Alabama at Birmingham, reported these findings comparing self-reported adherence with electronic monitoring of 6MP intake at the 2015 ASH Annual Meeting (abstract 82).
The investigators collected data over 6 months from 416 ALL patients who were 21 years at diagnosis or younger and were receiving 6MP as part of their maintenance therapy.
Investigators measured subjective self-reporting by a patient questionnaire, which included patient demographic information in addition to the number of days the patient took 6MP over the past month.
For the objective medication event-monitoring system (MEMS), patients received a 6MP bottle that was fitted with a TrackCapTM. The cap had a microprocessor chip that recorded the date and time of each bottle opening.
Investigators downloaded the data at the end of the study. They then compared the MEMS with the self-reported data.
The investigators classified perfect reporters as those whose self-report corresponded to their MEMS.
They classified over-reporters as those whose self-report was greater than their MEMS data for 5 days or more and 50% of the months.
The rest they classified as others.
Patients were a median age of 6.0 years, and 277 (66.6%) were male. Parents completed the survey for patients younger than 12.
Two hundred forty-two patients (60.9%) had fathers whose education was less than some college, 159 (38.4%) had NCI high-risk disease, and 168 (40.4%) were non-adherent to 6MP as determined by earlier analysis of the COG AALL03N1 study.
Thirty-six percent were non-Hispanic white, 37% were Hispanic, 14% Asian, and 13% African American.
The investigators monitored the patients’ 6MP intake for a total of 1344 patient-months at 87 COG sites.
And the correlation between subjective and objective reporting was moderate, Dr Landier said, with the correlation ranging from 0.36 to 0.58.
Twelve percent of the patients were perfect reporters, with no difference between the reporting methods.
Twenty-four percent over-reported their intake, 1% under-reported their intake, and 64% were other.
The investigators analyzed variables associated with over-reporting and found that age 12 years or older (P=0.02), being Hispanic (P=0.02), Asian (P=0.02), or African American (P<0.001), paternal education less than college (P=0.02), and being classified as 6MP non-adherent (P<0.001) were all significant.
“Over-reporting of 6MP ingestion is common,” Dr Landier said, with 88% of patients or parents over-reporting the number of days 6MP was taken.
“What we’ve learned from this study is that we cannot rely on patients’ self-report in the clinic,” she said. “What we found is that only 12% of our patients are perfect, so to speak, and that the others mainly over-estimate, and I don’t believe intentionally.”
“[W]e need to have a better way of identifying which patients are at risk for over-reporting their intake, whether they’re aware of it or not,” she added. ![]()

Photo courtesy of ASH
ORLANDO, FL—A study comparing subjective versus objective reporting of treatment compliance in patients with acute lymphoblastic leukemia (ALL) has shown that about a fourth of patients over-report how compliant they are with taking 6-mercaptopurine (6MP) as part of their maintenance therapy.
An earlier analysis of the Children’s Oncology Group (COG) AALL03N1 compliance study showed that adherence rates of less than 95% were associated with a 3.7-fold increased risk of relapse.
And about 40% of patients were non-adherent. Yet patients indicate they are taking their medication when questioned.
“We ask our patients if they are taking their meds,” said Wendy Landier, PhD, “and they tell us they are.”
“Even in this cohort who were being closely monitored and knew that they were being closely monitored electronically and were asked to self-report, we found over-reporting.”
Dr Landier, of the University of Alabama at Birmingham, reported these findings comparing self-reported adherence with electronic monitoring of 6MP intake at the 2015 ASH Annual Meeting (abstract 82).
The investigators collected data over 6 months from 416 ALL patients who were 21 years at diagnosis or younger and were receiving 6MP as part of their maintenance therapy.
Investigators measured subjective self-reporting by a patient questionnaire, which included patient demographic information in addition to the number of days the patient took 6MP over the past month.
For the objective medication event-monitoring system (MEMS), patients received a 6MP bottle that was fitted with a TrackCapTM. The cap had a microprocessor chip that recorded the date and time of each bottle opening.
Investigators downloaded the data at the end of the study. They then compared the MEMS with the self-reported data.
The investigators classified perfect reporters as those whose self-report corresponded to their MEMS.
They classified over-reporters as those whose self-report was greater than their MEMS data for 5 days or more and 50% of the months.
The rest they classified as others.
Patients were a median age of 6.0 years, and 277 (66.6%) were male. Parents completed the survey for patients younger than 12.
Two hundred forty-two patients (60.9%) had fathers whose education was less than some college, 159 (38.4%) had NCI high-risk disease, and 168 (40.4%) were non-adherent to 6MP as determined by earlier analysis of the COG AALL03N1 study.
Thirty-six percent were non-Hispanic white, 37% were Hispanic, 14% Asian, and 13% African American.
The investigators monitored the patients’ 6MP intake for a total of 1344 patient-months at 87 COG sites.
And the correlation between subjective and objective reporting was moderate, Dr Landier said, with the correlation ranging from 0.36 to 0.58.
Twelve percent of the patients were perfect reporters, with no difference between the reporting methods.
Twenty-four percent over-reported their intake, 1% under-reported their intake, and 64% were other.
The investigators analyzed variables associated with over-reporting and found that age 12 years or older (P=0.02), being Hispanic (P=0.02), Asian (P=0.02), or African American (P<0.001), paternal education less than college (P=0.02), and being classified as 6MP non-adherent (P<0.001) were all significant.
“Over-reporting of 6MP ingestion is common,” Dr Landier said, with 88% of patients or parents over-reporting the number of days 6MP was taken.
“What we’ve learned from this study is that we cannot rely on patients’ self-report in the clinic,” she said. “What we found is that only 12% of our patients are perfect, so to speak, and that the others mainly over-estimate, and I don’t believe intentionally.”
“[W]e need to have a better way of identifying which patients are at risk for over-reporting their intake, whether they’re aware of it or not,” she added. ![]()

Photo courtesy of ASH
ORLANDO, FL—A study comparing subjective versus objective reporting of treatment compliance in patients with acute lymphoblastic leukemia (ALL) has shown that about a fourth of patients over-report how compliant they are with taking 6-mercaptopurine (6MP) as part of their maintenance therapy.
An earlier analysis of the Children’s Oncology Group (COG) AALL03N1 compliance study showed that adherence rates of less than 95% were associated with a 3.7-fold increased risk of relapse.
And about 40% of patients were non-adherent. Yet patients indicate they are taking their medication when questioned.
“We ask our patients if they are taking their meds,” said Wendy Landier, PhD, “and they tell us they are.”
“Even in this cohort who were being closely monitored and knew that they were being closely monitored electronically and were asked to self-report, we found over-reporting.”
Dr Landier, of the University of Alabama at Birmingham, reported these findings comparing self-reported adherence with electronic monitoring of 6MP intake at the 2015 ASH Annual Meeting (abstract 82).
The investigators collected data over 6 months from 416 ALL patients who were 21 years at diagnosis or younger and were receiving 6MP as part of their maintenance therapy.
Investigators measured subjective self-reporting by a patient questionnaire, which included patient demographic information in addition to the number of days the patient took 6MP over the past month.
For the objective medication event-monitoring system (MEMS), patients received a 6MP bottle that was fitted with a TrackCapTM. The cap had a microprocessor chip that recorded the date and time of each bottle opening.
Investigators downloaded the data at the end of the study. They then compared the MEMS with the self-reported data.
The investigators classified perfect reporters as those whose self-report corresponded to their MEMS.
They classified over-reporters as those whose self-report was greater than their MEMS data for 5 days or more and 50% of the months.
The rest they classified as others.
Patients were a median age of 6.0 years, and 277 (66.6%) were male. Parents completed the survey for patients younger than 12.
Two hundred forty-two patients (60.9%) had fathers whose education was less than some college, 159 (38.4%) had NCI high-risk disease, and 168 (40.4%) were non-adherent to 6MP as determined by earlier analysis of the COG AALL03N1 study.
Thirty-six percent were non-Hispanic white, 37% were Hispanic, 14% Asian, and 13% African American.
The investigators monitored the patients’ 6MP intake for a total of 1344 patient-months at 87 COG sites.
And the correlation between subjective and objective reporting was moderate, Dr Landier said, with the correlation ranging from 0.36 to 0.58.
Twelve percent of the patients were perfect reporters, with no difference between the reporting methods.
Twenty-four percent over-reported their intake, 1% under-reported their intake, and 64% were other.
The investigators analyzed variables associated with over-reporting and found that age 12 years or older (P=0.02), being Hispanic (P=0.02), Asian (P=0.02), or African American (P<0.001), paternal education less than college (P=0.02), and being classified as 6MP non-adherent (P<0.001) were all significant.
“Over-reporting of 6MP ingestion is common,” Dr Landier said, with 88% of patients or parents over-reporting the number of days 6MP was taken.
“What we’ve learned from this study is that we cannot rely on patients’ self-report in the clinic,” she said. “What we found is that only 12% of our patients are perfect, so to speak, and that the others mainly over-estimate, and I don’t believe intentionally.”
“[W]e need to have a better way of identifying which patients are at risk for over-reporting their intake, whether they’re aware of it or not,” she added. ![]()
VIDEO: Top-line results from Tourmaline in multiple myeloma, plus ongoing trials and treatment selection
ORLANDO – The combination of the oral proteasome inhibitor ixazomib (Ninlaro, recently approved by the Food and Drug Administration) with lenalidomide and dexamethasone was associated with a 35% improvement in progression free survival in the Tourmaline trial.
In a video interview, Tourmaline investigator Dr. Shaji Kumar, professor of medicine at the Mayo Clinic, Rochester, Minn., discussed the top-line study results, the status of ongoing trials with ixazomib in other combination regimens, and the decision rationales that will need to be considered in selecting one of the newly approved multiple myeloma therapies.
Dr. Kumar has received funding from Takeda, the makers of ixazomib; he has also received funding from Celgene, Onyx, Janssen, and Sanofi.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – The combination of the oral proteasome inhibitor ixazomib (Ninlaro, recently approved by the Food and Drug Administration) with lenalidomide and dexamethasone was associated with a 35% improvement in progression free survival in the Tourmaline trial.
In a video interview, Tourmaline investigator Dr. Shaji Kumar, professor of medicine at the Mayo Clinic, Rochester, Minn., discussed the top-line study results, the status of ongoing trials with ixazomib in other combination regimens, and the decision rationales that will need to be considered in selecting one of the newly approved multiple myeloma therapies.
Dr. Kumar has received funding from Takeda, the makers of ixazomib; he has also received funding from Celgene, Onyx, Janssen, and Sanofi.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – The combination of the oral proteasome inhibitor ixazomib (Ninlaro, recently approved by the Food and Drug Administration) with lenalidomide and dexamethasone was associated with a 35% improvement in progression free survival in the Tourmaline trial.
In a video interview, Tourmaline investigator Dr. Shaji Kumar, professor of medicine at the Mayo Clinic, Rochester, Minn., discussed the top-line study results, the status of ongoing trials with ixazomib in other combination regimens, and the decision rationales that will need to be considered in selecting one of the newly approved multiple myeloma therapies.
Dr. Kumar has received funding from Takeda, the makers of ixazomib; he has also received funding from Celgene, Onyx, Janssen, and Sanofi.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASH 2015
ASH: Rituximab add-on therapy ‘new standard’ in BCP-ALL
ORLANDO – Adding rituximab to standard intensive chemotherapy significantly improved event-free survival in adults with Philadelphia-negative, CD20-positive B-cell precursor acute lymphoblastic leukemia in the phase III GRAALL-R 2005 study.
Rituximab (Rituxan) is already being used to improve outcomes in patients with lymphoma, and non-randomized data support addition of the anti-CD20 monoclonal antibody to chemotherapy in B-cell precursor (BCP) ALL, where the CD20 antigen is expressed in 30% to 40% of patients at diagnosis.
In the randomized GRAALL-R 2005, 2-year event-free survival (EFS) was 65% in the rituximab arm vs. 52% in the control arm (hazard ratio, 0.66; P = .038).
This difference is not explained by the early response rates, which were very close in both arms after one or two induction courses (92% vs. 90%; P = .63), Dr. Sébastien Maury, Hôpital Henri Mondor in Créteil, France, said during the plenary session at the annual meeting of the American Society of Hematology (Ab. 1).
The beneficial effect of rituximab, however, was clearly related to the cumulative incidence of relapse at 18% with vs. 32% without rituximab (HR, 0.52; P = .017).
Despite this advantage, overall survival was similar between patients given chemotherapy with and without rituximab (71% vs. 64%; HR, 0.70; P = .095), he said.
After censoring for patients not receiving allogeneic stem cell transplant in first complete remission, however, rituximab significantly prolonged 2-year EFS (HR, 0.59; P = .021) as well as overall survival (HR, 0.55; P = .018), Dr. Maury said.
“We thus recommend that the addition of rituximab become a new standard of care for these patients, although some aspects including the definition of the optimal dose needs to be determined in further studies,” he concluded.
Dr. Adele Fielding of University College London, who introduced the study at the meeting, said, “For me, the prior knowledge that the drug can be safely already added to chemotherapy in other settings provides profound comfort in a disease in which so many people are already damaged by the current therapies we offer.”
Also, of importance is the potential relevance of rituximab in patients in whom CD20 is present on fewer than 20% of blasts at diagnosis.
Key questions that remain in rituximab therapy of ALL beyond overall benefit include early and late toxicities and how best to judge response and when, she said. Synergies with other agents and the mechanism of action will also require clarification, especially which effector cells are relevant to ensure that agents are not used with rituximab that destroy the optimal chance for response.
“Finally, the cost of introducing novel agents cannot be ignored, even in well-developed economies, and I am hopeful that the cost of this drug will be variable for many countries and many patients.” Dr. Fielding said.
Study details
A total of 220 patients, aged 18-59 years, with newly diagnosed CD20-positive Ph-negative BCP-ALL were randomized to the pediatric-inspired Group for Research on Adult Acute Lymphoblastic Leukemia (GRAALL) chemotherapy protocol with or without rituximab 375 mg/m2 given during induction (day 1 and 7), salvage reinduction when needed (day 1 and 7), consolidation blocks (6 infusions), late intensification (day 1 and 7, and the first year of maintenance [6 infusions], for a total of 16-18 infusions. Allogeneic stem cell transplant (SCT) was offered after consolidation blocks 1 or 2 to patients with one or more high-risk criteria and an available donor. CD20-positivity was defined as expression of CD20 in more than 20% of leukemia blasts.
Eleven patients were excluded from the analysis because of non–ineligibility criteria, leaving 209 patients in the modified intent-to-treat analysis. Their median age was 40.2 years and 67% had high-risk ALL.
Rates of postinduction minimal residual disease less than 10–4 were 65% and 61% in the rituximab and control arms among 85 evaluable patients(P = .82), and rates of postconsolidation minimal residual disease less than 10–4 were 91% and 82% among 80 evaluable patients (P = .31), Dr. Maury reported.
Notably, more patients in the rituximab arm received allogeneic SCT in their first complete remission (34% vs. 20%; P = .029).
The cumulative incidence of death in first complete remission was 12% in both arms.
In multivariate analysis, rituximab impacted EFS, together with age, central nervous system involvement, white blood cells, or CD20 expression at diagnosis. A preferential effect with rituximab was seen in patients with high CD20 levels that deserves further evaluation, he observed.
There was no difference in the incidence of adverse events between the rituximab and control arms, although there was a trend for more infectious events with rituximab (71 events vs. 55 events), Dr. Maury said.
Allergic events – all but one from aspergillosis – were significantly more common in the control arm (2 events vs. 14 events; P = .002).
The Group for Research in Adult Acute Lymphoblastic Leukemia sponsored the study. Dr. Maury reported having no disclosures.
ORLANDO – Adding rituximab to standard intensive chemotherapy significantly improved event-free survival in adults with Philadelphia-negative, CD20-positive B-cell precursor acute lymphoblastic leukemia in the phase III GRAALL-R 2005 study.
Rituximab (Rituxan) is already being used to improve outcomes in patients with lymphoma, and non-randomized data support addition of the anti-CD20 monoclonal antibody to chemotherapy in B-cell precursor (BCP) ALL, where the CD20 antigen is expressed in 30% to 40% of patients at diagnosis.
In the randomized GRAALL-R 2005, 2-year event-free survival (EFS) was 65% in the rituximab arm vs. 52% in the control arm (hazard ratio, 0.66; P = .038).
This difference is not explained by the early response rates, which were very close in both arms after one or two induction courses (92% vs. 90%; P = .63), Dr. Sébastien Maury, Hôpital Henri Mondor in Créteil, France, said during the plenary session at the annual meeting of the American Society of Hematology (Ab. 1).
The beneficial effect of rituximab, however, was clearly related to the cumulative incidence of relapse at 18% with vs. 32% without rituximab (HR, 0.52; P = .017).
Despite this advantage, overall survival was similar between patients given chemotherapy with and without rituximab (71% vs. 64%; HR, 0.70; P = .095), he said.
After censoring for patients not receiving allogeneic stem cell transplant in first complete remission, however, rituximab significantly prolonged 2-year EFS (HR, 0.59; P = .021) as well as overall survival (HR, 0.55; P = .018), Dr. Maury said.
“We thus recommend that the addition of rituximab become a new standard of care for these patients, although some aspects including the definition of the optimal dose needs to be determined in further studies,” he concluded.
Dr. Adele Fielding of University College London, who introduced the study at the meeting, said, “For me, the prior knowledge that the drug can be safely already added to chemotherapy in other settings provides profound comfort in a disease in which so many people are already damaged by the current therapies we offer.”
Also, of importance is the potential relevance of rituximab in patients in whom CD20 is present on fewer than 20% of blasts at diagnosis.
Key questions that remain in rituximab therapy of ALL beyond overall benefit include early and late toxicities and how best to judge response and when, she said. Synergies with other agents and the mechanism of action will also require clarification, especially which effector cells are relevant to ensure that agents are not used with rituximab that destroy the optimal chance for response.
“Finally, the cost of introducing novel agents cannot be ignored, even in well-developed economies, and I am hopeful that the cost of this drug will be variable for many countries and many patients.” Dr. Fielding said.
Study details
A total of 220 patients, aged 18-59 years, with newly diagnosed CD20-positive Ph-negative BCP-ALL were randomized to the pediatric-inspired Group for Research on Adult Acute Lymphoblastic Leukemia (GRAALL) chemotherapy protocol with or without rituximab 375 mg/m2 given during induction (day 1 and 7), salvage reinduction when needed (day 1 and 7), consolidation blocks (6 infusions), late intensification (day 1 and 7, and the first year of maintenance [6 infusions], for a total of 16-18 infusions. Allogeneic stem cell transplant (SCT) was offered after consolidation blocks 1 or 2 to patients with one or more high-risk criteria and an available donor. CD20-positivity was defined as expression of CD20 in more than 20% of leukemia blasts.
Eleven patients were excluded from the analysis because of non–ineligibility criteria, leaving 209 patients in the modified intent-to-treat analysis. Their median age was 40.2 years and 67% had high-risk ALL.
Rates of postinduction minimal residual disease less than 10–4 were 65% and 61% in the rituximab and control arms among 85 evaluable patients(P = .82), and rates of postconsolidation minimal residual disease less than 10–4 were 91% and 82% among 80 evaluable patients (P = .31), Dr. Maury reported.
Notably, more patients in the rituximab arm received allogeneic SCT in their first complete remission (34% vs. 20%; P = .029).
The cumulative incidence of death in first complete remission was 12% in both arms.
In multivariate analysis, rituximab impacted EFS, together with age, central nervous system involvement, white blood cells, or CD20 expression at diagnosis. A preferential effect with rituximab was seen in patients with high CD20 levels that deserves further evaluation, he observed.
There was no difference in the incidence of adverse events between the rituximab and control arms, although there was a trend for more infectious events with rituximab (71 events vs. 55 events), Dr. Maury said.
Allergic events – all but one from aspergillosis – were significantly more common in the control arm (2 events vs. 14 events; P = .002).
The Group for Research in Adult Acute Lymphoblastic Leukemia sponsored the study. Dr. Maury reported having no disclosures.
ORLANDO – Adding rituximab to standard intensive chemotherapy significantly improved event-free survival in adults with Philadelphia-negative, CD20-positive B-cell precursor acute lymphoblastic leukemia in the phase III GRAALL-R 2005 study.
Rituximab (Rituxan) is already being used to improve outcomes in patients with lymphoma, and non-randomized data support addition of the anti-CD20 monoclonal antibody to chemotherapy in B-cell precursor (BCP) ALL, where the CD20 antigen is expressed in 30% to 40% of patients at diagnosis.
In the randomized GRAALL-R 2005, 2-year event-free survival (EFS) was 65% in the rituximab arm vs. 52% in the control arm (hazard ratio, 0.66; P = .038).
This difference is not explained by the early response rates, which were very close in both arms after one or two induction courses (92% vs. 90%; P = .63), Dr. Sébastien Maury, Hôpital Henri Mondor in Créteil, France, said during the plenary session at the annual meeting of the American Society of Hematology (Ab. 1).
The beneficial effect of rituximab, however, was clearly related to the cumulative incidence of relapse at 18% with vs. 32% without rituximab (HR, 0.52; P = .017).
Despite this advantage, overall survival was similar between patients given chemotherapy with and without rituximab (71% vs. 64%; HR, 0.70; P = .095), he said.
After censoring for patients not receiving allogeneic stem cell transplant in first complete remission, however, rituximab significantly prolonged 2-year EFS (HR, 0.59; P = .021) as well as overall survival (HR, 0.55; P = .018), Dr. Maury said.
“We thus recommend that the addition of rituximab become a new standard of care for these patients, although some aspects including the definition of the optimal dose needs to be determined in further studies,” he concluded.
Dr. Adele Fielding of University College London, who introduced the study at the meeting, said, “For me, the prior knowledge that the drug can be safely already added to chemotherapy in other settings provides profound comfort in a disease in which so many people are already damaged by the current therapies we offer.”
Also, of importance is the potential relevance of rituximab in patients in whom CD20 is present on fewer than 20% of blasts at diagnosis.
Key questions that remain in rituximab therapy of ALL beyond overall benefit include early and late toxicities and how best to judge response and when, she said. Synergies with other agents and the mechanism of action will also require clarification, especially which effector cells are relevant to ensure that agents are not used with rituximab that destroy the optimal chance for response.
“Finally, the cost of introducing novel agents cannot be ignored, even in well-developed economies, and I am hopeful that the cost of this drug will be variable for many countries and many patients.” Dr. Fielding said.
Study details
A total of 220 patients, aged 18-59 years, with newly diagnosed CD20-positive Ph-negative BCP-ALL were randomized to the pediatric-inspired Group for Research on Adult Acute Lymphoblastic Leukemia (GRAALL) chemotherapy protocol with or without rituximab 375 mg/m2 given during induction (day 1 and 7), salvage reinduction when needed (day 1 and 7), consolidation blocks (6 infusions), late intensification (day 1 and 7, and the first year of maintenance [6 infusions], for a total of 16-18 infusions. Allogeneic stem cell transplant (SCT) was offered after consolidation blocks 1 or 2 to patients with one or more high-risk criteria and an available donor. CD20-positivity was defined as expression of CD20 in more than 20% of leukemia blasts.
Eleven patients were excluded from the analysis because of non–ineligibility criteria, leaving 209 patients in the modified intent-to-treat analysis. Their median age was 40.2 years and 67% had high-risk ALL.
Rates of postinduction minimal residual disease less than 10–4 were 65% and 61% in the rituximab and control arms among 85 evaluable patients(P = .82), and rates of postconsolidation minimal residual disease less than 10–4 were 91% and 82% among 80 evaluable patients (P = .31), Dr. Maury reported.
Notably, more patients in the rituximab arm received allogeneic SCT in their first complete remission (34% vs. 20%; P = .029).
The cumulative incidence of death in first complete remission was 12% in both arms.
In multivariate analysis, rituximab impacted EFS, together with age, central nervous system involvement, white blood cells, or CD20 expression at diagnosis. A preferential effect with rituximab was seen in patients with high CD20 levels that deserves further evaluation, he observed.
There was no difference in the incidence of adverse events between the rituximab and control arms, although there was a trend for more infectious events with rituximab (71 events vs. 55 events), Dr. Maury said.
Allergic events – all but one from aspergillosis – were significantly more common in the control arm (2 events vs. 14 events; P = .002).
The Group for Research in Adult Acute Lymphoblastic Leukemia sponsored the study. Dr. Maury reported having no disclosures.
AT ASH 2015
Key clinical point: Adding rituximab to standard intensive chemotherapy is a new standard for CD20-positive, Philadelphia-negative, B-cell precursor acute lymphoblastic leukemia.
Major finding: Event-free survival was 65% in the rituximab arm vs. 52% in the control arm (HR, 0.66; P = .038).
Data source: Phase III study in 220 adults with CD20-positive, Ph-negative, BCP-ALL.
Disclosures: Group for Research in Adult Acute Lymphoblastic Leukemia sponsored the study. Dr. Maury reported having no disclosures.
VIDEO: Novel GBT440 improves blood parameters in sickle cell disease
ORLANDO – A novel small molecule agent improved hematologic parameters and was associated with significant reduction in sickling of red blood cells in patients with sickle cell disease.
The drug was shown to increase hemoglobin in both healthy volunteers and patients, reduce reticulocytosis, and improve biomarkers of hemolysis and inflammation.
In an interview, Dr. Claire Hemmaway of Queens Hospital in Romford, England, discusses early results from a phase I/II randomized, double-blind, placebo-controlled, parallel-group trial.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – A novel small molecule agent improved hematologic parameters and was associated with significant reduction in sickling of red blood cells in patients with sickle cell disease.
The drug was shown to increase hemoglobin in both healthy volunteers and patients, reduce reticulocytosis, and improve biomarkers of hemolysis and inflammation.
In an interview, Dr. Claire Hemmaway of Queens Hospital in Romford, England, discusses early results from a phase I/II randomized, double-blind, placebo-controlled, parallel-group trial.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – A novel small molecule agent improved hematologic parameters and was associated with significant reduction in sickling of red blood cells in patients with sickle cell disease.
The drug was shown to increase hemoglobin in both healthy volunteers and patients, reduce reticulocytosis, and improve biomarkers of hemolysis and inflammation.
In an interview, Dr. Claire Hemmaway of Queens Hospital in Romford, England, discusses early results from a phase I/II randomized, double-blind, placebo-controlled, parallel-group trial.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASH 2015