User login
EVIDENCE-BASED ANSWER:
Hydroxychloroquine and chloroquine improve the arthritis associated with mild systemic lupus erythematosus (SLE)—producing a 50% reduction in arthritis flares and articular involvement—and have few adverse effects (strength of recommendation [SOR]: A, systematic review of randomized controlled trials [RCTs]).
Methotrexate reduces arthralgias by as much as 79%, but produces adverse effects in up to 70% of patients (SOR: B, systematic review of RCTs with limited patient-oriented evidence).
Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids are often used for SLE joint pain (SOR: C, expert opinion).
Omega-3 fatty acids may reduce arthritis symptoms by about 35% (SOR: B, RCTs with inconsistent evidence).
Abatacept and dehydroepiandrosterone don’t produce clinically meaningful improvements in fatigue associated with SLE, and abatacept causes significant adverse effects (SOR: B, posthoc analysis of a single RCT).
Aerobic exercise may help fatigue (SOR: B, systematic review with inconsistent evidence).
EVIDENCE SUMMARY
A systematic review of pharmacotherapy for joint pain in patients with SLE found 4 poor-quality RCTs that evaluated hydroxychloroquine, chloroquine, and methotrexate.1 Of the 2 studies that examined the effect of hydroxychloroquine, one (47 patients) showed a statistically significant 50% reduction in SLE flares (including arthritis, pleuritis, and cutaneous symptoms) over 24 weeks in patients treated with hydroxychloroquine compared with placebo (TABLE1-8). The second study (71 subjects) found a nonquantified decrease in self-reported pain when hydroxychloroquine was compared with placebo, although some of the patients were also taking prednisone (10 mg/d).
An RCT that evaluated the effect of chloroquine showed a statistically significant reduction in unspecified “articular involvement” compared with placebo.
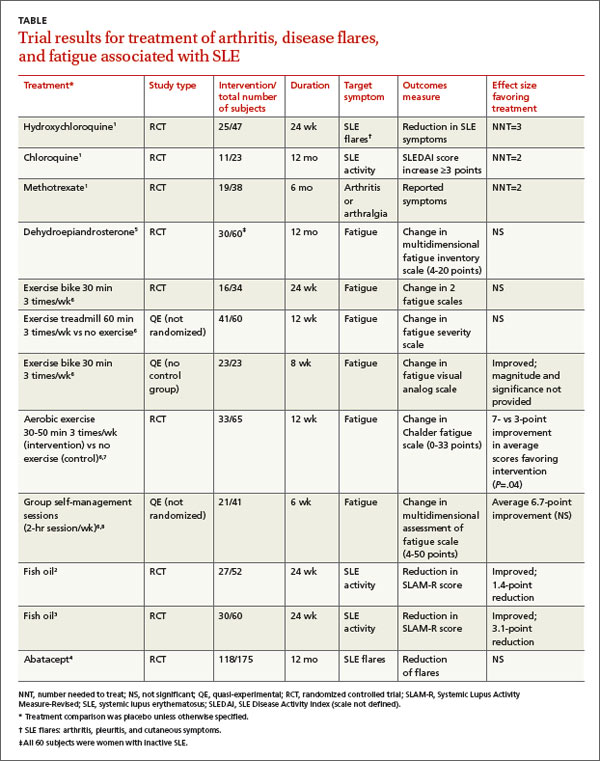
The fourth RCT, assessing methotrexate, found a statistically significant reduction by as much as 79% in patients with residual arthritis or arthralgia at 6 months compared with placebo, although 70% of patients taking methotrexate developed significant adverse effects, including infections, gastrointestinal symptoms, and elevated transaminases compared with 14% on placebo (number needed to harm [NNH]=2).
The authors of the review noted that consensus opinion holds that oral corticosteroids and NSAIDs reduce SLE-associated joint pain, but they found no studies that objectively evaluated either of these interventions.1
Fish oil also helps arthritis
Two RCTs on the effects of 3 g/d of omega-3 polyunsaturated fatty acids (fish oil) for 24 weeks in SLE patients with mild disease found a reduction in Systemic Lupus Activity Measure-Revised (SLAM-R) scores.2,3 SLAM-R is a validated measure of SLE disease activity, rated on a scale from 0 to 81, including 23 clinical and 7 laboratory manifestations of disease.
In the first study (52 subjects), disease activity decreased from an average SLAM-R score of 6.1 at baseline to 4.7 (P<.05). The second study (60 subjects) found a similar reduction in mean SLAM-R scores from 9.4 to 6.3 (P<.001) and joint pain scores from 1.27 to 0.83 (P=.047).
Drug treatments don’t significantly relieve fatigue
An industry-sponsored RCT that compared abatacept with placebo found improvements in fatigue that weren’t clinically meaningful in posthoc analysis (-9.45 points difference on a self-reported 0-to-100 visual analog scale; 95% confidence interval, -17.65 to -1.25, with a 10-point reduction considered to be clinically meaningful). Abatacept also had a high rate of serious adverse events, including facial edema, polyneuropathy, and serious infections (24/121 with abatacept vs 4/59 placebo; NNH=8).4
Another RCT found no effect of dehydroepiandrosterone on fatigue in women with inactive SLE.5
Nondrug treatments for fatigue produce mixed results
Studies of nondrug treatment of SLE-associated fatigue show inconsistent results. A systematic review of nonpharmacologic interventions for fatigue in several chronic diseases found 2 RCTs and 4 quasi-experimental studies that included 324 patients with SLE.6 Of 4 studies that evaluated the effect of exercise, 2 showed improvement and 2 didn’t. Neither group self-management nor relaxation therapy and telephone counseling significantly relieved fatigue.6-8 A small RCT (24 patients) found no benefit for acupuncture over sham needling in treating pain and fatigue in SLE.9
RECOMMENDATIONS
The American College of Rheumatology guideline for referral and management of SLE states that “NSAIDs are sometimes helpful for control of fever, arthritis, and mild serositis. Antimalarial agents (eg, hydroxychloroquine) are useful for skin and joint manifestations of SLE, for preventing flares, and for other constitutional symptoms of the disease. They may also reduce fatigue.”10
The European League Against Rheumatism recommends antimalarials or glucocorticoids to treat patients with SLE without major organ manifestations. They also say clinicians may try NSAIDs for limited periods of time in patients at low risk for the drugs’ complications.11
1. Madhok R, Wu O. Systemic lupus erythematosus. Clin Evid. 2009;7:1123.
2. Duffy EM, Meenagh GK, McMillan SA, et al. The clinical effect of dietary supplementation with omega-3 fish oils and/ or copper in systemic lupus erythematosus. J Rheumatol. 2004;31:1551-1556.
3. Wright SA, O’Prey FM, McHenry MT, et al. A randomised interventional trial of omega-3-polyunsaturated fatty acids on endothelial function and disease activity in systemic lupus erythematosus. Ann Rheum Dis. 2008;67:841-848.
4. Merrill JT, Burgos-Vargas R, Westhovens R, et al. The efficacy and safety of abatacept in patients with non-life-threatening manifestations of systemic lupus erythematosus: results of a twelve-month, multicenter, exploratory, phase IIb, randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2010;62:3077-3087.
5. Hartkamp A, Geenen R, Godaert GL, et al. Effects of dehydroepiandrosterone on fatigue and well-being in women with quiescent systemic lupus erythematosus: a randomized controlled trial. Ann Rheum Dis. 2010;69:1144-1147.
6. Neill J, Belan I, Reid K. Effectiveness of non-pharmacological interventions for fatigue in adults with multiple sclerosis, rheumatoid arthritis, or systemic lupus erythematosis: a systematic review. J Adv Nurs. 2006;56:617-635.
7. Tench CM, McCarthy J, McCurdie I, et al. Fatigue in systemic lupus erythematosus: a randomized controlled trial of exercise. Rheumatology (Oxford). 2003;42:1050-1054.
8. Sohng KY. Effects of a self-management course for patients with systemic lupus erythematosus. J Adv Nurs. 2003;42:479-486.
9. Greco CM, Kao AH, Maksimowicz-McKinnon K, et al. Acupuncture for systemic lupus erythematosus: a pilot RCT feasibility and safety study. Lupus. 2008;17:1108-1116.
10. American College of Rheumatology Ad Hoc Committee on Systemic Lupus Erythematosus Guidelines. Guidelines for referral and management of systemic lupus erythematosus in adults. Arthritis Rheum. 1999;42:1785-1796.
11. Bertsias G, Ioannidis JP, Boletis J, et al; Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics. EULAR recommendations for the management of systemic lupus erythematosus. Report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics. Ann Rheum Dis. 2008;67:195-205.
EVIDENCE-BASED ANSWER:
Hydroxychloroquine and chloroquine improve the arthritis associated with mild systemic lupus erythematosus (SLE)—producing a 50% reduction in arthritis flares and articular involvement—and have few adverse effects (strength of recommendation [SOR]: A, systematic review of randomized controlled trials [RCTs]).
Methotrexate reduces arthralgias by as much as 79%, but produces adverse effects in up to 70% of patients (SOR: B, systematic review of RCTs with limited patient-oriented evidence).
Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids are often used for SLE joint pain (SOR: C, expert opinion).
Omega-3 fatty acids may reduce arthritis symptoms by about 35% (SOR: B, RCTs with inconsistent evidence).
Abatacept and dehydroepiandrosterone don’t produce clinically meaningful improvements in fatigue associated with SLE, and abatacept causes significant adverse effects (SOR: B, posthoc analysis of a single RCT).
Aerobic exercise may help fatigue (SOR: B, systematic review with inconsistent evidence).
EVIDENCE SUMMARY
A systematic review of pharmacotherapy for joint pain in patients with SLE found 4 poor-quality RCTs that evaluated hydroxychloroquine, chloroquine, and methotrexate.1 Of the 2 studies that examined the effect of hydroxychloroquine, one (47 patients) showed a statistically significant 50% reduction in SLE flares (including arthritis, pleuritis, and cutaneous symptoms) over 24 weeks in patients treated with hydroxychloroquine compared with placebo (TABLE1-8). The second study (71 subjects) found a nonquantified decrease in self-reported pain when hydroxychloroquine was compared with placebo, although some of the patients were also taking prednisone (10 mg/d).
An RCT that evaluated the effect of chloroquine showed a statistically significant reduction in unspecified “articular involvement” compared with placebo.
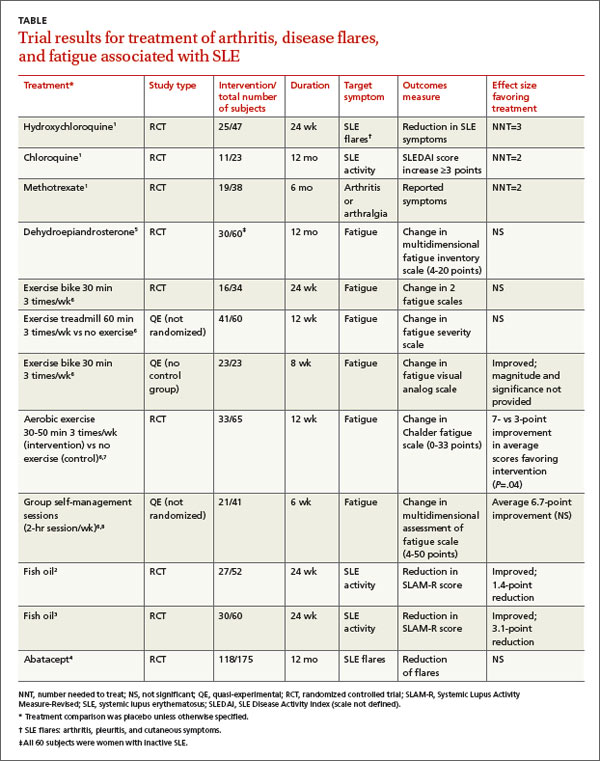
The fourth RCT, assessing methotrexate, found a statistically significant reduction by as much as 79% in patients with residual arthritis or arthralgia at 6 months compared with placebo, although 70% of patients taking methotrexate developed significant adverse effects, including infections, gastrointestinal symptoms, and elevated transaminases compared with 14% on placebo (number needed to harm [NNH]=2).
The authors of the review noted that consensus opinion holds that oral corticosteroids and NSAIDs reduce SLE-associated joint pain, but they found no studies that objectively evaluated either of these interventions.1
Fish oil also helps arthritis
Two RCTs on the effects of 3 g/d of omega-3 polyunsaturated fatty acids (fish oil) for 24 weeks in SLE patients with mild disease found a reduction in Systemic Lupus Activity Measure-Revised (SLAM-R) scores.2,3 SLAM-R is a validated measure of SLE disease activity, rated on a scale from 0 to 81, including 23 clinical and 7 laboratory manifestations of disease.
In the first study (52 subjects), disease activity decreased from an average SLAM-R score of 6.1 at baseline to 4.7 (P<.05). The second study (60 subjects) found a similar reduction in mean SLAM-R scores from 9.4 to 6.3 (P<.001) and joint pain scores from 1.27 to 0.83 (P=.047).
Drug treatments don’t significantly relieve fatigue
An industry-sponsored RCT that compared abatacept with placebo found improvements in fatigue that weren’t clinically meaningful in posthoc analysis (-9.45 points difference on a self-reported 0-to-100 visual analog scale; 95% confidence interval, -17.65 to -1.25, with a 10-point reduction considered to be clinically meaningful). Abatacept also had a high rate of serious adverse events, including facial edema, polyneuropathy, and serious infections (24/121 with abatacept vs 4/59 placebo; NNH=8).4
Another RCT found no effect of dehydroepiandrosterone on fatigue in women with inactive SLE.5
Nondrug treatments for fatigue produce mixed results
Studies of nondrug treatment of SLE-associated fatigue show inconsistent results. A systematic review of nonpharmacologic interventions for fatigue in several chronic diseases found 2 RCTs and 4 quasi-experimental studies that included 324 patients with SLE.6 Of 4 studies that evaluated the effect of exercise, 2 showed improvement and 2 didn’t. Neither group self-management nor relaxation therapy and telephone counseling significantly relieved fatigue.6-8 A small RCT (24 patients) found no benefit for acupuncture over sham needling in treating pain and fatigue in SLE.9
RECOMMENDATIONS
The American College of Rheumatology guideline for referral and management of SLE states that “NSAIDs are sometimes helpful for control of fever, arthritis, and mild serositis. Antimalarial agents (eg, hydroxychloroquine) are useful for skin and joint manifestations of SLE, for preventing flares, and for other constitutional symptoms of the disease. They may also reduce fatigue.”10
The European League Against Rheumatism recommends antimalarials or glucocorticoids to treat patients with SLE without major organ manifestations. They also say clinicians may try NSAIDs for limited periods of time in patients at low risk for the drugs’ complications.11
EVIDENCE-BASED ANSWER:
Hydroxychloroquine and chloroquine improve the arthritis associated with mild systemic lupus erythematosus (SLE)—producing a 50% reduction in arthritis flares and articular involvement—and have few adverse effects (strength of recommendation [SOR]: A, systematic review of randomized controlled trials [RCTs]).
Methotrexate reduces arthralgias by as much as 79%, but produces adverse effects in up to 70% of patients (SOR: B, systematic review of RCTs with limited patient-oriented evidence).
Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids are often used for SLE joint pain (SOR: C, expert opinion).
Omega-3 fatty acids may reduce arthritis symptoms by about 35% (SOR: B, RCTs with inconsistent evidence).
Abatacept and dehydroepiandrosterone don’t produce clinically meaningful improvements in fatigue associated with SLE, and abatacept causes significant adverse effects (SOR: B, posthoc analysis of a single RCT).
Aerobic exercise may help fatigue (SOR: B, systematic review with inconsistent evidence).
EVIDENCE SUMMARY
A systematic review of pharmacotherapy for joint pain in patients with SLE found 4 poor-quality RCTs that evaluated hydroxychloroquine, chloroquine, and methotrexate.1 Of the 2 studies that examined the effect of hydroxychloroquine, one (47 patients) showed a statistically significant 50% reduction in SLE flares (including arthritis, pleuritis, and cutaneous symptoms) over 24 weeks in patients treated with hydroxychloroquine compared with placebo (TABLE1-8). The second study (71 subjects) found a nonquantified decrease in self-reported pain when hydroxychloroquine was compared with placebo, although some of the patients were also taking prednisone (10 mg/d).
An RCT that evaluated the effect of chloroquine showed a statistically significant reduction in unspecified “articular involvement” compared with placebo.
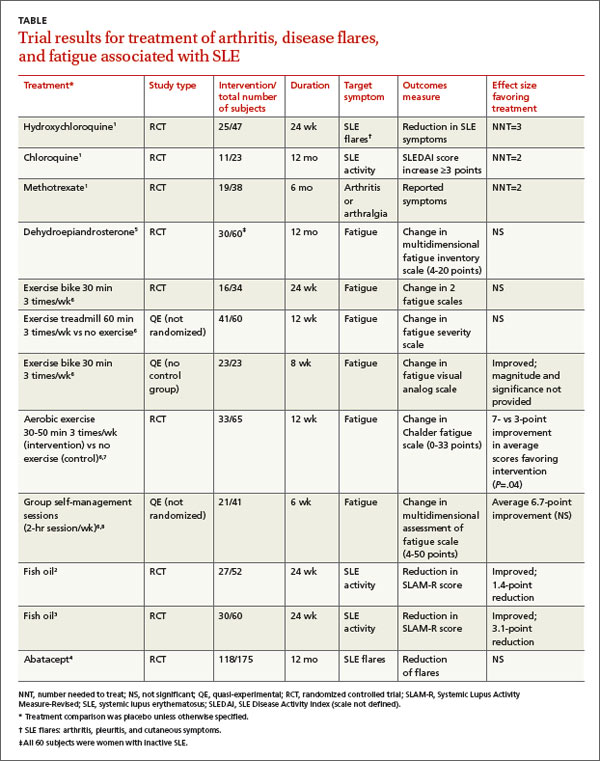
The fourth RCT, assessing methotrexate, found a statistically significant reduction by as much as 79% in patients with residual arthritis or arthralgia at 6 months compared with placebo, although 70% of patients taking methotrexate developed significant adverse effects, including infections, gastrointestinal symptoms, and elevated transaminases compared with 14% on placebo (number needed to harm [NNH]=2).
The authors of the review noted that consensus opinion holds that oral corticosteroids and NSAIDs reduce SLE-associated joint pain, but they found no studies that objectively evaluated either of these interventions.1
Fish oil also helps arthritis
Two RCTs on the effects of 3 g/d of omega-3 polyunsaturated fatty acids (fish oil) for 24 weeks in SLE patients with mild disease found a reduction in Systemic Lupus Activity Measure-Revised (SLAM-R) scores.2,3 SLAM-R is a validated measure of SLE disease activity, rated on a scale from 0 to 81, including 23 clinical and 7 laboratory manifestations of disease.
In the first study (52 subjects), disease activity decreased from an average SLAM-R score of 6.1 at baseline to 4.7 (P<.05). The second study (60 subjects) found a similar reduction in mean SLAM-R scores from 9.4 to 6.3 (P<.001) and joint pain scores from 1.27 to 0.83 (P=.047).
Drug treatments don’t significantly relieve fatigue
An industry-sponsored RCT that compared abatacept with placebo found improvements in fatigue that weren’t clinically meaningful in posthoc analysis (-9.45 points difference on a self-reported 0-to-100 visual analog scale; 95% confidence interval, -17.65 to -1.25, with a 10-point reduction considered to be clinically meaningful). Abatacept also had a high rate of serious adverse events, including facial edema, polyneuropathy, and serious infections (24/121 with abatacept vs 4/59 placebo; NNH=8).4
Another RCT found no effect of dehydroepiandrosterone on fatigue in women with inactive SLE.5
Nondrug treatments for fatigue produce mixed results
Studies of nondrug treatment of SLE-associated fatigue show inconsistent results. A systematic review of nonpharmacologic interventions for fatigue in several chronic diseases found 2 RCTs and 4 quasi-experimental studies that included 324 patients with SLE.6 Of 4 studies that evaluated the effect of exercise, 2 showed improvement and 2 didn’t. Neither group self-management nor relaxation therapy and telephone counseling significantly relieved fatigue.6-8 A small RCT (24 patients) found no benefit for acupuncture over sham needling in treating pain and fatigue in SLE.9
RECOMMENDATIONS
The American College of Rheumatology guideline for referral and management of SLE states that “NSAIDs are sometimes helpful for control of fever, arthritis, and mild serositis. Antimalarial agents (eg, hydroxychloroquine) are useful for skin and joint manifestations of SLE, for preventing flares, and for other constitutional symptoms of the disease. They may also reduce fatigue.”10
The European League Against Rheumatism recommends antimalarials or glucocorticoids to treat patients with SLE without major organ manifestations. They also say clinicians may try NSAIDs for limited periods of time in patients at low risk for the drugs’ complications.11
1. Madhok R, Wu O. Systemic lupus erythematosus. Clin Evid. 2009;7:1123.
2. Duffy EM, Meenagh GK, McMillan SA, et al. The clinical effect of dietary supplementation with omega-3 fish oils and/ or copper in systemic lupus erythematosus. J Rheumatol. 2004;31:1551-1556.
3. Wright SA, O’Prey FM, McHenry MT, et al. A randomised interventional trial of omega-3-polyunsaturated fatty acids on endothelial function and disease activity in systemic lupus erythematosus. Ann Rheum Dis. 2008;67:841-848.
4. Merrill JT, Burgos-Vargas R, Westhovens R, et al. The efficacy and safety of abatacept in patients with non-life-threatening manifestations of systemic lupus erythematosus: results of a twelve-month, multicenter, exploratory, phase IIb, randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2010;62:3077-3087.
5. Hartkamp A, Geenen R, Godaert GL, et al. Effects of dehydroepiandrosterone on fatigue and well-being in women with quiescent systemic lupus erythematosus: a randomized controlled trial. Ann Rheum Dis. 2010;69:1144-1147.
6. Neill J, Belan I, Reid K. Effectiveness of non-pharmacological interventions for fatigue in adults with multiple sclerosis, rheumatoid arthritis, or systemic lupus erythematosis: a systematic review. J Adv Nurs. 2006;56:617-635.
7. Tench CM, McCarthy J, McCurdie I, et al. Fatigue in systemic lupus erythematosus: a randomized controlled trial of exercise. Rheumatology (Oxford). 2003;42:1050-1054.
8. Sohng KY. Effects of a self-management course for patients with systemic lupus erythematosus. J Adv Nurs. 2003;42:479-486.
9. Greco CM, Kao AH, Maksimowicz-McKinnon K, et al. Acupuncture for systemic lupus erythematosus: a pilot RCT feasibility and safety study. Lupus. 2008;17:1108-1116.
10. American College of Rheumatology Ad Hoc Committee on Systemic Lupus Erythematosus Guidelines. Guidelines for referral and management of systemic lupus erythematosus in adults. Arthritis Rheum. 1999;42:1785-1796.
11. Bertsias G, Ioannidis JP, Boletis J, et al; Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics. EULAR recommendations for the management of systemic lupus erythematosus. Report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics. Ann Rheum Dis. 2008;67:195-205.
1. Madhok R, Wu O. Systemic lupus erythematosus. Clin Evid. 2009;7:1123.
2. Duffy EM, Meenagh GK, McMillan SA, et al. The clinical effect of dietary supplementation with omega-3 fish oils and/ or copper in systemic lupus erythematosus. J Rheumatol. 2004;31:1551-1556.
3. Wright SA, O’Prey FM, McHenry MT, et al. A randomised interventional trial of omega-3-polyunsaturated fatty acids on endothelial function and disease activity in systemic lupus erythematosus. Ann Rheum Dis. 2008;67:841-848.
4. Merrill JT, Burgos-Vargas R, Westhovens R, et al. The efficacy and safety of abatacept in patients with non-life-threatening manifestations of systemic lupus erythematosus: results of a twelve-month, multicenter, exploratory, phase IIb, randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2010;62:3077-3087.
5. Hartkamp A, Geenen R, Godaert GL, et al. Effects of dehydroepiandrosterone on fatigue and well-being in women with quiescent systemic lupus erythematosus: a randomized controlled trial. Ann Rheum Dis. 2010;69:1144-1147.
6. Neill J, Belan I, Reid K. Effectiveness of non-pharmacological interventions for fatigue in adults with multiple sclerosis, rheumatoid arthritis, or systemic lupus erythematosis: a systematic review. J Adv Nurs. 2006;56:617-635.
7. Tench CM, McCarthy J, McCurdie I, et al. Fatigue in systemic lupus erythematosus: a randomized controlled trial of exercise. Rheumatology (Oxford). 2003;42:1050-1054.
8. Sohng KY. Effects of a self-management course for patients with systemic lupus erythematosus. J Adv Nurs. 2003;42:479-486.
9. Greco CM, Kao AH, Maksimowicz-McKinnon K, et al. Acupuncture for systemic lupus erythematosus: a pilot RCT feasibility and safety study. Lupus. 2008;17:1108-1116.
10. American College of Rheumatology Ad Hoc Committee on Systemic Lupus Erythematosus Guidelines. Guidelines for referral and management of systemic lupus erythematosus in adults. Arthritis Rheum. 1999;42:1785-1796.
11. Bertsias G, Ioannidis JP, Boletis J, et al; Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics. EULAR recommendations for the management of systemic lupus erythematosus. Report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics. Ann Rheum Dis. 2008;67:195-205.
Evidence-based answers from the Family Physicians Inquiries Network