User login
Despite the availability of evidence‐based guidelines for the prevention of thromboembolic morbidity and mortality, venous thromboembolism (VTE) remains a pervasive threat to public health. Prophylaxis is underused for a variety of reasons, which were summarized in the first article of this Supplement. Overcoming these barriers and reducing the incidence of VTE has become a major priority for public health policy.
The Office of the Surgeon General released a report in September 2008 that reflects this sense of urgency and national focus by calling for a coordinated, multifaceted plan to reduce the incidence of VTE in the United States.1 The Surgeon General report is one of the latest in a string of national initiatives designed to improve outcomes in patients at risk of VTE. In the past several years, public and private agencies have launched a range of programs aimed at improving deficiencies in the awareness, prevention, and treatment of VTE in hospitalized patients (these are summarized in Table 1). New performance measures and improvement initiatives may reduce the discrepancies between recommendations and practice, ultimately improving patient outcomes. These measures may possibly become benchmarks for pay‐for‐performance initiatives or future hospital accreditation.
| Measure/Initiative | Description |
|---|---|
| |
| National Quality Forum/The Joint Commission (NQF/TJC) | Public reporting of hospital performance in 6 performance measures; will apply to all medical and surgical patients |
| Surgical Care Improvement Project (SCIP) | Two performance measures enacted with reimbursement implications; 2 outcomes measures |
| American Medical Association Physician Consortium for Performance Improvement (PCPI) | Medical societies collaborating to identify gaps in care and develop performance measures; 1 measure has been endorsed |
| Leapfrog Hospital Quality and Safety Survey | Web database allowing consumers to compare performance among participating hospitals; includes 2 NQF safe practices |
| TJC National Patient Safety Goals (NPSG) | Goals for solving patient safety problems; compliance required for Joint Commission accreditation, with online reporting of results (Quality Check website) |
| North American Thrombosis Forum (NATF) | Nonprofit organization addressing unmet needs related to VTE and other thrombotic disorders |
| American Venous Forum National Venous Screening Program | National VTE awareness campaign; promotes compliance with protocols |
Herein, we review a variety of VTE performance measures, including those from the National Quality Forum (NQF), The Joint Commission (TJC), and the Surgical Care Improvement Project (SCIP). To illustrate how performance measures may be applied in the hospital setting to improve patient care, performance improvement programs that have proven effective in select hospitals across the United States are described.
Performance Measures and Initiatives
National Quality Forum Performance Measures
The NQF and TJC (formerly known as the Joint Commission on Accreditation of Healthcare Organizations) have already enacted performance measures for pneumonia, heart failure, acute myocardial infarction (MI), and other conditions. Since 2005, the NQF and TJC have been collaborating to develop national consensus performance measures for the prevention and care of VTE. The VTE performance measures will apply to all medical and surgical patients and include process measures in the areas of prevention and treatment, as well as outcome measures. After pilot‐testing a range of measures for 3 years, TJC recommended 7 candidate measures in November 2007. In May 2008, the NQF endorsed 6 of these, embracing all TJC recommendations except one relating to the use and documentation of vena cava filter quality improvement (Table 2).2
|
| Risk assessment and prophylaxis |
| 1. Documentation of VTE risk/prophylaxis within 24 hours of hospital admission or surgery end‐time |
| 2. Documentation of VTE risk/prophylaxis within 24 hours after ICU admission, transfer to ICU, or surgery end‐time |
| Treatment |
| 3. Patients with VTE with overlap of parenteral and warfarin anticoagulation therapy for at least 5 days with an INR 2 before discontinuation of parenteral therapy; for > 5 days with an INR < 2 and discharged on overlap therapy; or discharged in < 5 days on overlap therapy |
| 4. Patients with VTE receiving UFH with dosages/platelet count monitoring by protocol or nomogram |
| 5. Patients with VTE or their caregivers are given written discharge instructions or other educational material addressing all of the following: follow‐up monitoring, compliance issues, dietary restrictions, and potential for adverse drug reactions and interactions |
| Outcomes |
| 6. Incidence of potentially preventable hospital‐acquired VTE measured by patients who received no VTE prophylaxis before VTE diagnosis |
The next step is for the NQF to develop a specification manual that defines which patients should be given prophylaxis using International Classification of Diseases, 9th edition (ICD‐9) codes and identifies which interventions are appropriate for each patient population. Current clinical guidelines provide important guidance for appropriate inclusion and exclusion criteria for medical and surgical prophylaxis, as well as evidence‐based recommendations for the treatment of VTE.3, 4
SCIP
The SCIP has a stated goal of reducing surgical complications by 25% by 2010.5 To accomplish this, the SCIP is targeting improvement in 4 areas: surgical‐site infection, cardiac events, postoperative pneumonia, and VTE prophylaxis. The SCIP performance measures for VTE prophylaxis in surgical patients are as follows:
-
Recommended VTE prophylaxis ordered during admission; and
-
Appropriate VTE prophylaxis received within 24 hours prior to surgical incision time to 24 hours after surgery end time.
After the success seen by a core group of hospitals who volunteered to participate, all Medicare‐accredited hospitals were required to submit SCIP data beginning with discharges in the first quarter of 2007 to obtain full reimbursement from the Centers for Medicare and Medicaid Services (CMS). Institutions can gauge whether they are in compliance with the SCIP VTE measures by answering a series of yes or no questions about whether prophylaxis has been ordered and received for specific patient groups and procedures. In a recent study, almost one‐half of all surgical patients at risk of VTE did not receive recommended and timely prophylaxis as specified by the SCIP performance measures.6
In addition to the 2 enacted SCIP performance measures for VTE prophylaxis, 2 outcome measures are under development. These measures address the rate at which intraoperative or postoperative pulmonary embolism (PE; SCIP VTE‐3) and deep vein thrombosis (DVT; SCIP VTE‐4) are diagnosed during the index hospitalization and within 30 days after surgery. If implemented, these measures will capture the efficacy of thromboprophylaxis.5
Other VTE Performance Initiatives
Several professional and consumer organizations are developing standards and compiling performance data for public reporting and other purposes:
-
The American Medical Association Physician Consortium for Performance Improvement (PCPI) comprises more than 100 national medical specialty and state medical societies working to identify gaps in care that can be addressed with evidence‐based medicine and formal performance measures. The PCPI has endorsed a measure requiring low‐molecular‐weight heparin (LMWH), low‐dose unfractionated heparin (UFH), adjusted‐dose warfarin, fondaparinux, or mechanical prophylaxis to be given within 24 hours prior to incision time or within 24 hours after surgery end‐time for adults undergoing a procedure for which prophylaxis is indicated.7
-
The Leapfrog Hospital Quality and Safety Survey hosts a searchable web‐based database that consumers can use to compare performance among participating hospitals in specific geographic regions. The Leapfrog survey includes NQF safe practices #28 (reduce occurrence of VTE) and #29 (ensure long‐term anticoagulation is effective and safe).8
-
TJC National Patient Safety Goals (NPSG) target specific improvements in patient safety by providing healthcare organizations with solutions to prevalent patient safety problems. Compliance is necessary for Joint Commission accreditation, and results are reported on the Quality Check website. NPSG Goal 3 is focused on improving the safety of medications, and Goal 3E specifically addresses patient harm associated with the use of anticoagulation therapy. The 2008 NPSG goals must be implemented by January 2009.2
-
The North American Thrombosis Forum (NATF), a nonprofit organization, was recently organized to address unmet needs in North America related to VTE and other thrombotic disorders. It is designed to complement existing organizations dealing with thrombosis‐related issues, with 5 major focus areas: basic translational research; clinical research; prevention and education; public policy; and advocacy. Each month, its website (
http://www.natfonline.org ) features several scientific papers dealing with venous and arterial thrombosis‐related issues. -
The American Venous Forum National Venous Screening Program is a national campaign designed to increase VTE awareness and promote the importance of compliance with prophylaxis protocols.9
As different organizations work to develop performance measures for VTE, conflicting standards have emerged. Although this remains a major challenge, the NQF is attempting to develop voluntary consensus standards that will harmonize VTE performance measures across all sites of care, including the acute medical, surgical, and oncology settings. Major clinical guidelines from the American College of Physicians (ACP), American College of Chest Physicians (ACCP), the American Society of Clinical Oncology (ASCO), the National Comprehensive Cancer Network (NCCN), the European Society of Cardiology (ESC), and other organizations provide data to support standardized, evidence‐based measures for VTE.
Implications of Performance Data
Hospital‐Level Performance Reporting
Performance results may affect an institution's ability to contract best rates with payors, obtain full reimbursement for services, and be eligible for bonus payments. For example, pay‐for‐reporting legislation from CMS provides targeted financial incentives to improve the rates at which hospitals report data on quality measures. The current legislation stipulates that hospitals must submit performance data, including data on compliance with the 2 SCIP‐VTE measures, or lose 2% of their annual CMS payment update. For a 500‐bed hospital with 80% occupancy and 50% CMS patients, failure to report data on SCIP‐VTE measures would result in an estimated annual loss of $2.6 million.10
In 2007, the first year of the CMS pay‐for‐reporting program, 93% of hospitals met the reporting goals. As penalties for nonreporting increase, an even higher compliance rate may be expected. CMS is proposing a new system that would withhold 5% of the base operating diagnosis‐related group payment from a hospital's budget; hospitals would be required to earn this back through reporting and meeting specific performance goals. Using a phase‐in system, CMS would reimburse 2.5% in the first year for pay‐for‐reporting and 2.5% for pay‐for‐performance. Ultimately, the full 5% bonus would be based on performance results.11
Performance ratings play a central role in hospital accreditation, which is critical for negotiating terms for tiered contracting arrangements with private insurers. In addition, hospital performance rankings are becoming more publicly accessible. TJC reports hospital performance in meeting the SCIP measures on its website (
Physician‐Level Performance Reporting
In new quality assessment programs, physicians will also be rewarded or penalized according to their individual performance. The CMS Physician Quality Reporting Initiative (PQRI) is a claims‐based, voluntary, pay‐for‐reporting initiative targeted to Medicare providers. The PQRI program currently pays physicians 2% of total charges for covered services in exchange for voluntary reporting, and it is moving toward results‐based reimbursement.12 The 2009 PQRI Measures List describes 186 quality measures, including 2 related to VTE:13
-
Quality Measure 23: Percentage of patients aged 18 years and older undergoing procedures for which VTE prophylaxis is indicated in all patients, who had an order for LMWH, low‐dose UFH, adjusted‐dose warfarin, fondaparinux, or mechanical prophylaxis to be given within 24 hours prior to incision time or within 24 hours after surgery end‐time; and
-
Quality Measure 31: Percentage of patients aged 18 years and older with a diagnosis of ischemic stroke or intracranial hemorrhage who received DVT prophylaxis by end of hospital day 2.
In the PQRI, physicians report quality measures on process and patient outcomes to CMS using G‐codes or current procedural terminology (CPT)‐II codes. Approximately one‐half of the 100,000 providers who submitted quality codes during the first PQRI reporting period (July 1 to December 31, 2007) qualified for the incentive payment, totaling $36 million.12
More stringent pay‐for‐performance initiatives that hold physicians personally accountable for performance results are being developed in the private sector. For example, the Consumer‐Purchaser Disclosure Project (CPDP) is a consumer‐advocacy group that aims to improve healthcare and lower costs by holding healthcare providers publicly accountable for their quality of treatment. The CPDP has partnered with the National Committee for Quality Assurance to develop guidelines for reporting NQF performance measures.14
VTE as a Nonreimbursable Never Event
In a program that began with hospital discharges on October 1, 2008, hospitals will not receive CMS payment for 12 selected conditions that were not present on admission and were caused by medical error. These hospital‐acquired conditions (HAC), commonly known as never events, include pressure ulcers, catheter‐associated urinary tract infections, postoperative infections, and other complications. Beginning in fiscal year 2009, CMS has added hospital‐acquired VTE following hip or knee replacement surgery as a nonreimbursable never event.15 While CMS acknowledges that prophylaxis will not prevent every occurrence of DVT/PE, they feel it is a reasonably preventable HAC.15 Similar policies are expanding to state and private payor programs that require neither the patient nor the payor to reimburse the hospital for care related to reasonably preventable complications.
Improving Performance and Patient Outcomes
Despite the growing volume of evidence supporting the use of thromboprophylaxis, its use remains inadequate. The consequences are clear: between 2004 and 2006, the number of cases of postoperative VTE increased by 11%.1 This lack of progress may be due to clinicians' lack of awareness of evidence‐based interventions and to hospitals' lack of protocols for the provision of high‐quality preventive treatment.1 Successful strategies for improving thromboprophylaxis and other VTE performance measures are urgently needed. Over the past several years, researchers have been evaluating the utility of different strategies for improving guideline compliance, such as computer‐aided decision‐making and auditing and feedback programs.
Several initiatives seem to have been successful. In one review, Tooher et al.16 found that computerized reminders are, in general, one of the most effective strategies for improving prescribing practice. Paper‐based systems are easier to ignore without a challenge, while electronic systems may force users to acknowledge alerts. Stand‐alone protocols and reminder systems at the point of care can improve prophylaxis rates by about 50%, and decision‐support systems that integrate orders for prophylaxis can increase rates by up to 85%. Importantly, education‐only programs have not been sufficiently effective.16
Regardless of the strategy chosen, Tooher et al identified.16 several general features that, when included as part of the initiative, increase the likelihood of program success:
-
A process for demonstrating the importance and relevance of VTE prophylaxis in the local clinical setting (eg, presenting findings of a local audit of current practice to clinical staff);
-
A process for improving clinician knowledge about VTE risk assessment and prophylaxis practice, such as through a continuing education program;
-
A method of reminding clinicians to assess patients for VTE risk, accompanied by aids to assist in the documentation of patient risk;
-
A process for assisting clinicians in prescribing the appropriate prophylaxis; and
-
A method for assessing the effectiveness of any changes and for refining local policy to further improve practice, such as through clinical audit and feedback.
Table 3 lists several resources and tools that may be useful when designing and implementing strategies to improve performance and quality of care for hospitalized patients at risk of VTE.
| Resource | Description |
|---|---|
| |
| Society of Hospital Medicine, VTE Resource Room* | A website with educational resources, prophylaxis and treatment algorithms, and sample VTE protocols for various patient populations |
| American Society of Clinical Oncology; VTE Prophylaxis Orders and Flow Sheet | A sheet to consult and fill out when prescribing pharmacologic VTE prophylaxis for cancer patients; includes justifications for use, contraindications, anticoagulant options and doses, and other important details |
| American College of Chest Physicians | A source of guidelines, clinical research, education, and other resources for building an evidence‐based VTE protocol |
| National Comprehensive Cancer Network, Clinical Practice GuidelinesVTE | A concise source of algorithms for VTE prophylaxis, diagnosis, and treatment in cancer patients; also includes tables detailing recommended prevention/treatment regimens and warnings/contraindications |
Case Studies in Performance Improvement
Several institutions have reported success stories and shared details of their quality improvement initiatives. Whether paper‐based, electronic, physician‐targeted, or pharmacist‐led, these programs were designed to meet the unique needs of each institution and can serve as models for other hospitals wishing to implement similar programs to improve VTE prophylaxis rates and patient outcomes.
Brigham and Women's Hospital, Boston, MA
In 2005, Kucher et al.17 published a landmark report illustrating the benefits of an electronic alert system in increasing thromboprophylaxis and reducing VTE rates among hospitalized patients. The randomized trial identified high‐risk patients who were not receiving prophylaxis and assigned them to the intervention group, in which the treating physician was alerted to the VTE risk (n = 1255), or to the control group, in which no alert was made (n = 1251). Compared with patients in the control arm, those in the intervention arm were more than twice as likely to receive mechanical or pharmacologic prophylaxis (14.5% vs. 33.5%) and 41% less likely to develop VTE within 90 days (P < 0.001).17
In 2008, this system was evaluated in a new cohort study to determine the ongoing effectiveness of electronic alerts in a real hospital setting.18 The following steps were taken:
-
Alerts were dispatched for all high‐risk cases; and
-
The responsible physician for each high‐risk patient not receiving prophylaxis was issued a single alert detailing the patient's risk and encouraging the use of thromboprophylaxis
During the study period, the use of prophylaxis increased by 50% (P < 0.001). Still, nearly two‐thirds of physicians ignored the electronic alerts.18 Thus, while computer alert systems are helpful, other strategies must be employed to further improve prophylaxis rates in high‐risk medical patients.18
Roswell Park Cancer Institute, Buffalo, NY
Roswell Park Cancer Institute (RPCI), a Comprehensive Cancer Center with 24,000 active patients, initiated an institute‐wide quality improvement initiative in 2006 to improve the rates of VTE prophylaxis for all adult inpatients.19 This initiative included efforts to improve compliance with NCCN guidelines on all medical services and follow guidelines in accordance with NCCN, surgical best practices, and published standards on all surgical services. To accomplish this objective, RPCI:
-
Implemented mandatory, computerized physician order entry forms;
-
Promoted VTE awareness via staff education, field in‐services, and seminars; and
-
Tracked compliance with manual audits of patient charts every 3 months.
When the initiative began in the fourth quarter of 2006, the rate of NCCN‐recommended VTE prophylaxis was 61% with the medical services and 86% with the surgical services. As of the second quarter of 2008, guideline compliance had increased to 90% and 100% with the medical and surgical services, respectively. Accompanying this increase in compliance was a corresponding decrease in the incidence of VTE, from 0.39% in the fourth quarter of 2006 to 0.08% in the second quarter of 2008 (P < 0.0001). The most pronounced reductions in VTE incidence were observed within the medical services and among outpatients.19
Hartford Hospital, Hartford, CT
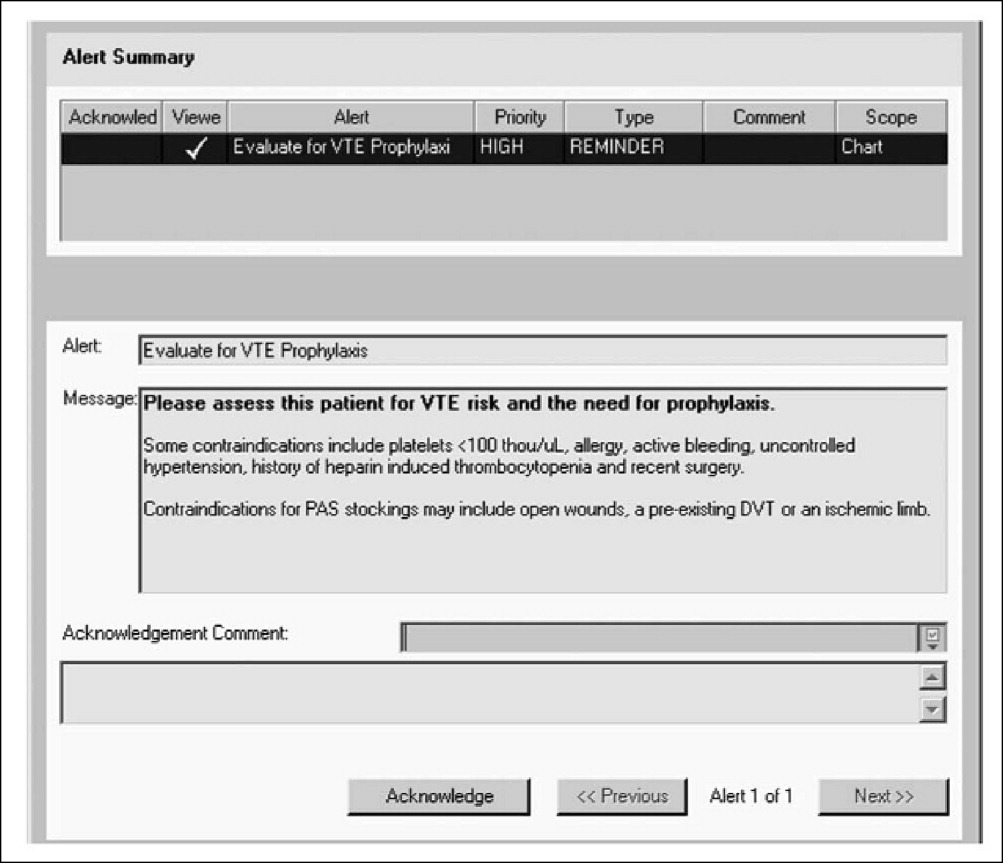
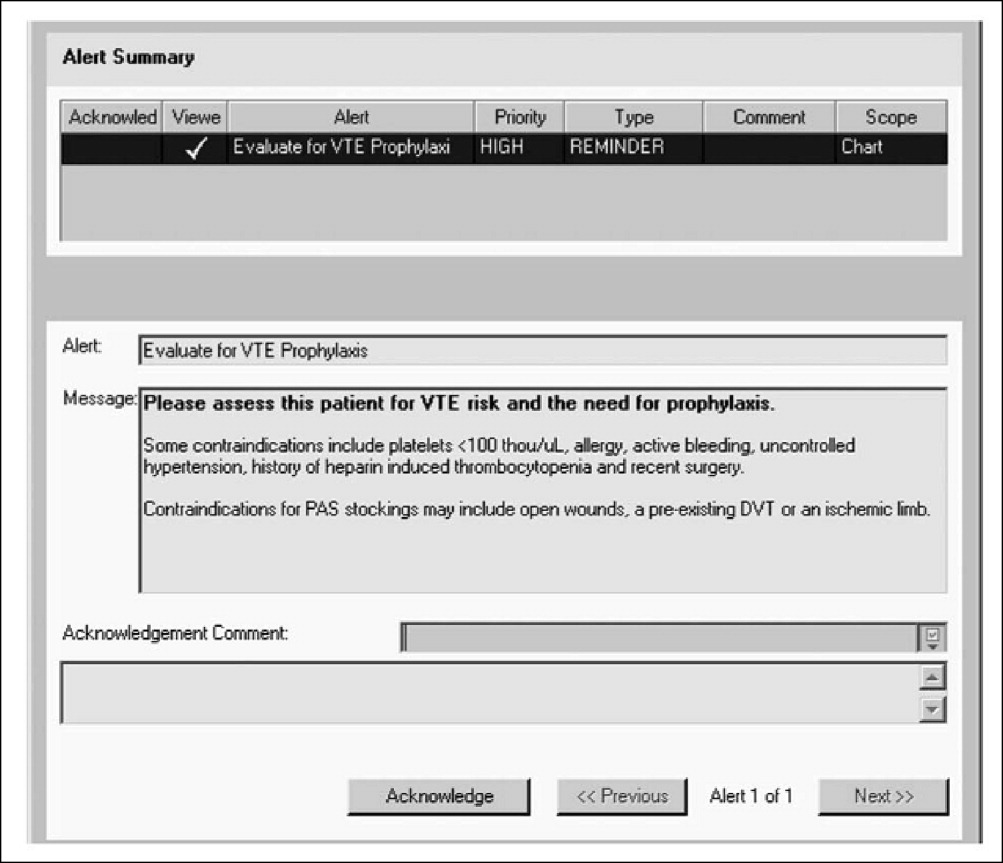
Hartford Hospital is an 819‐bed acute‐care community hospital with 300 designated medical beds. In an effort to improve thromboprophylaxis rates among medical patients, the pharmacy, medicine, and information technology departments collaborated to develop an alert within the computerized prescriber‐order‐entry system that reminded clinicians to assess patients for VTE risk factors and the need for prophylaxis.20 When a patient met predefined criteria for VTE risk, the message was displayed until either mechanical or pharmacologic VTE prophylaxis was an active order on the patient's treatment profile (Figure 1). The program was implemented in conjunction with an extensive educational program targeting hospital staff, pharmacists, physicians, nurse practitioners, physician assistants, and nurses.20
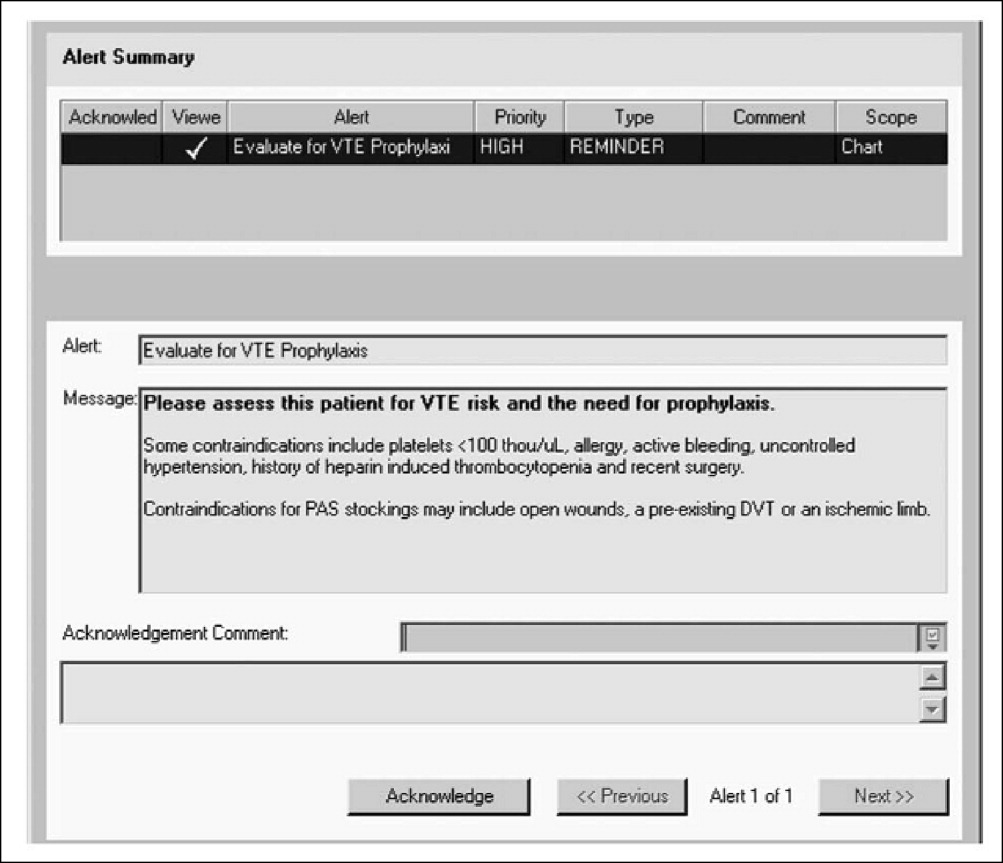
Compliance with institutional prophylaxis guidelines increased from 49% to 93% following implementation (P < 0.001). Interestingly, the initiative at Hartford Hospital was able to increase the use of mechanical prophylaxis among patients with a contradiction to pharmacologic therapy from 25% prior to the program to 100% after its implementation (P < 0.001).20
Saint Elizabeth's Hospital, Collinsville, IL
In 2008, Bauer et al.21 reported the benefits of a pharmacist‐led program for VTE prevention in Saint Elizabeth's Hospital, a 278‐bed hospital with more than 13,000 admissions per year. As part of the initiative, hospital pharmacists:
-
Received daily reports of all new admissions cross‐referenced with an accounting of patients currently prescribed UFH or LMWH;
-
Assessed the remaining patients at risk of VTE; and
-
Placed recommendations in patient charts in the form of a bold sticker alerting the physician to the patient's risk factors, their overall risk of VTE, and treatment recommendations (Figure 2).
The program ran 7 days per week, involved 1 pharmacist per day, and required an average of 4 hours per day. Patients in the maternity, nursery, pediatric, and psychiatric units were excluded from the program.
The program led to a significant increase in the use of VTE prophylaxis and a significant reduction in the rate of DVT (P < 0.002).21 These findings suggest that innovative programs tailored to the needs of individual institutions can dramatically increase thromboprophylaxis rates and decrease the incidence of VTE in at‐risk hospitalized patients.
Conclusions
VTE is a serious disease that leads to excess morbidity and mortality among hospitalized patients. The impact of hospital reporting on reimbursement and patient outcomes necessitates the adoption of strategies and protocols proven to enhance the management of VTE and improve patient outcomes. Several successful VTE initiatives have been described in the literature and can serve as models for institutions wishing to develop policies and procedures for preventing VTE. In addition, a number of online resources exist that can aid in the development of VTE protocols.
- U.S. Department of Health and Human Services. The surgeon general's call to action to prevent deep vein thrombosis and pulmonary embolism. Available at: http://www.surgeongeneral.gov/topics/deepvein/calltoaction/call‐to‐action‐on‐dvt‐2008.pdf. Accessed June2009.
- The Joint Commission. National consensus standards for prevention and care of venous thromboembolism (VTE). Last updated April 2009. Available at: http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/VTE.htm. Accessed June2009.
- , , , et al.Prevention of venous thromboembolism: American College of Chest Physicians evidence‐based clinical practice guidelines (8th edition).Chest2008;133(6 suppl):381S–453S.
- , , , , , ;American College of Chest Physicians.Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th edition).Chest.2008;133(6 suppl):454S–545S.
- The Joint Commission. Surgical Care Improvement Project Core Measure Set. Updated November 2008. Available at: http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/SCIP+Core+Measure+Set.htm. Accessed June2009.
- , , , et al.Are surgical patients at risk of venous thromboembolism current meeting the surgical care improvement performance target goal for appropriate and timely prophylaxis?Chest.2008;134:s46003.
- American Medical Association. Perioperative Care: Physician Performance Measurement Set. October 2006. Available at http://www.ama‐assn.org/ama1/pub/upload/mm/370/perioperativews1206.pdf. Accessed June2009.
- Leapfrog Group. The Leapfrog Group Hospital Quality and Safety Survey: What's New in the 2009 Survey (Version 5.1). Available at: https://leapfrog.medstat.com/pdf/final.pdf. Accessed June2009.
- , , , et al.Increasing awareness about venous disease: The American Venous Forum expands the National Venous Screening Program.J Vasc Surg.2008;48(2):394–399.
- Federal Register. Medicare Program; Proposed Changes to the Hospital Inpatient Prospective Payment Systems and Fiscal Year 2007 Rates. Available at: http://edocket.access.gpo.gov/2006/pdf/06‐3629.pdf. Accessed December 10,2008.
- Department of Health and Human Services, Centers for Medicare 241(3):397–415.
- , , , et al.Electronic alerts to prevent venous thromboembolism among hospitalized patients.N Engl J Med.2005;352(10):969–977.
- , , , et al.Electronic alerts for hospitalized high‐VTE risk patients not receiving prophylaxis: a cohort study.J Thromb Thrombolysis.2008;25(2):146–150.
- , , , et al. Improving compliance with guidelines for venous thromboembolism (VTE) prophylaxis significantly reduces VTE events. Presented at the 50th Annual Meeting of the American College of Hematology; San Francisco, CA; December 6‐9, 2008. Abstract 1288.
- .Development and implementation of a program to assess medical patients' need for venous thromboembolism prophylaxis.Am J Health Syst Pharm.2008;65(18):1755–1760.
- , , .Pharmacist‐led program to improve venous thromboembolism prophylaxis in a community hospital.Am J Health Syst Pharm.2008;65(17):1643–1647.
Despite the availability of evidence‐based guidelines for the prevention of thromboembolic morbidity and mortality, venous thromboembolism (VTE) remains a pervasive threat to public health. Prophylaxis is underused for a variety of reasons, which were summarized in the first article of this Supplement. Overcoming these barriers and reducing the incidence of VTE has become a major priority for public health policy.
The Office of the Surgeon General released a report in September 2008 that reflects this sense of urgency and national focus by calling for a coordinated, multifaceted plan to reduce the incidence of VTE in the United States.1 The Surgeon General report is one of the latest in a string of national initiatives designed to improve outcomes in patients at risk of VTE. In the past several years, public and private agencies have launched a range of programs aimed at improving deficiencies in the awareness, prevention, and treatment of VTE in hospitalized patients (these are summarized in Table 1). New performance measures and improvement initiatives may reduce the discrepancies between recommendations and practice, ultimately improving patient outcomes. These measures may possibly become benchmarks for pay‐for‐performance initiatives or future hospital accreditation.
| Measure/Initiative | Description |
|---|---|
| |
| National Quality Forum/The Joint Commission (NQF/TJC) | Public reporting of hospital performance in 6 performance measures; will apply to all medical and surgical patients |
| Surgical Care Improvement Project (SCIP) | Two performance measures enacted with reimbursement implications; 2 outcomes measures |
| American Medical Association Physician Consortium for Performance Improvement (PCPI) | Medical societies collaborating to identify gaps in care and develop performance measures; 1 measure has been endorsed |
| Leapfrog Hospital Quality and Safety Survey | Web database allowing consumers to compare performance among participating hospitals; includes 2 NQF safe practices |
| TJC National Patient Safety Goals (NPSG) | Goals for solving patient safety problems; compliance required for Joint Commission accreditation, with online reporting of results (Quality Check website) |
| North American Thrombosis Forum (NATF) | Nonprofit organization addressing unmet needs related to VTE and other thrombotic disorders |
| American Venous Forum National Venous Screening Program | National VTE awareness campaign; promotes compliance with protocols |
Herein, we review a variety of VTE performance measures, including those from the National Quality Forum (NQF), The Joint Commission (TJC), and the Surgical Care Improvement Project (SCIP). To illustrate how performance measures may be applied in the hospital setting to improve patient care, performance improvement programs that have proven effective in select hospitals across the United States are described.
Performance Measures and Initiatives
National Quality Forum Performance Measures
The NQF and TJC (formerly known as the Joint Commission on Accreditation of Healthcare Organizations) have already enacted performance measures for pneumonia, heart failure, acute myocardial infarction (MI), and other conditions. Since 2005, the NQF and TJC have been collaborating to develop national consensus performance measures for the prevention and care of VTE. The VTE performance measures will apply to all medical and surgical patients and include process measures in the areas of prevention and treatment, as well as outcome measures. After pilot‐testing a range of measures for 3 years, TJC recommended 7 candidate measures in November 2007. In May 2008, the NQF endorsed 6 of these, embracing all TJC recommendations except one relating to the use and documentation of vena cava filter quality improvement (Table 2).2
|
| Risk assessment and prophylaxis |
| 1. Documentation of VTE risk/prophylaxis within 24 hours of hospital admission or surgery end‐time |
| 2. Documentation of VTE risk/prophylaxis within 24 hours after ICU admission, transfer to ICU, or surgery end‐time |
| Treatment |
| 3. Patients with VTE with overlap of parenteral and warfarin anticoagulation therapy for at least 5 days with an INR 2 before discontinuation of parenteral therapy; for > 5 days with an INR < 2 and discharged on overlap therapy; or discharged in < 5 days on overlap therapy |
| 4. Patients with VTE receiving UFH with dosages/platelet count monitoring by protocol or nomogram |
| 5. Patients with VTE or their caregivers are given written discharge instructions or other educational material addressing all of the following: follow‐up monitoring, compliance issues, dietary restrictions, and potential for adverse drug reactions and interactions |
| Outcomes |
| 6. Incidence of potentially preventable hospital‐acquired VTE measured by patients who received no VTE prophylaxis before VTE diagnosis |
The next step is for the NQF to develop a specification manual that defines which patients should be given prophylaxis using International Classification of Diseases, 9th edition (ICD‐9) codes and identifies which interventions are appropriate for each patient population. Current clinical guidelines provide important guidance for appropriate inclusion and exclusion criteria for medical and surgical prophylaxis, as well as evidence‐based recommendations for the treatment of VTE.3, 4
SCIP
The SCIP has a stated goal of reducing surgical complications by 25% by 2010.5 To accomplish this, the SCIP is targeting improvement in 4 areas: surgical‐site infection, cardiac events, postoperative pneumonia, and VTE prophylaxis. The SCIP performance measures for VTE prophylaxis in surgical patients are as follows:
-
Recommended VTE prophylaxis ordered during admission; and
-
Appropriate VTE prophylaxis received within 24 hours prior to surgical incision time to 24 hours after surgery end time.
After the success seen by a core group of hospitals who volunteered to participate, all Medicare‐accredited hospitals were required to submit SCIP data beginning with discharges in the first quarter of 2007 to obtain full reimbursement from the Centers for Medicare and Medicaid Services (CMS). Institutions can gauge whether they are in compliance with the SCIP VTE measures by answering a series of yes or no questions about whether prophylaxis has been ordered and received for specific patient groups and procedures. In a recent study, almost one‐half of all surgical patients at risk of VTE did not receive recommended and timely prophylaxis as specified by the SCIP performance measures.6
In addition to the 2 enacted SCIP performance measures for VTE prophylaxis, 2 outcome measures are under development. These measures address the rate at which intraoperative or postoperative pulmonary embolism (PE; SCIP VTE‐3) and deep vein thrombosis (DVT; SCIP VTE‐4) are diagnosed during the index hospitalization and within 30 days after surgery. If implemented, these measures will capture the efficacy of thromboprophylaxis.5
Other VTE Performance Initiatives
Several professional and consumer organizations are developing standards and compiling performance data for public reporting and other purposes:
-
The American Medical Association Physician Consortium for Performance Improvement (PCPI) comprises more than 100 national medical specialty and state medical societies working to identify gaps in care that can be addressed with evidence‐based medicine and formal performance measures. The PCPI has endorsed a measure requiring low‐molecular‐weight heparin (LMWH), low‐dose unfractionated heparin (UFH), adjusted‐dose warfarin, fondaparinux, or mechanical prophylaxis to be given within 24 hours prior to incision time or within 24 hours after surgery end‐time for adults undergoing a procedure for which prophylaxis is indicated.7
-
The Leapfrog Hospital Quality and Safety Survey hosts a searchable web‐based database that consumers can use to compare performance among participating hospitals in specific geographic regions. The Leapfrog survey includes NQF safe practices #28 (reduce occurrence of VTE) and #29 (ensure long‐term anticoagulation is effective and safe).8
-
TJC National Patient Safety Goals (NPSG) target specific improvements in patient safety by providing healthcare organizations with solutions to prevalent patient safety problems. Compliance is necessary for Joint Commission accreditation, and results are reported on the Quality Check website. NPSG Goal 3 is focused on improving the safety of medications, and Goal 3E specifically addresses patient harm associated with the use of anticoagulation therapy. The 2008 NPSG goals must be implemented by January 2009.2
-
The North American Thrombosis Forum (NATF), a nonprofit organization, was recently organized to address unmet needs in North America related to VTE and other thrombotic disorders. It is designed to complement existing organizations dealing with thrombosis‐related issues, with 5 major focus areas: basic translational research; clinical research; prevention and education; public policy; and advocacy. Each month, its website (
http://www.natfonline.org ) features several scientific papers dealing with venous and arterial thrombosis‐related issues. -
The American Venous Forum National Venous Screening Program is a national campaign designed to increase VTE awareness and promote the importance of compliance with prophylaxis protocols.9
As different organizations work to develop performance measures for VTE, conflicting standards have emerged. Although this remains a major challenge, the NQF is attempting to develop voluntary consensus standards that will harmonize VTE performance measures across all sites of care, including the acute medical, surgical, and oncology settings. Major clinical guidelines from the American College of Physicians (ACP), American College of Chest Physicians (ACCP), the American Society of Clinical Oncology (ASCO), the National Comprehensive Cancer Network (NCCN), the European Society of Cardiology (ESC), and other organizations provide data to support standardized, evidence‐based measures for VTE.
Implications of Performance Data
Hospital‐Level Performance Reporting
Performance results may affect an institution's ability to contract best rates with payors, obtain full reimbursement for services, and be eligible for bonus payments. For example, pay‐for‐reporting legislation from CMS provides targeted financial incentives to improve the rates at which hospitals report data on quality measures. The current legislation stipulates that hospitals must submit performance data, including data on compliance with the 2 SCIP‐VTE measures, or lose 2% of their annual CMS payment update. For a 500‐bed hospital with 80% occupancy and 50% CMS patients, failure to report data on SCIP‐VTE measures would result in an estimated annual loss of $2.6 million.10
In 2007, the first year of the CMS pay‐for‐reporting program, 93% of hospitals met the reporting goals. As penalties for nonreporting increase, an even higher compliance rate may be expected. CMS is proposing a new system that would withhold 5% of the base operating diagnosis‐related group payment from a hospital's budget; hospitals would be required to earn this back through reporting and meeting specific performance goals. Using a phase‐in system, CMS would reimburse 2.5% in the first year for pay‐for‐reporting and 2.5% for pay‐for‐performance. Ultimately, the full 5% bonus would be based on performance results.11
Performance ratings play a central role in hospital accreditation, which is critical for negotiating terms for tiered contracting arrangements with private insurers. In addition, hospital performance rankings are becoming more publicly accessible. TJC reports hospital performance in meeting the SCIP measures on its website (
Physician‐Level Performance Reporting
In new quality assessment programs, physicians will also be rewarded or penalized according to their individual performance. The CMS Physician Quality Reporting Initiative (PQRI) is a claims‐based, voluntary, pay‐for‐reporting initiative targeted to Medicare providers. The PQRI program currently pays physicians 2% of total charges for covered services in exchange for voluntary reporting, and it is moving toward results‐based reimbursement.12 The 2009 PQRI Measures List describes 186 quality measures, including 2 related to VTE:13
-
Quality Measure 23: Percentage of patients aged 18 years and older undergoing procedures for which VTE prophylaxis is indicated in all patients, who had an order for LMWH, low‐dose UFH, adjusted‐dose warfarin, fondaparinux, or mechanical prophylaxis to be given within 24 hours prior to incision time or within 24 hours after surgery end‐time; and
-
Quality Measure 31: Percentage of patients aged 18 years and older with a diagnosis of ischemic stroke or intracranial hemorrhage who received DVT prophylaxis by end of hospital day 2.
In the PQRI, physicians report quality measures on process and patient outcomes to CMS using G‐codes or current procedural terminology (CPT)‐II codes. Approximately one‐half of the 100,000 providers who submitted quality codes during the first PQRI reporting period (July 1 to December 31, 2007) qualified for the incentive payment, totaling $36 million.12
More stringent pay‐for‐performance initiatives that hold physicians personally accountable for performance results are being developed in the private sector. For example, the Consumer‐Purchaser Disclosure Project (CPDP) is a consumer‐advocacy group that aims to improve healthcare and lower costs by holding healthcare providers publicly accountable for their quality of treatment. The CPDP has partnered with the National Committee for Quality Assurance to develop guidelines for reporting NQF performance measures.14
VTE as a Nonreimbursable Never Event
In a program that began with hospital discharges on October 1, 2008, hospitals will not receive CMS payment for 12 selected conditions that were not present on admission and were caused by medical error. These hospital‐acquired conditions (HAC), commonly known as never events, include pressure ulcers, catheter‐associated urinary tract infections, postoperative infections, and other complications. Beginning in fiscal year 2009, CMS has added hospital‐acquired VTE following hip or knee replacement surgery as a nonreimbursable never event.15 While CMS acknowledges that prophylaxis will not prevent every occurrence of DVT/PE, they feel it is a reasonably preventable HAC.15 Similar policies are expanding to state and private payor programs that require neither the patient nor the payor to reimburse the hospital for care related to reasonably preventable complications.
Improving Performance and Patient Outcomes
Despite the growing volume of evidence supporting the use of thromboprophylaxis, its use remains inadequate. The consequences are clear: between 2004 and 2006, the number of cases of postoperative VTE increased by 11%.1 This lack of progress may be due to clinicians' lack of awareness of evidence‐based interventions and to hospitals' lack of protocols for the provision of high‐quality preventive treatment.1 Successful strategies for improving thromboprophylaxis and other VTE performance measures are urgently needed. Over the past several years, researchers have been evaluating the utility of different strategies for improving guideline compliance, such as computer‐aided decision‐making and auditing and feedback programs.
Several initiatives seem to have been successful. In one review, Tooher et al.16 found that computerized reminders are, in general, one of the most effective strategies for improving prescribing practice. Paper‐based systems are easier to ignore without a challenge, while electronic systems may force users to acknowledge alerts. Stand‐alone protocols and reminder systems at the point of care can improve prophylaxis rates by about 50%, and decision‐support systems that integrate orders for prophylaxis can increase rates by up to 85%. Importantly, education‐only programs have not been sufficiently effective.16
Regardless of the strategy chosen, Tooher et al identified.16 several general features that, when included as part of the initiative, increase the likelihood of program success:
-
A process for demonstrating the importance and relevance of VTE prophylaxis in the local clinical setting (eg, presenting findings of a local audit of current practice to clinical staff);
-
A process for improving clinician knowledge about VTE risk assessment and prophylaxis practice, such as through a continuing education program;
-
A method of reminding clinicians to assess patients for VTE risk, accompanied by aids to assist in the documentation of patient risk;
-
A process for assisting clinicians in prescribing the appropriate prophylaxis; and
-
A method for assessing the effectiveness of any changes and for refining local policy to further improve practice, such as through clinical audit and feedback.
Table 3 lists several resources and tools that may be useful when designing and implementing strategies to improve performance and quality of care for hospitalized patients at risk of VTE.
| Resource | Description |
|---|---|
| |
| Society of Hospital Medicine, VTE Resource Room* | A website with educational resources, prophylaxis and treatment algorithms, and sample VTE protocols for various patient populations |
| American Society of Clinical Oncology; VTE Prophylaxis Orders and Flow Sheet | A sheet to consult and fill out when prescribing pharmacologic VTE prophylaxis for cancer patients; includes justifications for use, contraindications, anticoagulant options and doses, and other important details |
| American College of Chest Physicians | A source of guidelines, clinical research, education, and other resources for building an evidence‐based VTE protocol |
| National Comprehensive Cancer Network, Clinical Practice GuidelinesVTE | A concise source of algorithms for VTE prophylaxis, diagnosis, and treatment in cancer patients; also includes tables detailing recommended prevention/treatment regimens and warnings/contraindications |
Case Studies in Performance Improvement
Several institutions have reported success stories and shared details of their quality improvement initiatives. Whether paper‐based, electronic, physician‐targeted, or pharmacist‐led, these programs were designed to meet the unique needs of each institution and can serve as models for other hospitals wishing to implement similar programs to improve VTE prophylaxis rates and patient outcomes.
Brigham and Women's Hospital, Boston, MA
In 2005, Kucher et al.17 published a landmark report illustrating the benefits of an electronic alert system in increasing thromboprophylaxis and reducing VTE rates among hospitalized patients. The randomized trial identified high‐risk patients who were not receiving prophylaxis and assigned them to the intervention group, in which the treating physician was alerted to the VTE risk (n = 1255), or to the control group, in which no alert was made (n = 1251). Compared with patients in the control arm, those in the intervention arm were more than twice as likely to receive mechanical or pharmacologic prophylaxis (14.5% vs. 33.5%) and 41% less likely to develop VTE within 90 days (P < 0.001).17
In 2008, this system was evaluated in a new cohort study to determine the ongoing effectiveness of electronic alerts in a real hospital setting.18 The following steps were taken:
-
Alerts were dispatched for all high‐risk cases; and
-
The responsible physician for each high‐risk patient not receiving prophylaxis was issued a single alert detailing the patient's risk and encouraging the use of thromboprophylaxis
During the study period, the use of prophylaxis increased by 50% (P < 0.001). Still, nearly two‐thirds of physicians ignored the electronic alerts.18 Thus, while computer alert systems are helpful, other strategies must be employed to further improve prophylaxis rates in high‐risk medical patients.18
Roswell Park Cancer Institute, Buffalo, NY
Roswell Park Cancer Institute (RPCI), a Comprehensive Cancer Center with 24,000 active patients, initiated an institute‐wide quality improvement initiative in 2006 to improve the rates of VTE prophylaxis for all adult inpatients.19 This initiative included efforts to improve compliance with NCCN guidelines on all medical services and follow guidelines in accordance with NCCN, surgical best practices, and published standards on all surgical services. To accomplish this objective, RPCI:
-
Implemented mandatory, computerized physician order entry forms;
-
Promoted VTE awareness via staff education, field in‐services, and seminars; and
-
Tracked compliance with manual audits of patient charts every 3 months.
When the initiative began in the fourth quarter of 2006, the rate of NCCN‐recommended VTE prophylaxis was 61% with the medical services and 86% with the surgical services. As of the second quarter of 2008, guideline compliance had increased to 90% and 100% with the medical and surgical services, respectively. Accompanying this increase in compliance was a corresponding decrease in the incidence of VTE, from 0.39% in the fourth quarter of 2006 to 0.08% in the second quarter of 2008 (P < 0.0001). The most pronounced reductions in VTE incidence were observed within the medical services and among outpatients.19
Hartford Hospital, Hartford, CT
Hartford Hospital is an 819‐bed acute‐care community hospital with 300 designated medical beds. In an effort to improve thromboprophylaxis rates among medical patients, the pharmacy, medicine, and information technology departments collaborated to develop an alert within the computerized prescriber‐order‐entry system that reminded clinicians to assess patients for VTE risk factors and the need for prophylaxis.20 When a patient met predefined criteria for VTE risk, the message was displayed until either mechanical or pharmacologic VTE prophylaxis was an active order on the patient's treatment profile (Figure 1). The program was implemented in conjunction with an extensive educational program targeting hospital staff, pharmacists, physicians, nurse practitioners, physician assistants, and nurses.20
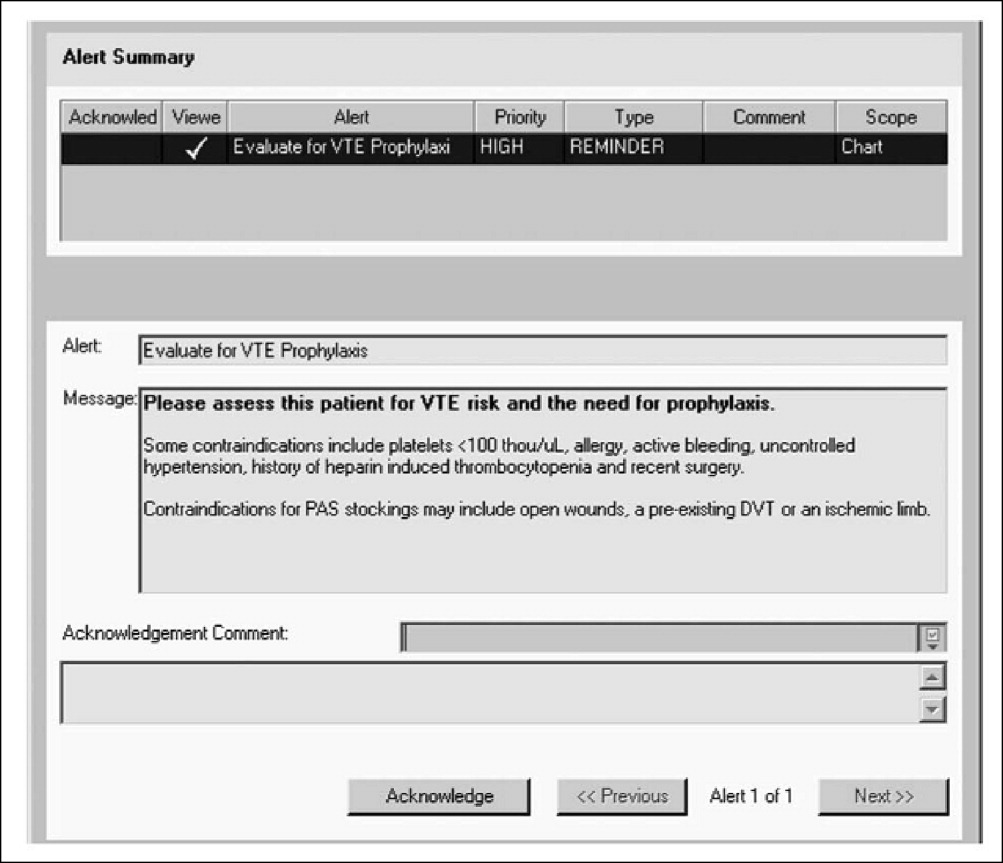
Compliance with institutional prophylaxis guidelines increased from 49% to 93% following implementation (P < 0.001). Interestingly, the initiative at Hartford Hospital was able to increase the use of mechanical prophylaxis among patients with a contradiction to pharmacologic therapy from 25% prior to the program to 100% after its implementation (P < 0.001).20
Saint Elizabeth's Hospital, Collinsville, IL
In 2008, Bauer et al.21 reported the benefits of a pharmacist‐led program for VTE prevention in Saint Elizabeth's Hospital, a 278‐bed hospital with more than 13,000 admissions per year. As part of the initiative, hospital pharmacists:
-
Received daily reports of all new admissions cross‐referenced with an accounting of patients currently prescribed UFH or LMWH;
-
Assessed the remaining patients at risk of VTE; and
-
Placed recommendations in patient charts in the form of a bold sticker alerting the physician to the patient's risk factors, their overall risk of VTE, and treatment recommendations (Figure 2).
The program ran 7 days per week, involved 1 pharmacist per day, and required an average of 4 hours per day. Patients in the maternity, nursery, pediatric, and psychiatric units were excluded from the program.
The program led to a significant increase in the use of VTE prophylaxis and a significant reduction in the rate of DVT (P < 0.002).21 These findings suggest that innovative programs tailored to the needs of individual institutions can dramatically increase thromboprophylaxis rates and decrease the incidence of VTE in at‐risk hospitalized patients.
Conclusions
VTE is a serious disease that leads to excess morbidity and mortality among hospitalized patients. The impact of hospital reporting on reimbursement and patient outcomes necessitates the adoption of strategies and protocols proven to enhance the management of VTE and improve patient outcomes. Several successful VTE initiatives have been described in the literature and can serve as models for institutions wishing to develop policies and procedures for preventing VTE. In addition, a number of online resources exist that can aid in the development of VTE protocols.
Despite the availability of evidence‐based guidelines for the prevention of thromboembolic morbidity and mortality, venous thromboembolism (VTE) remains a pervasive threat to public health. Prophylaxis is underused for a variety of reasons, which were summarized in the first article of this Supplement. Overcoming these barriers and reducing the incidence of VTE has become a major priority for public health policy.
The Office of the Surgeon General released a report in September 2008 that reflects this sense of urgency and national focus by calling for a coordinated, multifaceted plan to reduce the incidence of VTE in the United States.1 The Surgeon General report is one of the latest in a string of national initiatives designed to improve outcomes in patients at risk of VTE. In the past several years, public and private agencies have launched a range of programs aimed at improving deficiencies in the awareness, prevention, and treatment of VTE in hospitalized patients (these are summarized in Table 1). New performance measures and improvement initiatives may reduce the discrepancies between recommendations and practice, ultimately improving patient outcomes. These measures may possibly become benchmarks for pay‐for‐performance initiatives or future hospital accreditation.
| Measure/Initiative | Description |
|---|---|
| |
| National Quality Forum/The Joint Commission (NQF/TJC) | Public reporting of hospital performance in 6 performance measures; will apply to all medical and surgical patients |
| Surgical Care Improvement Project (SCIP) | Two performance measures enacted with reimbursement implications; 2 outcomes measures |
| American Medical Association Physician Consortium for Performance Improvement (PCPI) | Medical societies collaborating to identify gaps in care and develop performance measures; 1 measure has been endorsed |
| Leapfrog Hospital Quality and Safety Survey | Web database allowing consumers to compare performance among participating hospitals; includes 2 NQF safe practices |
| TJC National Patient Safety Goals (NPSG) | Goals for solving patient safety problems; compliance required for Joint Commission accreditation, with online reporting of results (Quality Check website) |
| North American Thrombosis Forum (NATF) | Nonprofit organization addressing unmet needs related to VTE and other thrombotic disorders |
| American Venous Forum National Venous Screening Program | National VTE awareness campaign; promotes compliance with protocols |
Herein, we review a variety of VTE performance measures, including those from the National Quality Forum (NQF), The Joint Commission (TJC), and the Surgical Care Improvement Project (SCIP). To illustrate how performance measures may be applied in the hospital setting to improve patient care, performance improvement programs that have proven effective in select hospitals across the United States are described.
Performance Measures and Initiatives
National Quality Forum Performance Measures
The NQF and TJC (formerly known as the Joint Commission on Accreditation of Healthcare Organizations) have already enacted performance measures for pneumonia, heart failure, acute myocardial infarction (MI), and other conditions. Since 2005, the NQF and TJC have been collaborating to develop national consensus performance measures for the prevention and care of VTE. The VTE performance measures will apply to all medical and surgical patients and include process measures in the areas of prevention and treatment, as well as outcome measures. After pilot‐testing a range of measures for 3 years, TJC recommended 7 candidate measures in November 2007. In May 2008, the NQF endorsed 6 of these, embracing all TJC recommendations except one relating to the use and documentation of vena cava filter quality improvement (Table 2).2
|
| Risk assessment and prophylaxis |
| 1. Documentation of VTE risk/prophylaxis within 24 hours of hospital admission or surgery end‐time |
| 2. Documentation of VTE risk/prophylaxis within 24 hours after ICU admission, transfer to ICU, or surgery end‐time |
| Treatment |
| 3. Patients with VTE with overlap of parenteral and warfarin anticoagulation therapy for at least 5 days with an INR 2 before discontinuation of parenteral therapy; for > 5 days with an INR < 2 and discharged on overlap therapy; or discharged in < 5 days on overlap therapy |
| 4. Patients with VTE receiving UFH with dosages/platelet count monitoring by protocol or nomogram |
| 5. Patients with VTE or their caregivers are given written discharge instructions or other educational material addressing all of the following: follow‐up monitoring, compliance issues, dietary restrictions, and potential for adverse drug reactions and interactions |
| Outcomes |
| 6. Incidence of potentially preventable hospital‐acquired VTE measured by patients who received no VTE prophylaxis before VTE diagnosis |
The next step is for the NQF to develop a specification manual that defines which patients should be given prophylaxis using International Classification of Diseases, 9th edition (ICD‐9) codes and identifies which interventions are appropriate for each patient population. Current clinical guidelines provide important guidance for appropriate inclusion and exclusion criteria for medical and surgical prophylaxis, as well as evidence‐based recommendations for the treatment of VTE.3, 4
SCIP
The SCIP has a stated goal of reducing surgical complications by 25% by 2010.5 To accomplish this, the SCIP is targeting improvement in 4 areas: surgical‐site infection, cardiac events, postoperative pneumonia, and VTE prophylaxis. The SCIP performance measures for VTE prophylaxis in surgical patients are as follows:
-
Recommended VTE prophylaxis ordered during admission; and
-
Appropriate VTE prophylaxis received within 24 hours prior to surgical incision time to 24 hours after surgery end time.
After the success seen by a core group of hospitals who volunteered to participate, all Medicare‐accredited hospitals were required to submit SCIP data beginning with discharges in the first quarter of 2007 to obtain full reimbursement from the Centers for Medicare and Medicaid Services (CMS). Institutions can gauge whether they are in compliance with the SCIP VTE measures by answering a series of yes or no questions about whether prophylaxis has been ordered and received for specific patient groups and procedures. In a recent study, almost one‐half of all surgical patients at risk of VTE did not receive recommended and timely prophylaxis as specified by the SCIP performance measures.6
In addition to the 2 enacted SCIP performance measures for VTE prophylaxis, 2 outcome measures are under development. These measures address the rate at which intraoperative or postoperative pulmonary embolism (PE; SCIP VTE‐3) and deep vein thrombosis (DVT; SCIP VTE‐4) are diagnosed during the index hospitalization and within 30 days after surgery. If implemented, these measures will capture the efficacy of thromboprophylaxis.5
Other VTE Performance Initiatives
Several professional and consumer organizations are developing standards and compiling performance data for public reporting and other purposes:
-
The American Medical Association Physician Consortium for Performance Improvement (PCPI) comprises more than 100 national medical specialty and state medical societies working to identify gaps in care that can be addressed with evidence‐based medicine and formal performance measures. The PCPI has endorsed a measure requiring low‐molecular‐weight heparin (LMWH), low‐dose unfractionated heparin (UFH), adjusted‐dose warfarin, fondaparinux, or mechanical prophylaxis to be given within 24 hours prior to incision time or within 24 hours after surgery end‐time for adults undergoing a procedure for which prophylaxis is indicated.7
-
The Leapfrog Hospital Quality and Safety Survey hosts a searchable web‐based database that consumers can use to compare performance among participating hospitals in specific geographic regions. The Leapfrog survey includes NQF safe practices #28 (reduce occurrence of VTE) and #29 (ensure long‐term anticoagulation is effective and safe).8
-
TJC National Patient Safety Goals (NPSG) target specific improvements in patient safety by providing healthcare organizations with solutions to prevalent patient safety problems. Compliance is necessary for Joint Commission accreditation, and results are reported on the Quality Check website. NPSG Goal 3 is focused on improving the safety of medications, and Goal 3E specifically addresses patient harm associated with the use of anticoagulation therapy. The 2008 NPSG goals must be implemented by January 2009.2
-
The North American Thrombosis Forum (NATF), a nonprofit organization, was recently organized to address unmet needs in North America related to VTE and other thrombotic disorders. It is designed to complement existing organizations dealing with thrombosis‐related issues, with 5 major focus areas: basic translational research; clinical research; prevention and education; public policy; and advocacy. Each month, its website (
http://www.natfonline.org ) features several scientific papers dealing with venous and arterial thrombosis‐related issues. -
The American Venous Forum National Venous Screening Program is a national campaign designed to increase VTE awareness and promote the importance of compliance with prophylaxis protocols.9
As different organizations work to develop performance measures for VTE, conflicting standards have emerged. Although this remains a major challenge, the NQF is attempting to develop voluntary consensus standards that will harmonize VTE performance measures across all sites of care, including the acute medical, surgical, and oncology settings. Major clinical guidelines from the American College of Physicians (ACP), American College of Chest Physicians (ACCP), the American Society of Clinical Oncology (ASCO), the National Comprehensive Cancer Network (NCCN), the European Society of Cardiology (ESC), and other organizations provide data to support standardized, evidence‐based measures for VTE.
Implications of Performance Data
Hospital‐Level Performance Reporting
Performance results may affect an institution's ability to contract best rates with payors, obtain full reimbursement for services, and be eligible for bonus payments. For example, pay‐for‐reporting legislation from CMS provides targeted financial incentives to improve the rates at which hospitals report data on quality measures. The current legislation stipulates that hospitals must submit performance data, including data on compliance with the 2 SCIP‐VTE measures, or lose 2% of their annual CMS payment update. For a 500‐bed hospital with 80% occupancy and 50% CMS patients, failure to report data on SCIP‐VTE measures would result in an estimated annual loss of $2.6 million.10
In 2007, the first year of the CMS pay‐for‐reporting program, 93% of hospitals met the reporting goals. As penalties for nonreporting increase, an even higher compliance rate may be expected. CMS is proposing a new system that would withhold 5% of the base operating diagnosis‐related group payment from a hospital's budget; hospitals would be required to earn this back through reporting and meeting specific performance goals. Using a phase‐in system, CMS would reimburse 2.5% in the first year for pay‐for‐reporting and 2.5% for pay‐for‐performance. Ultimately, the full 5% bonus would be based on performance results.11
Performance ratings play a central role in hospital accreditation, which is critical for negotiating terms for tiered contracting arrangements with private insurers. In addition, hospital performance rankings are becoming more publicly accessible. TJC reports hospital performance in meeting the SCIP measures on its website (
Physician‐Level Performance Reporting
In new quality assessment programs, physicians will also be rewarded or penalized according to their individual performance. The CMS Physician Quality Reporting Initiative (PQRI) is a claims‐based, voluntary, pay‐for‐reporting initiative targeted to Medicare providers. The PQRI program currently pays physicians 2% of total charges for covered services in exchange for voluntary reporting, and it is moving toward results‐based reimbursement.12 The 2009 PQRI Measures List describes 186 quality measures, including 2 related to VTE:13
-
Quality Measure 23: Percentage of patients aged 18 years and older undergoing procedures for which VTE prophylaxis is indicated in all patients, who had an order for LMWH, low‐dose UFH, adjusted‐dose warfarin, fondaparinux, or mechanical prophylaxis to be given within 24 hours prior to incision time or within 24 hours after surgery end‐time; and
-
Quality Measure 31: Percentage of patients aged 18 years and older with a diagnosis of ischemic stroke or intracranial hemorrhage who received DVT prophylaxis by end of hospital day 2.
In the PQRI, physicians report quality measures on process and patient outcomes to CMS using G‐codes or current procedural terminology (CPT)‐II codes. Approximately one‐half of the 100,000 providers who submitted quality codes during the first PQRI reporting period (July 1 to December 31, 2007) qualified for the incentive payment, totaling $36 million.12
More stringent pay‐for‐performance initiatives that hold physicians personally accountable for performance results are being developed in the private sector. For example, the Consumer‐Purchaser Disclosure Project (CPDP) is a consumer‐advocacy group that aims to improve healthcare and lower costs by holding healthcare providers publicly accountable for their quality of treatment. The CPDP has partnered with the National Committee for Quality Assurance to develop guidelines for reporting NQF performance measures.14
VTE as a Nonreimbursable Never Event
In a program that began with hospital discharges on October 1, 2008, hospitals will not receive CMS payment for 12 selected conditions that were not present on admission and were caused by medical error. These hospital‐acquired conditions (HAC), commonly known as never events, include pressure ulcers, catheter‐associated urinary tract infections, postoperative infections, and other complications. Beginning in fiscal year 2009, CMS has added hospital‐acquired VTE following hip or knee replacement surgery as a nonreimbursable never event.15 While CMS acknowledges that prophylaxis will not prevent every occurrence of DVT/PE, they feel it is a reasonably preventable HAC.15 Similar policies are expanding to state and private payor programs that require neither the patient nor the payor to reimburse the hospital for care related to reasonably preventable complications.
Improving Performance and Patient Outcomes
Despite the growing volume of evidence supporting the use of thromboprophylaxis, its use remains inadequate. The consequences are clear: between 2004 and 2006, the number of cases of postoperative VTE increased by 11%.1 This lack of progress may be due to clinicians' lack of awareness of evidence‐based interventions and to hospitals' lack of protocols for the provision of high‐quality preventive treatment.1 Successful strategies for improving thromboprophylaxis and other VTE performance measures are urgently needed. Over the past several years, researchers have been evaluating the utility of different strategies for improving guideline compliance, such as computer‐aided decision‐making and auditing and feedback programs.
Several initiatives seem to have been successful. In one review, Tooher et al.16 found that computerized reminders are, in general, one of the most effective strategies for improving prescribing practice. Paper‐based systems are easier to ignore without a challenge, while electronic systems may force users to acknowledge alerts. Stand‐alone protocols and reminder systems at the point of care can improve prophylaxis rates by about 50%, and decision‐support systems that integrate orders for prophylaxis can increase rates by up to 85%. Importantly, education‐only programs have not been sufficiently effective.16
Regardless of the strategy chosen, Tooher et al identified.16 several general features that, when included as part of the initiative, increase the likelihood of program success:
-
A process for demonstrating the importance and relevance of VTE prophylaxis in the local clinical setting (eg, presenting findings of a local audit of current practice to clinical staff);
-
A process for improving clinician knowledge about VTE risk assessment and prophylaxis practice, such as through a continuing education program;
-
A method of reminding clinicians to assess patients for VTE risk, accompanied by aids to assist in the documentation of patient risk;
-
A process for assisting clinicians in prescribing the appropriate prophylaxis; and
-
A method for assessing the effectiveness of any changes and for refining local policy to further improve practice, such as through clinical audit and feedback.
Table 3 lists several resources and tools that may be useful when designing and implementing strategies to improve performance and quality of care for hospitalized patients at risk of VTE.
| Resource | Description |
|---|---|
| |
| Society of Hospital Medicine, VTE Resource Room* | A website with educational resources, prophylaxis and treatment algorithms, and sample VTE protocols for various patient populations |
| American Society of Clinical Oncology; VTE Prophylaxis Orders and Flow Sheet | A sheet to consult and fill out when prescribing pharmacologic VTE prophylaxis for cancer patients; includes justifications for use, contraindications, anticoagulant options and doses, and other important details |
| American College of Chest Physicians | A source of guidelines, clinical research, education, and other resources for building an evidence‐based VTE protocol |
| National Comprehensive Cancer Network, Clinical Practice GuidelinesVTE | A concise source of algorithms for VTE prophylaxis, diagnosis, and treatment in cancer patients; also includes tables detailing recommended prevention/treatment regimens and warnings/contraindications |
Case Studies in Performance Improvement
Several institutions have reported success stories and shared details of their quality improvement initiatives. Whether paper‐based, electronic, physician‐targeted, or pharmacist‐led, these programs were designed to meet the unique needs of each institution and can serve as models for other hospitals wishing to implement similar programs to improve VTE prophylaxis rates and patient outcomes.
Brigham and Women's Hospital, Boston, MA
In 2005, Kucher et al.17 published a landmark report illustrating the benefits of an electronic alert system in increasing thromboprophylaxis and reducing VTE rates among hospitalized patients. The randomized trial identified high‐risk patients who were not receiving prophylaxis and assigned them to the intervention group, in which the treating physician was alerted to the VTE risk (n = 1255), or to the control group, in which no alert was made (n = 1251). Compared with patients in the control arm, those in the intervention arm were more than twice as likely to receive mechanical or pharmacologic prophylaxis (14.5% vs. 33.5%) and 41% less likely to develop VTE within 90 days (P < 0.001).17
In 2008, this system was evaluated in a new cohort study to determine the ongoing effectiveness of electronic alerts in a real hospital setting.18 The following steps were taken:
-
Alerts were dispatched for all high‐risk cases; and
-
The responsible physician for each high‐risk patient not receiving prophylaxis was issued a single alert detailing the patient's risk and encouraging the use of thromboprophylaxis
During the study period, the use of prophylaxis increased by 50% (P < 0.001). Still, nearly two‐thirds of physicians ignored the electronic alerts.18 Thus, while computer alert systems are helpful, other strategies must be employed to further improve prophylaxis rates in high‐risk medical patients.18
Roswell Park Cancer Institute, Buffalo, NY
Roswell Park Cancer Institute (RPCI), a Comprehensive Cancer Center with 24,000 active patients, initiated an institute‐wide quality improvement initiative in 2006 to improve the rates of VTE prophylaxis for all adult inpatients.19 This initiative included efforts to improve compliance with NCCN guidelines on all medical services and follow guidelines in accordance with NCCN, surgical best practices, and published standards on all surgical services. To accomplish this objective, RPCI:
-
Implemented mandatory, computerized physician order entry forms;
-
Promoted VTE awareness via staff education, field in‐services, and seminars; and
-
Tracked compliance with manual audits of patient charts every 3 months.
When the initiative began in the fourth quarter of 2006, the rate of NCCN‐recommended VTE prophylaxis was 61% with the medical services and 86% with the surgical services. As of the second quarter of 2008, guideline compliance had increased to 90% and 100% with the medical and surgical services, respectively. Accompanying this increase in compliance was a corresponding decrease in the incidence of VTE, from 0.39% in the fourth quarter of 2006 to 0.08% in the second quarter of 2008 (P < 0.0001). The most pronounced reductions in VTE incidence were observed within the medical services and among outpatients.19
Hartford Hospital, Hartford, CT
Hartford Hospital is an 819‐bed acute‐care community hospital with 300 designated medical beds. In an effort to improve thromboprophylaxis rates among medical patients, the pharmacy, medicine, and information technology departments collaborated to develop an alert within the computerized prescriber‐order‐entry system that reminded clinicians to assess patients for VTE risk factors and the need for prophylaxis.20 When a patient met predefined criteria for VTE risk, the message was displayed until either mechanical or pharmacologic VTE prophylaxis was an active order on the patient's treatment profile (Figure 1). The program was implemented in conjunction with an extensive educational program targeting hospital staff, pharmacists, physicians, nurse practitioners, physician assistants, and nurses.20
Compliance with institutional prophylaxis guidelines increased from 49% to 93% following implementation (P < 0.001). Interestingly, the initiative at Hartford Hospital was able to increase the use of mechanical prophylaxis among patients with a contradiction to pharmacologic therapy from 25% prior to the program to 100% after its implementation (P < 0.001).20
Saint Elizabeth's Hospital, Collinsville, IL
In 2008, Bauer et al.21 reported the benefits of a pharmacist‐led program for VTE prevention in Saint Elizabeth's Hospital, a 278‐bed hospital with more than 13,000 admissions per year. As part of the initiative, hospital pharmacists:
-
Received daily reports of all new admissions cross‐referenced with an accounting of patients currently prescribed UFH or LMWH;
-
Assessed the remaining patients at risk of VTE; and
-
Placed recommendations in patient charts in the form of a bold sticker alerting the physician to the patient's risk factors, their overall risk of VTE, and treatment recommendations (Figure 2).
The program ran 7 days per week, involved 1 pharmacist per day, and required an average of 4 hours per day. Patients in the maternity, nursery, pediatric, and psychiatric units were excluded from the program.
The program led to a significant increase in the use of VTE prophylaxis and a significant reduction in the rate of DVT (P < 0.002).21 These findings suggest that innovative programs tailored to the needs of individual institutions can dramatically increase thromboprophylaxis rates and decrease the incidence of VTE in at‐risk hospitalized patients.
Conclusions
VTE is a serious disease that leads to excess morbidity and mortality among hospitalized patients. The impact of hospital reporting on reimbursement and patient outcomes necessitates the adoption of strategies and protocols proven to enhance the management of VTE and improve patient outcomes. Several successful VTE initiatives have been described in the literature and can serve as models for institutions wishing to develop policies and procedures for preventing VTE. In addition, a number of online resources exist that can aid in the development of VTE protocols.
- U.S. Department of Health and Human Services. The surgeon general's call to action to prevent deep vein thrombosis and pulmonary embolism. Available at: http://www.surgeongeneral.gov/topics/deepvein/calltoaction/call‐to‐action‐on‐dvt‐2008.pdf. Accessed June2009.
- The Joint Commission. National consensus standards for prevention and care of venous thromboembolism (VTE). Last updated April 2009. Available at: http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/VTE.htm. Accessed June2009.
- , , , et al.Prevention of venous thromboembolism: American College of Chest Physicians evidence‐based clinical practice guidelines (8th edition).Chest2008;133(6 suppl):381S–453S.
- , , , , , ;American College of Chest Physicians.Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th edition).Chest.2008;133(6 suppl):454S–545S.
- The Joint Commission. Surgical Care Improvement Project Core Measure Set. Updated November 2008. Available at: http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/SCIP+Core+Measure+Set.htm. Accessed June2009.
- , , , et al.Are surgical patients at risk of venous thromboembolism current meeting the surgical care improvement performance target goal for appropriate and timely prophylaxis?Chest.2008;134:s46003.
- American Medical Association. Perioperative Care: Physician Performance Measurement Set. October 2006. Available at http://www.ama‐assn.org/ama1/pub/upload/mm/370/perioperativews1206.pdf. Accessed June2009.
- Leapfrog Group. The Leapfrog Group Hospital Quality and Safety Survey: What's New in the 2009 Survey (Version 5.1). Available at: https://leapfrog.medstat.com/pdf/final.pdf. Accessed June2009.
- , , , et al.Increasing awareness about venous disease: The American Venous Forum expands the National Venous Screening Program.J Vasc Surg.2008;48(2):394–399.
- Federal Register. Medicare Program; Proposed Changes to the Hospital Inpatient Prospective Payment Systems and Fiscal Year 2007 Rates. Available at: http://edocket.access.gpo.gov/2006/pdf/06‐3629.pdf. Accessed December 10,2008.
- Department of Health and Human Services, Centers for Medicare 241(3):397–415.
- , , , et al.Electronic alerts to prevent venous thromboembolism among hospitalized patients.N Engl J Med.2005;352(10):969–977.
- , , , et al.Electronic alerts for hospitalized high‐VTE risk patients not receiving prophylaxis: a cohort study.J Thromb Thrombolysis.2008;25(2):146–150.
- , , , et al. Improving compliance with guidelines for venous thromboembolism (VTE) prophylaxis significantly reduces VTE events. Presented at the 50th Annual Meeting of the American College of Hematology; San Francisco, CA; December 6‐9, 2008. Abstract 1288.
- .Development and implementation of a program to assess medical patients' need for venous thromboembolism prophylaxis.Am J Health Syst Pharm.2008;65(18):1755–1760.
- , , .Pharmacist‐led program to improve venous thromboembolism prophylaxis in a community hospital.Am J Health Syst Pharm.2008;65(17):1643–1647.
- U.S. Department of Health and Human Services. The surgeon general's call to action to prevent deep vein thrombosis and pulmonary embolism. Available at: http://www.surgeongeneral.gov/topics/deepvein/calltoaction/call‐to‐action‐on‐dvt‐2008.pdf. Accessed June2009.
- The Joint Commission. National consensus standards for prevention and care of venous thromboembolism (VTE). Last updated April 2009. Available at: http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/VTE.htm. Accessed June2009.
- , , , et al.Prevention of venous thromboembolism: American College of Chest Physicians evidence‐based clinical practice guidelines (8th edition).Chest2008;133(6 suppl):381S–453S.
- , , , , , ;American College of Chest Physicians.Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th edition).Chest.2008;133(6 suppl):454S–545S.
- The Joint Commission. Surgical Care Improvement Project Core Measure Set. Updated November 2008. Available at: http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/SCIP+Core+Measure+Set.htm. Accessed June2009.
- , , , et al.Are surgical patients at risk of venous thromboembolism current meeting the surgical care improvement performance target goal for appropriate and timely prophylaxis?Chest.2008;134:s46003.
- American Medical Association. Perioperative Care: Physician Performance Measurement Set. October 2006. Available at http://www.ama‐assn.org/ama1/pub/upload/mm/370/perioperativews1206.pdf. Accessed June2009.
- Leapfrog Group. The Leapfrog Group Hospital Quality and Safety Survey: What's New in the 2009 Survey (Version 5.1). Available at: https://leapfrog.medstat.com/pdf/final.pdf. Accessed June2009.
- , , , et al.Increasing awareness about venous disease: The American Venous Forum expands the National Venous Screening Program.J Vasc Surg.2008;48(2):394–399.
- Federal Register. Medicare Program; Proposed Changes to the Hospital Inpatient Prospective Payment Systems and Fiscal Year 2007 Rates. Available at: http://edocket.access.gpo.gov/2006/pdf/06‐3629.pdf. Accessed December 10,2008.
- Department of Health and Human Services, Centers for Medicare 241(3):397–415.
- , , , et al.Electronic alerts to prevent venous thromboembolism among hospitalized patients.N Engl J Med.2005;352(10):969–977.
- , , , et al.Electronic alerts for hospitalized high‐VTE risk patients not receiving prophylaxis: a cohort study.J Thromb Thrombolysis.2008;25(2):146–150.
- , , , et al. Improving compliance with guidelines for venous thromboembolism (VTE) prophylaxis significantly reduces VTE events. Presented at the 50th Annual Meeting of the American College of Hematology; San Francisco, CA; December 6‐9, 2008. Abstract 1288.
- .Development and implementation of a program to assess medical patients' need for venous thromboembolism prophylaxis.Am J Health Syst Pharm.2008;65(18):1755–1760.
- , , .Pharmacist‐led program to improve venous thromboembolism prophylaxis in a community hospital.Am J Health Syst Pharm.2008;65(17):1643–1647.