User login
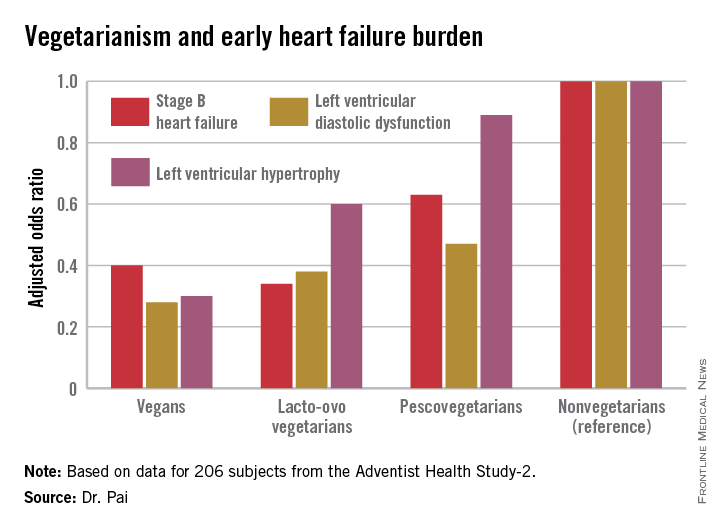
ORLANDO – Elderly individuals who consumed a vegan diet – no meat, fish, dairy, or eggs – were at an adjusted 72% lower risk of prevalent left ventricular diastolic dysfunction as well as 70% lower risk of left ventricular hypertrophy than were nonvegetarians in the Adventist Health Study-2.
The landmark Adventist Health Study-2 (AHS-2) is an ongoing observational epidemiologic study that includes 96,000 subjects. In previously reported findings from AHS-2, a vegetarian diet was associated with reduced risks of diabetes, hypertension, metabolic syndrome, overweight/obesity, all-cause mortality, and some cancers, compared with a nonvegetarian diet of similar caloric intake (Am J Clin Nutr. 2014 Jul;100[suppl 1]:353s-8s).
Because heart failure is a massive and growing problem, affecting 6 million Americans at a direct health care cost of $40 billion annually, AHS-2 investigators decided to look at the relationship between diet and heart failure, Dr. Ramdas G. Pai explained at the American Heart Association scientific sessions.
He and his coinvestigators at Loma Linda (Calif.) University brought in a random sample of 206 AHS-2 participants for a clinic visit which included a full echocardiographic assessment. The cohort had a mean age of 74 years. Echocardiography revealed that left ventricular diastolic dysfunction was present in 60% of subjects, left ventricular hypertrophy in 10%, and an increased left atrial volume index in 45%.
The study population consisted of roughly equal numbers of vegans, lacto-ovo vegetarians as defined by consumption of meat or fish less than once per month and dairy and/or eggs more than once weekly, pescovegetarians who eat fish more than once per month, and meat-eating nonvegetarians.
In a multivariate analysis adjusted for age, race, gender, body surface area, diabetes, hypertension, and history of coronary heart disease, a stepwise increase was seen in the prevalence of early stage B heart failure and its echocardiographic risk factors with increasing nonvegetarianism.
The implication is that a population shift toward a more vegetarian-oriented diet might reduce the overall burden of heart failure in the community, according to Dr. Pai.
He reported having no financial conflicts of interest regarding the AHS-2 analysis.
ORLANDO – Elderly individuals who consumed a vegan diet – no meat, fish, dairy, or eggs – were at an adjusted 72% lower risk of prevalent left ventricular diastolic dysfunction as well as 70% lower risk of left ventricular hypertrophy than were nonvegetarians in the Adventist Health Study-2.
The landmark Adventist Health Study-2 (AHS-2) is an ongoing observational epidemiologic study that includes 96,000 subjects. In previously reported findings from AHS-2, a vegetarian diet was associated with reduced risks of diabetes, hypertension, metabolic syndrome, overweight/obesity, all-cause mortality, and some cancers, compared with a nonvegetarian diet of similar caloric intake (Am J Clin Nutr. 2014 Jul;100[suppl 1]:353s-8s).
Because heart failure is a massive and growing problem, affecting 6 million Americans at a direct health care cost of $40 billion annually, AHS-2 investigators decided to look at the relationship between diet and heart failure, Dr. Ramdas G. Pai explained at the American Heart Association scientific sessions.
He and his coinvestigators at Loma Linda (Calif.) University brought in a random sample of 206 AHS-2 participants for a clinic visit which included a full echocardiographic assessment. The cohort had a mean age of 74 years. Echocardiography revealed that left ventricular diastolic dysfunction was present in 60% of subjects, left ventricular hypertrophy in 10%, and an increased left atrial volume index in 45%.
The study population consisted of roughly equal numbers of vegans, lacto-ovo vegetarians as defined by consumption of meat or fish less than once per month and dairy and/or eggs more than once weekly, pescovegetarians who eat fish more than once per month, and meat-eating nonvegetarians.
In a multivariate analysis adjusted for age, race, gender, body surface area, diabetes, hypertension, and history of coronary heart disease, a stepwise increase was seen in the prevalence of early stage B heart failure and its echocardiographic risk factors with increasing nonvegetarianism.
The implication is that a population shift toward a more vegetarian-oriented diet might reduce the overall burden of heart failure in the community, according to Dr. Pai.
He reported having no financial conflicts of interest regarding the AHS-2 analysis.
ORLANDO – Elderly individuals who consumed a vegan diet – no meat, fish, dairy, or eggs – were at an adjusted 72% lower risk of prevalent left ventricular diastolic dysfunction as well as 70% lower risk of left ventricular hypertrophy than were nonvegetarians in the Adventist Health Study-2.
The landmark Adventist Health Study-2 (AHS-2) is an ongoing observational epidemiologic study that includes 96,000 subjects. In previously reported findings from AHS-2, a vegetarian diet was associated with reduced risks of diabetes, hypertension, metabolic syndrome, overweight/obesity, all-cause mortality, and some cancers, compared with a nonvegetarian diet of similar caloric intake (Am J Clin Nutr. 2014 Jul;100[suppl 1]:353s-8s).
Because heart failure is a massive and growing problem, affecting 6 million Americans at a direct health care cost of $40 billion annually, AHS-2 investigators decided to look at the relationship between diet and heart failure, Dr. Ramdas G. Pai explained at the American Heart Association scientific sessions.
He and his coinvestigators at Loma Linda (Calif.) University brought in a random sample of 206 AHS-2 participants for a clinic visit which included a full echocardiographic assessment. The cohort had a mean age of 74 years. Echocardiography revealed that left ventricular diastolic dysfunction was present in 60% of subjects, left ventricular hypertrophy in 10%, and an increased left atrial volume index in 45%.
The study population consisted of roughly equal numbers of vegans, lacto-ovo vegetarians as defined by consumption of meat or fish less than once per month and dairy and/or eggs more than once weekly, pescovegetarians who eat fish more than once per month, and meat-eating nonvegetarians.
In a multivariate analysis adjusted for age, race, gender, body surface area, diabetes, hypertension, and history of coronary heart disease, a stepwise increase was seen in the prevalence of early stage B heart failure and its echocardiographic risk factors with increasing nonvegetarianism.
The implication is that a population shift toward a more vegetarian-oriented diet might reduce the overall burden of heart failure in the community, according to Dr. Pai.
He reported having no financial conflicts of interest regarding the AHS-2 analysis.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: The closer one gets to a vegan diet, the less likely are echocardiographic risk factors for early heart failure.
Major finding: Vegans were 60% less likely to have stage B heart failure than were nonvegetarians.
Data source: This study examined echocardiographic findings associated with early heart failure in 206 participants in the observational Adventist Health Study-2.
Disclosures: The presenter reported having no financial conflicts of interest regarding this study.