User login
Atherothrombosis triggered by plaque rupture reduces arterial blood flow, leading to myocardial ischemia and/or necrosis, in which the extent of occlusion relates to the clinical presentations of acute coronary syndrome (ACS): unstable angina (UA), non‐ST‐segment and ST‐segment elevated myocardial infarction (NSTEMI and STEMI, respectively). Although UA and NSTEMI may be indistinguishable at the time of presentation, NSTEMI is defined by myocardial necrosis and is differentiated by release of cardiac enzymes.1 In UA, the myocardial ischemia is reversible, without necrosis. Typically, STEMI results from the total occlusion of a large epicardial infarct‐related artery and is diagnosed by electrocardiography (ECG) and the release of cardiac enzymes.2 Strategies employed by emergency physicians and hospitalists to treat the spectrum of symptoms caused by ACS include pharmacotherapy and revascularization procedures. Coordination of care between these 2 groups of physicians, and appropriate handoff of patients from the ED to hospitalists, utilizing guideline‐based care pathways and treatment protocols, will ensure maximization of outcomes in patients with ACS.
TREATMENT STRATEGIES FOR ACUTE CORONARY SYNDROME
The American College of Cardiology and American Heart Association (ACC/AHA) guidelines indicate the need for rapid triage and aggressive treatment when managing patients with ACS.1, 2 Those patients with NSTEMI are quickly differentiated from those with STEMI, who are evaluated rapidly for pharmacological and/or revascularization therapy.2 Patients with UA/NSTEMI are further stratified according to their risk of death or nonfatal MI, and appropriate care pathways are instituted as indicated by their risk for adverse outcomes. These care pathways must be guideline driven to assure maximal effectiveness.
Percutaneous coronary intervention (PCI) and coronary artery bypass graft surgery (CABG) revascularization procedures have been highly successful with low complication rates in patients with ACS. Although revascularization in patients with UA/NSTEMI is determined in part by their risk stratification, those patients with STEMI are almost always candidates for PCI or CABG.
Unfortunately, vascular flow is not completely restored in many patients after undergoing revascularization, both STEMI and UA/NSTEMI. This may be attributed to microvascular damage caused by the formation of microemboli during the initial atherothrombotic event or revascularization.1, 2 Given that percutaneous catheters are incapable of restoring microvasculature patency, pharmacotherapy is the only alternative for this cohort of patients. Thus, acute antithrombotic therapies (antiplatelet agents and anticoagulants) are administered to maintain vascular flow in patients with ACS before and after revascularization. Maximization of the effectiveness of this antithrombotic therapy in the precatheterization period will decrease the occurrence of ischemia and the extent of infarction.
Patients with ACS often have multiple vulnerable plaques in addition to the culprit lesion responsible for the initial bout of ischemia. The presence of multiple vulnerable plaques increases the risk of secondary vascular events such as stroke, myocardial infarction (MI), or vascular death in patients with ACS.3, 4 Thus, ongoing anti‐inflammatory and antiplatelet therapies are needed to stabilize vulnerable plaques and prevent secondary vascular events.5 The ACC/AHA guidelines recommend sustained antiplatelet and antithrombin therapies to improve long‐term outcomes in patients with ACS.1
ASPIRIN THERAPY FOR ACUTE CORONARY SYNDROME
Aspirin effectively reduces the short‐term risk of myocardial ischemic events in patients with ACS. The RISC and ISIS‐2 studies showed a clinically relevant reduction in risk of MI or death after short durations of aspirin therapy in patients with UA (3 months) and suspected acute MI (5 weeks), respectively.6, 7 Although long‐term therapy with aspirin has not been tested among individual ACS subgroups, clinical studies have demonstrated that aspirin therapy effectively prevents MI, stroke, and vascular death in patients with prior MI or other vascular events. A meta‐analysis of 65 trials in patients with atherothrombosis showed that aspirin therapy reduces the odds of vascular events by 23% 2%.8 Moreover, aspirin has a class IA recommendation from the ACC/AHA for the management of patients with UA/NSTEMI or STEMI; in the absence of contraindications, it should be initiated as soon as possible and continued indefinitely.1, 2 On initial presentation of ACS, high‐dose aspirin is recommended (162‐325 mg), and lower doses (75‐162 mg), which minimize bleeding or gastrointestinal side effects, are indicated thereafter.1, 2
SUSTAINED ANTIPLATELET THERAPIES FORUA/NSTEMI
Clinical data have indicated that long‐term therapies may be more beneficial to patients with UA/NSTEMI than to those with STEMI. Antiplatelet therapy reduces the risk of vascular events in patients with UA/NSTEMI; benefits are noticeable soon after therapy is initiated. The sustained use of clopidogrel, an inhibitor of ADP‐dependent platelet activation, is at least as effective as aspirin in reducing long‐term vascular events in patients with atherothrombotic diseases, and the ACC/AHA recommends this agent be used when aspirin is contraindicated.1, 9
Recently, the Clopidogrel in Unstable Angina Recurrent Events (CURE) study demonstrated that the combination of clopidogrel and aspirin is superior to either agent alone in preventing vascular events in patients with UA/NSTEMI.10 Patients (N = 12,562) were randomized within 24 hours of UA/NSTEMI presentation to receive aspirin (75‐325 mg/day), an immediate loading dose of clopidogrel (300 mg) followed by once‐daily clopidogrel (75 mg), or a matching placebo for 3‐12 months.10 At the treating physicians' discretion, patients were treated with anticoagulants, revascularization procedures, or GP IIb/IIIa inhibitors after randomization. When used in combination with aspirin, clopidogrel reduced the risk of a major cardiovascular event by 20% (relative risk RR, 0.80; 95% CI, 0.72‐0.90; P < .001) compared with aspirin alone.10
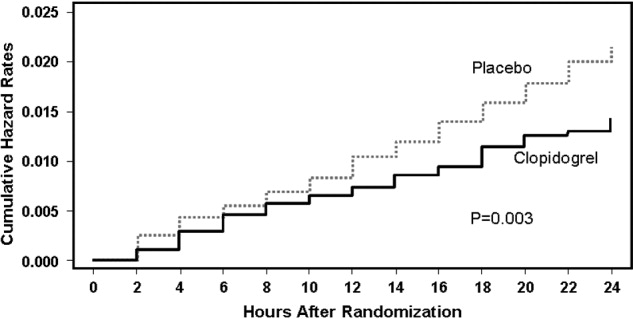
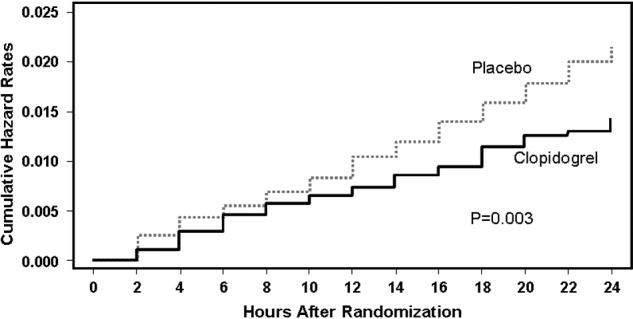
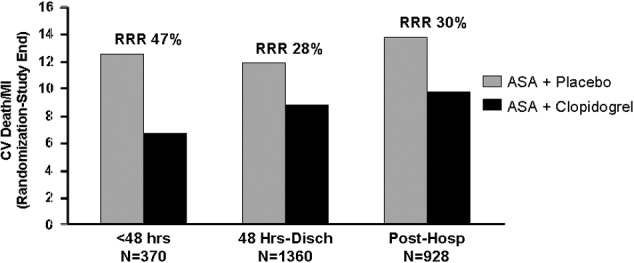
A retrospective subgroup analysis revealed that the therapeutic benefits of this drug combination increases as the risk of a vascular event increases in patients with UA/NSTEMI.11 In addition, the effects of clopidogrel and aspirin were apparent early after randomization (Fig. 1); a 34% reduction in the risk of major cardiovascular events (RR, 0.66; 95% CI, 0.51‐0.86; P < .003) was observed within 24 hours postrandomization.12 Thirty days after randomization, the relative risk reduction in the composite end point of cardiovascular death and nonfatal MI, stroke, and refractory ischemia was 17% (RR, 0.83; 95% CI, 0.73‐0.93; P < .002) for clopidogrel with aspirin.
The combination of clopidogrel and aspirin was associated with a 38% (RR, 1.38; 95% CI, 1.13‐1.67; P = .001) increase in major bleeding episodes compared with patients taking aspirin alone. Conversely, the incidence of bleeding requiring surgical intervention, hemorrhagic stroke, and fatal hemorrhage between treatment groups did not differ significantly.10 The clinical benefits of clopidogrel and aspirin outweighed the risk of life‐threatening bleeding (RR, 0.84; 95% CI, 0.76‐0.93), even when the number of deaths and the number of life‐threatening bleeds were taken into account in the efficacy‐safety analysis.13 As a result, the ACC/AHA guidelines for the management of patients with UA/NSTEMI recommend that clopidogrel and aspirin should be administered to hospitalized patients as soon as possible and should be continued for 1 month and up to 12 months after the initial presentation of symptoms.1 The new ACC/AHA guidelines recommend upstream clopidogrel as a class IA treatment for UA/non‐ST‐elevation MI in patients who are managed either invasively (catheterization within 6‐24 hours) or conservatively (selectively invasive medical management, followed by catheterization if needed). This latter recommendation is much stronger than the prior guidelines and illustrates the importance of antiplatelet therapy as a part of medical management for intermediate‐ to high‐risk ACS.
ANTIPLATELET THERAPIES WITH REVASCULARIZATION PROCEDURES IN UA/NSTEMI
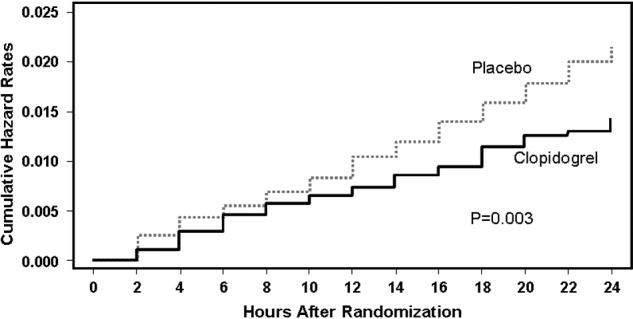
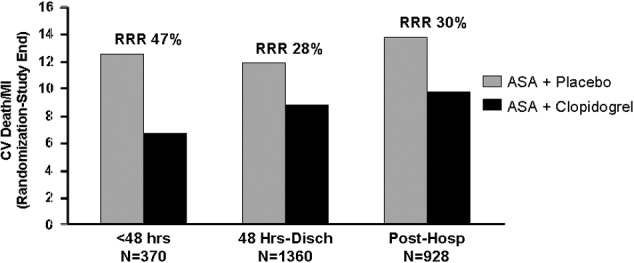
The efficacy of clopidogrel and aspirin has been examined in patients enrolled in the CURE study who underwent revascularization procedures (eg, PCI, CABG). These agents reduced the relative risk of cardiovascular death or nonfatal MI by 31% (RR, 0.69; 95% CI, 0.54‐0.87; P = .002) in patients who underwent PCI.14 Subgroup analysis of PCI timing relative to randomization showed that the risk of vascular events increased with time to revascularization. However, this relationship was not evident in patients treated with aspirin alone (Fig. 2).14 There was no significant difference in the incidence of major bleeding (RR, 1.2; 95% CI, 0.70‐1.78; P = .64) between the treatment groups from PCI to follow‐up.14, 15 Similar results have been reported elsewhere.16 As a result, ACC/AHA guidelines recommend the early administration of clopidogrel and aspirin to patients undergoing planned PCI, and should be continued up to 12 months following the procedure, unless it is contraindicated.1
Clopidogrel and aspirin also reduced the risk of vascular death by 11% (RR, 0.89; 95% CI, 0.71‐1.11) in patients who underwent CABG.13 Study medications were stopped prior to the procedure. Major bleeding was not observed in patients who stopped medication at least 5 days prior to surgery and did not differ significantly from those who stopped therapy less than 5 days before CABG.13 Thus, the ACC/AHA recommends withholding clopidogrel therapy for 5‐7 days prior to elective CABG.1
Platelet glycoprotein (GP) IIb/IIIa inhibitors are another class of antiplatelet therapy that can be beneficial to patients with UA/NSTEMI undergoing PCI. Analysis of the CAPTURE, PURSUIT, and PRISM‐PLUS trials of the GP IIb/IIIa inhibitors abciximab, eptifibatide, and tirofiban, respectively, showed they effectively reduce the rates of death and/or MI (odds ratio [OR], 0.66; 95% CI, 0.54‐0.81) in patients with UA/STEMI prior to PCI, which was more pronounced (OR, 0.59; 95% CI, 0.44‐0.81) when outcomes were measured 48 hours after revascularization.17
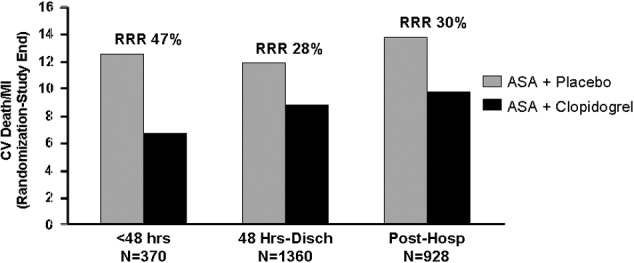
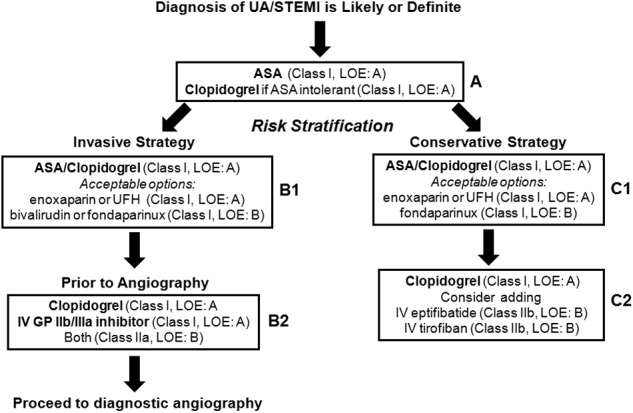
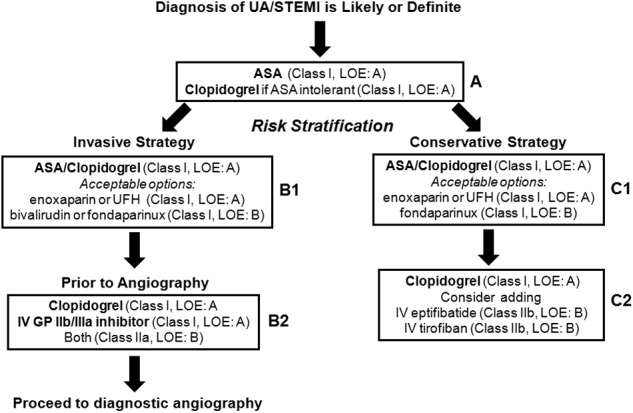
The ISAR‐REACT 2 study examined the efficacy of abciximab with clopidogrel and aspirin in patients with NSTEMI prior to PCI.18 The primary end point was a composite of death, MI, and secondary urgent target revascularization 30 days after randomization. The addition of abciximab to 600 mg of the clopidogrel loading dose and aspirin reduced the risk of major adverse cardiovascular events by 25% (RR, 0.75; 95% CI, 0.58‐0.97; P = .03) 30 days after the initiation of therapy. However, subgroup analysis revealed that this therapeutic benefit was confined to patients with elevated troponin levels.18 The ACC/AHA also recommends the concomitant administration of GP IIb/IIIa inhibitors to patients receiving heparin, aspirin, and clopidogrel and undergoing planned PCI.1 The guideline recommendation is for either clopidogrel or a GP IIb/IIIa inhibitor in the invasive pathway (class IA), but both are recommended in patients with elevated troponin, recurrent ischemia, or delay to catheterization (class IIaB). This triple antiplatelet therapy is considered advantageous in the highest=risk NSTEMI patients. The short‐term and long‐term benefits of antiplatelet therapies are consistent across the UA/NSTEMI‐risk spectrum and galvanize the ACC/AHA recommendations for antithrombotic therapy in patients with UA/NSTEMI (Fig. 3).1
ANTIPLATELET THERAPIES FOR STEMI
The ACC/AHA has made several recommendations regarding the administration of clopidogrel in patients with STEMI. Clopidogrel should be administered to patients with contraindications to aspirin. After placement of a bare metal or drug‐eluting stent, this agent should be administered at least 1 month and less than 12 months after surgery, respectively. It should also be withheld at least 5‐7 days prior to CABG.2 These guidelines are largely based on clinical trials in patients with UA/STEMI or ACS.9, 15 Fortunately, several more recent studies have examined the use of antiplatelet therapy in patients with STEMI.
In the Clopidogrel as Adjunctive Reperfusion TherapyThrombolysis in Myocardial Infarction (CLARITY‐TIMI) 28 study, 3491 patients with STEMI were randomized to receive clopidogrel (300 mg loading dose, then 75 mg/day) or placebo. Patients were also treated with a fibrinolytic agent, aspirin, and unfractionated heparin and underwent angiography 48‐192 hours after randomization. Clopidogrel reduced the risk of detecting an occluded infarct‐related artery by angiography or recurrent MI/death prior to angiography by 36% (OR, 0.64; 95% CI, 0.53‐0.76; P < .001) compared with placebo.19 It also reduced the risk of major adverse cardiovascular events 30 days after randomization by 20% (OR, 0.80; 95% CI, 0.65‐0.97; P = .03) compared with placebo, with no significant difference in the risk of bleeding between the treatment groups.
The PCI‐CLARITY study examined the efficacy of clopidogrel in patients undergoing PCI during the CLARITY‐TIMI 28 trial. Clopidogrel reduced the rate of major adverse cardiovascular events by 46% (OR, 0.54; 95% CI, 0.35‐0.85; P = .008) after PCI and 30 days after randomization, with no excess in major bleeding.20 Although the use of this agent along with contemporary reperfusion therapies in patients with STEMI is supported, further research into the sustained use of clopidogrel in STEMI is needed.
CONCLUSIONS
Patients with ACS require aggressive diagnosis and acute treatment. However, long‐term therapies are also needed to improve outcomes. Antiplatelet therapies are a key component of the treatment of ACS. The benefits of aspirin and clopidogrel combination therapy are evident early, and their sustained use improves the outcome of patients who receive medical therapy and/or revascularization procedures. Early initiation of antiplatelet therapy in patients with ACS is best accomplished with care pathways or ACS protocols that are guideline driven. Initiation of these protocols in the ED, with appropriate handoff to hospitalists, will ensure maximization of antiplatelet therapy for patients throughout the precatheterization medical management period. Although antiplatelet agents may be associated with an increased risk of bleeding in some patients, these risks can be minimized and are outweighed by the benefits of clopidogrel and aspirin.
- ,,, et al.ACC/AHA guidelines for the management of patients with unstable angina/non‐ST‐segment elevation myocardial infarction: executive summary.J Am Coll Cardiol.2007;50:e1–e157. Available at: http://www.acc.org.
- ,,, et al.ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction.Circulation.2004;110:82–292.
- Antiplatelet Trialists' Collaboration.Collaborative overview of randomized trials of antiplatelet therapy. Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients.BMJ.1994;308:81–106.
- ,,, et al.One‐year cardiovascular event rates in outpatients with atherothrombosis.JAMA.2007;297:1197–1206.
- ,,, et al.Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association.Circulation.2006;113:873–823.
- The RISC Group.Risk of myocardial infarction and death during treatment with low dose aspirin and intravenous heparin in men with unstable coronary artery disease.Lancet.1990;336:827–830.
- ISIS‐2 Collaborative Group.Randomized trial of intravenous streptokinase, oral aspirin, both or neither among 17,187 cases of suspected acute myocardial infarction: ISIS‐2.Lancet.1988;2:349–360.
- Antithrombotic Trialists' Collaboration.Collaborative meta‐analysis of randomized trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients.BMJ.2002;324:71–86.
- CAPRIE steering committee.A randomized, blinded, trial of clopidogrel versus aspirin in patients at risk of ischemic events (CAPRIE).Lancet.1996;348:1329–1339.
- CURE Trial Investigators.Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST‐segment elevation.N Engl J Med.2001;345:494–502.
- ,,, et al.Benefit of clopidogrel in patients with acute coronary syndromes without ST‐segment elevation in various risk groups.Circulation.2002;106:1622–1626.
- ,,, et al.Early and late effects of clopidogrel in patients with acute coronary syndromes.Circulation.2003;107:966–972.
- ,,, et al.Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non‐ST‐elevation acute coronary syndrome: The clopidogrel in unstable angina to prevent recurrent ischemic events (CURE) trial.Circulation.2004;110:1202–1208.
- ,,, et al.Benefit of clopidogrel according to timing of percutaneous coronary intervention in patients with acute coronary syndromes: Further results from the clopidogrel in unstable angina to prevent recurrent events (CURE) study.Am Heart J.2005;150:1177–1184.
- ,,, et al.Effects of pretreatment with clopidogrel and aspirin followed by long‐term therapy in patients undergoing percutaneous coronary intervention: the PCI‐CURE study.Lancet.2001;358:527–533.
- ,,, et al.Early and sustained dual oral antiplatelet therapy following percutaneous intervention. A randomized trial.JAMA.2002;288:2411–2420.
- ,,,,,.Platelet glycoprotein IIb/IIIa receptor inhibition in non‐ST‐elevation acute coronary syndromes: early benefit during medical treatment only, with additional protection during percutaneous coronary intervention.Circulation.1999;100:2045–2048.
- ,,, et al.Abciximab in patients with acute coronary syndromes undergoing percutaneous coronary intervention after clopidogrel pretreatment. The ISAR‐REACT2 randomized trial.JAMA.2006;295:1531–1538.
- ,,, et al.Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST‐segment elevation.N Engl J Med.2005;352:1179–1189.
- ,,, et al.Effect of clopidogrel pretreatment before percutaneous coronary intervention in patients with ST‐elevation myocardial infarction treated with fibrinolytics. The PCI‐CLARITY study.JAMA.2005;294:1224–1232.
Atherothrombosis triggered by plaque rupture reduces arterial blood flow, leading to myocardial ischemia and/or necrosis, in which the extent of occlusion relates to the clinical presentations of acute coronary syndrome (ACS): unstable angina (UA), non‐ST‐segment and ST‐segment elevated myocardial infarction (NSTEMI and STEMI, respectively). Although UA and NSTEMI may be indistinguishable at the time of presentation, NSTEMI is defined by myocardial necrosis and is differentiated by release of cardiac enzymes.1 In UA, the myocardial ischemia is reversible, without necrosis. Typically, STEMI results from the total occlusion of a large epicardial infarct‐related artery and is diagnosed by electrocardiography (ECG) and the release of cardiac enzymes.2 Strategies employed by emergency physicians and hospitalists to treat the spectrum of symptoms caused by ACS include pharmacotherapy and revascularization procedures. Coordination of care between these 2 groups of physicians, and appropriate handoff of patients from the ED to hospitalists, utilizing guideline‐based care pathways and treatment protocols, will ensure maximization of outcomes in patients with ACS.
TREATMENT STRATEGIES FOR ACUTE CORONARY SYNDROME
The American College of Cardiology and American Heart Association (ACC/AHA) guidelines indicate the need for rapid triage and aggressive treatment when managing patients with ACS.1, 2 Those patients with NSTEMI are quickly differentiated from those with STEMI, who are evaluated rapidly for pharmacological and/or revascularization therapy.2 Patients with UA/NSTEMI are further stratified according to their risk of death or nonfatal MI, and appropriate care pathways are instituted as indicated by their risk for adverse outcomes. These care pathways must be guideline driven to assure maximal effectiveness.
Percutaneous coronary intervention (PCI) and coronary artery bypass graft surgery (CABG) revascularization procedures have been highly successful with low complication rates in patients with ACS. Although revascularization in patients with UA/NSTEMI is determined in part by their risk stratification, those patients with STEMI are almost always candidates for PCI or CABG.
Unfortunately, vascular flow is not completely restored in many patients after undergoing revascularization, both STEMI and UA/NSTEMI. This may be attributed to microvascular damage caused by the formation of microemboli during the initial atherothrombotic event or revascularization.1, 2 Given that percutaneous catheters are incapable of restoring microvasculature patency, pharmacotherapy is the only alternative for this cohort of patients. Thus, acute antithrombotic therapies (antiplatelet agents and anticoagulants) are administered to maintain vascular flow in patients with ACS before and after revascularization. Maximization of the effectiveness of this antithrombotic therapy in the precatheterization period will decrease the occurrence of ischemia and the extent of infarction.
Patients with ACS often have multiple vulnerable plaques in addition to the culprit lesion responsible for the initial bout of ischemia. The presence of multiple vulnerable plaques increases the risk of secondary vascular events such as stroke, myocardial infarction (MI), or vascular death in patients with ACS.3, 4 Thus, ongoing anti‐inflammatory and antiplatelet therapies are needed to stabilize vulnerable plaques and prevent secondary vascular events.5 The ACC/AHA guidelines recommend sustained antiplatelet and antithrombin therapies to improve long‐term outcomes in patients with ACS.1
ASPIRIN THERAPY FOR ACUTE CORONARY SYNDROME
Aspirin effectively reduces the short‐term risk of myocardial ischemic events in patients with ACS. The RISC and ISIS‐2 studies showed a clinically relevant reduction in risk of MI or death after short durations of aspirin therapy in patients with UA (3 months) and suspected acute MI (5 weeks), respectively.6, 7 Although long‐term therapy with aspirin has not been tested among individual ACS subgroups, clinical studies have demonstrated that aspirin therapy effectively prevents MI, stroke, and vascular death in patients with prior MI or other vascular events. A meta‐analysis of 65 trials in patients with atherothrombosis showed that aspirin therapy reduces the odds of vascular events by 23% 2%.8 Moreover, aspirin has a class IA recommendation from the ACC/AHA for the management of patients with UA/NSTEMI or STEMI; in the absence of contraindications, it should be initiated as soon as possible and continued indefinitely.1, 2 On initial presentation of ACS, high‐dose aspirin is recommended (162‐325 mg), and lower doses (75‐162 mg), which minimize bleeding or gastrointestinal side effects, are indicated thereafter.1, 2
SUSTAINED ANTIPLATELET THERAPIES FORUA/NSTEMI
Clinical data have indicated that long‐term therapies may be more beneficial to patients with UA/NSTEMI than to those with STEMI. Antiplatelet therapy reduces the risk of vascular events in patients with UA/NSTEMI; benefits are noticeable soon after therapy is initiated. The sustained use of clopidogrel, an inhibitor of ADP‐dependent platelet activation, is at least as effective as aspirin in reducing long‐term vascular events in patients with atherothrombotic diseases, and the ACC/AHA recommends this agent be used when aspirin is contraindicated.1, 9
Recently, the Clopidogrel in Unstable Angina Recurrent Events (CURE) study demonstrated that the combination of clopidogrel and aspirin is superior to either agent alone in preventing vascular events in patients with UA/NSTEMI.10 Patients (N = 12,562) were randomized within 24 hours of UA/NSTEMI presentation to receive aspirin (75‐325 mg/day), an immediate loading dose of clopidogrel (300 mg) followed by once‐daily clopidogrel (75 mg), or a matching placebo for 3‐12 months.10 At the treating physicians' discretion, patients were treated with anticoagulants, revascularization procedures, or GP IIb/IIIa inhibitors after randomization. When used in combination with aspirin, clopidogrel reduced the risk of a major cardiovascular event by 20% (relative risk RR, 0.80; 95% CI, 0.72‐0.90; P < .001) compared with aspirin alone.10
A retrospective subgroup analysis revealed that the therapeutic benefits of this drug combination increases as the risk of a vascular event increases in patients with UA/NSTEMI.11 In addition, the effects of clopidogrel and aspirin were apparent early after randomization (Fig. 1); a 34% reduction in the risk of major cardiovascular events (RR, 0.66; 95% CI, 0.51‐0.86; P < .003) was observed within 24 hours postrandomization.12 Thirty days after randomization, the relative risk reduction in the composite end point of cardiovascular death and nonfatal MI, stroke, and refractory ischemia was 17% (RR, 0.83; 95% CI, 0.73‐0.93; P < .002) for clopidogrel with aspirin.
The combination of clopidogrel and aspirin was associated with a 38% (RR, 1.38; 95% CI, 1.13‐1.67; P = .001) increase in major bleeding episodes compared with patients taking aspirin alone. Conversely, the incidence of bleeding requiring surgical intervention, hemorrhagic stroke, and fatal hemorrhage between treatment groups did not differ significantly.10 The clinical benefits of clopidogrel and aspirin outweighed the risk of life‐threatening bleeding (RR, 0.84; 95% CI, 0.76‐0.93), even when the number of deaths and the number of life‐threatening bleeds were taken into account in the efficacy‐safety analysis.13 As a result, the ACC/AHA guidelines for the management of patients with UA/NSTEMI recommend that clopidogrel and aspirin should be administered to hospitalized patients as soon as possible and should be continued for 1 month and up to 12 months after the initial presentation of symptoms.1 The new ACC/AHA guidelines recommend upstream clopidogrel as a class IA treatment for UA/non‐ST‐elevation MI in patients who are managed either invasively (catheterization within 6‐24 hours) or conservatively (selectively invasive medical management, followed by catheterization if needed). This latter recommendation is much stronger than the prior guidelines and illustrates the importance of antiplatelet therapy as a part of medical management for intermediate‐ to high‐risk ACS.
ANTIPLATELET THERAPIES WITH REVASCULARIZATION PROCEDURES IN UA/NSTEMI
The efficacy of clopidogrel and aspirin has been examined in patients enrolled in the CURE study who underwent revascularization procedures (eg, PCI, CABG). These agents reduced the relative risk of cardiovascular death or nonfatal MI by 31% (RR, 0.69; 95% CI, 0.54‐0.87; P = .002) in patients who underwent PCI.14 Subgroup analysis of PCI timing relative to randomization showed that the risk of vascular events increased with time to revascularization. However, this relationship was not evident in patients treated with aspirin alone (Fig. 2).14 There was no significant difference in the incidence of major bleeding (RR, 1.2; 95% CI, 0.70‐1.78; P = .64) between the treatment groups from PCI to follow‐up.14, 15 Similar results have been reported elsewhere.16 As a result, ACC/AHA guidelines recommend the early administration of clopidogrel and aspirin to patients undergoing planned PCI, and should be continued up to 12 months following the procedure, unless it is contraindicated.1
Clopidogrel and aspirin also reduced the risk of vascular death by 11% (RR, 0.89; 95% CI, 0.71‐1.11) in patients who underwent CABG.13 Study medications were stopped prior to the procedure. Major bleeding was not observed in patients who stopped medication at least 5 days prior to surgery and did not differ significantly from those who stopped therapy less than 5 days before CABG.13 Thus, the ACC/AHA recommends withholding clopidogrel therapy for 5‐7 days prior to elective CABG.1
Platelet glycoprotein (GP) IIb/IIIa inhibitors are another class of antiplatelet therapy that can be beneficial to patients with UA/NSTEMI undergoing PCI. Analysis of the CAPTURE, PURSUIT, and PRISM‐PLUS trials of the GP IIb/IIIa inhibitors abciximab, eptifibatide, and tirofiban, respectively, showed they effectively reduce the rates of death and/or MI (odds ratio [OR], 0.66; 95% CI, 0.54‐0.81) in patients with UA/STEMI prior to PCI, which was more pronounced (OR, 0.59; 95% CI, 0.44‐0.81) when outcomes were measured 48 hours after revascularization.17
The ISAR‐REACT 2 study examined the efficacy of abciximab with clopidogrel and aspirin in patients with NSTEMI prior to PCI.18 The primary end point was a composite of death, MI, and secondary urgent target revascularization 30 days after randomization. The addition of abciximab to 600 mg of the clopidogrel loading dose and aspirin reduced the risk of major adverse cardiovascular events by 25% (RR, 0.75; 95% CI, 0.58‐0.97; P = .03) 30 days after the initiation of therapy. However, subgroup analysis revealed that this therapeutic benefit was confined to patients with elevated troponin levels.18 The ACC/AHA also recommends the concomitant administration of GP IIb/IIIa inhibitors to patients receiving heparin, aspirin, and clopidogrel and undergoing planned PCI.1 The guideline recommendation is for either clopidogrel or a GP IIb/IIIa inhibitor in the invasive pathway (class IA), but both are recommended in patients with elevated troponin, recurrent ischemia, or delay to catheterization (class IIaB). This triple antiplatelet therapy is considered advantageous in the highest=risk NSTEMI patients. The short‐term and long‐term benefits of antiplatelet therapies are consistent across the UA/NSTEMI‐risk spectrum and galvanize the ACC/AHA recommendations for antithrombotic therapy in patients with UA/NSTEMI (Fig. 3).1
ANTIPLATELET THERAPIES FOR STEMI
The ACC/AHA has made several recommendations regarding the administration of clopidogrel in patients with STEMI. Clopidogrel should be administered to patients with contraindications to aspirin. After placement of a bare metal or drug‐eluting stent, this agent should be administered at least 1 month and less than 12 months after surgery, respectively. It should also be withheld at least 5‐7 days prior to CABG.2 These guidelines are largely based on clinical trials in patients with UA/STEMI or ACS.9, 15 Fortunately, several more recent studies have examined the use of antiplatelet therapy in patients with STEMI.
In the Clopidogrel as Adjunctive Reperfusion TherapyThrombolysis in Myocardial Infarction (CLARITY‐TIMI) 28 study, 3491 patients with STEMI were randomized to receive clopidogrel (300 mg loading dose, then 75 mg/day) or placebo. Patients were also treated with a fibrinolytic agent, aspirin, and unfractionated heparin and underwent angiography 48‐192 hours after randomization. Clopidogrel reduced the risk of detecting an occluded infarct‐related artery by angiography or recurrent MI/death prior to angiography by 36% (OR, 0.64; 95% CI, 0.53‐0.76; P < .001) compared with placebo.19 It also reduced the risk of major adverse cardiovascular events 30 days after randomization by 20% (OR, 0.80; 95% CI, 0.65‐0.97; P = .03) compared with placebo, with no significant difference in the risk of bleeding between the treatment groups.
The PCI‐CLARITY study examined the efficacy of clopidogrel in patients undergoing PCI during the CLARITY‐TIMI 28 trial. Clopidogrel reduced the rate of major adverse cardiovascular events by 46% (OR, 0.54; 95% CI, 0.35‐0.85; P = .008) after PCI and 30 days after randomization, with no excess in major bleeding.20 Although the use of this agent along with contemporary reperfusion therapies in patients with STEMI is supported, further research into the sustained use of clopidogrel in STEMI is needed.
CONCLUSIONS
Patients with ACS require aggressive diagnosis and acute treatment. However, long‐term therapies are also needed to improve outcomes. Antiplatelet therapies are a key component of the treatment of ACS. The benefits of aspirin and clopidogrel combination therapy are evident early, and their sustained use improves the outcome of patients who receive medical therapy and/or revascularization procedures. Early initiation of antiplatelet therapy in patients with ACS is best accomplished with care pathways or ACS protocols that are guideline driven. Initiation of these protocols in the ED, with appropriate handoff to hospitalists, will ensure maximization of antiplatelet therapy for patients throughout the precatheterization medical management period. Although antiplatelet agents may be associated with an increased risk of bleeding in some patients, these risks can be minimized and are outweighed by the benefits of clopidogrel and aspirin.
Atherothrombosis triggered by plaque rupture reduces arterial blood flow, leading to myocardial ischemia and/or necrosis, in which the extent of occlusion relates to the clinical presentations of acute coronary syndrome (ACS): unstable angina (UA), non‐ST‐segment and ST‐segment elevated myocardial infarction (NSTEMI and STEMI, respectively). Although UA and NSTEMI may be indistinguishable at the time of presentation, NSTEMI is defined by myocardial necrosis and is differentiated by release of cardiac enzymes.1 In UA, the myocardial ischemia is reversible, without necrosis. Typically, STEMI results from the total occlusion of a large epicardial infarct‐related artery and is diagnosed by electrocardiography (ECG) and the release of cardiac enzymes.2 Strategies employed by emergency physicians and hospitalists to treat the spectrum of symptoms caused by ACS include pharmacotherapy and revascularization procedures. Coordination of care between these 2 groups of physicians, and appropriate handoff of patients from the ED to hospitalists, utilizing guideline‐based care pathways and treatment protocols, will ensure maximization of outcomes in patients with ACS.
TREATMENT STRATEGIES FOR ACUTE CORONARY SYNDROME
The American College of Cardiology and American Heart Association (ACC/AHA) guidelines indicate the need for rapid triage and aggressive treatment when managing patients with ACS.1, 2 Those patients with NSTEMI are quickly differentiated from those with STEMI, who are evaluated rapidly for pharmacological and/or revascularization therapy.2 Patients with UA/NSTEMI are further stratified according to their risk of death or nonfatal MI, and appropriate care pathways are instituted as indicated by their risk for adverse outcomes. These care pathways must be guideline driven to assure maximal effectiveness.
Percutaneous coronary intervention (PCI) and coronary artery bypass graft surgery (CABG) revascularization procedures have been highly successful with low complication rates in patients with ACS. Although revascularization in patients with UA/NSTEMI is determined in part by their risk stratification, those patients with STEMI are almost always candidates for PCI or CABG.
Unfortunately, vascular flow is not completely restored in many patients after undergoing revascularization, both STEMI and UA/NSTEMI. This may be attributed to microvascular damage caused by the formation of microemboli during the initial atherothrombotic event or revascularization.1, 2 Given that percutaneous catheters are incapable of restoring microvasculature patency, pharmacotherapy is the only alternative for this cohort of patients. Thus, acute antithrombotic therapies (antiplatelet agents and anticoagulants) are administered to maintain vascular flow in patients with ACS before and after revascularization. Maximization of the effectiveness of this antithrombotic therapy in the precatheterization period will decrease the occurrence of ischemia and the extent of infarction.
Patients with ACS often have multiple vulnerable plaques in addition to the culprit lesion responsible for the initial bout of ischemia. The presence of multiple vulnerable plaques increases the risk of secondary vascular events such as stroke, myocardial infarction (MI), or vascular death in patients with ACS.3, 4 Thus, ongoing anti‐inflammatory and antiplatelet therapies are needed to stabilize vulnerable plaques and prevent secondary vascular events.5 The ACC/AHA guidelines recommend sustained antiplatelet and antithrombin therapies to improve long‐term outcomes in patients with ACS.1
ASPIRIN THERAPY FOR ACUTE CORONARY SYNDROME
Aspirin effectively reduces the short‐term risk of myocardial ischemic events in patients with ACS. The RISC and ISIS‐2 studies showed a clinically relevant reduction in risk of MI or death after short durations of aspirin therapy in patients with UA (3 months) and suspected acute MI (5 weeks), respectively.6, 7 Although long‐term therapy with aspirin has not been tested among individual ACS subgroups, clinical studies have demonstrated that aspirin therapy effectively prevents MI, stroke, and vascular death in patients with prior MI or other vascular events. A meta‐analysis of 65 trials in patients with atherothrombosis showed that aspirin therapy reduces the odds of vascular events by 23% 2%.8 Moreover, aspirin has a class IA recommendation from the ACC/AHA for the management of patients with UA/NSTEMI or STEMI; in the absence of contraindications, it should be initiated as soon as possible and continued indefinitely.1, 2 On initial presentation of ACS, high‐dose aspirin is recommended (162‐325 mg), and lower doses (75‐162 mg), which minimize bleeding or gastrointestinal side effects, are indicated thereafter.1, 2
SUSTAINED ANTIPLATELET THERAPIES FORUA/NSTEMI
Clinical data have indicated that long‐term therapies may be more beneficial to patients with UA/NSTEMI than to those with STEMI. Antiplatelet therapy reduces the risk of vascular events in patients with UA/NSTEMI; benefits are noticeable soon after therapy is initiated. The sustained use of clopidogrel, an inhibitor of ADP‐dependent platelet activation, is at least as effective as aspirin in reducing long‐term vascular events in patients with atherothrombotic diseases, and the ACC/AHA recommends this agent be used when aspirin is contraindicated.1, 9
Recently, the Clopidogrel in Unstable Angina Recurrent Events (CURE) study demonstrated that the combination of clopidogrel and aspirin is superior to either agent alone in preventing vascular events in patients with UA/NSTEMI.10 Patients (N = 12,562) were randomized within 24 hours of UA/NSTEMI presentation to receive aspirin (75‐325 mg/day), an immediate loading dose of clopidogrel (300 mg) followed by once‐daily clopidogrel (75 mg), or a matching placebo for 3‐12 months.10 At the treating physicians' discretion, patients were treated with anticoagulants, revascularization procedures, or GP IIb/IIIa inhibitors after randomization. When used in combination with aspirin, clopidogrel reduced the risk of a major cardiovascular event by 20% (relative risk RR, 0.80; 95% CI, 0.72‐0.90; P < .001) compared with aspirin alone.10
A retrospective subgroup analysis revealed that the therapeutic benefits of this drug combination increases as the risk of a vascular event increases in patients with UA/NSTEMI.11 In addition, the effects of clopidogrel and aspirin were apparent early after randomization (Fig. 1); a 34% reduction in the risk of major cardiovascular events (RR, 0.66; 95% CI, 0.51‐0.86; P < .003) was observed within 24 hours postrandomization.12 Thirty days after randomization, the relative risk reduction in the composite end point of cardiovascular death and nonfatal MI, stroke, and refractory ischemia was 17% (RR, 0.83; 95% CI, 0.73‐0.93; P < .002) for clopidogrel with aspirin.
The combination of clopidogrel and aspirin was associated with a 38% (RR, 1.38; 95% CI, 1.13‐1.67; P = .001) increase in major bleeding episodes compared with patients taking aspirin alone. Conversely, the incidence of bleeding requiring surgical intervention, hemorrhagic stroke, and fatal hemorrhage between treatment groups did not differ significantly.10 The clinical benefits of clopidogrel and aspirin outweighed the risk of life‐threatening bleeding (RR, 0.84; 95% CI, 0.76‐0.93), even when the number of deaths and the number of life‐threatening bleeds were taken into account in the efficacy‐safety analysis.13 As a result, the ACC/AHA guidelines for the management of patients with UA/NSTEMI recommend that clopidogrel and aspirin should be administered to hospitalized patients as soon as possible and should be continued for 1 month and up to 12 months after the initial presentation of symptoms.1 The new ACC/AHA guidelines recommend upstream clopidogrel as a class IA treatment for UA/non‐ST‐elevation MI in patients who are managed either invasively (catheterization within 6‐24 hours) or conservatively (selectively invasive medical management, followed by catheterization if needed). This latter recommendation is much stronger than the prior guidelines and illustrates the importance of antiplatelet therapy as a part of medical management for intermediate‐ to high‐risk ACS.
ANTIPLATELET THERAPIES WITH REVASCULARIZATION PROCEDURES IN UA/NSTEMI
The efficacy of clopidogrel and aspirin has been examined in patients enrolled in the CURE study who underwent revascularization procedures (eg, PCI, CABG). These agents reduced the relative risk of cardiovascular death or nonfatal MI by 31% (RR, 0.69; 95% CI, 0.54‐0.87; P = .002) in patients who underwent PCI.14 Subgroup analysis of PCI timing relative to randomization showed that the risk of vascular events increased with time to revascularization. However, this relationship was not evident in patients treated with aspirin alone (Fig. 2).14 There was no significant difference in the incidence of major bleeding (RR, 1.2; 95% CI, 0.70‐1.78; P = .64) between the treatment groups from PCI to follow‐up.14, 15 Similar results have been reported elsewhere.16 As a result, ACC/AHA guidelines recommend the early administration of clopidogrel and aspirin to patients undergoing planned PCI, and should be continued up to 12 months following the procedure, unless it is contraindicated.1
Clopidogrel and aspirin also reduced the risk of vascular death by 11% (RR, 0.89; 95% CI, 0.71‐1.11) in patients who underwent CABG.13 Study medications were stopped prior to the procedure. Major bleeding was not observed in patients who stopped medication at least 5 days prior to surgery and did not differ significantly from those who stopped therapy less than 5 days before CABG.13 Thus, the ACC/AHA recommends withholding clopidogrel therapy for 5‐7 days prior to elective CABG.1
Platelet glycoprotein (GP) IIb/IIIa inhibitors are another class of antiplatelet therapy that can be beneficial to patients with UA/NSTEMI undergoing PCI. Analysis of the CAPTURE, PURSUIT, and PRISM‐PLUS trials of the GP IIb/IIIa inhibitors abciximab, eptifibatide, and tirofiban, respectively, showed they effectively reduce the rates of death and/or MI (odds ratio [OR], 0.66; 95% CI, 0.54‐0.81) in patients with UA/STEMI prior to PCI, which was more pronounced (OR, 0.59; 95% CI, 0.44‐0.81) when outcomes were measured 48 hours after revascularization.17
The ISAR‐REACT 2 study examined the efficacy of abciximab with clopidogrel and aspirin in patients with NSTEMI prior to PCI.18 The primary end point was a composite of death, MI, and secondary urgent target revascularization 30 days after randomization. The addition of abciximab to 600 mg of the clopidogrel loading dose and aspirin reduced the risk of major adverse cardiovascular events by 25% (RR, 0.75; 95% CI, 0.58‐0.97; P = .03) 30 days after the initiation of therapy. However, subgroup analysis revealed that this therapeutic benefit was confined to patients with elevated troponin levels.18 The ACC/AHA also recommends the concomitant administration of GP IIb/IIIa inhibitors to patients receiving heparin, aspirin, and clopidogrel and undergoing planned PCI.1 The guideline recommendation is for either clopidogrel or a GP IIb/IIIa inhibitor in the invasive pathway (class IA), but both are recommended in patients with elevated troponin, recurrent ischemia, or delay to catheterization (class IIaB). This triple antiplatelet therapy is considered advantageous in the highest=risk NSTEMI patients. The short‐term and long‐term benefits of antiplatelet therapies are consistent across the UA/NSTEMI‐risk spectrum and galvanize the ACC/AHA recommendations for antithrombotic therapy in patients with UA/NSTEMI (Fig. 3).1
ANTIPLATELET THERAPIES FOR STEMI
The ACC/AHA has made several recommendations regarding the administration of clopidogrel in patients with STEMI. Clopidogrel should be administered to patients with contraindications to aspirin. After placement of a bare metal or drug‐eluting stent, this agent should be administered at least 1 month and less than 12 months after surgery, respectively. It should also be withheld at least 5‐7 days prior to CABG.2 These guidelines are largely based on clinical trials in patients with UA/STEMI or ACS.9, 15 Fortunately, several more recent studies have examined the use of antiplatelet therapy in patients with STEMI.
In the Clopidogrel as Adjunctive Reperfusion TherapyThrombolysis in Myocardial Infarction (CLARITY‐TIMI) 28 study, 3491 patients with STEMI were randomized to receive clopidogrel (300 mg loading dose, then 75 mg/day) or placebo. Patients were also treated with a fibrinolytic agent, aspirin, and unfractionated heparin and underwent angiography 48‐192 hours after randomization. Clopidogrel reduced the risk of detecting an occluded infarct‐related artery by angiography or recurrent MI/death prior to angiography by 36% (OR, 0.64; 95% CI, 0.53‐0.76; P < .001) compared with placebo.19 It also reduced the risk of major adverse cardiovascular events 30 days after randomization by 20% (OR, 0.80; 95% CI, 0.65‐0.97; P = .03) compared with placebo, with no significant difference in the risk of bleeding between the treatment groups.
The PCI‐CLARITY study examined the efficacy of clopidogrel in patients undergoing PCI during the CLARITY‐TIMI 28 trial. Clopidogrel reduced the rate of major adverse cardiovascular events by 46% (OR, 0.54; 95% CI, 0.35‐0.85; P = .008) after PCI and 30 days after randomization, with no excess in major bleeding.20 Although the use of this agent along with contemporary reperfusion therapies in patients with STEMI is supported, further research into the sustained use of clopidogrel in STEMI is needed.
CONCLUSIONS
Patients with ACS require aggressive diagnosis and acute treatment. However, long‐term therapies are also needed to improve outcomes. Antiplatelet therapies are a key component of the treatment of ACS. The benefits of aspirin and clopidogrel combination therapy are evident early, and their sustained use improves the outcome of patients who receive medical therapy and/or revascularization procedures. Early initiation of antiplatelet therapy in patients with ACS is best accomplished with care pathways or ACS protocols that are guideline driven. Initiation of these protocols in the ED, with appropriate handoff to hospitalists, will ensure maximization of antiplatelet therapy for patients throughout the precatheterization medical management period. Although antiplatelet agents may be associated with an increased risk of bleeding in some patients, these risks can be minimized and are outweighed by the benefits of clopidogrel and aspirin.
- ,,, et al.ACC/AHA guidelines for the management of patients with unstable angina/non‐ST‐segment elevation myocardial infarction: executive summary.J Am Coll Cardiol.2007;50:e1–e157. Available at: http://www.acc.org.
- ,,, et al.ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction.Circulation.2004;110:82–292.
- Antiplatelet Trialists' Collaboration.Collaborative overview of randomized trials of antiplatelet therapy. Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients.BMJ.1994;308:81–106.
- ,,, et al.One‐year cardiovascular event rates in outpatients with atherothrombosis.JAMA.2007;297:1197–1206.
- ,,, et al.Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association.Circulation.2006;113:873–823.
- The RISC Group.Risk of myocardial infarction and death during treatment with low dose aspirin and intravenous heparin in men with unstable coronary artery disease.Lancet.1990;336:827–830.
- ISIS‐2 Collaborative Group.Randomized trial of intravenous streptokinase, oral aspirin, both or neither among 17,187 cases of suspected acute myocardial infarction: ISIS‐2.Lancet.1988;2:349–360.
- Antithrombotic Trialists' Collaboration.Collaborative meta‐analysis of randomized trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients.BMJ.2002;324:71–86.
- CAPRIE steering committee.A randomized, blinded, trial of clopidogrel versus aspirin in patients at risk of ischemic events (CAPRIE).Lancet.1996;348:1329–1339.
- CURE Trial Investigators.Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST‐segment elevation.N Engl J Med.2001;345:494–502.
- ,,, et al.Benefit of clopidogrel in patients with acute coronary syndromes without ST‐segment elevation in various risk groups.Circulation.2002;106:1622–1626.
- ,,, et al.Early and late effects of clopidogrel in patients with acute coronary syndromes.Circulation.2003;107:966–972.
- ,,, et al.Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non‐ST‐elevation acute coronary syndrome: The clopidogrel in unstable angina to prevent recurrent ischemic events (CURE) trial.Circulation.2004;110:1202–1208.
- ,,, et al.Benefit of clopidogrel according to timing of percutaneous coronary intervention in patients with acute coronary syndromes: Further results from the clopidogrel in unstable angina to prevent recurrent events (CURE) study.Am Heart J.2005;150:1177–1184.
- ,,, et al.Effects of pretreatment with clopidogrel and aspirin followed by long‐term therapy in patients undergoing percutaneous coronary intervention: the PCI‐CURE study.Lancet.2001;358:527–533.
- ,,, et al.Early and sustained dual oral antiplatelet therapy following percutaneous intervention. A randomized trial.JAMA.2002;288:2411–2420.
- ,,,,,.Platelet glycoprotein IIb/IIIa receptor inhibition in non‐ST‐elevation acute coronary syndromes: early benefit during medical treatment only, with additional protection during percutaneous coronary intervention.Circulation.1999;100:2045–2048.
- ,,, et al.Abciximab in patients with acute coronary syndromes undergoing percutaneous coronary intervention after clopidogrel pretreatment. The ISAR‐REACT2 randomized trial.JAMA.2006;295:1531–1538.
- ,,, et al.Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST‐segment elevation.N Engl J Med.2005;352:1179–1189.
- ,,, et al.Effect of clopidogrel pretreatment before percutaneous coronary intervention in patients with ST‐elevation myocardial infarction treated with fibrinolytics. The PCI‐CLARITY study.JAMA.2005;294:1224–1232.
- ,,, et al.ACC/AHA guidelines for the management of patients with unstable angina/non‐ST‐segment elevation myocardial infarction: executive summary.J Am Coll Cardiol.2007;50:e1–e157. Available at: http://www.acc.org.
- ,,, et al.ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction.Circulation.2004;110:82–292.
- Antiplatelet Trialists' Collaboration.Collaborative overview of randomized trials of antiplatelet therapy. Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients.BMJ.1994;308:81–106.
- ,,, et al.One‐year cardiovascular event rates in outpatients with atherothrombosis.JAMA.2007;297:1197–1206.
- ,,, et al.Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association.Circulation.2006;113:873–823.
- The RISC Group.Risk of myocardial infarction and death during treatment with low dose aspirin and intravenous heparin in men with unstable coronary artery disease.Lancet.1990;336:827–830.
- ISIS‐2 Collaborative Group.Randomized trial of intravenous streptokinase, oral aspirin, both or neither among 17,187 cases of suspected acute myocardial infarction: ISIS‐2.Lancet.1988;2:349–360.
- Antithrombotic Trialists' Collaboration.Collaborative meta‐analysis of randomized trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients.BMJ.2002;324:71–86.
- CAPRIE steering committee.A randomized, blinded, trial of clopidogrel versus aspirin in patients at risk of ischemic events (CAPRIE).Lancet.1996;348:1329–1339.
- CURE Trial Investigators.Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST‐segment elevation.N Engl J Med.2001;345:494–502.
- ,,, et al.Benefit of clopidogrel in patients with acute coronary syndromes without ST‐segment elevation in various risk groups.Circulation.2002;106:1622–1626.
- ,,, et al.Early and late effects of clopidogrel in patients with acute coronary syndromes.Circulation.2003;107:966–972.
- ,,, et al.Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non‐ST‐elevation acute coronary syndrome: The clopidogrel in unstable angina to prevent recurrent ischemic events (CURE) trial.Circulation.2004;110:1202–1208.
- ,,, et al.Benefit of clopidogrel according to timing of percutaneous coronary intervention in patients with acute coronary syndromes: Further results from the clopidogrel in unstable angina to prevent recurrent events (CURE) study.Am Heart J.2005;150:1177–1184.
- ,,, et al.Effects of pretreatment with clopidogrel and aspirin followed by long‐term therapy in patients undergoing percutaneous coronary intervention: the PCI‐CURE study.Lancet.2001;358:527–533.
- ,,, et al.Early and sustained dual oral antiplatelet therapy following percutaneous intervention. A randomized trial.JAMA.2002;288:2411–2420.
- ,,,,,.Platelet glycoprotein IIb/IIIa receptor inhibition in non‐ST‐elevation acute coronary syndromes: early benefit during medical treatment only, with additional protection during percutaneous coronary intervention.Circulation.1999;100:2045–2048.
- ,,, et al.Abciximab in patients with acute coronary syndromes undergoing percutaneous coronary intervention after clopidogrel pretreatment. The ISAR‐REACT2 randomized trial.JAMA.2006;295:1531–1538.
- ,,, et al.Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST‐segment elevation.N Engl J Med.2005;352:1179–1189.
- ,,, et al.Effect of clopidogrel pretreatment before percutaneous coronary intervention in patients with ST‐elevation myocardial infarction treated with fibrinolytics. The PCI‐CLARITY study.JAMA.2005;294:1224–1232.