User login
- Family practice primary care physicians, rotating family practice faculty hospitalists, and full-time specialist hospitalists provide comparable care for inpatients with pneumonia.
- Subspecialist hospitalists have higher hospital charges and longer lengths of stay and use more resources.
- The use of hospitalists by hospital systems or insurers should be not be mandated.
- Hospitalists and primary care physicians can better counsel inpatients about lifestyle modification and end-of-life issues.
- OBJECTIVES: To compare the care provided by family practice primary care physicians with that provided by 2 hospitalist models: critical care hospitalists and rotating residency faculty family physician hospitalists.
- STUDY DESIGN: Retrospective chart review. A health maintenance organization mandated that all patients be admitted to a critical care hospitalist team. The family physician hospitalists admitted all other residency patients and patients of some community family physicians. The primary care physicians admitted all their other patients. We adjusted for disease severity by using the Pneumonia Severity Index, age, sex, and comorbidities.
- POPULATION: Adults admitted with pneumonia to our private urban community hospital. Exclusions included patients with nosocomial pneumonia, human immunodeficiency virus, and acquired immunodeficiency syndrome.
- OUTCOMES MEASURED: Primary (adjusted for age, sex, comorbidities, and disease severity): hospital charges, length of stay, in-hospital mortality, readmissions, and returns to the emergency room. Secondary: chest radiographs, intensive care use, blood and sputum cultures, compliance with American Thoracic Society guidelines, lifestyle and end-of-life counseling.
- RESULTS: Of 97 patients, 21 were admitted to the critical care hospitalists, 53 to the family physician hospitalists, and 23 to primary care physicians. The mean charge ($5680) by the primary care physicians was significantly lower than that of the critical care hospitalists ($10,231; P = .005) and trended toward being lower than that of the family physician hospitalists ($7699; P = .08). The patients of critical care and family physician hospitalists had longer mean lengths of stay (critical care hospitalists, 3.8 days; family physician hospitalists, 3.9 days) than did those of the primary care physicians (2.6 days; P = .04 and .01, respectively). Compared with the primary care physicians, the critical care hospitalists were more likely to obtain at least 2 chest x-rays (odds ratio, 4.1; 95% confidence interval, 1.1–15.5) and trended toward increased odds of lengthy stay in the intensive care unit (odd ratio, 2.9; 95% confidence interval, 0.6–14.6). We found no other significant differences in primary or secondary outcomes.
- CONCLUSIONS: Claims of better and cheaper care by hospitalists need further investigation. Meanwhile, the use of hospitalists should not be mandated, and the use of family physicians as hospitalists should be considered a good alternative to the use of subspecialists.
The hospitalist movement has promised to improve the quality of inpatient care, increase patient satisfaction, and decrease costs.1 Many hospitals, practices, and managed care corporations have adopted this model of care,2 but whether this model has fulfilled its promises is unknown. Those who favor hospitalists have argued that hospitalists offer more efficient care by increasing quality and decreasing costs. Detractors are concerned about potential substandard quality through aggressive discharge policies and loss of continuity of care. Unfortunately, both positions are based largely on untested assumptions. We identified 6 peer-reviewed articles directly comparing hospitalists and primary care physicians.3-8 Another 314 were descriptive studies, editorials, letters, and news pieces arguing about the potential risks and benefits of the hospitalist movement.
Hospitalists have been described as physicians who spend over one fourth of their time exclusively in the hospital caring for other physicians’ patients only during that admission.9 Others believe the hospitalist movement more accurately encompasses a broad spectrum of how inpatient care is organized,10 including primary care physicians managing their own inpatients and seeing clinic patients, primary care physicians sharing week- or month-long periods of exclusive hospital care with partners, or excluding the primary care physician from inpatient care by using dedicated inpatient-only physicians who may be family physicians, internists, or specialists.
The scant literature comparing care provided by hospitalists and primary care physicians has several methodologic constraints including before and after designs that may have time-effect bias,11-15 inappropriately assigning subspecialists to the primary care group,3 restricting efficiency tools such as nurse managers and discharge planners to the intervention group,4-6 failing to account for differential involvement of house staff,7,11 using possibly unreliable outcomes,8 and relying exclusively on claims data.11,14 Two recent studies avoided many of these pitfalls and found no differences between different types of hospitalists, but did not compare them with primary care physicians.16,17 We designed our study to address multiple methodologic concerns and determine whether differences in outcomes, processes of care, and costs exist between these multiple models of inpatient care.
Methods
Setting
In 1997 a large regional health maintenance organization in Colorado mandated that all its inpatients be admitted by a pulmonology or critical care hospitalist team to the exclusion of their primary care physicians. Rose Medical Center, a 420-bed private community hospital in Denver, Colorado, serves as a family practice residency training site in which residents care for patients under the guidance of resident faculty and community primary care physicians. We recognized the health maintenance orgaization’s program as a natural experiment and an opportunity to address some of the design limitations of prior studies by comparing the care delivered simultaneously by these 3 inpatient models.
Subjects and study design
We conducted a retrospective cohort study of all patients admitted between April 1997 and March 1998 with a primary diagnosis of pneumonia as identified by codes from the International Classification of Diseases, Ninth Revision. We studied pneumonia care because of the high incidence of pneumonia in our institution and the existence of a valid, population-based measure of disease severity, the Pneumonia Severity Index (PSI; see Statistical Methods). In addition, focusing on 1 diagnosis allowed for a direct and detailed analysis of the process of care. To eliminate potential biases produced by different outpatient physician specialties, we excluded patients who did not have a family physician as a primary care provider. Patients also were excluded if they were younger than 18 years, had human immunodeficiency virus or acquired immunodeficiency syndrome, had exclusively nosocomial pneumonia, or had the diagnosis of pneumonia subsequently ruled out. Ninety-seven patients were included. Data were collected by standardized chart abstraction and entered into a Microsoft Access database. The chart abstraction was performed by research assistants who had no knowledge of whether the attending physician was a primary care physician or a hospitalist.
Patients were grouped based on the status of their inpatient attending physicians of record. The critical care hospitalists represented a group of subspecialty critical care pulmonologists contracted by a large health maintenance organization to care for all its inpatients. The family physician hospitalists represented rotating family medicine faculty who worked exclusively in the hospital for 8 weeks each year. Some patients under the care of family physician hospitalists originated from the residency’s continuity clinic, and others came from the practices of approximately 30 community family physicians for whom the family physician hospitalist acts as a hospitalist service. Community family medicine primary care physicians cared for their own patients and continued their outpatient practices. Family medicine house staff was involved in the care of inpatients from all groups.
Patients’ insurance plans rather than physician referral or self-referral determined whether they were assigned to the critical care hospitalist, family physician hospitalist, or primary care physician group. Accordingly, there were instances when a primary care physician had some patients admitted to the critical care hospitalist because the patient was a member of this particular health maintenance organization and also because the physician cared directly for his other patients in the hospital.
Outcome measures
We looked at 5 primary patient- and policy-oriented outcomes that have been validated as indicators of quality of inpatient care: in-hospital mortality, length of stay, hospital charges, 7-day readmissions, and 7- and 30-day returns to the emergency department.18,19 We included Colorado data from the Healthcare Cost and Utilization Project, when available, to serve as a reference standard.20 In addition, we chose 7 validated secondary “process of care”outcomes21 to further describe the practice behaviors of the 3 groups: documentation of lifestyle modification counseling (tobacco cessation, exercise, etc), documentation of end-of-life counseling, compliance with contemporary guidelines from the American Thoracic Society for treating community-acquired pneumonia,21 length of stay in intensive care, and the use of chest radiographs and blood and sputum cultures.
Statistical methods
All statistical analyses were performed with SAS version 6.12. Patient demographic and clinical characteristics were analyzed with chi-square test and analysis of variance, when appropriate. We controlled for disease severity with the PSI, a well-validated, population-based severity of illness score for inpatients with pneumonia.22,23
Multiple and logistic regressions were used to control for disease severity and potential confounders. Our models included the PSI class and those characteristics that were statistically significantly different (ie, diagnosis of hypertension) or showed a trend toward difference and were felt to be potentially clinically significant (diagnosis of diabetes, effusion on chest x-ray, mental status at admission), in addition to sex and age. Logarithmic transformations of non-normal data were conducted, when appropriate. We eliminated as extreme outliers 3 cases (2 under the care of critical care hospitalists and 1 under the care of family physician hospitalists) whose outcomes were 2 standard deviations or more beyond the mean. For example, 1 patient had a rare clotting disorder, stayed in intensive care for 30 days, required an orphan drug at $6000 per dose, and had charges well in excess of $1 million. This study was approved by the Rose Medical Center and Health One Institutional Review Board.
Results
Demographic and clinical characteristics
Table 1 provides the demographic and clinical descriptions of patients admitted by the different admitting physician models. Patients in the different groups were similar, with 2 exceptions: hypertension was significantly more common in the critical care hospitalist group than in the other groups (P < .05), and there was a trend toward more diabetes in the critical care hospitalist group that did not quite reach statistical significance. Nonsignificant trends also existed for PSI, effusion on chest x-ray, and mental status, with more effusions and acute mental status changes occurring in the critical care hospitalist group, more chronic altered mental status in the family physician hospitalist group, and greater severity of illness in the critical care hospitalist group. Otherwise, demographics, disease severity, and comorbidities were comparable.
TABLE 1
Demographic and clinical characteristics
| Admission group | |||
|---|---|---|---|
| Variable | Critical care hospitalists | Family physician hospitalists | Primary care physicians |
| Total† | 22 (21) | 54 (53) | 23 (23) |
| Demographics | |||
| Age, y‡ | 70 (4) | 66 (3) | 67 (4) |
| Male† | 57 (12) | 62 (33) | 48 (11) |
| Female† | 43 (9) | 38 (20) | 52 (12) |
| Comorbidities† | |||
| Hypertension* | 29 (6) | 23 (12) | 54 (12) |
| Diabetes§ | 0 (0) | 9 (5) | 22 (5) |
| Mental status | |||
| Acute changes | 14 (3) | 6 (3) | 0 (0) |
| Chronic changes | 14 (3) | 26 (14) | 17 (4) |
| Effusion on chest x-ray | 33 (7) | 24 (13) | 17 (4) |
| Renal disease | 10 (2) | 6 (3) | 4 (1) |
| Liver disease | 5 (1) | 2 (1) | 4 (1) |
| Cerebrovascular disease | 14 (3) | 11 (6) | 13 (3) |
| Coronary artery disease | 24 (5) | 27 (14) | 22 (5) |
| Heart failure | 24 (5) | 23 (12) | 18 (4) |
| Cancer | 0 (0) | 2 (1) | 4 (1) |
| Nursing home resident | 9 (2) | 4 (2) | 13 (3) |
| Smokers | 19 (4) | 37 (20) | 26 (6) |
| Vital signs/laboratory values‡ | |||
| Heart rate | 92 (5) | 94 (3) | 92 (5) |
| Respiratory rate | 24 (2) | 24 (1) | 23 (2) |
| Systolic blood pressure | 124 (6) | 127 (4) | 136 (6) |
| Temperature (°F) | 99 (0) | 99 (0) | 99 (0) |
| Pulse oximetry | 86 (2) | 88 (1) | 89 (2) |
| Blood urea nitrogen | 20 (3) | 20 (2) | 22 (3) |
| Glucose | 123 (16) | 130 (10) | 154 (16) |
| Hematocrit | 40 (1) | 41 (1) | 39 (1) |
| Sodium | 136 (1) | 136 (1) | 137 (1) |
| Disease severity | |||
| PSI, raw data‡ | 103 (10) | 85 (6) | 99 (9) |
| PSI risk† | |||
| Low | 10 (2) | 24 (13) | 22 (5) |
| Moderate | 29 (6) | 19 (10) | 26 (6) |
| High | 62 (13) | 55 (30) | 52 (12) |
| *P = .024. | |||
| †Percentage (number of patients). | |||
| ‡Mean (± standard deviation). | |||
| §P = .058; otherwise, P > .05 (chi-square for ordinal and categorical variables, analysis of variance for continuous variables). | |||
| PSI, Pneumonia Severity Index. | |||
Primary outcomes
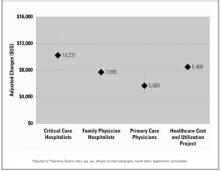
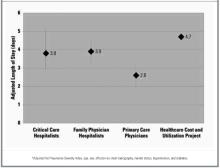
After controlling for severity of illness and intergroup differences, we found that the critical care hospitalist team had the highest mean hospital charge ($10,231), followed by the family physician hospitalist ($7699) and the primary care physician ($5680) groups (Figure 1). The difference in charges between the primary care physician and the critical care hospitalist groups was statistically significant (P = .005) and approached significance between the primary care physician and family physician hospitalist groups (P = .08). The critical care hospitalist and family physician hospitalist groups had longer mean lengths of stay than did the primary care physician group (P = .04 and .01, respectively; Figure 2). The other primary outcomes were rare: 1 primary care physician patient died (4.5%), 2 critical care hospitalist patients died (9.5%) and no family physician hospitalist patients died; no primary care physician patients were readmitted, 1 critical care hospitalist patient was readmitted (4.8%), and 2 family physician hospitalist patients were readmitted (3.8%). There was 1 return to the emergency room in the cohort, in the family physician hospitalist group (1.9%). No intergroup comparisons between these unadjusted rates were statistically significant (P > .05).
FIGURE 1
Hospital charges (in US dollars; with 95% confidence intervals)*
FIGURE 2
Length of stay (in days; with 95% confidence intervals)*
Secondary outcomes
After controlling for severity of illness and intergroup differences, we found that the critical care hospitalists were more likely to obtain 2 or more chest x-rays than the primary care physicians. There were nonsignificant trends toward longer stays in intensive care, greater likelihood of obtaining sputum cultures, and documenting end-of-life counseling by the critical care hospitalists compared with the primary care physicians. For the family physician hospitalists, there were nonsignificant trends toward better compliance with American Thoracic Society antibiotic guidelines and greater likelihood of documenting end-of-life and lifestyle modification counseling compared with the primary care physicians (Table 2).
TABLE 2
Secondary “process of care” outcomes*
| Outcome | Primary care physicians† | Critical care hospitalists | Family physician hospitalists |
|---|---|---|---|
| Chest x-ray (≥2) | 1 | 4.1 (1.1–15.5) | 0.9 (0.3–2.6) |
| ICU stay (≥1 d) | 1 | 2.9 (0.6–14.6) | 0.5 (0.1–3) |
| ATS guideline adherence | 1 | 1.4 (0.4–5.0) | 2.3 (0.8–7.0) |
| Sputum culture obtained | 1 | 2.3 (0.7–8.0) | 0.6 (0.2–1.7) |
| Blood culture obtained | 1 | 1.3 (0.4–4.8) | 1.2 (0.4–3.5) |
| End-of-life counseling documented | 1 | 3.0 (0.6–14.3) | 3.1 (0.7–12.9) |
| Lifestyle modification documented | 1 | 1.1 (0.3–4.5) | 2.7 (0.8–8.7) |
| *Data are presented as odds ratio (95% confidence interval). Odds ratios were adjusted for Pneumonia Severity Index, age, sex, effusion on chest radiography, mental status, hypertension, and diabetes. | |||
| †Reference group. | |||
| ATS, American Thoracic Society; ICU, intensive care unit. | |||
Discussion
Our study provided a unique perspective on the impact of different models of caring for inpatients on the quality, processes, and cost of care. We believe this is the first study to successfully address several methodologic limitations of previous studies: potential time-effect bias, inappropriate controls, differential assignment of house staff and case management resources, unvalidated outcomes, and lack of clinical data.
In addition, we reduced the potential biases inherent in comparing different hospitals and different outpatient physician specialties and used a standardized chart abstraction instrument to avoid the problems inherent in using claims data. As a result, we were able to examine processes of care and use the PSI, an extensively validated tool, to control for disease severity. This study represents an effectiveness study of a real-life intervention by a health maintenance organization to mandate the use of hospitalists. Although the retrospective design of this study may create the potential for bias, there was inadequate advanced notice of the implementation of this hospitalist plan to allow for prospective analysis. Despite not being randomly assigned to 1 of the 3 groups, patients were quite similar with the exceptions of hypertension and possibly diabetes and PSI, which we controlled for in the statistical analysis.
Unfortunately, this was a small study that lacked sufficient power to detect modest differences between groups because the health maintenance organization sponsoring the critical care hospitalist group abandoned the program after 1 year. In addition, the differences in disease severity might have been significant in a larger sample. However, even after controlling for these differences statistically, we found no large differences for mortality, readmission, or returns to the emergency room.
Despite insufficient power to observe statistically significant differences in these relatively rare but important pneumonia outcomes, we did detect a substantial difference in adjusted hospital charges and a modest difference in length of stay. Subspecialist hospitalists had significantly higher adjusted charges than did primary care family physicians. Although the comparison across groups failed to show statistically significant differences, we did see a trend of increasing charges as the degree of hospitalization increased. These higher costs may be explained in part by primary care physicians advising shorter lengths of stay and the subspecialists’ increased use of multiple chest x-rays and trends toward greater use of other resources (eg, intensive care and blood and sputum cultures). Alternatively, some of the difference in charges may reflect differing levels of continuity; the critical care hospitalists had no outpatient continuity with their inpatients, whereas the family physician hospitalists had continuity relationships with some inpatients and the primary care physicians had relationships with all their inpatients. Thus the primary care physicians and, to a lesser extent, the family physician hospitalists may have had information about prior care. Hence, knowledge of previous antibiotic use might argue for the low yield of blood and sputum cultures, and having obtained an outpatient x-ray might obviate the need for another in the hospital. The critical care hospitalists’ increased length of stay and x-ray use, in conjunction with the trend toward greater use of cultures and intensive care, may in turn reflect different degrees of comfort with uncertainty between family physicians and subspecialists. Also, we examined only hospital charges rather than total costs to the system.
Interestingly, we found a trend showing that family physician hospitalists were more likely to document lifestyle modification counseling than were primary care physicians. This result should be interpreted with some caution. Our findings may indicate a true lack of performance by primary care physicians, or they may show a failure to document advice on the hospital chart, reflecting some aspect of the continuity relationship in which such discussions are relegated to the outpatient setting.We also were surprised to see the trend toward decreased end-of-life counseling by the primary care physicians. This could reflect some adverse effect of continuity, the time constraints imposed on nonhospitalists, or not documenting outpatient counseling on the inpatient record.
There were other potential sources of confounding in this study. All patients in the critical care hospitalist group were members of the same health maintenance organization, which may have introduced unmeasured bias despite our attempts to control for differences between groups. Even though we purposefully avoided differential use of house staff, its involvement in each case may have decreased any potential differences across practices.
We draw 2 important conclusions from our results. First, our findings of increased costs and length of stay for mandated hospitalists without significantly different outcomes support the assertion of the American Academy of Family Physicians, the American College of Physicians–American Society of Internal Medicine, the American Medical Association, and the National Association of Inpatient Physicians: the practice of mandating the use of hospitalists should be abandoned pending larger, more comprehensive contemporaneous trials. Second, if hospitalists are to be employed on a voluntary basis, the use of subspecialists rather than generalists may result in more costly care.
Acknowledgments
The authors thank Ralph B. D’Agonstino, Jr., PhD, of the Bowman Gray School of Medicine for his invaluable assistance in statistical methods and Cary Foster, MD, and Promoda Mahupatra, MD, for their collection of the data.
1. Wachter RM. An introduction to the hospitalist model. Ann Intern Med 1999;130:338-42.
2. Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med 2000;109:648-53.
3. Stein MD, Hanson S, Tammaro D, Hanna L, Most AS. Economic effects of community vs hospital-based pneumonia care. J Gen Intern Med 1998;13:774-7.
4. Wachter RM, Katz P, Showstack J, Bindman AB, Goldman L. Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education. JAMA 1998;279:1560-5.
5. Palmer HC, Armistead NS, Elnicki D, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med 2001;111:627-32.
6. Davis KM, Koch KE, Harvey JK, et al. Effects of hospitalists on cost, outcomes, and patient satisfaction in a rural health system. Am J Med 2000;108:621-6.
7. Hackner D, Tu G, Braunstein GD, et al. The value of a hospitalist service: efficient care for the aging population? Chest 2001;119:580-9.
8. Molinari C, Short R. The effects of an HMO-hospitalist program on inpatient utilization. Am J Manag Care 2001;7:1051-17.
9. Wachter RM. An introduction to the hospitalist model. Ann Intern Med 1999;130:338-42.
10. Boschert S. “Hospitalists” may be an emerging specialty. Am Med News July 15, 1997;67.
11. Diamond HS, Goldberg E, Janosky JE. The effect of full-time faculty hospitalists on the efficiency of care at a community teaching hospital. Ann Intern Med 1998;129:197-203.
12. Bellet PS, Whitaker RC. Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges. Pediatrics 2000;105:478-84.
13. Freese RB. Clinical, logistical, and political issues in creating a hospitalist system. Ann Intern Med 1999;130:350-4.
14. Craig D, Hartka L, Likosky WH, et al. Implementation of a hospitalist system in a large health maintenance organization: the Kaiser Permanente experience. Ann Intern Med 1999;130:355-9.
15. Halpert AP, Pearson SD, LeWine HE, Mckean SC. The impact of an inpatient physician program on quality, utilization, and satisfaction. J Manag Care 2000;6:549-55.
16. Tingle LE, Lambert CT. Comparison of a family practice teaching service and a hospitalist model: costs, charges, length of stay, and mortality. Fam Med 2001;33:511-5.
17. Kearns PJ, Wang CC, Morris WJ, et al. Hospital care by hospitalbased and clinic-based faculty: a prospective, controlled trial. Arch Intern Med 2001;161:235-41.
18. Ashton CM, Del Junco DJ, Souchek J, Wray NP, Mansyur CL. The association between the quality of inpatient care and early readmission: a meta-analysis of the evidence. Med Care 1997;35:1044-59.
19. Rhew DC, Goetz MB, Shekelle PG. Evaluating quality indicators for patients with community-acquired pneumonia. Jt Comm J Qual Improv 2001;27:575-90.
20. HCUPnet Halthcare cost and utilization project. Agency for Healthcare Research and Quality, Rockville, MD. June 2002. Available at: http://www.ahrq.gov/data/hcup/hcupnet.htm. Accessed October 8, 2002.
21. Niederman MS, Bass JB, Campbell GD, et al. American Thoracic Society guidelines for the initial management of adults with community-acquired pneumonia: diagnosis, assessment of severity, and initial antimicrobial therapy. Am Rev Respir Dis 1993;148:1418-26.
22. Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify lowrisk patients with community-acquired pneumonia. N Engl J Med 1997;336:243-50.
23. Ewig S, Kleinfeld T, Bauer T, Seifert K, Schafer H, Goke N. Comparative validation of prognostic rules for community-acquired pneumonia in an elderly population. Eur Respir J 1999;14:370-5.
- Family practice primary care physicians, rotating family practice faculty hospitalists, and full-time specialist hospitalists provide comparable care for inpatients with pneumonia.
- Subspecialist hospitalists have higher hospital charges and longer lengths of stay and use more resources.
- The use of hospitalists by hospital systems or insurers should be not be mandated.
- Hospitalists and primary care physicians can better counsel inpatients about lifestyle modification and end-of-life issues.
- OBJECTIVES: To compare the care provided by family practice primary care physicians with that provided by 2 hospitalist models: critical care hospitalists and rotating residency faculty family physician hospitalists.
- STUDY DESIGN: Retrospective chart review. A health maintenance organization mandated that all patients be admitted to a critical care hospitalist team. The family physician hospitalists admitted all other residency patients and patients of some community family physicians. The primary care physicians admitted all their other patients. We adjusted for disease severity by using the Pneumonia Severity Index, age, sex, and comorbidities.
- POPULATION: Adults admitted with pneumonia to our private urban community hospital. Exclusions included patients with nosocomial pneumonia, human immunodeficiency virus, and acquired immunodeficiency syndrome.
- OUTCOMES MEASURED: Primary (adjusted for age, sex, comorbidities, and disease severity): hospital charges, length of stay, in-hospital mortality, readmissions, and returns to the emergency room. Secondary: chest radiographs, intensive care use, blood and sputum cultures, compliance with American Thoracic Society guidelines, lifestyle and end-of-life counseling.
- RESULTS: Of 97 patients, 21 were admitted to the critical care hospitalists, 53 to the family physician hospitalists, and 23 to primary care physicians. The mean charge ($5680) by the primary care physicians was significantly lower than that of the critical care hospitalists ($10,231; P = .005) and trended toward being lower than that of the family physician hospitalists ($7699; P = .08). The patients of critical care and family physician hospitalists had longer mean lengths of stay (critical care hospitalists, 3.8 days; family physician hospitalists, 3.9 days) than did those of the primary care physicians (2.6 days; P = .04 and .01, respectively). Compared with the primary care physicians, the critical care hospitalists were more likely to obtain at least 2 chest x-rays (odds ratio, 4.1; 95% confidence interval, 1.1–15.5) and trended toward increased odds of lengthy stay in the intensive care unit (odd ratio, 2.9; 95% confidence interval, 0.6–14.6). We found no other significant differences in primary or secondary outcomes.
- CONCLUSIONS: Claims of better and cheaper care by hospitalists need further investigation. Meanwhile, the use of hospitalists should not be mandated, and the use of family physicians as hospitalists should be considered a good alternative to the use of subspecialists.
The hospitalist movement has promised to improve the quality of inpatient care, increase patient satisfaction, and decrease costs.1 Many hospitals, practices, and managed care corporations have adopted this model of care,2 but whether this model has fulfilled its promises is unknown. Those who favor hospitalists have argued that hospitalists offer more efficient care by increasing quality and decreasing costs. Detractors are concerned about potential substandard quality through aggressive discharge policies and loss of continuity of care. Unfortunately, both positions are based largely on untested assumptions. We identified 6 peer-reviewed articles directly comparing hospitalists and primary care physicians.3-8 Another 314 were descriptive studies, editorials, letters, and news pieces arguing about the potential risks and benefits of the hospitalist movement.
Hospitalists have been described as physicians who spend over one fourth of their time exclusively in the hospital caring for other physicians’ patients only during that admission.9 Others believe the hospitalist movement more accurately encompasses a broad spectrum of how inpatient care is organized,10 including primary care physicians managing their own inpatients and seeing clinic patients, primary care physicians sharing week- or month-long periods of exclusive hospital care with partners, or excluding the primary care physician from inpatient care by using dedicated inpatient-only physicians who may be family physicians, internists, or specialists.
The scant literature comparing care provided by hospitalists and primary care physicians has several methodologic constraints including before and after designs that may have time-effect bias,11-15 inappropriately assigning subspecialists to the primary care group,3 restricting efficiency tools such as nurse managers and discharge planners to the intervention group,4-6 failing to account for differential involvement of house staff,7,11 using possibly unreliable outcomes,8 and relying exclusively on claims data.11,14 Two recent studies avoided many of these pitfalls and found no differences between different types of hospitalists, but did not compare them with primary care physicians.16,17 We designed our study to address multiple methodologic concerns and determine whether differences in outcomes, processes of care, and costs exist between these multiple models of inpatient care.
Methods
Setting
In 1997 a large regional health maintenance organization in Colorado mandated that all its inpatients be admitted by a pulmonology or critical care hospitalist team to the exclusion of their primary care physicians. Rose Medical Center, a 420-bed private community hospital in Denver, Colorado, serves as a family practice residency training site in which residents care for patients under the guidance of resident faculty and community primary care physicians. We recognized the health maintenance orgaization’s program as a natural experiment and an opportunity to address some of the design limitations of prior studies by comparing the care delivered simultaneously by these 3 inpatient models.
Subjects and study design
We conducted a retrospective cohort study of all patients admitted between April 1997 and March 1998 with a primary diagnosis of pneumonia as identified by codes from the International Classification of Diseases, Ninth Revision. We studied pneumonia care because of the high incidence of pneumonia in our institution and the existence of a valid, population-based measure of disease severity, the Pneumonia Severity Index (PSI; see Statistical Methods). In addition, focusing on 1 diagnosis allowed for a direct and detailed analysis of the process of care. To eliminate potential biases produced by different outpatient physician specialties, we excluded patients who did not have a family physician as a primary care provider. Patients also were excluded if they were younger than 18 years, had human immunodeficiency virus or acquired immunodeficiency syndrome, had exclusively nosocomial pneumonia, or had the diagnosis of pneumonia subsequently ruled out. Ninety-seven patients were included. Data were collected by standardized chart abstraction and entered into a Microsoft Access database. The chart abstraction was performed by research assistants who had no knowledge of whether the attending physician was a primary care physician or a hospitalist.
Patients were grouped based on the status of their inpatient attending physicians of record. The critical care hospitalists represented a group of subspecialty critical care pulmonologists contracted by a large health maintenance organization to care for all its inpatients. The family physician hospitalists represented rotating family medicine faculty who worked exclusively in the hospital for 8 weeks each year. Some patients under the care of family physician hospitalists originated from the residency’s continuity clinic, and others came from the practices of approximately 30 community family physicians for whom the family physician hospitalist acts as a hospitalist service. Community family medicine primary care physicians cared for their own patients and continued their outpatient practices. Family medicine house staff was involved in the care of inpatients from all groups.
Patients’ insurance plans rather than physician referral or self-referral determined whether they were assigned to the critical care hospitalist, family physician hospitalist, or primary care physician group. Accordingly, there were instances when a primary care physician had some patients admitted to the critical care hospitalist because the patient was a member of this particular health maintenance organization and also because the physician cared directly for his other patients in the hospital.
Outcome measures
We looked at 5 primary patient- and policy-oriented outcomes that have been validated as indicators of quality of inpatient care: in-hospital mortality, length of stay, hospital charges, 7-day readmissions, and 7- and 30-day returns to the emergency department.18,19 We included Colorado data from the Healthcare Cost and Utilization Project, when available, to serve as a reference standard.20 In addition, we chose 7 validated secondary “process of care”outcomes21 to further describe the practice behaviors of the 3 groups: documentation of lifestyle modification counseling (tobacco cessation, exercise, etc), documentation of end-of-life counseling, compliance with contemporary guidelines from the American Thoracic Society for treating community-acquired pneumonia,21 length of stay in intensive care, and the use of chest radiographs and blood and sputum cultures.
Statistical methods
All statistical analyses were performed with SAS version 6.12. Patient demographic and clinical characteristics were analyzed with chi-square test and analysis of variance, when appropriate. We controlled for disease severity with the PSI, a well-validated, population-based severity of illness score for inpatients with pneumonia.22,23
Multiple and logistic regressions were used to control for disease severity and potential confounders. Our models included the PSI class and those characteristics that were statistically significantly different (ie, diagnosis of hypertension) or showed a trend toward difference and were felt to be potentially clinically significant (diagnosis of diabetes, effusion on chest x-ray, mental status at admission), in addition to sex and age. Logarithmic transformations of non-normal data were conducted, when appropriate. We eliminated as extreme outliers 3 cases (2 under the care of critical care hospitalists and 1 under the care of family physician hospitalists) whose outcomes were 2 standard deviations or more beyond the mean. For example, 1 patient had a rare clotting disorder, stayed in intensive care for 30 days, required an orphan drug at $6000 per dose, and had charges well in excess of $1 million. This study was approved by the Rose Medical Center and Health One Institutional Review Board.
Results
Demographic and clinical characteristics
Table 1 provides the demographic and clinical descriptions of patients admitted by the different admitting physician models. Patients in the different groups were similar, with 2 exceptions: hypertension was significantly more common in the critical care hospitalist group than in the other groups (P < .05), and there was a trend toward more diabetes in the critical care hospitalist group that did not quite reach statistical significance. Nonsignificant trends also existed for PSI, effusion on chest x-ray, and mental status, with more effusions and acute mental status changes occurring in the critical care hospitalist group, more chronic altered mental status in the family physician hospitalist group, and greater severity of illness in the critical care hospitalist group. Otherwise, demographics, disease severity, and comorbidities were comparable.
TABLE 1
Demographic and clinical characteristics
| Admission group | |||
|---|---|---|---|
| Variable | Critical care hospitalists | Family physician hospitalists | Primary care physicians |
| Total† | 22 (21) | 54 (53) | 23 (23) |
| Demographics | |||
| Age, y‡ | 70 (4) | 66 (3) | 67 (4) |
| Male† | 57 (12) | 62 (33) | 48 (11) |
| Female† | 43 (9) | 38 (20) | 52 (12) |
| Comorbidities† | |||
| Hypertension* | 29 (6) | 23 (12) | 54 (12) |
| Diabetes§ | 0 (0) | 9 (5) | 22 (5) |
| Mental status | |||
| Acute changes | 14 (3) | 6 (3) | 0 (0) |
| Chronic changes | 14 (3) | 26 (14) | 17 (4) |
| Effusion on chest x-ray | 33 (7) | 24 (13) | 17 (4) |
| Renal disease | 10 (2) | 6 (3) | 4 (1) |
| Liver disease | 5 (1) | 2 (1) | 4 (1) |
| Cerebrovascular disease | 14 (3) | 11 (6) | 13 (3) |
| Coronary artery disease | 24 (5) | 27 (14) | 22 (5) |
| Heart failure | 24 (5) | 23 (12) | 18 (4) |
| Cancer | 0 (0) | 2 (1) | 4 (1) |
| Nursing home resident | 9 (2) | 4 (2) | 13 (3) |
| Smokers | 19 (4) | 37 (20) | 26 (6) |
| Vital signs/laboratory values‡ | |||
| Heart rate | 92 (5) | 94 (3) | 92 (5) |
| Respiratory rate | 24 (2) | 24 (1) | 23 (2) |
| Systolic blood pressure | 124 (6) | 127 (4) | 136 (6) |
| Temperature (°F) | 99 (0) | 99 (0) | 99 (0) |
| Pulse oximetry | 86 (2) | 88 (1) | 89 (2) |
| Blood urea nitrogen | 20 (3) | 20 (2) | 22 (3) |
| Glucose | 123 (16) | 130 (10) | 154 (16) |
| Hematocrit | 40 (1) | 41 (1) | 39 (1) |
| Sodium | 136 (1) | 136 (1) | 137 (1) |
| Disease severity | |||
| PSI, raw data‡ | 103 (10) | 85 (6) | 99 (9) |
| PSI risk† | |||
| Low | 10 (2) | 24 (13) | 22 (5) |
| Moderate | 29 (6) | 19 (10) | 26 (6) |
| High | 62 (13) | 55 (30) | 52 (12) |
| *P = .024. | |||
| †Percentage (number of patients). | |||
| ‡Mean (± standard deviation). | |||
| §P = .058; otherwise, P > .05 (chi-square for ordinal and categorical variables, analysis of variance for continuous variables). | |||
| PSI, Pneumonia Severity Index. | |||
Primary outcomes
After controlling for severity of illness and intergroup differences, we found that the critical care hospitalist team had the highest mean hospital charge ($10,231), followed by the family physician hospitalist ($7699) and the primary care physician ($5680) groups (Figure 1). The difference in charges between the primary care physician and the critical care hospitalist groups was statistically significant (P = .005) and approached significance between the primary care physician and family physician hospitalist groups (P = .08). The critical care hospitalist and family physician hospitalist groups had longer mean lengths of stay than did the primary care physician group (P = .04 and .01, respectively; Figure 2). The other primary outcomes were rare: 1 primary care physician patient died (4.5%), 2 critical care hospitalist patients died (9.5%) and no family physician hospitalist patients died; no primary care physician patients were readmitted, 1 critical care hospitalist patient was readmitted (4.8%), and 2 family physician hospitalist patients were readmitted (3.8%). There was 1 return to the emergency room in the cohort, in the family physician hospitalist group (1.9%). No intergroup comparisons between these unadjusted rates were statistically significant (P > .05).
FIGURE 1
Hospital charges (in US dollars; with 95% confidence intervals)*
FIGURE 2
Length of stay (in days; with 95% confidence intervals)*
Secondary outcomes
After controlling for severity of illness and intergroup differences, we found that the critical care hospitalists were more likely to obtain 2 or more chest x-rays than the primary care physicians. There were nonsignificant trends toward longer stays in intensive care, greater likelihood of obtaining sputum cultures, and documenting end-of-life counseling by the critical care hospitalists compared with the primary care physicians. For the family physician hospitalists, there were nonsignificant trends toward better compliance with American Thoracic Society antibiotic guidelines and greater likelihood of documenting end-of-life and lifestyle modification counseling compared with the primary care physicians (Table 2).
TABLE 2
Secondary “process of care” outcomes*
| Outcome | Primary care physicians† | Critical care hospitalists | Family physician hospitalists |
|---|---|---|---|
| Chest x-ray (≥2) | 1 | 4.1 (1.1–15.5) | 0.9 (0.3–2.6) |
| ICU stay (≥1 d) | 1 | 2.9 (0.6–14.6) | 0.5 (0.1–3) |
| ATS guideline adherence | 1 | 1.4 (0.4–5.0) | 2.3 (0.8–7.0) |
| Sputum culture obtained | 1 | 2.3 (0.7–8.0) | 0.6 (0.2–1.7) |
| Blood culture obtained | 1 | 1.3 (0.4–4.8) | 1.2 (0.4–3.5) |
| End-of-life counseling documented | 1 | 3.0 (0.6–14.3) | 3.1 (0.7–12.9) |
| Lifestyle modification documented | 1 | 1.1 (0.3–4.5) | 2.7 (0.8–8.7) |
| *Data are presented as odds ratio (95% confidence interval). Odds ratios were adjusted for Pneumonia Severity Index, age, sex, effusion on chest radiography, mental status, hypertension, and diabetes. | |||
| †Reference group. | |||
| ATS, American Thoracic Society; ICU, intensive care unit. | |||
Discussion
Our study provided a unique perspective on the impact of different models of caring for inpatients on the quality, processes, and cost of care. We believe this is the first study to successfully address several methodologic limitations of previous studies: potential time-effect bias, inappropriate controls, differential assignment of house staff and case management resources, unvalidated outcomes, and lack of clinical data.
In addition, we reduced the potential biases inherent in comparing different hospitals and different outpatient physician specialties and used a standardized chart abstraction instrument to avoid the problems inherent in using claims data. As a result, we were able to examine processes of care and use the PSI, an extensively validated tool, to control for disease severity. This study represents an effectiveness study of a real-life intervention by a health maintenance organization to mandate the use of hospitalists. Although the retrospective design of this study may create the potential for bias, there was inadequate advanced notice of the implementation of this hospitalist plan to allow for prospective analysis. Despite not being randomly assigned to 1 of the 3 groups, patients were quite similar with the exceptions of hypertension and possibly diabetes and PSI, which we controlled for in the statistical analysis.
Unfortunately, this was a small study that lacked sufficient power to detect modest differences between groups because the health maintenance organization sponsoring the critical care hospitalist group abandoned the program after 1 year. In addition, the differences in disease severity might have been significant in a larger sample. However, even after controlling for these differences statistically, we found no large differences for mortality, readmission, or returns to the emergency room.
Despite insufficient power to observe statistically significant differences in these relatively rare but important pneumonia outcomes, we did detect a substantial difference in adjusted hospital charges and a modest difference in length of stay. Subspecialist hospitalists had significantly higher adjusted charges than did primary care family physicians. Although the comparison across groups failed to show statistically significant differences, we did see a trend of increasing charges as the degree of hospitalization increased. These higher costs may be explained in part by primary care physicians advising shorter lengths of stay and the subspecialists’ increased use of multiple chest x-rays and trends toward greater use of other resources (eg, intensive care and blood and sputum cultures). Alternatively, some of the difference in charges may reflect differing levels of continuity; the critical care hospitalists had no outpatient continuity with their inpatients, whereas the family physician hospitalists had continuity relationships with some inpatients and the primary care physicians had relationships with all their inpatients. Thus the primary care physicians and, to a lesser extent, the family physician hospitalists may have had information about prior care. Hence, knowledge of previous antibiotic use might argue for the low yield of blood and sputum cultures, and having obtained an outpatient x-ray might obviate the need for another in the hospital. The critical care hospitalists’ increased length of stay and x-ray use, in conjunction with the trend toward greater use of cultures and intensive care, may in turn reflect different degrees of comfort with uncertainty between family physicians and subspecialists. Also, we examined only hospital charges rather than total costs to the system.
Interestingly, we found a trend showing that family physician hospitalists were more likely to document lifestyle modification counseling than were primary care physicians. This result should be interpreted with some caution. Our findings may indicate a true lack of performance by primary care physicians, or they may show a failure to document advice on the hospital chart, reflecting some aspect of the continuity relationship in which such discussions are relegated to the outpatient setting.We also were surprised to see the trend toward decreased end-of-life counseling by the primary care physicians. This could reflect some adverse effect of continuity, the time constraints imposed on nonhospitalists, or not documenting outpatient counseling on the inpatient record.
There were other potential sources of confounding in this study. All patients in the critical care hospitalist group were members of the same health maintenance organization, which may have introduced unmeasured bias despite our attempts to control for differences between groups. Even though we purposefully avoided differential use of house staff, its involvement in each case may have decreased any potential differences across practices.
We draw 2 important conclusions from our results. First, our findings of increased costs and length of stay for mandated hospitalists without significantly different outcomes support the assertion of the American Academy of Family Physicians, the American College of Physicians–American Society of Internal Medicine, the American Medical Association, and the National Association of Inpatient Physicians: the practice of mandating the use of hospitalists should be abandoned pending larger, more comprehensive contemporaneous trials. Second, if hospitalists are to be employed on a voluntary basis, the use of subspecialists rather than generalists may result in more costly care.
Acknowledgments
The authors thank Ralph B. D’Agonstino, Jr., PhD, of the Bowman Gray School of Medicine for his invaluable assistance in statistical methods and Cary Foster, MD, and Promoda Mahupatra, MD, for their collection of the data.
- Family practice primary care physicians, rotating family practice faculty hospitalists, and full-time specialist hospitalists provide comparable care for inpatients with pneumonia.
- Subspecialist hospitalists have higher hospital charges and longer lengths of stay and use more resources.
- The use of hospitalists by hospital systems or insurers should be not be mandated.
- Hospitalists and primary care physicians can better counsel inpatients about lifestyle modification and end-of-life issues.
- OBJECTIVES: To compare the care provided by family practice primary care physicians with that provided by 2 hospitalist models: critical care hospitalists and rotating residency faculty family physician hospitalists.
- STUDY DESIGN: Retrospective chart review. A health maintenance organization mandated that all patients be admitted to a critical care hospitalist team. The family physician hospitalists admitted all other residency patients and patients of some community family physicians. The primary care physicians admitted all their other patients. We adjusted for disease severity by using the Pneumonia Severity Index, age, sex, and comorbidities.
- POPULATION: Adults admitted with pneumonia to our private urban community hospital. Exclusions included patients with nosocomial pneumonia, human immunodeficiency virus, and acquired immunodeficiency syndrome.
- OUTCOMES MEASURED: Primary (adjusted for age, sex, comorbidities, and disease severity): hospital charges, length of stay, in-hospital mortality, readmissions, and returns to the emergency room. Secondary: chest radiographs, intensive care use, blood and sputum cultures, compliance with American Thoracic Society guidelines, lifestyle and end-of-life counseling.
- RESULTS: Of 97 patients, 21 were admitted to the critical care hospitalists, 53 to the family physician hospitalists, and 23 to primary care physicians. The mean charge ($5680) by the primary care physicians was significantly lower than that of the critical care hospitalists ($10,231; P = .005) and trended toward being lower than that of the family physician hospitalists ($7699; P = .08). The patients of critical care and family physician hospitalists had longer mean lengths of stay (critical care hospitalists, 3.8 days; family physician hospitalists, 3.9 days) than did those of the primary care physicians (2.6 days; P = .04 and .01, respectively). Compared with the primary care physicians, the critical care hospitalists were more likely to obtain at least 2 chest x-rays (odds ratio, 4.1; 95% confidence interval, 1.1–15.5) and trended toward increased odds of lengthy stay in the intensive care unit (odd ratio, 2.9; 95% confidence interval, 0.6–14.6). We found no other significant differences in primary or secondary outcomes.
- CONCLUSIONS: Claims of better and cheaper care by hospitalists need further investigation. Meanwhile, the use of hospitalists should not be mandated, and the use of family physicians as hospitalists should be considered a good alternative to the use of subspecialists.
The hospitalist movement has promised to improve the quality of inpatient care, increase patient satisfaction, and decrease costs.1 Many hospitals, practices, and managed care corporations have adopted this model of care,2 but whether this model has fulfilled its promises is unknown. Those who favor hospitalists have argued that hospitalists offer more efficient care by increasing quality and decreasing costs. Detractors are concerned about potential substandard quality through aggressive discharge policies and loss of continuity of care. Unfortunately, both positions are based largely on untested assumptions. We identified 6 peer-reviewed articles directly comparing hospitalists and primary care physicians.3-8 Another 314 were descriptive studies, editorials, letters, and news pieces arguing about the potential risks and benefits of the hospitalist movement.
Hospitalists have been described as physicians who spend over one fourth of their time exclusively in the hospital caring for other physicians’ patients only during that admission.9 Others believe the hospitalist movement more accurately encompasses a broad spectrum of how inpatient care is organized,10 including primary care physicians managing their own inpatients and seeing clinic patients, primary care physicians sharing week- or month-long periods of exclusive hospital care with partners, or excluding the primary care physician from inpatient care by using dedicated inpatient-only physicians who may be family physicians, internists, or specialists.
The scant literature comparing care provided by hospitalists and primary care physicians has several methodologic constraints including before and after designs that may have time-effect bias,11-15 inappropriately assigning subspecialists to the primary care group,3 restricting efficiency tools such as nurse managers and discharge planners to the intervention group,4-6 failing to account for differential involvement of house staff,7,11 using possibly unreliable outcomes,8 and relying exclusively on claims data.11,14 Two recent studies avoided many of these pitfalls and found no differences between different types of hospitalists, but did not compare them with primary care physicians.16,17 We designed our study to address multiple methodologic concerns and determine whether differences in outcomes, processes of care, and costs exist between these multiple models of inpatient care.
Methods
Setting
In 1997 a large regional health maintenance organization in Colorado mandated that all its inpatients be admitted by a pulmonology or critical care hospitalist team to the exclusion of their primary care physicians. Rose Medical Center, a 420-bed private community hospital in Denver, Colorado, serves as a family practice residency training site in which residents care for patients under the guidance of resident faculty and community primary care physicians. We recognized the health maintenance orgaization’s program as a natural experiment and an opportunity to address some of the design limitations of prior studies by comparing the care delivered simultaneously by these 3 inpatient models.
Subjects and study design
We conducted a retrospective cohort study of all patients admitted between April 1997 and March 1998 with a primary diagnosis of pneumonia as identified by codes from the International Classification of Diseases, Ninth Revision. We studied pneumonia care because of the high incidence of pneumonia in our institution and the existence of a valid, population-based measure of disease severity, the Pneumonia Severity Index (PSI; see Statistical Methods). In addition, focusing on 1 diagnosis allowed for a direct and detailed analysis of the process of care. To eliminate potential biases produced by different outpatient physician specialties, we excluded patients who did not have a family physician as a primary care provider. Patients also were excluded if they were younger than 18 years, had human immunodeficiency virus or acquired immunodeficiency syndrome, had exclusively nosocomial pneumonia, or had the diagnosis of pneumonia subsequently ruled out. Ninety-seven patients were included. Data were collected by standardized chart abstraction and entered into a Microsoft Access database. The chart abstraction was performed by research assistants who had no knowledge of whether the attending physician was a primary care physician or a hospitalist.
Patients were grouped based on the status of their inpatient attending physicians of record. The critical care hospitalists represented a group of subspecialty critical care pulmonologists contracted by a large health maintenance organization to care for all its inpatients. The family physician hospitalists represented rotating family medicine faculty who worked exclusively in the hospital for 8 weeks each year. Some patients under the care of family physician hospitalists originated from the residency’s continuity clinic, and others came from the practices of approximately 30 community family physicians for whom the family physician hospitalist acts as a hospitalist service. Community family medicine primary care physicians cared for their own patients and continued their outpatient practices. Family medicine house staff was involved in the care of inpatients from all groups.
Patients’ insurance plans rather than physician referral or self-referral determined whether they were assigned to the critical care hospitalist, family physician hospitalist, or primary care physician group. Accordingly, there were instances when a primary care physician had some patients admitted to the critical care hospitalist because the patient was a member of this particular health maintenance organization and also because the physician cared directly for his other patients in the hospital.
Outcome measures
We looked at 5 primary patient- and policy-oriented outcomes that have been validated as indicators of quality of inpatient care: in-hospital mortality, length of stay, hospital charges, 7-day readmissions, and 7- and 30-day returns to the emergency department.18,19 We included Colorado data from the Healthcare Cost and Utilization Project, when available, to serve as a reference standard.20 In addition, we chose 7 validated secondary “process of care”outcomes21 to further describe the practice behaviors of the 3 groups: documentation of lifestyle modification counseling (tobacco cessation, exercise, etc), documentation of end-of-life counseling, compliance with contemporary guidelines from the American Thoracic Society for treating community-acquired pneumonia,21 length of stay in intensive care, and the use of chest radiographs and blood and sputum cultures.
Statistical methods
All statistical analyses were performed with SAS version 6.12. Patient demographic and clinical characteristics were analyzed with chi-square test and analysis of variance, when appropriate. We controlled for disease severity with the PSI, a well-validated, population-based severity of illness score for inpatients with pneumonia.22,23
Multiple and logistic regressions were used to control for disease severity and potential confounders. Our models included the PSI class and those characteristics that were statistically significantly different (ie, diagnosis of hypertension) or showed a trend toward difference and were felt to be potentially clinically significant (diagnosis of diabetes, effusion on chest x-ray, mental status at admission), in addition to sex and age. Logarithmic transformations of non-normal data were conducted, when appropriate. We eliminated as extreme outliers 3 cases (2 under the care of critical care hospitalists and 1 under the care of family physician hospitalists) whose outcomes were 2 standard deviations or more beyond the mean. For example, 1 patient had a rare clotting disorder, stayed in intensive care for 30 days, required an orphan drug at $6000 per dose, and had charges well in excess of $1 million. This study was approved by the Rose Medical Center and Health One Institutional Review Board.
Results
Demographic and clinical characteristics
Table 1 provides the demographic and clinical descriptions of patients admitted by the different admitting physician models. Patients in the different groups were similar, with 2 exceptions: hypertension was significantly more common in the critical care hospitalist group than in the other groups (P < .05), and there was a trend toward more diabetes in the critical care hospitalist group that did not quite reach statistical significance. Nonsignificant trends also existed for PSI, effusion on chest x-ray, and mental status, with more effusions and acute mental status changes occurring in the critical care hospitalist group, more chronic altered mental status in the family physician hospitalist group, and greater severity of illness in the critical care hospitalist group. Otherwise, demographics, disease severity, and comorbidities were comparable.
TABLE 1
Demographic and clinical characteristics
| Admission group | |||
|---|---|---|---|
| Variable | Critical care hospitalists | Family physician hospitalists | Primary care physicians |
| Total† | 22 (21) | 54 (53) | 23 (23) |
| Demographics | |||
| Age, y‡ | 70 (4) | 66 (3) | 67 (4) |
| Male† | 57 (12) | 62 (33) | 48 (11) |
| Female† | 43 (9) | 38 (20) | 52 (12) |
| Comorbidities† | |||
| Hypertension* | 29 (6) | 23 (12) | 54 (12) |
| Diabetes§ | 0 (0) | 9 (5) | 22 (5) |
| Mental status | |||
| Acute changes | 14 (3) | 6 (3) | 0 (0) |
| Chronic changes | 14 (3) | 26 (14) | 17 (4) |
| Effusion on chest x-ray | 33 (7) | 24 (13) | 17 (4) |
| Renal disease | 10 (2) | 6 (3) | 4 (1) |
| Liver disease | 5 (1) | 2 (1) | 4 (1) |
| Cerebrovascular disease | 14 (3) | 11 (6) | 13 (3) |
| Coronary artery disease | 24 (5) | 27 (14) | 22 (5) |
| Heart failure | 24 (5) | 23 (12) | 18 (4) |
| Cancer | 0 (0) | 2 (1) | 4 (1) |
| Nursing home resident | 9 (2) | 4 (2) | 13 (3) |
| Smokers | 19 (4) | 37 (20) | 26 (6) |
| Vital signs/laboratory values‡ | |||
| Heart rate | 92 (5) | 94 (3) | 92 (5) |
| Respiratory rate | 24 (2) | 24 (1) | 23 (2) |
| Systolic blood pressure | 124 (6) | 127 (4) | 136 (6) |
| Temperature (°F) | 99 (0) | 99 (0) | 99 (0) |
| Pulse oximetry | 86 (2) | 88 (1) | 89 (2) |
| Blood urea nitrogen | 20 (3) | 20 (2) | 22 (3) |
| Glucose | 123 (16) | 130 (10) | 154 (16) |
| Hematocrit | 40 (1) | 41 (1) | 39 (1) |
| Sodium | 136 (1) | 136 (1) | 137 (1) |
| Disease severity | |||
| PSI, raw data‡ | 103 (10) | 85 (6) | 99 (9) |
| PSI risk† | |||
| Low | 10 (2) | 24 (13) | 22 (5) |
| Moderate | 29 (6) | 19 (10) | 26 (6) |
| High | 62 (13) | 55 (30) | 52 (12) |
| *P = .024. | |||
| †Percentage (number of patients). | |||
| ‡Mean (± standard deviation). | |||
| §P = .058; otherwise, P > .05 (chi-square for ordinal and categorical variables, analysis of variance for continuous variables). | |||
| PSI, Pneumonia Severity Index. | |||
Primary outcomes
After controlling for severity of illness and intergroup differences, we found that the critical care hospitalist team had the highest mean hospital charge ($10,231), followed by the family physician hospitalist ($7699) and the primary care physician ($5680) groups (Figure 1). The difference in charges between the primary care physician and the critical care hospitalist groups was statistically significant (P = .005) and approached significance between the primary care physician and family physician hospitalist groups (P = .08). The critical care hospitalist and family physician hospitalist groups had longer mean lengths of stay than did the primary care physician group (P = .04 and .01, respectively; Figure 2). The other primary outcomes were rare: 1 primary care physician patient died (4.5%), 2 critical care hospitalist patients died (9.5%) and no family physician hospitalist patients died; no primary care physician patients were readmitted, 1 critical care hospitalist patient was readmitted (4.8%), and 2 family physician hospitalist patients were readmitted (3.8%). There was 1 return to the emergency room in the cohort, in the family physician hospitalist group (1.9%). No intergroup comparisons between these unadjusted rates were statistically significant (P > .05).
FIGURE 1
Hospital charges (in US dollars; with 95% confidence intervals)*
FIGURE 2
Length of stay (in days; with 95% confidence intervals)*
Secondary outcomes
After controlling for severity of illness and intergroup differences, we found that the critical care hospitalists were more likely to obtain 2 or more chest x-rays than the primary care physicians. There were nonsignificant trends toward longer stays in intensive care, greater likelihood of obtaining sputum cultures, and documenting end-of-life counseling by the critical care hospitalists compared with the primary care physicians. For the family physician hospitalists, there were nonsignificant trends toward better compliance with American Thoracic Society antibiotic guidelines and greater likelihood of documenting end-of-life and lifestyle modification counseling compared with the primary care physicians (Table 2).
TABLE 2
Secondary “process of care” outcomes*
| Outcome | Primary care physicians† | Critical care hospitalists | Family physician hospitalists |
|---|---|---|---|
| Chest x-ray (≥2) | 1 | 4.1 (1.1–15.5) | 0.9 (0.3–2.6) |
| ICU stay (≥1 d) | 1 | 2.9 (0.6–14.6) | 0.5 (0.1–3) |
| ATS guideline adherence | 1 | 1.4 (0.4–5.0) | 2.3 (0.8–7.0) |
| Sputum culture obtained | 1 | 2.3 (0.7–8.0) | 0.6 (0.2–1.7) |
| Blood culture obtained | 1 | 1.3 (0.4–4.8) | 1.2 (0.4–3.5) |
| End-of-life counseling documented | 1 | 3.0 (0.6–14.3) | 3.1 (0.7–12.9) |
| Lifestyle modification documented | 1 | 1.1 (0.3–4.5) | 2.7 (0.8–8.7) |
| *Data are presented as odds ratio (95% confidence interval). Odds ratios were adjusted for Pneumonia Severity Index, age, sex, effusion on chest radiography, mental status, hypertension, and diabetes. | |||
| †Reference group. | |||
| ATS, American Thoracic Society; ICU, intensive care unit. | |||
Discussion
Our study provided a unique perspective on the impact of different models of caring for inpatients on the quality, processes, and cost of care. We believe this is the first study to successfully address several methodologic limitations of previous studies: potential time-effect bias, inappropriate controls, differential assignment of house staff and case management resources, unvalidated outcomes, and lack of clinical data.
In addition, we reduced the potential biases inherent in comparing different hospitals and different outpatient physician specialties and used a standardized chart abstraction instrument to avoid the problems inherent in using claims data. As a result, we were able to examine processes of care and use the PSI, an extensively validated tool, to control for disease severity. This study represents an effectiveness study of a real-life intervention by a health maintenance organization to mandate the use of hospitalists. Although the retrospective design of this study may create the potential for bias, there was inadequate advanced notice of the implementation of this hospitalist plan to allow for prospective analysis. Despite not being randomly assigned to 1 of the 3 groups, patients were quite similar with the exceptions of hypertension and possibly diabetes and PSI, which we controlled for in the statistical analysis.
Unfortunately, this was a small study that lacked sufficient power to detect modest differences between groups because the health maintenance organization sponsoring the critical care hospitalist group abandoned the program after 1 year. In addition, the differences in disease severity might have been significant in a larger sample. However, even after controlling for these differences statistically, we found no large differences for mortality, readmission, or returns to the emergency room.
Despite insufficient power to observe statistically significant differences in these relatively rare but important pneumonia outcomes, we did detect a substantial difference in adjusted hospital charges and a modest difference in length of stay. Subspecialist hospitalists had significantly higher adjusted charges than did primary care family physicians. Although the comparison across groups failed to show statistically significant differences, we did see a trend of increasing charges as the degree of hospitalization increased. These higher costs may be explained in part by primary care physicians advising shorter lengths of stay and the subspecialists’ increased use of multiple chest x-rays and trends toward greater use of other resources (eg, intensive care and blood and sputum cultures). Alternatively, some of the difference in charges may reflect differing levels of continuity; the critical care hospitalists had no outpatient continuity with their inpatients, whereas the family physician hospitalists had continuity relationships with some inpatients and the primary care physicians had relationships with all their inpatients. Thus the primary care physicians and, to a lesser extent, the family physician hospitalists may have had information about prior care. Hence, knowledge of previous antibiotic use might argue for the low yield of blood and sputum cultures, and having obtained an outpatient x-ray might obviate the need for another in the hospital. The critical care hospitalists’ increased length of stay and x-ray use, in conjunction with the trend toward greater use of cultures and intensive care, may in turn reflect different degrees of comfort with uncertainty between family physicians and subspecialists. Also, we examined only hospital charges rather than total costs to the system.
Interestingly, we found a trend showing that family physician hospitalists were more likely to document lifestyle modification counseling than were primary care physicians. This result should be interpreted with some caution. Our findings may indicate a true lack of performance by primary care physicians, or they may show a failure to document advice on the hospital chart, reflecting some aspect of the continuity relationship in which such discussions are relegated to the outpatient setting.We also were surprised to see the trend toward decreased end-of-life counseling by the primary care physicians. This could reflect some adverse effect of continuity, the time constraints imposed on nonhospitalists, or not documenting outpatient counseling on the inpatient record.
There were other potential sources of confounding in this study. All patients in the critical care hospitalist group were members of the same health maintenance organization, which may have introduced unmeasured bias despite our attempts to control for differences between groups. Even though we purposefully avoided differential use of house staff, its involvement in each case may have decreased any potential differences across practices.
We draw 2 important conclusions from our results. First, our findings of increased costs and length of stay for mandated hospitalists without significantly different outcomes support the assertion of the American Academy of Family Physicians, the American College of Physicians–American Society of Internal Medicine, the American Medical Association, and the National Association of Inpatient Physicians: the practice of mandating the use of hospitalists should be abandoned pending larger, more comprehensive contemporaneous trials. Second, if hospitalists are to be employed on a voluntary basis, the use of subspecialists rather than generalists may result in more costly care.
Acknowledgments
The authors thank Ralph B. D’Agonstino, Jr., PhD, of the Bowman Gray School of Medicine for his invaluable assistance in statistical methods and Cary Foster, MD, and Promoda Mahupatra, MD, for their collection of the data.
1. Wachter RM. An introduction to the hospitalist model. Ann Intern Med 1999;130:338-42.
2. Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med 2000;109:648-53.
3. Stein MD, Hanson S, Tammaro D, Hanna L, Most AS. Economic effects of community vs hospital-based pneumonia care. J Gen Intern Med 1998;13:774-7.
4. Wachter RM, Katz P, Showstack J, Bindman AB, Goldman L. Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education. JAMA 1998;279:1560-5.
5. Palmer HC, Armistead NS, Elnicki D, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med 2001;111:627-32.
6. Davis KM, Koch KE, Harvey JK, et al. Effects of hospitalists on cost, outcomes, and patient satisfaction in a rural health system. Am J Med 2000;108:621-6.
7. Hackner D, Tu G, Braunstein GD, et al. The value of a hospitalist service: efficient care for the aging population? Chest 2001;119:580-9.
8. Molinari C, Short R. The effects of an HMO-hospitalist program on inpatient utilization. Am J Manag Care 2001;7:1051-17.
9. Wachter RM. An introduction to the hospitalist model. Ann Intern Med 1999;130:338-42.
10. Boschert S. “Hospitalists” may be an emerging specialty. Am Med News July 15, 1997;67.
11. Diamond HS, Goldberg E, Janosky JE. The effect of full-time faculty hospitalists on the efficiency of care at a community teaching hospital. Ann Intern Med 1998;129:197-203.
12. Bellet PS, Whitaker RC. Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges. Pediatrics 2000;105:478-84.
13. Freese RB. Clinical, logistical, and political issues in creating a hospitalist system. Ann Intern Med 1999;130:350-4.
14. Craig D, Hartka L, Likosky WH, et al. Implementation of a hospitalist system in a large health maintenance organization: the Kaiser Permanente experience. Ann Intern Med 1999;130:355-9.
15. Halpert AP, Pearson SD, LeWine HE, Mckean SC. The impact of an inpatient physician program on quality, utilization, and satisfaction. J Manag Care 2000;6:549-55.
16. Tingle LE, Lambert CT. Comparison of a family practice teaching service and a hospitalist model: costs, charges, length of stay, and mortality. Fam Med 2001;33:511-5.
17. Kearns PJ, Wang CC, Morris WJ, et al. Hospital care by hospitalbased and clinic-based faculty: a prospective, controlled trial. Arch Intern Med 2001;161:235-41.
18. Ashton CM, Del Junco DJ, Souchek J, Wray NP, Mansyur CL. The association between the quality of inpatient care and early readmission: a meta-analysis of the evidence. Med Care 1997;35:1044-59.
19. Rhew DC, Goetz MB, Shekelle PG. Evaluating quality indicators for patients with community-acquired pneumonia. Jt Comm J Qual Improv 2001;27:575-90.
20. HCUPnet Halthcare cost and utilization project. Agency for Healthcare Research and Quality, Rockville, MD. June 2002. Available at: http://www.ahrq.gov/data/hcup/hcupnet.htm. Accessed October 8, 2002.
21. Niederman MS, Bass JB, Campbell GD, et al. American Thoracic Society guidelines for the initial management of adults with community-acquired pneumonia: diagnosis, assessment of severity, and initial antimicrobial therapy. Am Rev Respir Dis 1993;148:1418-26.
22. Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify lowrisk patients with community-acquired pneumonia. N Engl J Med 1997;336:243-50.
23. Ewig S, Kleinfeld T, Bauer T, Seifert K, Schafer H, Goke N. Comparative validation of prognostic rules for community-acquired pneumonia in an elderly population. Eur Respir J 1999;14:370-5.
1. Wachter RM. An introduction to the hospitalist model. Ann Intern Med 1999;130:338-42.
2. Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med 2000;109:648-53.
3. Stein MD, Hanson S, Tammaro D, Hanna L, Most AS. Economic effects of community vs hospital-based pneumonia care. J Gen Intern Med 1998;13:774-7.
4. Wachter RM, Katz P, Showstack J, Bindman AB, Goldman L. Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education. JAMA 1998;279:1560-5.
5. Palmer HC, Armistead NS, Elnicki D, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med 2001;111:627-32.
6. Davis KM, Koch KE, Harvey JK, et al. Effects of hospitalists on cost, outcomes, and patient satisfaction in a rural health system. Am J Med 2000;108:621-6.
7. Hackner D, Tu G, Braunstein GD, et al. The value of a hospitalist service: efficient care for the aging population? Chest 2001;119:580-9.
8. Molinari C, Short R. The effects of an HMO-hospitalist program on inpatient utilization. Am J Manag Care 2001;7:1051-17.
9. Wachter RM. An introduction to the hospitalist model. Ann Intern Med 1999;130:338-42.
10. Boschert S. “Hospitalists” may be an emerging specialty. Am Med News July 15, 1997;67.
11. Diamond HS, Goldberg E, Janosky JE. The effect of full-time faculty hospitalists on the efficiency of care at a community teaching hospital. Ann Intern Med 1998;129:197-203.
12. Bellet PS, Whitaker RC. Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges. Pediatrics 2000;105:478-84.
13. Freese RB. Clinical, logistical, and political issues in creating a hospitalist system. Ann Intern Med 1999;130:350-4.
14. Craig D, Hartka L, Likosky WH, et al. Implementation of a hospitalist system in a large health maintenance organization: the Kaiser Permanente experience. Ann Intern Med 1999;130:355-9.
15. Halpert AP, Pearson SD, LeWine HE, Mckean SC. The impact of an inpatient physician program on quality, utilization, and satisfaction. J Manag Care 2000;6:549-55.
16. Tingle LE, Lambert CT. Comparison of a family practice teaching service and a hospitalist model: costs, charges, length of stay, and mortality. Fam Med 2001;33:511-5.
17. Kearns PJ, Wang CC, Morris WJ, et al. Hospital care by hospitalbased and clinic-based faculty: a prospective, controlled trial. Arch Intern Med 2001;161:235-41.
18. Ashton CM, Del Junco DJ, Souchek J, Wray NP, Mansyur CL. The association between the quality of inpatient care and early readmission: a meta-analysis of the evidence. Med Care 1997;35:1044-59.
19. Rhew DC, Goetz MB, Shekelle PG. Evaluating quality indicators for patients with community-acquired pneumonia. Jt Comm J Qual Improv 2001;27:575-90.
20. HCUPnet Halthcare cost and utilization project. Agency for Healthcare Research and Quality, Rockville, MD. June 2002. Available at: http://www.ahrq.gov/data/hcup/hcupnet.htm. Accessed October 8, 2002.
21. Niederman MS, Bass JB, Campbell GD, et al. American Thoracic Society guidelines for the initial management of adults with community-acquired pneumonia: diagnosis, assessment of severity, and initial antimicrobial therapy. Am Rev Respir Dis 1993;148:1418-26.
22. Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify lowrisk patients with community-acquired pneumonia. N Engl J Med 1997;336:243-50.
23. Ewig S, Kleinfeld T, Bauer T, Seifert K, Schafer H, Goke N. Comparative validation of prognostic rules for community-acquired pneumonia in an elderly population. Eur Respir J 1999;14:370-5.