User login
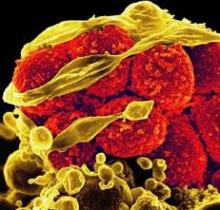
SAN DIEGO – Nasal colonization of methicillin-resistant Staphylococcus aureus was linked to an increase in surgical site infections and longer hospital stays in patients undergoing major gastrointestinal surgery in a large retrospective study, a finding that surprised investigators who had hypothesized that nasal colonization of the organism, which is not routinely found or colonized in the GI tract, would have little impact on outcome measures.
"Gastrointestinal operations are different from other surgeries in that infectious pathogens are typically organisms found in the gut, not bacteria that colonize in the skin, which is why we didn’t expect to find a correlation," lead investigator Dr. Harry T. Papaconstantinou said during a teleconference reporting the results, which he presented on Sunday, May 20, at the annual Digestive Disease Week conference.
While it’s unlikely that nasal colonization of MRSA necessarily increases the risk of developing a surgical site infection following GI surgery, "it is possible that it might be an indicator of the type of organism that is involved in the infection." For example, in the current analysis, wound culture data were available for 92 patients. In patients who tested positive for MRSA, 70% of the wound infections stemmed from MRSA, compared with only 8.5% in of those who tested negative, he said.
To evaluate the relationship between MRSA nasal colonization and surgical site infection, wound cultures, hospital length of stay, and mortality, Dr. Papaconstantinou, chief of colorectal surgery at Scott and White Memorial Hospital in Temple, Tex., and his colleagues examined the records of patients who underwent major GI surgery at the hospital between December 2007 and August 2009. The patients, who also had nasal swab tests within 24-48 hours after admission, were divided into one of three categories: MRSA-swab positive, methicillin-sensitive Staphylococcus aureus (MSSA)–swab positive, or negative for both.
Of the 1,137 patients, mean age 59.5 years, 73 (6.4%) were MRSA-swab positive, 167 (14.7%) were MSSA-swab positive, and 897 (78.9%) were negative, Dr. Papaconstantinou reported. Surgical site infection was identified in 101 patients (8.9%), and the rate of infection was highest, at 14%, in the MRSA-swab positive patients, compared with 4% and 9%, respectively, in the MSSA-swab positive and negative patients, he said. "When we controlled for other confounding factors, we didn’t find nasal swab to be an independent predictor of surgical site infection, but what we did find was a strong relationship between MRSA-positive nasal colonization and type of organism involved [in the surgical site infection]."
Regarding mean hospital length of stay, the respective durations for the MRSA-swab positive, MSSA-swab positive, and the negative groups overall were 12.5 days, 7.6 days, and 8.8 days, representing a significant increase, said Dr. Papaconstantinou. "By multiregression analysis, we found a MRSA-positive swab to be an independent risk factor for extended length of stay." However, when looking specifically at patients with surgical site infections, the presence of which increased hospital length of stay significantly from 6.2 days to 15.7 days, "there was no between group differences based on nasal swab," he said. Similarly, the 45 deaths in the study population wee distributed evenly across the nasal swab groups.
Based on the findings, Dr. Papaconstantinou said in an interview, "we can conclude that a positive MRSA nasal swab test for colonization is a strong predictor that MRSA-associated surgical site infections will occur in patients undergoing major GI surgery." As such, "we propose the possibility that it might be beneficial to preoperatively screen and decolonize these patients in an effort to reduce the incidence of these infections and improve patient outcomes following surgery." Toward this end, he and his colleagues are anticipating performing such a study and plan on including a cost-benefit analysis to determine whether screening is economically beneficial, he said.
Dr. Papaconstantinou disclosed a financial relationship with Covidien.
SAN DIEGO – Nasal colonization of methicillin-resistant Staphylococcus aureus was linked to an increase in surgical site infections and longer hospital stays in patients undergoing major gastrointestinal surgery in a large retrospective study, a finding that surprised investigators who had hypothesized that nasal colonization of the organism, which is not routinely found or colonized in the GI tract, would have little impact on outcome measures.
"Gastrointestinal operations are different from other surgeries in that infectious pathogens are typically organisms found in the gut, not bacteria that colonize in the skin, which is why we didn’t expect to find a correlation," lead investigator Dr. Harry T. Papaconstantinou said during a teleconference reporting the results, which he presented on Sunday, May 20, at the annual Digestive Disease Week conference.
While it’s unlikely that nasal colonization of MRSA necessarily increases the risk of developing a surgical site infection following GI surgery, "it is possible that it might be an indicator of the type of organism that is involved in the infection." For example, in the current analysis, wound culture data were available for 92 patients. In patients who tested positive for MRSA, 70% of the wound infections stemmed from MRSA, compared with only 8.5% in of those who tested negative, he said.
To evaluate the relationship between MRSA nasal colonization and surgical site infection, wound cultures, hospital length of stay, and mortality, Dr. Papaconstantinou, chief of colorectal surgery at Scott and White Memorial Hospital in Temple, Tex., and his colleagues examined the records of patients who underwent major GI surgery at the hospital between December 2007 and August 2009. The patients, who also had nasal swab tests within 24-48 hours after admission, were divided into one of three categories: MRSA-swab positive, methicillin-sensitive Staphylococcus aureus (MSSA)–swab positive, or negative for both.
Of the 1,137 patients, mean age 59.5 years, 73 (6.4%) were MRSA-swab positive, 167 (14.7%) were MSSA-swab positive, and 897 (78.9%) were negative, Dr. Papaconstantinou reported. Surgical site infection was identified in 101 patients (8.9%), and the rate of infection was highest, at 14%, in the MRSA-swab positive patients, compared with 4% and 9%, respectively, in the MSSA-swab positive and negative patients, he said. "When we controlled for other confounding factors, we didn’t find nasal swab to be an independent predictor of surgical site infection, but what we did find was a strong relationship between MRSA-positive nasal colonization and type of organism involved [in the surgical site infection]."
Regarding mean hospital length of stay, the respective durations for the MRSA-swab positive, MSSA-swab positive, and the negative groups overall were 12.5 days, 7.6 days, and 8.8 days, representing a significant increase, said Dr. Papaconstantinou. "By multiregression analysis, we found a MRSA-positive swab to be an independent risk factor for extended length of stay." However, when looking specifically at patients with surgical site infections, the presence of which increased hospital length of stay significantly from 6.2 days to 15.7 days, "there was no between group differences based on nasal swab," he said. Similarly, the 45 deaths in the study population wee distributed evenly across the nasal swab groups.
Based on the findings, Dr. Papaconstantinou said in an interview, "we can conclude that a positive MRSA nasal swab test for colonization is a strong predictor that MRSA-associated surgical site infections will occur in patients undergoing major GI surgery." As such, "we propose the possibility that it might be beneficial to preoperatively screen and decolonize these patients in an effort to reduce the incidence of these infections and improve patient outcomes following surgery." Toward this end, he and his colleagues are anticipating performing such a study and plan on including a cost-benefit analysis to determine whether screening is economically beneficial, he said.
Dr. Papaconstantinou disclosed a financial relationship with Covidien.
SAN DIEGO – Nasal colonization of methicillin-resistant Staphylococcus aureus was linked to an increase in surgical site infections and longer hospital stays in patients undergoing major gastrointestinal surgery in a large retrospective study, a finding that surprised investigators who had hypothesized that nasal colonization of the organism, which is not routinely found or colonized in the GI tract, would have little impact on outcome measures.
"Gastrointestinal operations are different from other surgeries in that infectious pathogens are typically organisms found in the gut, not bacteria that colonize in the skin, which is why we didn’t expect to find a correlation," lead investigator Dr. Harry T. Papaconstantinou said during a teleconference reporting the results, which he presented on Sunday, May 20, at the annual Digestive Disease Week conference.
While it’s unlikely that nasal colonization of MRSA necessarily increases the risk of developing a surgical site infection following GI surgery, "it is possible that it might be an indicator of the type of organism that is involved in the infection." For example, in the current analysis, wound culture data were available for 92 patients. In patients who tested positive for MRSA, 70% of the wound infections stemmed from MRSA, compared with only 8.5% in of those who tested negative, he said.
To evaluate the relationship between MRSA nasal colonization and surgical site infection, wound cultures, hospital length of stay, and mortality, Dr. Papaconstantinou, chief of colorectal surgery at Scott and White Memorial Hospital in Temple, Tex., and his colleagues examined the records of patients who underwent major GI surgery at the hospital between December 2007 and August 2009. The patients, who also had nasal swab tests within 24-48 hours after admission, were divided into one of three categories: MRSA-swab positive, methicillin-sensitive Staphylococcus aureus (MSSA)–swab positive, or negative for both.
Of the 1,137 patients, mean age 59.5 years, 73 (6.4%) were MRSA-swab positive, 167 (14.7%) were MSSA-swab positive, and 897 (78.9%) were negative, Dr. Papaconstantinou reported. Surgical site infection was identified in 101 patients (8.9%), and the rate of infection was highest, at 14%, in the MRSA-swab positive patients, compared with 4% and 9%, respectively, in the MSSA-swab positive and negative patients, he said. "When we controlled for other confounding factors, we didn’t find nasal swab to be an independent predictor of surgical site infection, but what we did find was a strong relationship between MRSA-positive nasal colonization and type of organism involved [in the surgical site infection]."
Regarding mean hospital length of stay, the respective durations for the MRSA-swab positive, MSSA-swab positive, and the negative groups overall were 12.5 days, 7.6 days, and 8.8 days, representing a significant increase, said Dr. Papaconstantinou. "By multiregression analysis, we found a MRSA-positive swab to be an independent risk factor for extended length of stay." However, when looking specifically at patients with surgical site infections, the presence of which increased hospital length of stay significantly from 6.2 days to 15.7 days, "there was no between group differences based on nasal swab," he said. Similarly, the 45 deaths in the study population wee distributed evenly across the nasal swab groups.
Based on the findings, Dr. Papaconstantinou said in an interview, "we can conclude that a positive MRSA nasal swab test for colonization is a strong predictor that MRSA-associated surgical site infections will occur in patients undergoing major GI surgery." As such, "we propose the possibility that it might be beneficial to preoperatively screen and decolonize these patients in an effort to reduce the incidence of these infections and improve patient outcomes following surgery." Toward this end, he and his colleagues are anticipating performing such a study and plan on including a cost-benefit analysis to determine whether screening is economically beneficial, he said.
Dr. Papaconstantinou disclosed a financial relationship with Covidien.
NEWS FROM DIGESTIVE DISEASE WEEK
Major Finding: The surgical site infection rate following major gastrointestinal surgery was 13.7% among patients with positive nasal swab results for MRSA, compared with 4.2% for patients testing positive for MSSA and 9.4% for patients with negative swabs. In patients with for whom wound culture data was available, the rate of MRSA-positive cultures was significantly higher, at 70%, in the MRSA-swab positive group, compared with 8.5% in noncolonized patients.
Data Source: Data were taken from retrospective analysis of medical records for 1,137 patients who underwent major gastrointestinal surgery and had nasal swab tests at Scott and White Memorial Hospital between December 2007 and August 2009. Wound culture data were available for 92 patients.
Disclosures: Dr. Papaconstantinou disclosed a financial relationship with Covidien.