User login
Lung transplant is the therapy of choice for a growing number of patients with end-stage lung diseases. Patients receiving a lung transplant are faced with many challenges including drug toxicities, infections, and the risk of rejection.1 Despite these challenges, lung transplant may significantly prolong survival and improve quality of life for many patients.
CANDIDATES FOR LUNG TRANSPLANT
Identifying patients who are appropriate candidates for lung transplant is important to achieving favorable transplant outcomes and to maximizing life expectancy for each patient. The most recent edition of International Society for Heart and Lung Transplant (ISHLT) Guidelines for the Selection of Lung Transplant Candidates is an excellent guide to help physicians identify when to refer potential patients and to how to identify patients who are the most likely to benefit from lung transplant.2
Adults with end-stage lung disease are generally candidates for lung transplant if they meet the following criteria:
- A greater than 50% risk of death from lung disease within 2 years if a lung transplant is not performed
- A greater than 80% likelihood of surviving at least 90 days after the lung transplant procedure
- A greater than 80% likelihood of a 5-year survival posttransplant if graft function is preserved.2
These can only be estimated by transplant programs and not by the referring team in most cases.
Once a patient is identified as a candidate for lung transplant, early referral of patients to a lung transplant program has several advantages and is essential for positive outcomes. Early patient referral allows for timely completion of the formal evaluation of candidacy, patient and family education, as well as the opportunity for the patient and family to raise funds or use other resources to overcome financial hurdles. Listing a patient on the transplant waitlist implies that the patient has a limited life expectancy without a lung transplant and that the risk-benefit ratio favors lung transplant since all other medical options have been exhausted.1
NONCANDIDATES FOR LUNG TRANSPLANT
There are very few absolute contraindications to lung transplant. Generally, most transplant centers in the United States agree that contraindications to lung transplant include conditions associated with increased risk of mortality, including:
- A recent history of a major malignancy. Patients with a 2-year, disease-free interval combined with a low predicted risk of recurrence may be considered in certain cases of localized, non-melanoma skin cancer. A 5-year, disease-free survival is strongly suggested in patients with a history of breast, bladder, or kidney cancer as well as in cases of sarcoma, melanoma, lymphoma and certain hematologic disorders.
- The presence of significant dysfunction of another major organ systems including the heart, liver, kidney, or brain unless a combined organ transplant can be considered and performed.
- Significant coronary heart disease not amenable to revascularization or intervention prior to or at the time of lung transplant.
- The presence of an acute medical condition including but not limited to sepsis and acute liver failure.
- Active Mycobacterium tuberculosis and other highly virulent or highly resistant microbes that are poorly controlled pretransplant.
- Severe obesity with a body mass index greater than 35.
- A history of nonadherence to medical therapy, psychiatric or psychological conditions that might lead to nonadherence, poor or limited social support system, and limited functional status not amenable to rehabilitation.
- Current substance abuse or dependence, including illicit substances, alcohol, and tobacco (nicotine-containing substances). Most centers require at least 6 months’ abstinence from illicit substances prior to being added to the lung transplant waitlist.2
CANDIDATE COMORBIDITIES
Age
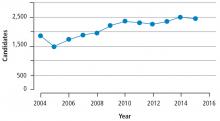
Many transplant centers in the US define the age cutoff for lung transplant at 65; however, some centers may consider candidates older than 65. Advanced age by itself should not be considered a contraindication to lung transplant. However, increased age is usually associated with other comorbid conditions that may increase perioperative and long-term morbidity and mortality. As mentioned previously, the number of older candidates for lung transplant has increased. In the US, 29% of the patients on the national waiting list in 2015 were over age 65.4
Past chest surgery
It is not uncommon for lung transplant candidates to have a history of chest surgery such as lung resection, pleurodesis, or coronary artery bypass grafting. The limited literature regarding the outcomes for these patients suggests they may experience higher rates of bleeding, re-exploration, and renal dysfunction.2 However, these patients should not be excluded from lung transplant and successful transplant outcomes have been achieved in this population by experienced centers.5 In candidates with a history of chronic obstructive pulmonary disease (COPD) and lung-volume reduction surgery (LVRS), early case series indicate that these patients did well after lung transplant.6 However, more recent data demonstrate that patients with prior LVRS who undergo lung transplant experience higher rates of bleeding, worse early graft dysfunction, and worse outcomes overall.7 As with lung transplant candidates with previous chest surgery, lung transplant candidates with previous LVRS are best served by experienced transplant centers.
Hepatitis and HIV
Patients with a history of infection with hepatitis B, hepatitis C, or human immunodeficiency virus (HIV) are candidates for lung transplant at centers experienced with lung transplant in patients with these infections. Most centers advocate that patients with a history of hepatitis B or C have viral infection levels that are controlled or reduced as low as possible and that there is no evidence of portal hypertension or severe cirrhosis.8,9 In the case of HIV, patients should have controlled disease with a negative or undetectable viral load and have no current acquired immunodeficiency defining illness.10 Patients colonized with particular species of Burkholderia cepacia or Mycobacterium abscessus subspecies can be considered for lung transplant only at centers with established preoperative and postoperative protocols for these infections due to the increased risk of perioperative mortality associated with these organisms.11,12
DISEASE-SPECIFIC INDICATIONS
Chronic obstructive pulmonary disease
COPD (both non- and alpha-1 antitrypsin deficiency) is the most common indication for lung transplant and accounts for almost 32% of lung transplants worldwide.13 Patients should be referred for lung transplant when medical therapies, surgical interventions (ie, LVRS) and pulmonary rehabilitation have been maximized. In COPD, the loss of lung function occurs over a long period of time but patients are often more limited by diminished quality of life as lung function slowly declines.
Patients with COPD should be referred for lung transplant if the body mass index, airflow obstruction, dyspnea, and exercise capacity (BODE) index is 5 to 6.2 The original BODE index developed by Celli et al,14 is a scoring system from 0 to 10 with a higher score indicating more severe disease and worse survival. A score of 5 to 6 indicates an estimated mortality of 60% at 4 yrs.2,14,15 Other considerations for referral for lung transplant include the presence of hypercapnia with partial pressure of carbon dioxide greater than 50 mm Hg or higher or hypoxemia with partial pressure of oxygen less than 60 mm Hg or a forced expiratory volume at 1 sec (FEV1) less than 25% predicted.
Patients with COPD should considered for listing for lung transplant if any one of the following criteria is met: BODE index of 7 or greater; FEV1 less than 15% to 20%; 3 of more severe exacerbations during the preceding year; 1 severe exacerbation with acute hypercapnic respiratory failure; or presence of moderate to severe pulmonary hypertension.2,16
Cystic fibrosis
In patients with cystic fibrosis, lung transplant should be considered in patients with an estimated 2-year survival of less than 50% and with a New York Heart Association (NYHA) Functional Classification III or IV. Referral for lung transplant is recommended for patients with a rapid decrease in FEV1 despite optimal therapy, female patients with declining weight and lung function, colonization or infection with nontuberculous mycobacterial disease, or cystic fibrosis-related diabetes. The development of pulmonary hypertension, reduction in walk distance, increasing antibiotic resistance, acute respiratory failure requiring noninvasive ventilation, worsening nutritional status, pneumothorax, and life-threatening hemoptysis despite embolization are all indications for referral for lung transplant.
Patients with cystic fibrosis with hypoxia or hypercapnia with declining lung function, needing long-term noninvasive ventilation, having more frequent exacerbations or exhibiting a decline in functional status should be listed for lung transplant.2,17–19
Restrictive lung disease
Patients with restrictive lung diseases, including interstitial pulmonary fibrosis (usual interstitial pneumonitis, nonspecific interstitial pneumonia), or interstitial lung disease, and hypersensitivity pneumonitis, should be referred for transplant evaluation at the time of diagnosis irrespective of lung function due to the unpredictable nature of these diseases.20 Some clinicians may advocate for a trial of medical therapy with antifibrotics, but this should be done in conjunction with transplant referral.
Patients should be listed for transplant if a 10% or greater decrease in FEV1 occurred in the past 6 months (of note, even a 5% decrease in FEV1 is associated with an overall poorer prognosis and warrants consideration of listing for transplant), if the diffusing capacity of the lung for carbon monoxide decreases 15% or greater during the 6-month follow-up, or if a decline of more than 50 meters is noted on the 6-minute walking test. A documented desaturation of less than 88% or a distance of less than 250 meters on the 6-minute walking test is another indication for listing. Any evidence of secondary pulmonary hypertension on right heart catheterization or on echocardiography or hospitalization for respiratory decline are also indications for listing.21 In cases of scleroderma-associated interstitial lung disease or mixed connective tissue interstitial lung disease, similar guidelines for referral and listing should be followed.2
Pulmonary arterial hypertension
Patients with pulmonary arterial hypertension should be referred for lung transplant if any 1 of the following conditions is present: rapidly progressive disease; NYHA Functional Classification III or IV symptoms during escalating therapy; use of parenteral pulmonary arterial hypertension therapy; or known or suspected pulmonary veno-occlusive disease or pulmonary capillary hemangiomatosis.2,22
Patients with pulmonary arterial hypertension should be listed for lung transplant if any of the following are present: NYHA Functional Classification III or IV symptoms despite combination therapy; right heart catheterization demonstrating a cardiac index less than 2 L/min/m2; mean right atrial pressure greater than 15 mm Hg; 6-minute walking test less than 350 meters; or development of pericardial effusion, hemoptysis, or signs of worsening right heart failure, including renal insufficiency, rising bilirubin or evidence of ascites.2,22
BRIDGE TO TRANSPLANT
Acute respiratory decompensation may occur in some candidates for lung transplant prior to listing for transplant or while on the transplant waitlist. In patients with failure of a single lung, a bridge to transplant may be necessary until a suitable organ is available. Mechanical ventilation and extracorporeal life support (ECLS) are 2 bridge strategies for lung transplant candidates. Mechanical ventilation is the most common lung transplant bridge strategy but it is less than ideal because it can lead to deconditioning and ventilator-associated infections that can negatively impact a patient’s suitability for transplant.
ECLS techniques that allow spontaneous breathing and potentially ambulation, known as awake or ambulatory ECLS, is a popular bridge therapy. Ambulatory ECLS is used as an alternative to mechanical ventilation to avoid the complications of mechanical ventilation and allow patients to avoid sedation and participate in rehabilitation.23 Irrespective of the therapy used as a bridge to transplant, patients considered for a bridge are optimally evaluated from a medical and psychosocial perspective prior to bridge therapy.
Both bridge therapies increase the risk of infection, bleeding, and neurologic events; thus, patients need to be assessed repeatedly for these risks to determine ongoing suitability for lung transplant. It is important to note that delayed referral of patients with advanced disease or patients in an acute exacerbation negatively impacts the evaluation for lung transplant, placement on the lung transplant waitlist, outcomes, and suitability for bridge transplant strategies.
CONCLUSION
To ensure good patient outcomes, the evaluation and selection of candidates for lung transplant requires communication between referring physicians and lung transplant centers. Physicians need basic knowledge of patient conditions appropriate for lung transplant and direct communication with lung transplant centers. The workup, required testing, and timing of listing for lung transplant varies among transplant centers across the country, making communication between the referring providers and transplant centers crucial to good patient care. An open, 2-way dialogue between referring providers and transplant centers facilitates listing patients for transplant in a timely manner, reduces delays, and improves outcomes.
- Kreider M, Hadjiliadis D, Kotloff R. Candidate selection, timing of listing, and choice of procedure for lung transplantation. Clin Chest Med 2011; 32:199–211.
- Weill D, Benden C, Corris P, et al. A consensus document for the selection of lung transplant candidates: 2014—An update from the Pulmonary Transplant Council of the International Society of Heart and Lung Transplantation. J Heart Lung Transplant 2015; 34:1–15.
- Tsuang WM. Contemporary issues in lung transplant allocation practices. Curr Transplant Rep 2017; 4:238–242.
- Valapour M, Skeans MA, Smith JM, et al. OPTN/SRTR 2015 annual data report: lung. Am J Transplant 2017; 17(suppl 1):357–424.
- Omara M, Okamoto T, Arafat A, Thuita L, Blackstone EH, McCurry KR. Lung transplantation in patients who have undergone prior cardiothoracic procedures. J Heart Lung Transplant 2016; 35:1462–1470.
- Senbaklavaci O, Wisser W, Ozpeker C, et al. Successful lung volume reduction surgery brings patients into better condition for later lung transplantation. Eur J Cardiothorac Surg 2002; 22:363–367.
- Shigemura N, Gilbert S, Bhama JK et al. Lung transplantation after lung volume reduction surgery. Transplantation 2013; 96:421–425.
- Sahi H, Zein NN, Mehta AC, Blazey HC, Meyer KH, Budev M. Outcomes after lung transplantation in patients with chronic hepatitis C virus infection. J Heart Lung Transplant 2007; 26:466–471.
- Kim EY, Ko HH, Yoshida EM. A concise review of hepatitis C in heart and lung transplantation. Can J Gastroenterol 2011; 25:445–448.
- Kern RM, Seethamraju H, Blanc PD, et al. The feasibility of lung transplantation in HIV-seropositive patients. Ann Am Thorac Soc 2014; 11:882–889.
- De Soyza A, Corris A, McDowell A, Archer L, et al. Burkholderia cepacia complex genomovars and pulmonary transplant outcomes in patients with cystic fibrosis. Lancet 2001; 358:1780–1781.
- De Soyza A, Meachery G, Hester HL, et al. Lung transplant for patients with cystic fibrosis and Burkholderia cepacia complex infection: a single center experience. J Heart Lung Transplant 2010; 29:1395–1404.
- Yusen RD, Edwards LB, Kucheryavaya AY, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-second official adult and heart-lung transplantation report—2015; focus theme: early graft failure. J Heart Lung Transplant 2015; 34:1264–1277.
- Celli BR, Cote CG, Marin JM, et al. The body–mass index, airflow obstruction, dyspna and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004; 350:1005–1012.
- Marchand E. The BODE index as a tool to predict survival in COPD lung transplant candidates. Eur Respir J 2010; 36:1494–1495.
- Lahzami S, Bridevaux PO, Soccal PM, et al. Survival impact of lung transplant for COPD. Eur Respir J 2010; 36:74–80.
- Rosenbluth DB, Wilson K, Ferkol T, Schuster DP. Lung function decline in cystic fibrosis patients and timing for lung transplantation referral. Chest 2004; 126:412–419.
- Mayer-Hamblett N, Rosenfield M, Emerson J, Goss CH, Aitken ML. Developing cystic fibrosis lung transplant referral criteria using predictors of 2-year mortality. Am J Respir Crit Care Med 2002; 166:1550–1556.
- Liou TG, Adler FR, Cahill BC, et al. Survival effect of lung transplantation among patients with cystic fibrosis. JAMA 2001; 286:2683–2689.
- Raghu G, Collard HR, Egan JJ, et al; ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidenced-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011; 183:788–824.
- Collard HR, King TE Jr, Bartelson BB, Vourlekis JS, Schwarz MI, Brown KK. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2003; 168:538–542.
- Edelman, JD. Navigating the road to transplantation for pulmonary arterial hypertension. Advances in Pulmonary Hypertension 2016; 15:14–18.
- Strueber M. Bridges to lung transplant. Curr Opin Organ Transplant 2011; 16:458–461.
Lung transplant is the therapy of choice for a growing number of patients with end-stage lung diseases. Patients receiving a lung transplant are faced with many challenges including drug toxicities, infections, and the risk of rejection.1 Despite these challenges, lung transplant may significantly prolong survival and improve quality of life for many patients.
CANDIDATES FOR LUNG TRANSPLANT
Identifying patients who are appropriate candidates for lung transplant is important to achieving favorable transplant outcomes and to maximizing life expectancy for each patient. The most recent edition of International Society for Heart and Lung Transplant (ISHLT) Guidelines for the Selection of Lung Transplant Candidates is an excellent guide to help physicians identify when to refer potential patients and to how to identify patients who are the most likely to benefit from lung transplant.2
Adults with end-stage lung disease are generally candidates for lung transplant if they meet the following criteria:
- A greater than 50% risk of death from lung disease within 2 years if a lung transplant is not performed
- A greater than 80% likelihood of surviving at least 90 days after the lung transplant procedure
- A greater than 80% likelihood of a 5-year survival posttransplant if graft function is preserved.2
These can only be estimated by transplant programs and not by the referring team in most cases.
Once a patient is identified as a candidate for lung transplant, early referral of patients to a lung transplant program has several advantages and is essential for positive outcomes. Early patient referral allows for timely completion of the formal evaluation of candidacy, patient and family education, as well as the opportunity for the patient and family to raise funds or use other resources to overcome financial hurdles. Listing a patient on the transplant waitlist implies that the patient has a limited life expectancy without a lung transplant and that the risk-benefit ratio favors lung transplant since all other medical options have been exhausted.1
NONCANDIDATES FOR LUNG TRANSPLANT
There are very few absolute contraindications to lung transplant. Generally, most transplant centers in the United States agree that contraindications to lung transplant include conditions associated with increased risk of mortality, including:
- A recent history of a major malignancy. Patients with a 2-year, disease-free interval combined with a low predicted risk of recurrence may be considered in certain cases of localized, non-melanoma skin cancer. A 5-year, disease-free survival is strongly suggested in patients with a history of breast, bladder, or kidney cancer as well as in cases of sarcoma, melanoma, lymphoma and certain hematologic disorders.
- The presence of significant dysfunction of another major organ systems including the heart, liver, kidney, or brain unless a combined organ transplant can be considered and performed.
- Significant coronary heart disease not amenable to revascularization or intervention prior to or at the time of lung transplant.
- The presence of an acute medical condition including but not limited to sepsis and acute liver failure.
- Active Mycobacterium tuberculosis and other highly virulent or highly resistant microbes that are poorly controlled pretransplant.
- Severe obesity with a body mass index greater than 35.
- A history of nonadherence to medical therapy, psychiatric or psychological conditions that might lead to nonadherence, poor or limited social support system, and limited functional status not amenable to rehabilitation.
- Current substance abuse or dependence, including illicit substances, alcohol, and tobacco (nicotine-containing substances). Most centers require at least 6 months’ abstinence from illicit substances prior to being added to the lung transplant waitlist.2
CANDIDATE COMORBIDITIES
Age
Many transplant centers in the US define the age cutoff for lung transplant at 65; however, some centers may consider candidates older than 65. Advanced age by itself should not be considered a contraindication to lung transplant. However, increased age is usually associated with other comorbid conditions that may increase perioperative and long-term morbidity and mortality. As mentioned previously, the number of older candidates for lung transplant has increased. In the US, 29% of the patients on the national waiting list in 2015 were over age 65.4
Past chest surgery
It is not uncommon for lung transplant candidates to have a history of chest surgery such as lung resection, pleurodesis, or coronary artery bypass grafting. The limited literature regarding the outcomes for these patients suggests they may experience higher rates of bleeding, re-exploration, and renal dysfunction.2 However, these patients should not be excluded from lung transplant and successful transplant outcomes have been achieved in this population by experienced centers.5 In candidates with a history of chronic obstructive pulmonary disease (COPD) and lung-volume reduction surgery (LVRS), early case series indicate that these patients did well after lung transplant.6 However, more recent data demonstrate that patients with prior LVRS who undergo lung transplant experience higher rates of bleeding, worse early graft dysfunction, and worse outcomes overall.7 As with lung transplant candidates with previous chest surgery, lung transplant candidates with previous LVRS are best served by experienced transplant centers.
Hepatitis and HIV
Patients with a history of infection with hepatitis B, hepatitis C, or human immunodeficiency virus (HIV) are candidates for lung transplant at centers experienced with lung transplant in patients with these infections. Most centers advocate that patients with a history of hepatitis B or C have viral infection levels that are controlled or reduced as low as possible and that there is no evidence of portal hypertension or severe cirrhosis.8,9 In the case of HIV, patients should have controlled disease with a negative or undetectable viral load and have no current acquired immunodeficiency defining illness.10 Patients colonized with particular species of Burkholderia cepacia or Mycobacterium abscessus subspecies can be considered for lung transplant only at centers with established preoperative and postoperative protocols for these infections due to the increased risk of perioperative mortality associated with these organisms.11,12
DISEASE-SPECIFIC INDICATIONS
Chronic obstructive pulmonary disease
COPD (both non- and alpha-1 antitrypsin deficiency) is the most common indication for lung transplant and accounts for almost 32% of lung transplants worldwide.13 Patients should be referred for lung transplant when medical therapies, surgical interventions (ie, LVRS) and pulmonary rehabilitation have been maximized. In COPD, the loss of lung function occurs over a long period of time but patients are often more limited by diminished quality of life as lung function slowly declines.
Patients with COPD should be referred for lung transplant if the body mass index, airflow obstruction, dyspnea, and exercise capacity (BODE) index is 5 to 6.2 The original BODE index developed by Celli et al,14 is a scoring system from 0 to 10 with a higher score indicating more severe disease and worse survival. A score of 5 to 6 indicates an estimated mortality of 60% at 4 yrs.2,14,15 Other considerations for referral for lung transplant include the presence of hypercapnia with partial pressure of carbon dioxide greater than 50 mm Hg or higher or hypoxemia with partial pressure of oxygen less than 60 mm Hg or a forced expiratory volume at 1 sec (FEV1) less than 25% predicted.
Patients with COPD should considered for listing for lung transplant if any one of the following criteria is met: BODE index of 7 or greater; FEV1 less than 15% to 20%; 3 of more severe exacerbations during the preceding year; 1 severe exacerbation with acute hypercapnic respiratory failure; or presence of moderate to severe pulmonary hypertension.2,16
Cystic fibrosis
In patients with cystic fibrosis, lung transplant should be considered in patients with an estimated 2-year survival of less than 50% and with a New York Heart Association (NYHA) Functional Classification III or IV. Referral for lung transplant is recommended for patients with a rapid decrease in FEV1 despite optimal therapy, female patients with declining weight and lung function, colonization or infection with nontuberculous mycobacterial disease, or cystic fibrosis-related diabetes. The development of pulmonary hypertension, reduction in walk distance, increasing antibiotic resistance, acute respiratory failure requiring noninvasive ventilation, worsening nutritional status, pneumothorax, and life-threatening hemoptysis despite embolization are all indications for referral for lung transplant.
Patients with cystic fibrosis with hypoxia or hypercapnia with declining lung function, needing long-term noninvasive ventilation, having more frequent exacerbations or exhibiting a decline in functional status should be listed for lung transplant.2,17–19
Restrictive lung disease
Patients with restrictive lung diseases, including interstitial pulmonary fibrosis (usual interstitial pneumonitis, nonspecific interstitial pneumonia), or interstitial lung disease, and hypersensitivity pneumonitis, should be referred for transplant evaluation at the time of diagnosis irrespective of lung function due to the unpredictable nature of these diseases.20 Some clinicians may advocate for a trial of medical therapy with antifibrotics, but this should be done in conjunction with transplant referral.
Patients should be listed for transplant if a 10% or greater decrease in FEV1 occurred in the past 6 months (of note, even a 5% decrease in FEV1 is associated with an overall poorer prognosis and warrants consideration of listing for transplant), if the diffusing capacity of the lung for carbon monoxide decreases 15% or greater during the 6-month follow-up, or if a decline of more than 50 meters is noted on the 6-minute walking test. A documented desaturation of less than 88% or a distance of less than 250 meters on the 6-minute walking test is another indication for listing. Any evidence of secondary pulmonary hypertension on right heart catheterization or on echocardiography or hospitalization for respiratory decline are also indications for listing.21 In cases of scleroderma-associated interstitial lung disease or mixed connective tissue interstitial lung disease, similar guidelines for referral and listing should be followed.2
Pulmonary arterial hypertension
Patients with pulmonary arterial hypertension should be referred for lung transplant if any 1 of the following conditions is present: rapidly progressive disease; NYHA Functional Classification III or IV symptoms during escalating therapy; use of parenteral pulmonary arterial hypertension therapy; or known or suspected pulmonary veno-occlusive disease or pulmonary capillary hemangiomatosis.2,22
Patients with pulmonary arterial hypertension should be listed for lung transplant if any of the following are present: NYHA Functional Classification III or IV symptoms despite combination therapy; right heart catheterization demonstrating a cardiac index less than 2 L/min/m2; mean right atrial pressure greater than 15 mm Hg; 6-minute walking test less than 350 meters; or development of pericardial effusion, hemoptysis, or signs of worsening right heart failure, including renal insufficiency, rising bilirubin or evidence of ascites.2,22
BRIDGE TO TRANSPLANT
Acute respiratory decompensation may occur in some candidates for lung transplant prior to listing for transplant or while on the transplant waitlist. In patients with failure of a single lung, a bridge to transplant may be necessary until a suitable organ is available. Mechanical ventilation and extracorporeal life support (ECLS) are 2 bridge strategies for lung transplant candidates. Mechanical ventilation is the most common lung transplant bridge strategy but it is less than ideal because it can lead to deconditioning and ventilator-associated infections that can negatively impact a patient’s suitability for transplant.
ECLS techniques that allow spontaneous breathing and potentially ambulation, known as awake or ambulatory ECLS, is a popular bridge therapy. Ambulatory ECLS is used as an alternative to mechanical ventilation to avoid the complications of mechanical ventilation and allow patients to avoid sedation and participate in rehabilitation.23 Irrespective of the therapy used as a bridge to transplant, patients considered for a bridge are optimally evaluated from a medical and psychosocial perspective prior to bridge therapy.
Both bridge therapies increase the risk of infection, bleeding, and neurologic events; thus, patients need to be assessed repeatedly for these risks to determine ongoing suitability for lung transplant. It is important to note that delayed referral of patients with advanced disease or patients in an acute exacerbation negatively impacts the evaluation for lung transplant, placement on the lung transplant waitlist, outcomes, and suitability for bridge transplant strategies.
CONCLUSION
To ensure good patient outcomes, the evaluation and selection of candidates for lung transplant requires communication between referring physicians and lung transplant centers. Physicians need basic knowledge of patient conditions appropriate for lung transplant and direct communication with lung transplant centers. The workup, required testing, and timing of listing for lung transplant varies among transplant centers across the country, making communication between the referring providers and transplant centers crucial to good patient care. An open, 2-way dialogue between referring providers and transplant centers facilitates listing patients for transplant in a timely manner, reduces delays, and improves outcomes.
Lung transplant is the therapy of choice for a growing number of patients with end-stage lung diseases. Patients receiving a lung transplant are faced with many challenges including drug toxicities, infections, and the risk of rejection.1 Despite these challenges, lung transplant may significantly prolong survival and improve quality of life for many patients.
CANDIDATES FOR LUNG TRANSPLANT
Identifying patients who are appropriate candidates for lung transplant is important to achieving favorable transplant outcomes and to maximizing life expectancy for each patient. The most recent edition of International Society for Heart and Lung Transplant (ISHLT) Guidelines for the Selection of Lung Transplant Candidates is an excellent guide to help physicians identify when to refer potential patients and to how to identify patients who are the most likely to benefit from lung transplant.2
Adults with end-stage lung disease are generally candidates for lung transplant if they meet the following criteria:
- A greater than 50% risk of death from lung disease within 2 years if a lung transplant is not performed
- A greater than 80% likelihood of surviving at least 90 days after the lung transplant procedure
- A greater than 80% likelihood of a 5-year survival posttransplant if graft function is preserved.2
These can only be estimated by transplant programs and not by the referring team in most cases.
Once a patient is identified as a candidate for lung transplant, early referral of patients to a lung transplant program has several advantages and is essential for positive outcomes. Early patient referral allows for timely completion of the formal evaluation of candidacy, patient and family education, as well as the opportunity for the patient and family to raise funds or use other resources to overcome financial hurdles. Listing a patient on the transplant waitlist implies that the patient has a limited life expectancy without a lung transplant and that the risk-benefit ratio favors lung transplant since all other medical options have been exhausted.1
NONCANDIDATES FOR LUNG TRANSPLANT
There are very few absolute contraindications to lung transplant. Generally, most transplant centers in the United States agree that contraindications to lung transplant include conditions associated with increased risk of mortality, including:
- A recent history of a major malignancy. Patients with a 2-year, disease-free interval combined with a low predicted risk of recurrence may be considered in certain cases of localized, non-melanoma skin cancer. A 5-year, disease-free survival is strongly suggested in patients with a history of breast, bladder, or kidney cancer as well as in cases of sarcoma, melanoma, lymphoma and certain hematologic disorders.
- The presence of significant dysfunction of another major organ systems including the heart, liver, kidney, or brain unless a combined organ transplant can be considered and performed.
- Significant coronary heart disease not amenable to revascularization or intervention prior to or at the time of lung transplant.
- The presence of an acute medical condition including but not limited to sepsis and acute liver failure.
- Active Mycobacterium tuberculosis and other highly virulent or highly resistant microbes that are poorly controlled pretransplant.
- Severe obesity with a body mass index greater than 35.
- A history of nonadherence to medical therapy, psychiatric or psychological conditions that might lead to nonadherence, poor or limited social support system, and limited functional status not amenable to rehabilitation.
- Current substance abuse or dependence, including illicit substances, alcohol, and tobacco (nicotine-containing substances). Most centers require at least 6 months’ abstinence from illicit substances prior to being added to the lung transplant waitlist.2
CANDIDATE COMORBIDITIES
Age
Many transplant centers in the US define the age cutoff for lung transplant at 65; however, some centers may consider candidates older than 65. Advanced age by itself should not be considered a contraindication to lung transplant. However, increased age is usually associated with other comorbid conditions that may increase perioperative and long-term morbidity and mortality. As mentioned previously, the number of older candidates for lung transplant has increased. In the US, 29% of the patients on the national waiting list in 2015 were over age 65.4
Past chest surgery
It is not uncommon for lung transplant candidates to have a history of chest surgery such as lung resection, pleurodesis, or coronary artery bypass grafting. The limited literature regarding the outcomes for these patients suggests they may experience higher rates of bleeding, re-exploration, and renal dysfunction.2 However, these patients should not be excluded from lung transplant and successful transplant outcomes have been achieved in this population by experienced centers.5 In candidates with a history of chronic obstructive pulmonary disease (COPD) and lung-volume reduction surgery (LVRS), early case series indicate that these patients did well after lung transplant.6 However, more recent data demonstrate that patients with prior LVRS who undergo lung transplant experience higher rates of bleeding, worse early graft dysfunction, and worse outcomes overall.7 As with lung transplant candidates with previous chest surgery, lung transplant candidates with previous LVRS are best served by experienced transplant centers.
Hepatitis and HIV
Patients with a history of infection with hepatitis B, hepatitis C, or human immunodeficiency virus (HIV) are candidates for lung transplant at centers experienced with lung transplant in patients with these infections. Most centers advocate that patients with a history of hepatitis B or C have viral infection levels that are controlled or reduced as low as possible and that there is no evidence of portal hypertension or severe cirrhosis.8,9 In the case of HIV, patients should have controlled disease with a negative or undetectable viral load and have no current acquired immunodeficiency defining illness.10 Patients colonized with particular species of Burkholderia cepacia or Mycobacterium abscessus subspecies can be considered for lung transplant only at centers with established preoperative and postoperative protocols for these infections due to the increased risk of perioperative mortality associated with these organisms.11,12
DISEASE-SPECIFIC INDICATIONS
Chronic obstructive pulmonary disease
COPD (both non- and alpha-1 antitrypsin deficiency) is the most common indication for lung transplant and accounts for almost 32% of lung transplants worldwide.13 Patients should be referred for lung transplant when medical therapies, surgical interventions (ie, LVRS) and pulmonary rehabilitation have been maximized. In COPD, the loss of lung function occurs over a long period of time but patients are often more limited by diminished quality of life as lung function slowly declines.
Patients with COPD should be referred for lung transplant if the body mass index, airflow obstruction, dyspnea, and exercise capacity (BODE) index is 5 to 6.2 The original BODE index developed by Celli et al,14 is a scoring system from 0 to 10 with a higher score indicating more severe disease and worse survival. A score of 5 to 6 indicates an estimated mortality of 60% at 4 yrs.2,14,15 Other considerations for referral for lung transplant include the presence of hypercapnia with partial pressure of carbon dioxide greater than 50 mm Hg or higher or hypoxemia with partial pressure of oxygen less than 60 mm Hg or a forced expiratory volume at 1 sec (FEV1) less than 25% predicted.
Patients with COPD should considered for listing for lung transplant if any one of the following criteria is met: BODE index of 7 or greater; FEV1 less than 15% to 20%; 3 of more severe exacerbations during the preceding year; 1 severe exacerbation with acute hypercapnic respiratory failure; or presence of moderate to severe pulmonary hypertension.2,16
Cystic fibrosis
In patients with cystic fibrosis, lung transplant should be considered in patients with an estimated 2-year survival of less than 50% and with a New York Heart Association (NYHA) Functional Classification III or IV. Referral for lung transplant is recommended for patients with a rapid decrease in FEV1 despite optimal therapy, female patients with declining weight and lung function, colonization or infection with nontuberculous mycobacterial disease, or cystic fibrosis-related diabetes. The development of pulmonary hypertension, reduction in walk distance, increasing antibiotic resistance, acute respiratory failure requiring noninvasive ventilation, worsening nutritional status, pneumothorax, and life-threatening hemoptysis despite embolization are all indications for referral for lung transplant.
Patients with cystic fibrosis with hypoxia or hypercapnia with declining lung function, needing long-term noninvasive ventilation, having more frequent exacerbations or exhibiting a decline in functional status should be listed for lung transplant.2,17–19
Restrictive lung disease
Patients with restrictive lung diseases, including interstitial pulmonary fibrosis (usual interstitial pneumonitis, nonspecific interstitial pneumonia), or interstitial lung disease, and hypersensitivity pneumonitis, should be referred for transplant evaluation at the time of diagnosis irrespective of lung function due to the unpredictable nature of these diseases.20 Some clinicians may advocate for a trial of medical therapy with antifibrotics, but this should be done in conjunction with transplant referral.
Patients should be listed for transplant if a 10% or greater decrease in FEV1 occurred in the past 6 months (of note, even a 5% decrease in FEV1 is associated with an overall poorer prognosis and warrants consideration of listing for transplant), if the diffusing capacity of the lung for carbon monoxide decreases 15% or greater during the 6-month follow-up, or if a decline of more than 50 meters is noted on the 6-minute walking test. A documented desaturation of less than 88% or a distance of less than 250 meters on the 6-minute walking test is another indication for listing. Any evidence of secondary pulmonary hypertension on right heart catheterization or on echocardiography or hospitalization for respiratory decline are also indications for listing.21 In cases of scleroderma-associated interstitial lung disease or mixed connective tissue interstitial lung disease, similar guidelines for referral and listing should be followed.2
Pulmonary arterial hypertension
Patients with pulmonary arterial hypertension should be referred for lung transplant if any 1 of the following conditions is present: rapidly progressive disease; NYHA Functional Classification III or IV symptoms during escalating therapy; use of parenteral pulmonary arterial hypertension therapy; or known or suspected pulmonary veno-occlusive disease or pulmonary capillary hemangiomatosis.2,22
Patients with pulmonary arterial hypertension should be listed for lung transplant if any of the following are present: NYHA Functional Classification III or IV symptoms despite combination therapy; right heart catheterization demonstrating a cardiac index less than 2 L/min/m2; mean right atrial pressure greater than 15 mm Hg; 6-minute walking test less than 350 meters; or development of pericardial effusion, hemoptysis, or signs of worsening right heart failure, including renal insufficiency, rising bilirubin or evidence of ascites.2,22
BRIDGE TO TRANSPLANT
Acute respiratory decompensation may occur in some candidates for lung transplant prior to listing for transplant or while on the transplant waitlist. In patients with failure of a single lung, a bridge to transplant may be necessary until a suitable organ is available. Mechanical ventilation and extracorporeal life support (ECLS) are 2 bridge strategies for lung transplant candidates. Mechanical ventilation is the most common lung transplant bridge strategy but it is less than ideal because it can lead to deconditioning and ventilator-associated infections that can negatively impact a patient’s suitability for transplant.
ECLS techniques that allow spontaneous breathing and potentially ambulation, known as awake or ambulatory ECLS, is a popular bridge therapy. Ambulatory ECLS is used as an alternative to mechanical ventilation to avoid the complications of mechanical ventilation and allow patients to avoid sedation and participate in rehabilitation.23 Irrespective of the therapy used as a bridge to transplant, patients considered for a bridge are optimally evaluated from a medical and psychosocial perspective prior to bridge therapy.
Both bridge therapies increase the risk of infection, bleeding, and neurologic events; thus, patients need to be assessed repeatedly for these risks to determine ongoing suitability for lung transplant. It is important to note that delayed referral of patients with advanced disease or patients in an acute exacerbation negatively impacts the evaluation for lung transplant, placement on the lung transplant waitlist, outcomes, and suitability for bridge transplant strategies.
CONCLUSION
To ensure good patient outcomes, the evaluation and selection of candidates for lung transplant requires communication between referring physicians and lung transplant centers. Physicians need basic knowledge of patient conditions appropriate for lung transplant and direct communication with lung transplant centers. The workup, required testing, and timing of listing for lung transplant varies among transplant centers across the country, making communication between the referring providers and transplant centers crucial to good patient care. An open, 2-way dialogue between referring providers and transplant centers facilitates listing patients for transplant in a timely manner, reduces delays, and improves outcomes.
- Kreider M, Hadjiliadis D, Kotloff R. Candidate selection, timing of listing, and choice of procedure for lung transplantation. Clin Chest Med 2011; 32:199–211.
- Weill D, Benden C, Corris P, et al. A consensus document for the selection of lung transplant candidates: 2014—An update from the Pulmonary Transplant Council of the International Society of Heart and Lung Transplantation. J Heart Lung Transplant 2015; 34:1–15.
- Tsuang WM. Contemporary issues in lung transplant allocation practices. Curr Transplant Rep 2017; 4:238–242.
- Valapour M, Skeans MA, Smith JM, et al. OPTN/SRTR 2015 annual data report: lung. Am J Transplant 2017; 17(suppl 1):357–424.
- Omara M, Okamoto T, Arafat A, Thuita L, Blackstone EH, McCurry KR. Lung transplantation in patients who have undergone prior cardiothoracic procedures. J Heart Lung Transplant 2016; 35:1462–1470.
- Senbaklavaci O, Wisser W, Ozpeker C, et al. Successful lung volume reduction surgery brings patients into better condition for later lung transplantation. Eur J Cardiothorac Surg 2002; 22:363–367.
- Shigemura N, Gilbert S, Bhama JK et al. Lung transplantation after lung volume reduction surgery. Transplantation 2013; 96:421–425.
- Sahi H, Zein NN, Mehta AC, Blazey HC, Meyer KH, Budev M. Outcomes after lung transplantation in patients with chronic hepatitis C virus infection. J Heart Lung Transplant 2007; 26:466–471.
- Kim EY, Ko HH, Yoshida EM. A concise review of hepatitis C in heart and lung transplantation. Can J Gastroenterol 2011; 25:445–448.
- Kern RM, Seethamraju H, Blanc PD, et al. The feasibility of lung transplantation in HIV-seropositive patients. Ann Am Thorac Soc 2014; 11:882–889.
- De Soyza A, Corris A, McDowell A, Archer L, et al. Burkholderia cepacia complex genomovars and pulmonary transplant outcomes in patients with cystic fibrosis. Lancet 2001; 358:1780–1781.
- De Soyza A, Meachery G, Hester HL, et al. Lung transplant for patients with cystic fibrosis and Burkholderia cepacia complex infection: a single center experience. J Heart Lung Transplant 2010; 29:1395–1404.
- Yusen RD, Edwards LB, Kucheryavaya AY, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-second official adult and heart-lung transplantation report—2015; focus theme: early graft failure. J Heart Lung Transplant 2015; 34:1264–1277.
- Celli BR, Cote CG, Marin JM, et al. The body–mass index, airflow obstruction, dyspna and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004; 350:1005–1012.
- Marchand E. The BODE index as a tool to predict survival in COPD lung transplant candidates. Eur Respir J 2010; 36:1494–1495.
- Lahzami S, Bridevaux PO, Soccal PM, et al. Survival impact of lung transplant for COPD. Eur Respir J 2010; 36:74–80.
- Rosenbluth DB, Wilson K, Ferkol T, Schuster DP. Lung function decline in cystic fibrosis patients and timing for lung transplantation referral. Chest 2004; 126:412–419.
- Mayer-Hamblett N, Rosenfield M, Emerson J, Goss CH, Aitken ML. Developing cystic fibrosis lung transplant referral criteria using predictors of 2-year mortality. Am J Respir Crit Care Med 2002; 166:1550–1556.
- Liou TG, Adler FR, Cahill BC, et al. Survival effect of lung transplantation among patients with cystic fibrosis. JAMA 2001; 286:2683–2689.
- Raghu G, Collard HR, Egan JJ, et al; ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidenced-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011; 183:788–824.
- Collard HR, King TE Jr, Bartelson BB, Vourlekis JS, Schwarz MI, Brown KK. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2003; 168:538–542.
- Edelman, JD. Navigating the road to transplantation for pulmonary arterial hypertension. Advances in Pulmonary Hypertension 2016; 15:14–18.
- Strueber M. Bridges to lung transplant. Curr Opin Organ Transplant 2011; 16:458–461.
- Kreider M, Hadjiliadis D, Kotloff R. Candidate selection, timing of listing, and choice of procedure for lung transplantation. Clin Chest Med 2011; 32:199–211.
- Weill D, Benden C, Corris P, et al. A consensus document for the selection of lung transplant candidates: 2014—An update from the Pulmonary Transplant Council of the International Society of Heart and Lung Transplantation. J Heart Lung Transplant 2015; 34:1–15.
- Tsuang WM. Contemporary issues in lung transplant allocation practices. Curr Transplant Rep 2017; 4:238–242.
- Valapour M, Skeans MA, Smith JM, et al. OPTN/SRTR 2015 annual data report: lung. Am J Transplant 2017; 17(suppl 1):357–424.
- Omara M, Okamoto T, Arafat A, Thuita L, Blackstone EH, McCurry KR. Lung transplantation in patients who have undergone prior cardiothoracic procedures. J Heart Lung Transplant 2016; 35:1462–1470.
- Senbaklavaci O, Wisser W, Ozpeker C, et al. Successful lung volume reduction surgery brings patients into better condition for later lung transplantation. Eur J Cardiothorac Surg 2002; 22:363–367.
- Shigemura N, Gilbert S, Bhama JK et al. Lung transplantation after lung volume reduction surgery. Transplantation 2013; 96:421–425.
- Sahi H, Zein NN, Mehta AC, Blazey HC, Meyer KH, Budev M. Outcomes after lung transplantation in patients with chronic hepatitis C virus infection. J Heart Lung Transplant 2007; 26:466–471.
- Kim EY, Ko HH, Yoshida EM. A concise review of hepatitis C in heart and lung transplantation. Can J Gastroenterol 2011; 25:445–448.
- Kern RM, Seethamraju H, Blanc PD, et al. The feasibility of lung transplantation in HIV-seropositive patients. Ann Am Thorac Soc 2014; 11:882–889.
- De Soyza A, Corris A, McDowell A, Archer L, et al. Burkholderia cepacia complex genomovars and pulmonary transplant outcomes in patients with cystic fibrosis. Lancet 2001; 358:1780–1781.
- De Soyza A, Meachery G, Hester HL, et al. Lung transplant for patients with cystic fibrosis and Burkholderia cepacia complex infection: a single center experience. J Heart Lung Transplant 2010; 29:1395–1404.
- Yusen RD, Edwards LB, Kucheryavaya AY, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-second official adult and heart-lung transplantation report—2015; focus theme: early graft failure. J Heart Lung Transplant 2015; 34:1264–1277.
- Celli BR, Cote CG, Marin JM, et al. The body–mass index, airflow obstruction, dyspna and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004; 350:1005–1012.
- Marchand E. The BODE index as a tool to predict survival in COPD lung transplant candidates. Eur Respir J 2010; 36:1494–1495.
- Lahzami S, Bridevaux PO, Soccal PM, et al. Survival impact of lung transplant for COPD. Eur Respir J 2010; 36:74–80.
- Rosenbluth DB, Wilson K, Ferkol T, Schuster DP. Lung function decline in cystic fibrosis patients and timing for lung transplantation referral. Chest 2004; 126:412–419.
- Mayer-Hamblett N, Rosenfield M, Emerson J, Goss CH, Aitken ML. Developing cystic fibrosis lung transplant referral criteria using predictors of 2-year mortality. Am J Respir Crit Care Med 2002; 166:1550–1556.
- Liou TG, Adler FR, Cahill BC, et al. Survival effect of lung transplantation among patients with cystic fibrosis. JAMA 2001; 286:2683–2689.
- Raghu G, Collard HR, Egan JJ, et al; ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidenced-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011; 183:788–824.
- Collard HR, King TE Jr, Bartelson BB, Vourlekis JS, Schwarz MI, Brown KK. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2003; 168:538–542.
- Edelman, JD. Navigating the road to transplantation for pulmonary arterial hypertension. Advances in Pulmonary Hypertension 2016; 15:14–18.
- Strueber M. Bridges to lung transplant. Curr Opin Organ Transplant 2011; 16:458–461.
KEY POINTS
- Lung transplant is the therapy of choice for a growing number of patients with end-stage lung disease.
- There are very few absolute contraindications to lung transplant. Potential contraindications and comorbidities can be discussed with the transplant center and vetted prior to listing for lung transplant.
- The workup for a lung transplant varies among transplant centers across the country, thus good communication between referring providers and transplant centers is crucial to quality care.