User login
As we enter 2015 and approach the golden (50th) anniversary of both the NP and PA professions, dating back to Dr. Loretta Ford1 at the University of Colorado and Dr. Eugene Stead2 at Duke University (circa 1965), it is important to reflect on not only where we have been but also where we want our professions to go in the next half-century.
Since I am a PA, some may suggest that it is dangerous and ambitious for me to speak/project for both professions. They may also note that the professions are distinct and my suggestions and reflections do not apply to NPs. Well, I guess I am willing to take that risk. As a colleague, friend, and co-Editor-in-Chief of Marie-Eileen Onieal, I have found that we agree much more often on issues (both political and practical) than we disagree.
NPs and PAs have worked diligently over the past half-century to develop our individual professions, in terms of reimbursement, prescribing privileges, state licensure, commissioning in the uniformed services, and expansion of scope of practice. Studies continue to show that we provide quality health care with similar outcomes as physicians, thus making us cost-effective members of the health care team.3-7
So, here we are in 2015. While it is difficult to get accurate data, Table 1 shows the number of clinicians reported in the most recent US Health Workforce Chartbook.8 As we well know, our professions have grown exponentially from our humble beginnings in the mid-1960s. (The first class of PAs comprised four students, if you recall.)
At the risk of sounding like a fossil (Oh never mind—I am a fossil!), let me be presumptuous and share with you six areas in which I think both professions can “do more” through the second half-century of our existence. In my opinion, we should focus on:
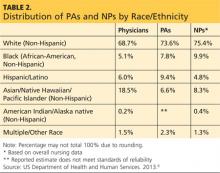
1. Diversity. As presented in Table 2, the majority of PAs and NPs are (non-Hispanic) white. Our efforts, should you agree with me, must start at the educational program level, through recruitment and retention of students from unrepresented and underrepresented groups. Another focal point should be the recruitment and retention of faculty and staff in these programs who reflect the diversity of our nation.
When I consider the origins of my profession, the key point is opportunity. Dr. Stead and other pioneers sought to fill a serious need for health care providers while also creating opportunities for military medics who were highly skilled but who did not meet requirements for many jobs within the medical community. Now it is time for us to ensure that other groups have similar opportunities to advance themselves and also fill gaps in the health care system.
Continue for more areas to focus on >>
2. Workforce planning and policy. This requires better data collection and an improved information infrastructure. In a 2014 editorial, Rod Hooker suggested that this is the golden age for PAs (about whom he was writing, although the same holds true for NPs) because US health care reform has identified our contributions to society and new policies place us upfront and center stage in producing labor solutions.9
It is time for our professions to do a better job in studying and reporting the important contributions we make in health care delivery. We need to have a place at the table—be it within a facility or at the state or federal level—whenever policy, utilization, and roles are discussed. Even if we as employees are subordinate to management in a particular setting, we should have a voice in how we are utilized in the workplace; we should ensure that those who make decisions—if we are not them—have the fullest picture of who we are and what we can do. It is not enough to use anecdotal evidence; we need to have data readily at hand that unequivocally support our assertions of value to patient care.
Hooker went so far as to call for the creation of a “physician assistant institute” to assist in the development and dissemination of reliable information about the profession. I think this is an idea whose time has come, but who will step up to the plate? If you are an NP, you may say, “What about us?” I would suggest this issue pertains to both of our professions—and in fact, this is an area in which I would encourage a collaborative effort. What a concept!
3. Ethics. In the past decade, there has been a renewed focus on maintaining an ethical culture in health care. As clinicians, we practice in an environment that affects the lives of everyone. Our patients and their family members expect high-quality care, patient safety, and use of the latest and most appropriate technology.
In the middle of this climate, we find a health care system that is probably the most entrepreneurial, corporatized, and profit-driven health system in the world. Most of our practice settings (outside the federal government) are for-profit entities. It is easy in this environment to fall victim to conflicts of interest and to acquire an economically oriented practice attitude.
If our first priority is the best possible health care for our patients, then integrity and ethical behavior naturally follow. Professionalism at its very heart places the patient’s interests ahead of our own. We must keep this in mind as we navigate the ever-changing health system.
Next page: Key area number four >>
4. Humanitarianism. I would encourage us to be actively engaged in promoting human welfare and social reforms with no prejudice on grounds of gender, sexual orientation, or religious or ethnic differences. Our goal should be to save lives, relieve suffering, and maintain human dignity.
How do we do this? Many of us have at some point in our careers volunteered our professional services at free clinics or other venues that provide health care to those who otherwise have difficulty accessing it. Some of us take that spirit a step further, traveling abroad on medical missions or responding to natural disasters or civil disturbances.
While using our medical and nursing skills for the good of society is ideal, we can also represent ourselves and our professions well by being good members of the community—not just the “medical” community. Perhaps we provide food and shelter to the homeless in our area or mentor young people.
Anything we do to help not only benefits us and the recipient; it also shows the community that our concept of “care” extends beyond the confines of the clinic or emergency department or operating theater in which we work. We have a very special calling, and I’m always pleased when our professional journals highlight the efforts of our colleagues to “help out”; their stories should inspire us all.
5. Appreciation. As NPs and PAs, we provide health care (whether from a medical or nursing standpoint), a revered calling since the days of Hippocrates. This privilege allows us to enter into a bond with our patients and assist them in a personal and fundamental way. It is no small thing to be involved in curing illness and promoting well-being. We should always remember that our role carries responsibility as well as provides rewards.
Despite the greater availability of diagnostic technologies and advancements in therapeutic abilities, we continue to see increasing disparities in the delivery of health care. Our professions must work diligently to find ways to address the issues of quality, accessibility, and cost of health care in the US. What kind of “stewards” will we be? That is our heritage!
Continue for the last area PAs and NPs need to grow in >>
6. Action. At the risk of sounding like a cheerleader, being part of the NP or PA profession is something special; it always has been and always will be. Our professions have grown impressively in numbers, utilization, and stature. We need to cultivate and support our professions and their representative organizations (ie, AANP and AAPA).
In the early decades of each profession, individuals with a great deal of passion and dedication created, advanced, and led these organizations on both state and national levels—and even an international level. You know who they are! Without them, we would not have made the strides that we have as professionals—the attainment of licensure, authority, and reimbursement.
Now that we are being truly recognized for our role in the health care team and our contributions to patient care, some of us may become complacent with regard to our professional organizations. But there will always be legislative and regulatory gains to make, and strong representation (and “strength in numbers”) is the best way to achieve our professional goals. Please, let’s continue to support our organizations not only via membership (which provides funding for initiatives) but also by participating in whatever ways we can to further our professions.
If we are going to fully cement our place in America’s health care system, NPs and PAs must strive to keep up the national dialogue about our patients, their needs, and how our contributions address those needs. I hope you agree. Please share your thoughts with me at PAEditor@frontline medcom.com.
REFERENCES
1. Ridgway S. Loretta Ford, founded nurse practitioner movement. Working Nurse. www.workingnurse.com/articles/loretta-ford-founded-nurse-practitioner-movement. Accessed January 16, 2015.
2. Physician Assistant History Society. Eugene A. Stead Jr, MD. http://pahx.org/stead-jr-eugene. Accessed January 16, 2015.
3. Kartha A, Restuccia J, Burgess J, et al. Nurse practitioner and physician assistant scope of practice in 118 acute care hospitals. J Hosp Med. 2014:9(10); 615-620.
4. Naylor MD, Kurtzman ET. The role of nurse practitioners in reinventing primary care. Health Affairs. 2010;29(5):893-899.
5. Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002;324:819-823.
6. Halter M, Drennan V, Chattopadhyay K, et al. The contribution of physician assistants in primary care: a systematic review. BMC Health Services Research. 2013;13:223-236.
7. Hooker RS, Everett CM. The contributions of physician assistants in primary care systems. Health Social Care Commun. 2012;20(1):20-31.
8. US Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis. The US Health Workforce Chartbook. Part 1: Clinicians. Rockville, MD; 2013.
9. Hooker R. A physician assistant institute [editorial]. J Phys Assist Ed. 2014;25(3):5-6.
As we enter 2015 and approach the golden (50th) anniversary of both the NP and PA professions, dating back to Dr. Loretta Ford1 at the University of Colorado and Dr. Eugene Stead2 at Duke University (circa 1965), it is important to reflect on not only where we have been but also where we want our professions to go in the next half-century.
Since I am a PA, some may suggest that it is dangerous and ambitious for me to speak/project for both professions. They may also note that the professions are distinct and my suggestions and reflections do not apply to NPs. Well, I guess I am willing to take that risk. As a colleague, friend, and co-Editor-in-Chief of Marie-Eileen Onieal, I have found that we agree much more often on issues (both political and practical) than we disagree.
NPs and PAs have worked diligently over the past half-century to develop our individual professions, in terms of reimbursement, prescribing privileges, state licensure, commissioning in the uniformed services, and expansion of scope of practice. Studies continue to show that we provide quality health care with similar outcomes as physicians, thus making us cost-effective members of the health care team.3-7
So, here we are in 2015. While it is difficult to get accurate data, Table 1 shows the number of clinicians reported in the most recent US Health Workforce Chartbook.8 As we well know, our professions have grown exponentially from our humble beginnings in the mid-1960s. (The first class of PAs comprised four students, if you recall.)
At the risk of sounding like a fossil (Oh never mind—I am a fossil!), let me be presumptuous and share with you six areas in which I think both professions can “do more” through the second half-century of our existence. In my opinion, we should focus on:
1. Diversity. As presented in Table 2, the majority of PAs and NPs are (non-Hispanic) white. Our efforts, should you agree with me, must start at the educational program level, through recruitment and retention of students from unrepresented and underrepresented groups. Another focal point should be the recruitment and retention of faculty and staff in these programs who reflect the diversity of our nation.
When I consider the origins of my profession, the key point is opportunity. Dr. Stead and other pioneers sought to fill a serious need for health care providers while also creating opportunities for military medics who were highly skilled but who did not meet requirements for many jobs within the medical community. Now it is time for us to ensure that other groups have similar opportunities to advance themselves and also fill gaps in the health care system.
Continue for more areas to focus on >>
2. Workforce planning and policy. This requires better data collection and an improved information infrastructure. In a 2014 editorial, Rod Hooker suggested that this is the golden age for PAs (about whom he was writing, although the same holds true for NPs) because US health care reform has identified our contributions to society and new policies place us upfront and center stage in producing labor solutions.9
It is time for our professions to do a better job in studying and reporting the important contributions we make in health care delivery. We need to have a place at the table—be it within a facility or at the state or federal level—whenever policy, utilization, and roles are discussed. Even if we as employees are subordinate to management in a particular setting, we should have a voice in how we are utilized in the workplace; we should ensure that those who make decisions—if we are not them—have the fullest picture of who we are and what we can do. It is not enough to use anecdotal evidence; we need to have data readily at hand that unequivocally support our assertions of value to patient care.
Hooker went so far as to call for the creation of a “physician assistant institute” to assist in the development and dissemination of reliable information about the profession. I think this is an idea whose time has come, but who will step up to the plate? If you are an NP, you may say, “What about us?” I would suggest this issue pertains to both of our professions—and in fact, this is an area in which I would encourage a collaborative effort. What a concept!
3. Ethics. In the past decade, there has been a renewed focus on maintaining an ethical culture in health care. As clinicians, we practice in an environment that affects the lives of everyone. Our patients and their family members expect high-quality care, patient safety, and use of the latest and most appropriate technology.
In the middle of this climate, we find a health care system that is probably the most entrepreneurial, corporatized, and profit-driven health system in the world. Most of our practice settings (outside the federal government) are for-profit entities. It is easy in this environment to fall victim to conflicts of interest and to acquire an economically oriented practice attitude.
If our first priority is the best possible health care for our patients, then integrity and ethical behavior naturally follow. Professionalism at its very heart places the patient’s interests ahead of our own. We must keep this in mind as we navigate the ever-changing health system.
Next page: Key area number four >>
4. Humanitarianism. I would encourage us to be actively engaged in promoting human welfare and social reforms with no prejudice on grounds of gender, sexual orientation, or religious or ethnic differences. Our goal should be to save lives, relieve suffering, and maintain human dignity.
How do we do this? Many of us have at some point in our careers volunteered our professional services at free clinics or other venues that provide health care to those who otherwise have difficulty accessing it. Some of us take that spirit a step further, traveling abroad on medical missions or responding to natural disasters or civil disturbances.
While using our medical and nursing skills for the good of society is ideal, we can also represent ourselves and our professions well by being good members of the community—not just the “medical” community. Perhaps we provide food and shelter to the homeless in our area or mentor young people.
Anything we do to help not only benefits us and the recipient; it also shows the community that our concept of “care” extends beyond the confines of the clinic or emergency department or operating theater in which we work. We have a very special calling, and I’m always pleased when our professional journals highlight the efforts of our colleagues to “help out”; their stories should inspire us all.
5. Appreciation. As NPs and PAs, we provide health care (whether from a medical or nursing standpoint), a revered calling since the days of Hippocrates. This privilege allows us to enter into a bond with our patients and assist them in a personal and fundamental way. It is no small thing to be involved in curing illness and promoting well-being. We should always remember that our role carries responsibility as well as provides rewards.
Despite the greater availability of diagnostic technologies and advancements in therapeutic abilities, we continue to see increasing disparities in the delivery of health care. Our professions must work diligently to find ways to address the issues of quality, accessibility, and cost of health care in the US. What kind of “stewards” will we be? That is our heritage!
Continue for the last area PAs and NPs need to grow in >>
6. Action. At the risk of sounding like a cheerleader, being part of the NP or PA profession is something special; it always has been and always will be. Our professions have grown impressively in numbers, utilization, and stature. We need to cultivate and support our professions and their representative organizations (ie, AANP and AAPA).
In the early decades of each profession, individuals with a great deal of passion and dedication created, advanced, and led these organizations on both state and national levels—and even an international level. You know who they are! Without them, we would not have made the strides that we have as professionals—the attainment of licensure, authority, and reimbursement.
Now that we are being truly recognized for our role in the health care team and our contributions to patient care, some of us may become complacent with regard to our professional organizations. But there will always be legislative and regulatory gains to make, and strong representation (and “strength in numbers”) is the best way to achieve our professional goals. Please, let’s continue to support our organizations not only via membership (which provides funding for initiatives) but also by participating in whatever ways we can to further our professions.
If we are going to fully cement our place in America’s health care system, NPs and PAs must strive to keep up the national dialogue about our patients, their needs, and how our contributions address those needs. I hope you agree. Please share your thoughts with me at PAEditor@frontline medcom.com.
REFERENCES
1. Ridgway S. Loretta Ford, founded nurse practitioner movement. Working Nurse. www.workingnurse.com/articles/loretta-ford-founded-nurse-practitioner-movement. Accessed January 16, 2015.
2. Physician Assistant History Society. Eugene A. Stead Jr, MD. http://pahx.org/stead-jr-eugene. Accessed January 16, 2015.
3. Kartha A, Restuccia J, Burgess J, et al. Nurse practitioner and physician assistant scope of practice in 118 acute care hospitals. J Hosp Med. 2014:9(10); 615-620.
4. Naylor MD, Kurtzman ET. The role of nurse practitioners in reinventing primary care. Health Affairs. 2010;29(5):893-899.
5. Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002;324:819-823.
6. Halter M, Drennan V, Chattopadhyay K, et al. The contribution of physician assistants in primary care: a systematic review. BMC Health Services Research. 2013;13:223-236.
7. Hooker RS, Everett CM. The contributions of physician assistants in primary care systems. Health Social Care Commun. 2012;20(1):20-31.
8. US Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis. The US Health Workforce Chartbook. Part 1: Clinicians. Rockville, MD; 2013.
9. Hooker R. A physician assistant institute [editorial]. J Phys Assist Ed. 2014;25(3):5-6.
As we enter 2015 and approach the golden (50th) anniversary of both the NP and PA professions, dating back to Dr. Loretta Ford1 at the University of Colorado and Dr. Eugene Stead2 at Duke University (circa 1965), it is important to reflect on not only where we have been but also where we want our professions to go in the next half-century.
Since I am a PA, some may suggest that it is dangerous and ambitious for me to speak/project for both professions. They may also note that the professions are distinct and my suggestions and reflections do not apply to NPs. Well, I guess I am willing to take that risk. As a colleague, friend, and co-Editor-in-Chief of Marie-Eileen Onieal, I have found that we agree much more often on issues (both political and practical) than we disagree.
NPs and PAs have worked diligently over the past half-century to develop our individual professions, in terms of reimbursement, prescribing privileges, state licensure, commissioning in the uniformed services, and expansion of scope of practice. Studies continue to show that we provide quality health care with similar outcomes as physicians, thus making us cost-effective members of the health care team.3-7
So, here we are in 2015. While it is difficult to get accurate data, Table 1 shows the number of clinicians reported in the most recent US Health Workforce Chartbook.8 As we well know, our professions have grown exponentially from our humble beginnings in the mid-1960s. (The first class of PAs comprised four students, if you recall.)
At the risk of sounding like a fossil (Oh never mind—I am a fossil!), let me be presumptuous and share with you six areas in which I think both professions can “do more” through the second half-century of our existence. In my opinion, we should focus on:
1. Diversity. As presented in Table 2, the majority of PAs and NPs are (non-Hispanic) white. Our efforts, should you agree with me, must start at the educational program level, through recruitment and retention of students from unrepresented and underrepresented groups. Another focal point should be the recruitment and retention of faculty and staff in these programs who reflect the diversity of our nation.
When I consider the origins of my profession, the key point is opportunity. Dr. Stead and other pioneers sought to fill a serious need for health care providers while also creating opportunities for military medics who were highly skilled but who did not meet requirements for many jobs within the medical community. Now it is time for us to ensure that other groups have similar opportunities to advance themselves and also fill gaps in the health care system.
Continue for more areas to focus on >>
2. Workforce planning and policy. This requires better data collection and an improved information infrastructure. In a 2014 editorial, Rod Hooker suggested that this is the golden age for PAs (about whom he was writing, although the same holds true for NPs) because US health care reform has identified our contributions to society and new policies place us upfront and center stage in producing labor solutions.9
It is time for our professions to do a better job in studying and reporting the important contributions we make in health care delivery. We need to have a place at the table—be it within a facility or at the state or federal level—whenever policy, utilization, and roles are discussed. Even if we as employees are subordinate to management in a particular setting, we should have a voice in how we are utilized in the workplace; we should ensure that those who make decisions—if we are not them—have the fullest picture of who we are and what we can do. It is not enough to use anecdotal evidence; we need to have data readily at hand that unequivocally support our assertions of value to patient care.
Hooker went so far as to call for the creation of a “physician assistant institute” to assist in the development and dissemination of reliable information about the profession. I think this is an idea whose time has come, but who will step up to the plate? If you are an NP, you may say, “What about us?” I would suggest this issue pertains to both of our professions—and in fact, this is an area in which I would encourage a collaborative effort. What a concept!
3. Ethics. In the past decade, there has been a renewed focus on maintaining an ethical culture in health care. As clinicians, we practice in an environment that affects the lives of everyone. Our patients and their family members expect high-quality care, patient safety, and use of the latest and most appropriate technology.
In the middle of this climate, we find a health care system that is probably the most entrepreneurial, corporatized, and profit-driven health system in the world. Most of our practice settings (outside the federal government) are for-profit entities. It is easy in this environment to fall victim to conflicts of interest and to acquire an economically oriented practice attitude.
If our first priority is the best possible health care for our patients, then integrity and ethical behavior naturally follow. Professionalism at its very heart places the patient’s interests ahead of our own. We must keep this in mind as we navigate the ever-changing health system.
Next page: Key area number four >>
4. Humanitarianism. I would encourage us to be actively engaged in promoting human welfare and social reforms with no prejudice on grounds of gender, sexual orientation, or religious or ethnic differences. Our goal should be to save lives, relieve suffering, and maintain human dignity.
How do we do this? Many of us have at some point in our careers volunteered our professional services at free clinics or other venues that provide health care to those who otherwise have difficulty accessing it. Some of us take that spirit a step further, traveling abroad on medical missions or responding to natural disasters or civil disturbances.
While using our medical and nursing skills for the good of society is ideal, we can also represent ourselves and our professions well by being good members of the community—not just the “medical” community. Perhaps we provide food and shelter to the homeless in our area or mentor young people.
Anything we do to help not only benefits us and the recipient; it also shows the community that our concept of “care” extends beyond the confines of the clinic or emergency department or operating theater in which we work. We have a very special calling, and I’m always pleased when our professional journals highlight the efforts of our colleagues to “help out”; their stories should inspire us all.
5. Appreciation. As NPs and PAs, we provide health care (whether from a medical or nursing standpoint), a revered calling since the days of Hippocrates. This privilege allows us to enter into a bond with our patients and assist them in a personal and fundamental way. It is no small thing to be involved in curing illness and promoting well-being. We should always remember that our role carries responsibility as well as provides rewards.
Despite the greater availability of diagnostic technologies and advancements in therapeutic abilities, we continue to see increasing disparities in the delivery of health care. Our professions must work diligently to find ways to address the issues of quality, accessibility, and cost of health care in the US. What kind of “stewards” will we be? That is our heritage!
Continue for the last area PAs and NPs need to grow in >>
6. Action. At the risk of sounding like a cheerleader, being part of the NP or PA profession is something special; it always has been and always will be. Our professions have grown impressively in numbers, utilization, and stature. We need to cultivate and support our professions and their representative organizations (ie, AANP and AAPA).
In the early decades of each profession, individuals with a great deal of passion and dedication created, advanced, and led these organizations on both state and national levels—and even an international level. You know who they are! Without them, we would not have made the strides that we have as professionals—the attainment of licensure, authority, and reimbursement.
Now that we are being truly recognized for our role in the health care team and our contributions to patient care, some of us may become complacent with regard to our professional organizations. But there will always be legislative and regulatory gains to make, and strong representation (and “strength in numbers”) is the best way to achieve our professional goals. Please, let’s continue to support our organizations not only via membership (which provides funding for initiatives) but also by participating in whatever ways we can to further our professions.
If we are going to fully cement our place in America’s health care system, NPs and PAs must strive to keep up the national dialogue about our patients, their needs, and how our contributions address those needs. I hope you agree. Please share your thoughts with me at PAEditor@frontline medcom.com.
REFERENCES
1. Ridgway S. Loretta Ford, founded nurse practitioner movement. Working Nurse. www.workingnurse.com/articles/loretta-ford-founded-nurse-practitioner-movement. Accessed January 16, 2015.
2. Physician Assistant History Society. Eugene A. Stead Jr, MD. http://pahx.org/stead-jr-eugene. Accessed January 16, 2015.
3. Kartha A, Restuccia J, Burgess J, et al. Nurse practitioner and physician assistant scope of practice in 118 acute care hospitals. J Hosp Med. 2014:9(10); 615-620.
4. Naylor MD, Kurtzman ET. The role of nurse practitioners in reinventing primary care. Health Affairs. 2010;29(5):893-899.
5. Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002;324:819-823.
6. Halter M, Drennan V, Chattopadhyay K, et al. The contribution of physician assistants in primary care: a systematic review. BMC Health Services Research. 2013;13:223-236.
7. Hooker RS, Everett CM. The contributions of physician assistants in primary care systems. Health Social Care Commun. 2012;20(1):20-31.
8. US Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis. The US Health Workforce Chartbook. Part 1: Clinicians. Rockville, MD; 2013.
9. Hooker R. A physician assistant institute [editorial]. J Phys Assist Ed. 2014;25(3):5-6.