User login
WASHINGTON – A program to enhance recovery from bowel surgery significantly decreased the incidence rate of both postoperative ileus and 30-day readmission.
Early walking and postoperative alimentation, beginning with three times on postop day 1, drove the improved outcomes, Dr. Terrence Loftus reported at the annual clinical congress of the American College of Surgeons.
His 3-year retrospective study compared outcomes before and after the program was implemented. In addition to confirming the benefits, the study says something about how change becomes part of a systemwide culture, said Dr. Loftus, medical director of surgical services and clinical resources for Banner Health, Phoenix.
"When you see a before-and-after picture, it gives you the sense that change is like clicking on a light switch, and then everything starts happening. In reality, it’s not. It’s something that catches on over time. It’s a social process that gets passed along. It’s not Dr. Loftus coming in and showing a few slides and saying, ‘Okay, now this is what you have to do.’ It’s surgeons having conversations in the lounge and saying, ‘I tried this and it worked. You should try it too.’ "
In 2010, Banner Health System’s Surgery Clinical Consensus Group decided to tackle the system’s less-than-stellar rates of postoperative ileus and readmission among patients who had bowel surgery.
While there are a number of published enhanced-care pathways, Dr. Loftus found a wide variety of applications over Banner Health’s large medical system. "In some places, people didn’t even know about them, and in others they were using their own version," he said. "We needed a systemwide approach to recovery – something that would be useful over a large, heterogeneous health care system."
The Banner consensus group came up with the Bowel Surgery Strategic Initiative, a program implemented in 19 hospitals spread over six states, covered by 119 surgeons. The system was widely diversified, including everything from an 18-bed critical access unit to a large 600-bed level I trauma center.
"The surgeons ranged from solo private practice, to group practices, hospital employed, and locum tenens, so you can begin to understand the wide diversity of practices and environments we were trying to implement this in," Dr. Loftus said.
The first step was to develop a literature-based GI care pathway that could be widely implemented. The group’s first version had 80 steps – vastly too many.
The final program was based on just two drivers: early alimentation and early ambulation. Eating began with the earliest possible removal of the nasogastric tube (if present), 200-250 cc of oral intake on postoperative day 1, and a progressively advancing diet. Ambulation started with getting up and walking three times on postop day 1, with progressively increasing physical activity.
The team studied a 3-year period spanning 18 months on either side of the implementation date of July 2011. The analysis included 5,000 patients who had undergone elective small- or large-bowel surgery during that time period.
Dr. Loftus said there was a significant increase in both ambulation and alimentation. Before the program, the mean ambulation rate was 53%; that increased to 73% afterward. Alimentation increased from 51% to 71%. The composite of both drivers increased from 53% to 72%.
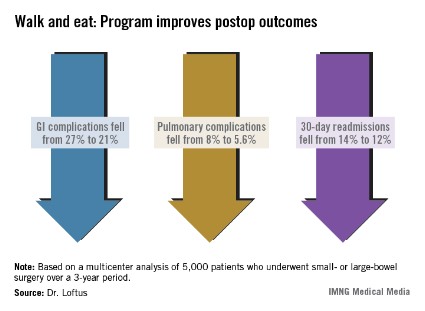
There were associated improvements in most of the clinical outcomes assessed. Overall, the complication rate decreased significantly, from 36% to 29%. Gastrointestinal complications fell from 27% to 21%, with the incidence of postoperative ileus declining from 27% to 21%. Pulmonary complications also decreased significantly, from 8% to 5.6%.
Thirty-day readmission declined from 14% to 12% – also a significant decrease. This was expected, Dr. Loftus said, because most of the readmissions were due to paralytic ileus.
Length of stay, however, was not significantly affected. There was no change in mortality.
The project also illuminated the importance of a facility’s own professional culture. Chart audits found that some facilities were only ambulating patients about a third of the time that it was ordered – even though nursing estimated the rate at 80% and surgeons at 70%.
Facilities that had particularly good postintervention outcomes were already ahead of the game before the project. "These already had a culture of activity. Nursing was getting patients up on day 1, and they set up their schedules in a way that says, ‘These patients will get up. We are going to do this no matter what.’ "
Dr. Loftus had no financial disclosures.
WASHINGTON – A program to enhance recovery from bowel surgery significantly decreased the incidence rate of both postoperative ileus and 30-day readmission.
Early walking and postoperative alimentation, beginning with three times on postop day 1, drove the improved outcomes, Dr. Terrence Loftus reported at the annual clinical congress of the American College of Surgeons.
His 3-year retrospective study compared outcomes before and after the program was implemented. In addition to confirming the benefits, the study says something about how change becomes part of a systemwide culture, said Dr. Loftus, medical director of surgical services and clinical resources for Banner Health, Phoenix.
"When you see a before-and-after picture, it gives you the sense that change is like clicking on a light switch, and then everything starts happening. In reality, it’s not. It’s something that catches on over time. It’s a social process that gets passed along. It’s not Dr. Loftus coming in and showing a few slides and saying, ‘Okay, now this is what you have to do.’ It’s surgeons having conversations in the lounge and saying, ‘I tried this and it worked. You should try it too.’ "
In 2010, Banner Health System’s Surgery Clinical Consensus Group decided to tackle the system’s less-than-stellar rates of postoperative ileus and readmission among patients who had bowel surgery.
While there are a number of published enhanced-care pathways, Dr. Loftus found a wide variety of applications over Banner Health’s large medical system. "In some places, people didn’t even know about them, and in others they were using their own version," he said. "We needed a systemwide approach to recovery – something that would be useful over a large, heterogeneous health care system."
The Banner consensus group came up with the Bowel Surgery Strategic Initiative, a program implemented in 19 hospitals spread over six states, covered by 119 surgeons. The system was widely diversified, including everything from an 18-bed critical access unit to a large 600-bed level I trauma center.
"The surgeons ranged from solo private practice, to group practices, hospital employed, and locum tenens, so you can begin to understand the wide diversity of practices and environments we were trying to implement this in," Dr. Loftus said.
The first step was to develop a literature-based GI care pathway that could be widely implemented. The group’s first version had 80 steps – vastly too many.
The final program was based on just two drivers: early alimentation and early ambulation. Eating began with the earliest possible removal of the nasogastric tube (if present), 200-250 cc of oral intake on postoperative day 1, and a progressively advancing diet. Ambulation started with getting up and walking three times on postop day 1, with progressively increasing physical activity.
The team studied a 3-year period spanning 18 months on either side of the implementation date of July 2011. The analysis included 5,000 patients who had undergone elective small- or large-bowel surgery during that time period.
Dr. Loftus said there was a significant increase in both ambulation and alimentation. Before the program, the mean ambulation rate was 53%; that increased to 73% afterward. Alimentation increased from 51% to 71%. The composite of both drivers increased from 53% to 72%.
There were associated improvements in most of the clinical outcomes assessed. Overall, the complication rate decreased significantly, from 36% to 29%. Gastrointestinal complications fell from 27% to 21%, with the incidence of postoperative ileus declining from 27% to 21%. Pulmonary complications also decreased significantly, from 8% to 5.6%.
Thirty-day readmission declined from 14% to 12% – also a significant decrease. This was expected, Dr. Loftus said, because most of the readmissions were due to paralytic ileus.
Length of stay, however, was not significantly affected. There was no change in mortality.
The project also illuminated the importance of a facility’s own professional culture. Chart audits found that some facilities were only ambulating patients about a third of the time that it was ordered – even though nursing estimated the rate at 80% and surgeons at 70%.
Facilities that had particularly good postintervention outcomes were already ahead of the game before the project. "These already had a culture of activity. Nursing was getting patients up on day 1, and they set up their schedules in a way that says, ‘These patients will get up. We are going to do this no matter what.’ "
Dr. Loftus had no financial disclosures.
WASHINGTON – A program to enhance recovery from bowel surgery significantly decreased the incidence rate of both postoperative ileus and 30-day readmission.
Early walking and postoperative alimentation, beginning with three times on postop day 1, drove the improved outcomes, Dr. Terrence Loftus reported at the annual clinical congress of the American College of Surgeons.
His 3-year retrospective study compared outcomes before and after the program was implemented. In addition to confirming the benefits, the study says something about how change becomes part of a systemwide culture, said Dr. Loftus, medical director of surgical services and clinical resources for Banner Health, Phoenix.
"When you see a before-and-after picture, it gives you the sense that change is like clicking on a light switch, and then everything starts happening. In reality, it’s not. It’s something that catches on over time. It’s a social process that gets passed along. It’s not Dr. Loftus coming in and showing a few slides and saying, ‘Okay, now this is what you have to do.’ It’s surgeons having conversations in the lounge and saying, ‘I tried this and it worked. You should try it too.’ "
In 2010, Banner Health System’s Surgery Clinical Consensus Group decided to tackle the system’s less-than-stellar rates of postoperative ileus and readmission among patients who had bowel surgery.
While there are a number of published enhanced-care pathways, Dr. Loftus found a wide variety of applications over Banner Health’s large medical system. "In some places, people didn’t even know about them, and in others they were using their own version," he said. "We needed a systemwide approach to recovery – something that would be useful over a large, heterogeneous health care system."
The Banner consensus group came up with the Bowel Surgery Strategic Initiative, a program implemented in 19 hospitals spread over six states, covered by 119 surgeons. The system was widely diversified, including everything from an 18-bed critical access unit to a large 600-bed level I trauma center.
"The surgeons ranged from solo private practice, to group practices, hospital employed, and locum tenens, so you can begin to understand the wide diversity of practices and environments we were trying to implement this in," Dr. Loftus said.
The first step was to develop a literature-based GI care pathway that could be widely implemented. The group’s first version had 80 steps – vastly too many.
The final program was based on just two drivers: early alimentation and early ambulation. Eating began with the earliest possible removal of the nasogastric tube (if present), 200-250 cc of oral intake on postoperative day 1, and a progressively advancing diet. Ambulation started with getting up and walking three times on postop day 1, with progressively increasing physical activity.
The team studied a 3-year period spanning 18 months on either side of the implementation date of July 2011. The analysis included 5,000 patients who had undergone elective small- or large-bowel surgery during that time period.
Dr. Loftus said there was a significant increase in both ambulation and alimentation. Before the program, the mean ambulation rate was 53%; that increased to 73% afterward. Alimentation increased from 51% to 71%. The composite of both drivers increased from 53% to 72%.
There were associated improvements in most of the clinical outcomes assessed. Overall, the complication rate decreased significantly, from 36% to 29%. Gastrointestinal complications fell from 27% to 21%, with the incidence of postoperative ileus declining from 27% to 21%. Pulmonary complications also decreased significantly, from 8% to 5.6%.
Thirty-day readmission declined from 14% to 12% – also a significant decrease. This was expected, Dr. Loftus said, because most of the readmissions were due to paralytic ileus.
Length of stay, however, was not significantly affected. There was no change in mortality.
The project also illuminated the importance of a facility’s own professional culture. Chart audits found that some facilities were only ambulating patients about a third of the time that it was ordered – even though nursing estimated the rate at 80% and surgeons at 70%.
Facilities that had particularly good postintervention outcomes were already ahead of the game before the project. "These already had a culture of activity. Nursing was getting patients up on day 1, and they set up their schedules in a way that says, ‘These patients will get up. We are going to do this no matter what.’ "
Dr. Loftus had no financial disclosures.
AT THE ACS CLINICAL CONGRESS
Major finding: A recovery program based on early ambulation and alimentation for patients with bowel surgery decreased readmission from 14% to 12%, and postoperative complications from 36% to 29%.
Data source: The retrospective study contained 5,000 patients who had elective small- or large-bowel surgery.
Disclosures: Dr. Loftus had no financial disclosures.