User login
CHICAGO – The novel reversible B-cell inhibitor XmAb5871 showed promise for delaying loss of improvement after steroid therapy in patients with systemic lupus erythematosus in a randomized, placebo-controlled, phase 2 study.
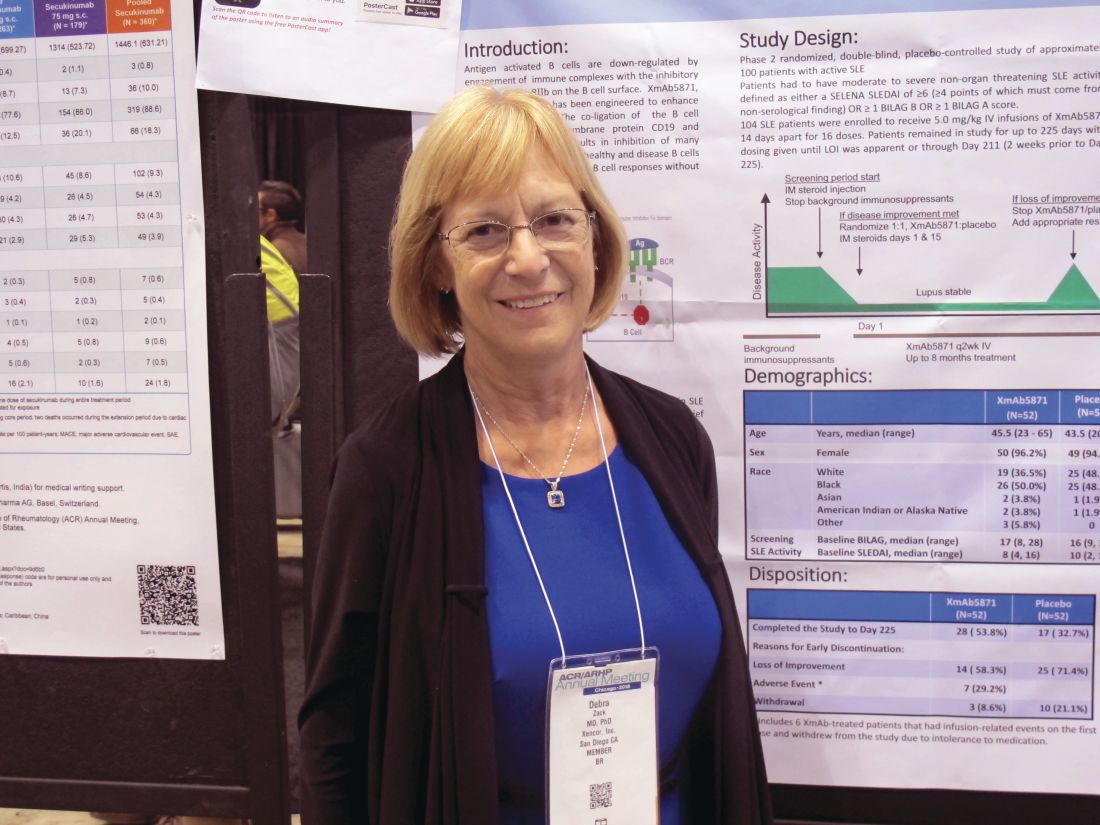
Patients with moderate to severe nonorgan-threatening systemic lupus erythematosus (SLE) who underwent biweekly treatment with XmAb5871 after intramuscular glucocorticoid therapy more often achieved the trial’s primary endpoint of no loss of improvement through day 225 than did patients who took placebo. Overall, 21 (42%) of 50 patients who were randomized to receive active treatment reached this outcome, compared with 12 (29%) of 42 who received placebo based on the “efficacy-evaluable” patient population, defined as those who completed day 225, had a loss of improvement, or discontinued because of a drug-related adverse even. The difference between the treatment and placebo groups with respect to loss of improvement through day 225 reflected a positive trend, but did not reach statistical significance (P = .18), Debra J. Zack, MD, of Xencor in Monrovia, Calif., and her colleagues reported in a poster at the annual meeting of the American College of Rheumatology.
Of the patients who didn’t achieve the primary endpoint, 23 (46%) in the XmAb5871 arm versus 30 (71%) in the placebo arm experienced loss of improvement at any visit, the investigators noted. Six patients in the treatment arm discontinued for toxicity and were also considered nonresponders.
Treatment with XmAb5871 also led to a longer median time to loss of improvement of 230 days in comparison with the 130 days observed in placebo-treated patients. The difference was statistically significant in the efficacy-evaluable population (hazard ratio, 0.53; P = .025) and nearly statistically significant in the intent-to-treat (ITT) population of 52 patients in each group (HR, 0.59; P = .06), they noted.
Maintenance of improvement, which was another secondary endpoint, did not differ significantly between the groups in the efficacy-evaluable population (58.0% vs. 40.5%, respectively; P = .11), but did differ significantly with treatment versus placebo at both day 225 (response rates of 44.0% vs. 23.1%, respectively; P = .06) and at day 169 (57.7% vs. 34.6%; P = .02) in the ITT population, they said.
Of note, patients in the treatment group stayed in the study longer (median of 6.9 vs. 3.6 months) and received more infusions (median of 15.0 vs. 8.5).
“Antigen-activated B cells are down-regulated by engagement of immune complexes with the inhibitory Fcy receptor FcyRIIB on the B cell surface. XmAb5871 is an anti-CD19 monoclonal antibody engineered to enhance binding to FcyRIIB,” they explained, adding that the study was designed using unique methodology to minimize background medication and placebo responses to allow for better interpretation of the results in patients with complex, heterogeneous disease.
Participants were adults with a median age of 44.5 years; most (99 of 104) were women. All received an intramuscular glucocorticoid injection at the start of the screening period as background immunosuppressants were stopped, and those who experienced at least a 4-point decrease on the SLE disease activity index or at least a 1-grade decrease in at least one British Isles Lupus Activity Group A or B score were eligible for enrollment. Background immunosuppressants had to be stopped by the time of enrollment, but patients were allowed to remain on hydroxychloroquine and prednisone 10 mg or less daily or the equivalent.
Those enrolled were randomized to receive intravenous XmAb5871 at a dose of 5 mg/kg or placebo every 14 days for up to 16 doses until day 225 or loss of improvement (at which time patients could receive standard of care and withdraw from the study); all received intramuscular glucocorticoids (Depo-Medrol 80 mg [methylprednisolone acetate]) on days 1 and 15.
XmAb5871 was well tolerated in this study and had a safety profile consistent with that seen in previous SLE studies, with the exception of six withdrawals caused by infusion reactions, the investigators said. They noted that a subcutaneous formulation showed no infusion reactions or gastrointestinal-related infusion reactions in a bioavailability study of 40 healthy subjects, and so a formulation for subcutaneous injection will be used in future studies.
The vast majority of the 149 treatment-related adverse events that occurred in 41 patients in the current study (including 26% in placebo group patients) were mild or moderate in severity. A total of 13 serious adverse events (SAEs) occurred in 11 patients, and included fever, SLE flare (lung), atrial fibrillation, worsening hypertension, iron deficiency anemia, pneumonia (occurring 36 days, or 10 half-lives, after the last dose), infusion-related reaction, and vertigo in the XmAb5871 patients, and anemia SLE flare, SLE flare (enteritis), angioedema, and migraine headache in the placebo group.
“All SAEs were considered not or unlikely related except the infusion-related reaction. There were no deaths and no opportunistic infections,” they wrote.
Although the primary endpoint of loss of improvement by day 225 was not significantly better in the treatment group in this study, a positive trend was noted, the median time to loss of improvement was extended by 76%, and the risk of increased SLE disease activity was reduced by 47% in those who received XmAb5871, they said, concluding that the findings support further evaluation of the agent in patients with SLE.
The study was supported by Xencor.
SOURCE: Zack DJ et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract L14.
CHICAGO – The novel reversible B-cell inhibitor XmAb5871 showed promise for delaying loss of improvement after steroid therapy in patients with systemic lupus erythematosus in a randomized, placebo-controlled, phase 2 study.
Patients with moderate to severe nonorgan-threatening systemic lupus erythematosus (SLE) who underwent biweekly treatment with XmAb5871 after intramuscular glucocorticoid therapy more often achieved the trial’s primary endpoint of no loss of improvement through day 225 than did patients who took placebo. Overall, 21 (42%) of 50 patients who were randomized to receive active treatment reached this outcome, compared with 12 (29%) of 42 who received placebo based on the “efficacy-evaluable” patient population, defined as those who completed day 225, had a loss of improvement, or discontinued because of a drug-related adverse even. The difference between the treatment and placebo groups with respect to loss of improvement through day 225 reflected a positive trend, but did not reach statistical significance (P = .18), Debra J. Zack, MD, of Xencor in Monrovia, Calif., and her colleagues reported in a poster at the annual meeting of the American College of Rheumatology.
Of the patients who didn’t achieve the primary endpoint, 23 (46%) in the XmAb5871 arm versus 30 (71%) in the placebo arm experienced loss of improvement at any visit, the investigators noted. Six patients in the treatment arm discontinued for toxicity and were also considered nonresponders.
Treatment with XmAb5871 also led to a longer median time to loss of improvement of 230 days in comparison with the 130 days observed in placebo-treated patients. The difference was statistically significant in the efficacy-evaluable population (hazard ratio, 0.53; P = .025) and nearly statistically significant in the intent-to-treat (ITT) population of 52 patients in each group (HR, 0.59; P = .06), they noted.
Maintenance of improvement, which was another secondary endpoint, did not differ significantly between the groups in the efficacy-evaluable population (58.0% vs. 40.5%, respectively; P = .11), but did differ significantly with treatment versus placebo at both day 225 (response rates of 44.0% vs. 23.1%, respectively; P = .06) and at day 169 (57.7% vs. 34.6%; P = .02) in the ITT population, they said.
Of note, patients in the treatment group stayed in the study longer (median of 6.9 vs. 3.6 months) and received more infusions (median of 15.0 vs. 8.5).
“Antigen-activated B cells are down-regulated by engagement of immune complexes with the inhibitory Fcy receptor FcyRIIB on the B cell surface. XmAb5871 is an anti-CD19 monoclonal antibody engineered to enhance binding to FcyRIIB,” they explained, adding that the study was designed using unique methodology to minimize background medication and placebo responses to allow for better interpretation of the results in patients with complex, heterogeneous disease.
Participants were adults with a median age of 44.5 years; most (99 of 104) were women. All received an intramuscular glucocorticoid injection at the start of the screening period as background immunosuppressants were stopped, and those who experienced at least a 4-point decrease on the SLE disease activity index or at least a 1-grade decrease in at least one British Isles Lupus Activity Group A or B score were eligible for enrollment. Background immunosuppressants had to be stopped by the time of enrollment, but patients were allowed to remain on hydroxychloroquine and prednisone 10 mg or less daily or the equivalent.
Those enrolled were randomized to receive intravenous XmAb5871 at a dose of 5 mg/kg or placebo every 14 days for up to 16 doses until day 225 or loss of improvement (at which time patients could receive standard of care and withdraw from the study); all received intramuscular glucocorticoids (Depo-Medrol 80 mg [methylprednisolone acetate]) on days 1 and 15.
XmAb5871 was well tolerated in this study and had a safety profile consistent with that seen in previous SLE studies, with the exception of six withdrawals caused by infusion reactions, the investigators said. They noted that a subcutaneous formulation showed no infusion reactions or gastrointestinal-related infusion reactions in a bioavailability study of 40 healthy subjects, and so a formulation for subcutaneous injection will be used in future studies.
The vast majority of the 149 treatment-related adverse events that occurred in 41 patients in the current study (including 26% in placebo group patients) were mild or moderate in severity. A total of 13 serious adverse events (SAEs) occurred in 11 patients, and included fever, SLE flare (lung), atrial fibrillation, worsening hypertension, iron deficiency anemia, pneumonia (occurring 36 days, or 10 half-lives, after the last dose), infusion-related reaction, and vertigo in the XmAb5871 patients, and anemia SLE flare, SLE flare (enteritis), angioedema, and migraine headache in the placebo group.
“All SAEs were considered not or unlikely related except the infusion-related reaction. There were no deaths and no opportunistic infections,” they wrote.
Although the primary endpoint of loss of improvement by day 225 was not significantly better in the treatment group in this study, a positive trend was noted, the median time to loss of improvement was extended by 76%, and the risk of increased SLE disease activity was reduced by 47% in those who received XmAb5871, they said, concluding that the findings support further evaluation of the agent in patients with SLE.
The study was supported by Xencor.
SOURCE: Zack DJ et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract L14.
CHICAGO – The novel reversible B-cell inhibitor XmAb5871 showed promise for delaying loss of improvement after steroid therapy in patients with systemic lupus erythematosus in a randomized, placebo-controlled, phase 2 study.
Patients with moderate to severe nonorgan-threatening systemic lupus erythematosus (SLE) who underwent biweekly treatment with XmAb5871 after intramuscular glucocorticoid therapy more often achieved the trial’s primary endpoint of no loss of improvement through day 225 than did patients who took placebo. Overall, 21 (42%) of 50 patients who were randomized to receive active treatment reached this outcome, compared with 12 (29%) of 42 who received placebo based on the “efficacy-evaluable” patient population, defined as those who completed day 225, had a loss of improvement, or discontinued because of a drug-related adverse even. The difference between the treatment and placebo groups with respect to loss of improvement through day 225 reflected a positive trend, but did not reach statistical significance (P = .18), Debra J. Zack, MD, of Xencor in Monrovia, Calif., and her colleagues reported in a poster at the annual meeting of the American College of Rheumatology.
Of the patients who didn’t achieve the primary endpoint, 23 (46%) in the XmAb5871 arm versus 30 (71%) in the placebo arm experienced loss of improvement at any visit, the investigators noted. Six patients in the treatment arm discontinued for toxicity and were also considered nonresponders.
Treatment with XmAb5871 also led to a longer median time to loss of improvement of 230 days in comparison with the 130 days observed in placebo-treated patients. The difference was statistically significant in the efficacy-evaluable population (hazard ratio, 0.53; P = .025) and nearly statistically significant in the intent-to-treat (ITT) population of 52 patients in each group (HR, 0.59; P = .06), they noted.
Maintenance of improvement, which was another secondary endpoint, did not differ significantly between the groups in the efficacy-evaluable population (58.0% vs. 40.5%, respectively; P = .11), but did differ significantly with treatment versus placebo at both day 225 (response rates of 44.0% vs. 23.1%, respectively; P = .06) and at day 169 (57.7% vs. 34.6%; P = .02) in the ITT population, they said.
Of note, patients in the treatment group stayed in the study longer (median of 6.9 vs. 3.6 months) and received more infusions (median of 15.0 vs. 8.5).
“Antigen-activated B cells are down-regulated by engagement of immune complexes with the inhibitory Fcy receptor FcyRIIB on the B cell surface. XmAb5871 is an anti-CD19 monoclonal antibody engineered to enhance binding to FcyRIIB,” they explained, adding that the study was designed using unique methodology to minimize background medication and placebo responses to allow for better interpretation of the results in patients with complex, heterogeneous disease.
Participants were adults with a median age of 44.5 years; most (99 of 104) were women. All received an intramuscular glucocorticoid injection at the start of the screening period as background immunosuppressants were stopped, and those who experienced at least a 4-point decrease on the SLE disease activity index or at least a 1-grade decrease in at least one British Isles Lupus Activity Group A or B score were eligible for enrollment. Background immunosuppressants had to be stopped by the time of enrollment, but patients were allowed to remain on hydroxychloroquine and prednisone 10 mg or less daily or the equivalent.
Those enrolled were randomized to receive intravenous XmAb5871 at a dose of 5 mg/kg or placebo every 14 days for up to 16 doses until day 225 or loss of improvement (at which time patients could receive standard of care and withdraw from the study); all received intramuscular glucocorticoids (Depo-Medrol 80 mg [methylprednisolone acetate]) on days 1 and 15.
XmAb5871 was well tolerated in this study and had a safety profile consistent with that seen in previous SLE studies, with the exception of six withdrawals caused by infusion reactions, the investigators said. They noted that a subcutaneous formulation showed no infusion reactions or gastrointestinal-related infusion reactions in a bioavailability study of 40 healthy subjects, and so a formulation for subcutaneous injection will be used in future studies.
The vast majority of the 149 treatment-related adverse events that occurred in 41 patients in the current study (including 26% in placebo group patients) were mild or moderate in severity. A total of 13 serious adverse events (SAEs) occurred in 11 patients, and included fever, SLE flare (lung), atrial fibrillation, worsening hypertension, iron deficiency anemia, pneumonia (occurring 36 days, or 10 half-lives, after the last dose), infusion-related reaction, and vertigo in the XmAb5871 patients, and anemia SLE flare, SLE flare (enteritis), angioedema, and migraine headache in the placebo group.
“All SAEs were considered not or unlikely related except the infusion-related reaction. There were no deaths and no opportunistic infections,” they wrote.
Although the primary endpoint of loss of improvement by day 225 was not significantly better in the treatment group in this study, a positive trend was noted, the median time to loss of improvement was extended by 76%, and the risk of increased SLE disease activity was reduced by 47% in those who received XmAb5871, they said, concluding that the findings support further evaluation of the agent in patients with SLE.
The study was supported by Xencor.
SOURCE: Zack DJ et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract L14.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point: XmAb5871 shows promise in systemic lupus erythematosus.
Major finding: There was no loss of improvement through day 225 in 42% of patients treated with XmAb5871 versus 29% with placebo.
Study details: A randomized, placebo-controlled, phase 2 study.
Disclosures: The study was supported by Xencor. Dr. Zack is an employee of Xencor.
Source: Zack DJ et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract L14.