User login
Using Plate Osteosynthesis to Treat Isolated Greater Tuberosity Fractures
Proximal humerus fractures are the second most common fracture in the upper extremity, accounting for 4% to 5% of all fractures.1-4 The majority of these injuries can be treated without an operation. For fractures that require surgery, there are multiple options, including closed reduction, percutaneous pinning, open reduction and internal fixation (ORIF), hemiarthroplasty, and reverse total shoulder arthroplasty.3-9
Isolated greater tuberosity fractures (AO [Arbeitsgemeinschaft für Osteosynthesefragen] 11.A1) make up a small subset of proximal humerus fractures. In general, patients who sustain an isolated greater tuberosity fracture are younger and more active than those who sustain other proximal humerus fractures.2,10 As a result, in the treatment of greater tuberosity fractures, there is increased emphasis on return to high activity and function. Nondisplaced or minimally displaced fractures typically are treated nonoperatively with good success.11,12 Patients with fractures displaced more than 5 mm, and highly active patients with fractures displaced more than 3 mm, usually are recommended for surgical treatment.2,11-14 The many options for treating these difficult fractures include suture fixation, percutaneous techniques, screw fixation, and, more recently, arthroscopic suture techniques.2,5,13,15,16 The goal of any of these operative interventions is to restore normal function and minimize pain around the injured shoulder. Although most of the operative techniques for greater tuberosity fractures have predictable results, none has been established as the gold standard for the treatment of displaced greater tuberosity fractures.2,5,13,15-18 Use of plate osteosynthesis for displaced proximal humerus fractures not isolated to the greater tuberosity is becoming more widespread in the orthopedic community.1,4,19,20 However, the orthopedic literature includes very few reports of using this technique for isolated displaced greater tuberosity fractures.18 This surgical approach potentially provides increased stability, improved maintenance of reduction, and earlier range of motion (ROM) in the postoperative period. These outcomes in turn may allow for improved pain control and earlier return to normal activities than is the case with other operative interventions for these difficult injuries.
We conducted a study to determine the radiographic and clinical outcomes of plate osteosynthesis for displaced greater tuberosity fractures. We hypothesized that excellent clinical and radiographic outcomes could be achieved using this surgical technique.
Patients and Methods
After obtaining institutional review board approval for this study, we retrospectively identified 11 consecutive patients with an isolated displaced greater tuberosity fracture (AO 11.A1) treated with plate osteosynthesis by Dr. Getz between December 2009 and May 2011 (Figures 1A, 1B). We collected data on age at time of surgery, sex, length of follow-up, worker’s compensation status, and complications. At a minimum of 21 months (mean, 27 months; SD, 8 months; range, 16-44 months), we assessed ROM and administered validated outcome scores, including the Single Assessment Numeric Evaluation (SANE)21,22 and the Penn Shoulder Score (PSS).23
Surgical Technique
The deltopectoral approach was used in all 11 patients. A standard incision was made over the deltopectoral interval starting at the coracoid and extending about 6 cm toward the deltoid insertion. After the internervous plane was entered between the deltoid and pectoralis major, the clavipectoral fascia was divided. The greater tuberosity fracture was identified with the leading edge of the fracture 1 cm posterior to the bicipital groove in all cases. Organized hematoma was removed from the fracture site to allow reduction. Three 1-mm braided polyester tapes were placed into the rotator cuff at the insertion onto the greater tuberosity fragment. The sutures thus captured the fragment and were used to obtain reduction and fixation. The fragment was provisionally pinned by placing a 2.0-mm Kirschner wire high on the fragment as to not block plate application. Fluoroscopic imaging was used to determine the appropriate position of the fracture reduction. A standard periarticular proximal humerus 3.5-mm locking compression plate (Zimmer) was used in all patients. The plate was contoured to achieve more compression in several cases in which plastic deformation or comminution was present. The sutures that were attached to the greater tuberosity were then brought through the plate. The plate was then slid down onto the humerus and pinned under fluoroscopic guidance. Three bicortical screws were used to affix the plate to the humeral shaft to compress the fracture into the fracture bed. Two to 4 locking screws were placed into the humeral head to improve the rotational stability of the construct. Last, the sutures through the plate were tied for added fixation.
Rehabilitation
In the immediate postoperative period, all patients were placed in a standard shoulder sling. The sling was worn for 6 weeks. At 2 weeks, patients started formal, standardized physical therapy, including passive ROM for elevation and external rotation. At 6 weeks, they began internal rotation stretching and active-assisted motion. Cuff strengthening began gently, as motion and pain allowed, after 8 weeks. Formal physical therapy continued until full or maximal improvement in motion and strength had been achieved.
Radiographic Measurements
Union/malunion was assessed by 2 orthopedic surgeons during their fellowship year in shoulder and elbow surgery. These surgeons were blinded to patients’ clinical outcomes. Each surgeon reviewed each patient’s radiographs twice to determine whether the reduction was anatomical. Anatomical reduction was achieved if the greater-tuberosity-to-head height was between 4 and 10 mm. Malunion was defined as loss of more than 3 mm of anatomical fracture reduction (from the original reduction) on any radiologic view at most recent follow-up. Loss of reduction was considered minimal if the fracture fragment was displaced less than 3 mm.
Statistical Analysis
A descriptive analysis of patient variables and outcomes was used for this small cohort of patients. Statistical significance was set at α = 0.05.
Results
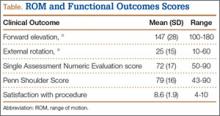
Eleven patients (7 women, 4 men) underwent plate osteosynthesis for an isolated greater tuberosity fracture (Figure 2). Mean age at surgery was 60 years (range, 37-71 years). All patients were right-hand–dominant; 7 of the 11 sustained the injury on the dominant side. For all 11 patients, final postoperative ROM and complications were recorded. No patient required additional surgery. Before injury, all patients felt their shoulder was 100% normal. Nine of the 11 patients were available for assessment of functional outcome and ROM at a mean (SD) of 27 (8) months (range, 16-44 months). At final follow-up, mean (SD) forward elevation was 147° (28°; range, 100°-180°), and mean (SD) external rotation was 25° (15°; range, 10°-60°). Mean (SD) SANE score was 72 (17; range, 50-90), and mean (SD) PSS was 79 (16; range 43-90). On a 1-to-10 scale, patients’ mean (SD) overall satisfaction was 8.6 (1.9; range, 4-10). Of the 9 patients who worked before injury, 8 returned to preoperative duty. Six patients reported stiffness (consistent with ROM). All patients said they would have the surgery again (Table).
All patients experienced radiographic union. Three of the 11 had minimal (<3 mm) loss of reduction. Mean (SD) time to union was 10.7 (4.2) weeks (range, 6.1-21.6 weeks). There were no wound complications and no need for any hardware removal.
Discussion
Isolated greater tuberosity fractures are less common than other types of proximal humerus fractures but often require surgical intervention for less displacement when compared with those fractures.2,14 Multiple techniques (eg, suture fixation, percutaneous pinning, arthroscopic techniques) have been used, but none has established itself as the gold standard for treatment of these difficult injuries.2,5,9,11,13-16 The results of the present study show that plate osteosynthesis can reliably be used to achieve anatomical reduction and good functional outcomes in isolated greater tuberosity fractures. Even with the added stability of the plate and suture construct, a small number of fractures still displaced. In addition, despite having achieved anatomical union, many patients in this study experienced stiffness and functional loss, which speaks to the challenges associated with management of these fractures.
Self-reported outcomes were less favorable for patients in our study (despite achieving mean forward elevation of 147°) than for patients who underwent greater tuberosity repair in other studies.2,5,10 In a study of 12 patients who underwent ORIF of a 2-part displaced fracture of the greater tuberosity of the proximal part of the humerus, Flatow and colleagues5 found half the patients had an excellent outcome, and the other half had a good outcome with active elevation averaging 170°. In another study, conducted over 11 years, 165 patients with a proximal humeral fracture were treated with transosseous suture fixation. Union occurred in all patients except the 2 patients with 3-part fractures, and 155 patients had excellent or very good fracture reduction.10 Therefore, final ROM for these patients may not be a good indicator of actual final function, and previous reports likely underestimated the functional loss experienced by these patients.
The incidence of isolated greater tuberosity fractures likely will increase as the population ages and becomes more active.2,14,16 Patients with isolated greater tuberosity fractures are more likely to be male, to be younger, and to have fewer medical problems than patients with other types of proximal humerus fractures.14 In addition, patient expectations regarding life after displaced greater tuberosity fractures are unique compared with expectations of patients who have other proximal humerus fractures; displaced greater tuberosity fractures usually occur in more active patients, who may expect to return to work and may place higher demands on themselves after treatment,2,14,16,24 possibly leading to lower subjective clinical outcomes.
Various operative treatment techniques for isolated greater tuberosity fractures have been described. Flatow and colleagues5 reported excellent return of forward elevation after ORIF with heavy suture, and half the patients reported excellent outcomes. Other techniques have had mixed results. Bhatia and colleagues11 reported on long-term outcomes of internal fixation using a double row of suture anchors in isolated, displaced greater tuberosity fractures in 21 patients. Outcomes were rated excellent in 8 patients, good in 10, satisfactory in 2, and unsatisfactory in 1. Braunstein and colleagues12 examined the biomechanical strength of various fixation constructs and found that tension band wiring or cancellous screws were superior to suture fixation. More recently, Ji and colleagues13 described encouraging outcomes of arthroscopic fixation of isolated displaced proximal humerus fractures in 16 patients. Mean postoperative American Shoulder and Elbow Surgeons (ASES) score was 88, and mean improvement in University of California, Los Angeles (UCLA) score was 31 points. In addition, mean forward elevation was 148.7° at most recent follow-up.
Our technique supplements the literature on greater tuberosity fracture fixation by using a plate as the point for suture fixation rather than suture anchors or screw fixation. As has been shown with 3- and 4-part fractures, plate osteosynthesis provides proximal suture fixation points and locking screws (often in poor-quality bone) that can prevent suture cut-out and isolated screw failure. In addition, compared with other techniques for greater tuberosity fixation, meta-diaphyseal cortical plate fixation bypasses the often poor bone quality of the greater tuberosity, preventing these modes of failure.18 Schoffl and colleagues18 reported on 10 patients who received a Bamberg plate; all 10 had excellent postoperative outcomes with no complications or secondary loss of reduction. Outcomes in the present study mirror those in the literature for operative fixation of displaced greater tuberosity fractures. Despite the near anatomical reduction in the majority of patients (mean forward elevation, 147°), functional results in this patient population remain guarded, with many patients reporting only good clinical outcomes.
This study had a few limitations. First is the inherent limitation of a retrospective study. Second, the small sample size limited the subgroup analysis. However, given the rarity of the injury and the single-surgeon series, we would have to have added considerable time to the study to increase its power. Third, there was no control group. This is a difficult situation with displaced fractures, as clinical outcomes are poorer with nonoperative management than with operative intervention.2,16,17 Compared with historical operative controls in the literature, our patients compare favorably over medium-term follow-up.2,5,15,16
Conclusion
Plate osteosynthesis is a novel technique in the treatment of displaced greater tuberosity fractures. It results in excellent fracture reduction, a 100% union rate, minimal fracture migration, and good return of ROM. However, self-reported functional assessment of the shoulder was about three-fourths of what is expected of normal or preinjury function.
1. Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant.
J Orthop Trauma. 2008;22(3):195-200.
2. Green A, Izzi J Jr. Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elbow Surg. 2003;12(6):641-649.
3. Neer CS 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077-1089.
4. Ricchetti ET, DeMola PM, Roman D, Abboud JA. The use of precontoured humeral locking plates in the management of displaced proximal humerus fracture. J Am Acad Orthop Surg. 2009;17(9):582-590.
5. Flatow EL, Cuomo F, Maday MG, Miller SR, McIlveen SJ, Bigliani LU. Open reduction and internal fixation of two-part displaced fractures of the greater tuberosity of the proximal part of the humerus. J Bone Joint Surg Am. 1991;73(8):1213-1218.
6. Lenarz C, Shishani Y, McCrum C, Nowinski RJ, Edwards TB, Gobezie R. Is reverse shoulder arthroplasty appropriate for the treatment of fractures in the older patient? Early observations. Clin Orthop Relat Res. 2011;469(12):3324-3331.
7. Park MC, Murthi AM, Roth NS, Blaine TA, Levine WN, Bigliani LU. Two-part and three-part fractures of the proximal humerus treated with suture fixation. J Orthop Trauma. 2003;17(5):319-325.
8. Young SW, Segal BS, Turner PC, Poon PC. Comparison of functional outcomes of reverse shoulder arthroplasty versus hemiarthroplasty in the primary treatment of acute proximal humerus fracture. ANZ J Surg. 2010;80(11):789-793.
9. Dimakopoulos P, Panagopoulos A, Kasimatis G. Transosseous suture fixation of proximal humeral fractures. J Bone Joint Surg Am. 2007;89(8):1700-1709.
10. Dimakopoulos P, Panagopoulos A, Kasimatis G. Transosseous suture fixation of proximal humeral fractures. Surgical technique. J Bone Joint Surg Am. 2009;91(suppl 2, pt 1):8-21.
11. Bhatia DN, van Rooyen KS, du Toit DF, de Beer JF. Surgical treatment of comminuted, displaced fractures of the greater tuberosity of the proximal humerus: a new technique of double-row suture-anchor fixation and long-term results. Injury. 2006;37(10):946-952.
12. Braunstein V, Wiedemann E, Plitz W, Muensterer OJ, Mutschler W, Hinterwimmer S. Operative treatment of greater tuberosity fractures of the humerus—a biomechanical analysis. Clin Biomech. 2007;22(6):652-657.
13. Ji JH, Shafi M, Song IS, Kim YY, McFarland EG, Moon CY. Arthroscopic fixation technique for comminuted, displaced greater tuberosity fracture. Arthroscopy. 2010;26(5):600-609.
14. Kim E, Shin HK, Kim CH. Characteristics of an isolated greater tuberosity fracture of the humerus. J Orthop Sci. 2005;10(5):441-444.
15. Lee SU, Jeong C, Park IJ. Arthroscopic fixation of displaced greater tuberosity fracture of the proximal humerus. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):378-380.
16. Mattyasovszky SG, Burkhart KJ, Ahlers C, et al. Isolated fractures of the greater tuberosity of the proximal humerus. Acta Orthop. 2011;82(6):714-720.
17. Platzer P, Thalhammer G, Oberleitner G, et al. Displaced fractures of the greater tuberosity: a comparison of operative and nonoperative treatment. J Trauma. 2008;65(4):843-848.
18. Schoffl V, Popp D, Strecker W. A simple and effective implant for displaced fractures of the greater tuberosity: the “Bamberg” plate. Arch Orthop Trauma Surg. 2011;131(4):509-512.
19. Gardner MJ, Boraiah S, Helfet DL, Lorich DG. The anterolateral acromial approach for fractures of the proximal humerus. J Orthop Trauma. 2008;22(2):132-137.
20. Ricchetti ET, Warrender WJ, Abboud JA. Use of locking plates in the treatment of proximal humerus fractures. J Shoulder Elbow Surg. 2010;19(2 suppl):66-75.
21. Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27(2):214-221.
22. Williams GN, Taylor DC, Gangel TJ, Uhorchak JM, Arciero RA. Comparison of the Single Assessment Numeric Evaluation method and the Lysholm score. Clin Orthop Relat Res. 2000;(373):184-192.
23. Leggin BG, Michener LA, Shaffer MA, Brenneman SK, Iannotti JP, Williams GR Jr. The Penn Shoulder Score: reliability and validity. J Orthop Sports Phys Ther. 2006;36(3):138-151.
24. Gruson KI, Ruchelsman DE, Tejwani NC. Isolated tuberosity fractures of the proximal humeral: current concepts. Injury. 2008;39(3):284-298.
Proximal humerus fractures are the second most common fracture in the upper extremity, accounting for 4% to 5% of all fractures.1-4 The majority of these injuries can be treated without an operation. For fractures that require surgery, there are multiple options, including closed reduction, percutaneous pinning, open reduction and internal fixation (ORIF), hemiarthroplasty, and reverse total shoulder arthroplasty.3-9
Isolated greater tuberosity fractures (AO [Arbeitsgemeinschaft für Osteosynthesefragen] 11.A1) make up a small subset of proximal humerus fractures. In general, patients who sustain an isolated greater tuberosity fracture are younger and more active than those who sustain other proximal humerus fractures.2,10 As a result, in the treatment of greater tuberosity fractures, there is increased emphasis on return to high activity and function. Nondisplaced or minimally displaced fractures typically are treated nonoperatively with good success.11,12 Patients with fractures displaced more than 5 mm, and highly active patients with fractures displaced more than 3 mm, usually are recommended for surgical treatment.2,11-14 The many options for treating these difficult fractures include suture fixation, percutaneous techniques, screw fixation, and, more recently, arthroscopic suture techniques.2,5,13,15,16 The goal of any of these operative interventions is to restore normal function and minimize pain around the injured shoulder. Although most of the operative techniques for greater tuberosity fractures have predictable results, none has been established as the gold standard for the treatment of displaced greater tuberosity fractures.2,5,13,15-18 Use of plate osteosynthesis for displaced proximal humerus fractures not isolated to the greater tuberosity is becoming more widespread in the orthopedic community.1,4,19,20 However, the orthopedic literature includes very few reports of using this technique for isolated displaced greater tuberosity fractures.18 This surgical approach potentially provides increased stability, improved maintenance of reduction, and earlier range of motion (ROM) in the postoperative period. These outcomes in turn may allow for improved pain control and earlier return to normal activities than is the case with other operative interventions for these difficult injuries.
We conducted a study to determine the radiographic and clinical outcomes of plate osteosynthesis for displaced greater tuberosity fractures. We hypothesized that excellent clinical and radiographic outcomes could be achieved using this surgical technique.
Patients and Methods
After obtaining institutional review board approval for this study, we retrospectively identified 11 consecutive patients with an isolated displaced greater tuberosity fracture (AO 11.A1) treated with plate osteosynthesis by Dr. Getz between December 2009 and May 2011 (Figures 1A, 1B). We collected data on age at time of surgery, sex, length of follow-up, worker’s compensation status, and complications. At a minimum of 21 months (mean, 27 months; SD, 8 months; range, 16-44 months), we assessed ROM and administered validated outcome scores, including the Single Assessment Numeric Evaluation (SANE)21,22 and the Penn Shoulder Score (PSS).23
Surgical Technique
The deltopectoral approach was used in all 11 patients. A standard incision was made over the deltopectoral interval starting at the coracoid and extending about 6 cm toward the deltoid insertion. After the internervous plane was entered between the deltoid and pectoralis major, the clavipectoral fascia was divided. The greater tuberosity fracture was identified with the leading edge of the fracture 1 cm posterior to the bicipital groove in all cases. Organized hematoma was removed from the fracture site to allow reduction. Three 1-mm braided polyester tapes were placed into the rotator cuff at the insertion onto the greater tuberosity fragment. The sutures thus captured the fragment and were used to obtain reduction and fixation. The fragment was provisionally pinned by placing a 2.0-mm Kirschner wire high on the fragment as to not block plate application. Fluoroscopic imaging was used to determine the appropriate position of the fracture reduction. A standard periarticular proximal humerus 3.5-mm locking compression plate (Zimmer) was used in all patients. The plate was contoured to achieve more compression in several cases in which plastic deformation or comminution was present. The sutures that were attached to the greater tuberosity were then brought through the plate. The plate was then slid down onto the humerus and pinned under fluoroscopic guidance. Three bicortical screws were used to affix the plate to the humeral shaft to compress the fracture into the fracture bed. Two to 4 locking screws were placed into the humeral head to improve the rotational stability of the construct. Last, the sutures through the plate were tied for added fixation.
Rehabilitation
In the immediate postoperative period, all patients were placed in a standard shoulder sling. The sling was worn for 6 weeks. At 2 weeks, patients started formal, standardized physical therapy, including passive ROM for elevation and external rotation. At 6 weeks, they began internal rotation stretching and active-assisted motion. Cuff strengthening began gently, as motion and pain allowed, after 8 weeks. Formal physical therapy continued until full or maximal improvement in motion and strength had been achieved.
Radiographic Measurements
Union/malunion was assessed by 2 orthopedic surgeons during their fellowship year in shoulder and elbow surgery. These surgeons were blinded to patients’ clinical outcomes. Each surgeon reviewed each patient’s radiographs twice to determine whether the reduction was anatomical. Anatomical reduction was achieved if the greater-tuberosity-to-head height was between 4 and 10 mm. Malunion was defined as loss of more than 3 mm of anatomical fracture reduction (from the original reduction) on any radiologic view at most recent follow-up. Loss of reduction was considered minimal if the fracture fragment was displaced less than 3 mm.
Statistical Analysis
A descriptive analysis of patient variables and outcomes was used for this small cohort of patients. Statistical significance was set at α = 0.05.
Results
Eleven patients (7 women, 4 men) underwent plate osteosynthesis for an isolated greater tuberosity fracture (Figure 2). Mean age at surgery was 60 years (range, 37-71 years). All patients were right-hand–dominant; 7 of the 11 sustained the injury on the dominant side. For all 11 patients, final postoperative ROM and complications were recorded. No patient required additional surgery. Before injury, all patients felt their shoulder was 100% normal. Nine of the 11 patients were available for assessment of functional outcome and ROM at a mean (SD) of 27 (8) months (range, 16-44 months). At final follow-up, mean (SD) forward elevation was 147° (28°; range, 100°-180°), and mean (SD) external rotation was 25° (15°; range, 10°-60°). Mean (SD) SANE score was 72 (17; range, 50-90), and mean (SD) PSS was 79 (16; range 43-90). On a 1-to-10 scale, patients’ mean (SD) overall satisfaction was 8.6 (1.9; range, 4-10). Of the 9 patients who worked before injury, 8 returned to preoperative duty. Six patients reported stiffness (consistent with ROM). All patients said they would have the surgery again (Table).
All patients experienced radiographic union. Three of the 11 had minimal (<3 mm) loss of reduction. Mean (SD) time to union was 10.7 (4.2) weeks (range, 6.1-21.6 weeks). There were no wound complications and no need for any hardware removal.
Discussion
Isolated greater tuberosity fractures are less common than other types of proximal humerus fractures but often require surgical intervention for less displacement when compared with those fractures.2,14 Multiple techniques (eg, suture fixation, percutaneous pinning, arthroscopic techniques) have been used, but none has established itself as the gold standard for treatment of these difficult injuries.2,5,9,11,13-16 The results of the present study show that plate osteosynthesis can reliably be used to achieve anatomical reduction and good functional outcomes in isolated greater tuberosity fractures. Even with the added stability of the plate and suture construct, a small number of fractures still displaced. In addition, despite having achieved anatomical union, many patients in this study experienced stiffness and functional loss, which speaks to the challenges associated with management of these fractures.
Self-reported outcomes were less favorable for patients in our study (despite achieving mean forward elevation of 147°) than for patients who underwent greater tuberosity repair in other studies.2,5,10 In a study of 12 patients who underwent ORIF of a 2-part displaced fracture of the greater tuberosity of the proximal part of the humerus, Flatow and colleagues5 found half the patients had an excellent outcome, and the other half had a good outcome with active elevation averaging 170°. In another study, conducted over 11 years, 165 patients with a proximal humeral fracture were treated with transosseous suture fixation. Union occurred in all patients except the 2 patients with 3-part fractures, and 155 patients had excellent or very good fracture reduction.10 Therefore, final ROM for these patients may not be a good indicator of actual final function, and previous reports likely underestimated the functional loss experienced by these patients.
The incidence of isolated greater tuberosity fractures likely will increase as the population ages and becomes more active.2,14,16 Patients with isolated greater tuberosity fractures are more likely to be male, to be younger, and to have fewer medical problems than patients with other types of proximal humerus fractures.14 In addition, patient expectations regarding life after displaced greater tuberosity fractures are unique compared with expectations of patients who have other proximal humerus fractures; displaced greater tuberosity fractures usually occur in more active patients, who may expect to return to work and may place higher demands on themselves after treatment,2,14,16,24 possibly leading to lower subjective clinical outcomes.
Various operative treatment techniques for isolated greater tuberosity fractures have been described. Flatow and colleagues5 reported excellent return of forward elevation after ORIF with heavy suture, and half the patients reported excellent outcomes. Other techniques have had mixed results. Bhatia and colleagues11 reported on long-term outcomes of internal fixation using a double row of suture anchors in isolated, displaced greater tuberosity fractures in 21 patients. Outcomes were rated excellent in 8 patients, good in 10, satisfactory in 2, and unsatisfactory in 1. Braunstein and colleagues12 examined the biomechanical strength of various fixation constructs and found that tension band wiring or cancellous screws were superior to suture fixation. More recently, Ji and colleagues13 described encouraging outcomes of arthroscopic fixation of isolated displaced proximal humerus fractures in 16 patients. Mean postoperative American Shoulder and Elbow Surgeons (ASES) score was 88, and mean improvement in University of California, Los Angeles (UCLA) score was 31 points. In addition, mean forward elevation was 148.7° at most recent follow-up.
Our technique supplements the literature on greater tuberosity fracture fixation by using a plate as the point for suture fixation rather than suture anchors or screw fixation. As has been shown with 3- and 4-part fractures, plate osteosynthesis provides proximal suture fixation points and locking screws (often in poor-quality bone) that can prevent suture cut-out and isolated screw failure. In addition, compared with other techniques for greater tuberosity fixation, meta-diaphyseal cortical plate fixation bypasses the often poor bone quality of the greater tuberosity, preventing these modes of failure.18 Schoffl and colleagues18 reported on 10 patients who received a Bamberg plate; all 10 had excellent postoperative outcomes with no complications or secondary loss of reduction. Outcomes in the present study mirror those in the literature for operative fixation of displaced greater tuberosity fractures. Despite the near anatomical reduction in the majority of patients (mean forward elevation, 147°), functional results in this patient population remain guarded, with many patients reporting only good clinical outcomes.
This study had a few limitations. First is the inherent limitation of a retrospective study. Second, the small sample size limited the subgroup analysis. However, given the rarity of the injury and the single-surgeon series, we would have to have added considerable time to the study to increase its power. Third, there was no control group. This is a difficult situation with displaced fractures, as clinical outcomes are poorer with nonoperative management than with operative intervention.2,16,17 Compared with historical operative controls in the literature, our patients compare favorably over medium-term follow-up.2,5,15,16
Conclusion
Plate osteosynthesis is a novel technique in the treatment of displaced greater tuberosity fractures. It results in excellent fracture reduction, a 100% union rate, minimal fracture migration, and good return of ROM. However, self-reported functional assessment of the shoulder was about three-fourths of what is expected of normal or preinjury function.
Proximal humerus fractures are the second most common fracture in the upper extremity, accounting for 4% to 5% of all fractures.1-4 The majority of these injuries can be treated without an operation. For fractures that require surgery, there are multiple options, including closed reduction, percutaneous pinning, open reduction and internal fixation (ORIF), hemiarthroplasty, and reverse total shoulder arthroplasty.3-9
Isolated greater tuberosity fractures (AO [Arbeitsgemeinschaft für Osteosynthesefragen] 11.A1) make up a small subset of proximal humerus fractures. In general, patients who sustain an isolated greater tuberosity fracture are younger and more active than those who sustain other proximal humerus fractures.2,10 As a result, in the treatment of greater tuberosity fractures, there is increased emphasis on return to high activity and function. Nondisplaced or minimally displaced fractures typically are treated nonoperatively with good success.11,12 Patients with fractures displaced more than 5 mm, and highly active patients with fractures displaced more than 3 mm, usually are recommended for surgical treatment.2,11-14 The many options for treating these difficult fractures include suture fixation, percutaneous techniques, screw fixation, and, more recently, arthroscopic suture techniques.2,5,13,15,16 The goal of any of these operative interventions is to restore normal function and minimize pain around the injured shoulder. Although most of the operative techniques for greater tuberosity fractures have predictable results, none has been established as the gold standard for the treatment of displaced greater tuberosity fractures.2,5,13,15-18 Use of plate osteosynthesis for displaced proximal humerus fractures not isolated to the greater tuberosity is becoming more widespread in the orthopedic community.1,4,19,20 However, the orthopedic literature includes very few reports of using this technique for isolated displaced greater tuberosity fractures.18 This surgical approach potentially provides increased stability, improved maintenance of reduction, and earlier range of motion (ROM) in the postoperative period. These outcomes in turn may allow for improved pain control and earlier return to normal activities than is the case with other operative interventions for these difficult injuries.
We conducted a study to determine the radiographic and clinical outcomes of plate osteosynthesis for displaced greater tuberosity fractures. We hypothesized that excellent clinical and radiographic outcomes could be achieved using this surgical technique.
Patients and Methods
After obtaining institutional review board approval for this study, we retrospectively identified 11 consecutive patients with an isolated displaced greater tuberosity fracture (AO 11.A1) treated with plate osteosynthesis by Dr. Getz between December 2009 and May 2011 (Figures 1A, 1B). We collected data on age at time of surgery, sex, length of follow-up, worker’s compensation status, and complications. At a minimum of 21 months (mean, 27 months; SD, 8 months; range, 16-44 months), we assessed ROM and administered validated outcome scores, including the Single Assessment Numeric Evaluation (SANE)21,22 and the Penn Shoulder Score (PSS).23
Surgical Technique
The deltopectoral approach was used in all 11 patients. A standard incision was made over the deltopectoral interval starting at the coracoid and extending about 6 cm toward the deltoid insertion. After the internervous plane was entered between the deltoid and pectoralis major, the clavipectoral fascia was divided. The greater tuberosity fracture was identified with the leading edge of the fracture 1 cm posterior to the bicipital groove in all cases. Organized hematoma was removed from the fracture site to allow reduction. Three 1-mm braided polyester tapes were placed into the rotator cuff at the insertion onto the greater tuberosity fragment. The sutures thus captured the fragment and were used to obtain reduction and fixation. The fragment was provisionally pinned by placing a 2.0-mm Kirschner wire high on the fragment as to not block plate application. Fluoroscopic imaging was used to determine the appropriate position of the fracture reduction. A standard periarticular proximal humerus 3.5-mm locking compression plate (Zimmer) was used in all patients. The plate was contoured to achieve more compression in several cases in which plastic deformation or comminution was present. The sutures that were attached to the greater tuberosity were then brought through the plate. The plate was then slid down onto the humerus and pinned under fluoroscopic guidance. Three bicortical screws were used to affix the plate to the humeral shaft to compress the fracture into the fracture bed. Two to 4 locking screws were placed into the humeral head to improve the rotational stability of the construct. Last, the sutures through the plate were tied for added fixation.
Rehabilitation
In the immediate postoperative period, all patients were placed in a standard shoulder sling. The sling was worn for 6 weeks. At 2 weeks, patients started formal, standardized physical therapy, including passive ROM for elevation and external rotation. At 6 weeks, they began internal rotation stretching and active-assisted motion. Cuff strengthening began gently, as motion and pain allowed, after 8 weeks. Formal physical therapy continued until full or maximal improvement in motion and strength had been achieved.
Radiographic Measurements
Union/malunion was assessed by 2 orthopedic surgeons during their fellowship year in shoulder and elbow surgery. These surgeons were blinded to patients’ clinical outcomes. Each surgeon reviewed each patient’s radiographs twice to determine whether the reduction was anatomical. Anatomical reduction was achieved if the greater-tuberosity-to-head height was between 4 and 10 mm. Malunion was defined as loss of more than 3 mm of anatomical fracture reduction (from the original reduction) on any radiologic view at most recent follow-up. Loss of reduction was considered minimal if the fracture fragment was displaced less than 3 mm.
Statistical Analysis
A descriptive analysis of patient variables and outcomes was used for this small cohort of patients. Statistical significance was set at α = 0.05.
Results
Eleven patients (7 women, 4 men) underwent plate osteosynthesis for an isolated greater tuberosity fracture (Figure 2). Mean age at surgery was 60 years (range, 37-71 years). All patients were right-hand–dominant; 7 of the 11 sustained the injury on the dominant side. For all 11 patients, final postoperative ROM and complications were recorded. No patient required additional surgery. Before injury, all patients felt their shoulder was 100% normal. Nine of the 11 patients were available for assessment of functional outcome and ROM at a mean (SD) of 27 (8) months (range, 16-44 months). At final follow-up, mean (SD) forward elevation was 147° (28°; range, 100°-180°), and mean (SD) external rotation was 25° (15°; range, 10°-60°). Mean (SD) SANE score was 72 (17; range, 50-90), and mean (SD) PSS was 79 (16; range 43-90). On a 1-to-10 scale, patients’ mean (SD) overall satisfaction was 8.6 (1.9; range, 4-10). Of the 9 patients who worked before injury, 8 returned to preoperative duty. Six patients reported stiffness (consistent with ROM). All patients said they would have the surgery again (Table).
All patients experienced radiographic union. Three of the 11 had minimal (<3 mm) loss of reduction. Mean (SD) time to union was 10.7 (4.2) weeks (range, 6.1-21.6 weeks). There were no wound complications and no need for any hardware removal.
Discussion
Isolated greater tuberosity fractures are less common than other types of proximal humerus fractures but often require surgical intervention for less displacement when compared with those fractures.2,14 Multiple techniques (eg, suture fixation, percutaneous pinning, arthroscopic techniques) have been used, but none has established itself as the gold standard for treatment of these difficult injuries.2,5,9,11,13-16 The results of the present study show that plate osteosynthesis can reliably be used to achieve anatomical reduction and good functional outcomes in isolated greater tuberosity fractures. Even with the added stability of the plate and suture construct, a small number of fractures still displaced. In addition, despite having achieved anatomical union, many patients in this study experienced stiffness and functional loss, which speaks to the challenges associated with management of these fractures.
Self-reported outcomes were less favorable for patients in our study (despite achieving mean forward elevation of 147°) than for patients who underwent greater tuberosity repair in other studies.2,5,10 In a study of 12 patients who underwent ORIF of a 2-part displaced fracture of the greater tuberosity of the proximal part of the humerus, Flatow and colleagues5 found half the patients had an excellent outcome, and the other half had a good outcome with active elevation averaging 170°. In another study, conducted over 11 years, 165 patients with a proximal humeral fracture were treated with transosseous suture fixation. Union occurred in all patients except the 2 patients with 3-part fractures, and 155 patients had excellent or very good fracture reduction.10 Therefore, final ROM for these patients may not be a good indicator of actual final function, and previous reports likely underestimated the functional loss experienced by these patients.
The incidence of isolated greater tuberosity fractures likely will increase as the population ages and becomes more active.2,14,16 Patients with isolated greater tuberosity fractures are more likely to be male, to be younger, and to have fewer medical problems than patients with other types of proximal humerus fractures.14 In addition, patient expectations regarding life after displaced greater tuberosity fractures are unique compared with expectations of patients who have other proximal humerus fractures; displaced greater tuberosity fractures usually occur in more active patients, who may expect to return to work and may place higher demands on themselves after treatment,2,14,16,24 possibly leading to lower subjective clinical outcomes.
Various operative treatment techniques for isolated greater tuberosity fractures have been described. Flatow and colleagues5 reported excellent return of forward elevation after ORIF with heavy suture, and half the patients reported excellent outcomes. Other techniques have had mixed results. Bhatia and colleagues11 reported on long-term outcomes of internal fixation using a double row of suture anchors in isolated, displaced greater tuberosity fractures in 21 patients. Outcomes were rated excellent in 8 patients, good in 10, satisfactory in 2, and unsatisfactory in 1. Braunstein and colleagues12 examined the biomechanical strength of various fixation constructs and found that tension band wiring or cancellous screws were superior to suture fixation. More recently, Ji and colleagues13 described encouraging outcomes of arthroscopic fixation of isolated displaced proximal humerus fractures in 16 patients. Mean postoperative American Shoulder and Elbow Surgeons (ASES) score was 88, and mean improvement in University of California, Los Angeles (UCLA) score was 31 points. In addition, mean forward elevation was 148.7° at most recent follow-up.
Our technique supplements the literature on greater tuberosity fracture fixation by using a plate as the point for suture fixation rather than suture anchors or screw fixation. As has been shown with 3- and 4-part fractures, plate osteosynthesis provides proximal suture fixation points and locking screws (often in poor-quality bone) that can prevent suture cut-out and isolated screw failure. In addition, compared with other techniques for greater tuberosity fixation, meta-diaphyseal cortical plate fixation bypasses the often poor bone quality of the greater tuberosity, preventing these modes of failure.18 Schoffl and colleagues18 reported on 10 patients who received a Bamberg plate; all 10 had excellent postoperative outcomes with no complications or secondary loss of reduction. Outcomes in the present study mirror those in the literature for operative fixation of displaced greater tuberosity fractures. Despite the near anatomical reduction in the majority of patients (mean forward elevation, 147°), functional results in this patient population remain guarded, with many patients reporting only good clinical outcomes.
This study had a few limitations. First is the inherent limitation of a retrospective study. Second, the small sample size limited the subgroup analysis. However, given the rarity of the injury and the single-surgeon series, we would have to have added considerable time to the study to increase its power. Third, there was no control group. This is a difficult situation with displaced fractures, as clinical outcomes are poorer with nonoperative management than with operative intervention.2,16,17 Compared with historical operative controls in the literature, our patients compare favorably over medium-term follow-up.2,5,15,16
Conclusion
Plate osteosynthesis is a novel technique in the treatment of displaced greater tuberosity fractures. It results in excellent fracture reduction, a 100% union rate, minimal fracture migration, and good return of ROM. However, self-reported functional assessment of the shoulder was about three-fourths of what is expected of normal or preinjury function.
1. Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant.
J Orthop Trauma. 2008;22(3):195-200.
2. Green A, Izzi J Jr. Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elbow Surg. 2003;12(6):641-649.
3. Neer CS 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077-1089.
4. Ricchetti ET, DeMola PM, Roman D, Abboud JA. The use of precontoured humeral locking plates in the management of displaced proximal humerus fracture. J Am Acad Orthop Surg. 2009;17(9):582-590.
5. Flatow EL, Cuomo F, Maday MG, Miller SR, McIlveen SJ, Bigliani LU. Open reduction and internal fixation of two-part displaced fractures of the greater tuberosity of the proximal part of the humerus. J Bone Joint Surg Am. 1991;73(8):1213-1218.
6. Lenarz C, Shishani Y, McCrum C, Nowinski RJ, Edwards TB, Gobezie R. Is reverse shoulder arthroplasty appropriate for the treatment of fractures in the older patient? Early observations. Clin Orthop Relat Res. 2011;469(12):3324-3331.
7. Park MC, Murthi AM, Roth NS, Blaine TA, Levine WN, Bigliani LU. Two-part and three-part fractures of the proximal humerus treated with suture fixation. J Orthop Trauma. 2003;17(5):319-325.
8. Young SW, Segal BS, Turner PC, Poon PC. Comparison of functional outcomes of reverse shoulder arthroplasty versus hemiarthroplasty in the primary treatment of acute proximal humerus fracture. ANZ J Surg. 2010;80(11):789-793.
9. Dimakopoulos P, Panagopoulos A, Kasimatis G. Transosseous suture fixation of proximal humeral fractures. J Bone Joint Surg Am. 2007;89(8):1700-1709.
10. Dimakopoulos P, Panagopoulos A, Kasimatis G. Transosseous suture fixation of proximal humeral fractures. Surgical technique. J Bone Joint Surg Am. 2009;91(suppl 2, pt 1):8-21.
11. Bhatia DN, van Rooyen KS, du Toit DF, de Beer JF. Surgical treatment of comminuted, displaced fractures of the greater tuberosity of the proximal humerus: a new technique of double-row suture-anchor fixation and long-term results. Injury. 2006;37(10):946-952.
12. Braunstein V, Wiedemann E, Plitz W, Muensterer OJ, Mutschler W, Hinterwimmer S. Operative treatment of greater tuberosity fractures of the humerus—a biomechanical analysis. Clin Biomech. 2007;22(6):652-657.
13. Ji JH, Shafi M, Song IS, Kim YY, McFarland EG, Moon CY. Arthroscopic fixation technique for comminuted, displaced greater tuberosity fracture. Arthroscopy. 2010;26(5):600-609.
14. Kim E, Shin HK, Kim CH. Characteristics of an isolated greater tuberosity fracture of the humerus. J Orthop Sci. 2005;10(5):441-444.
15. Lee SU, Jeong C, Park IJ. Arthroscopic fixation of displaced greater tuberosity fracture of the proximal humerus. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):378-380.
16. Mattyasovszky SG, Burkhart KJ, Ahlers C, et al. Isolated fractures of the greater tuberosity of the proximal humerus. Acta Orthop. 2011;82(6):714-720.
17. Platzer P, Thalhammer G, Oberleitner G, et al. Displaced fractures of the greater tuberosity: a comparison of operative and nonoperative treatment. J Trauma. 2008;65(4):843-848.
18. Schoffl V, Popp D, Strecker W. A simple and effective implant for displaced fractures of the greater tuberosity: the “Bamberg” plate. Arch Orthop Trauma Surg. 2011;131(4):509-512.
19. Gardner MJ, Boraiah S, Helfet DL, Lorich DG. The anterolateral acromial approach for fractures of the proximal humerus. J Orthop Trauma. 2008;22(2):132-137.
20. Ricchetti ET, Warrender WJ, Abboud JA. Use of locking plates in the treatment of proximal humerus fractures. J Shoulder Elbow Surg. 2010;19(2 suppl):66-75.
21. Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27(2):214-221.
22. Williams GN, Taylor DC, Gangel TJ, Uhorchak JM, Arciero RA. Comparison of the Single Assessment Numeric Evaluation method and the Lysholm score. Clin Orthop Relat Res. 2000;(373):184-192.
23. Leggin BG, Michener LA, Shaffer MA, Brenneman SK, Iannotti JP, Williams GR Jr. The Penn Shoulder Score: reliability and validity. J Orthop Sports Phys Ther. 2006;36(3):138-151.
24. Gruson KI, Ruchelsman DE, Tejwani NC. Isolated tuberosity fractures of the proximal humeral: current concepts. Injury. 2008;39(3):284-298.
1. Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant.
J Orthop Trauma. 2008;22(3):195-200.
2. Green A, Izzi J Jr. Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elbow Surg. 2003;12(6):641-649.
3. Neer CS 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077-1089.
4. Ricchetti ET, DeMola PM, Roman D, Abboud JA. The use of precontoured humeral locking plates in the management of displaced proximal humerus fracture. J Am Acad Orthop Surg. 2009;17(9):582-590.
5. Flatow EL, Cuomo F, Maday MG, Miller SR, McIlveen SJ, Bigliani LU. Open reduction and internal fixation of two-part displaced fractures of the greater tuberosity of the proximal part of the humerus. J Bone Joint Surg Am. 1991;73(8):1213-1218.
6. Lenarz C, Shishani Y, McCrum C, Nowinski RJ, Edwards TB, Gobezie R. Is reverse shoulder arthroplasty appropriate for the treatment of fractures in the older patient? Early observations. Clin Orthop Relat Res. 2011;469(12):3324-3331.
7. Park MC, Murthi AM, Roth NS, Blaine TA, Levine WN, Bigliani LU. Two-part and three-part fractures of the proximal humerus treated with suture fixation. J Orthop Trauma. 2003;17(5):319-325.
8. Young SW, Segal BS, Turner PC, Poon PC. Comparison of functional outcomes of reverse shoulder arthroplasty versus hemiarthroplasty in the primary treatment of acute proximal humerus fracture. ANZ J Surg. 2010;80(11):789-793.
9. Dimakopoulos P, Panagopoulos A, Kasimatis G. Transosseous suture fixation of proximal humeral fractures. J Bone Joint Surg Am. 2007;89(8):1700-1709.
10. Dimakopoulos P, Panagopoulos A, Kasimatis G. Transosseous suture fixation of proximal humeral fractures. Surgical technique. J Bone Joint Surg Am. 2009;91(suppl 2, pt 1):8-21.
11. Bhatia DN, van Rooyen KS, du Toit DF, de Beer JF. Surgical treatment of comminuted, displaced fractures of the greater tuberosity of the proximal humerus: a new technique of double-row suture-anchor fixation and long-term results. Injury. 2006;37(10):946-952.
12. Braunstein V, Wiedemann E, Plitz W, Muensterer OJ, Mutschler W, Hinterwimmer S. Operative treatment of greater tuberosity fractures of the humerus—a biomechanical analysis. Clin Biomech. 2007;22(6):652-657.
13. Ji JH, Shafi M, Song IS, Kim YY, McFarland EG, Moon CY. Arthroscopic fixation technique for comminuted, displaced greater tuberosity fracture. Arthroscopy. 2010;26(5):600-609.
14. Kim E, Shin HK, Kim CH. Characteristics of an isolated greater tuberosity fracture of the humerus. J Orthop Sci. 2005;10(5):441-444.
15. Lee SU, Jeong C, Park IJ. Arthroscopic fixation of displaced greater tuberosity fracture of the proximal humerus. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):378-380.
16. Mattyasovszky SG, Burkhart KJ, Ahlers C, et al. Isolated fractures of the greater tuberosity of the proximal humerus. Acta Orthop. 2011;82(6):714-720.
17. Platzer P, Thalhammer G, Oberleitner G, et al. Displaced fractures of the greater tuberosity: a comparison of operative and nonoperative treatment. J Trauma. 2008;65(4):843-848.
18. Schoffl V, Popp D, Strecker W. A simple and effective implant for displaced fractures of the greater tuberosity: the “Bamberg” plate. Arch Orthop Trauma Surg. 2011;131(4):509-512.
19. Gardner MJ, Boraiah S, Helfet DL, Lorich DG. The anterolateral acromial approach for fractures of the proximal humerus. J Orthop Trauma. 2008;22(2):132-137.
20. Ricchetti ET, Warrender WJ, Abboud JA. Use of locking plates in the treatment of proximal humerus fractures. J Shoulder Elbow Surg. 2010;19(2 suppl):66-75.
21. Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27(2):214-221.
22. Williams GN, Taylor DC, Gangel TJ, Uhorchak JM, Arciero RA. Comparison of the Single Assessment Numeric Evaluation method and the Lysholm score. Clin Orthop Relat Res. 2000;(373):184-192.
23. Leggin BG, Michener LA, Shaffer MA, Brenneman SK, Iannotti JP, Williams GR Jr. The Penn Shoulder Score: reliability and validity. J Orthop Sports Phys Ther. 2006;36(3):138-151.
24. Gruson KI, Ruchelsman DE, Tejwani NC. Isolated tuberosity fractures of the proximal humeral: current concepts. Injury. 2008;39(3):284-298.