User login
Tom Collins is a freelance writer in South Florida who has written about medical topics from nasty infections to ethical dilemmas, runaway tumors to tornado-chasing doctors. He travels the globe gathering conference health news and lives in West Palm Beach.
Patients with asthma and COPD lost ground in accessing care
Over the past 20 years, patients with asthma and chronic obstructive pulmonary disease (COPD) have seen next to no improvement in problems of delayed care because of cost or unaffordable medications, despite wider insurance coverage since the passage of the Affordable Care Act, a new analysis shows.
The long-view analysis illuminates the ongoing problem for people with these chronic diseases despite health care legislation that was considered historic.
“That long-term scope puts recent improvements in better context – whereas we have made improvements in coverage in recent years due to the Affordable Care Act, the longer-term picture is that people with asthma and COPD are struggling to obtain needed medical care and medications despite a substantial reduction in the uninsurance rate,” said Adam Gaffney, MD, MPH, assistant professor of medicine at Harvard Medical School, Boston who authored the paper with David Himmelstein, MD, professor of public health at City University of New York–Hunter College. The findings were published in Chest.
Researchers examined data from 1997 to 2018 for 76,843 adults with asthma and 30,548 adults with COPD, from the National Health Interview Survey, an annual survey by the Centers for Disease Control that is based on in-person interviews and health questionnaires completed by an adult in each family.
Insurance coverage up, patients losing ground
During 1997 and 2018, there was an overall 9.3% decrease in the rate of adults with asthma who were uninsured, a significant improvement (P < .001). Between the pre- and post-ACA years, there was modest improvement in those putting off care because of cost, a drop of 3.8%, or going without prescriptions, a drop of 4.0%. But those improvements didn’t correspond to the 7.2% drop in the uninsured rate after the AC , contributing to the finding that there was no significant improvement over the 20 years.
For adults with COPD, it was a slightly different story. Over those 2 decades, the uninsured rate dropped by 9.5%. But the number of patients foregoing care due to cost actually rose by 3.4%, which wasn’t statistically significant, but the rate of those unable to afford needed medications rose significantly by 7.8%.
Researchers found there was improvement between the pre- and post-ACA years among COPD patients putting off care and going without medications (decreases of 6.9% and 4.5%, respectively). That adhered fairly closely with the improvement in the uninsured rate, which fell by 7.1%. But over the 20-year study period, the percentage of those needing medications they couldn’t afford increased significantly by 7.8%. The rate of those delaying or foregoing care also increased, though this amount was not statistically significant.
After the ACA was created, Blacks and Hispanics with asthma had greater improvement in obtaining insurance, compared with other racial and ethnic groups. But over the 20 years, like all racial and ethnic groups, they saw no statistically significant improvement in rates of “inadequate coverage,” defined in this study as either being uninsured, having to delay care because of cost, or being unable to afford needed medications.
For those with COPD, only Whites had statistically significant improvement in the number of patients with inadequate coverage after the ACA, researchers found.
So despite obtaining insurance, patients lost ground in managing their disease because of the growing cost of care and medication.
“Medication affordability has actually worsened for those with COPD – a worrisome development given that medication nonadherence worsens outcomes for these vulnerable patients,” Dr. Gaffney said. “Policy makers should return to the issue of national health care reform. Both uninsurance and underinsurance undermines pulmonologists’ ability to care for their patients with chronic disease. A health care system without financial barriers, in contrast, might well improve these patients’ outcomes, and advance health equity.”
Insurance is no guarantee to access
Daniel Ouellette, MD, FCCP, a pulmonary and critical care specialist at Henry Ford Health System in Detroit, said it’s not surprising that access to care remains a problem despite the Affordable Care Act.
“It covers the hospitalizations and ER visits – patients in this segment of society were getting cared for there anyway,” he said. “And what the ACA didn’t always do was provide adequate prescription coverage or cover these outpatient gaps. So even though the patients have the ACA they still have unaffordable prescriptions, they still can’t buy them, and they still can’t pay for their outpatient clinic if they have a $500 or $1,000 deductible.” These patients also continue to struggle with more fundamental issues that affect access to care, such as lack of transportation and poor health literacy.
At Henry Ford, pharmacists work with patients to identify medications covered by their insurance and work to find discounts and coupons, he said. As for the ACA, “it’s a good first start, but we really need to identify what its limitations are.” Locally driven, less expensive solutions might be a better way forward than costly federal initiatives.
Brandon M. Seay, MD, a pediatric pulmonologist and sleep specialist at Children’s Healthcare of Atlanta, said the findings dovetail with what he has seen in the pediatric population.
“From my experience, the ACA has helped patients get their foot in the door and has helped patients decrease the possibility of serious financial burden in emergency situations, but the ability to afford medications has not changed very much,” he said. When patients struggle with sufficient prescription coverage, he helps patients fight for coverage and connects them with prescription assistance programs such as GoodRx.
“Instead of focusing on the access of insurance to patients, the goal of the system should be to make care as affordable as possible,” Dr. Seay said. “Access does not meet the needs of a patient if they cannot afford what they have access to. Transition to a nationalized health system where there is no question of access could help to drive down prescription drug prices by allowing the government to negotiate with pharmaceutical companies more adequately by removing the ‘middle man’ of the private insurance industry.”
The investigators reported no financial conflicts. Dr. Ouellette and Dr. Seay reported no financial conflicts.
Over the past 20 years, patients with asthma and chronic obstructive pulmonary disease (COPD) have seen next to no improvement in problems of delayed care because of cost or unaffordable medications, despite wider insurance coverage since the passage of the Affordable Care Act, a new analysis shows.
The long-view analysis illuminates the ongoing problem for people with these chronic diseases despite health care legislation that was considered historic.
“That long-term scope puts recent improvements in better context – whereas we have made improvements in coverage in recent years due to the Affordable Care Act, the longer-term picture is that people with asthma and COPD are struggling to obtain needed medical care and medications despite a substantial reduction in the uninsurance rate,” said Adam Gaffney, MD, MPH, assistant professor of medicine at Harvard Medical School, Boston who authored the paper with David Himmelstein, MD, professor of public health at City University of New York–Hunter College. The findings were published in Chest.
Researchers examined data from 1997 to 2018 for 76,843 adults with asthma and 30,548 adults with COPD, from the National Health Interview Survey, an annual survey by the Centers for Disease Control that is based on in-person interviews and health questionnaires completed by an adult in each family.
Insurance coverage up, patients losing ground
During 1997 and 2018, there was an overall 9.3% decrease in the rate of adults with asthma who were uninsured, a significant improvement (P < .001). Between the pre- and post-ACA years, there was modest improvement in those putting off care because of cost, a drop of 3.8%, or going without prescriptions, a drop of 4.0%. But those improvements didn’t correspond to the 7.2% drop in the uninsured rate after the AC , contributing to the finding that there was no significant improvement over the 20 years.
For adults with COPD, it was a slightly different story. Over those 2 decades, the uninsured rate dropped by 9.5%. But the number of patients foregoing care due to cost actually rose by 3.4%, which wasn’t statistically significant, but the rate of those unable to afford needed medications rose significantly by 7.8%.
Researchers found there was improvement between the pre- and post-ACA years among COPD patients putting off care and going without medications (decreases of 6.9% and 4.5%, respectively). That adhered fairly closely with the improvement in the uninsured rate, which fell by 7.1%. But over the 20-year study period, the percentage of those needing medications they couldn’t afford increased significantly by 7.8%. The rate of those delaying or foregoing care also increased, though this amount was not statistically significant.
After the ACA was created, Blacks and Hispanics with asthma had greater improvement in obtaining insurance, compared with other racial and ethnic groups. But over the 20 years, like all racial and ethnic groups, they saw no statistically significant improvement in rates of “inadequate coverage,” defined in this study as either being uninsured, having to delay care because of cost, or being unable to afford needed medications.
For those with COPD, only Whites had statistically significant improvement in the number of patients with inadequate coverage after the ACA, researchers found.
So despite obtaining insurance, patients lost ground in managing their disease because of the growing cost of care and medication.
“Medication affordability has actually worsened for those with COPD – a worrisome development given that medication nonadherence worsens outcomes for these vulnerable patients,” Dr. Gaffney said. “Policy makers should return to the issue of national health care reform. Both uninsurance and underinsurance undermines pulmonologists’ ability to care for their patients with chronic disease. A health care system without financial barriers, in contrast, might well improve these patients’ outcomes, and advance health equity.”
Insurance is no guarantee to access
Daniel Ouellette, MD, FCCP, a pulmonary and critical care specialist at Henry Ford Health System in Detroit, said it’s not surprising that access to care remains a problem despite the Affordable Care Act.
“It covers the hospitalizations and ER visits – patients in this segment of society were getting cared for there anyway,” he said. “And what the ACA didn’t always do was provide adequate prescription coverage or cover these outpatient gaps. So even though the patients have the ACA they still have unaffordable prescriptions, they still can’t buy them, and they still can’t pay for their outpatient clinic if they have a $500 or $1,000 deductible.” These patients also continue to struggle with more fundamental issues that affect access to care, such as lack of transportation and poor health literacy.
At Henry Ford, pharmacists work with patients to identify medications covered by their insurance and work to find discounts and coupons, he said. As for the ACA, “it’s a good first start, but we really need to identify what its limitations are.” Locally driven, less expensive solutions might be a better way forward than costly federal initiatives.
Brandon M. Seay, MD, a pediatric pulmonologist and sleep specialist at Children’s Healthcare of Atlanta, said the findings dovetail with what he has seen in the pediatric population.
“From my experience, the ACA has helped patients get their foot in the door and has helped patients decrease the possibility of serious financial burden in emergency situations, but the ability to afford medications has not changed very much,” he said. When patients struggle with sufficient prescription coverage, he helps patients fight for coverage and connects them with prescription assistance programs such as GoodRx.
“Instead of focusing on the access of insurance to patients, the goal of the system should be to make care as affordable as possible,” Dr. Seay said. “Access does not meet the needs of a patient if they cannot afford what they have access to. Transition to a nationalized health system where there is no question of access could help to drive down prescription drug prices by allowing the government to negotiate with pharmaceutical companies more adequately by removing the ‘middle man’ of the private insurance industry.”
The investigators reported no financial conflicts. Dr. Ouellette and Dr. Seay reported no financial conflicts.
Over the past 20 years, patients with asthma and chronic obstructive pulmonary disease (COPD) have seen next to no improvement in problems of delayed care because of cost or unaffordable medications, despite wider insurance coverage since the passage of the Affordable Care Act, a new analysis shows.
The long-view analysis illuminates the ongoing problem for people with these chronic diseases despite health care legislation that was considered historic.
“That long-term scope puts recent improvements in better context – whereas we have made improvements in coverage in recent years due to the Affordable Care Act, the longer-term picture is that people with asthma and COPD are struggling to obtain needed medical care and medications despite a substantial reduction in the uninsurance rate,” said Adam Gaffney, MD, MPH, assistant professor of medicine at Harvard Medical School, Boston who authored the paper with David Himmelstein, MD, professor of public health at City University of New York–Hunter College. The findings were published in Chest.
Researchers examined data from 1997 to 2018 for 76,843 adults with asthma and 30,548 adults with COPD, from the National Health Interview Survey, an annual survey by the Centers for Disease Control that is based on in-person interviews and health questionnaires completed by an adult in each family.
Insurance coverage up, patients losing ground
During 1997 and 2018, there was an overall 9.3% decrease in the rate of adults with asthma who were uninsured, a significant improvement (P < .001). Between the pre- and post-ACA years, there was modest improvement in those putting off care because of cost, a drop of 3.8%, or going without prescriptions, a drop of 4.0%. But those improvements didn’t correspond to the 7.2% drop in the uninsured rate after the AC , contributing to the finding that there was no significant improvement over the 20 years.
For adults with COPD, it was a slightly different story. Over those 2 decades, the uninsured rate dropped by 9.5%. But the number of patients foregoing care due to cost actually rose by 3.4%, which wasn’t statistically significant, but the rate of those unable to afford needed medications rose significantly by 7.8%.
Researchers found there was improvement between the pre- and post-ACA years among COPD patients putting off care and going without medications (decreases of 6.9% and 4.5%, respectively). That adhered fairly closely with the improvement in the uninsured rate, which fell by 7.1%. But over the 20-year study period, the percentage of those needing medications they couldn’t afford increased significantly by 7.8%. The rate of those delaying or foregoing care also increased, though this amount was not statistically significant.
After the ACA was created, Blacks and Hispanics with asthma had greater improvement in obtaining insurance, compared with other racial and ethnic groups. But over the 20 years, like all racial and ethnic groups, they saw no statistically significant improvement in rates of “inadequate coverage,” defined in this study as either being uninsured, having to delay care because of cost, or being unable to afford needed medications.
For those with COPD, only Whites had statistically significant improvement in the number of patients with inadequate coverage after the ACA, researchers found.
So despite obtaining insurance, patients lost ground in managing their disease because of the growing cost of care and medication.
“Medication affordability has actually worsened for those with COPD – a worrisome development given that medication nonadherence worsens outcomes for these vulnerable patients,” Dr. Gaffney said. “Policy makers should return to the issue of national health care reform. Both uninsurance and underinsurance undermines pulmonologists’ ability to care for their patients with chronic disease. A health care system without financial barriers, in contrast, might well improve these patients’ outcomes, and advance health equity.”
Insurance is no guarantee to access
Daniel Ouellette, MD, FCCP, a pulmonary and critical care specialist at Henry Ford Health System in Detroit, said it’s not surprising that access to care remains a problem despite the Affordable Care Act.
“It covers the hospitalizations and ER visits – patients in this segment of society were getting cared for there anyway,” he said. “And what the ACA didn’t always do was provide adequate prescription coverage or cover these outpatient gaps. So even though the patients have the ACA they still have unaffordable prescriptions, they still can’t buy them, and they still can’t pay for their outpatient clinic if they have a $500 or $1,000 deductible.” These patients also continue to struggle with more fundamental issues that affect access to care, such as lack of transportation and poor health literacy.
At Henry Ford, pharmacists work with patients to identify medications covered by their insurance and work to find discounts and coupons, he said. As for the ACA, “it’s a good first start, but we really need to identify what its limitations are.” Locally driven, less expensive solutions might be a better way forward than costly federal initiatives.
Brandon M. Seay, MD, a pediatric pulmonologist and sleep specialist at Children’s Healthcare of Atlanta, said the findings dovetail with what he has seen in the pediatric population.
“From my experience, the ACA has helped patients get their foot in the door and has helped patients decrease the possibility of serious financial burden in emergency situations, but the ability to afford medications has not changed very much,” he said. When patients struggle with sufficient prescription coverage, he helps patients fight for coverage and connects them with prescription assistance programs such as GoodRx.
“Instead of focusing on the access of insurance to patients, the goal of the system should be to make care as affordable as possible,” Dr. Seay said. “Access does not meet the needs of a patient if they cannot afford what they have access to. Transition to a nationalized health system where there is no question of access could help to drive down prescription drug prices by allowing the government to negotiate with pharmaceutical companies more adequately by removing the ‘middle man’ of the private insurance industry.”
The investigators reported no financial conflicts. Dr. Ouellette and Dr. Seay reported no financial conflicts.
FROM CHEST
Lifestyle coaching for obesity associated with improved cardiometabolic numbers in study
Patients who received intensive lifestyle training by coaches in the primary care setting experienced improvement in several indicators of cardiometabolic health in a 2-year trial.
The 803 trial participants comprised a racially diverse, low-income population with obesity. In this study, primary care clinics were randomly assigned to provide weight-loss coaching or usual care. Patients at the intensive training clinics lost significantly more weight than the other patients, as reported in a paper published in September in the New England Journal of Medicine on the PROmoting Successful Weight Loss in Primary CarE in Louisiana (PROPEL) trial. The patients who received weight loss coaching also had significantly more improvement in HDL cholesterol levels, total to HDL cholesterol ratios, and metabolic syndrome severity score, said researchers in the new paper on the PROPEL trial, which was published in Circulation on February 8 .
“We believe that one reason for success of the program was the use of a health coach [who] was embedded in the primary care office,” said lead author Peter Katzmarzyk, PhD, associate executive director for population and public health sciences at the Pennington Biomedical Research Center, Baton Rouge, La. “This way, the patients could get their counseling in a familiar environment and did not have to go to a different setting. The coaches developed close relationships with the patients over the 2 years, and this helped develop a sense of responsibility in the patients as the coaches were helping the patients to set goals and kept them accountable.”
In the PROPEL study, 67% of patients were Black and had low health literacy scores that corresponded with less than a ninth-grade education level. The intensive lifestyle intervention program included weekly sessions with the trained health coaches over the first 6 months — 16 face-to-face and 6 over the phone — and then at least monthly for the last 18 months. The coaches had higher education degrees in nutrition, physical activity, or behavioral medicine. Before the program started, the coaches also received training in the management of obesity and related health issues, health literacy, and patient communication and education. The goal of the program was 10% weight loss, using personalized action plans on eating, dieting, and physical activity.
Those in the usual-care clinics continued receiving normal care and received newsletters on health topics, such as the importance of sleep and tips for limiting time spent sitting. The primary care physicians at those clinics also were given a presentation with Centers for Medicare & Medicaid Services (CMS) information on intensive lifestyle interventions for obesity.
Cholesterol changes in intervention vs. control group
HDL cholesterol improved significantly among the coached patients, compared with the other patients, with a mean difference of 4.1 mg/dL at 1 year and 4.6 mg/dL at 2 years (P less than .01 for both). The total cholesterol to HDL cholesterol ratio showed a similarly significant difference in decline, with a between-group difference of –0.29 at 1 year and –0.31 at 2 years (P less than .01 for both). Also, the difference in the change in metabolic severity scores were –0.40 at 1 year and –0.21 at 2 years (P less than .01 for both).
Fasting blood glucose had declined after the 1st year by a significantly greater degree in the clinics with coaching, compared with the others, but not after the second year, researchers found.
There were no significant differences seen in total cholesterol, LDL cholesterol, non-HDL cholesterol, or blood pressure. Dr. Katzmarzyk said the likely reason for no change in blood pressure was that it was already relatively well-controlled at baseline for all the patients.
Funding barriers to obesity treatment
The CMS currently cover intensive training for obesity if delivered directly by a primary care physician, according to the authors of the new paper. Dr. Katzmarzyk said he hopes that will change.
“We are hoping that the evidence provided in this study may change the way that CMS funds obesity treatment in the future by allowing an expansion of the care team,” he said.
John Flack, MD, chair of internal medicine at Southern Illinois University, Springfield, said that the main achievement of the study was that it showed that intensive weight-loss training in the primary-care setting could be accomplished in a racially diverse population with low health literacy.
“You can’t just automatically assume just because you’ve seen it in some other populations that you can replicate this in every population, so they’ve done a really good job,” he said.
That programs are eligible for reimbursement only if they’re run by primary-care physicians is an ongoing problem, he said.
“You don’t necessarily need to be a physician to do this,” Dr. Flack said.
For best results, payment for coaching should not be tied to office visits, Dr. Flack noted.
“If they’re de-tethered from the office visits and you’re paid for quality ... you’re going to build out your infrastructure differently to care for people,” he said.
Andrew Freeman, MD, associate professor of medicine at the University of Colorado, Denver, and cochair of the American College of Cardiology’s nutrition and lifestyle work group, said the findings dovetail with his experience.
“I’m a huge believer that when people need to make lifestyle changes, having someone hold their hand and guide them through the effort is incredibly rewarding and incredibly powerful,” said Dr. Freeman, who also oversees the intensive cardiac rehab program at National Jewish Health in Denver.
A program like this needs proper funding in order to work, Dr, Freeman noted. He added that, even with coaches being paid well, “if you are able to prevent just one readmission for, say, heart failure a month . . . you could be saving millions of dollars over just a couple of years.”
Dr. Katzmarzyk, Dr. Flack, and Dr. Freeman reported no relevant disclosures. Louisiana State University, Pennington Biomedical Research Center, and Montclair State University have interest in the intellectual property surrounding a weight graph used in the study. The other researchers reported grants and/or fees from Bayer, Boehringer Ingelheim, Gilead, Takeda, Novo Nordisk, and other companies.
Patients who received intensive lifestyle training by coaches in the primary care setting experienced improvement in several indicators of cardiometabolic health in a 2-year trial.
The 803 trial participants comprised a racially diverse, low-income population with obesity. In this study, primary care clinics were randomly assigned to provide weight-loss coaching or usual care. Patients at the intensive training clinics lost significantly more weight than the other patients, as reported in a paper published in September in the New England Journal of Medicine on the PROmoting Successful Weight Loss in Primary CarE in Louisiana (PROPEL) trial. The patients who received weight loss coaching also had significantly more improvement in HDL cholesterol levels, total to HDL cholesterol ratios, and metabolic syndrome severity score, said researchers in the new paper on the PROPEL trial, which was published in Circulation on February 8 .
“We believe that one reason for success of the program was the use of a health coach [who] was embedded in the primary care office,” said lead author Peter Katzmarzyk, PhD, associate executive director for population and public health sciences at the Pennington Biomedical Research Center, Baton Rouge, La. “This way, the patients could get their counseling in a familiar environment and did not have to go to a different setting. The coaches developed close relationships with the patients over the 2 years, and this helped develop a sense of responsibility in the patients as the coaches were helping the patients to set goals and kept them accountable.”
In the PROPEL study, 67% of patients were Black and had low health literacy scores that corresponded with less than a ninth-grade education level. The intensive lifestyle intervention program included weekly sessions with the trained health coaches over the first 6 months — 16 face-to-face and 6 over the phone — and then at least monthly for the last 18 months. The coaches had higher education degrees in nutrition, physical activity, or behavioral medicine. Before the program started, the coaches also received training in the management of obesity and related health issues, health literacy, and patient communication and education. The goal of the program was 10% weight loss, using personalized action plans on eating, dieting, and physical activity.
Those in the usual-care clinics continued receiving normal care and received newsletters on health topics, such as the importance of sleep and tips for limiting time spent sitting. The primary care physicians at those clinics also were given a presentation with Centers for Medicare & Medicaid Services (CMS) information on intensive lifestyle interventions for obesity.
Cholesterol changes in intervention vs. control group
HDL cholesterol improved significantly among the coached patients, compared with the other patients, with a mean difference of 4.1 mg/dL at 1 year and 4.6 mg/dL at 2 years (P less than .01 for both). The total cholesterol to HDL cholesterol ratio showed a similarly significant difference in decline, with a between-group difference of –0.29 at 1 year and –0.31 at 2 years (P less than .01 for both). Also, the difference in the change in metabolic severity scores were –0.40 at 1 year and –0.21 at 2 years (P less than .01 for both).
Fasting blood glucose had declined after the 1st year by a significantly greater degree in the clinics with coaching, compared with the others, but not after the second year, researchers found.
There were no significant differences seen in total cholesterol, LDL cholesterol, non-HDL cholesterol, or blood pressure. Dr. Katzmarzyk said the likely reason for no change in blood pressure was that it was already relatively well-controlled at baseline for all the patients.
Funding barriers to obesity treatment
The CMS currently cover intensive training for obesity if delivered directly by a primary care physician, according to the authors of the new paper. Dr. Katzmarzyk said he hopes that will change.
“We are hoping that the evidence provided in this study may change the way that CMS funds obesity treatment in the future by allowing an expansion of the care team,” he said.
John Flack, MD, chair of internal medicine at Southern Illinois University, Springfield, said that the main achievement of the study was that it showed that intensive weight-loss training in the primary-care setting could be accomplished in a racially diverse population with low health literacy.
“You can’t just automatically assume just because you’ve seen it in some other populations that you can replicate this in every population, so they’ve done a really good job,” he said.
That programs are eligible for reimbursement only if they’re run by primary-care physicians is an ongoing problem, he said.
“You don’t necessarily need to be a physician to do this,” Dr. Flack said.
For best results, payment for coaching should not be tied to office visits, Dr. Flack noted.
“If they’re de-tethered from the office visits and you’re paid for quality ... you’re going to build out your infrastructure differently to care for people,” he said.
Andrew Freeman, MD, associate professor of medicine at the University of Colorado, Denver, and cochair of the American College of Cardiology’s nutrition and lifestyle work group, said the findings dovetail with his experience.
“I’m a huge believer that when people need to make lifestyle changes, having someone hold their hand and guide them through the effort is incredibly rewarding and incredibly powerful,” said Dr. Freeman, who also oversees the intensive cardiac rehab program at National Jewish Health in Denver.
A program like this needs proper funding in order to work, Dr, Freeman noted. He added that, even with coaches being paid well, “if you are able to prevent just one readmission for, say, heart failure a month . . . you could be saving millions of dollars over just a couple of years.”
Dr. Katzmarzyk, Dr. Flack, and Dr. Freeman reported no relevant disclosures. Louisiana State University, Pennington Biomedical Research Center, and Montclair State University have interest in the intellectual property surrounding a weight graph used in the study. The other researchers reported grants and/or fees from Bayer, Boehringer Ingelheim, Gilead, Takeda, Novo Nordisk, and other companies.
Patients who received intensive lifestyle training by coaches in the primary care setting experienced improvement in several indicators of cardiometabolic health in a 2-year trial.
The 803 trial participants comprised a racially diverse, low-income population with obesity. In this study, primary care clinics were randomly assigned to provide weight-loss coaching or usual care. Patients at the intensive training clinics lost significantly more weight than the other patients, as reported in a paper published in September in the New England Journal of Medicine on the PROmoting Successful Weight Loss in Primary CarE in Louisiana (PROPEL) trial. The patients who received weight loss coaching also had significantly more improvement in HDL cholesterol levels, total to HDL cholesterol ratios, and metabolic syndrome severity score, said researchers in the new paper on the PROPEL trial, which was published in Circulation on February 8 .
“We believe that one reason for success of the program was the use of a health coach [who] was embedded in the primary care office,” said lead author Peter Katzmarzyk, PhD, associate executive director for population and public health sciences at the Pennington Biomedical Research Center, Baton Rouge, La. “This way, the patients could get their counseling in a familiar environment and did not have to go to a different setting. The coaches developed close relationships with the patients over the 2 years, and this helped develop a sense of responsibility in the patients as the coaches were helping the patients to set goals and kept them accountable.”
In the PROPEL study, 67% of patients were Black and had low health literacy scores that corresponded with less than a ninth-grade education level. The intensive lifestyle intervention program included weekly sessions with the trained health coaches over the first 6 months — 16 face-to-face and 6 over the phone — and then at least monthly for the last 18 months. The coaches had higher education degrees in nutrition, physical activity, or behavioral medicine. Before the program started, the coaches also received training in the management of obesity and related health issues, health literacy, and patient communication and education. The goal of the program was 10% weight loss, using personalized action plans on eating, dieting, and physical activity.
Those in the usual-care clinics continued receiving normal care and received newsletters on health topics, such as the importance of sleep and tips for limiting time spent sitting. The primary care physicians at those clinics also were given a presentation with Centers for Medicare & Medicaid Services (CMS) information on intensive lifestyle interventions for obesity.
Cholesterol changes in intervention vs. control group
HDL cholesterol improved significantly among the coached patients, compared with the other patients, with a mean difference of 4.1 mg/dL at 1 year and 4.6 mg/dL at 2 years (P less than .01 for both). The total cholesterol to HDL cholesterol ratio showed a similarly significant difference in decline, with a between-group difference of –0.29 at 1 year and –0.31 at 2 years (P less than .01 for both). Also, the difference in the change in metabolic severity scores were –0.40 at 1 year and –0.21 at 2 years (P less than .01 for both).
Fasting blood glucose had declined after the 1st year by a significantly greater degree in the clinics with coaching, compared with the others, but not after the second year, researchers found.
There were no significant differences seen in total cholesterol, LDL cholesterol, non-HDL cholesterol, or blood pressure. Dr. Katzmarzyk said the likely reason for no change in blood pressure was that it was already relatively well-controlled at baseline for all the patients.
Funding barriers to obesity treatment
The CMS currently cover intensive training for obesity if delivered directly by a primary care physician, according to the authors of the new paper. Dr. Katzmarzyk said he hopes that will change.
“We are hoping that the evidence provided in this study may change the way that CMS funds obesity treatment in the future by allowing an expansion of the care team,” he said.
John Flack, MD, chair of internal medicine at Southern Illinois University, Springfield, said that the main achievement of the study was that it showed that intensive weight-loss training in the primary-care setting could be accomplished in a racially diverse population with low health literacy.
“You can’t just automatically assume just because you’ve seen it in some other populations that you can replicate this in every population, so they’ve done a really good job,” he said.
That programs are eligible for reimbursement only if they’re run by primary-care physicians is an ongoing problem, he said.
“You don’t necessarily need to be a physician to do this,” Dr. Flack said.
For best results, payment for coaching should not be tied to office visits, Dr. Flack noted.
“If they’re de-tethered from the office visits and you’re paid for quality ... you’re going to build out your infrastructure differently to care for people,” he said.
Andrew Freeman, MD, associate professor of medicine at the University of Colorado, Denver, and cochair of the American College of Cardiology’s nutrition and lifestyle work group, said the findings dovetail with his experience.
“I’m a huge believer that when people need to make lifestyle changes, having someone hold their hand and guide them through the effort is incredibly rewarding and incredibly powerful,” said Dr. Freeman, who also oversees the intensive cardiac rehab program at National Jewish Health in Denver.
A program like this needs proper funding in order to work, Dr, Freeman noted. He added that, even with coaches being paid well, “if you are able to prevent just one readmission for, say, heart failure a month . . . you could be saving millions of dollars over just a couple of years.”
Dr. Katzmarzyk, Dr. Flack, and Dr. Freeman reported no relevant disclosures. Louisiana State University, Pennington Biomedical Research Center, and Montclair State University have interest in the intellectual property surrounding a weight graph used in the study. The other researchers reported grants and/or fees from Bayer, Boehringer Ingelheim, Gilead, Takeda, Novo Nordisk, and other companies.
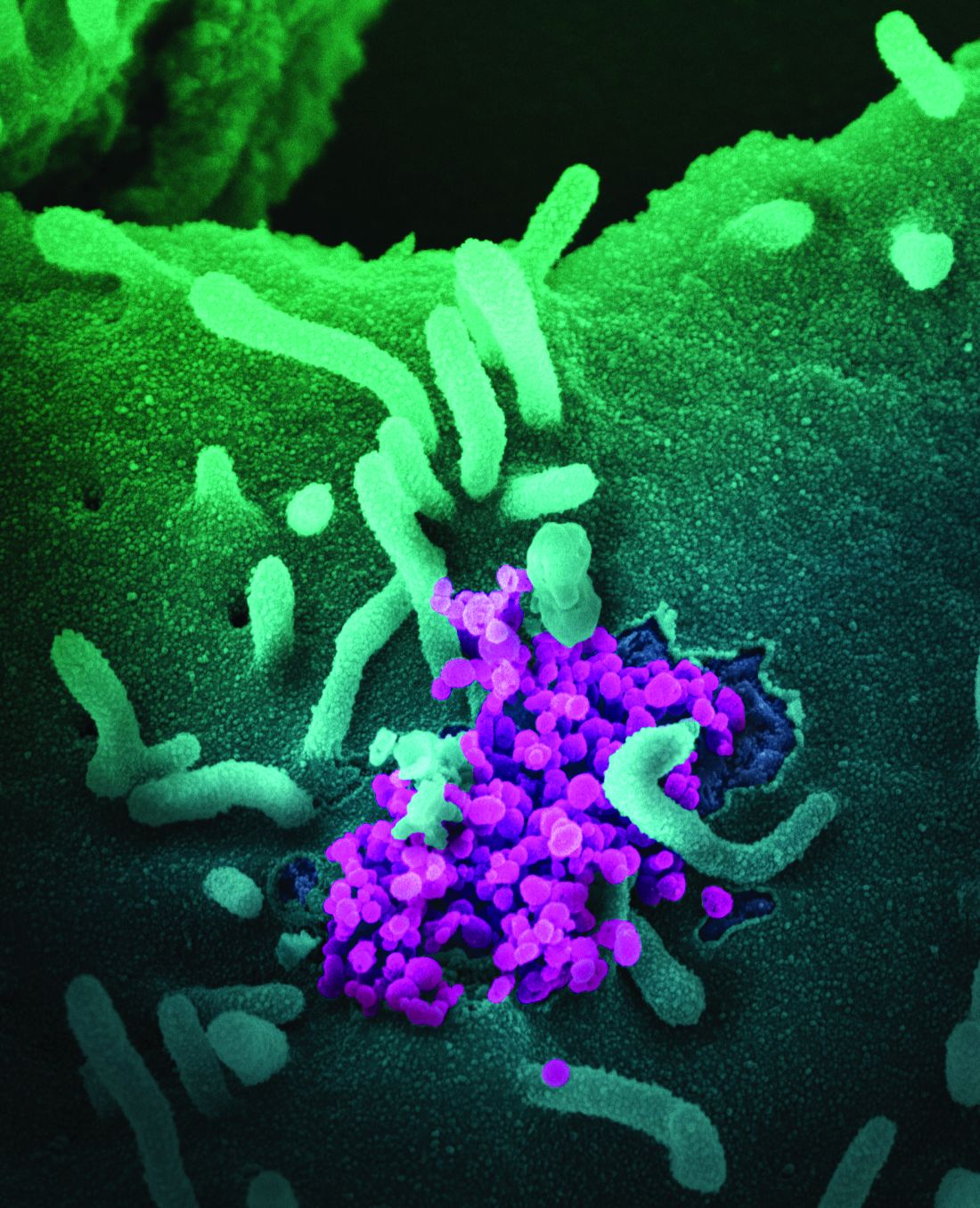
COVID-19 studies funded by rheumatology foundation
Five lines of research related to COVID-19 and people with rheumatic diseases will be explored with $1.65 million awarded recently by the Rheumatology Research Foundation.
Investigators will explore topics ranging from respiratory health to telemedicine with the awards, given by the foundation that is the largest private funding source for rheumatology research and training in the United States. The projects are an attempt to deepen the understanding about how people with rheumatic illnesses are affected by COVID-19.
“Our current understanding of why there are differences in severity of COVID-19 illness among rheumatology patients is limited,” Foundation President S. Louis Bridges, MD, PhD, said. “Additionally, there are many other gaps in our knowledge of the clinical aspects of SARS-CoV-2 infection in patients with rheumatic diseases, and how the pandemic has changed health care delivery. There is an urgent need to acquire new knowledge on COVID-19 in patients with [rheumatic and musculoskeletal diseases].”
These are the research projects funded:
- Scientist Development Award: Respiratory complications of coronavirus disease (COVID-19) in rheumatic diseases, led by Kristin D’Silva, MD, of Massachusetts General Hospital in Boston (3-year, $225,000 grant)
- Scientist Development Award: COVID-19 in patients with inflammatory arthritis: A prospective study on the effects of immunomodulatory therapy on susceptibility and clinical outcomes, by Rebecca Haberman, MD, of New York University (3-year, $225,000 grant)
- Innovative Research Award: Antiphospholipid antibodies in COVID-19, led by Jason Knight, MD, PhD, of the University of Michigan, Ann Arbor (2-year, $400,000 grant);
- Innovative Research Award: Effectiveness of telerheumatology for delivering high-quality rheumatology care during the COVID-19 crisis, led by Maria Danila, MD, MSc, MSPH, of University of Alabama at Birmingham (2-year, $400,000 grant)
- Norman B. Gaylis, MD, Clinical Research Award: Telehealth-delivered health care to improve care (THRIVE) in community-practice rheumatology, led by Swamy Venuturupalli, MD, of Beverly Hills, Calif.–based Attune Health (2-year, $400,000 grant)
Dr. Bridges said the foundation accepted submissions in basic science, translational science, clinical science, health services research, and patient- and practice-centered research.
“What differentiates these studies from our existing awards portfolio is they all explore the relationships between rheumatic and musculoskeletal diseases and SARS-CoV-2,” he said. “Ultimately, the outcomes of these projects will contribute to a more comprehensive knowledge base and advance avenues of patient care in the COVID-19 pandemic.”
Dr. Gaylis, a rheumatologist in private practice in Aventura, Fla., said he was pleased that a telehealth project was chosen as the award given in his name.
“From a COVID point of view, this has been extremely valuable in allowing us to continue to help out patients, connect with our patients, provide them treatment, even if it’s not hands on, at least guide them in how to deal with their chronic rheumatic illnesses,” he said.
This line of research can also help explore the feasibility of telemedicine in helping meet the needs of rural communities facing shortages of rheumatologists.
“Can telemedicine provide a source of rheumatologic access for people who really don’t have a live provider in close proximity?” he said. “I think that’s really why this particular award is very, very timely.”
“It’s so difficult for clinicians to get funding for their research, for their ideas and for the discoveries they were making on a day-to-day basis while they were practicing in a clinical community environment,” he said. “So for me it was really something that inspired me to really create this award.”
Five lines of research related to COVID-19 and people with rheumatic diseases will be explored with $1.65 million awarded recently by the Rheumatology Research Foundation.
Investigators will explore topics ranging from respiratory health to telemedicine with the awards, given by the foundation that is the largest private funding source for rheumatology research and training in the United States. The projects are an attempt to deepen the understanding about how people with rheumatic illnesses are affected by COVID-19.
“Our current understanding of why there are differences in severity of COVID-19 illness among rheumatology patients is limited,” Foundation President S. Louis Bridges, MD, PhD, said. “Additionally, there are many other gaps in our knowledge of the clinical aspects of SARS-CoV-2 infection in patients with rheumatic diseases, and how the pandemic has changed health care delivery. There is an urgent need to acquire new knowledge on COVID-19 in patients with [rheumatic and musculoskeletal diseases].”
These are the research projects funded:
- Scientist Development Award: Respiratory complications of coronavirus disease (COVID-19) in rheumatic diseases, led by Kristin D’Silva, MD, of Massachusetts General Hospital in Boston (3-year, $225,000 grant)
- Scientist Development Award: COVID-19 in patients with inflammatory arthritis: A prospective study on the effects of immunomodulatory therapy on susceptibility and clinical outcomes, by Rebecca Haberman, MD, of New York University (3-year, $225,000 grant)
- Innovative Research Award: Antiphospholipid antibodies in COVID-19, led by Jason Knight, MD, PhD, of the University of Michigan, Ann Arbor (2-year, $400,000 grant);
- Innovative Research Award: Effectiveness of telerheumatology for delivering high-quality rheumatology care during the COVID-19 crisis, led by Maria Danila, MD, MSc, MSPH, of University of Alabama at Birmingham (2-year, $400,000 grant)
- Norman B. Gaylis, MD, Clinical Research Award: Telehealth-delivered health care to improve care (THRIVE) in community-practice rheumatology, led by Swamy Venuturupalli, MD, of Beverly Hills, Calif.–based Attune Health (2-year, $400,000 grant)
Dr. Bridges said the foundation accepted submissions in basic science, translational science, clinical science, health services research, and patient- and practice-centered research.
“What differentiates these studies from our existing awards portfolio is they all explore the relationships between rheumatic and musculoskeletal diseases and SARS-CoV-2,” he said. “Ultimately, the outcomes of these projects will contribute to a more comprehensive knowledge base and advance avenues of patient care in the COVID-19 pandemic.”
Dr. Gaylis, a rheumatologist in private practice in Aventura, Fla., said he was pleased that a telehealth project was chosen as the award given in his name.
“From a COVID point of view, this has been extremely valuable in allowing us to continue to help out patients, connect with our patients, provide them treatment, even if it’s not hands on, at least guide them in how to deal with their chronic rheumatic illnesses,” he said.
This line of research can also help explore the feasibility of telemedicine in helping meet the needs of rural communities facing shortages of rheumatologists.
“Can telemedicine provide a source of rheumatologic access for people who really don’t have a live provider in close proximity?” he said. “I think that’s really why this particular award is very, very timely.”
“It’s so difficult for clinicians to get funding for their research, for their ideas and for the discoveries they were making on a day-to-day basis while they were practicing in a clinical community environment,” he said. “So for me it was really something that inspired me to really create this award.”
Five lines of research related to COVID-19 and people with rheumatic diseases will be explored with $1.65 million awarded recently by the Rheumatology Research Foundation.
Investigators will explore topics ranging from respiratory health to telemedicine with the awards, given by the foundation that is the largest private funding source for rheumatology research and training in the United States. The projects are an attempt to deepen the understanding about how people with rheumatic illnesses are affected by COVID-19.
“Our current understanding of why there are differences in severity of COVID-19 illness among rheumatology patients is limited,” Foundation President S. Louis Bridges, MD, PhD, said. “Additionally, there are many other gaps in our knowledge of the clinical aspects of SARS-CoV-2 infection in patients with rheumatic diseases, and how the pandemic has changed health care delivery. There is an urgent need to acquire new knowledge on COVID-19 in patients with [rheumatic and musculoskeletal diseases].”
These are the research projects funded:
- Scientist Development Award: Respiratory complications of coronavirus disease (COVID-19) in rheumatic diseases, led by Kristin D’Silva, MD, of Massachusetts General Hospital in Boston (3-year, $225,000 grant)
- Scientist Development Award: COVID-19 in patients with inflammatory arthritis: A prospective study on the effects of immunomodulatory therapy on susceptibility and clinical outcomes, by Rebecca Haberman, MD, of New York University (3-year, $225,000 grant)
- Innovative Research Award: Antiphospholipid antibodies in COVID-19, led by Jason Knight, MD, PhD, of the University of Michigan, Ann Arbor (2-year, $400,000 grant);
- Innovative Research Award: Effectiveness of telerheumatology for delivering high-quality rheumatology care during the COVID-19 crisis, led by Maria Danila, MD, MSc, MSPH, of University of Alabama at Birmingham (2-year, $400,000 grant)
- Norman B. Gaylis, MD, Clinical Research Award: Telehealth-delivered health care to improve care (THRIVE) in community-practice rheumatology, led by Swamy Venuturupalli, MD, of Beverly Hills, Calif.–based Attune Health (2-year, $400,000 grant)
Dr. Bridges said the foundation accepted submissions in basic science, translational science, clinical science, health services research, and patient- and practice-centered research.
“What differentiates these studies from our existing awards portfolio is they all explore the relationships between rheumatic and musculoskeletal diseases and SARS-CoV-2,” he said. “Ultimately, the outcomes of these projects will contribute to a more comprehensive knowledge base and advance avenues of patient care in the COVID-19 pandemic.”
Dr. Gaylis, a rheumatologist in private practice in Aventura, Fla., said he was pleased that a telehealth project was chosen as the award given in his name.
“From a COVID point of view, this has been extremely valuable in allowing us to continue to help out patients, connect with our patients, provide them treatment, even if it’s not hands on, at least guide them in how to deal with their chronic rheumatic illnesses,” he said.
This line of research can also help explore the feasibility of telemedicine in helping meet the needs of rural communities facing shortages of rheumatologists.
“Can telemedicine provide a source of rheumatologic access for people who really don’t have a live provider in close proximity?” he said. “I think that’s really why this particular award is very, very timely.”
“It’s so difficult for clinicians to get funding for their research, for their ideas and for the discoveries they were making on a day-to-day basis while they were practicing in a clinical community environment,” he said. “So for me it was really something that inspired me to really create this award.”
Afternoon napping associated with better cognition in elderly, study shows
according to a new study in General Psychiatry.
The findings add to those seen in other observational studies showing afternoon napping promotes cognitive function, said the authors of the paper, published in General Psychiatry.
“The prevalence of afternoon napping has been increasing in older adults much more than in younger individuals,” wrote Han Cai, MS, of the department of geriatrics at The Fourth People’s Hospital of Wuhu, Anhui, China, and coauthors. “The elderly individuals who took afternoon naps showed significantly higher cognitive performance compared with those who did not nap.”
The researchers enrolled 2,214 people in the study – all Han Chinese and aged 60 or older. Afternoon napping was considered any period of inactivity of at least 5 minutes but less than 2 hours after lunch and outside of the person’s main sleep schedule. Those who reported ever napping – 1,534 subjects – were included in the napping group, and the others – 680 – in the nonnapping group. Patients with major physical conditions were excluded.
The Montreal Cognitive Assessment (MoCA), the Mini-Mental State Examination (MMSE), and the Neuropsychological Test Battery (NTB) were used to measure cognitive function, and 739 patients agreed to blood tests for lipid values.
The average total MMSE score was higher for the napping group at 25.3 points out of 30, than for the nonnapping group, at 24.56 (P = .003). Those in the napping group also had significantly higher scores in the orientation portion of the MoCA test, at 5.55 out of 6 points, compared with 5.41 for the nonnapping group (P = .006).
Those in the napping group scored significantly higher on the digit span and language fluency parts of the Neuropsychological Test Battery (P = .009 and .020, respectively).
Dementia was assessed with face-to-face visits with clinicians, but diagnoses of dementia were not different between the groups.
Triglycerides were found to be higher – though still in the normal range – in the napping group compared with the nonnapping group, 1.80 mmol/L to 1.75 mmol/L, the researchers found (P = .001). No differences were seen for HDL or LDL cholesterol levels, or in hypertension or diabetes, the researchers reported.
The authors noted that inflammation is likely an important feature in the relationship between napping and cognitive function. Inflammatory cytokines have been found to play a role in sleep disorders, and strong inflammatory responses can lead to adverse events, including cognitive impairment.
“Sleep is known to be a regulator of the immune response that counters these inflammatory mediators, whereas napping, in particular, is thought to be an evolved response to inflammation,” they said.
The average age of patients in the napping group was 72.8 years, slightly older than those in the nonnapping group at 71.3 years, and this was a significant difference (P = .016).
The researchers acknowledged that the study “could not show direct causality of napping, whether beneficial or harmful,” and that “a lack of detailed information regarding napping duration ... also limited the description of napping status.”
Junxin Li, PhD, RN, assistant professor at Johns Hopkins School of Nursing, Baltimore, who has studied napping and cognition, said that previous research generally supports a U-shaped relationship between napping and mental acuity, with shorter or medium-length naps benefiting cognition and no naps or naps that are too long being detrimental.
“This study looked at no nap versus naps of less than 2 hours and may not be able to capture this potential U-shaped association,” she said.
For clinicians, the duration, timing, frequency, and purpose of naps are important factors in making recommendations to patients, she said.
“For example, timing – napping in the early evening close to older adult’s bedtime may delay their bedtime and interfere with their nighttime sleep quality. Taking naps after lunchtime is hypothesized to provide the most therapeutic values to the health and usually recommended,” she said. Regular napping is better than “randomly dozing off,” Dr. Li added.
There are also cultural considerations – in east Asia, napping tends to be considered part of a healthy lifestyle, while in western countries it is not – and this could impact napping behaviors and how these behaviors affect cognition, she said.
Phyllis C. Zee, MD, PhD, director of the Center for Circadian and Sleep Medicine at the Northwestern University, Chicago, said the results are consistent with early cross-sectional studies that showed that regular, scheduled naps in the afternoon were associated with positive cognitive performance and lower cardiometabolic disease risk.
Dr. Zee noted that it’s important to recognize that the positive data are associated with naps that are planned, while older adults napping because of excess sleepiness are at a higher risk for cognitive impairment and other health issues.
The study authors, Dr. Li, and Dr. Zee reported no relevant financial disclosures.
according to a new study in General Psychiatry.
The findings add to those seen in other observational studies showing afternoon napping promotes cognitive function, said the authors of the paper, published in General Psychiatry.
“The prevalence of afternoon napping has been increasing in older adults much more than in younger individuals,” wrote Han Cai, MS, of the department of geriatrics at The Fourth People’s Hospital of Wuhu, Anhui, China, and coauthors. “The elderly individuals who took afternoon naps showed significantly higher cognitive performance compared with those who did not nap.”
The researchers enrolled 2,214 people in the study – all Han Chinese and aged 60 or older. Afternoon napping was considered any period of inactivity of at least 5 minutes but less than 2 hours after lunch and outside of the person’s main sleep schedule. Those who reported ever napping – 1,534 subjects – were included in the napping group, and the others – 680 – in the nonnapping group. Patients with major physical conditions were excluded.
The Montreal Cognitive Assessment (MoCA), the Mini-Mental State Examination (MMSE), and the Neuropsychological Test Battery (NTB) were used to measure cognitive function, and 739 patients agreed to blood tests for lipid values.
The average total MMSE score was higher for the napping group at 25.3 points out of 30, than for the nonnapping group, at 24.56 (P = .003). Those in the napping group also had significantly higher scores in the orientation portion of the MoCA test, at 5.55 out of 6 points, compared with 5.41 for the nonnapping group (P = .006).
Those in the napping group scored significantly higher on the digit span and language fluency parts of the Neuropsychological Test Battery (P = .009 and .020, respectively).
Dementia was assessed with face-to-face visits with clinicians, but diagnoses of dementia were not different between the groups.
Triglycerides were found to be higher – though still in the normal range – in the napping group compared with the nonnapping group, 1.80 mmol/L to 1.75 mmol/L, the researchers found (P = .001). No differences were seen for HDL or LDL cholesterol levels, or in hypertension or diabetes, the researchers reported.
The authors noted that inflammation is likely an important feature in the relationship between napping and cognitive function. Inflammatory cytokines have been found to play a role in sleep disorders, and strong inflammatory responses can lead to adverse events, including cognitive impairment.
“Sleep is known to be a regulator of the immune response that counters these inflammatory mediators, whereas napping, in particular, is thought to be an evolved response to inflammation,” they said.
The average age of patients in the napping group was 72.8 years, slightly older than those in the nonnapping group at 71.3 years, and this was a significant difference (P = .016).
The researchers acknowledged that the study “could not show direct causality of napping, whether beneficial or harmful,” and that “a lack of detailed information regarding napping duration ... also limited the description of napping status.”
Junxin Li, PhD, RN, assistant professor at Johns Hopkins School of Nursing, Baltimore, who has studied napping and cognition, said that previous research generally supports a U-shaped relationship between napping and mental acuity, with shorter or medium-length naps benefiting cognition and no naps or naps that are too long being detrimental.
“This study looked at no nap versus naps of less than 2 hours and may not be able to capture this potential U-shaped association,” she said.
For clinicians, the duration, timing, frequency, and purpose of naps are important factors in making recommendations to patients, she said.
“For example, timing – napping in the early evening close to older adult’s bedtime may delay their bedtime and interfere with their nighttime sleep quality. Taking naps after lunchtime is hypothesized to provide the most therapeutic values to the health and usually recommended,” she said. Regular napping is better than “randomly dozing off,” Dr. Li added.
There are also cultural considerations – in east Asia, napping tends to be considered part of a healthy lifestyle, while in western countries it is not – and this could impact napping behaviors and how these behaviors affect cognition, she said.
Phyllis C. Zee, MD, PhD, director of the Center for Circadian and Sleep Medicine at the Northwestern University, Chicago, said the results are consistent with early cross-sectional studies that showed that regular, scheduled naps in the afternoon were associated with positive cognitive performance and lower cardiometabolic disease risk.
Dr. Zee noted that it’s important to recognize that the positive data are associated with naps that are planned, while older adults napping because of excess sleepiness are at a higher risk for cognitive impairment and other health issues.
The study authors, Dr. Li, and Dr. Zee reported no relevant financial disclosures.
according to a new study in General Psychiatry.
The findings add to those seen in other observational studies showing afternoon napping promotes cognitive function, said the authors of the paper, published in General Psychiatry.
“The prevalence of afternoon napping has been increasing in older adults much more than in younger individuals,” wrote Han Cai, MS, of the department of geriatrics at The Fourth People’s Hospital of Wuhu, Anhui, China, and coauthors. “The elderly individuals who took afternoon naps showed significantly higher cognitive performance compared with those who did not nap.”
The researchers enrolled 2,214 people in the study – all Han Chinese and aged 60 or older. Afternoon napping was considered any period of inactivity of at least 5 minutes but less than 2 hours after lunch and outside of the person’s main sleep schedule. Those who reported ever napping – 1,534 subjects – were included in the napping group, and the others – 680 – in the nonnapping group. Patients with major physical conditions were excluded.
The Montreal Cognitive Assessment (MoCA), the Mini-Mental State Examination (MMSE), and the Neuropsychological Test Battery (NTB) were used to measure cognitive function, and 739 patients agreed to blood tests for lipid values.
The average total MMSE score was higher for the napping group at 25.3 points out of 30, than for the nonnapping group, at 24.56 (P = .003). Those in the napping group also had significantly higher scores in the orientation portion of the MoCA test, at 5.55 out of 6 points, compared with 5.41 for the nonnapping group (P = .006).
Those in the napping group scored significantly higher on the digit span and language fluency parts of the Neuropsychological Test Battery (P = .009 and .020, respectively).
Dementia was assessed with face-to-face visits with clinicians, but diagnoses of dementia were not different between the groups.
Triglycerides were found to be higher – though still in the normal range – in the napping group compared with the nonnapping group, 1.80 mmol/L to 1.75 mmol/L, the researchers found (P = .001). No differences were seen for HDL or LDL cholesterol levels, or in hypertension or diabetes, the researchers reported.
The authors noted that inflammation is likely an important feature in the relationship between napping and cognitive function. Inflammatory cytokines have been found to play a role in sleep disorders, and strong inflammatory responses can lead to adverse events, including cognitive impairment.
“Sleep is known to be a regulator of the immune response that counters these inflammatory mediators, whereas napping, in particular, is thought to be an evolved response to inflammation,” they said.
The average age of patients in the napping group was 72.8 years, slightly older than those in the nonnapping group at 71.3 years, and this was a significant difference (P = .016).
The researchers acknowledged that the study “could not show direct causality of napping, whether beneficial or harmful,” and that “a lack of detailed information regarding napping duration ... also limited the description of napping status.”
Junxin Li, PhD, RN, assistant professor at Johns Hopkins School of Nursing, Baltimore, who has studied napping and cognition, said that previous research generally supports a U-shaped relationship between napping and mental acuity, with shorter or medium-length naps benefiting cognition and no naps or naps that are too long being detrimental.
“This study looked at no nap versus naps of less than 2 hours and may not be able to capture this potential U-shaped association,” she said.
For clinicians, the duration, timing, frequency, and purpose of naps are important factors in making recommendations to patients, she said.
“For example, timing – napping in the early evening close to older adult’s bedtime may delay their bedtime and interfere with their nighttime sleep quality. Taking naps after lunchtime is hypothesized to provide the most therapeutic values to the health and usually recommended,” she said. Regular napping is better than “randomly dozing off,” Dr. Li added.
There are also cultural considerations – in east Asia, napping tends to be considered part of a healthy lifestyle, while in western countries it is not – and this could impact napping behaviors and how these behaviors affect cognition, she said.
Phyllis C. Zee, MD, PhD, director of the Center for Circadian and Sleep Medicine at the Northwestern University, Chicago, said the results are consistent with early cross-sectional studies that showed that regular, scheduled naps in the afternoon were associated with positive cognitive performance and lower cardiometabolic disease risk.
Dr. Zee noted that it’s important to recognize that the positive data are associated with naps that are planned, while older adults napping because of excess sleepiness are at a higher risk for cognitive impairment and other health issues.
The study authors, Dr. Li, and Dr. Zee reported no relevant financial disclosures.
Income inequality plus race drive COVID incidence, death rates in U.S.
according to an analysis of U.S. county-level data.
The study, published in JAMA Network Open (2021 Jan 20. doi: 10.1001/jamanetworkopen.2020.34578), was led by Tim F. Liao, PhD, of the University of Illinois at Urbana-Champaign, and Fernando de Maio, of DePaul University, Chicago. They wrote: “This analysis confirms the association between racial/ethnic composition and COVID-19 incidence and mortality. A higher level of Black or Hispanic composition in a county is associated with a higher COVID-19 incidence and mortality; a higher level of economic inequality is also associated with a higher level of incidence and mortality.”
The analysis, which examined data from the first 200 days of the pandemic from January to August 2020, examined the joint associations between income inequality and racial and ethnic composition. Researchers mined data from the Centers for Disease Control and Prevention, the Census Bureau, the Kaiser Family Foundation, and other sources for 3,142 U.S. counties.
Income inequality was measured with the Gini index, on a 0-100 scale, with zero meaning perfect income equality (everyone has the same income) and 100 meaning perfect inequality (only one person or group has all of the income). The average Gini score across all the counties was 44.5, with a range of 25.6-66.5.
Researchers found that, for every 1.0% increase in a county’s Black population, there was a 1.9% increase in COVID-19 incidence (risk ratio, 1.019; 95% confidence interval, 1.016-1.022) and a 2.6% increase in COVID-19 mortality (RR, 1.026; 95% CI, 1.020-1.033). For every 1.0% increase in a county’s Hispanic population, there was a 2.4% increase in incidence (RR, 1.024; 95% CI, 1.012-1.025) and a 1.9% increase in mortality (RR, 1.019; 95% CI, 1.012-1.025).
Income inequality had an even greater effect on COVID-19 incidence and mortality. For each 1.0% rise in a county’s income inequality, there was a 2.0% rise in incidence (RR, 1.020; 95% CI, 1.012-1.027), and a 3.0% rise in mortality (RR, 1.030; 95% CI, 1.012-1.047).
In counties with lower percentages of Black and Hispanic population – up to about 50% for blacks and about 20%-30% for Hispanics – greater income inequality was correlated with higher COVID-19 incidence and mortality. But as the proportion of the Black and Hispanic population increased, race and ethnic population became the much more dominant predictive factor. In other words, the researchers said, income inequality seems to become less of a factor in COVID-related health as the minority population number grows in a given county.
“This finding implies that counties with relatively low proportions of Black or Hispanic residents may experience health effects of income inequality associated with the neomaterial pathway, which connects income inequality to population health through the breakdown of public infrastructure,” such as education, transportation and health care, the researchers said.
The study also examined the interaction between these factors and political attributes of a county, such as whether a governor faced a term limit, was Republican, or was male, and these were found to have no effect on COVID-19 incidence and mortality. Counties in states participating in Medicaid expansion under the Affordable Care Act had a 32% lower COVID-19 incidence rate, researchers found, but there was no correlation with mortality rates.
“This analysis found racial/ethnic composition, while important, does not reveal the full complexity of the story,” the researchers wrote. “Income inequality – a measure not typically included in public health county-level surveillance – also needs to be considered as a driver of the disproportionate burden borne by minoritized communities across the United States.”
The findings, they said, support using composite variables that “measure both income inequality and racial/ethnic composition simultaneously.”
The investigators had no disclosures.
according to an analysis of U.S. county-level data.
The study, published in JAMA Network Open (2021 Jan 20. doi: 10.1001/jamanetworkopen.2020.34578), was led by Tim F. Liao, PhD, of the University of Illinois at Urbana-Champaign, and Fernando de Maio, of DePaul University, Chicago. They wrote: “This analysis confirms the association between racial/ethnic composition and COVID-19 incidence and mortality. A higher level of Black or Hispanic composition in a county is associated with a higher COVID-19 incidence and mortality; a higher level of economic inequality is also associated with a higher level of incidence and mortality.”
The analysis, which examined data from the first 200 days of the pandemic from January to August 2020, examined the joint associations between income inequality and racial and ethnic composition. Researchers mined data from the Centers for Disease Control and Prevention, the Census Bureau, the Kaiser Family Foundation, and other sources for 3,142 U.S. counties.
Income inequality was measured with the Gini index, on a 0-100 scale, with zero meaning perfect income equality (everyone has the same income) and 100 meaning perfect inequality (only one person or group has all of the income). The average Gini score across all the counties was 44.5, with a range of 25.6-66.5.
Researchers found that, for every 1.0% increase in a county’s Black population, there was a 1.9% increase in COVID-19 incidence (risk ratio, 1.019; 95% confidence interval, 1.016-1.022) and a 2.6% increase in COVID-19 mortality (RR, 1.026; 95% CI, 1.020-1.033). For every 1.0% increase in a county’s Hispanic population, there was a 2.4% increase in incidence (RR, 1.024; 95% CI, 1.012-1.025) and a 1.9% increase in mortality (RR, 1.019; 95% CI, 1.012-1.025).
Income inequality had an even greater effect on COVID-19 incidence and mortality. For each 1.0% rise in a county’s income inequality, there was a 2.0% rise in incidence (RR, 1.020; 95% CI, 1.012-1.027), and a 3.0% rise in mortality (RR, 1.030; 95% CI, 1.012-1.047).
In counties with lower percentages of Black and Hispanic population – up to about 50% for blacks and about 20%-30% for Hispanics – greater income inequality was correlated with higher COVID-19 incidence and mortality. But as the proportion of the Black and Hispanic population increased, race and ethnic population became the much more dominant predictive factor. In other words, the researchers said, income inequality seems to become less of a factor in COVID-related health as the minority population number grows in a given county.
“This finding implies that counties with relatively low proportions of Black or Hispanic residents may experience health effects of income inequality associated with the neomaterial pathway, which connects income inequality to population health through the breakdown of public infrastructure,” such as education, transportation and health care, the researchers said.
The study also examined the interaction between these factors and political attributes of a county, such as whether a governor faced a term limit, was Republican, or was male, and these were found to have no effect on COVID-19 incidence and mortality. Counties in states participating in Medicaid expansion under the Affordable Care Act had a 32% lower COVID-19 incidence rate, researchers found, but there was no correlation with mortality rates.
“This analysis found racial/ethnic composition, while important, does not reveal the full complexity of the story,” the researchers wrote. “Income inequality – a measure not typically included in public health county-level surveillance – also needs to be considered as a driver of the disproportionate burden borne by minoritized communities across the United States.”
The findings, they said, support using composite variables that “measure both income inequality and racial/ethnic composition simultaneously.”
The investigators had no disclosures.
according to an analysis of U.S. county-level data.
The study, published in JAMA Network Open (2021 Jan 20. doi: 10.1001/jamanetworkopen.2020.34578), was led by Tim F. Liao, PhD, of the University of Illinois at Urbana-Champaign, and Fernando de Maio, of DePaul University, Chicago. They wrote: “This analysis confirms the association between racial/ethnic composition and COVID-19 incidence and mortality. A higher level of Black or Hispanic composition in a county is associated with a higher COVID-19 incidence and mortality; a higher level of economic inequality is also associated with a higher level of incidence and mortality.”
The analysis, which examined data from the first 200 days of the pandemic from January to August 2020, examined the joint associations between income inequality and racial and ethnic composition. Researchers mined data from the Centers for Disease Control and Prevention, the Census Bureau, the Kaiser Family Foundation, and other sources for 3,142 U.S. counties.
Income inequality was measured with the Gini index, on a 0-100 scale, with zero meaning perfect income equality (everyone has the same income) and 100 meaning perfect inequality (only one person or group has all of the income). The average Gini score across all the counties was 44.5, with a range of 25.6-66.5.
Researchers found that, for every 1.0% increase in a county’s Black population, there was a 1.9% increase in COVID-19 incidence (risk ratio, 1.019; 95% confidence interval, 1.016-1.022) and a 2.6% increase in COVID-19 mortality (RR, 1.026; 95% CI, 1.020-1.033). For every 1.0% increase in a county’s Hispanic population, there was a 2.4% increase in incidence (RR, 1.024; 95% CI, 1.012-1.025) and a 1.9% increase in mortality (RR, 1.019; 95% CI, 1.012-1.025).
Income inequality had an even greater effect on COVID-19 incidence and mortality. For each 1.0% rise in a county’s income inequality, there was a 2.0% rise in incidence (RR, 1.020; 95% CI, 1.012-1.027), and a 3.0% rise in mortality (RR, 1.030; 95% CI, 1.012-1.047).
In counties with lower percentages of Black and Hispanic population – up to about 50% for blacks and about 20%-30% for Hispanics – greater income inequality was correlated with higher COVID-19 incidence and mortality. But as the proportion of the Black and Hispanic population increased, race and ethnic population became the much more dominant predictive factor. In other words, the researchers said, income inequality seems to become less of a factor in COVID-related health as the minority population number grows in a given county.
“This finding implies that counties with relatively low proportions of Black or Hispanic residents may experience health effects of income inequality associated with the neomaterial pathway, which connects income inequality to population health through the breakdown of public infrastructure,” such as education, transportation and health care, the researchers said.
The study also examined the interaction between these factors and political attributes of a county, such as whether a governor faced a term limit, was Republican, or was male, and these were found to have no effect on COVID-19 incidence and mortality. Counties in states participating in Medicaid expansion under the Affordable Care Act had a 32% lower COVID-19 incidence rate, researchers found, but there was no correlation with mortality rates.
“This analysis found racial/ethnic composition, while important, does not reveal the full complexity of the story,” the researchers wrote. “Income inequality – a measure not typically included in public health county-level surveillance – also needs to be considered as a driver of the disproportionate burden borne by minoritized communities across the United States.”
The findings, they said, support using composite variables that “measure both income inequality and racial/ethnic composition simultaneously.”
The investigators had no disclosures.
FROM JAMA NETWORK OPEN
Hospitalists balance work, family as pandemic boosts stress
In a Q&A session at HM20 Virtual, hosted by the Society of Hospital Medicine, Heather Nye, MD, PhD, SFHM, professor of medicine at the University of California, San Francisco, and David J. Alfandre, MD, MPH, associate professor of medicine at New York University Langone, discussed strategies to help hospitalists tend to their personal wellness during the COVID-19 pandemic.
The speakers described the complicated logistics and emotional and psychological strain that has come from working during the pandemic, while balancing home responsibilities and parenting. The session was an opportunity to humanize hospitalists’ experience as they straddle work and family.
Dr. Nye said she was still “warming up to personal wellness” because there have been so many other demands over the past several months, but that taking the time to go for walks – to bring on a feeling of health even more than the physical benefits – has been helpful. Even before the pandemic, she said, she brought a guitar to the office to take a few minutes for a hobby for which she can’t seem to find uninterrupted time at home.
“Bringing a little bit of yourself into your work life goes a long way for a lot of people,” she said.
Child care and odd hours always have been a challenge for hospitalists, the presenters said, and for those in academia, any “wiggle room” in the schedule is often taken up by education, administration, and research projects.
Dr. Alfandre said etching out time for yourself must be “a priority, or it won’t happen.” Doing so, he said, “feels indulgent but it’s not. It’s central to being able to do the kind of work you do when you’re at the hospital, at the office, and when you’re back home again.”
Dr. Nye observed that, while working from home on nonclinical work, “recognizing how little I got done was a big surprise,” and she had to “grow comfortable with that” and learn to live with the uncertainty about when that was going to change.
Both physicians described the emotional toll of worrying about their children if they have to continue distance learning.
Dr. Alfandre said that a shared Google calendar for his wife and him – with appointments, work obligations, children’s doctor’s appointments, recitals – has been helpful, removing the strain of having to remind each other. He said that there are skills used at work that hospitalists can use at home – such as not getting upset with a child for crying about a spilled drink – in the same way that a physician wouldn’t get upset with a patient concerned about a test.
“We empathize with our patients, and we empathize with our kids and what their experience is,” he said. Similarly, seeing family members crowd around a smartphone video call to check in with a COVID-19 patient can be a helpful reminder to appreciate going home to family at the end of the day.
When her children get upset that she has to go in to work, Dr. Nye said, it has been helpful to explain that her many patients are suffering and scared and need her help.
“I feel like sharing that part of our job [with] our kids helps them understand that there are very, very big problems out there – that they don’t have to know too much about and be frightened about – but [that knowledge] just gives them a little perspective.”
Dr. Nye and Dr. Alfandre said they had no financial conflicts of interest.
In a Q&A session at HM20 Virtual, hosted by the Society of Hospital Medicine, Heather Nye, MD, PhD, SFHM, professor of medicine at the University of California, San Francisco, and David J. Alfandre, MD, MPH, associate professor of medicine at New York University Langone, discussed strategies to help hospitalists tend to their personal wellness during the COVID-19 pandemic.
The speakers described the complicated logistics and emotional and psychological strain that has come from working during the pandemic, while balancing home responsibilities and parenting. The session was an opportunity to humanize hospitalists’ experience as they straddle work and family.
Dr. Nye said she was still “warming up to personal wellness” because there have been so many other demands over the past several months, but that taking the time to go for walks – to bring on a feeling of health even more than the physical benefits – has been helpful. Even before the pandemic, she said, she brought a guitar to the office to take a few minutes for a hobby for which she can’t seem to find uninterrupted time at home.
“Bringing a little bit of yourself into your work life goes a long way for a lot of people,” she said.
Child care and odd hours always have been a challenge for hospitalists, the presenters said, and for those in academia, any “wiggle room” in the schedule is often taken up by education, administration, and research projects.
Dr. Alfandre said etching out time for yourself must be “a priority, or it won’t happen.” Doing so, he said, “feels indulgent but it’s not. It’s central to being able to do the kind of work you do when you’re at the hospital, at the office, and when you’re back home again.”
Dr. Nye observed that, while working from home on nonclinical work, “recognizing how little I got done was a big surprise,” and she had to “grow comfortable with that” and learn to live with the uncertainty about when that was going to change.
Both physicians described the emotional toll of worrying about their children if they have to continue distance learning.
Dr. Alfandre said that a shared Google calendar for his wife and him – with appointments, work obligations, children’s doctor’s appointments, recitals – has been helpful, removing the strain of having to remind each other. He said that there are skills used at work that hospitalists can use at home – such as not getting upset with a child for crying about a spilled drink – in the same way that a physician wouldn’t get upset with a patient concerned about a test.
“We empathize with our patients, and we empathize with our kids and what their experience is,” he said. Similarly, seeing family members crowd around a smartphone video call to check in with a COVID-19 patient can be a helpful reminder to appreciate going home to family at the end of the day.
When her children get upset that she has to go in to work, Dr. Nye said, it has been helpful to explain that her many patients are suffering and scared and need her help.
“I feel like sharing that part of our job [with] our kids helps them understand that there are very, very big problems out there – that they don’t have to know too much about and be frightened about – but [that knowledge] just gives them a little perspective.”
Dr. Nye and Dr. Alfandre said they had no financial conflicts of interest.
In a Q&A session at HM20 Virtual, hosted by the Society of Hospital Medicine, Heather Nye, MD, PhD, SFHM, professor of medicine at the University of California, San Francisco, and David J. Alfandre, MD, MPH, associate professor of medicine at New York University Langone, discussed strategies to help hospitalists tend to their personal wellness during the COVID-19 pandemic.
The speakers described the complicated logistics and emotional and psychological strain that has come from working during the pandemic, while balancing home responsibilities and parenting. The session was an opportunity to humanize hospitalists’ experience as they straddle work and family.
Dr. Nye said she was still “warming up to personal wellness” because there have been so many other demands over the past several months, but that taking the time to go for walks – to bring on a feeling of health even more than the physical benefits – has been helpful. Even before the pandemic, she said, she brought a guitar to the office to take a few minutes for a hobby for which she can’t seem to find uninterrupted time at home.
“Bringing a little bit of yourself into your work life goes a long way for a lot of people,” she said.
Child care and odd hours always have been a challenge for hospitalists, the presenters said, and for those in academia, any “wiggle room” in the schedule is often taken up by education, administration, and research projects.
Dr. Alfandre said etching out time for yourself must be “a priority, or it won’t happen.” Doing so, he said, “feels indulgent but it’s not. It’s central to being able to do the kind of work you do when you’re at the hospital, at the office, and when you’re back home again.”
Dr. Nye observed that, while working from home on nonclinical work, “recognizing how little I got done was a big surprise,” and she had to “grow comfortable with that” and learn to live with the uncertainty about when that was going to change.
Both physicians described the emotional toll of worrying about their children if they have to continue distance learning.
Dr. Alfandre said that a shared Google calendar for his wife and him – with appointments, work obligations, children’s doctor’s appointments, recitals – has been helpful, removing the strain of having to remind each other. He said that there are skills used at work that hospitalists can use at home – such as not getting upset with a child for crying about a spilled drink – in the same way that a physician wouldn’t get upset with a patient concerned about a test.
“We empathize with our patients, and we empathize with our kids and what their experience is,” he said. Similarly, seeing family members crowd around a smartphone video call to check in with a COVID-19 patient can be a helpful reminder to appreciate going home to family at the end of the day.
When her children get upset that she has to go in to work, Dr. Nye said, it has been helpful to explain that her many patients are suffering and scared and need her help.
“I feel like sharing that part of our job [with] our kids helps them understand that there are very, very big problems out there – that they don’t have to know too much about and be frightened about – but [that knowledge] just gives them a little perspective.”
Dr. Nye and Dr. Alfandre said they had no financial conflicts of interest.
FROM HM20 VIRTUAL
Drug allergy in the chart? Ask patients for specifics
Paige Wickner, MD, MPH, medical director for quality and safety at Brigham and Women’s Hospital and assistant professor at Harvard Medical School, both in Boston, described a scenario that might sound familiar to hospitalists.
A 72-year-old man is admitted to the hospital for a lung transplant, and has a listed allergy to “sulfa,” contained in antibiotics and other medications. His medical records say his reaction was “rash.”
What do you do?
The answer, Dr. Wickner said, speaking at HM20 Virtual, sponsored by the Society of Hospital Medicine, is to first ask more questions for clarification. How bad was the rash? Was it blistering? To what type of sulfa did the patient have a reaction?
These questions can help determine the next steps. For sulfa-based antibiotics, hospitalists can often desensitize patients with certain reaction characteristics using widely studied protocols to allow the patient to temporarily take a sulfa-containing medication.
The dominant message of Dr. Wickner’s talk on drug allergies was to get clear details on the allergic reaction –
“Please, for all of your patients, take an allergy history on every listed medication; often you will be able to remove or clarify the medical record and the changes can be life saving,” she said.
For instance, desensitization to sulfa for patients who’ve had a morbilliform rash without a fever can be done on an outpatient basis. But if the patient had hives, or became short of breath or anaphylactic, it needs to be done as an inpatient by an allergist, she said.
The question of drug allergies is substantial. About 35% of patients have at least one listed drug allergy, with penicillin, NSAIDs, and CT contrast agents topping the list, Dr. Wickner said. Although 10% of the general population and 15% of inpatients have a listed penicillin allergy, more than 90% of listed penicillin allergies turn out not to actually be allergic, in part because penicillin allergies are often diagnosed in childhood and are frequently outgrown over time. Having a listed allergy can impact treatment, Dr. Wickner said, with alternatives not always clear-cut.
She described one patient she saw who had 62 listed drug allergies, prompting her clinicians to wonder, “what can I safely give this patient?” Physicians, she said, subject to drug allergy “alert fatigue,” tend to override about 80% of allergy alerts, but this can sometimes have serious consequences.
“The best time to clarify is when a patient is healthy and well,” said Dr. Wickner, not when they are an inpatient and sick. It is much more difficult to test for an allergy, and to treat an allergic reaction, than when someone’s health is quickly declining.
She urged physicians to ask patients to be specific about the name of a drug they suspect they’re allergic to, about the indications, the symptoms, and the timing – an immediate reaction is much different than a symptom that showed up days later.
“Sometimes they’ll say they’re allergic to penicillin, but will tell you they’ve taken Augmentin or amoxicillin, so you can take that allergy off the list,” Dr. Wickner said.
At Brigham and Women’s Hospital and Massachusetts General Hospital, Boston, physicians have developed protocols for assessing and managing suspected allergies to penicillin, aspirin and NSAIDs, and trimethoprim/sulfamethoxazole – helpful tools, she said, because the nature and context of the reaction can matter a great deal in how to respond to the listed allergy.
If someone has a reaction, and you think it might be anaphylaxis, don’t spend time pondering it, Dr. Wickner said. “If that thought crosses your mind, treat it like anaphylaxis, then analyze after the fact.” Most patients with anaphylaxis have some cutaneous sign, even if it’s just flushing.
Dr. Wickner said that, if an allergist is available, take advantage of that. “If allergy is available in-house, utilize them. Often, skin testing and/or challenge can help patients receive first-line therapy.”
In a question-and-answer session after her presentation, Dr. Wickner said that hospitalists “have a huge role to play” in drug allergy delabeling.
“We would love to have a more standard practice of allergy reconciliation, just like we do with medication reconciliation,” she said. Asking questions to get more specifics is essential – and simply asking directly about each listed allergen is “step one, and you’ll really find it’s going to broaden the things that you can do for your patients.”
Asked about whether reactions listed as allergies are frequently just adverse effects, Dr. Wickner said that patients who say they are frequently nauseous – rather than breaking out into a rash, for example – might not be having a true allergic reaction. After careful consideration, they might be better managed with antinausea medication than avoidance of the drug.
Dr. Wickner reported no relevant financial disclosures.
Paige Wickner, MD, MPH, medical director for quality and safety at Brigham and Women’s Hospital and assistant professor at Harvard Medical School, both in Boston, described a scenario that might sound familiar to hospitalists.
A 72-year-old man is admitted to the hospital for a lung transplant, and has a listed allergy to “sulfa,” contained in antibiotics and other medications. His medical records say his reaction was “rash.”
What do you do?
The answer, Dr. Wickner said, speaking at HM20 Virtual, sponsored by the Society of Hospital Medicine, is to first ask more questions for clarification. How bad was the rash? Was it blistering? To what type of sulfa did the patient have a reaction?
These questions can help determine the next steps. For sulfa-based antibiotics, hospitalists can often desensitize patients with certain reaction characteristics using widely studied protocols to allow the patient to temporarily take a sulfa-containing medication.
The dominant message of Dr. Wickner’s talk on drug allergies was to get clear details on the allergic reaction –
“Please, for all of your patients, take an allergy history on every listed medication; often you will be able to remove or clarify the medical record and the changes can be life saving,” she said.
For instance, desensitization to sulfa for patients who’ve had a morbilliform rash without a fever can be done on an outpatient basis. But if the patient had hives, or became short of breath or anaphylactic, it needs to be done as an inpatient by an allergist, she said.
The question of drug allergies is substantial. About 35% of patients have at least one listed drug allergy, with penicillin, NSAIDs, and CT contrast agents topping the list, Dr. Wickner said. Although 10% of the general population and 15% of inpatients have a listed penicillin allergy, more than 90% of listed penicillin allergies turn out not to actually be allergic, in part because penicillin allergies are often diagnosed in childhood and are frequently outgrown over time. Having a listed allergy can impact treatment, Dr. Wickner said, with alternatives not always clear-cut.
She described one patient she saw who had 62 listed drug allergies, prompting her clinicians to wonder, “what can I safely give this patient?” Physicians, she said, subject to drug allergy “alert fatigue,” tend to override about 80% of allergy alerts, but this can sometimes have serious consequences.
“The best time to clarify is when a patient is healthy and well,” said Dr. Wickner, not when they are an inpatient and sick. It is much more difficult to test for an allergy, and to treat an allergic reaction, than when someone’s health is quickly declining.
She urged physicians to ask patients to be specific about the name of a drug they suspect they’re allergic to, about the indications, the symptoms, and the timing – an immediate reaction is much different than a symptom that showed up days later.
“Sometimes they’ll say they’re allergic to penicillin, but will tell you they’ve taken Augmentin or amoxicillin, so you can take that allergy off the list,” Dr. Wickner said.
At Brigham and Women’s Hospital and Massachusetts General Hospital, Boston, physicians have developed protocols for assessing and managing suspected allergies to penicillin, aspirin and NSAIDs, and trimethoprim/sulfamethoxazole – helpful tools, she said, because the nature and context of the reaction can matter a great deal in how to respond to the listed allergy.
If someone has a reaction, and you think it might be anaphylaxis, don’t spend time pondering it, Dr. Wickner said. “If that thought crosses your mind, treat it like anaphylaxis, then analyze after the fact.” Most patients with anaphylaxis have some cutaneous sign, even if it’s just flushing.
Dr. Wickner said that, if an allergist is available, take advantage of that. “If allergy is available in-house, utilize them. Often, skin testing and/or challenge can help patients receive first-line therapy.”
In a question-and-answer session after her presentation, Dr. Wickner said that hospitalists “have a huge role to play” in drug allergy delabeling.
“We would love to have a more standard practice of allergy reconciliation, just like we do with medication reconciliation,” she said. Asking questions to get more specifics is essential – and simply asking directly about each listed allergen is “step one, and you’ll really find it’s going to broaden the things that you can do for your patients.”
Asked about whether reactions listed as allergies are frequently just adverse effects, Dr. Wickner said that patients who say they are frequently nauseous – rather than breaking out into a rash, for example – might not be having a true allergic reaction. After careful consideration, they might be better managed with antinausea medication than avoidance of the drug.
Dr. Wickner reported no relevant financial disclosures.
Paige Wickner, MD, MPH, medical director for quality and safety at Brigham and Women’s Hospital and assistant professor at Harvard Medical School, both in Boston, described a scenario that might sound familiar to hospitalists.
A 72-year-old man is admitted to the hospital for a lung transplant, and has a listed allergy to “sulfa,” contained in antibiotics and other medications. His medical records say his reaction was “rash.”
What do you do?
The answer, Dr. Wickner said, speaking at HM20 Virtual, sponsored by the Society of Hospital Medicine, is to first ask more questions for clarification. How bad was the rash? Was it blistering? To what type of sulfa did the patient have a reaction?
These questions can help determine the next steps. For sulfa-based antibiotics, hospitalists can often desensitize patients with certain reaction characteristics using widely studied protocols to allow the patient to temporarily take a sulfa-containing medication.
The dominant message of Dr. Wickner’s talk on drug allergies was to get clear details on the allergic reaction –
“Please, for all of your patients, take an allergy history on every listed medication; often you will be able to remove or clarify the medical record and the changes can be life saving,” she said.
For instance, desensitization to sulfa for patients who’ve had a morbilliform rash without a fever can be done on an outpatient basis. But if the patient had hives, or became short of breath or anaphylactic, it needs to be done as an inpatient by an allergist, she said.
The question of drug allergies is substantial. About 35% of patients have at least one listed drug allergy, with penicillin, NSAIDs, and CT contrast agents topping the list, Dr. Wickner said. Although 10% of the general population and 15% of inpatients have a listed penicillin allergy, more than 90% of listed penicillin allergies turn out not to actually be allergic, in part because penicillin allergies are often diagnosed in childhood and are frequently outgrown over time. Having a listed allergy can impact treatment, Dr. Wickner said, with alternatives not always clear-cut.
She described one patient she saw who had 62 listed drug allergies, prompting her clinicians to wonder, “what can I safely give this patient?” Physicians, she said, subject to drug allergy “alert fatigue,” tend to override about 80% of allergy alerts, but this can sometimes have serious consequences.
“The best time to clarify is when a patient is healthy and well,” said Dr. Wickner, not when they are an inpatient and sick. It is much more difficult to test for an allergy, and to treat an allergic reaction, than when someone’s health is quickly declining.
She urged physicians to ask patients to be specific about the name of a drug they suspect they’re allergic to, about the indications, the symptoms, and the timing – an immediate reaction is much different than a symptom that showed up days later.
“Sometimes they’ll say they’re allergic to penicillin, but will tell you they’ve taken Augmentin or amoxicillin, so you can take that allergy off the list,” Dr. Wickner said.
At Brigham and Women’s Hospital and Massachusetts General Hospital, Boston, physicians have developed protocols for assessing and managing suspected allergies to penicillin, aspirin and NSAIDs, and trimethoprim/sulfamethoxazole – helpful tools, she said, because the nature and context of the reaction can matter a great deal in how to respond to the listed allergy.
If someone has a reaction, and you think it might be anaphylaxis, don’t spend time pondering it, Dr. Wickner said. “If that thought crosses your mind, treat it like anaphylaxis, then analyze after the fact.” Most patients with anaphylaxis have some cutaneous sign, even if it’s just flushing.
Dr. Wickner said that, if an allergist is available, take advantage of that. “If allergy is available in-house, utilize them. Often, skin testing and/or challenge can help patients receive first-line therapy.”
In a question-and-answer session after her presentation, Dr. Wickner said that hospitalists “have a huge role to play” in drug allergy delabeling.
“We would love to have a more standard practice of allergy reconciliation, just like we do with medication reconciliation,” she said. Asking questions to get more specifics is essential – and simply asking directly about each listed allergen is “step one, and you’ll really find it’s going to broaden the things that you can do for your patients.”
Asked about whether reactions listed as allergies are frequently just adverse effects, Dr. Wickner said that patients who say they are frequently nauseous – rather than breaking out into a rash, for example – might not be having a true allergic reaction. After careful consideration, they might be better managed with antinausea medication than avoidance of the drug.
Dr. Wickner reported no relevant financial disclosures.
FROM HM20 VIRTUAL
Population health can improve postdischarge care
With the United States spending the most per capita on health care among industrialized nations but having the worst aggregate health outcomes, there’s a stark need for improvement, according to an expert at HM20 Virtual, hosted by the Society of Hospital Medicine.
Broadening the focus beyond the four walls of the hospital can bring better results while also saving money, said Adam Myers, MD, chief of population health at Cleveland Clinic. Dr. Myers described the way his health system has begun to pay more careful attention to the needs of specific kinds of patients and tailoring posthospitalization care accordingly, with in-person and virtual home visits, and postdischarge clinics.
With an increasing attention to value, health care organizations have to change their structure or risk going the way of the Choluteca Bridge in Honduras, Dr. Myers said. The Choluteca Bridge was built to be hurricane proof, but was nonetheless rendered useless in 1998 after Hurricane Mitch shifted the very course of the river beneath it.
Similarly, the way health care is delivered often does not meet the needs of the population.
“Our national system has been focused almost entirely on inpatient care,” Dr. Myers said. “A lot of the transition in care is outside of facilities and outside the walls of our inpatient settings.”
Instead, he said a focus on population health – understanding and tending to the needs of people rather than just treating them when they show up at clinics – should involve more outpatient care that is less centralized, fees based on outcomes and patient experience rather than simply volume of services, team approaches rather than single-provider care, and a general attention to preserving health rather than treating sickness.
At Cleveland Clinic, care teams try to understand not just the care that is medically necessary, but what is wanted and justified, as well as how to deliver that care safely, reliably, and affordably with outcomes that patients and families desire.
The results are striking. After increasing the number of ambulatory patient “touches” for those with chronic disease, inpatient care – disliked by patients and costly to health centers – decreased. From the first quarter of 2018, outpatient visits increased 9%, while inpatient visits dropped 7.4%, Dr. Myers said.
“As we managed patients more effectively on an outpatient basis, their need for inpatient care diminished,” he said. “It works.”
Cleveland Clinic has also made changes designed to reduce costly readmissions, using virtual visits, house calls, time reserved for team meetings to identify patients with gaps in their care, and attention to nonmedical determinants of health, such as assessing fall risk at home and addressing lack of nutritious food options in a community.
The health system has seen a 28% reduction in the cost of care attributed to house calls, 12% cost reduction attributed to better care coordination, and a 49% decrease in hospital days for “superutilizers” of the ED, Dr. Myers said.
Postdischarge clinics – where patients can be seen for the first few visits after hospitalization – have also been valuable for many health systems, because they are closely in tune with what happened during the inpatient stay. These clinics are staffed by hospitalists, interns, residents, or ambulatory clinicians. Dr. Myers said hospitalists tend to have an improved perspective after working in a discharge clinic, with more concern about a patient’s needs once they leave the hospital bed.
“Those hospitalists that I know who have participated in programs like this start to act a bit more like primary care physicians,” he said.
In a Q&A session after Dr. Myers’ presentation, he discussed how hospitalists can affect the many layers of health care policy, factors that often overlap with population health.
He noted that medical care accounts for only about 20% of patient outcomes – the rest involve social and environmental factors.
“I don’t know about you , but I’m not satisfied only impacting 20% of health outcomes,” he said. First, physicians need to understand what is happening in their communities, and the health policies that are preventing improvement. Then, build partnerships to help fix these problems. He pointed to lead poisoning as an example.
“If you think about it, lead poisoning is a social housing problem that shows up as a health care issue. Unless we are getting out into the community and mitigating the root problem, we will have to treat it over and over again,” he said.
Dr. Myers reported no relevant financial disclosures.
With the United States spending the most per capita on health care among industrialized nations but having the worst aggregate health outcomes, there’s a stark need for improvement, according to an expert at HM20 Virtual, hosted by the Society of Hospital Medicine.
Broadening the focus beyond the four walls of the hospital can bring better results while also saving money, said Adam Myers, MD, chief of population health at Cleveland Clinic. Dr. Myers described the way his health system has begun to pay more careful attention to the needs of specific kinds of patients and tailoring posthospitalization care accordingly, with in-person and virtual home visits, and postdischarge clinics.
With an increasing attention to value, health care organizations have to change their structure or risk going the way of the Choluteca Bridge in Honduras, Dr. Myers said. The Choluteca Bridge was built to be hurricane proof, but was nonetheless rendered useless in 1998 after Hurricane Mitch shifted the very course of the river beneath it.
Similarly, the way health care is delivered often does not meet the needs of the population.
“Our national system has been focused almost entirely on inpatient care,” Dr. Myers said. “A lot of the transition in care is outside of facilities and outside the walls of our inpatient settings.”
Instead, he said a focus on population health – understanding and tending to the needs of people rather than just treating them when they show up at clinics – should involve more outpatient care that is less centralized, fees based on outcomes and patient experience rather than simply volume of services, team approaches rather than single-provider care, and a general attention to preserving health rather than treating sickness.
At Cleveland Clinic, care teams try to understand not just the care that is medically necessary, but what is wanted and justified, as well as how to deliver that care safely, reliably, and affordably with outcomes that patients and families desire.
The results are striking. After increasing the number of ambulatory patient “touches” for those with chronic disease, inpatient care – disliked by patients and costly to health centers – decreased. From the first quarter of 2018, outpatient visits increased 9%, while inpatient visits dropped 7.4%, Dr. Myers said.
“As we managed patients more effectively on an outpatient basis, their need for inpatient care diminished,” he said. “It works.”
Cleveland Clinic has also made changes designed to reduce costly readmissions, using virtual visits, house calls, time reserved for team meetings to identify patients with gaps in their care, and attention to nonmedical determinants of health, such as assessing fall risk at home and addressing lack of nutritious food options in a community.
The health system has seen a 28% reduction in the cost of care attributed to house calls, 12% cost reduction attributed to better care coordination, and a 49% decrease in hospital days for “superutilizers” of the ED, Dr. Myers said.
Postdischarge clinics – where patients can be seen for the first few visits after hospitalization – have also been valuable for many health systems, because they are closely in tune with what happened during the inpatient stay. These clinics are staffed by hospitalists, interns, residents, or ambulatory clinicians. Dr. Myers said hospitalists tend to have an improved perspective after working in a discharge clinic, with more concern about a patient’s needs once they leave the hospital bed.
“Those hospitalists that I know who have participated in programs like this start to act a bit more like primary care physicians,” he said.
In a Q&A session after Dr. Myers’ presentation, he discussed how hospitalists can affect the many layers of health care policy, factors that often overlap with population health.
He noted that medical care accounts for only about 20% of patient outcomes – the rest involve social and environmental factors.
“I don’t know about you , but I’m not satisfied only impacting 20% of health outcomes,” he said. First, physicians need to understand what is happening in their communities, and the health policies that are preventing improvement. Then, build partnerships to help fix these problems. He pointed to lead poisoning as an example.
“If you think about it, lead poisoning is a social housing problem that shows up as a health care issue. Unless we are getting out into the community and mitigating the root problem, we will have to treat it over and over again,” he said.
Dr. Myers reported no relevant financial disclosures.
With the United States spending the most per capita on health care among industrialized nations but having the worst aggregate health outcomes, there’s a stark need for improvement, according to an expert at HM20 Virtual, hosted by the Society of Hospital Medicine.
Broadening the focus beyond the four walls of the hospital can bring better results while also saving money, said Adam Myers, MD, chief of population health at Cleveland Clinic. Dr. Myers described the way his health system has begun to pay more careful attention to the needs of specific kinds of patients and tailoring posthospitalization care accordingly, with in-person and virtual home visits, and postdischarge clinics.
With an increasing attention to value, health care organizations have to change their structure or risk going the way of the Choluteca Bridge in Honduras, Dr. Myers said. The Choluteca Bridge was built to be hurricane proof, but was nonetheless rendered useless in 1998 after Hurricane Mitch shifted the very course of the river beneath it.
Similarly, the way health care is delivered often does not meet the needs of the population.
“Our national system has been focused almost entirely on inpatient care,” Dr. Myers said. “A lot of the transition in care is outside of facilities and outside the walls of our inpatient settings.”
Instead, he said a focus on population health – understanding and tending to the needs of people rather than just treating them when they show up at clinics – should involve more outpatient care that is less centralized, fees based on outcomes and patient experience rather than simply volume of services, team approaches rather than single-provider care, and a general attention to preserving health rather than treating sickness.
At Cleveland Clinic, care teams try to understand not just the care that is medically necessary, but what is wanted and justified, as well as how to deliver that care safely, reliably, and affordably with outcomes that patients and families desire.
The results are striking. After increasing the number of ambulatory patient “touches” for those with chronic disease, inpatient care – disliked by patients and costly to health centers – decreased. From the first quarter of 2018, outpatient visits increased 9%, while inpatient visits dropped 7.4%, Dr. Myers said.
“As we managed patients more effectively on an outpatient basis, their need for inpatient care diminished,” he said. “It works.”
Cleveland Clinic has also made changes designed to reduce costly readmissions, using virtual visits, house calls, time reserved for team meetings to identify patients with gaps in their care, and attention to nonmedical determinants of health, such as assessing fall risk at home and addressing lack of nutritious food options in a community.
The health system has seen a 28% reduction in the cost of care attributed to house calls, 12% cost reduction attributed to better care coordination, and a 49% decrease in hospital days for “superutilizers” of the ED, Dr. Myers said.
Postdischarge clinics – where patients can be seen for the first few visits after hospitalization – have also been valuable for many health systems, because they are closely in tune with what happened during the inpatient stay. These clinics are staffed by hospitalists, interns, residents, or ambulatory clinicians. Dr. Myers said hospitalists tend to have an improved perspective after working in a discharge clinic, with more concern about a patient’s needs once they leave the hospital bed.
“Those hospitalists that I know who have participated in programs like this start to act a bit more like primary care physicians,” he said.
In a Q&A session after Dr. Myers’ presentation, he discussed how hospitalists can affect the many layers of health care policy, factors that often overlap with population health.
He noted that medical care accounts for only about 20% of patient outcomes – the rest involve social and environmental factors.
“I don’t know about you , but I’m not satisfied only impacting 20% of health outcomes,” he said. First, physicians need to understand what is happening in their communities, and the health policies that are preventing improvement. Then, build partnerships to help fix these problems. He pointed to lead poisoning as an example.
“If you think about it, lead poisoning is a social housing problem that shows up as a health care issue. Unless we are getting out into the community and mitigating the root problem, we will have to treat it over and over again,” he said.
Dr. Myers reported no relevant financial disclosures.
Hospitalists share work-parent experience during pandemic
The week of March 13, Heather Nye, MD, PhD, SFHM, professor of medicine at the University of California, San Francisco, got word that schools were closing because of COVID-19.
“My first thought was, ‘You’re kidding, right?’ ” she said. That was the start of a series of reactions that included denial and bargaining and, finally, some semblance of acceptance.
In a session at HM20 Virtual, hosted by the Society of Hospital Medicine, she and David J. Alfandre, MD, MPH, associate professor of medicine at New York University Langone, described the complicated logistics and emotional and psychological strain that has come from working during a time of such great health care need while balancing home responsibilities and parenting.
At the time schools closed, Dr. Alfandre said, he was busy with clinical work while his wife’s work as an academic psychiatrist, including research activities, stopped for a time, allowing her to manage many of the family duties. Ever since her work picked back up, though, it’s been a juggling act.
“Our roles were dynamic and changing, sometimes week to week,” he said. “It was quite a shock to the system.”
Well before the pandemic struck, Dr. Nye and Dr. Alfandre had been scheduled to talk during the annual conference about work-parenting challenges. The pandemic has further underscored those challenges, they said. although they did make suggestions in that vein.
Child care and odd hours always have been a challenge for hospitalists, they said, and for those in academia, any “wiggle room” in the schedule is often taken up by education, administration, and research projects.
“And then, of course, there are those ever-important baseball games and ballet recitals and any number of school-related activities to help support your kids,” Dr. Nye said.
COVID-19 has brought a new degree of strain, she said. There is the concern that hospitalists’ very work brings a higher infection risk to their children. Extra work responsibilities have brought on guilt about perhaps not doing a well enough job helping their children with schoolwork “without having any definition of what ‘well enough’ actually looks like.” At the same time, she said, she’s felt “incredibly grateful to have a stable job.
“There is this spectrum of guilt and gratitude that is constant – it’s an undulating, never-stopping pendulum,” she said.
Dr. Alfandre noted that it was a “tremendously proud moment” to have people cheering for his colleagues and him at shift change in New York. Still, after several days off, he “felt guilty that I wasn’t in the hospital.”
Dr. Nye observed that, while working from home on nonclinical work, “recognizing how little I got done was a big surprise,” and she had to “grow comfortable with that” and learn to live with the uncertainty about when that was going to change.
Both physicians described the emotional toll of worrying about their children if they have to continue distance learning.
At work, her center seems to be in a constant state of instability – they’re either dealing with a surge or a reopening.
“It just goes on and on and on and on,” she said. “I find it overwhelming.”
Dr. Alfandre said that a shared Google calendar for his wife and him – with appointments, work obligations, children’s doctor’s appointments, recitals – has been helpful, removing the strain of having to remind each other.
“It’s really about cooperation with your partner,” he said. “I really think this is the most important aspect.”
He said that there are skills used at work that hospitalists can use at home – such as not getting upset with a child for crying about a spilled drink – in the same way that a physician wouldn’t get upset with a patient concerned about a test.
“We empathize with our patients, and we empathize with our kids and what their experience is,” he said. Similarly, seeing family members crowd around a smartphone video call to check in with a COVID-19 patient can be a helpful reminder to appreciate going home to family at the end of the day.
When her children get upset that she has to go in to work, Dr. Nye said, it has been helpful to explain that her many patients are suffering and scared and need her help.
“I feel like sharing that part of our job to our kids helps them understand that there are very, very big problems out there – that they don’t have to know too much about and be frightened about – but [that knowledge] just gives them a little perspective.”
Dr. Nye and Dr. Alfandre said they had no financial conflicts of interest.
The week of March 13, Heather Nye, MD, PhD, SFHM, professor of medicine at the University of California, San Francisco, got word that schools were closing because of COVID-19.
“My first thought was, ‘You’re kidding, right?’ ” she said. That was the start of a series of reactions that included denial and bargaining and, finally, some semblance of acceptance.
In a session at HM20 Virtual, hosted by the Society of Hospital Medicine, she and David J. Alfandre, MD, MPH, associate professor of medicine at New York University Langone, described the complicated logistics and emotional and psychological strain that has come from working during a time of such great health care need while balancing home responsibilities and parenting.
At the time schools closed, Dr. Alfandre said, he was busy with clinical work while his wife’s work as an academic psychiatrist, including research activities, stopped for a time, allowing her to manage many of the family duties. Ever since her work picked back up, though, it’s been a juggling act.
“Our roles were dynamic and changing, sometimes week to week,” he said. “It was quite a shock to the system.”
Well before the pandemic struck, Dr. Nye and Dr. Alfandre had been scheduled to talk during the annual conference about work-parenting challenges. The pandemic has further underscored those challenges, they said. although they did make suggestions in that vein.
Child care and odd hours always have been a challenge for hospitalists, they said, and for those in academia, any “wiggle room” in the schedule is often taken up by education, administration, and research projects.
“And then, of course, there are those ever-important baseball games and ballet recitals and any number of school-related activities to help support your kids,” Dr. Nye said.
COVID-19 has brought a new degree of strain, she said. There is the concern that hospitalists’ very work brings a higher infection risk to their children. Extra work responsibilities have brought on guilt about perhaps not doing a well enough job helping their children with schoolwork “without having any definition of what ‘well enough’ actually looks like.” At the same time, she said, she’s felt “incredibly grateful to have a stable job.
“There is this spectrum of guilt and gratitude that is constant – it’s an undulating, never-stopping pendulum,” she said.
Dr. Alfandre noted that it was a “tremendously proud moment” to have people cheering for his colleagues and him at shift change in New York. Still, after several days off, he “felt guilty that I wasn’t in the hospital.”
Dr. Nye observed that, while working from home on nonclinical work, “recognizing how little I got done was a big surprise,” and she had to “grow comfortable with that” and learn to live with the uncertainty about when that was going to change.
Both physicians described the emotional toll of worrying about their children if they have to continue distance learning.
At work, her center seems to be in a constant state of instability – they’re either dealing with a surge or a reopening.
“It just goes on and on and on and on,” she said. “I find it overwhelming.”
Dr. Alfandre said that a shared Google calendar for his wife and him – with appointments, work obligations, children’s doctor’s appointments, recitals – has been helpful, removing the strain of having to remind each other.
“It’s really about cooperation with your partner,” he said. “I really think this is the most important aspect.”
He said that there are skills used at work that hospitalists can use at home – such as not getting upset with a child for crying about a spilled drink – in the same way that a physician wouldn’t get upset with a patient concerned about a test.
“We empathize with our patients, and we empathize with our kids and what their experience is,” he said. Similarly, seeing family members crowd around a smartphone video call to check in with a COVID-19 patient can be a helpful reminder to appreciate going home to family at the end of the day.
When her children get upset that she has to go in to work, Dr. Nye said, it has been helpful to explain that her many patients are suffering and scared and need her help.
“I feel like sharing that part of our job to our kids helps them understand that there are very, very big problems out there – that they don’t have to know too much about and be frightened about – but [that knowledge] just gives them a little perspective.”
Dr. Nye and Dr. Alfandre said they had no financial conflicts of interest.
The week of March 13, Heather Nye, MD, PhD, SFHM, professor of medicine at the University of California, San Francisco, got word that schools were closing because of COVID-19.
“My first thought was, ‘You’re kidding, right?’ ” she said. That was the start of a series of reactions that included denial and bargaining and, finally, some semblance of acceptance.
In a session at HM20 Virtual, hosted by the Society of Hospital Medicine, she and David J. Alfandre, MD, MPH, associate professor of medicine at New York University Langone, described the complicated logistics and emotional and psychological strain that has come from working during a time of such great health care need while balancing home responsibilities and parenting.
At the time schools closed, Dr. Alfandre said, he was busy with clinical work while his wife’s work as an academic psychiatrist, including research activities, stopped for a time, allowing her to manage many of the family duties. Ever since her work picked back up, though, it’s been a juggling act.
“Our roles were dynamic and changing, sometimes week to week,” he said. “It was quite a shock to the system.”
Well before the pandemic struck, Dr. Nye and Dr. Alfandre had been scheduled to talk during the annual conference about work-parenting challenges. The pandemic has further underscored those challenges, they said. although they did make suggestions in that vein.
Child care and odd hours always have been a challenge for hospitalists, they said, and for those in academia, any “wiggle room” in the schedule is often taken up by education, administration, and research projects.
“And then, of course, there are those ever-important baseball games and ballet recitals and any number of school-related activities to help support your kids,” Dr. Nye said.
COVID-19 has brought a new degree of strain, she said. There is the concern that hospitalists’ very work brings a higher infection risk to their children. Extra work responsibilities have brought on guilt about perhaps not doing a well enough job helping their children with schoolwork “without having any definition of what ‘well enough’ actually looks like.” At the same time, she said, she’s felt “incredibly grateful to have a stable job.
“There is this spectrum of guilt and gratitude that is constant – it’s an undulating, never-stopping pendulum,” she said.
Dr. Alfandre noted that it was a “tremendously proud moment” to have people cheering for his colleagues and him at shift change in New York. Still, after several days off, he “felt guilty that I wasn’t in the hospital.”
Dr. Nye observed that, while working from home on nonclinical work, “recognizing how little I got done was a big surprise,” and she had to “grow comfortable with that” and learn to live with the uncertainty about when that was going to change.
Both physicians described the emotional toll of worrying about their children if they have to continue distance learning.
At work, her center seems to be in a constant state of instability – they’re either dealing with a surge or a reopening.
“It just goes on and on and on and on,” she said. “I find it overwhelming.”
Dr. Alfandre said that a shared Google calendar for his wife and him – with appointments, work obligations, children’s doctor’s appointments, recitals – has been helpful, removing the strain of having to remind each other.
“It’s really about cooperation with your partner,” he said. “I really think this is the most important aspect.”
He said that there are skills used at work that hospitalists can use at home – such as not getting upset with a child for crying about a spilled drink – in the same way that a physician wouldn’t get upset with a patient concerned about a test.
“We empathize with our patients, and we empathize with our kids and what their experience is,” he said. Similarly, seeing family members crowd around a smartphone video call to check in with a COVID-19 patient can be a helpful reminder to appreciate going home to family at the end of the day.
When her children get upset that she has to go in to work, Dr. Nye said, it has been helpful to explain that her many patients are suffering and scared and need her help.
“I feel like sharing that part of our job to our kids helps them understand that there are very, very big problems out there – that they don’t have to know too much about and be frightened about – but [that knowledge] just gives them a little perspective.”
Dr. Nye and Dr. Alfandre said they had no financial conflicts of interest.
FROM HM20 VIRTUAL
Cancer treatments bring concerns for hospitalists
Advances in cancer treatment have brought a range of potential issues hospitalists are likely to see in admitted patients – many of which can escalate quickly into life-threatening emergencies if they’re not handled properly, an oncologist said in a presentation at HM20 Virtual, hosted by the Society of Hospital Medicine.
Checkpoint inhibitors and CAR T-cell therapy – revolutions in fighting cancer but potential instigators of serious side effects because of the way they set the immune system in motion – can have consequences throughout the body, said Megan Kruse, MD, an oncologist at the Cleveland Clinic.
Checkpoint inhibitors, which cause the body to essentially take its foot off the break of the immune system, in particular have diverse effects, Dr. Kruse said.
“Suffice it to say that any odd symptom in any organ system in a patient on immunotherapy, or with a history of immunotherapy, can be cause for concern,” she said. Most common are skin, gut, endocrine, lung, and musculoskeletal involvement. Cardiovascular, hematologic, renal, neurologic, and ophthalmological effects are less common, but when they happen, they’re often dramatic and need urgent management.
With these medications –which include anti–programmed death-1 agents pembrolizumab and nivolumab and anti–PD-ligand 1 agents atezolizumab and avelumab, among others – rash is often seen first, followed by diarrhea and colitis. Hypophysitis, which requires intervention, and liver toxicity, which usually tapers off on its own, often occur about 6-8 weeks into treatment. There are no rigid rules for the arrival of these symptoms, however, Dr. Kruse said.
“We must have a high index of suspicion. ... They really can occur at any point after a patient has had even one dose of an immunologic agent,” she said.
In more serious cases, steroids are typically the go-to treatment, she added, because they will quickly tamp down the immune activation brought on by the medications.
“When these drugs first came out, we were all very concerned about adding steroids,” she said. “In follow-up studies, it actually looks like we don’t attenuate the anticancer response very much by instituting steroids when clinically appropriate. And so you all should feel very comfortable adding steroids while waiting to talk to oncology.”
In these cases, the steroid taper is done very slowly, over weeks or even months.
With CAR T-cell therapy – in which patients receive T cells to target liquid tumors – cytokine release syndrome (CRS) can occur, often within 14 days after treatment. Dr. Kruse cautioned that it can present with symptoms similar to tumor lysis syndrome or sepsis.
“Patients are at a high risk of bacterial infection, so antibiotics are advised,” she said.
In these cases, fever is often a harbinger, often arriving at least a day before the rest of the symptoms of CRS.
Early treatment with the interleukin-6 inhibitor tocilizumab is recommended for these patients, she said. This agent has been shown to have a 69% response rate in severe CRS and has no known effect on the efficacy of the CAR T-cell treatment.
Dr. Kruse also touched on several other conditions that can rise to the level of emergencies in cancer treatment:
- In cases of neutropenic fever, patients should be treated as soon as possible with antibiotics, and some solid-tumor patients at lower risk can be treated as outpatients, she said. Those with hematologic cancer, however, will need inpatient care.
- For tumor lysis syndrome with renal failure, fluids should be started quickly. Rasburicase, a recombinant urate oxidase enzyme, can be considered in some cases, but requires caution.
- In cases of spinal cord compression, a full spine MRI should be completed because about a third of patients have multilevel involvement. Steroids should be started as soon as possible.
In a question-and-answer session, much of the discussion focused on when outpatient care for neutropenic fever was possible. Dr. Kruse said those who need to be admitted for neutropenic fever treatment tend to be those with hematologic malignancies because their treatment is so myelosuppressive.
“Their window of complications is longer,” she said. Solid tumor patients, on the other hand, will usually improve “fairly rapidly” in about 3-4 days.
Many session viewers expressed surprise at the possibility of outpatient neutropenic fever treatment. Dr. Kruse said that the Cleveland Clinic’s incorporation of this approach has included the input of neutropenic fever risk index scoring into their electronic medical record and a good deal of in-service training.
Asked about appropriate swabbing of patients for COVID-19 before chemotherapy, Dr. Kruse said that her center screens only patients who need to be hospitalized for the treatment – those with a high incidence of prolonged neutropenia.
“For our typical outpatients who are receiving chemotherapy,” she said, “we are not swabbing them.” But they have intense fever screening and distance measures in place.
Dr. Kruse reported advisory board involvement for Novartis Oncology and consulting for Puma Biotechnology.
Advances in cancer treatment have brought a range of potential issues hospitalists are likely to see in admitted patients – many of which can escalate quickly into life-threatening emergencies if they’re not handled properly, an oncologist said in a presentation at HM20 Virtual, hosted by the Society of Hospital Medicine.
Checkpoint inhibitors and CAR T-cell therapy – revolutions in fighting cancer but potential instigators of serious side effects because of the way they set the immune system in motion – can have consequences throughout the body, said Megan Kruse, MD, an oncologist at the Cleveland Clinic.
Checkpoint inhibitors, which cause the body to essentially take its foot off the break of the immune system, in particular have diverse effects, Dr. Kruse said.
“Suffice it to say that any odd symptom in any organ system in a patient on immunotherapy, or with a history of immunotherapy, can be cause for concern,” she said. Most common are skin, gut, endocrine, lung, and musculoskeletal involvement. Cardiovascular, hematologic, renal, neurologic, and ophthalmological effects are less common, but when they happen, they’re often dramatic and need urgent management.
With these medications –which include anti–programmed death-1 agents pembrolizumab and nivolumab and anti–PD-ligand 1 agents atezolizumab and avelumab, among others – rash is often seen first, followed by diarrhea and colitis. Hypophysitis, which requires intervention, and liver toxicity, which usually tapers off on its own, often occur about 6-8 weeks into treatment. There are no rigid rules for the arrival of these symptoms, however, Dr. Kruse said.
“We must have a high index of suspicion. ... They really can occur at any point after a patient has had even one dose of an immunologic agent,” she said.
In more serious cases, steroids are typically the go-to treatment, she added, because they will quickly tamp down the immune activation brought on by the medications.
“When these drugs first came out, we were all very concerned about adding steroids,” she said. “In follow-up studies, it actually looks like we don’t attenuate the anticancer response very much by instituting steroids when clinically appropriate. And so you all should feel very comfortable adding steroids while waiting to talk to oncology.”
In these cases, the steroid taper is done very slowly, over weeks or even months.
With CAR T-cell therapy – in which patients receive T cells to target liquid tumors – cytokine release syndrome (CRS) can occur, often within 14 days after treatment. Dr. Kruse cautioned that it can present with symptoms similar to tumor lysis syndrome or sepsis.
“Patients are at a high risk of bacterial infection, so antibiotics are advised,” she said.
In these cases, fever is often a harbinger, often arriving at least a day before the rest of the symptoms of CRS.
Early treatment with the interleukin-6 inhibitor tocilizumab is recommended for these patients, she said. This agent has been shown to have a 69% response rate in severe CRS and has no known effect on the efficacy of the CAR T-cell treatment.
Dr. Kruse also touched on several other conditions that can rise to the level of emergencies in cancer treatment:
- In cases of neutropenic fever, patients should be treated as soon as possible with antibiotics, and some solid-tumor patients at lower risk can be treated as outpatients, she said. Those with hematologic cancer, however, will need inpatient care.
- For tumor lysis syndrome with renal failure, fluids should be started quickly. Rasburicase, a recombinant urate oxidase enzyme, can be considered in some cases, but requires caution.
- In cases of spinal cord compression, a full spine MRI should be completed because about a third of patients have multilevel involvement. Steroids should be started as soon as possible.
In a question-and-answer session, much of the discussion focused on when outpatient care for neutropenic fever was possible. Dr. Kruse said those who need to be admitted for neutropenic fever treatment tend to be those with hematologic malignancies because their treatment is so myelosuppressive.
“Their window of complications is longer,” she said. Solid tumor patients, on the other hand, will usually improve “fairly rapidly” in about 3-4 days.
Many session viewers expressed surprise at the possibility of outpatient neutropenic fever treatment. Dr. Kruse said that the Cleveland Clinic’s incorporation of this approach has included the input of neutropenic fever risk index scoring into their electronic medical record and a good deal of in-service training.
Asked about appropriate swabbing of patients for COVID-19 before chemotherapy, Dr. Kruse said that her center screens only patients who need to be hospitalized for the treatment – those with a high incidence of prolonged neutropenia.
“For our typical outpatients who are receiving chemotherapy,” she said, “we are not swabbing them.” But they have intense fever screening and distance measures in place.
Dr. Kruse reported advisory board involvement for Novartis Oncology and consulting for Puma Biotechnology.
Advances in cancer treatment have brought a range of potential issues hospitalists are likely to see in admitted patients – many of which can escalate quickly into life-threatening emergencies if they’re not handled properly, an oncologist said in a presentation at HM20 Virtual, hosted by the Society of Hospital Medicine.
Checkpoint inhibitors and CAR T-cell therapy – revolutions in fighting cancer but potential instigators of serious side effects because of the way they set the immune system in motion – can have consequences throughout the body, said Megan Kruse, MD, an oncologist at the Cleveland Clinic.
Checkpoint inhibitors, which cause the body to essentially take its foot off the break of the immune system, in particular have diverse effects, Dr. Kruse said.
“Suffice it to say that any odd symptom in any organ system in a patient on immunotherapy, or with a history of immunotherapy, can be cause for concern,” she said. Most common are skin, gut, endocrine, lung, and musculoskeletal involvement. Cardiovascular, hematologic, renal, neurologic, and ophthalmological effects are less common, but when they happen, they’re often dramatic and need urgent management.
With these medications –which include anti–programmed death-1 agents pembrolizumab and nivolumab and anti–PD-ligand 1 agents atezolizumab and avelumab, among others – rash is often seen first, followed by diarrhea and colitis. Hypophysitis, which requires intervention, and liver toxicity, which usually tapers off on its own, often occur about 6-8 weeks into treatment. There are no rigid rules for the arrival of these symptoms, however, Dr. Kruse said.
“We must have a high index of suspicion. ... They really can occur at any point after a patient has had even one dose of an immunologic agent,” she said.
In more serious cases, steroids are typically the go-to treatment, she added, because they will quickly tamp down the immune activation brought on by the medications.
“When these drugs first came out, we were all very concerned about adding steroids,” she said. “In follow-up studies, it actually looks like we don’t attenuate the anticancer response very much by instituting steroids when clinically appropriate. And so you all should feel very comfortable adding steroids while waiting to talk to oncology.”
In these cases, the steroid taper is done very slowly, over weeks or even months.
With CAR T-cell therapy – in which patients receive T cells to target liquid tumors – cytokine release syndrome (CRS) can occur, often within 14 days after treatment. Dr. Kruse cautioned that it can present with symptoms similar to tumor lysis syndrome or sepsis.
“Patients are at a high risk of bacterial infection, so antibiotics are advised,” she said.
In these cases, fever is often a harbinger, often arriving at least a day before the rest of the symptoms of CRS.
Early treatment with the interleukin-6 inhibitor tocilizumab is recommended for these patients, she said. This agent has been shown to have a 69% response rate in severe CRS and has no known effect on the efficacy of the CAR T-cell treatment.
Dr. Kruse also touched on several other conditions that can rise to the level of emergencies in cancer treatment:
- In cases of neutropenic fever, patients should be treated as soon as possible with antibiotics, and some solid-tumor patients at lower risk can be treated as outpatients, she said. Those with hematologic cancer, however, will need inpatient care.
- For tumor lysis syndrome with renal failure, fluids should be started quickly. Rasburicase, a recombinant urate oxidase enzyme, can be considered in some cases, but requires caution.
- In cases of spinal cord compression, a full spine MRI should be completed because about a third of patients have multilevel involvement. Steroids should be started as soon as possible.
In a question-and-answer session, much of the discussion focused on when outpatient care for neutropenic fever was possible. Dr. Kruse said those who need to be admitted for neutropenic fever treatment tend to be those with hematologic malignancies because their treatment is so myelosuppressive.
“Their window of complications is longer,” she said. Solid tumor patients, on the other hand, will usually improve “fairly rapidly” in about 3-4 days.
Many session viewers expressed surprise at the possibility of outpatient neutropenic fever treatment. Dr. Kruse said that the Cleveland Clinic’s incorporation of this approach has included the input of neutropenic fever risk index scoring into their electronic medical record and a good deal of in-service training.
Asked about appropriate swabbing of patients for COVID-19 before chemotherapy, Dr. Kruse said that her center screens only patients who need to be hospitalized for the treatment – those with a high incidence of prolonged neutropenia.
“For our typical outpatients who are receiving chemotherapy,” she said, “we are not swabbing them.” But they have intense fever screening and distance measures in place.
Dr. Kruse reported advisory board involvement for Novartis Oncology and consulting for Puma Biotechnology.
FROM HM20 VIRTUAL