User login
Still Burning
A celebratory mood pervaded the last week of service for my ward team at the end of the academic year. As the attending, it was just another day, but it was hard not to be caught up in the general feeling of a milestone flying past. Like most days in a hospital, this one passed in a rhythm of alternating mundanity and crisis. Late in the afternoon, one of the residents called me to a bedside for help. Imagining that my diagnostic skills were urgently required, I took the stairs. The problem, as it turned out, was not strictly medical.
I could hear the yelling before I cleared the locked entry doors to the ward. It doesn’t really matter what the yelling was about, just that there is often yelling and there is always very little I can do about the root cause of it. As I stepped into the middle of the conflagration, I remembered the story an intern told me about the night earlier in the month when it fell to her to wheel the same patient’s intoxicated parent down to the emergency department. After sleeping it off, the parent was diagnosed with an “allergic reaction” and given a prescription for diphenhydramine. We all knew the diagnosis was fantasy, and yet we all went along with it because there was simply no help available for the root cause of the problem. State social services was already involved, and we had a “safety” plan in place for discharge. As meager as that may have been, we had done the best we could to balance the risk with the available resources… or so we told ourselves.
As a nation, we have chosen not to provide much of a social safety net for our citizens who suffer from addiction and/or mental illness and, most importantly, for those who’ve just not had a leg up on the economic ladder. As a hospital-based clinician, I know that people in distress lose their cool and yell sometimes. Ironically, they may yell most loudly at people who sincerely want to help, simply because others do not engage them. Medical schools don’t teach us how to handle the yelling, though many would say it is part of the hidden curriculum. One thing that distinguishes many pediatricians like myself is a willingness to listen to the yelling, to engage with it, and to try to help. Not surprisingly, our reputation around the hospital is that we skew a bit naive.
It is worth asking, though: Are pediatricians naive? Sure, we make funny faces. We clown. We baby-talk. Those things are largely true, but there are other true things about pediatricians. Chief among them is the fact that we come to know some of the worst things there are to know about human beings. Everybody knows people can be awful, but we know exactly how awful they are to defenseless children in precise detail. For instance, I’ve seen a 4-year-old who was repeatedly starved as a regular punishment. She was so hungry she ate her hair, which turned out to be lucky for her because it caused an intestinal blockage that led to the discovery of the abuse. I gave her an apple one day and she immediately hid it under her shirt. Where you see a scab on a child’s inner arm, I see a cigarette burn. I’ve resuscitated a baby whose parents dipped his pacifier in heroin to stop his crying—the remarkable part of the story being that it was heroin cooked in the hospital bathroom. And then there are the things that I cannot even bring myself to write down.
Carrying this knowledge hollows out a gap between pediatricians and the rest of the world. The divergence between our expectations of how a society should treat its children and the reality of our daily experience grinds away any naivete. The gap becomes a canyon for some of us. We live with the sense that nobody would believe the things we’ve seen, so we rarely talk about them. Years ago, I was testifying in a (for me) routine child-abuse case where this fact hit home. It is common for juries to disbelieve that a caregiver could do the things we allege. I say allege, but if you work as a pediatrician long enough, the space between allegation and fact narrows. It is simply pattern recognition to you—abuse happens so consistently that we accept it as a diagnostic category. The case in question was a submersion burn, which is an almost unmistakable pattern. The other piece of the story is that it happens to toddlers during toilet training as caregivers lose their self-control and punish children for soiling themselves. For me, simple pattern recognition; for the jury, simply unbelievable. We lost the case.
We are almost always losing the case as pediatricians. Spending on children makes up less than 10% of the federal budget, whereas spending on the elderly, including Social Security, Medicare, and the adult component of Medicaid, dominates that budget.1 Moreover, twice as many children as adults over age 65 are living in poverty in the United States. The Temporary Assistance for Needy Families program is often debated in this country and frequently criticized as wasteful. However, what is not debatable is that the allocated budget ($16.5 billion) hasn’t changed since 1996, resulting in a functional 40% decrease due to inflation.2 Life, for poor children, gets a little tougher every year.
After the resident and I wrapped up our day, we talked a little about how hard it is to witness some of the things you see in a children’s hospital. I could see the gap between her and the outside world widening right in front of me. In my weaker moments, I want to tell trainees like her to run while they can. I want to warn them that they don’t want to know so many of the things we’re going to teach them. I know how the story usually ends. I know that our country doesn’t promise children safety from social deprivation, hunger, or physical abuse. Instead, we’ve created the conditions for those things to occur at embarrassingly high rates, and we prosecute the unlucky after the fact. The children are simply collateral damage.
We stood at our patient’s bedside and tried to imagine a happy future. Even without his medical problems, he would likely need a major investment of resources in order to thrive. Where would those resources come from? I saw the hospital crib, metal bars on all sides and a thick plastic roof to prevent escape, as a metaphor. Later, I took the elevator down and overheard a snippet of conversation between two residents. One of them asked the other, “How do you know when you’ve burned out?” The other replied, “I don’t know, I guess when you’ve stopped burning.” Burnout is a hot topic in medicine, and some may assume the reasons are obvious: long hours and intellectually demanding work. In reality, those drivers may be less important than the repeated exposure to profound injustice inherent to the practice of medicine in our country.
As hospitalists, we address acute decompensation in our patients and send them back out into the world knowing there will soon be a next time. We also know that the next time might be preventable, if only … This cycle sometimes feels inexorable, but it can also prompt us to think about our obligation to work toward a more just society. We have to imagine a better future even as we struggle to believe it is on the way.
Most of our hospitals are trying to help. They have community-engagement programs, they purchase housing for homeless patients, they provide large amounts of uncompensated care and sometimes operate at a loss. Yet none of this addresses the root cause of the problem. Medicine, either in the form of an institution or a doctor, can’t replace a just society, but the truth of this fact does not mean we should not try.
Pediatrics has always been a field disposed toward advocacy. The origin of our largest professional organization in the United States was the intraprofessional conflict within the American Medical Association (AMA) over the Sheppard-Towner Act of 1921, one of this country’s first attempts to address the social determinants of health with legislation.3 The American Academy of Pediatrics was formed in 1930 after the AMA House of Delegates rebuked the Pediatric section for advocating for continuance of the act during the late 1920s.3 Perhaps what Pediatrics has to teach the rest of medicine is the necessity of making advocacy a part of our professional identity. And perhaps that’s the reason that so many pediatricians are still burning and not burned out.
1. Committee for a Responsible Federal Budget. Chartbook: budgeting for the next generation. October 11, 2018. Accessed February 2, 2021. http://www.crfb.org/papers/chartbook-budgeting-next-generation
2. Center on Budget and Policy Priorities. Policy basics: temporary assistance for needy families. Updated March 31, 2021. Accessed February 2, 2021. https://www.cbpp.org/research/family-income-support/temporary-assistance-for-needy-families
3. van Dyck PC. A history of child health equity legislation in the United States. Pediatrics. 2003;112(3 pt 2):727-730.
A celebratory mood pervaded the last week of service for my ward team at the end of the academic year. As the attending, it was just another day, but it was hard not to be caught up in the general feeling of a milestone flying past. Like most days in a hospital, this one passed in a rhythm of alternating mundanity and crisis. Late in the afternoon, one of the residents called me to a bedside for help. Imagining that my diagnostic skills were urgently required, I took the stairs. The problem, as it turned out, was not strictly medical.
I could hear the yelling before I cleared the locked entry doors to the ward. It doesn’t really matter what the yelling was about, just that there is often yelling and there is always very little I can do about the root cause of it. As I stepped into the middle of the conflagration, I remembered the story an intern told me about the night earlier in the month when it fell to her to wheel the same patient’s intoxicated parent down to the emergency department. After sleeping it off, the parent was diagnosed with an “allergic reaction” and given a prescription for diphenhydramine. We all knew the diagnosis was fantasy, and yet we all went along with it because there was simply no help available for the root cause of the problem. State social services was already involved, and we had a “safety” plan in place for discharge. As meager as that may have been, we had done the best we could to balance the risk with the available resources… or so we told ourselves.
As a nation, we have chosen not to provide much of a social safety net for our citizens who suffer from addiction and/or mental illness and, most importantly, for those who’ve just not had a leg up on the economic ladder. As a hospital-based clinician, I know that people in distress lose their cool and yell sometimes. Ironically, they may yell most loudly at people who sincerely want to help, simply because others do not engage them. Medical schools don’t teach us how to handle the yelling, though many would say it is part of the hidden curriculum. One thing that distinguishes many pediatricians like myself is a willingness to listen to the yelling, to engage with it, and to try to help. Not surprisingly, our reputation around the hospital is that we skew a bit naive.
It is worth asking, though: Are pediatricians naive? Sure, we make funny faces. We clown. We baby-talk. Those things are largely true, but there are other true things about pediatricians. Chief among them is the fact that we come to know some of the worst things there are to know about human beings. Everybody knows people can be awful, but we know exactly how awful they are to defenseless children in precise detail. For instance, I’ve seen a 4-year-old who was repeatedly starved as a regular punishment. She was so hungry she ate her hair, which turned out to be lucky for her because it caused an intestinal blockage that led to the discovery of the abuse. I gave her an apple one day and she immediately hid it under her shirt. Where you see a scab on a child’s inner arm, I see a cigarette burn. I’ve resuscitated a baby whose parents dipped his pacifier in heroin to stop his crying—the remarkable part of the story being that it was heroin cooked in the hospital bathroom. And then there are the things that I cannot even bring myself to write down.
Carrying this knowledge hollows out a gap between pediatricians and the rest of the world. The divergence between our expectations of how a society should treat its children and the reality of our daily experience grinds away any naivete. The gap becomes a canyon for some of us. We live with the sense that nobody would believe the things we’ve seen, so we rarely talk about them. Years ago, I was testifying in a (for me) routine child-abuse case where this fact hit home. It is common for juries to disbelieve that a caregiver could do the things we allege. I say allege, but if you work as a pediatrician long enough, the space between allegation and fact narrows. It is simply pattern recognition to you—abuse happens so consistently that we accept it as a diagnostic category. The case in question was a submersion burn, which is an almost unmistakable pattern. The other piece of the story is that it happens to toddlers during toilet training as caregivers lose their self-control and punish children for soiling themselves. For me, simple pattern recognition; for the jury, simply unbelievable. We lost the case.
We are almost always losing the case as pediatricians. Spending on children makes up less than 10% of the federal budget, whereas spending on the elderly, including Social Security, Medicare, and the adult component of Medicaid, dominates that budget.1 Moreover, twice as many children as adults over age 65 are living in poverty in the United States. The Temporary Assistance for Needy Families program is often debated in this country and frequently criticized as wasteful. However, what is not debatable is that the allocated budget ($16.5 billion) hasn’t changed since 1996, resulting in a functional 40% decrease due to inflation.2 Life, for poor children, gets a little tougher every year.
After the resident and I wrapped up our day, we talked a little about how hard it is to witness some of the things you see in a children’s hospital. I could see the gap between her and the outside world widening right in front of me. In my weaker moments, I want to tell trainees like her to run while they can. I want to warn them that they don’t want to know so many of the things we’re going to teach them. I know how the story usually ends. I know that our country doesn’t promise children safety from social deprivation, hunger, or physical abuse. Instead, we’ve created the conditions for those things to occur at embarrassingly high rates, and we prosecute the unlucky after the fact. The children are simply collateral damage.
We stood at our patient’s bedside and tried to imagine a happy future. Even without his medical problems, he would likely need a major investment of resources in order to thrive. Where would those resources come from? I saw the hospital crib, metal bars on all sides and a thick plastic roof to prevent escape, as a metaphor. Later, I took the elevator down and overheard a snippet of conversation between two residents. One of them asked the other, “How do you know when you’ve burned out?” The other replied, “I don’t know, I guess when you’ve stopped burning.” Burnout is a hot topic in medicine, and some may assume the reasons are obvious: long hours and intellectually demanding work. In reality, those drivers may be less important than the repeated exposure to profound injustice inherent to the practice of medicine in our country.
As hospitalists, we address acute decompensation in our patients and send them back out into the world knowing there will soon be a next time. We also know that the next time might be preventable, if only … This cycle sometimes feels inexorable, but it can also prompt us to think about our obligation to work toward a more just society. We have to imagine a better future even as we struggle to believe it is on the way.
Most of our hospitals are trying to help. They have community-engagement programs, they purchase housing for homeless patients, they provide large amounts of uncompensated care and sometimes operate at a loss. Yet none of this addresses the root cause of the problem. Medicine, either in the form of an institution or a doctor, can’t replace a just society, but the truth of this fact does not mean we should not try.
Pediatrics has always been a field disposed toward advocacy. The origin of our largest professional organization in the United States was the intraprofessional conflict within the American Medical Association (AMA) over the Sheppard-Towner Act of 1921, one of this country’s first attempts to address the social determinants of health with legislation.3 The American Academy of Pediatrics was formed in 1930 after the AMA House of Delegates rebuked the Pediatric section for advocating for continuance of the act during the late 1920s.3 Perhaps what Pediatrics has to teach the rest of medicine is the necessity of making advocacy a part of our professional identity. And perhaps that’s the reason that so many pediatricians are still burning and not burned out.
A celebratory mood pervaded the last week of service for my ward team at the end of the academic year. As the attending, it was just another day, but it was hard not to be caught up in the general feeling of a milestone flying past. Like most days in a hospital, this one passed in a rhythm of alternating mundanity and crisis. Late in the afternoon, one of the residents called me to a bedside for help. Imagining that my diagnostic skills were urgently required, I took the stairs. The problem, as it turned out, was not strictly medical.
I could hear the yelling before I cleared the locked entry doors to the ward. It doesn’t really matter what the yelling was about, just that there is often yelling and there is always very little I can do about the root cause of it. As I stepped into the middle of the conflagration, I remembered the story an intern told me about the night earlier in the month when it fell to her to wheel the same patient’s intoxicated parent down to the emergency department. After sleeping it off, the parent was diagnosed with an “allergic reaction” and given a prescription for diphenhydramine. We all knew the diagnosis was fantasy, and yet we all went along with it because there was simply no help available for the root cause of the problem. State social services was already involved, and we had a “safety” plan in place for discharge. As meager as that may have been, we had done the best we could to balance the risk with the available resources… or so we told ourselves.
As a nation, we have chosen not to provide much of a social safety net for our citizens who suffer from addiction and/or mental illness and, most importantly, for those who’ve just not had a leg up on the economic ladder. As a hospital-based clinician, I know that people in distress lose their cool and yell sometimes. Ironically, they may yell most loudly at people who sincerely want to help, simply because others do not engage them. Medical schools don’t teach us how to handle the yelling, though many would say it is part of the hidden curriculum. One thing that distinguishes many pediatricians like myself is a willingness to listen to the yelling, to engage with it, and to try to help. Not surprisingly, our reputation around the hospital is that we skew a bit naive.
It is worth asking, though: Are pediatricians naive? Sure, we make funny faces. We clown. We baby-talk. Those things are largely true, but there are other true things about pediatricians. Chief among them is the fact that we come to know some of the worst things there are to know about human beings. Everybody knows people can be awful, but we know exactly how awful they are to defenseless children in precise detail. For instance, I’ve seen a 4-year-old who was repeatedly starved as a regular punishment. She was so hungry she ate her hair, which turned out to be lucky for her because it caused an intestinal blockage that led to the discovery of the abuse. I gave her an apple one day and she immediately hid it under her shirt. Where you see a scab on a child’s inner arm, I see a cigarette burn. I’ve resuscitated a baby whose parents dipped his pacifier in heroin to stop his crying—the remarkable part of the story being that it was heroin cooked in the hospital bathroom. And then there are the things that I cannot even bring myself to write down.
Carrying this knowledge hollows out a gap between pediatricians and the rest of the world. The divergence between our expectations of how a society should treat its children and the reality of our daily experience grinds away any naivete. The gap becomes a canyon for some of us. We live with the sense that nobody would believe the things we’ve seen, so we rarely talk about them. Years ago, I was testifying in a (for me) routine child-abuse case where this fact hit home. It is common for juries to disbelieve that a caregiver could do the things we allege. I say allege, but if you work as a pediatrician long enough, the space between allegation and fact narrows. It is simply pattern recognition to you—abuse happens so consistently that we accept it as a diagnostic category. The case in question was a submersion burn, which is an almost unmistakable pattern. The other piece of the story is that it happens to toddlers during toilet training as caregivers lose their self-control and punish children for soiling themselves. For me, simple pattern recognition; for the jury, simply unbelievable. We lost the case.
We are almost always losing the case as pediatricians. Spending on children makes up less than 10% of the federal budget, whereas spending on the elderly, including Social Security, Medicare, and the adult component of Medicaid, dominates that budget.1 Moreover, twice as many children as adults over age 65 are living in poverty in the United States. The Temporary Assistance for Needy Families program is often debated in this country and frequently criticized as wasteful. However, what is not debatable is that the allocated budget ($16.5 billion) hasn’t changed since 1996, resulting in a functional 40% decrease due to inflation.2 Life, for poor children, gets a little tougher every year.
After the resident and I wrapped up our day, we talked a little about how hard it is to witness some of the things you see in a children’s hospital. I could see the gap between her and the outside world widening right in front of me. In my weaker moments, I want to tell trainees like her to run while they can. I want to warn them that they don’t want to know so many of the things we’re going to teach them. I know how the story usually ends. I know that our country doesn’t promise children safety from social deprivation, hunger, or physical abuse. Instead, we’ve created the conditions for those things to occur at embarrassingly high rates, and we prosecute the unlucky after the fact. The children are simply collateral damage.
We stood at our patient’s bedside and tried to imagine a happy future. Even without his medical problems, he would likely need a major investment of resources in order to thrive. Where would those resources come from? I saw the hospital crib, metal bars on all sides and a thick plastic roof to prevent escape, as a metaphor. Later, I took the elevator down and overheard a snippet of conversation between two residents. One of them asked the other, “How do you know when you’ve burned out?” The other replied, “I don’t know, I guess when you’ve stopped burning.” Burnout is a hot topic in medicine, and some may assume the reasons are obvious: long hours and intellectually demanding work. In reality, those drivers may be less important than the repeated exposure to profound injustice inherent to the practice of medicine in our country.
As hospitalists, we address acute decompensation in our patients and send them back out into the world knowing there will soon be a next time. We also know that the next time might be preventable, if only … This cycle sometimes feels inexorable, but it can also prompt us to think about our obligation to work toward a more just society. We have to imagine a better future even as we struggle to believe it is on the way.
Most of our hospitals are trying to help. They have community-engagement programs, they purchase housing for homeless patients, they provide large amounts of uncompensated care and sometimes operate at a loss. Yet none of this addresses the root cause of the problem. Medicine, either in the form of an institution or a doctor, can’t replace a just society, but the truth of this fact does not mean we should not try.
Pediatrics has always been a field disposed toward advocacy. The origin of our largest professional organization in the United States was the intraprofessional conflict within the American Medical Association (AMA) over the Sheppard-Towner Act of 1921, one of this country’s first attempts to address the social determinants of health with legislation.3 The American Academy of Pediatrics was formed in 1930 after the AMA House of Delegates rebuked the Pediatric section for advocating for continuance of the act during the late 1920s.3 Perhaps what Pediatrics has to teach the rest of medicine is the necessity of making advocacy a part of our professional identity. And perhaps that’s the reason that so many pediatricians are still burning and not burned out.
1. Committee for a Responsible Federal Budget. Chartbook: budgeting for the next generation. October 11, 2018. Accessed February 2, 2021. http://www.crfb.org/papers/chartbook-budgeting-next-generation
2. Center on Budget and Policy Priorities. Policy basics: temporary assistance for needy families. Updated March 31, 2021. Accessed February 2, 2021. https://www.cbpp.org/research/family-income-support/temporary-assistance-for-needy-families
3. van Dyck PC. A history of child health equity legislation in the United States. Pediatrics. 2003;112(3 pt 2):727-730.
1. Committee for a Responsible Federal Budget. Chartbook: budgeting for the next generation. October 11, 2018. Accessed February 2, 2021. http://www.crfb.org/papers/chartbook-budgeting-next-generation
2. Center on Budget and Policy Priorities. Policy basics: temporary assistance for needy families. Updated March 31, 2021. Accessed February 2, 2021. https://www.cbpp.org/research/family-income-support/temporary-assistance-for-needy-families
3. van Dyck PC. A history of child health equity legislation in the United States. Pediatrics. 2003;112(3 pt 2):727-730.
© 2021 Society of Hospital Medicine
Gender Distribution in Pediatric Hospital Medicine Leadership
There is a growing appreciation of gender disparities in career advancement in medicine. By 2004, approximately 50% of medical school graduates were women, yet considerable differences persist between genders in compensation, faculty rank, and leadership positions.1-3 According to the Association of American Medical Colleges (AAMC), women account for only 25% of full professors, 18% of department chairs, and 18% of medical school deans.1 Women are also underrepresented in other areas of leadership such as division directors, professional society leadership, and hospital executives.4-6
Specialties that are predominantly women, including pediatrics, are not immune to gender disparities. Women represent 71% of pediatric residents1 and currently constitute two-thirds of active pediatricians in the United States.7 However, there is a disproportionately low number of women ascending the pediatric academic ladder, with only 35% of full professors2 and 28% of department chairs being women.1 Pediatrics also was noted to have the fifth-largest gender pay gap across 40 specialties.3 These disparities can contribute to burnout, poorer patient outcomes, and decreased advancement of women known as the “leaky pipeline.”1,8,9
There is some evidence that gender disparities may be improving among younger professionals with increasing percentages of women as leaders and decreasing pay gaps.10,11 These potential positive trends provide hope that fields in medicine early in their development may demonstrate fewer gender disparities. One of the youngest fields of medicine is pediatric hospital medicine (PHM), which officially became a recognized pediatric subspecialty in 2017.12 There is no literature to date describing gender disparities in PHM. We aimed to explore the gender distribution of university-based PHM program leadership and to compare this gender distribution with that seen in the broader field of PHM.
METHODS
This study was Institutional Review Board–approved as non–human subjects research through University of Chicago, Chicago, Illinois. From January to March 2020, the authors performed web-based searches for PHM division directors or program leaders in the United States. Because there is no single database of PHM programs in the United States, we used the AAMC list of Liaison Committee on Medical Education (LCME)–accredited US medical schools; medical schools in Puerto Rico were not included, nor were pending and provisional institutions. If an institution had multiple practice sites for its students, the primary site for third-year medical student clerkship rotations was included. If a medical school had multiple branches, each with its own primary inpatient pediatrics site, these sites were included. If there was no PHM division director, a program leader (lead hospitalist) was substituted and counted as long as the role was formally designated. This leadership role is herein referred to under the umbrella term of “division director.”
We searched medical school web pages, affiliated hospital web pages, and Google. All program leadership information (divisional and fellowship, if present) was confirmed through direct communication with the program, most commonly with division directors, and included name, gender, title, and presence of associate/assistant leader, gender, and title. Associate division directors were only included if it was a formal leadership position. Associate directors of research, quality, etc, were not included due to the limited number of formal positions noted on further review. Of note, the terms “associate” and “assistant” are referring to leadership positions and not academic ranks.
Fellowship leadership was included if affiliated with a US medical school in the primary list. Medical schools with multiple PHM fellowships were included as separate observations. The leadership was confirmed using the methods described above and cross-referenced through the PHM Fellowship Program website. PHM fellowship programs starting in 2020 were included if leadership was determined.
All leadership positions were verified by two authors, and all authors reviewed the master list to identify errors.
To determine the overall gender breakdown in the specialty, we used three estimates: 2019 American Board of Pediatrics (ABP) PHM Board Certification Exam applicants, the 2019 American Academy of Pediatrics Section on Hospital Medicine membership, and a random sample of all PHM faculty in 25% of the programs included in this study.4
Descriptive statistics using 95% confidence intervals for proportions were used. Differences between proportions were evaluated using a two-proportion z test with the null hypothesis that the two proportions are the same and significance set at P < .05.
RESULTS
Of the 150 AAMC LCME–accredited medical school departments of pediatrics evaluated, a total of 142 programs were included; eight programs were excluded due to not providing inpatient pediatric services.
Division Leadership
The proportion of women PHM division directors was 55% (95% CI, 47%-63%) in this sample of 146 leaders from 142 programs (4 programs had coleaders). In the 113 programs with standalone PHM divisions or sections, the proportion of women division directors was 56% (95% CI, 47%-64%). In the 29 hospitalist groups that were not standalone (ie, embedded in another division), the proportion of women leaders was similar at 52% (95% CI, 34%-69%). In 24 programs with 27 formally designated associate directors (1 program had 3 associate directors and 1 program had 2), 81% of associate directors were women (95% CI, 63%-92%).
Fellowship Leadership
A total of 51 PHM fellowship programs had 53 directors (2 had codirectors), and 66% of the fellowship directors were women (95% CI, 53%-77%). A total of 31 programs had 34 assistant directors (3 programs had 2 assistants), and 82% of the assistant fellowship directors were women (95% CI, 66%-92%).
Comparison With the Field at Large
The inaugural ABP PHM board certification exam in 2019 had 1,627 applicants with 70% women (95% CI, 68%-73%) (Suzanne Woods, MD, email communication, December 4, 2019). The American Academy of Pediatrics Section on Hospital Medicine, the largest PHM-specific organization, has 2,299 practicing physician members with 71% women (95% CI, 69%-73%) (Niccole Alexander, email communication, November 25, 2019). Our random sample of 25% of university-based PHM programs contained 1,063 faculty members with 72% women (95% CI, 69%-75%).
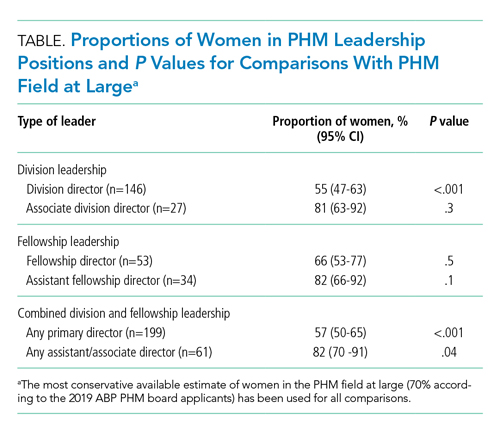
The Table provides P values for comparisons of the proportion of women in each of the above-described leadership roles compared to the most conservative estimate of women in the field from the estimates given above (ie, 70%). Compared with the field at large, women appear to be underrepresented as division directors (70% vs 55%; P < .001) but not as fellowship directors (70% vs 66%; P = .5). There is a higher proportion of women in all associate/assistant director roles, compared with the population (82% vs 70%; P = .04).
DISCUSSION
We found a significant difference between the proportion of women as PHM division directors (55%) when compared with the proportion of women physicians in PHM (70%), which suggests that women are underrepresented in clinical leadership at university-based pediatric hospitalist programs. Similar findings are described in other specialties, including notably adult hospital medicine.4 Burden et al found that only 16% of hospital medicine program leaders were women despite an equal number of women and men in the field. PHM has a much larger proportion of women, compared with that of hospital medicine, and yet women are still underrepresented as program leaders.
We found no disparities between the proportion of women as PHM fellowship directors and the field at large. These results are similar to those of other studies, which showed a higher number of women in educational leadership roles and lower representation in roles with influence over policy and allocation of resources.13,14 Although the proportion of women in educational roles itself is not a concern, there is evidence that these positions may be undervalued by some institutions, which provide these positions with lower salaries and fewer opportunities for career advancement.13,14
Interestingly, women are well-represented in associate/assistant director roles at both the division and fellowship leader level when comparing the distribution in those roles with that of the PHM field at large. This finding suggests that the pipeline of women is robust and potentially may indicate positive change. Alternatively, this finding may reflect a previously described phenomenon of the “sticky floor” in which women are “stuck” in these supportive roles and do not necessarily advance to higher-impact positions.15 We found a statistically significant higher proportion of women in the combined group of all associate/assistant directors compared with the overall population, which raises the concern that supportive leadership roles may represent “women’s work.”16 Future studies are needed to track whether these women truly advance or whether women are overrepresented in supportive leadership positions at the expense of primary leadership positions.
Adequate representation of women alone is not sufficient to achieve gender equity in medicine. We need to understand why there is a lower representation of women in leadership positions. Some barriers have already been described, including gender bias in promotions,17 higher demands outside of work,18 and lower pay,3 though none are specific to PHM. A further qualitative exploration of PHM leadership would help describe any barriers women in PHM specifically may be facing in their career trajectory. In addition, more information is needed to explore the experience of women with intersectional identities in PHM, especially since they may experience increased bias and discrimination.19
Limitations of this study include the lack of a centralized list of PHM programs and data on PHM workforce. Our three estimates for the proportion of women in PHM were similar at 70%-71%; however, these are only proxies for the true gender distribution of PHM physicians, which is unknown. PHM leadership targets of close to 70% women would be reflective of the field at large; however, institutional variation may exist, and ideally leadership should be diverse and reflective of its faculty members. Our study only describes university-based PHM programs and, therefore, is not necessarily generalizable to nonuniversity programs. Further studies are needed to evaluate any potential differences based on program type. In our study, gender was used in binary terms; however, we acknowledge that gender exists on a spectrum.
CONCLUSION
As a specialty early in development with a robust pipeline of women, PHM is in a unique position to lead the way in gender equity. However, women appear to be underrepresented as division directors at university-based PHM programs. Achieving proportional representation of women leaders is imperative for tapping into the full potential of the community and ensuring that the goals of the field are representative of the population.
Acknowledgment
Special thanks to Lucille Lester, MD, who asked the question that started this road to discovery.
1. Lautenberger DM, Dandar VM. State of Women in Academic Medicine 2018-2019 Exploring Pathways to Equity. AAMC; 2020. Accessed April 10, 2020. https://www.aamc.org/data-reports/data/2018-2019-state-women-academic-medicine-exploring-pathways-equity
2. Table 13: U.S. Medical School Faculty by Sex, Rank, and Department, 2017. AAMC; 2019. Accessed June 25, 2020. https://www.aamc.org/download/486102/data/17table13.pdf
3. 2019 Physician Compensation Report. Doximity; March 2019. Accessed April 11, 2020. https://s3.amazonaws.com/s3.doximity.com/press/doximity_third_annual_physician_compensation_report_round3.pdf
4. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340
5. Silver J, Ghalib R, Poorman JA, et al. Analysis of gender equity in leadership of physician-focused medical specialty societies, 2008-2017. JAMA Intern Med. 2019:179(3):433-435. https://doi.org/10.1001/jamainternmed.2018.5303
6. Thomas R, Cooper M, Konar E, et al. Lean In: Women in the Workplace 2019. McKinsey & Company; 2019. Accessed July 1, 2020. https://wiw-report.s3.amazonaws.com/Women_in_the_Workplace_2019.pdf
7. Table 1.3: Number and Percentage of Active Physicians by Sex and Specialty, 2017. AAMC; 2017. Accessed April 12, 2020. https://www.aamc.org/data-reports/workforce/interactive-data/active-physicians-sex-and-specialty-2017
8. Taka F, Nomura K, Horie S, et al. Organizational climate with gender equity and burnout among university academics in Japan. Ind Health. 2016;54(6):480-487. https://doi.org/10.2486/indhealth.2016-0126
9. Tsugawa Y, Jena A, Figueroa J, Orav EJ, Blumenthal DM, Jha AK. Comparison of hospital mortality and readmission rates for medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177(2):206-213. https://doi.org/10.1001/jamainternmed.2016.7875
10. Bissing MA, Lange EMS, Davila WF, et al. Status of women in academic anesthesiology: a 10-year update. Anesth Analg. 2019;128(1):137-143. https://doi.org/10.1213/ane.0000000000003691
11. Graf N, Brown A, Patten E. The narrowing, but persistent, gender gap in pay. Pew Research Center; March 22, 2019. Accessed April 20, 2020. https://www.pewresearch.org/fact-tank/2019/03/22/gender-pay-gap-facts/
12. American Board of Medical Specialties Officially Recognizes Pediatric Hospital Medicine Subspecialty Certification. News release. American Board of Medical Specialties; November 9, 2016. Accessed June 25, 2020. https://www.abms.org/media/120095/abms-recognizes-pediatric-hospital-medicine-as-a-subspecialty.pdf
13. Hofler LG, Hacker MR, Dodge LE, Schutzberg R, Ricciotti HA. Comparison of women in department leadership in obstetrics and gynecology with other specialties. Obstet Gynecol. 2016;127(3):442-447. https://doi.org/10.1097/aog.0000000000001290
14. Weiss A, Lee KC, Tapia V, et al. Equity in surgical leadership for women: more work to do. Am J Surg. 2014;208:494-498. https://doi.org/10.1016/j.amjsurg.2013.11.005
15. Tesch BJ, Wood HM, Helwig AL, Nattinger AB. Promotion of women physicians in academic medicine. Glass ceiling or sticky floor? JAMA. 1995;273(13):1022-1025.
16. Pelley E, Carnes M. When a specialty becomes “women’s work”: trends in and implications of specialty gender segregation in medicine. Acad Med. 2020;95(10):1499-1506. https://doi.org/10.1097/acm.0000000000003555
17. Steinpreis RE, Anders KA, Ritzke D. The impact of gender on the review of the curricula vitae of job applicants and tenure candidates: a national empirical study. Sex Roles. 1999;41(7):509-528. https://doi.org/10.1023/A:1018839203698
18. Jolly S, Griffith KA, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Intern Med. 2014;160(5):344-353. https://doi.org/10.7326/m13-0974
19. Ginther DK, Kahn S, Schaffer WT. Gender, race/ethnicity, and National Institutes of Health R01 research awards: is there evidence of a double bind for women of color? Acad Med. 2016;91(8):1098-1107. https://doi.org/10.1097/acm.0000000000001278
There is a growing appreciation of gender disparities in career advancement in medicine. By 2004, approximately 50% of medical school graduates were women, yet considerable differences persist between genders in compensation, faculty rank, and leadership positions.1-3 According to the Association of American Medical Colleges (AAMC), women account for only 25% of full professors, 18% of department chairs, and 18% of medical school deans.1 Women are also underrepresented in other areas of leadership such as division directors, professional society leadership, and hospital executives.4-6
Specialties that are predominantly women, including pediatrics, are not immune to gender disparities. Women represent 71% of pediatric residents1 and currently constitute two-thirds of active pediatricians in the United States.7 However, there is a disproportionately low number of women ascending the pediatric academic ladder, with only 35% of full professors2 and 28% of department chairs being women.1 Pediatrics also was noted to have the fifth-largest gender pay gap across 40 specialties.3 These disparities can contribute to burnout, poorer patient outcomes, and decreased advancement of women known as the “leaky pipeline.”1,8,9
There is some evidence that gender disparities may be improving among younger professionals with increasing percentages of women as leaders and decreasing pay gaps.10,11 These potential positive trends provide hope that fields in medicine early in their development may demonstrate fewer gender disparities. One of the youngest fields of medicine is pediatric hospital medicine (PHM), which officially became a recognized pediatric subspecialty in 2017.12 There is no literature to date describing gender disparities in PHM. We aimed to explore the gender distribution of university-based PHM program leadership and to compare this gender distribution with that seen in the broader field of PHM.
METHODS
This study was Institutional Review Board–approved as non–human subjects research through University of Chicago, Chicago, Illinois. From January to March 2020, the authors performed web-based searches for PHM division directors or program leaders in the United States. Because there is no single database of PHM programs in the United States, we used the AAMC list of Liaison Committee on Medical Education (LCME)–accredited US medical schools; medical schools in Puerto Rico were not included, nor were pending and provisional institutions. If an institution had multiple practice sites for its students, the primary site for third-year medical student clerkship rotations was included. If a medical school had multiple branches, each with its own primary inpatient pediatrics site, these sites were included. If there was no PHM division director, a program leader (lead hospitalist) was substituted and counted as long as the role was formally designated. This leadership role is herein referred to under the umbrella term of “division director.”
We searched medical school web pages, affiliated hospital web pages, and Google. All program leadership information (divisional and fellowship, if present) was confirmed through direct communication with the program, most commonly with division directors, and included name, gender, title, and presence of associate/assistant leader, gender, and title. Associate division directors were only included if it was a formal leadership position. Associate directors of research, quality, etc, were not included due to the limited number of formal positions noted on further review. Of note, the terms “associate” and “assistant” are referring to leadership positions and not academic ranks.
Fellowship leadership was included if affiliated with a US medical school in the primary list. Medical schools with multiple PHM fellowships were included as separate observations. The leadership was confirmed using the methods described above and cross-referenced through the PHM Fellowship Program website. PHM fellowship programs starting in 2020 were included if leadership was determined.
All leadership positions were verified by two authors, and all authors reviewed the master list to identify errors.
To determine the overall gender breakdown in the specialty, we used three estimates: 2019 American Board of Pediatrics (ABP) PHM Board Certification Exam applicants, the 2019 American Academy of Pediatrics Section on Hospital Medicine membership, and a random sample of all PHM faculty in 25% of the programs included in this study.4
Descriptive statistics using 95% confidence intervals for proportions were used. Differences between proportions were evaluated using a two-proportion z test with the null hypothesis that the two proportions are the same and significance set at P < .05.
RESULTS
Of the 150 AAMC LCME–accredited medical school departments of pediatrics evaluated, a total of 142 programs were included; eight programs were excluded due to not providing inpatient pediatric services.
Division Leadership
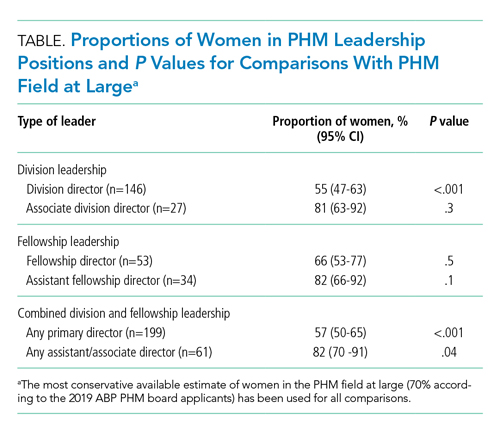
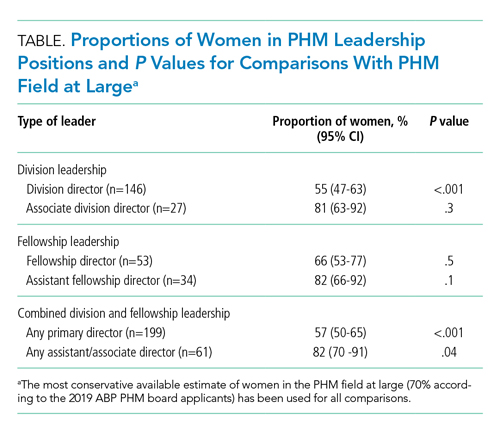
The proportion of women PHM division directors was 55% (95% CI, 47%-63%) in this sample of 146 leaders from 142 programs (4 programs had coleaders). In the 113 programs with standalone PHM divisions or sections, the proportion of women division directors was 56% (95% CI, 47%-64%). In the 29 hospitalist groups that were not standalone (ie, embedded in another division), the proportion of women leaders was similar at 52% (95% CI, 34%-69%). In 24 programs with 27 formally designated associate directors (1 program had 3 associate directors and 1 program had 2), 81% of associate directors were women (95% CI, 63%-92%).
Fellowship Leadership
A total of 51 PHM fellowship programs had 53 directors (2 had codirectors), and 66% of the fellowship directors were women (95% CI, 53%-77%). A total of 31 programs had 34 assistant directors (3 programs had 2 assistants), and 82% of the assistant fellowship directors were women (95% CI, 66%-92%).
Comparison With the Field at Large
The inaugural ABP PHM board certification exam in 2019 had 1,627 applicants with 70% women (95% CI, 68%-73%) (Suzanne Woods, MD, email communication, December 4, 2019). The American Academy of Pediatrics Section on Hospital Medicine, the largest PHM-specific organization, has 2,299 practicing physician members with 71% women (95% CI, 69%-73%) (Niccole Alexander, email communication, November 25, 2019). Our random sample of 25% of university-based PHM programs contained 1,063 faculty members with 72% women (95% CI, 69%-75%).
The Table provides P values for comparisons of the proportion of women in each of the above-described leadership roles compared to the most conservative estimate of women in the field from the estimates given above (ie, 70%). Compared with the field at large, women appear to be underrepresented as division directors (70% vs 55%; P < .001) but not as fellowship directors (70% vs 66%; P = .5). There is a higher proportion of women in all associate/assistant director roles, compared with the population (82% vs 70%; P = .04).
DISCUSSION
We found a significant difference between the proportion of women as PHM division directors (55%) when compared with the proportion of women physicians in PHM (70%), which suggests that women are underrepresented in clinical leadership at university-based pediatric hospitalist programs. Similar findings are described in other specialties, including notably adult hospital medicine.4 Burden et al found that only 16% of hospital medicine program leaders were women despite an equal number of women and men in the field. PHM has a much larger proportion of women, compared with that of hospital medicine, and yet women are still underrepresented as program leaders.
We found no disparities between the proportion of women as PHM fellowship directors and the field at large. These results are similar to those of other studies, which showed a higher number of women in educational leadership roles and lower representation in roles with influence over policy and allocation of resources.13,14 Although the proportion of women in educational roles itself is not a concern, there is evidence that these positions may be undervalued by some institutions, which provide these positions with lower salaries and fewer opportunities for career advancement.13,14
Interestingly, women are well-represented in associate/assistant director roles at both the division and fellowship leader level when comparing the distribution in those roles with that of the PHM field at large. This finding suggests that the pipeline of women is robust and potentially may indicate positive change. Alternatively, this finding may reflect a previously described phenomenon of the “sticky floor” in which women are “stuck” in these supportive roles and do not necessarily advance to higher-impact positions.15 We found a statistically significant higher proportion of women in the combined group of all associate/assistant directors compared with the overall population, which raises the concern that supportive leadership roles may represent “women’s work.”16 Future studies are needed to track whether these women truly advance or whether women are overrepresented in supportive leadership positions at the expense of primary leadership positions.
Adequate representation of women alone is not sufficient to achieve gender equity in medicine. We need to understand why there is a lower representation of women in leadership positions. Some barriers have already been described, including gender bias in promotions,17 higher demands outside of work,18 and lower pay,3 though none are specific to PHM. A further qualitative exploration of PHM leadership would help describe any barriers women in PHM specifically may be facing in their career trajectory. In addition, more information is needed to explore the experience of women with intersectional identities in PHM, especially since they may experience increased bias and discrimination.19
Limitations of this study include the lack of a centralized list of PHM programs and data on PHM workforce. Our three estimates for the proportion of women in PHM were similar at 70%-71%; however, these are only proxies for the true gender distribution of PHM physicians, which is unknown. PHM leadership targets of close to 70% women would be reflective of the field at large; however, institutional variation may exist, and ideally leadership should be diverse and reflective of its faculty members. Our study only describes university-based PHM programs and, therefore, is not necessarily generalizable to nonuniversity programs. Further studies are needed to evaluate any potential differences based on program type. In our study, gender was used in binary terms; however, we acknowledge that gender exists on a spectrum.
CONCLUSION
As a specialty early in development with a robust pipeline of women, PHM is in a unique position to lead the way in gender equity. However, women appear to be underrepresented as division directors at university-based PHM programs. Achieving proportional representation of women leaders is imperative for tapping into the full potential of the community and ensuring that the goals of the field are representative of the population.
Acknowledgment
Special thanks to Lucille Lester, MD, who asked the question that started this road to discovery.
There is a growing appreciation of gender disparities in career advancement in medicine. By 2004, approximately 50% of medical school graduates were women, yet considerable differences persist between genders in compensation, faculty rank, and leadership positions.1-3 According to the Association of American Medical Colleges (AAMC), women account for only 25% of full professors, 18% of department chairs, and 18% of medical school deans.1 Women are also underrepresented in other areas of leadership such as division directors, professional society leadership, and hospital executives.4-6
Specialties that are predominantly women, including pediatrics, are not immune to gender disparities. Women represent 71% of pediatric residents1 and currently constitute two-thirds of active pediatricians in the United States.7 However, there is a disproportionately low number of women ascending the pediatric academic ladder, with only 35% of full professors2 and 28% of department chairs being women.1 Pediatrics also was noted to have the fifth-largest gender pay gap across 40 specialties.3 These disparities can contribute to burnout, poorer patient outcomes, and decreased advancement of women known as the “leaky pipeline.”1,8,9
There is some evidence that gender disparities may be improving among younger professionals with increasing percentages of women as leaders and decreasing pay gaps.10,11 These potential positive trends provide hope that fields in medicine early in their development may demonstrate fewer gender disparities. One of the youngest fields of medicine is pediatric hospital medicine (PHM), which officially became a recognized pediatric subspecialty in 2017.12 There is no literature to date describing gender disparities in PHM. We aimed to explore the gender distribution of university-based PHM program leadership and to compare this gender distribution with that seen in the broader field of PHM.
METHODS
This study was Institutional Review Board–approved as non–human subjects research through University of Chicago, Chicago, Illinois. From January to March 2020, the authors performed web-based searches for PHM division directors or program leaders in the United States. Because there is no single database of PHM programs in the United States, we used the AAMC list of Liaison Committee on Medical Education (LCME)–accredited US medical schools; medical schools in Puerto Rico were not included, nor were pending and provisional institutions. If an institution had multiple practice sites for its students, the primary site for third-year medical student clerkship rotations was included. If a medical school had multiple branches, each with its own primary inpatient pediatrics site, these sites were included. If there was no PHM division director, a program leader (lead hospitalist) was substituted and counted as long as the role was formally designated. This leadership role is herein referred to under the umbrella term of “division director.”
We searched medical school web pages, affiliated hospital web pages, and Google. All program leadership information (divisional and fellowship, if present) was confirmed through direct communication with the program, most commonly with division directors, and included name, gender, title, and presence of associate/assistant leader, gender, and title. Associate division directors were only included if it was a formal leadership position. Associate directors of research, quality, etc, were not included due to the limited number of formal positions noted on further review. Of note, the terms “associate” and “assistant” are referring to leadership positions and not academic ranks.
Fellowship leadership was included if affiliated with a US medical school in the primary list. Medical schools with multiple PHM fellowships were included as separate observations. The leadership was confirmed using the methods described above and cross-referenced through the PHM Fellowship Program website. PHM fellowship programs starting in 2020 were included if leadership was determined.
All leadership positions were verified by two authors, and all authors reviewed the master list to identify errors.
To determine the overall gender breakdown in the specialty, we used three estimates: 2019 American Board of Pediatrics (ABP) PHM Board Certification Exam applicants, the 2019 American Academy of Pediatrics Section on Hospital Medicine membership, and a random sample of all PHM faculty in 25% of the programs included in this study.4
Descriptive statistics using 95% confidence intervals for proportions were used. Differences between proportions were evaluated using a two-proportion z test with the null hypothesis that the two proportions are the same and significance set at P < .05.
RESULTS
Of the 150 AAMC LCME–accredited medical school departments of pediatrics evaluated, a total of 142 programs were included; eight programs were excluded due to not providing inpatient pediatric services.
Division Leadership
The proportion of women PHM division directors was 55% (95% CI, 47%-63%) in this sample of 146 leaders from 142 programs (4 programs had coleaders). In the 113 programs with standalone PHM divisions or sections, the proportion of women division directors was 56% (95% CI, 47%-64%). In the 29 hospitalist groups that were not standalone (ie, embedded in another division), the proportion of women leaders was similar at 52% (95% CI, 34%-69%). In 24 programs with 27 formally designated associate directors (1 program had 3 associate directors and 1 program had 2), 81% of associate directors were women (95% CI, 63%-92%).
Fellowship Leadership
A total of 51 PHM fellowship programs had 53 directors (2 had codirectors), and 66% of the fellowship directors were women (95% CI, 53%-77%). A total of 31 programs had 34 assistant directors (3 programs had 2 assistants), and 82% of the assistant fellowship directors were women (95% CI, 66%-92%).
Comparison With the Field at Large
The inaugural ABP PHM board certification exam in 2019 had 1,627 applicants with 70% women (95% CI, 68%-73%) (Suzanne Woods, MD, email communication, December 4, 2019). The American Academy of Pediatrics Section on Hospital Medicine, the largest PHM-specific organization, has 2,299 practicing physician members with 71% women (95% CI, 69%-73%) (Niccole Alexander, email communication, November 25, 2019). Our random sample of 25% of university-based PHM programs contained 1,063 faculty members with 72% women (95% CI, 69%-75%).
The Table provides P values for comparisons of the proportion of women in each of the above-described leadership roles compared to the most conservative estimate of women in the field from the estimates given above (ie, 70%). Compared with the field at large, women appear to be underrepresented as division directors (70% vs 55%; P < .001) but not as fellowship directors (70% vs 66%; P = .5). There is a higher proportion of women in all associate/assistant director roles, compared with the population (82% vs 70%; P = .04).
DISCUSSION
We found a significant difference between the proportion of women as PHM division directors (55%) when compared with the proportion of women physicians in PHM (70%), which suggests that women are underrepresented in clinical leadership at university-based pediatric hospitalist programs. Similar findings are described in other specialties, including notably adult hospital medicine.4 Burden et al found that only 16% of hospital medicine program leaders were women despite an equal number of women and men in the field. PHM has a much larger proportion of women, compared with that of hospital medicine, and yet women are still underrepresented as program leaders.
We found no disparities between the proportion of women as PHM fellowship directors and the field at large. These results are similar to those of other studies, which showed a higher number of women in educational leadership roles and lower representation in roles with influence over policy and allocation of resources.13,14 Although the proportion of women in educational roles itself is not a concern, there is evidence that these positions may be undervalued by some institutions, which provide these positions with lower salaries and fewer opportunities for career advancement.13,14
Interestingly, women are well-represented in associate/assistant director roles at both the division and fellowship leader level when comparing the distribution in those roles with that of the PHM field at large. This finding suggests that the pipeline of women is robust and potentially may indicate positive change. Alternatively, this finding may reflect a previously described phenomenon of the “sticky floor” in which women are “stuck” in these supportive roles and do not necessarily advance to higher-impact positions.15 We found a statistically significant higher proportion of women in the combined group of all associate/assistant directors compared with the overall population, which raises the concern that supportive leadership roles may represent “women’s work.”16 Future studies are needed to track whether these women truly advance or whether women are overrepresented in supportive leadership positions at the expense of primary leadership positions.
Adequate representation of women alone is not sufficient to achieve gender equity in medicine. We need to understand why there is a lower representation of women in leadership positions. Some barriers have already been described, including gender bias in promotions,17 higher demands outside of work,18 and lower pay,3 though none are specific to PHM. A further qualitative exploration of PHM leadership would help describe any barriers women in PHM specifically may be facing in their career trajectory. In addition, more information is needed to explore the experience of women with intersectional identities in PHM, especially since they may experience increased bias and discrimination.19
Limitations of this study include the lack of a centralized list of PHM programs and data on PHM workforce. Our three estimates for the proportion of women in PHM were similar at 70%-71%; however, these are only proxies for the true gender distribution of PHM physicians, which is unknown. PHM leadership targets of close to 70% women would be reflective of the field at large; however, institutional variation may exist, and ideally leadership should be diverse and reflective of its faculty members. Our study only describes university-based PHM programs and, therefore, is not necessarily generalizable to nonuniversity programs. Further studies are needed to evaluate any potential differences based on program type. In our study, gender was used in binary terms; however, we acknowledge that gender exists on a spectrum.
CONCLUSION
As a specialty early in development with a robust pipeline of women, PHM is in a unique position to lead the way in gender equity. However, women appear to be underrepresented as division directors at university-based PHM programs. Achieving proportional representation of women leaders is imperative for tapping into the full potential of the community and ensuring that the goals of the field are representative of the population.
Acknowledgment
Special thanks to Lucille Lester, MD, who asked the question that started this road to discovery.
1. Lautenberger DM, Dandar VM. State of Women in Academic Medicine 2018-2019 Exploring Pathways to Equity. AAMC; 2020. Accessed April 10, 2020. https://www.aamc.org/data-reports/data/2018-2019-state-women-academic-medicine-exploring-pathways-equity
2. Table 13: U.S. Medical School Faculty by Sex, Rank, and Department, 2017. AAMC; 2019. Accessed June 25, 2020. https://www.aamc.org/download/486102/data/17table13.pdf
3. 2019 Physician Compensation Report. Doximity; March 2019. Accessed April 11, 2020. https://s3.amazonaws.com/s3.doximity.com/press/doximity_third_annual_physician_compensation_report_round3.pdf
4. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340
5. Silver J, Ghalib R, Poorman JA, et al. Analysis of gender equity in leadership of physician-focused medical specialty societies, 2008-2017. JAMA Intern Med. 2019:179(3):433-435. https://doi.org/10.1001/jamainternmed.2018.5303
6. Thomas R, Cooper M, Konar E, et al. Lean In: Women in the Workplace 2019. McKinsey & Company; 2019. Accessed July 1, 2020. https://wiw-report.s3.amazonaws.com/Women_in_the_Workplace_2019.pdf
7. Table 1.3: Number and Percentage of Active Physicians by Sex and Specialty, 2017. AAMC; 2017. Accessed April 12, 2020. https://www.aamc.org/data-reports/workforce/interactive-data/active-physicians-sex-and-specialty-2017
8. Taka F, Nomura K, Horie S, et al. Organizational climate with gender equity and burnout among university academics in Japan. Ind Health. 2016;54(6):480-487. https://doi.org/10.2486/indhealth.2016-0126
9. Tsugawa Y, Jena A, Figueroa J, Orav EJ, Blumenthal DM, Jha AK. Comparison of hospital mortality and readmission rates for medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177(2):206-213. https://doi.org/10.1001/jamainternmed.2016.7875
10. Bissing MA, Lange EMS, Davila WF, et al. Status of women in academic anesthesiology: a 10-year update. Anesth Analg. 2019;128(1):137-143. https://doi.org/10.1213/ane.0000000000003691
11. Graf N, Brown A, Patten E. The narrowing, but persistent, gender gap in pay. Pew Research Center; March 22, 2019. Accessed April 20, 2020. https://www.pewresearch.org/fact-tank/2019/03/22/gender-pay-gap-facts/
12. American Board of Medical Specialties Officially Recognizes Pediatric Hospital Medicine Subspecialty Certification. News release. American Board of Medical Specialties; November 9, 2016. Accessed June 25, 2020. https://www.abms.org/media/120095/abms-recognizes-pediatric-hospital-medicine-as-a-subspecialty.pdf
13. Hofler LG, Hacker MR, Dodge LE, Schutzberg R, Ricciotti HA. Comparison of women in department leadership in obstetrics and gynecology with other specialties. Obstet Gynecol. 2016;127(3):442-447. https://doi.org/10.1097/aog.0000000000001290
14. Weiss A, Lee KC, Tapia V, et al. Equity in surgical leadership for women: more work to do. Am J Surg. 2014;208:494-498. https://doi.org/10.1016/j.amjsurg.2013.11.005
15. Tesch BJ, Wood HM, Helwig AL, Nattinger AB. Promotion of women physicians in academic medicine. Glass ceiling or sticky floor? JAMA. 1995;273(13):1022-1025.
16. Pelley E, Carnes M. When a specialty becomes “women’s work”: trends in and implications of specialty gender segregation in medicine. Acad Med. 2020;95(10):1499-1506. https://doi.org/10.1097/acm.0000000000003555
17. Steinpreis RE, Anders KA, Ritzke D. The impact of gender on the review of the curricula vitae of job applicants and tenure candidates: a national empirical study. Sex Roles. 1999;41(7):509-528. https://doi.org/10.1023/A:1018839203698
18. Jolly S, Griffith KA, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Intern Med. 2014;160(5):344-353. https://doi.org/10.7326/m13-0974
19. Ginther DK, Kahn S, Schaffer WT. Gender, race/ethnicity, and National Institutes of Health R01 research awards: is there evidence of a double bind for women of color? Acad Med. 2016;91(8):1098-1107. https://doi.org/10.1097/acm.0000000000001278
1. Lautenberger DM, Dandar VM. State of Women in Academic Medicine 2018-2019 Exploring Pathways to Equity. AAMC; 2020. Accessed April 10, 2020. https://www.aamc.org/data-reports/data/2018-2019-state-women-academic-medicine-exploring-pathways-equity
2. Table 13: U.S. Medical School Faculty by Sex, Rank, and Department, 2017. AAMC; 2019. Accessed June 25, 2020. https://www.aamc.org/download/486102/data/17table13.pdf
3. 2019 Physician Compensation Report. Doximity; March 2019. Accessed April 11, 2020. https://s3.amazonaws.com/s3.doximity.com/press/doximity_third_annual_physician_compensation_report_round3.pdf
4. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340
5. Silver J, Ghalib R, Poorman JA, et al. Analysis of gender equity in leadership of physician-focused medical specialty societies, 2008-2017. JAMA Intern Med. 2019:179(3):433-435. https://doi.org/10.1001/jamainternmed.2018.5303
6. Thomas R, Cooper M, Konar E, et al. Lean In: Women in the Workplace 2019. McKinsey & Company; 2019. Accessed July 1, 2020. https://wiw-report.s3.amazonaws.com/Women_in_the_Workplace_2019.pdf
7. Table 1.3: Number and Percentage of Active Physicians by Sex and Specialty, 2017. AAMC; 2017. Accessed April 12, 2020. https://www.aamc.org/data-reports/workforce/interactive-data/active-physicians-sex-and-specialty-2017
8. Taka F, Nomura K, Horie S, et al. Organizational climate with gender equity and burnout among university academics in Japan. Ind Health. 2016;54(6):480-487. https://doi.org/10.2486/indhealth.2016-0126
9. Tsugawa Y, Jena A, Figueroa J, Orav EJ, Blumenthal DM, Jha AK. Comparison of hospital mortality and readmission rates for medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177(2):206-213. https://doi.org/10.1001/jamainternmed.2016.7875
10. Bissing MA, Lange EMS, Davila WF, et al. Status of women in academic anesthesiology: a 10-year update. Anesth Analg. 2019;128(1):137-143. https://doi.org/10.1213/ane.0000000000003691
11. Graf N, Brown A, Patten E. The narrowing, but persistent, gender gap in pay. Pew Research Center; March 22, 2019. Accessed April 20, 2020. https://www.pewresearch.org/fact-tank/2019/03/22/gender-pay-gap-facts/
12. American Board of Medical Specialties Officially Recognizes Pediatric Hospital Medicine Subspecialty Certification. News release. American Board of Medical Specialties; November 9, 2016. Accessed June 25, 2020. https://www.abms.org/media/120095/abms-recognizes-pediatric-hospital-medicine-as-a-subspecialty.pdf
13. Hofler LG, Hacker MR, Dodge LE, Schutzberg R, Ricciotti HA. Comparison of women in department leadership in obstetrics and gynecology with other specialties. Obstet Gynecol. 2016;127(3):442-447. https://doi.org/10.1097/aog.0000000000001290
14. Weiss A, Lee KC, Tapia V, et al. Equity in surgical leadership for women: more work to do. Am J Surg. 2014;208:494-498. https://doi.org/10.1016/j.amjsurg.2013.11.005
15. Tesch BJ, Wood HM, Helwig AL, Nattinger AB. Promotion of women physicians in academic medicine. Glass ceiling or sticky floor? JAMA. 1995;273(13):1022-1025.
16. Pelley E, Carnes M. When a specialty becomes “women’s work”: trends in and implications of specialty gender segregation in medicine. Acad Med. 2020;95(10):1499-1506. https://doi.org/10.1097/acm.0000000000003555
17. Steinpreis RE, Anders KA, Ritzke D. The impact of gender on the review of the curricula vitae of job applicants and tenure candidates: a national empirical study. Sex Roles. 1999;41(7):509-528. https://doi.org/10.1023/A:1018839203698
18. Jolly S, Griffith KA, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Intern Med. 2014;160(5):344-353. https://doi.org/10.7326/m13-0974
19. Ginther DK, Kahn S, Schaffer WT. Gender, race/ethnicity, and National Institutes of Health R01 research awards: is there evidence of a double bind for women of color? Acad Med. 2016;91(8):1098-1107. https://doi.org/10.1097/acm.0000000000001278
© 2021 Society of Hospital Medicine