User login
Just do it?
The typical American world view has always extolled the virtues of positive thinking. From the pilgrim fathers to the Western settlers, we pursued goals that were considered insurmountable. In the modern era, Ronald Reagan inspired us by stating that "Nothing is impossible," while President Obama informed us that "We can," and the sports company Nike tells us to "Just do it."
This optimistic and entrepreneurial spirit has also been adopted by vascular surgeons worldwide. It resulted in pioneering developments that have given us a whole new armamentarium that would never have been deemed possible 30 years ago. Without the benefit of the "We can" mentality, would we have been able to endograft aortic aneurysms or laser through blocked arteries? Who would have thought you could take out a saphenous vein, turn it upside down, and make it into a new artery?
However, this positive attitude, which has been absorbed into the communal psyche of vascular specialists, may have a dark side. I fear that vascular surgeons and other vascular interventionalists have developed an "I can" mantra that allows us to perform multiple hopeless procedures. We may stretch the indications for use of a new endograft, because it just might work. Like a football quarterback down by 4 points with 1 second left on the clock, we will perform a "Hail Mary" procedure, expecting to salvage a dying limb without concern that the attempt might raise the level of a subsequent amputation.
I know the famed mountaineer George Mallory tried to summit Mount Everest "Because it’s there," but why will cardiologists sometimes stent an intra-abdominal lesion just because they see it on their way to the coronaries? And why will they laser an occluded popliteal and stent a tibial, because they "can" – even though a tibial bypass would have achieved a better outcome? Is it then surprising that the "We can" and "Just do it" mentality has paved the road of good intentions with dismembered limbs and departed souls?
Of course, I do believe that a heroic attempt may be justified when faced with the alternative of loss of life or limb. But should we intervene on non–lifestyle limiting claudication just because we can? Should we stent, restent, and restent and reoperate ad infinitum until our patient begs us to stop?
Years ago, the comic newspaper The Onion published a macabre parody of an obituary, writing about a young man who "died following a brief, cowardly battle with stomach cancer. But is it cowardly to give up when things are inevitable? Is it justified to keep doing the impossible, knowing full well it will not work just because one has the self-delusion of invincibility? When should we not even try? When is enough enough?
We are not the only ones responsible for overzealous interventions. This positive attitude has caused many of our patients to have unrealistic expectations about what we are capable of achieving with our procedures.
I am sure we have all been implored by the children of a decrepit, elderly, and terminally ill patient to "Do everything. We know you can pull him through, save his leg, stop his stroke, bring him back to life, and make him young again!" How many times have such demands made us, against our better judgment, attempt the impossible?
But, lest I be accused of being overly pessimistic in this optimistic environment, let me say how proud I am to be part of the generation of vascular surgeons who have pioneered and embraced new procedures. However, I appeal to my colleagues, and especially to those who may not be vascular surgeons but who "treat" vascular patients, to sometimes say, "We won’t" even though "We can."
Dr. Samson is the medical editor of Vascular Specialist. He is a physician in the practice of Samson, Showalter, Lepore, and Nair, and a clinical professor of surgery, Florida State University.
The typical American world view has always extolled the virtues of positive thinking. From the pilgrim fathers to the Western settlers, we pursued goals that were considered insurmountable. In the modern era, Ronald Reagan inspired us by stating that "Nothing is impossible," while President Obama informed us that "We can," and the sports company Nike tells us to "Just do it."
This optimistic and entrepreneurial spirit has also been adopted by vascular surgeons worldwide. It resulted in pioneering developments that have given us a whole new armamentarium that would never have been deemed possible 30 years ago. Without the benefit of the "We can" mentality, would we have been able to endograft aortic aneurysms or laser through blocked arteries? Who would have thought you could take out a saphenous vein, turn it upside down, and make it into a new artery?
However, this positive attitude, which has been absorbed into the communal psyche of vascular specialists, may have a dark side. I fear that vascular surgeons and other vascular interventionalists have developed an "I can" mantra that allows us to perform multiple hopeless procedures. We may stretch the indications for use of a new endograft, because it just might work. Like a football quarterback down by 4 points with 1 second left on the clock, we will perform a "Hail Mary" procedure, expecting to salvage a dying limb without concern that the attempt might raise the level of a subsequent amputation.
I know the famed mountaineer George Mallory tried to summit Mount Everest "Because it’s there," but why will cardiologists sometimes stent an intra-abdominal lesion just because they see it on their way to the coronaries? And why will they laser an occluded popliteal and stent a tibial, because they "can" – even though a tibial bypass would have achieved a better outcome? Is it then surprising that the "We can" and "Just do it" mentality has paved the road of good intentions with dismembered limbs and departed souls?
Of course, I do believe that a heroic attempt may be justified when faced with the alternative of loss of life or limb. But should we intervene on non–lifestyle limiting claudication just because we can? Should we stent, restent, and restent and reoperate ad infinitum until our patient begs us to stop?
Years ago, the comic newspaper The Onion published a macabre parody of an obituary, writing about a young man who "died following a brief, cowardly battle with stomach cancer. But is it cowardly to give up when things are inevitable? Is it justified to keep doing the impossible, knowing full well it will not work just because one has the self-delusion of invincibility? When should we not even try? When is enough enough?
We are not the only ones responsible for overzealous interventions. This positive attitude has caused many of our patients to have unrealistic expectations about what we are capable of achieving with our procedures.
I am sure we have all been implored by the children of a decrepit, elderly, and terminally ill patient to "Do everything. We know you can pull him through, save his leg, stop his stroke, bring him back to life, and make him young again!" How many times have such demands made us, against our better judgment, attempt the impossible?
But, lest I be accused of being overly pessimistic in this optimistic environment, let me say how proud I am to be part of the generation of vascular surgeons who have pioneered and embraced new procedures. However, I appeal to my colleagues, and especially to those who may not be vascular surgeons but who "treat" vascular patients, to sometimes say, "We won’t" even though "We can."
Dr. Samson is the medical editor of Vascular Specialist. He is a physician in the practice of Samson, Showalter, Lepore, and Nair, and a clinical professor of surgery, Florida State University.
The typical American world view has always extolled the virtues of positive thinking. From the pilgrim fathers to the Western settlers, we pursued goals that were considered insurmountable. In the modern era, Ronald Reagan inspired us by stating that "Nothing is impossible," while President Obama informed us that "We can," and the sports company Nike tells us to "Just do it."
This optimistic and entrepreneurial spirit has also been adopted by vascular surgeons worldwide. It resulted in pioneering developments that have given us a whole new armamentarium that would never have been deemed possible 30 years ago. Without the benefit of the "We can" mentality, would we have been able to endograft aortic aneurysms or laser through blocked arteries? Who would have thought you could take out a saphenous vein, turn it upside down, and make it into a new artery?
However, this positive attitude, which has been absorbed into the communal psyche of vascular specialists, may have a dark side. I fear that vascular surgeons and other vascular interventionalists have developed an "I can" mantra that allows us to perform multiple hopeless procedures. We may stretch the indications for use of a new endograft, because it just might work. Like a football quarterback down by 4 points with 1 second left on the clock, we will perform a "Hail Mary" procedure, expecting to salvage a dying limb without concern that the attempt might raise the level of a subsequent amputation.
I know the famed mountaineer George Mallory tried to summit Mount Everest "Because it’s there," but why will cardiologists sometimes stent an intra-abdominal lesion just because they see it on their way to the coronaries? And why will they laser an occluded popliteal and stent a tibial, because they "can" – even though a tibial bypass would have achieved a better outcome? Is it then surprising that the "We can" and "Just do it" mentality has paved the road of good intentions with dismembered limbs and departed souls?
Of course, I do believe that a heroic attempt may be justified when faced with the alternative of loss of life or limb. But should we intervene on non–lifestyle limiting claudication just because we can? Should we stent, restent, and restent and reoperate ad infinitum until our patient begs us to stop?
Years ago, the comic newspaper The Onion published a macabre parody of an obituary, writing about a young man who "died following a brief, cowardly battle with stomach cancer. But is it cowardly to give up when things are inevitable? Is it justified to keep doing the impossible, knowing full well it will not work just because one has the self-delusion of invincibility? When should we not even try? When is enough enough?
We are not the only ones responsible for overzealous interventions. This positive attitude has caused many of our patients to have unrealistic expectations about what we are capable of achieving with our procedures.
I am sure we have all been implored by the children of a decrepit, elderly, and terminally ill patient to "Do everything. We know you can pull him through, save his leg, stop his stroke, bring him back to life, and make him young again!" How many times have such demands made us, against our better judgment, attempt the impossible?
But, lest I be accused of being overly pessimistic in this optimistic environment, let me say how proud I am to be part of the generation of vascular surgeons who have pioneered and embraced new procedures. However, I appeal to my colleagues, and especially to those who may not be vascular surgeons but who "treat" vascular patients, to sometimes say, "We won’t" even though "We can."
Dr. Samson is the medical editor of Vascular Specialist. He is a physician in the practice of Samson, Showalter, Lepore, and Nair, and a clinical professor of surgery, Florida State University.
'Walk out the snot'
Balloon embolectomy revolutionized the treatment of acute thromboembolism involving peripheral arteries. However, an often overlooked method that actually may be more beneficial is to "walk out the snot."
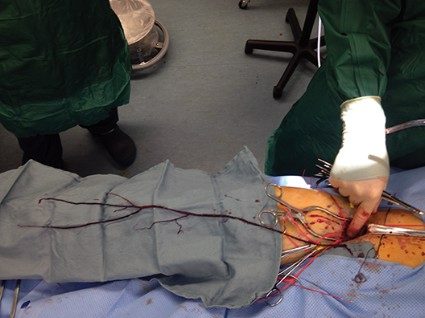
This may sound somewhat disgusting but as can be seen from the accompanying photograph, the surgeon can often retrieve the entire clot from the main artery including extensions into collateral vessels.
In this picture of a patient undergoing femoral embolectomy with this technique, we retrieved a cast of the entire superficial femoral artery as well as the peroneal and posterior tibial arteries and two major collaterals.
The technique is simple. With proximal control of the inflow artery, the visible clot is gently pulled out of the arteriotomy in a slow but deliberate fashion, hand over hand. Often back bleeding will aid in pushing the specimen out of the arteriotomy. The maneuver is very similar to what children do when they feel the need to empty their nostrils! (No adult would do that – would they?)
Retrieval of a specimen like the one in the photo will usually reassure the surgeon that there will not be more thrombus left behind.
The technique also prevents possible arterial injury from a balloon catheter. For both reasons a postcompletion arteriogram may sometimes be avoided.
Dr. Showalter is clinical assistant professor of surgery at Florida State University Medical School and attending vascular surgeon, Sarasota Vascular Specialists.
Dr. Samson is clinical professor of surgery at Florida State University Medical School, attending vascular surgeon, Sarasota Vascular Specialists, and the medical editor of Vascular Specialist.
Balloon embolectomy revolutionized the treatment of acute thromboembolism involving peripheral arteries. However, an often overlooked method that actually may be more beneficial is to "walk out the snot."
This may sound somewhat disgusting but as can be seen from the accompanying photograph, the surgeon can often retrieve the entire clot from the main artery including extensions into collateral vessels.
In this picture of a patient undergoing femoral embolectomy with this technique, we retrieved a cast of the entire superficial femoral artery as well as the peroneal and posterior tibial arteries and two major collaterals.
The technique is simple. With proximal control of the inflow artery, the visible clot is gently pulled out of the arteriotomy in a slow but deliberate fashion, hand over hand. Often back bleeding will aid in pushing the specimen out of the arteriotomy. The maneuver is very similar to what children do when they feel the need to empty their nostrils! (No adult would do that – would they?)
Retrieval of a specimen like the one in the photo will usually reassure the surgeon that there will not be more thrombus left behind.
The technique also prevents possible arterial injury from a balloon catheter. For both reasons a postcompletion arteriogram may sometimes be avoided.
Dr. Showalter is clinical assistant professor of surgery at Florida State University Medical School and attending vascular surgeon, Sarasota Vascular Specialists.
Dr. Samson is clinical professor of surgery at Florida State University Medical School, attending vascular surgeon, Sarasota Vascular Specialists, and the medical editor of Vascular Specialist.
Balloon embolectomy revolutionized the treatment of acute thromboembolism involving peripheral arteries. However, an often overlooked method that actually may be more beneficial is to "walk out the snot."
This may sound somewhat disgusting but as can be seen from the accompanying photograph, the surgeon can often retrieve the entire clot from the main artery including extensions into collateral vessels.
In this picture of a patient undergoing femoral embolectomy with this technique, we retrieved a cast of the entire superficial femoral artery as well as the peroneal and posterior tibial arteries and two major collaterals.
The technique is simple. With proximal control of the inflow artery, the visible clot is gently pulled out of the arteriotomy in a slow but deliberate fashion, hand over hand. Often back bleeding will aid in pushing the specimen out of the arteriotomy. The maneuver is very similar to what children do when they feel the need to empty their nostrils! (No adult would do that – would they?)
Retrieval of a specimen like the one in the photo will usually reassure the surgeon that there will not be more thrombus left behind.
The technique also prevents possible arterial injury from a balloon catheter. For both reasons a postcompletion arteriogram may sometimes be avoided.
Dr. Showalter is clinical assistant professor of surgery at Florida State University Medical School and attending vascular surgeon, Sarasota Vascular Specialists.
Dr. Samson is clinical professor of surgery at Florida State University Medical School, attending vascular surgeon, Sarasota Vascular Specialists, and the medical editor of Vascular Specialist.