User login
2016 Update on abnormal uterine bleeding
How abnormal uterine bleeding (AUB) is managed has a significant impact on health care. In the United States, almost one-third of all gynecologic visits are related to AUB, with estimated annual direct costs of up to $1.55 billion and indirect costs as high as $36 billion.1 Not surprisingly, office-based procedures for AUB are being emphasized. While in the short term it is more cost efficient to perform surgery in the office rather than in the operating room, questions have arisen regarding the long-term efficacy and durability of in-office procedures. Insurers are undoubtedly raising these questions as well.
Notably, some ObGyns are early adopters of office-based surgery while others tend to adopt in-office procedures more slowly. As the literature for such procedures for AUB matures to provide more data on efficacy and acceptability, we will have a greater evidence base for understanding which procedures are more appropriate for the office. And while practice shifts sometimes occur due to cost-containment initiatives, some shifts are patient driven. Studies that address these driving variables, as well as efficacy considerations, are helpful. As we counsel women about procedures for AUB, the relative advantages and disadvantages of available treatment settings likely will become a greater part of that discussion so that they can make an informed decision.
In this Update, we discuss the results of 3 studies that examined various procedures and settings for AUB management:
- outpatient vs inpatient polypectomy
- hysteroscopic morcellation of polyps and myomas in an office vs ambulatory surgical center
- comparative costs of endometrial ablation and hysterectomy.
Outpatient vs inpatient polypectomy: Similar success rates in the short term
Cooper NA, Clark TJ, Middleton L, et al; OPT Trial Collaborative Group. Outpatient versus inpatient uterine polyp treatment for abnormal uterine bleeding: randomised controlled non-inferiority study. BMJ. 2015;350:h1398. doi:10.1136/bmj.h1398.
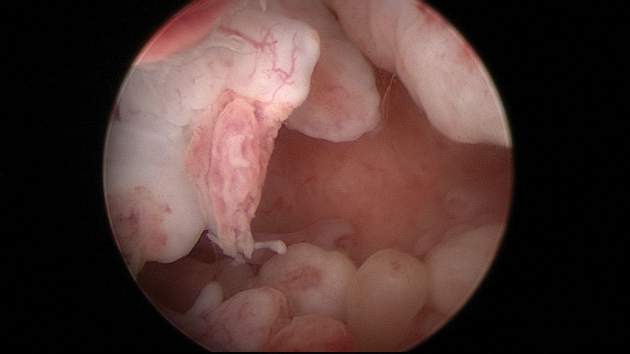
A collaborative group in the United Kingdom studied the common problem of endometrial polyps. Their objective was to evaluate whether outpatient polypectomy was as effective and well accepted as polypectomy performed in the operating room (OR).
Patients with a hysteroscopically diagnosed polyp were randomly assigned to hysteroscopic polyp removal in either a hysteroscopy clinic or an OR; polyp removal was performed using miniature mechanical or electrosurgical instruments. The primary outcome was successful treatment, determined by the participants’ assessment of their bleeding at 6 months.
Overall, 73% of women (166 of 228) in the clinic group and 80% (168 of 211) in the OR group reported a successful response to surgery at 6 months, with treatment effects being maintained at 12 and 24 months. A “see and treat” approach—that is, treatment carried out at the same time as diagnosis—was possible in 72% of women (174 of 242).
Partial or failed polyp removal occurred in 46 of 242 women (19%) in the clinic group, mostly because of pain issues, and in 18 of 233 women (7%) in the OR group (relative risk, 2.5; 95% confidence interval, 1.5−4.1; P<.001). Four uterine perforations (2% of patients) occurred in the OR group.
Mean pain scores were higher in the clinic group, and treatment was unacceptable for 2% of the women in each group.
The results of this trial show that clinic polypectomy has some limitations, but the outpatient procedure was deemed noninferior to polypectomy performed in the OR for the successful alleviation of uterine bleeding associated with uterine polyps.
What this EVIDENCE means for practice
Office-based polypectomy allowed a “see and treat” model in 72% of cases. Office polypectomy had similar successful therapeutic responses as inpatient polypectomy; however, over a 2-year follow-up period, women treated in the office were twice as likely to undergo at least 1 further polyp removal and were 1.6 times more likely to have further gynecologic surgery.
In-office hysteroscopic morcellation of polyps and myomas improves health-related quality of life
Rubino RJ, Lukes AS. Twelve-month outcomes for patients undergoing hysteroscopic morcellation of uterine polyps and myomas in an office or ambulatory surgical center. J Minim Invasive Gynecol. 2015;22(2):285–290.
Is it feasible to morcellate fibroids, as well as polyps, in the clinic? Rubino and colleagues investigated this question in a randomized, prospective clinical trial. They examined the efficacy of hysteroscopic removal of polyps and myomas on health-related quality of life and symptom severity at 1-year postprocedure. Women aged 18 to 55 years, with hysteroscopic and saline-infusion sonogram–assessed polyps and/or type 0 or I myomas (1.5−3.0 cm), were enrolled from 9 US clinical sites. Some patient populations were excluded, such as women with a long narcotic abuse history, current intrauterine device (IUD), type II submucous myomas, and type I fundal myomas.
A total of 118 pathologies were removed in 74 patients. Forty-two women were treated in the office setting; 32 were treated in the OR setting. Among the 118 pathologies removed, 53 were removed in the office (28 myomas and 25 polyps), and 55 were removed in the OR (14 myomas and 41 polyps).
The percentage of patients who reported being satisfied or highly satisfied was higher in the OR cohort (96.5%) compared with the office cohort (83.3%), although this difference was not statistically significant (P = .06). The percentage of patients who had 100% of their pathology removed was significantly higher in those with polyps compared with patients with myomas (96.0% vs 63.6%, respectively; P<.01).
These findings indicate that there were several cases in which the majority of a myoma was removed but a small residual portion remained. This disparity was especially pronounced in the office setting, where 96% of polyps were completely removed, compared with 52% of fibroids. There was no statistically significant difference in health-related quality of life between patients with complete removal and those with residual pathology, and there was no difference in satisfaction rates between patients who were treated in the office and those treated in the OR.
What this EVIDENCE means for practice
In general, office-based hysteroscopic myomectomy and polypectomy using morcellation for small- to medium-size lesions was associated with low rates of adverse events, high physician acceptance, and significant durable health-related quality-of-life improvements for up to 12 months post‑ procedure. Partial removal of myomas did not seem to be a significant factor in patients’ perceived outcomes.
Endometrial ablation for AUB costs less, has fewer complications at 1 year than hysterectomy
Miller JD, Lenhart GM, Bonafede MM, Lukes AS, Laughlin-Tommaso SK. Cost-effectiveness of global endometrial ablation vs hysterectomy for treatment of abnormal uterine bleeding: US commercial and Medicaid payer perspectives. Popul Health Manag. 2015;18(5):373–382.
Endometrial ablation often is performed in the office for AUB management. Miller and colleagues suggested that cost-effectiveness modeling studies of endometrial ablation for AUB treatment from a US perspective are lacking. They therefore designed a study to model the cost-effectiveness of endometrial ablation versus hysterectomy for treatment of AUB from both commercial and Medicaid payer perspectives.
They developed a decision-tree, state-transition (semi-Markov) model to simulate 2 hypothetical patient cohorts of women with AUB: one treated with endometrial ablation and the other with hysterectomy. Twenty-one health states were included in the model of intervention with endometrial ablation or hysterectomy; these comprised postablation reintervention with secondary ablation, tranexamic acid, or a levonorgestrel-containing IUD due to AUB, use of adjunctive pharmacotherapy following ablation, and a small probability of death from hysterectomy or actuarial death from all other causes.
The 1-year direct costs of endometrial ablation were $7,352 and $6,306 in the commercial payer and Medicaid payer perspectives, respectively; these were about half the costs of hysterectomy. The cost differential between the 2 treatments narrowed over time but, even at 5 years, endometrial ablation costs were still one-third less than hysterectomy costs.
In the first year, 35.6% of patients who had a hysterectomy and only 17.1% of patients undergoing ablation had complications. Short-term results were similar under the Medicaid perspective. By 5 years intervention/reintervention, however, complications of endometrial ablation were higher than those for hysterectomy by about 1.6%.
Over a 5-year time frame, direct costs of endometrial ablation were lower than those of hysterectomy from both the commercial payer and Medicaid perspectives. In the commercial payer analysis, the indirect costs of endometrial ablation were also lower than for hysterectomy, with 38.5 workdays lost for endometrial ablation compared with 55.3 days lost for hysterectomy, resulting in indirect costs of $8,976 versus $13,087.
What this EVIDENCE means for practice
Costs and cost-effectiveness of endometrial ablation from a US perspective are understudied. This model estimates a financial advantage for endometrial ablation over hysterectomy from both the commercial payer and Medicaid payer perspectives. Over a variety of time frames, endometrial ablation may save costs while reducing treatment complications and lost workdays. From the patient perspective, this model suggests better quality of life in the short term after endometrial ablation. It will be interesting to see whether longer term impacts show this model to be predictive.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Reference
- Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health-related quality of life, work impairment, and healthcare costs and utilization in abnormal uterine bleeding. Value Health. 2007;10(3):183–194.
How abnormal uterine bleeding (AUB) is managed has a significant impact on health care. In the United States, almost one-third of all gynecologic visits are related to AUB, with estimated annual direct costs of up to $1.55 billion and indirect costs as high as $36 billion.1 Not surprisingly, office-based procedures for AUB are being emphasized. While in the short term it is more cost efficient to perform surgery in the office rather than in the operating room, questions have arisen regarding the long-term efficacy and durability of in-office procedures. Insurers are undoubtedly raising these questions as well.
Notably, some ObGyns are early adopters of office-based surgery while others tend to adopt in-office procedures more slowly. As the literature for such procedures for AUB matures to provide more data on efficacy and acceptability, we will have a greater evidence base for understanding which procedures are more appropriate for the office. And while practice shifts sometimes occur due to cost-containment initiatives, some shifts are patient driven. Studies that address these driving variables, as well as efficacy considerations, are helpful. As we counsel women about procedures for AUB, the relative advantages and disadvantages of available treatment settings likely will become a greater part of that discussion so that they can make an informed decision.
In this Update, we discuss the results of 3 studies that examined various procedures and settings for AUB management:
- outpatient vs inpatient polypectomy
- hysteroscopic morcellation of polyps and myomas in an office vs ambulatory surgical center
- comparative costs of endometrial ablation and hysterectomy.
Outpatient vs inpatient polypectomy: Similar success rates in the short term
Cooper NA, Clark TJ, Middleton L, et al; OPT Trial Collaborative Group. Outpatient versus inpatient uterine polyp treatment for abnormal uterine bleeding: randomised controlled non-inferiority study. BMJ. 2015;350:h1398. doi:10.1136/bmj.h1398.
A collaborative group in the United Kingdom studied the common problem of endometrial polyps. Their objective was to evaluate whether outpatient polypectomy was as effective and well accepted as polypectomy performed in the operating room (OR).
Patients with a hysteroscopically diagnosed polyp were randomly assigned to hysteroscopic polyp removal in either a hysteroscopy clinic or an OR; polyp removal was performed using miniature mechanical or electrosurgical instruments. The primary outcome was successful treatment, determined by the participants’ assessment of their bleeding at 6 months.
Overall, 73% of women (166 of 228) in the clinic group and 80% (168 of 211) in the OR group reported a successful response to surgery at 6 months, with treatment effects being maintained at 12 and 24 months. A “see and treat” approach—that is, treatment carried out at the same time as diagnosis—was possible in 72% of women (174 of 242).
Partial or failed polyp removal occurred in 46 of 242 women (19%) in the clinic group, mostly because of pain issues, and in 18 of 233 women (7%) in the OR group (relative risk, 2.5; 95% confidence interval, 1.5−4.1; P<.001). Four uterine perforations (2% of patients) occurred in the OR group.
Mean pain scores were higher in the clinic group, and treatment was unacceptable for 2% of the women in each group.
The results of this trial show that clinic polypectomy has some limitations, but the outpatient procedure was deemed noninferior to polypectomy performed in the OR for the successful alleviation of uterine bleeding associated with uterine polyps.
What this EVIDENCE means for practice
Office-based polypectomy allowed a “see and treat” model in 72% of cases. Office polypectomy had similar successful therapeutic responses as inpatient polypectomy; however, over a 2-year follow-up period, women treated in the office were twice as likely to undergo at least 1 further polyp removal and were 1.6 times more likely to have further gynecologic surgery.
In-office hysteroscopic morcellation of polyps and myomas improves health-related quality of life
Rubino RJ, Lukes AS. Twelve-month outcomes for patients undergoing hysteroscopic morcellation of uterine polyps and myomas in an office or ambulatory surgical center. J Minim Invasive Gynecol. 2015;22(2):285–290.
Is it feasible to morcellate fibroids, as well as polyps, in the clinic? Rubino and colleagues investigated this question in a randomized, prospective clinical trial. They examined the efficacy of hysteroscopic removal of polyps and myomas on health-related quality of life and symptom severity at 1-year postprocedure. Women aged 18 to 55 years, with hysteroscopic and saline-infusion sonogram–assessed polyps and/or type 0 or I myomas (1.5−3.0 cm), were enrolled from 9 US clinical sites. Some patient populations were excluded, such as women with a long narcotic abuse history, current intrauterine device (IUD), type II submucous myomas, and type I fundal myomas.
A total of 118 pathologies were removed in 74 patients. Forty-two women were treated in the office setting; 32 were treated in the OR setting. Among the 118 pathologies removed, 53 were removed in the office (28 myomas and 25 polyps), and 55 were removed in the OR (14 myomas and 41 polyps).
The percentage of patients who reported being satisfied or highly satisfied was higher in the OR cohort (96.5%) compared with the office cohort (83.3%), although this difference was not statistically significant (P = .06). The percentage of patients who had 100% of their pathology removed was significantly higher in those with polyps compared with patients with myomas (96.0% vs 63.6%, respectively; P<.01).
These findings indicate that there were several cases in which the majority of a myoma was removed but a small residual portion remained. This disparity was especially pronounced in the office setting, where 96% of polyps were completely removed, compared with 52% of fibroids. There was no statistically significant difference in health-related quality of life between patients with complete removal and those with residual pathology, and there was no difference in satisfaction rates between patients who were treated in the office and those treated in the OR.
What this EVIDENCE means for practice
In general, office-based hysteroscopic myomectomy and polypectomy using morcellation for small- to medium-size lesions was associated with low rates of adverse events, high physician acceptance, and significant durable health-related quality-of-life improvements for up to 12 months post‑ procedure. Partial removal of myomas did not seem to be a significant factor in patients’ perceived outcomes.
Endometrial ablation for AUB costs less, has fewer complications at 1 year than hysterectomy
Miller JD, Lenhart GM, Bonafede MM, Lukes AS, Laughlin-Tommaso SK. Cost-effectiveness of global endometrial ablation vs hysterectomy for treatment of abnormal uterine bleeding: US commercial and Medicaid payer perspectives. Popul Health Manag. 2015;18(5):373–382.
Endometrial ablation often is performed in the office for AUB management. Miller and colleagues suggested that cost-effectiveness modeling studies of endometrial ablation for AUB treatment from a US perspective are lacking. They therefore designed a study to model the cost-effectiveness of endometrial ablation versus hysterectomy for treatment of AUB from both commercial and Medicaid payer perspectives.
They developed a decision-tree, state-transition (semi-Markov) model to simulate 2 hypothetical patient cohorts of women with AUB: one treated with endometrial ablation and the other with hysterectomy. Twenty-one health states were included in the model of intervention with endometrial ablation or hysterectomy; these comprised postablation reintervention with secondary ablation, tranexamic acid, or a levonorgestrel-containing IUD due to AUB, use of adjunctive pharmacotherapy following ablation, and a small probability of death from hysterectomy or actuarial death from all other causes.
The 1-year direct costs of endometrial ablation were $7,352 and $6,306 in the commercial payer and Medicaid payer perspectives, respectively; these were about half the costs of hysterectomy. The cost differential between the 2 treatments narrowed over time but, even at 5 years, endometrial ablation costs were still one-third less than hysterectomy costs.
In the first year, 35.6% of patients who had a hysterectomy and only 17.1% of patients undergoing ablation had complications. Short-term results were similar under the Medicaid perspective. By 5 years intervention/reintervention, however, complications of endometrial ablation were higher than those for hysterectomy by about 1.6%.
Over a 5-year time frame, direct costs of endometrial ablation were lower than those of hysterectomy from both the commercial payer and Medicaid perspectives. In the commercial payer analysis, the indirect costs of endometrial ablation were also lower than for hysterectomy, with 38.5 workdays lost for endometrial ablation compared with 55.3 days lost for hysterectomy, resulting in indirect costs of $8,976 versus $13,087.
What this EVIDENCE means for practice
Costs and cost-effectiveness of endometrial ablation from a US perspective are understudied. This model estimates a financial advantage for endometrial ablation over hysterectomy from both the commercial payer and Medicaid payer perspectives. Over a variety of time frames, endometrial ablation may save costs while reducing treatment complications and lost workdays. From the patient perspective, this model suggests better quality of life in the short term after endometrial ablation. It will be interesting to see whether longer term impacts show this model to be predictive.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
How abnormal uterine bleeding (AUB) is managed has a significant impact on health care. In the United States, almost one-third of all gynecologic visits are related to AUB, with estimated annual direct costs of up to $1.55 billion and indirect costs as high as $36 billion.1 Not surprisingly, office-based procedures for AUB are being emphasized. While in the short term it is more cost efficient to perform surgery in the office rather than in the operating room, questions have arisen regarding the long-term efficacy and durability of in-office procedures. Insurers are undoubtedly raising these questions as well.
Notably, some ObGyns are early adopters of office-based surgery while others tend to adopt in-office procedures more slowly. As the literature for such procedures for AUB matures to provide more data on efficacy and acceptability, we will have a greater evidence base for understanding which procedures are more appropriate for the office. And while practice shifts sometimes occur due to cost-containment initiatives, some shifts are patient driven. Studies that address these driving variables, as well as efficacy considerations, are helpful. As we counsel women about procedures for AUB, the relative advantages and disadvantages of available treatment settings likely will become a greater part of that discussion so that they can make an informed decision.
In this Update, we discuss the results of 3 studies that examined various procedures and settings for AUB management:
- outpatient vs inpatient polypectomy
- hysteroscopic morcellation of polyps and myomas in an office vs ambulatory surgical center
- comparative costs of endometrial ablation and hysterectomy.
Outpatient vs inpatient polypectomy: Similar success rates in the short term
Cooper NA, Clark TJ, Middleton L, et al; OPT Trial Collaborative Group. Outpatient versus inpatient uterine polyp treatment for abnormal uterine bleeding: randomised controlled non-inferiority study. BMJ. 2015;350:h1398. doi:10.1136/bmj.h1398.
A collaborative group in the United Kingdom studied the common problem of endometrial polyps. Their objective was to evaluate whether outpatient polypectomy was as effective and well accepted as polypectomy performed in the operating room (OR).
Patients with a hysteroscopically diagnosed polyp were randomly assigned to hysteroscopic polyp removal in either a hysteroscopy clinic or an OR; polyp removal was performed using miniature mechanical or electrosurgical instruments. The primary outcome was successful treatment, determined by the participants’ assessment of their bleeding at 6 months.
Overall, 73% of women (166 of 228) in the clinic group and 80% (168 of 211) in the OR group reported a successful response to surgery at 6 months, with treatment effects being maintained at 12 and 24 months. A “see and treat” approach—that is, treatment carried out at the same time as diagnosis—was possible in 72% of women (174 of 242).
Partial or failed polyp removal occurred in 46 of 242 women (19%) in the clinic group, mostly because of pain issues, and in 18 of 233 women (7%) in the OR group (relative risk, 2.5; 95% confidence interval, 1.5−4.1; P<.001). Four uterine perforations (2% of patients) occurred in the OR group.
Mean pain scores were higher in the clinic group, and treatment was unacceptable for 2% of the women in each group.
The results of this trial show that clinic polypectomy has some limitations, but the outpatient procedure was deemed noninferior to polypectomy performed in the OR for the successful alleviation of uterine bleeding associated with uterine polyps.
What this EVIDENCE means for practice
Office-based polypectomy allowed a “see and treat” model in 72% of cases. Office polypectomy had similar successful therapeutic responses as inpatient polypectomy; however, over a 2-year follow-up period, women treated in the office were twice as likely to undergo at least 1 further polyp removal and were 1.6 times more likely to have further gynecologic surgery.
In-office hysteroscopic morcellation of polyps and myomas improves health-related quality of life
Rubino RJ, Lukes AS. Twelve-month outcomes for patients undergoing hysteroscopic morcellation of uterine polyps and myomas in an office or ambulatory surgical center. J Minim Invasive Gynecol. 2015;22(2):285–290.
Is it feasible to morcellate fibroids, as well as polyps, in the clinic? Rubino and colleagues investigated this question in a randomized, prospective clinical trial. They examined the efficacy of hysteroscopic removal of polyps and myomas on health-related quality of life and symptom severity at 1-year postprocedure. Women aged 18 to 55 years, with hysteroscopic and saline-infusion sonogram–assessed polyps and/or type 0 or I myomas (1.5−3.0 cm), were enrolled from 9 US clinical sites. Some patient populations were excluded, such as women with a long narcotic abuse history, current intrauterine device (IUD), type II submucous myomas, and type I fundal myomas.
A total of 118 pathologies were removed in 74 patients. Forty-two women were treated in the office setting; 32 were treated in the OR setting. Among the 118 pathologies removed, 53 were removed in the office (28 myomas and 25 polyps), and 55 were removed in the OR (14 myomas and 41 polyps).
The percentage of patients who reported being satisfied or highly satisfied was higher in the OR cohort (96.5%) compared with the office cohort (83.3%), although this difference was not statistically significant (P = .06). The percentage of patients who had 100% of their pathology removed was significantly higher in those with polyps compared with patients with myomas (96.0% vs 63.6%, respectively; P<.01).
These findings indicate that there were several cases in which the majority of a myoma was removed but a small residual portion remained. This disparity was especially pronounced in the office setting, where 96% of polyps were completely removed, compared with 52% of fibroids. There was no statistically significant difference in health-related quality of life between patients with complete removal and those with residual pathology, and there was no difference in satisfaction rates between patients who were treated in the office and those treated in the OR.
What this EVIDENCE means for practice
In general, office-based hysteroscopic myomectomy and polypectomy using morcellation for small- to medium-size lesions was associated with low rates of adverse events, high physician acceptance, and significant durable health-related quality-of-life improvements for up to 12 months post‑ procedure. Partial removal of myomas did not seem to be a significant factor in patients’ perceived outcomes.
Endometrial ablation for AUB costs less, has fewer complications at 1 year than hysterectomy
Miller JD, Lenhart GM, Bonafede MM, Lukes AS, Laughlin-Tommaso SK. Cost-effectiveness of global endometrial ablation vs hysterectomy for treatment of abnormal uterine bleeding: US commercial and Medicaid payer perspectives. Popul Health Manag. 2015;18(5):373–382.
Endometrial ablation often is performed in the office for AUB management. Miller and colleagues suggested that cost-effectiveness modeling studies of endometrial ablation for AUB treatment from a US perspective are lacking. They therefore designed a study to model the cost-effectiveness of endometrial ablation versus hysterectomy for treatment of AUB from both commercial and Medicaid payer perspectives.
They developed a decision-tree, state-transition (semi-Markov) model to simulate 2 hypothetical patient cohorts of women with AUB: one treated with endometrial ablation and the other with hysterectomy. Twenty-one health states were included in the model of intervention with endometrial ablation or hysterectomy; these comprised postablation reintervention with secondary ablation, tranexamic acid, or a levonorgestrel-containing IUD due to AUB, use of adjunctive pharmacotherapy following ablation, and a small probability of death from hysterectomy or actuarial death from all other causes.
The 1-year direct costs of endometrial ablation were $7,352 and $6,306 in the commercial payer and Medicaid payer perspectives, respectively; these were about half the costs of hysterectomy. The cost differential between the 2 treatments narrowed over time but, even at 5 years, endometrial ablation costs were still one-third less than hysterectomy costs.
In the first year, 35.6% of patients who had a hysterectomy and only 17.1% of patients undergoing ablation had complications. Short-term results were similar under the Medicaid perspective. By 5 years intervention/reintervention, however, complications of endometrial ablation were higher than those for hysterectomy by about 1.6%.
Over a 5-year time frame, direct costs of endometrial ablation were lower than those of hysterectomy from both the commercial payer and Medicaid perspectives. In the commercial payer analysis, the indirect costs of endometrial ablation were also lower than for hysterectomy, with 38.5 workdays lost for endometrial ablation compared with 55.3 days lost for hysterectomy, resulting in indirect costs of $8,976 versus $13,087.
What this EVIDENCE means for practice
Costs and cost-effectiveness of endometrial ablation from a US perspective are understudied. This model estimates a financial advantage for endometrial ablation over hysterectomy from both the commercial payer and Medicaid payer perspectives. Over a variety of time frames, endometrial ablation may save costs while reducing treatment complications and lost workdays. From the patient perspective, this model suggests better quality of life in the short term after endometrial ablation. It will be interesting to see whether longer term impacts show this model to be predictive.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Reference
- Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health-related quality of life, work impairment, and healthcare costs and utilization in abnormal uterine bleeding. Value Health. 2007;10(3):183–194.
Reference
- Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health-related quality of life, work impairment, and healthcare costs and utilization in abnormal uterine bleeding. Value Health. 2007;10(3):183–194.
IN THIS ARTICLE
- Polypectomy in the clinic vs OR
- In-office polyp, fibroid morcellation
- Cost-effectiveness of endometrial ablation