User login
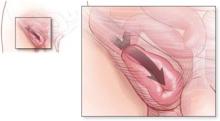
What is the risk of bowel strangulation in an adult with an untreated inguinal hernia?
The risk of bowel strangulation is estimated to be small—less than 1% per year (strength of recommendation [SOR]: B, based on small cohort studies with short follow-up). Experts recommend repair for patients with risk factors for poor outcomes after potential strangulation. These risk factors include advanced age, limited access to emergency care, significant concomitant illness, inability to recognize symptoms of bowel incarceration, and poor operative risk (American society of Anesthesiologists class III and IV) (SOR: C, based on expert opinion and case series). It is reasonable to offer elective surgery or watchful waiting to low-risk patients who understand the risks of strangulation (SOR: C, based on expert opinion and case series).
Watchful waiting, yes, but not for high-risk seniors
Michael K. Park, MD
University of Colorado Health Sciences Center, Rose Family Medicine Residency, Denver
The evidence reinforces “watchful waiting” as a reasonable management approach. However, certain patients—say, a 66-year-old diabetic farmer—should probably undergo elective herniorrhaphy to preempt the increased risk of complications with emergent repair.
shared decision-making is an essential process in accounting for individual preferences. In addition to knowing the risks of strangulation, patients opting for surgery also need to be aware of the differences between open and laparoscopic techniques. The former may be done under local anesthesia; the latter decreases postoperative pain and recovery time, but requires general anesthesia and increases the rates of serious complications.
Evidence summary
In 2 randomized controlled trials (RCTs) comparing elective repair of inguinal hernias with watchful waiting, the cohorts who made up the control groups experienced strangulation rates of 1.8 per thousand (0.18%) and 7.9 per thousand (0.79%) occurrences per patient-year.1,2 In the first of these 2 trials,1 with 364 control group patients, median follow-up was only 3.2 years (maximum 4.5 years), and by 4 years 31% of patients had crossed over to the treatment group for elective repair. The mean follow-up time in the second trial,2 which had 80 control group participants, was 1.6 years; 29% of patients eventually crossed over for repair.
Spanish study may have overestimated the risk. A retrospective study3 of 70 patients with incarcerated inguinal hernias presenting for emergency surgery in Northern Spain reported a cumulative 2.8% probability of strangulation at 3 months, rising to 4.5% after 2 years. This study did not include patients presenting for elective repair of hernias, and therefore it likely overestimated the rate of strangulation among patients in a primary care setting.
When to repair inguinal hernia
Experts recommend repair of an inguinal hernia in patients with risk factors for poor outcomes after potential strangulation. Risk factors include advanced age and significant concomitant illness.
In 2001, a prospective study4 of 669 patients presenting for elective hernia repair in London found that only 0.3% of patients required resection of bowel or omentum.
Risk appears to be <1% a year. Collectively, these studies suggest that the risk of strangulation is less than 1% per year (0.18% to 0.79%) among all patients with inguinal hernias, at least in the first few years of the onset of the hernia. As you’d expect, the risk of strangulation is higher (2.8% to 4.5%) among patients presenting for emergency repair of incarcerated hernias. We found no prospective studies that followed patients for more than 4.5 years.
Age factors into poor outcomes
A number of studies5,6 have examined risk factors for increased rates of strangulation and poor outcomes. Older age increases the risk of a poor outcome, peaking in the seventh decade. Patient comorbidity and late hospitalization also make emergent repair more risky.3,5
Retrospective studies3,5,7 of the temporal duration and the natural history of inguinal hernias, as well as operative complication rates, have shown conflicting results.
70- and 80-year olds have greater risk. A Turkish study5 of patients needing emergent surgical repair found morbidity to be significantly related to American Society of Anesthesiologists (ASA) class, with mortality rates of 3% and 14% for ASA class III and IV patients, respectively. This was a retrospective chart review that analyzed factors responsible for unfavorable outcomes; it found increased complications in hernia patients who had coexisting disease, hernias of longer duration, as well as higher ASA class. This study5 and another retrospective study6 found the need for emergent repair peaked for patients 70 to 80 years of age.
longer history of herniation may more postop complications. The Spanish retrospective review3 of emergent surgical repair of incarcerated hernias (noted earlier) reported a 3.4% postoperative mortality rate. All deaths were among patients over 65 years of age and ASA class III or IV. This review also found more postoperative complications and a higher mortality for hernias present for more than 10 years.
Another study raises questions. A retrospective study from Israel8 also showed that patients who underwent emergency repair were older, had a longer history of herniation than those undergoing elective repair, and had higher ASA scores. However, a case-control study7 and a chart review9 found that the risk of strangulation was higher for hernias of shorter duration.
We found no studies addressing potential exacerbating conditions of inguinal hernia, such as chronic cough, bladder outlet obstruction with straining, constipation, obesity, or bilateral hernias.
Recommendations from others
All the textbooks and guidelines we identified acknowledge that many patients forego operation and remain minimally symptomatic for long periods of time, and that operations themselves have risks and complications.10–12 The avoidable risks of strangulation and emergent operation lead most experts to favor operative treatment.
In ACS Surgery: Principles & Practice 2007,10 the authors lament the difficulty of obtaining accurate studies of the natural history of inguinal hernia because surgeons have been taught that it is best to operate at diagnosis, making it hard to find an adequate population to study. The authors acknowledge that while many primary care physicians advise their patients to delay operations if the hernia is minimally asymptomatic, they do not share this belief.
The American College of Physicians’ PIER: The Physicians’ Information and Education Resource11 recommends assessing the hernia and the patient on a case-by-case basis. They recommend deferring an operation for poor-risk patients with minimal symptoms if the hernia is easily reducible and is unquestionably an inguinal hernia, if there are no past episodes of obstruction, and if the risks of untreated hernia are fully understood by the patient. Sabiston Textbook of Surgery makes virtually the same points and recommendations.12
1. Fitzgibbons RJ, Giobbie-Hurder A, Gibbs JO, et al. watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomized clinical trial. JAMA 2006;295:285-292.
2. O’Dwyer PJ, Norrie J, Alani A, walker A, Duffy F, Horgan P. Observation or operation for patients with an asymptomatic inguinal hernia: A randomised clinical trial. Ann Surg 2006;244:167-173.
3. Alvarez JA, Baldonedo RF, Bear IG, Solis JAS, Alvarez A, Alvarez JI. Incarcerated groin hernias in adults: Presentation and outcome. Hernia 2004;8:121-126.
4. Hair A, Paterson C, Wright D, Baxter JN, O’Dwyer PJ. What effect does the duration of an inguinal hernia have on patient symptoms? J Am Coll Surg 2001;193:125-129.
5. Kulah B, Duzgun AP, Moran M, Kulacoglu IH, Ozmen MM, Coskun F. Emergency hernia repairs in elderly patients. Am J Surg 2001;182:455-459.
6. McEntee G, O’carroll A, Mooney B, Egan TJ, Delaney PV. Timing of strangulation in adult hernias. Br J Surg 1989;76:725-726.
7. Rai S, Chandra SS, Smile SR. A study of the risk of strangulation and obstruction in groin hernias. Aust N Z J Surg 1998;68:650-654.
8. Ohana manevwitch I, Weil R, et al. Inguinal hernia: challenging the traditional indication for surgery in asymptomatic patients. Hernia 2004;8:117-120.
9. Gallegos NC, Dawson J, Jarvis M, Hobsley M. Risk of strangulation in groin hernias. Br J Surg 1991;78:1171-1173.
10. Fitzgibbons RJ, Richards AT, Quinn TH. Open hernia repair. In: Souba WW, Wilmore DW, Fink MP, et al, eds.ACS Surgery: Principles and Practice 2007.New York, NY: webMD Professional Publishing; 2007. Available at: www.acssurgery.com. Accessed on June 22, 2007.
11. Kingsnorth AN, Khan JA. Hernia. In: PIER—The Physicians’ Information and Education Resource [database online]. Philadelphia, Pa: American College of Physicians; 2007.
12. Malangoni MA, Gagliardi RJ. Hernias. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 17th ed. Philadelphia, Pa: Saunders; 2004:1199–1217. Available at: www.mdconsult.com/das/book/0/view/1235/394.html. Accessed on November 8, 2007.
The risk of bowel strangulation is estimated to be small—less than 1% per year (strength of recommendation [SOR]: B, based on small cohort studies with short follow-up). Experts recommend repair for patients with risk factors for poor outcomes after potential strangulation. These risk factors include advanced age, limited access to emergency care, significant concomitant illness, inability to recognize symptoms of bowel incarceration, and poor operative risk (American society of Anesthesiologists class III and IV) (SOR: C, based on expert opinion and case series). It is reasonable to offer elective surgery or watchful waiting to low-risk patients who understand the risks of strangulation (SOR: C, based on expert opinion and case series).
Watchful waiting, yes, but not for high-risk seniors
Michael K. Park, MD
University of Colorado Health Sciences Center, Rose Family Medicine Residency, Denver
The evidence reinforces “watchful waiting” as a reasonable management approach. However, certain patients—say, a 66-year-old diabetic farmer—should probably undergo elective herniorrhaphy to preempt the increased risk of complications with emergent repair.
shared decision-making is an essential process in accounting for individual preferences. In addition to knowing the risks of strangulation, patients opting for surgery also need to be aware of the differences between open and laparoscopic techniques. The former may be done under local anesthesia; the latter decreases postoperative pain and recovery time, but requires general anesthesia and increases the rates of serious complications.
Evidence summary
In 2 randomized controlled trials (RCTs) comparing elective repair of inguinal hernias with watchful waiting, the cohorts who made up the control groups experienced strangulation rates of 1.8 per thousand (0.18%) and 7.9 per thousand (0.79%) occurrences per patient-year.1,2 In the first of these 2 trials,1 with 364 control group patients, median follow-up was only 3.2 years (maximum 4.5 years), and by 4 years 31% of patients had crossed over to the treatment group for elective repair. The mean follow-up time in the second trial,2 which had 80 control group participants, was 1.6 years; 29% of patients eventually crossed over for repair.
Spanish study may have overestimated the risk. A retrospective study3 of 70 patients with incarcerated inguinal hernias presenting for emergency surgery in Northern Spain reported a cumulative 2.8% probability of strangulation at 3 months, rising to 4.5% after 2 years. This study did not include patients presenting for elective repair of hernias, and therefore it likely overestimated the rate of strangulation among patients in a primary care setting.
When to repair inguinal hernia
Experts recommend repair of an inguinal hernia in patients with risk factors for poor outcomes after potential strangulation. Risk factors include advanced age and significant concomitant illness.
In 2001, a prospective study4 of 669 patients presenting for elective hernia repair in London found that only 0.3% of patients required resection of bowel or omentum.
Risk appears to be <1% a year. Collectively, these studies suggest that the risk of strangulation is less than 1% per year (0.18% to 0.79%) among all patients with inguinal hernias, at least in the first few years of the onset of the hernia. As you’d expect, the risk of strangulation is higher (2.8% to 4.5%) among patients presenting for emergency repair of incarcerated hernias. We found no prospective studies that followed patients for more than 4.5 years.
Age factors into poor outcomes
A number of studies5,6 have examined risk factors for increased rates of strangulation and poor outcomes. Older age increases the risk of a poor outcome, peaking in the seventh decade. Patient comorbidity and late hospitalization also make emergent repair more risky.3,5
Retrospective studies3,5,7 of the temporal duration and the natural history of inguinal hernias, as well as operative complication rates, have shown conflicting results.
70- and 80-year olds have greater risk. A Turkish study5 of patients needing emergent surgical repair found morbidity to be significantly related to American Society of Anesthesiologists (ASA) class, with mortality rates of 3% and 14% for ASA class III and IV patients, respectively. This was a retrospective chart review that analyzed factors responsible for unfavorable outcomes; it found increased complications in hernia patients who had coexisting disease, hernias of longer duration, as well as higher ASA class. This study5 and another retrospective study6 found the need for emergent repair peaked for patients 70 to 80 years of age.
longer history of herniation may more postop complications. The Spanish retrospective review3 of emergent surgical repair of incarcerated hernias (noted earlier) reported a 3.4% postoperative mortality rate. All deaths were among patients over 65 years of age and ASA class III or IV. This review also found more postoperative complications and a higher mortality for hernias present for more than 10 years.
Another study raises questions. A retrospective study from Israel8 also showed that patients who underwent emergency repair were older, had a longer history of herniation than those undergoing elective repair, and had higher ASA scores. However, a case-control study7 and a chart review9 found that the risk of strangulation was higher for hernias of shorter duration.
We found no studies addressing potential exacerbating conditions of inguinal hernia, such as chronic cough, bladder outlet obstruction with straining, constipation, obesity, or bilateral hernias.
Recommendations from others
All the textbooks and guidelines we identified acknowledge that many patients forego operation and remain minimally symptomatic for long periods of time, and that operations themselves have risks and complications.10–12 The avoidable risks of strangulation and emergent operation lead most experts to favor operative treatment.
In ACS Surgery: Principles & Practice 2007,10 the authors lament the difficulty of obtaining accurate studies of the natural history of inguinal hernia because surgeons have been taught that it is best to operate at diagnosis, making it hard to find an adequate population to study. The authors acknowledge that while many primary care physicians advise their patients to delay operations if the hernia is minimally asymptomatic, they do not share this belief.
The American College of Physicians’ PIER: The Physicians’ Information and Education Resource11 recommends assessing the hernia and the patient on a case-by-case basis. They recommend deferring an operation for poor-risk patients with minimal symptoms if the hernia is easily reducible and is unquestionably an inguinal hernia, if there are no past episodes of obstruction, and if the risks of untreated hernia are fully understood by the patient. Sabiston Textbook of Surgery makes virtually the same points and recommendations.12
The risk of bowel strangulation is estimated to be small—less than 1% per year (strength of recommendation [SOR]: B, based on small cohort studies with short follow-up). Experts recommend repair for patients with risk factors for poor outcomes after potential strangulation. These risk factors include advanced age, limited access to emergency care, significant concomitant illness, inability to recognize symptoms of bowel incarceration, and poor operative risk (American society of Anesthesiologists class III and IV) (SOR: C, based on expert opinion and case series). It is reasonable to offer elective surgery or watchful waiting to low-risk patients who understand the risks of strangulation (SOR: C, based on expert opinion and case series).
Watchful waiting, yes, but not for high-risk seniors
Michael K. Park, MD
University of Colorado Health Sciences Center, Rose Family Medicine Residency, Denver
The evidence reinforces “watchful waiting” as a reasonable management approach. However, certain patients—say, a 66-year-old diabetic farmer—should probably undergo elective herniorrhaphy to preempt the increased risk of complications with emergent repair.
shared decision-making is an essential process in accounting for individual preferences. In addition to knowing the risks of strangulation, patients opting for surgery also need to be aware of the differences between open and laparoscopic techniques. The former may be done under local anesthesia; the latter decreases postoperative pain and recovery time, but requires general anesthesia and increases the rates of serious complications.
Evidence summary
In 2 randomized controlled trials (RCTs) comparing elective repair of inguinal hernias with watchful waiting, the cohorts who made up the control groups experienced strangulation rates of 1.8 per thousand (0.18%) and 7.9 per thousand (0.79%) occurrences per patient-year.1,2 In the first of these 2 trials,1 with 364 control group patients, median follow-up was only 3.2 years (maximum 4.5 years), and by 4 years 31% of patients had crossed over to the treatment group for elective repair. The mean follow-up time in the second trial,2 which had 80 control group participants, was 1.6 years; 29% of patients eventually crossed over for repair.
Spanish study may have overestimated the risk. A retrospective study3 of 70 patients with incarcerated inguinal hernias presenting for emergency surgery in Northern Spain reported a cumulative 2.8% probability of strangulation at 3 months, rising to 4.5% after 2 years. This study did not include patients presenting for elective repair of hernias, and therefore it likely overestimated the rate of strangulation among patients in a primary care setting.
When to repair inguinal hernia
Experts recommend repair of an inguinal hernia in patients with risk factors for poor outcomes after potential strangulation. Risk factors include advanced age and significant concomitant illness.
In 2001, a prospective study4 of 669 patients presenting for elective hernia repair in London found that only 0.3% of patients required resection of bowel or omentum.
Risk appears to be <1% a year. Collectively, these studies suggest that the risk of strangulation is less than 1% per year (0.18% to 0.79%) among all patients with inguinal hernias, at least in the first few years of the onset of the hernia. As you’d expect, the risk of strangulation is higher (2.8% to 4.5%) among patients presenting for emergency repair of incarcerated hernias. We found no prospective studies that followed patients for more than 4.5 years.
Age factors into poor outcomes
A number of studies5,6 have examined risk factors for increased rates of strangulation and poor outcomes. Older age increases the risk of a poor outcome, peaking in the seventh decade. Patient comorbidity and late hospitalization also make emergent repair more risky.3,5
Retrospective studies3,5,7 of the temporal duration and the natural history of inguinal hernias, as well as operative complication rates, have shown conflicting results.
70- and 80-year olds have greater risk. A Turkish study5 of patients needing emergent surgical repair found morbidity to be significantly related to American Society of Anesthesiologists (ASA) class, with mortality rates of 3% and 14% for ASA class III and IV patients, respectively. This was a retrospective chart review that analyzed factors responsible for unfavorable outcomes; it found increased complications in hernia patients who had coexisting disease, hernias of longer duration, as well as higher ASA class. This study5 and another retrospective study6 found the need for emergent repair peaked for patients 70 to 80 years of age.
longer history of herniation may more postop complications. The Spanish retrospective review3 of emergent surgical repair of incarcerated hernias (noted earlier) reported a 3.4% postoperative mortality rate. All deaths were among patients over 65 years of age and ASA class III or IV. This review also found more postoperative complications and a higher mortality for hernias present for more than 10 years.
Another study raises questions. A retrospective study from Israel8 also showed that patients who underwent emergency repair were older, had a longer history of herniation than those undergoing elective repair, and had higher ASA scores. However, a case-control study7 and a chart review9 found that the risk of strangulation was higher for hernias of shorter duration.
We found no studies addressing potential exacerbating conditions of inguinal hernia, such as chronic cough, bladder outlet obstruction with straining, constipation, obesity, or bilateral hernias.
Recommendations from others
All the textbooks and guidelines we identified acknowledge that many patients forego operation and remain minimally symptomatic for long periods of time, and that operations themselves have risks and complications.10–12 The avoidable risks of strangulation and emergent operation lead most experts to favor operative treatment.
In ACS Surgery: Principles & Practice 2007,10 the authors lament the difficulty of obtaining accurate studies of the natural history of inguinal hernia because surgeons have been taught that it is best to operate at diagnosis, making it hard to find an adequate population to study. The authors acknowledge that while many primary care physicians advise their patients to delay operations if the hernia is minimally asymptomatic, they do not share this belief.
The American College of Physicians’ PIER: The Physicians’ Information and Education Resource11 recommends assessing the hernia and the patient on a case-by-case basis. They recommend deferring an operation for poor-risk patients with minimal symptoms if the hernia is easily reducible and is unquestionably an inguinal hernia, if there are no past episodes of obstruction, and if the risks of untreated hernia are fully understood by the patient. Sabiston Textbook of Surgery makes virtually the same points and recommendations.12
1. Fitzgibbons RJ, Giobbie-Hurder A, Gibbs JO, et al. watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomized clinical trial. JAMA 2006;295:285-292.
2. O’Dwyer PJ, Norrie J, Alani A, walker A, Duffy F, Horgan P. Observation or operation for patients with an asymptomatic inguinal hernia: A randomised clinical trial. Ann Surg 2006;244:167-173.
3. Alvarez JA, Baldonedo RF, Bear IG, Solis JAS, Alvarez A, Alvarez JI. Incarcerated groin hernias in adults: Presentation and outcome. Hernia 2004;8:121-126.
4. Hair A, Paterson C, Wright D, Baxter JN, O’Dwyer PJ. What effect does the duration of an inguinal hernia have on patient symptoms? J Am Coll Surg 2001;193:125-129.
5. Kulah B, Duzgun AP, Moran M, Kulacoglu IH, Ozmen MM, Coskun F. Emergency hernia repairs in elderly patients. Am J Surg 2001;182:455-459.
6. McEntee G, O’carroll A, Mooney B, Egan TJ, Delaney PV. Timing of strangulation in adult hernias. Br J Surg 1989;76:725-726.
7. Rai S, Chandra SS, Smile SR. A study of the risk of strangulation and obstruction in groin hernias. Aust N Z J Surg 1998;68:650-654.
8. Ohana manevwitch I, Weil R, et al. Inguinal hernia: challenging the traditional indication for surgery in asymptomatic patients. Hernia 2004;8:117-120.
9. Gallegos NC, Dawson J, Jarvis M, Hobsley M. Risk of strangulation in groin hernias. Br J Surg 1991;78:1171-1173.
10. Fitzgibbons RJ, Richards AT, Quinn TH. Open hernia repair. In: Souba WW, Wilmore DW, Fink MP, et al, eds.ACS Surgery: Principles and Practice 2007.New York, NY: webMD Professional Publishing; 2007. Available at: www.acssurgery.com. Accessed on June 22, 2007.
11. Kingsnorth AN, Khan JA. Hernia. In: PIER—The Physicians’ Information and Education Resource [database online]. Philadelphia, Pa: American College of Physicians; 2007.
12. Malangoni MA, Gagliardi RJ. Hernias. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 17th ed. Philadelphia, Pa: Saunders; 2004:1199–1217. Available at: www.mdconsult.com/das/book/0/view/1235/394.html. Accessed on November 8, 2007.
1. Fitzgibbons RJ, Giobbie-Hurder A, Gibbs JO, et al. watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomized clinical trial. JAMA 2006;295:285-292.
2. O’Dwyer PJ, Norrie J, Alani A, walker A, Duffy F, Horgan P. Observation or operation for patients with an asymptomatic inguinal hernia: A randomised clinical trial. Ann Surg 2006;244:167-173.
3. Alvarez JA, Baldonedo RF, Bear IG, Solis JAS, Alvarez A, Alvarez JI. Incarcerated groin hernias in adults: Presentation and outcome. Hernia 2004;8:121-126.
4. Hair A, Paterson C, Wright D, Baxter JN, O’Dwyer PJ. What effect does the duration of an inguinal hernia have on patient symptoms? J Am Coll Surg 2001;193:125-129.
5. Kulah B, Duzgun AP, Moran M, Kulacoglu IH, Ozmen MM, Coskun F. Emergency hernia repairs in elderly patients. Am J Surg 2001;182:455-459.
6. McEntee G, O’carroll A, Mooney B, Egan TJ, Delaney PV. Timing of strangulation in adult hernias. Br J Surg 1989;76:725-726.
7. Rai S, Chandra SS, Smile SR. A study of the risk of strangulation and obstruction in groin hernias. Aust N Z J Surg 1998;68:650-654.
8. Ohana manevwitch I, Weil R, et al. Inguinal hernia: challenging the traditional indication for surgery in asymptomatic patients. Hernia 2004;8:117-120.
9. Gallegos NC, Dawson J, Jarvis M, Hobsley M. Risk of strangulation in groin hernias. Br J Surg 1991;78:1171-1173.
10. Fitzgibbons RJ, Richards AT, Quinn TH. Open hernia repair. In: Souba WW, Wilmore DW, Fink MP, et al, eds.ACS Surgery: Principles and Practice 2007.New York, NY: webMD Professional Publishing; 2007. Available at: www.acssurgery.com. Accessed on June 22, 2007.
11. Kingsnorth AN, Khan JA. Hernia. In: PIER—The Physicians’ Information and Education Resource [database online]. Philadelphia, Pa: American College of Physicians; 2007.
12. Malangoni MA, Gagliardi RJ. Hernias. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 17th ed. Philadelphia, Pa: Saunders; 2004:1199–1217. Available at: www.mdconsult.com/das/book/0/view/1235/394.html. Accessed on November 8, 2007.
Evidence-based answers from the Family Physicians Inquiries Network