User login
Shared Medical Appointments for Glycemic Management in Rural Veterans
In 2005, the VA mandated shared medical appointments (SMAs) to improve clinic efficiency and quality of care. Both local and national Advanced Clinic Access meetings endorsed this method for decreasing wait times, improving patient outcome measures, and minimizing cost. Additionally, SMAs offer an opportunity to use nonphysician providers to their fullest potential. The VA has recognized the important role nonphysicians play in improving care for patients, especially patients with chronic illnesses, such as diabetes mellitus (DM).1
Based on the chronic care model, SMAs are patient medical appointments in which a multidisciplinary/multiexpertise team of providers sees a group of 8 to 20 patients in a 1.5- to 2-hour visit. Chronic illnesses, such as DM, are right for this approach.1
Diabetes mellitus is the leading cause of kidney failure, nontraumatic lower-limb amputations, and new cases of blindness among adults. It also is a major cause of heart disease and stroke, and the seventh leading cause of death in the U.S. The total cost of diagnosed DM in the U.S. in 2012 was $245 billion compared with $174 billion in 2007.2 Direct medical costs accounted for $176 billion, and $69 billion accounted for indirect costs, such as disability, work loss, and premature mortality.2 After adjusting for population age and sex differences, the average medical expenses among people diagnosed with DM were 2.3 times higher than medical expenses for those without DM. This figure does not include the cost of undiagnosed diabetes, prediabetes, or gestational diabetes.2
The purpose of this quality improvement study is to describe the results of SMA for management of DM conducted largely among rural veterans. The effectiveness of DM SMAs has been documented in several previous studies.3-10 However, this study focuses on using SMAs to manage veterans with DM in a rural environment.
Methods
The authors used the Primary Care Almanac (PCA) of the VHA Support Service Center to identify potential study participants at Lake City VAMC in Florida. The PCA is a database of VA primary care patients. The authors identified patients with hemoglobin A1c (HbA1c) level > 9% through the DM Cohort Reports Menu. Veterans with behavioral issues and those with high no-show rates were excluded.
The clinic staff called the eligible participants, educated them about SMA, and asked whether they would be interested in attending a DM SMA. If interested, they were scheduled for the next SMA. If uninterested, they were offered DM home telehealth follow-up, an appointment with the DM pharmacist, an appointment with the dietitian, enrollment into a DM education class, or routine follow-up with their primary care provider (PCP). Using this method, 18 patients were scheduled for the DM SMA between November 2010 and April 2013.
SMA Procedures
A physician or advanced registered nurse practitioner (ARNP) led each appointment, and in most cases other staff attended, including a clinical pharmacist, physical therapist (PT), kinesiotherapist (KT), dietician, social worker, registered nurse (RN), patient educator, and mental health provider. A pharmacist and RN attended all SMA appointments. The basic format consisted of a 90-minute appointment and included an abbreviated, clothed physical exam, which included vital signs; auscultation of heart, lungs, and abdomen; and foot exam. If a veteran had not received an eye exam within the year, an eye clinic consult was ordered. There were 10- to 30-minute blocks of time for the support staff who attended. The physician or ARNP usually led the appointment, and in addition to speaking to the group and discussing a daily topic, also spoke one-on-one with each veteran while support staff spoke to other group members.
During the appointment, the pharmacist answered questions and reviewed and adjusted medications as needed. The RN educator acted as a transcriptionist and answered questions. The PT/KT led interactive exercises. The dietitian answered questions, gave out educational materials, and did cooking demonstrations. The psychologist discussed behavioral health goals and asked each veteran to set a health goal to evaluate at the next meeting. The nursing staff in the primary care clinic checked in the patients. One nurse checked-in 1 to 2 patients and gave the patient a medication list.
Appointments were held every 2 to 3 months. All veterans attending were invited to come to the next appointment, and new patients were enrolled throughout the study. The new veterans were invited based on HbA1c readings pulled from the PCA database.
Hemoglobin A1c, blood pressure (BP), weight, and lipid level data were collected. Participation ended when HbA1c improved to < 8%, a patient was no longer interested, or after the patient did not show up for an appointment and did not call to cancel.
Results
Eighteen patients met the inclusion criteria (Table). Participants mean age was 62 years with most aged 50 to 70 years. Most participants were male (94%) and white (61%). Thirty-nine percent of the participants were African American. Twelve group appointments were held from November 2010 through April 2013. The mean enrollment per session was 5.8 patients (range 3-9). The median number of sessions each patient participated in was 3 (range 1 to 10).
SMA Outcomes
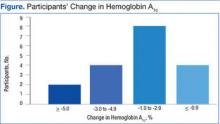
Among the 18 participants, the absolute change in HbA1c was -2.2% ± 2.0, representing a relative decrease in HbA1c of 18.2%. The study criterion for success was either a relative decrease of HbA1c by 13.5% or an absolute decrease in HbA1c of 1.5%. Of 18 patients participating in SMA, 14 (78%) patients achieved this goal. Of the 4 patients that were not successful, 2 patients had a relative HbA1c increase of 13% and 14%, respectively, 1 patient had no change at all, and 1 patient had a 9% relative decrease (Figure). Fourteen patients had improvement in their HbA1c after the first appointment, 2 patients had improvement after the second appointment, 1 patient had improvement after the fourth appointment, and 1 patient had no improvement.
In this population of rural veterans with poorly controlled diabetes, participation in SMAs was associated with marked improvement in measures of glucose control. Fourteen of the 18 (78%) veterans who participated in the DM SMA exhibited clinically significant decreases in HbA1c and achieved the defined goal.
Discussion
The effectiveness of DM SMAs has been documented in several previous studies. Sadur and colleagues found that a 6-month cluster visit group model of care for adults with DM improved glycemic control by 1.3% in the intervention subjects vs 0.2% in the control subjects in a randomized, controlled trial (RCT) with 185 participants.3 The intervention group received multidisciplinary outpatient diabetes management delivered by a diabetes nurse educator, a psychologist, a nutritionist, and a pharmacist in cluster visit settings of 10 to 18 patients per month for 6 months.
Metabolic Control
In another RCT trial of 112 patients, Trento and colleagues found that physician-led group consultations may improve metabolic control in the medium term by inducing more appropriate health behaviors.4 The consultations are feasible in everyday clinical practice without increasing working hours. After 2 years, HbA1c levels remained stable in patients seen in groups but had worsened in control subjects.
In a quasi-experiment with concurrent but nonrandomized controls, Kirsh and colleagues concluded that SMAs for DM constitute a practical system redesign that may help improve quality of care.5 Participants included 44 veterans from a VA primary care clinic who attended at least 1 physician-led SMA from April 2005 to September 2005 and from May 2006 to August 2006. Results showed levels of HbA1c, low-density lipoprotein cholesterol (LDL-C), and systolic BP (SBP) fell significantly postintervention with a mean decrease of HbA1c 1.4%, LDL-C 14.8 mg/dL, and SBP 16.0 mm Hg. The reductions in HbA1c and SBP were greater in the intervention group relative to the control group. The LDL-C reduction also was greater in the intervention group; however, the difference was not statistically significant.
Similarly, Sanchez concluded that patients who participated in a physician and nurse practitioner-led SMA using the diabetes self-management education (DSME) process had improvements in their HbA1c, self-management skills, and satisfaction.6 The study was considered a quality improvement project. Data were collected on 70 patients who were 96% Mexican American and received DSME via SMA during a 3-month span. The average HbA1c on visit 1 was 7.95%, 7.48% on visit 2, and 7.51% on visit 3. There were 34 patients with a decrease in HbA1c on visit 2 and 12 patients with a decrease in HbA1c on visit 3. Also, in a study on the effectiveness of SMAs in DM care, Guirguis and colleagues found that veterans showed an average decline in HbA1c whether they attended 1, 2, 3, or 4 SMAs.7 However, the decline was only statistically significant (P = .02) for those who had a baseline HbA1c > 9% prior to the study.
In contrast, other studies found no significant difference in improvement of DM patients in a SMA vs DM patients not in a SMA. Wagner and colleagues found periodic primary care sessions organized to meet the complex needs of diabetic patients improved the process of diabetes care and were associated with better outcomes.11 Primary care practices with a total of 700 patients were randomized within clinics to either a chronic care clinic (intervention) group or a usual care (control) group. Each chronic care clinic consisted of an assessment; individual visits with the primary care physician, nurse, and clinical pharmacist; and a group educational/peer support session. Although they found that the primary care group sessions improved the process of DM care and were associated with better outcomes, the mean HbA1c levels and cholesterol levels were comparable between the 2 groups.
In a 12-month RCT of 186 diabetic patients, Clancy and colleagues concluded physician and RN co-led group visits can improve the quality of care for diabetic patients, but modifications to the content and style of group visits may be necessary to achieve improved clinical outcomes.12 Results showed at both measurement points, HbA1c, BP, and lipid levels did not differ significantly for patients attending group visits vs those in usual care. Similarly, Edelman and colleaguesfound that provider-run group medical appointments are a potent strategy for improving BP but not HbA1c levels in DM patients in a RCT that compared a group medical appointment intervention with usual care among 239 primary care diabetic patients at the Durham VAMC in North Carolina and Hunter Holmes McGuire VAMC in Richmond, Virginia.10 Of note, the HbA1c levels in the group medical clinics did improve from 9.2% at baseline to a final of 8.3%, whereas the HbA1c level in the usual care group only improved from 9.2 to 8.6%.
Pharmacist-Led SMAs
In comparison to physician or nurse practitioner-led SMA, there also have been studies regarding pharmacist-led group medical appointments that have shown to be beneficial. Taveira and colleagues found that pharmacist-led group medical visits were feasible and efficacious for improving cardiac risk factors in patients with DM.8 This RCT with 118 VA patient participants showed a greater proportion of the intervention group vs the usual care alone group achieved a HbA1c of < 7%, and a SBP < 130 mm Hg.
In a separate study, Taveira and colleagues found that pharmacist-led group SMA visits are effective for glycemic control in patients with DM and depression without a change in depression symptoms.9 This RCT compared standard care and VA Multidisciplinary Education in Diabetes and Intervention for Cardiac Risk Reduction in Depression vs standard care alone in 88 depressed patients with DM with HbA1c > 6.5%. Also, Cohen and colleagues concluded that pharmacist-led group intervention program was an effective and sustainable collaborative care approach to managing DM and reducing associated cardiovascular risks.10 This study was a RCT that compared standard primary care alone to a 6-month pharmacist-led SMA program added to standard primary care. A total of 99 VA patients were included in the final analysis.
Other studies have looked at patient experiences involving SMAs. In a separate study, Cohen and colleagues explored the experiences of veterans who participated in SMAs.14 Veterans reported improvement in their overall health and well-being, improved self-management skills, and satisfaction with the SMA format.
Benefits to Veteran Patients
The SMA revealed the need for improved glycemic control in the participating patients. All the rural veteran patients included in the SMA had uncontrolled DM, which placed them at risk for many other health problems, such as renal failure, lower-limb amputations, blindness, cardiac disease, and stroke. In addition patients were given individual attention from several health care disciplines. Patients received one-on-one care from the physician or ARNP, nurse, pharmacist, dietitian, and psychologist in the same appointment. This arrangement benefited the patients in regard to their health, well-being, time, and money.
Limitations
Limitations of this study included its small sample size (18 patients), age of the patients, and the gender of patients. Patients average age was about 62 years, and most were aged in their 50s to 70s. Only 1 patient was in her 30s. Patients were predominantly male (17 men, 1 woman).
A second limitation was managing other PCP’s patients. It would be beneficial to see the outcomes of this same study if it were led by the patient’s PCP to find out whether the outcomes would be different regarding participation, no-show rates, and decrease in HbA1c.
A third limitation was the absence of information on time and resource use. Clinical staff members took time to prepare and participate in the SMA, and follow-up afterward. However, comparing the SMA with a regular PCP appointment in which an uncontrolled diabetic patient may be referred to diabetic education classes led by nurse educators and/or dietitians, to an individual nutritionist, to an individual clinical pharmacist, and to a behavioral therapist, the SMA may be a time and resource saver.
Conclusion
The study shows the practicality of implementing an effective SMA using a group interdisciplinary team approach to care for rural veterans with DM. The DM SMA may assist in improving quality of care and improve diabetic patients’ blood glucose. The SMA also may benefit patients who are nonadherent by educating them more thoroughly and letting them express themselves or share life experiences with fellow veterans who have the same diagnoses. Future studies are needed to determine the efficacy of DM SMAs especially with patients’ own PCPs.
1. Kirsh S, Watts S, Schaub K, et al. VA shared medical appointments for patients with diabetes: maximizing patient & provider expertise to strengthen care management. U.S. Department of Veterans Affairs website. http://www.queri.research.va.gov/tools/diabetes/shared-med-appt.pdf. Published December 2008. Accessed May 10, 2016.
2. American Diabetes Association. Statistics about diabetes. American Diabetes Association website. http://www.diabetes.org/diabetes-basics/diabetes-statistics. Updated April 1, 2016. Accessed May 14, 2016.
3. Sadur CN, Moline N, Costa M, et al. Diabetes management in a health maintenance organization. Efficacy of care management using cluster visits. Diabetes Care. 1999;22(12):2011-2017.
4. Trento M, Passera P, Tomalino M, et al. Group visits improve metabolic control in type 2 diabetes: a 2-year follow-up. Diabetes Care. 2001;24(6):995-1000.
5. Kirsh S, Watts S, Pascuzzi K, et al. Shared medical appointments based on the chronic care model: a quality improvement project to address the challenges of patients with diabetes with high cardiovascular risk. Qual Saf Health Care. 2007;16(5):349-353.
6. Sanchez I. Implementation of a diabetes self-management education program in primary care for adults using shared medical appointments. Diabetes Educ. 2011;37(3):381-391.
7. Guirguis AB, Lugovich J, Jay J, et al. Improving diabetes control using shared medical appointments. Am J Med. 2013;126(12):1043-1044.
8. Taveira TH, Friedmann PD, Cohen LB, et al. Pharmacist-led group medical appointment model in type 2 diabetes. Diabetes Educ. 2010;36(1):109-117.
9. Taveira TH, Dooley AG, Cohen LB, Khatana SA, Wu WC. Pharmacist-led group medical appointments for the management of type 2 diabetes with comorbid depression in older adults. Ann Pharmacother. 2011;45(11):1346-1355.
10. Cohen LB, Taveira TH, Khatana SA, Dooley AG, Pirraglia PA, Wu WC. Pharmacist-led shared medical appointments for multiple cardiovascular risk reduction in patients with type 2 diabetes. Diabetes Educ. 2011;37(6):801-812.
11. Wagner EH, Grothaus LC, Sandhu N, et al. Chronic care clinics for diabetes in primary care: a system-wide randomized trial. Diabetes Care. 2001;24(4):695-700.
12. Clancy DE, Huang P, Okonofua E, Yeager D, Magruder KM. Group visits: promoting adherence to diabetes guidelines. J Gen Intern Med. 2007;22(5):620-624.
13. Edelman D, Fredrickson SK, Melnyk SD, et al. Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Ann Intern Med. 2010;152(11):689-696.
14. Cohen S, Hartley S, Mavi J, Vest B, Wilson M. Veteran experiences related to participation in shared medical appointments. Mil Med. 2012;177(11):1287-1292.
In 2005, the VA mandated shared medical appointments (SMAs) to improve clinic efficiency and quality of care. Both local and national Advanced Clinic Access meetings endorsed this method for decreasing wait times, improving patient outcome measures, and minimizing cost. Additionally, SMAs offer an opportunity to use nonphysician providers to their fullest potential. The VA has recognized the important role nonphysicians play in improving care for patients, especially patients with chronic illnesses, such as diabetes mellitus (DM).1
Based on the chronic care model, SMAs are patient medical appointments in which a multidisciplinary/multiexpertise team of providers sees a group of 8 to 20 patients in a 1.5- to 2-hour visit. Chronic illnesses, such as DM, are right for this approach.1
Diabetes mellitus is the leading cause of kidney failure, nontraumatic lower-limb amputations, and new cases of blindness among adults. It also is a major cause of heart disease and stroke, and the seventh leading cause of death in the U.S. The total cost of diagnosed DM in the U.S. in 2012 was $245 billion compared with $174 billion in 2007.2 Direct medical costs accounted for $176 billion, and $69 billion accounted for indirect costs, such as disability, work loss, and premature mortality.2 After adjusting for population age and sex differences, the average medical expenses among people diagnosed with DM were 2.3 times higher than medical expenses for those without DM. This figure does not include the cost of undiagnosed diabetes, prediabetes, or gestational diabetes.2
The purpose of this quality improvement study is to describe the results of SMA for management of DM conducted largely among rural veterans. The effectiveness of DM SMAs has been documented in several previous studies.3-10 However, this study focuses on using SMAs to manage veterans with DM in a rural environment.
Methods
The authors used the Primary Care Almanac (PCA) of the VHA Support Service Center to identify potential study participants at Lake City VAMC in Florida. The PCA is a database of VA primary care patients. The authors identified patients with hemoglobin A1c (HbA1c) level > 9% through the DM Cohort Reports Menu. Veterans with behavioral issues and those with high no-show rates were excluded.
The clinic staff called the eligible participants, educated them about SMA, and asked whether they would be interested in attending a DM SMA. If interested, they were scheduled for the next SMA. If uninterested, they were offered DM home telehealth follow-up, an appointment with the DM pharmacist, an appointment with the dietitian, enrollment into a DM education class, or routine follow-up with their primary care provider (PCP). Using this method, 18 patients were scheduled for the DM SMA between November 2010 and April 2013.
SMA Procedures
A physician or advanced registered nurse practitioner (ARNP) led each appointment, and in most cases other staff attended, including a clinical pharmacist, physical therapist (PT), kinesiotherapist (KT), dietician, social worker, registered nurse (RN), patient educator, and mental health provider. A pharmacist and RN attended all SMA appointments. The basic format consisted of a 90-minute appointment and included an abbreviated, clothed physical exam, which included vital signs; auscultation of heart, lungs, and abdomen; and foot exam. If a veteran had not received an eye exam within the year, an eye clinic consult was ordered. There were 10- to 30-minute blocks of time for the support staff who attended. The physician or ARNP usually led the appointment, and in addition to speaking to the group and discussing a daily topic, also spoke one-on-one with each veteran while support staff spoke to other group members.
During the appointment, the pharmacist answered questions and reviewed and adjusted medications as needed. The RN educator acted as a transcriptionist and answered questions. The PT/KT led interactive exercises. The dietitian answered questions, gave out educational materials, and did cooking demonstrations. The psychologist discussed behavioral health goals and asked each veteran to set a health goal to evaluate at the next meeting. The nursing staff in the primary care clinic checked in the patients. One nurse checked-in 1 to 2 patients and gave the patient a medication list.
Appointments were held every 2 to 3 months. All veterans attending were invited to come to the next appointment, and new patients were enrolled throughout the study. The new veterans were invited based on HbA1c readings pulled from the PCA database.
Hemoglobin A1c, blood pressure (BP), weight, and lipid level data were collected. Participation ended when HbA1c improved to < 8%, a patient was no longer interested, or after the patient did not show up for an appointment and did not call to cancel.
Results
Eighteen patients met the inclusion criteria (Table). Participants mean age was 62 years with most aged 50 to 70 years. Most participants were male (94%) and white (61%). Thirty-nine percent of the participants were African American. Twelve group appointments were held from November 2010 through April 2013. The mean enrollment per session was 5.8 patients (range 3-9). The median number of sessions each patient participated in was 3 (range 1 to 10).
SMA Outcomes
Among the 18 participants, the absolute change in HbA1c was -2.2% ± 2.0, representing a relative decrease in HbA1c of 18.2%. The study criterion for success was either a relative decrease of HbA1c by 13.5% or an absolute decrease in HbA1c of 1.5%. Of 18 patients participating in SMA, 14 (78%) patients achieved this goal. Of the 4 patients that were not successful, 2 patients had a relative HbA1c increase of 13% and 14%, respectively, 1 patient had no change at all, and 1 patient had a 9% relative decrease (Figure). Fourteen patients had improvement in their HbA1c after the first appointment, 2 patients had improvement after the second appointment, 1 patient had improvement after the fourth appointment, and 1 patient had no improvement.
In this population of rural veterans with poorly controlled diabetes, participation in SMAs was associated with marked improvement in measures of glucose control. Fourteen of the 18 (78%) veterans who participated in the DM SMA exhibited clinically significant decreases in HbA1c and achieved the defined goal.
Discussion
The effectiveness of DM SMAs has been documented in several previous studies. Sadur and colleagues found that a 6-month cluster visit group model of care for adults with DM improved glycemic control by 1.3% in the intervention subjects vs 0.2% in the control subjects in a randomized, controlled trial (RCT) with 185 participants.3 The intervention group received multidisciplinary outpatient diabetes management delivered by a diabetes nurse educator, a psychologist, a nutritionist, and a pharmacist in cluster visit settings of 10 to 18 patients per month for 6 months.
Metabolic Control
In another RCT trial of 112 patients, Trento and colleagues found that physician-led group consultations may improve metabolic control in the medium term by inducing more appropriate health behaviors.4 The consultations are feasible in everyday clinical practice without increasing working hours. After 2 years, HbA1c levels remained stable in patients seen in groups but had worsened in control subjects.
In a quasi-experiment with concurrent but nonrandomized controls, Kirsh and colleagues concluded that SMAs for DM constitute a practical system redesign that may help improve quality of care.5 Participants included 44 veterans from a VA primary care clinic who attended at least 1 physician-led SMA from April 2005 to September 2005 and from May 2006 to August 2006. Results showed levels of HbA1c, low-density lipoprotein cholesterol (LDL-C), and systolic BP (SBP) fell significantly postintervention with a mean decrease of HbA1c 1.4%, LDL-C 14.8 mg/dL, and SBP 16.0 mm Hg. The reductions in HbA1c and SBP were greater in the intervention group relative to the control group. The LDL-C reduction also was greater in the intervention group; however, the difference was not statistically significant.
Similarly, Sanchez concluded that patients who participated in a physician and nurse practitioner-led SMA using the diabetes self-management education (DSME) process had improvements in their HbA1c, self-management skills, and satisfaction.6 The study was considered a quality improvement project. Data were collected on 70 patients who were 96% Mexican American and received DSME via SMA during a 3-month span. The average HbA1c on visit 1 was 7.95%, 7.48% on visit 2, and 7.51% on visit 3. There were 34 patients with a decrease in HbA1c on visit 2 and 12 patients with a decrease in HbA1c on visit 3. Also, in a study on the effectiveness of SMAs in DM care, Guirguis and colleagues found that veterans showed an average decline in HbA1c whether they attended 1, 2, 3, or 4 SMAs.7 However, the decline was only statistically significant (P = .02) for those who had a baseline HbA1c > 9% prior to the study.
In contrast, other studies found no significant difference in improvement of DM patients in a SMA vs DM patients not in a SMA. Wagner and colleagues found periodic primary care sessions organized to meet the complex needs of diabetic patients improved the process of diabetes care and were associated with better outcomes.11 Primary care practices with a total of 700 patients were randomized within clinics to either a chronic care clinic (intervention) group or a usual care (control) group. Each chronic care clinic consisted of an assessment; individual visits with the primary care physician, nurse, and clinical pharmacist; and a group educational/peer support session. Although they found that the primary care group sessions improved the process of DM care and were associated with better outcomes, the mean HbA1c levels and cholesterol levels were comparable between the 2 groups.
In a 12-month RCT of 186 diabetic patients, Clancy and colleagues concluded physician and RN co-led group visits can improve the quality of care for diabetic patients, but modifications to the content and style of group visits may be necessary to achieve improved clinical outcomes.12 Results showed at both measurement points, HbA1c, BP, and lipid levels did not differ significantly for patients attending group visits vs those in usual care. Similarly, Edelman and colleaguesfound that provider-run group medical appointments are a potent strategy for improving BP but not HbA1c levels in DM patients in a RCT that compared a group medical appointment intervention with usual care among 239 primary care diabetic patients at the Durham VAMC in North Carolina and Hunter Holmes McGuire VAMC in Richmond, Virginia.10 Of note, the HbA1c levels in the group medical clinics did improve from 9.2% at baseline to a final of 8.3%, whereas the HbA1c level in the usual care group only improved from 9.2 to 8.6%.
Pharmacist-Led SMAs
In comparison to physician or nurse practitioner-led SMA, there also have been studies regarding pharmacist-led group medical appointments that have shown to be beneficial. Taveira and colleagues found that pharmacist-led group medical visits were feasible and efficacious for improving cardiac risk factors in patients with DM.8 This RCT with 118 VA patient participants showed a greater proportion of the intervention group vs the usual care alone group achieved a HbA1c of < 7%, and a SBP < 130 mm Hg.
In a separate study, Taveira and colleagues found that pharmacist-led group SMA visits are effective for glycemic control in patients with DM and depression without a change in depression symptoms.9 This RCT compared standard care and VA Multidisciplinary Education in Diabetes and Intervention for Cardiac Risk Reduction in Depression vs standard care alone in 88 depressed patients with DM with HbA1c > 6.5%. Also, Cohen and colleagues concluded that pharmacist-led group intervention program was an effective and sustainable collaborative care approach to managing DM and reducing associated cardiovascular risks.10 This study was a RCT that compared standard primary care alone to a 6-month pharmacist-led SMA program added to standard primary care. A total of 99 VA patients were included in the final analysis.
Other studies have looked at patient experiences involving SMAs. In a separate study, Cohen and colleagues explored the experiences of veterans who participated in SMAs.14 Veterans reported improvement in their overall health and well-being, improved self-management skills, and satisfaction with the SMA format.
Benefits to Veteran Patients
The SMA revealed the need for improved glycemic control in the participating patients. All the rural veteran patients included in the SMA had uncontrolled DM, which placed them at risk for many other health problems, such as renal failure, lower-limb amputations, blindness, cardiac disease, and stroke. In addition patients were given individual attention from several health care disciplines. Patients received one-on-one care from the physician or ARNP, nurse, pharmacist, dietitian, and psychologist in the same appointment. This arrangement benefited the patients in regard to their health, well-being, time, and money.
Limitations
Limitations of this study included its small sample size (18 patients), age of the patients, and the gender of patients. Patients average age was about 62 years, and most were aged in their 50s to 70s. Only 1 patient was in her 30s. Patients were predominantly male (17 men, 1 woman).
A second limitation was managing other PCP’s patients. It would be beneficial to see the outcomes of this same study if it were led by the patient’s PCP to find out whether the outcomes would be different regarding participation, no-show rates, and decrease in HbA1c.
A third limitation was the absence of information on time and resource use. Clinical staff members took time to prepare and participate in the SMA, and follow-up afterward. However, comparing the SMA with a regular PCP appointment in which an uncontrolled diabetic patient may be referred to diabetic education classes led by nurse educators and/or dietitians, to an individual nutritionist, to an individual clinical pharmacist, and to a behavioral therapist, the SMA may be a time and resource saver.
Conclusion
The study shows the practicality of implementing an effective SMA using a group interdisciplinary team approach to care for rural veterans with DM. The DM SMA may assist in improving quality of care and improve diabetic patients’ blood glucose. The SMA also may benefit patients who are nonadherent by educating them more thoroughly and letting them express themselves or share life experiences with fellow veterans who have the same diagnoses. Future studies are needed to determine the efficacy of DM SMAs especially with patients’ own PCPs.
In 2005, the VA mandated shared medical appointments (SMAs) to improve clinic efficiency and quality of care. Both local and national Advanced Clinic Access meetings endorsed this method for decreasing wait times, improving patient outcome measures, and minimizing cost. Additionally, SMAs offer an opportunity to use nonphysician providers to their fullest potential. The VA has recognized the important role nonphysicians play in improving care for patients, especially patients with chronic illnesses, such as diabetes mellitus (DM).1
Based on the chronic care model, SMAs are patient medical appointments in which a multidisciplinary/multiexpertise team of providers sees a group of 8 to 20 patients in a 1.5- to 2-hour visit. Chronic illnesses, such as DM, are right for this approach.1
Diabetes mellitus is the leading cause of kidney failure, nontraumatic lower-limb amputations, and new cases of blindness among adults. It also is a major cause of heart disease and stroke, and the seventh leading cause of death in the U.S. The total cost of diagnosed DM in the U.S. in 2012 was $245 billion compared with $174 billion in 2007.2 Direct medical costs accounted for $176 billion, and $69 billion accounted for indirect costs, such as disability, work loss, and premature mortality.2 After adjusting for population age and sex differences, the average medical expenses among people diagnosed with DM were 2.3 times higher than medical expenses for those without DM. This figure does not include the cost of undiagnosed diabetes, prediabetes, or gestational diabetes.2
The purpose of this quality improvement study is to describe the results of SMA for management of DM conducted largely among rural veterans. The effectiveness of DM SMAs has been documented in several previous studies.3-10 However, this study focuses on using SMAs to manage veterans with DM in a rural environment.
Methods
The authors used the Primary Care Almanac (PCA) of the VHA Support Service Center to identify potential study participants at Lake City VAMC in Florida. The PCA is a database of VA primary care patients. The authors identified patients with hemoglobin A1c (HbA1c) level > 9% through the DM Cohort Reports Menu. Veterans with behavioral issues and those with high no-show rates were excluded.
The clinic staff called the eligible participants, educated them about SMA, and asked whether they would be interested in attending a DM SMA. If interested, they were scheduled for the next SMA. If uninterested, they were offered DM home telehealth follow-up, an appointment with the DM pharmacist, an appointment with the dietitian, enrollment into a DM education class, or routine follow-up with their primary care provider (PCP). Using this method, 18 patients were scheduled for the DM SMA between November 2010 and April 2013.
SMA Procedures
A physician or advanced registered nurse practitioner (ARNP) led each appointment, and in most cases other staff attended, including a clinical pharmacist, physical therapist (PT), kinesiotherapist (KT), dietician, social worker, registered nurse (RN), patient educator, and mental health provider. A pharmacist and RN attended all SMA appointments. The basic format consisted of a 90-minute appointment and included an abbreviated, clothed physical exam, which included vital signs; auscultation of heart, lungs, and abdomen; and foot exam. If a veteran had not received an eye exam within the year, an eye clinic consult was ordered. There were 10- to 30-minute blocks of time for the support staff who attended. The physician or ARNP usually led the appointment, and in addition to speaking to the group and discussing a daily topic, also spoke one-on-one with each veteran while support staff spoke to other group members.
During the appointment, the pharmacist answered questions and reviewed and adjusted medications as needed. The RN educator acted as a transcriptionist and answered questions. The PT/KT led interactive exercises. The dietitian answered questions, gave out educational materials, and did cooking demonstrations. The psychologist discussed behavioral health goals and asked each veteran to set a health goal to evaluate at the next meeting. The nursing staff in the primary care clinic checked in the patients. One nurse checked-in 1 to 2 patients and gave the patient a medication list.
Appointments were held every 2 to 3 months. All veterans attending were invited to come to the next appointment, and new patients were enrolled throughout the study. The new veterans were invited based on HbA1c readings pulled from the PCA database.
Hemoglobin A1c, blood pressure (BP), weight, and lipid level data were collected. Participation ended when HbA1c improved to < 8%, a patient was no longer interested, or after the patient did not show up for an appointment and did not call to cancel.
Results
Eighteen patients met the inclusion criteria (Table). Participants mean age was 62 years with most aged 50 to 70 years. Most participants were male (94%) and white (61%). Thirty-nine percent of the participants were African American. Twelve group appointments were held from November 2010 through April 2013. The mean enrollment per session was 5.8 patients (range 3-9). The median number of sessions each patient participated in was 3 (range 1 to 10).
SMA Outcomes
Among the 18 participants, the absolute change in HbA1c was -2.2% ± 2.0, representing a relative decrease in HbA1c of 18.2%. The study criterion for success was either a relative decrease of HbA1c by 13.5% or an absolute decrease in HbA1c of 1.5%. Of 18 patients participating in SMA, 14 (78%) patients achieved this goal. Of the 4 patients that were not successful, 2 patients had a relative HbA1c increase of 13% and 14%, respectively, 1 patient had no change at all, and 1 patient had a 9% relative decrease (Figure). Fourteen patients had improvement in their HbA1c after the first appointment, 2 patients had improvement after the second appointment, 1 patient had improvement after the fourth appointment, and 1 patient had no improvement.
In this population of rural veterans with poorly controlled diabetes, participation in SMAs was associated with marked improvement in measures of glucose control. Fourteen of the 18 (78%) veterans who participated in the DM SMA exhibited clinically significant decreases in HbA1c and achieved the defined goal.
Discussion
The effectiveness of DM SMAs has been documented in several previous studies. Sadur and colleagues found that a 6-month cluster visit group model of care for adults with DM improved glycemic control by 1.3% in the intervention subjects vs 0.2% in the control subjects in a randomized, controlled trial (RCT) with 185 participants.3 The intervention group received multidisciplinary outpatient diabetes management delivered by a diabetes nurse educator, a psychologist, a nutritionist, and a pharmacist in cluster visit settings of 10 to 18 patients per month for 6 months.
Metabolic Control
In another RCT trial of 112 patients, Trento and colleagues found that physician-led group consultations may improve metabolic control in the medium term by inducing more appropriate health behaviors.4 The consultations are feasible in everyday clinical practice without increasing working hours. After 2 years, HbA1c levels remained stable in patients seen in groups but had worsened in control subjects.
In a quasi-experiment with concurrent but nonrandomized controls, Kirsh and colleagues concluded that SMAs for DM constitute a practical system redesign that may help improve quality of care.5 Participants included 44 veterans from a VA primary care clinic who attended at least 1 physician-led SMA from April 2005 to September 2005 and from May 2006 to August 2006. Results showed levels of HbA1c, low-density lipoprotein cholesterol (LDL-C), and systolic BP (SBP) fell significantly postintervention with a mean decrease of HbA1c 1.4%, LDL-C 14.8 mg/dL, and SBP 16.0 mm Hg. The reductions in HbA1c and SBP were greater in the intervention group relative to the control group. The LDL-C reduction also was greater in the intervention group; however, the difference was not statistically significant.
Similarly, Sanchez concluded that patients who participated in a physician and nurse practitioner-led SMA using the diabetes self-management education (DSME) process had improvements in their HbA1c, self-management skills, and satisfaction.6 The study was considered a quality improvement project. Data were collected on 70 patients who were 96% Mexican American and received DSME via SMA during a 3-month span. The average HbA1c on visit 1 was 7.95%, 7.48% on visit 2, and 7.51% on visit 3. There were 34 patients with a decrease in HbA1c on visit 2 and 12 patients with a decrease in HbA1c on visit 3. Also, in a study on the effectiveness of SMAs in DM care, Guirguis and colleagues found that veterans showed an average decline in HbA1c whether they attended 1, 2, 3, or 4 SMAs.7 However, the decline was only statistically significant (P = .02) for those who had a baseline HbA1c > 9% prior to the study.
In contrast, other studies found no significant difference in improvement of DM patients in a SMA vs DM patients not in a SMA. Wagner and colleagues found periodic primary care sessions organized to meet the complex needs of diabetic patients improved the process of diabetes care and were associated with better outcomes.11 Primary care practices with a total of 700 patients were randomized within clinics to either a chronic care clinic (intervention) group or a usual care (control) group. Each chronic care clinic consisted of an assessment; individual visits with the primary care physician, nurse, and clinical pharmacist; and a group educational/peer support session. Although they found that the primary care group sessions improved the process of DM care and were associated with better outcomes, the mean HbA1c levels and cholesterol levels were comparable between the 2 groups.
In a 12-month RCT of 186 diabetic patients, Clancy and colleagues concluded physician and RN co-led group visits can improve the quality of care for diabetic patients, but modifications to the content and style of group visits may be necessary to achieve improved clinical outcomes.12 Results showed at both measurement points, HbA1c, BP, and lipid levels did not differ significantly for patients attending group visits vs those in usual care. Similarly, Edelman and colleaguesfound that provider-run group medical appointments are a potent strategy for improving BP but not HbA1c levels in DM patients in a RCT that compared a group medical appointment intervention with usual care among 239 primary care diabetic patients at the Durham VAMC in North Carolina and Hunter Holmes McGuire VAMC in Richmond, Virginia.10 Of note, the HbA1c levels in the group medical clinics did improve from 9.2% at baseline to a final of 8.3%, whereas the HbA1c level in the usual care group only improved from 9.2 to 8.6%.
Pharmacist-Led SMAs
In comparison to physician or nurse practitioner-led SMA, there also have been studies regarding pharmacist-led group medical appointments that have shown to be beneficial. Taveira and colleagues found that pharmacist-led group medical visits were feasible and efficacious for improving cardiac risk factors in patients with DM.8 This RCT with 118 VA patient participants showed a greater proportion of the intervention group vs the usual care alone group achieved a HbA1c of < 7%, and a SBP < 130 mm Hg.
In a separate study, Taveira and colleagues found that pharmacist-led group SMA visits are effective for glycemic control in patients with DM and depression without a change in depression symptoms.9 This RCT compared standard care and VA Multidisciplinary Education in Diabetes and Intervention for Cardiac Risk Reduction in Depression vs standard care alone in 88 depressed patients with DM with HbA1c > 6.5%. Also, Cohen and colleagues concluded that pharmacist-led group intervention program was an effective and sustainable collaborative care approach to managing DM and reducing associated cardiovascular risks.10 This study was a RCT that compared standard primary care alone to a 6-month pharmacist-led SMA program added to standard primary care. A total of 99 VA patients were included in the final analysis.
Other studies have looked at patient experiences involving SMAs. In a separate study, Cohen and colleagues explored the experiences of veterans who participated in SMAs.14 Veterans reported improvement in their overall health and well-being, improved self-management skills, and satisfaction with the SMA format.
Benefits to Veteran Patients
The SMA revealed the need for improved glycemic control in the participating patients. All the rural veteran patients included in the SMA had uncontrolled DM, which placed them at risk for many other health problems, such as renal failure, lower-limb amputations, blindness, cardiac disease, and stroke. In addition patients were given individual attention from several health care disciplines. Patients received one-on-one care from the physician or ARNP, nurse, pharmacist, dietitian, and psychologist in the same appointment. This arrangement benefited the patients in regard to their health, well-being, time, and money.
Limitations
Limitations of this study included its small sample size (18 patients), age of the patients, and the gender of patients. Patients average age was about 62 years, and most were aged in their 50s to 70s. Only 1 patient was in her 30s. Patients were predominantly male (17 men, 1 woman).
A second limitation was managing other PCP’s patients. It would be beneficial to see the outcomes of this same study if it were led by the patient’s PCP to find out whether the outcomes would be different regarding participation, no-show rates, and decrease in HbA1c.
A third limitation was the absence of information on time and resource use. Clinical staff members took time to prepare and participate in the SMA, and follow-up afterward. However, comparing the SMA with a regular PCP appointment in which an uncontrolled diabetic patient may be referred to diabetic education classes led by nurse educators and/or dietitians, to an individual nutritionist, to an individual clinical pharmacist, and to a behavioral therapist, the SMA may be a time and resource saver.
Conclusion
The study shows the practicality of implementing an effective SMA using a group interdisciplinary team approach to care for rural veterans with DM. The DM SMA may assist in improving quality of care and improve diabetic patients’ blood glucose. The SMA also may benefit patients who are nonadherent by educating them more thoroughly and letting them express themselves or share life experiences with fellow veterans who have the same diagnoses. Future studies are needed to determine the efficacy of DM SMAs especially with patients’ own PCPs.
1. Kirsh S, Watts S, Schaub K, et al. VA shared medical appointments for patients with diabetes: maximizing patient & provider expertise to strengthen care management. U.S. Department of Veterans Affairs website. http://www.queri.research.va.gov/tools/diabetes/shared-med-appt.pdf. Published December 2008. Accessed May 10, 2016.
2. American Diabetes Association. Statistics about diabetes. American Diabetes Association website. http://www.diabetes.org/diabetes-basics/diabetes-statistics. Updated April 1, 2016. Accessed May 14, 2016.
3. Sadur CN, Moline N, Costa M, et al. Diabetes management in a health maintenance organization. Efficacy of care management using cluster visits. Diabetes Care. 1999;22(12):2011-2017.
4. Trento M, Passera P, Tomalino M, et al. Group visits improve metabolic control in type 2 diabetes: a 2-year follow-up. Diabetes Care. 2001;24(6):995-1000.
5. Kirsh S, Watts S, Pascuzzi K, et al. Shared medical appointments based on the chronic care model: a quality improvement project to address the challenges of patients with diabetes with high cardiovascular risk. Qual Saf Health Care. 2007;16(5):349-353.
6. Sanchez I. Implementation of a diabetes self-management education program in primary care for adults using shared medical appointments. Diabetes Educ. 2011;37(3):381-391.
7. Guirguis AB, Lugovich J, Jay J, et al. Improving diabetes control using shared medical appointments. Am J Med. 2013;126(12):1043-1044.
8. Taveira TH, Friedmann PD, Cohen LB, et al. Pharmacist-led group medical appointment model in type 2 diabetes. Diabetes Educ. 2010;36(1):109-117.
9. Taveira TH, Dooley AG, Cohen LB, Khatana SA, Wu WC. Pharmacist-led group medical appointments for the management of type 2 diabetes with comorbid depression in older adults. Ann Pharmacother. 2011;45(11):1346-1355.
10. Cohen LB, Taveira TH, Khatana SA, Dooley AG, Pirraglia PA, Wu WC. Pharmacist-led shared medical appointments for multiple cardiovascular risk reduction in patients with type 2 diabetes. Diabetes Educ. 2011;37(6):801-812.
11. Wagner EH, Grothaus LC, Sandhu N, et al. Chronic care clinics for diabetes in primary care: a system-wide randomized trial. Diabetes Care. 2001;24(4):695-700.
12. Clancy DE, Huang P, Okonofua E, Yeager D, Magruder KM. Group visits: promoting adherence to diabetes guidelines. J Gen Intern Med. 2007;22(5):620-624.
13. Edelman D, Fredrickson SK, Melnyk SD, et al. Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Ann Intern Med. 2010;152(11):689-696.
14. Cohen S, Hartley S, Mavi J, Vest B, Wilson M. Veteran experiences related to participation in shared medical appointments. Mil Med. 2012;177(11):1287-1292.
1. Kirsh S, Watts S, Schaub K, et al. VA shared medical appointments for patients with diabetes: maximizing patient & provider expertise to strengthen care management. U.S. Department of Veterans Affairs website. http://www.queri.research.va.gov/tools/diabetes/shared-med-appt.pdf. Published December 2008. Accessed May 10, 2016.
2. American Diabetes Association. Statistics about diabetes. American Diabetes Association website. http://www.diabetes.org/diabetes-basics/diabetes-statistics. Updated April 1, 2016. Accessed May 14, 2016.
3. Sadur CN, Moline N, Costa M, et al. Diabetes management in a health maintenance organization. Efficacy of care management using cluster visits. Diabetes Care. 1999;22(12):2011-2017.
4. Trento M, Passera P, Tomalino M, et al. Group visits improve metabolic control in type 2 diabetes: a 2-year follow-up. Diabetes Care. 2001;24(6):995-1000.
5. Kirsh S, Watts S, Pascuzzi K, et al. Shared medical appointments based on the chronic care model: a quality improvement project to address the challenges of patients with diabetes with high cardiovascular risk. Qual Saf Health Care. 2007;16(5):349-353.
6. Sanchez I. Implementation of a diabetes self-management education program in primary care for adults using shared medical appointments. Diabetes Educ. 2011;37(3):381-391.
7. Guirguis AB, Lugovich J, Jay J, et al. Improving diabetes control using shared medical appointments. Am J Med. 2013;126(12):1043-1044.
8. Taveira TH, Friedmann PD, Cohen LB, et al. Pharmacist-led group medical appointment model in type 2 diabetes. Diabetes Educ. 2010;36(1):109-117.
9. Taveira TH, Dooley AG, Cohen LB, Khatana SA, Wu WC. Pharmacist-led group medical appointments for the management of type 2 diabetes with comorbid depression in older adults. Ann Pharmacother. 2011;45(11):1346-1355.
10. Cohen LB, Taveira TH, Khatana SA, Dooley AG, Pirraglia PA, Wu WC. Pharmacist-led shared medical appointments for multiple cardiovascular risk reduction in patients with type 2 diabetes. Diabetes Educ. 2011;37(6):801-812.
11. Wagner EH, Grothaus LC, Sandhu N, et al. Chronic care clinics for diabetes in primary care: a system-wide randomized trial. Diabetes Care. 2001;24(4):695-700.
12. Clancy DE, Huang P, Okonofua E, Yeager D, Magruder KM. Group visits: promoting adherence to diabetes guidelines. J Gen Intern Med. 2007;22(5):620-624.
13. Edelman D, Fredrickson SK, Melnyk SD, et al. Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Ann Intern Med. 2010;152(11):689-696.
14. Cohen S, Hartley S, Mavi J, Vest B, Wilson M. Veteran experiences related to participation in shared medical appointments. Mil Med. 2012;177(11):1287-1292.