User login
A practical approach to prescribing antidepressants
With the variety of drugs available for treating depression, choosing one can be daunting. Different agents have characteristics that may make them a better choice for different types of patients, but even so, treating any kind of mental illness often requires an element of trial and error.
Primary care providers are on the frontline of treating mental illness, often evaluating patients before they are seen by a psychiatrist. The purpose of this article is to provide insight into the art of prescribing antidepressants in the primary care setting. We will discuss common patient presentations, including depressed patients without other medical comorbidities as well as those with common comorbidities, with our recommendations for first-line treatment.
We hope our recommendations will help you to navigate the uncertainty more confidently, resulting in more efficient and tailored treatment for your patients.
BASELINE TESTING
When starting a patient on antidepressant drug therapy, we recommend obtaining a set of baseline laboratory tests to rule out underlying medical conditions that may be contributing to the patient’s depression or that may preclude the use of a given drug. (For example, elevation of liver enzymes may preclude the use of duloxetine.) Tests should include:
- A complete blood cell count
- A complete metabolic panel
- A thyroid-stimulating hormone level.
Electrocardiography may also be useful, as some antidepressants can prolong the QT interval or elevate the blood levels of other drugs with this effect.
GENERAL TREATMENT CONSIDERATIONS
There are several classes of antidepressants, and each class has a number of agents. Research has found little difference in efficacy among agents. So to simplify choosing which one to use, we recommend becoming comfortable with an agent from each class, ie:
- A selective serotonin reuptake inhibitor (SSRI)
- A selective serotonin-norepinephrine reuptake inhibitor (SNRI)
- A tricyclic antidepressant (TCA)
- A monoamine oxidase (MAO) inhibitor.
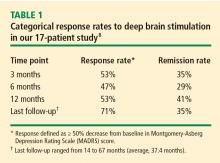
Each class includes generic agents, many of which are on the discount lists of retail pharmacies. Table 1 shows representative drugs from each class, with their relative costs.
Start low and go slow. In general, when starting an antidepressant, consider starting at half the normal dose, titrating upward as tolerated about every 14 days. This approach can minimize side effects. For example, if prescribing fluoxetine, start with 10 mg and titrate every 2 weeks based on tolerance and patient response. That said, each patient may respond differently, requiring perhaps a lower starting dose or a longer titration schedule.
Anticipate side effects. Most of the side effects of an antidepressant drug can be explained by its mechanism of action. Although side effects should certainly be considered when choosing an agent, patients can be reassured that most are transient and benign. A detailed discussion of side effects of antidepressant drugs is beyond the scope of this article, but a review by Khawam et al1 was published earlier in this journal.
Reassess. If after 4 to 6 weeks the patient has had little or no response, it is reasonable to switch agents. For a patient who was on an SSRI, the change can be to another SSRI or to an SNRI. However, if two SSRIs have already failed, then choose an SNRI. Agents are commonly cross-tapered during the switch to avoid abrupt cessation of one drug or the increased risk of adverse events such as cytochrome P450 interactions, serotonin syndrome, or hypertensive crisis (when switching to an MAO inhibitor).
Beware of interactions. All SSRIs and SNRIs are metabolized through the P450 system in the liver and therefore have the potential for drug-drug interactions. Care must be taken when giving these agents together with drugs whose metabolism can be altered by P450 inhibition. For TCAs, blood levels can be checked if there is concern about toxicity; however, dosing is not strictly based on this level. Great care should be taken if a TCA is given together with an SNRI or an SSRI, as the TCA blood level can become significantly elevated. This may result in QT interval prolongation, as mentioned earlier.
Refer. Referral to a psychiatrist is appropriate for patients for whom multiple classes have failed, for patients who have another psychiatric comorbidity (such as psychosis, hypomania, or mania), or for patients who may need hospitalization. Referral is also appropriate if the physician is concerned about suicide risk.
PATIENTS WITH MAJOR DEPRESSION ONLY
For a patient presenting with depression but no other significant medical comorbidity, the first-line therapy is often an SSRI. Several generic SSRIs are available, and some are on the discount lists at retail pharmacies.
Symptoms should start to improve in about 2 weeks, and the optimal response should be achieved in 4 to 6 weeks of treatment. If this does not occur, consider either adding an augmenting agent or switching to a different antidepressant.
PATIENTS WITH CHRONIC PAIN
Chronic pain and depression often go hand in hand and can potentiate each other. When considering an antidepressant in a patient who has both conditions, the SNRIs and TCAs are typically preferred. Some SNRIs, namely duloxetine and milnacipran, are approved for certain chronic pain conditions, such as fibromyalgia. SNRIs are frequently used off-label for other chronic pain conditions such as headache and neuropathic pain.2
TCAs such as amitriptyline, nortriptyline, and doxepin are also often used in patients with chronic pain. These agents, like the SNRIs, inhibit the reuptake of serotonin and norepinephrine and are used off-label for neuropathic pain,3,4 migraine, interstitial cystitis,5 and other pain conditions.6–9
For TCAs and SNRIs, the effective dose range for chronic pain overlaps that for depression. However, TCAs are often given at lower doses to patients without depression. We recommend starting at a low dose and slowly titrating upward to an effective dose. SNRIs are often preferred over TCAs because they do not have anticholinergic side effects and because an overdose is much less likely to be lethal.
PATIENTS WITH SEXUAL DYSFUNCTION
One of the more commonly reported side effects of antidepressants is sexual dysfunction, generally in the form of delayed orgasm or decreased libido.10 Typically, these complaints are attributed to SSRIs and SNRIs; however, TCAs and MAO inhibitors have also been associated wth sexual dysfunction.
Both erectile dysfunction and priapism have been linked to certain antidepressants. In particular, trazodone is a known cause of priapism. Even if using low doses for sleep, male patients should be made aware of this adverse effect.
Switching from one agent to another in the same class is not likely to improve sexual side effects. In particular, all the SSRIs are similar in their likelihood of causing sexual dysfunction. In a patient taking an SSRI who experiences this side effect, switching to bupropion11 or mirtazapine12 can be quite useful. Bupropion acts primarily on dopamine and norepinephrine, whereas mirtazapine acts on serotonin and norepinephrine but in a different manner from SSRIs and SNRIs.
Adjunctive treatment such as a cholinergic agonist, yohimbine (contraindicated with MAO inhibitors), a serotonergic agent (eg, buspirone), or a drug that acts on nitric oxide (eg, sildenafil, tadalafil) may have some utility but is often ineffective. Dose reduction, if possible, can be of value.
PATIENTS WITH ANXIETY
Many antidepressants are also approved for anxiety disorders, and still more are used off-label for this purpose. Anxiety and depression often occur together, so being able to treat both conditions with one drug can be quite useful.13 In general, the antidepressant effects are seen at lower doses of SSRIs and SNRIs, whereas more of the anxiolytic effects are seen at higher doses, particularly for obsessive-compulsive disorder.14
First-line treatment would be an SSRI or SNRI. Most anxiety disorders respond to either class, but there are some more-specific recommendations. SSRIs are best studied in panic disorder, generalized anxiety disorder, social anxiety disorder, posttraumatic stress disorder, and obsessive-compulsive disorder. Fluoxetine, citalopram, escitalopram, and sertraline15 can all be effective in both major depressive disorder and generalized anxiety disorder. Panic disorder also tends to respond well to SSRIs. SNRIs have been evaluated primarily in generalized anxiety disorder but may also be useful in many of the other conditions.
Additionally, mirtazapine (used off-label)12 and the TCAs16–18 can help treat anxiety. Clomipramine is used to treat obsessive-compulsive disorder.19 These drugs are especially useful for nighttime anxiety, as they can aid sleep. Of note, the anxiolytic effect of mirtazapine may be greater at higher doses.
MAO inhibitors often go unused because of the dietary and medication restrictions involved. However, very refractory cases of certain anxiety disorders may respond preferentially to these agents.
Bupropion tends to be more activating than other antidepressants, so is often avoided in anxious patients. However, some research suggests this is not always necessary.20 If the anxiety is secondary to depression, it will often improve significantly with this agent.
When starting or increasing the dose of an antidepressant, patients may experience increased anxiety or feel “jittery.” This feeling usually passes within the first week of treatment, and it is important to inform patients about this effect. “Start low and go slow” in patients with significant comorbid anxiety. Temporarily using a benzodiazepine such as clonazepam may make the transition more tolerable.
PATIENTS WITH CHRONIC FATIGUE SYNDROME OR FIBROMYALGIA
Increasing recognition of both chronic fatigue syndrome and fibromyalgia has led to more proactive treatment for these disorders. Depression can go hand in hand with these disorders, and certain antidepressants, namely the SNRIs, can be useful in this population.
More data exist for the treatment of fibromyalgia. Both duloxetine and milnacipran are approved by the US Food and Drug Administration (FDA) for the treatment of fibromyalgia.21 Venlafaxine is also used off-label for this purpose. SSRIs such as fluoxetine and citalopram have had mixed results.21–23 TCAs have been used with some success; however, their side effects and lethal potential are often limiting.21,24,25 A recent study in Spain also suggested there may be benefit from using MAO inhibitors for fibromyalgia, but data are quite limited.26
The data for treating chronic fatigue syndrome with SSRIs, SNRIs, or MAO inhibitors are conflicting.27–29 However, managing the co-existing depression may provide some relief in and of itself.
PATIENTS WITH FREQUENT INSOMNIA
Insomnia can be a symptom of depression, but it can also be a side effect of certain antidepressants. The SSRIs and SNRIs can disrupt sleep patterns in some patients by shortening the rapid-eye-movement (REM) stage.30,31
In patients with severe insomnia, it may be best to first recommend taking the antidepressant in the morning if they notice worsening sleep after initiating treatment. Patients can be told with any antidepressant, “If it makes you tired, take it at night, and if it wakes you up, take it in the morning.” Of note, a recent South African study suggested that escitalopram may be able to improve sleep.32
If that does not solve the problem, there are other options. For instance, mirtazapine, particularly in doses of 15 mg or 30 mg, aids depression and insomnia. At higher doses (45 mg), the sleep-aiding effect may be reduced. Low doses of TCAs, particularly doxepin, maprotiline (technically speaking, a tetracyclic antidepressant), amitriptyline, and nortriptyline can be effective sleep aids. These agents may be used as an adjunct to another antidepressant to enhance sleep and mood. However, the TCAs also shorten the REM stage of sleep.33
The previously mentioned drug interactions with SSRIs and SNRIs also need to be considered. Caution should be used when discontinuing these medications, as patients may experience rebound symptoms in the form of much more vivid dreams. MAO inhibitors may worsen insomnia because they suppress REM sleep.34
Trazodone is another agent that at lower doses (25–150 mg) can be an effective, nonaddicting sleep aid. When used as an antidepressant, it is generally prescribed at higher doses (300–400 mg), but its sedating effects can be quite limiting at these levels. It is important to remember the possibility of priapism in male patients.
GERIATRIC PATIENTS
Old age brings its own set of concerns when treating depression. Elderly patients are more susceptible to potential bradycardia caused by SSRIs. The TCAs have the more worrisome cardiac side effect of QTc prolongation. TCAs can slow cognitive function, whereas the SSRIs, bupropion, and the SNRIs tend not to affect cognition. Escitalopram and duloxetine have been suggested to be particularly effective in the elderly.35,36 A study from the Netherlands linked SSRIs with increased risk of falling in geriatric patients with dementia.37 Constipation, which could lead to ileus, is increased with TCAs and certain other agents (ie, paroxetine) in the geriatric population.
Mirtazapine is often very useful in elderly patients for many reasons: it treats both anxiety and depression, stimulates appetite and weight gain, can help with nausea, and is an effective sleep aid. Concerns about weight, appetite, and sleep are particularly common in the elderly, whereas younger patients can be less tolerant of drugs that make them gain weight and sleep more. Normal age-related changes to the sleep cycle contribute to decreased satisfaction with sleep as we age. In addition, depression often further impairs sleep. So, in the elderly, optimizing sleep is key. Research has also shown mirtazapine to be effective in patients with both Alzheimer dementia and depression.38
DIABETIC PATIENTS
One of the more worrisome side effects of psychiatric medications in diabetic patients is weight gain. Certain antidepressants have a greater propensity for weight gain and should likely be avoided as first-line treatments in this population.12 Typically, these agents include those that have more antihistamine action such as paroxetine and the TCAs. These agents also may lead to constipation, which could potentially worsen gastroparesis. Mirtazapine and the MAO inhibitors are also known to cause weight gain.
Bupropion and nefazodone are the most weight-neutral of all antidepressants. Nefazodone has fallen out of favor because of its potential to cause fulminant liver failure in rare cases. However, it remains a reasonable option for patients with comorbid anxiety and depression who have significant weight gain with other agents.
SSRIs and MAO inhibitors may improve or be neutral toward glucose metabolism, and some data suggest that SNRIs may impair this process.39
PATIENTS WITH CARDIAC CONDITIONS
Major depression often coexists with cardiac conditions. In particular, many patients develop depression after suffering a myocardial infarction, and increasingly they are being treated for it.40 Treatment in this situation is appropriate, since depression, if untreated, can increase the risk of recurrence of myocardial infarction.41
However, there are many concerns that accompany treating depression in cardiac patients. Therefore, a baseline electrocardiogram should be obtained before starting an antidepressant.
TCAs and tetracyclic agents have a tendency to prolong the QTc interval and potentiate ventricular arrhythmias,42 so it may be prudent to avoid these in patients at risk. These agents can also significantly increase the pulse rate. This tachycardia increases the risk of angina or myocardial infarction from the anticholinergic effects of these drugs.
In February 2013, the FDA issued a warning about possible arrhythmias with citalopram at doses greater than 40 mg in adult patients43; however, research has suggested citalopram is effective in treating depression in cardiac patients.44 Research has not shown an increase in efficacy at doses greater than 40 mg daily, so we recommend following the black-box warning.
TCAs and MAO inhibitors can also cause orthostatic hypotension. On the other hand, consuming large amounts of tyramine, in foods such as aged cheese, can precipitate a hypertensive crisis in patients taking MAO inhibitors.
Which antidepressants tend to be safer in cardiac patients? Sertraline has been shown to be safe in congestive heart failure and coronary artery disease,45–47 but the SSRIs are typically safe. Fluoxetine has shown efficacy in patients who have had a myocardial infarction.48 Mirtazapine has also been shown to be efficacious in cardiac patients.49 Nefazodone, mirtazapine, bupropion, SSRIs, and SNRIs have little or no tendency toward orthostatic hypotension.
- Khawam EA, Laurencic G, Malone DA. Side effects of antidepressants: an overview. Cleve Clin J Med 2006; 73:351–361.
- Ziegler D. Painful diabetic neuropathy: treatment and future aspects. Diabetes Metab Res Rev 2008; 24(suppl 1):S52–S57.
- Saarto T, Wiffen PJ. Antidepressants for neuropathic pain: a Cochrane review. J Neurol Neurosurg Psychiatry 2010; 81:1372–1373.
- Tanenberg RJ, Irving GA, Risser RC, et al. Duloxetine, pregabalin, and duloxetine plus gabapentin for diabetic peripheral neuropathic pain management in patients with inadequate pain response to gabapentin: an open-label, randomized, noninferiority comparison. Mayo Clin Proc 2011; 86:615–626.
- Hertle L, van Ophoven A. Long-term results of amitriptyline treatment for interstitial cystitis. Aktuelle Urol 2010; 41(suppl 1):S61–S65.
- Nguyen TM, Eslick GD. Systematic review: the treatment of noncardiac chest pain with antidepressants. Aliment Pharmacol Ther 2012; 35:493–500.
- Lee H, Kim JH, Min BH, et al. Efficacy of venlafaxine for symptomatic relief in young adult patients with functional chest pain: a randomized, double-blind, placebo-controlled, crossover trial. Am J Gastroenterol 2010; 105:1504–1512.
- Varia I, Logue E, O’Connor C, et al. Randomized trial of sertraline in patients with unexplained chest pain of noncardiac origin. Am Heart J 2000; 140:367–372.
- Doraiswamy PM, Varia I, Hellegers C, et al. A randomized controlled trial of paroxetine for noncardiac chest pain. Psychopharmacol Bull 2006; 39:15–24.
- Clayton AH. Understanding antidepressant mechanism of action and its effect on efficacy and safety. J Clin Psychiatry 2012; 73:e11.
- Gartlehner G, Hansen RA, Morgan LC, et al. Second-generation antidepressants in the pharmacologic treatment of adult depression: an update of the 2007 comparative effectiveness review (Internet). Rockville (MD): Agency for Healthcare Research and Quality (US); 2011 Dec. Comparative Effectiveness Reviews, No. 46. http://www.ncbi.nlm.nih.gov/books/NBK83442/. Accessed February 27, 2013.
- Watanabe N, Omori IM, Nakagawa A, et al. Mirtazapine versus other antidepressive agents for depression. Cochrane Database Syst Rev 2011; 12:CD006528.
- Hofmeijer-Sevink MK, Batelaan NM, van Megen HJ, et al. Clinical relevance of comorbidity in anxiety disorders: a report from the Netherlands Study of Depression and Anxiety (NESDA). J Affect Disord 2012; 137:106–112.
- Koen N, Stein DJ. Pharmacotherapy of anxiety disorders: a critical review. Dialogues Clin Neurosci 2011; 13:423–437.
- Sheehan DV, Kamijima K. An evidence-based review of the clinical use of sertraline in mood and anxiety disorders. Int Clin Psychopharmacol 2009; 24:43–60.
- Huh J, Goebert D, Takeshita J, Lu BY, Kang M. Treatment of generalized anxiety disorder: a comprehensive review of the literature for psychopharmacologic alternatives to newer antidepressants and benzodiazepines. Prim Care Companion CNS Disord 2011; 13: 4088/PCC.08r00709blu.
- Rickels K, Downing R, Schweizer E, Hassman H. Antidepressants for the treatment of generalized anxiety disorder. A placebo-controlled comparison of imipramine, trazodone, and diazepam. Arch Gen Psychiatry 1993; 50:884–895.
- Uher R, Maier W, Hauser J, et al. Differential efficacy of escitalopram and nortriptyline on dimensional measures of depression. Br J Psychiatry 2009; 194:252–259.
- Kellner M. Drug treatment of obsessive-compulsive disorder. Dialogues Clin Neurosci 2010; 12:187–197.
- Rush AJ, Trivedi MH, Carmody TJ, et al. Response in relation to baseline anxiety levels in major depressive disorder treated with bupropion sustained release or sertraline. Neuropsychopharmacology 2001; 25:131–138.
- Mease PJ, Dundon K, Sarzi-Puttini P. Pharmacotherapy of fibromyalgia. Best Pract Res Clin Rheumatol 2011; 25:285–297.
- Wolfe F, Cathey MA, Hawley DJ. A double-blind placebo controlled trial of fluoxetine in fibromyalgia. Scand J Rheumatol 1994; 23:255–259.
- Arnold LM, Hess EV, Hudson JI, Welge JA, Berno SE, Keck PE. A randomized, placebo-controlled, double-blind, flexible-dose study of fluoxetine in the treatment of women with fibromyalgia. Am J Med 2002; 112:191–197.
- Arnold LM, Keck PE, Welge JA. Antidepressant treatment of fibromyalgia. A meta-analysis and review. Psychosomatics 2000; 41:104–113.
- Goldenberg DL, Burckhardt C, Crofford L. Management of fibromyalgia syndrome. JAMA 2004; 292:2388–2395.
- Tort S, Urrútia G, Nishishinya MB, Walitt B. Monoamine oxidase inhibitors (MAOIs) for fibromyalgia syndrome. Cochrane Database Syst Rev 2012; 4:CD009807.
- Vercoulen JH, Swanink CM, Zitman FG, et al. Randomised, double-blind, placebo-controlled study of fluoxetine in chronic fatigue syndrome. Lancet 1996; 347:858–861.
- Natelson BH, Cheu J, Pareja J, Ellis SP, Policastro T, Findley TW. Randomized, double blind, controlled placebo-phase in trial of low dose phenelzine in the chronic fatigue syndrome. Psychopharmacology (Berl) 1996; 124:226–230.
- Reid S, Chalder T, Cleare A, Hotopf M, Wessely S. Chronic fatigue syndrome. BMJ 2000; 320:292–296.
- Kupfer DJ, Spiker DG, Coble PA, Neil JF, Ulrich R, Shaw DH. Sleep and treatment prediction in endogenous depression. Am J Psychiatry 1981; 138:429–434.
- Argyropoulos SV, Hicks JA, Nash JR, et al. Redistribution of slow wave activity of sleep during pharmacological treatment of depression with paroxetine but not with nefazodone. J Sleep Res 2009; 18:342–348.
- Stein DJ, Lopez AG. Effects of escitalopram on sleep problems in patients with major depression or generalized anxiety disorder. Adv Ther 2011; 28:1021–1037.
- Ehlers CL, Havstad JW, Kupfer DJ. Estimation of the time course of slow-wave sleep over the night in depressed patients: effects of clomipramine and clinical response. Biol Psychiatry 1996; 39:171–181.
- Landolt HP, Raimo EB, Schnierow BJ, Kelsoe JR, Rapaport MH, Gillin JC. Sleep and sleep electroencephalogram in depressed patients treated with phenelzine. Arch Gen Psychiatry 2001; 58:268–276.
- Chen YM, Huang XM, Thompson R, Zhao YB. Clinical features and efficacy of escitalopram treatment for geriatric depression. J Int Med Res 2011; 39:1946–1953.
- Dolder C, Nelson M, Stump A. Pharmacological and clinical profile of newer antidepressants: implications for the treatment of elderly patients. Drugs Aging 2010; 27:625–640.
- Sterke CS, Ziere G, van Beeck EF, Looman CW, van der Cammen TJ. Dose-response relationship between selective serotonin re-uptake inhibitors and injurious falls: a study in nursing home residents with dementia. Br J Clin Pharmacol 2012; 73:812–820.
- Raji MA, Brady SR. Mirtazapine for treatment of depression and comorbidities in Alzheimer disease. Ann Pharmacother 2001; 35:1024–1027.
- Hennings JM, Schaaf L, Fulda S. Glucose metabolism and antidepressant medication. Curr Pharm Des 2012; 18:5900–5919.
- Czarny MJ, Arthurs E, Coffie DF, et al. Prevalence of antidepressant prescription or use in patients with acute coronary syndrome: a systematic review. PLoS One 2011; 6:e27671.
- Zuidersma M, Ormel J, Conradi HJ, de Jonge P. An increase in depressive symptoms after myocardial infarction predicts new cardiac events irrespective of depressive symptoms before myocardial infarction. Psychol Med 2012; 42:683–693.
- van Noord C, Straus SM, Sturkenboom MC, et al. Psychotropic drugs associated with corrected QT interval prolongation. J Clin Psychopharmacol 2009; 29:9–15.
- US Food and Drug Administration (FDA). FDA Drug Safety Communication: abnormal heart rhythms associated with high doses of Celexa (citalopram hydrobromide). http://www.fda.gov/Drugs/DrugSafety/ucm269086.htm. Accessed August 25, 2013.
- Lespérance F, Frasure-Smith N, Koszycki D, et al; CREATE Investigators. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA 2007; 297:367–379.
- O’Connor CM, Jiang W, Kuchibhatla M, et al; SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol 2010; 56:692–699.
- Glassman AH, O’Connor CM, Califf RM, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHEART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288:701–709.
- Swenson JR, O’Connor CM, Barton D, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) Group. Influence of depression and effect of treatment with sertraline on quality of life after hospitalization for acute coronary syndrome. Am J Cardiol 2003; 92:1271–1276.
- Strik JJ, Honig A, Lousberg R, et al. Efficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction: findings from a double-blind, placebo-controlled trial. Psychosom Med 2000; 62:783–789.
- Honig A, Kuyper AM, Schene AH, et al; MIND-IT investigators. Treatment of post-myocardial infarction depressive disorder: a randomized, placebo-controlled trial with mirtazapine. Psychosom Med 2007; 69:606–613.
With the variety of drugs available for treating depression, choosing one can be daunting. Different agents have characteristics that may make them a better choice for different types of patients, but even so, treating any kind of mental illness often requires an element of trial and error.
Primary care providers are on the frontline of treating mental illness, often evaluating patients before they are seen by a psychiatrist. The purpose of this article is to provide insight into the art of prescribing antidepressants in the primary care setting. We will discuss common patient presentations, including depressed patients without other medical comorbidities as well as those with common comorbidities, with our recommendations for first-line treatment.
We hope our recommendations will help you to navigate the uncertainty more confidently, resulting in more efficient and tailored treatment for your patients.
BASELINE TESTING
When starting a patient on antidepressant drug therapy, we recommend obtaining a set of baseline laboratory tests to rule out underlying medical conditions that may be contributing to the patient’s depression or that may preclude the use of a given drug. (For example, elevation of liver enzymes may preclude the use of duloxetine.) Tests should include:
- A complete blood cell count
- A complete metabolic panel
- A thyroid-stimulating hormone level.
Electrocardiography may also be useful, as some antidepressants can prolong the QT interval or elevate the blood levels of other drugs with this effect.
GENERAL TREATMENT CONSIDERATIONS
There are several classes of antidepressants, and each class has a number of agents. Research has found little difference in efficacy among agents. So to simplify choosing which one to use, we recommend becoming comfortable with an agent from each class, ie:
- A selective serotonin reuptake inhibitor (SSRI)
- A selective serotonin-norepinephrine reuptake inhibitor (SNRI)
- A tricyclic antidepressant (TCA)
- A monoamine oxidase (MAO) inhibitor.
Each class includes generic agents, many of which are on the discount lists of retail pharmacies. Table 1 shows representative drugs from each class, with their relative costs.
Start low and go slow. In general, when starting an antidepressant, consider starting at half the normal dose, titrating upward as tolerated about every 14 days. This approach can minimize side effects. For example, if prescribing fluoxetine, start with 10 mg and titrate every 2 weeks based on tolerance and patient response. That said, each patient may respond differently, requiring perhaps a lower starting dose or a longer titration schedule.
Anticipate side effects. Most of the side effects of an antidepressant drug can be explained by its mechanism of action. Although side effects should certainly be considered when choosing an agent, patients can be reassured that most are transient and benign. A detailed discussion of side effects of antidepressant drugs is beyond the scope of this article, but a review by Khawam et al1 was published earlier in this journal.
Reassess. If after 4 to 6 weeks the patient has had little or no response, it is reasonable to switch agents. For a patient who was on an SSRI, the change can be to another SSRI or to an SNRI. However, if two SSRIs have already failed, then choose an SNRI. Agents are commonly cross-tapered during the switch to avoid abrupt cessation of one drug or the increased risk of adverse events such as cytochrome P450 interactions, serotonin syndrome, or hypertensive crisis (when switching to an MAO inhibitor).
Beware of interactions. All SSRIs and SNRIs are metabolized through the P450 system in the liver and therefore have the potential for drug-drug interactions. Care must be taken when giving these agents together with drugs whose metabolism can be altered by P450 inhibition. For TCAs, blood levels can be checked if there is concern about toxicity; however, dosing is not strictly based on this level. Great care should be taken if a TCA is given together with an SNRI or an SSRI, as the TCA blood level can become significantly elevated. This may result in QT interval prolongation, as mentioned earlier.
Refer. Referral to a psychiatrist is appropriate for patients for whom multiple classes have failed, for patients who have another psychiatric comorbidity (such as psychosis, hypomania, or mania), or for patients who may need hospitalization. Referral is also appropriate if the physician is concerned about suicide risk.
PATIENTS WITH MAJOR DEPRESSION ONLY
For a patient presenting with depression but no other significant medical comorbidity, the first-line therapy is often an SSRI. Several generic SSRIs are available, and some are on the discount lists at retail pharmacies.
Symptoms should start to improve in about 2 weeks, and the optimal response should be achieved in 4 to 6 weeks of treatment. If this does not occur, consider either adding an augmenting agent or switching to a different antidepressant.
PATIENTS WITH CHRONIC PAIN
Chronic pain and depression often go hand in hand and can potentiate each other. When considering an antidepressant in a patient who has both conditions, the SNRIs and TCAs are typically preferred. Some SNRIs, namely duloxetine and milnacipran, are approved for certain chronic pain conditions, such as fibromyalgia. SNRIs are frequently used off-label for other chronic pain conditions such as headache and neuropathic pain.2
TCAs such as amitriptyline, nortriptyline, and doxepin are also often used in patients with chronic pain. These agents, like the SNRIs, inhibit the reuptake of serotonin and norepinephrine and are used off-label for neuropathic pain,3,4 migraine, interstitial cystitis,5 and other pain conditions.6–9
For TCAs and SNRIs, the effective dose range for chronic pain overlaps that for depression. However, TCAs are often given at lower doses to patients without depression. We recommend starting at a low dose and slowly titrating upward to an effective dose. SNRIs are often preferred over TCAs because they do not have anticholinergic side effects and because an overdose is much less likely to be lethal.
PATIENTS WITH SEXUAL DYSFUNCTION
One of the more commonly reported side effects of antidepressants is sexual dysfunction, generally in the form of delayed orgasm or decreased libido.10 Typically, these complaints are attributed to SSRIs and SNRIs; however, TCAs and MAO inhibitors have also been associated wth sexual dysfunction.
Both erectile dysfunction and priapism have been linked to certain antidepressants. In particular, trazodone is a known cause of priapism. Even if using low doses for sleep, male patients should be made aware of this adverse effect.
Switching from one agent to another in the same class is not likely to improve sexual side effects. In particular, all the SSRIs are similar in their likelihood of causing sexual dysfunction. In a patient taking an SSRI who experiences this side effect, switching to bupropion11 or mirtazapine12 can be quite useful. Bupropion acts primarily on dopamine and norepinephrine, whereas mirtazapine acts on serotonin and norepinephrine but in a different manner from SSRIs and SNRIs.
Adjunctive treatment such as a cholinergic agonist, yohimbine (contraindicated with MAO inhibitors), a serotonergic agent (eg, buspirone), or a drug that acts on nitric oxide (eg, sildenafil, tadalafil) may have some utility but is often ineffective. Dose reduction, if possible, can be of value.
PATIENTS WITH ANXIETY
Many antidepressants are also approved for anxiety disorders, and still more are used off-label for this purpose. Anxiety and depression often occur together, so being able to treat both conditions with one drug can be quite useful.13 In general, the antidepressant effects are seen at lower doses of SSRIs and SNRIs, whereas more of the anxiolytic effects are seen at higher doses, particularly for obsessive-compulsive disorder.14
First-line treatment would be an SSRI or SNRI. Most anxiety disorders respond to either class, but there are some more-specific recommendations. SSRIs are best studied in panic disorder, generalized anxiety disorder, social anxiety disorder, posttraumatic stress disorder, and obsessive-compulsive disorder. Fluoxetine, citalopram, escitalopram, and sertraline15 can all be effective in both major depressive disorder and generalized anxiety disorder. Panic disorder also tends to respond well to SSRIs. SNRIs have been evaluated primarily in generalized anxiety disorder but may also be useful in many of the other conditions.
Additionally, mirtazapine (used off-label)12 and the TCAs16–18 can help treat anxiety. Clomipramine is used to treat obsessive-compulsive disorder.19 These drugs are especially useful for nighttime anxiety, as they can aid sleep. Of note, the anxiolytic effect of mirtazapine may be greater at higher doses.
MAO inhibitors often go unused because of the dietary and medication restrictions involved. However, very refractory cases of certain anxiety disorders may respond preferentially to these agents.
Bupropion tends to be more activating than other antidepressants, so is often avoided in anxious patients. However, some research suggests this is not always necessary.20 If the anxiety is secondary to depression, it will often improve significantly with this agent.
When starting or increasing the dose of an antidepressant, patients may experience increased anxiety or feel “jittery.” This feeling usually passes within the first week of treatment, and it is important to inform patients about this effect. “Start low and go slow” in patients with significant comorbid anxiety. Temporarily using a benzodiazepine such as clonazepam may make the transition more tolerable.
PATIENTS WITH CHRONIC FATIGUE SYNDROME OR FIBROMYALGIA
Increasing recognition of both chronic fatigue syndrome and fibromyalgia has led to more proactive treatment for these disorders. Depression can go hand in hand with these disorders, and certain antidepressants, namely the SNRIs, can be useful in this population.
More data exist for the treatment of fibromyalgia. Both duloxetine and milnacipran are approved by the US Food and Drug Administration (FDA) for the treatment of fibromyalgia.21 Venlafaxine is also used off-label for this purpose. SSRIs such as fluoxetine and citalopram have had mixed results.21–23 TCAs have been used with some success; however, their side effects and lethal potential are often limiting.21,24,25 A recent study in Spain also suggested there may be benefit from using MAO inhibitors for fibromyalgia, but data are quite limited.26
The data for treating chronic fatigue syndrome with SSRIs, SNRIs, or MAO inhibitors are conflicting.27–29 However, managing the co-existing depression may provide some relief in and of itself.
PATIENTS WITH FREQUENT INSOMNIA
Insomnia can be a symptom of depression, but it can also be a side effect of certain antidepressants. The SSRIs and SNRIs can disrupt sleep patterns in some patients by shortening the rapid-eye-movement (REM) stage.30,31
In patients with severe insomnia, it may be best to first recommend taking the antidepressant in the morning if they notice worsening sleep after initiating treatment. Patients can be told with any antidepressant, “If it makes you tired, take it at night, and if it wakes you up, take it in the morning.” Of note, a recent South African study suggested that escitalopram may be able to improve sleep.32
If that does not solve the problem, there are other options. For instance, mirtazapine, particularly in doses of 15 mg or 30 mg, aids depression and insomnia. At higher doses (45 mg), the sleep-aiding effect may be reduced. Low doses of TCAs, particularly doxepin, maprotiline (technically speaking, a tetracyclic antidepressant), amitriptyline, and nortriptyline can be effective sleep aids. These agents may be used as an adjunct to another antidepressant to enhance sleep and mood. However, the TCAs also shorten the REM stage of sleep.33
The previously mentioned drug interactions with SSRIs and SNRIs also need to be considered. Caution should be used when discontinuing these medications, as patients may experience rebound symptoms in the form of much more vivid dreams. MAO inhibitors may worsen insomnia because they suppress REM sleep.34
Trazodone is another agent that at lower doses (25–150 mg) can be an effective, nonaddicting sleep aid. When used as an antidepressant, it is generally prescribed at higher doses (300–400 mg), but its sedating effects can be quite limiting at these levels. It is important to remember the possibility of priapism in male patients.
GERIATRIC PATIENTS
Old age brings its own set of concerns when treating depression. Elderly patients are more susceptible to potential bradycardia caused by SSRIs. The TCAs have the more worrisome cardiac side effect of QTc prolongation. TCAs can slow cognitive function, whereas the SSRIs, bupropion, and the SNRIs tend not to affect cognition. Escitalopram and duloxetine have been suggested to be particularly effective in the elderly.35,36 A study from the Netherlands linked SSRIs with increased risk of falling in geriatric patients with dementia.37 Constipation, which could lead to ileus, is increased with TCAs and certain other agents (ie, paroxetine) in the geriatric population.
Mirtazapine is often very useful in elderly patients for many reasons: it treats both anxiety and depression, stimulates appetite and weight gain, can help with nausea, and is an effective sleep aid. Concerns about weight, appetite, and sleep are particularly common in the elderly, whereas younger patients can be less tolerant of drugs that make them gain weight and sleep more. Normal age-related changes to the sleep cycle contribute to decreased satisfaction with sleep as we age. In addition, depression often further impairs sleep. So, in the elderly, optimizing sleep is key. Research has also shown mirtazapine to be effective in patients with both Alzheimer dementia and depression.38
DIABETIC PATIENTS
One of the more worrisome side effects of psychiatric medications in diabetic patients is weight gain. Certain antidepressants have a greater propensity for weight gain and should likely be avoided as first-line treatments in this population.12 Typically, these agents include those that have more antihistamine action such as paroxetine and the TCAs. These agents also may lead to constipation, which could potentially worsen gastroparesis. Mirtazapine and the MAO inhibitors are also known to cause weight gain.
Bupropion and nefazodone are the most weight-neutral of all antidepressants. Nefazodone has fallen out of favor because of its potential to cause fulminant liver failure in rare cases. However, it remains a reasonable option for patients with comorbid anxiety and depression who have significant weight gain with other agents.
SSRIs and MAO inhibitors may improve or be neutral toward glucose metabolism, and some data suggest that SNRIs may impair this process.39
PATIENTS WITH CARDIAC CONDITIONS
Major depression often coexists with cardiac conditions. In particular, many patients develop depression after suffering a myocardial infarction, and increasingly they are being treated for it.40 Treatment in this situation is appropriate, since depression, if untreated, can increase the risk of recurrence of myocardial infarction.41
However, there are many concerns that accompany treating depression in cardiac patients. Therefore, a baseline electrocardiogram should be obtained before starting an antidepressant.
TCAs and tetracyclic agents have a tendency to prolong the QTc interval and potentiate ventricular arrhythmias,42 so it may be prudent to avoid these in patients at risk. These agents can also significantly increase the pulse rate. This tachycardia increases the risk of angina or myocardial infarction from the anticholinergic effects of these drugs.
In February 2013, the FDA issued a warning about possible arrhythmias with citalopram at doses greater than 40 mg in adult patients43; however, research has suggested citalopram is effective in treating depression in cardiac patients.44 Research has not shown an increase in efficacy at doses greater than 40 mg daily, so we recommend following the black-box warning.
TCAs and MAO inhibitors can also cause orthostatic hypotension. On the other hand, consuming large amounts of tyramine, in foods such as aged cheese, can precipitate a hypertensive crisis in patients taking MAO inhibitors.
Which antidepressants tend to be safer in cardiac patients? Sertraline has been shown to be safe in congestive heart failure and coronary artery disease,45–47 but the SSRIs are typically safe. Fluoxetine has shown efficacy in patients who have had a myocardial infarction.48 Mirtazapine has also been shown to be efficacious in cardiac patients.49 Nefazodone, mirtazapine, bupropion, SSRIs, and SNRIs have little or no tendency toward orthostatic hypotension.
With the variety of drugs available for treating depression, choosing one can be daunting. Different agents have characteristics that may make them a better choice for different types of patients, but even so, treating any kind of mental illness often requires an element of trial and error.
Primary care providers are on the frontline of treating mental illness, often evaluating patients before they are seen by a psychiatrist. The purpose of this article is to provide insight into the art of prescribing antidepressants in the primary care setting. We will discuss common patient presentations, including depressed patients without other medical comorbidities as well as those with common comorbidities, with our recommendations for first-line treatment.
We hope our recommendations will help you to navigate the uncertainty more confidently, resulting in more efficient and tailored treatment for your patients.
BASELINE TESTING
When starting a patient on antidepressant drug therapy, we recommend obtaining a set of baseline laboratory tests to rule out underlying medical conditions that may be contributing to the patient’s depression or that may preclude the use of a given drug. (For example, elevation of liver enzymes may preclude the use of duloxetine.) Tests should include:
- A complete blood cell count
- A complete metabolic panel
- A thyroid-stimulating hormone level.
Electrocardiography may also be useful, as some antidepressants can prolong the QT interval or elevate the blood levels of other drugs with this effect.
GENERAL TREATMENT CONSIDERATIONS
There are several classes of antidepressants, and each class has a number of agents. Research has found little difference in efficacy among agents. So to simplify choosing which one to use, we recommend becoming comfortable with an agent from each class, ie:
- A selective serotonin reuptake inhibitor (SSRI)
- A selective serotonin-norepinephrine reuptake inhibitor (SNRI)
- A tricyclic antidepressant (TCA)
- A monoamine oxidase (MAO) inhibitor.
Each class includes generic agents, many of which are on the discount lists of retail pharmacies. Table 1 shows representative drugs from each class, with their relative costs.
Start low and go slow. In general, when starting an antidepressant, consider starting at half the normal dose, titrating upward as tolerated about every 14 days. This approach can minimize side effects. For example, if prescribing fluoxetine, start with 10 mg and titrate every 2 weeks based on tolerance and patient response. That said, each patient may respond differently, requiring perhaps a lower starting dose or a longer titration schedule.
Anticipate side effects. Most of the side effects of an antidepressant drug can be explained by its mechanism of action. Although side effects should certainly be considered when choosing an agent, patients can be reassured that most are transient and benign. A detailed discussion of side effects of antidepressant drugs is beyond the scope of this article, but a review by Khawam et al1 was published earlier in this journal.
Reassess. If after 4 to 6 weeks the patient has had little or no response, it is reasonable to switch agents. For a patient who was on an SSRI, the change can be to another SSRI or to an SNRI. However, if two SSRIs have already failed, then choose an SNRI. Agents are commonly cross-tapered during the switch to avoid abrupt cessation of one drug or the increased risk of adverse events such as cytochrome P450 interactions, serotonin syndrome, or hypertensive crisis (when switching to an MAO inhibitor).
Beware of interactions. All SSRIs and SNRIs are metabolized through the P450 system in the liver and therefore have the potential for drug-drug interactions. Care must be taken when giving these agents together with drugs whose metabolism can be altered by P450 inhibition. For TCAs, blood levels can be checked if there is concern about toxicity; however, dosing is not strictly based on this level. Great care should be taken if a TCA is given together with an SNRI or an SSRI, as the TCA blood level can become significantly elevated. This may result in QT interval prolongation, as mentioned earlier.
Refer. Referral to a psychiatrist is appropriate for patients for whom multiple classes have failed, for patients who have another psychiatric comorbidity (such as psychosis, hypomania, or mania), or for patients who may need hospitalization. Referral is also appropriate if the physician is concerned about suicide risk.
PATIENTS WITH MAJOR DEPRESSION ONLY
For a patient presenting with depression but no other significant medical comorbidity, the first-line therapy is often an SSRI. Several generic SSRIs are available, and some are on the discount lists at retail pharmacies.
Symptoms should start to improve in about 2 weeks, and the optimal response should be achieved in 4 to 6 weeks of treatment. If this does not occur, consider either adding an augmenting agent or switching to a different antidepressant.
PATIENTS WITH CHRONIC PAIN
Chronic pain and depression often go hand in hand and can potentiate each other. When considering an antidepressant in a patient who has both conditions, the SNRIs and TCAs are typically preferred. Some SNRIs, namely duloxetine and milnacipran, are approved for certain chronic pain conditions, such as fibromyalgia. SNRIs are frequently used off-label for other chronic pain conditions such as headache and neuropathic pain.2
TCAs such as amitriptyline, nortriptyline, and doxepin are also often used in patients with chronic pain. These agents, like the SNRIs, inhibit the reuptake of serotonin and norepinephrine and are used off-label for neuropathic pain,3,4 migraine, interstitial cystitis,5 and other pain conditions.6–9
For TCAs and SNRIs, the effective dose range for chronic pain overlaps that for depression. However, TCAs are often given at lower doses to patients without depression. We recommend starting at a low dose and slowly titrating upward to an effective dose. SNRIs are often preferred over TCAs because they do not have anticholinergic side effects and because an overdose is much less likely to be lethal.
PATIENTS WITH SEXUAL DYSFUNCTION
One of the more commonly reported side effects of antidepressants is sexual dysfunction, generally in the form of delayed orgasm or decreased libido.10 Typically, these complaints are attributed to SSRIs and SNRIs; however, TCAs and MAO inhibitors have also been associated wth sexual dysfunction.
Both erectile dysfunction and priapism have been linked to certain antidepressants. In particular, trazodone is a known cause of priapism. Even if using low doses for sleep, male patients should be made aware of this adverse effect.
Switching from one agent to another in the same class is not likely to improve sexual side effects. In particular, all the SSRIs are similar in their likelihood of causing sexual dysfunction. In a patient taking an SSRI who experiences this side effect, switching to bupropion11 or mirtazapine12 can be quite useful. Bupropion acts primarily on dopamine and norepinephrine, whereas mirtazapine acts on serotonin and norepinephrine but in a different manner from SSRIs and SNRIs.
Adjunctive treatment such as a cholinergic agonist, yohimbine (contraindicated with MAO inhibitors), a serotonergic agent (eg, buspirone), or a drug that acts on nitric oxide (eg, sildenafil, tadalafil) may have some utility but is often ineffective. Dose reduction, if possible, can be of value.
PATIENTS WITH ANXIETY
Many antidepressants are also approved for anxiety disorders, and still more are used off-label for this purpose. Anxiety and depression often occur together, so being able to treat both conditions with one drug can be quite useful.13 In general, the antidepressant effects are seen at lower doses of SSRIs and SNRIs, whereas more of the anxiolytic effects are seen at higher doses, particularly for obsessive-compulsive disorder.14
First-line treatment would be an SSRI or SNRI. Most anxiety disorders respond to either class, but there are some more-specific recommendations. SSRIs are best studied in panic disorder, generalized anxiety disorder, social anxiety disorder, posttraumatic stress disorder, and obsessive-compulsive disorder. Fluoxetine, citalopram, escitalopram, and sertraline15 can all be effective in both major depressive disorder and generalized anxiety disorder. Panic disorder also tends to respond well to SSRIs. SNRIs have been evaluated primarily in generalized anxiety disorder but may also be useful in many of the other conditions.
Additionally, mirtazapine (used off-label)12 and the TCAs16–18 can help treat anxiety. Clomipramine is used to treat obsessive-compulsive disorder.19 These drugs are especially useful for nighttime anxiety, as they can aid sleep. Of note, the anxiolytic effect of mirtazapine may be greater at higher doses.
MAO inhibitors often go unused because of the dietary and medication restrictions involved. However, very refractory cases of certain anxiety disorders may respond preferentially to these agents.
Bupropion tends to be more activating than other antidepressants, so is often avoided in anxious patients. However, some research suggests this is not always necessary.20 If the anxiety is secondary to depression, it will often improve significantly with this agent.
When starting or increasing the dose of an antidepressant, patients may experience increased anxiety or feel “jittery.” This feeling usually passes within the first week of treatment, and it is important to inform patients about this effect. “Start low and go slow” in patients with significant comorbid anxiety. Temporarily using a benzodiazepine such as clonazepam may make the transition more tolerable.
PATIENTS WITH CHRONIC FATIGUE SYNDROME OR FIBROMYALGIA
Increasing recognition of both chronic fatigue syndrome and fibromyalgia has led to more proactive treatment for these disorders. Depression can go hand in hand with these disorders, and certain antidepressants, namely the SNRIs, can be useful in this population.
More data exist for the treatment of fibromyalgia. Both duloxetine and milnacipran are approved by the US Food and Drug Administration (FDA) for the treatment of fibromyalgia.21 Venlafaxine is also used off-label for this purpose. SSRIs such as fluoxetine and citalopram have had mixed results.21–23 TCAs have been used with some success; however, their side effects and lethal potential are often limiting.21,24,25 A recent study in Spain also suggested there may be benefit from using MAO inhibitors for fibromyalgia, but data are quite limited.26
The data for treating chronic fatigue syndrome with SSRIs, SNRIs, or MAO inhibitors are conflicting.27–29 However, managing the co-existing depression may provide some relief in and of itself.
PATIENTS WITH FREQUENT INSOMNIA
Insomnia can be a symptom of depression, but it can also be a side effect of certain antidepressants. The SSRIs and SNRIs can disrupt sleep patterns in some patients by shortening the rapid-eye-movement (REM) stage.30,31
In patients with severe insomnia, it may be best to first recommend taking the antidepressant in the morning if they notice worsening sleep after initiating treatment. Patients can be told with any antidepressant, “If it makes you tired, take it at night, and if it wakes you up, take it in the morning.” Of note, a recent South African study suggested that escitalopram may be able to improve sleep.32
If that does not solve the problem, there are other options. For instance, mirtazapine, particularly in doses of 15 mg or 30 mg, aids depression and insomnia. At higher doses (45 mg), the sleep-aiding effect may be reduced. Low doses of TCAs, particularly doxepin, maprotiline (technically speaking, a tetracyclic antidepressant), amitriptyline, and nortriptyline can be effective sleep aids. These agents may be used as an adjunct to another antidepressant to enhance sleep and mood. However, the TCAs also shorten the REM stage of sleep.33
The previously mentioned drug interactions with SSRIs and SNRIs also need to be considered. Caution should be used when discontinuing these medications, as patients may experience rebound symptoms in the form of much more vivid dreams. MAO inhibitors may worsen insomnia because they suppress REM sleep.34
Trazodone is another agent that at lower doses (25–150 mg) can be an effective, nonaddicting sleep aid. When used as an antidepressant, it is generally prescribed at higher doses (300–400 mg), but its sedating effects can be quite limiting at these levels. It is important to remember the possibility of priapism in male patients.
GERIATRIC PATIENTS
Old age brings its own set of concerns when treating depression. Elderly patients are more susceptible to potential bradycardia caused by SSRIs. The TCAs have the more worrisome cardiac side effect of QTc prolongation. TCAs can slow cognitive function, whereas the SSRIs, bupropion, and the SNRIs tend not to affect cognition. Escitalopram and duloxetine have been suggested to be particularly effective in the elderly.35,36 A study from the Netherlands linked SSRIs with increased risk of falling in geriatric patients with dementia.37 Constipation, which could lead to ileus, is increased with TCAs and certain other agents (ie, paroxetine) in the geriatric population.
Mirtazapine is often very useful in elderly patients for many reasons: it treats both anxiety and depression, stimulates appetite and weight gain, can help with nausea, and is an effective sleep aid. Concerns about weight, appetite, and sleep are particularly common in the elderly, whereas younger patients can be less tolerant of drugs that make them gain weight and sleep more. Normal age-related changes to the sleep cycle contribute to decreased satisfaction with sleep as we age. In addition, depression often further impairs sleep. So, in the elderly, optimizing sleep is key. Research has also shown mirtazapine to be effective in patients with both Alzheimer dementia and depression.38
DIABETIC PATIENTS
One of the more worrisome side effects of psychiatric medications in diabetic patients is weight gain. Certain antidepressants have a greater propensity for weight gain and should likely be avoided as first-line treatments in this population.12 Typically, these agents include those that have more antihistamine action such as paroxetine and the TCAs. These agents also may lead to constipation, which could potentially worsen gastroparesis. Mirtazapine and the MAO inhibitors are also known to cause weight gain.
Bupropion and nefazodone are the most weight-neutral of all antidepressants. Nefazodone has fallen out of favor because of its potential to cause fulminant liver failure in rare cases. However, it remains a reasonable option for patients with comorbid anxiety and depression who have significant weight gain with other agents.
SSRIs and MAO inhibitors may improve or be neutral toward glucose metabolism, and some data suggest that SNRIs may impair this process.39
PATIENTS WITH CARDIAC CONDITIONS
Major depression often coexists with cardiac conditions. In particular, many patients develop depression after suffering a myocardial infarction, and increasingly they are being treated for it.40 Treatment in this situation is appropriate, since depression, if untreated, can increase the risk of recurrence of myocardial infarction.41
However, there are many concerns that accompany treating depression in cardiac patients. Therefore, a baseline electrocardiogram should be obtained before starting an antidepressant.
TCAs and tetracyclic agents have a tendency to prolong the QTc interval and potentiate ventricular arrhythmias,42 so it may be prudent to avoid these in patients at risk. These agents can also significantly increase the pulse rate. This tachycardia increases the risk of angina or myocardial infarction from the anticholinergic effects of these drugs.
In February 2013, the FDA issued a warning about possible arrhythmias with citalopram at doses greater than 40 mg in adult patients43; however, research has suggested citalopram is effective in treating depression in cardiac patients.44 Research has not shown an increase in efficacy at doses greater than 40 mg daily, so we recommend following the black-box warning.
TCAs and MAO inhibitors can also cause orthostatic hypotension. On the other hand, consuming large amounts of tyramine, in foods such as aged cheese, can precipitate a hypertensive crisis in patients taking MAO inhibitors.
Which antidepressants tend to be safer in cardiac patients? Sertraline has been shown to be safe in congestive heart failure and coronary artery disease,45–47 but the SSRIs are typically safe. Fluoxetine has shown efficacy in patients who have had a myocardial infarction.48 Mirtazapine has also been shown to be efficacious in cardiac patients.49 Nefazodone, mirtazapine, bupropion, SSRIs, and SNRIs have little or no tendency toward orthostatic hypotension.
- Khawam EA, Laurencic G, Malone DA. Side effects of antidepressants: an overview. Cleve Clin J Med 2006; 73:351–361.
- Ziegler D. Painful diabetic neuropathy: treatment and future aspects. Diabetes Metab Res Rev 2008; 24(suppl 1):S52–S57.
- Saarto T, Wiffen PJ. Antidepressants for neuropathic pain: a Cochrane review. J Neurol Neurosurg Psychiatry 2010; 81:1372–1373.
- Tanenberg RJ, Irving GA, Risser RC, et al. Duloxetine, pregabalin, and duloxetine plus gabapentin for diabetic peripheral neuropathic pain management in patients with inadequate pain response to gabapentin: an open-label, randomized, noninferiority comparison. Mayo Clin Proc 2011; 86:615–626.
- Hertle L, van Ophoven A. Long-term results of amitriptyline treatment for interstitial cystitis. Aktuelle Urol 2010; 41(suppl 1):S61–S65.
- Nguyen TM, Eslick GD. Systematic review: the treatment of noncardiac chest pain with antidepressants. Aliment Pharmacol Ther 2012; 35:493–500.
- Lee H, Kim JH, Min BH, et al. Efficacy of venlafaxine for symptomatic relief in young adult patients with functional chest pain: a randomized, double-blind, placebo-controlled, crossover trial. Am J Gastroenterol 2010; 105:1504–1512.
- Varia I, Logue E, O’Connor C, et al. Randomized trial of sertraline in patients with unexplained chest pain of noncardiac origin. Am Heart J 2000; 140:367–372.
- Doraiswamy PM, Varia I, Hellegers C, et al. A randomized controlled trial of paroxetine for noncardiac chest pain. Psychopharmacol Bull 2006; 39:15–24.
- Clayton AH. Understanding antidepressant mechanism of action and its effect on efficacy and safety. J Clin Psychiatry 2012; 73:e11.
- Gartlehner G, Hansen RA, Morgan LC, et al. Second-generation antidepressants in the pharmacologic treatment of adult depression: an update of the 2007 comparative effectiveness review (Internet). Rockville (MD): Agency for Healthcare Research and Quality (US); 2011 Dec. Comparative Effectiveness Reviews, No. 46. http://www.ncbi.nlm.nih.gov/books/NBK83442/. Accessed February 27, 2013.
- Watanabe N, Omori IM, Nakagawa A, et al. Mirtazapine versus other antidepressive agents for depression. Cochrane Database Syst Rev 2011; 12:CD006528.
- Hofmeijer-Sevink MK, Batelaan NM, van Megen HJ, et al. Clinical relevance of comorbidity in anxiety disorders: a report from the Netherlands Study of Depression and Anxiety (NESDA). J Affect Disord 2012; 137:106–112.
- Koen N, Stein DJ. Pharmacotherapy of anxiety disorders: a critical review. Dialogues Clin Neurosci 2011; 13:423–437.
- Sheehan DV, Kamijima K. An evidence-based review of the clinical use of sertraline in mood and anxiety disorders. Int Clin Psychopharmacol 2009; 24:43–60.
- Huh J, Goebert D, Takeshita J, Lu BY, Kang M. Treatment of generalized anxiety disorder: a comprehensive review of the literature for psychopharmacologic alternatives to newer antidepressants and benzodiazepines. Prim Care Companion CNS Disord 2011; 13: 4088/PCC.08r00709blu.
- Rickels K, Downing R, Schweizer E, Hassman H. Antidepressants for the treatment of generalized anxiety disorder. A placebo-controlled comparison of imipramine, trazodone, and diazepam. Arch Gen Psychiatry 1993; 50:884–895.
- Uher R, Maier W, Hauser J, et al. Differential efficacy of escitalopram and nortriptyline on dimensional measures of depression. Br J Psychiatry 2009; 194:252–259.
- Kellner M. Drug treatment of obsessive-compulsive disorder. Dialogues Clin Neurosci 2010; 12:187–197.
- Rush AJ, Trivedi MH, Carmody TJ, et al. Response in relation to baseline anxiety levels in major depressive disorder treated with bupropion sustained release or sertraline. Neuropsychopharmacology 2001; 25:131–138.
- Mease PJ, Dundon K, Sarzi-Puttini P. Pharmacotherapy of fibromyalgia. Best Pract Res Clin Rheumatol 2011; 25:285–297.
- Wolfe F, Cathey MA, Hawley DJ. A double-blind placebo controlled trial of fluoxetine in fibromyalgia. Scand J Rheumatol 1994; 23:255–259.
- Arnold LM, Hess EV, Hudson JI, Welge JA, Berno SE, Keck PE. A randomized, placebo-controlled, double-blind, flexible-dose study of fluoxetine in the treatment of women with fibromyalgia. Am J Med 2002; 112:191–197.
- Arnold LM, Keck PE, Welge JA. Antidepressant treatment of fibromyalgia. A meta-analysis and review. Psychosomatics 2000; 41:104–113.
- Goldenberg DL, Burckhardt C, Crofford L. Management of fibromyalgia syndrome. JAMA 2004; 292:2388–2395.
- Tort S, Urrútia G, Nishishinya MB, Walitt B. Monoamine oxidase inhibitors (MAOIs) for fibromyalgia syndrome. Cochrane Database Syst Rev 2012; 4:CD009807.
- Vercoulen JH, Swanink CM, Zitman FG, et al. Randomised, double-blind, placebo-controlled study of fluoxetine in chronic fatigue syndrome. Lancet 1996; 347:858–861.
- Natelson BH, Cheu J, Pareja J, Ellis SP, Policastro T, Findley TW. Randomized, double blind, controlled placebo-phase in trial of low dose phenelzine in the chronic fatigue syndrome. Psychopharmacology (Berl) 1996; 124:226–230.
- Reid S, Chalder T, Cleare A, Hotopf M, Wessely S. Chronic fatigue syndrome. BMJ 2000; 320:292–296.
- Kupfer DJ, Spiker DG, Coble PA, Neil JF, Ulrich R, Shaw DH. Sleep and treatment prediction in endogenous depression. Am J Psychiatry 1981; 138:429–434.
- Argyropoulos SV, Hicks JA, Nash JR, et al. Redistribution of slow wave activity of sleep during pharmacological treatment of depression with paroxetine but not with nefazodone. J Sleep Res 2009; 18:342–348.
- Stein DJ, Lopez AG. Effects of escitalopram on sleep problems in patients with major depression or generalized anxiety disorder. Adv Ther 2011; 28:1021–1037.
- Ehlers CL, Havstad JW, Kupfer DJ. Estimation of the time course of slow-wave sleep over the night in depressed patients: effects of clomipramine and clinical response. Biol Psychiatry 1996; 39:171–181.
- Landolt HP, Raimo EB, Schnierow BJ, Kelsoe JR, Rapaport MH, Gillin JC. Sleep and sleep electroencephalogram in depressed patients treated with phenelzine. Arch Gen Psychiatry 2001; 58:268–276.
- Chen YM, Huang XM, Thompson R, Zhao YB. Clinical features and efficacy of escitalopram treatment for geriatric depression. J Int Med Res 2011; 39:1946–1953.
- Dolder C, Nelson M, Stump A. Pharmacological and clinical profile of newer antidepressants: implications for the treatment of elderly patients. Drugs Aging 2010; 27:625–640.
- Sterke CS, Ziere G, van Beeck EF, Looman CW, van der Cammen TJ. Dose-response relationship between selective serotonin re-uptake inhibitors and injurious falls: a study in nursing home residents with dementia. Br J Clin Pharmacol 2012; 73:812–820.
- Raji MA, Brady SR. Mirtazapine for treatment of depression and comorbidities in Alzheimer disease. Ann Pharmacother 2001; 35:1024–1027.
- Hennings JM, Schaaf L, Fulda S. Glucose metabolism and antidepressant medication. Curr Pharm Des 2012; 18:5900–5919.
- Czarny MJ, Arthurs E, Coffie DF, et al. Prevalence of antidepressant prescription or use in patients with acute coronary syndrome: a systematic review. PLoS One 2011; 6:e27671.
- Zuidersma M, Ormel J, Conradi HJ, de Jonge P. An increase in depressive symptoms after myocardial infarction predicts new cardiac events irrespective of depressive symptoms before myocardial infarction. Psychol Med 2012; 42:683–693.
- van Noord C, Straus SM, Sturkenboom MC, et al. Psychotropic drugs associated with corrected QT interval prolongation. J Clin Psychopharmacol 2009; 29:9–15.
- US Food and Drug Administration (FDA). FDA Drug Safety Communication: abnormal heart rhythms associated with high doses of Celexa (citalopram hydrobromide). http://www.fda.gov/Drugs/DrugSafety/ucm269086.htm. Accessed August 25, 2013.
- Lespérance F, Frasure-Smith N, Koszycki D, et al; CREATE Investigators. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA 2007; 297:367–379.
- O’Connor CM, Jiang W, Kuchibhatla M, et al; SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol 2010; 56:692–699.
- Glassman AH, O’Connor CM, Califf RM, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHEART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288:701–709.
- Swenson JR, O’Connor CM, Barton D, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) Group. Influence of depression and effect of treatment with sertraline on quality of life after hospitalization for acute coronary syndrome. Am J Cardiol 2003; 92:1271–1276.
- Strik JJ, Honig A, Lousberg R, et al. Efficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction: findings from a double-blind, placebo-controlled trial. Psychosom Med 2000; 62:783–789.
- Honig A, Kuyper AM, Schene AH, et al; MIND-IT investigators. Treatment of post-myocardial infarction depressive disorder: a randomized, placebo-controlled trial with mirtazapine. Psychosom Med 2007; 69:606–613.
- Khawam EA, Laurencic G, Malone DA. Side effects of antidepressants: an overview. Cleve Clin J Med 2006; 73:351–361.
- Ziegler D. Painful diabetic neuropathy: treatment and future aspects. Diabetes Metab Res Rev 2008; 24(suppl 1):S52–S57.
- Saarto T, Wiffen PJ. Antidepressants for neuropathic pain: a Cochrane review. J Neurol Neurosurg Psychiatry 2010; 81:1372–1373.
- Tanenberg RJ, Irving GA, Risser RC, et al. Duloxetine, pregabalin, and duloxetine plus gabapentin for diabetic peripheral neuropathic pain management in patients with inadequate pain response to gabapentin: an open-label, randomized, noninferiority comparison. Mayo Clin Proc 2011; 86:615–626.
- Hertle L, van Ophoven A. Long-term results of amitriptyline treatment for interstitial cystitis. Aktuelle Urol 2010; 41(suppl 1):S61–S65.
- Nguyen TM, Eslick GD. Systematic review: the treatment of noncardiac chest pain with antidepressants. Aliment Pharmacol Ther 2012; 35:493–500.
- Lee H, Kim JH, Min BH, et al. Efficacy of venlafaxine for symptomatic relief in young adult patients with functional chest pain: a randomized, double-blind, placebo-controlled, crossover trial. Am J Gastroenterol 2010; 105:1504–1512.
- Varia I, Logue E, O’Connor C, et al. Randomized trial of sertraline in patients with unexplained chest pain of noncardiac origin. Am Heart J 2000; 140:367–372.
- Doraiswamy PM, Varia I, Hellegers C, et al. A randomized controlled trial of paroxetine for noncardiac chest pain. Psychopharmacol Bull 2006; 39:15–24.
- Clayton AH. Understanding antidepressant mechanism of action and its effect on efficacy and safety. J Clin Psychiatry 2012; 73:e11.
- Gartlehner G, Hansen RA, Morgan LC, et al. Second-generation antidepressants in the pharmacologic treatment of adult depression: an update of the 2007 comparative effectiveness review (Internet). Rockville (MD): Agency for Healthcare Research and Quality (US); 2011 Dec. Comparative Effectiveness Reviews, No. 46. http://www.ncbi.nlm.nih.gov/books/NBK83442/. Accessed February 27, 2013.
- Watanabe N, Omori IM, Nakagawa A, et al. Mirtazapine versus other antidepressive agents for depression. Cochrane Database Syst Rev 2011; 12:CD006528.
- Hofmeijer-Sevink MK, Batelaan NM, van Megen HJ, et al. Clinical relevance of comorbidity in anxiety disorders: a report from the Netherlands Study of Depression and Anxiety (NESDA). J Affect Disord 2012; 137:106–112.
- Koen N, Stein DJ. Pharmacotherapy of anxiety disorders: a critical review. Dialogues Clin Neurosci 2011; 13:423–437.
- Sheehan DV, Kamijima K. An evidence-based review of the clinical use of sertraline in mood and anxiety disorders. Int Clin Psychopharmacol 2009; 24:43–60.
- Huh J, Goebert D, Takeshita J, Lu BY, Kang M. Treatment of generalized anxiety disorder: a comprehensive review of the literature for psychopharmacologic alternatives to newer antidepressants and benzodiazepines. Prim Care Companion CNS Disord 2011; 13: 4088/PCC.08r00709blu.
- Rickels K, Downing R, Schweizer E, Hassman H. Antidepressants for the treatment of generalized anxiety disorder. A placebo-controlled comparison of imipramine, trazodone, and diazepam. Arch Gen Psychiatry 1993; 50:884–895.
- Uher R, Maier W, Hauser J, et al. Differential efficacy of escitalopram and nortriptyline on dimensional measures of depression. Br J Psychiatry 2009; 194:252–259.
- Kellner M. Drug treatment of obsessive-compulsive disorder. Dialogues Clin Neurosci 2010; 12:187–197.
- Rush AJ, Trivedi MH, Carmody TJ, et al. Response in relation to baseline anxiety levels in major depressive disorder treated with bupropion sustained release or sertraline. Neuropsychopharmacology 2001; 25:131–138.
- Mease PJ, Dundon K, Sarzi-Puttini P. Pharmacotherapy of fibromyalgia. Best Pract Res Clin Rheumatol 2011; 25:285–297.
- Wolfe F, Cathey MA, Hawley DJ. A double-blind placebo controlled trial of fluoxetine in fibromyalgia. Scand J Rheumatol 1994; 23:255–259.
- Arnold LM, Hess EV, Hudson JI, Welge JA, Berno SE, Keck PE. A randomized, placebo-controlled, double-blind, flexible-dose study of fluoxetine in the treatment of women with fibromyalgia. Am J Med 2002; 112:191–197.
- Arnold LM, Keck PE, Welge JA. Antidepressant treatment of fibromyalgia. A meta-analysis and review. Psychosomatics 2000; 41:104–113.
- Goldenberg DL, Burckhardt C, Crofford L. Management of fibromyalgia syndrome. JAMA 2004; 292:2388–2395.
- Tort S, Urrútia G, Nishishinya MB, Walitt B. Monoamine oxidase inhibitors (MAOIs) for fibromyalgia syndrome. Cochrane Database Syst Rev 2012; 4:CD009807.
- Vercoulen JH, Swanink CM, Zitman FG, et al. Randomised, double-blind, placebo-controlled study of fluoxetine in chronic fatigue syndrome. Lancet 1996; 347:858–861.
- Natelson BH, Cheu J, Pareja J, Ellis SP, Policastro T, Findley TW. Randomized, double blind, controlled placebo-phase in trial of low dose phenelzine in the chronic fatigue syndrome. Psychopharmacology (Berl) 1996; 124:226–230.
- Reid S, Chalder T, Cleare A, Hotopf M, Wessely S. Chronic fatigue syndrome. BMJ 2000; 320:292–296.
- Kupfer DJ, Spiker DG, Coble PA, Neil JF, Ulrich R, Shaw DH. Sleep and treatment prediction in endogenous depression. Am J Psychiatry 1981; 138:429–434.
- Argyropoulos SV, Hicks JA, Nash JR, et al. Redistribution of slow wave activity of sleep during pharmacological treatment of depression with paroxetine but not with nefazodone. J Sleep Res 2009; 18:342–348.
- Stein DJ, Lopez AG. Effects of escitalopram on sleep problems in patients with major depression or generalized anxiety disorder. Adv Ther 2011; 28:1021–1037.
- Ehlers CL, Havstad JW, Kupfer DJ. Estimation of the time course of slow-wave sleep over the night in depressed patients: effects of clomipramine and clinical response. Biol Psychiatry 1996; 39:171–181.
- Landolt HP, Raimo EB, Schnierow BJ, Kelsoe JR, Rapaport MH, Gillin JC. Sleep and sleep electroencephalogram in depressed patients treated with phenelzine. Arch Gen Psychiatry 2001; 58:268–276.
- Chen YM, Huang XM, Thompson R, Zhao YB. Clinical features and efficacy of escitalopram treatment for geriatric depression. J Int Med Res 2011; 39:1946–1953.
- Dolder C, Nelson M, Stump A. Pharmacological and clinical profile of newer antidepressants: implications for the treatment of elderly patients. Drugs Aging 2010; 27:625–640.
- Sterke CS, Ziere G, van Beeck EF, Looman CW, van der Cammen TJ. Dose-response relationship between selective serotonin re-uptake inhibitors and injurious falls: a study in nursing home residents with dementia. Br J Clin Pharmacol 2012; 73:812–820.
- Raji MA, Brady SR. Mirtazapine for treatment of depression and comorbidities in Alzheimer disease. Ann Pharmacother 2001; 35:1024–1027.
- Hennings JM, Schaaf L, Fulda S. Glucose metabolism and antidepressant medication. Curr Pharm Des 2012; 18:5900–5919.
- Czarny MJ, Arthurs E, Coffie DF, et al. Prevalence of antidepressant prescription or use in patients with acute coronary syndrome: a systematic review. PLoS One 2011; 6:e27671.
- Zuidersma M, Ormel J, Conradi HJ, de Jonge P. An increase in depressive symptoms after myocardial infarction predicts new cardiac events irrespective of depressive symptoms before myocardial infarction. Psychol Med 2012; 42:683–693.
- van Noord C, Straus SM, Sturkenboom MC, et al. Psychotropic drugs associated with corrected QT interval prolongation. J Clin Psychopharmacol 2009; 29:9–15.
- US Food and Drug Administration (FDA). FDA Drug Safety Communication: abnormal heart rhythms associated with high doses of Celexa (citalopram hydrobromide). http://www.fda.gov/Drugs/DrugSafety/ucm269086.htm. Accessed August 25, 2013.
- Lespérance F, Frasure-Smith N, Koszycki D, et al; CREATE Investigators. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA 2007; 297:367–379.
- O’Connor CM, Jiang W, Kuchibhatla M, et al; SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol 2010; 56:692–699.
- Glassman AH, O’Connor CM, Califf RM, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHEART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288:701–709.
- Swenson JR, O’Connor CM, Barton D, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) Group. Influence of depression and effect of treatment with sertraline on quality of life after hospitalization for acute coronary syndrome. Am J Cardiol 2003; 92:1271–1276.
- Strik JJ, Honig A, Lousberg R, et al. Efficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction: findings from a double-blind, placebo-controlled trial. Psychosom Med 2000; 62:783–789.
- Honig A, Kuyper AM, Schene AH, et al; MIND-IT investigators. Treatment of post-myocardial infarction depressive disorder: a randomized, placebo-controlled trial with mirtazapine. Psychosom Med 2007; 69:606–613.
KEY POINTS
- We suggest that clinicians become familiar with one drug from each class of antidepressants.
- Many antidepressants are also approved for conditions other than depression, and for patients who have both depression and one or more of these comcomitant conditions, these drugs can have a “two-for-one” benefit.
- Adverse effects of an antidepressant are usually predictable on the basis of the drug’s mechanism of action.
Use of deep brain stimulation in treatment-resistant depression
Deep brain stimulation (DBS) for severe, treatment-refractory depression has evolved out of both the troubled history of psychosurgery in the middle of the 20th century and the recent promising application of DBS for movement disorders and other neurologic and psychiatric conditions. This review describes the context in which DBS has emerged as an experimental therapy for refractory depression, explains the rationale for targeting stimulation to the ventral capsule/ventral striatum, and reviews promising results of preliminary clinical studies of DBS for depression.
PSYCHOSURGERY: A CLOUDED HISTORICAL BACKDROP
The use of DBS for depression is best understood within the context of the problematic history of neurosurgery for psychiatric conditions (psychosurgery), which dates back to the development of frontal leucotomy (ie, frontal lobotomy) by Egas Moniz and Pedro Lima in 1935. Walter Freeman, an American neurologist and psychiatrist without surgical training, performed the first prefrontal lobotomy in the United States in 1936. In 1945 Freeman pioneered the transorbital (“ice pick”) lobotomy, which accessed the frontal lobes through the eye sockets rather than by holes drilled in the skull. Freeman’s advocacy of lobotomy as an expedient therapy for psychiatric conditions helped fuel the procedure’s midcentury popularity, as more than 20,000 psychosurgery procedures were performed in the United States for various indications between 1936 and 1955.
Although some symptomatic improvement was seen with these psychosurgery procedures, they quickly became controversial because of their adverse effects, which included personality changes, as well as their perceived barbaric nature and their indiscriminate use by some practitioners. Moreover, little systematic research of these procedures was done, with most studies being poorly designed with little attention to long-term outcomes.
By the 1960s psychosurgery was in decline, largely because of the advent of effective psychopharmacology.
FROM BRAIN LESIONING TO BRAIN STIMULATION
Despite this decline, research on neurosurgery for the treatment of psychiatric conditions continued with small-scale studies of procedures involving smaller brain lesions, such as anterior capsulotomy and anterior cingulotomy using radiofrequency lesioning or gamma knife irradiation. Some of these studies demonstrated significant improvements, particularly in patients with severe obsessive-compulsive disorder (OCD).
These results prompted consideration of DBS for treatment of patients with severe psychiatric illness, especially since DBS offered several potential advantages relative to lesioning:
- Reversibility
- The ability to perform double-blind crossover studies
- The ability to vary stimulation sites and parameters.
Briefly, DBS for psychiatric applications involves bilateral implantation of electrodes in the anterior limb of the ventral internal capsule extending into the ventral striatum. Each electrode has four individually programmable contacts. The neurostimulator is placed in a pocket created in the subclavicular area. The leads are connected to each neurostimulator by tunneling under the scalp and the skin of the neck to the pocket, permitting noninvasive adjustment of the electrical stimulation.
EXPERIENCE WITH STIMULATION IN OBSESSIVE-COMPULSIVE DISORDER
Greenberg et al reported outcomes of the use of DBS in 26 patients with severe and highly treatment-resistant OCD treated at four collaborating centers from 2000 to 2005.1 The target for stimulation was the ventral internal capsule/ventral striatum (VC/VS); this target evolved slightly over the course of the study as it became evident that outcomes were superior with targets that were more posterior. Concomitant pharmacotherapy was permitted throughout the study.
At 3 to 6 months after initiation of chronic DBS, scores on the Yale-Brown Obsessive Compulsive Scale, a measure of OCD severity, improved by an average of nearly 50% in these patients with severe refractory disease,1 which is notably better than the 35% improvement often used as the threshold for response in OCD trials. Improvement in mood was a beneficial side effect of DBS in the study, and in patients with comorbid depression, mood improved to a greater degree than did symptoms of anxiety and OCD.
In the wake of the initial release of this study by Greenberg et al (published online in May 2008) and similar findings, the US Food and Drug Administration (FDA) in February 2009 approved DBS for use in refractory OCD under a humanitarian device exemption. Such exemptions are granted to facilitate the development of devices for rare conditions, and the exemption was applicable in light of the rarity of severe, treatment-resistant, disabling OCD.
RATIONALE FOR BRAIN STIMULATION IN DEPRESSION
A large refractory and disabled population
In contrast to OCD, treatment-refractory depression is rather common, as approximately 20% of patients with depression—roughly 4.4 million US patients—have disease that is resistant to the mainstay treatment options of antidepressant medications and psychotherapy.2 The fact that electroconvulsive therapy is performed more than 100,000 times annually in the United States is another testament to how widespread treatment-resistant depression remains. Even if only some of these patients with severely disabling and refractory depression may be candidates for DBS, they represent a considerable potential patient population.
A pathophysiologic role for the VC/VS
The target for stimulation in OCD—the VC/VS—also has a known anatomic and physiologic role in depression, which makes it an appropriate surgical target for treatment of depression as well. Significantly less VS response to positive stimuli has been observed in depressed patients compared with controls.3 Moreover, the subgenual cingulate region is known to be metabolically hyperactive in patients with major depressive disorder, and positron emission tomography studies of OCD patients who underwent DBS of the VC/VS showed a reduction in subgenual cingulate activity over time.4
White matter tracts in the area 25 region adjacent to the subgenual cingulate cortex represent another target for stimulation. In a pilot study by Mayberg et al, DBS electrodes implanted bilaterally in the subgenual cingulate cortices of 6 patients with treatment-resistant depression resulted in sustained remission of depression in 4 patients at 6 months.5 The benefit of stimulation continued for up to 4 weeks after stimulation ended.
MULTICENTER STUDY OF STIMULATION FOR HIGHLY REFRACTORY DEPRESSION
Our team at Cleveland Clinic partnered with colleagues from Brown Medical School and Massachusetts General Hospital to build on these pilot study findings and evaluate DBS of the VC/VS in patients with chronic, severe refractory depression in a multicenter investigation. The results from the first 15 patients in this series were published in early 2009;6 results from an additional 2 patients, for a total sample of 17, are now available and summarized below.
Patients and study design
Patients had at least a 5-year history of chronic or recurrent depression that was refractory to at least five courses of medication, an adequate trial of psychotherapy, and at least one trial of bilateral electroconvulsive therapy. Exclusion criteria included significant substance abuse, severe personality disorder that could potentially affect safety or compliance, and psychotic depression.
Outcome measures included the Hamilton Depression Rating Scale (HDRS), the Montgomery-Asberg Depression Rating Scale (MADRS), and the Global Assessment of Function Scale (GAF). Assessments were performed at baseline, postoperatively, and monthly thereafter. A detailed neuropsychological battery was performed at baseline and again at 6 months.
At the time of electrode implantation, mean patient age was 46.3 years and mean duration of illness was 21.0 years. In their current depressive episode, patients had had an average of 6.1 antidepressant trials and 6.1 trials of augmentation or combination of antidepressant medications. The average number of lifetime electroconvulsive therapy treatments was 30.5; of the 17 patients, 15 had an adequate trial of electroconvulsive therapy in their current depressive episode.
Electrodes were implanted bilaterally in the VC/VS. Following a postoperative recovery phase of 2 to 4 weeks, stimulation parameters were titrated over several days on an outpatient basis. The stimulation parameters were selected on the basis of positive mood benefit and absence of adverse effects. Stimulation was at a frequency of 100 to 130 Hz and an amplitude of 2.5 to 8 V. These stimulation amplitudes are higher than those used for treatment of movement disorders, reflecting the different targets (white matter vs gray matter) for the different conditions.
The two ventral contacts (referred to as contact 0 and contact 1) tend to be the most active, providing the best response. Contact 0 is the most distal contact, at the VS below the level of the anterior commissure. Contact 1 is near the junction of the VS and VC.
The time to battery replacement (due to depletion) ranged from 10 to 18 months.
Outcomes
Patients’ mean baseline MADRS score was 34.7, indicating very severe depression. The mean MADRS score improved to 20.6 by 1 month, and declined further to 16.0 at 3 months. This benefit has been maintained to the most recent follow-up (average, 37.4 months; range, 14–67 months). Similar improvements from baseline to most recent follow-up were observed in the HDRS and GAF scores. Additionally, a substantial reduction in suicidality (as measured by mean MADRS suicide subscale score) was observed by 1 month (P = .01) and was maintained through 12 months of follow-up (P < .001).7
Adverse effects
Adverse effects of DBS were observed on occasion and can generally be divided into those related to surgical implantation and those related to stimulation itself.
Effects related to surgical implantation have included infection from lead or battery implantation, adverse cosmetic effects (from placement of the battery-operated neurostimulators into the chest), and repeat surgeries for neurostimulator replacements. A rechargeable battery has recently become available and should enhance tolerability and acceptability by reducing the frequency of replacement surgeries.
Stimulation-induced acute adverse events have included paresthesias, anxiety, mood changes, and autonomic effects. All were reversible with adjustment of stimulation parameters.
DIRECTION AND GUIDANCE FOR FUTURE RESEARCH
A number of recent developments have enhanced the prospects for better understanding of the use of DBS in treatment-refractory depression:
- The recent FDA approval of DBS for severe, refractory OCD should broaden the base of experience with DBS for psychiatric disorders.
- Two large studies of DBS of the VC/VS and the area 25/subgenual cingulate region in depressed patients are currently under way.
- The aforementioned recent development of a rechargeable stimulator battery should improve patient acceptance of DBS therapy.
- Neuroimaging studies using functional magnetic resonance imaging and positron emission tomography may help to elucidate neuroanatomic pathways in depression and other psychiatric disorders.
- Ongoing studies of DBS for Tourette syndrome will broaden the experience base with DBS and perhaps yield insights for depression.
As investigation of DBS for depression moves forward, it must be conducted in keeping with some basic principles for patient selection and fundamental ethical guidelines, especially in light of the troubled early history of psychosurgery. From the individual patient perspective, patients should be selected only if they meet the following criteria:
- Accurate diagnosis. This may seem obvious, yet inaccurate diagnoses in the psychiatric realm are far more widespread than is appreciated but clearly must be avoided when embarking on an intervention as significant as DBS.
- Ability to provide informed consent
- Sufficient severity of illness
- Nonresponse to less-invasive options (ie, reasonable trials of both pharmacotherapy and psychotherapy).
From the ethical and procedural perspective, research of DBS for psychiatric disease must ensure the involvement of expert and dedicated psychiatric neurosurgery teams, led by psychiatrists, as well as full ethical review (by institutional review boards) and method-safety review (in keeping with FDA policy). Additionally, expert centers must be prepared to make the long-term commitment necessary to follow these difficult-to-treat patients. Centers and investigators must also ensure that DBS be used only to alleviate suffering and improve patients’ lives, and never to “augment” normal function or for social or political reasons.9
- Greenberg BD, Gabriels LA, Malone DA, et al Deep brain stimulation of the ventral internal capsule/ventral striatum for obsessive-compulsive disorder: worldwide experience. Molecular Psychiatry 2010; 15:64–79.
- Fava M. Diagnosis and definition of treatment-resistant depression. Biol Psychiatry 2003; 53:649–659.
- Epstein J, Pan H, Kocsis JH, et al Lack of ventral striatal response to positive stimuli in depressed versus normal subjects. Am J Psychiatry 2006; 163:1784–1790.
- Rauch SL, Dougherty DD, Malone D, et al A functional neuroimaging investigation of deep brain stimulation in patients with obsessive-compulsive disorder. J Neurosurg 2006; 104:558–565.
- Mayberg LS, Lozano AM, Voon V, et al Deep brain stimulation for treatment-resistant depression. Neuron 2005; 45:651–660.
- Malone DA, Dougherty DD, Rezai AR, et al Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression. Biol Psychiatry 2009; 65:267–275.
- Mathews M, Greenberg B, Dougherty D, et al Change in suicidal ideation in patients undergoing DBS for depression. Presented at: 2008 Biennial Meeting of the American Society for Stereotactic and Functional Neurosurgery; June 1–4, 2008; Vancouver, BC, Canada. Abstract 124. http://www.assfn.org/project/oral/124.pdf.
- Malone DA, Dougherty DD, Rezai AR, et al Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression. Presented at: Annual Meeting of the American Psychiatric Association; May 16–21, 2009; San Francisco, CA. Abstract NR6-009.
- OCD-DBS Collaborative Group. Deep brain stimulation for psychiatric disorders. Neurosurgery 2002; 51:519.
Deep brain stimulation (DBS) for severe, treatment-refractory depression has evolved out of both the troubled history of psychosurgery in the middle of the 20th century and the recent promising application of DBS for movement disorders and other neurologic and psychiatric conditions. This review describes the context in which DBS has emerged as an experimental therapy for refractory depression, explains the rationale for targeting stimulation to the ventral capsule/ventral striatum, and reviews promising results of preliminary clinical studies of DBS for depression.
PSYCHOSURGERY: A CLOUDED HISTORICAL BACKDROP
The use of DBS for depression is best understood within the context of the problematic history of neurosurgery for psychiatric conditions (psychosurgery), which dates back to the development of frontal leucotomy (ie, frontal lobotomy) by Egas Moniz and Pedro Lima in 1935. Walter Freeman, an American neurologist and psychiatrist without surgical training, performed the first prefrontal lobotomy in the United States in 1936. In 1945 Freeman pioneered the transorbital (“ice pick”) lobotomy, which accessed the frontal lobes through the eye sockets rather than by holes drilled in the skull. Freeman’s advocacy of lobotomy as an expedient therapy for psychiatric conditions helped fuel the procedure’s midcentury popularity, as more than 20,000 psychosurgery procedures were performed in the United States for various indications between 1936 and 1955.
Although some symptomatic improvement was seen with these psychosurgery procedures, they quickly became controversial because of their adverse effects, which included personality changes, as well as their perceived barbaric nature and their indiscriminate use by some practitioners. Moreover, little systematic research of these procedures was done, with most studies being poorly designed with little attention to long-term outcomes.
By the 1960s psychosurgery was in decline, largely because of the advent of effective psychopharmacology.
FROM BRAIN LESIONING TO BRAIN STIMULATION
Despite this decline, research on neurosurgery for the treatment of psychiatric conditions continued with small-scale studies of procedures involving smaller brain lesions, such as anterior capsulotomy and anterior cingulotomy using radiofrequency lesioning or gamma knife irradiation. Some of these studies demonstrated significant improvements, particularly in patients with severe obsessive-compulsive disorder (OCD).
These results prompted consideration of DBS for treatment of patients with severe psychiatric illness, especially since DBS offered several potential advantages relative to lesioning:
- Reversibility
- The ability to perform double-blind crossover studies
- The ability to vary stimulation sites and parameters.
Briefly, DBS for psychiatric applications involves bilateral implantation of electrodes in the anterior limb of the ventral internal capsule extending into the ventral striatum. Each electrode has four individually programmable contacts. The neurostimulator is placed in a pocket created in the subclavicular area. The leads are connected to each neurostimulator by tunneling under the scalp and the skin of the neck to the pocket, permitting noninvasive adjustment of the electrical stimulation.
EXPERIENCE WITH STIMULATION IN OBSESSIVE-COMPULSIVE DISORDER
Greenberg et al reported outcomes of the use of DBS in 26 patients with severe and highly treatment-resistant OCD treated at four collaborating centers from 2000 to 2005.1 The target for stimulation was the ventral internal capsule/ventral striatum (VC/VS); this target evolved slightly over the course of the study as it became evident that outcomes were superior with targets that were more posterior. Concomitant pharmacotherapy was permitted throughout the study.
At 3 to 6 months after initiation of chronic DBS, scores on the Yale-Brown Obsessive Compulsive Scale, a measure of OCD severity, improved by an average of nearly 50% in these patients with severe refractory disease,1 which is notably better than the 35% improvement often used as the threshold for response in OCD trials. Improvement in mood was a beneficial side effect of DBS in the study, and in patients with comorbid depression, mood improved to a greater degree than did symptoms of anxiety and OCD.
In the wake of the initial release of this study by Greenberg et al (published online in May 2008) and similar findings, the US Food and Drug Administration (FDA) in February 2009 approved DBS for use in refractory OCD under a humanitarian device exemption. Such exemptions are granted to facilitate the development of devices for rare conditions, and the exemption was applicable in light of the rarity of severe, treatment-resistant, disabling OCD.
RATIONALE FOR BRAIN STIMULATION IN DEPRESSION
A large refractory and disabled population
In contrast to OCD, treatment-refractory depression is rather common, as approximately 20% of patients with depression—roughly 4.4 million US patients—have disease that is resistant to the mainstay treatment options of antidepressant medications and psychotherapy.2 The fact that electroconvulsive therapy is performed more than 100,000 times annually in the United States is another testament to how widespread treatment-resistant depression remains. Even if only some of these patients with severely disabling and refractory depression may be candidates for DBS, they represent a considerable potential patient population.
A pathophysiologic role for the VC/VS
The target for stimulation in OCD—the VC/VS—also has a known anatomic and physiologic role in depression, which makes it an appropriate surgical target for treatment of depression as well. Significantly less VS response to positive stimuli has been observed in depressed patients compared with controls.3 Moreover, the subgenual cingulate region is known to be metabolically hyperactive in patients with major depressive disorder, and positron emission tomography studies of OCD patients who underwent DBS of the VC/VS showed a reduction in subgenual cingulate activity over time.4
White matter tracts in the area 25 region adjacent to the subgenual cingulate cortex represent another target for stimulation. In a pilot study by Mayberg et al, DBS electrodes implanted bilaterally in the subgenual cingulate cortices of 6 patients with treatment-resistant depression resulted in sustained remission of depression in 4 patients at 6 months.5 The benefit of stimulation continued for up to 4 weeks after stimulation ended.
MULTICENTER STUDY OF STIMULATION FOR HIGHLY REFRACTORY DEPRESSION
Our team at Cleveland Clinic partnered with colleagues from Brown Medical School and Massachusetts General Hospital to build on these pilot study findings and evaluate DBS of the VC/VS in patients with chronic, severe refractory depression in a multicenter investigation. The results from the first 15 patients in this series were published in early 2009;6 results from an additional 2 patients, for a total sample of 17, are now available and summarized below.
Patients and study design
Patients had at least a 5-year history of chronic or recurrent depression that was refractory to at least five courses of medication, an adequate trial of psychotherapy, and at least one trial of bilateral electroconvulsive therapy. Exclusion criteria included significant substance abuse, severe personality disorder that could potentially affect safety or compliance, and psychotic depression.
Outcome measures included the Hamilton Depression Rating Scale (HDRS), the Montgomery-Asberg Depression Rating Scale (MADRS), and the Global Assessment of Function Scale (GAF). Assessments were performed at baseline, postoperatively, and monthly thereafter. A detailed neuropsychological battery was performed at baseline and again at 6 months.
At the time of electrode implantation, mean patient age was 46.3 years and mean duration of illness was 21.0 years. In their current depressive episode, patients had had an average of 6.1 antidepressant trials and 6.1 trials of augmentation or combination of antidepressant medications. The average number of lifetime electroconvulsive therapy treatments was 30.5; of the 17 patients, 15 had an adequate trial of electroconvulsive therapy in their current depressive episode.
Electrodes were implanted bilaterally in the VC/VS. Following a postoperative recovery phase of 2 to 4 weeks, stimulation parameters were titrated over several days on an outpatient basis. The stimulation parameters were selected on the basis of positive mood benefit and absence of adverse effects. Stimulation was at a frequency of 100 to 130 Hz and an amplitude of 2.5 to 8 V. These stimulation amplitudes are higher than those used for treatment of movement disorders, reflecting the different targets (white matter vs gray matter) for the different conditions.
The two ventral contacts (referred to as contact 0 and contact 1) tend to be the most active, providing the best response. Contact 0 is the most distal contact, at the VS below the level of the anterior commissure. Contact 1 is near the junction of the VS and VC.
The time to battery replacement (due to depletion) ranged from 10 to 18 months.
Outcomes
Patients’ mean baseline MADRS score was 34.7, indicating very severe depression. The mean MADRS score improved to 20.6 by 1 month, and declined further to 16.0 at 3 months. This benefit has been maintained to the most recent follow-up (average, 37.4 months; range, 14–67 months). Similar improvements from baseline to most recent follow-up were observed in the HDRS and GAF scores. Additionally, a substantial reduction in suicidality (as measured by mean MADRS suicide subscale score) was observed by 1 month (P = .01) and was maintained through 12 months of follow-up (P < .001).7
Adverse effects
Adverse effects of DBS were observed on occasion and can generally be divided into those related to surgical implantation and those related to stimulation itself.
Effects related to surgical implantation have included infection from lead or battery implantation, adverse cosmetic effects (from placement of the battery-operated neurostimulators into the chest), and repeat surgeries for neurostimulator replacements. A rechargeable battery has recently become available and should enhance tolerability and acceptability by reducing the frequency of replacement surgeries.
Stimulation-induced acute adverse events have included paresthesias, anxiety, mood changes, and autonomic effects. All were reversible with adjustment of stimulation parameters.
DIRECTION AND GUIDANCE FOR FUTURE RESEARCH
A number of recent developments have enhanced the prospects for better understanding of the use of DBS in treatment-refractory depression:
- The recent FDA approval of DBS for severe, refractory OCD should broaden the base of experience with DBS for psychiatric disorders.
- Two large studies of DBS of the VC/VS and the area 25/subgenual cingulate region in depressed patients are currently under way.
- The aforementioned recent development of a rechargeable stimulator battery should improve patient acceptance of DBS therapy.
- Neuroimaging studies using functional magnetic resonance imaging and positron emission tomography may help to elucidate neuroanatomic pathways in depression and other psychiatric disorders.
- Ongoing studies of DBS for Tourette syndrome will broaden the experience base with DBS and perhaps yield insights for depression.
As investigation of DBS for depression moves forward, it must be conducted in keeping with some basic principles for patient selection and fundamental ethical guidelines, especially in light of the troubled early history of psychosurgery. From the individual patient perspective, patients should be selected only if they meet the following criteria:
- Accurate diagnosis. This may seem obvious, yet inaccurate diagnoses in the psychiatric realm are far more widespread than is appreciated but clearly must be avoided when embarking on an intervention as significant as DBS.
- Ability to provide informed consent
- Sufficient severity of illness
- Nonresponse to less-invasive options (ie, reasonable trials of both pharmacotherapy and psychotherapy).
From the ethical and procedural perspective, research of DBS for psychiatric disease must ensure the involvement of expert and dedicated psychiatric neurosurgery teams, led by psychiatrists, as well as full ethical review (by institutional review boards) and method-safety review (in keeping with FDA policy). Additionally, expert centers must be prepared to make the long-term commitment necessary to follow these difficult-to-treat patients. Centers and investigators must also ensure that DBS be used only to alleviate suffering and improve patients’ lives, and never to “augment” normal function or for social or political reasons.9
Deep brain stimulation (DBS) for severe, treatment-refractory depression has evolved out of both the troubled history of psychosurgery in the middle of the 20th century and the recent promising application of DBS for movement disorders and other neurologic and psychiatric conditions. This review describes the context in which DBS has emerged as an experimental therapy for refractory depression, explains the rationale for targeting stimulation to the ventral capsule/ventral striatum, and reviews promising results of preliminary clinical studies of DBS for depression.
PSYCHOSURGERY: A CLOUDED HISTORICAL BACKDROP
The use of DBS for depression is best understood within the context of the problematic history of neurosurgery for psychiatric conditions (psychosurgery), which dates back to the development of frontal leucotomy (ie, frontal lobotomy) by Egas Moniz and Pedro Lima in 1935. Walter Freeman, an American neurologist and psychiatrist without surgical training, performed the first prefrontal lobotomy in the United States in 1936. In 1945 Freeman pioneered the transorbital (“ice pick”) lobotomy, which accessed the frontal lobes through the eye sockets rather than by holes drilled in the skull. Freeman’s advocacy of lobotomy as an expedient therapy for psychiatric conditions helped fuel the procedure’s midcentury popularity, as more than 20,000 psychosurgery procedures were performed in the United States for various indications between 1936 and 1955.
Although some symptomatic improvement was seen with these psychosurgery procedures, they quickly became controversial because of their adverse effects, which included personality changes, as well as their perceived barbaric nature and their indiscriminate use by some practitioners. Moreover, little systematic research of these procedures was done, with most studies being poorly designed with little attention to long-term outcomes.
By the 1960s psychosurgery was in decline, largely because of the advent of effective psychopharmacology.
FROM BRAIN LESIONING TO BRAIN STIMULATION
Despite this decline, research on neurosurgery for the treatment of psychiatric conditions continued with small-scale studies of procedures involving smaller brain lesions, such as anterior capsulotomy and anterior cingulotomy using radiofrequency lesioning or gamma knife irradiation. Some of these studies demonstrated significant improvements, particularly in patients with severe obsessive-compulsive disorder (OCD).
These results prompted consideration of DBS for treatment of patients with severe psychiatric illness, especially since DBS offered several potential advantages relative to lesioning:
- Reversibility
- The ability to perform double-blind crossover studies
- The ability to vary stimulation sites and parameters.
Briefly, DBS for psychiatric applications involves bilateral implantation of electrodes in the anterior limb of the ventral internal capsule extending into the ventral striatum. Each electrode has four individually programmable contacts. The neurostimulator is placed in a pocket created in the subclavicular area. The leads are connected to each neurostimulator by tunneling under the scalp and the skin of the neck to the pocket, permitting noninvasive adjustment of the electrical stimulation.
EXPERIENCE WITH STIMULATION IN OBSESSIVE-COMPULSIVE DISORDER
Greenberg et al reported outcomes of the use of DBS in 26 patients with severe and highly treatment-resistant OCD treated at four collaborating centers from 2000 to 2005.1 The target for stimulation was the ventral internal capsule/ventral striatum (VC/VS); this target evolved slightly over the course of the study as it became evident that outcomes were superior with targets that were more posterior. Concomitant pharmacotherapy was permitted throughout the study.
At 3 to 6 months after initiation of chronic DBS, scores on the Yale-Brown Obsessive Compulsive Scale, a measure of OCD severity, improved by an average of nearly 50% in these patients with severe refractory disease,1 which is notably better than the 35% improvement often used as the threshold for response in OCD trials. Improvement in mood was a beneficial side effect of DBS in the study, and in patients with comorbid depression, mood improved to a greater degree than did symptoms of anxiety and OCD.
In the wake of the initial release of this study by Greenberg et al (published online in May 2008) and similar findings, the US Food and Drug Administration (FDA) in February 2009 approved DBS for use in refractory OCD under a humanitarian device exemption. Such exemptions are granted to facilitate the development of devices for rare conditions, and the exemption was applicable in light of the rarity of severe, treatment-resistant, disabling OCD.
RATIONALE FOR BRAIN STIMULATION IN DEPRESSION
A large refractory and disabled population
In contrast to OCD, treatment-refractory depression is rather common, as approximately 20% of patients with depression—roughly 4.4 million US patients—have disease that is resistant to the mainstay treatment options of antidepressant medications and psychotherapy.2 The fact that electroconvulsive therapy is performed more than 100,000 times annually in the United States is another testament to how widespread treatment-resistant depression remains. Even if only some of these patients with severely disabling and refractory depression may be candidates for DBS, they represent a considerable potential patient population.
A pathophysiologic role for the VC/VS
The target for stimulation in OCD—the VC/VS—also has a known anatomic and physiologic role in depression, which makes it an appropriate surgical target for treatment of depression as well. Significantly less VS response to positive stimuli has been observed in depressed patients compared with controls.3 Moreover, the subgenual cingulate region is known to be metabolically hyperactive in patients with major depressive disorder, and positron emission tomography studies of OCD patients who underwent DBS of the VC/VS showed a reduction in subgenual cingulate activity over time.4
White matter tracts in the area 25 region adjacent to the subgenual cingulate cortex represent another target for stimulation. In a pilot study by Mayberg et al, DBS electrodes implanted bilaterally in the subgenual cingulate cortices of 6 patients with treatment-resistant depression resulted in sustained remission of depression in 4 patients at 6 months.5 The benefit of stimulation continued for up to 4 weeks after stimulation ended.
MULTICENTER STUDY OF STIMULATION FOR HIGHLY REFRACTORY DEPRESSION
Our team at Cleveland Clinic partnered with colleagues from Brown Medical School and Massachusetts General Hospital to build on these pilot study findings and evaluate DBS of the VC/VS in patients with chronic, severe refractory depression in a multicenter investigation. The results from the first 15 patients in this series were published in early 2009;6 results from an additional 2 patients, for a total sample of 17, are now available and summarized below.
Patients and study design
Patients had at least a 5-year history of chronic or recurrent depression that was refractory to at least five courses of medication, an adequate trial of psychotherapy, and at least one trial of bilateral electroconvulsive therapy. Exclusion criteria included significant substance abuse, severe personality disorder that could potentially affect safety or compliance, and psychotic depression.
Outcome measures included the Hamilton Depression Rating Scale (HDRS), the Montgomery-Asberg Depression Rating Scale (MADRS), and the Global Assessment of Function Scale (GAF). Assessments were performed at baseline, postoperatively, and monthly thereafter. A detailed neuropsychological battery was performed at baseline and again at 6 months.
At the time of electrode implantation, mean patient age was 46.3 years and mean duration of illness was 21.0 years. In their current depressive episode, patients had had an average of 6.1 antidepressant trials and 6.1 trials of augmentation or combination of antidepressant medications. The average number of lifetime electroconvulsive therapy treatments was 30.5; of the 17 patients, 15 had an adequate trial of electroconvulsive therapy in their current depressive episode.
Electrodes were implanted bilaterally in the VC/VS. Following a postoperative recovery phase of 2 to 4 weeks, stimulation parameters were titrated over several days on an outpatient basis. The stimulation parameters were selected on the basis of positive mood benefit and absence of adverse effects. Stimulation was at a frequency of 100 to 130 Hz and an amplitude of 2.5 to 8 V. These stimulation amplitudes are higher than those used for treatment of movement disorders, reflecting the different targets (white matter vs gray matter) for the different conditions.
The two ventral contacts (referred to as contact 0 and contact 1) tend to be the most active, providing the best response. Contact 0 is the most distal contact, at the VS below the level of the anterior commissure. Contact 1 is near the junction of the VS and VC.
The time to battery replacement (due to depletion) ranged from 10 to 18 months.
Outcomes
Patients’ mean baseline MADRS score was 34.7, indicating very severe depression. The mean MADRS score improved to 20.6 by 1 month, and declined further to 16.0 at 3 months. This benefit has been maintained to the most recent follow-up (average, 37.4 months; range, 14–67 months). Similar improvements from baseline to most recent follow-up were observed in the HDRS and GAF scores. Additionally, a substantial reduction in suicidality (as measured by mean MADRS suicide subscale score) was observed by 1 month (P = .01) and was maintained through 12 months of follow-up (P < .001).7
Adverse effects
Adverse effects of DBS were observed on occasion and can generally be divided into those related to surgical implantation and those related to stimulation itself.
Effects related to surgical implantation have included infection from lead or battery implantation, adverse cosmetic effects (from placement of the battery-operated neurostimulators into the chest), and repeat surgeries for neurostimulator replacements. A rechargeable battery has recently become available and should enhance tolerability and acceptability by reducing the frequency of replacement surgeries.
Stimulation-induced acute adverse events have included paresthesias, anxiety, mood changes, and autonomic effects. All were reversible with adjustment of stimulation parameters.
DIRECTION AND GUIDANCE FOR FUTURE RESEARCH
A number of recent developments have enhanced the prospects for better understanding of the use of DBS in treatment-refractory depression:
- The recent FDA approval of DBS for severe, refractory OCD should broaden the base of experience with DBS for psychiatric disorders.
- Two large studies of DBS of the VC/VS and the area 25/subgenual cingulate region in depressed patients are currently under way.
- The aforementioned recent development of a rechargeable stimulator battery should improve patient acceptance of DBS therapy.
- Neuroimaging studies using functional magnetic resonance imaging and positron emission tomography may help to elucidate neuroanatomic pathways in depression and other psychiatric disorders.
- Ongoing studies of DBS for Tourette syndrome will broaden the experience base with DBS and perhaps yield insights for depression.
As investigation of DBS for depression moves forward, it must be conducted in keeping with some basic principles for patient selection and fundamental ethical guidelines, especially in light of the troubled early history of psychosurgery. From the individual patient perspective, patients should be selected only if they meet the following criteria:
- Accurate diagnosis. This may seem obvious, yet inaccurate diagnoses in the psychiatric realm are far more widespread than is appreciated but clearly must be avoided when embarking on an intervention as significant as DBS.
- Ability to provide informed consent
- Sufficient severity of illness
- Nonresponse to less-invasive options (ie, reasonable trials of both pharmacotherapy and psychotherapy).
From the ethical and procedural perspective, research of DBS for psychiatric disease must ensure the involvement of expert and dedicated psychiatric neurosurgery teams, led by psychiatrists, as well as full ethical review (by institutional review boards) and method-safety review (in keeping with FDA policy). Additionally, expert centers must be prepared to make the long-term commitment necessary to follow these difficult-to-treat patients. Centers and investigators must also ensure that DBS be used only to alleviate suffering and improve patients’ lives, and never to “augment” normal function or for social or political reasons.9
- Greenberg BD, Gabriels LA, Malone DA, et al Deep brain stimulation of the ventral internal capsule/ventral striatum for obsessive-compulsive disorder: worldwide experience. Molecular Psychiatry 2010; 15:64–79.
- Fava M. Diagnosis and definition of treatment-resistant depression. Biol Psychiatry 2003; 53:649–659.
- Epstein J, Pan H, Kocsis JH, et al Lack of ventral striatal response to positive stimuli in depressed versus normal subjects. Am J Psychiatry 2006; 163:1784–1790.
- Rauch SL, Dougherty DD, Malone D, et al A functional neuroimaging investigation of deep brain stimulation in patients with obsessive-compulsive disorder. J Neurosurg 2006; 104:558–565.
- Mayberg LS, Lozano AM, Voon V, et al Deep brain stimulation for treatment-resistant depression. Neuron 2005; 45:651–660.
- Malone DA, Dougherty DD, Rezai AR, et al Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression. Biol Psychiatry 2009; 65:267–275.
- Mathews M, Greenberg B, Dougherty D, et al Change in suicidal ideation in patients undergoing DBS for depression. Presented at: 2008 Biennial Meeting of the American Society for Stereotactic and Functional Neurosurgery; June 1–4, 2008; Vancouver, BC, Canada. Abstract 124. http://www.assfn.org/project/oral/124.pdf.
- Malone DA, Dougherty DD, Rezai AR, et al Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression. Presented at: Annual Meeting of the American Psychiatric Association; May 16–21, 2009; San Francisco, CA. Abstract NR6-009.
- OCD-DBS Collaborative Group. Deep brain stimulation for psychiatric disorders. Neurosurgery 2002; 51:519.
- Greenberg BD, Gabriels LA, Malone DA, et al Deep brain stimulation of the ventral internal capsule/ventral striatum for obsessive-compulsive disorder: worldwide experience. Molecular Psychiatry 2010; 15:64–79.
- Fava M. Diagnosis and definition of treatment-resistant depression. Biol Psychiatry 2003; 53:649–659.
- Epstein J, Pan H, Kocsis JH, et al Lack of ventral striatal response to positive stimuli in depressed versus normal subjects. Am J Psychiatry 2006; 163:1784–1790.
- Rauch SL, Dougherty DD, Malone D, et al A functional neuroimaging investigation of deep brain stimulation in patients with obsessive-compulsive disorder. J Neurosurg 2006; 104:558–565.
- Mayberg LS, Lozano AM, Voon V, et al Deep brain stimulation for treatment-resistant depression. Neuron 2005; 45:651–660.
- Malone DA, Dougherty DD, Rezai AR, et al Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression. Biol Psychiatry 2009; 65:267–275.
- Mathews M, Greenberg B, Dougherty D, et al Change in suicidal ideation in patients undergoing DBS for depression. Presented at: 2008 Biennial Meeting of the American Society for Stereotactic and Functional Neurosurgery; June 1–4, 2008; Vancouver, BC, Canada. Abstract 124. http://www.assfn.org/project/oral/124.pdf.
- Malone DA, Dougherty DD, Rezai AR, et al Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression. Presented at: Annual Meeting of the American Psychiatric Association; May 16–21, 2009; San Francisco, CA. Abstract NR6-009.
- OCD-DBS Collaborative Group. Deep brain stimulation for psychiatric disorders. Neurosurgery 2002; 51:519.