User login
Systemic Racism and Health Disparities: A Statement from Editors of Family Medicine Journals
The year 2020 was marked by historic protests across the United States and the globe sparked by the deaths of George Floyd, Ahmaud Arbery, Breonna Taylor, and so many other Black people. The protests heightened awareness of racism as a public health crisis and triggered an antiracism movement. Racism is a pervasive and systemic issue that has profound adverse effects on health.1,2 Racism is associated with poorer mental and physical health outcomes and negative patient experiences in the health care system.3,4 As evidenced by the current coronavirus pandemic, race is a sociopolitical construct that continues to disadvantage Black, Latinx, Indigenous, and other People of Color.5,6,7,8 The association between racism and adverse health outcomes has been discussed for decades in the medical literature, including the family medicine literature. Today there is a renewed call to action for family medicine, a specialty that emerged as a counterculture to reform mainstream medicine,9 to both confront systemic racism and eliminate health disparities. This effort will require collaboration, commitment, education, and transformative conversations around racism, health inequity, and advocacy so that we can better serve our patients and our communities.
The editors of several North American family medicine publications have come together to address this call to action and share resources on racism across our readerships. We acknowledge those members of the family medicine scholar community who have been fighting for equity consistent with the Black Lives Matter movement by writing about racism, health inequities, and personal experiences of practicing as Black family physicians. While we recognize that much more work is needed, we want to amplify these voices. We have compiled a bibliography of scholarship generated by the family medicine community on the topic of racism in medicine.
The collection can be accessed here.
While this list is likely not complete, it does include over 250 published manuscripts and demonstrates expertise as well as a commitment to addressing these complex issues. For example, in 2016, Dr. J. Nwando Olayiwola, chair of the Department of Family Medicine at Ohio State University, wrote an essay on her experiences taking care of patients as a Black family physician.10 In January of 2019, Family Medicine published an entire issue devoted to racism in education and training.11 Dr. Eduardo Medina, a family physician and public health scholar, co-authored a call to action in 2016 for health professionals to dismantle structural racism and support Black lives to achieve health equity. His recent 2020 article builds on that theme and describes the disproportionate deaths of Black people due to racial injustice and the COVID-19 pandemic as converging public health emergencies.12,13 In the wake of these emergencies a fundamental transformation is warranted, and family physicians can play a key role.
We, the editors of family medicine journals, commit to actively examine the effects of racism on society and health and to take action to eliminate structural racism in our editorial processes. As an intellectual home for our profession, we have a unique responsibility and opportunity to educate and continue the conversation about institutional racism, health inequities, and antiracism in medicine. We will take immediate steps to enact tangible advances on these fronts. We will encourage and mentor authors from groups underrepresented in medicine. We will ensure that content includes an emphasis on cultural humility, diversity and inclusion, implicit bias, and the impact of racism on medicine and health. We will recruit editors and editorial board members from groups underrepresented in medicine. We will encourage collaboration and accountability within our specialty to confront systemic racism through content and processes in all of our individual publications. We recognize that these are small steps in an ongoing process of active antiracism, but we believe these steps are crucial. As editors in family medicine, we are committed to progress toward equity and justice.
Simultaneously published in American Family Physician, Annals of Family Medicine, Canadian Family Physician, Family Medicine, FP Essentials, FPIN/Evidence Based Practice, FPM, Journal of the American Board of Family Medicine, The Journal of Family Practice, and PRiMER.
Acknowledgement –
The authors thank Renee Crichlow, MD, Byron Jasper, MD, MPH, and Victoria Murrain, DO, for their insightful comments on this editorial.
1. Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Smedley BD, Stith AY, Nelson AR, eds. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003.
2. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453-1463.
3. Ben J, Cormack D, Harris R, Paradies Y. Racism and health service utilisation: A systematic review and meta-analysis. PLoS One. 2017;12(12):e0189900.
4. Paradies Y, Ben J, Denson N, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0138511.
5. American Academy of Family Physicians. Institutional racism in the health care system. Published 2019. Accessed Sept. 15, 2020. https://www.aafp.org/about/policies/all/institutional-racism.html.
6. Yaya S, Yeboah H, Charles CH, Otu A, Labonte R. Ethnic and racial disparities in COVID-19-related deaths: counting the trees, hiding the forest. BMJ Glob Health. 2020;5(6):e002913.
7. Egede LE, Walker RJ. Structural Racism, Social Risk Factors, and Covid-19 — A Dangerous Convergence for Black Americans [published online ahead of print, 2020 Jul 22]. N Engl J Med. 2020;10.1056/NEJMp2023616.
8. Centers for Disease Control and Prevention. Health equity considerations and racial and ethnic minority groups. Updated July 24, 2020. Accessed Sept. 15, 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html
9. Stephens GG. Family medicine as counterculture. Fam Med. 1989;21(2):103-109.
10. Olayiwola JN. Racism in medicine: shifting the power. Ann Fam Med. 2016;14(3):267-269. https://doi.org/10.1370/afm.1932.
11. Saultz J, ed. Racism. Fam Med. 2019;51(1, theme issue):1-66.
12. Hardeman RR, Medina EM, Kozhimannil KB. Structural racism and supporting black lives - the role of health professionals. N Engl J Med. 2016;375(22):2113-2115. https://doi.org/10.1056/NEJMp1609535.
13. Hardeman RR, Medina EM, Boyd RW. Stolen breaths. N Engl J Med. 2020;383(3):197-199. 10.1056/NEJMp2021072.
The year 2020 was marked by historic protests across the United States and the globe sparked by the deaths of George Floyd, Ahmaud Arbery, Breonna Taylor, and so many other Black people. The protests heightened awareness of racism as a public health crisis and triggered an antiracism movement. Racism is a pervasive and systemic issue that has profound adverse effects on health.1,2 Racism is associated with poorer mental and physical health outcomes and negative patient experiences in the health care system.3,4 As evidenced by the current coronavirus pandemic, race is a sociopolitical construct that continues to disadvantage Black, Latinx, Indigenous, and other People of Color.5,6,7,8 The association between racism and adverse health outcomes has been discussed for decades in the medical literature, including the family medicine literature. Today there is a renewed call to action for family medicine, a specialty that emerged as a counterculture to reform mainstream medicine,9 to both confront systemic racism and eliminate health disparities. This effort will require collaboration, commitment, education, and transformative conversations around racism, health inequity, and advocacy so that we can better serve our patients and our communities.
The editors of several North American family medicine publications have come together to address this call to action and share resources on racism across our readerships. We acknowledge those members of the family medicine scholar community who have been fighting for equity consistent with the Black Lives Matter movement by writing about racism, health inequities, and personal experiences of practicing as Black family physicians. While we recognize that much more work is needed, we want to amplify these voices. We have compiled a bibliography of scholarship generated by the family medicine community on the topic of racism in medicine.
The collection can be accessed here.
While this list is likely not complete, it does include over 250 published manuscripts and demonstrates expertise as well as a commitment to addressing these complex issues. For example, in 2016, Dr. J. Nwando Olayiwola, chair of the Department of Family Medicine at Ohio State University, wrote an essay on her experiences taking care of patients as a Black family physician.10 In January of 2019, Family Medicine published an entire issue devoted to racism in education and training.11 Dr. Eduardo Medina, a family physician and public health scholar, co-authored a call to action in 2016 for health professionals to dismantle structural racism and support Black lives to achieve health equity. His recent 2020 article builds on that theme and describes the disproportionate deaths of Black people due to racial injustice and the COVID-19 pandemic as converging public health emergencies.12,13 In the wake of these emergencies a fundamental transformation is warranted, and family physicians can play a key role.
We, the editors of family medicine journals, commit to actively examine the effects of racism on society and health and to take action to eliminate structural racism in our editorial processes. As an intellectual home for our profession, we have a unique responsibility and opportunity to educate and continue the conversation about institutional racism, health inequities, and antiracism in medicine. We will take immediate steps to enact tangible advances on these fronts. We will encourage and mentor authors from groups underrepresented in medicine. We will ensure that content includes an emphasis on cultural humility, diversity and inclusion, implicit bias, and the impact of racism on medicine and health. We will recruit editors and editorial board members from groups underrepresented in medicine. We will encourage collaboration and accountability within our specialty to confront systemic racism through content and processes in all of our individual publications. We recognize that these are small steps in an ongoing process of active antiracism, but we believe these steps are crucial. As editors in family medicine, we are committed to progress toward equity and justice.
Simultaneously published in American Family Physician, Annals of Family Medicine, Canadian Family Physician, Family Medicine, FP Essentials, FPIN/Evidence Based Practice, FPM, Journal of the American Board of Family Medicine, The Journal of Family Practice, and PRiMER.
Acknowledgement –
The authors thank Renee Crichlow, MD, Byron Jasper, MD, MPH, and Victoria Murrain, DO, for their insightful comments on this editorial.
The year 2020 was marked by historic protests across the United States and the globe sparked by the deaths of George Floyd, Ahmaud Arbery, Breonna Taylor, and so many other Black people. The protests heightened awareness of racism as a public health crisis and triggered an antiracism movement. Racism is a pervasive and systemic issue that has profound adverse effects on health.1,2 Racism is associated with poorer mental and physical health outcomes and negative patient experiences in the health care system.3,4 As evidenced by the current coronavirus pandemic, race is a sociopolitical construct that continues to disadvantage Black, Latinx, Indigenous, and other People of Color.5,6,7,8 The association between racism and adverse health outcomes has been discussed for decades in the medical literature, including the family medicine literature. Today there is a renewed call to action for family medicine, a specialty that emerged as a counterculture to reform mainstream medicine,9 to both confront systemic racism and eliminate health disparities. This effort will require collaboration, commitment, education, and transformative conversations around racism, health inequity, and advocacy so that we can better serve our patients and our communities.
The editors of several North American family medicine publications have come together to address this call to action and share resources on racism across our readerships. We acknowledge those members of the family medicine scholar community who have been fighting for equity consistent with the Black Lives Matter movement by writing about racism, health inequities, and personal experiences of practicing as Black family physicians. While we recognize that much more work is needed, we want to amplify these voices. We have compiled a bibliography of scholarship generated by the family medicine community on the topic of racism in medicine.
The collection can be accessed here.
While this list is likely not complete, it does include over 250 published manuscripts and demonstrates expertise as well as a commitment to addressing these complex issues. For example, in 2016, Dr. J. Nwando Olayiwola, chair of the Department of Family Medicine at Ohio State University, wrote an essay on her experiences taking care of patients as a Black family physician.10 In January of 2019, Family Medicine published an entire issue devoted to racism in education and training.11 Dr. Eduardo Medina, a family physician and public health scholar, co-authored a call to action in 2016 for health professionals to dismantle structural racism and support Black lives to achieve health equity. His recent 2020 article builds on that theme and describes the disproportionate deaths of Black people due to racial injustice and the COVID-19 pandemic as converging public health emergencies.12,13 In the wake of these emergencies a fundamental transformation is warranted, and family physicians can play a key role.
We, the editors of family medicine journals, commit to actively examine the effects of racism on society and health and to take action to eliminate structural racism in our editorial processes. As an intellectual home for our profession, we have a unique responsibility and opportunity to educate and continue the conversation about institutional racism, health inequities, and antiracism in medicine. We will take immediate steps to enact tangible advances on these fronts. We will encourage and mentor authors from groups underrepresented in medicine. We will ensure that content includes an emphasis on cultural humility, diversity and inclusion, implicit bias, and the impact of racism on medicine and health. We will recruit editors and editorial board members from groups underrepresented in medicine. We will encourage collaboration and accountability within our specialty to confront systemic racism through content and processes in all of our individual publications. We recognize that these are small steps in an ongoing process of active antiracism, but we believe these steps are crucial. As editors in family medicine, we are committed to progress toward equity and justice.
Simultaneously published in American Family Physician, Annals of Family Medicine, Canadian Family Physician, Family Medicine, FP Essentials, FPIN/Evidence Based Practice, FPM, Journal of the American Board of Family Medicine, The Journal of Family Practice, and PRiMER.
Acknowledgement –
The authors thank Renee Crichlow, MD, Byron Jasper, MD, MPH, and Victoria Murrain, DO, for their insightful comments on this editorial.
1. Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Smedley BD, Stith AY, Nelson AR, eds. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003.
2. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453-1463.
3. Ben J, Cormack D, Harris R, Paradies Y. Racism and health service utilisation: A systematic review and meta-analysis. PLoS One. 2017;12(12):e0189900.
4. Paradies Y, Ben J, Denson N, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0138511.
5. American Academy of Family Physicians. Institutional racism in the health care system. Published 2019. Accessed Sept. 15, 2020. https://www.aafp.org/about/policies/all/institutional-racism.html.
6. Yaya S, Yeboah H, Charles CH, Otu A, Labonte R. Ethnic and racial disparities in COVID-19-related deaths: counting the trees, hiding the forest. BMJ Glob Health. 2020;5(6):e002913.
7. Egede LE, Walker RJ. Structural Racism, Social Risk Factors, and Covid-19 — A Dangerous Convergence for Black Americans [published online ahead of print, 2020 Jul 22]. N Engl J Med. 2020;10.1056/NEJMp2023616.
8. Centers for Disease Control and Prevention. Health equity considerations and racial and ethnic minority groups. Updated July 24, 2020. Accessed Sept. 15, 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html
9. Stephens GG. Family medicine as counterculture. Fam Med. 1989;21(2):103-109.
10. Olayiwola JN. Racism in medicine: shifting the power. Ann Fam Med. 2016;14(3):267-269. https://doi.org/10.1370/afm.1932.
11. Saultz J, ed. Racism. Fam Med. 2019;51(1, theme issue):1-66.
12. Hardeman RR, Medina EM, Kozhimannil KB. Structural racism and supporting black lives - the role of health professionals. N Engl J Med. 2016;375(22):2113-2115. https://doi.org/10.1056/NEJMp1609535.
13. Hardeman RR, Medina EM, Boyd RW. Stolen breaths. N Engl J Med. 2020;383(3):197-199. 10.1056/NEJMp2021072.
1. Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Smedley BD, Stith AY, Nelson AR, eds. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003.
2. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453-1463.
3. Ben J, Cormack D, Harris R, Paradies Y. Racism and health service utilisation: A systematic review and meta-analysis. PLoS One. 2017;12(12):e0189900.
4. Paradies Y, Ben J, Denson N, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0138511.
5. American Academy of Family Physicians. Institutional racism in the health care system. Published 2019. Accessed Sept. 15, 2020. https://www.aafp.org/about/policies/all/institutional-racism.html.
6. Yaya S, Yeboah H, Charles CH, Otu A, Labonte R. Ethnic and racial disparities in COVID-19-related deaths: counting the trees, hiding the forest. BMJ Glob Health. 2020;5(6):e002913.
7. Egede LE, Walker RJ. Structural Racism, Social Risk Factors, and Covid-19 — A Dangerous Convergence for Black Americans [published online ahead of print, 2020 Jul 22]. N Engl J Med. 2020;10.1056/NEJMp2023616.
8. Centers for Disease Control and Prevention. Health equity considerations and racial and ethnic minority groups. Updated July 24, 2020. Accessed Sept. 15, 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html
9. Stephens GG. Family medicine as counterculture. Fam Med. 1989;21(2):103-109.
10. Olayiwola JN. Racism in medicine: shifting the power. Ann Fam Med. 2016;14(3):267-269. https://doi.org/10.1370/afm.1932.
11. Saultz J, ed. Racism. Fam Med. 2019;51(1, theme issue):1-66.
12. Hardeman RR, Medina EM, Kozhimannil KB. Structural racism and supporting black lives - the role of health professionals. N Engl J Med. 2016;375(22):2113-2115. https://doi.org/10.1056/NEJMp1609535.
13. Hardeman RR, Medina EM, Boyd RW. Stolen breaths. N Engl J Med. 2020;383(3):197-199. 10.1056/NEJMp2021072.
Alzheimer Disease: A Pragmatic Approach
Alzheimer disease (AD), the most common form of dementia, affects more than 5 million Americans.1 Estimates suggest that by 2050, the prevalence could triple, reaching 13 to 16 million.1 To effectively care for patients with AD and their families, primary care providers need to be familiar with the latest evidence on all facets of care, from initial detection to patient management and end-of-life care.
This evidence-based review will help you toward that end by answering common questions regarding Alzheimer care, including whether routine screening is advisable, what tests should be ordered, which interventions (including nonpharmacologic options) are worth considering, and how best to counsel patients and families about end-of-life care.
ROUTINE SCREENING? STILL SUBJECT TO DEBATE
The key question regarding routine dementia screening in primary care is whether it improves outcomes. Advocates note that individuals with dementia may appear unimpaired during office visits and may not report symptoms due to lack of insight; they point out, too, that waiting for an event that makes cognitive impairment obvious (eg, driving mishap) is risky.2 Those who advocate routine screening also note that only about half of those who have dementia are ever diagnosed.3
Others, including the US Preventive Services Task Force (USPSTF), disagree. In its 2014 evidence review, the USPSTF indicated that there is “insufficient evidence to assess the balance of benefits and harms of screening for cognitive impairment in older adults.”4
Mixed messages
The dearth of evidence is also reflected in the conflicting recommendations of the Affordable Care Act (ACA) and the Centers for Medicare and Medicaid Services (CMS). The ACA requires clinicians to assess cognitive function during Medicare patients’ annual wellness visits. CMS, however, instructs providers to screen for dementia only if observation or concerns raised by the patient or family suggest the possibility of impairment and does not recommend any particular test.5
Cost-effectiveness analyses also raise questions about the value of routine screening. Evidence suggests that screening 300 older patients will yield 39 positive results. But only about half of those will agree to a diagnostic evaluation, and no more than nine will ultimately be diagnosed with dementia. The estimated cost of identifying nine cases is nearly $40,000—all in the absence of a treatment to cure or stop the progression of the disorder.6
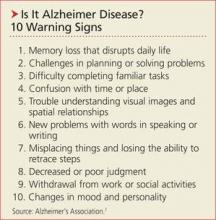
The bottom line: Evidence does not support routine dementia screening of older adults. When cognitive impairment is suspected, however, clinicians should conduct a diagnostic evaluation—and consider educating patients and families about the Alzheimer’s Association (AA)’s 10 Warning Signs of AD (see box, above).7 A longer version (www.alz.org/national/documents/checklist_10signs.pdf) outlines the cognitive changes that are characteristic of healthy aging and compares them to changes suggestive of early dementia.7
Next: How to proceed when you suspect AD >>
HOW TO PROCEED WHEN YOU SUSPECT AD
Step 1: Screening instrument. The first step in the diagnostic evaluation of a patient with suspected AD is to determine if, in fact, cognitive impairment is present. This can be assessed with in-office screening instruments, such as the Mini-Cog (http://bit.ly/1FwQAkG) or Mini-Mental State Examination (MMSE; http://bit.ly/18Djin5), among others.8
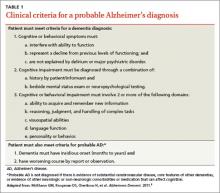
Step 2: Clinical evaluation. If observation and test results suggest cognitive impairment, the next step is to determine whether clinical findings are consistent with the diagnostic criteria for AD (see Table 1)9 developed by workgroups from the National Institute on Aging (NIA) and the AA in 2011. A work-up is necessary to identify conditions that can mimic dementia (eg, depression) and behaviors that suggest another type of dementia, such as frontotemporal or Lewy body dementia.10 Lab testing should be included to rule out potentially reversible causes of cognitive dysfunction (eg, hypothyroidism, vitamin D deficiency).
Step 3: Neuropsychologic evaluation. The NIA/AA recommends neuropsychologic testing when the brief cognitive tests, history, and clinical work-up are not sufficient for a definitive diagnosis of dementia.9 This generally involves a referral to a neuropsychologist, who conducts a battery of standardized tests to evaluate attention, memory, language, visual-spatial abilities, and executive functions, among others. Neuropsychologic testing can confirm the presence of cognitive impairment and aid in the differential diagnosis by comparing the patient’s performance in these domains with characteristic features of different dementia syndromes.
Step 4: Brain imaging with either CT or MRI can be included in the work-up for patients with suspected AD to rule out abnormalities (eg, metastatic cancer, hydrocephalus, or occult chronic subdural hematoma) that could be causing cognitive impairment.9,10 Clinical features that generally warrant brain imaging include onset of cognitive impairment before age 60; unexplained focal neurologic signs or symptoms; abrupt onset or rapid decline; and/or predisposing conditions (eg, cancer or anticoagulant treatment).10
The role of biomarkers and advanced brain imaging
Biomarkers that might provide confirmation of AD in patients who exhibit early symptoms of dementia have been studied extensively.11 The NIA/AA identified two categories of AD biomarkers
• Tests for β-amyloid deposition in the brain, including spinal fluid assays for β-amyloid (Aβ42) and positron emission tomography (PET) scans after IV injection of florbetapir or flutemetamol, which bind to amyloid in the brain; and
• Tests for neuronal degeneration, which would include spinal fluid assays for tau protein and PET scans after injection of fluorodeoxyglucose (FDG), which shows decreased uptake in patients with AD.9
Research reveals the promise of these biomarkers as diagnostic tools, particularly in patients with an atypical presentation of dementia or mild cognitive impairment (MCI) that may be associated with early AD.12 (More on MCI in a moment.) However, the NIA/AA concluded that additional research is needed to validate these tests for routine diagnostic purposes. Medicare covers PET scans with FDG only for the differential diagnosis of AD versus frontotemporal dementia.13
Continue for mild cognitive impairment >>
MILD COGNITIVE IMPAIRMENT: HOW LIKELY THAT IT WILL PROGRESS?
Along with diagnostic criteria for AD, the NIA/AA developed criteria for a symptomatic predementia phase of AD—often referred to as MCI.14 According to the workgroup, MCI is diagnosed when
1. The patient, an informant, or a clinician is concerned about the individual’s cognitive decline from previous levels of functioning
2. There is evidence of cognitive impairment, ideally through psychometric testing, revealing performance below expectation based on the patient’s age and education
3. The patient is able to maintain independent functioning in daily life, despite mild problems or the need for minimal assistance
4. There is no significant impairment in social or occupational functioning.14
Progression: Less likely than you might think
Patients with MCI are at risk for progression to overt dementia, with an overall annual conversion rate from MCI to dementia estimated at 10% to 15%.15,16 This estimate must be interpreted with caution, however, because most studies were conducted prior to the 2011 guidelines, when different diagnostic criteria were used. Observers have noted, too, that the numbers largely reflect data collected in specialty clinics and that community-based studies reveal substantially lower conversion rates (3% to 6% per year).16 In addition, evidence suggests that many patients with MCI demonstrate long-term stability or even reversal of deficits.17
While there is some consideration of the use of biomarkers and amyloid imaging tests to help determine which patients with MCI will progress to AD, practice guidelines do not currently recommend such testing and it is not covered by Medicare.
WHEN EVIDENCE INDICATES AN AD DIAGNOSIS
When faced with the need to communicate an AD diagnosis, follow the general recommendations for delivering any bad news or discouraging prognosis.
Prioritize and limit the information you provide, determining not only what the patient and family want to hear but also how much they are able to comprehend.
Confirm that the patient and family understand the information you’ve provided.
Offer emotional support and recommend additional resources (see Table 2).18
Given the progressive cognitive decline that characterizes AD, it is important to address the primary caregiver’s understanding of, and ability to cope with, the disease. It is also important to explore beliefs and attitudes regarding AD. Keep in mind that cultural groups tend to differ in their beliefs about the nature, cause, and appropriate management of AD, as well as the role of spirituality, help-seeking, and stigma.19,20
The progressive and ultimately fatal nature of AD also makes planning for the future a priority. Ideally, patients should be engaged in discussions regarding end-of-life care as early as possible, while they are still able to make informed decisions and express their preferences. Discussing end-of-life care can be overwhelming for newly diagnosed patients and their families, however, so it is important that you address issues—medical, financial, and legal planning, for example—that families should be considering.
Next: Medication for cognitive and behaviorial function >>
Drugs address cognitive and behavioral function
No currently available treatments can cure or significantly alter the progression of AD, but two classes of medications are used in an attempt to improve cognitive function. One is cholinesterase inhibitors (ChEIs), which potentiate acetylcholine synaptic transmission. The other is N-methyl-D-aspartate (NMDA) glutamate receptor blockers. Other classes of drugs are sometimes used to treat behavioral symptoms, such as agitation, aggression, mood disorders, and psychosis (eg, delusions, hallucinations).
Cognitive function. Results from studies of pharmacologic management of MCI vary widely, but recent reviews have found no convincing evidence that either ChEIs or NMDA receptor blockers have an effect on progression from MCI to dementia.21,22 Neither class is FDA-approved for treatment of MCI.
In patients with dementia, the effects of ChEIs and NMDA receptor blockers on cognition are statistically significant but modest and often of questionable clinical relevance.23 Nonetheless, among ChEIs, donepezil is approved by the FDA for mild, moderate, and severe dementia, and galantamine and rivastigmine are approved for mild and moderate dementia. There is no evidence that one ChEI is more effective than another,24 and the choice is often guided by cost, adverse effects, and health plan formularies. Memantine, the only FDA-approved NMDA receptor blocker, is approved for moderate to severe dementia and can be used alone or in combination with a ChEI.
If these drugs are used in an attempt to improve cognition in AD, guidelines recommend the following approach for initial therapy: Prescribe a ChEI for the mild stage, a ChEI plus memantine for the moderate stage, and memantine (with or without a ChEI) for the severe stage.25 The recommendations also include monitoring every six months.
There is no consensus about when to discontinue medication. Various published recommendations call for continuing treatment until the patient has “lost all cognitive and functional abilities;”22 until the patient’s MMSE score falls below 10 and there is no indication that the drug is having a “worthwhile effect;”21 or until he or she has reached stage 7 on the Reisberg Functional Assessment Staging scale, indicating nonambulatory status with speech limited to one to five words a day.10
Behavioral function. A variety of drugs are used to treat behavioral symptoms in AD. While not FDA-approved for this use, the most widely prescribed agents are second-generation antipsychotics (aripiprazole, olanzapine, quetiapine, and risperidone). The main effect of these drugs is often nothing more than sedation, and one large multisite clinical trial concluded that the adverse effects offset the benefits for patients with AD.26 Indeed, the FDA has issued an advisory on the use of second-generation antipsychotics in AD patients, stating that they are associated with increased mortality risk.27 The recently updated Beers Criteria strongly recommend avoiding these drugs for treatment of behavioral disturbances in AD unless nonpharmacologic options have failed and the patient is a threat to self or others.28
Because of the black-box warning that antipsychotics increase the risk for death, some clinicians have advocated obtaining informed consent prior to prescribing such medications.29 At the very least, when family or guardians are involved, a conversation about risks versus benefits should take place and be documented in the medical record.
Other drug classes are also sometimes used in an attempt to improve behavioral function, including antiseizure medications (valproic acid, carbamazepine), antidepressants (trazodone and selective serotonin reuptake inhibitors), and anxiolytics (benzodiazepines and buspirone). Other than their sedating effects, there is no strong evidence that these drugs are effective for treating dementia-related behavioral disorders. If used, caution is required due to potential adverse effects.
NONPHARMACOLOGIC MANAGEMENT IS "PROMISING"
A recent systematic review of nonpharmacologic interventions for MCI evaluated exercise, training in compensatory strategies, and engagement in cognitively stimulating activities and found “promising but inconclusive” results. The researchers found that studies show mostly positive effects on cognition but have significant methodologic limitations.30 Importantly, there is no evidence of delayed or reduced conversion to dementia.
For patients who already have mild-to-moderate dementia, cognitive stimulation seems to help in the short term.31 There is also some evidence that exercise and occupational therapy may slow functional decline,32 but the effects are small to modest and their actual clinical significance (eg, the ability to delay institutionalization) is unclear. There is promising but preliminary evidence that cognitive rehabilitation (helping patients devise strategies to complete daily activities) may improve functioning in everyday life.33
While behavioral symptoms are often due to the dementia itself, it is important to identify and treat medical and environmental causes that may be contributing, such as infection, pain, and loud or unsafe environments. As noted before, nonpharmacologic treatments are generally preferred for behavioral problems and should be considered prior to drug therapy. Approaches that identify and modify both the antecedents and consequences of problem behaviors and increase pleasant events have empiric support for the management of behavioral symptoms.34 Interventions including massage therapy, aromatherapy, exercise, and music therapy may also be effective in the short term for agitated behavior.35
Caregivers should be encouraged to receive training in these strategies through organizations such as AA. Caregiver education and support can reduce caregivers’ distress and increase their self-efficacy and coping skills.36
Continue: Is it time for hospice? >>
END-OF-LIFE CARE MUST BE ADDRESSED
Perhaps the most important aspect of end-of-life care in AD is assuring that families (or health care proxies) understand that AD is a fatal illness, with most patients dying within four to eight years of diagnosis.1 Evidence indicates that patients whose proxies have a clear recognition of this are less likely to experience “burdensome” interventions such as parenteral therapy, emergency department visits, hospital admissions, and tube feedings in their last three months of life.37
Overall, decisions regarding discontinuing medical treatments in advanced AD should be made by balancing the likelihood of benefit with the potential for adverse effects.38 For example, the American Geriatrics Society recently recommended against feeding tubes because they often result in discomfort due to agitation, use of restraints, and worsening pressure ulcers.39
Unfortunately, only a minority of families receives straightforward information on the course and prognosis of AD, including the fact that patients eventually stop eating and that the natural cause of death is often an acute infection. Studies also show that patients with dementia are at risk for inadequate treatment of pain.40 Assuring adequate pain control is an essential component of end-of-life care.
Hospice. End-of-life care can often be improved with hospice care. This service is underused by patients with dementia, even though hospice care is available at no cost through Medicare. Hospice eligibility criteria for patients with AD are shown in Table 3.41,42
Next page: Prevention >>
FINALLY, A WORD ABOUT PREVENTION
Numerous risk factors have been associated with an increased risk for AD (see Table 4).2,3 Some, like age and genetics, are nonmodifiable, while others—particularly cardiovascular risk factors—can be modified.1 There are also factors associated with decreased risks—most notably, physical exercise and participation in cognitively stimulating activities.3 Identification of these factors has led to the hope that addressing them can prevent AD.
But association does not equal causation. In 2010, a report from the National Institutes of Health concluded that, although there are modifiable factors associated with AD, there is insufficient evidence that addressing any of them will actually prevent AD.43 In fact, there is good evidence that some of these factors (eg, statin therapy) are not effective in reducing the incidence of dementia and that others (eg, vitamin E and estrogen therapy) are potentially harmful.44
The absence of empirically supported preventive interventions does not mean, however, that we should disregard these risks and protective factors. Encouraging social engagement, for example, may improve both emotional health and quality of life. Addressing cardiovascular risk factors can reduce the rate of coronary and cerebrovascular disease, potentially including vascular dementia, even if it does not reduce the rate of AD.
Studies are evaluating the use of monoclonal antibodies with anti-amyloid properties for prevention of AD in individuals who have APOE ε4 genotypes or high amyloid loads on neuroimaging.45 It will be several years before results are available, however, and the outcome of these studies is uncertain, as the use of anti-amyloid agents for treating established dementia has not been effective.46,47
REFERENCES
1. Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. www.alz.org/downloads/facts_figures_2013.pdf. Accessed March 21, 2015.
2. Román GC, Nash DT, Fillit H. Translating current knowledge into dementia prevention. Alzheimer Dis Assoc Disord. 2012;26:295-299.
3. Jak AJ. The impact of physical and mental activity on cognitive aging. Curr Top Behav Neurosci. 2012;10:273-291.
4. US Preventive Services Task Force. Cognitive impairment in older adults: screening. www.uspreventiveservicestaskforce.org/Page/Topic/recommendation-summary/cognitive-impairment-in-older-adults-screening. Accessed March 21, 2015.
5. Centers for Medicare & Medicaid Services. The Guide to Medicare Preventive Services. 4th ed. 2011. www.curemd.com/fqhc/The%20Guide%20to%20Medicare%20Preventative%20Services%20for%20Physicans,%20Providers%20and%20Suppliers.pdf. Accessed March 21, 2015.
6. Boustani M. Dementia screening in primary care: not too fast! J Amer Geriatr Soc. 2013;61:1205-1207.
7. Alzheimer’s Association. Know the 10 signs: early detection matters. www.alz.org/national/documents/checklist_10signs.pdf. Accessed March 21, 2015.
8. Cordell CB, Borson S, Boustani M, et al; Medicare Detection of Cognitive Impairment Workgroup. Alzheimer’s Association recommendations for operationalizing the detection of cognitive impairment during the Medicare Annual Wellness Visit in a primary care setting. Alzheimers Dement. 2013;9:141-150.
9. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263-269.
10. The American Geriatrics Society. A guide to dementia diagnosis and treatment. http://dementia.americangeriatrics.org/documents/AGS_PC_Dementia_Sheet_2010v2.pdf. Accessed March 21, 2015.
11. Jack CR, Knopman DS, Jagust WJ, et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12:207-216.
12. Johnson KA, Minoshima S, Bohnen NI, et al; Alzheimer’s Association; Society of Nuclear Medicine and Molecular Imaging; Amyloid Imaging Taskforce. Appropriate use criteria for amyloid PET: a report of the Amyloid Imaging Task Force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer’s Association. Alzheimers Dement. 2013;9:e1-e16.
13. Centers for Medicare and Medicaid Services. National coverage determination (NCD) for FDG PET for dementia and neurodegenerative diseases (220.6.13). www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=288&ncdver=3&bc=BAABAAAAAAAA&. Accessed March 21, 2015.
14. Albert MS, DeKosky ST, Ruckson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270-179.
15. Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia—meta-analysis of 41 robust inception studies. Acta Psychiatr Scand. 2009;119:252-265.
16. Farias ST, Mungas D, Reed BR, et al. Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts. Arch Neurol. 2009;66:1151-1157.
17. Bensadon BA, Odenheimer GL. Current management decisions in mild cognitive impairment. Clin Geriatr Med. 2013;29:847-871.
18. Ngo-Metzger Q, August KJ, Srinivasan M, et al. End-of-life care: guidelines for patient-centered communication. Am Fam Physician. 2008;77: 167-174.
19. Sayegh P, Knight BG. Cross-cultural differences in dementia: the Sociocultural Health Belief Model. Int Psychogeriatr. 2013;25:517-530.
20. McDaniel SH, Campbell TL, Hepworth J, et al. Family-Oriented Primary Care. 2nd ed. New York, NY: Springer; 2005.
21. Bensadon BA, Odenheimer GL. Current management decisions in mild cognitive impairment. Clin Geriatr Med. 2013:29;847-871.
22. Russ TC, Morling JR. Cholinesterase inhibitors for mild cognitive impairment. Cochrane Database Syst Rev. 2012;9:CD009132.
23. Sadowsky CH, Galvin JE. Guidelines for the management of cognitive and behavioral problems in dementia. J Am Board Fam Med. 2012;25: 350-366.
24. Birks J. Cholinesterase inhibitors for Alzheimer’s disease. Cochrane Database Syst Rev. 2006;(1):CD005593.
25. Fillit HM, Doody RS, Binaso K, et al. Recommendations for best practices in the treatment of Alzheimer’s disease in managed care. Am J Geriatr Pharmacother. 2006;4(suppl A):S9-S24;quiz S25-S28.
26. Schneider LS, Tariot PN, Dagerman KS, et al; CATIE-AD Study Group. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer’s disease. N Engl J Med. 2006;355:1525-1538.
27. FDA. Public health advisory: Deaths with antipsychotics in elderly patients with behavioral disturbances. www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm053171.htm. Updated August 16, 2013. Accessed March 21, 2015.
28. The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60: 616-631.
29. Brummel-Smith K. It’s time to require written informed consent when using antipsychotics in dementia. Br J Med Pract. 2008;1:4-6.
30. Huckans M, Hutson L, Twamley E, et al. Efficacy of cognitive rehabilitation therapies for mild cognitive impairment (MCI) in older adults: working toward a theoretical model and evidence-based interventions. Neuropsychol Rev. 2013;23:63-80.
31. Woods B, Aguirre E, Spector AE, et al. Cognitive stimulation to improve cognitive functioning in people with dementia. Cochrane Database Syst Rev. 2012;2:CD005562.
32. McLaren AN, Lamantia MA, Callahan CM. Systematic review of non-pharmacologic interventions to delay functional decline in community-dwelling patients with dementia. Aging Ment Health. 2013;17:655-666.
33. Bahar-Fuchs A, Clare L, Woods B. Cognitive training and cognitive rehabilitation for mild to moderate Alzheimer’s disease and vascular dementia. Cochrane Database Syst Rev. 2013;6:CD003260.
34. Logsdon RG, McCurry SM, Teri L. Evidence-based psychological treatments for disruptive behaviors in individuals with dementia. Psychol Aging. 2007;22:28-36.
35. Raetz J. A nondrug approach to dementia. J Fam Pract. 2013;62:548-557.
36. Gallagher-Thompson D, Coon DW. Evidence-based psychological treatments for distress in family caregivers of older adults. Psychol Aging. 2007;22:37-51.
37. Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009:361:1529-1538.
38. Parsons C, Hughes CM, Passmore AP, et al. Withholding, discontinuing and withdrawing medications in dementia patients at the end of life: a neglected problem in the disadvantaged dying? Drugs Aging. 2010; 27:435-449.
39. The American Geriatrics Society. Feeding tubes in advanced dementia position statement. www.americangeriatrics.org/files/documents/feeding.tubes.advanced.dementia.pdf. Accessed March 21, 2015.
40. Goodman C, Evans C, Wilcock J, et al. End of life care for community dwelling older people with dementia: an integrated review. Int J Geriatr Psychiatry. 2010;25:329-337.
41. Storey CP. A quick-reference guide to the hospice and palliative care training for physicians: UNIPAC self-study program. American Academy of Hospice and Palliative Medicine. Chicago; 2009.
42. Kaszniak AW, Kligman EW. Hospice care for patients with dementia. Elder Care. 2013. http://azalz.org/wp-content/uploads/2013/07/Hospice-Care-for-Pts-with-Dementia.pdf. Accessed March 21, 2015.
43. Daviglus ML, Bell CC, Berrettini W, et al. NIH state-of-the-science conference statement: Preventing Alzheimer’s disease and cognitive decline. NIH Consens State Sci Statements. 2010;27:1-30.
44. Patterson C, Feightner JW, Garcia A, et al. Diagnosis and treatment of dementia: 1. Risk assessment and primary prevention of Alzheimer disease. CMAJ. 2008;178:548-556.
45. Carrillo MC, Brashear HR, Logovinsky V, et al. Can we prevent Alzheimer’s disease? Secondary “prevention” trials in Alzheimer’s disease. Alzheimers Dement. 2013;9:123-131.e1.
46. Salloway S, Sperling R, Fox NC, et al; Bapineuzumab 301 and 302 Clinical Trial Investigators. Two phase 3 trials of bapineuzumab in mild-to-moderate Alzheimer’s Disease. N Engl J Med. 2014;370:322-333.
47. Doody RS, Thomas RG, Farlow M, et al; Alheimer’s Disease Cooperative Study Steering Committee; Solanezumab Study Group. Phase 3 trials of solanezumab for mild-to-moderate Alzheimer’s Disease. N Engl J Med. 2014;370:311-321.
Alzheimer disease (AD), the most common form of dementia, affects more than 5 million Americans.1 Estimates suggest that by 2050, the prevalence could triple, reaching 13 to 16 million.1 To effectively care for patients with AD and their families, primary care providers need to be familiar with the latest evidence on all facets of care, from initial detection to patient management and end-of-life care.
This evidence-based review will help you toward that end by answering common questions regarding Alzheimer care, including whether routine screening is advisable, what tests should be ordered, which interventions (including nonpharmacologic options) are worth considering, and how best to counsel patients and families about end-of-life care.
ROUTINE SCREENING? STILL SUBJECT TO DEBATE
The key question regarding routine dementia screening in primary care is whether it improves outcomes. Advocates note that individuals with dementia may appear unimpaired during office visits and may not report symptoms due to lack of insight; they point out, too, that waiting for an event that makes cognitive impairment obvious (eg, driving mishap) is risky.2 Those who advocate routine screening also note that only about half of those who have dementia are ever diagnosed.3
Others, including the US Preventive Services Task Force (USPSTF), disagree. In its 2014 evidence review, the USPSTF indicated that there is “insufficient evidence to assess the balance of benefits and harms of screening for cognitive impairment in older adults.”4
Mixed messages
The dearth of evidence is also reflected in the conflicting recommendations of the Affordable Care Act (ACA) and the Centers for Medicare and Medicaid Services (CMS). The ACA requires clinicians to assess cognitive function during Medicare patients’ annual wellness visits. CMS, however, instructs providers to screen for dementia only if observation or concerns raised by the patient or family suggest the possibility of impairment and does not recommend any particular test.5
Cost-effectiveness analyses also raise questions about the value of routine screening. Evidence suggests that screening 300 older patients will yield 39 positive results. But only about half of those will agree to a diagnostic evaluation, and no more than nine will ultimately be diagnosed with dementia. The estimated cost of identifying nine cases is nearly $40,000—all in the absence of a treatment to cure or stop the progression of the disorder.6
The bottom line: Evidence does not support routine dementia screening of older adults. When cognitive impairment is suspected, however, clinicians should conduct a diagnostic evaluation—and consider educating patients and families about the Alzheimer’s Association (AA)’s 10 Warning Signs of AD (see box, above).7 A longer version (www.alz.org/national/documents/checklist_10signs.pdf) outlines the cognitive changes that are characteristic of healthy aging and compares them to changes suggestive of early dementia.7
Next: How to proceed when you suspect AD >>
HOW TO PROCEED WHEN YOU SUSPECT AD
Step 1: Screening instrument. The first step in the diagnostic evaluation of a patient with suspected AD is to determine if, in fact, cognitive impairment is present. This can be assessed with in-office screening instruments, such as the Mini-Cog (http://bit.ly/1FwQAkG) or Mini-Mental State Examination (MMSE; http://bit.ly/18Djin5), among others.8
Step 2: Clinical evaluation. If observation and test results suggest cognitive impairment, the next step is to determine whether clinical findings are consistent with the diagnostic criteria for AD (see Table 1)9 developed by workgroups from the National Institute on Aging (NIA) and the AA in 2011. A work-up is necessary to identify conditions that can mimic dementia (eg, depression) and behaviors that suggest another type of dementia, such as frontotemporal or Lewy body dementia.10 Lab testing should be included to rule out potentially reversible causes of cognitive dysfunction (eg, hypothyroidism, vitamin D deficiency).
Step 3: Neuropsychologic evaluation. The NIA/AA recommends neuropsychologic testing when the brief cognitive tests, history, and clinical work-up are not sufficient for a definitive diagnosis of dementia.9 This generally involves a referral to a neuropsychologist, who conducts a battery of standardized tests to evaluate attention, memory, language, visual-spatial abilities, and executive functions, among others. Neuropsychologic testing can confirm the presence of cognitive impairment and aid in the differential diagnosis by comparing the patient’s performance in these domains with characteristic features of different dementia syndromes.
Step 4: Brain imaging with either CT or MRI can be included in the work-up for patients with suspected AD to rule out abnormalities (eg, metastatic cancer, hydrocephalus, or occult chronic subdural hematoma) that could be causing cognitive impairment.9,10 Clinical features that generally warrant brain imaging include onset of cognitive impairment before age 60; unexplained focal neurologic signs or symptoms; abrupt onset or rapid decline; and/or predisposing conditions (eg, cancer or anticoagulant treatment).10
The role of biomarkers and advanced brain imaging
Biomarkers that might provide confirmation of AD in patients who exhibit early symptoms of dementia have been studied extensively.11 The NIA/AA identified two categories of AD biomarkers
• Tests for β-amyloid deposition in the brain, including spinal fluid assays for β-amyloid (Aβ42) and positron emission tomography (PET) scans after IV injection of florbetapir or flutemetamol, which bind to amyloid in the brain; and
• Tests for neuronal degeneration, which would include spinal fluid assays for tau protein and PET scans after injection of fluorodeoxyglucose (FDG), which shows decreased uptake in patients with AD.9
Research reveals the promise of these biomarkers as diagnostic tools, particularly in patients with an atypical presentation of dementia or mild cognitive impairment (MCI) that may be associated with early AD.12 (More on MCI in a moment.) However, the NIA/AA concluded that additional research is needed to validate these tests for routine diagnostic purposes. Medicare covers PET scans with FDG only for the differential diagnosis of AD versus frontotemporal dementia.13
Continue for mild cognitive impairment >>
MILD COGNITIVE IMPAIRMENT: HOW LIKELY THAT IT WILL PROGRESS?
Along with diagnostic criteria for AD, the NIA/AA developed criteria for a symptomatic predementia phase of AD—often referred to as MCI.14 According to the workgroup, MCI is diagnosed when
1. The patient, an informant, or a clinician is concerned about the individual’s cognitive decline from previous levels of functioning
2. There is evidence of cognitive impairment, ideally through psychometric testing, revealing performance below expectation based on the patient’s age and education
3. The patient is able to maintain independent functioning in daily life, despite mild problems or the need for minimal assistance
4. There is no significant impairment in social or occupational functioning.14
Progression: Less likely than you might think
Patients with MCI are at risk for progression to overt dementia, with an overall annual conversion rate from MCI to dementia estimated at 10% to 15%.15,16 This estimate must be interpreted with caution, however, because most studies were conducted prior to the 2011 guidelines, when different diagnostic criteria were used. Observers have noted, too, that the numbers largely reflect data collected in specialty clinics and that community-based studies reveal substantially lower conversion rates (3% to 6% per year).16 In addition, evidence suggests that many patients with MCI demonstrate long-term stability or even reversal of deficits.17
While there is some consideration of the use of biomarkers and amyloid imaging tests to help determine which patients with MCI will progress to AD, practice guidelines do not currently recommend such testing and it is not covered by Medicare.
WHEN EVIDENCE INDICATES AN AD DIAGNOSIS
When faced with the need to communicate an AD diagnosis, follow the general recommendations for delivering any bad news or discouraging prognosis.
Prioritize and limit the information you provide, determining not only what the patient and family want to hear but also how much they are able to comprehend.
Confirm that the patient and family understand the information you’ve provided.
Offer emotional support and recommend additional resources (see Table 2).18
Given the progressive cognitive decline that characterizes AD, it is important to address the primary caregiver’s understanding of, and ability to cope with, the disease. It is also important to explore beliefs and attitudes regarding AD. Keep in mind that cultural groups tend to differ in their beliefs about the nature, cause, and appropriate management of AD, as well as the role of spirituality, help-seeking, and stigma.19,20
The progressive and ultimately fatal nature of AD also makes planning for the future a priority. Ideally, patients should be engaged in discussions regarding end-of-life care as early as possible, while they are still able to make informed decisions and express their preferences. Discussing end-of-life care can be overwhelming for newly diagnosed patients and their families, however, so it is important that you address issues—medical, financial, and legal planning, for example—that families should be considering.
Next: Medication for cognitive and behaviorial function >>
Drugs address cognitive and behavioral function
No currently available treatments can cure or significantly alter the progression of AD, but two classes of medications are used in an attempt to improve cognitive function. One is cholinesterase inhibitors (ChEIs), which potentiate acetylcholine synaptic transmission. The other is N-methyl-D-aspartate (NMDA) glutamate receptor blockers. Other classes of drugs are sometimes used to treat behavioral symptoms, such as agitation, aggression, mood disorders, and psychosis (eg, delusions, hallucinations).
Cognitive function. Results from studies of pharmacologic management of MCI vary widely, but recent reviews have found no convincing evidence that either ChEIs or NMDA receptor blockers have an effect on progression from MCI to dementia.21,22 Neither class is FDA-approved for treatment of MCI.
In patients with dementia, the effects of ChEIs and NMDA receptor blockers on cognition are statistically significant but modest and often of questionable clinical relevance.23 Nonetheless, among ChEIs, donepezil is approved by the FDA for mild, moderate, and severe dementia, and galantamine and rivastigmine are approved for mild and moderate dementia. There is no evidence that one ChEI is more effective than another,24 and the choice is often guided by cost, adverse effects, and health plan formularies. Memantine, the only FDA-approved NMDA receptor blocker, is approved for moderate to severe dementia and can be used alone or in combination with a ChEI.
If these drugs are used in an attempt to improve cognition in AD, guidelines recommend the following approach for initial therapy: Prescribe a ChEI for the mild stage, a ChEI plus memantine for the moderate stage, and memantine (with or without a ChEI) for the severe stage.25 The recommendations also include monitoring every six months.
There is no consensus about when to discontinue medication. Various published recommendations call for continuing treatment until the patient has “lost all cognitive and functional abilities;”22 until the patient’s MMSE score falls below 10 and there is no indication that the drug is having a “worthwhile effect;”21 or until he or she has reached stage 7 on the Reisberg Functional Assessment Staging scale, indicating nonambulatory status with speech limited to one to five words a day.10
Behavioral function. A variety of drugs are used to treat behavioral symptoms in AD. While not FDA-approved for this use, the most widely prescribed agents are second-generation antipsychotics (aripiprazole, olanzapine, quetiapine, and risperidone). The main effect of these drugs is often nothing more than sedation, and one large multisite clinical trial concluded that the adverse effects offset the benefits for patients with AD.26 Indeed, the FDA has issued an advisory on the use of second-generation antipsychotics in AD patients, stating that they are associated with increased mortality risk.27 The recently updated Beers Criteria strongly recommend avoiding these drugs for treatment of behavioral disturbances in AD unless nonpharmacologic options have failed and the patient is a threat to self or others.28
Because of the black-box warning that antipsychotics increase the risk for death, some clinicians have advocated obtaining informed consent prior to prescribing such medications.29 At the very least, when family or guardians are involved, a conversation about risks versus benefits should take place and be documented in the medical record.
Other drug classes are also sometimes used in an attempt to improve behavioral function, including antiseizure medications (valproic acid, carbamazepine), antidepressants (trazodone and selective serotonin reuptake inhibitors), and anxiolytics (benzodiazepines and buspirone). Other than their sedating effects, there is no strong evidence that these drugs are effective for treating dementia-related behavioral disorders. If used, caution is required due to potential adverse effects.
NONPHARMACOLOGIC MANAGEMENT IS "PROMISING"
A recent systematic review of nonpharmacologic interventions for MCI evaluated exercise, training in compensatory strategies, and engagement in cognitively stimulating activities and found “promising but inconclusive” results. The researchers found that studies show mostly positive effects on cognition but have significant methodologic limitations.30 Importantly, there is no evidence of delayed or reduced conversion to dementia.
For patients who already have mild-to-moderate dementia, cognitive stimulation seems to help in the short term.31 There is also some evidence that exercise and occupational therapy may slow functional decline,32 but the effects are small to modest and their actual clinical significance (eg, the ability to delay institutionalization) is unclear. There is promising but preliminary evidence that cognitive rehabilitation (helping patients devise strategies to complete daily activities) may improve functioning in everyday life.33
While behavioral symptoms are often due to the dementia itself, it is important to identify and treat medical and environmental causes that may be contributing, such as infection, pain, and loud or unsafe environments. As noted before, nonpharmacologic treatments are generally preferred for behavioral problems and should be considered prior to drug therapy. Approaches that identify and modify both the antecedents and consequences of problem behaviors and increase pleasant events have empiric support for the management of behavioral symptoms.34 Interventions including massage therapy, aromatherapy, exercise, and music therapy may also be effective in the short term for agitated behavior.35
Caregivers should be encouraged to receive training in these strategies through organizations such as AA. Caregiver education and support can reduce caregivers’ distress and increase their self-efficacy and coping skills.36
Continue: Is it time for hospice? >>
END-OF-LIFE CARE MUST BE ADDRESSED
Perhaps the most important aspect of end-of-life care in AD is assuring that families (or health care proxies) understand that AD is a fatal illness, with most patients dying within four to eight years of diagnosis.1 Evidence indicates that patients whose proxies have a clear recognition of this are less likely to experience “burdensome” interventions such as parenteral therapy, emergency department visits, hospital admissions, and tube feedings in their last three months of life.37
Overall, decisions regarding discontinuing medical treatments in advanced AD should be made by balancing the likelihood of benefit with the potential for adverse effects.38 For example, the American Geriatrics Society recently recommended against feeding tubes because they often result in discomfort due to agitation, use of restraints, and worsening pressure ulcers.39
Unfortunately, only a minority of families receives straightforward information on the course and prognosis of AD, including the fact that patients eventually stop eating and that the natural cause of death is often an acute infection. Studies also show that patients with dementia are at risk for inadequate treatment of pain.40 Assuring adequate pain control is an essential component of end-of-life care.
Hospice. End-of-life care can often be improved with hospice care. This service is underused by patients with dementia, even though hospice care is available at no cost through Medicare. Hospice eligibility criteria for patients with AD are shown in Table 3.41,42
Next page: Prevention >>
FINALLY, A WORD ABOUT PREVENTION
Numerous risk factors have been associated with an increased risk for AD (see Table 4).2,3 Some, like age and genetics, are nonmodifiable, while others—particularly cardiovascular risk factors—can be modified.1 There are also factors associated with decreased risks—most notably, physical exercise and participation in cognitively stimulating activities.3 Identification of these factors has led to the hope that addressing them can prevent AD.
But association does not equal causation. In 2010, a report from the National Institutes of Health concluded that, although there are modifiable factors associated with AD, there is insufficient evidence that addressing any of them will actually prevent AD.43 In fact, there is good evidence that some of these factors (eg, statin therapy) are not effective in reducing the incidence of dementia and that others (eg, vitamin E and estrogen therapy) are potentially harmful.44
The absence of empirically supported preventive interventions does not mean, however, that we should disregard these risks and protective factors. Encouraging social engagement, for example, may improve both emotional health and quality of life. Addressing cardiovascular risk factors can reduce the rate of coronary and cerebrovascular disease, potentially including vascular dementia, even if it does not reduce the rate of AD.
Studies are evaluating the use of monoclonal antibodies with anti-amyloid properties for prevention of AD in individuals who have APOE ε4 genotypes or high amyloid loads on neuroimaging.45 It will be several years before results are available, however, and the outcome of these studies is uncertain, as the use of anti-amyloid agents for treating established dementia has not been effective.46,47
REFERENCES
1. Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. www.alz.org/downloads/facts_figures_2013.pdf. Accessed March 21, 2015.
2. Román GC, Nash DT, Fillit H. Translating current knowledge into dementia prevention. Alzheimer Dis Assoc Disord. 2012;26:295-299.
3. Jak AJ. The impact of physical and mental activity on cognitive aging. Curr Top Behav Neurosci. 2012;10:273-291.
4. US Preventive Services Task Force. Cognitive impairment in older adults: screening. www.uspreventiveservicestaskforce.org/Page/Topic/recommendation-summary/cognitive-impairment-in-older-adults-screening. Accessed March 21, 2015.
5. Centers for Medicare & Medicaid Services. The Guide to Medicare Preventive Services. 4th ed. 2011. www.curemd.com/fqhc/The%20Guide%20to%20Medicare%20Preventative%20Services%20for%20Physicans,%20Providers%20and%20Suppliers.pdf. Accessed March 21, 2015.
6. Boustani M. Dementia screening in primary care: not too fast! J Amer Geriatr Soc. 2013;61:1205-1207.
7. Alzheimer’s Association. Know the 10 signs: early detection matters. www.alz.org/national/documents/checklist_10signs.pdf. Accessed March 21, 2015.
8. Cordell CB, Borson S, Boustani M, et al; Medicare Detection of Cognitive Impairment Workgroup. Alzheimer’s Association recommendations for operationalizing the detection of cognitive impairment during the Medicare Annual Wellness Visit in a primary care setting. Alzheimers Dement. 2013;9:141-150.
9. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263-269.
10. The American Geriatrics Society. A guide to dementia diagnosis and treatment. http://dementia.americangeriatrics.org/documents/AGS_PC_Dementia_Sheet_2010v2.pdf. Accessed March 21, 2015.
11. Jack CR, Knopman DS, Jagust WJ, et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12:207-216.
12. Johnson KA, Minoshima S, Bohnen NI, et al; Alzheimer’s Association; Society of Nuclear Medicine and Molecular Imaging; Amyloid Imaging Taskforce. Appropriate use criteria for amyloid PET: a report of the Amyloid Imaging Task Force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer’s Association. Alzheimers Dement. 2013;9:e1-e16.
13. Centers for Medicare and Medicaid Services. National coverage determination (NCD) for FDG PET for dementia and neurodegenerative diseases (220.6.13). www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=288&ncdver=3&bc=BAABAAAAAAAA&. Accessed March 21, 2015.
14. Albert MS, DeKosky ST, Ruckson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270-179.
15. Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia—meta-analysis of 41 robust inception studies. Acta Psychiatr Scand. 2009;119:252-265.
16. Farias ST, Mungas D, Reed BR, et al. Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts. Arch Neurol. 2009;66:1151-1157.
17. Bensadon BA, Odenheimer GL. Current management decisions in mild cognitive impairment. Clin Geriatr Med. 2013;29:847-871.
18. Ngo-Metzger Q, August KJ, Srinivasan M, et al. End-of-life care: guidelines for patient-centered communication. Am Fam Physician. 2008;77: 167-174.
19. Sayegh P, Knight BG. Cross-cultural differences in dementia: the Sociocultural Health Belief Model. Int Psychogeriatr. 2013;25:517-530.
20. McDaniel SH, Campbell TL, Hepworth J, et al. Family-Oriented Primary Care. 2nd ed. New York, NY: Springer; 2005.
21. Bensadon BA, Odenheimer GL. Current management decisions in mild cognitive impairment. Clin Geriatr Med. 2013:29;847-871.
22. Russ TC, Morling JR. Cholinesterase inhibitors for mild cognitive impairment. Cochrane Database Syst Rev. 2012;9:CD009132.
23. Sadowsky CH, Galvin JE. Guidelines for the management of cognitive and behavioral problems in dementia. J Am Board Fam Med. 2012;25: 350-366.
24. Birks J. Cholinesterase inhibitors for Alzheimer’s disease. Cochrane Database Syst Rev. 2006;(1):CD005593.
25. Fillit HM, Doody RS, Binaso K, et al. Recommendations for best practices in the treatment of Alzheimer’s disease in managed care. Am J Geriatr Pharmacother. 2006;4(suppl A):S9-S24;quiz S25-S28.
26. Schneider LS, Tariot PN, Dagerman KS, et al; CATIE-AD Study Group. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer’s disease. N Engl J Med. 2006;355:1525-1538.
27. FDA. Public health advisory: Deaths with antipsychotics in elderly patients with behavioral disturbances. www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm053171.htm. Updated August 16, 2013. Accessed March 21, 2015.
28. The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60: 616-631.
29. Brummel-Smith K. It’s time to require written informed consent when using antipsychotics in dementia. Br J Med Pract. 2008;1:4-6.
30. Huckans M, Hutson L, Twamley E, et al. Efficacy of cognitive rehabilitation therapies for mild cognitive impairment (MCI) in older adults: working toward a theoretical model and evidence-based interventions. Neuropsychol Rev. 2013;23:63-80.
31. Woods B, Aguirre E, Spector AE, et al. Cognitive stimulation to improve cognitive functioning in people with dementia. Cochrane Database Syst Rev. 2012;2:CD005562.
32. McLaren AN, Lamantia MA, Callahan CM. Systematic review of non-pharmacologic interventions to delay functional decline in community-dwelling patients with dementia. Aging Ment Health. 2013;17:655-666.
33. Bahar-Fuchs A, Clare L, Woods B. Cognitive training and cognitive rehabilitation for mild to moderate Alzheimer’s disease and vascular dementia. Cochrane Database Syst Rev. 2013;6:CD003260.
34. Logsdon RG, McCurry SM, Teri L. Evidence-based psychological treatments for disruptive behaviors in individuals with dementia. Psychol Aging. 2007;22:28-36.
35. Raetz J. A nondrug approach to dementia. J Fam Pract. 2013;62:548-557.
36. Gallagher-Thompson D, Coon DW. Evidence-based psychological treatments for distress in family caregivers of older adults. Psychol Aging. 2007;22:37-51.
37. Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009:361:1529-1538.
38. Parsons C, Hughes CM, Passmore AP, et al. Withholding, discontinuing and withdrawing medications in dementia patients at the end of life: a neglected problem in the disadvantaged dying? Drugs Aging. 2010; 27:435-449.
39. The American Geriatrics Society. Feeding tubes in advanced dementia position statement. www.americangeriatrics.org/files/documents/feeding.tubes.advanced.dementia.pdf. Accessed March 21, 2015.
40. Goodman C, Evans C, Wilcock J, et al. End of life care for community dwelling older people with dementia: an integrated review. Int J Geriatr Psychiatry. 2010;25:329-337.
41. Storey CP. A quick-reference guide to the hospice and palliative care training for physicians: UNIPAC self-study program. American Academy of Hospice and Palliative Medicine. Chicago; 2009.
42. Kaszniak AW, Kligman EW. Hospice care for patients with dementia. Elder Care. 2013. http://azalz.org/wp-content/uploads/2013/07/Hospice-Care-for-Pts-with-Dementia.pdf. Accessed March 21, 2015.
43. Daviglus ML, Bell CC, Berrettini W, et al. NIH state-of-the-science conference statement: Preventing Alzheimer’s disease and cognitive decline. NIH Consens State Sci Statements. 2010;27:1-30.
44. Patterson C, Feightner JW, Garcia A, et al. Diagnosis and treatment of dementia: 1. Risk assessment and primary prevention of Alzheimer disease. CMAJ. 2008;178:548-556.
45. Carrillo MC, Brashear HR, Logovinsky V, et al. Can we prevent Alzheimer’s disease? Secondary “prevention” trials in Alzheimer’s disease. Alzheimers Dement. 2013;9:123-131.e1.
46. Salloway S, Sperling R, Fox NC, et al; Bapineuzumab 301 and 302 Clinical Trial Investigators. Two phase 3 trials of bapineuzumab in mild-to-moderate Alzheimer’s Disease. N Engl J Med. 2014;370:322-333.
47. Doody RS, Thomas RG, Farlow M, et al; Alheimer’s Disease Cooperative Study Steering Committee; Solanezumab Study Group. Phase 3 trials of solanezumab for mild-to-moderate Alzheimer’s Disease. N Engl J Med. 2014;370:311-321.
Alzheimer disease (AD), the most common form of dementia, affects more than 5 million Americans.1 Estimates suggest that by 2050, the prevalence could triple, reaching 13 to 16 million.1 To effectively care for patients with AD and their families, primary care providers need to be familiar with the latest evidence on all facets of care, from initial detection to patient management and end-of-life care.
This evidence-based review will help you toward that end by answering common questions regarding Alzheimer care, including whether routine screening is advisable, what tests should be ordered, which interventions (including nonpharmacologic options) are worth considering, and how best to counsel patients and families about end-of-life care.
ROUTINE SCREENING? STILL SUBJECT TO DEBATE
The key question regarding routine dementia screening in primary care is whether it improves outcomes. Advocates note that individuals with dementia may appear unimpaired during office visits and may not report symptoms due to lack of insight; they point out, too, that waiting for an event that makes cognitive impairment obvious (eg, driving mishap) is risky.2 Those who advocate routine screening also note that only about half of those who have dementia are ever diagnosed.3
Others, including the US Preventive Services Task Force (USPSTF), disagree. In its 2014 evidence review, the USPSTF indicated that there is “insufficient evidence to assess the balance of benefits and harms of screening for cognitive impairment in older adults.”4
Mixed messages
The dearth of evidence is also reflected in the conflicting recommendations of the Affordable Care Act (ACA) and the Centers for Medicare and Medicaid Services (CMS). The ACA requires clinicians to assess cognitive function during Medicare patients’ annual wellness visits. CMS, however, instructs providers to screen for dementia only if observation or concerns raised by the patient or family suggest the possibility of impairment and does not recommend any particular test.5
Cost-effectiveness analyses also raise questions about the value of routine screening. Evidence suggests that screening 300 older patients will yield 39 positive results. But only about half of those will agree to a diagnostic evaluation, and no more than nine will ultimately be diagnosed with dementia. The estimated cost of identifying nine cases is nearly $40,000—all in the absence of a treatment to cure or stop the progression of the disorder.6
The bottom line: Evidence does not support routine dementia screening of older adults. When cognitive impairment is suspected, however, clinicians should conduct a diagnostic evaluation—and consider educating patients and families about the Alzheimer’s Association (AA)’s 10 Warning Signs of AD (see box, above).7 A longer version (www.alz.org/national/documents/checklist_10signs.pdf) outlines the cognitive changes that are characteristic of healthy aging and compares them to changes suggestive of early dementia.7
Next: How to proceed when you suspect AD >>
HOW TO PROCEED WHEN YOU SUSPECT AD
Step 1: Screening instrument. The first step in the diagnostic evaluation of a patient with suspected AD is to determine if, in fact, cognitive impairment is present. This can be assessed with in-office screening instruments, such as the Mini-Cog (http://bit.ly/1FwQAkG) or Mini-Mental State Examination (MMSE; http://bit.ly/18Djin5), among others.8
Step 2: Clinical evaluation. If observation and test results suggest cognitive impairment, the next step is to determine whether clinical findings are consistent with the diagnostic criteria for AD (see Table 1)9 developed by workgroups from the National Institute on Aging (NIA) and the AA in 2011. A work-up is necessary to identify conditions that can mimic dementia (eg, depression) and behaviors that suggest another type of dementia, such as frontotemporal or Lewy body dementia.10 Lab testing should be included to rule out potentially reversible causes of cognitive dysfunction (eg, hypothyroidism, vitamin D deficiency).
Step 3: Neuropsychologic evaluation. The NIA/AA recommends neuropsychologic testing when the brief cognitive tests, history, and clinical work-up are not sufficient for a definitive diagnosis of dementia.9 This generally involves a referral to a neuropsychologist, who conducts a battery of standardized tests to evaluate attention, memory, language, visual-spatial abilities, and executive functions, among others. Neuropsychologic testing can confirm the presence of cognitive impairment and aid in the differential diagnosis by comparing the patient’s performance in these domains with characteristic features of different dementia syndromes.
Step 4: Brain imaging with either CT or MRI can be included in the work-up for patients with suspected AD to rule out abnormalities (eg, metastatic cancer, hydrocephalus, or occult chronic subdural hematoma) that could be causing cognitive impairment.9,10 Clinical features that generally warrant brain imaging include onset of cognitive impairment before age 60; unexplained focal neurologic signs or symptoms; abrupt onset or rapid decline; and/or predisposing conditions (eg, cancer or anticoagulant treatment).10
The role of biomarkers and advanced brain imaging
Biomarkers that might provide confirmation of AD in patients who exhibit early symptoms of dementia have been studied extensively.11 The NIA/AA identified two categories of AD biomarkers
• Tests for β-amyloid deposition in the brain, including spinal fluid assays for β-amyloid (Aβ42) and positron emission tomography (PET) scans after IV injection of florbetapir or flutemetamol, which bind to amyloid in the brain; and
• Tests for neuronal degeneration, which would include spinal fluid assays for tau protein and PET scans after injection of fluorodeoxyglucose (FDG), which shows decreased uptake in patients with AD.9
Research reveals the promise of these biomarkers as diagnostic tools, particularly in patients with an atypical presentation of dementia or mild cognitive impairment (MCI) that may be associated with early AD.12 (More on MCI in a moment.) However, the NIA/AA concluded that additional research is needed to validate these tests for routine diagnostic purposes. Medicare covers PET scans with FDG only for the differential diagnosis of AD versus frontotemporal dementia.13
Continue for mild cognitive impairment >>
MILD COGNITIVE IMPAIRMENT: HOW LIKELY THAT IT WILL PROGRESS?
Along with diagnostic criteria for AD, the NIA/AA developed criteria for a symptomatic predementia phase of AD—often referred to as MCI.14 According to the workgroup, MCI is diagnosed when
1. The patient, an informant, or a clinician is concerned about the individual’s cognitive decline from previous levels of functioning
2. There is evidence of cognitive impairment, ideally through psychometric testing, revealing performance below expectation based on the patient’s age and education
3. The patient is able to maintain independent functioning in daily life, despite mild problems or the need for minimal assistance
4. There is no significant impairment in social or occupational functioning.14
Progression: Less likely than you might think
Patients with MCI are at risk for progression to overt dementia, with an overall annual conversion rate from MCI to dementia estimated at 10% to 15%.15,16 This estimate must be interpreted with caution, however, because most studies were conducted prior to the 2011 guidelines, when different diagnostic criteria were used. Observers have noted, too, that the numbers largely reflect data collected in specialty clinics and that community-based studies reveal substantially lower conversion rates (3% to 6% per year).16 In addition, evidence suggests that many patients with MCI demonstrate long-term stability or even reversal of deficits.17
While there is some consideration of the use of biomarkers and amyloid imaging tests to help determine which patients with MCI will progress to AD, practice guidelines do not currently recommend such testing and it is not covered by Medicare.
WHEN EVIDENCE INDICATES AN AD DIAGNOSIS
When faced with the need to communicate an AD diagnosis, follow the general recommendations for delivering any bad news or discouraging prognosis.
Prioritize and limit the information you provide, determining not only what the patient and family want to hear but also how much they are able to comprehend.
Confirm that the patient and family understand the information you’ve provided.
Offer emotional support and recommend additional resources (see Table 2).18
Given the progressive cognitive decline that characterizes AD, it is important to address the primary caregiver’s understanding of, and ability to cope with, the disease. It is also important to explore beliefs and attitudes regarding AD. Keep in mind that cultural groups tend to differ in their beliefs about the nature, cause, and appropriate management of AD, as well as the role of spirituality, help-seeking, and stigma.19,20
The progressive and ultimately fatal nature of AD also makes planning for the future a priority. Ideally, patients should be engaged in discussions regarding end-of-life care as early as possible, while they are still able to make informed decisions and express their preferences. Discussing end-of-life care can be overwhelming for newly diagnosed patients and their families, however, so it is important that you address issues—medical, financial, and legal planning, for example—that families should be considering.
Next: Medication for cognitive and behaviorial function >>
Drugs address cognitive and behavioral function
No currently available treatments can cure or significantly alter the progression of AD, but two classes of medications are used in an attempt to improve cognitive function. One is cholinesterase inhibitors (ChEIs), which potentiate acetylcholine synaptic transmission. The other is N-methyl-D-aspartate (NMDA) glutamate receptor blockers. Other classes of drugs are sometimes used to treat behavioral symptoms, such as agitation, aggression, mood disorders, and psychosis (eg, delusions, hallucinations).
Cognitive function. Results from studies of pharmacologic management of MCI vary widely, but recent reviews have found no convincing evidence that either ChEIs or NMDA receptor blockers have an effect on progression from MCI to dementia.21,22 Neither class is FDA-approved for treatment of MCI.
In patients with dementia, the effects of ChEIs and NMDA receptor blockers on cognition are statistically significant but modest and often of questionable clinical relevance.23 Nonetheless, among ChEIs, donepezil is approved by the FDA for mild, moderate, and severe dementia, and galantamine and rivastigmine are approved for mild and moderate dementia. There is no evidence that one ChEI is more effective than another,24 and the choice is often guided by cost, adverse effects, and health plan formularies. Memantine, the only FDA-approved NMDA receptor blocker, is approved for moderate to severe dementia and can be used alone or in combination with a ChEI.
If these drugs are used in an attempt to improve cognition in AD, guidelines recommend the following approach for initial therapy: Prescribe a ChEI for the mild stage, a ChEI plus memantine for the moderate stage, and memantine (with or without a ChEI) for the severe stage.25 The recommendations also include monitoring every six months.
There is no consensus about when to discontinue medication. Various published recommendations call for continuing treatment until the patient has “lost all cognitive and functional abilities;”22 until the patient’s MMSE score falls below 10 and there is no indication that the drug is having a “worthwhile effect;”21 or until he or she has reached stage 7 on the Reisberg Functional Assessment Staging scale, indicating nonambulatory status with speech limited to one to five words a day.10
Behavioral function. A variety of drugs are used to treat behavioral symptoms in AD. While not FDA-approved for this use, the most widely prescribed agents are second-generation antipsychotics (aripiprazole, olanzapine, quetiapine, and risperidone). The main effect of these drugs is often nothing more than sedation, and one large multisite clinical trial concluded that the adverse effects offset the benefits for patients with AD.26 Indeed, the FDA has issued an advisory on the use of second-generation antipsychotics in AD patients, stating that they are associated with increased mortality risk.27 The recently updated Beers Criteria strongly recommend avoiding these drugs for treatment of behavioral disturbances in AD unless nonpharmacologic options have failed and the patient is a threat to self or others.28
Because of the black-box warning that antipsychotics increase the risk for death, some clinicians have advocated obtaining informed consent prior to prescribing such medications.29 At the very least, when family or guardians are involved, a conversation about risks versus benefits should take place and be documented in the medical record.
Other drug classes are also sometimes used in an attempt to improve behavioral function, including antiseizure medications (valproic acid, carbamazepine), antidepressants (trazodone and selective serotonin reuptake inhibitors), and anxiolytics (benzodiazepines and buspirone). Other than their sedating effects, there is no strong evidence that these drugs are effective for treating dementia-related behavioral disorders. If used, caution is required due to potential adverse effects.
NONPHARMACOLOGIC MANAGEMENT IS "PROMISING"
A recent systematic review of nonpharmacologic interventions for MCI evaluated exercise, training in compensatory strategies, and engagement in cognitively stimulating activities and found “promising but inconclusive” results. The researchers found that studies show mostly positive effects on cognition but have significant methodologic limitations.30 Importantly, there is no evidence of delayed or reduced conversion to dementia.
For patients who already have mild-to-moderate dementia, cognitive stimulation seems to help in the short term.31 There is also some evidence that exercise and occupational therapy may slow functional decline,32 but the effects are small to modest and their actual clinical significance (eg, the ability to delay institutionalization) is unclear. There is promising but preliminary evidence that cognitive rehabilitation (helping patients devise strategies to complete daily activities) may improve functioning in everyday life.33
While behavioral symptoms are often due to the dementia itself, it is important to identify and treat medical and environmental causes that may be contributing, such as infection, pain, and loud or unsafe environments. As noted before, nonpharmacologic treatments are generally preferred for behavioral problems and should be considered prior to drug therapy. Approaches that identify and modify both the antecedents and consequences of problem behaviors and increase pleasant events have empiric support for the management of behavioral symptoms.34 Interventions including massage therapy, aromatherapy, exercise, and music therapy may also be effective in the short term for agitated behavior.35
Caregivers should be encouraged to receive training in these strategies through organizations such as AA. Caregiver education and support can reduce caregivers’ distress and increase their self-efficacy and coping skills.36
Continue: Is it time for hospice? >>
END-OF-LIFE CARE MUST BE ADDRESSED
Perhaps the most important aspect of end-of-life care in AD is assuring that families (or health care proxies) understand that AD is a fatal illness, with most patients dying within four to eight years of diagnosis.1 Evidence indicates that patients whose proxies have a clear recognition of this are less likely to experience “burdensome” interventions such as parenteral therapy, emergency department visits, hospital admissions, and tube feedings in their last three months of life.37
Overall, decisions regarding discontinuing medical treatments in advanced AD should be made by balancing the likelihood of benefit with the potential for adverse effects.38 For example, the American Geriatrics Society recently recommended against feeding tubes because they often result in discomfort due to agitation, use of restraints, and worsening pressure ulcers.39
Unfortunately, only a minority of families receives straightforward information on the course and prognosis of AD, including the fact that patients eventually stop eating and that the natural cause of death is often an acute infection. Studies also show that patients with dementia are at risk for inadequate treatment of pain.40 Assuring adequate pain control is an essential component of end-of-life care.
Hospice. End-of-life care can often be improved with hospice care. This service is underused by patients with dementia, even though hospice care is available at no cost through Medicare. Hospice eligibility criteria for patients with AD are shown in Table 3.41,42
Next page: Prevention >>
FINALLY, A WORD ABOUT PREVENTION
Numerous risk factors have been associated with an increased risk for AD (see Table 4).2,3 Some, like age and genetics, are nonmodifiable, while others—particularly cardiovascular risk factors—can be modified.1 There are also factors associated with decreased risks—most notably, physical exercise and participation in cognitively stimulating activities.3 Identification of these factors has led to the hope that addressing them can prevent AD.
But association does not equal causation. In 2010, a report from the National Institutes of Health concluded that, although there are modifiable factors associated with AD, there is insufficient evidence that addressing any of them will actually prevent AD.43 In fact, there is good evidence that some of these factors (eg, statin therapy) are not effective in reducing the incidence of dementia and that others (eg, vitamin E and estrogen therapy) are potentially harmful.44
The absence of empirically supported preventive interventions does not mean, however, that we should disregard these risks and protective factors. Encouraging social engagement, for example, may improve both emotional health and quality of life. Addressing cardiovascular risk factors can reduce the rate of coronary and cerebrovascular disease, potentially including vascular dementia, even if it does not reduce the rate of AD.
Studies are evaluating the use of monoclonal antibodies with anti-amyloid properties for prevention of AD in individuals who have APOE ε4 genotypes or high amyloid loads on neuroimaging.45 It will be several years before results are available, however, and the outcome of these studies is uncertain, as the use of anti-amyloid agents for treating established dementia has not been effective.46,47
REFERENCES
1. Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. www.alz.org/downloads/facts_figures_2013.pdf. Accessed March 21, 2015.
2. Román GC, Nash DT, Fillit H. Translating current knowledge into dementia prevention. Alzheimer Dis Assoc Disord. 2012;26:295-299.
3. Jak AJ. The impact of physical and mental activity on cognitive aging. Curr Top Behav Neurosci. 2012;10:273-291.
4. US Preventive Services Task Force. Cognitive impairment in older adults: screening. www.uspreventiveservicestaskforce.org/Page/Topic/recommendation-summary/cognitive-impairment-in-older-adults-screening. Accessed March 21, 2015.
5. Centers for Medicare & Medicaid Services. The Guide to Medicare Preventive Services. 4th ed. 2011. www.curemd.com/fqhc/The%20Guide%20to%20Medicare%20Preventative%20Services%20for%20Physicans,%20Providers%20and%20Suppliers.pdf. Accessed March 21, 2015.
6. Boustani M. Dementia screening in primary care: not too fast! J Amer Geriatr Soc. 2013;61:1205-1207.
7. Alzheimer’s Association. Know the 10 signs: early detection matters. www.alz.org/national/documents/checklist_10signs.pdf. Accessed March 21, 2015.
8. Cordell CB, Borson S, Boustani M, et al; Medicare Detection of Cognitive Impairment Workgroup. Alzheimer’s Association recommendations for operationalizing the detection of cognitive impairment during the Medicare Annual Wellness Visit in a primary care setting. Alzheimers Dement. 2013;9:141-150.
9. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263-269.
10. The American Geriatrics Society. A guide to dementia diagnosis and treatment. http://dementia.americangeriatrics.org/documents/AGS_PC_Dementia_Sheet_2010v2.pdf. Accessed March 21, 2015.
11. Jack CR, Knopman DS, Jagust WJ, et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12:207-216.
12. Johnson KA, Minoshima S, Bohnen NI, et al; Alzheimer’s Association; Society of Nuclear Medicine and Molecular Imaging; Amyloid Imaging Taskforce. Appropriate use criteria for amyloid PET: a report of the Amyloid Imaging Task Force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer’s Association. Alzheimers Dement. 2013;9:e1-e16.
13. Centers for Medicare and Medicaid Services. National coverage determination (NCD) for FDG PET for dementia and neurodegenerative diseases (220.6.13). www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=288&ncdver=3&bc=BAABAAAAAAAA&. Accessed March 21, 2015.
14. Albert MS, DeKosky ST, Ruckson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270-179.
15. Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia—meta-analysis of 41 robust inception studies. Acta Psychiatr Scand. 2009;119:252-265.
16. Farias ST, Mungas D, Reed BR, et al. Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts. Arch Neurol. 2009;66:1151-1157.
17. Bensadon BA, Odenheimer GL. Current management decisions in mild cognitive impairment. Clin Geriatr Med. 2013;29:847-871.
18. Ngo-Metzger Q, August KJ, Srinivasan M, et al. End-of-life care: guidelines for patient-centered communication. Am Fam Physician. 2008;77: 167-174.
19. Sayegh P, Knight BG. Cross-cultural differences in dementia: the Sociocultural Health Belief Model. Int Psychogeriatr. 2013;25:517-530.
20. McDaniel SH, Campbell TL, Hepworth J, et al. Family-Oriented Primary Care. 2nd ed. New York, NY: Springer; 2005.
21. Bensadon BA, Odenheimer GL. Current management decisions in mild cognitive impairment. Clin Geriatr Med. 2013:29;847-871.
22. Russ TC, Morling JR. Cholinesterase inhibitors for mild cognitive impairment. Cochrane Database Syst Rev. 2012;9:CD009132.
23. Sadowsky CH, Galvin JE. Guidelines for the management of cognitive and behavioral problems in dementia. J Am Board Fam Med. 2012;25: 350-366.
24. Birks J. Cholinesterase inhibitors for Alzheimer’s disease. Cochrane Database Syst Rev. 2006;(1):CD005593.
25. Fillit HM, Doody RS, Binaso K, et al. Recommendations for best practices in the treatment of Alzheimer’s disease in managed care. Am J Geriatr Pharmacother. 2006;4(suppl A):S9-S24;quiz S25-S28.
26. Schneider LS, Tariot PN, Dagerman KS, et al; CATIE-AD Study Group. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer’s disease. N Engl J Med. 2006;355:1525-1538.
27. FDA. Public health advisory: Deaths with antipsychotics in elderly patients with behavioral disturbances. www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm053171.htm. Updated August 16, 2013. Accessed March 21, 2015.
28. The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60: 616-631.
29. Brummel-Smith K. It’s time to require written informed consent when using antipsychotics in dementia. Br J Med Pract. 2008;1:4-6.
30. Huckans M, Hutson L, Twamley E, et al. Efficacy of cognitive rehabilitation therapies for mild cognitive impairment (MCI) in older adults: working toward a theoretical model and evidence-based interventions. Neuropsychol Rev. 2013;23:63-80.
31. Woods B, Aguirre E, Spector AE, et al. Cognitive stimulation to improve cognitive functioning in people with dementia. Cochrane Database Syst Rev. 2012;2:CD005562.
32. McLaren AN, Lamantia MA, Callahan CM. Systematic review of non-pharmacologic interventions to delay functional decline in community-dwelling patients with dementia. Aging Ment Health. 2013;17:655-666.
33. Bahar-Fuchs A, Clare L, Woods B. Cognitive training and cognitive rehabilitation for mild to moderate Alzheimer’s disease and vascular dementia. Cochrane Database Syst Rev. 2013;6:CD003260.
34. Logsdon RG, McCurry SM, Teri L. Evidence-based psychological treatments for disruptive behaviors in individuals with dementia. Psychol Aging. 2007;22:28-36.
35. Raetz J. A nondrug approach to dementia. J Fam Pract. 2013;62:548-557.
36. Gallagher-Thompson D, Coon DW. Evidence-based psychological treatments for distress in family caregivers of older adults. Psychol Aging. 2007;22:37-51.
37. Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009:361:1529-1538.
38. Parsons C, Hughes CM, Passmore AP, et al. Withholding, discontinuing and withdrawing medications in dementia patients at the end of life: a neglected problem in the disadvantaged dying? Drugs Aging. 2010; 27:435-449.
39. The American Geriatrics Society. Feeding tubes in advanced dementia position statement. www.americangeriatrics.org/files/documents/feeding.tubes.advanced.dementia.pdf. Accessed March 21, 2015.
40. Goodman C, Evans C, Wilcock J, et al. End of life care for community dwelling older people with dementia: an integrated review. Int J Geriatr Psychiatry. 2010;25:329-337.
41. Storey CP. A quick-reference guide to the hospice and palliative care training for physicians: UNIPAC self-study program. American Academy of Hospice and Palliative Medicine. Chicago; 2009.
42. Kaszniak AW, Kligman EW. Hospice care for patients with dementia. Elder Care. 2013. http://azalz.org/wp-content/uploads/2013/07/Hospice-Care-for-Pts-with-Dementia.pdf. Accessed March 21, 2015.
43. Daviglus ML, Bell CC, Berrettini W, et al. NIH state-of-the-science conference statement: Preventing Alzheimer’s disease and cognitive decline. NIH Consens State Sci Statements. 2010;27:1-30.
44. Patterson C, Feightner JW, Garcia A, et al. Diagnosis and treatment of dementia: 1. Risk assessment and primary prevention of Alzheimer disease. CMAJ. 2008;178:548-556.
45. Carrillo MC, Brashear HR, Logovinsky V, et al. Can we prevent Alzheimer’s disease? Secondary “prevention” trials in Alzheimer’s disease. Alzheimers Dement. 2013;9:123-131.e1.
46. Salloway S, Sperling R, Fox NC, et al; Bapineuzumab 301 and 302 Clinical Trial Investigators. Two phase 3 trials of bapineuzumab in mild-to-moderate Alzheimer’s Disease. N Engl J Med. 2014;370:322-333.
47. Doody RS, Thomas RG, Farlow M, et al; Alheimer’s Disease Cooperative Study Steering Committee; Solanezumab Study Group. Phase 3 trials of solanezumab for mild-to-moderate Alzheimer’s Disease. N Engl J Med. 2014;370:311-321.
Addressing Alzheimer’s: A pragmatic approach
› Refer patients for formal neuropsychological testing when dementia is suspected but the history, clinical interview, and brief cognitive tests do not result in a definitive diagnosis. C
› Use non-drug therapies as first-line treatment for behavioral symptoms of Alzheimer’s disease (AD), as the adverse effects of drug therapy generally offset any benefit. B
› Recommend against feeding tubes for patients with late-stage AD as they are more apt to cause discomfort than to provide benefit. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Alzheimer’s disease (AD), the most common form of dementia, affects more than 5 million Americans.1 Estimates suggest that by 2050, the prevalence could triple, reaching 13 to 16 million.1 To effectively care for patients with AD and their families, family physicians need to be familiar with the latest evidence on all facets of care, from initial detection to patient management and end-of-life care.
This evidence-based review will help you toward that end by answering common questions regarding Alzheimer’s care, including whether routine screening is advisable, what tests should be ordered, which interventions (including nonpharmacologic options) are worth considering, and how best to counsel patients and families about end-of-life care.
Routine screening? Still subject to debate
In considering routine dementia screening in primary care, the key question is whether screening improves outcomes. Advocates note that individuals with dementia may appear unimpaired during office visits and may not report symptoms due to lack of insight; they point out, too, that waiting for an event that makes cognitive impairment obvious, such as a driving mishap, is risky.2 Those who advocate routine screening also note that only about half of those who have dementia are ever diagnosed.3
Others, including the US Preventive Services Task Force (USPSTF), disagree. In its 2014 evidence review, the USPSTF indicated that there is “insufficient evidence to assess the balance of benefits and harms of screening for cognitive impairment in older adults.”4
Mixed messages
The dearth of evidence is also reflected in the conflicting recommendations of the Affordable Care Act (ACA) and the Centers for Medicare and Medicaid Services (CMS). The ACA requires physicians to assess the cognitive function of Medicare patients during their annual wellness visits. CMS, however, instructs providers to screen for dementia only if observation or concerns raised by the patient or family suggest the possibility of impairment, and does not recommend any particular test.5
Cost-effectiveness analyses raise questions about the value of routine screening, as well. Evidence suggests that if a primary care physician screens 300 older patients, 39 will have a positive screen. But only about half of those 39 will agree to a diagnostic evaluation, and no more than 9 will ultimately be diagnosed with dementia. The estimated cost of identifying 9 cases is nearly $40,000—all in the absence of a treatment to cure or stop the progression of the disorder.6
The bottom line: Evidence does not support routine dementia screening of older adults. When cognitive impairment is suspected, however, physicians should conduct a diagnostic evaluation—and consider educating patients and families about the Alzheimer’s Association (AA)’s 10 warning signs of AD.7 (See “Is it Alzheimer’s? 10 warning signs”7 below.) A longer version, available at http://www.alz.org/national/documents/checklist_10signs.pdf, outlines the cognitive changes that are characteristic of healthy aging and compares them to changes suggestive of early dementia.7
Is it Alzheimer’s? 10 warning signs7 1. Memory loss that disrupts daily life |
How to proceed when you suspect AD
Step 1: Screening instrument. The first step in the diagnostic evaluation of a patient with suspected AD is to determine if, in fact, cognitive impairment is present. This can be done by screening with in-office screening instruments, such as the Mini-Cog (available at alz.org/documents_custom/minicog.pdf) or Mini-Mental State Examination (MMSE; health.gov.bc.ca/pharmacare/adti/clinician/pdf/ADTI%20SMMSE-GDS%20Reference%20Card.pdf), among others.8
Step 2: Clinical evaluation. If observation and test results suggest cognitive impairment, the next step is to determine whether clinical findings are consistent with the diagnostic criteria for AD (TABLE 1)9 developed by workgroups from the National Institute on Aging (NIA)/AA in 2011. A work-up is necessary to identify conditions that can mimic dementia (eg, depression) and behaviors that suggest another type of dementia, such as frontotemporal or Lewy body dementia.10 Lab testing should be included to rule out potentially reversible causes of cognitive dysfunction (eg, hypothyroidism, vitamin D deficiency).
Step 3: Neuropsychological evaluation. The NIA/AA recommends neuropsychological testing when the brief cognitive tests, history, and clinical work-up are not sufficient for a definitive diagnosis of dementia.9This generally involves a referral to a neuropsychologist, who conducts a battery of standardized tests to evaluate attention, memory, language, visual-spatial abilities, and executive functions, among others. Neuropsychological testing can confirm the presence of cognitive impairment and aid in the differential diagnosis by comparing the patient’s performance in these domains with characteristic features of different dementia syndromes.
Step 4: Brain imaging with either computed tomography or magnetic resonance imaging can be included in the work-up for patients with suspected AD to rule out abnormalities—eg, metastatic cancer, hydrocephalus, or occult chronic subdural hematoma—that could be causing cognitive impairment.9,10 Clinical features that generally warrant brain imaging include onset of cognitive impairment before age 60; unexplained focal neurologic signs or symptoms; abrupt onset or rapid decline; and/or predisposing conditions, such as cancer or anticoagulant treatment.10
The role of biomarkers and advanced brain imaging
Biomarkers that might provide confirmation of AD in patients who exhibit early symptoms of dementia have been studied extensively.11 The NIA/AA identified 2 categories of AD biomarkers:
- tests for β-amyloid deposition in the brain, including spinal fluid assays for β-amyloid (Aβ42) and positron emission tomography (PET) scans after intravenous injection of florbetapir or flutemetamol, which bind to amyloid in the brain; and
- tests for neuronal degeneration, which would include spinal fluid assays for tau protein and PET scans after injection of fluorodeoxyglucose (FDG), which shows decreased uptake in patients with AD.9
Research reveals the promise of these biomarkers as diagnostic tools, particularly in patients with an atypical presentation of dementia or mild cognitive impairment (MCI) that may be associated with early AD.12 (More on MCI in a moment.) However, the NIA/AA concluded that additional research is needed to validate these tests for routine diagnostic purposes. Medicare covers PET scans with FDG only for the differential diagnosis of AD vs frontotemporal dementia.13
Mild cognitive impairment: How likely that it will progress?
Along with diagnostic criteria for AD, the NIA/AA developed criteria for a symptomatic predementia phase of AD—often referred to as MCI.14 According to the workgroup, MCI is diagnosed when:
2. there is evidence of cognitive impairment, ideally through psychometric testing, revealing performance below expectation based on the patient’s age and education;
3. the patient is able to maintain independent functioning in daily life, despite mild problems or the need for minimal assistance; and
4. there is no significant impairment in social or occupational functioning.14
Progression: Less likely than you might think
Patients with MCI are at risk for progression to overt dementia, with an overall annual conversion rate from MCI to dementia estimated at 10% to 15%.15,16 This estimate must be interpreted with caution, however, because most studies were conducted prior to the 2011 guidelines, when different diagnostic criteria were used. Observers have noted, too, that the numbers largely reflect data collected in specialty clinics and that community-based studies reveal substantially lower conversion rates (3%-6% per year).16 In addition, evidence suggests that many patients with MCI demonstrate long-term stability or even reversal of deficits.17
While there is some consideration of the use of biomarkers and amyloid imaging tests to help determine which patients with MCI will progress to AD, practice guidelines do not currently recommend such testing and it is not covered by Medicare.
When evidence indicates an AD diagnosis
When faced with the need to communicate an AD diagnosis, follow the general recommendations for delivering any bad news or discouraging prognosis:
Prioritize and limit the information you provide, determining not only what the patient and family want to hear, but also how much they are able to comprehend.
Confirm that the patient and family understand the information you’ve provided.
Offer emotional support and recommend additional resources18 (TABLE 2).
Given the progressive cognitive decline that characterizes AD, it is important to address the primary caregiver’s understanding of, and ability to cope with, the disease. It is also important to explore beliefs and attitudes regarding AD. Keep in mind that different cultural groups tend to differ in their beliefs about the nature, cause, and appropriate management of AD, as well as the role of spirituality, help-seeking, and stigma.19,20
The progressive and ultimately fatal nature of AD also makes planning for the future a priority. Ideally, patients should be engaged in discussions regarding end-of-life care as early as possible, while they are still able to make informed decisions and express their preferences. Discussing end-of-life care can be overwhelming for newly diagnosed patients and their families, however, so it is important that you address issues—medical, financial, and legal planning, for example—that families should be considering.
TABLE 2
| Resources for newly diagnosed patients and families | |
| Issue | Resources |
| Education | Alzheimer’s and Dementia Caregiver Center http://www.alz.org/care/overview.asp NIA Alzheimer’s Disease Education and Referral Center http://www.nia.nih.gov/alzheimers/ |
| Planning (medical, financial, legal)/benefits | AARP Caregiving Resource Center http://www.aarp.org/home-family/caregiving Alzheimer’s Association Alzheimer’s Navigator https://www.alzheimersnavigator.org/ National Council on Aging Benefits Checkup https://www.benefitscheckup.org/ |
| Safety | Association for Driver Rehabilitation Specialists: Driving and Alzheimer’s/Dementia https://c.ymcdn.com/sites/www.aded.net/resource/resmgr/fact_Sheets/ADED_alzheimers-Dementia_fac.pdf NIA’s Home Safety for People with Alzheimer’s booklet http://www.nia.nih.gov/alzheimers/publication/home-safety-people-alzheimers-disease |
| Support | Caregiver Action Network http://caregiveraction.org/ |
Drugs address cognitive and behavioral function
No currently available treatments can cure or significantly alter the progression of AD, but 2 classes of medications are used in an attempt to improve cognitive function. One is cholinesterase inhibitors (ChEIs), which potentiate acetylcholine synaptic transmission. The other is N-methyl-D-aspartate (NMDA) glutamate receptor blockers. Other classes of drugs are sometimes used to treat behavioral symptoms of dementia, such as agitation, aggression, mood disorders, and psychosis (eg, delusions and hallucinations).
Cognitive function. Results from studies of pharmacologic management of MCI vary widely, but recent reviews have found no convincing evidence that either ChEIs or NMDA receptor blockers have an effect on progression from MCI to dementia.21,22 Neither class is FDA-approved for treating MCI.
In patients with dementia, the effects of ChEIs and NMDA receptor blockers on cognition are statistically significant but modest, and often of questionable clinical relevance.23 Nonetheless, among ChEIs, donepezil is approved by the US Food and Drug Administration (FDA) for mild, moderate, and severe dementia and galantamine and rivastigmine are approved for mild and moderate dementia. There is no evidence that any one ChEI is more effective than any other,24 and the choice of drugs is often guided by cost, adverse effects, and health plan formularies. Memantine, the only FDA-approved NMDA receptor blocker, is approved for moderate to severe dementia and can be used alone or in combination with a ChEI.
If these drugs are used in an attempt to improve cognition in AD, guidelines recommend the following approach for initial therapy: Prescribe a ChEI for the mild stage, a ChEI plus memantine for the moderate stage, and memantine (with or without a ChEI) for the severe stage.25 The recommendations also include monitoring every 6 months.
There is no consensus about when to discontinue medication. Various published recommendations call for continuing treatment until the patient has “lost all cognitive and functional abilities;”22 until the patient’s MMSE score falls below 10 and there is no indication that the drug is having a “worthwhile effect;”21 or until he or she has reached stage 7 on the Reisberg Functional Assessment Staging scale, indicating nonambulatory status with speech limited to one to 5 words a day.10
Behavioral function. A variety of drugs are used to treat behavioral symptoms in AD. While not FDA-approved for this use, the most widely prescribed agents are second-generation antipsychotics (aripiprazole, olanzapine, quetiapine, and risperidone). The main effect of these drugs is often nothing more than sedation, and one large multisite clinical trial concluded that the adverse effects offset the benefits for patients with AD.26 Indeed, the FDA has issued an advisory on the use of second-generation antipsychotics in AD patients, stating that they are associated with an increased risk of death.27 The recently updated Beers Criteria strongly recommend avoiding these drugs for treating behavioral disturbances in AD unless nonpharmacologic options have failed and the patient is a threat to self or others.28
Because of the black-box warning that antipsychotics increase the risk of death, some physicians have advocated obtaining informed consent prior to prescribing such medications.29 At the very least, when family or guardians are involved, a conversation about risks vs benefits should take place and be documented in the medical record.
Other drug classes are also sometimes used in an attempt to improve behavioral function, including anti-seizure medications (valproic acid, carbamazepine), antidepressants (trazodone and selective serotonin reuptake inhibitors), and anxiolytics (benzodiazepines and buspirone). Other than their sedating effects, there is no strong evidence that these drugs are effective for treating dementia-related behavioral disorders. If used, caution is required due to potential adverse effects.
Nonpharmacologic management is “promising”
A recent systematic review of nonpharmacologic interventions for MCI evaluated exercise, training in compensatory strategies, and engagement in cognitively stimulating activities and found “promising but inconclusive” results. The researchers found that studies show mostly positive effects on cognition but have significant methodologic limitations.30 Importantly, there is no evidence of delayed or reduced conversion to dementia.
For patients who already have mild-to-moderate dementia, cognitive stimulation seems to help in the short term.31 There is also some evidence that exercise and occupational therapy may slow functional decline,32 but the effects are small to modest and their actual clinical significance (eg, the ability to delay institutionalization) is unclear. There is promising but preliminary evidence that cognitive rehabilitation (helping patients devise strategies to complete daily activities) may improve functioning in everyday life.33
While behavioral symptoms are often due to the dementia itself, it is important to identify and treat medical and environmental causes that may be contributing, such as infection, pain, and loud or unsafe environments. As noted before, nonpharmacologic treatments are generally preferred for behavioral problems and should be considered prior to drug therapy. Approaches that identify and modify both the antecedents and consequences of problem behaviors and increase pleasant events have empirical support for the management of behavioral symptoms.34 Interventions including massage therapy, aromatherapy, exercise, and music therapy may also be effective in the short term for agitated behavior.35
Caregivers should be encouraged to receive training in these strategies through organizations like AA. Caregiver education and support can reduce caregivers’ distress and increase their self-efficacy and coping skills.36
End-of-life care must be addressed
Perhaps the most important aspect of end-of-life care in AD is assuring that families (or health care proxies) understand that AD is a fatal illness, with most patients dying within 4 to 8 years of diagnosis.1 Evidence indicates that patients whose proxies have a clear recognition of this are less likely to experience “burdensome” interventions such as parenteral therapy, emergency department visits, hospital admissions, and tube feedings in their last 3 months of life.37
Overall, decisions regarding discontinuing medical treatments in advanced AD should be made by balancing the likelihood of benefit with the potential for adverse effects.38 For example, the American Geriatrics Society recently recommended against feeding tubes because they often result in discomfort due to agitation, use of restraints, and worsening pressure ulcers.39
Unfortunately, only a minority of families receives straightforward information on the course and prognosis of AD, including the fact that patients eventually stop eating and that the natural cause of death is often an acute infection. Studies also show that patients with dementia are at risk for inadequate treatment of pain.40 Assuring adequate pain control is an essential component of end-of-life care.
Hospice. End-of-life care can often be improved with hospice care. This service is underused by patients with dementia, even though hospice care is available at no cost through Medicare. Hospice eligibility criteria for patients with AD are shown in
TABLE 3.41,42
Finally, a word about prevention
Numerous risk factors have been associated with an increased risk of AD (TABLE 4)2,3. Some, like age and genetics, are nonmodifiable, while others—particularly cardiovascular risk factors—can be modified.1 There are also factors associated with decreased risk, most notably, physical exercise and participating in cognitively stimulating activities.3 Identification of these factors has led to the hope that addressing them can prevent AD.
But association does not equal causation. In 2010, a report from the National Institutes of Health concluded that, although there are modifiable factors associated with AD, there is insufficient evidence that addressing any of them will actually prevent AD.43 In fact, there is good evidence that some of these factors (eg, statin therapy) are not effective in reducing the incidence of dementia, and that others (eg, vitamin E and estrogen therapy) are potentially harmful.44
The absence of empirically supported preventive interventions does not mean, however, that we should disregard these risks and protective factors. Encouraging social engagement, for example, may improve both emotional health and quality of life. Addressing cardiovascular risk factors can reduce the rate of coronary and cerebrovascular disease, potentially including vascular dementia, even if it does not reduce the rate of AD.
Studies are evaluating the use of monoclonal antibodies with anti-amyloid properties for preventing AD in individuals who have APOE ε4 genotypes or high amyloid loads on neuroimaging.45 It will be several years before results are available, however, and the outcome of these studies is uncertain as the use of anti-amyloid agents for treating established dementia has not been effective.46,47
CORRESPONDENCE
Marisa Menchola, PhD, Department of Psychiatry, University of Arizona College of Medicine, 1501 N. Campbell Ave., 7OPC. Tucson, AZ 85724; marisam@psychiatry.arizona.edu
1. Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimer’s Association Web site. Available at: http://www.alz.org/downloads/facts_figures_2013.pdf. Accessed December 2, 2014.
2. Román GC, Nash DT, Fillit H. Translating current knowledge into dementia prevention. Alzheimer Dis Assoc Disord. 2012;26:295-299.
3. Jak, AJ. The impact of physical and mental activity on cognitive aging. Curr Top Behav Neurosci. 2012;10:273-291.
4. US Preventive Services Task Force. Cognitive impairment in older adults: Screening. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/Page/Topic/recommendation-summary/cognitive-impairment-in-older-adults-screening. Accessed November 28, 2014.
5. Centers for Medicare & Medicaid Services. The guide to Medicare preventive services. 4th ed. 2011. Available at: http://www.curemd.com/fqhc/The%20Guide%20to%20Medicare%20Preventative%20Services%20for%20Physicans,%20Providers%20and%20Suppliers.pdf. Accessed December 2, 2014.
6. Boustani, M. Dementia screening in primary care: not too fast! J Amer Geriatr Soc. 2013;61:1205-1207.
7. Alzheimer’s Association. Know the 10 signs: Early detection matters. Alzheimer’s Association Web site. Available at: http://www.alz.org/national/documents/checklist_10signs.pdf. Accessed December 2, 2014.
8. Cordell CB, Borson S, Boustani M, et al; Medicare Detection of Cognitive Impairment Workgroup. Alzheimer’s Association recommendations for operationalizing the detection of cognitive impairment during the Medicare Annual Wellness Visit in a primary care setting. Alzheimers Dement. 2013;9:141-150.
9. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263-269.
10. The American Geriatrics Society. A guide to dementia diagnosis and treatment. The American Geriatrics Society Web site. Available at: http://dementia.americangeriatrics.org/documents/AGS_PC_Dementia_Sheet_2010v2.pdf. Accessed December
2, 2014.
11. Jack CR, Knopman DS, Jagust WJ, et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12:207-216.
12. Johnson KA, Minoshima S, Bohnen NI, et al; Alzheimer’s Association; Society of Nuclear Medicine and Molecular Imaging; Amyloid Imaging Taskforce. Appropriate use criteria for amyloid PET: a report of the Amyloid Imaging Task Force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer’s Association. Alzheimers Dement. 2013;9:e1-e16.
13. Centers for Medicare and Medicaid Services. National coverage determination (NCD) for FDG PET for dementia and neurodegenerative diseases (220.6.13). Centers for Medicare and Medicaid Services Web site. Available at: http://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=288&ncdver=3&bc=BAABAAAAAAAA&. Accessed December 2, 2014.
14. Albert MS, DeKosky ST, Ruckson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270-179.
15. Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia—meta-analysis of 41 robust inception studies. Acta Psychiatr Scand. 2009;119:252-265.
16. Farias ST, Mungas D, Reed BR, et al. Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts. Arch Neurol. 2009;66:1151-1157.
17. Bensadon BA, Odenheimer GL. Current management decisions in mild cognitive impairment. Clin Geriatr Med. 2013;29:847-871.
18. Ngo-Metzger Q, August KJ, Srinivasan M, et al. End-of-life care: guidelines for patient-centered communication. Am Fam Physician. 2008;77:167-174.
19. Sayegh P, Knight BG. Cross-cultural differences in dementia: the Sociocultural Health Belief Model. Int Psychogeriatr. 2013;25:517-530.
20. McDaniel SH, Campbell TL, Hepworth J, et al. Family-Oriented Primary Care. 2nd ed. New York, NY: Springer; 2005.
21. Bensadon BA, Odenheimer GL. Current management decisions in mild cognitive impairment. Clin Geriatr Med. 2013:29;847-871.
22. Russ TC, Morling JR. Cholinesterase inhibitors for mild cognitive impairment. Cochrane Database Syst Rev. 2012;9:CD009132.
23. Sadowsky CH, Galvin JE. Guidelines for the management of cognitive and behavioral problems in dementia. J Am Board Fam Med. 2012;25:350-366.
24. Birks J. Cholinesterase inhibitors for Alzheimer’s disease. Cochrane Database Syst Rev. 2006;(1):CD005593.
25. Fillit HM, Doody RS, Binaso K, et al. Recommendations for best practices in the treatment of Alzheimer’s disease in managed care. Am J Geriatr Pharmacother. 2006;4(suppl A):S9-S24;quiz S25-S28.
26. Schneider LS, Tariot PN, Dagerman KS, et al; CATIE-AD Study Group. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer’s disease. N Engl J Med. 2006;355:1525-1538.
27. US Food and Drug Administration. Public health advisory: Deaths with antipsychotics in elderly patients with behavioral disturbances. US Food and Drug Administration Web site. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm053171.htm. Published April 11, 2005. Updated August 16, 2013. Accessed December 2, 2014.
28. The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60:616-631.
29. Brummel-Smith K. It’s time to require written informed consent when using antipsychotics in dementia. Br J Med Pract. 2008;1:4-6.
30. Huckans M, Hutson L, Twamley E, et al. Efficacy of cognitive rehabilitation therapies for mild cognitive impairment (MCI) in older adults: working toward a theoretical model and evidence-based interventions. Neuropsychol Rev. 2013;23:63-80.
31. Woods B, Aguirre E, Spector AE, et al. Cognitive stimulation to improve cognitive functioning in people with dementia. Cochrane Database Syst Rev. 2012;2:CD005562.
32. McLaren AN, Lamantia MA, Callahan CM. Systematic review of non-pharmacologic interventions to delay functional decline in community-dwelling patients with dementia. Aging Ment Health. 2013;17:655-666.
33. Bahar-Fuchs A, Clare L, Woods B. Cognitive training and cognitive rehabilitation for mild to moderate Alzheimer’s disease and vascular dementia. Cochrane Database Syst Rev. 2013;6:CD003260.
34. Logsdon RG, McCurry SM, Teri L. Evidence-based psychological treatments for disruptive behaviors in individuals with dementia. Psychol Aging. 2007;22:28-36.
35. Raetz J. A nondrug approach to dementia. J Fam Pract. 2013;62:548-557.
36. Gallagher-Thompson D, Coon DW. Evidence-based psychological treatments for distress in family caregivers of older adults. Psychol Aging. 2007;22:37-51.
37. Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009:361:1529-1538.
38. Parsons C, Hughes CM, Passmore AP, et al. Withholding, discontinuing and withdrawing medications in dementia patients at the end of life: a neglected problem in the disadvantaged dying? Drugs Aging. 2010;27:435-449.
39. The American Geriatrics Society. Feeding tubes in advanced dementia position statement. The American Geriatrics Society Web site. Available at: http://www.americangeriatrics.org/files/documents/feeding.tubes.advanced.dementia.pdf. Accessed November 19, 2013.
40. Goodman C, Evans C, Wilcock J, et al. End of life care for community dwelling older people with dementia: an integrated review. Int J Geriatr Psychiatry. 2010;25:329-337.
41. Storey CP. A quick-reference guide to the hospice and palliative care training for physicians: UNIPAC self-study program. American Academy of Hospice and Palliative Medicine. Chicago; 2009.
42. Kaszniak AW, Kligman EW. Hospice care for patients with dementia. Elder Care. 2013. Arizona Alzheimer's Consortium Web site. Available at: http://azalz.org/wp-content/uploads/2013/07/Hospice-Care-for-Pts-with-Dementia.pdf. Accessed December 2, 2014.
43. Daviglus ML, Bell CC, Berrettini W, et al. NIH state-of-the-science conference statement: Preventing Alzheimer’s disease and cognitive decline. NIH Consens State Sci Statements. 2010;27:1-30.
44. Patterson C, Feightner JW, Garcia A, et al. Diagnosis and treatment of dementia: 1. Risk assessment and primary prevention of Alzheimer disease. CMAJ. 2008;178:548-556.
45. Carrillo MC, Brashear HR, Logovinsky V, et al. Can we prevent Alzheimer’s disease? Secondary “prevention” trials in Alzheimer’s disease. Alzheimers Dement. 2013;9:123-131.e1.
46. Salloway S, Sperling R, Fox NC, et al; Bapineuzumab 301 and 302 Clinical Trial Investigators. Two phase 3 trials of bapineuzumab in mild-to-moderate Alzheimer’s Disease. N Engl J Med. 2014;370:322-333.
47. Doody RS, Thomas RG, Farlow M, et al; Alheimer’s Disease Cooperative Study Steering Committee; Solanezumab Study Group. Phase 3 trials of solanezumab for mild-to-moderate Alzheimer’s Disease. N Engl J Med. 2014:370:311-321.
› Refer patients for formal neuropsychological testing when dementia is suspected but the history, clinical interview, and brief cognitive tests do not result in a definitive diagnosis. C
› Use non-drug therapies as first-line treatment for behavioral symptoms of Alzheimer’s disease (AD), as the adverse effects of drug therapy generally offset any benefit. B
› Recommend against feeding tubes for patients with late-stage AD as they are more apt to cause discomfort than to provide benefit. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Alzheimer’s disease (AD), the most common form of dementia, affects more than 5 million Americans.1 Estimates suggest that by 2050, the prevalence could triple, reaching 13 to 16 million.1 To effectively care for patients with AD and their families, family physicians need to be familiar with the latest evidence on all facets of care, from initial detection to patient management and end-of-life care.
This evidence-based review will help you toward that end by answering common questions regarding Alzheimer’s care, including whether routine screening is advisable, what tests should be ordered, which interventions (including nonpharmacologic options) are worth considering, and how best to counsel patients and families about end-of-life care.
Routine screening? Still subject to debate
In considering routine dementia screening in primary care, the key question is whether screening improves outcomes. Advocates note that individuals with dementia may appear unimpaired during office visits and may not report symptoms due to lack of insight; they point out, too, that waiting for an event that makes cognitive impairment obvious, such as a driving mishap, is risky.2 Those who advocate routine screening also note that only about half of those who have dementia are ever diagnosed.3
Others, including the US Preventive Services Task Force (USPSTF), disagree. In its 2014 evidence review, the USPSTF indicated that there is “insufficient evidence to assess the balance of benefits and harms of screening for cognitive impairment in older adults.”4
Mixed messages
The dearth of evidence is also reflected in the conflicting recommendations of the Affordable Care Act (ACA) and the Centers for Medicare and Medicaid Services (CMS). The ACA requires physicians to assess the cognitive function of Medicare patients during their annual wellness visits. CMS, however, instructs providers to screen for dementia only if observation or concerns raised by the patient or family suggest the possibility of impairment, and does not recommend any particular test.5
Cost-effectiveness analyses raise questions about the value of routine screening, as well. Evidence suggests that if a primary care physician screens 300 older patients, 39 will have a positive screen. But only about half of those 39 will agree to a diagnostic evaluation, and no more than 9 will ultimately be diagnosed with dementia. The estimated cost of identifying 9 cases is nearly $40,000—all in the absence of a treatment to cure or stop the progression of the disorder.6
The bottom line: Evidence does not support routine dementia screening of older adults. When cognitive impairment is suspected, however, physicians should conduct a diagnostic evaluation—and consider educating patients and families about the Alzheimer’s Association (AA)’s 10 warning signs of AD.7 (See “Is it Alzheimer’s? 10 warning signs”7 below.) A longer version, available at http://www.alz.org/national/documents/checklist_10signs.pdf, outlines the cognitive changes that are characteristic of healthy aging and compares them to changes suggestive of early dementia.7
Is it Alzheimer’s? 10 warning signs7 1. Memory loss that disrupts daily life |
How to proceed when you suspect AD
Step 1: Screening instrument. The first step in the diagnostic evaluation of a patient with suspected AD is to determine if, in fact, cognitive impairment is present. This can be done by screening with in-office screening instruments, such as the Mini-Cog (available at alz.org/documents_custom/minicog.pdf) or Mini-Mental State Examination (MMSE; health.gov.bc.ca/pharmacare/adti/clinician/pdf/ADTI%20SMMSE-GDS%20Reference%20Card.pdf), among others.8
Step 2: Clinical evaluation. If observation and test results suggest cognitive impairment, the next step is to determine whether clinical findings are consistent with the diagnostic criteria for AD (TABLE 1)9 developed by workgroups from the National Institute on Aging (NIA)/AA in 2011. A work-up is necessary to identify conditions that can mimic dementia (eg, depression) and behaviors that suggest another type of dementia, such as frontotemporal or Lewy body dementia.10 Lab testing should be included to rule out potentially reversible causes of cognitive dysfunction (eg, hypothyroidism, vitamin D deficiency).
Step 3: Neuropsychological evaluation. The NIA/AA recommends neuropsychological testing when the brief cognitive tests, history, and clinical work-up are not sufficient for a definitive diagnosis of dementia.9This generally involves a referral to a neuropsychologist, who conducts a battery of standardized tests to evaluate attention, memory, language, visual-spatial abilities, and executive functions, among others. Neuropsychological testing can confirm the presence of cognitive impairment and aid in the differential diagnosis by comparing the patient’s performance in these domains with characteristic features of different dementia syndromes.
Step 4: Brain imaging with either computed tomography or magnetic resonance imaging can be included in the work-up for patients with suspected AD to rule out abnormalities—eg, metastatic cancer, hydrocephalus, or occult chronic subdural hematoma—that could be causing cognitive impairment.9,10 Clinical features that generally warrant brain imaging include onset of cognitive impairment before age 60; unexplained focal neurologic signs or symptoms; abrupt onset or rapid decline; and/or predisposing conditions, such as cancer or anticoagulant treatment.10
The role of biomarkers and advanced brain imaging
Biomarkers that might provide confirmation of AD in patients who exhibit early symptoms of dementia have been studied extensively.11 The NIA/AA identified 2 categories of AD biomarkers:
- tests for β-amyloid deposition in the brain, including spinal fluid assays for β-amyloid (Aβ42) and positron emission tomography (PET) scans after intravenous injection of florbetapir or flutemetamol, which bind to amyloid in the brain; and
- tests for neuronal degeneration, which would include spinal fluid assays for tau protein and PET scans after injection of fluorodeoxyglucose (FDG), which shows decreased uptake in patients with AD.9
Research reveals the promise of these biomarkers as diagnostic tools, particularly in patients with an atypical presentation of dementia or mild cognitive impairment (MCI) that may be associated with early AD.12 (More on MCI in a moment.) However, the NIA/AA concluded that additional research is needed to validate these tests for routine diagnostic purposes. Medicare covers PET scans with FDG only for the differential diagnosis of AD vs frontotemporal dementia.13
Mild cognitive impairment: How likely that it will progress?
Along with diagnostic criteria for AD, the NIA/AA developed criteria for a symptomatic predementia phase of AD—often referred to as MCI.14 According to the workgroup, MCI is diagnosed when:
2. there is evidence of cognitive impairment, ideally through psychometric testing, revealing performance below expectation based on the patient’s age and education;
3. the patient is able to maintain independent functioning in daily life, despite mild problems or the need for minimal assistance; and
4. there is no significant impairment in social or occupational functioning.14
Progression: Less likely than you might think
Patients with MCI are at risk for progression to overt dementia, with an overall annual conversion rate from MCI to dementia estimated at 10% to 15%.15,16 This estimate must be interpreted with caution, however, because most studies were conducted prior to the 2011 guidelines, when different diagnostic criteria were used. Observers have noted, too, that the numbers largely reflect data collected in specialty clinics and that community-based studies reveal substantially lower conversion rates (3%-6% per year).16 In addition, evidence suggests that many patients with MCI demonstrate long-term stability or even reversal of deficits.17
While there is some consideration of the use of biomarkers and amyloid imaging tests to help determine which patients with MCI will progress to AD, practice guidelines do not currently recommend such testing and it is not covered by Medicare.
When evidence indicates an AD diagnosis
When faced with the need to communicate an AD diagnosis, follow the general recommendations for delivering any bad news or discouraging prognosis:
Prioritize and limit the information you provide, determining not only what the patient and family want to hear, but also how much they are able to comprehend.
Confirm that the patient and family understand the information you’ve provided.
Offer emotional support and recommend additional resources18 (TABLE 2).
Given the progressive cognitive decline that characterizes AD, it is important to address the primary caregiver’s understanding of, and ability to cope with, the disease. It is also important to explore beliefs and attitudes regarding AD. Keep in mind that different cultural groups tend to differ in their beliefs about the nature, cause, and appropriate management of AD, as well as the role of spirituality, help-seeking, and stigma.19,20
The progressive and ultimately fatal nature of AD also makes planning for the future a priority. Ideally, patients should be engaged in discussions regarding end-of-life care as early as possible, while they are still able to make informed decisions and express their preferences. Discussing end-of-life care can be overwhelming for newly diagnosed patients and their families, however, so it is important that you address issues—medical, financial, and legal planning, for example—that families should be considering.
TABLE 2
| Resources for newly diagnosed patients and families | |
| Issue | Resources |
| Education | Alzheimer’s and Dementia Caregiver Center http://www.alz.org/care/overview.asp NIA Alzheimer’s Disease Education and Referral Center http://www.nia.nih.gov/alzheimers/ |
| Planning (medical, financial, legal)/benefits | AARP Caregiving Resource Center http://www.aarp.org/home-family/caregiving Alzheimer’s Association Alzheimer’s Navigator https://www.alzheimersnavigator.org/ National Council on Aging Benefits Checkup https://www.benefitscheckup.org/ |
| Safety | Association for Driver Rehabilitation Specialists: Driving and Alzheimer’s/Dementia https://c.ymcdn.com/sites/www.aded.net/resource/resmgr/fact_Sheets/ADED_alzheimers-Dementia_fac.pdf NIA’s Home Safety for People with Alzheimer’s booklet http://www.nia.nih.gov/alzheimers/publication/home-safety-people-alzheimers-disease |
| Support | Caregiver Action Network http://caregiveraction.org/ |
Drugs address cognitive and behavioral function
No currently available treatments can cure or significantly alter the progression of AD, but 2 classes of medications are used in an attempt to improve cognitive function. One is cholinesterase inhibitors (ChEIs), which potentiate acetylcholine synaptic transmission. The other is N-methyl-D-aspartate (NMDA) glutamate receptor blockers. Other classes of drugs are sometimes used to treat behavioral symptoms of dementia, such as agitation, aggression, mood disorders, and psychosis (eg, delusions and hallucinations).
Cognitive function. Results from studies of pharmacologic management of MCI vary widely, but recent reviews have found no convincing evidence that either ChEIs or NMDA receptor blockers have an effect on progression from MCI to dementia.21,22 Neither class is FDA-approved for treating MCI.
In patients with dementia, the effects of ChEIs and NMDA receptor blockers on cognition are statistically significant but modest, and often of questionable clinical relevance.23 Nonetheless, among ChEIs, donepezil is approved by the US Food and Drug Administration (FDA) for mild, moderate, and severe dementia and galantamine and rivastigmine are approved for mild and moderate dementia. There is no evidence that any one ChEI is more effective than any other,24 and the choice of drugs is often guided by cost, adverse effects, and health plan formularies. Memantine, the only FDA-approved NMDA receptor blocker, is approved for moderate to severe dementia and can be used alone or in combination with a ChEI.
If these drugs are used in an attempt to improve cognition in AD, guidelines recommend the following approach for initial therapy: Prescribe a ChEI for the mild stage, a ChEI plus memantine for the moderate stage, and memantine (with or without a ChEI) for the severe stage.25 The recommendations also include monitoring every 6 months.
There is no consensus about when to discontinue medication. Various published recommendations call for continuing treatment until the patient has “lost all cognitive and functional abilities;”22 until the patient’s MMSE score falls below 10 and there is no indication that the drug is having a “worthwhile effect;”21 or until he or she has reached stage 7 on the Reisberg Functional Assessment Staging scale, indicating nonambulatory status with speech limited to one to 5 words a day.10
Behavioral function. A variety of drugs are used to treat behavioral symptoms in AD. While not FDA-approved for this use, the most widely prescribed agents are second-generation antipsychotics (aripiprazole, olanzapine, quetiapine, and risperidone). The main effect of these drugs is often nothing more than sedation, and one large multisite clinical trial concluded that the adverse effects offset the benefits for patients with AD.26 Indeed, the FDA has issued an advisory on the use of second-generation antipsychotics in AD patients, stating that they are associated with an increased risk of death.27 The recently updated Beers Criteria strongly recommend avoiding these drugs for treating behavioral disturbances in AD unless nonpharmacologic options have failed and the patient is a threat to self or others.28
Because of the black-box warning that antipsychotics increase the risk of death, some physicians have advocated obtaining informed consent prior to prescribing such medications.29 At the very least, when family or guardians are involved, a conversation about risks vs benefits should take place and be documented in the medical record.
Other drug classes are also sometimes used in an attempt to improve behavioral function, including anti-seizure medications (valproic acid, carbamazepine), antidepressants (trazodone and selective serotonin reuptake inhibitors), and anxiolytics (benzodiazepines and buspirone). Other than their sedating effects, there is no strong evidence that these drugs are effective for treating dementia-related behavioral disorders. If used, caution is required due to potential adverse effects.
Nonpharmacologic management is “promising”
A recent systematic review of nonpharmacologic interventions for MCI evaluated exercise, training in compensatory strategies, and engagement in cognitively stimulating activities and found “promising but inconclusive” results. The researchers found that studies show mostly positive effects on cognition but have significant methodologic limitations.30 Importantly, there is no evidence of delayed or reduced conversion to dementia.
For patients who already have mild-to-moderate dementia, cognitive stimulation seems to help in the short term.31 There is also some evidence that exercise and occupational therapy may slow functional decline,32 but the effects are small to modest and their actual clinical significance (eg, the ability to delay institutionalization) is unclear. There is promising but preliminary evidence that cognitive rehabilitation (helping patients devise strategies to complete daily activities) may improve functioning in everyday life.33
While behavioral symptoms are often due to the dementia itself, it is important to identify and treat medical and environmental causes that may be contributing, such as infection, pain, and loud or unsafe environments. As noted before, nonpharmacologic treatments are generally preferred for behavioral problems and should be considered prior to drug therapy. Approaches that identify and modify both the antecedents and consequences of problem behaviors and increase pleasant events have empirical support for the management of behavioral symptoms.34 Interventions including massage therapy, aromatherapy, exercise, and music therapy may also be effective in the short term for agitated behavior.35
Caregivers should be encouraged to receive training in these strategies through organizations like AA. Caregiver education and support can reduce caregivers’ distress and increase their self-efficacy and coping skills.36
End-of-life care must be addressed
Perhaps the most important aspect of end-of-life care in AD is assuring that families (or health care proxies) understand that AD is a fatal illness, with most patients dying within 4 to 8 years of diagnosis.1 Evidence indicates that patients whose proxies have a clear recognition of this are less likely to experience “burdensome” interventions such as parenteral therapy, emergency department visits, hospital admissions, and tube feedings in their last 3 months of life.37
Overall, decisions regarding discontinuing medical treatments in advanced AD should be made by balancing the likelihood of benefit with the potential for adverse effects.38 For example, the American Geriatrics Society recently recommended against feeding tubes because they often result in discomfort due to agitation, use of restraints, and worsening pressure ulcers.39
Unfortunately, only a minority of families receives straightforward information on the course and prognosis of AD, including the fact that patients eventually stop eating and that the natural cause of death is often an acute infection. Studies also show that patients with dementia are at risk for inadequate treatment of pain.40 Assuring adequate pain control is an essential component of end-of-life care.
Hospice. End-of-life care can often be improved with hospice care. This service is underused by patients with dementia, even though hospice care is available at no cost through Medicare. Hospice eligibility criteria for patients with AD are shown in
TABLE 3.41,42
Finally, a word about prevention
Numerous risk factors have been associated with an increased risk of AD (TABLE 4)2,3. Some, like age and genetics, are nonmodifiable, while others—particularly cardiovascular risk factors—can be modified.1 There are also factors associated with decreased risk, most notably, physical exercise and participating in cognitively stimulating activities.3 Identification of these factors has led to the hope that addressing them can prevent AD.
But association does not equal causation. In 2010, a report from the National Institutes of Health concluded that, although there are modifiable factors associated with AD, there is insufficient evidence that addressing any of them will actually prevent AD.43 In fact, there is good evidence that some of these factors (eg, statin therapy) are not effective in reducing the incidence of dementia, and that others (eg, vitamin E and estrogen therapy) are potentially harmful.44
The absence of empirically supported preventive interventions does not mean, however, that we should disregard these risks and protective factors. Encouraging social engagement, for example, may improve both emotional health and quality of life. Addressing cardiovascular risk factors can reduce the rate of coronary and cerebrovascular disease, potentially including vascular dementia, even if it does not reduce the rate of AD.
Studies are evaluating the use of monoclonal antibodies with anti-amyloid properties for preventing AD in individuals who have APOE ε4 genotypes or high amyloid loads on neuroimaging.45 It will be several years before results are available, however, and the outcome of these studies is uncertain as the use of anti-amyloid agents for treating established dementia has not been effective.46,47
CORRESPONDENCE
Marisa Menchola, PhD, Department of Psychiatry, University of Arizona College of Medicine, 1501 N. Campbell Ave., 7OPC. Tucson, AZ 85724; marisam@psychiatry.arizona.edu
› Refer patients for formal neuropsychological testing when dementia is suspected but the history, clinical interview, and brief cognitive tests do not result in a definitive diagnosis. C
› Use non-drug therapies as first-line treatment for behavioral symptoms of Alzheimer’s disease (AD), as the adverse effects of drug therapy generally offset any benefit. B
› Recommend against feeding tubes for patients with late-stage AD as they are more apt to cause discomfort than to provide benefit. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Alzheimer’s disease (AD), the most common form of dementia, affects more than 5 million Americans.1 Estimates suggest that by 2050, the prevalence could triple, reaching 13 to 16 million.1 To effectively care for patients with AD and their families, family physicians need to be familiar with the latest evidence on all facets of care, from initial detection to patient management and end-of-life care.
This evidence-based review will help you toward that end by answering common questions regarding Alzheimer’s care, including whether routine screening is advisable, what tests should be ordered, which interventions (including nonpharmacologic options) are worth considering, and how best to counsel patients and families about end-of-life care.
Routine screening? Still subject to debate
In considering routine dementia screening in primary care, the key question is whether screening improves outcomes. Advocates note that individuals with dementia may appear unimpaired during office visits and may not report symptoms due to lack of insight; they point out, too, that waiting for an event that makes cognitive impairment obvious, such as a driving mishap, is risky.2 Those who advocate routine screening also note that only about half of those who have dementia are ever diagnosed.3
Others, including the US Preventive Services Task Force (USPSTF), disagree. In its 2014 evidence review, the USPSTF indicated that there is “insufficient evidence to assess the balance of benefits and harms of screening for cognitive impairment in older adults.”4
Mixed messages
The dearth of evidence is also reflected in the conflicting recommendations of the Affordable Care Act (ACA) and the Centers for Medicare and Medicaid Services (CMS). The ACA requires physicians to assess the cognitive function of Medicare patients during their annual wellness visits. CMS, however, instructs providers to screen for dementia only if observation or concerns raised by the patient or family suggest the possibility of impairment, and does not recommend any particular test.5
Cost-effectiveness analyses raise questions about the value of routine screening, as well. Evidence suggests that if a primary care physician screens 300 older patients, 39 will have a positive screen. But only about half of those 39 will agree to a diagnostic evaluation, and no more than 9 will ultimately be diagnosed with dementia. The estimated cost of identifying 9 cases is nearly $40,000—all in the absence of a treatment to cure or stop the progression of the disorder.6
The bottom line: Evidence does not support routine dementia screening of older adults. When cognitive impairment is suspected, however, physicians should conduct a diagnostic evaluation—and consider educating patients and families about the Alzheimer’s Association (AA)’s 10 warning signs of AD.7 (See “Is it Alzheimer’s? 10 warning signs”7 below.) A longer version, available at http://www.alz.org/national/documents/checklist_10signs.pdf, outlines the cognitive changes that are characteristic of healthy aging and compares them to changes suggestive of early dementia.7
Is it Alzheimer’s? 10 warning signs7 1. Memory loss that disrupts daily life |
How to proceed when you suspect AD
Step 1: Screening instrument. The first step in the diagnostic evaluation of a patient with suspected AD is to determine if, in fact, cognitive impairment is present. This can be done by screening with in-office screening instruments, such as the Mini-Cog (available at alz.org/documents_custom/minicog.pdf) or Mini-Mental State Examination (MMSE; health.gov.bc.ca/pharmacare/adti/clinician/pdf/ADTI%20SMMSE-GDS%20Reference%20Card.pdf), among others.8
Step 2: Clinical evaluation. If observation and test results suggest cognitive impairment, the next step is to determine whether clinical findings are consistent with the diagnostic criteria for AD (TABLE 1)9 developed by workgroups from the National Institute on Aging (NIA)/AA in 2011. A work-up is necessary to identify conditions that can mimic dementia (eg, depression) and behaviors that suggest another type of dementia, such as frontotemporal or Lewy body dementia.10 Lab testing should be included to rule out potentially reversible causes of cognitive dysfunction (eg, hypothyroidism, vitamin D deficiency).
Step 3: Neuropsychological evaluation. The NIA/AA recommends neuropsychological testing when the brief cognitive tests, history, and clinical work-up are not sufficient for a definitive diagnosis of dementia.9This generally involves a referral to a neuropsychologist, who conducts a battery of standardized tests to evaluate attention, memory, language, visual-spatial abilities, and executive functions, among others. Neuropsychological testing can confirm the presence of cognitive impairment and aid in the differential diagnosis by comparing the patient’s performance in these domains with characteristic features of different dementia syndromes.
Step 4: Brain imaging with either computed tomography or magnetic resonance imaging can be included in the work-up for patients with suspected AD to rule out abnormalities—eg, metastatic cancer, hydrocephalus, or occult chronic subdural hematoma—that could be causing cognitive impairment.9,10 Clinical features that generally warrant brain imaging include onset of cognitive impairment before age 60; unexplained focal neurologic signs or symptoms; abrupt onset or rapid decline; and/or predisposing conditions, such as cancer or anticoagulant treatment.10
The role of biomarkers and advanced brain imaging
Biomarkers that might provide confirmation of AD in patients who exhibit early symptoms of dementia have been studied extensively.11 The NIA/AA identified 2 categories of AD biomarkers:
- tests for β-amyloid deposition in the brain, including spinal fluid assays for β-amyloid (Aβ42) and positron emission tomography (PET) scans after intravenous injection of florbetapir or flutemetamol, which bind to amyloid in the brain; and
- tests for neuronal degeneration, which would include spinal fluid assays for tau protein and PET scans after injection of fluorodeoxyglucose (FDG), which shows decreased uptake in patients with AD.9
Research reveals the promise of these biomarkers as diagnostic tools, particularly in patients with an atypical presentation of dementia or mild cognitive impairment (MCI) that may be associated with early AD.12 (More on MCI in a moment.) However, the NIA/AA concluded that additional research is needed to validate these tests for routine diagnostic purposes. Medicare covers PET scans with FDG only for the differential diagnosis of AD vs frontotemporal dementia.13
Mild cognitive impairment: How likely that it will progress?
Along with diagnostic criteria for AD, the NIA/AA developed criteria for a symptomatic predementia phase of AD—often referred to as MCI.14 According to the workgroup, MCI is diagnosed when:
2. there is evidence of cognitive impairment, ideally through psychometric testing, revealing performance below expectation based on the patient’s age and education;
3. the patient is able to maintain independent functioning in daily life, despite mild problems or the need for minimal assistance; and
4. there is no significant impairment in social or occupational functioning.14
Progression: Less likely than you might think
Patients with MCI are at risk for progression to overt dementia, with an overall annual conversion rate from MCI to dementia estimated at 10% to 15%.15,16 This estimate must be interpreted with caution, however, because most studies were conducted prior to the 2011 guidelines, when different diagnostic criteria were used. Observers have noted, too, that the numbers largely reflect data collected in specialty clinics and that community-based studies reveal substantially lower conversion rates (3%-6% per year).16 In addition, evidence suggests that many patients with MCI demonstrate long-term stability or even reversal of deficits.17
While there is some consideration of the use of biomarkers and amyloid imaging tests to help determine which patients with MCI will progress to AD, practice guidelines do not currently recommend such testing and it is not covered by Medicare.
When evidence indicates an AD diagnosis
When faced with the need to communicate an AD diagnosis, follow the general recommendations for delivering any bad news or discouraging prognosis:
Prioritize and limit the information you provide, determining not only what the patient and family want to hear, but also how much they are able to comprehend.
Confirm that the patient and family understand the information you’ve provided.
Offer emotional support and recommend additional resources18 (TABLE 2).
Given the progressive cognitive decline that characterizes AD, it is important to address the primary caregiver’s understanding of, and ability to cope with, the disease. It is also important to explore beliefs and attitudes regarding AD. Keep in mind that different cultural groups tend to differ in their beliefs about the nature, cause, and appropriate management of AD, as well as the role of spirituality, help-seeking, and stigma.19,20
The progressive and ultimately fatal nature of AD also makes planning for the future a priority. Ideally, patients should be engaged in discussions regarding end-of-life care as early as possible, while they are still able to make informed decisions and express their preferences. Discussing end-of-life care can be overwhelming for newly diagnosed patients and their families, however, so it is important that you address issues—medical, financial, and legal planning, for example—that families should be considering.
TABLE 2
| Resources for newly diagnosed patients and families | |
| Issue | Resources |
| Education | Alzheimer’s and Dementia Caregiver Center http://www.alz.org/care/overview.asp NIA Alzheimer’s Disease Education and Referral Center http://www.nia.nih.gov/alzheimers/ |
| Planning (medical, financial, legal)/benefits | AARP Caregiving Resource Center http://www.aarp.org/home-family/caregiving Alzheimer’s Association Alzheimer’s Navigator https://www.alzheimersnavigator.org/ National Council on Aging Benefits Checkup https://www.benefitscheckup.org/ |
| Safety | Association for Driver Rehabilitation Specialists: Driving and Alzheimer’s/Dementia https://c.ymcdn.com/sites/www.aded.net/resource/resmgr/fact_Sheets/ADED_alzheimers-Dementia_fac.pdf NIA’s Home Safety for People with Alzheimer’s booklet http://www.nia.nih.gov/alzheimers/publication/home-safety-people-alzheimers-disease |
| Support | Caregiver Action Network http://caregiveraction.org/ |
Drugs address cognitive and behavioral function
No currently available treatments can cure or significantly alter the progression of AD, but 2 classes of medications are used in an attempt to improve cognitive function. One is cholinesterase inhibitors (ChEIs), which potentiate acetylcholine synaptic transmission. The other is N-methyl-D-aspartate (NMDA) glutamate receptor blockers. Other classes of drugs are sometimes used to treat behavioral symptoms of dementia, such as agitation, aggression, mood disorders, and psychosis (eg, delusions and hallucinations).
Cognitive function. Results from studies of pharmacologic management of MCI vary widely, but recent reviews have found no convincing evidence that either ChEIs or NMDA receptor blockers have an effect on progression from MCI to dementia.21,22 Neither class is FDA-approved for treating MCI.
In patients with dementia, the effects of ChEIs and NMDA receptor blockers on cognition are statistically significant but modest, and often of questionable clinical relevance.23 Nonetheless, among ChEIs, donepezil is approved by the US Food and Drug Administration (FDA) for mild, moderate, and severe dementia and galantamine and rivastigmine are approved for mild and moderate dementia. There is no evidence that any one ChEI is more effective than any other,24 and the choice of drugs is often guided by cost, adverse effects, and health plan formularies. Memantine, the only FDA-approved NMDA receptor blocker, is approved for moderate to severe dementia and can be used alone or in combination with a ChEI.
If these drugs are used in an attempt to improve cognition in AD, guidelines recommend the following approach for initial therapy: Prescribe a ChEI for the mild stage, a ChEI plus memantine for the moderate stage, and memantine (with or without a ChEI) for the severe stage.25 The recommendations also include monitoring every 6 months.
There is no consensus about when to discontinue medication. Various published recommendations call for continuing treatment until the patient has “lost all cognitive and functional abilities;”22 until the patient’s MMSE score falls below 10 and there is no indication that the drug is having a “worthwhile effect;”21 or until he or she has reached stage 7 on the Reisberg Functional Assessment Staging scale, indicating nonambulatory status with speech limited to one to 5 words a day.10
Behavioral function. A variety of drugs are used to treat behavioral symptoms in AD. While not FDA-approved for this use, the most widely prescribed agents are second-generation antipsychotics (aripiprazole, olanzapine, quetiapine, and risperidone). The main effect of these drugs is often nothing more than sedation, and one large multisite clinical trial concluded that the adverse effects offset the benefits for patients with AD.26 Indeed, the FDA has issued an advisory on the use of second-generation antipsychotics in AD patients, stating that they are associated with an increased risk of death.27 The recently updated Beers Criteria strongly recommend avoiding these drugs for treating behavioral disturbances in AD unless nonpharmacologic options have failed and the patient is a threat to self or others.28
Because of the black-box warning that antipsychotics increase the risk of death, some physicians have advocated obtaining informed consent prior to prescribing such medications.29 At the very least, when family or guardians are involved, a conversation about risks vs benefits should take place and be documented in the medical record.
Other drug classes are also sometimes used in an attempt to improve behavioral function, including anti-seizure medications (valproic acid, carbamazepine), antidepressants (trazodone and selective serotonin reuptake inhibitors), and anxiolytics (benzodiazepines and buspirone). Other than their sedating effects, there is no strong evidence that these drugs are effective for treating dementia-related behavioral disorders. If used, caution is required due to potential adverse effects.
Nonpharmacologic management is “promising”
A recent systematic review of nonpharmacologic interventions for MCI evaluated exercise, training in compensatory strategies, and engagement in cognitively stimulating activities and found “promising but inconclusive” results. The researchers found that studies show mostly positive effects on cognition but have significant methodologic limitations.30 Importantly, there is no evidence of delayed or reduced conversion to dementia.
For patients who already have mild-to-moderate dementia, cognitive stimulation seems to help in the short term.31 There is also some evidence that exercise and occupational therapy may slow functional decline,32 but the effects are small to modest and their actual clinical significance (eg, the ability to delay institutionalization) is unclear. There is promising but preliminary evidence that cognitive rehabilitation (helping patients devise strategies to complete daily activities) may improve functioning in everyday life.33
While behavioral symptoms are often due to the dementia itself, it is important to identify and treat medical and environmental causes that may be contributing, such as infection, pain, and loud or unsafe environments. As noted before, nonpharmacologic treatments are generally preferred for behavioral problems and should be considered prior to drug therapy. Approaches that identify and modify both the antecedents and consequences of problem behaviors and increase pleasant events have empirical support for the management of behavioral symptoms.34 Interventions including massage therapy, aromatherapy, exercise, and music therapy may also be effective in the short term for agitated behavior.35
Caregivers should be encouraged to receive training in these strategies through organizations like AA. Caregiver education and support can reduce caregivers’ distress and increase their self-efficacy and coping skills.36
End-of-life care must be addressed
Perhaps the most important aspect of end-of-life care in AD is assuring that families (or health care proxies) understand that AD is a fatal illness, with most patients dying within 4 to 8 years of diagnosis.1 Evidence indicates that patients whose proxies have a clear recognition of this are less likely to experience “burdensome” interventions such as parenteral therapy, emergency department visits, hospital admissions, and tube feedings in their last 3 months of life.37
Overall, decisions regarding discontinuing medical treatments in advanced AD should be made by balancing the likelihood of benefit with the potential for adverse effects.38 For example, the American Geriatrics Society recently recommended against feeding tubes because they often result in discomfort due to agitation, use of restraints, and worsening pressure ulcers.39
Unfortunately, only a minority of families receives straightforward information on the course and prognosis of AD, including the fact that patients eventually stop eating and that the natural cause of death is often an acute infection. Studies also show that patients with dementia are at risk for inadequate treatment of pain.40 Assuring adequate pain control is an essential component of end-of-life care.
Hospice. End-of-life care can often be improved with hospice care. This service is underused by patients with dementia, even though hospice care is available at no cost through Medicare. Hospice eligibility criteria for patients with AD are shown in
TABLE 3.41,42
Finally, a word about prevention
Numerous risk factors have been associated with an increased risk of AD (TABLE 4)2,3. Some, like age and genetics, are nonmodifiable, while others—particularly cardiovascular risk factors—can be modified.1 There are also factors associated with decreased risk, most notably, physical exercise and participating in cognitively stimulating activities.3 Identification of these factors has led to the hope that addressing them can prevent AD.
But association does not equal causation. In 2010, a report from the National Institutes of Health concluded that, although there are modifiable factors associated with AD, there is insufficient evidence that addressing any of them will actually prevent AD.43 In fact, there is good evidence that some of these factors (eg, statin therapy) are not effective in reducing the incidence of dementia, and that others (eg, vitamin E and estrogen therapy) are potentially harmful.44
The absence of empirically supported preventive interventions does not mean, however, that we should disregard these risks and protective factors. Encouraging social engagement, for example, may improve both emotional health and quality of life. Addressing cardiovascular risk factors can reduce the rate of coronary and cerebrovascular disease, potentially including vascular dementia, even if it does not reduce the rate of AD.
Studies are evaluating the use of monoclonal antibodies with anti-amyloid properties for preventing AD in individuals who have APOE ε4 genotypes or high amyloid loads on neuroimaging.45 It will be several years before results are available, however, and the outcome of these studies is uncertain as the use of anti-amyloid agents for treating established dementia has not been effective.46,47
CORRESPONDENCE
Marisa Menchola, PhD, Department of Psychiatry, University of Arizona College of Medicine, 1501 N. Campbell Ave., 7OPC. Tucson, AZ 85724; marisam@psychiatry.arizona.edu
1. Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimer’s Association Web site. Available at: http://www.alz.org/downloads/facts_figures_2013.pdf. Accessed December 2, 2014.
2. Román GC, Nash DT, Fillit H. Translating current knowledge into dementia prevention. Alzheimer Dis Assoc Disord. 2012;26:295-299.
3. Jak, AJ. The impact of physical and mental activity on cognitive aging. Curr Top Behav Neurosci. 2012;10:273-291.
4. US Preventive Services Task Force. Cognitive impairment in older adults: Screening. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/Page/Topic/recommendation-summary/cognitive-impairment-in-older-adults-screening. Accessed November 28, 2014.
5. Centers for Medicare & Medicaid Services. The guide to Medicare preventive services. 4th ed. 2011. Available at: http://www.curemd.com/fqhc/The%20Guide%20to%20Medicare%20Preventative%20Services%20for%20Physicans,%20Providers%20and%20Suppliers.pdf. Accessed December 2, 2014.
6. Boustani, M. Dementia screening in primary care: not too fast! J Amer Geriatr Soc. 2013;61:1205-1207.
7. Alzheimer’s Association. Know the 10 signs: Early detection matters. Alzheimer’s Association Web site. Available at: http://www.alz.org/national/documents/checklist_10signs.pdf. Accessed December 2, 2014.
8. Cordell CB, Borson S, Boustani M, et al; Medicare Detection of Cognitive Impairment Workgroup. Alzheimer’s Association recommendations for operationalizing the detection of cognitive impairment during the Medicare Annual Wellness Visit in a primary care setting. Alzheimers Dement. 2013;9:141-150.
9. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263-269.
10. The American Geriatrics Society. A guide to dementia diagnosis and treatment. The American Geriatrics Society Web site. Available at: http://dementia.americangeriatrics.org/documents/AGS_PC_Dementia_Sheet_2010v2.pdf. Accessed December
2, 2014.
11. Jack CR, Knopman DS, Jagust WJ, et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12:207-216.
12. Johnson KA, Minoshima S, Bohnen NI, et al; Alzheimer’s Association; Society of Nuclear Medicine and Molecular Imaging; Amyloid Imaging Taskforce. Appropriate use criteria for amyloid PET: a report of the Amyloid Imaging Task Force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer’s Association. Alzheimers Dement. 2013;9:e1-e16.
13. Centers for Medicare and Medicaid Services. National coverage determination (NCD) for FDG PET for dementia and neurodegenerative diseases (220.6.13). Centers for Medicare and Medicaid Services Web site. Available at: http://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=288&ncdver=3&bc=BAABAAAAAAAA&. Accessed December 2, 2014.
14. Albert MS, DeKosky ST, Ruckson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270-179.
15. Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia—meta-analysis of 41 robust inception studies. Acta Psychiatr Scand. 2009;119:252-265.
16. Farias ST, Mungas D, Reed BR, et al. Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts. Arch Neurol. 2009;66:1151-1157.
17. Bensadon BA, Odenheimer GL. Current management decisions in mild cognitive impairment. Clin Geriatr Med. 2013;29:847-871.
18. Ngo-Metzger Q, August KJ, Srinivasan M, et al. End-of-life care: guidelines for patient-centered communication. Am Fam Physician. 2008;77:167-174.
19. Sayegh P, Knight BG. Cross-cultural differences in dementia: the Sociocultural Health Belief Model. Int Psychogeriatr. 2013;25:517-530.
20. McDaniel SH, Campbell TL, Hepworth J, et al. Family-Oriented Primary Care. 2nd ed. New York, NY: Springer; 2005.
21. Bensadon BA, Odenheimer GL. Current management decisions in mild cognitive impairment. Clin Geriatr Med. 2013:29;847-871.
22. Russ TC, Morling JR. Cholinesterase inhibitors for mild cognitive impairment. Cochrane Database Syst Rev. 2012;9:CD009132.
23. Sadowsky CH, Galvin JE. Guidelines for the management of cognitive and behavioral problems in dementia. J Am Board Fam Med. 2012;25:350-366.
24. Birks J. Cholinesterase inhibitors for Alzheimer’s disease. Cochrane Database Syst Rev. 2006;(1):CD005593.
25. Fillit HM, Doody RS, Binaso K, et al. Recommendations for best practices in the treatment of Alzheimer’s disease in managed care. Am J Geriatr Pharmacother. 2006;4(suppl A):S9-S24;quiz S25-S28.
26. Schneider LS, Tariot PN, Dagerman KS, et al; CATIE-AD Study Group. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer’s disease. N Engl J Med. 2006;355:1525-1538.
27. US Food and Drug Administration. Public health advisory: Deaths with antipsychotics in elderly patients with behavioral disturbances. US Food and Drug Administration Web site. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm053171.htm. Published April 11, 2005. Updated August 16, 2013. Accessed December 2, 2014.
28. The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60:616-631.
29. Brummel-Smith K. It’s time to require written informed consent when using antipsychotics in dementia. Br J Med Pract. 2008;1:4-6.
30. Huckans M, Hutson L, Twamley E, et al. Efficacy of cognitive rehabilitation therapies for mild cognitive impairment (MCI) in older adults: working toward a theoretical model and evidence-based interventions. Neuropsychol Rev. 2013;23:63-80.
31. Woods B, Aguirre E, Spector AE, et al. Cognitive stimulation to improve cognitive functioning in people with dementia. Cochrane Database Syst Rev. 2012;2:CD005562.
32. McLaren AN, Lamantia MA, Callahan CM. Systematic review of non-pharmacologic interventions to delay functional decline in community-dwelling patients with dementia. Aging Ment Health. 2013;17:655-666.
33. Bahar-Fuchs A, Clare L, Woods B. Cognitive training and cognitive rehabilitation for mild to moderate Alzheimer’s disease and vascular dementia. Cochrane Database Syst Rev. 2013;6:CD003260.
34. Logsdon RG, McCurry SM, Teri L. Evidence-based psychological treatments for disruptive behaviors in individuals with dementia. Psychol Aging. 2007;22:28-36.
35. Raetz J. A nondrug approach to dementia. J Fam Pract. 2013;62:548-557.
36. Gallagher-Thompson D, Coon DW. Evidence-based psychological treatments for distress in family caregivers of older adults. Psychol Aging. 2007;22:37-51.
37. Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009:361:1529-1538.
38. Parsons C, Hughes CM, Passmore AP, et al. Withholding, discontinuing and withdrawing medications in dementia patients at the end of life: a neglected problem in the disadvantaged dying? Drugs Aging. 2010;27:435-449.
39. The American Geriatrics Society. Feeding tubes in advanced dementia position statement. The American Geriatrics Society Web site. Available at: http://www.americangeriatrics.org/files/documents/feeding.tubes.advanced.dementia.pdf. Accessed November 19, 2013.
40. Goodman C, Evans C, Wilcock J, et al. End of life care for community dwelling older people with dementia: an integrated review. Int J Geriatr Psychiatry. 2010;25:329-337.
41. Storey CP. A quick-reference guide to the hospice and palliative care training for physicians: UNIPAC self-study program. American Academy of Hospice and Palliative Medicine. Chicago; 2009.
42. Kaszniak AW, Kligman EW. Hospice care for patients with dementia. Elder Care. 2013. Arizona Alzheimer's Consortium Web site. Available at: http://azalz.org/wp-content/uploads/2013/07/Hospice-Care-for-Pts-with-Dementia.pdf. Accessed December 2, 2014.
43. Daviglus ML, Bell CC, Berrettini W, et al. NIH state-of-the-science conference statement: Preventing Alzheimer’s disease and cognitive decline. NIH Consens State Sci Statements. 2010;27:1-30.
44. Patterson C, Feightner JW, Garcia A, et al. Diagnosis and treatment of dementia: 1. Risk assessment and primary prevention of Alzheimer disease. CMAJ. 2008;178:548-556.
45. Carrillo MC, Brashear HR, Logovinsky V, et al. Can we prevent Alzheimer’s disease? Secondary “prevention” trials in Alzheimer’s disease. Alzheimers Dement. 2013;9:123-131.e1.
46. Salloway S, Sperling R, Fox NC, et al; Bapineuzumab 301 and 302 Clinical Trial Investigators. Two phase 3 trials of bapineuzumab in mild-to-moderate Alzheimer’s Disease. N Engl J Med. 2014;370:322-333.
47. Doody RS, Thomas RG, Farlow M, et al; Alheimer’s Disease Cooperative Study Steering Committee; Solanezumab Study Group. Phase 3 trials of solanezumab for mild-to-moderate Alzheimer’s Disease. N Engl J Med. 2014:370:311-321.
1. Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimer’s Association Web site. Available at: http://www.alz.org/downloads/facts_figures_2013.pdf. Accessed December 2, 2014.
2. Román GC, Nash DT, Fillit H. Translating current knowledge into dementia prevention. Alzheimer Dis Assoc Disord. 2012;26:295-299.
3. Jak, AJ. The impact of physical and mental activity on cognitive aging. Curr Top Behav Neurosci. 2012;10:273-291.
4. US Preventive Services Task Force. Cognitive impairment in older adults: Screening. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/Page/Topic/recommendation-summary/cognitive-impairment-in-older-adults-screening. Accessed November 28, 2014.
5. Centers for Medicare & Medicaid Services. The guide to Medicare preventive services. 4th ed. 2011. Available at: http://www.curemd.com/fqhc/The%20Guide%20to%20Medicare%20Preventative%20Services%20for%20Physicans,%20Providers%20and%20Suppliers.pdf. Accessed December 2, 2014.
6. Boustani, M. Dementia screening in primary care: not too fast! J Amer Geriatr Soc. 2013;61:1205-1207.
7. Alzheimer’s Association. Know the 10 signs: Early detection matters. Alzheimer’s Association Web site. Available at: http://www.alz.org/national/documents/checklist_10signs.pdf. Accessed December 2, 2014.
8. Cordell CB, Borson S, Boustani M, et al; Medicare Detection of Cognitive Impairment Workgroup. Alzheimer’s Association recommendations for operationalizing the detection of cognitive impairment during the Medicare Annual Wellness Visit in a primary care setting. Alzheimers Dement. 2013;9:141-150.
9. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263-269.
10. The American Geriatrics Society. A guide to dementia diagnosis and treatment. The American Geriatrics Society Web site. Available at: http://dementia.americangeriatrics.org/documents/AGS_PC_Dementia_Sheet_2010v2.pdf. Accessed December
2, 2014.
11. Jack CR, Knopman DS, Jagust WJ, et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12:207-216.
12. Johnson KA, Minoshima S, Bohnen NI, et al; Alzheimer’s Association; Society of Nuclear Medicine and Molecular Imaging; Amyloid Imaging Taskforce. Appropriate use criteria for amyloid PET: a report of the Amyloid Imaging Task Force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer’s Association. Alzheimers Dement. 2013;9:e1-e16.
13. Centers for Medicare and Medicaid Services. National coverage determination (NCD) for FDG PET for dementia and neurodegenerative diseases (220.6.13). Centers for Medicare and Medicaid Services Web site. Available at: http://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=288&ncdver=3&bc=BAABAAAAAAAA&. Accessed December 2, 2014.
14. Albert MS, DeKosky ST, Ruckson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270-179.
15. Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia—meta-analysis of 41 robust inception studies. Acta Psychiatr Scand. 2009;119:252-265.
16. Farias ST, Mungas D, Reed BR, et al. Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts. Arch Neurol. 2009;66:1151-1157.
17. Bensadon BA, Odenheimer GL. Current management decisions in mild cognitive impairment. Clin Geriatr Med. 2013;29:847-871.
18. Ngo-Metzger Q, August KJ, Srinivasan M, et al. End-of-life care: guidelines for patient-centered communication. Am Fam Physician. 2008;77:167-174.
19. Sayegh P, Knight BG. Cross-cultural differences in dementia: the Sociocultural Health Belief Model. Int Psychogeriatr. 2013;25:517-530.
20. McDaniel SH, Campbell TL, Hepworth J, et al. Family-Oriented Primary Care. 2nd ed. New York, NY: Springer; 2005.
21. Bensadon BA, Odenheimer GL. Current management decisions in mild cognitive impairment. Clin Geriatr Med. 2013:29;847-871.
22. Russ TC, Morling JR. Cholinesterase inhibitors for mild cognitive impairment. Cochrane Database Syst Rev. 2012;9:CD009132.
23. Sadowsky CH, Galvin JE. Guidelines for the management of cognitive and behavioral problems in dementia. J Am Board Fam Med. 2012;25:350-366.
24. Birks J. Cholinesterase inhibitors for Alzheimer’s disease. Cochrane Database Syst Rev. 2006;(1):CD005593.
25. Fillit HM, Doody RS, Binaso K, et al. Recommendations for best practices in the treatment of Alzheimer’s disease in managed care. Am J Geriatr Pharmacother. 2006;4(suppl A):S9-S24;quiz S25-S28.
26. Schneider LS, Tariot PN, Dagerman KS, et al; CATIE-AD Study Group. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer’s disease. N Engl J Med. 2006;355:1525-1538.
27. US Food and Drug Administration. Public health advisory: Deaths with antipsychotics in elderly patients with behavioral disturbances. US Food and Drug Administration Web site. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm053171.htm. Published April 11, 2005. Updated August 16, 2013. Accessed December 2, 2014.
28. The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60:616-631.
29. Brummel-Smith K. It’s time to require written informed consent when using antipsychotics in dementia. Br J Med Pract. 2008;1:4-6.
30. Huckans M, Hutson L, Twamley E, et al. Efficacy of cognitive rehabilitation therapies for mild cognitive impairment (MCI) in older adults: working toward a theoretical model and evidence-based interventions. Neuropsychol Rev. 2013;23:63-80.
31. Woods B, Aguirre E, Spector AE, et al. Cognitive stimulation to improve cognitive functioning in people with dementia. Cochrane Database Syst Rev. 2012;2:CD005562.
32. McLaren AN, Lamantia MA, Callahan CM. Systematic review of non-pharmacologic interventions to delay functional decline in community-dwelling patients with dementia. Aging Ment Health. 2013;17:655-666.
33. Bahar-Fuchs A, Clare L, Woods B. Cognitive training and cognitive rehabilitation for mild to moderate Alzheimer’s disease and vascular dementia. Cochrane Database Syst Rev. 2013;6:CD003260.
34. Logsdon RG, McCurry SM, Teri L. Evidence-based psychological treatments for disruptive behaviors in individuals with dementia. Psychol Aging. 2007;22:28-36.
35. Raetz J. A nondrug approach to dementia. J Fam Pract. 2013;62:548-557.
36. Gallagher-Thompson D, Coon DW. Evidence-based psychological treatments for distress in family caregivers of older adults. Psychol Aging. 2007;22:37-51.
37. Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009:361:1529-1538.
38. Parsons C, Hughes CM, Passmore AP, et al. Withholding, discontinuing and withdrawing medications in dementia patients at the end of life: a neglected problem in the disadvantaged dying? Drugs Aging. 2010;27:435-449.
39. The American Geriatrics Society. Feeding tubes in advanced dementia position statement. The American Geriatrics Society Web site. Available at: http://www.americangeriatrics.org/files/documents/feeding.tubes.advanced.dementia.pdf. Accessed November 19, 2013.
40. Goodman C, Evans C, Wilcock J, et al. End of life care for community dwelling older people with dementia: an integrated review. Int J Geriatr Psychiatry. 2010;25:329-337.
41. Storey CP. A quick-reference guide to the hospice and palliative care training for physicians: UNIPAC self-study program. American Academy of Hospice and Palliative Medicine. Chicago; 2009.
42. Kaszniak AW, Kligman EW. Hospice care for patients with dementia. Elder Care. 2013. Arizona Alzheimer's Consortium Web site. Available at: http://azalz.org/wp-content/uploads/2013/07/Hospice-Care-for-Pts-with-Dementia.pdf. Accessed December 2, 2014.
43. Daviglus ML, Bell CC, Berrettini W, et al. NIH state-of-the-science conference statement: Preventing Alzheimer’s disease and cognitive decline. NIH Consens State Sci Statements. 2010;27:1-30.
44. Patterson C, Feightner JW, Garcia A, et al. Diagnosis and treatment of dementia: 1. Risk assessment and primary prevention of Alzheimer disease. CMAJ. 2008;178:548-556.
45. Carrillo MC, Brashear HR, Logovinsky V, et al. Can we prevent Alzheimer’s disease? Secondary “prevention” trials in Alzheimer’s disease. Alzheimers Dement. 2013;9:123-131.e1.
46. Salloway S, Sperling R, Fox NC, et al; Bapineuzumab 301 and 302 Clinical Trial Investigators. Two phase 3 trials of bapineuzumab in mild-to-moderate Alzheimer’s Disease. N Engl J Med. 2014;370:322-333.
47. Doody RS, Thomas RG, Farlow M, et al; Alheimer’s Disease Cooperative Study Steering Committee; Solanezumab Study Group. Phase 3 trials of solanezumab for mild-to-moderate Alzheimer’s Disease. N Engl J Med. 2014:370:311-321.
AGING: Is your patient taking too many pills?
• Consider the possibility that an adverse drug effect—rather than a new condition—is at play when a patient taking multiple medications develops a new symptom. C
• Use an online interaction checker, which can be accessed via a smart phone or tablet, to check for potential drug-drug interactions in patients on multiple medications. C
• Cross-check patients’ medications with a list of their medical problems, with the goal of discontinuing any drug that duplicates the action of another or is age-inappropriate, ineffective, or not indicated for the condition for which it was prescribed. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Older adults are taking more medications than ever before. Nearly 9 out of 10 US residents who are 60 years of age or older take at least one prescription drug, more than a third take 5 to 9 medications, and 12% take 10 or more.1
The increase is largely driven by newer medications to effectively treat a variety of medical conditions, and by practice guidelines that often recommend multidrug regimens.2
As a result, the term “polypharmacy,” which once referred to a specific number of medications, is now used more broadly to mean “a large number” of drugs.
From a safety standpoint, the number of medications a patient takes matters. The risk of adverse drug effects and dangerous drug-drug interactions increases significantly when an individual takes ≥5 medications.3
More than 4.5 million adverse drug effects occur each year in the United States, and nearly three quarters of them are initially evaluated in outpatient settings.4 Research suggests that about 80% of the time, these adverse effects are not recognized as such by the patient’s physician. So instead of discontinuing the offending medication, physicians treat the drug-related symptoms by adding yet another medication—a phenomenon known as “the prescribing cascade.”5
This review can help you safeguard older patients taking multiple medications by recognizing and responding to drug-related problems, identifying drugs that can be safely eliminated (or, in some cases, drugs that should be added), and checking regularly to ensure that the medication regimen is appropriate and up to date.
CASE Mrs. R, a 79-year-old woman who recently moved to town, is brought to your office by her daughter and son-in-law. The patient has a hard time reporting her medical history, but her daughter tells you her mother has chronic obstructive pulmonary disease (COPD), heart failure, type 2 diabetes, and mild urinary incontinence, and was recently diagnosed with early dementia.
Mrs. R’s daughter has brought in a bagful of medications, but she’s not sure which ones her mother takes regularly. The medications are an albuterol inhaler, alprazolam, digoxin, diphenhydramine, donepezil, furosemide, glargine insulin, guaifenesin, levothyroxine, metformin, extended-release metoprolol, naproxen, omeprazole, simvastatin, tolterodine, and zolpidem—a total of 16 different drugs.
If Mrs. R were your patient, how would you manage her multidrug regimen?
Start with a medication review
The first step in evaluating a patient’s medication regimen is to find out whether the drugs in the patient’s possession and/or in the medical record are the ones he or she is actually taking. Ask older patients who haven’t brought in their medications, or the caregiver of a confused patient, to bring them to the next visit.
The next step: Determine whether the medication regimen is right for the patient.
Polypharmacy may be indicated
Despite the risks associated with polypharmacy, do not assume that it is inappropriate. For some conditions, multiple medications are routinely recommended. Patients with heart failure, for example, have been shown to have better outcomes when they take 3 to 5 medications, including beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, and diuretics.2
Some treatment guidelines also call for multiple medications. Achieving the more stringent blood pressure goals recommended in the Seventh Report of the Joint National Committee on Prevention, for instance, often requires 2 or more antihypertensive agents.6 In many cases, however, patients end up taking more drugs than necessary.
Is the patient taking the right drugs?
Medication reconciliation (determining whether the treatment regimen is appropriate for the patient’s diagnoses) is the way to find out.
The most widely recommended approach to medication reconciliation is to create a table and do a systematic review.7 List all the patient’s medical conditions in the first column and all current medications in the second column. Use the third column to note whether each medication is one the patient should be on, based not only on his or her medical conditions and other drugs being taken but also on current renal and hepatic function and body size, and contraindications.
A medication may be inappropriate if it duplicates, cancels out the action of, or otherwise interacts with another drug the patient is taking; is contraindicated in older patients; or is ineffective for the condition for which it was prescribed. In one key study of nearly 200 patients 65 years and older who took 5 or more medications, more than half had been prescribed at least one drug that was ineffective for the patient’s condition or that duplicated the action of another medication.8
In addition to finding drugs that the patient should not be taking, medication reconciliation may also reveal that the patient is not receiving optimal therapy and that one or more drugs should be added to his or her treatment regimen.
Check meds after transitions. A move from home to hospital, from emergency department to home, or any other transition relating to patient care should prompt a medication reconciliation. Medications are often added or inadvertently discontinued at such times,9,10 and instructions relating to medication are often misunderstood.11 In one study of 384 frail elderly patients being discharged from a hospital, for example, 44% were found to have been given at least one unnecessary prescription—most commonly for a medication that was neither indicated nor effective for any of the patient’s medical problems.12 It was also common for patients to be given drugs that duplicated the action of others they were already taking.
Even in the absence of such transitions, medication reconciliation should occur at regular intervals. Many physicians do a medication reconciliation at every visit to ensure that the medical record is accurate and the patient’s medication regimen is optimal.
Managing polypharmacy: These resources can help
Numerous tools are available to help you evaluate and monitor patients’ medication regimens, including some that were developed specifically for older patients.
START (Screening Tool to Alert doctors to Right Treatment) identifies drugs and drug classes that are underused with older patients.13 START criteria (TABLE 1)13-17 focus on medications that should be used yet are often omitted in older patients who have the appropriate indications.
TABLE 1
START criteria: Drug therapy that should be given to older patients13-17
Cardiovascular
|
Endocrine
|
Gastrointestinal
|
Musculoskeletal
|
Nervous system
|
Respiratory
|
| ACE, angiotensin-converting enzyme; BP, blood pressure; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease; FEV1, forced expiratory volume in 1 second; GI, gastrointestinal; MI, myocardial infarction; PPI, proton-pump inhibitor; START, Screening Tool to alert doctors to right Treatment. |
In using START or any other drug-related tool, it is important to keep in mind that therapy should be individualized. Not all the medications in the START criteria are appropriate for every patient, and a medication that is indicated for a given medical condition may or may not provide real benefit for a particular patient. That would depend on the individual’s overall health and life expectancy, the goals of treatment, and how long it would take for the patient to realize any benefit from the drug in question.18 A vigorous 79-year-old might benefit from statin therapy for prevention of cardiovascular events, for instance, while a patient like Mrs. R, who is also 79 but has dementia and multiple other medical problems, would be unlikely to live long enough to realize such a benefit.
”Age” assessment tool. One criterion in deciding whether medication(s) are appropriate for an older patient is his or her “physiologic age”—calculated on the basis of the individual’s chronological age and self-reported health status (TABLE 2).19
TABLE 2
Calculating your patient’s “real” age19
| Actual age (y) | Physiologic age (y) | |||||||
|---|---|---|---|---|---|---|---|---|
| Self-reported health | ||||||||
| Excellent | Good | Fair | Poor | |||||
| Male | Female | Male | Female | Male | Female | Male | Female | |
| 65 | 58 | 60 | 64 | 64 | 68 | 66 | 73 | 72 |
| 70 | 62 | 65 | 69 | 69 | 73 | 71 | 78 | 77 |
| 75 | 67 | 70 | 74 | 74 | 78 | 76 | 83 | 82 |
| 80 | 72 | 75 | 79 | 79 | 83 | 81 | 85+ | 85+ |
Flagging drugs that may be inappropriate
Several tools have been developed to aid clinicians in identifying medications that are potentially inappropriate for older adults, although here, too, decisions about their use must be individualized. Two of the most widely used tools are the Beers criteria and STOPP (Screening Tool of Older Persons’ potentially inappropriate Prescriptions).
Beers criteria were developed by Mark Beers et al in 199120 and have been updated at regular intervals, most recently by the American Geriatrics Society in 2012.21 The drugs and drug classes included in the Beers criteria should not be prescribed for older patients in most cases, either because the risk of using them outweighs the benefit or because safer alternatives are available. Key components are listed in TABLE 3.21
TABLE 3
Beers criteria:* Drug classes that may be inappropriate for older adults21
| Drug class | Concern |
|---|---|
| Alpha-blockers with peripheral activity | Orthostatic hypotension |
| Anticholinergics | Cognitive impairment, urinary retention |
| Antipsychotics | Increased death rate when used for behavior control in patients with dementia |
| NSAIDs | Renal dysfunction, GI bleeding, fluid retention, exacerbation of heart failure |
| Sedative hypnotics | Cognitive impairment, delirium |
| Tricyclic antidepressants | Cognitive impairment, delirium, urinary retention |
| GI, gastrointestinal; NSAIDs, nonsteroidal anti-inflammatory drugs. *The full Beers criteria contains 53 drugs and drug classes that are generally inappropriate for older adults. The full list is available from the American Geriatrics Society at: www.americangeriatrics.org/files/documents/beers/2012BeersCriteria_JAGS.pdf. | |
One limitation of the Beers criteria has been its all-or-nothing approach, with many of the medications on the list deemed inappropriate for all older adults regardless of their circumstances. The 2012 update does a better job of individualizing recommendations: Medications are now categorized as those that should be avoided in older patients regardless of their diseases or conditions, those that should be avoided only in patients with certain diseases or conditions, and those that may be used for this patient population but require caution.21
STOPP is similar to the Beers criteria, but uses a different approach: Most medications on this list are considered in the context of specific medical problems.22 While the Beers criteria classify digoxin >0.125 mg/d as generally inappropriate for older adults, for example, STOPP criteria state that long-term dosing at that level is inappropriate only for those with impaired renal function.22 A list of medications identified by STOPP as contributing to hospitalization due to adverse drug effects is available at http://ageing.oxfordjournals.org/content/37/6/673.
Both tools address this drug category. Cumulative anticholinergic burden is a concept applied to the use of anticholinergic medications, which are included in both the Beers and STOPP criteria. Although isolated short-term exposure to a drug with anticholinergic properties may be tolerated by a healthy and cognitively intact older patient, repetitive exposure to such drugs, even if separated in time, has negative effects. One study evaluated more than 500 community-dwelling older adults and found that the more exposure an individual had to anticholinergic medications over the course of a year, the greater the impairment in short-term memory and activities of daily living.23 Another study, this one involving more than 13,000 community-dwelling and institutionalized patients, showed that the longer an older patient takes an anticholinergic medication, the more likely there is to be a measurable decline in performance on the Mini-Mental State Examination.24
Programs that flag potential interactions
Drug-drug interactions are a key concern of polypharmacy, and electronic medical records and prescribing systems that flag potential drug-drug interactions when a new medication is ordered are designed to help physicians avoid them. Unfortunately, clinicians only react to 3% to 9% of such notifications, overriding them because computerized systems often fail to distinguish between important and unimportant interactions.25-27 Thus, clinicians often must decide whether to react to or override warnings, an often difficult decision with patient safety and medicolegal implications. The best advice we can offer is to carefully evaluate drug interaction warnings using common sense, and seek consultation with a clinical pharmacist when uncertainty exists. This approach should prevent prescribing medications that have potentially harmful interactions with drugs the patient is already taking.
For physicians who do not have access to an electronic prescribing system that provides such notification, several online resources are available, some by subscription (eg, Lexicomp, www.lexi.com; Micromedex, www.micromedex.com/index.html; and Pepid, www.pepid.com) and others with free access (eg, AARP, healthtools.aarp.org/drug-interactions; Drugs.com (www.drugs.com/drug_interactions.php; and HealthLine, www.healthline.com/druginteractions).
CASE After doing a medication reconciliation for Mrs. R, you find that she is taking tolterodine, an anticholinergic medication for urge urinary incontinence, and donepezil, a procholinergic medication for dementia. This type of drug-drug interaction, in which the action of one drug effectively cancels out the effect of another, should not be ignored.
Overall, you identify 8 of her medications that could be discontinued: The list includes guaifenesin (a nonessential medication of questionable efficacy); naproxen (inappropriate per Beers criteria; inappropriate in patients with heart failure, according to STOPP); alprazolam, zolpidem, and diphenhydramine (duplicate medications that are all on the Beers criteria as inappropriate for chronic use and ill-advised in patients with cognitive impairment); and omeprazole and levothyroxine (for which nothing in the patient’s history suggests a need), as well as tolterodine. Depending on dose, digoxin is yet another candidate for discontinuation.
Discontinuing medications: Proceed carefully
Physicians are often reluctant to discontinue chronic medications in older patients—even in those with advanced disease who are not likely to benefit from treatment. Focus groups have identified a number of reasons for their hesitation, including:
- the assumption that patients have no problem taking large numbers of drugs
- the fear that patients may misinterpret a plan to discontinue medications as evidence that the physician is giving up on them
- the belief that physicians must comply with practice guidelines that recommend multiple drug treatments
- concern that proposing discontinuation of medications often leads to a discussion of life expectancy and end-of-life care.28
Physicians may also fear that discontinuation of certain drugs will increase the risk of adverse outcomes. More than 30 studies have evaluated discontinuation of chronic medications in older adults, however, and found that drugs as diverse as antihypertensives, antipsychotics, benzodiazepines, and selective serotonin reuptake inhibitors (SSRIs) can often be discontinued without adverse outcomes. In many cases, improvement in patient function results.29 Medications that present the most difficulty are those that patients often become physically or psychologically dependent on, such as benzodiazepines, guaifenesin, proton-pump inhibitors, nonsteroidal anti-inflammatory drugs, and SSRIs. Some (eg, benzodiazepines, SSRIs) require a gradual reduction; for others, no taper is required
(TABLE 4).30-37
TABLE 4
Recommendations for discontinuing hard-to-stop drugs
| Medication or drug class | Discontinuation regimen | Comments |
|---|---|---|
| Benzodiazepines30 | Taper dose by 25% q 2 wk | No withdrawal symptoms reported with this taper regimen. Subtle cognitive improvement noted over a period of months |
| Guaifenesin31 | Can be discontinued without tapering if not combined with opioids or other medications. Elimination half-life is approximately 1 hour | Guaifenesin is often marketed as a combination product with opioids; such combination products require tapering |
| PPIs32-34 | Decrease dose by 50% q 2 wk; supplement with H2 blocker if needed, but tapering of H2 blocker may be required | Abrupt discontinuation after long-term use causes rebound gastric acid hypersecretion and lowers rate of success. Higher success rates with taper regimen and in patients who do not have documented GERD |
| NSAIDs35 | No taper required | Short-term use (<3 mo) acceptable for patients with no contraindications |
| SSRIs36,37 | Gradual reduction in dose over 6-8 wk | Highest rate of success in patients without a clear diagnosis of depression |
| GERD, gastroesophageal reflux disease; NSAIDs, nonsteroidal anti-inflammatory drugs; PPIs, proton-pump inhibitors; SSRIs, selective serotonin reuptake inhibitors. | ||
CASE You trim down Mrs. R’s regimen by discontinuing each of the 8 drugs, one at a time, and carefully monitor the patient during the withdrawal period. Because she had been taking alprazolam daily, the dose is tapered slowly to avoid withdrawal. Omeprazole also requires a gradual taper to avoid rebound hyperacidity.3
After confirming that Mrs. R has heart failure and COPD, you identify 2 medications that should be added to her drug regimen—an ACE inhibitor for heart failure and an inhaled anticholinergic for COPD.
Going from 16 medications to 10 saves money, decreases the likelihood of adverse events and drug-drug interactions, and helps with adherence. Mrs. R’s new drug regimen is expected to lead to improvements in memory and overall quality of life, as well.
CORRESPONDENCE
Barry D. Weiss, MD, Department of Family and Community Medicine, University of Arizona College of Medicine, Tucson, AZ 85724; bdweiss@email.arizona.edu
1. Gu Q, Dillon CF, Burt V. Prescription drug use continued to increase: US prescription drug data for 2007-2008. CDC/NCHS Data Brief. 2010;42:1-2.
2. Jessup K, Abraham WT, Casey DE, et al. 2009 focused update: ACCF/AHA guidelines for the diagnosis and management of heart failure in adults. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;119:1977-2016.
3. Johnell K, Klarin I. The relationship between number of drugs and potential drug-drug interactions in the elderly: a study of over 600,000 elderly patients from the Swedish Prescribed Drug Register. Drug Saf. 2007;30:911-918.
4. Sarkar U, Lopez A, Maselli JH, et al. Adverse drug events in US adult ambulatory medical care. Health Services Res. 2011;46:1517-1533.
5. Rollason V, Vogt N. Reduction of polypharmacy in the elderly. A systematic review of the role of the pharmacist. Drugs Aging. 2003;20:817-832.
6. National Heart, Lung, and Blood Institute. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Available at: www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf. Accessed October 11, 2012.
7. Steinman MA, Hanlon JT. Managing medications in clinically complex elders. JAMA. 2010;304:1592-1601.
8. Steinman MA, Landefeld CS, Rosenthal GE, et al. Polypharmacy and prescribing quality in older people. J Am Geriatr Soc. 2006;54:1516-23.
9. Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuations of medications for chronic disease. JAMA. 2011;306:840-847.
10. Moore C, Wisnivesky J, Williams S, et al. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18:646-651.
11. Ziaeian B, Arauho KL, Van Ness PH, et al. Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge. J Gen Intern Med. 2012 July 12. ePub ahead of print.
12. Hajjar ER, Hanlon JT, Sloane RJ, et al. Unnecessary drug use in frail older people at hospital discharge. J Am Geriatr Soc. 2005;53:1518-1523.
13. O’Mahony D, Gallagher P, Ryan C, et al. STOPP & START criteria: a new approach to detecting potentially inappropriate prescribing in old age. Eur Geriatr Med. 2010;1:45-51.
14. Denneboom W, Dautzenberg KGH, Grol R, et al. Analysis of polypharmacy in older patients in primary acre using a multidisciplinary expert panel. Br J Gen Pract. 2006;56:504-510.
15. Ko DT, Mamdani M, Alter DA. Lipid-lowering therapy with statins in high-risk elderly patients. JAMA. 2004;291:1864-70.
16. Wright RM, Sloane R, Pieper CF, et al. Underuse of indicated medications among physically frail older US veterans at the time of hospital discharge: results of a cross-sectional analysis of data from the Geriatric Evaluation and Management Drug Study. Am J Geriatr Pharmacother. 2009;7:271-280.
17. Garwood CL. Use of anticoagulation in elderly patients with atrial fibrillation who are risk for falls. Ann Pharmacother. 2008;42:523-532.
18. Holmes HM, Hayley DC, Alexander GC, et al. Reconsidering medication appropriateness for patients late in life. Arch Intern Med. 2006;166:605-609.
19. Simplified Methods for Estimating Life Expectancy. Available at: http://painconsortium.nih.gov/symptomresearch/chapter_14/Part_3/sec4/chspt3s4pg1.htm. Accessed October 9, 2012.
20. Beers MH, Ouslander JG, Rollingher I, et al. Explicit criteria for determining inappropriate medication use in nursing home residents. Arch Intern Med. 1991;151:1825-1832.
21. The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society Update Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60:616-631.
22. Gallagher P, O’Mahony D. STOPP (Screening Tool of Older Persons’ potentially inappropriate Prescriptions): application to acutely ill elderly patients and comparison with Beers’ criteria. Age Aging. 2008;37:673-379.
23. Han L, Agostini JV, Allore HG. Cumulative anticholinergic exposure is associated with poor memory and executive function in older men. J Am Geriatr Soc. 2008;56:2203-2210.
24. Fox C, Richardson K, Maidment ID, et al. Anticholinergic medication use and cognitive impairment in the older population: the medical research council cognitive function and ageing study. J Am Geriatr Soc. 2011;59:1477-1483.
25. Knight A, Falade O, Maygers J, et al. Factors associated with medication warning acceptance [abstract]. J Hosp Med. 2012;7(suppl 2):515.-
26. Isaac T, Weissman JS, Davis RB, et al. Overrides of medication alerts in ambulatory care. Arch Intern Med. 2009;169:305-311.
27. Van Der Sijs H, Aarts J, Vulto A, et al. Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc. 2006;12:138-147.
28. Schuling J, Gebben H, Veehof LJG, et al. Deprescribing medication in very elderly patients with multimorbidity: the view of Dutch GPs. A qualitative study. BMC Family Practice. 2012;13:56. http://www.biomedcentral.com/1471-2296/13/56.
29. Iyer S, Naganathan V, McLachlan AJ, et al. Medication withdrawal trials in people aged 65 years and older. A systematic review. Drugs Aging. 2008;25:1021-1031.
30. Curran HV, Collins R, Fletcher S, et al. Older adults and withdrawal from benzodiazepine hypnotics in general practice: effects on cognitive function, sleep, mood and quality of life. Psychol Med. 2003;33:1223-1237.
31. Krinsky DL, Berardi RR, Ferreris SP, et al. Handbook of Nonprescription Drugs: An Interactive Approach to Self-Care. Washington, DC: American Pharmacists Association; 2012:209.
32. Bjornsson E, Abrahamsson H, Simren M, et al. Discontinuation of proton pump inhibitors in patients on long-term therapy: a double-blind, placebo-controlled trial. Aliment Pharmacol Ther. 2006;24:945-954.
33. Inadomi JM, Jamai R, Murata GH, et al. Step-down management of gastroesophageal reflux disease. Gastroenterology. 2001;131:1095-1100.
34. Hester SA. Proton pump inhibitors and rebound acid hypersecretion. Pharm Lett. 2009;25:250920.-
35. Taylor R, Jr, Lemtouni S, Weiss K, et al. Pain management in the elderly: an FDA safe use initiative expert panel’s view on preventable harm associated with NSAID therapy. Curr Gerontol Geriatr Res. 2012;196159.-
36. Ulfvarson J, Adami J, Wredling R, et al. Controlled withdrawal of selective serotonin reuptake inhibitor drugs in elderly patients in nursing homes with no indication of depression. Eur J Clin Pharmacol. 2003;59:735-740.
37. Lindstrom K, Ekedahl A, Carlsten A, et al. Can selective serotonin inhibitor drugs in elderly patients in nursing homes be reduced? Scand J Prim Health Care. 2007;25:3-8.
• Consider the possibility that an adverse drug effect—rather than a new condition—is at play when a patient taking multiple medications develops a new symptom. C
• Use an online interaction checker, which can be accessed via a smart phone or tablet, to check for potential drug-drug interactions in patients on multiple medications. C
• Cross-check patients’ medications with a list of their medical problems, with the goal of discontinuing any drug that duplicates the action of another or is age-inappropriate, ineffective, or not indicated for the condition for which it was prescribed. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Older adults are taking more medications than ever before. Nearly 9 out of 10 US residents who are 60 years of age or older take at least one prescription drug, more than a third take 5 to 9 medications, and 12% take 10 or more.1
The increase is largely driven by newer medications to effectively treat a variety of medical conditions, and by practice guidelines that often recommend multidrug regimens.2
As a result, the term “polypharmacy,” which once referred to a specific number of medications, is now used more broadly to mean “a large number” of drugs.
From a safety standpoint, the number of medications a patient takes matters. The risk of adverse drug effects and dangerous drug-drug interactions increases significantly when an individual takes ≥5 medications.3
More than 4.5 million adverse drug effects occur each year in the United States, and nearly three quarters of them are initially evaluated in outpatient settings.4 Research suggests that about 80% of the time, these adverse effects are not recognized as such by the patient’s physician. So instead of discontinuing the offending medication, physicians treat the drug-related symptoms by adding yet another medication—a phenomenon known as “the prescribing cascade.”5
This review can help you safeguard older patients taking multiple medications by recognizing and responding to drug-related problems, identifying drugs that can be safely eliminated (or, in some cases, drugs that should be added), and checking regularly to ensure that the medication regimen is appropriate and up to date.
CASE Mrs. R, a 79-year-old woman who recently moved to town, is brought to your office by her daughter and son-in-law. The patient has a hard time reporting her medical history, but her daughter tells you her mother has chronic obstructive pulmonary disease (COPD), heart failure, type 2 diabetes, and mild urinary incontinence, and was recently diagnosed with early dementia.
Mrs. R’s daughter has brought in a bagful of medications, but she’s not sure which ones her mother takes regularly. The medications are an albuterol inhaler, alprazolam, digoxin, diphenhydramine, donepezil, furosemide, glargine insulin, guaifenesin, levothyroxine, metformin, extended-release metoprolol, naproxen, omeprazole, simvastatin, tolterodine, and zolpidem—a total of 16 different drugs.
If Mrs. R were your patient, how would you manage her multidrug regimen?
Start with a medication review
The first step in evaluating a patient’s medication regimen is to find out whether the drugs in the patient’s possession and/or in the medical record are the ones he or she is actually taking. Ask older patients who haven’t brought in their medications, or the caregiver of a confused patient, to bring them to the next visit.
The next step: Determine whether the medication regimen is right for the patient.
Polypharmacy may be indicated
Despite the risks associated with polypharmacy, do not assume that it is inappropriate. For some conditions, multiple medications are routinely recommended. Patients with heart failure, for example, have been shown to have better outcomes when they take 3 to 5 medications, including beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, and diuretics.2
Some treatment guidelines also call for multiple medications. Achieving the more stringent blood pressure goals recommended in the Seventh Report of the Joint National Committee on Prevention, for instance, often requires 2 or more antihypertensive agents.6 In many cases, however, patients end up taking more drugs than necessary.
Is the patient taking the right drugs?
Medication reconciliation (determining whether the treatment regimen is appropriate for the patient’s diagnoses) is the way to find out.
The most widely recommended approach to medication reconciliation is to create a table and do a systematic review.7 List all the patient’s medical conditions in the first column and all current medications in the second column. Use the third column to note whether each medication is one the patient should be on, based not only on his or her medical conditions and other drugs being taken but also on current renal and hepatic function and body size, and contraindications.
A medication may be inappropriate if it duplicates, cancels out the action of, or otherwise interacts with another drug the patient is taking; is contraindicated in older patients; or is ineffective for the condition for which it was prescribed. In one key study of nearly 200 patients 65 years and older who took 5 or more medications, more than half had been prescribed at least one drug that was ineffective for the patient’s condition or that duplicated the action of another medication.8
In addition to finding drugs that the patient should not be taking, medication reconciliation may also reveal that the patient is not receiving optimal therapy and that one or more drugs should be added to his or her treatment regimen.
Check meds after transitions. A move from home to hospital, from emergency department to home, or any other transition relating to patient care should prompt a medication reconciliation. Medications are often added or inadvertently discontinued at such times,9,10 and instructions relating to medication are often misunderstood.11 In one study of 384 frail elderly patients being discharged from a hospital, for example, 44% were found to have been given at least one unnecessary prescription—most commonly for a medication that was neither indicated nor effective for any of the patient’s medical problems.12 It was also common for patients to be given drugs that duplicated the action of others they were already taking.
Even in the absence of such transitions, medication reconciliation should occur at regular intervals. Many physicians do a medication reconciliation at every visit to ensure that the medical record is accurate and the patient’s medication regimen is optimal.
Managing polypharmacy: These resources can help
Numerous tools are available to help you evaluate and monitor patients’ medication regimens, including some that were developed specifically for older patients.
START (Screening Tool to Alert doctors to Right Treatment) identifies drugs and drug classes that are underused with older patients.13 START criteria (TABLE 1)13-17 focus on medications that should be used yet are often omitted in older patients who have the appropriate indications.
TABLE 1
START criteria: Drug therapy that should be given to older patients13-17
Cardiovascular
|
Endocrine
|
Gastrointestinal
|
Musculoskeletal
|
Nervous system
|
Respiratory
|
| ACE, angiotensin-converting enzyme; BP, blood pressure; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease; FEV1, forced expiratory volume in 1 second; GI, gastrointestinal; MI, myocardial infarction; PPI, proton-pump inhibitor; START, Screening Tool to alert doctors to right Treatment. |
In using START or any other drug-related tool, it is important to keep in mind that therapy should be individualized. Not all the medications in the START criteria are appropriate for every patient, and a medication that is indicated for a given medical condition may or may not provide real benefit for a particular patient. That would depend on the individual’s overall health and life expectancy, the goals of treatment, and how long it would take for the patient to realize any benefit from the drug in question.18 A vigorous 79-year-old might benefit from statin therapy for prevention of cardiovascular events, for instance, while a patient like Mrs. R, who is also 79 but has dementia and multiple other medical problems, would be unlikely to live long enough to realize such a benefit.
”Age” assessment tool. One criterion in deciding whether medication(s) are appropriate for an older patient is his or her “physiologic age”—calculated on the basis of the individual’s chronological age and self-reported health status (TABLE 2).19
TABLE 2
Calculating your patient’s “real” age19
| Actual age (y) | Physiologic age (y) | |||||||
|---|---|---|---|---|---|---|---|---|
| Self-reported health | ||||||||
| Excellent | Good | Fair | Poor | |||||
| Male | Female | Male | Female | Male | Female | Male | Female | |
| 65 | 58 | 60 | 64 | 64 | 68 | 66 | 73 | 72 |
| 70 | 62 | 65 | 69 | 69 | 73 | 71 | 78 | 77 |
| 75 | 67 | 70 | 74 | 74 | 78 | 76 | 83 | 82 |
| 80 | 72 | 75 | 79 | 79 | 83 | 81 | 85+ | 85+ |
Flagging drugs that may be inappropriate
Several tools have been developed to aid clinicians in identifying medications that are potentially inappropriate for older adults, although here, too, decisions about their use must be individualized. Two of the most widely used tools are the Beers criteria and STOPP (Screening Tool of Older Persons’ potentially inappropriate Prescriptions).
Beers criteria were developed by Mark Beers et al in 199120 and have been updated at regular intervals, most recently by the American Geriatrics Society in 2012.21 The drugs and drug classes included in the Beers criteria should not be prescribed for older patients in most cases, either because the risk of using them outweighs the benefit or because safer alternatives are available. Key components are listed in TABLE 3.21
TABLE 3
Beers criteria:* Drug classes that may be inappropriate for older adults21
| Drug class | Concern |
|---|---|
| Alpha-blockers with peripheral activity | Orthostatic hypotension |
| Anticholinergics | Cognitive impairment, urinary retention |
| Antipsychotics | Increased death rate when used for behavior control in patients with dementia |
| NSAIDs | Renal dysfunction, GI bleeding, fluid retention, exacerbation of heart failure |
| Sedative hypnotics | Cognitive impairment, delirium |
| Tricyclic antidepressants | Cognitive impairment, delirium, urinary retention |
| GI, gastrointestinal; NSAIDs, nonsteroidal anti-inflammatory drugs. *The full Beers criteria contains 53 drugs and drug classes that are generally inappropriate for older adults. The full list is available from the American Geriatrics Society at: www.americangeriatrics.org/files/documents/beers/2012BeersCriteria_JAGS.pdf. | |
One limitation of the Beers criteria has been its all-or-nothing approach, with many of the medications on the list deemed inappropriate for all older adults regardless of their circumstances. The 2012 update does a better job of individualizing recommendations: Medications are now categorized as those that should be avoided in older patients regardless of their diseases or conditions, those that should be avoided only in patients with certain diseases or conditions, and those that may be used for this patient population but require caution.21
STOPP is similar to the Beers criteria, but uses a different approach: Most medications on this list are considered in the context of specific medical problems.22 While the Beers criteria classify digoxin >0.125 mg/d as generally inappropriate for older adults, for example, STOPP criteria state that long-term dosing at that level is inappropriate only for those with impaired renal function.22 A list of medications identified by STOPP as contributing to hospitalization due to adverse drug effects is available at http://ageing.oxfordjournals.org/content/37/6/673.
Both tools address this drug category. Cumulative anticholinergic burden is a concept applied to the use of anticholinergic medications, which are included in both the Beers and STOPP criteria. Although isolated short-term exposure to a drug with anticholinergic properties may be tolerated by a healthy and cognitively intact older patient, repetitive exposure to such drugs, even if separated in time, has negative effects. One study evaluated more than 500 community-dwelling older adults and found that the more exposure an individual had to anticholinergic medications over the course of a year, the greater the impairment in short-term memory and activities of daily living.23 Another study, this one involving more than 13,000 community-dwelling and institutionalized patients, showed that the longer an older patient takes an anticholinergic medication, the more likely there is to be a measurable decline in performance on the Mini-Mental State Examination.24
Programs that flag potential interactions
Drug-drug interactions are a key concern of polypharmacy, and electronic medical records and prescribing systems that flag potential drug-drug interactions when a new medication is ordered are designed to help physicians avoid them. Unfortunately, clinicians only react to 3% to 9% of such notifications, overriding them because computerized systems often fail to distinguish between important and unimportant interactions.25-27 Thus, clinicians often must decide whether to react to or override warnings, an often difficult decision with patient safety and medicolegal implications. The best advice we can offer is to carefully evaluate drug interaction warnings using common sense, and seek consultation with a clinical pharmacist when uncertainty exists. This approach should prevent prescribing medications that have potentially harmful interactions with drugs the patient is already taking.
For physicians who do not have access to an electronic prescribing system that provides such notification, several online resources are available, some by subscription (eg, Lexicomp, www.lexi.com; Micromedex, www.micromedex.com/index.html; and Pepid, www.pepid.com) and others with free access (eg, AARP, healthtools.aarp.org/drug-interactions; Drugs.com (www.drugs.com/drug_interactions.php; and HealthLine, www.healthline.com/druginteractions).
CASE After doing a medication reconciliation for Mrs. R, you find that she is taking tolterodine, an anticholinergic medication for urge urinary incontinence, and donepezil, a procholinergic medication for dementia. This type of drug-drug interaction, in which the action of one drug effectively cancels out the effect of another, should not be ignored.
Overall, you identify 8 of her medications that could be discontinued: The list includes guaifenesin (a nonessential medication of questionable efficacy); naproxen (inappropriate per Beers criteria; inappropriate in patients with heart failure, according to STOPP); alprazolam, zolpidem, and diphenhydramine (duplicate medications that are all on the Beers criteria as inappropriate for chronic use and ill-advised in patients with cognitive impairment); and omeprazole and levothyroxine (for which nothing in the patient’s history suggests a need), as well as tolterodine. Depending on dose, digoxin is yet another candidate for discontinuation.
Discontinuing medications: Proceed carefully
Physicians are often reluctant to discontinue chronic medications in older patients—even in those with advanced disease who are not likely to benefit from treatment. Focus groups have identified a number of reasons for their hesitation, including:
- the assumption that patients have no problem taking large numbers of drugs
- the fear that patients may misinterpret a plan to discontinue medications as evidence that the physician is giving up on them
- the belief that physicians must comply with practice guidelines that recommend multiple drug treatments
- concern that proposing discontinuation of medications often leads to a discussion of life expectancy and end-of-life care.28
Physicians may also fear that discontinuation of certain drugs will increase the risk of adverse outcomes. More than 30 studies have evaluated discontinuation of chronic medications in older adults, however, and found that drugs as diverse as antihypertensives, antipsychotics, benzodiazepines, and selective serotonin reuptake inhibitors (SSRIs) can often be discontinued without adverse outcomes. In many cases, improvement in patient function results.29 Medications that present the most difficulty are those that patients often become physically or psychologically dependent on, such as benzodiazepines, guaifenesin, proton-pump inhibitors, nonsteroidal anti-inflammatory drugs, and SSRIs. Some (eg, benzodiazepines, SSRIs) require a gradual reduction; for others, no taper is required
(TABLE 4).30-37
TABLE 4
Recommendations for discontinuing hard-to-stop drugs
| Medication or drug class | Discontinuation regimen | Comments |
|---|---|---|
| Benzodiazepines30 | Taper dose by 25% q 2 wk | No withdrawal symptoms reported with this taper regimen. Subtle cognitive improvement noted over a period of months |
| Guaifenesin31 | Can be discontinued without tapering if not combined with opioids or other medications. Elimination half-life is approximately 1 hour | Guaifenesin is often marketed as a combination product with opioids; such combination products require tapering |
| PPIs32-34 | Decrease dose by 50% q 2 wk; supplement with H2 blocker if needed, but tapering of H2 blocker may be required | Abrupt discontinuation after long-term use causes rebound gastric acid hypersecretion and lowers rate of success. Higher success rates with taper regimen and in patients who do not have documented GERD |
| NSAIDs35 | No taper required | Short-term use (<3 mo) acceptable for patients with no contraindications |
| SSRIs36,37 | Gradual reduction in dose over 6-8 wk | Highest rate of success in patients without a clear diagnosis of depression |
| GERD, gastroesophageal reflux disease; NSAIDs, nonsteroidal anti-inflammatory drugs; PPIs, proton-pump inhibitors; SSRIs, selective serotonin reuptake inhibitors. | ||
CASE You trim down Mrs. R’s regimen by discontinuing each of the 8 drugs, one at a time, and carefully monitor the patient during the withdrawal period. Because she had been taking alprazolam daily, the dose is tapered slowly to avoid withdrawal. Omeprazole also requires a gradual taper to avoid rebound hyperacidity.3
After confirming that Mrs. R has heart failure and COPD, you identify 2 medications that should be added to her drug regimen—an ACE inhibitor for heart failure and an inhaled anticholinergic for COPD.
Going from 16 medications to 10 saves money, decreases the likelihood of adverse events and drug-drug interactions, and helps with adherence. Mrs. R’s new drug regimen is expected to lead to improvements in memory and overall quality of life, as well.
CORRESPONDENCE
Barry D. Weiss, MD, Department of Family and Community Medicine, University of Arizona College of Medicine, Tucson, AZ 85724; bdweiss@email.arizona.edu
• Consider the possibility that an adverse drug effect—rather than a new condition—is at play when a patient taking multiple medications develops a new symptom. C
• Use an online interaction checker, which can be accessed via a smart phone or tablet, to check for potential drug-drug interactions in patients on multiple medications. C
• Cross-check patients’ medications with a list of their medical problems, with the goal of discontinuing any drug that duplicates the action of another or is age-inappropriate, ineffective, or not indicated for the condition for which it was prescribed. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Older adults are taking more medications than ever before. Nearly 9 out of 10 US residents who are 60 years of age or older take at least one prescription drug, more than a third take 5 to 9 medications, and 12% take 10 or more.1
The increase is largely driven by newer medications to effectively treat a variety of medical conditions, and by practice guidelines that often recommend multidrug regimens.2
As a result, the term “polypharmacy,” which once referred to a specific number of medications, is now used more broadly to mean “a large number” of drugs.
From a safety standpoint, the number of medications a patient takes matters. The risk of adverse drug effects and dangerous drug-drug interactions increases significantly when an individual takes ≥5 medications.3
More than 4.5 million adverse drug effects occur each year in the United States, and nearly three quarters of them are initially evaluated in outpatient settings.4 Research suggests that about 80% of the time, these adverse effects are not recognized as such by the patient’s physician. So instead of discontinuing the offending medication, physicians treat the drug-related symptoms by adding yet another medication—a phenomenon known as “the prescribing cascade.”5
This review can help you safeguard older patients taking multiple medications by recognizing and responding to drug-related problems, identifying drugs that can be safely eliminated (or, in some cases, drugs that should be added), and checking regularly to ensure that the medication regimen is appropriate and up to date.
CASE Mrs. R, a 79-year-old woman who recently moved to town, is brought to your office by her daughter and son-in-law. The patient has a hard time reporting her medical history, but her daughter tells you her mother has chronic obstructive pulmonary disease (COPD), heart failure, type 2 diabetes, and mild urinary incontinence, and was recently diagnosed with early dementia.
Mrs. R’s daughter has brought in a bagful of medications, but she’s not sure which ones her mother takes regularly. The medications are an albuterol inhaler, alprazolam, digoxin, diphenhydramine, donepezil, furosemide, glargine insulin, guaifenesin, levothyroxine, metformin, extended-release metoprolol, naproxen, omeprazole, simvastatin, tolterodine, and zolpidem—a total of 16 different drugs.
If Mrs. R were your patient, how would you manage her multidrug regimen?
Start with a medication review
The first step in evaluating a patient’s medication regimen is to find out whether the drugs in the patient’s possession and/or in the medical record are the ones he or she is actually taking. Ask older patients who haven’t brought in their medications, or the caregiver of a confused patient, to bring them to the next visit.
The next step: Determine whether the medication regimen is right for the patient.
Polypharmacy may be indicated
Despite the risks associated with polypharmacy, do not assume that it is inappropriate. For some conditions, multiple medications are routinely recommended. Patients with heart failure, for example, have been shown to have better outcomes when they take 3 to 5 medications, including beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, and diuretics.2
Some treatment guidelines also call for multiple medications. Achieving the more stringent blood pressure goals recommended in the Seventh Report of the Joint National Committee on Prevention, for instance, often requires 2 or more antihypertensive agents.6 In many cases, however, patients end up taking more drugs than necessary.
Is the patient taking the right drugs?
Medication reconciliation (determining whether the treatment regimen is appropriate for the patient’s diagnoses) is the way to find out.
The most widely recommended approach to medication reconciliation is to create a table and do a systematic review.7 List all the patient’s medical conditions in the first column and all current medications in the second column. Use the third column to note whether each medication is one the patient should be on, based not only on his or her medical conditions and other drugs being taken but also on current renal and hepatic function and body size, and contraindications.
A medication may be inappropriate if it duplicates, cancels out the action of, or otherwise interacts with another drug the patient is taking; is contraindicated in older patients; or is ineffective for the condition for which it was prescribed. In one key study of nearly 200 patients 65 years and older who took 5 or more medications, more than half had been prescribed at least one drug that was ineffective for the patient’s condition or that duplicated the action of another medication.8
In addition to finding drugs that the patient should not be taking, medication reconciliation may also reveal that the patient is not receiving optimal therapy and that one or more drugs should be added to his or her treatment regimen.
Check meds after transitions. A move from home to hospital, from emergency department to home, or any other transition relating to patient care should prompt a medication reconciliation. Medications are often added or inadvertently discontinued at such times,9,10 and instructions relating to medication are often misunderstood.11 In one study of 384 frail elderly patients being discharged from a hospital, for example, 44% were found to have been given at least one unnecessary prescription—most commonly for a medication that was neither indicated nor effective for any of the patient’s medical problems.12 It was also common for patients to be given drugs that duplicated the action of others they were already taking.
Even in the absence of such transitions, medication reconciliation should occur at regular intervals. Many physicians do a medication reconciliation at every visit to ensure that the medical record is accurate and the patient’s medication regimen is optimal.
Managing polypharmacy: These resources can help
Numerous tools are available to help you evaluate and monitor patients’ medication regimens, including some that were developed specifically for older patients.
START (Screening Tool to Alert doctors to Right Treatment) identifies drugs and drug classes that are underused with older patients.13 START criteria (TABLE 1)13-17 focus on medications that should be used yet are often omitted in older patients who have the appropriate indications.
TABLE 1
START criteria: Drug therapy that should be given to older patients13-17
Cardiovascular
|
Endocrine
|
Gastrointestinal
|
Musculoskeletal
|
Nervous system
|
Respiratory
|
| ACE, angiotensin-converting enzyme; BP, blood pressure; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease; FEV1, forced expiratory volume in 1 second; GI, gastrointestinal; MI, myocardial infarction; PPI, proton-pump inhibitor; START, Screening Tool to alert doctors to right Treatment. |
In using START or any other drug-related tool, it is important to keep in mind that therapy should be individualized. Not all the medications in the START criteria are appropriate for every patient, and a medication that is indicated for a given medical condition may or may not provide real benefit for a particular patient. That would depend on the individual’s overall health and life expectancy, the goals of treatment, and how long it would take for the patient to realize any benefit from the drug in question.18 A vigorous 79-year-old might benefit from statin therapy for prevention of cardiovascular events, for instance, while a patient like Mrs. R, who is also 79 but has dementia and multiple other medical problems, would be unlikely to live long enough to realize such a benefit.
”Age” assessment tool. One criterion in deciding whether medication(s) are appropriate for an older patient is his or her “physiologic age”—calculated on the basis of the individual’s chronological age and self-reported health status (TABLE 2).19
TABLE 2
Calculating your patient’s “real” age19
| Actual age (y) | Physiologic age (y) | |||||||
|---|---|---|---|---|---|---|---|---|
| Self-reported health | ||||||||
| Excellent | Good | Fair | Poor | |||||
| Male | Female | Male | Female | Male | Female | Male | Female | |
| 65 | 58 | 60 | 64 | 64 | 68 | 66 | 73 | 72 |
| 70 | 62 | 65 | 69 | 69 | 73 | 71 | 78 | 77 |
| 75 | 67 | 70 | 74 | 74 | 78 | 76 | 83 | 82 |
| 80 | 72 | 75 | 79 | 79 | 83 | 81 | 85+ | 85+ |
Flagging drugs that may be inappropriate
Several tools have been developed to aid clinicians in identifying medications that are potentially inappropriate for older adults, although here, too, decisions about their use must be individualized. Two of the most widely used tools are the Beers criteria and STOPP (Screening Tool of Older Persons’ potentially inappropriate Prescriptions).
Beers criteria were developed by Mark Beers et al in 199120 and have been updated at regular intervals, most recently by the American Geriatrics Society in 2012.21 The drugs and drug classes included in the Beers criteria should not be prescribed for older patients in most cases, either because the risk of using them outweighs the benefit or because safer alternatives are available. Key components are listed in TABLE 3.21
TABLE 3
Beers criteria:* Drug classes that may be inappropriate for older adults21
| Drug class | Concern |
|---|---|
| Alpha-blockers with peripheral activity | Orthostatic hypotension |
| Anticholinergics | Cognitive impairment, urinary retention |
| Antipsychotics | Increased death rate when used for behavior control in patients with dementia |
| NSAIDs | Renal dysfunction, GI bleeding, fluid retention, exacerbation of heart failure |
| Sedative hypnotics | Cognitive impairment, delirium |
| Tricyclic antidepressants | Cognitive impairment, delirium, urinary retention |
| GI, gastrointestinal; NSAIDs, nonsteroidal anti-inflammatory drugs. *The full Beers criteria contains 53 drugs and drug classes that are generally inappropriate for older adults. The full list is available from the American Geriatrics Society at: www.americangeriatrics.org/files/documents/beers/2012BeersCriteria_JAGS.pdf. | |
One limitation of the Beers criteria has been its all-or-nothing approach, with many of the medications on the list deemed inappropriate for all older adults regardless of their circumstances. The 2012 update does a better job of individualizing recommendations: Medications are now categorized as those that should be avoided in older patients regardless of their diseases or conditions, those that should be avoided only in patients with certain diseases or conditions, and those that may be used for this patient population but require caution.21
STOPP is similar to the Beers criteria, but uses a different approach: Most medications on this list are considered in the context of specific medical problems.22 While the Beers criteria classify digoxin >0.125 mg/d as generally inappropriate for older adults, for example, STOPP criteria state that long-term dosing at that level is inappropriate only for those with impaired renal function.22 A list of medications identified by STOPP as contributing to hospitalization due to adverse drug effects is available at http://ageing.oxfordjournals.org/content/37/6/673.
Both tools address this drug category. Cumulative anticholinergic burden is a concept applied to the use of anticholinergic medications, which are included in both the Beers and STOPP criteria. Although isolated short-term exposure to a drug with anticholinergic properties may be tolerated by a healthy and cognitively intact older patient, repetitive exposure to such drugs, even if separated in time, has negative effects. One study evaluated more than 500 community-dwelling older adults and found that the more exposure an individual had to anticholinergic medications over the course of a year, the greater the impairment in short-term memory and activities of daily living.23 Another study, this one involving more than 13,000 community-dwelling and institutionalized patients, showed that the longer an older patient takes an anticholinergic medication, the more likely there is to be a measurable decline in performance on the Mini-Mental State Examination.24
Programs that flag potential interactions
Drug-drug interactions are a key concern of polypharmacy, and electronic medical records and prescribing systems that flag potential drug-drug interactions when a new medication is ordered are designed to help physicians avoid them. Unfortunately, clinicians only react to 3% to 9% of such notifications, overriding them because computerized systems often fail to distinguish between important and unimportant interactions.25-27 Thus, clinicians often must decide whether to react to or override warnings, an often difficult decision with patient safety and medicolegal implications. The best advice we can offer is to carefully evaluate drug interaction warnings using common sense, and seek consultation with a clinical pharmacist when uncertainty exists. This approach should prevent prescribing medications that have potentially harmful interactions with drugs the patient is already taking.
For physicians who do not have access to an electronic prescribing system that provides such notification, several online resources are available, some by subscription (eg, Lexicomp, www.lexi.com; Micromedex, www.micromedex.com/index.html; and Pepid, www.pepid.com) and others with free access (eg, AARP, healthtools.aarp.org/drug-interactions; Drugs.com (www.drugs.com/drug_interactions.php; and HealthLine, www.healthline.com/druginteractions).
CASE After doing a medication reconciliation for Mrs. R, you find that she is taking tolterodine, an anticholinergic medication for urge urinary incontinence, and donepezil, a procholinergic medication for dementia. This type of drug-drug interaction, in which the action of one drug effectively cancels out the effect of another, should not be ignored.
Overall, you identify 8 of her medications that could be discontinued: The list includes guaifenesin (a nonessential medication of questionable efficacy); naproxen (inappropriate per Beers criteria; inappropriate in patients with heart failure, according to STOPP); alprazolam, zolpidem, and diphenhydramine (duplicate medications that are all on the Beers criteria as inappropriate for chronic use and ill-advised in patients with cognitive impairment); and omeprazole and levothyroxine (for which nothing in the patient’s history suggests a need), as well as tolterodine. Depending on dose, digoxin is yet another candidate for discontinuation.
Discontinuing medications: Proceed carefully
Physicians are often reluctant to discontinue chronic medications in older patients—even in those with advanced disease who are not likely to benefit from treatment. Focus groups have identified a number of reasons for their hesitation, including:
- the assumption that patients have no problem taking large numbers of drugs
- the fear that patients may misinterpret a plan to discontinue medications as evidence that the physician is giving up on them
- the belief that physicians must comply with practice guidelines that recommend multiple drug treatments
- concern that proposing discontinuation of medications often leads to a discussion of life expectancy and end-of-life care.28
Physicians may also fear that discontinuation of certain drugs will increase the risk of adverse outcomes. More than 30 studies have evaluated discontinuation of chronic medications in older adults, however, and found that drugs as diverse as antihypertensives, antipsychotics, benzodiazepines, and selective serotonin reuptake inhibitors (SSRIs) can often be discontinued without adverse outcomes. In many cases, improvement in patient function results.29 Medications that present the most difficulty are those that patients often become physically or psychologically dependent on, such as benzodiazepines, guaifenesin, proton-pump inhibitors, nonsteroidal anti-inflammatory drugs, and SSRIs. Some (eg, benzodiazepines, SSRIs) require a gradual reduction; for others, no taper is required
(TABLE 4).30-37
TABLE 4
Recommendations for discontinuing hard-to-stop drugs
| Medication or drug class | Discontinuation regimen | Comments |
|---|---|---|
| Benzodiazepines30 | Taper dose by 25% q 2 wk | No withdrawal symptoms reported with this taper regimen. Subtle cognitive improvement noted over a period of months |
| Guaifenesin31 | Can be discontinued without tapering if not combined with opioids or other medications. Elimination half-life is approximately 1 hour | Guaifenesin is often marketed as a combination product with opioids; such combination products require tapering |
| PPIs32-34 | Decrease dose by 50% q 2 wk; supplement with H2 blocker if needed, but tapering of H2 blocker may be required | Abrupt discontinuation after long-term use causes rebound gastric acid hypersecretion and lowers rate of success. Higher success rates with taper regimen and in patients who do not have documented GERD |
| NSAIDs35 | No taper required | Short-term use (<3 mo) acceptable for patients with no contraindications |
| SSRIs36,37 | Gradual reduction in dose over 6-8 wk | Highest rate of success in patients without a clear diagnosis of depression |
| GERD, gastroesophageal reflux disease; NSAIDs, nonsteroidal anti-inflammatory drugs; PPIs, proton-pump inhibitors; SSRIs, selective serotonin reuptake inhibitors. | ||
CASE You trim down Mrs. R’s regimen by discontinuing each of the 8 drugs, one at a time, and carefully monitor the patient during the withdrawal period. Because she had been taking alprazolam daily, the dose is tapered slowly to avoid withdrawal. Omeprazole also requires a gradual taper to avoid rebound hyperacidity.3
After confirming that Mrs. R has heart failure and COPD, you identify 2 medications that should be added to her drug regimen—an ACE inhibitor for heart failure and an inhaled anticholinergic for COPD.
Going from 16 medications to 10 saves money, decreases the likelihood of adverse events and drug-drug interactions, and helps with adherence. Mrs. R’s new drug regimen is expected to lead to improvements in memory and overall quality of life, as well.
CORRESPONDENCE
Barry D. Weiss, MD, Department of Family and Community Medicine, University of Arizona College of Medicine, Tucson, AZ 85724; bdweiss@email.arizona.edu
1. Gu Q, Dillon CF, Burt V. Prescription drug use continued to increase: US prescription drug data for 2007-2008. CDC/NCHS Data Brief. 2010;42:1-2.
2. Jessup K, Abraham WT, Casey DE, et al. 2009 focused update: ACCF/AHA guidelines for the diagnosis and management of heart failure in adults. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;119:1977-2016.
3. Johnell K, Klarin I. The relationship between number of drugs and potential drug-drug interactions in the elderly: a study of over 600,000 elderly patients from the Swedish Prescribed Drug Register. Drug Saf. 2007;30:911-918.
4. Sarkar U, Lopez A, Maselli JH, et al. Adverse drug events in US adult ambulatory medical care. Health Services Res. 2011;46:1517-1533.
5. Rollason V, Vogt N. Reduction of polypharmacy in the elderly. A systematic review of the role of the pharmacist. Drugs Aging. 2003;20:817-832.
6. National Heart, Lung, and Blood Institute. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Available at: www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf. Accessed October 11, 2012.
7. Steinman MA, Hanlon JT. Managing medications in clinically complex elders. JAMA. 2010;304:1592-1601.
8. Steinman MA, Landefeld CS, Rosenthal GE, et al. Polypharmacy and prescribing quality in older people. J Am Geriatr Soc. 2006;54:1516-23.
9. Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuations of medications for chronic disease. JAMA. 2011;306:840-847.
10. Moore C, Wisnivesky J, Williams S, et al. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18:646-651.
11. Ziaeian B, Arauho KL, Van Ness PH, et al. Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge. J Gen Intern Med. 2012 July 12. ePub ahead of print.
12. Hajjar ER, Hanlon JT, Sloane RJ, et al. Unnecessary drug use in frail older people at hospital discharge. J Am Geriatr Soc. 2005;53:1518-1523.
13. O’Mahony D, Gallagher P, Ryan C, et al. STOPP & START criteria: a new approach to detecting potentially inappropriate prescribing in old age. Eur Geriatr Med. 2010;1:45-51.
14. Denneboom W, Dautzenberg KGH, Grol R, et al. Analysis of polypharmacy in older patients in primary acre using a multidisciplinary expert panel. Br J Gen Pract. 2006;56:504-510.
15. Ko DT, Mamdani M, Alter DA. Lipid-lowering therapy with statins in high-risk elderly patients. JAMA. 2004;291:1864-70.
16. Wright RM, Sloane R, Pieper CF, et al. Underuse of indicated medications among physically frail older US veterans at the time of hospital discharge: results of a cross-sectional analysis of data from the Geriatric Evaluation and Management Drug Study. Am J Geriatr Pharmacother. 2009;7:271-280.
17. Garwood CL. Use of anticoagulation in elderly patients with atrial fibrillation who are risk for falls. Ann Pharmacother. 2008;42:523-532.
18. Holmes HM, Hayley DC, Alexander GC, et al. Reconsidering medication appropriateness for patients late in life. Arch Intern Med. 2006;166:605-609.
19. Simplified Methods for Estimating Life Expectancy. Available at: http://painconsortium.nih.gov/symptomresearch/chapter_14/Part_3/sec4/chspt3s4pg1.htm. Accessed October 9, 2012.
20. Beers MH, Ouslander JG, Rollingher I, et al. Explicit criteria for determining inappropriate medication use in nursing home residents. Arch Intern Med. 1991;151:1825-1832.
21. The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society Update Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60:616-631.
22. Gallagher P, O’Mahony D. STOPP (Screening Tool of Older Persons’ potentially inappropriate Prescriptions): application to acutely ill elderly patients and comparison with Beers’ criteria. Age Aging. 2008;37:673-379.
23. Han L, Agostini JV, Allore HG. Cumulative anticholinergic exposure is associated with poor memory and executive function in older men. J Am Geriatr Soc. 2008;56:2203-2210.
24. Fox C, Richardson K, Maidment ID, et al. Anticholinergic medication use and cognitive impairment in the older population: the medical research council cognitive function and ageing study. J Am Geriatr Soc. 2011;59:1477-1483.
25. Knight A, Falade O, Maygers J, et al. Factors associated with medication warning acceptance [abstract]. J Hosp Med. 2012;7(suppl 2):515.-
26. Isaac T, Weissman JS, Davis RB, et al. Overrides of medication alerts in ambulatory care. Arch Intern Med. 2009;169:305-311.
27. Van Der Sijs H, Aarts J, Vulto A, et al. Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc. 2006;12:138-147.
28. Schuling J, Gebben H, Veehof LJG, et al. Deprescribing medication in very elderly patients with multimorbidity: the view of Dutch GPs. A qualitative study. BMC Family Practice. 2012;13:56. http://www.biomedcentral.com/1471-2296/13/56.
29. Iyer S, Naganathan V, McLachlan AJ, et al. Medication withdrawal trials in people aged 65 years and older. A systematic review. Drugs Aging. 2008;25:1021-1031.
30. Curran HV, Collins R, Fletcher S, et al. Older adults and withdrawal from benzodiazepine hypnotics in general practice: effects on cognitive function, sleep, mood and quality of life. Psychol Med. 2003;33:1223-1237.
31. Krinsky DL, Berardi RR, Ferreris SP, et al. Handbook of Nonprescription Drugs: An Interactive Approach to Self-Care. Washington, DC: American Pharmacists Association; 2012:209.
32. Bjornsson E, Abrahamsson H, Simren M, et al. Discontinuation of proton pump inhibitors in patients on long-term therapy: a double-blind, placebo-controlled trial. Aliment Pharmacol Ther. 2006;24:945-954.
33. Inadomi JM, Jamai R, Murata GH, et al. Step-down management of gastroesophageal reflux disease. Gastroenterology. 2001;131:1095-1100.
34. Hester SA. Proton pump inhibitors and rebound acid hypersecretion. Pharm Lett. 2009;25:250920.-
35. Taylor R, Jr, Lemtouni S, Weiss K, et al. Pain management in the elderly: an FDA safe use initiative expert panel’s view on preventable harm associated with NSAID therapy. Curr Gerontol Geriatr Res. 2012;196159.-
36. Ulfvarson J, Adami J, Wredling R, et al. Controlled withdrawal of selective serotonin reuptake inhibitor drugs in elderly patients in nursing homes with no indication of depression. Eur J Clin Pharmacol. 2003;59:735-740.
37. Lindstrom K, Ekedahl A, Carlsten A, et al. Can selective serotonin inhibitor drugs in elderly patients in nursing homes be reduced? Scand J Prim Health Care. 2007;25:3-8.
1. Gu Q, Dillon CF, Burt V. Prescription drug use continued to increase: US prescription drug data for 2007-2008. CDC/NCHS Data Brief. 2010;42:1-2.
2. Jessup K, Abraham WT, Casey DE, et al. 2009 focused update: ACCF/AHA guidelines for the diagnosis and management of heart failure in adults. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;119:1977-2016.
3. Johnell K, Klarin I. The relationship between number of drugs and potential drug-drug interactions in the elderly: a study of over 600,000 elderly patients from the Swedish Prescribed Drug Register. Drug Saf. 2007;30:911-918.
4. Sarkar U, Lopez A, Maselli JH, et al. Adverse drug events in US adult ambulatory medical care. Health Services Res. 2011;46:1517-1533.
5. Rollason V, Vogt N. Reduction of polypharmacy in the elderly. A systematic review of the role of the pharmacist. Drugs Aging. 2003;20:817-832.
6. National Heart, Lung, and Blood Institute. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Available at: www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf. Accessed October 11, 2012.
7. Steinman MA, Hanlon JT. Managing medications in clinically complex elders. JAMA. 2010;304:1592-1601.
8. Steinman MA, Landefeld CS, Rosenthal GE, et al. Polypharmacy and prescribing quality in older people. J Am Geriatr Soc. 2006;54:1516-23.
9. Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuations of medications for chronic disease. JAMA. 2011;306:840-847.
10. Moore C, Wisnivesky J, Williams S, et al. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18:646-651.
11. Ziaeian B, Arauho KL, Van Ness PH, et al. Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge. J Gen Intern Med. 2012 July 12. ePub ahead of print.
12. Hajjar ER, Hanlon JT, Sloane RJ, et al. Unnecessary drug use in frail older people at hospital discharge. J Am Geriatr Soc. 2005;53:1518-1523.
13. O’Mahony D, Gallagher P, Ryan C, et al. STOPP & START criteria: a new approach to detecting potentially inappropriate prescribing in old age. Eur Geriatr Med. 2010;1:45-51.
14. Denneboom W, Dautzenberg KGH, Grol R, et al. Analysis of polypharmacy in older patients in primary acre using a multidisciplinary expert panel. Br J Gen Pract. 2006;56:504-510.
15. Ko DT, Mamdani M, Alter DA. Lipid-lowering therapy with statins in high-risk elderly patients. JAMA. 2004;291:1864-70.
16. Wright RM, Sloane R, Pieper CF, et al. Underuse of indicated medications among physically frail older US veterans at the time of hospital discharge: results of a cross-sectional analysis of data from the Geriatric Evaluation and Management Drug Study. Am J Geriatr Pharmacother. 2009;7:271-280.
17. Garwood CL. Use of anticoagulation in elderly patients with atrial fibrillation who are risk for falls. Ann Pharmacother. 2008;42:523-532.
18. Holmes HM, Hayley DC, Alexander GC, et al. Reconsidering medication appropriateness for patients late in life. Arch Intern Med. 2006;166:605-609.
19. Simplified Methods for Estimating Life Expectancy. Available at: http://painconsortium.nih.gov/symptomresearch/chapter_14/Part_3/sec4/chspt3s4pg1.htm. Accessed October 9, 2012.
20. Beers MH, Ouslander JG, Rollingher I, et al. Explicit criteria for determining inappropriate medication use in nursing home residents. Arch Intern Med. 1991;151:1825-1832.
21. The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society Update Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60:616-631.
22. Gallagher P, O’Mahony D. STOPP (Screening Tool of Older Persons’ potentially inappropriate Prescriptions): application to acutely ill elderly patients and comparison with Beers’ criteria. Age Aging. 2008;37:673-379.
23. Han L, Agostini JV, Allore HG. Cumulative anticholinergic exposure is associated with poor memory and executive function in older men. J Am Geriatr Soc. 2008;56:2203-2210.
24. Fox C, Richardson K, Maidment ID, et al. Anticholinergic medication use and cognitive impairment in the older population: the medical research council cognitive function and ageing study. J Am Geriatr Soc. 2011;59:1477-1483.
25. Knight A, Falade O, Maygers J, et al. Factors associated with medication warning acceptance [abstract]. J Hosp Med. 2012;7(suppl 2):515.-
26. Isaac T, Weissman JS, Davis RB, et al. Overrides of medication alerts in ambulatory care. Arch Intern Med. 2009;169:305-311.
27. Van Der Sijs H, Aarts J, Vulto A, et al. Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc. 2006;12:138-147.
28. Schuling J, Gebben H, Veehof LJG, et al. Deprescribing medication in very elderly patients with multimorbidity: the view of Dutch GPs. A qualitative study. BMC Family Practice. 2012;13:56. http://www.biomedcentral.com/1471-2296/13/56.
29. Iyer S, Naganathan V, McLachlan AJ, et al. Medication withdrawal trials in people aged 65 years and older. A systematic review. Drugs Aging. 2008;25:1021-1031.
30. Curran HV, Collins R, Fletcher S, et al. Older adults and withdrawal from benzodiazepine hypnotics in general practice: effects on cognitive function, sleep, mood and quality of life. Psychol Med. 2003;33:1223-1237.
31. Krinsky DL, Berardi RR, Ferreris SP, et al. Handbook of Nonprescription Drugs: An Interactive Approach to Self-Care. Washington, DC: American Pharmacists Association; 2012:209.
32. Bjornsson E, Abrahamsson H, Simren M, et al. Discontinuation of proton pump inhibitors in patients on long-term therapy: a double-blind, placebo-controlled trial. Aliment Pharmacol Ther. 2006;24:945-954.
33. Inadomi JM, Jamai R, Murata GH, et al. Step-down management of gastroesophageal reflux disease. Gastroenterology. 2001;131:1095-1100.
34. Hester SA. Proton pump inhibitors and rebound acid hypersecretion. Pharm Lett. 2009;25:250920.-
35. Taylor R, Jr, Lemtouni S, Weiss K, et al. Pain management in the elderly: an FDA safe use initiative expert panel’s view on preventable harm associated with NSAID therapy. Curr Gerontol Geriatr Res. 2012;196159.-
36. Ulfvarson J, Adami J, Wredling R, et al. Controlled withdrawal of selective serotonin reuptake inhibitor drugs in elderly patients in nursing homes with no indication of depression. Eur J Clin Pharmacol. 2003;59:735-740.
37. Lindstrom K, Ekedahl A, Carlsten A, et al. Can selective serotonin inhibitor drugs in elderly patients in nursing homes be reduced? Scand J Prim Health Care. 2007;25:3-8.