User login
What's the best way to monitor low-risk patients with a history of differentiated thyroid cancer?
A recombinant human thyrotropin (rhTSH)-stimulated serum thyroglobulin (Tg) level alone is sufficient to monitor for recurrent disease in low-risk patients with a history of differentiated thyroid cancer (DTC) (strength of recommendation [SOR] A, meta-analysis). Low-risk patients are defined as patients who have undergone total thyroidectomy and radioactive iodine (I131) remnant ablation therapy and show no clinical evidence of recurrent disease.
Evidence summary
An estimated 37,340 new cases of thyroid cancer are diagnosed annually in the United States, typically in people between 20 and 55 years of age. The most common type of thyroid cancer is DTC, which includes papillary and follicular carcinoma. Papillary carcinoma accounts for 80% of all thyroid cancers, and follicular carcinoma accounts for 10%.
The 5-year survival rate for all cases of DTC is 97%. Although the disease has a favorable prognosis, an estimated 1630 patients were expected to die of it in 2009 because of its prevalence.1
The goal: Find recurrent disease early
The purpose of surveillance protocols in thyroid cancer is early detection of recurrent disease. Expert debate about DTC surveillance centers on the disease’s low incidence and prolonged clinical course, as well as a lack of prospective randomized clinical trials. Current guidelines were developed from large retrospective cohort studies of patients observed over several decades.
rhTSH-stimulated Tg is the new surveillance standard
All major professional organizations support the consensus that an rhTSH-stimulated serum Tg is adequate to follow-up low-risk patients. This test replaces the previous accepted standard of thyroid hormone withdrawal (THW)-stimulated measurements. Moreover, rhTSH-stimulated serum Tg is comparable to a THW-stimulated measurement for detecting recurrent disease, when a cutoff value of 2 mcg/L is used.2
rhTSH testing has similar sensitivity to THW
A 2004 meta-analysis examined 46 studies with a total of 9094 patients. THW-stimulated Tg measurements after thyroid remnant ablation had a sensitivity of 96% (95% confidence interval [CI], 93.5%-98.7%) and a specificity of 94% (95% CI, 93.3%-96.1%). For rhTSH-stimulated serum Tg measurements, sensitivity and specificity were 92% (95% CI, 88.9%-96.1%) and 88% (95% CI, 85.4%-90.6%), respectively.
Because the difference in sensitivity between THW-stimulated and rhTSH-stimulated serum Tg isn’t statistically significant, rhTSH can be used for Tg testing without significantly decreasing detection of DTC recurrence. The slightly lower specificity of rhTSH may lead to unnecessary additional testing because of a few more false-positive results. However, this risk should be weighed against the benefits of reducing morbidity by avoiding the need to withhold thyroid hormone replacement therapy before testing.3
Thyroglobulin measurements: How they compare to body scanning
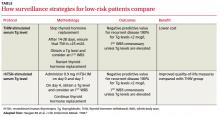
A 1999 prospective cohort study of 229 patients with DTC compared the accuracy of I131 whole body scanning with serum Tg measurement after both rhTSH and THW stimulation (TABLE). The results of the whole body scan were concordant with the rhTSH-stimulated and THW-stimulated Tg measurements in 89% of the patients (P=.108).
Using a cutoff value of ≥2 mcg/L for recurrent disease, an elevated Tg level was detected in 52% of patients with localized thyroid bed disease after rhTSH stimulation and in 56% of patients after THW stimulation. An elevated Tg level after rhTSH stimulation was found in 100% of patients with metastatic disease. Symptoms of hypothyroidism, including overall quality-of-life scores, were significantly better in the rhTSH group than the THW group (P<.01).4
rhTSH-stimulated Tg: Accuracy with a lower cost
A retrospective cohort study of 107 patients determined that rhTSH-stimulated serum Tg levels alone are sensitive enough to identify recurrent disease in low-risk patients. Levels greater than 2 mcg/L had a sensitivity and negative predictive value of 100% and a false-positive rate of 9%—a statistically and clinically significant improvement in accuracy over a whole body scan obtained after rhTSH stimulation, which had a sensitivity of only 27%, negative predictive value of 92%, and false-positive rate of 9% (P<.05). In low-risk patients, rhTSH-stimulated serum Tg measurement is the most accurate and least costly method of surveillance because of its high negative predictive value.5
Whole body scanning doesn’t enhance surveillance accuracy
This conclusion is supported by a cohort study that prospectively followed 99 patients with a history of DTC who underwent serum Tg measurement and an I131 whole body scan obtained after rhTSH stimulation and were followed by neck ultrasound 6 to 12 months after ablation treatment. The whole body scan was negative in 95% of the patients, with a sensitivity of 0%. Serum Tg was positive in 19 of these patients. Neck ultrasound confirmed positive lymph nodes in 7 patients, of whom 5 were Tg-positive. The I131 whole body scan added no benefit to the accuracy of surveillance.6
Recommendations
The British Thyroid Association and the American Thyroid Association recommend performing a physical examination with serum TSH, Tg, and antithyroglobulin antibodies at 6 and 12 months postablation, then annually if the patient is disease free.7,8
In low-risk patients, stimulated serum Tg measurement alone is an acceptable initial follow-up; a value of ≥2 mcg/L indicates a need for further evaluation. If serum Tg is undetectable under TSH stimulation, subsequent long-term follow-up by serum Tg levels alone while under TSH suppression is sufficient. TSH stimulation can be achieved by THW or rhTSH.7-9
A whole body scan rarely adds valuable additional information. Periodic neck ultrasound should be performed, however.7-9
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
A recombinant human thyrotropin (rhTSH)-stimulated serum thyroglobulin (Tg) level alone is sufficient to monitor for recurrent disease in low-risk patients with a history of differentiated thyroid cancer (DTC) (strength of recommendation [SOR] A, meta-analysis). Low-risk patients are defined as patients who have undergone total thyroidectomy and radioactive iodine (I131) remnant ablation therapy and show no clinical evidence of recurrent disease.
Evidence summary
An estimated 37,340 new cases of thyroid cancer are diagnosed annually in the United States, typically in people between 20 and 55 years of age. The most common type of thyroid cancer is DTC, which includes papillary and follicular carcinoma. Papillary carcinoma accounts for 80% of all thyroid cancers, and follicular carcinoma accounts for 10%.
The 5-year survival rate for all cases of DTC is 97%. Although the disease has a favorable prognosis, an estimated 1630 patients were expected to die of it in 2009 because of its prevalence.1
The goal: Find recurrent disease early
The purpose of surveillance protocols in thyroid cancer is early detection of recurrent disease. Expert debate about DTC surveillance centers on the disease’s low incidence and prolonged clinical course, as well as a lack of prospective randomized clinical trials. Current guidelines were developed from large retrospective cohort studies of patients observed over several decades.
rhTSH-stimulated Tg is the new surveillance standard
All major professional organizations support the consensus that an rhTSH-stimulated serum Tg is adequate to follow-up low-risk patients. This test replaces the previous accepted standard of thyroid hormone withdrawal (THW)-stimulated measurements. Moreover, rhTSH-stimulated serum Tg is comparable to a THW-stimulated measurement for detecting recurrent disease, when a cutoff value of 2 mcg/L is used.2
rhTSH testing has similar sensitivity to THW
A 2004 meta-analysis examined 46 studies with a total of 9094 patients. THW-stimulated Tg measurements after thyroid remnant ablation had a sensitivity of 96% (95% confidence interval [CI], 93.5%-98.7%) and a specificity of 94% (95% CI, 93.3%-96.1%). For rhTSH-stimulated serum Tg measurements, sensitivity and specificity were 92% (95% CI, 88.9%-96.1%) and 88% (95% CI, 85.4%-90.6%), respectively.
Because the difference in sensitivity between THW-stimulated and rhTSH-stimulated serum Tg isn’t statistically significant, rhTSH can be used for Tg testing without significantly decreasing detection of DTC recurrence. The slightly lower specificity of rhTSH may lead to unnecessary additional testing because of a few more false-positive results. However, this risk should be weighed against the benefits of reducing morbidity by avoiding the need to withhold thyroid hormone replacement therapy before testing.3
Thyroglobulin measurements: How they compare to body scanning
A 1999 prospective cohort study of 229 patients with DTC compared the accuracy of I131 whole body scanning with serum Tg measurement after both rhTSH and THW stimulation (TABLE). The results of the whole body scan were concordant with the rhTSH-stimulated and THW-stimulated Tg measurements in 89% of the patients (P=.108).
Using a cutoff value of ≥2 mcg/L for recurrent disease, an elevated Tg level was detected in 52% of patients with localized thyroid bed disease after rhTSH stimulation and in 56% of patients after THW stimulation. An elevated Tg level after rhTSH stimulation was found in 100% of patients with metastatic disease. Symptoms of hypothyroidism, including overall quality-of-life scores, were significantly better in the rhTSH group than the THW group (P<.01).4
rhTSH-stimulated Tg: Accuracy with a lower cost
A retrospective cohort study of 107 patients determined that rhTSH-stimulated serum Tg levels alone are sensitive enough to identify recurrent disease in low-risk patients. Levels greater than 2 mcg/L had a sensitivity and negative predictive value of 100% and a false-positive rate of 9%—a statistically and clinically significant improvement in accuracy over a whole body scan obtained after rhTSH stimulation, which had a sensitivity of only 27%, negative predictive value of 92%, and false-positive rate of 9% (P<.05). In low-risk patients, rhTSH-stimulated serum Tg measurement is the most accurate and least costly method of surveillance because of its high negative predictive value.5
Whole body scanning doesn’t enhance surveillance accuracy
This conclusion is supported by a cohort study that prospectively followed 99 patients with a history of DTC who underwent serum Tg measurement and an I131 whole body scan obtained after rhTSH stimulation and were followed by neck ultrasound 6 to 12 months after ablation treatment. The whole body scan was negative in 95% of the patients, with a sensitivity of 0%. Serum Tg was positive in 19 of these patients. Neck ultrasound confirmed positive lymph nodes in 7 patients, of whom 5 were Tg-positive. The I131 whole body scan added no benefit to the accuracy of surveillance.6
Recommendations
The British Thyroid Association and the American Thyroid Association recommend performing a physical examination with serum TSH, Tg, and antithyroglobulin antibodies at 6 and 12 months postablation, then annually if the patient is disease free.7,8
In low-risk patients, stimulated serum Tg measurement alone is an acceptable initial follow-up; a value of ≥2 mcg/L indicates a need for further evaluation. If serum Tg is undetectable under TSH stimulation, subsequent long-term follow-up by serum Tg levels alone while under TSH suppression is sufficient. TSH stimulation can be achieved by THW or rhTSH.7-9
A whole body scan rarely adds valuable additional information. Periodic neck ultrasound should be performed, however.7-9
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
A recombinant human thyrotropin (rhTSH)-stimulated serum thyroglobulin (Tg) level alone is sufficient to monitor for recurrent disease in low-risk patients with a history of differentiated thyroid cancer (DTC) (strength of recommendation [SOR] A, meta-analysis). Low-risk patients are defined as patients who have undergone total thyroidectomy and radioactive iodine (I131) remnant ablation therapy and show no clinical evidence of recurrent disease.
Evidence summary
An estimated 37,340 new cases of thyroid cancer are diagnosed annually in the United States, typically in people between 20 and 55 years of age. The most common type of thyroid cancer is DTC, which includes papillary and follicular carcinoma. Papillary carcinoma accounts for 80% of all thyroid cancers, and follicular carcinoma accounts for 10%.
The 5-year survival rate for all cases of DTC is 97%. Although the disease has a favorable prognosis, an estimated 1630 patients were expected to die of it in 2009 because of its prevalence.1
The goal: Find recurrent disease early
The purpose of surveillance protocols in thyroid cancer is early detection of recurrent disease. Expert debate about DTC surveillance centers on the disease’s low incidence and prolonged clinical course, as well as a lack of prospective randomized clinical trials. Current guidelines were developed from large retrospective cohort studies of patients observed over several decades.
rhTSH-stimulated Tg is the new surveillance standard
All major professional organizations support the consensus that an rhTSH-stimulated serum Tg is adequate to follow-up low-risk patients. This test replaces the previous accepted standard of thyroid hormone withdrawal (THW)-stimulated measurements. Moreover, rhTSH-stimulated serum Tg is comparable to a THW-stimulated measurement for detecting recurrent disease, when a cutoff value of 2 mcg/L is used.2
rhTSH testing has similar sensitivity to THW
A 2004 meta-analysis examined 46 studies with a total of 9094 patients. THW-stimulated Tg measurements after thyroid remnant ablation had a sensitivity of 96% (95% confidence interval [CI], 93.5%-98.7%) and a specificity of 94% (95% CI, 93.3%-96.1%). For rhTSH-stimulated serum Tg measurements, sensitivity and specificity were 92% (95% CI, 88.9%-96.1%) and 88% (95% CI, 85.4%-90.6%), respectively.
Because the difference in sensitivity between THW-stimulated and rhTSH-stimulated serum Tg isn’t statistically significant, rhTSH can be used for Tg testing without significantly decreasing detection of DTC recurrence. The slightly lower specificity of rhTSH may lead to unnecessary additional testing because of a few more false-positive results. However, this risk should be weighed against the benefits of reducing morbidity by avoiding the need to withhold thyroid hormone replacement therapy before testing.3
Thyroglobulin measurements: How they compare to body scanning
A 1999 prospective cohort study of 229 patients with DTC compared the accuracy of I131 whole body scanning with serum Tg measurement after both rhTSH and THW stimulation (TABLE). The results of the whole body scan were concordant with the rhTSH-stimulated and THW-stimulated Tg measurements in 89% of the patients (P=.108).
Using a cutoff value of ≥2 mcg/L for recurrent disease, an elevated Tg level was detected in 52% of patients with localized thyroid bed disease after rhTSH stimulation and in 56% of patients after THW stimulation. An elevated Tg level after rhTSH stimulation was found in 100% of patients with metastatic disease. Symptoms of hypothyroidism, including overall quality-of-life scores, were significantly better in the rhTSH group than the THW group (P<.01).4
rhTSH-stimulated Tg: Accuracy with a lower cost
A retrospective cohort study of 107 patients determined that rhTSH-stimulated serum Tg levels alone are sensitive enough to identify recurrent disease in low-risk patients. Levels greater than 2 mcg/L had a sensitivity and negative predictive value of 100% and a false-positive rate of 9%—a statistically and clinically significant improvement in accuracy over a whole body scan obtained after rhTSH stimulation, which had a sensitivity of only 27%, negative predictive value of 92%, and false-positive rate of 9% (P<.05). In low-risk patients, rhTSH-stimulated serum Tg measurement is the most accurate and least costly method of surveillance because of its high negative predictive value.5
Whole body scanning doesn’t enhance surveillance accuracy
This conclusion is supported by a cohort study that prospectively followed 99 patients with a history of DTC who underwent serum Tg measurement and an I131 whole body scan obtained after rhTSH stimulation and were followed by neck ultrasound 6 to 12 months after ablation treatment. The whole body scan was negative in 95% of the patients, with a sensitivity of 0%. Serum Tg was positive in 19 of these patients. Neck ultrasound confirmed positive lymph nodes in 7 patients, of whom 5 were Tg-positive. The I131 whole body scan added no benefit to the accuracy of surveillance.6
Recommendations
The British Thyroid Association and the American Thyroid Association recommend performing a physical examination with serum TSH, Tg, and antithyroglobulin antibodies at 6 and 12 months postablation, then annually if the patient is disease free.7,8
In low-risk patients, stimulated serum Tg measurement alone is an acceptable initial follow-up; a value of ≥2 mcg/L indicates a need for further evaluation. If serum Tg is undetectable under TSH stimulation, subsequent long-term follow-up by serum Tg levels alone while under TSH suppression is sufficient. TSH stimulation can be achieved by THW or rhTSH.7-9
A whole body scan rarely adds valuable additional information. Periodic neck ultrasound should be performed, however.7-9
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
Evidence-based answers from the Family Physicians Inquiries Network